
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Complications
- Association of Muscle Mass Loss with Diabetes Development in Liver Transplantation Recipients
- Sejeong Lee, Minyoung Lee, Young-Eun Kim, Hae Kyung Kim, Sook Jung Lee, Jiwon Kim, Yurim Yang, Chul Hoon Kim, Hyangkyu Lee, Dong Jin Joo, Myoung Soo Kim, Eun Seok Kang
- Diabetes Metab J. 2024;48(1):146-156. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0100
- 935 View
- 120 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
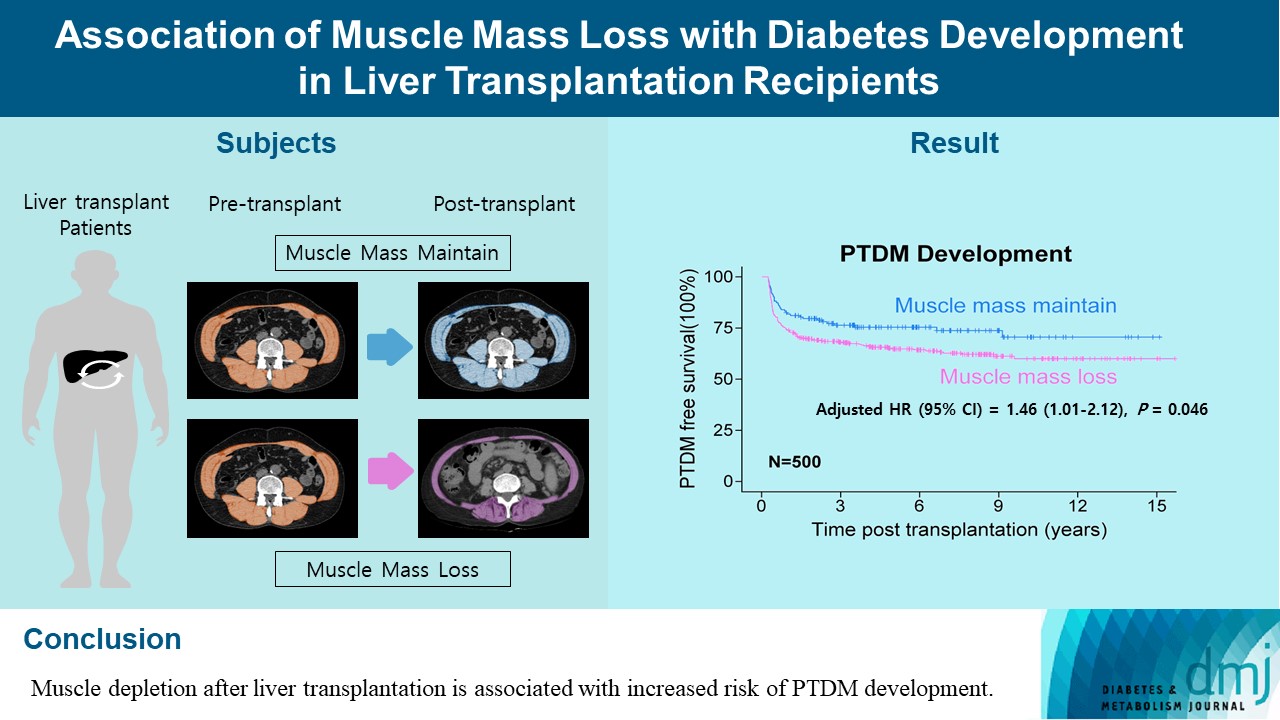
Post-transplant diabetes mellitus (PTDM) is one of the most significant complications after transplantation. Patients with end-stage liver diseases requiring transplantation are prone to sarcopenia, but the association between sarcopenia and PTDM remains to be elucidated. We aimed to investigate the effect of postoperative muscle mass loss on PTDM development.
Methods
A total of 500 patients who underwent liver transplantation at a tertiary care hospital between 2005 and 2020 were included. Skeletal muscle area at the level of the L3–L5 vertebrae was measured using computed tomography scans performed before and 1 year after the transplantation. The associations between the change in the muscle area after the transplantation and the incidence of PTDM was investigated using a Cox proportional hazard model.
Results
During the follow-up period (median, 4.9 years), PTDM occurred in 165 patients (33%). The muscle mass loss was greater in patients who developed PTDM than in those without PTDM. Muscle depletion significantly increased risk of developing PTDM after adjustment for other confounding factors (hazard ratio, 1.50; 95% confidence interval, 1.23 to 1.84; P=0.001). Of the 357 subjects who had muscle mass loss, 124 (34.7%) developed PTDM, whereas of the 143 patients in the muscle mass maintenance group, 41 (28.7%) developed PTDM. The cumulative incidence of PTDM was significantly higher in patients with muscle loss than in patients without muscle loss (P=0.034).
Conclusion
Muscle depletion after liver transplantation is associated with increased risk of PTDM development.
- Lifestyle
- Type 2 Diabetes Mellitus and Sarcopenia as Comorbid Chronic Diseases in Older Adults: Established and Emerging Treatments and Therapies
- Jakub Mesinovic, Jackson J. Fyfe, Jason Talevski, Michael J. Wheeler, Gloria K.W. Leung, Elena S. George, Melkamu T. Hunegnaw, Costas Glavas, Paul Jansons, Robin M. Daly, David Scott
- Diabetes Metab J. 2023;47(6):719-742. Published online September 14, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0112
- 4,571 View
- 438 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
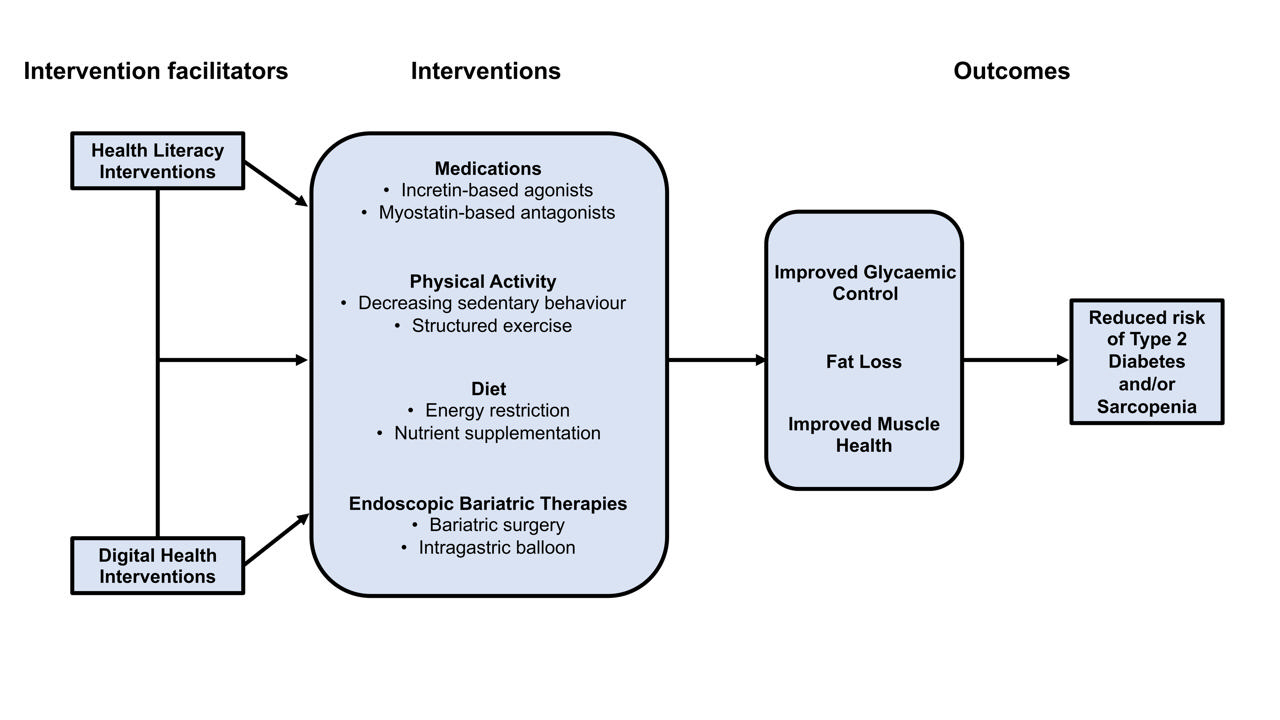
ePub - Type 2 diabetes mellitus (T2DM) and sarcopenia (low skeletal muscle mass and function) share a bidirectional relationship. The prevalence of these diseases increases with age and they share common risk factors. Skeletal muscle fat infiltration, commonly referred to as myosteatosis, may be a major contributor to both T2DM and sarcopenia in older adults via independent effects on insulin resistance and muscle health. Many strategies to manage T2DM result in energy restriction and subsequent weight loss, and this can lead to significant declines in muscle mass in the absence of resistance exercise, which is also a first-line treatment for sarcopenia. In this review, we highlight recent evidence on established treatments and emerging therapies targeting weight loss and muscle mass and function improvements in older adults with, or at risk of, T2DM and/or sarcopenia. This includes dietary, physical activity and exercise interventions, new generation incretin-based agonists and myostatin-based antagonists, and endoscopic bariatric therapies. We also highlight how digital health technologies and health literacy interventions can increase uptake of, and adherence to, established and emerging treatments and therapies in older adults with T2DM and/or sarcopenia.
