
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Guideline/Fact Sheet
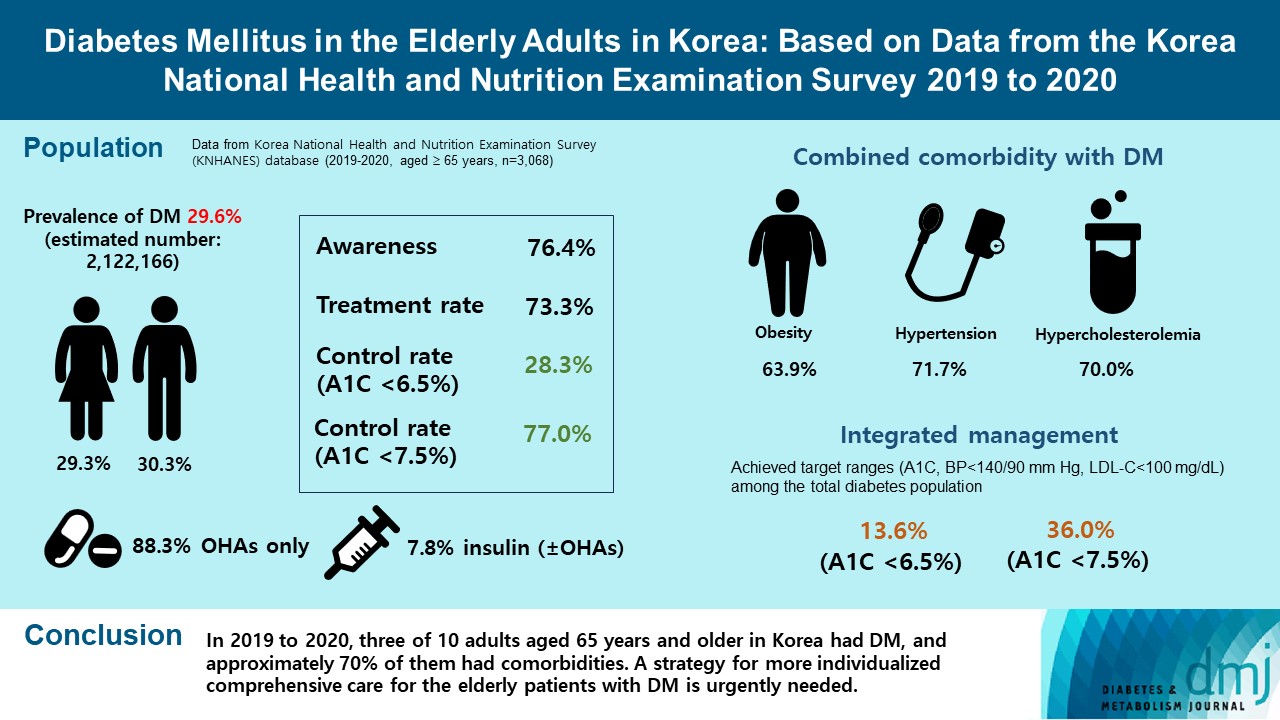
- Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
- Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
- Diabetes Metab J. 2023;47(5):643-652. Published online August 7, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0041
- 2,266 View
- 208 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We evaluated the prevalence and management of diabetes mellitus (DM) in elderly Korean patients based on data from the Korea National Health and Nutrition Examination Survey (KNHANES).
Methods
A total of 3,068 adults aged 65 years and older (19.8% of total population) were analyzed using KNHANES from 2019 to 2020. Prevalence, awareness, treatment, and control rates, and comorbidities were analyzed. Lifestyle behaviors and energy intake were also measured.
Results
The prevalence of DM and prediabetes was 29.6% and 50.5%, respectively. The awareness, treatment and control rates were 76.4%, 73.3%, and 28.3%, respectively. The control rate was 77.0% if A1C <7.5% criteria was used. The mean A1C value of individuals with known DM was 7.1%, and 14.5% of the known DM patients had A1C ≥8.0%. Abdominal obesity, hypertension, and hypercholesterolemia were combined with DM in 63.9%, 71.7%, and 70.7%, respectively, and the rate of integrated management was 36.0% (A1C <7.5% criteria). A total of 40.1% of those with DM walked regularly. The percentage of energy intake from carbohydrates was higher in those with DM than in those without DM (P=0.044), while those of fat (P=0.003) and protein (P=0.025) were lower in those with DM than in those without DM in women.
Conclusion
In 2019 to 2020, three of 10 adults aged 65 years and older in Korea had DM, and approximately 70% of them had comorbidities. A strategy for more individualized comprehensive care for the elderly patients with DM is urgently needed. -
Citations
Citations to this article as recorded by- Association Between High Blood Folate Levels and Glaucoma in a Representative Korean Population
Ji Young Lee, Jin A. Choi, Sung Pyo Park, Donghyun Jee
Investigative Opthalmology & Visual Science.2024; 65(1): 6. CrossRef - The Growing Challenge of Diabetes Management in an Aging Society
Seung-Hwan Lee
Diabetes & Metabolism Journal.2023; 47(5): 630. CrossRef
- Association Between High Blood Folate Levels and Glaucoma in a Representative Korean Population
- Basic Research
- Regulation of Cellular Senescence in Type 2 Diabetes Mellitus: From Mechanisms to Clinical Applications
- Kanako Iwasaki, Cristian Abarca, Cristina Aguayo-Mazzucato
- Diabetes Metab J. 2023;47(4):441-453. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0416

- 4,691 View
- 417 Download
- 3 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Cellular senescence is accelerated by hyperglycemia through multiple pathways. Therefore, senescence is an important cellular mechanism to consider in the pathophysiology of type 2 diabetes mellitus (T2DM) and an additional therapeutic target. The use of drugs that remove senescent cells has led to improvements in blood glucose levels and diabetic complications in animal studies. Although the removal of senescent cells is a promising approach for the treatment of T2DM, two main challenges limit its clinical application: the molecular basis of cellular senescence in each organ is yet to be understood, and the specific effect of removing senescent cells in each organ has to be determined. This review aims to discuss future applications of targeting senescence as a therapeutic option in T2DM and elucidate the characteristics of cellular senescence and senescence-associated secretory phenotype in the tissues important for regulating glucose levels: pancreas, liver, adipocytes, and skeletal muscle.
-
Citations
Citations to this article as recorded by- Amide Alkaloids as Privileged Sources of Senomodulators for Therapeutic Purposes in Age-Related Diseases
Mazzarine Dotou, Aurore L’honoré, Roba Moumné, Chahrazade El Amri
Journal of Natural Products.2024; 87(3): 617. CrossRef - Study on the Pathogenesis of Cell Senescence in Non-Alcoholic Fatty Liver
丽媛 黄
Medical Diagnosis.2024; 14(01): 76. CrossRef - Senescent adipocytes and type 2 diabetes – current knowledge and perspective concepts
Weronika Kruczkowska, Julia Gałęziewska, Mateusz Kciuk, Adrianna Gielecińska, Elżbieta Płuciennik, Zbigniew Pasieka, Lin-Yong Zhao, Yi-Jin Yu, Damian Kołat, Żaneta Kałuzińska-Kołat
Biomolecular Concepts.2024;[Epub] CrossRef - The Effect of Long-Term Passage on Porcine SMCs’ Function and the Improvement of TGF-β1 on Porcine SMCs’ Secretory Function in Late Passage
Yan-Yan Zheng, Ze-Nan Hu, Zheng Liu, Yi-Chen Jiang, Ren-Peng Guo, Shi-Jie Ding, Guang-Hong Zhou
Foods.2023; 12(14): 2682. CrossRef - Exploring the Relationship between Cellular Senescence Markers and Aging-Related Diseases
怡 罗
Advances in Clinical Medicine.2023; 13(08): 12298. CrossRef
- Amide Alkaloids as Privileged Sources of Senomodulators for Therapeutic Purposes in Age-Related Diseases
- Guideline/Fact Sheet
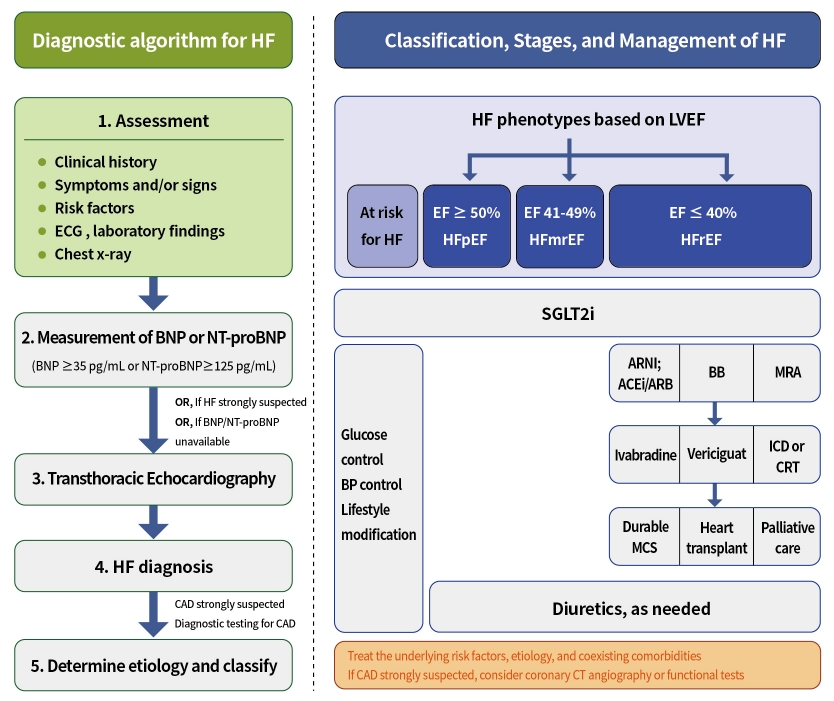
- Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
- Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon, The Committee of Clinical Practice Guidelines, Korean Diabetes Association and Committee of Clinical Practice Guidelines, Korean Society of Heart Failure
- Diabetes Metab J. 2023;47(1):10-26. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0420
- 4,340 View
- 411 Download
- 4 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Diabetes mellitus is a major risk factor for the development of heart failure. Furthermore, the prognosis of heart failure is worse in patients with diabetes mellitus than in those without it. Therefore, early diagnosis and proper management of heart failure in patients with diabetes mellitus are important. This review discusses the current criteria for diagnosis and screening tools for heart failure and the currently recommended pharmacological therapies for heart failure. We also highlight the effects of anti-diabetic medications on heart failure.
-
Citations
Citations to this article as recorded by- A Multicenter, Randomized, Open-Label Study to Compare the Effects of Gemigliptin Add-on or Escalation of Metformin Dose on Glycemic Control and Safety in Patients with Inadequately Controlled Type 2 Diabetes Mellitus Treated with Metformin and SGLT-2 Inh
Hae Jin Kim, Jung Hyun Noh, Min Kyong Moon, Sung Hee Choi, Seung-Hyun Ko, Eun-Jung Rhee, Kyu Yeon Hur, In-Kyung Jeong, Mark Yorek
Journal of Diabetes Research.2024; 2024: 1. CrossRef - Comparison of the effects of gemigliptin versus glimepiride on cardiac function in patients with type 2 diabetes uncontrolled with metformin: The gemi‐heart study
Seung Min Chung, Jun Sung Moon, Jun Hwa Hong, In‐Chang Hwang, Soo Lim
Diabetes, Obesity and Metabolism.2023; 25(8): 2181. CrossRef - Optimization of guideline-directed medical treatment for heart failure patients with reduced ejection fraction
Minjung Bak, Jin-Oh Choi
The Korean Journal of Internal Medicine.2023; 38(5): 595. CrossRef
- A Multicenter, Randomized, Open-Label Study to Compare the Effects of Gemigliptin Add-on or Escalation of Metformin Dose on Glycemic Control and Safety in Patients with Inadequately Controlled Type 2 Diabetes Mellitus Treated with Metformin and SGLT-2 Inh
- Pathophysiology
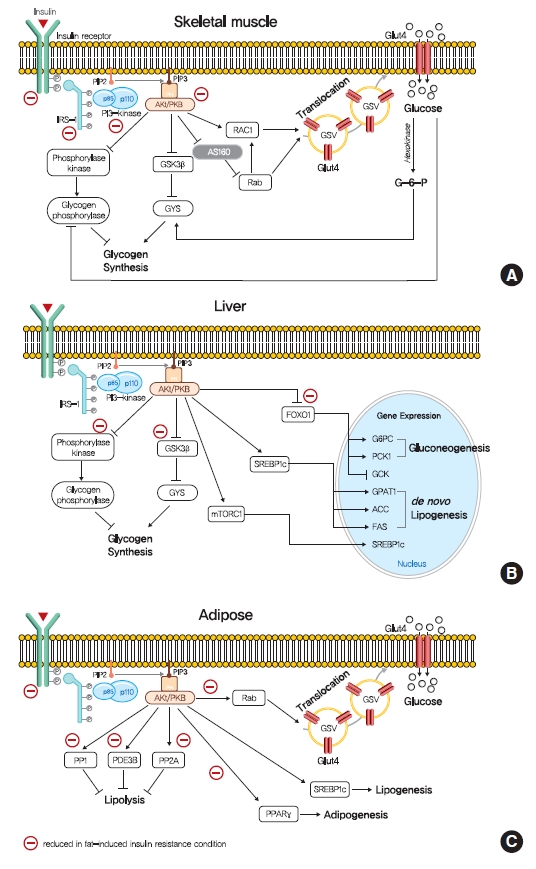
- Insulin Resistance: From Mechanisms to Therapeutic Strategies
- Shin-Hae Lee, Shi-Young Park, Cheol Soo Choi
- Diabetes Metab J. 2022;46(1):15-37. Published online December 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0280
- 30,270 View
- 2,648 Download
- 158 Web of Science
- 191 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Insulin resistance is the pivotal pathogenic component of many metabolic diseases, including type 2 diabetes mellitus, and is defined as a state of reduced responsiveness of insulin-targeting tissues to physiological levels of insulin. Although the underlying mechanism of insulin resistance is not fully understood, several credible theories have been proposed. In this review, we summarize the functions of insulin in glucose metabolism in typical metabolic tissues and describe the mechanisms proposed to underlie insulin resistance, that is, ectopic lipid accumulation in liver and skeletal muscle, endoplasmic reticulum stress, and inflammation. In addition, we suggest potential therapeutic strategies for addressing insulin resistance.
-
Citations
Citations to this article as recorded by- Diabetic Encephalopathy: Role of Oxidative and Nitrosative Factors in Type 2 Diabetes
Debashree Mazumdar, Santosh Singh
Indian Journal of Clinical Biochemistry.2024; 39(1): 3. CrossRef - Materials and structure of polysaccharide-based delivery carriers for oral insulin: A review
Xinran Wang, Hongnan Sun, Taihua Mu
Carbohydrate Polymers.2024; 323: 121364. CrossRef - β-Thalassemia and Diabetes Mellitus: Current State and Future
Directions
Jalal Taneera, Eglal Mahgoub, Reem Qannita, Ayah Alalami, Ola Al Shehadat, Mona Youssef, Ayah Dib, Alaa Al Hajji, Amani Al Hajji, Fatheya Al-Khaja, Hany Dewedar, Mawieh Hamad
Hormone and Metabolic Research.2024; 56(04): 272. CrossRef - Mulberry leaf multi-components exert hypoglycemic effects through regulation of the PI-3K/Akt insulin signaling pathway in type 2 diabetic rats
Yue Zhang, Liang Li, Tao Chai, Han Xu, Hong-yan Du, Yan Jiang
Journal of Ethnopharmacology.2024; 319: 117307. CrossRef - Thyroid cancer and insulin resistance
Gabriela Brenta, Fernando Di Fermo
Reviews in Endocrine and Metabolic Disorders.2024; 25(1): 19. CrossRef - Comparative profiling of gut microbiota and metabolome in diet-induced obese and insulin-resistant C57BL/6J mice
Hobby Aggarwal, Jyoti Gautam, Deepika Kumari, Sonu Kumar Gupta, Sneh Bajpai, Kartikey Chaturvedi, Yashwant Kumar, Madhu Dikshit
Biochimica et Biophysica Acta (BBA) - Molecular Cell Research.2024; 1871(2): 119643. CrossRef - CD248 promotes insulin resistance by binding to the insulin receptor and dampening its insulin-induced autophosphorylation
Patricia O. Benedet, Nooshin S. Safikhan, Maria J. Pereira, Bryan M. Lum, José Diego Botezelli, Cheng-Hsiang Kuo, Hua-Lin Wu, Barbara P. Craddock, W. Todd Miller, Jan W. Eriksson, Jessica T.Y. Yue, Edward M. Conway
eBioMedicine.2024; 99: 104906. CrossRef - The Antiobesity Effects and Potential Mechanisms of Theaflavins
Yi Fang, Jun Wang, Yu Cao, Wenrui Liu, Lianxiang Duan, Jing Hu, Jinghua Peng
Journal of Medicinal Food.2024; 27(1): 1. CrossRef - The role of zinc finger proteins in the fate determination of mesenchymal stem cells during osteogenic and adipogenic differentiation
Bolun Li, Shibo Liu, Ze He, En Luo, Hanghang Liu
The International Journal of Biochemistry & Cell Biology.2024; 167: 106507. CrossRef - Gentianella turkestanorum (Gand.) Holub, a Chinese Herbal Medicine that can Alleviate T2DM in Db/db Mice, and its Active Mechanism of Action
Ying Wei, Jiaxin Sun, Liya Su, Tunhai Xu
Pharmacognosy Magazine.2024; 20(2): 646. CrossRef - Hyperglycemia affects axial signs in patients with Parkinson’s disease through mechanisms of insulin resistance or non-insulin resistance
Ruidan Wang, Zhaohui Jin, Qiaoxia Zhen, Lin Qi, Cui Liu, Ping Wang, Yonghong Liu, Jinping Fang, Yanjun Liu, Yuan Su, Yixuan Wang, Detao Meng, Hongjiao Yan, Yi Zhen, Zhenzhen Li, Boyan Fang
Neurological Sciences.2024; 45(5): 2011. CrossRef - Insulin resistance: Risk factors, diagnostic approaches and mathematical models for clinical practice, epidemiological studies, and beyond
Janusz Krzymien, Piotr Ladyzynski
Biocybernetics and Biomedical Engineering.2024; 44(1): 55. CrossRef - Effects of silybin supplementation on growth performance, serum indexes and liver transcriptome of Peking ducks
Ziyue Zhang, Bozhi Shi, Xueze Lv, Yingchao Dong, Lei Li, Zhaofei Xia
Frontiers in Veterinary Science.2024;[Epub] CrossRef - Effects of Consuming Beverages Sweetened with Fructose, Glucose, High-Fructose Corn Syrup, Sucrose, or Aspartame on OGTT-Derived Indices of Insulin Sensitivity in Young Adults
Bettina Hieronimus, Valentina Medici, Vivien Lee, Marinelle V. Nunez, Desiree M. Sigala, Andrew A. Bremer, Chad L. Cox, Nancy L. Keim, Jean-Marc Schwarz, Giovanni Pacini, Andrea Tura, Peter J. Havel, Kimber L. Stanhope
Nutrients.2024; 16(1): 151. CrossRef - Association Between Insulin Resistance Markers and Poor Prognosis in Patients With Acute Ischemic Stroke After Intravenous Thrombolysis
Haimei Liu, Denglu Liu, Peng Zuo
The Neurologist.2024;[Epub] CrossRef - Interplay of Angiotensin Peptides, Vasopressin, and Insulin in the Heart: Experimental and Clinical Evidence of Altered Interactions in Obesity and Diabetes Mellitus
Ewa Szczepanska-Sadowska
International Journal of Molecular Sciences.2024; 25(2): 1310. CrossRef - High-Density Lipoprotein Is Located Alongside Insulin in the Islets of Langerhans of Normal and Rodent Models of Diabetes
Sahar Mohsin, Haba Elabadlah, Mariam K. Alotaiba, Suhail AlAmry, Shamma J. Almehairbi, Maha M. K. Harara, Aisha M. H. Almuhsin, Saeed Tariq, Frank Christopher Howarth, Ernest A. Adeghate
Nutrients.2024; 16(2): 313. CrossRef - Sweet triterpenoid glycoside from Cyclocarya paliurus ameliorates obesity-induced insulin resistance through inhibiting the TLR4/NF-κB/NLRP3 inflammatory pathway
Jie Li, Junyu He, Haibo He, Xiao Wang, Shuran Zhang, Yumin He, Jihong Zhang, Chengfu Yuan, HongWu Wang, Daoxiang Xu, Chaowang Pan, Huifan Yu, Kun Zou
Current Research in Food Science.2024; 8: 100677. CrossRef - Effect of supplementation with probiotics or synbiotics on cardiovascular risk factors in patients with metabolic syndrome: a systematic review and meta-analysis of randomized clinical trials
TingRui Chen, Jing Wang, ZeKun Liu, Fei Gao
Frontiers in Endocrinology.2024;[Epub] CrossRef - Diabetes mellitus progression in β-thalassaemia major patients: The impact of iron overload
Eglal Omer Mahgoub, Reem Qannita, Ayah Alalami, Ola Al Shehadat, Rabah Al Mahmoud, Ayah Dib, Alaa Al Hajji, Amani Al Hajji, Fatheya Al Khaja, Hany Dewedar, Mawieh Hamad, Jalal Taneera
Advances in Biomedical and Health Sciences.2024; 3(1): 5. CrossRef - Dietary Tomato Pectin Attenuates Hepatic Insulin Resistance and Inflammation in High-Fat-Diet Mice by Regulating the PI3K/AKT Pathway
Jing Sun, Kongyan Wu, Pan Wang, Yubin Wang, Dan Wang, Wenting Zhao, Yuanyuan Zhao, Chunhong Zhang, Xiaoyan Zhao
Foods.2024; 13(3): 444. CrossRef - Atractylodes macrocephala Koidz. and Cuscuta chinensis Lam. extract relieves insulin resistance via PI3K/Akt signalling in diabetic Drosophila
Yinghong Li, Ye Xu, Biwei Zhang, Zhigang Wang, Leilei Ma, Longyu Sun, Xiuping Wang, Yimin Lin, Ji-an Li, Chenxi Wu
Journal of Traditional and Complementary Medicine.2024;[Epub] CrossRef - Ketogenic diet ameliorates high-fat diet-induced insulin resistance in mouse skeletal muscle by alleviating endoplasmic reticulum stress
Qin Ma, Lincheng Jiang, Yuehua You, Hongbing Ni, Li Ma, Xiaojing Lin, Zhuyun Wang, Weiyan Yan, Xiaoqiu Xiao, Xinyu Li, Jibin Li
Biochemical and Biophysical Research Communications.2024; 702: 149559. CrossRef - Brain insulin resistance and Alzheimer’s disease: a systematic review
Luis Jesuino de Oliveira Andrade, Luís Matos de Oliveira, Alcina Maria Vinhaes Bittencourt, Letícia Góes de Carvalho Lourenço, Gabriela Correia Matos de Oliveira
Dementia & Neuropsychologia.2024;[Epub] CrossRef - Poorly controlled glycemia and worse beta cell function associate with higher resting and total energy expenditure in adults with obesity and type 2 diabetes: A doubly labeled water study
Kate Lillegard, John A. Del Castillo, Heidi J. Silver
Clinical Nutrition.2024; 43(3): 729. CrossRef - Gut microbiota in insulin resistance: a bibliometric analysis
Weiwei Tian, Li Liu, Ruirui Wang, Yunyun Quan, Bihua Tang, Dongmei Yu, Lei Zhang, Hua Hua, Junning Zhao
Journal of Diabetes & Metabolic Disorders.2024;[Epub] CrossRef - Association of the triglyceride glucose index with all-cause and cardiovascular mortality in a general population of Iranian adults
Ghazaal Alavi Tabatabaei, Noushin Mohammadifard, Hamed Rafiee, Fatemeh Nouri, Asieh Maghami mehr, Jamshid Najafian, Masoumeh Sadeghi, Maryam Boshtam, Hamidreza Roohafza, Fahimeh Haghighatdoost, Marzieh Taheri, Nizal Sarrafzadegan
Cardiovascular Diabetology.2024;[Epub] CrossRef - Changes in Cells Associated with Insulin Resistance
Leszek Szablewski
International Journal of Molecular Sciences.2024; 25(4): 2397. CrossRef - Evaluación de la resistencia a la insulina mediante el índice HOMA: un enfoque comparativo entre mujeres premenopáusicas y posmenopáusicas
Carlos Fernando Yauli Flores, Ericka Jazmín Tubón Luisa
Salud, Ciencia y Tecnología.2024; 4: 729. CrossRef - Insulin Resistance: The Increased Risk of Cancers
Leszek Szablewski
Current Oncology.2024; 31(2): 998. CrossRef - Muscle strength and non-alcoholic fatty liver disease/metabolic-associated fatty liver disease
Xuan-Yu Hao, Kai Zhang, Xing-Yong Huang, Fei Yang, Si-Yu Sun
World Journal of Gastroenterology.2024; 30(7): 636. CrossRef - Outcomes With Finerenone in Patients With Chronic Kidney Disease and Type 2 Diabetes by Baseline Insulin Resistance
Thomas Ebert, Stefan D. Anker, Luis M. Ruilope, Paola Fioretto, Vivian Fonseca, Guillermo E. Umpierrez, Andreas L. Birkenfeld, Robert Lawatscheck, Charlie Scott, Katja Rohwedder, Peter Rossing
Diabetes Care.2024; 47(3): 362. CrossRef - Influence of Obesity and Insulin Resistance on the Reproductive Outcome of Iraqi Women Undergoing Intracytoplasmic Sperm Injection
Sundus Ali Dawood, Hayder Ali Lafta Mossa, Mufeeda Ali Jwad
Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 ).2024; 6(1): 179. CrossRef - Metabolic memory: mechanisms and diseases
Hao Dong, Yuezhang Sun, Lulingxiao Nie, Aimin Cui, Pengfei Zhao, Wai Keung Leung, Qi Wang
Signal Transduction and Targeted Therapy.2024;[Epub] CrossRef - Effect of preoperative oral carbohydrates on insulin resistance in patients undergoing laparoscopic cholecystectomy: a randomized controlled trial
Xiaohan Wang, Jingwen Zhuang, Jianxin Cheng, Zeyang Wang, Jingyi Sheng, Shanshan Guo, Rui Wang, Zhiping Wang
Langenbeck's Archives of Surgery.2024;[Epub] CrossRef - Beta‐Cell Tipe1 Orchestrates Insulin Secretion and Cell Proliferation by Promoting Gαs/cAMP Signaling via USP5
Lu Ding, Yang Sun, Yan Liang, Jie Zhang, Zhendong Fu, Caiyue Ren, Pengfei Li, Wen Liu, Rong Xiao, Hao Wang, Zhaoying Zhang, Xuetian Yue, Chunyang Li, Zhuanchang Wu, Yuemin Feng, Xiaohong Liang, Chunhong Ma, Lifen Gao
Advanced Science.2024;[Epub] CrossRef - Metabolic syndrome awareness in the general Korean population: results from a nationwide survey
Hyun-Jin Kim, Mi-Seung Shin, Kyung-Hee Kim, Mi-Hyang Jung, Dong-Hyuk Cho, Ju-Hee Lee, Kwang Kon Koh
The Korean Journal of Internal Medicine.2024; 39(2): 272. CrossRef - Pregnane X receptor knockout mitigates weight gain and hepatic metabolic dysregulation in female C57BL/6 J mice on a long-term high-fat diet
Lidya H. Gebreyesus, Sora Choi, Prince Neequaye, Mattia Mahmoud, Mia Mahmoud, Malvin Ofosu-Boateng, Elizabeth Twum, Daniel O. Nnamani, Lijin Wang, Nour Yadak, Sujoy Ghosh, Frank J. Gonzalez, Maxwell A. Gyamfi
Biomedicine & Pharmacotherapy.2024; 173: 116341. CrossRef - TyG-GGT is a Reliable Non-Invasive Predictor of Advanced Liver Fibrosis in Overweight or Obese Individuals
Lei Jin, Jing Gu, Zhe Zhang, Cheng-Fei Du, Fei-Qi Xu, Xiao-Kun Huang, Zhen-Yu Gao, Ying Li, Li-Li Yu, Xin Zhang, Guo-Qing Ru, Jun-Wei Liu, Lei Liang, Xiao-Dong Sun, Zun-Qiang Xiao
Obesity Surgery.2024; 34(4): 1333. CrossRef - Excess homocysteine inhibits pancreatic β-cell secretory function by repressing Zbtb20 expression
Tianqi Ding, Bo Wen, Jian Chen, Wenbin Chu, Rong Fan, Xuewei Chen
Molecular and Cellular Endocrinology.2024; 586: 112195. CrossRef - Testosterone therapy reduces insulin resistance in men with adult‐onset testosterone deficiency and metabolic syndrome. Results from the Moscow Study, a randomized controlled trial with an open‐label phase
Yuliya Tishova, Svetlana Kalinchenko, George Mskhalaya, Geoffrey Hackett, Mark Livingston, Carola König, Richard Strange, Michael Zitzmann, Amar Mann, Amro Maarouf, Sudarshan Ramachandran
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Preoperative contributing factors and the remission of diabetes after metabolic surgery: the mediating role of preoperative triglyceride
Lijuan Niu, Liqian Mu, Runda Wu, Shan Tong, Zhongqi Mao, Yi Yang, Jun Yin
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity.2024;[Epub] CrossRef - Mechanisms of Action of Potentilla discolor Bunge in Type 2 Diabetes Mellitus Based on Network Pharmacology and Experimental Verification in Drosophila
Yinghong Li, Fanwu Wu, Jianbo Zhang, Ye Xu, Hong Chang, Yueyue Yu, Chunhua Jiang, Xiujuan Gao, Huijuan Liu, Zhen Chen, Chenxi Wu, Ji-An Li
Drug Design, Development and Therapy.2024; Volume 18: 747. CrossRef - Diabetes and diabetic associative diseases: An overview of epigenetic regulations of TUG1
Mohammed Ageeli Hakami
Saudi Journal of Biological Sciences.2024; 31(5): 103976. CrossRef - Sleep quality of patients with diabetes mellitus: association with anxiety trait and state
Lidiane Bernardes Faria Vilela, Larissa Cristina dos Santos Camargos, Guilherme Rocha Rodrigues, Adelzí Auto Alves Júnior, Renato Canevari Dutra da Silva, Elton Brás Camargo Júnior
Revista Gaúcha de Enfermagem.2024;[Epub] CrossRef - Qualidade do sono de pacientes com diabetes mellitus: associação com ansiedade traço e estado
Lidiane Bernardes Faria Vilela, Larissa Cristina dos Santos Camargos, Guilherme Rocha Rodrigues, Adelzí Auto Alves Júnior, Renato Canevari Dutra da Silva, Elton Brás Camargo Júnior
Revista Gaúcha de Enfermagem.2024;[Epub] CrossRef - Association of the triglyceride-glucose index with severity of coronary stenosis and in-hospital mortality in patients with acute ST elevation myocardial infarction after percutaneous coronary intervention: a multicentre retrospective analysis cohort stud
Xin Lu, Xin Lin, Yingying Cai, Xiaoxiao Zhang, Haoyu Meng, Weiwei Chen, Peng Yu, Xiaohu Chen
BMJ Open.2024; 14(3): e081727. CrossRef - Effects of a Diabetic Microenvironment on Neurodegeneration: Special Focus on Neurological Cells
Vishal Chavda, Dhananjay Yadav, Snehal Patel, Minseok Song
Brain Sciences.2024; 14(3): 284. CrossRef - Mechanisms of body fat distribution and gluteal-femoral fat protection against metabolic disorders
Maha Alser, Khaled Naja, Mohamed A. Elrayess
Frontiers in Nutrition.2024;[Epub] CrossRef - Regulation of lipid metabolism by E3 ubiquitin ligases in lipid-associated metabolic diseases
Yuanming Zou, Ying Zhang, Mohan Li, Kexin Cao, Chunyu Song, Zhaobo Zhang, Kexin Cai, Danxi Geng, Shuxian Chen, Yanjiao Wu, Naijin Zhang, Guozhe Sun, Jing Wang, Yixiao Zhang, Yingxian Sun
International Journal of Biological Macromolecules.2024; 265: 130961. CrossRef - METS-IR and all-cause mortality in Korean over 60 years old: Korean genome and epidemiology study-health examinees (KoGES-HEXA) cohorts
Ha Eun Ryu, Dong Hyuk Jung, Seok-Jae Heo, Byoungjin Park, Yong Jae Lee
Frontiers in Endocrinology.2024;[Epub] CrossRef - Effects of vitamin family members on insulin resistance and diabetes complications
Hong-Jin Chen, Min Wang, Ding-Min Zou, Gui-You Liang, Si-Yuan Yang
World Journal of Diabetes.2024; 15(3): 568. CrossRef - Alleviative effects of the parthenolide derivative ACT001 on insulin resistance induced by sodium propionate combined with a high-fat diet and its potential mechanisms
Qian Yu, Xiang Zuo, Huijuan Bai, Shuhui Zhang, Jialu Luan, Qili Zhao, Xin Zhao, Xizeng Feng
European Journal of Pharmacology.2024; 971: 176529. CrossRef - The genetic causal relationship between type 2 diabetes, glycemic traits and venous thromboembolism, deep vein thrombosis, pulmonary embolism: a two-sample Mendelian randomization study
Mingyi Yang, Xianjie Wan, Yani Su, Ke Xu, Pengfei Wen, Binfei Zhang, Lin Liu, Zhi Yang, Peng Xu
Thrombosis Journal.2024;[Epub] CrossRef - Transgenerational inheritance of insulin resistance in offspring of white rice-fed female fruit flies
Kehinde Ahmad Adeshina, Kasimu Ghandi Ibrahim, Murtala Bello Abubakar, Mustapha Umar Imam
Scientific African.2024; 24: e02208. CrossRef - PPARβ/δ as a promising molecular drug target for liver diseases: A focused review
Xin Meng, Lin Wang, Yan-Chao Du, Dong Cheng, Tao Zeng
Clinics and Research in Hepatology and Gastroenterology.2024; 48(6): 102343. CrossRef - EPA and DHA Differentially Improve Insulin Resistance by Reducing Adipose Tissue Inflammation — Targeting GPR120/PPARγ Pathway
Xian Yang, Xudong Li, Manjiang Hu, Jie Huang, Siyan Yu, Huanting Zeng, Limei Mao
The Journal of Nutritional Biochemistry.2024; : 109648. CrossRef - The impact of diabetes mellitus on the development of psychiatric and neurological disorders
Olivia Kelly, Jillian Sullivan, Natalie Carris, Samantha Geci, Athena Martinez, Varvara Liashenko, James Colvin, Emily Misko, Gary Vanderlaan, He Liu, Prasad S. Dalvi
Brain Disorders.2024; 14: 100135. CrossRef - Oligonucleotide therapies for nonalcoholic steatohepatitis
Sixu Li, Feng Xiong, Songbo Zhang, Jinghua Liu, Guangping Gao, Jun Xie, Yi Wang
Molecular Therapy - Nucleic Acids.2024; 35(2): 102184. CrossRef - The Contribution of Type 2 Diabetes to Parkinson’s Disease Aetiology
Samo Ribarič
International Journal of Molecular Sciences.2024; 25(8): 4358. CrossRef - Dose-response associations of triglyceride to high-density lipoprotein cholesterol ratio and triglyceride–glucose index with arterial stiffness risk
Wenkai Zhang, Weifeng Huo, Huifang Hu, Tianze Li, Lijun Yuan, Jinli Zhang, Yifei Feng, Yuying Wu, Xueru Fu, Yamin Ke, Mengmeng Wang, Longkang Wang, Yaobing Chen, Yajuan Gao, Xi Li, Liang Sun, Jinyuan Pang, Zeqiang Zheng, Fulan Hu, Ming Zhang, Yu Liu, Dong
Lipids in Health and Disease.2024;[Epub] CrossRef - Unraveling PCOS: Exploring its causes and diagnostic challenges
Mohd Altaf Dar, Mudasir Maqbool, Zulfkar Qadrie, Irfat Ara, Afshana Qadir
Open Health.2024;[Epub] CrossRef - Association Between Triglyceride-Glucose Index and Diabetic
Retinopathy: A Meta-Analysis
Lanchu Yu, Bingqing Li
Hormone and Metabolic Research.2024;[Epub] CrossRef - Serum Klotho and insulin resistance: Insights from a cross-sectional analysis
Laisha Yan, Xiaoyan Hu, Shanshan Wu, Shunying Zhao
Medicine.2024; 103(17): e37971. CrossRef - Research Progress of Correlation between Triglyceride Glucose Index and Kidney Disease
伊琳 黄
Advances in Clinical Medicine.2024; 14(04): 2137. CrossRef - Oxygen-Dependent Aspects of Asprosin Action
V. V. Zinchuk, J. S. O. Al-Jebur
Journal of Evolutionary Biochemistry and Physiology.2024; 60(2): 818. CrossRef - Prevalence of Metabolic Syndrome and Insulin Resistance in Adult Patients with Acne: Association with Traditional Cardiovascular Risk Factors and Acne Severity
Ana Cecília Arcanjo Carneiro, Jozélio Freire de Carvalho, Daniel Coelho de Sá, Carlos Ewerton Maia Rodrigues
Metabolic Syndrome and Related Disorders.2023; 21(2): 109. CrossRef - Metabolic and Genetic Association of Vitamin D with Calcium Signaling and Insulin Resistance
Najeebul Tarfeen, Khair Ul Nisa, Mir Bilal Ahmad, Ajaz Ahmad Waza, Bashir Ahmad Ganai
Indian Journal of Clinical Biochemistry.2023; 38(4): 407. CrossRef - Tinosporaside from Tinospora cordifolia Encourages Skeletal Muscle Glucose Transport through Both PI-3-Kinase- and AMPK-Dependent Mechanisms
Akansha Mishra, Khushbu Sharma, Jyotsana Pandey, Kapil Dev, Sleman Kadan, Mahendra Sahai, Ishbal Ahmad, Arvind K. Srivastava, Akhilesh K. Tamrakar, Hilal Zaid, Rakesh Maurya
Molecules.2023; 28(2): 483. CrossRef - Pathophysiology of obesity and its associated diseases
Xin Jin, Tingting Qiu, Li Li, Rilei Yu, Xiguang Chen, Changgui Li, Christopher G. Proud, Tao Jiang
Acta Pharmaceutica Sinica B.2023; 13(6): 2403. CrossRef - Hypertension, type 2 diabetes, obesity, and p53 mutations negatively correlate with metastatic colorectal cancer patients’ survival
Alessandro Ottaiano, Mariachiara Santorsola, Luisa Circelli, Francesco Perri, Marco Cascella, Francesco Sabbatino, Maurizio Capuozzo, Vincenza Granata, Silvia Zappavigna, Angela Lombardi, Marianna Scrima, Nadia Petrillo, Monica Ianniello, Marika Casillo,
Frontiers in Medicine.2023;[Epub] CrossRef - Triglyceride glucose index and poor sleep patterns in non-diabetic adults: Evidence from NHANES 2005–2016
Chi-Feng Liu, Li-Wei Chien
Frontiers in Nutrition.2023;[Epub] CrossRef - Polyphenol-Rich Extract of Fermented Chili Pepper Alleviates Insulin Resistance in HepG2 Cells via Regulating INSR, PTP1B, PPAR-γ, and AMPK Pathways
Tao Wang, Meiqi Li, Shengbao Cai, Linyan Zhou, Xiaosong Hu, Junjie Yi
Fermentation.2023; 9(2): 84. CrossRef - Effects of preoperative oral enzyme-hydrolyzed rice flour solution on gastric emptying and insulin resistance in patients undergoing laparoscopic cholecystectomy: a prospective randomized controlled trial
Yang Yuan, Guangjun Shi, Huailong Chen, Mingshan Wang, Haofei Liu, Xiao Zhang, Bin Wang, Gaofeng Zhang, Lixin Sun
BMC Anesthesiology.2023;[Epub] CrossRef - Roles of endoplasmic reticulum stress in the pathophysiology of polycystic ovary syndrome
Hiroshi Koike, Miyuki Harada, Akari Kusamoto, Zixin Xu, Tsurugi Tanaka, Nanoka Sakaguchi, Chisato Kunitomi, Jerilee M. K. Azhary, Nozomi Takahashi, Yoko Urata, Yutaka Osuga
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Metabolic Score for Insulin Resistance (METS-IR) Predicts Cardiovascular Disease and Its Subtypes in Patients with Hypertension and Obstructive Sleep Apnea
Wenbo Yang, Xintian Cai, Junli Hu, Wen Wen, Heizhati Mulalibieke, Xiaoguang Yao, Ling Yao, Qing Zhu, Jing Hong, Qin Luo, Shasha Liu, Nanfang Li
Clinical Epidemiology.2023; Volume 15: 177. CrossRef - Sperm DNA damage: The possible link between obesity and male infertility, an update of the current literature
Andrew Peel, Anmol Saini, Joshua C. Deluao, Nicole O. McPherson
Andrology.2023; 11(8): 1635. CrossRef - Glucose Homeostasis, Diabetes Mellitus, and Gender-Affirming Treatment
Charalampos Milionis, Ioannis Ilias, Evangelia Venaki, Eftychia Koukkou
Biomedicines.2023; 11(3): 670. CrossRef - From Metabolic Syndrome to Type 2 Diabetes in Youth
Dario Iafusco, Roberto Franceschi, Alice Maguolo, Salvatore Guercio Nuzio, Antonino Crinò, Maurizio Delvecchio, Lorenzo Iughetti, Claudio Maffeis, Valeria Calcaterra, Melania Manco
