
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Previous issues
- Page Path
- HOME > Browse > Previous issues
Reviews
- Drug/Regimen
- New, Novel Lipid-Lowering Agents for Reducing Cardiovascular Risk: Beyond Statins
- Kyuho Kim, Henry N. Ginsberg, Sung Hee Choi
- Diabetes Metab J. 2022;46(4):517-532. Published online July 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0198
- Correction in: Diabetes Metab J 2022;46(5):817
- 9,937 View
- 864 Download
- 25 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
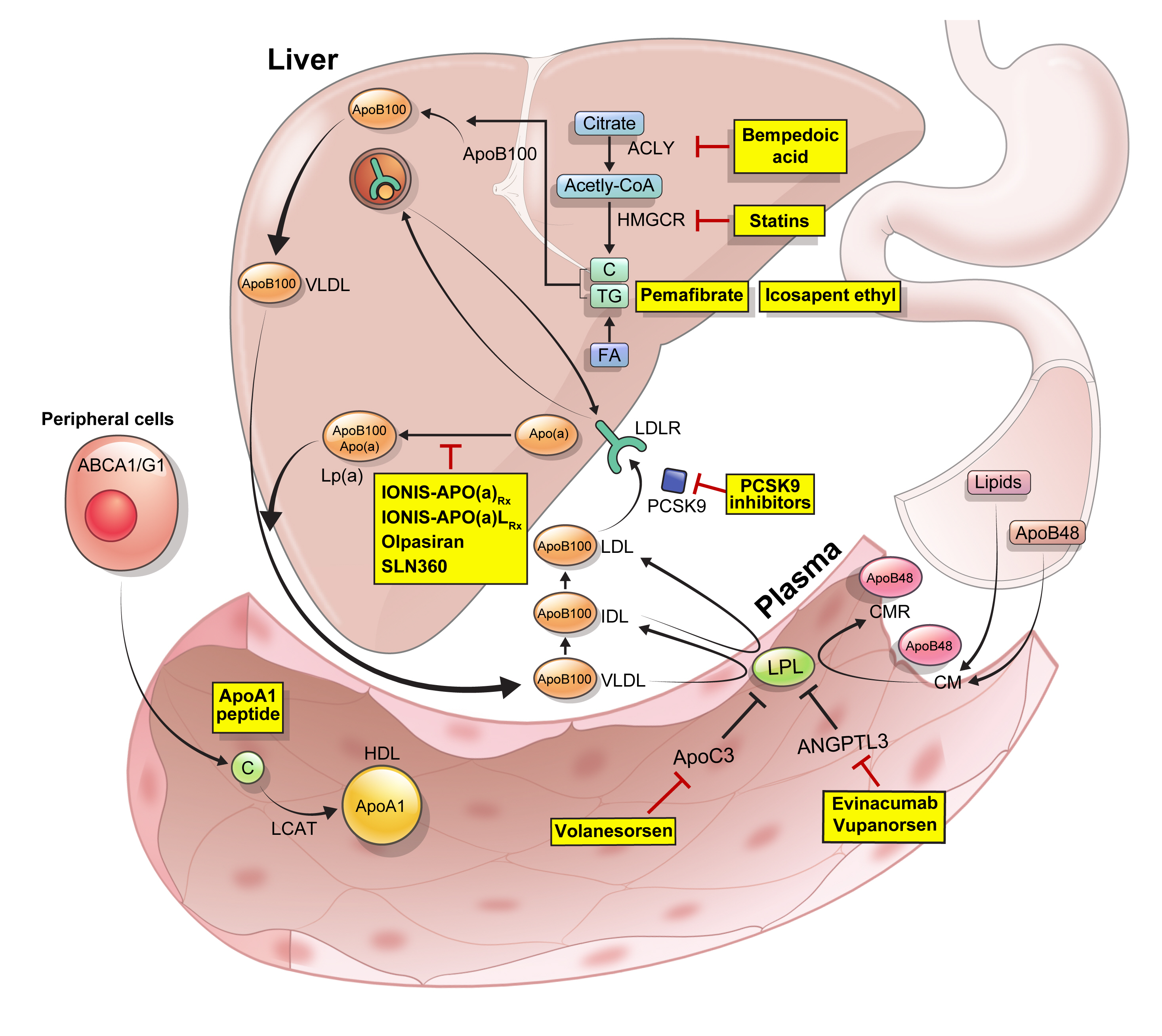
ePub - Statins are the cornerstone of the prevention and treatment of atherosclerotic cardiovascular disease (ASCVD). However, even under optimal statin therapy, a significant residual ASCVD risk remains. Therefore, there has been an unmet clinical need for novel lipid-lowering agents that can target low-density lipoprotein cholesterol (LDL-C) and other atherogenic particles. During the past decade, several drugs have been developed for the treatment of dyslipidemia. Inclisiran, a small interfering RNA that targets proprotein convertase subtilisin/kexin type 9 (PCSK9), shows comparable effects to that of PCSK9 monoclonal antibodies. Bempedoic acid, an ATP citrate lyase inhibitor, is a valuable treatment option for the patients with statin intolerance. Pemafibrate, the first selective peroxisome proliferator-activated receptor alpha modulator, showed a favorable benefit-risk balance in phase 2 trial, but the large clinical phase 3 trial (PROMINENT) was recently stopped for futility based on a late interim analysis. High dose icosapent ethyl, a modified eicosapentaenoic acid preparation, shows cardiovascular benefits. Evinacumab, an angiopoietin-like 3 (ANGPTL3) monoclonal antibody, reduces plasma LDL-C levels in patients with refractory hypercholesterolemia. Novel antisense oligonucleotides targeting apolipoprotein C3 (apoC3), ANGPTL3, and lipoprotein(a) have significantly attenuated the levels of their target molecules with beneficial effects on associated dyslipidemias. Apolipoprotein A1 (apoA1) is considered as a potential treatment to exploit the athero-protective effects of high-density lipoprotein cholesterol (HDL-C), but solid clinical evidence is necessary. In this review, we discuss the mode of action and clinical outcomes of these novel lipid-lowering agents beyond statins.
-
Citations
Citations to this article as recorded by- The role of adherence in patients with chronic diseases
Michel Burnier
European Journal of Internal Medicine.2024; 119: 1. CrossRef - Bempedoic acid: new evidence and recommendations on use
Kristina Paponja, Ivan Pećin, Željko Reiner, Maciej Banach
Current Opinion in Lipidology.2024; 35(1): 41. CrossRef - Genetic insights into repurposing statins for hyperthyroidism prevention: a drug-target Mendelian randomization study
Anqi Huang, Xinyi Wu, Jiaqi Lin, Chiju Wei, Wencan Xu
Frontiers in Endocrinology.2024;[Epub] CrossRef - Targeting host-specific metabolic pathways—opportunities and challenges for anti-infective therapy
Monika I. Konaklieva, Balbina J. Plotkin
Frontiers in Molecular Biosciences.2024;[Epub] CrossRef - Neutrophil Extracellular Traps (NETs) and Atherosclerosis: Does Hypolipidemic Treatment Have an Effect?
Petros Adamidis, Despoina Pantazi, Iraklis Moschonas, Evangelos Liberopoulos, Alexandros Tselepis
Journal of Cardiovascular Development and Disease.2024; 11(3): 72. CrossRef - Modulating effects of crocin on lipids and lipoproteins: Mechanisms and potential benefits
Habib Yaribeygi, Mina Maleki, Farin Rashid-Farrokhi, Payman Raise Abdullahi, Mohammad Amin Hemmati, Tannaz Jamialahmadi, Amirhossein Sahebkar
Heliyon.2024; 10(7): e28837. CrossRef - Assessing the Benefits of Lifestyle Influences on Cardiovascu-lar Health After Acute Coronary Syndrome
Marius Rus, Claudia Elena Stanis, Paula Marian, Lilliana Oana Pobirci, Loredana Ioana Banszki, Veronica Huplea, Gheorghe Adrian Osiceanu, Bianca-Maria Pop, Gabriela Dogaru, Felicia Liana Andronie-Cioara
Balneo and PRM Research Journal.2024; 15(Vol.15, no): 660. CrossRef - Liver cancer cells as the model for developing liver-targeted RNAi therapeutics
Beibei Hou, Linhui Qin, Linfeng Huang
Biochemical and Biophysical Research Communications.2023; 644: 85. CrossRef - Insights into Causal Cardiovascular Risk Factors from Mendelian Randomization
C. M. Schooling, J. V. Zhao
Current Cardiology Reports.2023; 25(2): 67. CrossRef - Secoisolariciresinol diglucoside and anethole ameliorate lipid abnormalities, oxidative injury, hypercholesterolemia, heart, and liver conditions
Sana Noreen, Habib‐ur Rehman, Tabussam Tufail, Huma Badar Ul Ain, Chinaza Godswill Awuchi
Food Science & Nutrition.2023; 11(6): 2620. CrossRef - Colesterol remanente, riesgo vascular y prevención de la arteriosclerosis
Xavier Pintó, Marta Fanlo, Virginia Esteve, Jesús Millán, Agustín Blanco, Mariano Blasco, José Luís Díaz Díaz, Ángel Díaz Rodríguez, Alipio Mangas, Vicente Pascual, Juan Pedro Botet, Pablo Pérez Martínez
Clínica e Investigación en Arteriosclerosis.2023; 35(4): 206. CrossRef - Evolving Management of Low‐Density Lipoprotein Cholesterol: A Personalized Approach to Preventing Atherosclerotic Cardiovascular Disease Across the Risk Continuum
Michael J. Wilkinson, Norman E. Lepor, Erin D. Michos
Journal of the American Heart Association.2023;[Epub] CrossRef - The cell origins of foam cell and lipid metabolism regulated by mechanical stress in atherosclerosis
Zhi Ouyang, Jian Zhong, Junyi Shen, Ye Zeng
Frontiers in Physiology.2023;[Epub] CrossRef - Triglyceride-Rich Lipoprotein Metabolism: Key Regulators of Their Flux
Alejandro Gugliucci
Journal of Clinical Medicine.2023; 12(13): 4399. CrossRef - Remnant cholesterol, vascular risk, and prevention of atherosclerosis
Xavier Pintó, Marta Fanlo, Virginia Esteve, Jesús Millán
Clínica e Investigación en Arteriosclerosis (English Edition).2023; 35(4): 206. CrossRef - Antibiotics and Lipid-Modifying Agents: Potential Drug–Drug Interactions and Their Clinical Implications
Marios Spanakis, Danny Alon-Ellenbogen, Petros Ioannou, Nikolaos Spernovasilis
Pharmacy.2023; 11(4): 130. CrossRef - Advances in Treatment of Dyslipidemia
Jill Dybiec, Wiktoria Baran, Bartłomiej Dąbek, Piotr Fularski, Ewelina Młynarska, Ewa Radzioch, Jacek Rysz, Beata Franczyk