-
Citations
Citations to this article as recorded by- Fucoidan ameliorates diabetic skeletal muscle atrophy through PI3K/Akt pathway
Caixia Li, Yaping Liu, Mingzhi Yang, Haoyue Huang, Lulu Tang, Yufan Miao, Wenjie Li, Xing Li
Journal of Functional Foods.2024; 114: 106076. CrossRef
- Fucoidan ameliorates diabetic skeletal muscle atrophy through PI3K/Akt pathway
- Metabolic Risk/Epidemiology
- Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography
- Hwi Seung Kim, Jiwoo Lee, Eun Hee Kim, Min Jung Lee, In Young Bae, Woo Je Lee, Joong-Yeol Park, Hong-Kyu Kim, Chang Hee Jung
- Diabetes Metab J. 2023;47(1):104-117. Published online January 26, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0081
- 3,242 View
- 176 Download
- 7 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
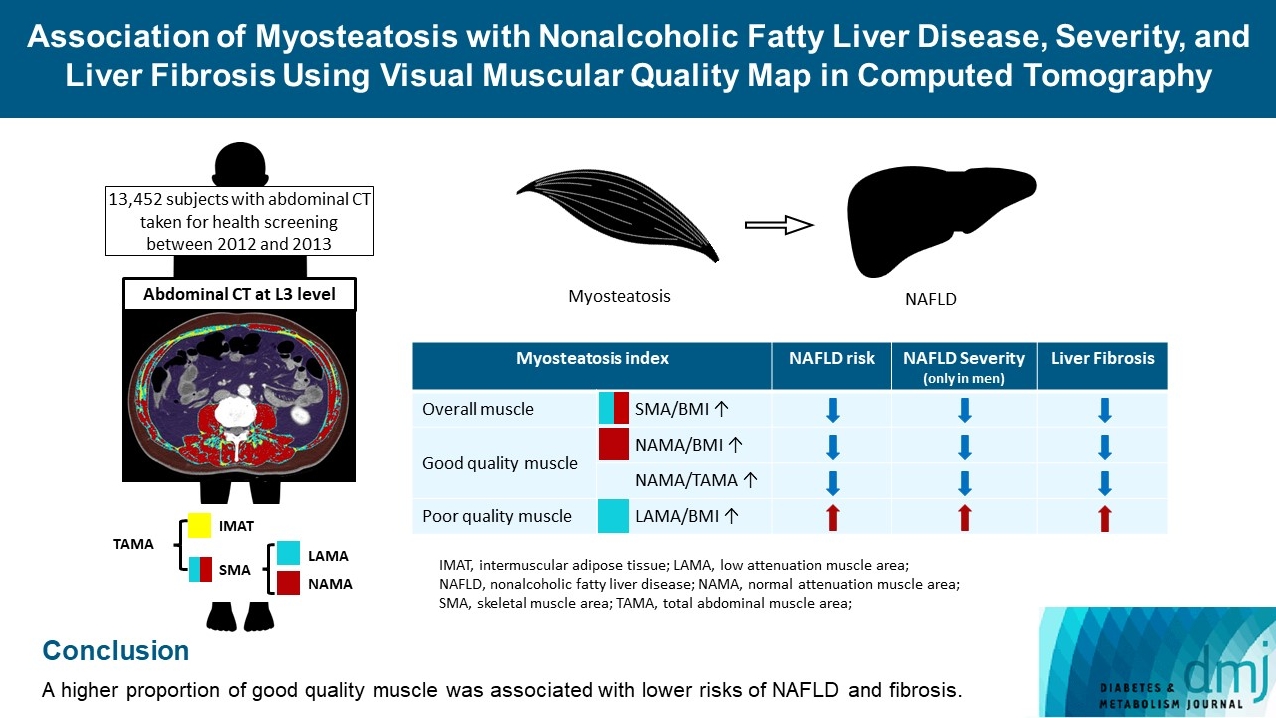
The association of myosteatosis measured using visual muscular quality map in computed tomography (CT) with nonalcoholic fatty liver disease (NAFLD), its severity, and fibrosis was analyzed in a large population.
Methods
Subjects (n=13,452) with abdominal CT between 2012 and 2013 were measured total abdominal muscle area (TAMA) at L3 level. TAMA was segmented into intramuscular adipose tissue and skeletal muscle area (SMA), which was further classified into normal attenuation muscle area (NAMA) and low attenuation muscle area (LAMA). The following variables were adopted as indicators of myosteatosis: SMA/body mass index (BMI), NAMA/BMI, NAMA/TAMA, and LAMA/BMI. NAFLD and its severity were assessed by ultrasonography, and liver fibrosis was measured by calculating the NAFLD fibrosis score (NFS) and fibrosis-4 index (FIB-4) scores.
Results
According to multiple logistic regression analyses, as quartiles of SMA/BMI, NAMA/BMI, and NAMA/TAMA increased, the odds ratios (ORs) for NAFLD decreased in each sex (P for trend <0.001 for all). The ORs of moderate/severe NAFLD were significantly higher in the Q1 group than in the Q4 group for SMA/BMI, NAMA/BMI, and NAMA/TAMA in men. The ORs of intermediate/high liver fibrosis scores assessed by NFS and FIB-4 scores increased linearly with decreasing quartiles for SMA/BMI, NAMA/BMI, and NAMA/TAMA in each sex (P for trend <0.001 for all). Conversely, the risk for NAFLD and fibrosis were positively associated with LAMA/BMI quartiles in each sex (P for trend <0.001 for all).
Conclusion
A higher proportion of good quality muscle was associated with lower risks of NAFLD and fibrosis. -
Citations
Citations to this article as recorded by- Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography (Diabetes Metab J 2023;47:104-17)
Hwi Seung Kim, Hong-Kyu Kim, Chang Hee Jung
Diabetes & Metabolism Journal.2023; 47(2): 304. CrossRef - Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography (Diabetes Metab J 2023;47:104-17)
Eun Roh
Diabetes & Metabolism Journal.2023; 47(2): 301. CrossRef - Sarcopenia, a condition shared by various diseases: can we alleviate or delay the progression?