Children.2023; 10(3): 516. CrossRef - Kcnma1 is involved in mitochondrial homeostasis in diabetes‐related skeletal muscle atrophy
Shan‐Yan Gao, Yong‐Ping Liu, Ri Wen, Xin‐Mei Huang, Ping Li, Yu‐Hang Yang, Ni Yang, Tie‐Ning Zhang
The FASEB Journal.2023;[Epub] CrossRef - Capsaicin and Zinc Signalling Pathways as Promising Targets for Managing Insulin Resistance and Type 2 Diabetes
Parisa Vahidi Ferdowsi, Kiran D. K. Ahuja, Jeffrey M. Beckett, Stephen Myers
Molecules.2023; 28(6): 2861. CrossRef - Mouse Models with SGLT2 Mutations: Toward Understanding the Role of SGLT2 beyond Glucose Reabsorption
Keiko Unno, Kyoko Taguchi, Yoshiichi Takagi, Tadashi Hase, Shinichi Meguro, Yoriyuki Nakamura
International Journal of Molecular Sciences.2023; 24(7): 6278. CrossRef - Association between triglyceride-glucose index and carotid atherosclerosis in patients with psoriatic arthritis
Wenhui Xie, Wei Bian, Zhibo Song, Xuerong Deng, Jiahao Qu, Zhuoli Zhang
Rheumatology.2023; 62(11): 3584. CrossRef - The relationship between HMGB1 and autophagy in the pathogenesis of diabetes and its complications
Kun Yang, Feng Cao, Weili Wang, Zhenyu Tian, Lu Yang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association of long-term triglyceride-glucose index level and change with the risk of cardiometabolic diseases
Wenqi Xu, Haiyan Zhao, Lishu Gao, Lu Guo, Jianrong Liu, Haixia Li, Junyan Sun, Aijun Xing, Shuohua Chen, Shouling Wu, Yuntao Wu
Frontiers in Endocrinology.2023;[Epub] CrossRef - White Adipose Tissue Dysfunction: Pathophysiology and Emergent Measurements
Natalia Santillana, Camila Astudillo-Guerrero, Amanda D’Espessailles, Gonzalo Cruz
Nutrients.2023; 15(7): 1722. CrossRef - Soy protein compared with whey protein ameliorates insulin resistance by regulating lipid metabolism, AMPK/mTOR pathway and gut microbiota in high-fat diet-fed mice
Andong Ji, Wei Chen, Chang Liu, Tianyu Zhang, Runjia Shi, Xinqi Wang, Huina Xu, Duo Li
Food & Function.2023; 14(12): 5752. CrossRef - Hepatic Insulin Resistance Model in the Male Wistar Rat Using Exogenous Insulin Glargine Administration
Victor Enrique Sarmiento-Ortega, Diana Moroni-González, Alfonso Diaz, Miguel Ángel García-González, Eduardo Brambila, Samuel Treviño
Metabolites.2023; 13(4): 572. CrossRef - Pathophysiological Effects of Contemporary Lifestyle on Evolutionary-Conserved Survival Mechanisms in Polycystic Ovary Syndrome
Jim Parker
Life.2023; 13(4): 1056. CrossRef - Metabolic dysfunction correction as a method of restoring the function of the reproductive system in women
G. E. Chernukha, V. A. Pronina
Meditsinskiy sovet = Medical Council.2023; (5): 90. CrossRef - Associations between TyG-BMI and normal-high blood pressure values and hypertension: cross-sectional evidence from a non-diabetic population
Nan Peng, Maobin Kuang, Yi Peng, Hang Yu, Shuhua Zhang, Guobo Xie, Guotai Sheng, Yang Zou
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Inverse Correlation of Superoxide Dismutase and Catalase with Type 2 Diabetes among Rural Thais
Natnicha Promyos, Pornpimol Panprathip Phienluphon, Naruemon Wechjakwen, Jirayu Lainampetch, Pattaneeya Prangthip, Karunee Kwanbunjan
Nutrients.2023; 15(9): 2071. CrossRef - Interplay of skeletal muscle and adipose tissue: sarcopenic obesity
Min Jeong Park, Kyung Mook Choi
Metabolism.2023; 144: 155577. CrossRef - Oxygen-binding properties of blood in insulin resistance with different asprosin content
V.V. Zinchuk, J.S.O. Al-Jebur, N.V. Glutkina
Biomeditsinskaya Khimiya.2023; 69(2): 133. CrossRef - Associations between basal metabolic rate and insulin resistance in non-diabetic obese adults: Evidence from NHANES 2011–2018
Hai Guo, Dilihumaier Duolikun, Qiaoling Yao
International Journal of Diabetes in Developing Countries.2023; 43(6): 946. CrossRef - Biomarkers of Spinal Cord Injury in Patients Undergoing Complex Endovascular Aortic Repair Procedures—A Narrative Review of Current Literature
Anna Sotir, Johannes Klopf, Christine Brostjan, Christoph Neumayer, Wolf Eilenberg
Biomedicines.2023; 11(5): 1317. CrossRef - The Hypoglycemic Activities and Underlying Mechanisms of Two Saponins‐Rich Components from Fried Ziziphus jujuba Mill. Kernel
Yi‐Meng Li, Ke‐xin Hao, Hong Xie, Jian‐Guo Jiang
Molecular Nutrition & Food Research.2023;[Epub] CrossRef - Long-term outcomes and potential mechanisms of offspring exposed to intrauterine hyperglycemia
Yi-Shang Yan, Chun Feng, Dan-Qing Yu, Shen Tian, Yin Zhou, Yi-Ting Huang, Yi-Ting Cai, Jian Chen, Miao-Miao Zhu, Min Jin
Frontiers in Nutrition.2023;[Epub] CrossRef - The Function of MondoA and ChREBP Nutrient—Sensing Factors in Metabolic Disease
Byungyong Ahn
International Journal of Molecular Sciences.2023; 24(10): 8811. CrossRef - An Update on the Molecular and Cellular Basis of Pharmacotherapy in Type 2 Diabetes Mellitus
Mohamed Omer Mahgoub, Ifrah Ismail Ali, Jennifer O. Adeghate, Kornélia Tekes, Huba Kalász, Ernest A. Adeghate
International Journal of Molecular Sciences.2023; 24(11): 9328. CrossRef - Study on the therapeutic effect and mechanism of Tangningtongluo Tablet on diabetic mice
Zengxiaorui Cai, Xiangka Hu, Liuming Gui, Mushuang Qi, Wanjun Zhu, Ying Ren, Shuyu Yang, Chunmei Dai
Journal of Diabetes and its Complications.2023; 37(8): 108523. CrossRef - A Descriptive Review of the Action Mechanisms of Berberine, Quercetin and Silymarin on Insulin Resistance/Hyperinsulinemia and Cardiovascular Prevention
Paolo Bellavite, Serafino Fazio, Flora Affuso
Molecules.2023; 28(11): 4491. CrossRef - Relationships of neck circumference and abdominal obesity with insulin resistance considering relative handgrip strength in middle-aged and older individuals
Kayoung Lee
Archives of Gerontology and Geriatrics.2023; 114: 105097. CrossRef - Acute exposure to realistic concentrations of Bisphenol-A trigger health damage in fish: Blood parameters, gene expression, oxidative stress
Gustavo Axel Elizalde-Velázquez, Leobardo Manuel Gómez-Oliván, Selene Elizabeth Herrera-Vázquez, Karina Elisa Rosales-Pérez, Nely SanJuan-Reyes, Sandra García-Medina, Marcela Galar-Martínez
Aquatic Toxicology.2023; 261: 106610. CrossRef - Gαi‐coupled GPR41 activation increases Ca2+ influx in C2C12 cells and shows a therapeutic effect in diabetic animals
Do‐Hyung Lee, Kyung‐Sun Heo, Chang‐Seon Myung
Obesity.2023; 31(7): 1871. CrossRef - Physical inactivity induces insulin resistance in plantaris muscle through protein tyrosine phosphatase 1B activation in mice
Saori Kakehi, Yoshifumi Tamura, Shin-ichi Ikeda, Naoko Kaga, Hikari Taka, Yuya Nishida, Ryuzo Kawamori, Hirotaka Watada
Frontiers in Physiology.2023;[Epub] CrossRef - Metabolic-Associated Fatty Liver Disease and Insulin Resistance: A Review of Complex Interlinks
Thomas M. Barber, Stefan Kabisch, Andreas F. H. Pfeiffer, Martin O. Weickert
Metabolites.2023; 13(6): 757. CrossRef - Metabolic Markers Associated with Progression of Type 2 Diabetes Induced by High-Fat Diet and Single Low Dose Streptozotocin in Rats
Maria Andonova, Petko Dzhelebov, Krastina Trifonova, Penka Yonkova, Nikola Kostadinov, Krasimira Nancheva, Veselin Ivanov, Krasimira Gospodinova, Nikola Nizamov, Ilia Tsachev, Chavdar Chernev
Veterinary Sciences.2023; 10(7): 431. CrossRef - Research Progress Into Adipose Tissue Macrophages and Insulin Resistance
M Fu, L Yang, H Wang, Y Chen, X Chen, Q Hu, H Sun
Physiological Research.2023;[Epub] CrossRef - Effects of aerobic exercises in prediabetes patients: a systematic review and meta-analysis
Yifei Wang, Honglei Li, Dongxue Yang, Mengzhao Wang, Yanbai Han, Hongli Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Associations of C-peptide with cardiometabolic parameters in women aged 25–44 years with different metabolic phenotypes
S. V. Mustafina, V. I. Alferova, L. V. Shcherbakova, E. V. Kashtanova, D. V. Denisova
Ateroscleroz.2023; 19(2): 115. CrossRef - Adipose-derived Mesenchymal Stem Cells Therapy as a new Treatment Option for Diabetes Mellitus
Agnieszka Mikłosz, Adrian Chabowski
The Journal of Clinical Endocrinology & Metabolism.2023; 108(8): 1889. CrossRef - Anthropometric Indices With Insulin Resistance in Obese Patients: A Literature Review
Khalid Khan, Anil Wanjari, Sourya Acharya, Sabiha Quazi
Cureus.2023;[Epub] CrossRef - Preventive and therapeutic effects of natural products and herbal extracts on nonalcoholic fatty liver disease/nonalcoholic steatohepatitis
Yiming Cao, Xiaoxue Fang, Mingyang Sun, Yegang Zhang, Mengyao Shan, Xintian Lan, Difu Zhu, Haoming Luo
Phytotherapy Research.2023; 37(9): 3867. CrossRef - Tuina (Chinese massage) for insulin resistance and sensitivity: A protocol for systematic review and meta-analysis of animal and human studies
Zhixuan Zhao, Jun Yan, Yuxin Ding, Yingji Wang, Yan Li, Ricardo Ney Oliveira Cobucci
PLOS ONE.2023; 18(7): e0288414. CrossRef - Rubus chingii Hu relieved the polycystic ovary syndrome with enhanced insulin sensitivity through inhibiting TXNIP/NLRP3 inflammasome signaling
Huizhen Li, Yongping Li, Ying Zhang, Li Tong, Yuping Sa, Wenping Sun
Gynecological Endocrinology.2023;[Epub] CrossRef - The Research Role of Triglyceride Glucose Index in Pre-Type 2 Diabetes
士博 徐
Advances in Clinical Medicine.2023; 13(07): 11762. CrossRef - Underlying mechanisms and molecular targets of genistein in the management of type 2 diabetes mellitus and related complications
Tao Jiang, Yuhe Dong, Wanying Zhu, Tong Wu, Linyan Chen, Yuantong Cao, Xi Yu, Ye Peng, Ling Wang, Ying Xiao, Tian Zhong
Critical Reviews in Food Science and Nutrition.2023; : 1. CrossRef - Gentiopicroside modulates glucose homeostasis in high-fat-diet and streptozotocin-induced type 2 diabetic mice
Xing Wang, Dongmei Long, Xianghong Hu, Nan Guo
Frontiers in Pharmacology.2023;[Epub] CrossRef - Review of the Case Reports on Metformin, Sulfonylurea, and Thiazolidinedione Therapies in Type 2 Diabetes Mellitus Patients
Elis Susilawati, Jutti Levita, Yasmiwar Susilawati, Sri Adi Sumiwi
Medical Sciences.2023; 11(3): 50. CrossRef - Effects of AIM2 and IFI16 on Infectious Diseases and Inflammation
Zhen Fan, Rui Chen, Wen Yin, Xiaomei Xie, Shan Wang, Chunbo Hao
Viral Immunology.2023; 36(7): 438. CrossRef - PREDICTING PROGRESSION TYPE 2 DIABETES MELLITUS: A 3-YEAR FOLLOW-UP STUDY EXAMINING RISK FACTORS FOR TYPE 2 DIABETES IN PATIENTS WITH PREDIABETES
Taras I. Griadil, Mykhaylo V. Bychko, Mykhaylo M. Hechko, Ksenia I. Chubirko, Ivan V. Chopey
Polski Merkuriusz Lekarski.2023; 51(3): 245. CrossRef - GABA Prevents Age-Related Sarcopenic Obesity in Mice with High-Fat-Diet-Induced Obesity
Heegu Jin, Hyun-Ji Oh, Boo-Yong Lee
Cells.2023; 12(17): 2146. CrossRef - Bio-Hacking Better Health—Leveraging Metabolic Biochemistry to Maximise Healthspan
Isabella D. Cooper, Yvoni Kyriakidou, Lucy Petagine, Kurtis Edwards, Bradley T. Elliott
Antioxidants.2023; 12(9): 1749. CrossRef - Hyperinsulinemia Impairs Clathrin-Mediated Endocytosis of the Insulin Receptor and Activation of Endothelial Nitric Oxide Synthase in Brain Endothelial Cells
Stephanie G. DiLucia, B. Jacob Kendrick, Catrina Sims-Robinson
International Journal of Molecular Sciences.2023; 24(19): 14670. CrossRef - Validation of a physiological type 2 diabetes model in human periodontal ligament stem cells
Dongqing Ai, Yuanyuan Yin, Xuyun Xia, Sihan Yang, Yu Sun, Jie Zhou, Han Qin, Xiaohui Xu, Jinlin Song
Oral Diseases.2023;[Epub] CrossRef - Flavonoids from Lophatherum gracile Brongn. Ameliorate Liver Damages in High-Fat Diet and Streptozotocin-Induced Diabetic Mice by Regulating PI3K/AKT and NF-Kappa B Pathways
Jian-Hua Zheng, Song-Xia Lin, Xiao-Yi Li, Chun-Yan Shen, Shao-Wei Zheng, Wen-Bin Chen, Walid Elfalleh
Journal of Food Biochemistry.2023; 2023: 1. CrossRef - Asprosin, a novel glucogenic adipokine implicated in type 2 diabetes mellitus
Hongcui Diao, Xue Li, Yeqiu Xu, Xiuli Xing, Shuguang Pang
Journal of Diabetes and its Complications.2023; 37(11): 108614. CrossRef - Impact of Fixed Combination of Metformin and Pioglitazone on Insulin Resistance of Patients with Type 2 Diabetes: Results of a Randomized Open-Label Study
Rui Sun, Lu Yuan, Yun Shen, Ziyang Shen, Bo Ding, Jianhua Ma
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2911. CrossRef - Integrating network analysis and experimental validation to reveal the mechanism of pinocembrin in alleviating high glucose and free fatty acid-induced lipid accumulation in HepG2 cells
Kun Hu, Yongjin Sun, Jie Wang, Shaojun Wu, Jie Ren, Dan Su, Lidan Tang, Jinhong Gong, Hufeng Fang, Shan Xu, Hao Yang
Journal of Functional Foods.2023; 110: 105879. CrossRef - A Literature Review and a Proposed Classification of the Relationships between Ovulatory Infertility and Lifestyle Factors Based on the Three Groups of Ovulation Disorders Classified by WHO
Magdalena Skowrońska, Michał Pawłowski, Robert Milewski
Journal of Clinical Medicine.2023; 12(19): 6275. CrossRef - Targeting of insulin receptor endocytosis as a treatment to insulin resistance
Bryce Tim, Valentina L. Kouznetsova, Santosh Kesari, Igor F. Tsigelny
Journal of Diabetes and its Complications.2023; 37(11): 108615. CrossRef - A U-shaped association between the triglyceride to high-density lipoprotein cholesterol ratio and the risk of incident type 2 diabetes mellitus in Japanese men with normal glycemic levels: a population-based longitudinal cohort study
Bei Song, Kun Wang, Weilin Lu, Xiaofang Zhao, Tianci Yao, Ting Liu, Guangyu Gao, Haohui Fan, Chengyun Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association of triglyceride-glucose index levels with gestational diabetes mellitus in the US pregnant women: a cross-sectional study
Yan Zeng, Li Yin, Xiaoping Yin, Danqing Zhao
Frontiers in Endocrinology.2023;[Epub] CrossRef - The protective role of resveratrol in diabetic wound healing
Minglei Bi, Yonghong Qin, Lerong Wang, Jin Zhang
Phytotherapy Research.2023; 37(11): 5193. CrossRef - Correlation between alternative insulin resistance indexes and diabetic kidney disease: a retrospective study
Xiaodie Mu, Aihua Wu, Huiyue Hu, Min Yang, Hua Zhou
Endocrine.2023; 84(1): 136. CrossRef - Enhancing Muscle Intracellular Ca2+ Homeostasis and Glucose Uptake: Passive Pulsatile Shear Stress Treatment in Type 2 Diabetes
Arkady Uryash, Jordan Umlas, Alfredo Mijares, Jose A. Adams, Jose R. Lopez
Biomedicines.2023; 11(10): 2596. CrossRef - Review of Related Research on Type 2 Diabetes Related Macroangiopathy
珊珊 李
Advances in Clinical Medicine.2023; 13(09): 15001. CrossRef - Association between lipoprotein(a) and insulin resistance in Chinese adults: results from the China health and nutrition survey
Heng Wang, Jia-Li Fan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association between the Triglyceride–Glucose Index and Non-Alcoholic Fatty Liver Disease in patients with Atrial Fibrillation
Xiaozhong Li, Fenfang Zhan, Tian Peng, Zhen Xia, Juxiang Li
European Journal of Medical Research.2023;[Epub] CrossRef - Resveratrol as a potential protective compound against skeletal muscle insulin resistance
Arash Bahramzadeh, Kosar Bolandnazar, Reza Meshkani
Heliyon.2023; 9(11): e21305. CrossRef - The Potential Role of C-Reactive Protein in Metabolic-Dysfunction-Associated Fatty Liver Disease and Aging
Zheng Ding, Yuqiu Wei, Jing Peng, Siyu Wang, Guixi Chen, Jiazeng Sun
Biomedicines.2023; 11(10): 2711. CrossRef - Obesity and Bone Mineral Density Protection Paradox in Chronic Kidney Disease: Secreted Protein Acidic and Rich in Cysteine as a Piece of the Puzzle?
Abdelaziz Ghanemi, Fabrice Mac-Way
Life.2023; 13(11): 2172. CrossRef - Correlation of Lipid Profile and Apolipoprotein B/A-I Ratio with Insulin Resistance in Non-Diabetes Mellitus Subjects
Andi Heriadi Palloge, Liong Boy Kurniawan, Yuyun Widyaningsih, Husaini Umar, Nurahmi Nurahmi, Andi Alfian Zainuddin
INDONESIAN JOURNAL OF CLINICAL PATHOLOGY AND MEDICAL LABORATORY.2023; 30(1): 6. CrossRef - Endothelial progenitor cells as biomarkers of diabetes-related cardiovascular complications
Josefa Benítez-Camacho, Antonio Ballesteros, Lucía Beltrán-Camacho, Marta Rojas-Torres, Antonio Rosal-Vela, Margarita Jimenez-Palomares, Ismael Sanchez-Gomar, Mª Carmen Durán-Ruiz
Stem Cell Research & Therapy.2023;[Epub] CrossRef - Effects of ginseng peptides on the hypoglycemic activity and gut microbiota of a type 2 diabetes mellitus mice model
Caijing Han, Xiaoting Kong, Xiaohong Xia, Xinyu Huang, Zhaojie Mao, Jiaxin Han, Fuyan Shi, Yaohui Liang, Anning Wang, Fengxiang Zhang
Journal of Functional Foods.2023; 111: 105897. CrossRef - Effects of theasaponin E1 on the regulationglucose uptake of C2C12 myoblasts PI3K/Akt/mTOR signaling pathway
Ming Zhang, Zhiyun Chen, Di Tian, Zaiqiao Li, Shaning Wang, Yujie Huo, Ling Song, Juan Lu, Jun Sheng, Xu Ji, Xiao Ma
CyTA - Journal of Food.2023; 21(1): 682. CrossRef - Efficacy and underlying mechanisms of berberine against lipid metabolic diseases: a review
Yajie Cai, Qiaoning Yang, Yanqiao Yu, Furong Yang, Ruina Bai, Xiaodi Fan
Frontiers in Pharmacology.2023;[Epub] CrossRef - Adipocyte-derived exosomal miR-22-3p modulated by circadian rhythm disruption regulates insulin sensitivity in skeletal muscle cells
Haohao Zhang, Xiaoning Zhang, Saifei Wang, Lu Zheng, Hengru Guo, Yanqi Ren, Bo Qiao, Jing Wu, Di Zhao, Lijun Xu, Shengnan Ma, Xiao Hao, Yushan Yan
Journal of Biological Chemistry.2023; 299(12): 105476. CrossRef - Total Astragalus saponins can reverse type 2 diabetes mellitus-related intestinal dysbiosis and hepatic insulin resistance in vivo
Leilei Ma, Xiaojin La, Biwei Zhang, Wenxuan Xu, Chunyu Tian, Qianru Fu, Meng Wang, Chenxi Wu, Zhen Chen, Hong Chang, Ji-an Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Interplay between Vitamin D and Adipose Tissue: Implications for Adipogenesis and Adipose Tissue Function
Shiqi Lu, Zhen-Bo Cao
Nutrients.2023; 15(22): 4832. CrossRef - Alanine aminotransferase to high- density lipoprotein cholesterol ratio is positively correlated with the occurrence of diabetes in the Chinese population: a population-based cohort study
Shiming He, Changhui Yu, Maobin Kuang, Jiajun Qiu, Ruijuan Yang, Shuhua Zhang, Guotai Sheng, Yang Zou
Frontiers in Endocrinology.2023;[Epub] CrossRef - The association between the metabolic score for insulin resistance (METS-IR) index and urinary incontinence in the United States: results from the National Health and Nutrition Examination Survey (NHANES) 2001–2018
Shangqi Cao, Linghao Meng, Lede Lin, Xu Hu, Xiang Li
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Adipose Tissue, Non-Communicable Diseases, and Physical Exercise: An Imperfect Triangle
Francisco A. Monsalve, Fernando Delgado-López, Barbra Fernández-Tapia, Daniel R. González
International Journal of Molecular Sciences.2023; 24(24): 17168. CrossRef - Risk of metabolic abnormalities in osteoarthritis: a new perspective to understand its pathological mechanisms
Guizheng Wei, Ke Lu, Muhammad Umar, Zhenglin Zhu, William W. Lu, John R. Speakman, Yan Chen, Liping Tong, Di Chen
Bone Research.2023;[Epub] CrossRef - Influence of Sociodemographic Variables and Healthy Habits on the Values of Insulin Resistance Indicators in 386,924 Spanish Workers
Miguel Mestre Font, Carla Busquets-Cortés, José Ignacio Ramírez-Manent, Pilar Tomás-Gil, Hernán Paublini, Ángel Arturo López-González
Nutrients.2023; 15(24): 5122. CrossRef - Konjac flour-mediated gut microbiota alleviates insulin resistance and improves placental angiogenesis of obese sows
Deyuan Wu, Wenyu Xiong, Shuo Ma, Jinxi Luo, Hongxuan Ye, Shuangbo Huang, Fuyong Li, Xi’en Xiang, Qiling Chen, Binghui Gao, Jinping Deng, Yulong Yin, Chengquan Tan
AMB Express.2023;[Epub] CrossRef - Physiological Adaptations to Life in Space: An Update
Isadora de Carvalho e Silva, Thais Russomano, Ricardo Alves Ferreira, Marli do Carmo Cupertino, Fabíola Alves Alcântara, Mauro Geller, Oswaldo Monteiro Del Cima, Rodrigo Siqueira-Batista
Journal of Aerospace Technology and Management.2023;[Epub] CrossRef - Blood and Brain Metabolites after Cerebral Ischemia
Eva Baranovicova, Dagmar Kalenska, Peter Kaplan, Maria Kovalska, Zuzana Tatarkova, Jan Lehotsky
International Journal of Molecular Sciences.2023; 24(24): 17302. CrossRef - Key Therapeutic Targets to Treat Hyperglycemia-Induced Atherosclerosis Analyzed Using a Petri Net-Based Model
Agnieszka Rybarczyk, Dorota Formanowicz, Piotr Formanowicz
Metabolites.2023; 13(12): 1191. CrossRef - Exploration of the Mechanism of the Comorbidity Relationship between Alzheimer’s Disease and Diabetes Mellitus
涛 温
Medical Diagnosis.2023; 13(04): 440. CrossRef - Postbiyotikler ve İnsülin Direnci
Betül SARIDAĞ DEVRAN, Mendane SAKA
Van Sağlık Bilimleri Dergisi.2023; 16(3): 268. CrossRef - The Anti-Diabetic Potential of Baicalin: Evidence from Rodent Studies
Tomasz Szkudelski, Katarzyna Szkudelska
International Journal of Molecular Sciences.2023; 25(1): 431. CrossRef - Clinical application of Momordica charantia (Bitter Melon) for reducing blood sugar in type 2 diabetes mellitus
Ashley Dahlquist, Dana Jandali, Mirielle C. Nauman, Jeremy J. Johnson, Sasho Stoleski
International Journal of Nutrition.2023; 7(4): 8. CrossRef - Alkaloids as Promising Agents for the Management of Insulin Resistance:
A Review
Ayoub Amssayef, Mohamed Eddouks
Current Pharmaceutical Design.2023; 29(39): 3123. CrossRef - Potential Mechanisms for How Long-Term Physical Activity May Reduce Insulin Resistance
Sindre Lee-Ødegård, Thomas Olsen, Frode Norheim, Christian Andre Drevon, Kåre Inge Birkeland
Metabolites.2022; 12(3): 208. CrossRef - Pathophysiological Link between Insulin Resistance and Adrenal Incidentalomas
Jordan A. Higgs, Alyssa P. Quinn, Kevin D. Seely, Zeke Richards, Shad P. Mortensen, Cody S. Crandall, Amanda E. Brooks
International Journal of Molecular Sciences.2022; 23(8): 4340. CrossRef - The Dose-Response Effects of Consuming High Fructose Corn Syrup-Sweetened Beverages on Hepatic Lipid Content and Insulin Sensitivity in Young Adults
Desiree M. Sigala, Bettina Hieronimus, Valentina Medici, Vivien Lee, Marinelle V. Nunez, Andrew A. Bremer, Chad L. Cox, Candice A. Price, Yanet Benyam, Yasser Abdelhafez, John P. McGahan, Nancy L. Keim, Michael I. Goran, Giovanni Pacini, Andrea Tura, Clau
Nutrients.2022; 14(8): 1648. CrossRef - Association of β-cell function and cognitive impairment in patients with abnormal glucose metabolism
Mengyi Guo, Jiaokun Jia, Jia Zhang, Mingyue Zhou, Anxin Wang, Shengyun Chen, Xingquan Zhao
BMC Neurology.2022;[Epub] CrossRef - The Role of Insulin Resistance in Fueling NAFLD Pathogenesis: From Molecular Mechanisms to Clinical Implications
Rossella Palma, Annamaria Pronio, Mario Romeo, Flavia Scognamiglio, Lorenzo Ventriglia, Vittorio Maria Ormando, Antonietta Lamazza, Stefano Pontone, Alessandro Federico, Marcello Dallio
Journal of Clinical Medicine.2022; 11(13): 3649. CrossRef - Crosstalk between Schizophrenia and Metabolic Syndrome: The Role of Oxytocinergic Dysfunction
Kah Kheng Goh, Cynthia Yi-An Chen, Tzu-Hua Wu, Chun-Hsin Chen, Mong-Liang Lu
International Journal of Molecular Sciences.2022; 23(13): 7092. CrossRef - TyG index is positively associated with risk of CHD and coronary atherosclerosis severity among NAFLD patients
Jianqi Zhao, Hongxuan Fan, Ting Wang, Bing Yu, Shaobin Mao, Xun Wang, Wenjing Zhang, Leigang Wang, Yao Zhang, Zhaoyu Ren, Bin Liang
Cardiovascular Diabetology.2022;[Epub] CrossRef - The Association of Acute Phase Proteins in Stress and Inflammation-Induced T2D
Tammy Speelman, Lieke Dale, Ann Louw, Nicolette J. D. Verhoog
Cells.2022; 11(14): 2163. CrossRef - Probiotic Mechanisms Affecting Glucose Homeostasis: A Scoping Review
Maša Pintarič, Tomaž Langerholc
Life.2022; 12(8): 1187. CrossRef - Potential Molecular Targets of Oleanolic Acid in Insulin Resistance and Underlying Oxidative Stress: A Systematic Review
Ángel Fernández-Aparicio, María Correa-Rodríguez, Jose M. Castellano, Jacqueline Schmidt-RioValle, Javier S. Perona, Emilio González-Jiménez
Antioxidants.2022; 11(8): 1517. CrossRef - Impact of Highly Saturated versus Unsaturated Fat Intake on Carbohydrate Metabolism and Vascular Reactivity in Rat
Youzan Ferdinand Djohan, Fabrice Raynaud, Karen Lambert, Jean-Paul Cristol, Charles Coudray, Christine Feillet-Coudray, Anne Virsolvy, Eric Badia, Néstor Gutiérrez-Méndez
Biochemistry Research International.2022; 2022: 1. CrossRef - Mitophagy: A potential therapeutic target for insulin resistance
Peng Ning, Xiaobo Jiang, Jing Yang, Jiaxing Zhang, Fan Yang, Hongyi Cao
Frontiers in Physiology.2022;[Epub] CrossRef - Higher neutrophil to lymphocyte ratio is associated with renal dysfunction and cardiac adverse remodeling in elderly with metabolic syndrome
Yuqi Zhu, Gang Li, Jari A. Laukkanen, Xing Song, Jing Zhang, Linping Wei, Xinrui Chen, Yufeng Li, Cheng Liu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Lipid droplet accumulation in β cells in patients with type 2 diabetes is associated with insulin resistance, hyperglycemia and β cell dysfunction involving decreased insulin granules
Tomomi Horii, Junji Kozawa, Yukari Fujita, Satoshi Kawata, Harutoshi Ozawa, Chisaki Ishibashi, Sho Yoneda, Takao Nammo, Jun-ichiro Miyagawa, Hidetoshi Eguchi, Iichiro Shimomura
Frontiers in Endocrinology.2022;[Epub] CrossRef - Comparing the long non-coding RNA expression profiles of skeletal muscle and kidney tissues from patients with diabetes
Young-Kook Kim, Takahiro Nemoto
PLOS ONE.2022; 17(9): e0274794. CrossRef - The CCR2+ Monocyte Subsets Increase in Obese Boys but Not Girls with Abnormally High Carotid Intima-Media Thickness: A Pilot Study
María José Garcés-Hernández, Karen Pedraza-Escudero, Nayely Garibay-Nieto, Joselin Hernández-Ruiz, Jessica Lakshmi Prieto-Chávez, Lourdes Andrea Arriaga-Pizano, Eréndira Villanueva-Ortega, Galileo Escobedo, Aaron Noe Manjarrez-Reyna, Juan Carlos López-Alv
Journal of Cardiovascular Development and Disease.2022; 9(10): 330. CrossRef - Effect of honey bee venom on the histological changes of testes and hormonal disturbance in diabetic mice
Sattar J. J. AL-Shaeli, Talal Jabal Hussen, Ali M. Ethaeb
Veterinary World.2022; : 2357. CrossRef - Establishment and Validation of a New Predictive Model for Insulin Resistance based on 2 Chinese Cohorts: A Cross-Sectional Study
Shi Zhang, Xin-Cheng Wang, Jing Li, Xiao-He Wang, Yi Wang, Yan-Ju Zhang, Mei-Yang Du, Min-Ying Zhang, Jing-Na Lin, Chun-Jun Li, Aman Rajpal
International Journal of Endocrinology.2022; 2022: 1. CrossRef - Zishen Pill alleviates diabetes in Db/db mice via activation of PI3K/AKT pathway in the liver
You Wu, Boju Sun, Xiaoyuan Guo, Lili Wu, Yaomu Hu, Lingling Qin, Tao Yang, Mei Li, Tianyu Qin, Miao Jiang, Tonghua Liu
Chinese Medicine.2022;[Epub] CrossRef - Effect of Insulin and Pioglitazone on Protein Phosphatase 2A Interaction Partners in Primary Human Skeletal Muscle Cells Derived from Obese Insulin-Resistant Participants
Lana Alghanem, Xiangmin Zhang, Ruchi Jaiswal, Berhane Seyoum, Abdullah Mallisho, Zaher Msallaty, Zhengping Yi
ACS Omega.2022; 7(47): 42763. CrossRef - Dietary Plant Protein Intake Can Reduce Maternal Insulin Resistance during Pregnancy
Yuting Hong, Chen Yang, Jinjing Zhong, Yanmei Hou, Kui Xie, Linlin Wang
Nutrients.2022; 14(23): 5039. CrossRef - Preventive effect of probiotics supplementation on occurrence of gestational diabetes mellitus: A systematic review and meta-analysis of randomized controlled trials
Azin Pakmehr, Hanieh-Sadat Ejtahed, Nooshin Shirzad, Mahboobeh Hemmatabadi, Sara Farhat, Bagher Larijani
Frontiers in Medicine.2022;[Epub] CrossRef - Insulin resistance in ischemic stroke: Mechanisms and therapeutic approaches
Peng-Fei Ding, Hua-Sheng Zhang, Jie Wang, Yong-Yue Gao, Jian-Nan Mao, Chun-Hua Hang, Wei Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - Long Noncoding RNAs in the Pathogenesis of Insulin Resistance
Weili Yang, Yixiang Lyu, Rui Xiang, Jichun Yang
International Journal of Molecular Sciences.2022; 23(24): 16054. CrossRef - Predictability of HOMA-IR for Gestational Diabetes Mellitus in Early Pregnancy Based on Different First Trimester BMI Values
Yanbei Duo, Shuoning Song, Yuemei Zhang, Xiaolin Qiao, Jiyu Xu, Jing Zhang, Zhenyao Peng, Yan Chen, Xiaorui Nie, Qiujin Sun, Xianchun Yang, Ailing Wang, Wei Sun, Yong Fu, Yingyue Dong, Zechun Lu, Tao Yuan, Weigang Zhao
Journal of Personalized Medicine.2022; 13(1): 60. CrossRef - MODERN CONCEPTS OF THE PATHOGENESIS OF TYPE 2 DIABETES MELLITUS
D.V. Kurkin, E.I. Morkovin, D.A. Bakulin, Yu.V. Gorbunova, A.V. Strygin, A.I. Robertus, I.E. Makarenko, V.B. Saparova, R.V. Drai, V.I. Petrov
Journal of Volgograd State Medical University.2022; 19(4): 34. CrossRef
- Diabetic Encephalopathy: Role of Oxidative and Nitrosative Factors in Type 2 Diabetes
- Guideline/Fact Sheet
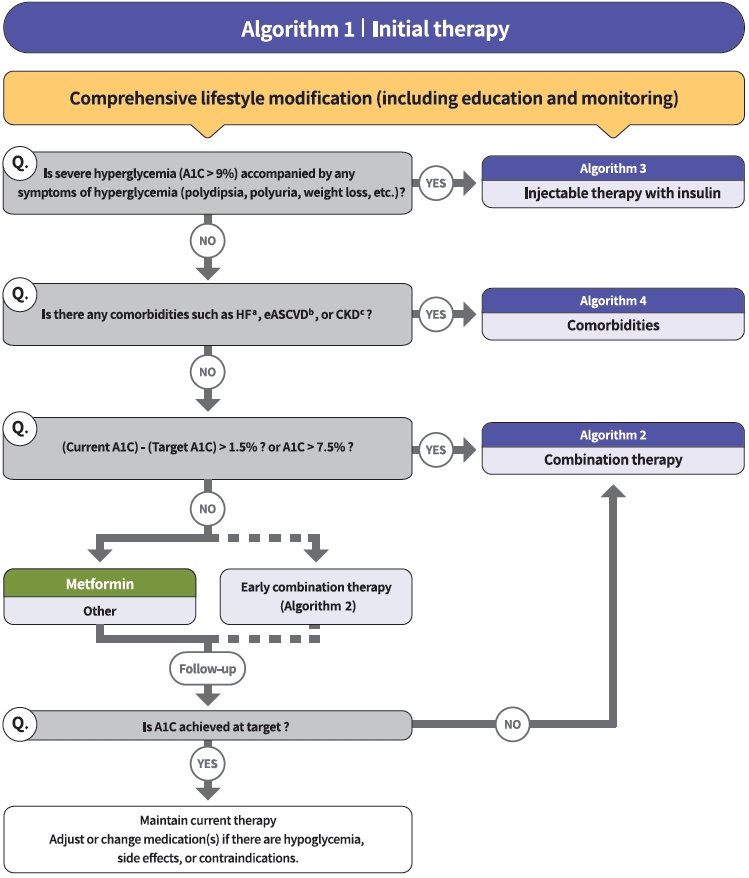
- 2021 Clinical Practice Guidelines for Diabetes Mellitus in Korea
- Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim, Sang Youl Rhee, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim, Chong Hwa Kim, Dae Jung Kim, SungWan Chun, Eun-Jung Rhee, Hyun Min Kim, Hyun Jung Kim, Donghyun Jee, Jae Hyun Kim, Won Seok Choi, Eun-Young Lee, Kun-Ho Yoon, Seung-Hyun Ko, Committee of Clinical Practice Guidelines, Korean Diabetes Association
- Diabetes Metab J. 2021;45(4):461-481. Published online July 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0156
- 23,956 View
- 1,626 Download
- 122 Web of Science
- 141 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 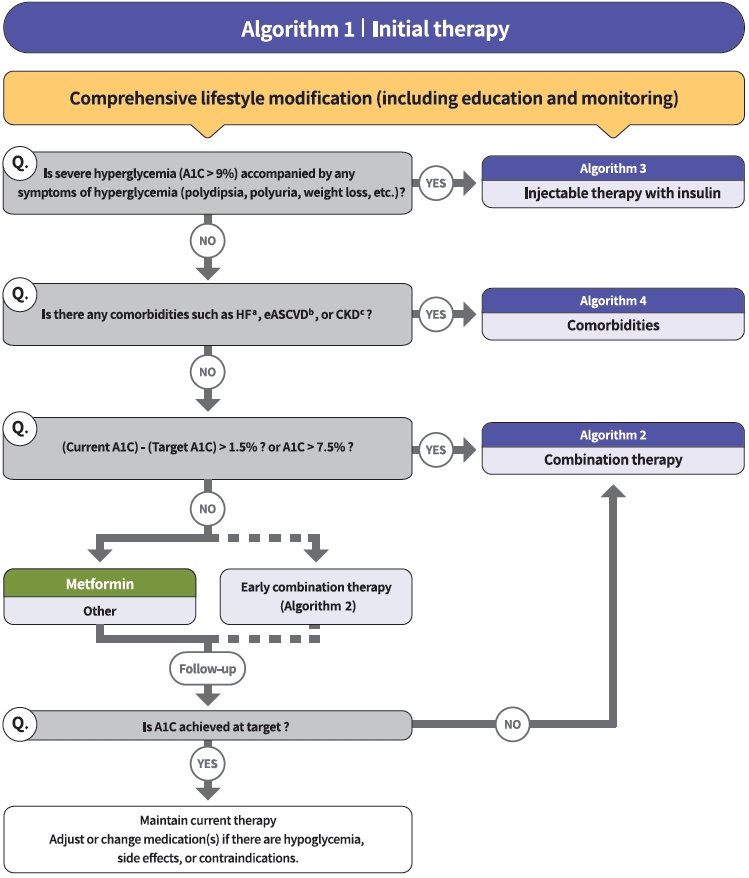
- The Committee of Clinical Practice Guidelines of the Korean Diabetes Association (KDA) updated the previous clinical practice guidelines for Korean adults with diabetes and prediabetes and published the seventh edition in May 2021. We performed a comprehensive systematic review of recent clinical trials and evidence that could be applicable in real-world practice and suitable for the Korean population. The guideline is provided for all healthcare providers including physicians, diabetes experts, and certified diabetes educators across the country who manage patients with diabetes or the individuals at the risk of developing diabetes mellitus. The recommendations for screening diabetes and glucose-lowering agents have been revised and updated. New sections for continuous glucose monitoring, insulin pump use, and non-alcoholic fatty liver disease in patients with diabetes mellitus have been added. The KDA recommends active vaccination for coronavirus disease 2019 in patients with diabetes during the pandemic. An abridgement that contains practical information for patient education and systematic management in the clinic was published separately.
