- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 45(5); 2021 > Article
-
Original ArticleMetabolic Risk/Epidemiology Longitudinal Change in Myocardial Function and Clinical Parameters in Middle-Aged Subjects: A 3-Year Follow-up Study
-
Dong-Hyuk Cho1
 , Hyung Joon Joo2, Mi-Na Kim2, Hee-Dong Kim3, Do-Sun Lim2
, Hyung Joon Joo2, Mi-Na Kim2, Hee-Dong Kim3, Do-Sun Lim2 , Seong-Mi Park2
, Seong-Mi Park2
-
Diabetes & Metabolism Journal 2021;45(5):719-729.
DOI: https://doi.org/10.4093/dmj.2020.0132
Published online: June 15, 2021
1Division of Cardiology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
2Division of Cardiology, Department of Internal Medicine, Korea University College of Medicine, Seoul, Korea
3Division of Cardiology, Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Soonchunhyang University College of Medicine, Cheonan, Korea
- Corresponding authors: Seong-Mi Park https://orcid.org/0000-0002-6710-685X Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, 73 Goryeodae-ro, Seongbuk-gu, Seoul 02841, Korea E-mail: smparkmd@korea.ac.kr
-
Do-Sun Lim
 Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, 73 Goryeodae-ro, Seongbuk-gu, Seoul 02841, Korea E-mail: dslmd@kumc.or.kr
Division of Cardiology, Department of Internal Medicine, Korea University Anam Hospital, Korea University College of Medicine, 73 Goryeodae-ro, Seongbuk-gu, Seoul 02841, Korea E-mail: dslmd@kumc.or.kr
Copyright © 2021 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Metabolic syndrome (MetS) is closely associated with the aging process. However, changes in metabolic conditions and cardiac function that occur in middle aged population remain unclear. We evaluated longitudinal changes in metabolic parameters and cardiac function during a 3-year period in subjects with suspected MetS.
-
Methods
- We studied 191 participants with suspected MetS at baseline and after 3 years. Anthropometric parameters, including waist circumference (WC), and metabolic parameters, including fasting blood glucose and lipid profile were measured. Conventional echocardiography with two-dimensional speckle tracking was performed.
-
Results
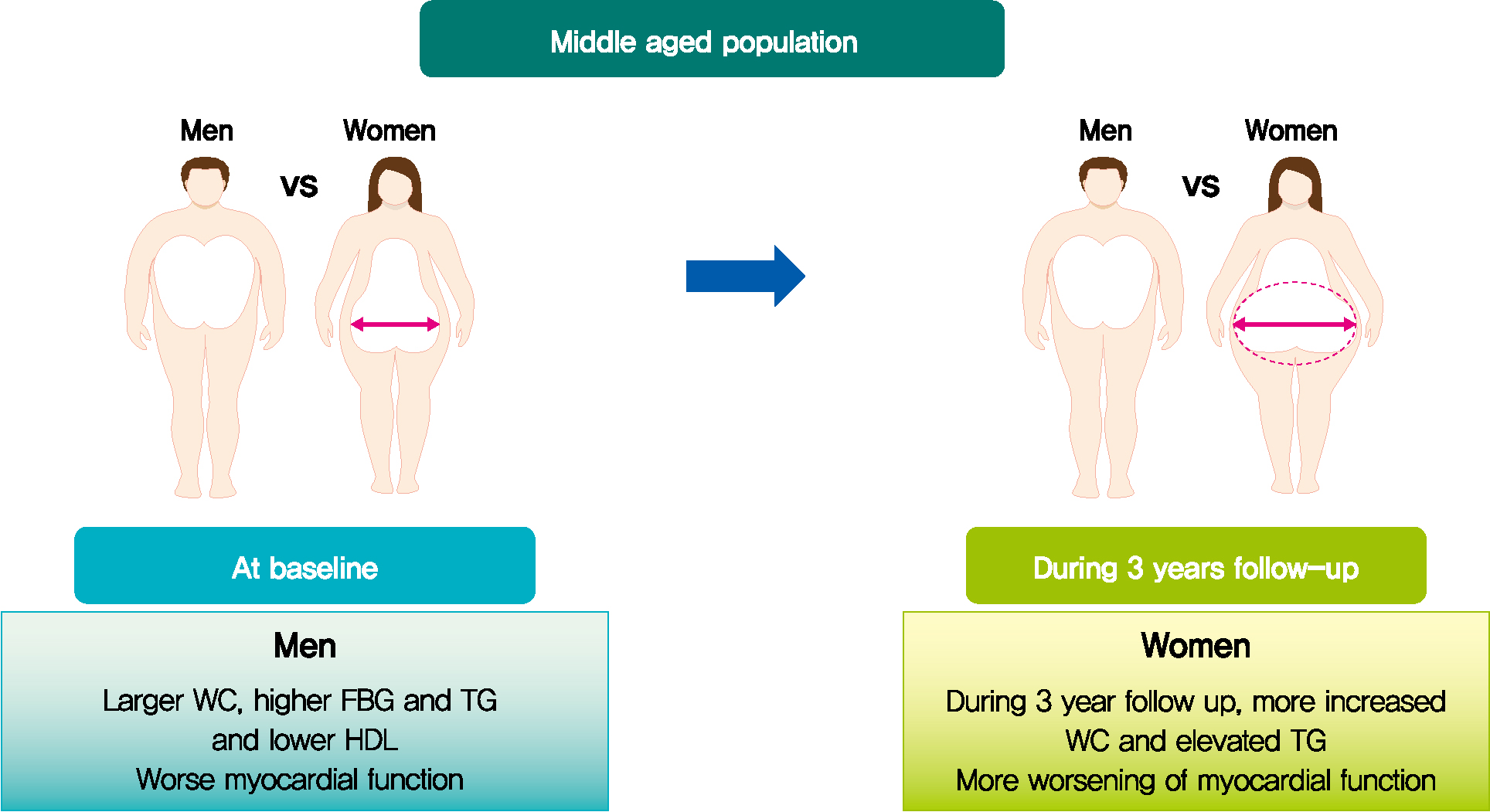
- Mean age was 56.2±4.4 years, and there were 97 women (50.8%). Men had increased WC and triglycerides (TG) (WC 91.2±6.8 cm vs. 84.0±8.0 cm, P<0.001; TG 184.4±116.3 mg/dL vs. 128.2±53.6 mg/dL, P<0.001), and reduced global longitudinal strain (GLS) (–15.4%±2.1% vs. –17.1%±2.0%, P<0.001) compared to women. After 3.4 years, values of WC and TG did not change in men but increased in women (all P<0.05). The absolute value of left ventricular (LV) GLS did not change in men but was reduced in women (P=0.011). Change in TG was independently associated with worsening of LV GLS only in women (standardized β, –0.309; 95% confidence interval, –0.130 to –0.009; P=0.025).
-
Conclusion
- In middle aged population, a vulnerable period for metabolic disturbance, cardiac remodeling tended to progress, which was prominent in women. Progression of adiposity and dyslipidemia after menopause may accelerate subclinical cardiac remodeling in middle-aged women. Lifestyle modification and medical interventions may help prevent further cardiac dysfunction in these subjects.
- The burden of metabolic syndrome (MetS) increases over the life course and metabolic disturbances are closely associated with cardiac remodeling [1-4]. Each metabolic component, such as hypertension, insulin resistance, dyslipidemia, and adiposity, is considered a fundamental determinant of cardiac concentric remodeling and dysfunction [5,6]. During the aging process, subclinical cardiac dysfunction appears early in the course of heart failure. Therefore, recent heart failure guidelines emphasize early detection of subclinical cardiac dysfunction and management of metabolic risk factors which can lead to overt heart failure [7,8].