Giovanni Tarantino, Gaia Sinatti, Vincenzo Citro, Silvano Santini, Clara Balsano
Internal and Emergency Medicine.2023; 18(7): 1887. CrossRef - Association of Visceral Fat Obesity, Sarcopenia, and Myosteatosis with Non-Alcoholic Fatty Liver Disease without Obesity
Hong-Kyu Kim, Sung-Jin Bae, Min Jung Lee, Eun Hee Kim, Hana Park, Hwi Seung Kim, Yun Kyung Cho, Chang Hee Jung, Woo Je Lee, Jaewon Choe
Clinical and Molecular Hepatology.2023; 29(4): 987. CrossRef - Current view of the surgical anatomy of the anterolateral abdominal wall muscles and their aponeuroses
A.V. Pavlov, A.S. Baranova, A.V. Fedoseyev, A.I. Vvedensky, G.S. Lazutina, N.V. Ovchinnikova, I.V. Bakharev
Operativnaya khirurgiya i klinicheskaya anatomiya (Pirogovskii nauchnyi zhurnal).2023; 7(3): 44. CrossRef - Muscle Fat Content Is Associated with Nonalcoholic Fatty Liver Disease and Liver Fibrosis in Chinese Adults
W. Guo, X. Zhao, D. Cheng, X. Liang, M. Miao, X. Li, J. Lu, N. Xu, Shuang Hu, Qun Zhang
The Journal of nutrition, health and aging.2023; 27(11): 960. CrossRef
- Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography (Diabetes Metab J 2023;47:104-17)
- Complications
- Non-Alcoholic Fatty Liver Disease with Sarcopenia and Carotid Plaque Progression Risk in Patients with Type 2 Diabetes Mellitus
- Yongin Cho, Hye-Sun Park, Byung Wook Huh, Yong-ho Lee, Seong Ha Seo, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, So Hun Kim
- Diabetes Metab J. 2023;47(2):232-241. Published online January 19, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0355
- 3,609 View
- 222 Download
- 1 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
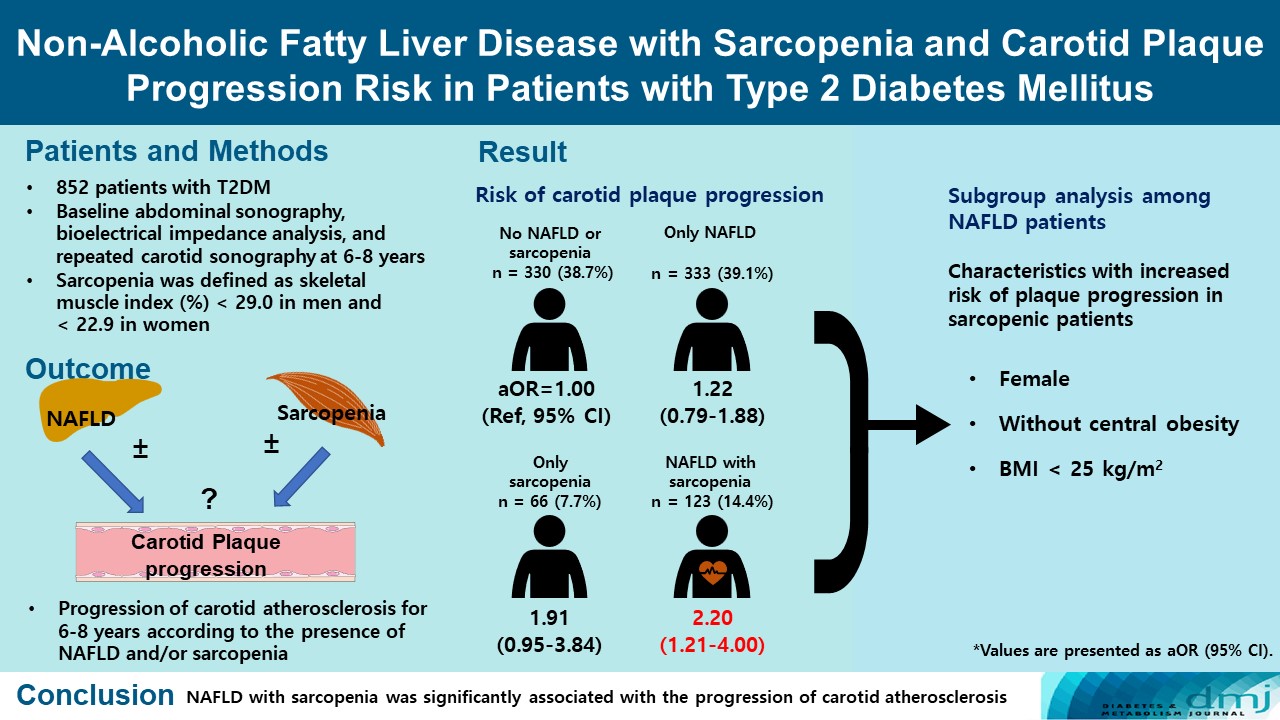
We aimed to evaluate whether non-alcoholic fatty liver disease (NAFLD) with or without sarcopenia is associated with progression of carotid atherosclerosis in patients with type 2 diabetes mellitus (T2DM).
Methods
We investigated 852 T2DM patients who underwent abdominal ultrasonography, bioelectrical impedance analysis, and carotid artery ultrasonography at baseline and repeated carotid ultrasonography after 6 to 8 years. NAFLD was confirmed by abdominal ultrasonography, and sarcopenia was defined as a sex-specific skeletal muscle mass index (SMI) value <2 standard deviations below the mean for healthy young adults. SMI was calculated by dividing the sum of appendicular skeletal mass by body weight. We investigated the association between NAFLD with or without sarcopenia and the progression of carotid atherosclerosis.
Results
Of the 852 patients, 333 (39.1%) were classified as NAFLD without sarcopenia, 66 (7.7%) were classified as sarcopenia without NAFLD, and 123 (14.4%) had NAFLD with sarcopenia at baseline. After 6 to 8 years, patients with both NAFLD and sarcopenia had a higher risk of atherosclerosis progression (adjusted odds ratio, 2.20; P<0.009) than controls without NAFLD and sarcopenia. When a subgroup analysis was performed on only patients with NAFLD, female sex, absence of central obesity, and non-obesity were significant factors related to increased risk of plaque progression risk in sarcopenic patients.