-
Citations
Citations to this article as recorded by- Impact of Subclinical Atrial Function on the Prognosis of Patients With Atrial Fibrillation and Metabolic Syndrome
Hyun-Jin Kim
CardioMetabolic Syndrome Journal.2024; 4(1): 36. CrossRef - Associations of omega-3 fatty acids vs. fenofibrate with adverse cardiovascular outcomes in people with metabolic syndrome: propensity matched cohort study
Nam Hoon Kim, Ji Yoon Kim, Jimi Choi, Sin Gon Kim
European Heart Journal - Cardiovascular Pharmacotherapy.2024; 10(2): 118. CrossRef - A Multicenter, Randomized, Open-Label Study to Compare the Effects of Gemigliptin Add-on or Escalation of Metformin Dose on Glycemic Control and Safety in Patients with Inadequately Controlled Type 2 Diabetes Mellitus Treated with Metformin and SGLT-2 Inh
Hae Jin Kim, Jung Hyun Noh, Min Kyong Moon, Sung Hee Choi, Seung-Hyun Ko, Eun-Jung Rhee, Kyu Yeon Hur, In-Kyung Jeong, Mark Yorek
Journal of Diabetes Research.2024; 2024: 1. CrossRef - Efficacy and Safety of Once-Weekly Semaglutide Versus Once-Daily Sitagliptin as Metformin Add-on in a Korean Population with Type 2 Diabetes
Byung-Wan Lee, Young Min Cho, Sin Gon Kim, Seung-Hyun Ko, Soo Lim, Amine Dahaoui, Jin Sook Jeong, Hyo Jin Lim, Jae Myung Yu
Diabetes Therapy.2024; 15(2): 547. CrossRef - Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
Ji Yoon Kim, Sang-Man Jin, Sarah B. Andrade, Boyang Chen, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2024;[Epub] CrossRef - Association between Dyslipidemia and Glycated Hemoglobin in a Population-Based Study
Purum Kang, Ka Young Kim, Hye Young Shin
Metabolites.2024; 14(2): 92. CrossRef - Outcomes of Various Classes of Oral Antidiabetic Drugs on Nonalcoholic Fatty Liver Disease
Heejoon Jang, Yeonjin Kim, Dong Hyeon Lee, Sae Kyung Joo, Bo Kyung Koo, Soo Lim, Woojoo Lee, Won Kim
JAMA Internal Medicine.2024; 184(4): 375. CrossRef - View on Metformin: Antidiabetic and Pleiotropic Effects, Pharmacokinetics, Side Effects, and Sex-Related Differences
Guglielmina Froldi
Pharmaceuticals.2024; 17(4): 478. CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - Inhibition of sodium-glucose cotransporter-2 and liver-related complications in individuals with diabetes: a Mendelian randomization and population-based cohort study
Sung Won Chung, Hye-Sung Moon, Hyunjae Shin, Hyein Han, Sehoon Park, Heejin Cho, Jeayeon Park, Moon Haeng Hur, Min Kyung Park, Sung-Ho Won, Yun Bin Lee, Eun Ju Cho, Su Jong Yu, Dong Ki Kim, Jung-Hwan Yoon, Jeong-Hoon Lee, Yoon Jun Kim
Hepatology.2024;[Epub] CrossRef - Efficacy of intermittent short‐term use of a real‐time continuous glucose monitoring system in non‐insulin–treated patients with type 2 diabetes: A randomized controlled trial
Sun Joon Moon, Kyung‐Soo Kim, Woo Je Lee, Mi Yeon Lee, Robert Vigersky, Cheol‐Young Park
Diabetes, Obesity and Metabolism.2023; 25(1): 110. CrossRef - Therapeutic Effects of Switching to Anagliptin from Other DPP-4 Inhibitors in T2DM Patients with Inadequate Glycemic Control: A Non-interventional, Single-Arm, Open-Label, Multicenter Observational Study
Sang-Yong Kim, Sungrae Kim
Diabetes Therapy.2023; 14(1): 109. CrossRef - Low Skeletal Muscle Mass Accompanied by Abdominal Obesity Additively Increases the Risk of Incident Type 2 Diabetes
Ji Eun Jun, Seung-Eun Lee, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Jae Hwan Jee, Jae Hyeon Kim
The Journal of Clinical Endocrinology & Metabolism.2023; 108(5): 1173. CrossRef - Diabetes screening in South Korea: a new estimate of the number needed to screen to detect diabetes
Kyoung Hwa Ha, Kyung Ae Lee, Kyung-Do Han, Min Kyong Moon, Dae Jung Kim
The Korean Journal of Internal Medicine.2023; 38(1): 93. CrossRef - Justicia carnea extracts ameliorated hepatocellular damage in streptozotocin-induced type 1 diabetic male rats via decrease in oxidative stress, inflammation and increasing other risk markers
John Adeolu Falode, Oluwaseun Igbekele Ajayi, Tolulope Victoria Isinkaye, Akinwunmi Oluwaseun Adeoye, Basiru Olaitan Ajiboye, Bartholomew I. C. Brai
Biomarkers.2023; 28(2): 177. CrossRef - Sex differences in the impact of diabetes mellitus on tuberculosis recurrence: a retrospective national cohort study
Dararat Eksombatchai, Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Hongjo Choi, Young Ae Kang
International Journal of Infectious Diseases.2023; 127: 1. CrossRef - The Predictive Ability of C-Peptide in Distinguishing Type 1 Diabetes From Type 2 Diabetes: A Systematic Review and Meta-Analysis
Sajid Iqbal, Abdulrahim Abu Jayyab, Ayah Mohammad Alrashdi, Silvia Reverté-Villarroya
Endocrine Practice.2023; 29(5): 379. CrossRef - Anagliptin twice‐daily regimen improves glycaemic variability in subjects with type 2 diabetes: A double‐blind, randomized controlled trial
Yong‐ho Lee, Doo‐Man Kim, Jae Myung Yu, Kyung Mook Choi, Sin Gon Kim, Kang Seo Park, Hyun‐Shik Son, Choon Hee Chung, Kyu Jeung Ahn, Soon Hee Lee, Ki‐Ho Song, Su Kyoung Kwon, Hyeong Kyu Park, Kyu Chang Won, Hak Chul Jang
Diabetes, Obesity and Metabolism.2023; 25(5): 1174. CrossRef - Implementation of five machine learning methods to predict the 52-week blood glucose level in patients with type 2 diabetes
Xiaomin Fu, Yuhan Wang, Ryan S. Cates, Nan Li, Jing Liu, Dianshan Ke, Jinghua Liu, Hongzhou Liu, Shuangtong Yan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - The Efficacy of Treatment Intensification by Quadruple Oral Therapy Compared to GLP-1RA Therapy in Poorly Controlled Type 2 Diabetes Mellitus Patients: A Real-world Data Study
Minyoung Kim, Hosu Kim, Kyong Young Kim, Soo Kyoung Kim, Junghwa Jung, Jong Ryeal Hahm, Jaehoon Jung, Jong Ha Baek
Diabetes & Metabolism Journal.2023; 47(1): 135. CrossRef - Safety and Effectiveness of Empagliflozin in Korean Patients with Type 2 Diabetes Mellitus: Results from a Nationwide Post-Marketing Surveillance
Jun Sung Moon, Nam Hoon Kim, Jin Oh Na, Jae Hyoung Cho, In-Kyung Jeong, Soon Hee Lee, Ji-Oh Mok, Nan Hee Kim, Dong Jin Chung, Jinhong Cho, Dong Woo Lee, Sun Woo Lee, Kyu Chang Won
Diabetes & Metabolism Journal.2023; 47(1): 82. CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Influenza vaccination trend and related factors among patients with diabetes in Korea: Analysis using a nationwide database
Dong-Hwa Lee, Bumhee Yang, Seonhye Gu, Eung-Gook Kim, Youlim Kim, Hyung Koo Kang, Yeong Hun Choe, Hyun Jeong Jeon, Seungyong Park, Hyun Lee
Frontiers in Endocrinology.2023;[Epub] CrossRef - Optimal Low-Density Lipoprotein Cholesterol Level for Primary Prevention in Koreans with Type 2 Diabetes Mellitus
Ji Yoon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(1): 42. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Association between Low-Density Lipoprotein Cholesterol Level and Cardiovascular Outcomes in Korean Adults: A Nationwide Cohort Study
Junghyun Noh, Min Kyong Moon, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(1): 59. CrossRef - Analysis of the Incidence of Type 2 Diabetes, Requirement of Insulin Treatment, and Diabetes-Related Complications among Patients with Cancer
Su Jung Lee, Chulho Kim, Hyunjae Yu, Dong-Kyu Kim
Cancers.2023; 15(4): 1094. CrossRef - The 2022 focused update of the 2018 Korean Hypertension Society Guidelines for the management of hypertension
Hack-Lyoung Kim, Eun Mi Lee, Shin Young Ahn, Kwang-il Kim, Hyeon Chang Kim, Ju Han Kim, Hae-Young Lee, Jang Hoon Lee, Jong-Moo Park, Eun Joo Cho, Sungha Park, Jinho Shin, Young-Kwon Kim
Clinical Hypertension.2023;[Epub] CrossRef - Consistency of 1-day and 3-day average dietary intake and the relationship of dietary intake with blood glucose, hbA1c, BMI, and lipids in patients with type 2 diabetes
DaeEun Lee, Haejung Lee, Sangeun Lee, MinJin Lee, Ah Reum Khang
Journal of Korean Biological Nursing Science.2023; 25(1): 20. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Effect of olmesartan and amlodipine on serum angiotensin-(1–7) levels and kidney and vascular function in patients with type 2 diabetes and hypertension
Kyuho Kim, Ji Hye Moon, Chang Ho Ahn, Soo Lim
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Menopausal hormone therapy and the risk of type 2 diabetes mellitus: Health Insurance Database in South Korea–based retrospective cohort study
Jin-Sung Yuk, Jung Min Kim
Menopause.2023; 30(5): 497. CrossRef - Intensified Multifactorial Intervention in Patients with Type 2 Diabetes Mellitus
Takayoshi Sasako, Toshimasa Yamauchi, Kohjiro Ueki
Diabetes & Metabolism Journal.2023; 47(2): 185. CrossRef - Association between antidiabetic drugs and the incidence of atrial fibrillation in patients with type 2 diabetes: A nationwide cohort study in South Korea
Sunyoung Kim, So Young Park, Bongseong Kim, Chanyang Min, Wonyoung Cho, Dong Keon Yon, Joo Young Kim, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee, Sang Youl Rhee
Diabetes Research and Clinical Practice.2023; 198: 110626. CrossRef - Totally robotic Roux-en-Y gastric bypass in a morbidly obese patient in Korea: a case report
Ji Won Seo, Kyong-Hwa Jun
Journal of Minimally Invasive Surgery.2023; 26(1): 40. CrossRef - Effect of diabetes-specific oral nutritional supplements with allulose on weight and glycemic profiles in overweight or obese type 2 diabetic patients
Jihye Tak, Minkyung Bok, Hyunkyung Rho, Ju Hyun Park, Yunsook Lim, Suk Chon, Hyunjung Lim
Nutrition Research and Practice.2023; 17(2): 241. CrossRef - Associations Between Modifiable Risk Factors and Changes in Glycemic Status Among Individuals With Prediabetes
Salma Nabila, Ji-Eun Kim, Jaesung Choi, JooYong Park, Aesun Shin, Sang-Ah Lee, Jong-koo Lee, Daehee Kang, Ji-Yeob Choi
Diabetes Care.2023; 46(3): 535. CrossRef - Efficacy and safety of enavogliflozin, a novel SGLT2 inhibitor, in Korean people with type 2 diabetes: A 24‐week, multicentre, randomized, double‐blind, placebo‐controlled, phase III trial
Soo Heon Kwak, Kyung Ah Han, Kyung‐Soo Kim, Jae Myung Yu, EunSook Kim, Jong Chul Won, Jun Goo Kang, Choon Hee Chung, Seungjoon Oh, Sung Hee Choi, Kyu Chang Won, Sin Gon Kim, Seung Ah Cho, Bo Young Cho, Kyong Soo Park
Diabetes, Obesity and Metabolism.2023; 25(7): 1865. CrossRef - Adjusting the Use of Glucose-Lowering Agents in the Real-World Clinical Management of People with Type 2 Diabetes: A Narrative Review
Siew Pheng Chan, Lee-Ling Lim, Juliana C. N. Chan, David R. Matthews
Diabetes Therapy.2023; 14(5): 823. CrossRef - The association of perfluoroalkyl substances (PFAS) exposure and kidney function in Korean adolescents using data from Korean National Environmental Health Survey (KoNEHS) cycle 4 (2018–2020): a cross-sectional study
Jisuk Yun, Eun-Chul Jang, Soon-Chan Kwon, Young-Sun Min, Yong-Jin Lee
Annals of Occupational and Environmental Medicine.2023;[Epub] CrossRef - A Comparison of the Pharmacokinetics and Safety of Dapagliflozin Formate, an Ester Prodrug of Dapagliflozin, to Dapagliflozin Propanediol Monohydrate in Healthy Subjects
Hyun Chul Kim, Sangmi Lee, Siyoung Sung, Eunjin Kim, In-Jin Jang, Jae-Yong Chung
Drug Design, Development and Therapy.2023; Volume 17: 1203. CrossRef - Efficacy and safety of monotherapy with enavogliflozin in Korean patients with type 2 diabetes mellitus: Results of a 12‐week, multicentre, randomized, double‐blind, placebo‐controlled, phase 2 trial
Ye Seul Yang, Kyung Wan Min, Seok‐O Park, Kyung‐Soo Kim, Jae Myung Yu, Eun‐Gyoung Hong, Sung Rae Cho, Kyu Chang Won, Yong Hyun Kim, Seungjoon Oh, Sung Hee Choi, Gwanpyo Koh, Wan Huh, Su Young Kim, Kyong Soo Park
Diabetes, Obesity and Metabolism.2023; 25(8): 2096. CrossRef - An Integrated Digital Health Care Platform for Diabetes Management With AI-Based Dietary Management: 48-Week Results From a Randomized Controlled Trial
You-Bin Lee, Gyuri Kim, Ji Eun Jun, Hyunjin Park, Woo Je Lee, You-Cheol Hwang, Jae Hyeon Kim
Diabetes Care.2023; 46(5): 959. CrossRef - Performance of Simple Fibrosis Score in Non-Alcoholic Fatty Liver Disease with and without Type 2 Diabetes
Seung Min Chung, Min Kyu Kang, Jun Sung Moon, Jung Gil Park
Endocrinology and Metabolism.2023; 38(2): 277. CrossRef - Correlation analysis of cancer incidence after pravastatin treatment
Jin Yu, Raeun Kim, Jiwon Shinn, Man Young Park, Hun-Sung Kim
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 61. CrossRef - Comparison of the effects of gemigliptin versus glimepiride on cardiac function in patients with type 2 diabetes uncontrolled with metformin: The gemi‐heart study
Seung Min Chung, Jun Sung Moon, Jun Hwa Hong, In‐Chang Hwang, Soo Lim
Diabetes, Obesity and Metabolism.2023; 25(8): 2181. CrossRef - The era of continuous glucose monitoring and its expanded role in type 2 diabetes
Jin Yu, Jae‐Hyoung Cho, Seung‐Hwan Lee
Journal of Diabetes Investigation.2023; 14(7): 841. CrossRef - Impact of continuous glucose monitoring on glycemic control and its derived metrics in type 1 diabetes: a longitudinal study
So Hyun Cho, Seohyun Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Gyuri Kim, Jae Hyeon Kim
Frontiers in Endocrinology.2023;[Epub] CrossRef - Impact of mental disorders on the risk of heart failure among Korean patients with diabetes: a cohort study
Tae Kyung Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Diabetology.2023;[Epub] CrossRef - Asia-Pacific consensus recommendations for application of continuous glucose monitoring in diabetes management
Alice P.S. Kong, Soo Lim, Seung-Hyun Yoo, Linong Ji, Liming Chen, Yuqian Bao, Ester Yeoh, Siew-Pheng Chan, Chih-Yuan Wang, Viswanathan Mohan, Neale Cohen, Margaret J. McGill, Stephen M. Twigg
Diabetes Research and Clinical Practice.2023; 201: 110718. CrossRef - Chronic disease management program applied to type 2 diabetes patients and prevention of diabetic complications: a retrospective cohort study using nationwide data
Min Kyung Hyun, Jang Won Lee, Seung-Hyun Ko
BMC Public Health.2023;[Epub] CrossRef - Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(3): 347. CrossRef - Opening the Precision Diabetes Care through Digital Healthcare
Joonyub Lee, Jin Yu, Kun-Ho Yoon
Diabetes & Metabolism Journal.2023; 47(3): 307. CrossRef - Glycemia according to the Use of Continuous Glucose Monitoring among Adults with Type 1 Diabetes Mellitus in Korea: A Real-World Study
You-Bin Lee, Minjee Kim, Jae Hyeon Kim
Diabetes & Metabolism Journal.2023; 47(3): 405. CrossRef - Navigating the Seas of Glycemic Control: The Role of Continuous Glucose Monitoring in Type 1 Diabetes Mellitus
Jun Sung Moon
Diabetes & Metabolism Journal.2023; 47(3): 345. CrossRef - Lost in translation: assessing the nomenclature change for diabetic kidney disease in Japan
Tetsuya Babazono, Tatsumi Moriya
Diabetology International.2023; 14(4): 319. CrossRef - Effects of dapagliflozin compared with glimepiride on body composition in Asian patients with type 2 diabetes inadequately controlled with metformin: The BEYOND study
Hyeong Kyu Park, Kyoung‐Ah Kim, Kyung‐Wan Min, Tae‐Seo Sohn, In Kyung Jeong, Chul Woo Ahn, Nan‐Hee Kim, Ie Byung Park, Ho Chan Cho, Choon Hee Chung, Sung Hee Choi, Kang Seo Park, Seoung‐Oh Yang, Kwan Woo Lee
Diabetes, Obesity and Metabolism.2023; 25(9): 2743. CrossRef - Topic Modeling Analysis of Diabetes-Related Health Information during the Coronavirus Disease Pandemic
Soyoon Min, Jeongwon Han
Healthcare.2023; 11(13): 1871. CrossRef - Screening Test for Evaluation of Cardiovascular Disease in Patients with Diabetes
Ji-Oh Mok, Chan-Hee Jung
The Journal of Korean Diabetes.2023; 24(2): 76. CrossRef - Paradigm Shift in Management of Hyperglycemia in Patients with Type 2 Diabetes: Glucocentric versus Organ Protection
Jong Chul Won
The Journal of Korean Diabetes.2023; 24(2): 59. CrossRef - Association between type 2 diabetes mellitus and depression among Korean midlife women: a cross-sectional analysis study
You Lee Yang, Eun-Ok Im, Yunmi Kim
BMC Nursing.2023;[Epub] CrossRef - Fibrotic Burden in the Liver Differs Across Metabolic Dysfunction-Associated Fatty Liver Disease Subtypes
Tae Seop Lim, Ho Soo Chun, Soon Sun Kim, Ja Kyung Kim, Minjong Lee, Hyo Jung Cho, Seung Up Kim, Jae Youn Cheong
Gut and Liver.2023; 17(4): 610. CrossRef - Association between the number of pregnancies and cardiac target organ damages: a cross-sectional analysis of data from the Korean women’s chest pain registry (KoROSE)
Hack-Lyoung Kim, Hyun-Jin Kim, Mina Kim, Sang Min Park, Hyun Ju Yoon, Young Sup Byun, Seong-Mi Park, Mi-Seung Shin, Kyung-Soon Hong, Myung-A Kim
BMC Women's Health.2023;[Epub] CrossRef - Exercise therapy for diabetes mellitus
Chaiho Jeong, Tae-Seo Sohn
Journal of the Korean Medical Association.2023; 66(7): 427. CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef - Identification of individuals at risk of hepatocellular carcinoma: screening for clinically significant liver fibrosis in patients with T2DM
Tina Reinson, Ryan M Buchanan, Christopher D Byrne
Expert Review of Endocrinology & Metabolism.2023; 18(5): 355. CrossRef - Additive impact of diabetes and sarcopenia on all-cause and cardiovascular mortality: A longitudinal nationwide population-based study
Eyun Song, Soon Young Hwang, Min Jeong Park, Ahreum Jang, Kyeong Jin Kim, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Metabolism.2023; 148: 155678. CrossRef - Exposure to perfluoroalkyl and polyfluoroalkyl substances and risk of stroke in adults: a meta-analysis
Min Cheol Chang, Seung Min Chung, Sang Gyu Kwak
Reviews on Environmental Health.2023;[Epub] CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Incident infection risks depending on oral antidiabetic exposure in insulin-treated type 2 diabetes patients
Sanghwa Park, Jiseon Jeong, Yunna Woo, Yeo Jin Choi, Sooyoung Shin
Scientific Reports.2023;[Epub] CrossRef - Dyslipidemia Fact Sheet in South Korea, 2022
Eun-Sun Jin, Jee-Seon Shim, Sung Eun Kim, Jae Hyun Bae, Shinae Kang, Jong Chul Won, Min-Jeong Shin, Heung Yong Jin, Jenny Moon, Hokyou Lee, Hyeon Chang Kim, In-Kyung Jeong
Journal of Lipid and Atherosclerosis.2023; 12(3): 237. CrossRef - Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
Diabetes & Metabolism Journal.2023; 47(5): 643. CrossRef - Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD): A State-of-the-Art Review
Wah-Kheong Chan, Kee-Huat Chuah, Ruveena Bhavani Rajaram, Lee-Ling Lim, Jeyakantha Ratnasingam, Shireene Ratna Vethakkan
Journal of Obesity & Metabolic Syndrome.2023; 32(3): 197. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - 2023 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk Factors
Ye Seul Yang
The Journal of Korean Diabetes.2023; 24(3): 135. CrossRef - Dyslipidemia Fact Sheet in South Korea, 2022
Eun-Sun Jin, Jee-Seon Shim, Sung Eun Kim, Jae Hyun Bae, Shinae Kang, Jong Chul Won, Min-Jeong Shin, Heung Yong Jin, Jenny Moon, Hokyou Lee, Hyeon Chang Kim, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(5): 632. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Riesgo residual. Conclusiones
Ángel Cequier, José Luis Zamorano
Revista Española de Cardiología Suplementos.2023; 23: 25. CrossRef - Intake of Fruit and Glycemic Control in Korean Patients with Diabetes Mellitus Using the Korea National Health and Nutrition Examination Survey
Eunju Yoon, Ji Cheol Bae, Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 538. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef - Coleus forskohlii Root Extract (ForcslimTM) as a Prospective Antidiabetic Agent: In vitro Glucose Uptake Stimulation and α-Amylase Inhibitory Effects
Firoz Hirehal Hussain Mi, Channangihalli Thimmegowda Sadashiva, Neethumol Benny, Sreedrisya Ayippakkari Kuttiattu, Ravi Subban
International Journal of Pharmacology.2023; 19(5): 730. CrossRef - Comparison of on-Statin Lipid and Lipoprotein Levels for the Prediction of First Cardiovascular Event in Type 2 Diabetes Mellitus
Ji Yoon Kim, Jimi Choi, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2023; 47(6): 837. CrossRef - Differential Impact of Obesity on the Risk of Diabetes Development in Two Age Groups: Analysis from the National Health Screening Program
Tae Kyung Yoo, Kyung-Do Han, Yang-Hyun Kim, Ga Eun Nam, Sang Hyun Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2023; 47(6): 846. CrossRef - Strategies to Maintain the Remission of Diabetes Following Metabolic Surgery
Mi Kyung Kim, Hye Soon Kim
Journal of Metabolic and Bariatric Surgery.2023; 12(2): 26. CrossRef - East Asian perspectives in metabolic and bariatric surgery
Tae Jung Oh, Hyuk‐Joon Lee, Young Min Cho
Journal of Diabetes Investigation.2022; 13(5): 756. CrossRef - Recent Updates to Clinical Practice Guidelines for Diabetes Mellitus
Jin Yu, Seung-Hwan Lee, Mee Kyoung Kim
Endocrinology and Metabolism.2022; 37(1): 26. CrossRef - Association between Physical Exercise and Glycated Hemoglobin Levels in Korean Patients Diagnosed with Diabetes
Il Yun, Hye Jin Joo, Yu Shin Park, Eun-Cheol Park
International Journal of Environmental Research and Public Health.2022; 19(6): 3280. CrossRef - Effectiveness and safety of teneligliptin added to patients with type 2 diabetes inadequately controlled by oral triple combination therapy: A multicentre, randomized, double‐blind, and placebo‐controlled study
Minyoung Lee, Woo‐je Lee, Jae Hyeon Kim, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(6): 1105. CrossRef - Trends of severe hypoglycemia in patients with type 2 diabetes in Korea: A longitudinal nationwide cohort study
Jae‐Seung Yun, Kyungdo Han, Seung‐Hyun Ko
Journal of Diabetes Investigation.2022; 13(8): 1438. CrossRef - GLP-1 receptor agonists in diabetic kidney disease: current evidence and future directions
Ji Hee Yu, So Young Park, Da Young Lee, Nan Hee Kim, Ji A Seo
Kidney Research and Clinical Practice.2022; 41(2): 136. CrossRef - Cardiorenal Risk Profiles Among Data-Driven Type 2 Diabetes Sub-Phenotypes: A Post-Hoc Analysis of the China Health and Nutrition Survey
Hui Gao, Kan Wang, Wensui Zhao, Jianlin Zhuang, Yu Jiang, Lei Zhang, Qingping Liu, Fariba Ahmadizar
Frontiers in Endocrinology.2022;[Epub] CrossRef - Individualized Medical Nutrition Therapy for Diabetic Patients according to Diabetes Medication
Juyeon Park
The Journal of Korean Diabetes.2022; 23(1): 50. CrossRef - Critical shear stress of red blood cells as a novel integrated biomarker for screening chronic kidney diseases in cases of type 2 diabetes
Il Rae Park, Jimi Choi, Eun Young Ha, Seung Min Chung, Jun Sung Moon, Sehyun Shin, Sin Gon Kim, Kyu Chang Won
Clinical Hemorheology and Microcirculation.2022; 81(4): 293. CrossRef - Effects of exercise on reducing diabetes risk in Korean women according to menopausal status
Jung-Hwan Cho, Hye-Mi Kwon, Se-Eun Park, Ju-Hwan Yoo, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2022; 4(2): 75. CrossRef - Novel Glycemic Index Based on Continuous Glucose Monitoring to Predict Poor Clinical Outcomes in Critically Ill Patients: A Pilot Study
Eun Yeong Ha, Seung Min Chung, Il Rae Park, Yin Young Lee, Eun Young Choi, Jun Sung Moon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Free Versus Fixed-Ratio Combination of Basal Insulin and GLP-1 Receptor Agonists in Type 2 Diabetes Uncontrolled With GLP-1 Receptor Agonists: A Systematic Review and Indirect Treatment Comparison
Han Na Jung, Yun Kyung Cho, Se Hee Min, Hwi Seung Kim, Ye-Jee Kim, Joong-Yeol Park, Woo Je Lee, Chang Hee Jung
Frontiers in Endocrinology.2022;[Epub] CrossRef - Obesity, hypertension, diabetes mellitus, and hypercholesterolemia in Korean adults before and during the COVID-19 pandemic: a special report of the 2020 Korea National Health and Nutrition Examination Survey
Ga Bin Lee, Yoonjung Kim, Suyeon Park, Hyeon Chang Kim, Kyungwon Oh
Epidemiology and Health.2022; 44: e2022041. CrossRef - Adherence to healthy lifestyle behaviors as a preventable risk factor for severe hypoglycemia in people with type 2 diabetes: A longitudinal nationwide cohort study
Jae‐Seung Yun, Kyungdo Han, Yong‐Moon Park, Eugene Han, Yong‐ho Lee, Seung‐Hyun Ko
Journal of Diabetes Investigation.2022; 13(9): 1533. CrossRef - Diabetes Fact Sheet in Korea 2021
Jae Hyun Bae, Kyung-Do Han, Seung-Hyun Ko, Ye Seul Yang, Jong Han Choi, Kyung Mook Choi, Hyuk-Sang Kwon, Kyu Chang Won
Diabetes & Metabolism Journal.2022; 46(3): 417. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Diabetes & Metabolism Journal.2022; 46(3): 355. CrossRef - Effect of carbohydrate-restricted diets and intermittent fasting on obesity, type 2 diabetes mellitus, and hypertension management: consensus statement of the Korean Society for the Study of obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Clinical Hypertension.2022;[Epub] CrossRef - Efficacy of Personalized Diabetes Self-care Using an Electronic Medical Record–Integrated Mobile App in Patients With Type 2 Diabetes: 6-Month Randomized Controlled Trial
Eun Young Lee, Seon-Ah Cha, Jae-Seung Yun, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Min Kyung Hyun, Seung-Hyun Ko
Journal of Medical Internet Research.2022; 24(7): e37430. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Hypoglycemic agents and glycemic variability in individuals with type 2 diabetes: A systematic review and network meta-analysis
SuA Oh, Sujata Purja, Hocheol Shin, Minji Kim, Eunyoung Kim
Diabetes and Vascular Disease Research.2022; 19(3): 147916412211068. CrossRef - Tolerability and Effectiveness of Switching to Dulaglutide in Patients With Type 2 Diabetes Inadequately Controlled With Insulin Therapy
Youngsook Kim, Ji Hye Huh, Minyoung Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef - Factors Influencing the Utilization of Diabetes Complication Tests Under the COVID-19 Pandemic: Machine Learning Approach
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Association of prediabetes with death and diabetic complications in older adults: the pros and cons of active screening for prediabetes
Giwoong Choi, Hojun Yoon, Hyun Ho Choi, Kyoung Hwa Ha, Dae Jung Kim
Age and Ageing.2022;[Epub] CrossRef - Recent information on test utilization and intraindividual change in anti-glutamic acid decarboxylase antibody in Korea: a retrospective study
Rihwa Choi, Wonseo Park, Gayoung Chun, Jiwon Lee, Sang Gon Lee, Eun Hee Lee
BMJ Open Diabetes Research & Care.2022; 10(3): e002739. CrossRef - Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(3): 415. CrossRef - Pharmacological Treatment of Nonalcoholic Fatty Liver Disease: Antidiabetic Agents
Kyung-Soo Kim
The Journal of Korean Diabetes.2022; 23(2): 83. CrossRef - Maintaining Physical Activity Is Associated with Reduced Major Adverse Cardiovascular Events in People Newly Diagnosed with Diabetes
Duhoe Kim, Jaehun Seo, Kyoung Hwa Ha, Dae Jung Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 187. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 100. CrossRef - Advanced Glycation End Products and Their Effect on Vascular Complications in Type 2 Diabetes Mellitus
Jeongmin Lee, Jae-Seung Yun, Seung-Hyun Ko
Nutrients.2022; 14(15): 3086. CrossRef - Severe hypoglycemia as a risk factor for cardiovascular outcomes in patients with type 2 diabetes: is it preventable?
Seung-Hyun Ko
Cardiovascular Prevention and Pharmacotherapy.2022; 4(3): 106. CrossRef - New, Novel Lipid-Lowering Agents for Reducing Cardiovascular Risk: Beyond Statins
Kyuho Kim, Henry N. Ginsberg, Sung Hee Choi
Diabetes & Metabolism Journal.2022; 46(4): 517. CrossRef - Current status of obesity treatment in Korea: based on the 2020 Korean Society for the Study of Obesity guidelines for obesity management
Eun-Jung Rhee
Journal of the Korean Medical Association.2022; 65(7): 388. CrossRef - Experiences of Using Wearable Continuous Glucose Monitors in Adults With Diabetes: A Qualitative Descriptive Study
Hee Sun Kang, Hyang Rang Park, Chun-Ja Kim, Savitri Singh-Carlson
The Science of Diabetes Self-Management and Care.2022; 48(5): 362. CrossRef - 젊은 2형 당뇨병 환자의 관리
재현 배
Public Health Weekly Report.2022; 15(35): 2474. CrossRef - Real-World Prescription Patterns and Barriers Related to the Use of Sodium-Glucose Cotransporter 2 Inhibitors among Korean Patients with Type 2 Diabetes Mellitus and Cardiovascular Disease
Jong Ha Baek, Ye Seul Yang, Seung-Hyun Ko, Kyung Do Han, Jae Hyeon Kim, Min Kyong Moon, Jong Suk Park, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Jong Han Choi, Kyu Yeon Hur
Diabetes & Metabolism Journal.2022; 46(5): 701. CrossRef - Low-Density Lipoprotein Cholesterol Level, Statin Use and Myocardial Infarction Risk in Young Adults
Heekyoung Jeong, Kyungdo Han, Soon Jib Yoo, Mee Kyoung Kim
Journal of Lipid and Atherosclerosis.2022; 11(3): 288. CrossRef - Blood Pressure Target in Type 2 Diabetes Mellitus
Hyun-Jin Kim, Kwang-il Kim
Diabetes & Metabolism Journal.2022; 46(5): 667. CrossRef - Association of underweight status with the risk of tuberculosis: a nationwide population-based cohort study
Su Hwan Cho, Hyun Lee, Hyuktae Kwon, Dong Wook Shin, Hee-Kyung Joh, Kyungdo Han, Jin Ho Park, Belong Cho
Scientific Reports.2022;[Epub] CrossRef - Exploring the risk factors of impaired fasting glucose in middle-aged population living in South Korean communities by using categorical boosting machine
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - External validation and clinical application of the predictive model for severe hypoglycemia
Jae-Seung Yun, Kyungdo Han, Soo-Yeon Choi, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effect of Euonymus alatus Extracts on Diabetes Related Markers in Pancreatic β-Cells and C57BL/Ksj-db/db Mice
Ye Rin Kim, Eun-young Kim, Seong Uk Lee, Young Wan Kim, Yoon Hee Kim
Journal of the Korean Society of Food Science and Nutrition.2022; 51(9): 894. CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Correlation between shift work and non-alcoholic fatty liver disease among male workers in the steel manufacturing company of Korea: a cross-sectional study
Kiseok Kim, Yong-Jin Lee, Soon-Chan Kwon, Young-Sun Min, Hyun Kyo Lee, Gwangin Baek, Sang Hyeon Kim, Eun-Chul Jang
Annals of Occupational and Environmental Medicine.2022;[Epub] CrossRef - FGM-based remote intervention for adults with type 1 diabetes: The FRIEND randomized clinical trial
Jinju Lee, Myeong Hoon Lee, Jiyun Park, Kyung-Soo Kim, Soo-Kyung Kim, Yong-Wook Cho, Hyun Wook Han, Young Shin Song
Frontiers in Endocrinology.2022;[Epub] CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Blood Pressure Control in Patients with Diabetic Kidney Disease
Yaeni Kim, Won Kim, Jwa-Kyung Kim, Ju Young Moon, Samel Park, Cheol Whee Park, Hoon Suk Park, Sang Heon Song, Tae-Hyun Yoo, So-Young Lee, Eun Young Lee, Jeonghwan Lee, Kyubok Jin, Dae Ryong Cha, Jin Joo Cha, Sang Youb Han
Electrolytes & Blood Pressure.2022; 20(2): 39. CrossRef - The Gangwon Obesity and Metabolic Syndrome Study: Methods and Initial Baseline Data
Yoon Jeong Cho, Sohyun Park, Sung Soo Kim, Hyo Jin Park, Jang Won Son, Tae Kyung Lee, Sangmo Hong, Jee-Hyun Kang, Seon Mee Kim, Yang-Hyun Kim, Won Jun Kim, Young Eun Seo, Yoosuk An, Sang Youl Rhee, Suk Chon, Sookyoung Jeon, Kyungho Park, Bong-Soo Kim, Cha
Journal of Obesity & Metabolic Syndrome.2022; 31(4): 303. CrossRef - Oral Semaglutide, the First Ingestible Glucagon-Like Peptide-1 Receptor Agonist: Could It Be a Magic Bullet for Type 2 Diabetes?
Hwi Seung Kim, Chang Hee Jung
International Journal of Molecular Sciences.2021; 22(18): 9936. CrossRef - Long-term effectiveness and safety of quadruple combination therapy with empagliflozin versus dapagliflozin in patients with type 2 diabetes: 3-year prospective observational study
Eu Jeong Ku, Dong-Hwa Lee, Hyun Jeong Jeon, Tae Keun Oh
Diabetes Research and Clinical Practice.2021; 182: 109123. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2021;45:698-707)
Mi-kyung Kim
Diabetes & Metabolism Journal.2021; 45(6): 968. CrossRef - Incidence and Risk Factors for Progression to Diabetes Mellitus: A Retrospective Cohort Study
Min Kyung Hyun, Jong Heon Park, Kyoung Hoon Kim, Soon-Ki Ahn, Seon Mi Ji
International Journal of Environmental Research and Public Health.2021; 19(1): 123. CrossRef - 2021 Clinical Practice Guidelines for Diabetes: Pharmacotherapy and the Korean Diabetes Association Support System
Kyu Yeon Hur
The Journal of Korean Diabetes.2021; 22(4): 250. CrossRef - 2021 Clinical Practice Guidelines for Diabetes: Management of Cardiovascular Risk
Min Kyong Moon
The Journal of Korean Diabetes.2021; 22(4): 259. CrossRef
- Impact of Subclinical Atrial Function on the Prognosis of Patients With Atrial Fibrillation and Metabolic Syndrome
- Metabolic Risk/Epidemiology
- Nonalcoholic Fatty Liver Disease: A Drug Revolution Is Coming
- Soung Won Jeong
- Diabetes Metab J. 2020;44(5):640-657. Published online October 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0115
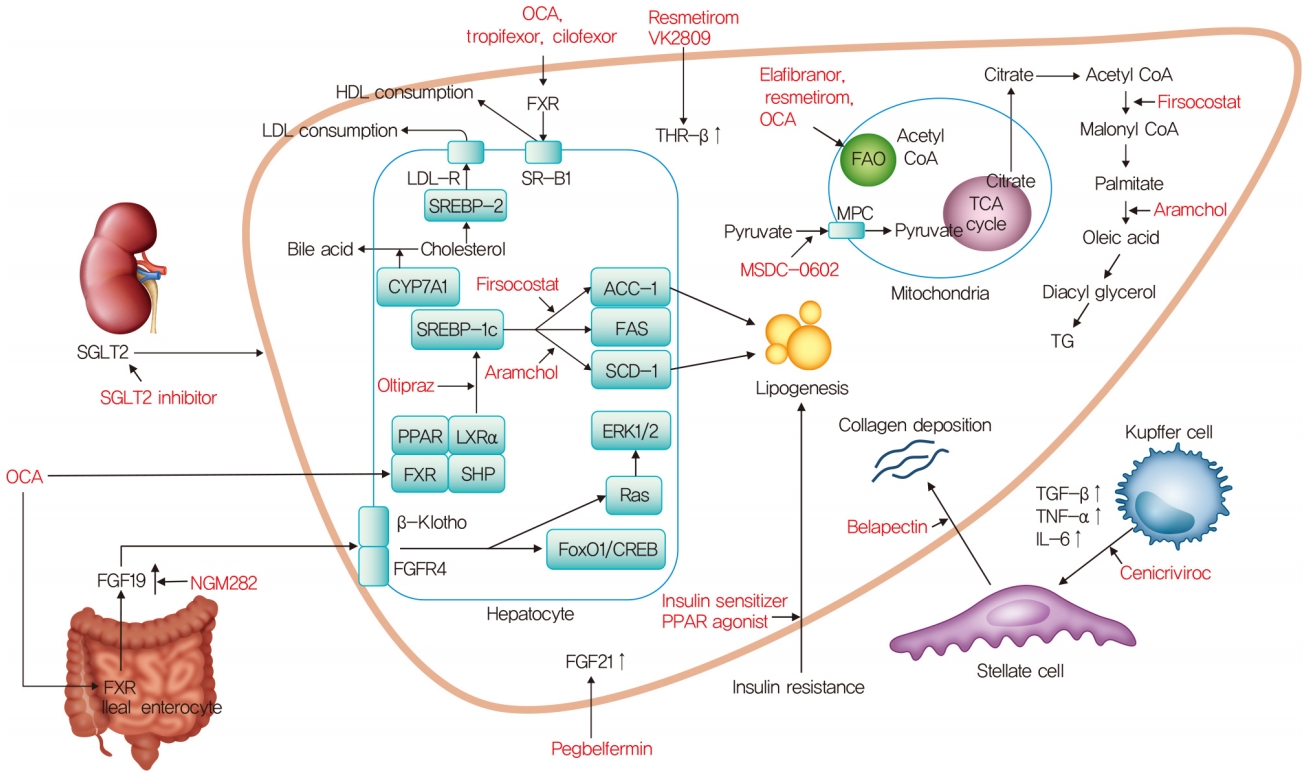
- 11,909 View
- 547 Download
- 16 Web of Science
- 16 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - The worldwide prevalence of non-alcoholic fatty liver disease is around 25%, and that of nonalcoholic steatohepatitis (NASH) ranges from 1.5% to 6.45%. Patients with NASH, especially those with fibrosis, are at higher risk for adverse outcomes such as cirrhosis and liver-related mortality. Although vitamin E, pioglitazone, and liraglutide improved liver histology in randomized trials, there are currently no Food and Drug Administration-approved drugs for NASH. Five pharmacologic agents—obeticholic acid, elafibranor, cenicriviroc, resmetirom, and aramchol—are being evaluated in large, histology-based phase 3 trials. Within 2 to 4 years, new and effective drugs for the treatment of NASH are expected. Additionally, many phase 2 trials are ongoing for various agents. Based on the results of phase 2 and 3 trials, combination treatments are also being investigated. Future treatment strategies will comprise drug combinations and precision medicine based on the different phenotypes of NASH and treatment response of the individual patient.