- Longitudinal community-based studies have identified that hypertension, insulin resistance and obesity are important factors for cardiac concentric remodeling and dysfunction [2,3,5,9,10]. However, these studies focused on long-term follow-up from adolescence or early adulthood. The prevalence of MetS differs by age and sex, and in particular, increases rapidly in individuals between the ages of 50 to 60 [1,11]. After menopause, sexual dimorphism in hormone, glucose, and lipid metabolism accelerates the progression of cardiometabolic diseases in middle-aged women [12]. MetS is more common in men than women until 50 years of age, while this sex difference is attenuated during aging [11]. Given the increased burden of metabolic components during the transition period between 50 and 60 years of age, it is important to understand the impact of dysmetabolic changes on cardiac remodeling, which characterizes the early stage of overt heart failure [7,13].
- Therefore, we evaluated the longitudinal changes in metabolic parameters and its association with cardiac remodeling during a 3-year period in middle-aged subjects with suspected MetS.
INTRODUCTION
- Study population
- The Seoul Metabolic Syndrome study is a prospective cohort study to evaluate the characteristics and outcomes of subjects with suspected MetS. Participants were enrolled from 25 public health care centers in the Seoul metropolitan area. Detailed study protocols have been reported in previous studies [14,15]. This study is registered at www.clinicaltrials.gov (NCT02077530). A total of 191 consecutive participants who underwent conventional and two-dimensional speckle (2DS) echocardiography at baseline and after 3 years were enrolled in this study. Subjects with angina pectoris, myocardial infarction, any coronary revascularization procedure, or previous history of stroke were excluded. At baseline and follow-up, demographic data, concomitant medications, and previous medical history were evaluated, and a physical examination was performed. Data including body mass index (BMI), waist circumference (WC), and systolic and diastolic blood pressure (SBP and DBP) were measured at baseline and at the 3-year follow-up. Blood samples were collected from each subject after an 8-hour fast at baseline and follow-up. Total cholesterol, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, triglycerides (TG), and fasting blood glucose (FBG) values were obtained, along with written informed consent from all participants. The Institutional Review Board of Korea University Anam Hospital approved the current study (IRB NO. ED13087).
- Echocardiographic study
- All subjects underwent both conventional and 2DS echocardiography by using a commercially available echocardiographic system (Vivid-E9 with an M5Sc transducer; Vingmed-General Electric, Horten, Norway). Echocardiographic views were obtained based on the previously reported protocol [16]. Chamber size and function were measured by using 2D echocardiography images. Left ventricular end diastolic volume (LVEDV), left ventricular end systolic volume (LVESV), and left ventricular ejection fraction (LV EF) were measured and calculated using the biplane Simpson’s method from the apical 4- and 2-chamber view. Regional wall thickness (RWT), left atrial volume index (LAVI), and left atrial mass index (LVMI) were calculated using the formula recommended by the American Society of Echocardiography [16]. Early diastolic velocity of mitral inflow (E) was derived using pulsed-wave Doppler in the apical four-chamber view. Systolic and early diastolic velocities (s´ and e´) of the septal and lateral mitral annulus were evaluated using the pulsed-wave tissue Doppler image [17].
- A 2DS echocardiography was performed for each participant based on the recommended guidelines of the American Society of Echocardiography [16]. Images of three consecutive cardiac beats were derived while holding the breath. The second-harmonic B-mode images of 4-, 2-, and 3- chamber apical views of the left ventricular (LV) were derived and stored in digital cineloop images. The LV global longitudinal strain (GLS) was analyzed using EchoPac-PC version 201.67.0 (GE Healthcare, Chicago, IL, USA) and was defined as the mean value of longitudinal peak negative strain from 18 apical segments.
- Statistical analysis
- Continuous variables are presented as mean±standard deviation. Categorical variables are expressed as frequencies (percentages). A chi-square test or Student’s t-test was used to compare differences in clinical, laboratory, and echocardiographic variables between men and women. A paired t-test was performed to evaluate longitudinal changes in the parameters at baseline and follow-up. The correlation between changes in metabolic components and LV GLS was evaluated by correlation analysis. Multiple linear regression analysis was performed to investigate the association between the metabolic parameters and myocardial function (GLS) after adjustment for age, BMI, WC, SBP, DBP, FBG, total cholesterol, TG, LDL, and HDL levels. SPSS version 25.0 (IBM, Armonk, NY, USA) was used to perform the statistical analysis. Two-sided P values <0.05 were considered statistically significant.
METHODS
- Baseline clinical, laboratory, and echocardiographic characteristics
- Table 1 presents the baseline characteristics of the study population. Among 191 subjects, the mean age was 56.2±4.4 years, and there were 97 women in the study (50.8%). At baseline, mean BMI, WC, SBP, and DBP were 25.7±3.0 kg/m2, 87.5±8.2 cm, 124.3±15.0 mm Hg, and 76.0±9.8 mm Hg. Mean FBG, TG, and HDL were 99.5±14.2, 155.9±94.2, and 51.5±14.1 mg/dL. Twelve (6.3%) and three (1.5%) subjects were taking antihypertensive and oral hypoglycemic medications, respectively, while 19 (9.9%) subjects were taking statins.
- Mean age, BMI, and SBP were comparable between the sexes, while WC and DBP were increased in men compared to women. The prevalence of underlying cardiovascular diseases was also comparable between men and women. Metabolic laboratory values, including FBG, TG, and HDL, were consistently more impaired, in men than women.
- Table 2 shows the echocardiographic parameters. The mean LVMI, LV EF, and LV GLS were 76.7±14.9 g/cm2, 59.3%±6.3%, and –16.3%±2.2%, respectively. The LVMI, LVEDV, and LVESV were higher in men than in women; however, the LAVI and LV EF were not different between the sexes. Women had higher E/e´, but the difference in e´ velocity between the sexes was not significant. The LV GLS was more impaired in men.