Conclusion
NAFLD with sarcopenia was significantly associated with the progression of carotid atherosclerosis in T2DM patients. -
Citations
Citations to this article as recorded by- Metabolic-associated fatty liver disease and sarcopenia: A double whammy
Aditya Viswanath, Sherouk Fouda, Cornelius James Fernandez, Joseph M Pappachan
World Journal of Hepatology.2024; 16(2): 152. CrossRef - Prevalence and outcome of sarcopenia in non-alcoholic fatty liver disease
Suprabhat Giri, Prajna Anirvan, Sumaswi Angadi, Ankita Singh, Anurag Lavekar
World Journal of Gastrointestinal Pathophysiology.2024;[Epub] CrossRef - Association of nonalcoholic fatty liver disease and carotid media‐intima thickness: A systematic review and a meta‐analysis
Manouchehr Khoshbaten, Sepideh H. Maleki, Sara Hadad, Amrit Baral, Ana V. Rocha, Laxmi Poudel, Alireza Abdshah
Health Science Reports.2023;[Epub] CrossRef - Cardiometabolic risk factors in patients with type 2 diabetes and sarcopenia
Yu. G. Samoilova, M. V. Matveeva, E. A. Khoroshunova, D. V. Podchinenova, L. L. Maksimova, G. G. Gorbach, A. B. Trivozhenko, V. A. Avkhimenko
Cardiovascular Therapy and Prevention.2023; 23(1): 3655. CrossRef
- Metabolic-associated fatty liver disease and sarcopenia: A double whammy
- Basic Research
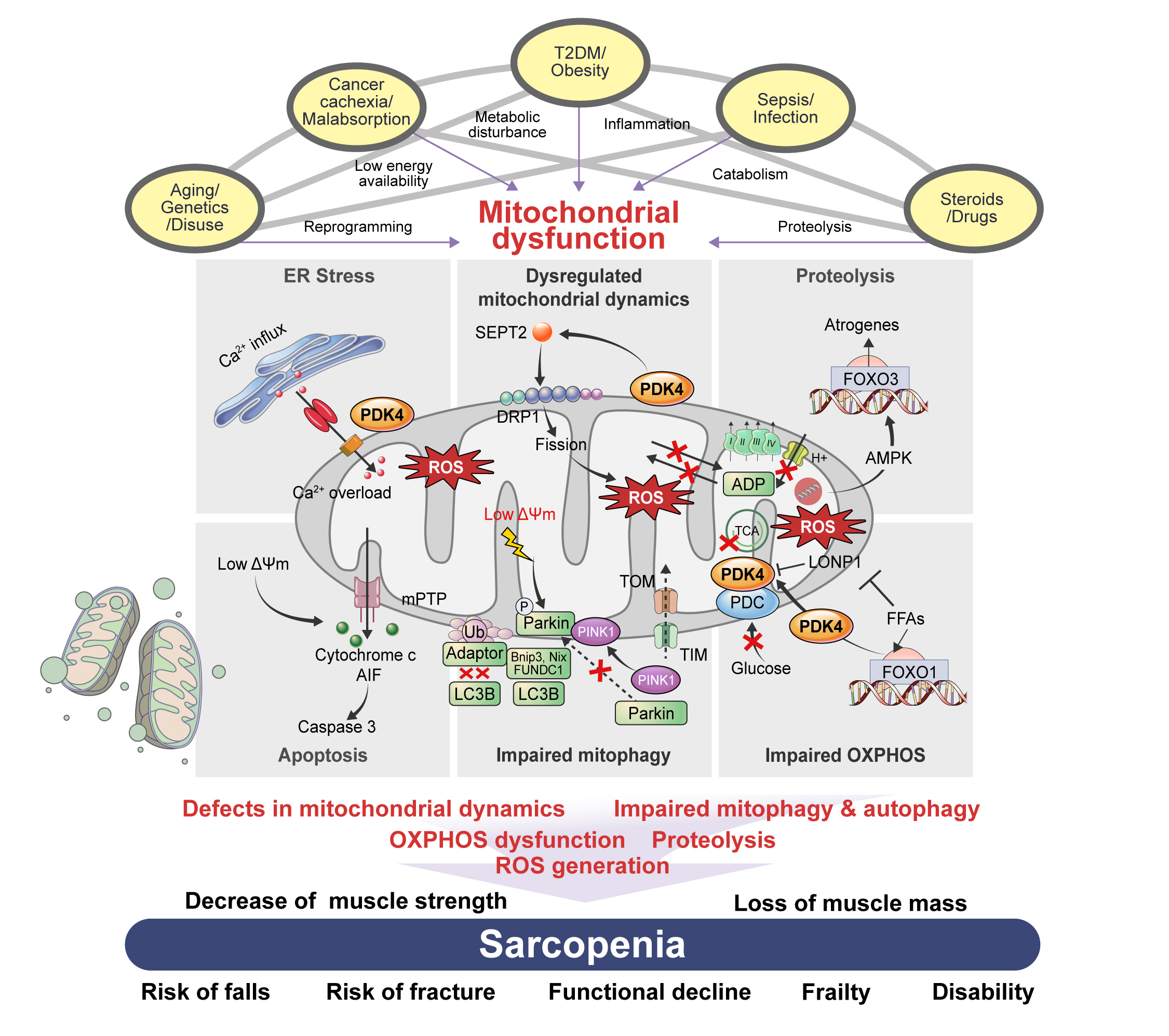
- The Link between Mitochondrial Dysfunction and Sarcopenia: An Update Focusing on the Role of Pyruvate Dehydrogenase Kinase 4
- Min-Ji Kim, Ibotombi Singh Sinam, Zerwa Siddique, Jae-Han Jeon, In-Kyu Lee
- Diabetes Metab J. 2023;47(2):153-163. Published online January 12, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0305
- 4,867 View
- 367 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Sarcopenia, defined as a progressive loss of muscle mass and function, is typified by mitochondrial dysfunction and loss of mitochondrial resilience. Sarcopenia is associated not only with aging, but also with various metabolic diseases characterized by mitochondrial dyshomeostasis. Pyruvate dehydrogenase kinases (PDKs) are mitochondrial enzymes that inhibit the pyruvate dehydrogenase complex, which controls pyruvate entry into the tricarboxylic acid cycle and the subsequent adenosine triphosphate production required for normal cellular activities. PDK4 is upregulated in mitochondrial dysfunction-related metabolic diseases, especially pathologic muscle conditions associated with enhanced muscle proteolysis and aberrant myogenesis. Increases in PDK4 are associated with perturbation of mitochondria-associated membranes and mitochondrial quality control, which are emerging as a central mechanism in the pathogenesis of metabolic disease-associated muscle atrophy. Here, we review how mitochondrial dysfunction affects sarcopenia, focusing on the role of PDK4 in mitochondrial homeostasis. We discuss the molecular mechanisms underlying the effects of PDK4 on mitochondrial dysfunction in sarcopenia and show that targeting mitochondria could be a therapeutic target for treating sarcopenia.
-
Citations
Citations to this article as recorded by- Synthesis, activatory effects, molecular docking and ADME studies as rabbit muscle pyruvate kinase activators of ureido phenyl substituted 1,4-dihydropyridine derivatives
Mustafa Oğuzhan Kaya, Tuna Demirci, Ümit Çalışır, Oğuzhan Özdemir, Yeşim Kaya, Mustafa Arslan
Research on Chemical Intermediates.2024; 50(1): 437. CrossRef - Unraveling the causes of sarcopenia: Roles of neuromuscular junction impairment and mitochondrial dysfunction
Yanmei Miao, Leiyu Xie, Jiamei Song, Xing Cai, Jinghe Yang, Xinglong Ma, Shaolin Chen, Peng Xie
Physiological Reports.2024;[Epub] CrossRef - Metabolic clues to aging: exploring the role of circulating metabolites in frailty, sarcopenia and vascular aging related traits and diseases
Zonghao Qian, Yuzhen Huang, Yucong Zhang, Ni Yang, Ziwei Fang, Cuntai Zhang, Le Zhang
Frontiers in Genetics.2024;[Epub] CrossRef - Inhibition of Pyruvate Dehydrogenase Kinase 4 Protects Cardiomyocytes from lipopolysaccharide-Induced Mitochondrial Damage by Reducing Lactate Accumulation
Tangtian Chen, Qiumin Xie, Bin Tan, Qin Yi, Han Xiang, Rui Wang, Qin Zhou, Bolin He, Jie Tian, Jing Zhu, Hao Xu
Inflammation.2024;[Epub] CrossRef - Effect of resistance training plus enriched probiotic supplement on sestrin2, oxidative stress, and mitophagy markers in elderly male Wistar rats
Majid Mohabbat, Hamid Arazi
Scientific Reports.2024;[Epub] CrossRef - Neuroprotective Effects and Therapeutic Potential of Dichloroacetate: Targeting Metabolic Disorders in Nervous System Diseases
Yue Zhang, Meiyan Sun, Hongxiang Zhao, Zhengyan Wang, Yanan Shi, Jianxin Dong, Kaifang Wang, Xi Wang, Xingyue Li, Haiyan Qi, Xiaoyong Zhao
International Journal of Nanomedicine.2023; Volume 18: 7559. CrossRef
- Synthesis, activatory effects, molecular docking and ADME studies as rabbit muscle pyruvate kinase activators of ureido phenyl substituted 1,4-dihydropyridine derivatives
- Metabolic Risk/Epidemiology
- Associations between Weight-Adjusted Waist Index and Abdominal Fat and Muscle Mass: Multi-Ethnic Study of Atherosclerosis
- Ji Yoon Kim, Jimi Choi, Chantal A. Vella, Michael H. Criqui, Matthew A. Allison, Nam Hoon Kim
- Diabetes Metab J. 2022;46(5):747-755. Published online March 30, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0294
- 5,483 View
- 256 Download
- 30 Web of Science
- 35 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The weight-adjusted waist index (WWI) reflected body compositional changes with aging. This study was to investigate the association of WWI with abdominal fat and muscle mass in a diverse race/ethnic population.