International Journal of Molecular Sciences.2023; 24(17): 13288. CrossRef - Peroxisome Proliferator-Activated Receptor α in Lipoprotein Metabolism and Atherosclerotic Cardiovascular Disease
Elena Valeria Fuior, Evangelia Zvintzou, Theodosios Filippatos, Katerina Giannatou, Victoria Mparnia, Maya Simionescu, Anca Violeta Gafencu, Kyriakos E. Kypreos
Biomedicines.2023; 11(10): 2696. CrossRef - Preparation, characterization and in vivo pharmacokinetic study of ginsenoside Rb1-PLGA nanoparticles
Lixin Du, Huiling Lu, Yifei Xiao, Zhihua Guo, Ya Li
Scientific Reports.2023;[Epub] CrossRef - Dysregulation of Cholesterol Homeostasis in Ovarian Cancer
Zahraa Qusairy, Anne Gangloff, Shuk On Annie Leung
Current Oncology.2023; 30(9): 8386. CrossRef - Riesgo residual. Conclusiones
Ángel Cequier, José Luis Zamorano
Revista Española de Cardiología Suplementos.2023; 23: 25. CrossRef - Causal effects of circulating lipids and lipid-lowering drugs on the risk of urinary stones: a Mendelian randomization study
Zilong Tan, Jing Hong, Aochuan Sun, Mengdi Ding, Jianwu Shen
Frontiers in Endocrinology.2023;[Epub] CrossRef - Bibliometric analysis of residual cardiovascular risk: trends and frontiers
Lin Wang, Sutong Wang, Chaoyuan Song, Yiding Yu, Yuehua Jiang, Yongcheng Wang, Xiao Li
Journal of Health, Population and Nutrition.2023;[Epub] CrossRef - Current Understanding on the Genetic Basis of Key Metabolic Disorders: A Review
Kenneth Francis Rodrigues, Wilson Thau Lym Yong, Md. Safiul Alam Bhuiyan, Shafiquzzaman Siddiquee, Muhammad Dawood Shah, Balu Alagar Venmathi Maran
Biology.2022; 11(9): 1308. CrossRef - Lipoprotein Lipase: Is It a Magic Target for the Treatment of Hypertriglyceridemia
Joon Ho Moon, Kyuho Kim, Sung Hee Choi
Endocrinology and Metabolism.2022; 37(4): 575. CrossRef
- The role of adherence in patients with chronic diseases
- Pathophysiology
- Endoplasmic Reticulum Stress and Dysregulated Autophagy in Human Pancreatic Beta Cells
- Seoil Moon, Hye Seung Jung
- Diabetes Metab J. 2022;46(4):533-542. Published online July 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0070
- 4,530 View
- 250 Download
- 8 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
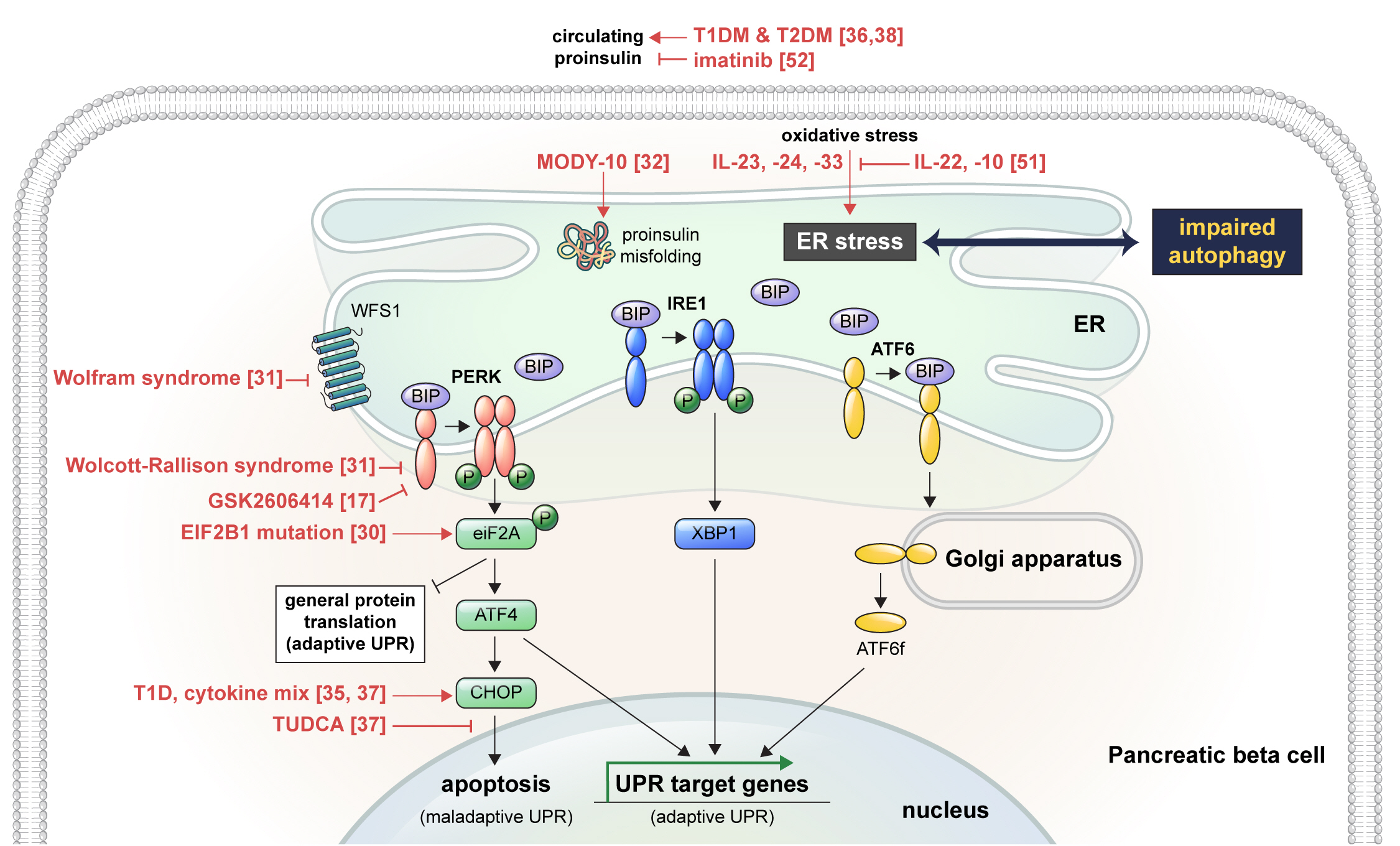
ePub - Pancreatic beta cell homeostasis is crucial for the synthesis and secretion of insulin; disruption of homeostasis causes diabetes, and is a treatment target. Adaptation to endoplasmic reticulum (ER) stress through the unfolded protein response (UPR) and adequate regulation of autophagy, which are closely linked, play essential roles in this homeostasis. In diabetes, the UPR and autophagy are dysregulated, which leads to beta cell failure and death. Various studies have explored methods to preserve pancreatic beta cell function and mass by relieving ER stress and regulating autophagic activity. To promote clinical translation of these research results to potential therapeutics for diabetes, we summarize the current knowledge on ER stress and autophagy in human insulin-secreting cells.
-
Citations
Citations to this article as recorded by- Glucolipotoxicity Suppressed Autophagy and Insulin Contents in Human Islets, and Attenuation of PERK Activity Enhanced Them in an ATG7-Dependent Manner
Seoil Moon, Ji Yoon Lim, Mirang Lee, Youngmin Han, Hongbeom Kim, Wooil Kwon, Jin-Young Jang, Mi Na Kim, Kyong Soo Park, Hye Seung Jung
Diabetes & Metabolism Journal.2024; 48(2): 231. CrossRef - Endoplasmic reticulum stress: A possible connection between intestinal inflammation and neurodegenerative disorders
Giorgio Vivacqua, Romina Mancinelli, Stefano Leone, Rosa Vaccaro, Ludovica Garro, Simone Carotti, Ludovica Ceci, Paolo Onori, Luigi Pannarale, Antonio Franchitto, Eugenio Gaudio, Arianna Casini
Neurogastroenterology & Motility.2024;[Epub] CrossRef - Docosahexanoic Acid Attenuates Palmitate-Induced Apoptosis by Autophagy Upregulation via GPR120/mTOR Axis in Insulin-Secreting Cells
Seok-Woo Hong, Jinmi Lee, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2024; 39(2): 353. CrossRef - Pancreatic islet remodeling in cotadutide-treated obese mice
Renata Spezani, Thatiany Souza Marinho, Luiz E. Macedo Cardoso, Marcia Barbosa Aguila, Carlos Alberto Mandarim-de-Lacerda
Life Sciences.2023; 327: 121858. CrossRef - Modulation of Unfolded Protein Response Restores Survival and Function of β-Cells Exposed to the Endocrine Disruptor Bisphenol A
Laura Maria Daian, Gabriela Tanko, Andrei Mircea Vacaru, Luiza Ghila, Simona Chera, Ana-Maria Vacaru
International Journal of Molecular Sciences.2023; 24(3): 2023. CrossRef - Interplay of skeletal muscle and adipose tissue: sarcopenic obesity
Min Jeong Park, Kyung Mook Choi
Metabolism.2023; 144: 155577. CrossRef - Identification and analysis of type 2 diabetes-mellitus-associated autophagy-related genes
Kun Cui, Zhizheng Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Sestrin2 in diabetes and diabetic complications
Xiaodan Zhang, Zirui Luo, Jiahong Li, Yaxuan Lin, Yu Li, Wangen Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Crosstalk between autophagy and insulin resistance: evidence from different tissues
Asie Sadeghi, Maryam Niknam, Mohammad Amin Momeni-Moghaddam, Maryam Shabani, Hamid Aria, Alireza Bastin, Maryam Teimouri, Reza Meshkani, Hamed Akbari
European Journal of Medical Research.2023;[Epub] CrossRef - Beta cell lipotoxicity in the development of type 2 diabetes: the need for species-specific understanding
Patricia Thomas, Meurig T. Gallagher, Gabriela Da Silva Xavier
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Glucolipotoxicity Suppressed Autophagy and Insulin Contents in Human Islets, and Attenuation of PERK Activity Enhanced Them in an ATG7-Dependent Manner
- Pathophysiology
- Renoprotective Mechanism of Sodium-Glucose Cotransporter 2 Inhibitors: Focusing on Renal Hemodynamics
- Nam Hoon Kim, Nan Hee Kim
- Diabetes Metab J. 2022;46(4):543-551. Published online July 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0209
- 6,376 View
- 674 Download
- 11 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
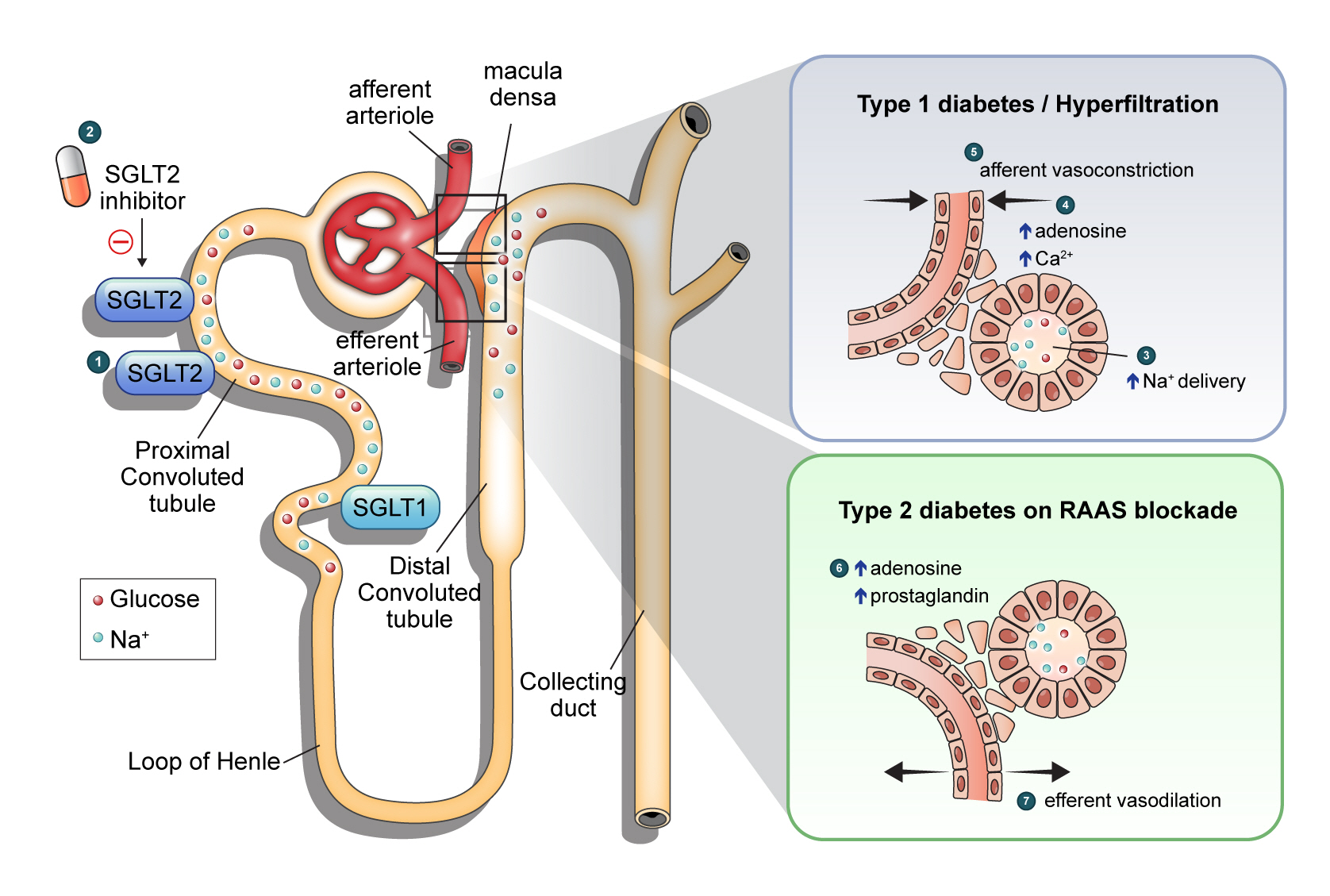