- Longitudinal changes in clinical and laboratory parameters
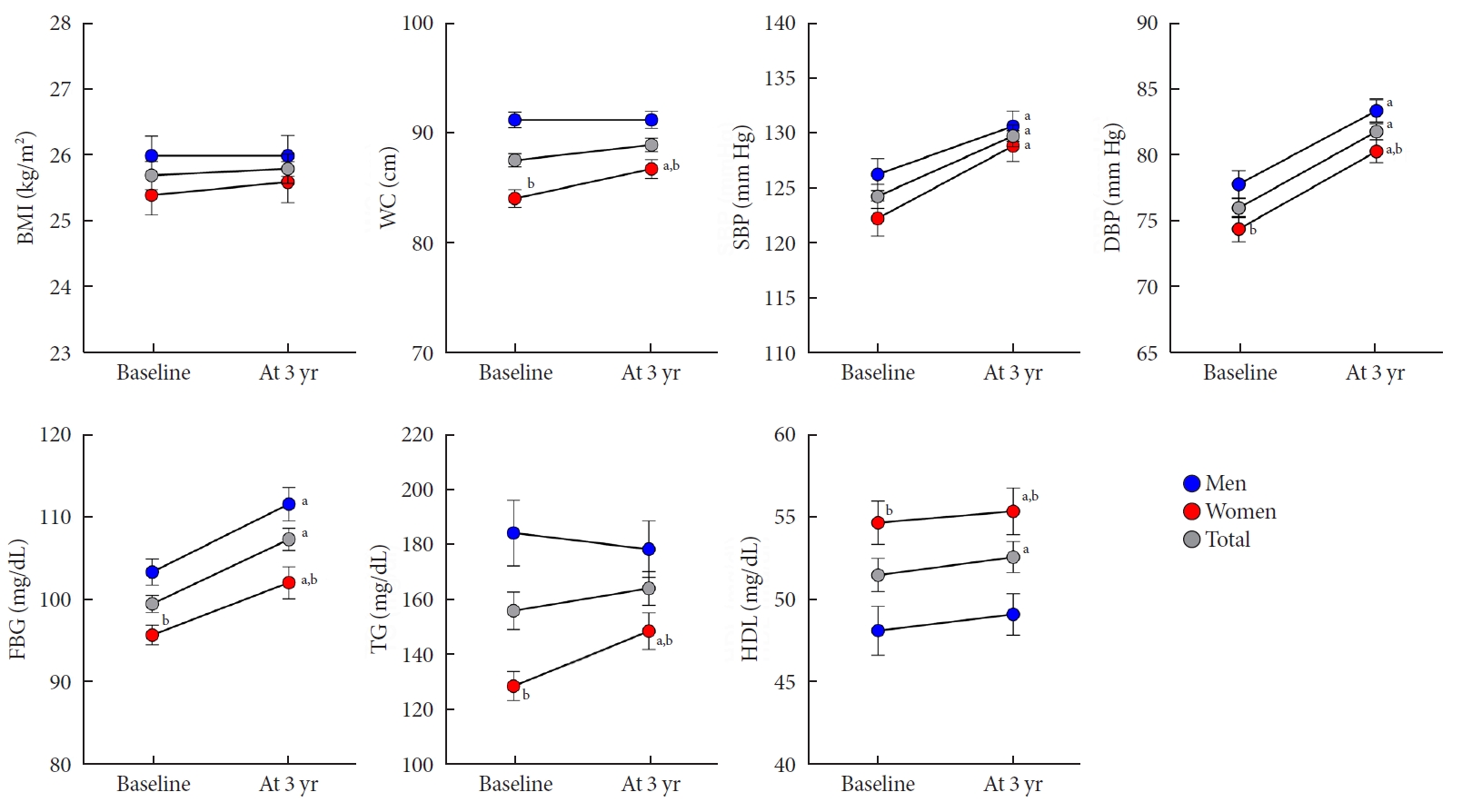
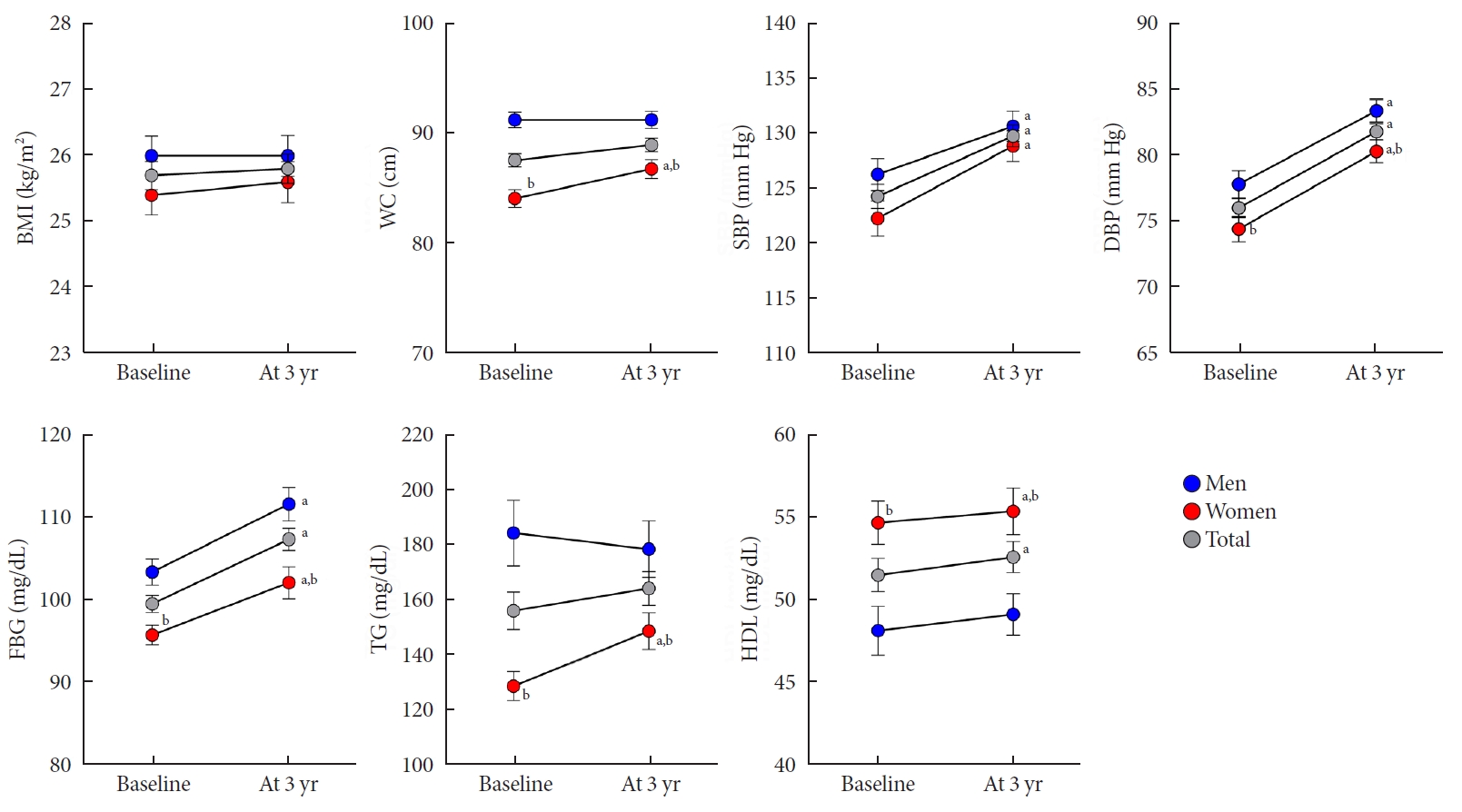
- The median follow-up was 3.4 years (5th to 95th percentile, 3.1 to 3.7). At follow-up, the mean age of the study population was 58.7±4.5 years. Table 1 also shows the clinical and laboratory characteristics at the 3-year follow-up. From baseline to follow-up, BMI, WC, and TG level did not change over time. In contrast, SBP, DBP, FBG, and HDL level increased significantly by 5.6±14.6 mm Hg, 5.8±8.4 mm Hg, 7.8±16.3 mg/dL, and 1.1±11.3 mg/dL, respectively (all P<0.05) (Fig. 1). In the subgroup analysis by sex, the WC, and TG level significantly increased by 2.7±5.4 cm and 21.7±68.5 mg/dL, respectively, only in women (all P<0.05), not in men. However, the WC and TG level was higher in men compared to women at follow-up.