Methods
Computed tomography (CT) data from 1,946 participants for abdominal fat and muscle areas from the Multi-Ethnic Study of Atherosclerosis (785 Whites, 252 Asians, 406 African American, and 503 Hispanics) were used. Among them, 595 participants underwent repeated CT. The WWI was calculated as waist circumference (cm) divided by the square root of body weight (kg). The associations of WWI with abdominal fat and muscle measures were examined, and longitudinal changes in abdominal composition measures were compared.
Results
In all race/ethnic groups, WWI was positively correlated with total abdominal fat area (TFA), subcutaneous fat area, and visceral fat area, but negatively correlated with total abdominal muscle area (TMA) and abdominal muscle radiodensity (P<0.001 for all). WWI showed a linear increase with aging regardless of race and there were no significant differences in the WWI distribution between Whites, Asians, and African Americans. In longitudinal analyses, over 38.6 months of follow-up, all abdominal fat measures increased but muscle measures decreased, along with increase in WWI. The more the WWI increased, the more the TFA increased and the more the TMA decreased.
Conclusion
WWI showed positive associations with abdominal fat mass and negative associations with abdominal muscle mass, which likely reflects the abdominal compositional changes with aging in a multi-ethnic population. -
Citations
Citations to this article as recorded by- The association between weight-adjusted-waist index and depression: Results from NHANES 2005–2018
Meng Li, Xue Yu, Wenhui Zhang, Jiahui Yin, Lu Zhang, Guoshuai Luo, Yuanxiang Liu, Jiguo Yang
Journal of Affective Disorders.2024; 347: 299. CrossRef - Association between weight-adjusted-waist index and gallstones: an analysis of the National Health and Nutrition Examination Survey
Si-Hua Wen, Xin Tang, Tao Tang, Zheng-Rong Ye
BMC Gastroenterology.2024;[Epub] CrossRef - Association between weight-adjusted waist index and myopia in adolescents and young adults: results from NHANES 1999–2008
Xu Han Shi, Li Dong, Rui Heng Zhang, Wen Bin Wei
BMC Ophthalmology.2024;[Epub] CrossRef - Association between the weight-adjusted waist index and the odds of type 2 diabetes mellitus in United States adults: a cross-sectional study
Dongdong Zheng, Suzhen Zhao, Dan Luo, Feng Lu, Zhishen Ruan, Xiaokang Dong, Wenjing Chen
Frontiers in Endocrinology.2024;[Epub] CrossRef - Association between Weight-Adjusted Waist Index and depressive symptoms: A nationally representative cross-sectional study from NHANES 2005 to 2018
Hangyu Liu, Jin Zhi, Chuzhao Zhang, Shiyi Huang, Yang Ma, Dandan Luo, Lungang Shi
Journal of Affective Disorders.2024; 350: 49. CrossRef - Relationship between cognitive function and weight-adjusted waist index in people ≥ 60 years old in NHANES 2011–2014
Xue-li Wang, Hong-lin Feng, Xiao-zhuo Xu, Jing Liu, Xu Han
Aging Clinical and Experimental Research.2024;[Epub] CrossRef - Association between weight-adjusted waist index and non-alcoholic fatty liver disease: a population-based study
Changhui Yu, Shiming He, Maobin Kuang, Chao Wang, Xin Huang, Guotai Sheng, Yang Zou
BMC Endocrine Disorders.2024;[Epub] CrossRef - Association between weight-adjusted waist index and serum total testosterone in males aged 6–19 years in the United States: Data from NHANES 2013–2016
Zhifei Wu, Lingling Bao, Haiyan Wang, Jiajing Zheng, Yu Chen, Wenjuan Wang, Dongkai Qiu
Heliyon.2024; 10(6): e27520. CrossRef - Associations of weight-adjusted-waist index and depression with secondary infertility
Fei Sun, Min Liu, Shanshan Hu, Ruijie Xie, Huijuan Chen, Zhaona Sun, Huiya Bi
Frontiers in Endocrinology.2024;[Epub] CrossRef - Association between weight-adjusted-waist index and depression in US adults: A cross-sectional study
Yun Shen, Yahui Wu, Panru Luo, Minghan Fu, Kai Zhu, Jinsheng Wang
Journal of Affective Disorders.2024; 355: 299. CrossRef - Age differences in the association of body mass index-defined obesity with abdominal aortic calcification
Tangmeng Guo, Lili Huang, Zhijian Luo, Huabo Zheng, Shengshuai Shan, Bei Cheng
Frontiers in Endocrinology.2024;[Epub] CrossRef - The relationship between weight-adjusted-waist index and diabetic kidney disease in patients with type 2 diabetes mellitus
Zhaoxiang Wang, Xuejing Shao, Wei Xu, Bingshuang Xue, Shao Zhong, Qichao Yang
Frontiers in Endocrinology.2024;[Epub] CrossRef - Assessment of existing anthropometric indices for screening sarcopenic obesity in older adults
Jin Eui Kim, Jimi Choi, Miji Kim, Chang Won Won
British Journal of Nutrition.2023; 129(5): 875. CrossRef - Relationship Between Weight-Adjusted Waist Index and Osteoporosis in the Senile in the United States from the National Health and Nutrition Examination Survey, 2017-2020
Yuxiang Lin, Zijie Liang, Anxin Zhang, Nuo Xu, Xuewen Pei, Nanbu Wang, Liang Zheng, Danghan Xu
Journal of Clinical Densitometry.2023; 26(2): 101361. CrossRef - The association of asthma duration with body mass index and Weight-Adjusted-Waist index in a nationwide study of the U.S. adults
Xiaoxiao Han, Xiaofang He, Gui Hao, Lifang Cao, Yinliang Qi, Kexing Han
European Journal of Medical Research.2023;[Epub] CrossRef - Relationship between weight-adjusted-waist index and erectile dysfunction in the United State: results from NHANES 2001-2004
Shangqi Cao, Xu Hu, Yanxiang Shao, Yaohui Wang, Yaxiong Tang, Shangqing Ren, Xiang Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - The association between weight-adjusted-waist index and total bone mineral density in adolescents: NHANES 2011–2018
Xiaohua Wang, Shuo Yang, Gansheng He, Lin Xie
Frontiers in Endocrinology.2023;[Epub] CrossRef - Asthma prevalence is increased in patients with high metabolism scores for visceral fat: study reports from the US
Qiushi Liu, Xiaoxiao Han, Yan Chen, Ying Gao, Wei Yang, Lewei Huang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Positive association between weight-adjusted-waist index and dementia in the Chinese population with hypertension: a cross-sectional study
Wei Zhou, Yanyou Xie, Lingling Yu, Chao Yu, Huihui Bao, Xiaoshu Cheng
BMC Psychiatry.2023;[Epub] CrossRef - Associations between weight-adjusted waist index and bone mineral density: results of a nationwide survey
Ya Zhang, Haiyang Wu, Cheng Li, Changxiong Liu, Mingjiang Liu, Xiaozhu Liu, Qiming Yin, Xianzhe Li, Ruijie Xie
BMC Endocrine Disorders.2023;[Epub] CrossRef - Association of weight-adjusted-waist index with non-alcoholic fatty liver disease and liver fibrosis: a cross-sectional study based on NHANES
Qinggang Hu, Kexing Han, Jiapei Shen, Weijie Sun, Long Gao, Yufeng Gao
European Journal of Medical Research.2023;[Epub] CrossRef - Weight‐adjusted waist as an integrated index for fat, muscle and bone health in adults
Kyoung Jin Kim, Serhim Son, Kyeong Jin Kim, Sin Gon Kim, Nam Hoon Kim
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(5): 2196. CrossRef - Association between weight-adjusted-waist index and female infertility: a population-based study
Zujun Wen, Xiang Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association between weight-adjusted-waist index and risk of cardiovascular diseases in United States adults: a cross-sectional study
Haiyang Fang, Feng Xie, Kai Li, Meng Li, Yanqing Wu
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Association between the weight-adjusted waist index and stroke: a cross-sectional study
Jiayi Ye, Yanjie Hu, Xinrong Chen, Zhe Yin, Xingzhu Yuan, Liping Huang, Ka Li