ePub - Diabetic kidney disease (DKD) is a prevalent renal complication of diabetes mellitus that ultimately develops into end-stage kidney disease (ESKD) when not managed appropriately. Substantial risk of ESKD remains even with intensive management of hyperglycemia and risk factors of DKD and timely use of renin-angiotensin-aldosterone inhibitors. Sodium-glucose cotransporter 2 (SGLT2) inhibitors reduce hyperglycemia primarily by inhibiting glucose and sodium reabsorption in the renal proximal tubule. Currently, their effects expand to prevent or delay cardiovascular and renal adverse events, even in those without diabetes. In dedicated renal outcome trials, SGLT2 inhibitors significantly reduced the risk of composite renal adverse events, including the development of ESKD or renal replacement therapy, which led to the positioning of SGLT2 inhibitors as the mainstay of chronic kidney disease management. Multiple mechanisms of action of SGLT2 inhibitors, including hemodynamic, metabolic, and anti-inflammatory effects, have been proposed. Restoration of tubuloglomerular feedback is a plausible explanation for the alteration in renal hemodynamics induced by SGLT2 inhibition and for the associated renal benefit. This review discusses the clinical rationale and mechanism related to the protection SGLT2 inhibitors exert on the kidney, focusing on renal hemodynamic effects.
-
Citations
Citations to this article as recorded by- Using intravoxel incoherent motion imaging to evaluate uric acid-induced renal injury and efficacy after treatment
Zhong-Yuan Cheng, Shang-Ao Gong, Ping-Kang Chen, Zong-Chao Yu, Chen Qiu, Ji-Xin Lin, Jia-Bin Mo, Long Qian, You-Zhen Feng, Xiang-Ran Cai
British Journal of Radiology.2024; 97(1153): 274. CrossRef - Rethinking eGFR Comparisons in SGLT2 Inhibitor Research
Yuzuru Ohshiro
Journal of the American College of Cardiology.2024; 83(9): e87. CrossRef - SGLT2 Inhibitors and Diabetes: Where Does It Come from and Where Does It Go?
Ji Yoon Kim, Sin Gon Kim
The Journal of Korean Diabetes.2024; 25(1): 9. CrossRef - Cardiorenal outcomes and mortality after sodium‐glucose cotransporter‐2 inhibitor initiation in type 2 diabetes patients with percutaneous coronary intervention history
Jin Hwa Kim, Young Sang Lyu, BongSeong Kim, Mee Kyung Kim, Sang Yong Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Baseline eGFR, albuminuria and renal outcomes in patients with SGLT2 inhibitor treatment: an updated meta-analysis
Yunke Ma, Chu Lin, Xiaoling Cai, Suiyuan Hu, Xingyun Zhu, Fang Lv, Wenjia Yang, Linong Ji
Acta Diabetologica.2023; 60(3): 435. CrossRef - Effects of sodium-glucose cotransporter 2 inhibitors on renal risk factors in patients with abnormal glucose metabolism: a meta-analysis of randomized controlled trials
Mengnan Li, Jian Zhang, Guimei Yang, Jiaxin Zhang, Minmin Han, Yi Zhang, Yunfeng Liu
European Journal of Clinical Pharmacology.2023; 79(6): 859. CrossRef - Age at Mortality in Patients with Type 2 Diabetes Who Underwent Kidney Transplantation: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Sun Ok Song, Eugene Han, Kang Ju Son, Bong-Soo Cha, Byung-Wan Lee
Journal of Clinical Medicine.2023; 12(9): 3160. CrossRef - Exposure–Response Analysis of the Sodium–Glucose Cotransporter-2 Inhibitors Dapagliflozin and Empagliflozin on Kidney Hemodynamics in Patients with Type 2 Diabetes
Sjoukje van der Hoek, Jeroen V. Koomen, Erik J. M. van Bommel, Charlotte M. Mosterd, Rosalie A. Scholtes, Anne C. Hesp, Jasper Stevens, Daniel H. van Raalte, Hiddo J. L. Heerspink
Journal of Personalized Medicine.2023; 13(5): 747. CrossRef - Osteopontin as a Biomarker in Chronic Kidney Disease
Satyesh K. Sinha, Michael Mellody, Maria Beatriz Carpio, Robert Damoiseaux, Susanne B. Nicholas
Biomedicines.2023; 11(5): 1356. CrossRef - Increased expression of sodium-glucose cotransporter 2 and O-GlcNAcylation in hepatocytes drives non-alcoholic steatohepatitis
Hye Jin Chun, Eun Ran Kim, Minyoung Lee, Da Hyun Choi, Soo Hyun Kim, Eugene Shin, Jin-Hong Kim, Jin Won Cho, Dai Hoon Han, Bong-Soo Cha, Yong-ho Lee
Metabolism.2023; 145: 155612. CrossRef - Synthesis and biological profile of benzoxazolone derivatives
Parteek Prasher, Tanisqa Mall, Mousmee Sharma
Archiv der Pharmazie.2023;[Epub] CrossRef - SGLT2 inhibitors prevent LPS-induced M1 macrophage polarization and alleviate inflammatory bowel disease by downregulating NHE1 expression
Ye Jin Kim, Jonghwa Jin, Dong-Ho Kim, Daehoon Kim, You Mie Lee, Jun-Kyu Byun, Yeon-Kyung Choi, Keun-Gyu Park
Inflammation Research.2023; 72(10-11): 1981. CrossRef
- Using intravoxel incoherent motion imaging to evaluate uric acid-induced renal injury and efficacy after treatment
- Others
- Current Trends of Big Data Research Using the Korean National Health Information Database
- Mee Kyoung Kim, Kyungdo Han, Seung-Hwan Lee
- Diabetes Metab J. 2022;46(4):552-563. Published online July 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0193

- 5,721 View
- 277 Download
- 32 Web of Science
- 33 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Recently, medical research using big data has become very popular, and its value has become increasingly recognized. The Korean National Health Information Database (NHID) is representative of big data that combines information obtained from the National Health Insurance Service collected for claims and reimbursement of health care services and results obtained from general health examinations provided to all Korean adults. This database has several strengths and limitations. Given the large size, various laboratory data, and questionnaires obtained from medical check-ups, their longitudinal nature, and long-term accumulation of data since 2002, carefully designed studies may provide valuable information that is difficult to obtain from other forms of research. However, consideration of possible bias and careful interpretation when defining causal relationships is also important because the data were not collected for research purposes. After the NHID became publicly available, research and publications based on this database have increased explosively, especially in the field of diabetes and metabolism. This article reviews the history, structure, and characteristics of the Korean NHID. Recent trends in big data research using this database, commonly used operational diagnosis, and representative studies have been introduced. We expect further progress and expansion of big data research using the Korean NHID.