-
Citations
Citations to this article as recorded by- Recent Progresses on Pathophysiology, Diagnosis, Therapeutic Modalities,
and Management of Non-alcoholic Fatty Liver Disorder
Mahdi Barazesh, Sajad Jalili, Morteza Akhzari, Fouzieyeh Faraji, Ebrahim Khorramdin
Current Drug Therapy.2024; 19(1): 20. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Mortality: A Population-Based Cohort Study
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(2): 220. CrossRef - Increased expression of sodium-glucose cotransporter 2 and O-GlcNAcylation in hepatocytes drives non-alcoholic steatohepatitis
Hye Jin Chun, Eun Ran Kim, Minyoung Lee, Da Hyun Choi, Soo Hyun Kim, Eugene Shin, Jin-Hong Kim, Jin Won Cho, Dai Hoon Han, Bong-Soo Cha, Yong-ho Lee
Metabolism.2023; 145: 155612. CrossRef - Effect of bariatric surgery on NAFLD/NASH: a single-centre observational prospective cohort study
Willy B Theel, Bianca M Boxma-de Klerk, Femme Dirksmeier-Harinck, Elisabeth FC van Rossum, Danny A Kanhai, Jan A Apers, Bas M van Dalen, Robert J De Knegt, Bojou Neecke, Ellen M van der Zwan, Diederick E Grobbee, Thomas Hankemeier, Janneke Wiebolt, Manuel
BMJ Open.2023; 13(7): e070431. CrossRef - Ameliorative role of bioactive phytoconstituents targeting obesity associated NAFLD by modulation of inflammation and lipogenesis pathways: a comprehensive review
Pervej Alom Barbhuiya, Saikat Sen, Manash Pratim Pathak
Phytochemistry Reviews.2023;[Epub] CrossRef - Inflammatory and fibrotic mechanisms in NAFLD—Implications for new treatment strategies
Youngmin A. Lee, Scott L. Friedman
Journal of Internal Medicine.2022; 291(1): 11. CrossRef - Efficacy and safety of evogliptin in patients with type 2 diabetes and non‐alcoholic fatty liver disease: A multicentre, double‐blind, randomized, comparative trial
Eugene Han, Ji Hye Huh, Eun Y. Lee, Ji C. Bae, Sung W. Chun, Sung H. Yu, Soo H. Kwak, Kyong S. Park, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(4): 752. CrossRef - Triglyceride and glucose index is a simple and easy‐to‐calculate marker associated with nonalcoholic fatty liver disease
Kyung‐Soo Kim, Sangmo Hong, Hong‐Yup Ahn, Cheol‐Young Park
Obesity.2022; 30(6): 1279. CrossRef - Thyroid diseases and new approaches for their treatment
E. A. Fokina, A. O. Shpakov
The Siberian Journal of Clinical and Experimental Medicine.2022; 37(3): 90. CrossRef - Gemigliptin Alleviates Succinate-Induced Hepatic Stellate Cell Activation by Ameliorating Mitochondrial Dysfunction
Giang Nguyen, So Young Park, Dinh Vinh Do, Dae-Hee Choi, Eun-Hee Cho
Endocrinology and Metabolism.2022; 37(6): 918. CrossRef - Inhibition of 11β-hydroxysteroid dehydrogenase 1 relieves fibrosis through depolarizing of hepatic stellate cell in NASH
Su-Yeon Lee, Sanghwa Kim, Inhee Choi, Yeonhwa Song, Namjeong Kim, Hyung Chul Ryu, Jee Woong Lim, Hyo Jin Kang, Jason Kim, Haeng Ran Seo
Cell Death & Disease.2022;[Epub] CrossRef - Lessons on Drug Development: A Literature Review of Challenges Faced in Nonalcoholic Fatty Liver Disease (NAFLD) Clinical Trials
Joel Yeh Siang Chen, Damien Chua, Carissa Odelia Lim, Wan Xi Ho, Nguan Soon Tan
International Journal of Molecular Sciences.2022; 24(1): 158. CrossRef - Metabolic Spectrum of Liver Failure in Type 2 Diabetes and Obesity: From NAFLD to NASH to HCC
Hyunmi Kim, Da Som Lee, Tae Hyeon An, Hyun-Ju Park, Won Kon Kim, Kwang-Hee Bae, Kyoung-Jin Oh
International Journal of Molecular Sciences.2021; 22(9): 4495. CrossRef - Allopurinol ameliorates high fructose diet induced hepatic steatosis in diabetic rats through modulation of lipid metabolism, inflammation, and ER stress pathway
In-Jin Cho, Da-Hee Oh, Jin Yoo, You-Cheol Hwang, Kyu Jeung Ahn, Ho-Yeon Chung, Soung Won Jeong, Ju-Young Moon, Sang-Ho Lee, Sung-Jig Lim, In-Kyung Jeong
Scientific Reports.2021;[Epub] CrossRef - Effects of intragastric balloon placement in metabolic dysfunction-associated fatty liver disease: A systematic review and meta-analysis
João Remí de Freitas Júnior, Igor Braga Ribeiro, Diogo Turiani Hourneaux de Moura, Vitor Massaro Takamatsu Sagae, Gabriel Mayo Vieira de Souza, Guilherme Henrique Peixoto de Oliveira, Sergio A Sánchez-Luna, Thiago Ferreira de Souza, Eduardo Turiani Hourne
World Journal of Hepatology.2021; 13(7): 815. CrossRef - The New Therapeutic Approaches in the Treatment of Non-Alcoholic Fatty Liver Disease
Branka Filipovic, Snezana Lukic, Dragana Mijac, Marija Marjanovic-Haljilji, Marko Vojnovic, Jelena Bogdanovic, Tijana Glisic, Natasa Filipovic, Jamal Al Kiswani, Aleksandra Djokovic, Suncica Kapor, Slobodan Kapor, Zoran Bukumiric, Ana Starcevic
International Journal of Molecular Sciences.2021; 22(24): 13219. CrossRef
- Recent Progresses on Pathophysiology, Diagnosis, Therapeutic Modalities,
and Management of Non-alcoholic Fatty Liver Disorder
- Metabolic Risk/Epidemiology
- Importance of Awareness and Treatment for Diabetes in Influenza Vaccination Coverage of Diabetic Patients under 65 Years: A Population-Based Study
- Yu Mi Ko, Seung Hyun Ko, Kyoungdo Han, Yong-Moon Park, Joon Young Choi, Shin Young Kim, So Hyang Song, Chi Hong Kim, Sung Kyoung Kim
- Diabetes Metab J. 2021;45(1):55-66. Published online May 29, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0189
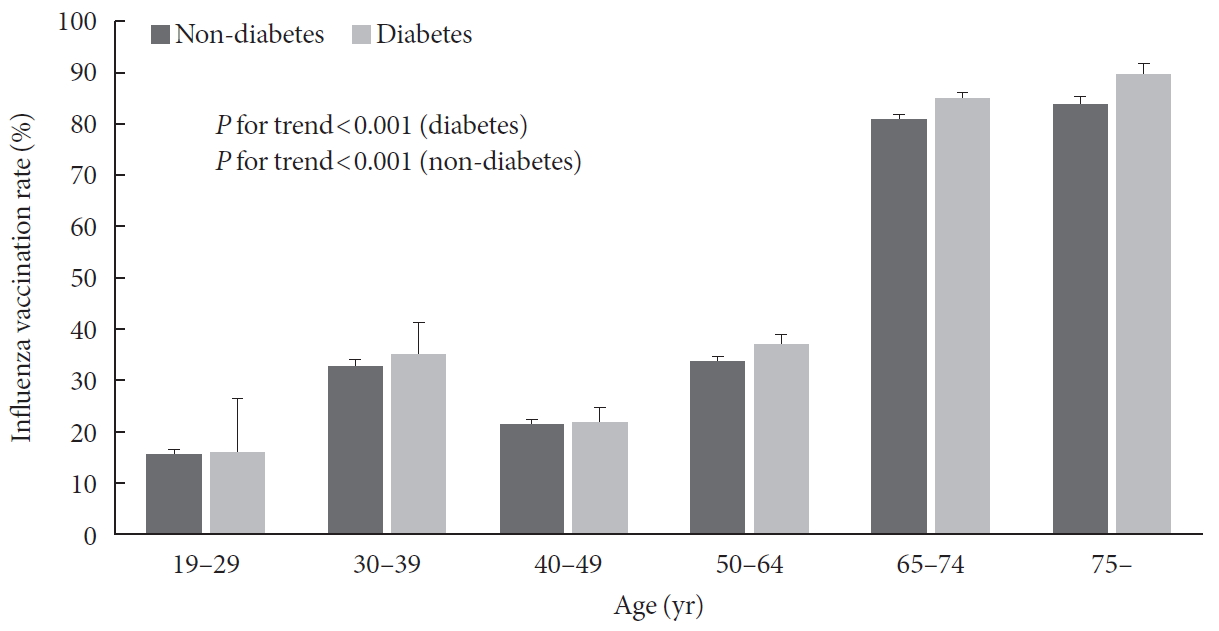
- 6,972 View
- 138 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub Background Influenza is a global public health problem causing considerable morbidity and mortality. Although vaccination is the most effective way to prevent infection, vaccination coverage is insufficient in people with chronic disease under 65 years, especially diabetes. The purpose of this study was to evaluate influenza vaccination coverage and identify factors associated with influenza vaccination in Korean diabetic adults under 65 years.
Methods Data were obtained from 24,821 subjects in the Korea National Health and Nutrition Examination Survey (2014 to 2017). Socioeconomic, health-related, and diabetic factors were investigated for their relations with influenza vaccination in diabetic patients under 65 years using univariate and multivariate analyses.
Results Among 24,821 subjects, 1,185 were diabetic patients under 65 years and their influenza vaccination rate was 36.5%. Socioeconomic (older age, female gender, non-smoker, light alcohol drinker, lower educational level, and employed status), health-related factors (lower fasting glucose and glycosylated hemoglobin level, good self-perceived health status, more comorbidities, recent health screening, more outpatient visits, and diet therapy), and diabetic factors (more awareness and getting treated) were associated with influenza vaccination. In multivariate analysis, more awareness and getting treated for diabetes were associated with influenza vaccination in diabetic patients under 65 years (odds ratio, 1.496 and 1.413; 95% confidence interval, 1.022 to 2.188 and 1.018 to 2.054, respectively).
Conclusion Influenza vaccination rate was low in diabetic patients under 65 years, especially in those with unawareness and not getting treated for diabetes. Active screening and treatment for diabetes may be helpful to improve the influenza vaccination rate in these patients.
-
Citations
Citations to this article as recorded by- Adherence to Advisory Committee on Immunization Practices in diabetes mellitus patients in Saudi Arabia: A multicenter retrospective study
Saleh Fahad Alqifari, Aya K Esmail, Dalal M Alarifi, Ghalya Y Alsuliman, Maram M Alhati, May R Mutlaq, Mohammed Aldhaeefi, Shaden A Alshuaibi, Palanisamy Amirthalingam, Abrar Abdallah, Afaf S Wasel, Heba R Hamad, Shoroq Alamin, Tasneem H Atia, Tariq Alqah
World Journal of Diabetes.2024; 15(3): 440. CrossRef - ЕГДЕ ЖАСТАҒЫ АДАМДАРДА COVID-19 ВАКЦИНАЦИЯСЫНЫҢ ТИІМДІЛІГІ
Ю.Р. АБДУСАТТАРОВА, Д.С. ӘБЕН, Н. АБДОЛЛА, Р.Т. ТЛЕУЛИЕВА, А. КАЛИ, Ю.В. ПЕРФИЛЬЕВА
Vestnik.2023; (2(65)): 59. CrossRef - Comorbidities associated with high-risk obstructive sleep apnea based on the STOP-BANG questionnaire: a nationwide population-based study
Gene Huh, Kyoung do Han, Yong-Moon Park, Chan-Soon Park, Kyu-na Lee, Eun Young Lee, Jung-Hae Cho
The Korean Journal of Internal Medicine.2023; 38(1): 80. CrossRef - Influenza vaccination trend and related factors among patients with diabetes in Korea: Analysis using a nationwide database
Dong-Hwa Lee, Bumhee Yang, Seonhye Gu, Eung-Gook Kim, Youlim Kim, Hyung Koo Kang, Yeong Hun Choe, Hyun Jeong Jeon, Seungyong Park, Hyun Lee
Frontiers in Endocrinology.2023;[Epub] CrossRef - Factors associated with seasonal influenza immunization in people with chronic diseases
Slađana Arsenović, Tatjana Gazibara
Medicinski podmladak.2021; 72(2): 19. CrossRef
- Adherence to Advisory Committee on Immunization Practices in diabetes mellitus patients in Saudi Arabia: A multicenter retrospective study
- Clinical Care/Education
- 2019 Clinical Practice Guidelines for Type 2 Diabetes Mellitus in Korea
- Mee Kyoung Kim, Seung-Hyun Ko, Bo-Yeon Kim, Eun Seok Kang, Junghyun Noh, Soo-Kyung Kim, Seok-O Park, Kyu Yeon Hur, Suk Chon, Min Kyong Moon, Nan-Hee Kim, Sang Yong Kim, Sang Youl Rhee, Kang-Woo Lee, Jae Hyeon Kim, Eun-Jung Rhee, SungWan Chun, Sung Hoon Yu, Dae Jung Kim, Hyuk-Sang Kwon, Kyong Soo Park
- Diabetes Metab J. 2019;43(4):398-406. Published online August 20, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0137
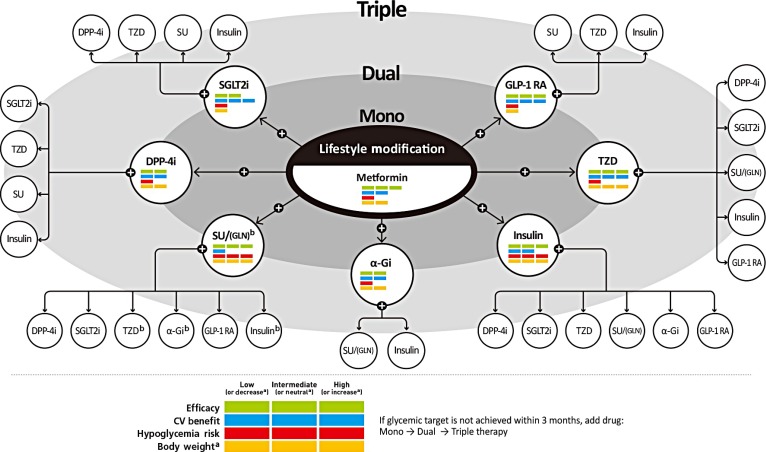
- 16,333 View
- 477 Download
- 160 Web of Science
- 171 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The Committee of Clinical Practice Guidelines of the Korean Diabetes Association revised and updated the 6th Clinical Practice Guidelines in 2019. Targets of glycemic, blood pressure, and lipid control in type 2 diabetes mellitus (T2DM) were updated. The obese and overweight population is increasing steadily in Korea, and half of the Koreans with diabetes are obese. Evidence-based recommendations for weight-loss therapy for obesity management as treatment for hyperglycemia in T2DM were provided. In addition, evidence from large clinical studies assessing cardiovascular outcomes following the use of sodium-glucose cotransporter-2 inhibitors and glucagon-like peptide 1 receptor agonists in patients with T2DM were incorporated into the recommendations.
-
Citations
Citations to this article as recorded by- Serum-based ATR-FTIR spectroscopy combined with multivariate analysis for the diagnosis of pre-diabetes and diabetes
Weiyi Pang, Yu Xing, Camilo L. M. Morais, Qiufeng Lao, Shengle Li, Zipeng Qiao, You Li, Maneesh N. Singh, Valério G. Barauna, Francis L. Martin, Zhiyong Zhang
The Analyst.2024; 149(2): 497. CrossRef - Fruits and the Risk of Type 2 Diabetes: The Korean Genome and Epidemiology Study Cohort
Hojun Yu, Cheol Min Lee, Seung-Won Oh
Korean Journal of Family Medicine.2024; 45(1): 44. CrossRef - Effectiveness and Safety of Sodium-Glucose Cotransporter 2 Inhibitors Added to Dual or Triple Treatment in Patients with Type 2 Diabetes Mellitus
Yesol Hong, Yoomin Jeon, Yoona Choi, Tae Kyu Chung, Howard Lee
Diabetes Therapy.2024; 15(2): 487. CrossRef - Risk factors for carotid plaque formation in type 2 diabetes mellitus
Jin Chen, Wenwen Li, Jingzhu Cao, Yuhan Lu, Chaoqun Wang, Jin Lu
Journal of Translational Medicine.2024;[Epub] CrossRef - Cumulative exposure to impaired fasting glucose and gastrointestinal cancer risk: A nationwide cohort study
Byeong Yun Ahn, Bokyung Kim, Sanghyun Park, Sang Gyun Kim, Kyungdo Han, Soo‐Jeong Cho
Cancer.2024;[Epub] CrossRef - Effects of a Health Partnership Program Using Mobile Health Application for Male Workers with Cardiovascular Risk Factors in Small and Medium Enterprises: A Randomized Controlled Trial
Eun Jin Kim, Seon Young Hwang
Journal of Korean Academy of Nursing.2024; 54(1): 44. CrossRef - The clinical relevance of a polygenic risk score for type 2 diabetes mellitus in the Korean population
Na Yeon Kim, Haekyung Lee, Sehee Kim, Ye-Jee Kim, Hyunsuk Lee, Junhyeong Lee, Soo Heon Kwak, Seunggeun Lee
Scientific Reports.2024;[Epub] CrossRef - Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
Eun-Gyoung Hong, Kyung-Wan Min, Jung Soo Lim, Kyu-Jeung Ahn, Chul Woo Ahn, Jae-Myung Yu, Hye Soon Kim, Hyun Jin Kim, Won Kim, Dong Han Kim, Hak Chul Jang
Advances in Therapy.2024;[Epub] CrossRef - The Potential Role of Presepsin in Predicting Severe Infection in Patients with Diabetic Foot Ulcers
Eun Yeong Ha, Il Rae Park, Seung Min Chung, Young Nam Roh, Chul Hyun Park, Tae-Gon Kim, Woong Kim, Jun Sung Moon
Journal of Clinical Medicine.2024; 13(8): 2311. CrossRef - Safety of sodium–glucose cotransporter 2 inhibitors in Asian type 2 diabetes populations
Jaime A Davidson, Norlela Sukor, Fen‐Lee Hew, Mafauzy Mohamed, Zanariah Hussein
Journal of Diabetes Investigation.2023; 14(2): 167. CrossRef - β-hydroxybutyrate as a biomarker of β-cell function in new-onset type 2 diabetes and its association with treatment response at 6 months
Minyoung Lee, Yongin Cho, Yong-ho Lee, Eun Seok Kang, Bong-soo Cha, Byung-Wan Lee
Diabetes & Metabolism.2023; 49(4): 101427. CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Cardiovascular Outcomes according to Comorbidities and Low-Density Lipoprotein Cholesterol in Korean People with Type 2 Diabetes Mellitus
Min Kyong Moon, Junghyun Noh, Eun-Jung Rhee, Sang Hyun Park, Hyeon Chang Kim, Byung Jin Kim, Hae Jin Kim, Seonghoon Choi, Jin Oh Na, Young Youl Hyun, Bum Joon Kim, Kyung-Do Han, In-Kyung Jeong
Diabetes & Metabolism Journal.2023; 47(1): 45. CrossRef - Impaired ketogenesis is associated with metabolic-associated fatty liver disease in subjects with type 2 diabetes
Sejeong Lee, Jaehyun Bae, Doo Ri Jo, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2023;[Epub] CrossRef - Identifying the Associations of Nightly Fasting Duration and Meal Timing with Type 2 Diabetes Mellitus Using Data from the 2016–2020 Korea National Health and Nutrition Survey
Junkyung Kwak, Kyeong-A Jang, Haeng-Ran Kim, Min-Sook Kang, Kyung Won Lee, Dayeon Shin
Nutrients.2023; 15(6): 1385. CrossRef - Development and Adaptability of Smartphone-based Dietary Coaching Program for Patients Undergoing Diabetes and Prediabetes with Continuous Glucose Monitoring Device
Myoung Soo Kim, Jung Mi Ryu, Minkyeong Kang, Jiwon Park, Yeh Chan Ahn, Yang Seok Kim
Journal of Health Informatics and Statistics.2023; 48(1): 36. CrossRef - Glucose Control in Korean Patients with Type 2 Diabetes Mellitus according to Body Mass Index
Ye-lim Shin, Heesoh Yoo, Joo Young Hong, Jooeun Kim, Kyung-do Han, Kyu-Na Lee, Yang-Hyun Kim
Journal of Obesity & Metabolic Syndrome.2023; 32(1): 55. CrossRef - Diabetes severity is strongly associated with the risk of active tuberculosis in people with type 2 diabetes: a nationwide cohort study with a 6-year follow-up
Ji Young Kang, Kyungdo Han, Seung-Hwan Lee, Mee Kyoung Kim
Respiratory Research.2023;[Epub] CrossRef - Developing a Classification Algorithm for Prediabetes Risk Detection From Home Care Nursing Notes
Eunjoo Jeon, Aeri Kim, Jisoo Lee, Hyunsook Heo, Hana Lee, Kyungmi Woo
CIN: Computers, Informatics, Nursing.2023; 41(7): 539. CrossRef - Predictive value of the Framingham steatosis index for cardiovascular risk: a nationwide population-based cohort study
Yun Kyung Cho, Myungjin Kim, Ye-Jee Kim, Chang Hee Jung, Woo Je Lee, Joong-Yeol Park
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Association of low muscle strength with metabolic dysfunction-associated fatty liver disease: A nationwide study
Gyu Bae Lee, Youn Huh, Sang Hyun Lee, Byoungduck Han, Yang-Hyun Kim, Do-Hoon Kim, Seon Mee Kim, Youn Seon Choi, Kyung Hwan Cho, Ga Eun Nam
World Journal of Gastroenterology.2023; 29(45): 5962. CrossRef - Low fasting glucose‐to‐estimated average glucose ratio was associated with superior response to insulin degludec/aspart compared with basal insulin in patients with type 2 diabetes
Han Na Jang, Ye Seul Yang, Tae Jung Oh, Bo Kyung Koo, Seong Ok Lee, Kyong Soo Park, Hak Chul Jang, Hye Seung Jung
Journal of Diabetes Investigation.2022; 13(1): 85. CrossRef - Relationship between the early initiation of insulin treatment and diabetic complications in patients newly diagnosed with type 2 diabetes mellitus in Korea: A nationwide cohort study
Ha‐Lim Jeon, Won Kim, Bongseong Kim, Ju‐Young Shin
Journal of Diabetes Investigation.2022; 13(5): 830. CrossRef - Relationship of the Triglyceride-Glucose Index with Subclinical White Matter Hypersensitivities of Presumed Vascular Origin Among Community-Dwelling Koreans
Dong-Hyuk Jung, Byoungjin Park, Yong-Jae Lee
International Journal of General Medicine.2022; Volume 15: 603. CrossRef - Prevalence of vitamin B12 deficiency and its association with metformin-treated type 2 diabetic patients: A cross sectional study
Shaimaa B. Almatrafi, El-Sayed H. Bakr, Asem A. Almatrafi, Manal M. Altayeb
Human Nutrition & Metabolism.2022; 27: 200138. CrossRef - Retinal Vascular Caliber Changes in Early Type 2 Diabetic Patients without Retinopathy
Jeong Woo Park, Jeong Hun Bae, Su Jeong Song, Joon Mo Kim
Journal of the Korean Ophthalmological Society.2022; 63(1): 20. CrossRef - Renal Tubular Damage Marker, Urinary N-acetyl-β-D-Glucosaminidase, as a Predictive Marker of Hepatic Fibrosis in Type 2 Diabetes Mellitus
Hae Kyung Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Diabetes & Metabolism Journal.2022; 46(1): 104. CrossRef - Efficacy and Safety of Self-Titration Algorithms of Insulin Glargine 300 units/mL in Individuals with Uncontrolled Type 2 Diabetes Mellitus (The Korean TITRATION Study): A Randomized Controlled Trial
Jae Hyun Bae, Chang Ho Ahn, Ye Seul Yang, Sun Joon Moon, Soo Heon Kwak, Hye Seung Jung, Kyong Soo Park, Young Min Cho
Diabetes & Metabolism Journal.2022; 46(1): 71. CrossRef - Sodium-Glucose Cotransporter-2 Inhibitor-Related Diabetic Ketoacidosis: Accuracy Verification of Operational Definition
Dong Yoon Kang, Hyunah Kim, SooJeong Ko, HyungMin Kim, Jiwon Shinn, Min-Gyu Kang, Sun-ju Byeon, Jeong-Hee Choi, Soo-Yong Shin, Hun-Sung Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Relationship between the dynamics of non-alcoholic fatty liver disease and incident diabetes mellitus
Ji Eun Han, Han-Bit Shin, Young Hwan Ahn, Hyo Jung Cho, Jae Youn Cheong, Bumhee Park, Soon Sun Kim
Scientific Reports.2022;[Epub] CrossRef - Position of Sulfonylureas in the Current ERA: Review of National and International Guidelines
Viswanathan Mohan, Banshi Saboo, Jabbar Khader, Kirtikumar D Modi, Sushil Jindal, Subhash Kumar Wangnoo, Sugumaran Amarnath
Clinical Medicine Insights: Endocrinology and Diabetes.2022; 15: 117955142210746. CrossRef - Real-world comparison of mono and dual combination therapies of metformin, sulfonylurea, and dipeptidyl peptidase-4 inhibitors using a common data model
Kyung Ae Lee, Heung Yong Jin, Yu Ji Kim, Sang Soo Kim, Eun-Hee Cho, Tae Sun Park
Medicine.2022; 101(8): e28823. CrossRef - Atherogenic Index of Plasma and Its Association with Risk Factors of Coronary Artery Disease and Nutrient Intake in Korean Adult Men: The 2013–2014 KNHANES
Hye Ran Shin, SuJin Song, Jin Ah Cho, Sun Yung Ly
Nutrients.2022; 14(5): 1071. CrossRef - Sodium–glucose cotransporter 2 inhibitors do not increase the risk of fractures in real‐world clinical practice in Korea: A national observational cohort study
Kyoung Hwa Ha, Dae Jung Kim, Yong Jun Choi
Journal of Diabetes Investigation.2022; 13(6): 986. CrossRef - Performance of Diabetes and Kidney Disease Screening Scores in Contemporary United States and Korean Populations
Liela Meng, Keun-Sang Kwon, Dae Jung Kim, Yong-ho Lee, Jeehyoung Kim, Abhijit V. Kshirsagar, Heejung Bang
Diabetes & Metabolism Journal.2022; 46(2): 273. CrossRef - Integrated metagenomics and metabolomics analysis illustrates the systemic impact of the gut microbiota on host metabolism after bariatric surgery
Yeyoung Han, Gihyeon Kim, Eunyong Ahn, Sunhee Jung, Youngae Jung, Yunjae Kim, Eunyoung Ha, Yoonseok Heo, Do Hyun Ryu, Hansoo Park, Geum‐Sook Hwang
Diabetes, Obesity and Metabolism.2022; 24(7): 1224. CrossRef - The use of complex marketing analysis and QSPR methodology for the necessity of a drug development grounding for the treatment of type 2 diabetes mellitus with increased bioavailability
Inna Kovalevska, Olena Ruban, Alina Volkova, Alla Kotvitska, Alina Cherkashyna
Pharmacia.2022; 69(2): 303. CrossRef - Comparative Study of Ex Vivo Antiplatelet Activity of Aspirin and Cilostazol in Patients with Diabetes and High Risk of Cardiovascular Disease
Sangmo Hong, Woo Je Lee, Cheol-Young Park
Endocrinology and Metabolism.2022; 37(2): 233. CrossRef - Long-term effect of the eradication of Helicobacter pylori on the hemoglobin A1c in type 2 diabetes or prediabetes patients
Won Seok Kim, Yonghoon Choi, Nayoung Kim, Seon Hee Lim, Gitark Noh, Ki Wook Kim, Jaehyung Park, Hyeongho Jo, Hyuk Yoon, Cheol Min Shin, Young Soo Park, Dong Ho Lee
The Korean Journal of Internal Medicine.2022; 37(3): 579. CrossRef - Novel Glycemic Index Based on Continuous Glucose Monitoring to Predict Poor Clinical Outcomes in Critically Ill Patients: A Pilot Study
Eun Yeong Ha, Seung Min Chung, Il Rae Park, Yin Young Lee, Eun Young Choi, Jun Sung Moon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Understanding and Utilizing Claim Data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) Database for Research
Dae-Sung Kyoung, Hun-Sung Kim
Journal of Lipid and Atherosclerosis.2022; 11(2): 103. CrossRef - Association of the atherogenic index of plasma with cardiovascular risk beyond the traditional risk factors: a nationwide population-based cohort study
Si Hyoung Kim, Yun Kyung Cho, Ye-Jee Kim, Chang Hee Jung, Woo Je Lee, Joong-Yeol Park, Ji Hye Huh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Cardiovascular Diabetology.2022;[Epub] CrossRef - Current Status of Low-Density Lipoprotein Cholesterol Target Achievement in Patients with Type 2 Diabetes Mellitus in Korea Compared with Recent Guidelines
Soo Jin Yun, In-Kyung Jeong, Jin-Hye Cha, Juneyoung Lee, Ho Chan Cho, Sung Hee Choi, SungWan Chun, Hyun Jeong Jeon, Ho-Cheol Kang, Sang Soo Kim, Seung-Hyun Ko, Gwanpyo Koh, Su Kyoung Kwon, Jae Hyuk Lee, Min Kyong Moon, Junghyun Noh, Cheol-Young Park, Sung
Diabetes & Metabolism Journal.2022; 46(3): 464. CrossRef - Sodium Glucose Cotransporter-2 Inhibitors as an Add-on Therapy to Metformin Plus Dipeptidyl Peptidase-4 Inhibitor in Patients with Type 2 Diabetes
Jaehyun Bae, Young-eun Kim, Minyoung Lee, Yong-ho Lee, Byung-Wan Lee, Bong-Soo Cha, Eun Seok Kang
Yonsei Medical Journal.2022; 63(6): 539. CrossRef - Predictors for successful weight reduction during treatment with Dapagliflozin among patients with type 2 diabetes mellitus in primary care
Youn Huh, Young Sik Kim
BMC Primary Care.2022;[Epub] CrossRef - Implications of the heterogeneity between guideline recommendations for the use of low dose aspirin in primary prevention of cardiovascular disease
Xiao-Ying Li, Li Li, Sang-Hoon Na, Francesca Santilli, Zhongwei Shi, Michael Blaha
American Journal of Preventive Cardiology.2022; 11: 100363. CrossRef - Factors Influencing the Utilization of Diabetes Complication Tests Under the COVID-19 Pandemic: Machine Learning Approach
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effects of exercise initiation and smoking cessation after new-onset type 2 diabetes mellitus on risk of mortality and cardiovascular outcomes
Mee Kyoung Kim, Kyungdo Han, Bongsung Kim, Jinyoung Kim, Hyuk-Sang Kwon
Scientific Reports.2022;[Epub] CrossRef - Improvement in Age at Mortality and Changes in Causes of Death in the Population with Diabetes: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Eugene Han, Sun Ok Song, Hye Soon Kim, Kang Ju Son, Sun Ha Jee, Bong-Soo Cha, Byung-Wan Lee
Endocrinology and Metabolism.2022; 37(3): 466. CrossRef - Analysis of Continuity of Care and Its Related Factors in Diabetic Patients: A Cross-Sectional Study
Ji Yeh Shin, Ha Jin Kim, BeLong Cho, Yun Jun Yang, Jae Moon Yun
Korean Journal of Family Medicine.2022; 43(4): 246. CrossRef - Development of Various Diabetes Prediction Models Using Machine Learning Techniques
Juyoung Shin, Jaewon Kim, Chanjung Lee, Joon Young Yoon, Seyeon Kim, Seungjae Song, Hun-Sung Kim
Diabetes & Metabolism Journal.2022; 46(4): 650. CrossRef - A causal relationship between alcohol intake and type 2 diabetes mellitus: A two-sample Mendelian randomization study
Meiling Liu, Sunmin Park
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(12): 2865. CrossRef - Early glycaemic variability increases 28-day mortality and prolongs intensive care unit stay in critically ill patients with pneumonia
Seong Ho Kim, Ji Young Kim, Eun Song Kim, Il Rae Park, Eun Yeong Ha, Seung Min Chung, Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Annals of Medicine.2022; 54(1): 2724. CrossRef - Association of the Estimated Pulse Wave Velocity with Cardio-Vascular Disease Outcomes among Men and Women Aged 40–69 Years in the Korean Population: An 18-Year Follow-Up Report on the Ansung–Ansan Cohort in the Korean Genome Environment Study
Byung Sik Kim, Yonggu Lee, Jin-Kyu Park, Young-Hyo Lim, Jeong-Hun Shin
Journal of Personalized Medicine.2022; 12(10): 1611. CrossRef - Perfluorinated compounds in adults and their association with fasting glucose and incident diabetes: a prospective cohort study
Seung Min Chung, Dong-Gyu Heo, Ju-Hyun Kim, Ji Sung Yoon, Hyoung Woo Lee, Jong-Yeon Kim, Jun Sung Moon, Kyu Chang Won
Environmental Health.2022;[Epub] CrossRef - Differences in health behavior and nutrient intake status between diabetes-aware and unaware Korean adults based on the Korea national health and nutrition examination survey 2016–18 data: A cross-sectional study
Anshul Sharma, Chen Lulu, Kee-Ho Song, Hae-Jeung Lee
Frontiers in Public Health.2022;[Epub] CrossRef - Improving Machine Learning Diabetes Prediction Models for the Utmost Clinical Effectiveness
Juyoung Shin, Joonyub Lee, Taehoon Ko, Kanghyuck Lee, Yera Choi, Hun-Sung Kim
Journal of Personalized Medicine.2022; 12(11): 1899. CrossRef - Does Pitavastatin Therapy for Patients with Type 2 Diabetes and Dyslipidemia Affect Serum Adiponectin Levels and Insulin Sensitivity?