BMC Public Health.2023;[Epub] CrossRef - Association between weight-adjusted-waist index and chronic kidney disease: a cross-sectional study
Xiaowan Li, Lanyu Wang, Hongyi Zhou, Hongyang Xu
BMC Nephrology.2023;[Epub] CrossRef - Sex Differences in the Association of Weight-Adjusted-Waist Index with Sarcopenic Obesity: A Cross-Sectional Study of Hemodialysis Patients
Maolu Tian, Qin Lan, Fangfang Yu, Pinghong He, Shanshan Hu, Yan Zha
Metabolic Syndrome and Related Disorders.2023; 21(10): 596. CrossRef - Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
Eugene Han, Yong-ho Lee
Clinical and Molecular Hepatology.2023; 29(4): 980. CrossRef - The association of body mass index and weight waist adjustment index with serum ferritin in a national study of US adults
Hao Han, Ping Ni, Siqi Zhang, Xiaojuan Ji, Mingli Zhu, Wanyu Ma, Hongfeng Ge, Hailiang Chu
European Journal of Medical Research.2023;[Epub] CrossRef - The weight-adjusted-waist index and cognitive impairment among U.S. older adults: a population-based study
Xiao-tong Huang, Xiang Lv, Hong Jiang
Frontiers in Endocrinology.2023;[Epub] CrossRef - The relationship between weight-adjusted-waist index and total bone mineral density in adults aged 20-59
Meiqian Guo, Yi Lei, Xueqing Liu, Xiang Li, Yong Xu, Donghui Zheng
Frontiers in Endocrinology.2023;[Epub] CrossRef - Associations between weight-adjusted-waist index and infertility: Results from NHANES 2013 to 2020
Huanxin Zhong, Bin Yu, Fen Zhao, Hongyin Cui, Lifang You, Dao Feng, Yi Lu
Medicine.2023; 102(48): e36388. CrossRef - The association between weight-adjusted-waist index and increased urinary albumin excretion in adults: A population-based study
Zheng Qin, Kaixi Chang, Qinbo Yang, Qiao Yu, Ruoxi Liao, Baihai Su
Frontiers in Nutrition.2022;[Epub] CrossRef - Association between the weight-adjusted-waist index and abdominal aortic calcification in United States adults: Results from the national health and nutrition examination survey 2013–2014
Feng Xie, Yuan Xiao, Xiaozhong Li, Yanqing Wu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - The association between weight-adjusted-waist index and abdominal aortic calcification in adults aged ≥ 40 years: results from NHANES 2013–2014
Zheng Qin, Dongru Du, Yupei Li, Kaixi Chang, Qinbo Yang, Zhuyun Zhang, Ruoxi Liao, Baihai Su
Scientific Reports.2022;[Epub] CrossRef
- The association between weight-adjusted-waist index and depression: Results from NHANES 2005–2018
- Metabolic Risk/Epidemiology
-
- Effect of Sarcopenia and Body Shape on Cardiovascular Disease According to Obesity Phenotypes
- Hyun-Woong Cho, Wankyo Chung, Shinje Moon, Ohk-Hyun Ryu, Min Kyung Kim, Jun Goo Kang
- Diabetes Metab J. 2021;45(2):209-218. Published online July 10, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0223

- 8,316 View
- 212 Download
- 21 Web of Science
- 20 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub Background This study aimed to assess the effects of sarcopenia and A Body Shape Index (ABSI) on cardiovascular disease (CVD) risk according to obesity phenotypes.
Methods We used data from the National Health and Nutrition Examination Survey 1999 to 2012. A total of 25,270 adults were included and classified into the following groups: metabolically healthy normal weight (MHNW), metabolically healthy overweight/obese (MHO), metabolically unhealthy normal weight (MUNW), and metabolically unhealthy overweight/obese (MUO). Sarcopenia was defined as the appendicular skeletal mass index <7 kg/m2 in men and <5.5kg/m2 in women. A multivariate logistic regression analysis was performed to evaluate the odds ratio (OR) of sarcopenia and ABSI for CVD events according to the obesity phenotype.
Results The MHNW participants with sarcopenia had higher risk for CVD than those without sarcopenia (OR, 2.69; 95% confidence interval [CI], 1.56 to 4.64). In the analysis with MHNW participants without sarcopenia as a reference, the participants with sarcopenia showed a higher OR for CVD than those without sarcopenia in both MHO (OR in participants without sarcopenia, 3.31; 95% CI, 1.94 to 5.64) (OR in participants with sarcopenia, 8.59; 95% CI, 2.63 to 28.04) and MUO participants (OR in participants without sarcopenia, 5.11; 95% CI, 3.21 to 8.15) (OR in participants with sarcopenia, 8.12; 95% CI, 4.04 to 16.32). Participants within the second and third tertiles of ABSI had higher ORs for CVDs than the counterpart of obesity phenotypes within the first tertile.
Conclusion These results suggest that clinical approaches that consider muscle and body shape are required.
-
Citations
Citations to this article as recorded by- Association of low muscle mass and obesity with increased all‐cause and cardiovascular disease mortality in US adults
Donghyun Kim, Junghoon Lee, Raekil Park, Chang‐Myung Oh, Shinje Moon
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(1): 240. CrossRef - Metabolic-associated fatty liver disease and sarcopenia: A double whammy
Aditya Viswanath, Sherouk Fouda, Cornelius James Fernandez, Joseph M Pappachan
World Journal of Hepatology.2024; 16(2): 152. CrossRef - Association of Myosteatosis with Nonalcoholic Fatty Liver Disease, Severity, and Liver Fibrosis Using Visual Muscular Quality Map in Computed Tomography
Hwi Seung Kim, Jiwoo Lee, Eun Hee Kim, Min Jung Lee, In Young Bae, Woo Je Lee, Joong-Yeol Park, Hong-Kyu Kim, Chang Hee Jung
Diabetes & Metabolism Journal.2023; 47(1): 104. CrossRef - Additive impact of diabetes and sarcopenia on all-cause and cardiovascular mortality: A longitudinal nationwide population-based study
Eyun Song, Soon Young Hwang, Min Jeong Park, Ahreum Jang, Kyeong Jin Kim, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Metabolism.2023; 148: 155678. CrossRef - Association between a body shape index and abdominal aortic calcification in general population: A cross-sectional study
Wei Li, Zhenwei Wang, Min Li, Jing Xie, Jing Gong, Naifeng Liu
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Metabolic Impact of Frailty Changes Diabetes Trajectory
Alan J. Sinclair, Ahmed H. Abdelhafiz
Metabolites.2023; 13(2): 295. CrossRef - Association between sarcopenic obesity and poor muscle quality based on muscle quality map and abdominal computed tomography
Yun Kyung Cho, Han Na Jung, Eun Hee Kim, Min Jung Lee, Joong‐Yeol Park, Woo Je Lee, Hong‐Kyu Kim, Chang Hee Jung
Obesity.2023; 31(6): 1547. CrossRef - Metabolic Characteristics of Frail Older People with Diabetes Mellitus—A Systematic Search for Phenotypes
Ahmed H. Abdelhafiz, Grace L. Keegan, Alan J. Sinclair
Metabolites.2023; 13(6): 705. CrossRef - Risk of Cardiovascular Diseases Among Different Metabolic Obesity Phenotypes: A Prospective Observational Study
Xiaowei Liu, Chan Yang, Yuanyuan Dang, Zhenqi Chang, Juan Li, Yi Zhao, Yuhong Zhang
Metabolic Syndrome and Related Disorders.2023; 21(6): 306. CrossRef - Effect of Hypoxia Conditioning on Body Composition in Middle-Aged and Older Adults: A Systematic Review and Meta-Analysis
Zhijian He, Lijun Qiang, Yusheng Liu, Wenfeng Gao, Tao Feng, Yang Li, Bing Yan, Olivier Girard
Sports Medicine - Open.2023;[Epub] CrossRef - Association Between a Body Shape Index and Subclinical Carotid Atherosclerosis in Population Free of Cardiovascular and Cerebrovascular Diseases
Xiaotian Ma, Lihong Chen, Wenchao Hu, Lanjie He
Journal of Atherosclerosis and Thrombosis.2022; 29(8): 1140. CrossRef - Impact of Sarcopenia on the Severity of the Liver Damage in Patients With Non-alcoholic Fatty Liver Disease