-
Citations
Citations to this article as recorded by- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Jinyoung Kim, Bongseong Kim, Mee Kyoung Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(2): 567. CrossRef - Repeated detection of non‐alcoholic fatty liver disease increases the incidence risk of type 2 diabetes in young adults
Jin Hwa Kim, Young Sang Lyu, Mee Kyoung Kim, Sang Yong Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(1): 180. CrossRef - Diabetes severity and the risk of depression: A nationwide population-based study
Yunjung Cho, Bongsung Kim, Hyuk-Sang Kwon, Kyungdo Han, Mee Kyoung Kim
Journal of Affective Disorders.2024; 351: 694. CrossRef - Diabetes Duration, Cholesterol Levels, and Risk of Cardiovascular Diseases in Individuals With Type 2 Diabetes
Mee Kyoung Kim, Kyu Na Lee, Kyungdo Han, Seung-Hwan Lee
The Journal of Clinical Endocrinology & Metabolism.2024;[Epub] CrossRef - Remnant cholesterol is an independent risk factor for the incidence of chronic kidney disease in newly-diagnosed type 2 diabetes: A nationwide population-based study
Soo Yeon Jang, Minwoong Kang, Eyun Song, Ahreum Jang, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Diabetes Research and Clinical Practice.2024; 210: 111639. CrossRef - Association of the Intensive Blood Pressure Target and Cardiovascular Outcomes in the Population With Chronic Kidney Disease: A Retrospective Study in Korea
Soo‐Young Yoon, Ji Yoon Kong, Su Jin Jeong, Jin Sug Kim, Hyeon Seok Hwang, Kyunghwan Jeong
Journal of the American Heart Association.2024;[Epub] CrossRef - Risk of Depression according to Cumulative Exposure to a Low-Household Income Status in Individuals with Type 2 Diabetes Mellitus: A Nationwide Population- Based Study
So Hee Park, You-Bin Lee, Kyu-na Lee, Bongsung Kim, So Hyun Cho, So Yoon Kwon, Jiyun Park, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Kyungdo Han, Jae Hyeon Kim
Diabetes & Metabolism Journal.2024; 48(2): 290. CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - A nationwide cohort study on diabetes severity and risk of Parkinson disease
Kyungdo Han, Bongsung Kim, Seung Hwan Lee, Mee Kyoung Kim
npj Parkinson's Disease.2023;[Epub] CrossRef - Predicting the Risk of Insulin-Requiring Gestational Diabetes before Pregnancy: A Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Jin Yu, Kyungdo Han, Seung Woo Lee, Sang Youn You, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2023; 38(1): 129. CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
Jong Ha Baek, Yong-Moon Park, Kyung Do Han, Min Kyong Moon, Jong Han Choi, Seung-Hyun Ko
Diabetes & Metabolism Journal.2023; 47(2): 201. CrossRef - Comorbidity Differences by Trajectory Groups as a Reference for Identifying Patients at Risk for Late Mortality in Childhood Cancer Survivors: Longitudinal National Cohort Study
Hyery Kim, Hae Reong Kim, Sung Han Kang, Kyung-Nam Koh, Ho Joon Im, Yu Rang Park
JMIR Public Health and Surveillance.2023; 9: e41203. CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Investigation of the Relationship Between Psychiatry Visit and Suicide After Deliberate Self-harm: Longitudinal National Cohort Study
Hye Hyeon Kim, Chanyoung Ko, Ji Ae Park, In Han Song, Yu Rang Park
JMIR Public Health and Surveillance.2023; 9: e41261. CrossRef - Reply
Yeonghee Eun, Hyungjin Kim, Jaejoon Lee
Arthritis & Rheumatology.2023; 75(6): 1081. CrossRef - Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(3): 347. CrossRef - Comparison of Cefepime with Piperacillin/Tazobactam Treatment in Patients with Hospital-Acquired Pneumonia
Bo-Guen Kim, Danbee Kang, Kyung Hoon Min, Juhee Cho, Kyeongman Jeon
Antibiotics.2023; 12(6): 984. CrossRef - Cumulative exposure to metabolic syndrome increases thyroid cancer risk in young adults: a population-based cohort study
Jinyoung Kim, Kyungdo Han, Mee Kyoung Kim, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
The Korean Journal of Internal Medicine.2023; 38(4): 526. CrossRef - Risk of developing chronic kidney disease in young-onset Type 2 diabetes in Korea
Joonyub Lee, Seung-Hwan Lee, Kun-Ho Yoon, Jae Hyoung Cho, Kyungdo Han, Yeoree Yang
Scientific Reports.2023;[Epub] CrossRef - Factors Affecting High Body Weight Variability
Kyungdo Han, Mee Kyoung Kim
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 163. CrossRef - Physical activity and reduced risk of fracture in thyroid cancer patients after thyroidectomy — a nationwide cohort study
Jinyoung Kim, Kyungdo Han, Jin-Hyung Jung, Jeonghoon Ha, Chaiho Jeong, Jun-Young Heu, Se-Won Lee, Jeongmin Lee, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Ki-Hyun Baek
Frontiers in Endocrinology.2023;[Epub] CrossRef - The impact of diabetes status on total and site-specific cancer risk in the elderly population: A nationwide cohort study
Kyuho Kim, Bongseong Kim, Hyunho Kim, Hyung Soon Park, Yu-Bae Ahn, Seung-Hyun Ko, Kyungdo Han, Jae-Seung Yun
Diabetes Research and Clinical Practice.2023; 203: 110866. CrossRef - Response to comments of Lai et al. “Proposal of one option for patient-centered, heterogeneous selection of antidiabetic drug”
Sunyoung Kim, Sang Youl Rhee
Diabetes Research and Clinical Practice.2023; 203: 110864. CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Increased risk of ischemic stroke associated with elevated gamma-glutamyl transferase level in adult cancer survivors: a population-based cohort study
Kyuwoong Kim, Hyeyun Jung, Edvige Di Giovanna, Tae Joon Jun, Young-Hak Kim
Scientific Reports.2023;[Epub] CrossRef - Real-world data analysis on effectiveness of integrative therapies: A practical guide to study design and data analysis using healthcare databases
Ye-Seul Lee, Yoon Jae Lee, In-Hyuk Ha
Integrative Medicine Research.2023; 12(4): 101000. CrossRef - Possible Applications of the Korean Experience in the Development of Croatian Healthcare System
Predrag Bejakovic, Romina P Družeta, Ohmin Kwon
Science, Art and Religion.2023; 2(1--2): 26. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - Alcohol consumption and the risk of liver disease: a nationwide, population-based study
Sang Yi Moon, Minkook Son, Yeo Wool Kang, Myeongseok Koh, Jong Yoon Lee, Yang Hyun Baek
Frontiers in Medicine.2023;[Epub] CrossRef - Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
Han-Sang Baek, Bongseong Kim, Seung-Hwan Lee, Dong-Jun Lim, Hyuk-Sang Kwon, Sang-Ah Chang, Kyungdo Han, Jae-Seung Yun
Endocrinology and Metabolism.2023; 38(6): 770. CrossRef - Sodium-glucose cotransporter 2 inhibitors for non-alcoholic fatty liver disease in patients with type 2 diabetes mellitus: A nationwide propensity-score matched cohort study
Jinyoung Kim, Kyungdo Han, Bongsung Kim, Ki-Hyun Baek, Ki-Ho Song, Mee Kyoung Kim, Hyuk-Sang Kwon
Diabetes Research and Clinical Practice.2022; 194: 110187. CrossRef - Chronic viral hepatitis accelerates lung function decline in smokers
Suh-Young Lee, Sun-Sin Kim, So-Hee Lee, Heung-Woo Park
Clinical and Experimental Medicine.2022; 23(6): 2159. CrossRef
- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Editorial
- Beyond Liver Disease: Non-Alcoholic Fatty Liver Disease and Advanced Liver Fibrosis in Kidney Disease
- Eugene Han
- Diabetes Metab J. 2022;46(4):564-566. Published online July 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0203
- 2,350 View
- 130 Download
Original Articles
- Cardiovascular Risk/Epidemiology
- Comparative Effects of Sodium-Glucose Cotransporter 2 Inhibitor and Thiazolidinedione Treatment on Risk of Stroke among Patients with Type 2 Diabetes Mellitus
- Seung Eun Lee, Hyewon Nam, Han Seok Choi, Hoseob Kim, Dae-Sung Kyoung, Kyoung-Ah Kim
- Diabetes Metab J. 2022;46(4):567-577. Published online February 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0160
- 5,420 View
- 358 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
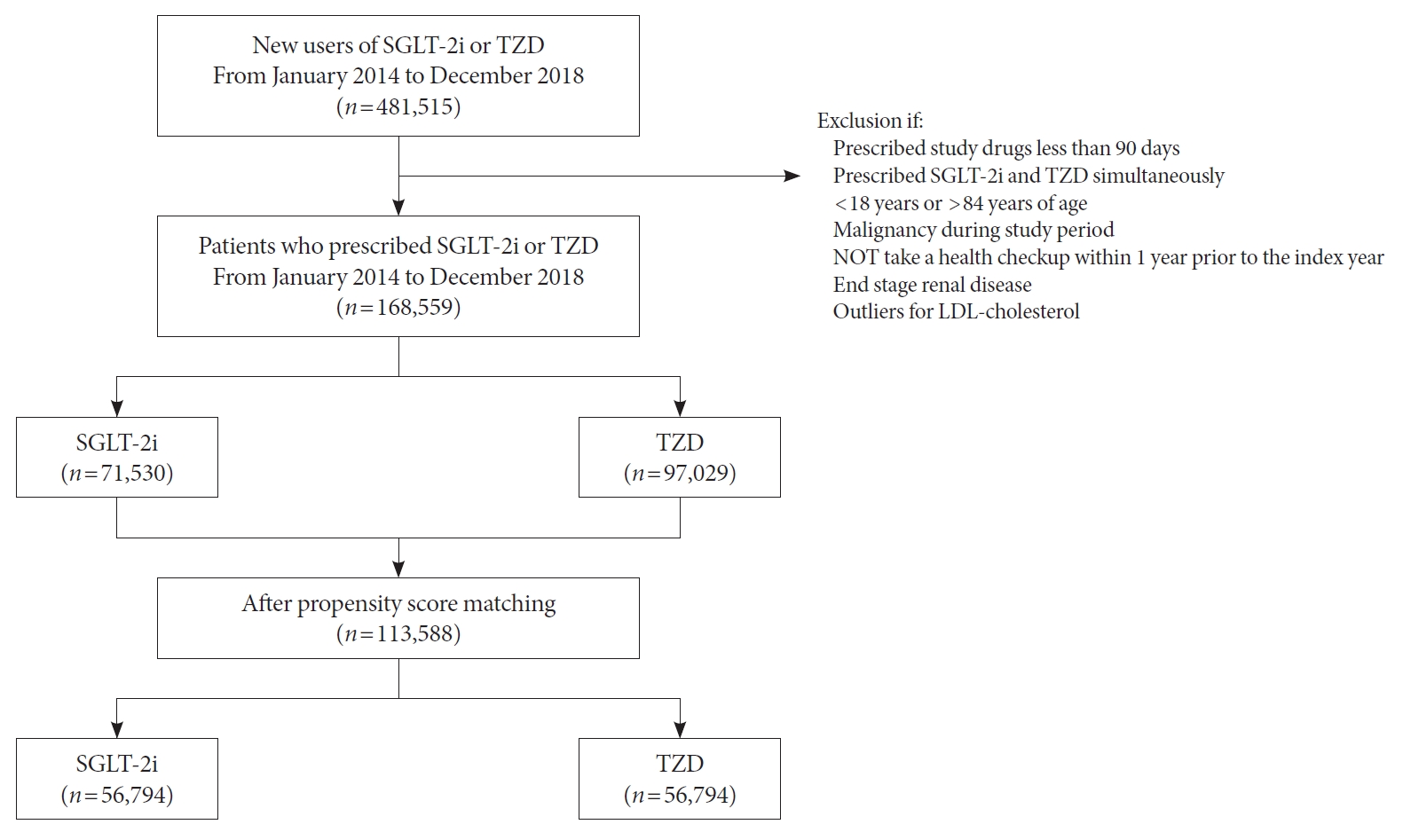
Although cardiovascular outcome trials using sodium-glucose cotransporter-2 inhibitors (SGLT-2i) showed a reduction in risk of 3-point major adverse cardiovascular events (MACE), they did not demonstrate beneficial effects on stroke risk. Additionally, meta-analysis showed SGLT-2i potentially had an adverse effect on stroke risk. Contrarily, pioglitazone, a type of thiazolidinedione (TZD), has been shown to reduce recurrent stroke risk. Thus, we aimed to compare the effect of SGLT-2i and TZD on the risk of stroke in type 2 diabetes mellitus (T2DM) patients.