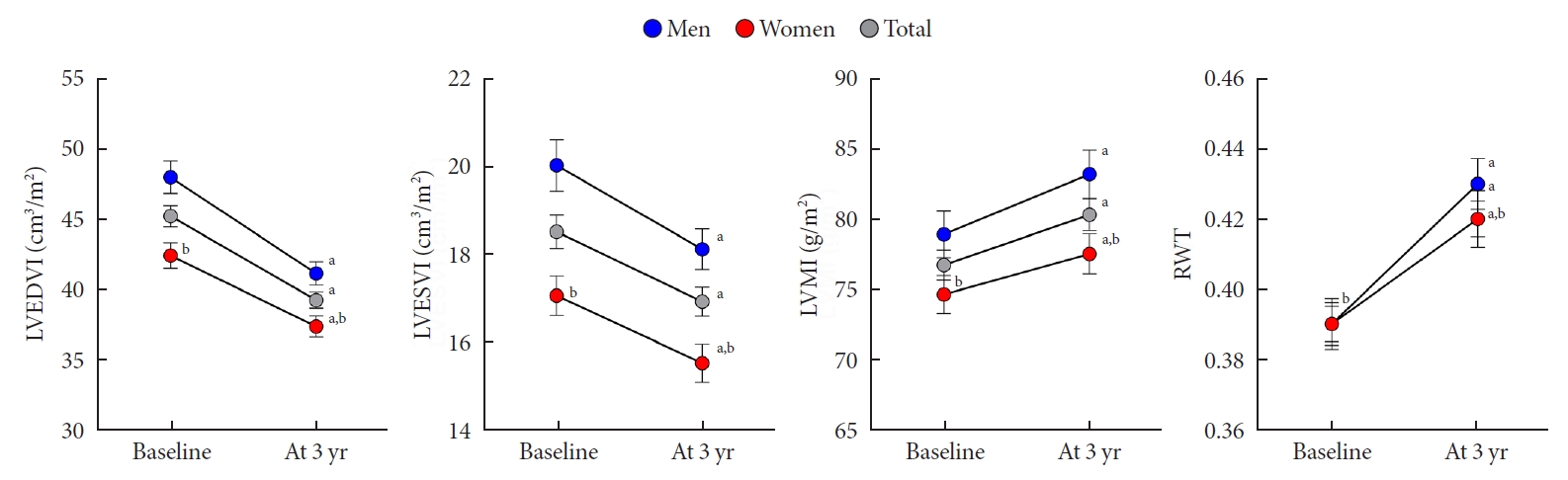
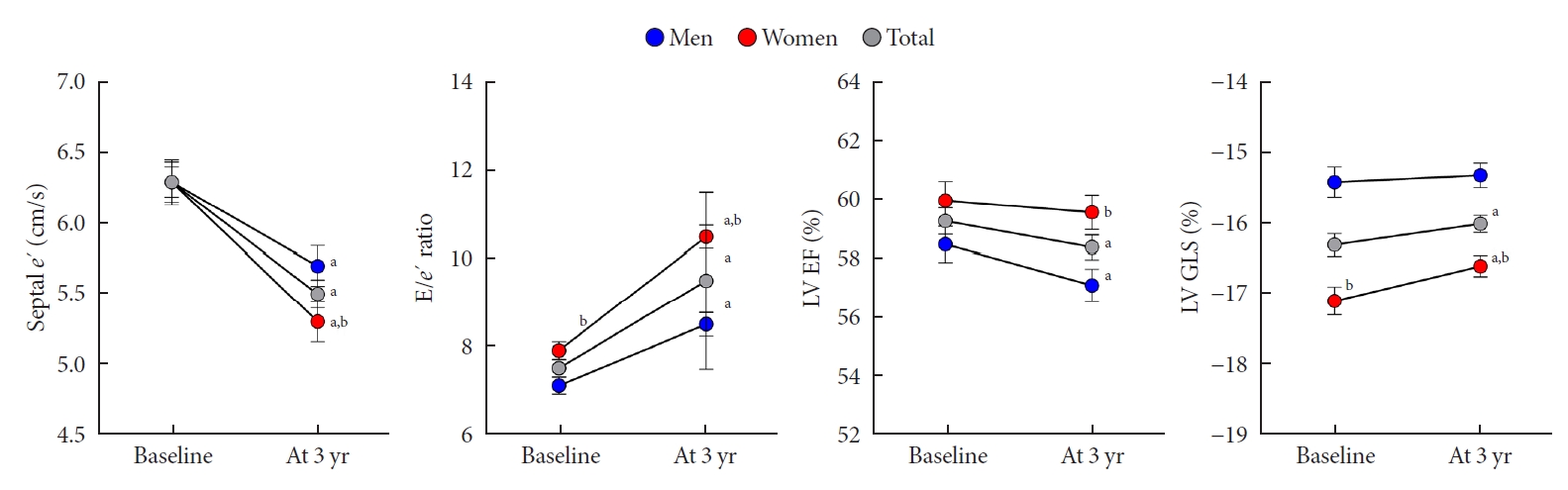
- Longitudinal changes in cardiac geometry and functional parameters
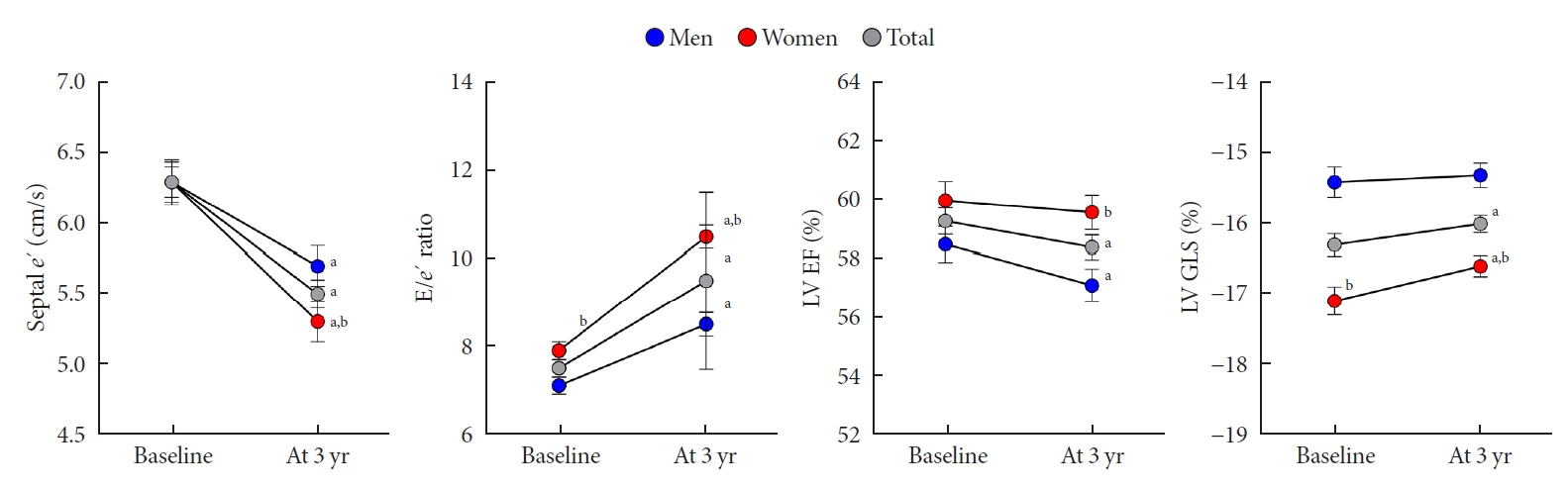
- A comparison of echocardiographic parameters related to cardiac structure and functional remodeling at baseline and follow-up was performed. Cardiac structural remodeling over the 3-year period is characterized by a concentric pattern of increasing RWT and LVMI, and decreasing LVEDV and LVESV (all P<0.05) (Fig. 2). However, no change in the LAVI was observed for all subjects. In both men and women, RWT and LVMI increased, and LVEDV and LVESV decreased over the 3-year period.