Jeongmin Lee, Min-Hee Kim, Jung-Min Lee, Sang-Ah Chang
Journal of Clinical Medicine.2022; 11(22): 6756. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Efficacy and Safety of Once Weekly Dulaglutide in East Asian Patients with Type 2 Diabetes: Subgroup Analysis by Potential Influential Factors
Jianhua Ma, Bin Zhang, Jianing Hou, Yongde Peng
Diabetes Therapy.2021; 12(1): 211. CrossRef - Early combination versus initial metformin monotherapy in the management of newly diagnosed type 2 diabetes: AnEast Asianperspective
Linong Ji, Juliana C. N. Chan, Miao Yu, Kun Ho Yoon, Sin Gon Kim, Sung Hee Choi, Chien‐Ning Huang, Shih Te Tu, Chih‐Yuan Wang, Päivi Maria Paldánius, Wayne H. H. Sheu
Diabetes, Obesity and Metabolism.2021; 23(1): 3. CrossRef - Effectiveness and safety of sodium‐glucose co‐transporter‐2 inhibitors compared with dipeptidyl peptidase‐4 inhibitors in older adults with type 2 diabetes: A nationwide population‐based study
Seung Jin Han, Kyoung Hwa Ha, Nami Lee, Dae Jung Kim
Diabetes, Obesity and Metabolism.2021; 23(3): 682. CrossRef - Glucodynamics and glucocracy in type 2 diabetes mellitus: clinical evidence and practice-based opinion on modern sulfonylurea use, from an International Expert Group (South Asia, Middle East & Africa) via modified Delphi method
Sanjay Kalra, Das A. K., Fariduddin Md., Shaikh K., Shah P., Rehim A. A., John M., Shaikh S., Orabi A., Saraswati M. R., Shahjada Selim, Baruah M. P., K. K. Gangopadhyay, Langi Y. A., Nair T., Dhanwal D., Thapa S. D., Deshmukh V., D. Dutta, Khalfan H., Ma
Current Medical Research and Opinion.2021; 37(3): 403. CrossRef - The association between lipoprotein (a) and carotid atherosclerosis in patients with type 2 diabetes without pre-existing cardiovascular disease: A cross-sectional study
Ji Eun Jun, Hongsun Kang, You-Cheol Hwang, Kyu Jeung Ahn, Ho-Yeon Chung, In-Kyung Jeong
Diabetes Research and Clinical Practice.2021; 171: 108622. CrossRef - Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
Jaehyun Bae, Ji Hye Huh, Minyoung Lee, Yong‐Ho Lee, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2021; 23(2): 609. CrossRef - Effect of Tai Chi on Quality of Life, Body Mass Index, and Waist-Hip Ratio in Patients With Type 2 Diabetes Mellitus: A Systematic Review and Meta-Analysis
Jiawei Qin, Yannan Chen, Shuai Guo, Yue You, Ying Xu, Jingsong Wu, Zhizhen Liu, Jia Huang, Lidian Chen, Jing Tao
Frontiers in Endocrinology.2021;[Epub] CrossRef - Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
Soo-Yeon Choi, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 263. CrossRef - Diabetes Fact Sheets in Korea, 2020: An Appraisal of Current Status
Chan-Hee Jung, Jang Won Son, Shinae Kang, Won Jun Kim, Hun-Sung Kim, Hae Soon Kim, Mihae Seo, Hye-Jung Shin, Seong-Su Lee, Su Jin Jeong, Yongin Cho, Seung Jin Han, Hyang Mi Jang, Mira Rho, Shinbi Lee, Mihyun Koo, Been Yoo, Jung-Wha Moon, Hye Young Lee, Ja
Diabetes & Metabolism Journal.2021; 45(1): 1. CrossRef - Estimation of sodium‐glucose cotransporter 2 inhibitor–related genital and urinary tract infections via electronic medical record–based common data model
SooJeong Ko, HyungMin Kim, Jiwon Shinn, Sun‐ju Byeon, Jeong‐Hee Choi, Hun‐Sung Kim
Journal of Clinical Pharmacy and Therapeutics.2021; 46(4): 975. CrossRef - Pharmacokinetic and Pharmacodynamic Comparison of Two Formulations of a Fixed-Dose Combination of Gemigliptin/Rosuvastatin 50/20 mg: A Randomized, Open-Label, Single-Dose, Two-Way Crossover Study
Eunsol Yang, Hyounggyoon Yoo, In-Jin Jang, Kyung-Sang Yu, SeungHwan Lee
Drug Design, Development and Therapy.2021; Volume 15: 651. CrossRef - Severe hypoglycemia and the risk of end stage renal disease in type 2 diabetes
Jae-Seung Yun, Yong-Moon Park, Kyungdo Han, Hyung-Wook Kim, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Scientific Reports.2021;[Epub] CrossRef - Long-term HbA1c variability and the development and progression of diabetic retinopathy in subjects with type 2 diabetes
Han Ul Kim, Sung Pyo Park, Yong-Kyu Kim
Scientific Reports.2021;[Epub] CrossRef - Impaired fasting glucose levels in overweight or obese subjects for screening of type 2 diabetes in Korea
Jin-Hee Lee, Suk Chon, Seon-Ah Cha, Sun-Young Lim, Kook-Rye Kim, Jae-Seung Yun, Sang Youl Rhee, Kun-Ho Yoon, Yu-Bae Ahn, Jeong-Taek Woo, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 382. CrossRef - Simple Sugar Intake in Diabetics and Non-Diabetic Patients Who Visit Primary Care Clinic
Seo Young Park, Geun Bae Moon, Young Sik Kim, Seung Hee Kim
Korean Journal of Family Practice.2021; 11(1): 29. CrossRef - Effect of Teneligliptin versus Sulfonylurea on Major Adverse Cardiovascular Outcomes in People with Type 2 Diabetes Mellitus: A Real-World Study in Korea
Da Hea Seo, Kyoung Hwa Ha, So Hun Kim, Dae Jung Kim
Endocrinology and Metabolism.2021; 36(1): 70. CrossRef - Best Achievements in Clinical Medicine in Diabetes and Dyslipidemia in 2020
Eun-Jung Rhee, Mee-Kyung Kim, Won-Young Lee
Endocrinology and Metabolism.2021; 36(1): 41. CrossRef - Factors Associated with Poor Glycemic Control Amongst Rural Residents with Diabetes in Korea
Junhee Ahn, Youngran Yang
Healthcare.2021; 9(4): 391. CrossRef - Diabetes and Stroke
Junghyun Noh
The Journal of Korean Diabetes.2021; 22(1): 26. CrossRef - Epidemiology of cardiovascular disease and its risk factors in Korea
Hyeon Chang Kim
Global Health & Medicine.2021; 3(3): 134. CrossRef - Cumulative exposure to impaired fasting glucose and future risk of type 2 diabetes mellitus
Mee Kyoung Kim, Kyungdo Han, Eun Sil Koh, Oak-Kee Hong, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Diabetes Research and Clinical Practice.2021; 175: 108799. CrossRef - No Relevant Pharmacokinetic Drug–Drug Interaction Between the Sodium-Glucose Co-Transporter-2 Inhibitor Empagliflozin and Lobeglitazone, a Peroxisome Proliferator-Activated Receptor-γ Agonist, in Healthy Subjects
Yu Kyong Kim, Jun Gi Hwang, Min Kyu Park
Drug Design, Development and Therapy.2021; Volume 15: 1725. CrossRef - Comparative Renal Effects of Dipeptidyl Peptidase-4 Inhibitors and Sodium-Glucose Cotransporter 2 Inhibitors on Individual Outcomes in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis
Jae Hyun Bae, Eun-Gee Park, Sunhee Kim, Sin Gon Kim, Seokyung Hahn, Nam Hoon Kim
Endocrinology and Metabolism.2021; 36(2): 388. CrossRef - The Association Between Second-Line Oral Antihyperglycemic Medication on Types of Dementia in Type 2 Diabetes: A Nationwide Real-World Longitudinal Study
Won Jun Kim, Jung Hyun Noh, Kyungdo Han, Cheol-Young Park
Journal of Alzheimer's Disease.2021; 81(3): 1263. CrossRef - Personalized Type 2 Diabetes Management Using a Mobile Application Integrated with Electronic Medical Records: An Ongoing Randomized Controlled Trial
Eun-Young Lee, Jae-Seung Yun, Seon-Ah Cha, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Seung-Hyun Ko
International Journal of Environmental Research and Public Health.2021; 18(10): 5300. CrossRef - Cerium Oxide Nanoparticle-Containing Colorimetric Contact Lenses for Noninvasively Monitoring Human Tear Glucose
Sijin Park, Juil Hwang, Hee-Jae Jeon, Woo Ri Bae, In-Kyung Jeong, Tae Gi Kim, Jaheon Kang, Young-Geun Han, Euiheon Chung, Dong Yun Lee
ACS Applied Nano Materials.2021; 4(5): 5198. CrossRef - Low nutritional status links to the prevalence of pre-metabolic syndrome and its cluster in metabolically high-risk Korean adults
Jieun Kim, Kyoungsik Jeong, Siwoo Lee, Bok-Nam Seo, Younghwa Baek
Medicine.2021; 100(20): e25905. CrossRef - Dynamics of Serum Retinol and Alpha-Tocopherol Levels According to Non-Alcoholic Fatty Liver Disease Status
Dongsub Jeon, Minkook Son, Juhyun Shim
Nutrients.2021; 13(5): 1720. CrossRef - Classification and Prediction on the Effects of Nutritional Intake on Overweight/Obesity, Dyslipidemia, Hypertension and Type 2 Diabetes Mellitus Using Deep Learning Model: 4–7th Korea National Health and Nutrition Examination Survey
Hyerim Kim, Dong Hoon Lim, Yoona Kim
International Journal of Environmental Research and Public Health.2021; 18(11): 5597. CrossRef - Comparison of insulin glargine 300 U/mL versus glargine 100 U/mL on glycemic control and hypoglycemic events in East Asian patients with type 2 diabetes: A Patient-level meta-analysis of phase 3 studies
Linong Ji, Yan Bi, Shandong Ye, Yun Huang, Xia Zhang, Shuhua Shang, Nan Cui, Huiqiu Yin, Minlu Zhang
Diabetes Research and Clinical Practice.2021; 176: 108848. CrossRef - Modifiable Risk Factors for Cardiovascular Disease in Korea and Japan
Ahmed Arafa, Hyeok-Hee Lee, Ehab S. Eshak, Kokoro Shirai, Keyang Liu, Jiaqi Li, Naharin Sultana Anni, Sun Young Shim, Hyeon Chang Kim, Hiroyasu Iso
Korean Circulation Journal.2021; 51(8): 643. CrossRef - Sodium-Glucose Cotransporter-2 Inhibitors Ameliorate Liver Enzyme Abnormalities in Korean Patients With Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Won Euh, Soo Lim, Jin-Wook Kim
Frontiers in Endocrinology.2021;[Epub] CrossRef - Effect of serum isoniazid level on treatment outcomes among tuberculosis patients with slow response – A retrospective cohort study
Hyung Woo Kim, Ah Young Shin, Jick Hwan Ha, Joong Hyun Ahn, Hye Seon Kang, Ju Sang Kim
Journal of Infection and Chemotherapy.2021; 27(11): 1555. CrossRef - Recent Perspective of Metformin
Sangmo Hong
The Journal of Korean Diabetes.2021; 22(2): 85. CrossRef - Diabetes Monotherapies versus Metformin-Based Combination Therapy for the Treatment of Type 2 Diabetes
Awadhesh K Singh, Ritu Singh, Partha Pratim Chakraborty
International Journal of General Medicine.2021; Volume 14: 3833. CrossRef - The Metabolic Score for Insulin Resistance (METS-IR) as a Predictor of Incident Ischemic Heart Disease: A Longitudinal Study among Korean without Diabetes
Jihyun Yoon, Donghyuk Jung, Yongjae Lee, Byoungjin Park
Journal of Personalized Medicine.2021; 11(8): 742. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study (Diabetes Metab J 2021;45:368-78)
Ja Young Jeon
Diabetes & Metabolism Journal.2021; 45(4): 613. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim,
Diabetes & Metabolism Journal.2021; 45(4): 461. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study (Diabetes Metab J 2021;45:368-78)
Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2021; 45(4): 617. CrossRef - Cardiovascular Safety of SGLT2 Inhibitors Compared to DPP4 Inhibitors and Sulfonylureas as the Second-Line of Therapy in T2DM Using Large, Real-World Clinical Data in Korea
Kyuho Kim, Sung Hee Choi
Diabetes & Metabolism Journal.2021; 45(4): 502. CrossRef - The Effects of Dietary Education Interventions on Individuals with Type 2 Diabetes: A Systematic Review and Meta-Analysis
Juri Kim, Myung-Haeng Hur
International Journal of Environmental Research and Public Health.2021; 18(16): 8439. CrossRef - Treatment Patterns of Type 2 Diabetes Assessed Using a Common Data Model Based on Electronic Health Records of 2000–2019
Kyung Ae Lee, Heung Yong Jin, Yu Ji Kim, Yong-Jin Im, Eun-Young Kim, Tae Sun Park
Journal of Korean Medical Science.2021;[Epub] CrossRef - Nonalcoholic fatty liver disease and the risk of insulin-requiring gestational diabetes
Sang Youn You, Kyungdo Han, Seung-Hawn Lee, Mee Kyoung Kim
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef - Comparison of the Effects of Various Antidiabetic Medication on Bone Mineral Density in Patients with Type 2 Diabetes Mellitus
Jeonghoon Ha, Yejee Lim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Ho Song, Seung Hyun Ko, Moo Il Kang, Sung Dae Moon, Ki-Hyun Baek
Endocrinology and Metabolism.2021; 36(4): 895. CrossRef - Non-Laboratory-Based Simple Screening Model for Nonalcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Developed Using Multi-Center Cohorts
Jiwon Kim, Minyoung Lee, Soo Yeon Kim, Ji-Hye Kim, Ji Sun Nam, Sung Wan Chun, Se Eun Park, Kwang Joon Kim, Yong-ho Lee, Joo Young Nam, Eun Seok Kang
Endocrinology and Metabolism.2021; 36(4): 823. CrossRef - High Fibrosis-4 Index Is Related with Worse Clinical Outcome in Patients with Coronavirus Disease 2019 and Diabetes Mellitus: A Multicenter Observational Study
Sung-Woo Kim, Jae-Han Jeon, Jun Sung Moon, Mi Kyung Kim
Endocrinology and Metabolism.2021; 36(4): 800. CrossRef - Predictive Value of the Atherogenic Index of Plasma (AIP) for the Risk of Incident Ischemic Heart Disease among Non-Diabetic Koreans
Julie J. Kim, Jihyun Yoon, Yong-Jae Lee, Byoungjin Park, Dong-Hyuk Jung
Nutrients.2021; 13(9): 3231. CrossRef - Quantity and quality of complementary and alternative medicine recommendations in clinical practice guidelines for type 2 diabetes mellitus: A systematic review
Jeremy Y. Ng, Kiran D. Verma, Kevin Gilotra
Nutrition, Metabolism and Cardiovascular Diseases.2021; 31(11): 3004. CrossRef - Framingham Risk Score Assessment in Subjects with Pre-diabetes and Diabetes: A Cross-Sectional Study in Korea
Hyuk Sang Kwon, Kee Ho Song, Jae Myung Yu, Dong Sun Kim, Ho Sang Shon, Kyu Jeung Ahn, Sung Hee Choi, Seung Hyun Ko, Won Kim, Kyoung Hwa Lee, Il Seong Nam-Goong, Tae Sun Park
Journal of Obesity & Metabolic Syndrome.2021; 30(3): 261. CrossRef - Frequency of Exposure to Impaired Fasting Glucose and Risk of Mortality and Cardiovascular Outcomes
Seung-Hwan Lee, Kyungdo Han, Hyuk-Sang Kwon, Mee Kyoung Kim
Endocrinology and Metabolism.2021; 36(5): 1007. CrossRef - How Can We Adopt the Glucose Tolerance Test to Facilitate Predicting Pregnancy Outcome in Gestational Diabetes Mellitus?
Kyeong Jin Kim, Nam Hoon Kim, Jimi Choi, Sin Gon Kim, Kyung Ju Lee
Endocrinology and Metabolism.2021; 36(5): 988. CrossRef - Symptom Clusters and Quality of Life in Patients with Type 2 Diabetes Mellitus
Su-Yeon Hong, Yang-Sook Yoo
Korean Journal of Adult Nursing.2021; 33(5): 498. CrossRef - Long-term effectiveness and safety of quadruple combination therapy with empagliflozin versus dapagliflozin in patients with type 2 diabetes: 3-year prospective observational study
Eu Jeong Ku, Dong-Hwa Lee, Hyun Jeong Jeon, Tae Keun Oh
Diabetes Research and Clinical Practice.2021; 182: 109123. CrossRef - Long-term effects of the mean hemoglobin A1c levels after percutaneous coronary intervention in patients with diabetes
Jaekyung Bae, Ji-Hyung Yoon, Jung-Hee Lee, Jong-Ho Nam, Chan-Hee Lee, Jang-Won Son, Ung Kim, Jong-Seon Park, Dong-Gu Shin
The Korean Journal of Internal Medicine.2021; 36(6): 1365. CrossRef - Role of Leptin with hypothyroidism in Iraqi diabetic type 2 patients
Sulaiman M. Hasan
Bionatura.2021; 6(4): 2274. CrossRef - Impacts of statin and metformin on neuropathy in patients with type 2 diabetes mellitus: Korean Health Insurance data
Hong Ki Min, Se Hee Kim, Jong Han Choi, Kyomin Choi, Hae-Rim Kim, Sang-Heon Lee
World Journal of Clinical Cases.2021; 9(33): 10198. CrossRef - Muscle strength, an independent determinant of glycemic control in older adults with long-standing type 2 diabetes: a prospective cohort study
Bo Kyung Koo, Seoil Moon, Min Kyong Moon
BMC Geriatrics.2021;[Epub] CrossRef - Comparisons of Neuropsychological Characteristics of Elderly Subjects With Versus Without History of Agent Orange Exposure
Seunggyu Han, Jinhee Choi, Hyung Seok So, Hayun Choi, Hong Jin Jeon, Jinseob Kim, Kiwon Kim
Journal of Korean Neuropsychiatric Association.2021; 60(4): 346. CrossRef - Uric Acid Variability as a Predictive Marker of Newly Developed Cardiovascular Events in Type 2 Diabetes
Hae Kyung Kim, Minyoung Lee, Yong-ho Lee, Byung-Wan Lee, Bong-Soo Cha, Eun Seok Kang
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Metformin use and cardiovascular outcomes in patients with diabetes and chronic kidney disease: a nationwide cohort study
Min Ho Kim, Hyung Jung Oh, Soon Hyo Kwon, Jin Seok Jeon, Hyunjin Noh, Dong Cheol Han, Hyoungnae Kim, Dong-Ryeol Ryu
Kidney Research and Clinical Practice.2021; 40(4): 660. CrossRef - Sleep Duration and Its Associations with Mortality and Quality of Life in Chronic Obstructive Pulmonary Disease: Results from the 2007–2015 KNAHNES
So Jeong Kim, Nakwon Kwak, Sun Mi Choi, Jinwoo Lee, Young Sik Park, Chang-Hoon Lee, Sang-Min Lee, Chul-Gyu Yoo, Jaeyoung Cho
Respiration.2021; 100(11): 1043. CrossRef - Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 382. CrossRef - Effects of Co‐administration of Sulfonylureas and Antimicrobial Drugs on Hypoglycemia in Patients with Type 2 Diabetes Using a Case‐Crossover Design
Sera Lee, Miyoung Ock, Hun‐Sung Kim, Hyunah Kim
Pharmacotherapy: The Journal of Human Pharmacology and Drug Therapy.2020; 40(9): 902. CrossRef - Diabetic kidney disease: seven questions
Dong Ho Yang, So-Young Lee
Journal of the Korean Medical Association.2020; 63(1): 6. CrossRef -
Diabetes and Metabolism Journal in 2020: Good to Great
In-Kyung Jeong
Diabetes & Metabolism Journal.2020; 44(1): 1. CrossRef - The Use of Mobile Personal Health Records for Hemoglobin A1c Regulation in Patients With Diabetes: Retrospective Observational Study
Dongjin Seo, Yu Rang Park, Yura Lee, Ji Young Kim, Joong-Yeol Park, Jae-Ho Lee
Journal of Medical Internet Research.2020; 22(6): e15372. CrossRef - Non-glucose risk factors in the pathogenesis of diabetic peripheral neuropathy
Kyung Ae Lee, Tae Sun Park, Heung Yong Jin
Endocrine.2020; 70(3): 465. CrossRef - An Assessment of Pharmacokinetic Interaction Between Lobeglitazone and Sitagliptin After Multiple Oral Administrations in Healthy Men
Seol Ju Moon, Kyung-Sang Yu, Min-Gul Kim
Clinical Therapeutics.2020; 42(6): 1047. CrossRef - The Clinical Characteristics and Outcomes of Patients with Moderate-to-Severe Coronavirus Disease 2019 Infection and Diabetes in Daegu, South Korea
Mi Kyung Kim, Jae-Han Jeon, Sung-Woo Kim, Jun Sung Moon, Nan Hee Cho, Eugene Han, Ji Hong You, Ji Yeon Lee, Miri Hyun, Jae Seok Park, Yong Shik Kwon, Yeon-Kyung Choi, Ki Tae Kwon, Shin Yup Lee, Eon Ju Jeon, Jin-Woo Kim, Hyo-Lim Hong, Hyun Hee Kwon, Chi Yo
Diabetes & Metabolism Journal.2020; 44(4): 602. CrossRef - The Risk of Diabetes on Clinical Outcomes in Patients with Coronavirus Disease 2019: A Retrospective Cohort Study
Seung Min Chung, Yin Young Lee, Eunyeong Ha, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee, Jian Hur, Kyung Soo Hong, Jong Geol Jang, Hyun Jung Jin, Eun Young Choi, Kyeong-Cheol Shin, Jin Hong Chung, Kwan Ho Lee, June Hong Ahn, Jun Sung Moon
Diabetes & Metabolism Journal.2020; 44(3): 405. CrossRef - A model to predict risk of stroke in middle-aged adults with type 2 diabetes generated from a nationwide population-based cohort study in Korea
Mee-Kyoung Kim, Kyungdo Han, Jae-Hyoung Cho, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Diabetes Research and Clinical Practice.2020; 163: 108157. CrossRef - Effects of Cardiovascular Risk Factor Variability on Health Outcomes
Seung-Hwan Lee, Mee Kyoung Kim, Eun-Jung Rhee
Endocrinology and Metabolism.2020; 35(2): 217. CrossRef - Sodium-Glucose Cotransporter-2 Inhibitor for Renal Function Preservation in Patients with Type 2 Diabetes Mellitus: A Korean Diabetes Association and Korean Society of Nephrology Consensus Statement
Tae Jung Oh, Ju-Young Moon, Kyu Yeon Hur, Seung Hyun Ko, Hyun Jung Kim, Taehee Kim, Dong Won Lee, Min Kyong Moon
Diabetes & Metabolism Journal.2020; 44(4): 489. CrossRef - Metformin Treatment for Patients with Diabetes and Chronic Kidney Disease: A Korean Diabetes Association and Korean Society of Nephrology Consensus Statement
Kyu Yeon Hur, Mee Kyoung Kim, Seung Hyun Ko, Miyeun Han, Dong Won Lee, Hyuk-Sang Kwon
Diabetes & Metabolism Journal.2020; 44(1): 3. CrossRef - Prevalence and Current Management of Cardiovascular Risk Factors in Korean Adults Based on Fact Sheets
Eun-Jung Rhee
Endocrinology and Metabolism.2020; 35(1): 85. CrossRef - Using adult stem cells to monitor endothelial dysfunction in diabetes mellitus
Rohit Jain, Hassan Awal, Sabyasachi Sen
Journal of Diabetes and its Complications.2020; 34(7): 107588. CrossRef - Fibrates Revisited: Potential Role in Cardiovascular Risk Reduction
Nam Hoon Kim, Sin Gon Kim
Diabetes & Metabolism Journal.2020; 44(2): 213. CrossRef - Metformin treatment for patients with diabetes and chronic kidney disease: A Korean Diabetes Association and Korean Society of Nephrology consensus statement
Kyu Yeon Hur, Mee Kyoung Kim, Seung Hyun Ko, Miyeun Han, Dong Won Lee, Hyuk-Sang Kwon
Kidney Research and Clinical Practice.2020; 39(1): 32. CrossRef - Generation of iPSC-derived insulin-producing cells from patients with type 1 and type 2 diabetes compared with healthy control
Min Jung Kim, Eun Young Lee, Young-Hye You, Hae Kyung Yang, Kun-Ho Yoon, Ji-Won Kim
Stem Cell Research.2020; 48: 101958. CrossRef - Glucose-Lowering Effect of Home-Delivered Therapeutic Meals in Patients with Type 2 Diabetes
Jong Han Choi, Se Hee Min, Kyeong Hye Lim, Uoon Jeong Shin, Min-Seon Kim
The Journal of Korean Diabetes.2020; 21(1): 46. CrossRef - Subclinical thyroid dysfunction in the first trimester of pregnancy: ‘Disease’ versus physiological (pulsatile) variation in TSH concentrations
Krzysztof C. Lewandowski, Karolina Garnysz, Wojciech Horzelski, Joanna Kawalec, Karolina Budzen, Mariusz Grzesiak, Andrzej Lewinski
Clinical Endocrinology.2020; 93(6): 739. CrossRef - Usefulness of carotid ultrasonography and treatment of carotid disease
Seung Min Kim, Yeon Jung Kim, Keonwoo Kim, Bum Joon Kim
Journal of the Korean Medical Association.2020; 63(6): 342. CrossRef - Clinical Characteristics and Prevalence of Comorbidities according to Metformin Use in Korean Patients with Type 2 Diabetes
Sang Ouk Chin, In Gyoon Ha, Sang Youl Rhee, Su Jin Jeong, Suk Chon, Sung Hoon Kim, Kyu Jeung Ahn, Sei Hyun Baik, Yongsoo Park, Moon Suk Nam, Kwan Woo Lee, Jeong Taek Woo
International Journal of Endocrinology.2020; 2020: 1. CrossRef - Prepregnancy smoking and the risk of gestational diabetes requiring insulin therapy
Mee Kyoung Kim, Kyungdo Han, Sang Youn You, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Scientific Reports.2020;[Epub] CrossRef - Use of SGLT-2 Inhibitors in Patients with Type 2 Diabetes Mellitus and Abdominal Obesity: An Asian Perspective and Expert Recommendations
Wayne Huey-Herng Sheu, Siew Pheng Chan, Bien J. Matawaran, Chaicharn Deerochanawong, Ambrish Mithal, Juliana Chan, Ketut Suastika, Chin Meng Khoo, Huu Man Nguyen, Ji Linong, Andrea Luk, Kun-Ho Yoon
Diabetes & Metabolism Journal.2020; 44(1): 11. CrossRef - Response: The Risk of Diabetes on Clinical Outcomes in Patients with Coronavirus Disease 2019: A Retrospective Cohort Study (Diabetes Metab J 2020;44:405–13)
Seung Min Chung, June Hong Ahn, Jun Sung Moon
Diabetes & Metabolism Journal.2020; 44(4): 625. CrossRef - Effect of roux-en Y gastric bypass surgery on patients with type 2 diabetes mellitus
Ke-Yan Chen, Ying-Li Liu, Jin-Cai Shang, De-Wang Su, Rong-Rong Yao, De-Zhi Ke, Hao Tian
Medicine.2020; 99(23): e20382. CrossRef - Comparison and Implication of the Contemporary Blood Pressure Guidelines on Korean Population
So Mi Jemma Cho, Hokyou Lee, Hyeon Chang Kim
Korean Circulation Journal.2020; 50(6): 485. CrossRef - Efficacy and safety of evogliptin treatment in patients with type 2 diabetes: A multicentre, active‐controlled, randomized, double‐blind study with open‐label extension (the EVERGREEN study)
Gyuri Kim, Soo Lim, Hyuk‐Sang Kwon, Ie B. Park, Kyu J. Ahn, Cheol‐Young Park, Su K. Kwon, Hye S. Kim, Seok W. Park, Sin G. Kim, Min K. Moon, Eun S. Kim, Choon H. Chung, Kang S. Park, Mikyung Kim, Dong J. Chung, Chang B. Lee, Tae H. Kim, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2020; 22(9): 1527. CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef - Predicting the Development of Myocardial Infarction in Middle-Aged Adults with Type 2 Diabetes: A Risk Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2020; 35(3): 636. CrossRef - Fasting Plasma Glucose Level Independently Predicts the Mortality of Patients with Coronavirus Disease 2019 Infection: A Multicenter, Retrospective Cohort Study
Min Cheol Chang, Jong-Moon Hwang, Jae-Han Jeon, Sang Gyu Kwak, Donghwi Park, Jun Sung Moon
Endocrinology and Metabolism.2020; 35(3): 595. CrossRef - Sodium-glucose cotransporter-2 inhibitor for renal function preservation in patients with type 2 diabetes mellitus: A Korean Diabetes Association and Korean Society of Nephrology consensus statement
Tae Jung Oh, Ju-Young Moon, Kyu Yeon Hur, Seung Hyun Ko, Hyun Jung Kim, Taehee Kim, Dong Won Lee, Min Kyong Moon
Kidney Research and Clinical Practice.2020; 39(3): 269. CrossRef - Dynamic changes in nocturnal blood glucose levels are associated with sleep-related features in patients with obstructive sleep apnea
Jung-Ick Byun, Kwang Su Cha, Ji Eun Jun, Tae-Joon Kim, Ki-Young Jung, In-Kyung Jeong, Won Chul Shin
Scientific Reports.2020;[Epub] CrossRef Effect of Switching from Linagliptin to Teneligliptin Dipeptidyl Peptidase-4 Inhibitors in Older Patients with Type 2 Diabetes Mellitus
Eugene Han, Minyoung Lee, Yong-ho Lee, Hye Soon Kim, Byung-wan Lee, Bong-Soo Cha, Eun Seok Kang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4113. CrossRef- A prospective cohort study on effects of gemigliptin on cardiovascular outcomes in patients with type 2 diabetes (OPTIMUS study)
Eun Heui Kim, Sang Soo Kim, Dong Jun Kim, Young Sik Choi, Chang Won Lee, Bon Jeong Ku, Kwang Soo Cha, Kee Ho Song, Dae Kyeong Kim, In Joo Kim
Scientific Reports.2020;[Epub] CrossRef - Effect of Variability in Blood Pressure, Glucose and Cholesterol Concentrations, and Body Weight on Emergency Hospitalization and 30‐Day Mortality in the General Population
Seung‐Hwan Lee, Kyungdo Han, Hyuk‐Sang Kwon, Kun‐Ho Yoon, Mee Kyoung Kim
Journal of the American Heart Association.2020;[Epub] CrossRef - Systematic review of clinical practice guidelines to identify recommendations for sleep in type 2 diabetes mellitus management
Aisling Smyth, Mark Jenkins, Melissa Dunham, Yvonne Kutzer, Shahrad Taheri, Lisa Whitehead
Diabetes Research and Clinical Practice.2020; 170: 108532. CrossRef - The risk factors for treatment-related mortality within first three months after kidney transplantation
Ye Na Kim, Do Hyoung Kim, Ho Sik Shin, Sangjin Lee, Nuri Lee, Min-Jeong Park, Wonkeun Song, Seri Jeong, Robert Jeenchen Chen
PLOS ONE.2020; 15(12): e0243586. CrossRef - The triglyceride glucose index is a simple and low-cost marker associated with atherosclerotic cardiovascular disease: a population-based study
Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMC Medicine.2020;[Epub] CrossRef - The triglyceride-glucose index predicts ischemic heart disease risk in Koreans: a prospective study using National Health Insurance Service data
Byoungjin Park, Yong-Jae Lee, Hye Sun Lee, Dong-Hyuk Jung
Cardiovascular Diabetology.2020;[Epub] CrossRef - Increased Age of Death and Change in Causes of Death Among Persons With Diabetes Mellitus From the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Eugene Han, Sun Ok Song, Hye Soon Kim, Kang Ju Son, Sun Ha Jee, Bong-Soo Cha, Byung-Wan Lee
SSRN Electronic Journal .2020;[Epub] CrossRef - Letter: Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study (Diabetes Metab J 2019;43:640–8)
Jun Sung Moon
Diabetes & Metabolism Journal.2019; 43(6): 911. CrossRef - Differences in prevalence of hypertension subtypes according to the 2018 Korean Society of Hypertension and 2017 American College of Cardiology/American Heart Association guidelines: The Korean National Health and Nutrition Examination Survey, 2007–2017 (
So Mi Jemma Cho, Hokyou Lee, Hyeon Chang Kim
Clinical Hypertension.2019;[Epub] CrossRef - Adult Stem Cells: Beyond Regenerative Tool, More as a Bio-Marker in Obesity and Diabetes
Sabyasachi Sen
Diabetes & Metabolism Journal.2019; 43(6): 744. CrossRef - Cholesterol levels and development of cardiovascular disease in Koreans with type 2 diabetes mellitus and without pre-existing cardiovascular disease
Mee Kyoung Kim, Kyungdo Han, Han Na Joung, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Cardiovascular Diabetology.2019;[Epub] CrossRef - Management of Cardiovascular Risk Factors in Elderly Diabetes Mellitus Patients
Sung Hoon Yu
The Journal of Korean Diabetes.2019; 20(4): 233. CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - An Age of Sodium-Glucose Cotransporter-2 Inhibitor Priority: Are We Ready?
Ji A Seo
Diabetes & Metabolism Journal.2019; 43(5): 578. CrossRef - Association between Diabetes and the Use of Removable Dental Prostheses among the Korean Population
Jae-Hyun Lee, Jung-Suk Han, Kyungdo Han, Su-Young Lee
Journal of Korean Medical Science.2019;[Epub] CrossRef - Metabolic Surgery and Diabetes Mellitus: Its Effects and Side Effects
Mee Kyoung Kim
The Journal of Korean Diabetes.2019; 20(4): 205. CrossRef
- Serum-based ATR-FTIR spectroscopy combined with multivariate analysis for the diagnosis of pre-diabetes and diabetes
- Clinical Diabetes & Therapeutics
- Nonalcoholic Fatty Liver Disease and Diabetes: Part II: Treatment
- Kyung-Soo Kim, Byung-Wan Lee, Yong Jin Kim, Dae Ho Lee, Bong-Soo Cha, Cheol-Young Park
- Diabetes Metab J. 2019;43(2):127-143. Published online April 15, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0034
- 7,673 View
- 140 Download
- 25 Web of Science
- 35 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Nonalcoholic fatty liver disease (NAFLD) and diabetes are common metabolic disorders that are often comorbid conditions. Among many proposed treatments, weight reduction is the only approved option for NAFLD to date. However, it is not easy to maintain weight loss by lifestyle modification alone; pharmacological treatments are helpful in this regard. Although many drugs have been investigated, pioglitazone could be a first-line therapy in patients with NAFLD and diabetes. Many more drugs are currently being developed and investigated, and it is likely that combination strategies will be used for future treatment of NAFLD and diabetes. Attention should be paid to the management of NAFLD and diabetes and efforts should be made to intervene early and individualize treatment of NAFLD in patients with diabetes.
-
Citations
Citations to this article as recorded by- Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMJ.2024; : e076388. CrossRef - Research Progress of Traditional Chinese Medicine and Western Medicine on Non-Alcoholic Fatty Liver Disease
强江 郭
Advances in Clinical Medicine.2024; 14(03): 561. CrossRef - Liver and cardiovascular disease outcomes in metabolic syndrome and diabetic populations: Bi-directional opportunities to multiply preventive strategies
Alhussain Yasin, Madison Nguyen, Angad Sidhu, Priyanka Majety, Jared Spitz, Amon Asgharpour, Mohammad S. Siddiqui, Laurence S. Sperling, Arshed A. Quyyumi, Anurag Mehta
Diabetes Research and Clinical Practice.2024; 211: 111650. CrossRef - Effect of aerobic training with silymarin consumption on glycemic indices and liver enzymes in men with type 2 diabetes
Keyvan Ghalandari, Mojtaba Shabani, Ali Khajehlandi, Amin Mohammadi
Archives of Physiology and Biochemistry.2023; 129(1): 76. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Mortality: A Population-Based Cohort Study
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(2): 220. CrossRef - Comparative antihypertensive efficacy of combinations of azilsartan medoxomil or olmesartan medoxomil with amlodipine in patients with arterial hypertension, type 2 diabetes mellitus and non-alcoholic fatty liver disease
I. А. Lukonin, V. V. Skibitsky, A. V. Fendrikova, A. V. Skibitsky, I. A. Antipov
South Russian Journal of Therapeutic Practice.2023; 4(1): 68. CrossRef - An Ethyl Acetate Extract of Eryngium carlinae Inflorescences Attenuates Oxidative Stress and Inflammation in the Liver of Streptozotocin-Induced Diabetic Rats
Cristian M. Trejo-Hurtado, Cinthia I. Landa-Moreno, Jenaro Lemus-de la Cruz, Donovan J. Peña-Montes, Rocío Montoya-Pérez, Rafael Salgado-Garciglia, Salvador Manzo-Avalos, Christian Cortés-Rojo, Juan Luis Monribot-Villanueva, José Antonio Guerrero-Analco,
Antioxidants.2023; 12(6): 1235. CrossRef - Pharmacogenetics of glucagon-like peptide-1 agonists in the treatment of type 2 diabetes mellitus
Iu.G. Samoilova, A.E. Stankova, M.V. Matveeva, O.E. Vaizova, D.V. Podchinenova, D.A. Kudlay, T.A. Filippova, I.R. Grishkevich
Profilakticheskaya meditsina.2023; 26(12): 95. CrossRef - Obesity is an important determinant of severity in newly defined metabolic dysfunction-associated fatty liver disease
Ji Hye Huh, Kwang Joon Kim, Seung Up Kim, Bong-Soo Cha, Byung-Wan Lee
Hepatobiliary & Pancreatic Diseases International.2022; 21(3): 241. CrossRef - Triglyceride and glucose index is a simple and easy‐to‐calculate marker associated with nonalcoholic fatty liver disease
Kyung‐Soo Kim, Sangmo Hong, Hong‐Yup Ahn, Cheol‐Young Park
Obesity.2022; 30(6): 1279. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Pharmacological Treatment of Nonalcoholic Fatty Liver Disease: Antidiabetic Agents
Kyung-Soo Kim
The Journal of Korean Diabetes.2022; 23(2): 83. CrossRef - Efficacy and mechanism of Jiedu Tongluo Tiaogan Formula in treating type 2 diabetes mellitus combined with non-alcoholic fatty liver disease: Study protocol for a parallel-armed, randomized controlled trial
Jinghan Xu, Chunli Piao, Yue Qu, Tianjiao Liu, Yuting Peng, Qi Li, Xiaohua Zhao, Pei Li, Xuemin Wu, Yawen Fan, Binqin Chen, Jie Yang
Frontiers in Pharmacology.2022;[Epub] CrossRef - Intestinal microbiota in the treatment of metabolically associated fatty liver disease
Ji-Shuai Wang, Jin-Chun Liu
World Journal of Clinical Cases.2022; 10(31): 11240. CrossRef - Efficiency of combined antihypertensive pharmacotherapy in patients with arterial hypertension, combined with type 2 diabetes mellitus and non-alcoholic fatty liver disease
I. A. Lukonin, V. V. Skibitsky, A. V. Fendrikova, I. I. Pavlyuchenko, K. Yu. Lazarev, F. A. Kovalenko
Systemic Hypertension.2022; 19(1): 31. CrossRef - Diosgenin Ameliorated Type II Diabetes-Associated Nonalcoholic Fatty Liver Disease through Inhibiting De Novo Lipogenesis and Improving Fatty Acid Oxidation and Mitochondrial Function in Rats
Yujie Zhong, Zhiman Li, Ruyi Jin, Yanpeng Yao, Silan He, Min Lei, Xin Wang, Chao Shi, Li Gao, Xiaoli Peng
Nutrients.2022; 14(23): 4994. CrossRef - Pluchea indica Leaf Extract Alleviates Dyslipidemia and Hepatic Steatosis by Modifying the Expression of Lipid Metabolism-Related Genes in Rats Fed a High Fat-High Fructose Diet
Patcharin Singdam, Jarinyaporn Naowaboot, Laddawan Senggunprai, Kampeebhorn Boonloh, Patchareewan Pannangpetch
Preventive Nutrition and Food Science.2022; 27(4): 384. CrossRef - NAFLDin type 2 diabetes mellitus: Still many challenging questions
Simona Cernea, Itamar Raz
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Umbilical Cord-Mesenchymal Stem Cell-Conditioned Medium Improves Insulin Resistance in C2C12 Cell
Kyung-Soo Kim, Yeon Kyung Choi, Mi Jin Kim, Jung Wook Hwang, Kyunghoon Min, Sang Youn Jung, Soo-Kyung Kim, Yong-Soo Choi, Yong-Wook Cho
Diabetes & Metabolism Journal.2021; 45(2): 260. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: Diagnosis and Treatment
Sook Jung Lee, Byung-Wan Lee
The Journal of Korean Diabetes.2021; 22(1): 38. CrossRef - Patient Management in Non-Alcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus
A. E. Bagriy, A. D. Zubov, M. V. Khomenko, E. S. Mikhailichenko, E. A. Pylaeva, N. A. Khaustova, E. V. Bryukhovetskaya
Russian Journal of Gastroenterology, Hepatology, Coloproctology.2021; 31(2): 14. CrossRef - NAFLD and its link with diabetes: Why we should be worried
Louise Cremonesini, Emma Harkin
Independent Nurse.2021; 2021(8): 20. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef - Fatty liver index and development of cardiovascular disease in Koreans without pre-existing myocardial infarction and ischemic stroke: a large population-based study
Jun Hyung Kim, Jin Sil Moon, Seok Joon Byun, Jun Hyeok Lee, Dae Ryong Kang, Ki Chul Sung, Jang Young Kim, Ji Hye Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Novel antisense inhibition of diacylglycerol O-acyltransferase 2 for treatment of non-alcoholic fatty liver disease: a multicentre, double-blind, randomised, placebo-controlled phase 2 trial
Rohit Loomba, Erin Morgan, Lynnetta Watts, Shuting Xia, Lisa A Hannan, Richard S Geary, Brenda F Baker, Sanjay Bhanot
The Lancet Gastroenterology & Hepatology.2020; 5(9): 829. CrossRef - Hepatic fibrosis is associated with total proteinuria in Korean patients with type 2 diabetes
Eugene Han, Yongin Cho, Kyung-won Kim, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-wan Lee
Medicine.2020; 99(33): e21038. CrossRef - Metabolic liver disease in diabetes – From mechanisms to clinical trials
Bedair Dewidar, Sabine Kahl, Kalliopi Pafili, Michael Roden
Metabolism.2020; 111: 154299. CrossRef - Managing NAFLD in Type 2 Diabetes: The Effect of Lifestyle Interventions, a Narrative Review
Siôn A. Parry, Leanne Hodson
Advances in Therapy.2020; 37(4): 1381. CrossRef -
Diabetes and Metabolism Journal in 2020: Good to Great
In-Kyung Jeong
Diabetes & Metabolism Journal.2020; 44(1): 1. CrossRef - Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 382. CrossRef - Molecular mechanisms of hepatic insulin resistance in nonalcoholic fatty liver disease and potential treatment strategies
Chang-hua Zhang, Bu-gao Zhou, Jun-qing Sheng, Yang Chen, Ying-qian Cao, Chen Chen
Pharmacological Research.2020; 159: 104984. CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef - Effects of sodium–glucose cotransporter 2 inhibitors on non‐alcoholic fatty liver disease in patients with type 2 diabetes: A meta‐analysis of randomized controlled trials
Baodi Xing, Yuhang Zhao, Bingzi Dong, Yue Zhou, Wenshan Lv, Wenjuan Zhao
Journal of Diabetes Investigation.2020; 11(5): 1238. CrossRef - Empaglifozin mitigates NAFLD in high-fat-fed mice by alleviating insulin resistance, lipogenesis and ER stress
Tamiris Ingrid Petito-da-Silva, Vanessa Souza-Mello, Sandra Barbosa-da-Silva
Molecular and Cellular Endocrinology.2019; 498: 110539. CrossRef
- Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
- Clinical Diabetes & Therapeutics
-
- Asian Subpopulations May Exhibit Greater Cardiovascular Benefit from Long-Acting Glucagon-Like Peptide 1 Receptor Agonists: A Meta-Analysis of Cardiovascular Outcome Trials
- Yu Mi Kang, Yun Kyung Cho, Jiwoo Lee, Seung Eun Lee, Woo Je Lee, Joong-Yeol Park, Ye-Jee Kim, Chang Hee Jung, Michael A. Nauck
- Diabetes Metab J. 2019;43(4):410-421. Published online December 27, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0070
- 6,322 View
- 137 Download
- 18 Web of Science
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Based on reported results of three large cardiovascular outcome trials (CVOTs) of glucagon-like peptide 1 receptor agonists (GLP-1 RAs), we aimed to investigate the overall effect of GLP-1 RAs on major adverse cardiovascular events (MACEs) and to identify subpopulations exhibiting the greatest cardiovascular (CV) benefit.
Methods Three CVOTs reporting effects of long-acting GLP-1 RAs were included: LEADER (liraglutide), SUSTAIN-6 (semaglutide), and EXSCEL (exenatide once weekly). In all studies, the primary endpoint was three-point MACE, comprising CV death, non-fatal myocardial infarction, and non-fatal stroke. Overall effect estimates were calculated as hazard ratios and 95% confidence intervals (CIs) using the random-effects model; subgroup analyses reported in the original studies were similarly analyzed.
Results Overall, statistically significant risk reductions in MACE and CV death were observed. Subgroup analysis indicated a significant racial difference with respect to CV benefit (
P for interaction <0.001), and more substantial risk reductions were observed in subjects of African origin (relative risk [RR], 0.78; 95% CI, 0.60 to 0.99) and in Asians (RR, 0.35; 95% CI, 0.09 to 1.32). However,post hoc analysis (Bonferroni method) revealed that only Asians exhibited a significantly greater CV benefit from treatment, compared with white subjects (P <0.0001).Conclusion Long-acting GLP-1 RAs reduced risks of MACE and CV deaths in high-risk patients with type 2 diabetes mellitus. Our findings of a particularly effective reduction in CV events with GLP-1 RA in Asian populations merits further exploration and dedicated trials in specific populations.