Methods
Using the Korean National Health Insurance Service data, we compared a 1:1 propensity score-matched cohort of patients who used SGLT-2i or TZD from January 2014 to December 2018. The primary outcome was stroke. The secondary outcomes were myocardial infarction (MI), cardiovascular death, 3-point MACE, and heart failure (HF).
Results
After propensity-matching, each group included 56,794 patients. Baseline characteristics were well balanced. During the follow-up, 862 patients were newly hospitalized for stroke. The incidence rate of stroke was 4.11 and 4.22 per 1,000 person-years for the TZD and SGLT-2i groups respectively. The hazard ratio (HR) of stroke was 1.054 (95% confidence interval [CI], 0.904 to 1.229) in the SGLT-2i group compared to the TZD group. There was no difference in the risk of MI, cardiovascular death, 3-point MACE between groups. Hospitalization for HF was significantly decreased in SGLT-2i-treated patients (HR, 0.645; 95% CI, 0.466 to 0.893). Results were consistent regardless of prior cardiovascular disease.
Conclusion
In this real-world data, the risk of stroke was comparable in T2DM patients treated with SGLT-2i or TZD. -
Citations
Citations to this article as recorded by- Similar incidence of stroke with SGLT2 inhibitors and GLP-1 receptor agonists in real-world cohort studies among patients with type 2 diabetes
André J. Scheen
Diabetes Epidemiology and Management.2024; 13: 100179. CrossRef - Lobeglitazone, a novel thiazolidinedione, for secondary prevention in patients with ischemic stroke: a nationwide nested case-control study
Joonsang Yoo, Jimin Jeon, Minyoul Baik, Jinkwon Kim
Cardiovascular Diabetology.2023;[Epub] CrossRef - Do SGLT2 inhibitors and GLP-1 receptor agonists modulate differently the risk of stroke ? Discordance between randomised controlled trials and observational studies
André J. Scheen
Diabetes & Metabolism.2023; 49(5): 101474. CrossRef
- Similar incidence of stroke with SGLT2 inhibitors and GLP-1 receptor agonists in real-world cohort studies among patients with type 2 diabetes
- Metabolic Risk/Epidemiology
- Reproductive Life Span and Severe Hypoglycemia Risk in Postmenopausal Women with Type 2 Diabetes Mellitus
- Soyeon Kang, Yong-Moon Park, Dong Jin Kwon, Youn-Jee Chung, Jeong Namkung, Kyungdo Han, Seung-Hyun Ko
- Diabetes Metab J. 2022;46(4):578-591. Published online January 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0135
- 5,903 View
- 230 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Estrogen promotes glucose homeostasis, enhances insulin sensitivity, and maintains counterregulatory responses in recurrent hypoglycemia in women of reproductive age. Postmenopausal women with type 2 diabetes mellitus (T2DM) might be more vulnerable to severe hypoglycemia (SH) events. However, the relationship between reproductive factors and SH occurrence in T2DM remains unelucidated.
Methods
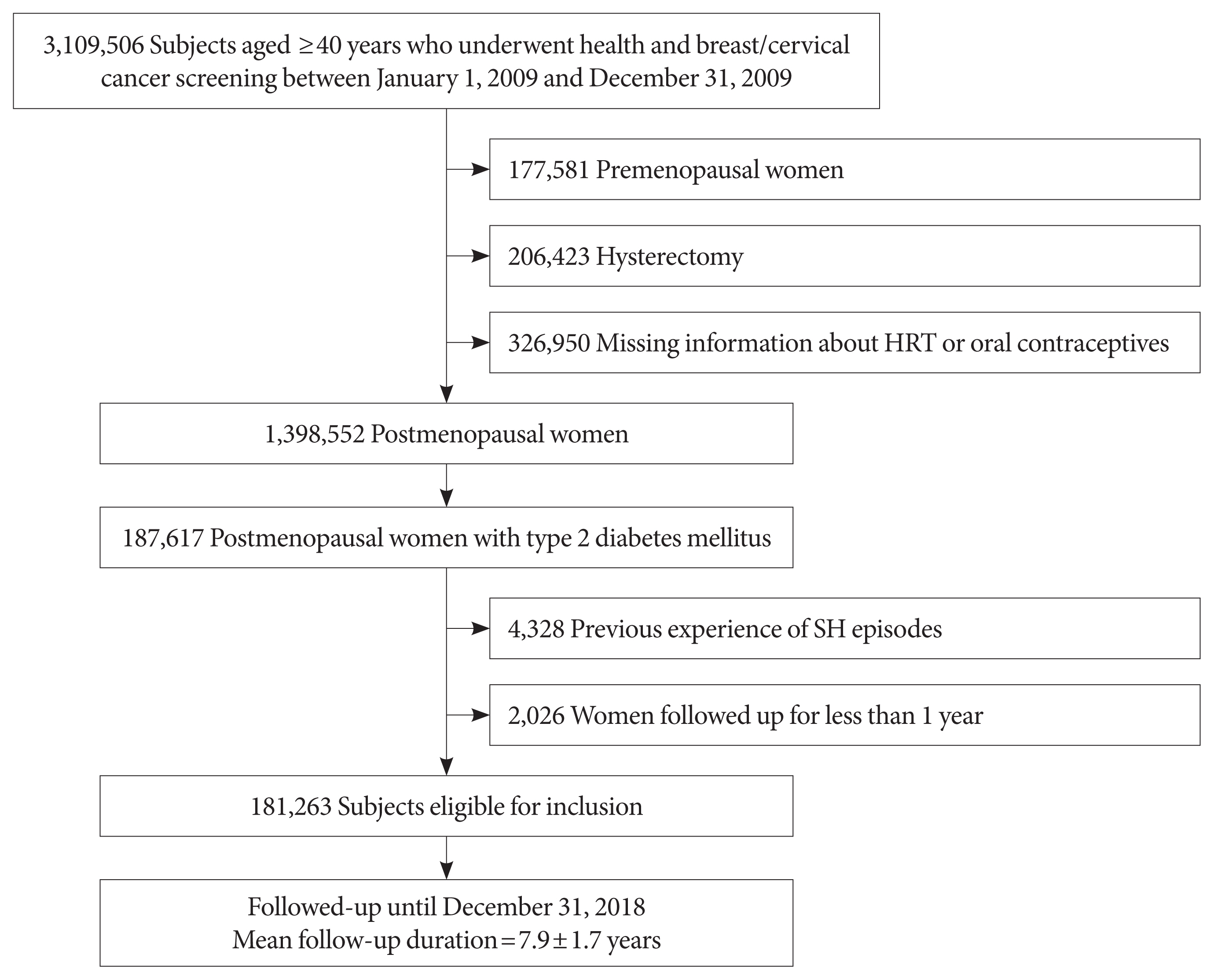
This study included data on 181,263 women with postmenopausal T2DM who participated in a national health screening program from January 1 to December 31, 2009, obtained using the Korean National Health Insurance System database. Outcome data were obtained until December 31, 2018. Associations between reproductive factors and SH incidence were assessed using Cox proportional hazards models.
Results
During the mean follow-up of 7.9 years, 11,279 (6.22%) postmenopausal women with T2DM experienced SH episodes. A longer reproductive life span (RLS) (≥40 years) was associated with a lower SH risk compared to a shorter RLS (<30 years) (adjusted hazard ratio [HR], 0.74; 95% confidence interval [CI], 0.69 to 0.80; P for trend <0.001) after multivariable adjustment. SH risk decreased with every 5-year increment of RLS (with <30 years as a reference [adjusted HR, 0.91; 95% CI, 0.86 to 0.95; P=0.0001 for 30−34 years], [adjusted HR, 0.80; 95% CI, 0.76 to 0.84; P<0.001 for 35−39 years], [adjusted HR, 0.74; 95% CI, 0.68 to 0.81; P<0.001 for ≥40 years]). The use of hormone replacement therapy (HRT) was associated with a lower SH risk than HRT nonuse.