- Systolic functional parameters represented by s´ velocity, LV EF, and GLS and diastolic functional parameters represented by e´ and E/e´ ratio tended to be deteriorated throughout the 3-year period (Fig. 3). The s´ velocity, LV EF, the absolute value of LV GLS, and e´ velocity decreased by –1.4±1.6 cm/sec, –2.0%±5.3%, 0.8%±2.4%, and –0.8±1.6 cm/sec, respectively (all P<0.05). The E/e´ ratio increased by 2.1%±2.5%, respectively (P<0.05). In both men and women, all cardiac functional parameters, except the LV GLS, tended to be deteriorated (all P<0.05). The subtle parameter of myocardial deformation, represented by the absolute value of LV GLS, did not change in men; however, this value was significantly reduced in women (P=0.011). Nevertheless, the LV GLS was more impaired in men than in women at follow-up (–15.3±1.7 vs. –16.6±1.5, P<0.001).
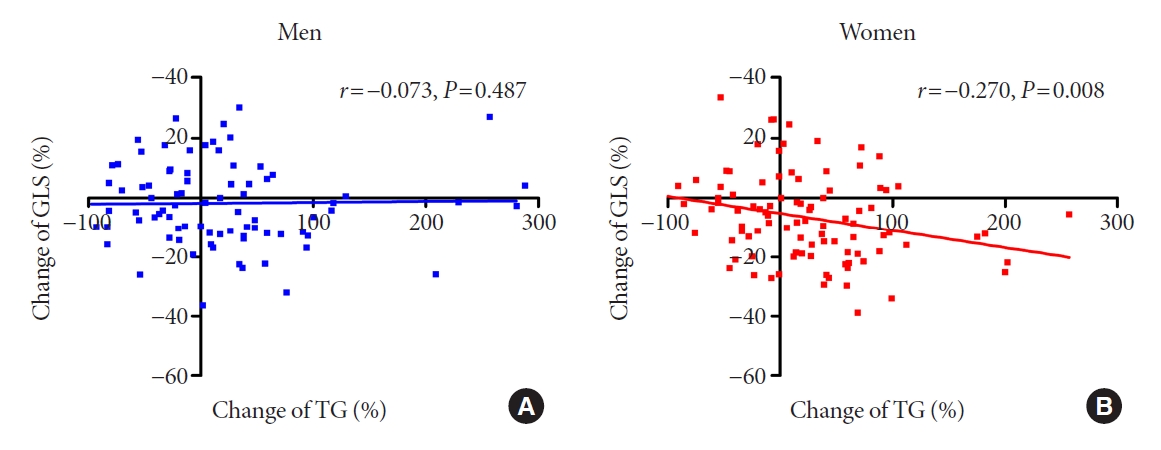
- The association between changes in metabolic profile and cardiac function
- The association between changes in metabolic profile and cardiac function over the 3-year period was analyzed by using multiple linear regression analysis (Table 3). Overall, in our population, the metabolic parameters were not independently related to changes in the LV GLS. In analysis by sex, the change in TG was independently associated with worsening of LV GLS, but only in women (standardized β, –0.309; 95% confidence interval, –0.130 to –0.009; P=0.025). Fig. 4 demonstrates the association between the change in the TG level and LV GLS in men and women.
RESULTS
- To our knowledge, this is the first study to demonstrate sex differences related to longitudinal changes in myocardial function in middle-aged subjects with suspected MetS, but without apparent cardiovascular diseases. Furthermore, we obtained the following results. The values obtained for FBG and BP significantly increased during the 3-year period. Moreover, cardiac structural remodeling was characterized by a concentric pattern and worsened cardiac systolic and diastolic functions over the 3-year period of the study. In subgroup analysis by sex, the WC and TG level were higher in men, and men had worse LV GLS compared to women at baseline. After 3 years, the values of the WC and TG were still higher in men; however, there was a longitudinal increase in the values of WC and TG, but only in women. The LV GLS did not change in men in our study; however, it significantly increased in women. Finally, the change in TG level was both inversely and independently associated with changes in LV GLS in women, but not in men.
- Aging and the myocardium
- Cardiac structural and functional changes progress over time throughout adulthood, and this dynamic process is termed ‘cardiac remodeling’ [18]. The Framingham study demonstrated increasing LV mass and concentricity over both a short-term and long-term period [3,5]. Several longitudinal studies have demonstrated cardiac systolic and diastolic functional deterioration on tracking using tissue Doppler and 2DS echocardiography [2,6]. LV strain assessed by using 2DS echocardiography has recently been reported as a sensitive and useful tool in the evaluation of myocardial function focusing on myocardial deformation [19]. Our previous studies reported that epicardial and visceral adiposity correlated well with myocardial dysfunction as assessed using GLS in a cross-sectional study [14,15]. A community study demonstrated that subclinical myocardial dysfunction as assessed using GLS reflected early myocardial contractile deterioration and independently predicted the development of major cardiovascular events [20]. The results of this study using 2DS echocardiography demonstrated that LV concentric remodeling and dysfunction progressed over a 3-year period in patients with suspected MetS, and these results are consistent with those of previous studies. However, it is notable that the change in cardiac remodeling was recognized only in a 3-year period, which suggests that the myocardium is vulnerable to the aging process as well as to metabolic disturbances in middle-aged subjects.
- Although LV GLS assessed using 2DS echocardiography is a novel and emerging tool, the clinical application of LV GLS requires the definition of a normal range. The Seoul Metabolic Syndrome study enrolled only consecutive participants with MetS. In a meta-analysis of LV GLS, the normal GLS was –19.7% with a narrow 95% confidence interval (–20.4% to –18.9%) [21]. The Korean Society of Echocardiography also suggested a normal value of LV GLS (−20.4%±2.2%) in the healthy Korean population [22]. The subclinical myocardial dysfunction assessed by LV GLS in subjects with MetS was more impaired compared to controls in the Korean single-center study [23]. Compared to the normal value of LV GLS in reference studies, the present study revealed that the mean value of LV GLS (–16.3%±2.2%) in subjects with MetS was more impaired, and LV GLS became more deteriorated during the 3-year follow-up. Our findings, though consistent with the previous study, elaborate on the longitudinal change in subclinical cardiac remodeling assessed by LV GLS in middle-aged subjects with MetS.
- Metabolic parameters and the myocardium
- Metabolic profiles deteriorate with age. The Korean National Health and Nutrition Examination Surveys (KNHANES) revealed that metabolic components were gradually more impaired with aging [24]. When mean WC and TG were compared between groups with 50 to 54 and 55 to 59 years in the KNHANES population, they were not significantly different [24]. The Korean Genome and Epidemiology Study, which is a community-based longitudinal study and included 10,038 adults aged 40 to 69 years, reported that the mean WC increased by 1.71 and 1.85 cm in men and women, respectively, during the 8-year period [25]. Compared to findings from the general population, the progress of metabolic impairment, especially mean WC and TG, over 3 years was remarkable in middle-aged women with MetS in the present study.
- In previous longitudinal studies, higher blood pressure, central obesity, and insulin resistance were significantly associated with cardiac structural and functional remodeling [9,10,26]. MetS is a constellation of various metabolic disturbances, which have multifactorial effects on the myocardium. High blood pressure is related to arterial stiffness and increased cardiac afterload, and central obesity is associated with higher cardiac output and volume overload [27]. Insulin resistance induces extracellular collagen deposition and reactive interstitial fibrosis that lead to myocardial stiffness [28]. Cross sectional studies investigated the impact of TG on cardiac remodeling. In 15 healthy subjects, myocardial TG contents were associated with LV mass and systolic dysfunction [29]. In hypertensive patients, plasma TG contributed to LV hypertrophy and arterial stiffness independently from hormonal and hemodynamic factors [30]. However, there is scarce data regarding whether long-term exposure to high TG is related to cardiac remodeling. In the present study, it is notable that changes in the TG level were negatively and independently associated with cardiac functional remodeling in women.