Vittoria Zambon Azevedo, Cristina Alina Silaghi, Thomas Maurel, Horatiu Silaghi, Vlad Ratziu, Raluca Pais
Frontiers in Nutrition.2022;[Epub] CrossRef - Identification of sarcopenic obesity in adults undergoing orthopaedic surgery: Relationship between “a body shape index” (ABSI) and fat-free mass. A cross -sectional study
Ana Tomažič, Boštjan Žvanut, Lilijana Vouk Grbac, Mihaela Jurdana, Fatih Özden
PLOS ONE.2022; 17(6): e0269956. CrossRef - Associations of Dynapenic Obesity and Sarcopenic Obesity with the Risk of Complications in COVID-19
Laura Pérez-Campos Mayoral, Carlos Alberto Matias-Cervantes, Eduardo Pérez-Campos, Carlos Romero Díaz, Luis Ángel Laguna Barrios, María del Socorro Pina Canseco, Margarito Martínez Cruz, Eduardo Pérez-Campos Mayoral, Carlos Josué Solórzano Mata, Francisco
International Journal of Molecular Sciences.2022; 23(15): 8277. CrossRef - Sex Differences in Adiposity and Cardiovascular Diseases
Haoyun Li, Daniels Konja, Luyao Wang, Yu Wang
International Journal of Molecular Sciences.2022; 23(16): 9338. CrossRef - The Applicability of the ESPEN and EASO-Defined Diagnostic Criteria for Sarcopenic Obesity in Japanese Patients after Stroke: Prevalence and Association with Outcomes
Yoshihiro Yoshimura, Hidetaka Wakabayashi, Fumihiko Nagano, Ayaka Matsumoto, Sayuri Shimazu, Ai Shiraishi, Yoshifumi Kido, Takahiro Bise
Nutrients.2022; 14(19): 4205. CrossRef - The value of combining the simple anthropometric obesity parameters, Body Mass Index (BMI) and a Body Shape Index (ABSI), to assess the risk of non-alcoholic fatty liver disease
Maobin Kuang, Guotai Sheng, Chong Hu, Song Lu, Nan Peng, Yang Zou
Lipids in Health and Disease.2022;[Epub] CrossRef - Sarcopenia and cardiovascular disease in patients with and without kidney disease: what do we know?
Ozkan Gungor, Mustafa Sevinc, Sena Ulu, Ismail Kocyigit
International Urology and Nephrology.2022; 55(5): 1161. CrossRef - Skeletal Muscle Should Not Be Overlooked
Ji A Seo
Diabetes & Metabolism Journal.2021; 45(2): 173. CrossRef - The Role of Sarcopenic Obesity in Cancer and Cardiovascular Disease: A Synthesis of the Evidence on Pathophysiological Aspects and Clinical Implications
Erika Aparecida Silveira, Rômulo Roosevelt da Silva Filho, Maria Claudia Bernardes Spexoto, Fahimeh Haghighatdoost, Nizal Sarrafzadegan, Cesar de Oliveira
International Journal of Molecular Sciences.2021; 22(9): 4339. CrossRef
- Association of low muscle mass and obesity with increased all‐cause and cardiovascular disease mortality in US adults
- Metabolic Risk/Epidemiology
- Association between the Thigh Muscle and Insulin Resistance According to Body Mass Index in Middle-Aged Korean Adults
- Ji Eun Heo, Jee-Seon Shim, Hokyou Lee, Hyeon Chang Kim
- Diabetes Metab J. 2020;44(3):446-457. Published online April 16, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0110
- 6,743 View
- 89 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We examined the associations between thigh muscle area (TMA) and insulin resistance (IR) according to body mass index (BMI) in middle-aged Korean general population.
Methods TMA was measured using quantitative computed tomography and corrected by body weight (TMA/Wt) in 1,263 men, 788 premenopausal women, and 1,476 postmenopausal women all aged 30 to 64 years. The tertiles of TMA/Wt were calculated separately for men and for premenopausal and postmenopausal women. Homeostatic model assessment for insulin resistance (HOMA-IR) was performed using fasting blood glucose and insulin levels, and increased IR was defined according to sex-specific, top quartiles of HOMA-IR. Associations between the TMA/Wt tertiles and increased IR according to the BMI categories (<25 and ≥25 kg/m2) were assessed using multivariable logistic regression analysis.
Results In men with higher BMIs, but not in those with lower BMIs, the presence of an increased IR had significantly higher odds ratios in the lower TMA/Wt tertiles, even after adjustment for visceral fat area. However, in premenopausal and postmenopausal women, there was no significant inverse association between TMA/Wt tertiles and increased IR, regardless of BMI category.
Conclusion Our findings suggest that the thigh muscle is inversely associated with IR in men, particularly in those with higher BMIs.
-
Citations
Citations to this article as recorded by- Risk of sleep apnea associated with higher blood pressure among Chinese and Korean Americans
Brittany N. Morey, Yuxi Shi, Soomin Ryu, Susan Redline, Ichiro Kawachi, Hye Won Park, Sunmin Lee
Ethnicity & Health.2024; 29(3): 295. CrossRef - Sex-specific equations to estimate body composition: Derivation and validation of diagnostic prediction models using UK Biobank
Yueqi Lu, Ying Shan, Liang Dai, Xiaosen Jiang, Congying Song, Bangwei Chen, Jingwen Zhang, Jing Li, Yue Zhang, Junjie Xu, Tao Li, Zuying Xiong, Yong Bai, Xiaoyan Huang
Clinical Nutrition.2023; 42(4): 511. CrossRef - Gender Differences in Relation to Body Composition, Insulin Resistance, and Islet Beta Cell Function in Newly Diagnosed Diabetic or Pre-Diabetic Patients
Minglei Ma, Tao Jiang, Zhen Wen, Dongxue Zhang, Lei Xiu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 723. CrossRef - Non-Alcoholic Fatty Liver Disease with Sarcopenia and Carotid Plaque Progression Risk in Patients with Type 2 Diabetes Mellitus
Yongin Cho, Hye-Sun Park, Byung Wook Huh, Yong-ho Lee, Seong Ha Seo, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes & Metabolism Journal.2023; 47(2): 232. CrossRef - Prospective External Validation of an Algorithm Predicting Hourly
Basal Insulin Infusion Rates from Characteristics of Patients with Type 1
Diabetes Treated with Insulin Pumps
Jana S. Schmelzer, Melanie Kahle-Stephan, Juris J. Meier, Michael A. Nauck
Experimental and Clinical Endocrinology & Diabetes.2023; 131(10): 539. CrossRef - Establishing reference values for percentage of appendicular skeletal muscle mass and their association with metabolic syndrome in Korean adolescents
Da Hye Lee, Sung-Chan Kang, Seung-Sik Hwang, Yun Jeong Lee, Hwa Young Kim, Seong Yong Lee, Choong Ho Shin, Jaehyun Kim
Annals of Pediatric Endocrinology & Metabolism.2023; 28(4): 237. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Association between Lower-to-Upper Ratio of Appendicular Skeletal Muscle and Metabolic Syndrome
Hyun Eui Moon, Tae Sic Lee, Tae-Ha Chung
Journal of Clinical Medicine.2022; 11(21): 6309. CrossRef
- Risk of sleep apnea associated with higher blood pressure among Chinese and Korean Americans
- Lifesytle
- Combined Aerobic and Resistance Exercise Training Reduces Circulating Apolipoprotein J Levels and Improves Insulin Resistance in Postmenopausal Diabetic Women
- Yun Kyung Jeon, Sang Soo Kim, Jong Ho Kim, Hyun Jeong Kim, Hyun Jun Kim, Jang Jun Park, Yuen Suk Cho, So Hee Joung, Ji Ryang Kim, Bo Hyun Kim, Sang Heon Song, In Joo Kim, Yong Ki Kim, Young-Bum Kim
- Diabetes Metab J. 2020;44(1):103-112. Published online February 21, 2020
- DOI: https://doi.org/10.4093/dmj.2018.0160
- 8,468 View
- 152 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Circulating apolipoprotein J (ApoJ) is closely associated with insulin resistance; however, the effect of exercise on circulating ApoJ levels and the association of ApoJ with metabolic indices remain unknown. Here, we investigated whether a combined exercise can alter the circulating ApoJ level, and whether these changes are associated with metabolic indices in patients with type 2 diabetes mellitus.