-
Citations
Citations to this article as recorded by- Sex, racial, ethnic, and geographical disparities in major adverse cardiovascular outcome of glucagon-like peptide-1 receptor agonists among patients with and without diabetes mellitus: A meta-analysis of placebo-controlled randomized controlled trials,
Frederick Berro Rivera, Nathan Ross B. Bantayan, John Paul Aparece, Linnaeus Louisse A. Cruz, John Vincent Magallong, Polyn Luz Pine, Anne Mira Nicca Idian-Javier, Grace Nooriza O. Lumbang, Edgar V. Lerma, Kyla M. Lara-Breitinger, Martha Gulati, Krishnasw
Journal of Clinical Lipidology.2024;[Epub] CrossRef - Coronary Artery Disease in South Asian Patients: Cardiovascular Risk Factors, Pathogenesis and Treatments
Vincenzo Sucato, Giuseppe Coppola, Girolamo Manno, Giuseppe Vadalà, Giuseppina Novo, Egle Corrado, Alfredo Ruggero Galassi
Current Problems in Cardiology.2023; 48(8): 101228. CrossRef - Retrospective Analysis of the Effectiveness of Oral Semaglutide in Type 2 Diabetes Mellitus and Its Effect on Cardiometabolic Parameters in Japanese Clinical Settings
Hodaka Yamada, Masashi Yoshida, Shunsuke Funazaki, Jun Morimoto, Shiori Tonezawa, Asuka Takahashi, Shuichi Nagashima, Kimura Masahiko, Otsuka Kiyoshi, Kazuo Hara
Journal of Cardiovascular Development and Disease.2023; 10(4): 176. CrossRef - Efficacy of treatment with glucagon-like peptide receptor agonists-1 in Asian patients with type 2 diabetes mellitus
L. Yu. Khamnueva, L. S. Andreeva
Problems of Endocrinology.2023; 69(2): 38. CrossRef - Role of diabetes in stroke: Recent advances in pathophysiology and clinical management
Sian A. Bradley, Kevin J. Spring, Roy G. Beran, Dimitrios Chatzis, Murray C. Killingsworth, Sonu M. M. Bhaskar
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - Obesity Pillars Roundtable: Obesity and East Asians
Harold Edward Bays, Jennifer Ng, Jeffrey Sicat, Michelle Look
Obesity Pillars.2022; 2: 100011. CrossRef - Pathophysiology, phenotypes and management of type 2 diabetes mellitus in Indian and Chinese populations
Calvin Ke, K. M. Venkat Narayan, Juliana C. N. Chan, Prabhat Jha, Baiju R. Shah
Nature Reviews Endocrinology.2022; 18(7): 413. CrossRef - Effect of race on cardiometabolic responses to once-weekly exenatide: insights from the Exenatide Study of Cardiovascular Event Lowering (EXSCEL)
Timothy M. E. Davis, Anna Giczewska, Yuliya Lokhnygina, Robert J. Mentz, Naveed Sattar, Rury R. Holman
Cardiovascular Diabetology.2022;[Epub] CrossRef - Generalizability of the Results of Cardiovascular Outcome Trials of Glucagon-Like Peptide 1 Receptor Agonists in Chinese Patients with Type 2 Diabetes Mellitus
Xiaoling Cai, Linong Ji
Diabetes Therapy.2021; 12(7): 1861. CrossRef - Current trends in epidemiology of cardiovascular disease and cardiovascular risk management in type 2 diabetes
Jae-Seung Yun, Seung-Hyun Ko
Metabolism.2021; 123: 154838. CrossRef - Sex and ethnic differences in the cardiovascular complications of type 2 diabetes
Jian L. Yeo, Emer M. Brady, Gerry P. McCann, Gaurav S. Gulsin
Therapeutic Advances in Endocrinology and Metabolism.2021; 12: 204201882110342. CrossRef - Efficacy and Safety of GLP-1 Receptor Agonists in Patients With Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis
Yuan Zhu, Jiao Xu, Dong Zhang, Xingyu Mu, Yi Shi, Shangtao Chen, Zengxiang Wu, Shuangqing Li
Frontiers in Endocrinology.2021;[Epub] CrossRef - Efficacy and safety of dulaglutide in type 2 diabetes patients in endocrinology clinics of Islamabad, Pakistan
Matiullah Kamin, SajjadAli Khan, UmarYousaf Raja, Osama Ishtiaq, Asmara Malik, Tejhmal Rehman, MuhammadUmar Wahab
Indian Journal of Endocrinology and Metabolism.2021; 25(5): 456. CrossRef - Type 2 Diabetes and Atherosclerotic Cardiovascular Disease in South Asians: a Unique Population with a Growing Challenge
Afreen I. Shariff, Nitya Kumar, William S. Yancy, Leonor Corsino
Current Diabetes Reports.2020;[Epub] CrossRef - Antihypertensive and Renal Mechanisms of SGLT2 (Sodium-Glucose Linked Transporter 2) Inhibitors
Christopher S. Wilcox
Hypertension.2020; 75(4): 894. CrossRef - Subpopulation Differences in the Cardiovascular Efficacy of Long-Acting Glucagon-Like Peptide 1 Receptor Agonists in Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis
Liyun He, Na Yang, Lingling Xu, Fan Ping, Wei Li, Yuxiu Li, Huabing Zhang
Diabetes Therapy.2020; 11(9): 2121. CrossRef - 2020 Consensus of Taiwan Society of Cardiology on the pharmacological management of patients with type 2 diabetes and cardiovascular diseases
Chern-En Chiang, Kwo-Chang Ueng, Ting-Hsing Chao, Tsung-Hsien Lin, Yih-Jer Wu, Kang-Ling Wang, Shih-Hsien Sung, Hung-I Yeh, Yi-Heng Li, Ping-Yen Liu, Kuan-Cheng Chang, Kou-Gi Shyu, Jin-Long Huang, Cheng-Dao Tsai, Huei-Fong Hung, Ming-En Liu, Tze-Fan Chao,
Journal of the Chinese Medical Association.2020; 83(7): 587. CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef
- Sex, racial, ethnic, and geographical disparities in major adverse cardiovascular outcome of glucagon-like peptide-1 receptor agonists among patients with and without diabetes mellitus: A meta-analysis of placebo-controlled randomized controlled trials,
- Complications
- Update on the Impact, Diagnosis and Management of Cardiovascular Autonomic Neuropathy in Diabetes: What Is Defined, What Is New, and What Is Unmet
- Vincenza Spallone
- Diabetes Metab J. 2019;43(1):3-30. Published online November 2, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0259
- 16,037 View
- 402 Download
- 153 Web of Science
- 156 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The burden of diabetic cardiovascular autonomic neuropathy (CAN) is expected to increase due to the diabetes epidemic and its early and widespread appearance. CAN has a definite prognostic role for mortality and cardiovascular morbidity. Putative mechanisms for this are tachycardia, QT interval prolongation, orthostatic hypotension, reverse dipping, and impaired heart rate variability, while emerging mechanisms like inflammation support the pervasiveness of autonomic dysfunction. Efforts to overcome CAN under-diagnosis are on the table: by promoting screening for symptoms and signs; by simplifying cardiovascular reflex tests; and by selecting the candidates for screening. CAN assessment allows for treatment of its manifestations, cardiovascular risk stratification, and tailoring therapeutic targets. Risk factors for CAN are mainly glycaemic control in type 1 diabetes mellitus (T1DM) and, in addition, hypertension, dyslipidaemia, and obesity in type 2 diabetes mellitus (T2DM), while preliminary data regard glycaemic variability, vitamin B12 and D changes, oxidative stress, inflammation, and genetic biomarkers. Glycaemic control prevents CAN in T1DM, whereas multifactorial intervention might be effective in T2DM. Lifestyle intervention improves autonomic function mostly in pre-diabetes. While there is no conclusive evidence for a disease-modifying therapy, treatment of CAN manifestations is available. The modulation of autonomic function by SGLT2i represents a promising research field with possible clinical relevance.
-
Citations
Citations to this article as recorded by- Rectal sensitivity correlated with gastrointestinal‐mediated glucose disposal, but not the incretin effect
Sondre Meling, Erling Tjora, Heike Eichele, Rasmus B. Nedergaard, Filip K. Knop, Niels Ejskjaer, Siri Carlsen, Pål R. Njølstad, Christina Brock, Eirik Søfteland
Endocrinology, Diabetes & Metabolism.2024;[Epub] CrossRef - Glucose metabolism and autonomic function in healthy individuals and patients with type 2 diabetes mellitus at rest and during exercise
Takuto Hamaoka, Urs A. Leuenberger, Rachel C. Drew, Matthew Murray, Cheryl Blaha, Jonathan Carter Luck, Lawrence I. Sinoway, Jian Cui
Experimental Physiology.2024; 109(2): 214. CrossRef - Quantification of lipoproteins by proton nuclear magnetic resonance spectroscopy (1H-NMRS) improves the prediction of cardiac autonomic dysfunction in patients with type 1 diabetes
L. Nattero-Chávez, M. Insenser, N. Amigó, S. Samino, N. Martínez-Micaelo, B. Dorado Avendaño, A. Quintero Tobar, H. F. Escobar-Morreale, M. Luque-Ramírez
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Predictors of pacemaker requirement in patients with implantable loop recorder and unexplained syncope: A systematic review and meta‐analysis
Moein Zangiabadian, Kiarash Soltani, Yasaman Gholinejad, Reyhane Yahya, Shayan Bastami, Mohammad Ali Akbarzadeh, Mohammad Sharifian Ardestani, Azadeh Aletaha
Clinical Cardiology.2024;[Epub] CrossRef - No clear evidence of neuropathy among patients with high risk for the development of prediabetes/diabetes—a pilot study
Anna E. Körei, Magdolna Békeffy, Adrienn Menyhárt, Karola Osgyán, Ildikó Istenes, Viktor J. Horváth, Péter Kempler
Frontiers in Endocrinology.2024;[Epub] CrossRef - Effects of Physical Cues on Stem Cell-Derived Extracellular Vesicles toward Neuropathy Applications
Danyale Berry, Justice Ene, Aakash Nathani, Mandip Singh, Yan Li, Changchun Zeng
Biomedicines.2024; 12(3): 489. CrossRef - Oxidative stress, endothelial dysfunction, and N-acetylcysteine in type-2 diabetes mellitus
Xin Li, Junyong Zou, Aiping Lin, Jingshu Chi, Hong Hao, Hong Chen, Zhenguo Liu
Antioxidants & Redox Signaling.2024;[Epub] CrossRef - High dose cholecalciferol supplementation causing morning blood pressure reduction in patients with type 1 diabetes mellitus and cardiovascular autonomic neuropathy
João Felício, Lorena Moraes, Gabriela Lemos, Ícaro Souza, Giovana Vieira, Lilian Silva, Natércia Queiroz, Ana Carolina Souza, Franciane Melo, João Felício Abrahão Neto, Hana Britto, Manuela Lemos, Márcia Santos, Priscila Figueiredo, Ana Regina Motta, Meli
Scientific Reports.2024;[Epub] CrossRef - Transcutaneous vagal nerve stimulation for treating gastrointestinal symptoms in individuals with diabetes: a randomised, double-blind, sham-controlled, multicentre trial
Ditte S. Kornum, Davide Bertoli, Huda Kufaishi, Anne-Marie Wegeberg, Tina Okdahl, Esben B. Mark, Katrine L. Høyer, Jens B. Frøkjær, Birgitte Brock, Klaus Krogh, Christian S. Hansen, Filip K. Knop, Christina Brock, Asbjørn M. Drewes
Diabetologia.2024;[Epub] CrossRef - Independent and interactive associations of heart rate and obesity with type 2 diabetes mellites: A population‐based study
Tianxin Zhu, Qingyu Chen, Hongxing Chen, Lili You, Dan Liu, Xiaoyun Zhang, Feng Li, Hongshi Wu, Juying Tang, Diaozhu Lin, Kan Sun, Li Yan, Meng Ren
Journal of Diabetes.2024;[Epub] CrossRef - Mortality risk factors in newly diagnosed diabetic cardiac autonomic neuropathy
Bruce A. Chase, Sylwia Pocica, Roberta Frigerio, Katerina Markopoulou, Demetrius M. Maraganore, Navamon Aunaetitrakul, Alexander Epshteyn, Alexandru C. Barboi
Clinical Autonomic Research.2023; 33(6): 903. CrossRef - Autonomic symptoms and associated factors in patients with chronic heart failure
Hellen Da Silva, Sofie Pardaens, Marc Vanderheyden, Johan De Sutter, Heleen Demeyer, Michel De Pauw, Laurent Demulier, Jan Stautemas, Patrick Calders
Acta Cardiologica.2023; 78(2): 203. CrossRef - Incretins and microvascular complications of diabetes: neuropathy, nephropathy, retinopathy and microangiopathy
Jonathan Goldney, Jack A. Sargeant, Melanie J. Davies
Diabetologia.2023; 66(10): 1832. CrossRef - Functional and morphometric assessment of small-fibre damage in late-onset hereditary transthyretin amyloidosis with polyneuropathy: the controversial relation between small-fibre-related symptoms and diagnostic test findings
Eleonora Galosi, Luca Leonardi, Pietro Falco, Giuseppe Di Pietro, Alessandra Fasolino, Nicoletta Esposito, Caterina Leone, Giulia Di Stefano, Maurizio Inghilleri, Marco Luigetti, Antonini Giovanni, Andrea Truini
Amyloid.2023; 30(1): 59. CrossRef - In vivo molecular imaging of cardiac angiogenesis in persons with and without type 2 diabetes: A cross‐sectional 68 Ga‐RGD‐PET study
Jens Christian Laursen, Ida Kirstine Bull Rasmussen, Emilie Hein Zobel, Philip Hasbak, Lene Holmvang, Christian Stevns Hansen, Bernt Johan von Scholten, Marie Frimodt‐Møller, Peter Rossing, Tine Willum Hansen, Andreas Kjaer, Rasmus Sejersten Ripa
Diabetic Medicine.2023;[Epub] CrossRef - Cardiac innervations in diabetes mellitus—Anatomical evidence of neuropathy
Natalija Filipović, Maja Marinović Guić, Vana Košta, Katarina Vukojević
The Anatomical Record.2023; 306(9): 2345. CrossRef - Clinical Predictors of Pacing Device Implantation in Implantable Cardiac Monitor Recipients for Unexplained Syncope
Reina Tonegawa-Kuji, Yuko Y. Inoue, Michikazu Nakai, Koshiro Kanaoka, Yoko Sumita, Yuichiro Miyazaki, Akinori Wakamiya, Keiko Shimamoto, Nobuhiko Ueda, Kenzaburo Nakajima, Naoya Kataoka, Mitsuru Wada, Kenichiro Yamagata, Kohei Ishibashi, Koji Miyamoto, Sa
CJC Open.2023; 5(4): 259. CrossRef - Cardiovascular autonomic reflex tests using a handheld device in the diagnosis of cardiovascular autonomic neuropathy in patients with schizophrenia
Laura Blok-Husum, Milka Ane Rank Brcelic, Hanin Kawa Farman Kawal Bassi, Svend Eggert Jensen, Rene Ernst Nielsen, Kristian Kragholm, Jesper Fleischer, Esben Laugesen, Christoffer Polcwiartek
American Heart Journal Plus: Cardiology Research and Practice.2023; 26: 100252. CrossRef - Causal association between vitamin D and diabetic neuropathy: a Mendelian randomization analysis
Wei Huang, Lei Gu, Jingwen Wang, Yiqi Wang, Fangzheng Cao, Tianyu Jin, Yifan Cheng
Endocrine.2023; 80(2): 328. CrossRef - Diabetes Mellitus and Heart Failure: Epidemiology, Pathophysiologic Mechanisms, and the Role of SGLT2 Inhibitors
Panagiotis Theofilis, Evangelos Oikonomou, Konstantinos Tsioufis, Dimitris Tousoulis
Life.2023; 13(2): 497. CrossRef - Sex differences and sex steroids influence on the presentation and severity of cardiovascular autonomic neuropathy of patients with type 1 diabetes
Lía Nattero-Chávez, María Insenser, Alejandra Quintero Tobar, Elena Fernández-Durán, Beatriz Dorado Avendaño, Tom Fiers, Jean-Marc Kaufman, Manuel Luque-Ramírez, Héctor F. Escobar-Morreale
Cardiovascular Diabetology.2023;[Epub] CrossRef - Early Gastrointestinal Neuropathy Assessed by Wireless Motility Capsules in Adolescents with Type 1 Diabetes
Vinni Faber Rasmussen, Mathilde Thrysøe, Páll Karlsson, Esben Thyssen Vestergaard, Kurt Kristensen, Ann-Margrethe Rønholt Christensen, Jens Randel Nyengaard, Astrid Juhl Terkelsen, Christina Brock, Klaus Krogh
Journal of Clinical Medicine.2023; 12(5): 1925. CrossRef - Heart rate variability in people with metabolic syndrome
Kostiantyn Apykhtin, Svitlana Drozdovska, Olha Hurenko, Anastasiia Nahorna, Anatoly Pisaruk, Yuliia Panchenko, Olena Andrieieva
Ageing & Longevity.2023; (1 2023): 1. CrossRef - Heart rate variability in people with metabolic syndrome
Kostiantyn Apykhtin, Svitlana Drozdovska, Olha Hurenko, Anastasiia Nahorna, Anatoly Pisaruk, Yuliia Panchenko, Olena Andrieieva
JOURNAL OF THE NATIONAL ACADEMY OF MEDICAL SCIENCES OF UKRAINE.2023; (1 2023): 1. CrossRef - Potential of electronic devices for detection of health problems in older adults at home: A systematic review and meta-analysis
Yu-ting Cao, Xin-xin Zhao, Yi-ting Yang, Shi-jie Zhu, Liang-dong Zheng, Ting Ying, Zhou Sha, Rui Zhu, Tao Wu
Geriatric Nursing.2023; 51: 54. CrossRef - Diabetes mellitus in der Akut- und Notfallmedizin
Leo Benning, Julian Krehl, Felix Patricius Hans
Notfallmedizin up2date.2023; 18(01): 45. CrossRef - Correlation between Heart rate recovery and Left Atrial phasic functions evaluated by 2D speckle-tracking Echocardiography after Acute Myocardial infarction
Behruz Mashayekhi, Reza Mohseni-Badalabadi, Ali Hosseinsabet, Tahereh Ahmadian
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Pancreatic sympathetic innervation disturbance in type 1 diabetes
Senlin Li, Huimin Yuan, Keshan Yang, Qing Li, Ming Xiang
Clinical Immunology.2023; 250: 109319. CrossRef - A Nonrandomized Trial of the Effects of Passive Simulated Jogging on Short-Term Heart Rate Variability in Type 2 Diabetic Subjects
Jose A. Adams, Jose R. Lopez, Veronica Banderas, Marvin A. Sackner, Mark Yorek
Journal of Diabetes Research.2023; 2023: 1. CrossRef - Evaluating treatment options for cardiovascular autonomic neuropathy in patients with diabetes mellitus: a systematic review
Jasmine KaiLi Goh, Leroy Koh
Diabetology International.2023; 14(3): 224. CrossRef - Autonomic neuropathic symptoms in patients with diabetes: practical tools for screening in daily routine
Ana Raquel Souza de Azevedo Vieira, Lara Benigno Porto-Dantas, Flaviene Alves do Prado Romani, Patrícia Souza Carvalho, Rodica Pop-Busui, Hermelinda Cordeiro Pedrosa
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - “Arterial stiffness is not associated with changes in the circadian pattern of blood pressure in patients with type 1 diabetes mellitus and cardiovascular autonomic dysfunction”
Lía Nattero-Chávez, Ane Bayona Cebada, Elena Fernández-Durán, Alejandra Quintero Tobar, Beatriz Dorado Avendaño, Héctor Escobar-Morreale, Manuel Luque-Ramírez
Diabetes and Vascular Disease Research.2023; 20(3): 147916412311736. CrossRef - Frontiers in diagnostic and therapeutic approaches in diabetic sensorimotor neuropathy (DSPN)
Sanjeev Sharma, Gerry Rayman
Frontiers in Endocrinology.2023;[Epub] CrossRef - In Type 2 Diabetes Mellitus, normalization of hemoglobin A1c accompanies reduced sensitivity to pressure at the sternum
Jens Faber, Søren Ballegaard, Nanna Ørsted, Ebbe Eldrup, Benny Karpatschof, Finn Gyntelberg, Sofie Korsgaard Hecquet, Albert Gjedde
Frontiers in Neuroscience.2023;[Epub] CrossRef - Functional status associated with postural dizziness, but not postural hypotension, in older adults: a community-based study
Hsiang-Ju Cheng, Zih-Jie Sun, Feng-Hwa Lu, Yi-Ching Yang, Chih-Jen Chang, Jin-Shang Wu
BMC Geriatrics.2023;[Epub] CrossRef - Effects of baricitinib, empagliflozin, linagliptin and telmisartan on cardiovascular autonomic neuropathy in type 1 diabetes: An exploratory, randomized, open‐label, crossover trial
Jens Christian Laursen, Viktor Rotbain Curovic, Marjolein Y. A. M. Kroonen, Niels Jongs, Emilie H. Zobel, Tine W. Hansen, Marie Frimodt‐Møller, Gozewijn D. Laverman, Adriaan Kooy, Frederik Persson, Hiddo J. L. Heerspink, Christian Stevns Hansen, Peter Ros
Diabetes, Obesity and Metabolism.2023; 25(10): 3064. CrossRef - The Retinal Nerve Fiber Layer Thickness Is Associated with Systemic Neurodegeneration in Long-Term Type 1 Diabetes
Christina Brock, Anne-Marie Wegeberg, Thomas Arendt Nielsen, Bassam Karout, Per M. Hellström, Asbjørn Mohr Drewes, Henrik Vorum
Translational Vision Science & Technology.2023; 12(6): 23. CrossRef - The Use of Empirical Mode Decomposition on Heart Rate Variability Signals to Assess Autonomic Neuropathy Progression in Type 2 Diabetes
Sandra Cossul, Felipe Rettore Andreis, Mateus Andre Favretto, Jefferson Luiz Brum Marques
Applied Sciences.2023; 13(13): 7824. CrossRef - Topical capsaicin for the management of painful diabetic neuropathy: a narrative systematic review
Brandon Goodwin, Maanas Chiplunkar, Ryan Salerno, Kylon Coombs, Umar Sannoh, Vrushank Shah, Nicholas Averell, Usmaan Al-Shebab, Deanna Janora
Pain Management.2023; 13(5): 309. CrossRef - Adynamic response to cold pain reflects dysautonomia in type 1 diabetes and polyneuropathy
Thomas Arendt Nielsen, Søren Lundbye-Christensen, Yoanna Krasimirova Dimitrova, Sam Riahi, Birgitte Brock, Asbjørn Mohr Drewes, Christina Brock
Scientific Reports.2023;[Epub] CrossRef - Autonomic Nerve Function Tests in Patients with Diabetes
Heung Yong Jin, Tae Sun Park
The Journal of Korean Diabetes.2023; 24(2): 71. CrossRef - Understanding the role of hyperglycemia and the molecular mechanism associated with diabetic neuropathy and possible therapeutic strategies
Mandeep Kaur, Sakshi Misra, Priyanka Swarnkar, Preeti Patel, Balak Das Kurmi, Ghanshyam Das Gupta, Amrita Singh
Biochemical Pharmacology.2023; 215: 115723. CrossRef - A three-month physical training program improves cardiovascular autonomic function in patients with metabolic syndrome with and without diabetes – a pilot study
Anna Vágvölgyi, Judit Erzsébet Ábrahám, Éva Máthéné Köteles, Andrea Korom, Mária Barnai, Mónika Szűcs, Andrea Orosz, Péter Kempler, Adrienn Menyhárt, Attila Nemes, Tamás Várkonyi, István Baczkó, István Kósa, Csaba Lengyel
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cardiovascular autonomic neuropathy in patients with type 2 diabetes with and without sensorimotor polyneuropathy
Emil Peters, Mustapha Itani, Alexander G. Kristensen, Astrid Juhl Terkelsen, Thomas Krøigård, Hatice Tankisi, Troels S. Jensen, Nanna B. Finnerup, Sandra Sif Gylfadottir
Journal of the Peripheral Nervous System.2023; 28(3): 450. CrossRef - Cardiac Autonomic Neuropathy in Prediabetes: A Case-Control Study
Pavan Gujjar, Y. S. Ravikumar, Lakshmi Nagendra, Hiya Boro, Saptarshi Bhattacharya
Indian Journal of Endocrinology and Metabolism.2023; 27(4): 325. CrossRef - Diabetic Neuropathies
Melissa A. Elafros, Brian C. Callaghan
CONTINUUM: Lifelong Learning in Neurology.2023; 29(5): 1401. CrossRef - Determinants of the heart rate variability in type 1 diabetes mellitus
Máté Hajdu, Konstandia Garmpis, Vivien Vértes, Noémi Vorobcsuk-Varga, Gergő Attila Molnár, László Hejjel, István Wittmann, Réka Faludi
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Effect of Exercise on Cardiovascular Autonomic Nervous Function in Patients with Diabetes: A Systematic Review
Hidetaka Hamasaki
Healthcare.2023; 11(19): 2668. CrossRef - Influence of Fibrinogen/Albumin Ratio and Fibrinogen/Pre-Albumin Ratio on Cardiac Autonomic Neuropathy in Type 2 Diabetes
Subei Zhao, Zheng Yang, Meng Yu, Linyu Xiang, Yuhuan Lv, Chunyan Tian, Rong Li
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3249. CrossRef - In Ischemic Heart Disease, Reduced Sensitivity to Pressure at the Sternum Accompanies Lower Mortality after Five Years: Evidence from a Randomized Controlled Trial
Søren Ballegaard, Jens Faber, Christian Selmer, Finn Gyntelberg, Svend Kreiner, Benny Karpatschof, Tobias Wirenfeldt Klausen, Åke Hjalmarson, Albert Gjedde
Journal of Clinical Medicine.2023; 12(24): 7585. CrossRef - Assessment of the relationship of systemic vascular dysfunction and cardiac autonomic neuropathy (CAN) with diabetic retinopathy
KJ Hari Prakash, Sucheta Parija, Manisha Kar
Journal of Family Medicine and Primary Care.2023; 12(12): 3236. CrossRef - Autonomic Neuropathy in Ambulatory Type 2 Diabetes Mellitus Patients: A Single-arm Prospective, Observational Study
Kaustav Saha, Shatavisa Mukherjee, Animesh Maiti, Santanu Kumar Tripathi
Journal of the Practice of Cardiovascular Sciences.2023; 9(3): 178. CrossRef - Insomnia and type 2 diabetes: how to help the patient. Modern view of a neurologist
E. S. Akarachkova, O. V. Kotova, V. L. Klimov, D. I. Lebedeva
FOCUS. Endocrinology.2023; 4(4): 12. CrossRef - Impaired Cardiovagal Activity as a Link Between Hyperglycemia and Arterial Stiffness in Adults With Type 2 Diabetes Mellitus Patients Among an Eastern Indian Population: A Cross-sectional Study
Nibedita Priyadarsini, Devineni Likhitha, Madumathy Ramachandran, Kishore Kumar Behera
Canadian Journal of Diabetes.2023;[Epub] CrossRef - Carvedilol improves heart rate variability indices, biomarkers but not cardiac nerve density in streptozotocin-induced T2DM model of diabetic cardiac autonomic neuropathy
Olawale Mathias Akinlade, Bamidele Owoyele, Olufemi Ayodele Soladoye
Journal of Basic and Clinical Physiology and Pharmacology.2022; 33(2): 213. CrossRef - Cardiovascular autonomic responses during head-up tilt test in newly diagnosed type 2 diabetes
Esteban Jorge-Galarza, Margarita Torres-Tamayo, María del Rocío Martínez-Alvarado, Berenice Peña-Aparicio, Carmen González-Salazar, Juan Reyes-Barrera, Manuel Sierra-Beltrán, Erika Fajardo-Flores, Andrey Kostin, J. Antonio González-Hermosillo
Irish Journal of Medical Science (1971 -).2022; 191(5): 2077. CrossRef - Cardiovascular autonomic neuropathy and incident diabetic kidney disease in patients with type 2 diabetes
Ji Eun Jun, Min Sun Choi, Jae Hyeon Kim
Diabetes Research and Clinical Practice.2022; 184: 109181. CrossRef - Kardiovaskuläre Risiken in der 4.–6. Lebensdekade mit Diabetes mellitus Typ 1
Young Hee Lee-Barkey, Bernd Stratmann, Diethelm Tschöpe
Der Diabetologe.2022; 18(2): 131. CrossRef - Mechanisms of cardiac dysfunction in diabetic cardiomyopathy: molecular abnormalities and phenotypical variants
Francesca Romana Prandi, Isabella Evangelista, Domenico Sergi, Alberto Palazzuoli, Francesco Romeo
Heart Failure Reviews.2022; 28(3): 597. CrossRef - Comparison of Risk Assessment Strategies for Patients with Diabetes Mellitus and Stable Chest Pain: A Coronary Computed Tomography Angiography Study
Jia Zhao, Shuo Wang, Pengyu Zhao, Yong Huo, Chunjie Li, Jia Zhou, Pawel Kleczynski
Journal of Diabetes Research.2022; 2022: 1. CrossRef - BOND study: a randomised double-blind, placebo-controlled trial over 12 months to assess the effects of benfotiamine on morphometric, neurophysiological and clinical measures in patients with type 2 diabetes with symptomatic polyneuropathy
Gidon J Bönhof, Gundega Sipola, Alexander Strom, Christian Herder, Klaus Strassburger, Birgit Knebel, Claudia Reule, Jan-Christoph Wollmann, Andrea Icks, Hadi Al-Hasani, Michael Roden, Oliver Kuss, Dan Ziegler
BMJ Open.2022; 12(2): e057142. CrossRef - Pragmatic Clinic-Based Investigation of Glycemic Variability in Patients With Type 1 Diabetes in Routine Clinical Practice and Its Association With Cardiovascular Autonomic Neuropathy: A Pilot Study
Lucianne R.M. Tannus, Marilia B. Gomes
Endocrine Practice.2022; 28(5): 465. CrossRef - Longitudinal effects of one‐leg standing time on neuropathy outcomes in association with glycemic control in non‐elderly patients with type 2 diabetes
Kazuhiro Sugimoto, Takashi Sozu, Takehiko Hoshino, Yuko Watanabe, Akira Tamura, Toshiro Yamazaki, Setsu Ohta, Susumu Suzuki, Takuro Shimbo
Journal of Diabetes Investigation.2022; 13(6): 1039. CrossRef - Thermal quantitative sensory testing as a screening tool for cardiac autonomic neuropathy in patients with diabetes mellitus
Veronika Potockova, Sarka Mala, Lucie Hoskovcova, Vaclav Capek, Tomas Nedelka, Lucie Riedlbauchova, Daniel Baumgartner, Livie Mensova, Radim Mazanec
Brain and Behavior.2022;[Epub] CrossRef - Cardiovascular Autonomic Reflex Tests and 7 Heart Rate Variability Indices for Early Diagnosis of Cardiovascular Autonomic Neuropathy in Type 2 Diabetes Individuals
Yeelen Ballesteros Atala, Mozânia Reis De Matos, Denise Engelbrecht Zantut-Wittmann, Alejandro Rosell Castillo, Daniele P Santos-Bezerra, Maria Lucia Correa-Giannella, Maria Cândida Ribeiro Parisi
Current Diabetes Reviews.2022;[Epub] CrossRef - Design, synthesis, in vitro and in silico studies of naproxen derivatives as dual lipoxygenase and α-glucosidase inhibitors
Asma Sardar, Obaid-ur-Rahman Abid, Saima Daud, M. Fakhar-e-Alam, Muhammad Hussnain Siddique, Muhammad Ashraf, Wardah Shahid, Syeda Abida Ejaz, M. Atif, Shafiq Ahmad, Sulman Shafeeq, Muhammad Afzal
Journal of Saudi Chemical Society.2022; 26(3): 101468. CrossRef - Clinical manifestations and evaluation of cardiac autonomic neuropathy in diabetes mellitus and metabolic syndrome
L. S. Moshkhoeva, A. N. Barinov
Neurology, Neuropsychiatry, Psychosomatics.2022; 14(2): 71. CrossRef - The relationship between vitamin B12 levels and electrocardiographic ventricular repolarization markers
Emre Yılmaz, Devrim Kurt, Aslı Vural, Ertan Aydın, Sencer Çamcı, Ercan Aydın
Nutrición Hospitalaria.2022;[Epub] CrossRef - The effect of liraglutide on cardiac autonomic function in type 2 diabetes: A prespecified secondary analysis from the LIRAFLAME randomized, double‐blinded, placebo‐controlled trial
Suvanjaa Sivalingam, Emilie Hein Zobel, Christian S. Hansen, Rasmus S. Ripa, Bernt J. von Scholten, Viktor Rotbain Curovic, Andreas Kjaer, Jacob K. Jensen, Tine W. Hansen, Peter Rossing
Diabetes, Obesity and Metabolism.2022; 24(8): 1638. CrossRef - Heart Rate Variability and Chronic Kidney Disease in Patients with Type 2 Diabetes
Wei Shi, Jing Zhang, Dan Chen, Xiaolei Chen, Wei Duan, Hongmei Zhang, Fahd Abd Algalil
Applied Bionics and Biomechanics.2022; 2022: 1. CrossRef - Spectrum of cardiac autonomic neuropathy in patients with type 2 diabetes mellitus: A North India perspective
PrativaPriyadarshani Sethi, Basavraj Jatteppanavar, Ravi Kant, Monika Pathania, MukeshChand Bairwa
Journal of Cardio-diabetes and metabolic disorders.2022; 2(1): 23. CrossRef - Cardiac Autonomic Dysfunction Is Associated With Risk of Diabetic Kidney Disease Progression in Type 2 Diabetes Mellitus
Haixia Zeng, Jianmo Liu, Zheng Chen, Peng Yu, Jianping Liu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Diagnostic Tools, Biomarkers, and Treatments in Diabetic polyneuropathy
and Cardiovascular Autonomic Neuropathy
Gidon J. Bönhof, Christian Herder, Dan Ziegler
Current Diabetes Reviews.2022;[Epub] CrossRef - Triglyceride glucose index is related with cardiac autonomic dysfunction in patients with metabolic syndrome
Akif Serhat Balcıoğlu, Ekrem Aksu, Ahmet Çağrı Aykan
Kardiologiia.2022; 62(6): 45. CrossRef - Pathogenesis of Distal Symmetrical Polyneuropathy in Diabetes
Sasha Smith, Pasha Normahani, Tristan Lane, David Hohenschurz-Schmidt, Nick Oliver, Alun Huw Davies
Life.2022; 12(7): 1074. CrossRef - Correlation between impaired hemodynamic response and cardiopulmonary fitness in middle-aged type 2 diabetes mellitus patients: a case–control study
Jinjin Xie, Lianhua Yin, Jia Huang, Ying Xu, Yannan Chen, Jiawei Qin, Zhizhen Liu, Jing Tao
European Journal of Applied Physiology.2022; 122(10): 2295. CrossRef - Higher frequency of cardiovascular autonomic neuropathy in youth with type 2 compared to type 1 diabetes: Role of cardiometabolic risk factors
Benjamin J. Varley, Megan L. Gow, Yoon Hi Cho, Paul Benitez‐Aguirre, Janine Cusumano, Alison Pryke, Albert Chan, Vallimayil Velayutham, Kim C. Donaghue, Maria E. Craig
Pediatric Diabetes.2022; 23(7): 1073. CrossRef - The role of protein kinase C in diabetic microvascular complications
Deng Pan, Lin Xu, Ming Guo
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effect of SGLT-2 inhibitors on cardiac autonomic function in type 2 diabetes mellitus: a meta-analysis of randomized controlled trials
Dimitrios Patoulias, Alexandra Katsimardou, Nikolaos Fragakis, Christodoulos Papadopoulos, Michael Doumas
Acta Diabetologica.2022; 60(1): 1. CrossRef - Association between blood glucose levels and autonomic symptoms in Peru
Gabriel Angeles-Zurita, Margorie Narro-Fuentes, Antonio Bernabe-Ortiz
Primary Care Diabetes.2022; 16(5): 709. CrossRef - Clinical scoring systems for the risk of cardiovascular autonomic neuropathy in type 1 and type 2 diabetes: A simple tool
Marika Menduni, Cinzia D'Amato, Martina Leoni, Valentina Izzo, Mariateresa Staltari, Carla Greco, Andrea Abbatepassero, Giuseppe Seminara, Ilenia D'Ippolito, Davide Lauro, Vincenza Spallone
Journal of the Peripheral Nervous System.2022; 27(4): 259. CrossRef - Vagus nerve stimulation as a novel treatment for systemic lupus erythematous: study protocol for a randomised, parallel-group, sham-controlled investigator-initiated clinical trial, the SLE-VNS study
Amanda Hempel Zinglersen, Ida Lynghøj Drange, Katrine Aagaard Myhr, Andreas Fuchs, Mogens Pfeiffer-Jensen, Christina Brock, Søren Jacobsen
BMJ Open.2022; 12(9): e064552. CrossRef - To the interpretation of frequency components of the heart rate variability
N. V. Kuzmenko, V. A. Tsyrlin, M. G. Pliss
Translational Medicine.2022; 9(3): 35. CrossRef - Protein pyrrole adducts are associated with elevated glucose indices and clinical features of diabetic diffuse neuropathies
Xiao Chen, Zhuyi Jiang, Lianjing Zhang, Wei Liu, Xiaohu Ren, Luling Nie, Desheng Wu, Zhiwei Guo, Weimin Liu, Xifei Yang, Yan Wu, Zhen Liang, Peter Spencer, Jianjun Liu
Journal of Diabetes.2022; 14(10): 646. CrossRef - Cardiac Autonomic Neuropathy in Type 1 and 2 Diabetes: Epidemiology, Pathophysiology, and Management
Scott Williams, Siddig Abdel Raheim, Muhammad Ilyas Khan, Umme Rubab, Prathap Kanagala, Sizheng Steven Zhao, Anne Marshall, Emily Brown, Uazman Alam
Clinical Therapeutics.2022; 44(10): 1394. CrossRef - Pathophysiological and clinical aspects of the circadian rhythm of arterial stiffness in diabetes mellitus: A minireview
Victoria A. Serhiyenko, Ludmila M. Serhiyenko, Volodymyr B. Sehin, Alexandr A. Serhiyenko
Endocrine Regulations.2022; 56(4): 284. CrossRef - Heart rate-corrected QT interval prolongation is associated with decreased heart rate variability in patients with type 2 diabetes
Seon-Ah Cha
Medicine.2022; 101(45): e31511. CrossRef - Effect of the Glucagon-Like Peptide-1 Receptor Agonists on Autonomic Function in Subjects with Diabetes: A Systematic Review and Meta-Analysis
Carla Greco, Daniele Santi, Giulia Brigante, Chiara Pacchioni, Manuela Simoni
Diabetes & Metabolism Journal.2022; 46(6): 901. CrossRef - Diabetes-Induced Cardiac Autonomic Neuropathy: Impact on Heart Function and Prognosis
Susumu Z. Sudo, Tadeu L. Montagnoli, Bruna de S. Rocha, Aimeé D. Santos, Mauro P. L. de Sá, Gisele Zapata-Sudo
Biomedicines.2022; 10(12): 3258. CrossRef - The Relationship Between Orthostatic Hypotension and Vitamin D Deficiency in Patients with Uncontrolled Type 2 Diabetes Mellitus
Ece YİĞİT, Ridvan SİVRİTEPE, Dilay KARABULUT, Umut KARABULUT
Online Türk Sağlık Bilimleri Dergisi.2022; 7(2): 313. CrossRef - A study of heart rate variability in diabetic mellitus patients
Srinivasa Jayachandra, Satyanath Reddy Kodidala
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 153. CrossRef - The prevalence of cardiac autonomic neuropathy in prediabetes: a systematic review
Aikaterini Eleftheriadou, Scott Williams, Sarah Nevitt, Emily Brown, Rebecca Roylance, John P. H. Wilding, Daniel J. Cuthbertson, Uazman Alam
Diabetologia.2021; 64(2): 288. CrossRef - Risk of cardiac autonomic neuropathy in latent autoimmune diabetes in adults is similar to type 1 diabetes and lower compared to type 2 diabetes: A cross‐sectional study
Ernesto Maddaloni, Chiara Moretti, Rossella Del Toro, Sara Sterpetti, Maria Vittoria Ievolella, Gabriele Arnesano, Rocky Strollo, Silvia Irina Briganti, Luca D'Onofrio, Paolo Pozzilli, Raffaella Buzzetti
Diabetic Medicine.2021;[Epub] CrossRef - Effects of lunar cycle on fasting plasma glucose, heart rate and blood pressure in type 2 diabetic patients
Sutanu Dutta Chowdhury, Subhasish Pramanik, Koena Bhattacharjee, Lakshmi Kanta Mondal
Chronobiology International.2021; 38(2): 270. CrossRef - Intensive Risk Factor Management and Cardiovascular Autonomic Neuropathy in Type 2 Diabetes: The ACCORD Trial
Yaling Tang, Hetal Shah, Carlos Roberto Bueno Junior, Xiuqin Sun, Joanna Mitri, Maria Sambataro, Luisa Sambado, Hertzel C. Gerstein, Vivian Fonseca, Alessandro Doria, Rodica Pop-Busui
Diabetes Care.2021; 44(1): 164. CrossRef - Decreased glomerular filtration rate and increased albuminuria for identification of cardiovascular autonomic neuropathy in subjects with and without diabetes
Ying-Chuen Lai, Hung-Yuan Li, Yi-Dier Jiang, Tien-Jyun Chang, Lee-Ming Chuang
Autonomic Neuroscience.2021; 230: 102757. CrossRef - Exposures influencing the developing central autonomic nervous system
Sarah D. Schlatterer, Adre J. du Plessis
Birth Defects Research.2021; 113(11): 845. CrossRef - Vitamin B12 Supplementation in Diabetic Neuropathy: A 1-Year, Randomized, Double-Blind, Placebo-Controlled Trial
Triantafyllos Didangelos, Eleni Karlafti, Evangelia Kotzakioulafi, Eleni Margariti, Parthena Giannoulaki, Georgios Batanis, Solomon Tesfaye, Kοnstantinos Kantartzis
Nutrients.2021; 13(2): 395. CrossRef - The Association Between Continuous Glucose Monitoring-Derived Metrics and Cardiovascular Autonomic Neuropathy in Outpatients with Type 2 Diabetes
Min Young Kim, Gyuri Kim, Ji Yun Park, Min Sun Choi, Ji Eun Jun, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2021; 23(6): 434. CrossRef - Insulin resistance is independently associated with cardiovascular autonomic neuropathy in type 2 diabetes
Yingshan Liu, Yu Peng, Jing Jin, Yanshan Chen, Chuna Chen, Zhenguo Chen, Haishan Huang, Lingling Xu
Journal of Diabetes Investigation.2021; 12(9): 1651. CrossRef - SGLT2 inhibitors and the autonomic nervous system in diabetes: A promising challenge to better understand multiple target improvement
Vincenza Spallone, Paul Valensi
Diabetes & Metabolism.2021; 47(4): 101224. CrossRef - Reduction of Pressure Pain Sensitivity as Novel Non-pharmacological Therapeutic Approach to Type 2 Diabetes: A Randomized Trial
Jens Faber, Ebbe Eldrup, Christian Selmer, Caroline Pichat, Sofie Korsgaard Hecquet, Torquil Watt, Svend Kreiner, Benny Karpatschof, Finn Gyntelberg, Søren Ballegaard, Albert Gjedde
Frontiers in Neuroscience.2021;[Epub] CrossRef - Relationship between cardiac autonomic neuropathy and cardio-metabolic risk profile in adults with type 1 diabetes
M. Serdarova, R. Dimova, N. Chakarova, G. Grozeva, A. Todorova, T. Tankova
Diabetes Research and Clinical Practice.2021; 174: 108721. CrossRef - Differences and Similarities in Neuropathy in Type 1 and 2 Diabetes: A Systematic Review
Mar Sempere-Bigorra, Iván Julián-Rochina, Omar Cauli
Journal of Personalized Medicine.2021; 11(3): 230. CrossRef - Assessment of Gastrointestinal Autonomic Dysfunction: Present and Future Perspectives
Ditte S. Kornum, Astrid J. Terkelsen, Davide Bertoli, Mette W. Klinge, Katrine L. Høyer, Huda H. A. Kufaishi, Per Borghammer, Asbjørn M. Drewes, Christina Brock, Klaus Krogh
Journal of Clinical Medicine.2021; 10(7): 1392. CrossRef - Diabetic heart disease: A clinical update
Jake Rajbhandari, Cornelius James Fernandez, Mayuri Agarwal, Beverly Xin Yi Yeap, Joseph M Pappachan
World Journal of Diabetes.2021; 12(4): 383. CrossRef - Novel and Emerging Electrophysiological Biomarkers of Diabetic Neuropathy and Painful Diabetic Neuropathy
Anne Marshall, Uazman Alam, Andreas Themistocleous, Nigel Calcutt, Andrew Marshall
Clinical Therapeutics.2021; 43(9): 1441. CrossRef - Cardiac Autonomic Neuropathy Is Not Reversed by Euglycemia Following Islet Transplantation
Tejas Deshmukh, Peter Emerson, Patricia Anderson, Eddy Kizana, Philip J. O’Connell, D. Jane Holmes-Walker, James J.H. Chong
Transplantation.2021; 105(5): 1125. CrossRef - Attenuation of Muscle Mass and Density Is Associated With Poor Outcomes Among Patients Undergoing Major Gynecologic Surgery: A Retrospective Cohort Study
Lu Che, Yan Zhang, Jiawen Yu, Li Xu, Yuguang Huang
Anesthesia & Analgesia.2021; 132(6): 1692. CrossRef - Association of Urinary N-Acetyl-β-D-Glucosaminidase with Cardiovascular Autonomic Neuropathy in Type 1 Diabetes Mellitus without Nephropathy
Min Sun Choi, Ji Eun Jun, Sung Woon Park, Jee Hee Yoo, Jiyeon Ahn, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Moon-Kyu Lee, Jae Hyeon Kim
Diabetes & Metabolism Journal.2021; 45(3): 349. CrossRef - Pathogenesis, diagnosis and clinical management of diabetic sensorimotor peripheral neuropathy
Gordon Sloan, Dinesh Selvarajah, Solomon Tesfaye
Nature Reviews Endocrinology.2021; 17(7): 400. CrossRef - Heart Rate Variability as a Potential Non-invasive Marker of Blood Glucose Level
L. R. Jarman, J. L. Elliott, T. Lees, R. Clifton-Bligh, A. M. Simpson, N. Nassif, S. Lal
Human Physiology.2021; 47(2): 209. CrossRef - Cardiovascular autonomic neuropathy in diabetes: Pathophysiology, clinical assessment and implications
Alice Duque, Mauro Felippe Felix Mediano, Andrea De Lorenzo, Luiz Fernando Rodrigues Jr
World Journal of Diabetes.2021; 12(6): 855. CrossRef - Gaussian process-based kernel as a diagnostic model for prediction of type 2 diabetes mellitus risk using non-linear heart rate variability features
R. Shashikant, Uttam Chaskar, Leena Phadke, Chetankumar Patil
Biomedical Engineering Letters.2021; 11(3): 273. CrossRef - Possible Preventative/Rehabilitative Role of Gliflozins in OSA and T2DM. A Systematic Literature Review-Based Hypothesis
Vincenzo Maria Monda, Francesca Porcellati, Felice Strollo, Alessandro Fucili, Marcello Monesi, Ersilia Satta, Sandro Gentile
Advances in Therapy.2021; 38(8): 4195. CrossRef - Characteristics of cardiovascular autonomic dysfunction and association with quality of life in patients with systemic lupus erythematosus
Amanda Hempel Zinglersen, Katrine Kjær Iversen, Henrik Christian Bidstrup Leffers, Esben Laugesen, Jesper Fleischer, Søren Jacobsen
Lupus Science & Medicine.2021; 8(1): e000507. CrossRef - Impaired vagal adaptation to an exercise task in women with gestational diabetes mellitus versus women with uncomplicated pregnancies
Marieta P. Theodorakopoulou, Areti Triantafyllou, Andreas Zafeiridis, Afroditi Κ. Boutou, Iris Grigoriadou, Evangelia Kintiraki, Stella Douma, Dimitrios G. Goulis, Konstantina Dipla
Hormones.2021; 20(4): 753. CrossRef - Cardioprotective Effects of Sodium-glucose Cotransporter 2 Inhibitors Regardless of Type 2 Diabetes Mellitus: A Meta-analysis
Lucas Silva Sousa, Felipe de Araújo Nascimento, Juliano Rocha, Michelle Rocha-Parise
International Journal of Cardiovascular Sciences.2021;[Epub] CrossRef - Management of diabetic neuropathy
Simona Cernea, Itamar Raz
Metabolism.2021; 123: 154867. CrossRef - Large fibre, small fibre and autonomic neuropathy in adolescents with type 1 diabetes: A systematic review
Vinni Faber Rasmussen, Troels Staehelin Jensen, Hatice Tankisi, Páll Karlsson, Esben Thyssen Vestergaard, Kurt Kristensen, Jens Randel Nyengaard, Astrid Juhl Terkelsen
Journal of Diabetes and its Complications.2021; 35(11): 108027. CrossRef - Cardiovascular Risk Management in Type 1 Diabetes
I. H. Teoh, P. Elisaus, J. D. Schofield
Current Diabetes Reports.2021;[Epub] CrossRef - Disturbances in the intraventricular conduction system in teenagers with type 1 diabetes. A pilot study
Agnieszka Zubkiewicz-Kucharska, Anna Noczyńska, Małgorzata Sobieszczańska, Małgorzata Poręba, Joanna Chrzanowska, Rafał Poręba, Monika Seifert, Anna Janocha, Krystyna Laszki-Szcząchor
Journal of Diabetes and its Complications.2021; 35(11): 108043. CrossRef - Peripheral and Autonomic Neuropathy Status of Young Patients With Type 1 Diabetes Mellitus at the Time of Transition From Pediatric Care to Adult-Oriented Diabetes Care
Anna Vágvölgyi, Ágnes Maróti, Mónika Szűcs, Csongor Póczik, Dóra Urbán-Pap, István Baczkó, Attila Nemes, Éva Csajbók, Krisztián Sepp, Péter Kempler, Andrea Orosz, Tamás Várkonyi, Csaba Lengyel
Frontiers in Endocrinology.2021;[Epub] CrossRef - Pancreatic exocrine insufficiency in diabetes is associated with autonomic dysfunction
Dag André Sangnes, Elisabeth Sandvik Bergmann, Rose Marie Moss, Trond Engjom, Eirik Søfteland
Scandinavian Journal of Gastroenterology.2021; 56(10): 1222. CrossRef - Dependence of Heart Rate Variability Indices on the Mean Heart Rate in Women with Well-Controlled Type 2 Diabetes
Adriana Robles-Cabrera, José M. Torres-Arellano, Ruben Fossion, Claudia Lerma
Journal of Clinical Medicine.2021; 10(19): 4386. CrossRef - Normative data on cardiovascular autonomic function in Greenlandic Inuit
Marie Mathilde Bjerg Christensen, Christian Stevns Hansen, Jesper Fleischer, Dorte Vistisen, Stine Byberg, Trine Larsen, Jens Christian Laursen, Marit Eika Jørgensen
BMJ Open Diabetes Research & Care.2021; 9(1): e002121. CrossRef - What Is in the Field for Genetics and Epigenetics of Diabetic Neuropathy: The Role of MicroRNAs
V. Spallone, C. Ciccacci, A. Latini, P. Borgiani, Karim Gariani
Journal of Diabetes Research.2021; 2021: 1. CrossRef - Evaluation and treatment of peripheral nervous system dysfunction in patients with prediabetes
O. E. Zinovyeva, T. M. Ostroumova, M. V. Koniashova, N. A. Gorbachev
Neurology, Neuropsychiatry, Psychosomatics.2021; 13(5): 116. CrossRef - Manifestazioni cliniche della neuropatia autonomica diabetica: valutazione dei sintomi
Carla Greco, Chiara Pacchioni, Manuela Simoni
L'Endocrinologo.2021; 22(6): 514. CrossRef - Perspectives of glycemic variability in diabetic neuropathy: a comprehensive review
Xiaochun Zhang, Xue Yang, Bao Sun, Chunsheng Zhu
Communications Biology.2021;[Epub] CrossRef - The Association Between Cardiovascular Autonomic Function and Changes in Kidney and Myocardial Function in Type 2 Diabetes and Healthy Controls
Jens Christian Laursen, Ida Kirstine B. Rasmussen, Emilie H. Zobel, Philip Hasbak, Bernt Johan von Scholten, Lene Holmvang, Rasmus S. Ripa, Christian S. Hansen, Marie Frimodt-Moeller, Andreas Kjaer, Peter Rossing, Tine W. Hansen
Frontiers in Endocrinology.2021;[Epub] CrossRef - Dependence of heart rate variability on indicators of type 1 diabetes mellitus control.