- Sex differences
- Out study demonstrated a predominant association between TG level and cardiac remodeling in women. However, the pathophysiology of this association is still unclear. The mean age of natural menopause is approximately 50 years. Menopause increases cardiovascular risk burden, and indeed, menopause status is independently associated with the serum lipid profile [31]. Menopause-related increases in TG levels may contribute to this sex difference. With respect to lifestyle factors, the men in our study tended to be more physically active and engage in regular exercise compared to the women. Indeed, active cardiovascular fitness may protect individuals from metabolic disturbances and cardiac remodeling during the transition period from 50 to 60 years of age.
- Clinical implication
- Weight loss is associated with cardiac structure and function, and body weight is a well-known parameter to monitor the effects of medical or surgical intervention [32,33]. In our study, the change in TG level was significantly correlated with LV functional remodeling over a 3-year period. These findings suggest that lifestyle changes targeting TG levels may be associated with beneficial cardiac remodeling in middle-aged subjects.
- Strengths and limitations
- Our study has several considerable merits, including the longitudinal design and the aim of evaluating serial echocardiography using 2DS to track subtle cardiac remodeling. However, our study also has several limitations. In patients without apparent cardiovascular diseases, a large sample size should be used to evaluate longitudinal changes in metabolic disturbances and cardiac remodeling. Although our study had a small sample size, the delicate and subtle parameters associated with cardiac remodeling evaluated by 2DS echocardiography demonstrated significant longitudinal changes in cardiac remodeling and its association with metabolic parameters. Cardiac remodeling is a well-known subclinical status of heart failure; however, during the 3-year follow-up period, there were no new developments, specifically major cardiovascular events including heart failure. Our cohort is an ongoing, prospective study, and we aim to investigate changes in metabolic disturbances and their relationship with cardiovascular events in a follow-up study. In the present study, a healthy control group was not included, and thus, a direct comparison of the metabolic profiles and LV GLS values between subjects with MetS and healthy controls was not available. Further studies are needed to compare the metabolic profiles and LV GLS between subjects with MetS and healthy controls. Finally, our study evaluated sex differences regarding longitudinal changes in metabolic parameters and cardiac remodeling over the transitional period from middle-aged to elderly. The change in hormone status, including the sex hormones, can pose as a potent pathologic mechanism; however, we were unable to evaluate the level of sex hormones in this study. Further studies are needed to evaluate hormonal changes and their impact on cardiac remodeling in middle-aged men and women.
- In middle-aged subjects with suspected MetS, but with no apparent cardiovascular diseases, LV dysfunction tended to progress more in women than men during a 3-year follow-up period. The results of our study suggest that the myocardium in women is more vulnerable to dysmetabolic changes from middle-aged to elderly, which is a transitional period for metabolic disturbances. Sexual dimorphism in the progression of lipid metabolism and central adiposity may accelerate subclinical myocardial dysfunction during this period. Lifestyle changes and medical interventions should be considered to prevent further cardiac dysfunction in middle-aged subjects with suspected MetS, particularly in women.
DISCUSSION
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conception or design: D.S.L., S.M.P.
Acquisition, analysis, or interpretation of data: D.H.C., H.J.J., M.N.K., H.D.K., D.S.L.
Drafting the work or revising: D.H.C., D.S.L., S.M.P
Final approval of the manuscript: S.M.P.
-
FUNDING
This study was supported by a grant from the Seoul Metropolitan Government.
NOTES
-
Acknowledgements
- The authors appreciate the participation of all the subjects in the Seoul Metabolic Syndrome study.
| Variable |
Baseline study |
Follow-up study after 3 years |
||||||
|---|---|---|---|---|---|---|---|---|
| Total (n=191) | Men (n=94) | Women (n=97) | P valuea | Total (n=191) | Men (n=94) | Women (n=97) | P valuea | |
| Age, yr | 56.2±4.4 | 56.2±4.7 | 56.2±4.1 | 0.993 | 58.7±4.5 | 58.7±4.6 | 58.8±4.3 | 0.861 |
| BMI, kg/m2 | 25.7±3.0 | 26.0±2.9 | 25.4±3.0 | 0.186 | 25.8±3.1 | 26.0±3.0 | 25.6±3.1 | 0.390 |
| WC, cm | 87.5±8.2 | 91.2±6.8 | 84.0±8.0 | <0.001 | 88.9±8.4 | 91.2±7.6 | 86.7±8.5 | <0.001 |
| WHR | 0.87±0.05 | 0.90±0.04 | 0.85±0.05 | <0.001 | 0.92±0.06 | 0.94±0.05 | 0.90±0.06 | <0.001 |
| SBP, mm Hg | 124.3±15.0 | 126.3±14.1 | 122.3±15.7 | 0.066 | 129.8±13.7 | 130.7±13.6 | 128.9±13.8 | 0.372 |
| DBP, mm Hg | 76.0±9.8 | 77.8±10.0 | 74.4±9.4 | 0.015 | 81.8±8.5 | 83.4±8.4 | 80.3±8.5 | 0.010 |
| PP, mm Hg | 48.2±9.7 | 48.5±8.7 | 47.9±10.7 | 0.684 | 48.0±9.9 | 47.3±9.5 | 48.7±10.4 | 0.341 |
| Underlying diseases | ||||||||
| HTN | 12 (6.3) | 4 (4.3) | 8 (8.8) | 0.367 | 30 (15.7) | 13 (13.4) | 17 (18.1) | 0.245 |
| DM | 3 (1.5) | 1 (1.1) | 2 (2.2) | 0.598 | 16 (8.4) | 6 (6.2) | 10 (10.6) | 0.198 |
| Dyslipidemia | 19 (9.9) | 13 (14.0) | 6 (6.7) | 0.105 | 48 (25.1) | 32 (33.0) | 16 (17.0) | 0.008 |
| Lifestyle | ||||||||
| Current smoker | 24 (12.7) | 24 (25.8) | 0 (0.0) | < 0.001 | 22 (11.5) | 22 (23.4) | 0 (0.0) | <0.001 |
| Alcohol intake | 117 (61.9) | 75 (80.6) | 42 (43.8) | < 0.001 | 103 (53.9) | 75 (79.8) | 28 (28.9) | <0.001 |
| Regular exercise | 128 (67.4) | 68 (73.1) | 60 (61.9) | 0.067 | 104 (54.5) | 55 (58.5) | 49 (50.5) | 0.168 |
| Laboratory parameters | ||||||||
| FBG, mg/dL | 99.5±14.2 | 103.4±15.4 | 95.7±11.8 | <0.001 | 107.4±18.7 | 111.7±20.0 | 102.1±19.4 | 0.001 |
| TC, mg/dL | 198.3±31.2 | 190.7±27.9 | 205.7±32.6 | 0.001 | 190.9±36.8 | 183.6±32.8 | 198.1±39.3 | 0.007 |
| TG, mg/dL | 155.9±94.2 | 184.4±116.3 | 128.2±53.6 | <0.001 | 164.1±85.1 | 178.5±100.2 | 148.4±66.0 | 0.015 |
| HDL, mg/dL | 51.5±14.1 | 48.1±14.5 | 54.7±13.0 | 0.001 | 52.6±13.1 | 49.1±12.3 | 55.4±14.1 | 0.001 |
| TG/HDL ratio | 3.50±3.52 | 4.47±4.60 | 2.56±1.52 | <0.001 | 3.5±2.8 | 4.09±3.44 | 2.94±1.76 | 0.004 |
Values are presented as mean±standard deviation or number (%).