Conclusion
Extended exposure to endogenous ovarian hormone during lifetime may decrease the number of SH events in women with T2DM after menopause. -
Citations
Citations to this article as recorded by- Association between serum copper level and reproductive health of Women in the United States: a cross-sectional study
Yi Yuan, Tong-Yu Peng, Guang-Yuan Yu, Zhao Zou, Meng-Ze Wu, Ruofei Zhu, Shuang Wu, Zi Lv, Su-Xin Luo
International Journal of Environmental Health Research.2023; : 1. CrossRef - Reproductive Lifespan and Motor Progression of Parkinson’s Disease
Ruwei Ou, Qianqian Wei, Yanbing Hou, Lingyu Zhang, Kuncheng Liu, Junyu Lin, Tianmi Yang, Jing Yang, Zheng Jiang, Wei Song, Bei Cao, Huifang Shang
Journal of Clinical Medicine.2022; 11(20): 6163. CrossRef - Menopause and development of Alzheimer’s disease: Roles of neural glucose metabolism and Wnt signaling
Paulina Villaseca, Pedro Cisternas, Nibaldo C. Inestrosa
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Association between serum copper level and reproductive health of Women in the United States: a cross-sectional study
- Metabolic Risk/Epidemiology
- Effect of Low-Dose Persistent Organic Pollutants on Mitochondrial Function: Human and in Vitro Evidence
- Se-A Kim, Hoyul Lee, Sung-Mi Park, Mi-Jin Kim, Yu-Mi Lee, Young-Ran Yoon, Hyun-Kyung Lee, Hyo-Bang Moon, In-Kyu Lee, Duk-Hee Lee
- Diabetes Metab J. 2022;46(4):592-604. Published online January 26, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0132
- 5,168 View
- 237 Download
- 5 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Chronic exposure to low-dose persistent organic pollutants (POPs) can induce mitochondrial dysfunction. This study evaluated the association between serum POP concentrations and oxygen consumption rate (OCR) as a marker of mitochondrial function in humans and in vitro cells.
Methods
Serum concentrations of organochlorine pesticides (OCPs) and polychlorinated biphenyls (PCBs) were measured in 323 adults. The OCRs of platelets and peripheral blood mononuclear cells (PBMCs) were assessed in 20 mL of fresh blood using a Seahorse XF analyzer. Additionally, the in vitro effects of Arochlor-1254, β-hexachlorocyclohexane, and p,p´-dichlorodiphenyltrichloroethane at concentrations of 0.1 pM to 100 nM were evaluated in human platelets, human PBMCs, and Jurkat T-cells.
Results
The association between serum POP concentrations and OCR differed depending on the cell type. As serum OCP concentrations increased, basal platelet OCR levels decreased significantly; according to the OCP quintiles of summary measure, they were 8.6, 9.6, 8.2, 8.0, and 7.1 pmol/min/μg (P trend=0.005). Notably, the basal PBMC OCR levels decreased remarkably as the serum PCB concentration increased. PBMC OCR levels were 46.5, 34.3, 29.1, 16.5, and 13.1 pmol/min/μg according to the PCB quintiles of summary measure (P trend <0.001), and this inverse association was consistently observed in all subgroups stratified by age, sex, obesity, type 2 diabetes mellitus, and hypertension, respectively. In vitro experimental studies have also demonstrated that chronic exposure to low-dose POPs could decrease OCR levels.
Conclusion
The findings from human and in vitro studies suggest that chronic exposure to low-dose POPs can induce mitochondrial dysfunction by impairing oxidative phosphorylation. -
Citations
Citations to this article as recorded by- Persistent Organic Pollutants released from decomposed adipose tissue affect mitochondrial enzyme function in the brain and eyes other than the liver
Dongshin Yang, Eun Ko, Hwayeon Lim, Hyojin Lee, Kitae Kim, Moonsung Choi, Sooim Shin
Environmental Science and Pollution Research.2024; 31(7): 10648. CrossRef - Can lipophilic pollutants in adipose tissue explain weight change‐related risk in type 2 diabetes mellitus?
Duk‐Hee Lee, In‐Kyu Lee
Journal of Diabetes Investigation.2023; 14(4): 528. CrossRef - Mitochondrial and metabolic features of salugenesis and the healing cycle
Robert K. Naviaux
Mitochondrion.2023; 70: 131. CrossRef - Obesity Paradox in Sepsis: Role of Adipose Tissue in Storing Mitochondrial Toxins
Duk-Hee Lee
Critical Care Medicine.2023; 51(8): e172. CrossRef - Human Preadipocytes Differentiated under Hypoxia following PCB126 Exposure during Proliferation: Effects on Differentiation, Glucose Uptake and Adipokine Profile
Zeinab El Amine, Jean-François Mauger, Pascal Imbeault
Cells.2023; 12(18): 2326. CrossRef - Is micronucleus assay in oral exfoliated cells a useful biomarker for biomonitoring populations exposed to pesticides? A systematic review with meta-analysis
Ingra Tais Malacarne, Wilton Mitsunari Takeshita, Daniel Vitor de Souza, Barbara dos Anjos Rosario, Milena de Barros Viana, Ana Claudia Muniz Renno, Daisy Maria Favero Salvadori, Daniel Araki Ribeiro
Environmental Science and Pollution Research.2022; 29(43): 64392. CrossRef - Comment on: Obesity is Associated with Improved Postoperative Overall Survival, Independent of Skeletal Muscle Mass in Lung Adenocarcinoma by Lee et al.
Duk‐Hee Lee
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(5): 2576. CrossRef
- Persistent Organic Pollutants released from decomposed adipose tissue affect mitochondrial enzyme function in the brain and eyes other than the liver
- Metabolic Risk/Epidemiology
- Effect of Different Types of Diagnostic Criteria for Gestational Diabetes Mellitus on Adverse Neonatal Outcomes: A Systematic Review, Meta-Analysis, and Meta-Regression
- Fahimeh Ramezani Tehrani, Marzieh Saei Ghare Naz, Razieh Bidhendi-Yarandi, Samira Behboudi-Gandevani
- Diabetes Metab J. 2022;46(4):605-619. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0178
- 5,087 View
- 298 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Evidence supporting various diagnostic criteria for diagnose gestational diabetes mellitus (GDM) are consensus-based, needs for additional evidence related to outcomes. Therefore, the aim of this systematic-review and meta-analysis was to assess the impact of different GDM diagnostic-criteria on the risk of adverse-neonatal-outcomes.
Methods
Electronic databases including Scopus, PubMed, and Web of Sciences were searched to retrieve English original, population-based studies with the universal GDM screening approach, up to January-2020. GDM diagnostic criteria were classified in seven groups and International Association of the Diabetes and Pregnancy Study Groups (IADPSG) was considered as reference one. We used the Mantel–Haenszel method to calculate the pooled odds of events. The possibility of publication bias was examined by Begg’s test.
Results
A total of 55 population-based studies consisting of 1,604,391 pregnant women with GDM and 7,770,855 non-GDM counterparts were included. Results showed that in all diagnostic-criteria subgroups, the risk of adverse neonatal outcomes including macrosomia, hyperbilirubinemia, respiratory distress syndrome, neonatal hypoglycemia, neonatal intensive care unit admission, preterm birth, and birth-trauma were significantly higher than the non-GDM counterparts were significantly higher than non-GDM counterparts. Meta-regression analysis revealed that the magnitude of neonatal risks in all diagnostic-criteria subgroups are similar.
Conclusion
Our results showed that the risk of adverse-neonatal-outcome increased among women with GDM, but the magnitude of risk was not different among those women who were diagnosed through more or less intensive strategies. These findings may help health-care-providers and policy-makers to select the most cost-effective approach for the screening of GDM among pregnant women. -
Citations
Citations to this article as recorded by- Hyperglycemia in pregnancy did not worsen the short-term outcomes of very preterm infants: a propensity score matching study
Ying Li, Wei Shen, Rong Zhang, Jian Mao, Ling Liu, Yan-Mei Chang, Xiu-Zhen Ye, Yin-Ping Qiu, Li Ma, Rui Cheng, Hui Wu, Dong-Mei Chen, Ling Chen, Ping Xu, Hua Mei, San-Nan Wang, Fa-Lin Xu, Rong Ju, Xiao-Mei Tong, Xin-Zhu Lin, Fan Wu
Frontiers in Pediatrics.2024;[Epub] CrossRef - Diabetesscreening in der Schwangerschaft
Ute Schäfer-Graf
Die Gynäkologie.2023; 56(2): 103. CrossRef - One-step versus two-step screening for diagnosis of gestational diabetes mellitus in Iranian population: A randomized community trial
Fahimeh Ramezani Tehrani, Maryam Rahmati, Farshad Farzadfar, Mehrandokht Abedini, Maryam Farahmand, Farhad Hosseinpanah, Farzad Hadaegh, Farahnaz Torkestani, Majid Valizadeh, Fereidoun Azizi, Samira Behboudi-Gandevani
Frontiers in Endocrinology.2023;[Epub] CrossRef - Predictors of Neonatal Intensive Care Unit Admission and Adverse Outcomes Related to Gestational Diabetes
Abdullah M Al-shahrani
Cureus.2023;[Epub] CrossRef - Positive association between circulating Caveolin-1 and microalbuminuria in overt diabetes mellitus in pregnancy
Y. Shu, Y. Xiong, Y. Song, S. Jin, X. Bai
Journal of Endocrinological Investigation.2023; 47(1): 201. CrossRef - Early-to-mid pregnancy sleep and circadian markers in relation to birth outcomes: An epigenetics pilot study
Erica C. Jansen, Kelvin Pengyuan Zhang, Dana C. Dolinoy, Helen J. Burgess, Louise M. O’Brien, Elizabeth Langen, Naquia Unwala, Jessa Ehlinger, Molly C. Mulcahy, Jaclyn M. Goodrich
Chronobiology International.2023; 40(9): 1224. CrossRef - Various screening and diagnosis approaches for gestational diabetes mellitus and adverse pregnancy outcomes: a secondary analysis of a randomized non-inferiority field trial
Fahimeh Ramezani Tehrani, Ali Sheidaei, Maryam Rahmati, Farshad Farzadfar, Mahsa Noroozzadeh, Farhad Hosseinpanah, Mehrandokht Abedini, Farzad Hadaegh, Majid Valizadeh, Farahnaz Torkestani, Davood Khalili, Faegheh Firouzi, Masoud Solaymani-Dodaran, Afshin
BMJ Open Diabetes Research & Care.2023; 11(6): e003510. CrossRef
- Hyperglycemia in pregnancy did not worsen the short-term outcomes of very preterm infants: a propensity score matching study
- Complications
- Prevalence of Diabetic Retinopathy in Undiagnosed Diabetic Patients: A Nationwide Population-Based Study
- Han Na Jang, Min Kyong Moon, Bo Kyung Koo
- Diabetes Metab J. 2022;46(4):620-629. Published online February 23, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0099
- 4,024 View
- 215 Download
- 2 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated the prevalence of diabetic retinopathy (DR) in patients with undiagnosed diabetes through a nationwide survey, compared to those with known diabetes.