N. O. Pertseva, O. V. Gurzhiy, K. I. Moshenets
Medicni perspektivi (Medical perspectives).2020; 25(1): 88. CrossRef - Efficacy and safety of evogliptin treatment in patients with type 2 diabetes: A multicentre, active‐controlled, randomized, double‐blind study with open‐label extension (the EVERGREEN study)
Gyuri Kim, Soo Lim, Hyuk‐Sang Kwon, Ie B. Park, Kyu J. Ahn, Cheol‐Young Park, Su K. Kwon, Hye S. Kim, Seok W. Park, Sin G. Kim, Min K. Moon, Eun S. Kim, Choon H. Chung, Kang S. Park, Mikyung Kim, Dong J. Chung, Chang B. Lee, Tae H. Kim, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2020; 22(9): 1527. CrossRef - Diabetes mellitus and comorbidities: A bad romance
Niki Katsiki, Dimitrios Tousoulis
Hellenic Journal of Cardiology.2020; 61(1): 23. CrossRef - Features of the glucose influence on the heart activity and the changes in the potentials of the stomach and the intestines at the heart insufficiency conditions
V. V. Soltanov, L. M. Komarovskaya
Doklady of the National Academy of Sciences of Belarus.2020; 63(6): 736. CrossRef - Living Day to Day
Gerald Kayingo, Virginia McCoy Hass
Physician Assistant Clinics.2020; 5(2): 213. CrossRef - Source specific PM2.5 associated with heart rate variability in the elderly with coronary heart disease: A community-based panel study
Xi Chen, Bing Qiu, Qinpei Zou, Tian Qiu, Runkui Li, Ashley Truong, Yanmin Qi, Tao Liu, Limin Han, Tiebing Liu, Junrui Chang, Qi Sun, Ying Zhu, Dongqun Xu
Chemosphere.2020; 260: 127399. CrossRef - The Association of Autonomic Nervous System Function With Ischemic Stroke, and Treatment Strategies
Mengxi Zhao, Ling Guan, Yilong Wang
Frontiers in Neurology.2020;[Epub] CrossRef - Cardiac diabetic autonomic neuropathy
L. T. Akhmedzhanova, T. A. Belyakova, Yu. A. Podkovko, Yu. M. Shor
Medical Council.2020; (21): 94. CrossRef - Diabetes, and its treatment, as an effector of autonomic nervous system circuits and its functions
Liliana Espinoza, Carie R Boychuk
Current Opinion in Pharmacology.2020; 54: 18. CrossRef - Morning blood pressure surge is associated with autonomic neuropathy and peripheral vascular disease in patients with diabetes
Federica Di Gennaro, Cinzia D’Amato, Roberto Morganti, Carla Greco, Susanna Longo, Diana Corradini, Davide Lauro, Vincenza Spallone
Journal of Human Hypertension.2020; 34(7): 495. CrossRef - The Compound Expression of HSP90 and INOS in the Testis of Diabetic Rats as Cellular and Pathologic Adverse Effects of Diabetes
Ali Alsarhan, Kawther Faisal Amawi, Inas Saleh Al-Mazari, Hashem Abu Hurirah, Ahed J. Alkhatib
Analytical Cellular Pathology.2020; 2020: 1. CrossRef - Heart rate variability features from nonlinear cardiac dynamics in identification of diabetes using artificial neural network and support vector machine
Yogender Aggarwal, Joyani Das, Papiya Mitra Mazumder, Rohit Kumar, Rakesh Kumar Sinha
Biocybernetics and Biomedical Engineering.2020; 40(3): 1002. CrossRef - Distal Symmetric and Cardiovascular Autonomic Neuropathies in Brazilian Individuals with Type 2 Diabetes Followed in a Primary Health Care Unit: A Cross-Sectional Study
Mozania Reis de Matos, Daniele Pereira Santos-Bezerra, Cristiane das Graças Dias Cavalcante, Jacira Xavier de Carvalho, Juliana Leite, Jose Antonio Januario Neves, Sharon Nina Admoni, Marisa Passarelli, Maria Candida Parisi, Maria Lucia Correa-Giannella
International Journal of Environmental Research and Public Health.2020; 17(9): 3232. CrossRef - Awareness of hypoglycemia and spectral analysis of heart rate variability in type 1 diabetes
Ticiana Paes, L. Clemente Rolim, Celso Sallum Filho, João Roberto de Sa, Sérgio A. Dib
Journal of Diabetes and its Complications.2020; 34(8): 107617. CrossRef - Is there cardiac autonomic neuropathy in prediabetes?
Lindsay A. Zilliox, James W. Russell
Autonomic Neuroscience.2020; 229: 102722. CrossRef - Chronic Microvascular Complications in Prediabetic States—An Overview
Angelika Baranowska-Jurkun, Wojciech Matuszewski, Elżbieta Bandurska-Stankiewicz
Journal of Clinical Medicine.2020; 9(10): 3289. CrossRef - Cardiac vagal tone as a novel screening tool to recognize asymptomatic cardiovascular autonomic neuropathy: Aspects of utility in type 1 diabetes
Anne-Marie Wegeberg, Elin D Lunde, Sam Riahi, Niels Ejskjaer, Asbjørn M Drewes, Birgitte Brock, Rodica Pop-Busui, Christina Brock
Diabetes Research and Clinical Practice.2020; 170: 108517. CrossRef - Assessment of baroreceptor reflex sensitivity in young obese Saudi males at rest and in response to physiological challenges
Abdullah N. AlShahrani, Lubna I. Al‐Asoom, Ahmed A. Alsunni, Nabil S. Elbahai, Talay Yar
Physiological Reports.2020;[Epub] CrossRef - The relationship between QT interval indices with cardiac autonomic neuropathy in diabetic patients: a case control study
Maryam Vasheghani, Farzaneh Sarvghadi, Mohammad Reza Beyranvand, Habib Emami
Diabetology & Metabolic Syndrome.2020;[Epub] CrossRef - Myocardial ischaemia reperfusion injury and cardioprotection in the presence of sensory neuropathy: Therapeutic options
Péter Bencsik, Kamilla Gömöri, Tamara Szabados, Péter Sántha, Zsuzsanna Helyes, Gábor Jancsó, Péter Ferdinandy, Anikó Görbe
British Journal of Pharmacology.2020; 177(23): 5336. CrossRef - Biological Activity of c-Peptide in Microvascular Complications of Type 1 Diabetes—Time for Translational Studies or Back to the Basics?
Aleksandra Ryk, Aleksandra Łosiewicz, Arkadiusz Michalak, Wojciech Fendler
International Journal of Molecular Sciences.2020; 21(24): 9723. CrossRef - Diabetes and cardiovascular disease: inter-relation of risk factors and treatment
Aman Sharma, Shweta Mittal, Rohan Aggarwal, Meenakshi K. Chauhan
Future Journal of Pharmaceutical Sciences.2020;[Epub] CrossRef - Diabetic Autonomic Neuropathy: A Clinical Update
Jugal Kishor Sharma, Anshu Rohatgi, Dinesh Sharma
Journal of the Royal College of Physicians of Edinburgh.2020; 50(3): 269. CrossRef - Obesity, Metabolic Syndrome and the Risk of Microvascular Complications in Patients with Diabetes mellitus
Niki Katsiki, Panagiotis Anagnostis, Kalliopi Kotsa, Dimitrios G. Goulis, Dimitri P. Mikhailidis
Current Pharmaceutical Design.2019; 25(18): 2051. CrossRef - Cardiac Autonomic Neuropathy in Obesity, the Metabolic Syndrome and Prediabetes: A Narrative Review
Scott M. Williams, Aikaterini Eleftheriadou, Uazman Alam, Daniel J. Cuthbertson, John P. H. Wilding
Diabetes Therapy.2019; 10(6): 1995. CrossRef
- Rectal sensitivity correlated with gastrointestinal‐mediated glucose disposal, but not the incretin effect
- Hyperglycemia as a Risk Factor for Cancer Progression
- Tae Young Ryu, Jiyoung Park, Philipp E. Scherer
- Diabetes Metab J. 2014;38(5):330-336. Published online October 17, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.5.330
- 7,215 View
- 104 Download
- 195 Web of Science
- 193 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader As the prevalence of diabetes mellitus is substantially increasing worldwide, associated diseases such as renal failure, cardiovascular diseases, fatty liver, and cancers have also increased. A number of cancers such as pancreatic, liver, breast, and female reproductive cancers have shown an increased prevalence and a higher mortality rate in diabetic patients compared to healthy subjects. Thus, this suggests an association between diabetes, especially type 2 diabetes and cancer incidence and progression. Recent studies have suggested that hyperinsulinemia, chronic inflammation and hyperglycemia, all frequently seen in diabetics, may lead to increased tumor growth; the underlying molecular mechanisms of this association are not fully understood. In particular, chronic hyperglycemic episodes could serve as a direct or indirect mediator of the increase in tumor cell growth. Here, we will discuss our current understanding how hyperglycemia and cancer risk may be linked, and what the implications are for the treatment of diabetic cancer patients.
-
Citations
Citations to this article as recorded by- Enhanced degradation of epidermal growth factor receptor by metformin
Mayuka Yamagata, Sen Higashi, Noboru Yaida, Akane Ichihara, Manabu Habu, Masaaki Sasaguri, Kazuhiro Tominaga, Hiroshi Takeuchi
Oral Science International.2024; 21(1): 59. CrossRef - Development and Validation of a Fluorogenic Probe for Lysosomal Zinc Release
Adarash Kumar Shukla, Ashutosh Mahale, Savita Choudhary, Pravesh Sharma, Onkar Prakash Kulkarni, Anupam Bhattacharya
ChemBioChem.2024;[Epub] CrossRef - Type 2 diabetes, glycaemic traits and upper gastrointestinal cancer risk: a prospective cohort study
Luyao Cao, Tianpei Wang, Huizhang Li, Fadoua El Hafa, Xia Zhu, Yuhui Yu, Caiwang Yan, Lingbin Du, Meng Zhu, Guangfu Jin
Journal of Epidemiology and Community Health.2024; 78(3): 145. CrossRef - Extrahepatic malignancies in metabolic dysfunction‐associated fatty liver disease: A nationwide cohort study
Min Kyung Park, Moon Haeng Hur, Hye‐Sung Moon, Hyunjae Shin, Sung Won Chung, Sungho Won, Yun Bin Lee, Eun Ju Cho, Jeong‐Hoon Lee, Su Jong Yu, Jung‐Hwan Yoon, Yoon Jun Kim
Liver International.2024; 44(3): 799. CrossRef - Effects of the Mediterranean Diet on metabolic indices and quality of life in cancer patients: A systematic review and meta-analysis of randomized controlled trials
Shuai Lu, Xibo Sun, Weihao Zhang, Xiangqi Li, Zhongbao Zhou, Ruixue Xiao, Qingchen Lv, Huazhen Tang, Bing Wang, Jinxiu Qu, Rui Cao, Jia He, Shiwan Wang, Penghui Yang, Zhenpeng Yang, Benqiang Rao
Journal of Functional Foods.2024; 114: 106074. CrossRef - M1-derived extracellular vesicles polarize recipient macrophages into M2-like macrophages and alter skeletal muscle homeostasis in a hyper-glucose environment
Stefano Tacconi, Francesco Vari, Carolina Sbarigia, Diana Vardanyan, Serena Longo, Francesco Mura, Federica Angilè, Audrey Jalabert, Ferninand Blangero, Assia Eljaafari, Laurence Canaple, Daniele Vergara, Francesco Paolo Fanizzi, Marco Rossi, Claire Crola
Cell Communication and Signaling.2024;[Epub] CrossRef - The complex landscape of intracellular signalling in protein modification under hyperglycaemic stress leading to metabolic disorders
Hamda Khan, Afreen Khanam, Adnan Ahmad Khan, Rizwan Ahmad, Arbab Husain, Safia Habib, Saheem Ahmad, Moinuddin
The Protein Journal.2024;[Epub] CrossRef - Nuclear translocation of metabolic enzyme PKM2 participates in high glucose-promoted HCC metastasis by strengthening immunosuppressive environment
Jiali Qian, Chuxin Huang, Mimi Wang, Ying Liu, Yingying Zhao, Miao Li, Xi Zhang, Xiangyu Gao, Yawen Zhang, Yi Wang, Jinya Huang, Jiajun Li, Qiwen Zhou, Rui Liu, Xuanchun Wang, Jiefeng Cui, Yehong Yang
Redox Biology.2024; 71: 103103. CrossRef - Macrophages, IL-10, and nitric oxide increase, induced by hyperglycemic conditions, impact the development of murine melanoma B16F10-Nex2
Tarciso A. Sellani, Samanta L. Tomaz, Jéssica M. Gonçalves, Adriana Lima, Carolina C. de Amat Herbozo, Gabrielli N. Silva, Mônica Gambero, Ieda M. Longo-Maugéri, Karin A. Simon, Hugo P. Monteiro, Elaine G. Rodrigues
Nitric Oxide.2024; 148: 1. CrossRef - Designing of potent anti-diabetic molecules by targeting SIK2 using computational approaches
Prajisha Jayaprakash, Jayashree Biswal, Raghu Rangaswamy, Jeyaraman Jeyakanthan
Molecular Diversity.2023; 27(3): 1101. CrossRef - Asprosin in health and disease, a new glucose sensor with central and peripheral metabolic effects
Mariam Farrag, Djedjiga Ait Eldjoudi, María González-Rodríguez, Alfonso Cordero-Barreal, Clara Ruiz-Fernández, Maurizio Capuozzo, Miguel Angel González-Gay, Antonio Mera, Francisca Lago, Ahmed Soffar, Amina Essawy, Jesus Pino, Yousof Farrag, Oreste Gualil
Frontiers in Endocrinology.2023;[Epub] CrossRef - HIPK2 as a Novel Regulator of Fibrosis
Alessia Garufi, Giuseppa Pistritto, Gabriella D’Orazi
Cancers.2023; 15(4): 1059. CrossRef - Cancer—A Pragmatic Switch to Combat Metabolic Syndrome?
John Claras
Oncology Reviews.2023;[Epub] CrossRef - Could Vaspin Be a Potential Diagnostic Marker in Endometrial Cancer?
Dominika Pietrzyk, Piotr Tkacz, Mateusz Kozłowski, Sebastian Kwiatkowski, Małgorzata Rychlicka, Ewa Pius-Sadowska, Bogusław Machaliński, Aneta Cymbaluk-Płoska
International Journal of Environmental Research and Public Health.2023; 20(6): 4999. CrossRef - Diabetes and Cancer
Jae Won Hong
The Journal of Korean Diabetes.2023; 24(1): 12. CrossRef - The Sweet Side of HIPK2
Alessia Garufi, Valerio D’Orazi, Giuseppa Pistritto, Mara Cirone, Gabriella D’Orazi
Cancers.2023; 15(10): 2678. CrossRef - Glucose-induced CRL4COP1-p53 axis amplifies glycometabolism to drive tumorigenesis
Yang Su, Yifan Luo, Peitao Zhang, Hong Lin, Weijie Pu, Hongyun Zhang, Huifang Wang, Yi Hao, Yihang Xiao, Xiaozhe Zhang, Xiayun Wei, Siyue Nie, Keren Zhang, Qiuyu Fu, Hao Chen, Niu Huang, Yan Ren, Mingxuan Wu, Billy Kwok Chong Chow, Xing Chen, Wenfei Jin,
Molecular Cell.2023; 83(13): 2316. CrossRef - SGLT2 Inhibitors as Potential Anticancer Agents
Debasish Basak, David Gamez, Subrata Deb
Biomedicines.2023; 11(7): 1867. CrossRef - Diabetes mellitus and cancer
Jae Won Hong
Cardiovascular Prevention and Pharmacotherapy.2023; 5(3): 69. CrossRef - Risk Factors of Renal Cell Carcinoma
云治 秦
Medical Diagnosis.2023; 13(03): 335. CrossRef - The Role of Meteorin-Like Peptide and Asprosin in Colon Carcinoma
Elif Onat, Nevin Kocaman, Hilal Balta
Cureus.2023;[Epub] CrossRef - Diabetes-associated breast cancer is molecularly distinct and shows a DNA damage repair deficiency
Gatikrushna Panigrahi, Julián Candia, Tiffany H. Dorsey, Wei Tang, Yuuki Ohara, Jung S. Byun, Tsion Zewdu Minas, Amy Zhang, Anuoluwapo Ajao, Ashley Cellini, Harris G. Yfantis, Amy L. Flis, Dean Mann, Olga Ioffe, Xin W. Wang, Huaitian Liu, Christopher A. L
JCI Insight.2023;[Epub] CrossRef - The classification of obesity based on metabolic status redefines the readmission of non-Hodgkin’s lymphoma—an observational study
Hang Dong, Honglin Guo, Jing Du, Yiping Cheng, Dawei Wang, Junming Han, Zinuo Yuan, Zhenyu Yao, Ran An, Xiaoqin Wu, Kyle L. Poulsen, Zhixiang Wang, Shanshan Shao, Xiude Fan, Zhen Wang, Jiajun Zhao
Cancer & Metabolism.2023;[Epub] CrossRef - Dose‐dependent effects of aerobic exercise on clinically relevant biomarkers among healthy women at high genetic risk for breast cancer: A secondary analysis of a randomized controlled study
Christopher J. Ehret, Shouhao Zhou, Julia C. Tchou, Kathryn H. Schmitz, Kathleen M. Sturgeon
Cancer Reports.2022;[Epub] CrossRef - Do diabetic complications influence cancer-related events in people with type 2 diabetes? A cohort approach
Evelyne Liuu, Pierre-Jean Saulnier, Elise Gand, Gautier Defossez, Amélie Jamet, Stéphanie Ragot, Marc Paccalin, Samy Hadjadj
Diabetes & Metabolism.2022; 48(2): 101289. CrossRef - Unraveling the Role of STK11/LKB1 in Non-small Cell Lung Cancer
Vikram Sumbly, Ian Landry
Cureus.2022;[Epub] CrossRef - Impact of Diabetes Mellitus and Its Comorbidities on Elderly Patients Hospitalized in Internal Medicine Wards: Data from the RePoSi Registry
Christiano Argano, Giuseppe Natoli, Salvatore Mularo, Alessandro Nobili, Marika Lo Monaco, Pier Mannuccio Mannucci, Francesco Perticone, Antonello Pietrangelo, Salvatore Corrao
Healthcare.2022; 10(1): 86. CrossRef - Type 2 Diabetes and Risk of Early-Onset Colorectal Cancer
Zitong Li, Hanyu Chen, Cassandra D.L. Fritz, Xiaobin Zheng, Xiaoyu Zong, Katelin B. Nickel, Andrew Tipping, Long H. Nguyen, Andrew T. Chan, Edward L. Giovannucci, Graham A. Colditz, Margaret A. Olsen, Peter T. Campbell, Nicholas O. Davidson, Ryan C. Field
Gastro Hep Advances.2022; 1(2): 186. CrossRef - Metformin Downregulates the Expression of Epidermal Growth Factor Receptor Independent of Lowering Blood Glucose in Oral Squamous Cell Carcinoma
Wei-Ming Wang, Si-Si Yang, Shu-Hui Shao, Huan-Quan Nie, Jing Zhang, Tong Su
Frontiers in Endocrinology.2022;[Epub] CrossRef - Exploring the Impact of the Obesity Paradox on Lung Cancer and Other Malignancies
Lindsay Joyce Nitsche, Sarbajit Mukherjee, Kareena Cheruvu, Cathleen Krabak, Rohit Rachala, Kalyan Ratnakaram, Priyanka Sharma, Maddy Singh, Sai Yendamuri
Cancers.2022; 14(6): 1440. CrossRef - Modern lifestyle, stress and metabolism: possible risk factors for oral carcinogenesis in the young generation
Monal Yuwanati, Sachin C Sarode, Amol Gadbail, Shailesh Gondivkar, Gargi Sarode
Future Oncology.2022; 18(15): 1801. CrossRef - Effects of In Vitro Digestion on Anti-α-Amylase and Cytotoxic Potentials of Sargassum spp.
Sovannary Un, Nguyen Van Quan, La Hoang Anh, Vu Quang Lam, Akiyoshi Takami, Tran Dang Khanh, Tran Dang Xuan
Molecules.2022; 27(7): 2307. CrossRef - Consumption of “Diabetes Risk Reduction Diet” and Odds of Breast Cancer Among Women in a Middle Eastern Country
Sara Ebrahimi Mousavi, Amir Bagheri, Sanaz Benisi-Kohansal, Leila Azadbakht, Ahmad Esmaillzadeh
Frontiers in Nutrition.2022;[Epub] CrossRef - Fasting Insulin and Risk of Overall and 14 Site-Specific Cancers: Evidence From Genetic Data
Han Zhang, Doudou Li, Xiaozhuan Liu, Zhongxiao Wan, Zengli Yu, Yuming Wang, Xue Li
Frontiers in Oncology.2022;[Epub] CrossRef - A Nutritional Metabolism Related Prognostic Scoring System for Patients With Newly Diagnosed Osteosarcoma
Longqing Li, Zhuangzhuang Li, Xuanhong He, Yang Wang, Minxun Lu, Taojun Gong, Qing Chang, Jingqi Lin, Yi Luo, Li Min, Yong Zhou, Chongqi Tu
Frontiers in Nutrition.2022;[Epub] CrossRef - Review of Mendelian Randomization Studies on Endometrial Cancer
Jian-Zeng Guo, Qi-Jun Wu, Fang-Hua Liu, Chang Gao, Ting-Ting Gong, Gang Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - PROBLEMS AND EDUCATIONAL NEEDS RELATED TO PORT CATHETER IN CANCER PATIENTS
Mehmet Zeki AVCI, Sevda ŞAHİN, Betülay KILIÇ, Hatice SUTCU CICEK
İnönü Üniversitesi Sağlık Hizmetleri Meslek Yüksek Okulu Dergisi.2022; 10(3): 849. CrossRef - Association of Physical Activity and Sedentary Behavior With the Risk of Colorectal Cancer
Sanghyun An, Sungjin Park
Journal of Korean Medical Science.2022;[Epub] CrossRef - Sleep Disruption and Cancer: Chicken or the Egg?
Adrian Berisha, Kyle Shutkind, Jeremy C. Borniger
Frontiers in Neuroscience.2022;[Epub] CrossRef - Role of anti-angiogenic factors in the pathogenesis of breast cancer: A review of therapeutic potential
Liwei Ruan, Songou Zhang, Xiaozhen Chen, Wenqing Liang, Qiong Xie
Pathology - Research and Practice.2022; 236: 153956. CrossRef - Cancer-cell-secreted extracellular vesicles suppress insulin secretion through miR-122 to impair systemic glucose homeostasis and contribute to tumour growth
Minghui Cao, Roi Isaac, Wei Yan, Xianhui Ruan, Li Jiang, Yuhao Wan, Jessica Wang, Emily Wang, Christine Caron, Steven Neben, Denis Drygin, Donald P. Pizzo, Xiwei Wu, Xuxiang Liu, Andrew R. Chin, Miranda Y. Fong, Ziting Gao, Kaizhu Guo, Oluwole Fadare, Ric
Nature Cell Biology.2022; 24(6): 954. CrossRef - Association between haemoglobin A1c and all-cause and cause-specific mortality in middle-aged and older Koreans: a prospective cohort study
Bo Mi Song, Jung Hyun Lee, Hae Dong Woo, Mi Jin Cho, Sung Soo Kim
Nutrition & Metabolism.2022;[Epub] CrossRef - Antidiabetic and antiradical effects of Garcinia kola seeds in dexamethasone-induced hyperglycemic rats
BarnabéLucien Nkono Ya Nkono, Ablassé Rouamba, McJesus Kinyok, JeanGuy Stéphane, BalthazarTchouanka Tcheudi, BenjaminArnaud Tigui, PaulD Djomeni Dzeufiet, SélestinDongmo Sokeng, Pierre Kamtchouing
International Journal of Applied and Basic Medical Research.2022; 12(3): 203. CrossRef - The “Diabetes Comorbidome”: A Different Way for Health Professionals to Approach the Comorbidity Burden of Diabetes
Salvatore Corrao, Giuseppe Natoli, Alessandro Nobili, Pier Mannucci, Francesco Perticone, Vincenzo Arcoraci, Christiano Argano
Healthcare.2022; 10(8): 1459. CrossRef - New insights into the prognosis of intraocular malignancy: Interventions for association mechanisms between cancer and diabetes
Lingwen Gu, Guofeng Ma, Cui Li, Jing Lin, Guiqiu Zhao
Frontiers in Oncology.2022;[Epub] CrossRef - Glucose deprivation reduces proliferation and motility, and enhances the anti-proliferative effects of paclitaxel and doxorubicin in breast cell lines in vitro
Maitham A. Khajah, Sarah Khushaish, Yunus A. Luqmani, Yi-Hsien Hsieh
PLOS ONE.2022; 17(8): e0272449. CrossRef - Chronic hyperglycemia based on diabetes is independently associated with decreased survival in patients with advanced cancer treated with immune checkpoint inhibitors
Emre Yekedüz, Elif Berna Köksoy, Sati Coşkun Yazgan, Göktürk Karataş, Filiz Çay Şenler, Güngör Utkan, Hakan Akbulut, Ahmet Demirkazik, Yüksel Ürün
Anti-Cancer Drugs.2022; 33(10): 1145. CrossRef - HIF-1α Expression Increases Preoperative Concurrent Chemoradiotherapy Resistance in Hyperglycemic Rectal Cancer
Yi-Jung Huang, Yi-Ting Chen, Chun-Ming Huang, Shih-Hsun Kuo, Yan-You Liao, Wun-Ya Jhang, Shuo-Hung Wang, Chien-Chih Ke, Yu-Hsiang Huang, Chiu-Min Cheng, Ming-Yii Huang, Chih-Hung Chuang
Cancers.2022; 14(16): 4053. CrossRef - Multifaceted entrancing role of glucose and its analogue, 2-deoxy-D-glucose in cancer cell proliferation, inflammation, and virus infection
Sananda Dey, Nensina Murmu, Tanushree Mondal, Ishita Saha, Soumendranath Chatterjee, Rahul Manna, Subhash Haldar, Sandeep K. Dash, Tapasree Roy Sarkar, Biplab Giri
Biomedicine & Pharmacotherapy.2022; 156: 113801. CrossRef - Evaluation of Tissue Expression of Vaspin and Serum Vaspin Concentration as a Prognostic and Risk Factor in Endometrial Cancer
Mateusz Kozłowski, Dominika Pietrzyk, Małgorzata Rychlicka, Katarzyna Piotrowska, Katarzyna Nowak, Sebastian Kwiatkowski, Aneta Cymbaluk-Płoska
Cells.2022; 11(20): 3196. CrossRef - Exploring the role of neutrophil-to-lymphocyte ratio and blood chemistry in head and neck adenoid cystic carcinomas treated with carbon ion radiotherapy
Amelia Barcellini, Giulia Fontana, Daria Maria Filippini, Sara Ronchi, Maria Bonora, Barbara Vischioni, Rossana Ingargiola, Anna Maria Camarda, Pierre Loap, Nadia Facchinetti, Lisa Licitra, Guido Baroni, Ester Orlandi
Radiotherapy and Oncology.2022; 177: 143. CrossRef - Diabetic hyperglycemia promotes primary tumor progression through glycation-induced tumor extracellular matrix stiffening
Wenjun Wang, Lauren A. Hapach, Lauren Griggs, Kyra Smart, Yusheng Wu, Paul V. Taufalele, Matthew M. Rowe, Katherine M. Young, Madison E. Bates, Andrew C. Johnson, Nicholas J. Ferrell, Ambra Pozzi, Cynthia A. Reinhart-King
Science Advances.2022;[Epub] CrossRef - The Relationship between Type 2 Diabetes Mellitus with the Occurrence and Progression of Prostate Cancer
树森 贾
Advances in Clinical Medicine.2022; 12(11): 10748. CrossRef - Palliative urinary diversion in patients with malignant ureteric obstruction due to gynaecological cancer
Tamar Perri, Elad Meller, Gilad Ben-Baruch, Yael Inbar, Sara Apter, Lee Heyman, Zohar Dotan, Jacob Korach
BMJ Supportive & Palliative Care.2022; 12(e6): e855. CrossRef - Onkodiabetológia I.