BMI, body mass index; WC, waist circumference; WHR, waist hip ratio; SBP, systolic blood pressure; DBP, diastolic blood pressure; PP, pulse pressure; HTN, hypertension; DM, diabetes mellitus; FBG, fasting blood glucose; TC, total cholesterol; TG, triglycerides; HDL, high-density lipoprotein.
a P value for comparison between men and women.
Values are presented as mean±standard deviation.
LVEDD, left ventricular end diastolic dimension; LVESD, left ventricular end systolic dimension; RWT, relative wall thickness; LVMI, left ventricular mass index; LAVI, left atrial volume index; LVEDVI, left ventricular end diastolic volume index; LVESVI, left ventricular end systolic volume index; LV, left ventricular; EF, ejection fraction; E, early diastolic mitral inflow velocity; DT, deceleration time; e´, early mitral tissue velocity; s´, systolic mitral tissue velocity; GLS, global longitudinal strain.
a P value for comparison between men and women.
LV, left ventricular; GLS, global longitudinal strain; β, regression coefficient; CI, confidence interval; BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; DBP, diastolic blood pressure; TC, total cholesterol; TG, triglycerides; LDL, low-density lipoprotein; HDL, high-density lipoprotein.
- 1. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics: 2019 update. A report from the American Heart Association. Circulation 2019;139:e56-528.PubMed
- 2. Kuznetsova T, Thijs L, Knez J, Cauwenberghs N, Petit T, Gu YM, et al. Longitudinal changes in left ventricular diastolic function in a general population. Circ Cardiovasc Imaging 2015;8:e002882.ArticlePubMed
- 3. Cheng S, Xanthakis V, Sullivan LM, Lieb W, Massaro J, Aragam J, et al. Correlates of echocardiographic indices of cardiac remodeling over the adult life course: longitudinal observations from the Framingham Heart Study. Circulation 2010;122:570-8.ArticlePubMedPMC
- 4. Gates PE, Gentile CL, Seals DR, Christou DD. Adiposity contributes to differences in left ventricular structure and diastolic function with age in healthy men. J Clin Endocrinol Metab 2003;88:4884-90.ArticlePubMedPDF
- 5. Lieb W, Xanthakis V, Sullivan LM, Aragam J, Pencina MJ, Larson MG, et al. Longitudinal tracking of left ventricular mass over the adult life course: clinical correlates of short- and long-term change in the Framingham offspring study. Circulation 2009;119:3085-92.ArticlePubMedPMC
- 6. Yang H, Huynh QL, Venn AJ, Dwyer T, Marwick TH. Associations of childhood and adult obesity with left ventricular structure and function. Int J Obes (Lond) 2017;41:560-8.ArticlePubMedPDF
- 7. Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, et al. 2016 ESC guidelines for the diagnosis and treatment of acute and chronic heart failure: the task force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC). Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur J Heart Fail 2016;18:891-975.ArticlePubMedPDF
- 8. Lee HY, Oh BH. Paradigm shifts of heart failure therapy: do we need another paradigm? Int J Heart Fail 2020;2:145-56.ArticlePubMedPMCPDF
- 9. Lieb W, Gona P, Larson MG, Aragam J, Zile MR, Cheng S, et al. The natural history of left ventricular geometry in the community: clinical correlates and prognostic significance of change in LV geometric pattern. JACC Cardiovasc Imaging 2014;7:870-8.PubMedPMC
- 10. Kishi S, Gidding SS, Reis JP, Colangelo LA, Venkatesh BA, Armstrong AC, et al. Association of insulin resistance and glycemic metabolic abnormalities with LV structure and function in middle age: the CARDIA Study. JACC Cardiovasc Imaging 2017;10:105-14.PubMed
- 11. Huh JH, Kang DR, Jang JY, Shin JH, Kim JY, Choi S, et al. Metabolic syndrome epidemic among Korean adults: Korean survey of Cardiometabolic Syndrome (2018). Atherosclerosis 2018;277:47-52.ArticlePubMed
- 12. Matthews KA, Crawford SL, Chae CU, Everson-Rose SA, Sowers MF, Sternfeld B, et al. Are changes in cardiovascular disease risk factors in midlife women due to chronological aging or to the menopausal transition? J Am Coll Cardiol 2009;54:2366-73.ArticlePubMedPMC
- 13. Kim KJ, Cho HJ, Kim MS, Kang J, Kim KH, Kim D, et al. Focused update of 2016 Korean Society of Heart Failure guidelines for the management of chronic heart failure. Int J Heart Fail 2019;1:4-24.ArticlePubMedPMCPDF
- 14. Cho DH, Joo HJ, Kim MN, Lim DS, Shim WJ, Park SM. Association between epicardial adipose tissue, high-sensitivity C-reactive protein and myocardial dysfunction in middle-aged men with suspected metabolic syndrome. Cardiovasc Diabetol 2018;17:95.ArticlePubMedPMCPDF
- 15. Cho DH, Kim MN, Joo HJ, Shim WJ, Lim DS, Park SM. Visceral obesity, but not central obesity, is associated with cardiac remodeling in subjects with suspected metabolic syndrome. Nutr Metab Cardiovasc Dis 2019;29:360-6.ArticlePubMed
- 16. Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. J Am Soc Echocardiogr 2015;28:1-39.ArticlePubMed
- 17. Nagueh SF, Smiseth OA, Appleton CP, Byrd BF 3rd, Dokainish H, Edvardsen T, et al. Recommendations for the evaluation of left ventricular diastolic function by echocardiography: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2016;17:1321-60.ArticlePubMed
- 18. Cohn JN, Ferrari R, Sharpe N. Cardiac remodeling: concepts and clinical implications. A consensus paper from an international forum on cardiac remodeling. Behalf of an international forum on cardiac remodeling. J Am Coll Cardiol 2000;35:569-82.PubMed
- 19. Geyer H, Caracciolo G, Abe H, Wilansky S, Carerj S, Gentile F, et al. Assessment of myocardial mechanics using speckle tracking echocardiography: fundamentals and clinical applications. J Am Soc Echocardiogr 2010;23:351-69.ArticlePubMed
- 20. Russo C, Jin Z, Elkind MS, Rundek T, Homma S, Sacco RL, et al. Prevalence and prognostic value of subclinical left ventricular systolic dysfunction by global longitudinal strain in a community-based cohort. Eur J Heart Fail 2014;16:1301-9.ArticlePubMed
- 21. Yingchoncharoen T, Agarwal S, Popovic ZB, Marwick TH. Normal ranges of left ventricular strain: a meta-analysis. J Am Soc Echocardiogr 2013;26:185-91.ArticlePubMed
- 22. Park JH, Lee JH, Lee SY, Choi JO, Shin MS, Kim MJ, et al. Normal 2-dimensional strain values of the left ventricle: a substudy of the normal echocardiographic measurements in Korean population study. J Cardiovasc Ultrasound 2016;24:285-93.ArticlePubMedPMCPDF
- 23. Lee HJ, Kim HL, Lim WH, Seo JB, Kim SH, Zo JH, et al. Subclinical alterations in left ventricular structure and function according to obesity and metabolic health status. PLoS One 2019;14:e0222118.ArticlePubMedPMC
- 24. Division of Health Policy; Ministry of Health and Welfare. Korea Health Statistics 2018: Korea National Health and Nutrition Examination Survey (KNHANES VII-3). Osong: Ministry of Health and Welfare; 2019.