Methods
Among the participants of the Korean National Health and Nutrition Examination Surveys (KNHANES) from 2017 to 2018, individuals aged ≥40 years with diabetes and fundus exam results were enrolled. Sampling weights were applied to represent the entire Korean population. Newly detected diabetes patients through KNHANES were classified under “undiagnosed diabetes.”
Results
Among a total of 9,108 participants aged ≥40 years, 951 were selected for analysis. Of them, 31.3% (standard error, ±2.0%) were classified under “undiagnosed diabetes.” The prevalence of DR in patients with known and undiagnosed diabetes was 24.5%±2.0% and 10.7%±2.2%, respectively (P<0.001). The DR prevalence increased with rising glycosylated hemoglobin (HbA1c) levels in patients with known and undiagnosed diabetes (P for trend=0.001 in both). Among those with undiagnosed diabetes, the prevalence of DR was 6.9%±2.1%, 8.0%±3.4%, 5.6%±5.7%, 16.7%±9.4%, and 42.6%±14.8% for HbA1c levels of <7.0%, 7.0%–7.9%, 8.0%–8.9%, 9.0%–9.9%, and ≥10.0% respectively. There was no difference in the prevalence of hypertension, dyslipidemia, hypertriglyceridemia, or obesity according to the presence or absence of DR.
Conclusion
About one-third of patients with diabetes were unaware of their diabetes, and 10% of them have already developed DR. Considering increasing the prevalence of DR according to HbA1c level was found in patients with undiagnosed diabetes like those with known diabetes, screening and early detection of diabetes and DR are important. -
Citations
Citations to this article as recorded by- Risk factors of peripheral occlusive arterial disease in patients with diabetic retinopathy due to type 2 diabetes
Milos Maksimovic
Srpski arhiv za celokupno lekarstvo.2024; 152(1-2): 50. CrossRef - Gene Expression Analysis in T2DM and Its Associated Microvascular Diabetic Complications: Focus on Risk Factor and RAAS Pathway
Laxmipriya Jena, Prabhsimran Kaur, Tashvinder Singh, Kangan Sharma, Sushil Kotru, Anjana Munshi
Molecular Neurobiology.2024;[Epub] CrossRef - Novel Asian-Specific Visceral Adiposity Indices Are Associated with Chronic Kidney Disease in Korean Adults
Jonghwa Jin, Hyein Woo, Youngeun Jang, Won-Ki Lee, Jung-Guk Kim, In-Kyu Lee, Keun-Gyu Park, Yeon-Kyung Choi
Diabetes & Metabolism Journal.2023; 47(3): 426. CrossRef - Prevalence of osteosarcopenic obesity and related factors among Iranian older people: Bushehr Elderly Health (BEH) program
Mozhgan Ahmadinezhad, Mohammad Ali Mansournia, Noushin Fahimfar, Gita Shafiee, Iraj Nabipour, Mahnaz Sanjari, Kazem Khalagi, Mohammad Javad Mansourzadeh, Bagher Larijani, Afshin Ostovar
Archives of Osteoporosis.2023;[Epub] CrossRef
- Risk factors of peripheral occlusive arterial disease in patients with diabetic retinopathy due to type 2 diabetes
- Complications
- Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
- Da Hea Seo, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongha Seo, Seongbin Hong, Yong-ho Lee, Young Ju Choi, Eunjig Lee, So Hun Kim
- Diabetes Metab J. 2022;46(4):630-639. Published online January 26, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0130
- 5,528 View
- 274 Download
- 14 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Nonalcoholic fatty liver disease (NAFLD) is associated with chronic kidney disease (CKD). However, the causal relationship between NAFLD and CKD is uncertain, particularly in patients with type 2 diabetes mellitus (T2DM). We aimed to investigate the association between the presence and severity of NAFLD and incident CKD in patients with T2DM.
Methods
In this longitudinal cohort study of patients with T2DM, 3,188 patients with preserved renal function were followed up for the occurrence of incident CKD. NAFLD was defined as the presence of hepatic steatosis on ultrasonography, without any other causes of chronic liver disease. Advanced liver fibrosis of NAFLD was defined as a fibrosis-4 index ≥2.67. CKD was defined as an estimated glomerular filtration rate <60 mL/min/1.73 m2.
Results
At baseline, 1,729 (54.2%) patients had NAFLD, of whom 94 (5.4%) had advanced liver fibrosis. During the follow-up of 8.3±3.6 years, 472 (14.8%) patients developed incident CKD: 220 (15.1%) in the non-NAFLD group, 231 (14.1%) in the NAFLD without advanced fibrosis group and 28 (31.1%) in the NAFLD with advanced fibrosis group. There was no increased risk of incident CKD in the NAFLD group compared to the non-NAFLD group (P=0.435). However, among patients with NAFLD, advanced liver fibrosis was associated with an increased risk of CKD (adjusted hazard ratio, 1.75; 95% confidence interval, 1.15 to 2.66; P=0.009).
Conclusion
Advanced liver fibrosis in patients with NAFLD is independently associated with an increased risk of incident CKD in patients with T2DM. -
Citations
Citations to this article as recorded by- Esteatosis hepática metabólica y nefropatía diabética: una llamada a la acción
Salvador Benlloch, Francesc Moncho, Jose Luis Górriz
Nefrología.2024; 44(2): 129. CrossRef - Longitudinal Outcomes Associated With Metabolic Dysfunction-Associated Steatotic Liver Disease: A Meta-analysis of 129 Studies
Kai En Chan, Elden Yen Hng Ong, Charlotte Hui Chung, Christen En Ya Ong, Benjamin Koh, Darren Jun Hao Tan, Wen Hui Lim, Jie Ning Yong, Jieling Xiao, Zhen Yu Wong, Nicholas Syn, Apichat Kaewdech, Margaret Teng, Jiong-Wei Wang, Nicholas Chew, Dan Yock Young
Clinical Gastroenterology and Hepatology.2024; 22(3): 488. CrossRef - Association of NAFLD/NASH, and MAFLD/MASLD with chronic kidney disease: an updated narrative review
Amedeo Lonardo
Metabolism and Target Organ Damage.2024;[Epub] CrossRef - Targeting metabolic-associated fatty liver disease in diabetic kidney disease: A call to action
Salvador Benlloch, Francesc Moncho, Jose Luis Górriz
Nefrología (English Edition).2024;[Epub] CrossRef - MAFLD and NAFLD in the prediction of incident chronic kidney disease
So Yoon Kwon, Jiyun Park, So Hee Park, You-Bin Lee, Gyuri Kim, Kyu Yeon Hur, Janghyun Koh, Jae Hwan Jee, Jae Hyeon Kim, Mira Kang, Sang-Man Jin
Scientific Reports.2023;[Epub] CrossRef - Associations of non-invasive indices of liver steatosis and fibrosis with progressive kidney impairment in adults with type 2 diabetes
Mei Chung Moh, Sharon Li Ting Pek, Kenny Ching Pan Sze, Serena Low, Tavintharan Subramaniam, Keven Ang, Wern Ee Tang, Simon Biing Ming Lee, Chee Fang Sum, Su Chi Lim
Acta Diabetologica.2023; 60(6): 827. CrossRef - Pancreatic beta-cell specific BAG3 knockout results in chronic hyperinsulinemia inducing insulin resistance
Verena Damiani, Alessia Lamolinara, Ilaria Cicalini, Maria Concetta Cufaro, Francesco Del Pizzo, Federica Di Marco, Piero Del Boccio, Beatrice Dufrusine, Michael Hahne, Rossano Lattanzio, Damiana Pieragostino, Manuela Iezzi, Massimo Federici, Maria Cateri
Molecular Metabolism.2023; 74: 101752. CrossRef - Utility of non-invasive liver fibrosis markers to predict the incidence of chronic kidney disease (CKD): A systematic review, meta-analysis, and meta-regression
Rudi Supriyadi, Theo Audi Yanto, Timotius Ivan Hariyanto, Ketut Suastika
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(8): 102814. CrossRef - Significance of Diabetic Kidney Disease Biomarkers in Predicting Metabolic-Associated Fatty Liver Disease
Jaehyun Bae, Byung-Wan Lee
Biomedicines.2023; 11(7): 1928. CrossRef - Hepatic Fibrosis Evaluated in Patients with Type 2 Diabetes with and without Chronic Kidney Disease
Therese Adrian, Mads Hornum, Filip Krag Knop, Karl Bang Christensen, Thomas Almdal, Peter Rossing, Lisa Í Lídaa, Niels Søndergaard Heinrich, Vincent Oltman Boer, Anouk Marsman, Esben Thade Petersen, Hartwig Roman Siebner, Bo Feldt-Rasmussen
Nephron.2023; 147(11): 673. CrossRef - Clinical Interest of Serum Alpha-2 Macroglobulin, Apolipoprotein A1, and Haptoglobin in Patients with Non-Alcoholic Fatty Liver Disease, with and without Type 2 Diabetes, before or during COVID-19
Olivier Deckmyn, Thierry Poynard, Pierre Bedossa, Valérie Paradis, Valentina Peta, Raluca Pais, Vlad Ratziu, Dominique Thabut, Angelique Brzustowski, Jean-François Gautier, Patrice Cacoub, Dominique Valla
Biomedicines.2022; 10(3): 699. CrossRef - Fibrosis Risk in Nonalcoholic Fatty Liver Disease Is Related to Chronic Kidney Disease in Older Type 2 Diabetes Patients
Yifan Sun, Liang Hong, Zhe Huang, Lihong Wang, Yanqin Xiong, Shuhang Zong, Rui Zhang, Jun Liu, Shufei Zang
The Journal of Clinical Endocrinology & Metabolism.2022; 107(9): e3661. CrossRef - Beyond Liver Disease: Non-Alcoholic Fatty Liver Disease and Advanced Liver Fibrosis in Kidney Disease
Eugene Han
Diabetes & Metabolism Journal.2022; 46(4): 564. CrossRef - A higher FIB‐4 index is associated with an increased incidence of renal failure in the general population
Eva Maria Schleicher, Simon Johannes Gairing, Peter Robert Galle, Julia Weinmann‐Menke, Jörn M. Schattenberg, Karel Kostev, Christian Labenz
Hepatology Communications.2022; 6(12): 3505. CrossRef - Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2022;46:630-9)
Ji Hye Huh
Diabetes & Metabolism Journal.2022; 46(6): 953. CrossRef - Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2022;46:630-9)
Da Hea Seo, So Hun Kim
Diabetes & Metabolism Journal.2022; 46(6): 956. CrossRef
- Esteatosis hepática metabólica y nefropatía diabética: una llamada a la acción
- Complications
- Fatty Acid-Binding Protein 4 in Patients with and without Diabetic Retinopathy
- Ping Huang, Xiaoqin Zhao, Yi Sun, Xinlei Wang, Rong Ouyang, Yanqiu Jiang, Xiaoquan Zhang, Renyue Hu, Zhuqi Tang, Yunjuan Gu
- Diabetes Metab J. 2022;46(4):640-649. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0195
- 3,407 View
- 193 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Fatty acid-binding protein 4 (FABP4) has been demonstrated to be a predictor of early diabetic nephropathy. However, little is known about the relationship between FABP4 and diabetic retinopathy (DR). This study explored the value of FABP4 as a biomarker of DR in patients with type 2 diabetes mellitus (T2DM).