Róbert János Bánhegyi, Andrea Gazdag, Beatrix Rácz, Szilvia Beke, Norbert Fülöp
Orvosi Hetilap.2022; 163(39): 1535. CrossRef - AGE-RAGE synergy influences programmed cell death signaling to promote cancer
Bhargav N. Waghela, Foram U. Vaidya, Kishu Ranjan, Abu Sufiyan Chhipa, Budhi Sagar Tiwari, Chandramani Pathak
Molecular and Cellular Biochemistry.2021; 476(2): 585. CrossRef - Diabetes mellitus and oral cancer/oral potentially malignant disorders: A systematic review and meta‐analysis
Pablo Ramos‐Garcia, Maria del Mar Roca‐Rodriguez, Manuel Aguilar‐Diosdado, Miguel Angel Gonzalez‐Moles
Oral Diseases.2021; 27(3): 404. CrossRef - High pre-operative fasting blood glucose levels predict a poor prognosis in patients with pancreatic neuroendocrine tumour
Yitao Gong, Zhiyao Fan, Pin Zhang, Yunzhen Qian, Qiuyi Huang, Shengming Deng, Guopei Luo, He Cheng, Kaizhou Jin, Quanxing Ni, Xianjun Yu, Chen Liu
Endocrine.2021; 71(2): 494. CrossRef - Thrombospondin‐4 mediates hyperglycemia‐ and TGF‐beta‐induced inflammation in breast cancer
Santoshi Muppala, Roy Xiao, Jasmine Gajeton, Irene Krukovets, Dmitriy Verbovetskiy, Olga Stenina‐Adognravi
International Journal of Cancer.2021; 148(8): 2010. CrossRef - The predictive power of CD3+ T cell infiltration of oral squamous cell tumors is limited to non-diabetic patients
Gerrit Spanier, Ines Ugele, Felix Nieberle, Luisa Symeou, Sandra Schmidhofer, Almut Brand, Johannes Meier, Steffen Spoerl, Rosemarie Krupar, Petra Rümmele, Peter Siska, Kathrin Renner, Katrin Peter, Michael Gerken, Philipp Beckhove, Torsten E. Reichert, M
Cancer Letters.2021; 499: 209. CrossRef - Contribution of RAGE axis activation to the association between metabolic syndrome and cancer
Ma. Eugenia Garay-Sevilla, Armando Gomez-Ojeda, Ileana González, Claudia Luévano-Contreras, Armando Rojas
Molecular and Cellular Biochemistry.2021; 476(3): 1555. CrossRef - PKC Regulates YAP Expression through Alternative Splicing of YAP 3′UTR Pre-mRNA by hnRNP F
Wing-Keung Chu, Li-Man Hung, Chun-Wei Hou, Jan-Kan Chen
International Journal of Molecular Sciences.2021; 22(2): 694. CrossRef - The Taming of Nuclear Factor Erythroid-2-Related Factor-2 (Nrf2) Deglycation by Fructosamine-3-Kinase (FN3K)-Inhibitors-A Novel Strategy to Combat Cancers
Narasimha M. Beeraka, Venugopal R. Bovilla, Shalini H. Doreswamy, Sujatha Puttalingaiah, Asha Srinivasan, SubbaRao V. Madhunapantula
Cancers.2021; 13(2): 281. CrossRef - Body Habitus Across the Lifespan and Risk of Pituitary Adenoma
David J Cote, Timothy R Smith, Ursula B Kaiser, Edward R Laws, Meir J Stampfer
The Journal of Clinical Endocrinology & Metabolism.2021; 106(4): 1591. CrossRef - Dairy Consumption and Incidence of Breast Cancer in the ‘Seguimiento Universidad de Navarra’ (SUN) Project
Inmaculada Aguilera-Buenosvinos, Cesar Ignacio Fernandez-Lazaro, Andrea Romanos-Nanclares, Alfredo Gea, Rodrigo Sánchez-Bayona, Jose M. Martín-Moreno, Miguel Ángel Martínez-González, Estefanía Toledo
Nutrients.2021; 13(2): 687. CrossRef - Hyperglycemia-Induced miR-467 Drives Tumor Inflammation and Growth in Breast Cancer
Jasmine Gajeton, Irene Krukovets, Santoshi Muppala, Dmitriy Verbovetskiy, Jessica Zhang, Olga Stenina-Adognravi
Cancers.2021; 13(6): 1346. CrossRef - Prevalent diabetes and risk of total, colorectal, prostate and breast cancers in an ageing population: meta-analysis of individual participant data from cohorts of the CHANCES consortium
Amina Amadou, Heinz Freisling, Mazda Jenab, Konstantinos K. Tsilidis, Antonia Trichopoulou, Paolo Boffetta, Bethany Van Guelpen, Olatz Mokoroa, Tom Wilsgaard, Frank Kee, Ben Schöttker, José M. Ordóñez-Mena, Satu Männistö, Stefan Söderberg, Roel C. H. Verm
British Journal of Cancer.2021; 124(11): 1882. CrossRef - Preexisting Type 2 Diabetes and Survival among Patients with Colorectal Cancer
Chen Yuan, Xuehong Zhang, Ana Babic, Vicente Morales-Oyarvide, Yin Zhang, Stephanie A. Smith-Warner, Kana Wu, Molin Wang, Brian M. Wolpin, Jeffrey A. Meyerhardt, Andrew T. Chan, Frank B. Hu, Charles S. Fuchs, Shuji Ogino, Edward L. Giovannucci, Kimmie Ng
Cancer Epidemiology, Biomarkers & Prevention.2021; 30(4): 757. CrossRef - Food anticipatory hormonal responses: A systematic review of animal and human studies
Aleksandrina Skvortsova, Dieuwke S. Veldhuijzen, Iris E.M. Kloosterman, Gustavo Pacheco-López, Andrea W.M. Evers
Neuroscience & Biobehavioral Reviews.2021; 126: 447. CrossRef - Gut Microbiota and Gynecological Cancers: A Summary of Pathogenetic Mechanisms and Future Directions
Fulvio Borella, Andrea Roberto Carosso, Stefano Cosma, Mario Preti, Giammarco Collemi, Paola Cassoni, Luca Bertero, Chiara Benedetto
ACS Infectious Diseases.2021; 7(5): 987. CrossRef - Diabetes and Cancer: Metabolic Association, Therapeutic Challenges, and the Role of Natural Products
Wamidh H. Talib, Asma Ismail Mahmod, Sara Feras. Abuarab, Eliza Hasen, Amer A. Munaim, Shatha Khaled Haif, Amani Marwan Ayyash, Samar Khater, Intisar Hadi AL-Yasari, Lina T. Al Kury
Molecules.2021; 26(8): 2179. CrossRef - Diabetes increases the risk of meningioma: A systematic review and meta-analysis of observational studies
Dongjie Shi, Lei Ao, Hua Yu, Juan Li, Yongzhi Xia, Xuedong Wu, Dahai He, Wenjie Zhong, Haijian Xia
Cancer Epidemiology.2021; 73: 101946. CrossRef - High glucose: an emerging association between diabetes mellitus and cancer progression
Suangson Supabphol, Wunchana Seubwai, Sopit Wongkham, Charupong Saengboonmee
Journal of Molecular Medicine.2021; 99(9): 1175. CrossRef - Normalizing glucose levels reconfigures the mammary tumor immune and metabolic microenvironment and decreases metastatic seeding
Heba Allah M. Alsheikh, Brandon J. Metge, Chae‐Myeong Ha, Dominique C. Hinshaw, Mateus S.V. Mota, Sarah C. Kammerud, Tshering Lama-Sherpa, Noha Sharafeldin, Adam R. Wende, Rajeev S. Samant, Lalita A. Shevde
Cancer Letters.2021; 517: 24. CrossRef - The prognostic outcome of ‘type 2 diabetes mellitus and breast cancer’ association pivots on hypoxia-hyperglycemia axis
Ilhaam Ayaz Durrani, Attya Bhatti, Peter John
Cancer Cell International.2021;[Epub] CrossRef - Insulin-like Growth Factor 2 mRNA-Binding Protein 2—a Potential Link Between Type 2 Diabetes Mellitus and Cancer
Junguo Cao, Weijia Yan, Xiujian Ma, Haiyan Huang, Hong Yan
The Journal of Clinical Endocrinology & Metabolism.2021; 106(10): 2807. CrossRef - Fatty acid synthase mediates high glucose‐induced EGFR activation in oral dysplastic keratinocytes
David J. Wisniewski, Tao Ma, Abraham Schneider
Journal of Oral Pathology & Medicine.2021; 50(9): 919. CrossRef - Moringa Oleifera Seed Extract Concomitantly Supplemented with Chemotherapy Worsens Tumor Progression in Mice with Triple Negative Breast Cancer and Obesity
Elizabeth R. M. Zunica, Shengping Yang, Ann Coulter, Christy White, John P. Kirwan, Linda A. Gilmore
Nutrients.2021; 13(9): 2923. CrossRef - Investigation of Causal Effect of Type 2 Diabetes Mellitus on Lung Cancer: A Mendelian Randomization Study
Tongtong Hong, Na Qin, Xiaoyu Zhao, Cheng Wang, Yue Jiang, Hongxia Ma, Juncheng Dai
Frontiers in Genetics.2021;[Epub] CrossRef - Glucose Intolerance and Cancer Risk: A Community-Based Prospective Cohort Study in Shanghai, China
Juzhong Ke, Tao Lin, Xiaolin Liu, Kang Wu, Xiaonan Ruan, Yibo Ding, Wenbin Liu, Hua Qiu, Xiaojie Tan, Xiaonan Wang, Xi Chen, Zhitao Li, Guangwen Cao
Frontiers in Oncology.2021;[Epub] CrossRef - Hyperglycemic conditions proliferate triple negative breast cancer cells: role of ornithine decarboxylase
Caleb C. Capellen, Jose Ortega-Rodas, M. Jane Morwitzer, Hadassha M. N. Tofilau, Matthew Dunworth, Robert A. Casero, Surabhi Chandra
Breast Cancer Research and Treatment.2021; 190(2): 255. CrossRef - Diabetes Mellitus and Obesity as Risk Factors for Bladder Cancer Prognosis: A Systematic Review and Meta-Analysis
Yu Lu, Jing Tao
Frontiers in Endocrinology.2021;[Epub] CrossRef - Breast cancer growth and proliferation is suppressed by the mitochondrial targeted furazano[3,4-b]pyrazine BAM15
Elizabeth R. M. Zunica, Christopher L. Axelrod, Eunhan Cho, Guillaume Spielmann, Gangarao Davuluri, Stephanie J. Alexopoulos, Martina Beretta, Kyle L. Hoehn, Wagner S. Dantas, Krisztian Stadler, William T. King, Kathryn Pergola, Brian A. Irving, Ingeborg
Cancer & Metabolism.2021;[Epub] CrossRef - How cancer cells remodel lipid metabolism: strategies targeting transcription factors
Do-Won Jeong, Seulbee Lee, Yang-Sook Chun
Lipids in Health and Disease.2021;[Epub] CrossRef - Diabetes and Colorectal Cancer Risk: A New Look at Molecular Mechanisms and Potential Role of Novel Antidiabetic Agents
Jelena Vekic, Aleksandra Zeljkovic, Aleksandra Stefanovic, Rosaria Vincenza Giglio, Marcello Ciaccio, Manfredi Rizzo
International Journal of Molecular Sciences.2021; 22(22): 12409. CrossRef - Diet and Obesity-Induced Methylglyoxal Production and Links to Metabolic Disease
Carlos Hernandez-Castillo, Sarah C. Shuck
Chemical Research in Toxicology.2021; 34(12): 2424. CrossRef - Оцінка прогнозованого ризику онкологічних захворювань у хворих на цукровий діабет 2-го типу
T.S. Vatseba, L.K. Sokolova, N.M. Koshel
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2021; 17(1): 86. CrossRef - Can novel adipokines, asprosin and meteorin-like, be biomarkers for malignant mesothelioma?
N. Kocaman, G. Artaş
Biotechnic & Histochemistry.2020; 95(3): 171. CrossRef - Metformin attenuates adhesion between cancer and endothelial cells in chronic hyperglycemia by recovery of the endothelial glycocalyx barrier
Marta Targosz-Korecka, Katarzyna Ewa Malek-Zietek, Damian Kloska, Zenon Rajfur, Ewa Łucja Stepien, Anna Grochot-Przeczek, Marek Szymonski
Biochimica et Biophysica Acta (BBA) - General Subjects.2020; 1864(4): 129533. CrossRef - Mitigation of Glucolipotoxicity-Induced Apoptosis, Mitochondrial Dysfunction, and Metabolic Stress by N-Acetyl Cysteine in Pancreatic β-Cells
Arwa Alnahdi, Annie John, Haider Raza
Biomolecules.2020; 10(2): 239. CrossRef - Antitumour Property ofPterocarpus santalinusSeeds Against DMBA-Induced Breast Cancer in Rats
Vivek Akhouri, Arun Kumar, Manorma Kumari
Breast Cancer: Basic and Clinical Research.2020; 14: 117822342095119. CrossRef - Sensitization of hepatocellular carcinoma cells towards doxorubicin and sorafenib is facilitated by glucose-dependent alterations in reactive oxygen species, P-glycoprotein and DKK4
Surbhi Chouhan, Snahlata Singh, Dipti Athavale, Pranay Ramteke, Muralidharan Vanuopadath, Bipin G Nair, Sudarslal Sadasivan Nair, Manoj Kumar Bhat
Journal of Biosciences.2020;[Epub] CrossRef - IGF-1 and hyperglycaemia-induced FOXA1 and IGFBP-2 affect epithelial to mesenchymal transition in prostate epithelial cells
Rehanna Mansor, Jeff Holly, Rachel Barker, Kalina Biernacka, Hanna Zielinska, Anthony Koupparis, Edward Rowe, Jon Oxley, Alex Sewell, Richard M. Martin, Athene Lane, Lucy Hackshaw-McGeagh, Claire Perks
Oncotarget.2020; 11(26): 2543. CrossRef - Doxorubicin delivery by polymer nanocarrier based on N-methylglucamine resorcinarene
Tatiana Yu. Sergeeva, Rezeda K. Mukhitova, Leysan R. Bakhtiozina, Irek R. Nizameev, Marsil K. Kadirov, Anastasia S. Sapunova, Alexandra D. Voloshina, Albina Y. Ziganshina, Igor S. Antipin
Supramolecular Chemistry.2020; 32(2): 150. CrossRef - Counteracting Chemoresistance with Metformin in Breast Cancers: Targeting Cancer Stem Cells
Samson Mathews Samuel, Elizabeth Varghese, Lenka Koklesová, Alena Líšková, Peter Kubatka, Dietrich Büsselberg
Cancers.2020; 12(9): 2482. CrossRef - Metformin in breast cancer: preclinical and clinical evidence
Anindita De, Gowthamarajan Kuppusamy
Current Problems in Cancer.2020; 44(1): 100488. CrossRef - The Role of Metabolic Factors in Renal Cancers
Jacek Rysz, Beata Franczyk, Janusz Ławiński, Robert Olszewski, Anna Gluba-Brzózka
International Journal of Molecular Sciences.2020; 21(19): 7246. CrossRef - Pre-operative dysglycemia is associated with decreased survival in patients with pancreatic neuroendocrine neoplasms
Marta Sandini, Oliver Strobel, Thomas Hank, Magdalena Lewosinska, Anna Nießen, Thilo Hackert, Markus W. Büchler, Simon Schimmack
Surgery.2020; 167(3): 575. CrossRef - Recent advances in cancer chemoprevention with phytochemicals
Yen-Chun Koh, Chi-Tang Ho, Min-Hsiung Pan
Journal of Food and Drug Analysis.2020; 28(1): 14. CrossRef - NF-κB and STAT3 co-operation enhances high glucose induced aggressiveness of cholangiocarcinoma cells
Charupong Saengboonmee, Chatchai Phoomak, Suangson Supabphol, Kyle R. Covington, Oliver Hampton, Chaisiri Wongkham, Richard A. Gibbs, Kazuo Umezawa, Wunchana Seubwai, Marie-Claude Gingras, Sopit Wongkham
Life Sciences.2020; 262: 118548. CrossRef - The Impact of obesity and diabetes mellitus on pancreatic cancer: Molecular mechanisms and clinical perspectives
Bao Quoc Lam, Sushant K. Shrivastava, Anju Shrivastava, Sharmila Shankar, Rakesh K. Srivastava
Journal of Cellular and Molecular Medicine.2020; 24(14): 7706. CrossRef - Chronic Diabetes Complications: The Need to Move beyond Classical Concepts
Dídac Mauricio, Núria Alonso, Mònica Gratacòs
Trends in Endocrinology & Metabolism.2020; 31(4): 287. CrossRef -
O
-GlcNAcylation on LATS2 disrupts the Hippo pathway by inhibiting its activity
Eunah Kim, Jeong Gu Kang, Min Jueng Kang, Jae Hyung Park, Yeon Jung Kim, Tae Hyun Kweon, Han-Woong Lee, Eek‐hoon Jho, Yong-ho Lee, Seung-Il Kim, Eugene C. Yi, Hyun Woo Park, Won Ho Yang, Jin Won Cho
Proceedings of the National Academy of Sciences.2020; 117(25): 14259. CrossRef - Circulating free methylglyoxal as a metabolic tumor biomarker in a rat colon adenocarcinoma model
Philippe Irigaray, Dominique Belpomme
Molecular and Clinical Oncology.2020;[Epub] CrossRef - Therapeutic effect of Aegle marmelos fruit extract against DMBA induced breast cancer in rats
Vivek Akhouri, Manorma Kumari, Arun Kumar
Scientific Reports.2020;[Epub] CrossRef - Biomechanical and Biophysical Properties of Breast Cancer Cells Under Varying Glycemic Regimens
Diganta Dutta, Xavier-Lewis Palmer, Jose Ortega-Rodas, Vasundhara Balraj, Indrani Ghosh Dastider, Surabhi Chandra
Breast Cancer: Basic and Clinical Research.2020; 14: 117822342097236. CrossRef - NLRP3 as Putative Marker of Ipilimumab-Induced Cardiotoxicity in the Presence of Hyperglycemia in Estrogen-Responsive and Triple-Negative Breast Cancer Cells
Vincenzo Quagliariello, Michelino De Laurentiis, Stefania Cocco, Giuseppina Rea, Annamaria Bonelli, Antonietta Caronna, Maria Cristina Lombari, Gabriele Conforti, Massimiliano Berretta, Gerardo Botti, Nicola Maurea
International Journal of Molecular Sciences.2020; 21(20): 7802. CrossRef - Glucose Concentration in Cell Culture Medium Influences the BRCA1-Mediated Regulation of the Lipogenic Action of IGF-I in Breast Cancer Cells
Moses O. Koobotse, Dayane Schmidt, Jeff M. P. Holly, Claire M. Perks
International Journal of Molecular Sciences.2020; 21(22): 8674. CrossRef - Diabetes, Glycated Hemoglobin, and Risk of Cancer in the UK Biobank Study
Rita Peila, Thomas E. Rohan
Cancer Epidemiology, Biomarkers & Prevention.2020; 29(6): 1107. CrossRef - ASSOCIATION OF IRISIN WITH THE OXIDANT-ANTI OXIDANT PARAMETERS IN TYPE 2 DIABETIC PATIENTS ACCORDING TO AGE IN THI-QAR PROVINCE/ IRAQ
Saad H. Al-Badry, Khalid G. Al-Fartoosi
International Journal of Research in Science and Technology.2020; 10(01): 10. CrossRef - Metabolomic profiling of blood plasma in patients with primary brain tumours: Basal plasma metabolites correlated with tumour grade and plasma biomarker analysis predicts feasibility of the successful statistical discrimination from healthy subjects – a p
Eva Baranovičová, Tomáš Galanda, Miroslav Galanda, Jozef Hatok, Branislav Kolarovszki, Romana Richterová, Peter Račay
IUBMB Life.2019; 71(12): 1994. CrossRef - Metformin as an adjuvant in breast cancer treatment
Mohsin HK Roshan, Yan K Shing, Nikolai P Pace
SAGE Open Medicine.2019; 7: 205031211986511. CrossRef - The added value of fasting blood glucose to serum squamous cell carcinoma antigen for predicting oncological outcomes in cervical cancer patients receiving neoadjuvant chemotherapy followed by radical hysterectomy
Miao‐Fang Wu, Mei‐Mei Guan, Chang‐Hao Liu, Jie‐Ying Wu, Qun‐Xian Rao, Jing Li
Cancer Medicine.2019; 8(11): 5068. CrossRef - Visit-to-Visit Hemoglobin A1c Variability Is Associated With Later Cancer Development in Patients With Diabetes Mellitus
Yuki Saito, Hiroshi Noto, Osamu Takahashi, Daiki Kobayashi
The Cancer Journal.2019; 25(4): 237. CrossRef - O-GlcNAcylation of GLI transcription factors in hyperglycemic conditions augments Hedgehog activity
Shamik Das, Sarah K. Bailey, Brandon J. Metge, Ann Hanna, Dominique C. Hinshaw, Mateus Mota, Andres Forero-Torres, John C. Chatham, Rajeev S. Samant, Lalita A. Shevde
Laboratory Investigation.2019; 99(2): 260. CrossRef - Diabetes and Cancer: Cancer Should Be Screened in Routine Diabetes Assessment
Sunghwan Suh, Kwang-Won Kim
Diabetes & Metabolism Journal.2019; 43(6): 733. CrossRef - Herbal Medicines Attenuate PD-L1 Expression to Induce Anti-Proliferation in Obesity-Related Cancers
Yu-Chen S.H. Yang, Zi-Lin Li, Ya-Jung Shih, James A. Bennett, Jaqueline Whang-Peng, Hung-Yun Lin, Paul J. Davis, Kuan Wang
Nutrients.2019; 11(12): 2979. CrossRef - Gestational diabetes mellitus and maternal breast cancer risk: a meta-analysis of the literature
Chuanbo Xie, Wei Wang, Xiuhong Li, Nan Shao, Weidong Li
The Journal of Maternal-Fetal & Neonatal Medicine.2019; 32(6): 1022. CrossRef - HIPK2 role in the tumor–host interaction: Impact on fibroblasts transdifferentiation CAF‐like
Alessia Garufi, Gianandrea Traversi, Mara Cirone, Gabriella D'Orazi
IUBMB Life.2019; 71(12): 2055. CrossRef - Blood glucose, glucose balance, and disease-specific survival after prostate cancer diagnosis in the Finnish Randomized Study of Screening for Prostate Cancer
Teemu J. Murtola, Samueli M. Sälli, Kirsi Talala, Kimmo Taari, Teuvo L. J. Tammela, Anssi Auvinen
Prostate Cancer and Prostatic Diseases.2019; 22(3): 453. CrossRef - Reduced chemotherapeutic sensitivity in high glucose condition: implication of antioxidant response
Alessia Garufi, Gianandrea Traversi, Maria Saveria Gilardini Montani, Valerio D’Orazi, Giuseppa Pistritto, Mara Cirone, Gabriella D’Orazi
Oncotarget.2019; 10(45): 4691. CrossRef - Hyperglycemia Associated Metabolic and Molecular Alterations in Cancer Risk, Progression, Treatment, and Mortality
Ramteke, Deb, Shepal, Bhat
Cancers.2019; 11(9): 1402. CrossRef - Flaxseed Lignans as Important Dietary Polyphenols for Cancer Prevention and Treatment: Chemistry, Pharmacokinetics, and Molecular Targets
S. Franklyn De Silva, Jane Alcorn
Pharmaceuticals.2019; 12(2): 68. CrossRef - Serum gamma-glutamyltransferase and the overall survival of metastatic pancreatic cancer
Yuanyuan Xiao, Haijun Yang, Jian Lu, Dehui Li, Chuanzhi Xu, Harvey A. Risch
BMC Cancer.2019;[Epub] CrossRef - N-acetyl cysteine attenuates oxidative stress and glutathione-dependent redox imbalance caused by high glucose/high palmitic acid treatment in pancreatic Rin-5F cells
Arwa Alnahdi, Annie John, Haider Raza, M. Firoze Khan
PLOS ONE.2019; 14(12): e0226696. CrossRef - Targeting receptors of advanced glycation end products (RAGE): Preventing diabetes induced cancer and diabetic complications
Abu Sufiyan Chhipa, Swapnil P. Borse, Ruma Baksi, Sunali Lalotra, Manish Nivsarkar
Pathology - Research and Practice.2019; 215(11): 152643. CrossRef - Methylglyoxal, a potent inducer of AGEs, connects between diabetes and cancer
Justine Bellier, Marie-Julie Nokin, Eva Lardé, Philippe Karoyan, Olivier Peulen, Vincent Castronovo, Akeila Bellahcène
Diabetes Research and Clinical Practice.2019; 148: 200. CrossRef - Molecular Mechanisms of Cancer-Induced Sleep Disruption
William H. Walker, Jeremy C. Borniger
International Journal of Molecular Sciences.2019; 20(11): 2780. CrossRef - Addition of zoledronic acid to neoadjuvant chemotherapy is not beneficial in patients with HER2-negative stage II/III breast cancer: 5-year survival analysis of the NEOZOTAC trial (BOOG 2010-01)
Stefanie de Groot, Hanno Pijl, Ayoub Charehbili, Saskia van de Ven, Vincent T. H. B. M. Smit, Elma Meershoek-Klein Kranenbarg, Joan B. Heijns, Laurence J. C. van Warmerdam, Lonneke W. Kessels, M. Wouter Dercksen, Manon J. A. E. Pepels, Hanneke W. M. van L
Breast Cancer Research.2019;[Epub] CrossRef - Assessing the Effect of Various Blood Glucose Levels on 18F-FDG Activity in the Brain, Liver, and Blood Pool
Ismet Sarikaya, Ali Sarikaya, Prem Sharma
Journal of Nuclear Medicine Technology.2019; 47(4): 313. CrossRef - Efficacy of Complementary Therapies in the Quality of Life of Breast Cancer Survivors
Sahar Zaidi, Showket Hussain, Shalini Verma, Zubia Veqar, Asiya Khan, Sheeraz Un Nazir, Neha Singh, Jamal Ali Moiz, Pranay Tanwar, Anurag Srivastava, G. K. Rath, Ravi Mehrotra
Frontiers in Oncology.2018;[Epub] CrossRef - A Role for Hypocretin/Orexin in Metabolic and Sleep Abnormalities in a Mouse Model of Non-metastatic Breast Cancer
Jeremy C. Borniger, William H. Walker II, Surbhi, Kathryn M. Emmer, Ning Zhang, Abigail A. Zalenski, Stevie L. Muscarella, Julie A. Fitzgerald, Alexandra N. Smith, Cornelius J. Braam, Tial TinKai, Ulysses J. Magalang, Maryam B. Lustberg, Randy J. Nelson,
Cell Metabolism.2018; 28(1): 118. CrossRef - Model-based in silico analysis of the PI3K/Akt pathway: the elucidation of cross-talk between diabetes and breast cancer
Sammia Rehman, Ayesha Obaid, Anam Naz, Amjad Ali, Shahzina Kanwal, Jamil Ahmad
PeerJ.2018; 6: e5917. CrossRef - Inhibitory Effect of Anoectochilus formosanus Extract on Hyperglycemia-Related PD-L1 Expression and Cancer Proliferation
Yih Ho, Yan-Fang Chen, Li-Hsuan Wang, Kuang-Yang Hsu, Yu-Tang Chin, Yu-Chen S. H. Yang, Shwu-Huey Wang, Yi-Ru Chen, Ya-Jung Shih, Leroy F. Liu, Kuan Wang, Jacqueline Whang-Peng, Heng-Yuan Tang, Hung-Yun Lin, Hsuan-Liang Liu, Shwu-Jiuan Lin
Frontiers in Pharmacology.2018;[Epub] CrossRef - Hypoxia driven glycation: Mechanisms and therapeutic opportunities
Mohammad Imran Khan, Suvasmita Rath, Vaqar Mustafa Adhami, Hasan Mukhtar
Seminars in Cancer Biology.2018; 49: 75. CrossRef - Metformin reduces glucose intolerance caused by rapamycin treatment in genetically heterogeneous female mice
Roxanne Weiss, Elizabeth Fernandez, Yuhong Liu, Randy Strong, Adam B. Salmon
Aging.2018; 10(3): 386. CrossRef - High glucose induces epithelial‑mesenchymal transition and results in the migration and invasion of colorectal cancer cells
Jiayan Wu, Jiayi Chen, Yang Xi, Fuyan Wang, Hongcun Sha, Lin Luo, Yabin Zhu, Xiaoming Hong, Shizhong Bu
Experimental and Therapeutic Medicine.2018;[Epub] CrossRef - Laminar shear stress inhibits high glucose-induced migration and invasion in human bladder cancer cells
Yu-Hsiang Lee, Chien-Hsuan Yeh
In Vitro Cellular & Developmental Biology - Animal.2018; 54(2): 120. CrossRef - Methylglyoxal-derived stress: An emerging biological factor involved in the onset and progression of cancer
Akeila Bellahcène, Marie-Julie Nokin, Vincent Castronovo, Casper Schalkwijk
Seminars in Cancer Biology.2018; 49: 64. CrossRef - Extracellular matrix glycation and receptor for advanced glycation end-products activation: a missing piece in the puzzle of the association between diabetes and cancer
Armando Rojas, Carolina Añazco, Ileana González, Paulina Araya
Carcinogenesis.2018; 39(4): 515. CrossRef - Good glycaemic control is associated with a better prognosis in breast cancer patients with type 2 diabetes mellitus
Yen-Lin Chang, Wayne Huey-Herng Sheu, Shih-Yi Lin, Wen-Shyong Liou
Clinical and Experimental Medicine.2018; 18(3): 383. CrossRef - High glucose contributes to the proliferation and migration of non-small-cell lung cancer cells via GAS5-TRIB3 axis
Cheng-Zhi Ding, Xu-Feng Guo, Guo-Lei Wang, Hong-Tao Wang, Guang-Hui Xu, Yuan-Yuan Liu, Zhen-Jiang Wu, Yu-Hang Chen, Jiao Wang, Wen-Guang Wang
Bioscience Reports.2018;[Epub] CrossRef - Challenges and perspectives in the treatment of diabetes associated breast cancer
Samson Mathews Samuel, Elizabeth Varghese, Sharon Varghese, Dietrich Büsselberg
Cancer Treatment Reviews.2018; 70: 98. CrossRef - Linking type 2 diabetes and gynecological cancer: an introductory overview
Emanuela Anastasi, Tiziana Filardi, Sara Tartaglione, Andrea Lenzi, Antonio Angeloni, Susanna Morano
Clinical Chemistry and Laboratory Medicine (CCLM).2018; 56(9): 1413. CrossRef - Hyperglycaemia and Survival in Solid Tumours: A Systematic Review and Meta-analysis
R. Barua, A.J. Templeton, B. Seruga, A. Ocana, E. Amir, J.-L. Ethier
Clinical Oncology.2018; 30(4): 215. CrossRef - Hepatocellular carcinoma-associated hypercholesterolemia: involvement of proprotein-convertase-subtilisin-kexin type-9 (PCSK9)
Dipti Athavale, Surbhi Chouhan, Vimal Pandey, Shyamananda Singh Mayengbam, Snahlata Singh, Manoj Kumar Bhat
Cancer & Metabolism.2018;[Epub] CrossRef - An insight on the association of glycation with hepatocellular carcinoma
Nasimudeen R. Jabir, Saheem Ahmad, Shams Tabrez
Seminars in Cancer Biology.2018; 49: 56. CrossRef - Risk score system for the prediction of hepatocellular carcinoma in patients with type 2 diabetes: Taiwan Diabetes Study
Tsai-Chung Li, Chia-Ing Li, Chiu-Shong Liu, Wen-Yuan Lin, Chih-Hsueh Lin, Sing-Yu Yang, Cheng-Chieh Lin
Seminars in Oncology.2018; 45(5-6): 264. CrossRef - RAGE and Its Ligands: Molecular Interplay Between Glycation, Inflammation, and Hallmarks of Cancer—a Review
Gowri Palanissami, Solomon F. D. Paul
Hormones and Cancer.2018; 9(5): 295. CrossRef - Beta-hydroxybutyrate (3-OHB) can influence the energetic phenotype of breast cancer cells, but does not impact their proliferation and the response to chemotherapy or radiation
Catharina Bartmann, Sudha R. Janaki Raman, Jessica Flöter, Almut Schulze, Katrin Bahlke, Jana Willingstorfer, Maria Strunz, Achim Wöckel, Rainer J. Klement, Michaela Kapp, Cholpon S. Djuzenova, Christoph Otto, Ulrike Kämmerer
Cancer & Metabolism.2018;[Epub] CrossRef - Obesity, Diabetes and Gastrointestinal Malignancy: The role of Metformin and other Anti-diabetic Therapy
McFarlane Samy I
Global Journal of Obesity, Diabetes and Metabolic Syndrome.2018; : 008. CrossRef - Pretreatment glycemic control status is an independent prognostic factor for cervical cancer patients receiving neoadjuvant chemotherapy for locally advanced disease
Jing Li, Ni-ya Ning, Qun-xian Rao, Rong Chen, Li-juan Wang, Zhong-qiu Lin
BMC Cancer.2017;[Epub] CrossRef - Differences in risk factors of malignancy between men and women with type 2 diabetes: A retrospective case-control study
Mariusz Dąbrowski, Elektra Szymańska-Garbacz, Zofia Miszczyszyn, Tadeusz Dereziński, Leszek Czupryniak
Oncotarget.2017; 8(40): 66940. CrossRef - Beta-glucans and cancer: The influence of inflammation and gut peptide
Sara Baldassano, Giulia Accardi, Sonya Vasto
European Journal of Medicinal Chemistry.2017; 142: 486. CrossRef - Enemies or weapons in hands: investigational anti-diabetic drug glibenclamide and cancer risk
Rui Gao, Tao Yang, Wei Xu
Expert Opinion on Investigational Drugs.2017; 26(7): 853. CrossRef - Hyperglycemia triggers HIPK2 protein degradation
Silvia Baldari, Alessia Garufi, Marisa Granato, Laura Cuomo, Giuseppa Pistritto, Mara Cirone, Gabriella D’Orazi
Oncotarget.2017; 8(1): 1190. CrossRef - Monitoring p53 by MDM2 and MDMX is required for endocrine pancreas development and function in a spatio-temporal manner
Yiwei Zhang, Shelya X. Zeng, Qian Hao, Hua Lu
Developmental Biology.2017; 423(1): 34. CrossRef - Modulation of Mammary Stromal Cell Lactate Dynamics by Ambient Glucose and Epithelial Factors
Nicolas Tobar, Omar Porras, Patricio C. Smith, L. Felipe Barros, Jorge Martínez
Journal of Cellular Physiology.2017; 232(1): 136. CrossRef - Energy metabolism in glioblastoma stem cells: PPARα a metabolic adaptor to intratumoral microenvironment
Alessia Fidoamore, Loredana Cristiano, Chiara Laezza, Renato Galzio, Elisabetta Benedetti, Benedetta Cinque, Andrea Antonosante, Michele d’Angelo, Vanessa Castelli, Maria Grazia Cifone, Rodolfo Ippoliti, Antonio Giordano, Annamaria Cimini
Oncotarget.2017; 8(65): 108430. CrossRef - Hyperglycemia is Associated with Poor Survival in Primary Central Nervous System Lymphoma Patients
Ayumi Debata, Koichi Yoshida, Kenta Ujifuku, Haruna Yasui, Kensaku Kamada, Daisuke Niino, Takayuki Matsuo
Tumori Journal.2017; 103(3): 272. CrossRef - Micronucleus, cell-free DNA, and plasma glycan composition in the newborns of healthy and diabetic mothers
Aleksandra Fucic, Vedrana Guszak, Toma Keser, Jasenka Wagner, Emilja Juretić, Davor Plavec, Ranko Stojković, Olga Gornik, Gordan Lauc
Mutation Research/Genetic Toxicology and Environmental Mutagenesis.2017; 815: 6. CrossRef - Hyperglycemia exacerbates colon cancer malignancy through hexosamine biosynthetic pathway
A Vasconcelos-dos-Santos, H F B R Loponte, N R Mantuano, I A Oliveira, I F de Paula, L K Teixeira, J C M de-Freitas-Junior, K C Gondim, N Heise, R Mohana-Borges, J A Morgado-Díaz, W B Dias, A R Todeschini
Oncogenesis.2017; 6(3): e306. CrossRef - Associations between prediagnostic blood glucose levels, diabetes, and glioma
Judith Schwartzbaum, Michael Edlinger, Victoria Zigmont, Pär Stattin, Grzegorz A. Rempala, Gabriele Nagel, Niklas Hammar, Hanno Ulmer, Bernhard Föger, Göran Walldius, Jonas Manjer, Håkan Malmström, Maria Feychting
Scientific Reports.2017;[Epub] CrossRef - Gestational diabetes mellitus may be associated with increased risk of breast cancer
Yong-Moon Mark Park, Katie M O'Brien, Shanshan Zhao, Clarice R Weinberg, Donna D Baird, Dale P Sandler
British Journal of Cancer.2017; 116(7): 960. CrossRef - The transcription factor carbohydrate-response element-binding protein (ChREBP): A possible link between metabolic disease and cancer
Katsumi Iizuka
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2017; 1863(2): 474. CrossRef - The essential role of YAP O-GlcNAcylation in high-glucose-stimulated liver tumorigenesis
Xiao Zhang, Yongxia Qiao, Qi Wu, Yan Chen, Shaowu Zou, Xiangfan Liu, Guoqing Zhu, Yinghui Zhao, Yuxin Chen, Yongchun Yu, Qiuhui Pan, Jiayi Wang, Fenyong Sun
Nature Communications.2017;[Epub] CrossRef - Anthocyanins from Purple Corn Ameliorated Tumor Necrosis Factor‐α‐Induced Inflammation and Insulin Resistance in 3T3‐L1 Adipocytes via Activation of Insulin Signaling and Enhanced GLUT4 Translocation
Diego Luna‐Vital, Matthew Weiss, Elvira Gonzalez de Mejia
Molecular Nutrition & Food Research.2017;[Epub] CrossRef - Hyperglycaemia and aberrated insulin signalling stimulate tumour progression via induction of the extracellular matrix component hyaluronan
Sören Twarock, Christina Reichert, Ulrike Peters, Daniel J. Gorski, Katharina Röck, Jens W. Fischer
International Journal of Cancer.2017; 141(4): 791. CrossRef - Das Karzinom in der Polarität zwischen Stoffwechsel- und Nerven-Sinnes-System – Konsequenzen für die Therapie
H. Schramm
Der Merkurstab.2017; 70(3): 221. CrossRef - Addressing the Role of Obesity in Endometrial Cancer Risk, Prevention, and Treatment
Michaela A. Onstad, Rosemarie E. Schmandt, Karen H. Lu
Journal of Clinical Oncology.2016; 34(35): 4225. CrossRef - Mechanisms through which diabetes mellitus influences renal cell carcinoma development and treatment: A review of the literature
Dominika Labochka, Barbara Moszczuk, Wojciech Kukwa, Cezary Szczylik, Anna M. Czarnecka
International Journal of Molecular Medicine.2016; 38(6): 1887. CrossRef - Cancer Risk in Patients With Empyema
Chung-Jen Teng, Yu-Wen Hu, Chiu-Mei Yeh, Tzeng-Ji Chen, Chia-Jen Liu
Medicine.2016; 95(9): e2934. CrossRef - High Glucose Stimulates Tumorigenesis in Hepatocellular Carcinoma Cells Through AGER-Dependent O-GlcNAcylation of c-Jun
Yongxia Qiao, Xiao Zhang, Yue Zhang, Yulan Wang, Yanfeng Xu, Xiangfan Liu, Fenyong Sun, Jiayi Wang
Diabetes.2016; 65(3): 619. CrossRef - Association between baseline serum glucose, triglycerides and total cholesterol, and prostate cancer risk categories
Rhonda Arthur, Henrik Møller, Hans Garmo, Lars Holmberg, Pår Stattin, Håkan Malmstrom, Mats Lambe, Niklas Hammar, Göran Walldius, David Robinson, Ingmar Jungner, Mieke Van Hemelrijck
Cancer Medicine.2016; 5(6): 1307. CrossRef - Risk factors for cancer development in type 2 diabetes: A retrospective case-control study
Mariusz Dąbrowski, Elektra Szymańska-Garbacz, Zofia Miszczyszyn, Tadeusz Dereziński, Leszek Czupryniak
BMC Cancer.2016;[Epub] CrossRef - High-fat Western diet–induced obesity contributes to increased tumor growth in mouse models of human colon cancer
Ann Marie O'Neill, Christine M. Burrington, Erin A. Gillaspie, Darin T. Lynch, Melissa J. Horsman, Michael W. Greene
Nutrition Research.2016; 36(12): 1325. CrossRef - Diabetes Pharmacotherapies and Bladder Cancer: A Medicare Epidemiologic Study
Todd A. Mackenzie, Rebecca Zaha, Jeremy Smith, Margaret R. Karagas, Nancy E. Morden
Diabetes Therapy.2016; 7(1): 61. CrossRef - Diabetes mellitus stimulates pancreatic cancer growth and epithelial-mesenchymal transition-mediated metastasis via a p38 MAPK pathway
Lishan Wang, Ying-Ying Bai, Yang Yang, Fangfang Hu, Yonghui Wang, Zeqian Yu, Zhangjun Cheng, Jiahua Zhou
Oncotarget.2016; 7(25): 38539. CrossRef - Prognostic Significance of Hyperglycemia in Patients with Brain Tumors: a Meta-Analysis
Hongwei Liu, Zhixiong Liu, Bing Jiang, Xiping Ding, Lei Huo, Xin Wan, Jinfang Liu, Zhenyun Xia
Molecular Neurobiology.2016; 53(3): 1654. CrossRef - Impact of Hyperglycemia on Outcomes among Patients Receiving Neoadjuvant Chemotherapy for Bulky Early Stage Cervical Cancer
Jing Li, Miao-fang Wu, Huai-wu Lu, Bing-zhong Zhang, Li-juan Wang, Zhong-qiu Lin, Xing Xie
PLOS ONE.2016; 11(11): e0166612. CrossRef - Obesity, Inflammation, and Cancer
Tuo Deng, Christopher J. Lyon, Stephen Bergin, Michael A. Caligiuri, Willa A. Hsueh
Annual Review of Pathology: Mechanisms of Disease.2016; 11(1): 421. CrossRef - Hyperglycemia, tumorigenesis, and chronic inflammation
Shu-Chun Chang, Wei-Chung Vivian Yang
Critical Reviews in Oncology/Hematology.2016; 108: 146. CrossRef - Methylglyoxal, a glycolysis side-product, induces Hsp90 glycation and YAP-mediated tumor growth and metastasis
Marie-Julie Nokin, Florence Durieux, Paul Peixoto, Barbara Chiavarina, Olivier Peulen, Arnaud Blomme, Andrei Turtoi, Brunella Costanza, Nicolas Smargiasso, Dominique Baiwir, Jean L Scheijen, Casper G Schalkwijk, Justine Leenders, Pascal De Tullio, Elettra
eLife.2016;[Epub] CrossRef - ZnCl2 sustains the adriamycin-induced cell death inhibited by high glucose
A Garufi, D Trisciuoglio, M Cirone, G D'Orazi
Cell Death & Disease.2016; 7(6): e2280. CrossRef - Controlling Malglycemia in Patients Undergoing Treatment for Cancer
Susan Storey, Veronica Brady, Ashley Leak Bryant, Ellen Davis, Marilyn Hammer, Denise Hershey, Jill Olausson, Jane Seley
Clinical Journal of Oncology Nursing.2016; 20(1): 92. CrossRef - Metformin, Diabetes, and Survival among U.S. Veterans with Colorectal Cancer
Jessica K. Paulus, Christina D. Williams, Furha I. Cossor, Michael J. Kelley, Robert E. Martell
Cancer Epidemiology, Biomarkers & Prevention.2016; 25(10): 1418. CrossRef - Thymic emigration patterns in patients with type 2 diabetes treated with metformin
Grzegorz Dworacki, Olzhas Urazayev, Yerbol Bekmukhambetov, Saule Iskakova, Bartosz A. Frycz, Paweł P. Jagodziński, Marzena Dworacka
Immunology.2015; 146(3): 456. CrossRef - Resveratrol in the treatment of pancreatic cancer
Qinhong Xu, Liang Zong, Xin Chen, Zhengdong Jiang, Ligang Nan, Jiahui Li, Wanxing Duan, Jianjun Lei, Lun Zhang, Jiguang Ma, Xuqi Li, Zheng Wang, Zheng Wu, Qingyong Ma, Zhenhua Ma
Annals of the New York Academy of Sciences.2015; 1348(1): 10. CrossRef - Effect of hyperglycemia on hepatocellular carcinoma development in diabetes
Yasuhiro Niwa, Kota Ishikawa, Masatoshi Ishigami, Takashi Honda, Koichi Achiwa, Takako Izumoto, Ryuya Maekawa, Kaori Hosokawa, Atsushi Iida, Yusuke Seino, Yoji Hamada, Hidemi Goto, Yutaka Oiso, Hiroshi Arima, Shin Tsunekawa
Biochemical and Biophysical Research Communications.2015; 463(3): 344. CrossRef - The insulin-like growth factor I system: Physiological and pathophysiological implication in cardiovascular diseases associated with metabolic syndrome
Jun Ren, Piero Anversa
Biochemical Pharmacology.2015; 93(4): 409. CrossRef - Diabetes and risk of cancer
Toshiya Atsumi
Diabetology International.2015; 6(3): 190. CrossRef - The influencing factors associated with glycemic control among adult diabetes patients
Kisook Kim
Journal of the Korea Academia-Industrial cooperation Society.2015; 16(5): 3284. CrossRef - Reply to “Preoperative Evaluation of Pancreatic Adenocarcinoma”
Siva P. Raman
American Journal of Roentgenology.2015; 205(2): W226. CrossRef
- Enhanced degradation of epidermal growth factor receptor by metformin

 KDA
KDA
 First
First Prev
Prev