- 25. Son IH, Han YH, Hyun T. Changes in weight, waist circumference, prevalence of obesity, and dietary factors associated with weight gain over 8 years in Korean adults: longitudinal data from the Korean Genome and Epidemiology Study. J Nutr Health 2017;50:336-49.ArticlePDF
- 26. van den Hurk K, Alssema M, Kamp O, Henry RM, Stehouwer CD, Smulders YM, et al. Independent associations of glucose status and arterial stiffness with left ventricular diastolic dysfunction: an 8-year follow-up of the Hoorn Study. Diabetes Care 2012;35:1258-64.PubMedPMC
- 27. Krzesinski P, Stanczyk A, Piotrowicz K, Gielerak G, Uziebto-Zyczkowska B, Skrobowski A. Abdominal obesity and hypertension: a double burden to the heart. Hypertens Res 2016;39:349-55.ArticlePubMedPDF
- 28. Mewton N, Liu CY, Croisille P, Bluemke D, Lima JA. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J Am Coll Cardiol 2011;57:891-903.ArticlePubMedPMC
- 29. Szczepaniak LS, Dobbins RL, Metzger GJ, Sartoni-D’Ambrosia G, Arbique D, Vongpatanasin W, et al. Myocardial triglycerides and systolic function in humans: in vivo evaluation by localized proton spectroscopy and cardiac imaging. Magn Reson Med 2003;49:417-23.ArticlePubMed
- 30. Legedz L, Bricca G, Lantelme P, Rial MO, Champomier P, Vincent M, et al. Insulin resistance and plasma triglyceride level are differently related to cardiac hypertrophy and arterial stiffening in hypertensive subjects. Vasc Health Risk Manag 2006;2:485-90.ArticlePubMedPMC
- 31. Park HA, Park JK, Park SA, Lee JS. Age, menopause, and cardiovascular risk factors among Korean middle-aged women: the 2005 Korea National Health and Nutrition Examination Survey. J Womens Health (Larchmt) 2010;19:869-76.ArticlePubMed
- 32. Shin SH, Lee YJ, Heo YS, Park SD, Kwon SW, Woo SI, et al. Beneficial effects of bariatric surgery on cardiac structure and function in obesity. Obes Surg 2017;27:620-5.ArticlePubMedPDF
- 33. Shah RV, Murthy VL, Abbasi SA, Eng J, Wu C, Ouyang P, et al. Weight loss and progressive left ventricular remodelling: the Multi-Ethnic Study of Atherosclerosis (MESA). Eur J Prev Cardiol 2015;22:1408-18.ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations

- Positive additive interaction effects of age, sex, obesity, and metabolic syndrome on left ventricular dysfunction
Dan Zhou, Zhongwen Ye, Zhiqiang Nie, Chaolei Chen, Songyuan Luo, Mengqi Yan, Jiabin Wang, Yingqing Feng
Journal of Diabetes.2024;[Epub] CrossRef - Lung-Heart Outcomes and Mortality through the 2020 COVID-19 Pandemic in a Prospective Cohort of Breast Cancer Radiotherapy Patients
Vincent Vinh-Hung, Olena Gorobets, Nele Adriaenssens, Hilde Van Parijs, Guy Storme, Dirk Verellen, Nam P. Nguyen, Nicolas Magne, Mark De Ridder
Cancers.2022; 14(24): 6241. CrossRef

 KDA
KDA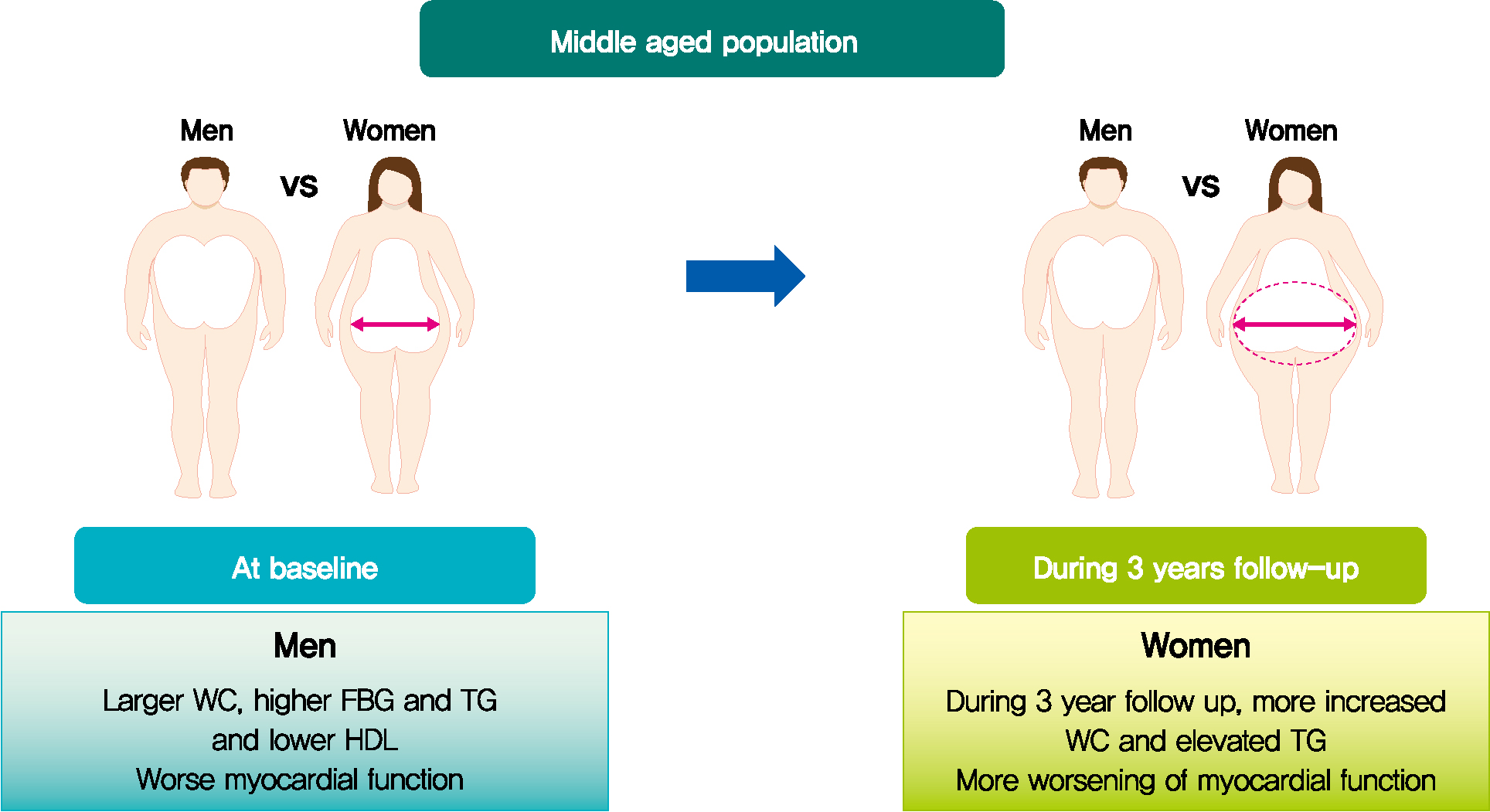
 PubReader
PubReader ePub Link
ePub Link Cite
Cite