Methods
A total of 238 subjects were enrolled, including 20 healthy controls and 218 T2DM patients. Serum FABP4 levels were measured using a sandwich enzyme-linked immunosorbent assay. The grade of DR was determined using fundus fluorescence angiography. Based on the international classification of DR, all T2DM patients were classified into the following three subgroups: non-DR group, non-proliferative diabetic retinopathy (NPDR) group, and proliferative diabetic retinopathy (PDR) group. Multivariate logistic regression analyses were employed to assess the correlation between FABP4 levels and DR severity.
Results
FABP4 correlated positively with DR severity (r=0.225, P=0.001). Receiver operating characteristic curve analysis was used to assess the diagnostic potential of FABP4 in identifying DR, with an area under the curve of 0.624 (37% sensitivity, 83.6% specificity) and an optimum cut-off value of 76.4 μg/L. Multivariate logistic regression model including FABP4 as a categorized binary variable using the cut-off value of 76.4 μg/L showed that the concentration of FABP4 above the cut-off value increased the risk of NPDR (odds ratio [OR], 3.231; 95% confidence interval [CI], 1.574 to 6.632; P=0.001) and PDR (OR, 3.689; 95% CI, 1.306 to 10.424; P=0.014).
Conclusion
FABP4 may be used as a serum biomarker for the diagnosis of DR. -
Citations
Citations to this article as recorded by- Circulating AFABP, FGF21, and PEDF Levels as Prognostic Biomarkers of Sight-threatening Diabetic Retinopathy
Chi-Ho Lee, David Tak-Wai Lui, Chloe Yu-Yan Cheung, Carol Ho-Yi Fong, Michele Mae-Ann Yuen, Yu-Cho Woo, Wing-Sun Chow, Ian Yat-Hin Wong, Aimin Xu, Karen Siu-Ling Lam
The Journal of Clinical Endocrinology & Metabolism.2023; 108(9): e799. CrossRef - A Prediction Model for Sight-Threatening Diabetic Retinopathy Based on Plasma Adipokines among Patients with Mild Diabetic Retinopathy
Yaxin An, Bin Cao, Kun Li, Yongsong Xu, Wenying Zhao, Dong Zhao, Jing Ke, Takayuki Masaki
Journal of Diabetes Research.2023; 2023: 1. CrossRef
- Circulating AFABP, FGF21, and PEDF Levels as Prognostic Biomarkers of Sight-threatening Diabetic Retinopathy
- Others
- Development of Various Diabetes Prediction Models Using Machine Learning Techniques
- Juyoung Shin, Jaewon Kim, Chanjung Lee, Joon Young Yoon, Seyeon Kim, Seungjae Song, Hun-Sung Kim
- Diabetes Metab J. 2022;46(4):650-657. Published online March 11, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0115
- 4,795 View
- 294 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There are many models for predicting diabetes mellitus (DM), but their clinical implication remains vague. Therefore, we aimed to create various DM prediction models using easily accessible health screening test parameters.
Methods
Two sets of variables were used to develop eight DM prediction models. One set comprised 62 easily accessible examination results of commonly used variables from a tertiary university hospital. The second set comprised 27 of the 62 variables included in the national routine health checkups. Gradient boosting and random forest algorithms were used to develop the models. Internal validation was performed using the stratified 10-fold cross-validation method.
Results
The area under the receiver operating characteristic curve (ROC-AUC) for the 62-variable DM model making 12-month predictions for subjects without diabetes was the largest (0.928) among those of the eight DM prediction models. The ROC-AUC dropped by more than 0.04 when training with the simplified 27-variable set but still showed fairly good performance with ROC-AUCs between 0.842 and 0.880. The accuracy was up to 11.5% higher (from 0.807 to 0.714) when fasting glucose was included.
Conclusion
We created easily applicable diabetes prediction models that deliver good performance using parameters commonly assessed during tertiary university hospital and national routine health checkups. We plan to perform prospective external validation, hoping that the developed DM prediction models will be widely used in clinical practice. -
Citations
Citations to this article as recorded by- Predictive modeling for the development of diabetes mellitus using key factors in various machine learning approaches
Marenao Tanaka, Yukinori Akiyama, Kazuma Mori, Itaru Hosaka, Kenichi Kato, Keisuke Endo, Toshifumi Ogawa, Tatsuya Sato, Toru Suzuki, Toshiyuki Yano, Hirofumi Ohnishi, Nagisa Hanawa, Masato Furuhashi
Diabetes Epidemiology and Management.2024; 13: 100191. CrossRef - Validation of the Framingham Diabetes Risk Model Using Community-Based KoGES Data
Hye Ah Lee, Hyesook Park, Young Sun Hong
Journal of Korean Medical Science.2024;[Epub] CrossRef - Integrated Embedded system for detecting diabetes mellitus using various machine learning techniques
Rishita Konda, Anuraag Ramineni, Jayashree J, Niharika Singavajhala, Sai Akshaj Vanka
EAI Endorsed Transactions on Pervasive Health and Technology.2024;[Epub] CrossRef - The Present and Future of Artificial Intelligence-Based Medical Image in Diabetes Mellitus: Focus on Analytical Methods and Limitations of Clinical Use
Ji-Won Chun, Hun-Sung Kim
Journal of Korean Medical Science.2023;[Epub] CrossRef - Machine learning for predicting diabetic metabolism in the Indian population using polar metabolomic and lipidomic features
Nikita Jain, Bhaumik Patel, Manjesh Hanawal, Anurag R. Lila, Saba Memon, Tushar Bandgar, Ashutosh Kumar
Metabolomics.2023;[Epub] CrossRef - Retrospective cohort analysis comparing changes in blood glucose level and body composition according to changes in thyroid‐stimulating hormone level
Hyunah Kim, Da Young Jung, Seung‐Hwan Lee, Jae‐Hyoung Cho, Hyeon Woo Yim, Hun‐Sung Kim
Journal of Diabetes.2022; 14(9): 620. CrossRef - Improving Machine Learning Diabetes Prediction Models for the Utmost Clinical Effectiveness
Juyoung Shin, Joonyub Lee, Taehoon Ko, Kanghyuck Lee, Yera Choi, Hun-Sung Kim
Journal of Personalized Medicine.2022; 12(11): 1899. CrossRef
- Predictive modeling for the development of diabetes mellitus using key factors in various machine learning approaches
Short Communication
- Drug/Regimen
- Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study
- Hwi Seung Kim, Taekwan Yoon, Chang Hee Jung, Joong-Yeol Park, Woo Je Lee
- Diabetes Metab J. 2022;46(4):658-662. Published online November 8, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0232
- 65,535 View
- 387 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Sodium-glucose cotransporter 2 inhibitor (SGLT2i) and glucagon-like peptide-1 receptor agonist (GLP-1RA) are novel anti-diabetic drugs whose glucose-lowering effect and cardiovascular and renal benefits were evidenced in clinical trials. We investigated the real-world efficacy and safety of the combination of SGLT2i and GLP-1RA in patients with type 2 diabetes mellitus in Korea. The medical records of 104 patients who maintained the combination for at least 1 year were retrospectively reviewed. The change in glycosylated hemoglobin (HbA1c) after 6 months and 1 year of treatment was evaluated. The mean age was 51 years, and 41% were female. The mean baseline HbA1c, body mass index, and duration of diabetes were 9.0%, 28.8 kg/m2, and 11.7 years, respectively. Compared with baseline, the HbA1c decreased by 1.5% (95% confidence interval [CI], 1.27 to 1.74; P<0.001) after 6 months and by 1.4% (95% CI, 1.19 to 1.70; P<0.001) after 1 year. Over 1 year, the bodyweight change was −2.8 kg (95% CI, −4.21 to −1.47; P<0.001). The combination of SGLT2i and GLP-1RA is effective and tolerable in type 2 diabetes mellitus patients in real-world practice.
-
Citations
Citations to this article as recorded by- Effectiveness and safety of the combination of sodium–glucose transport protein 2 inhibitors and glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of observational studies
Aftab Ahmad, Hani Sabbour
Cardiovascular Diabetology.2024;[Epub] CrossRef - Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - All‐cause mortality and cardiovascular outcomes with sodium‐glucose Co‐transporter 2 inhibitors, glucagon‐like peptide‐1 receptor agonists and with combination therapy in people with type 2 diabetes
David R. Riley, Hani Essa, Philip Austin, Frank Preston, Isatu Kargbo, Gema Hernández Ibarburu, Ramandeep Ghuman, Daniel J. Cuthbertson, Gregory Y. H. Lip, Uazman Alam
Diabetes, Obesity and Metabolism.2023; 25(10): 2897. CrossRef - The Efficacy and Safety of the Combination Therapy With GLP-1 Receptor Agonists and SGLT-2 Inhibitors in Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis
Chen Li, Jie Luo, Mingyan Jiang, Keke Wang
Frontiers in Pharmacology.2022;[Epub] CrossRef - Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study (Diabetes Metab J 2022;46: 658-62)
Hwi Seung Kim, Woo Je Lee
Diabetes & Metabolism Journal.2022; 46(4): 665. CrossRef - Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study (Diabetes Metab J 2022;46: 658-62)
Tomoyuki Kawada
Diabetes & Metabolism Journal.2022; 46(4): 663. CrossRef - Durability of glucose-lowering effect of dulaglutide in patients with type 2 diabetes mellitus: A real-world data study
Hwi Seung Kim, Yun Kyung Cho, Myung Jin Kim, Chang Hee Jung, Joong-Yeol Park, Woo Je Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Effectiveness and safety of the combination of sodium–glucose transport protein 2 inhibitors and glucagon-like peptide-1 receptor agonists in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of observational studies
Letter
- Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study (Diabetes Metab J 2022;46: 658-62)
- Tomoyuki Kawada
- Diabetes Metab J. 2022;46(4):663-664. Published online July 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0131
- [Original]
- 2,415 View
- 139 Download

 KDA
KDA


 First
First Prev
Prev