Methods Postmenopausal women with type 2 diabetes mellitus were randomly assigned into either an exercise (EXE,
n =30) or control (CON,n =15) group. Participants in the EXE group were enrolled in a 12-week program consisting of a combination of aerobic and resistance exercises. At baseline, 4, 8, and 12 weeks, body composition and metabolic parameters including homeostatic model assessment of insulin resistance (HOMA-IR) and serum ApoJ levels were assessed.Results In the EXE group, ApoJ levels decreased 26.3% and 19.4%, relative to baseline, at 8 and 12 weeks, respectively. Between-group differences were significant at 8 and 12 weeks (
P <0.05 andP <0.001, respectively). In the EXE group, 12 weeks of exercise resulted in significant decreases in body weight, percent body fat, and HOMA-IR indices. Concurrently, weight-adjusted appendicular skeletal muscle mass (ASM/wt) was increased in the EXE group compared with the CON group. Importantly, changes in the ApoJ level were significantly correlated with changes in ASM/wt.Conclusion Exercise training resulted in a significant decrease in the circulating ApoJ level, with changes in ApoJ associated with an improvement in some insulin resistance indices. These data suggest that circulating ApoJ may be a useful metabolic marker for assessing the effects of exercise on insulin resistance.
-
Citations
Citations to this article as recorded by- The function of previously unappreciated exerkines secreted by muscle in regulation of neurodegenerative diseases
Xuepeng Bian, Qian Wang, Yibing Wang, Shujie Lou
Frontiers in Molecular Neuroscience.2024;[Epub] CrossRef - Exercise modalities for type 2 diabetes: A systematic review and network meta‐analysis of randomized trials
Liangying Hou, Qi Wang, Bei Pan, Rui Li, Yanfei Li, Juanjuan He, Tianzhu Qin, Liujiao Cao, Na Zhang, Changhao Cao, Long Ge, Kehu Yang
Diabetes/Metabolism Research and Reviews.2023;[Epub] CrossRef - Estimating the Effect of Aerobic Exercise Training on Novel Lipid Biomarkers: A Systematic Review and Multivariate Meta-Analysis of Randomized Controlled Trials
Gina Wood, Emily Taylor, Vanessa Ng, Anna Murrell, Aditya Patil, Tom van der Touw, Mitch Wolden, Nick Andronicos, Neil A. Smart
Sports Medicine.2023; 53(4): 871. CrossRef - 2023 update on Italian guidelines for the treatment of type 2 diabetes
Edoardo Mannucci, Riccardo Candido, Lina delle Monache, Marco Gallo, Andrea Giaccari, Maria Luisa Masini, Angela Mazzone, Gerardo Medea, Basilio Pintaudi, Giovanni Targher, Marina Trento, Giuseppe Turchetti, Valentina Lorenzoni, Matteo Monami
Acta Diabetologica.2023; 60(8): 1119. CrossRef - The Effect of Eight Weeks of Concurrent Training on Serum Levels of Paraxonase-1, Irisin, Lipid Profile, and Insulin Resistance in Men With Metabolic Syndrome
Seyed Amir Hosain Diba Hosaini, Morvarid Vafaee, Bahram Abedi
Hormozgan Medical Journal.2023; 27(1): 43. CrossRef - An Overview of the TRP-Oxidative Stress Axis in Metabolic Syndrome: Insights for Novel Therapeutic Approaches
Mizael C. Araújo, Suzany H. S. Soczek, Jaqueline P. Pontes, Leonardo A. C. Marques, Gabriela S. Santos, Gisele Simão, Laryssa R. Bueno, Daniele Maria-Ferreira, Marcelo N. Muscará, Elizabeth S. Fernandes
Cells.2022; 11(8): 1292. CrossRef - Effect of Yijinjing combined with elastic band exercise on muscle mass and function in middle-aged and elderly patients with prediabetes: A randomized controlled trial
Yunda Huang, Junhua Han, Qing Gu, Yanwei Cai, Jingyuan Li, Shasha Wang, Suijun Wang, Ru Wang, Xiangyun Liu
Frontiers in Medicine.2022;[Epub] CrossRef - Effect of combined aerobic and resistance exercise on blood pressure in postmenopausal women: A systematic review and meta-analysis of randomized controlled trials
Huihui Xi, Yayu He, Yirou Niu, Xin Sui, Jun Zhang, Ruiting Zhu, Haiyan Xu, Shuang Zhang, Yang Li, Yuan Yuan, Lirong Guo
Experimental Gerontology.2021; 155: 111560. CrossRef - Effects of Augmented-Reality-Based Exercise on Muscle Parameters, Physical Performance, and Exercise Self-Efficacy for Older Adults
Sangwan Jeon, Jiyoun Kim
International Journal of Environmental Research and Public Health.2020; 17(9): 3260. CrossRef - Apolipoprotein J is a hepatokine regulating muscle glucose metabolism and insulin sensitivity
Ji A Seo, Min-Cheol Kang, Won-Mo Yang, Won Min Hwang, Sang Soo Kim, Soo Hyun Hong, Jee-In Heo, Achana Vijyakumar, Leandro Pereira de Moura, Aykut Uner, Hu Huang, Seung Hwan Lee, Inês S. Lima, Kyong Soo Park, Min Seon Kim, Yossi Dagon, Thomas E. Willnow, V
Nature Communications.2020;[Epub] CrossRef - Impact of Skeletal Muscle Mass on Metabolic Health
Gyuri Kim, Jae Hyeon Kim
Endocrinology and Metabolism.2020; 35(1): 1. CrossRef - Habitual Combined Exercise Protects against Age-Associated Decline in Vascular Function and Lipid Profiles in Elderly Postmenopausal Women
Elizabeth J. Pekas, John Shin, Won-Mok Son, Ronald J. Headid, Song-Young Park
International Journal of Environmental Research and Public Health.2020; 17(11): 3893. CrossRef
- The function of previously unappreciated exerkines secreted by muscle in regulation of neurodegenerative diseases
- Epidemiology
- Lower Leg Fat Depots Are Associated with Albuminuria Independently of Obesity, Insulin Resistance, and Metabolic Syndrome (Korea National Health and Nutrition Examination Surveys 2008 to 2011)
- Eugene Han, Nan Hee Cho, Mi Kyung Kim, Hye Soon Kim
- Diabetes Metab J. 2019;43(4):461-473. Published online March 7, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0081
- 5,004 View
- 39 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Although the involvement of obesity in metabolic disorders is well known, leg fat depot influences on albuminuria have not been determined.
Methods This population-based, cross-sectional study used a nationally representative sample of 2,076 subjects aged ≥20 years from the Korea National Health and Nutrition Examination Surveys of 2008 to 2011. The ratio of leg fat to total fat (LF/TF ratio) was assessed by dual X-ray absorptiometry, and albuminuria was defined as more than one positive dipstick test or an albumin-to-creatinine ratio of ≥30 mg/g.
Results Individuals whose LF/TF ratio was in the lowest tertile showed a higher proportion of albuminuria than those in the highest tertile (odds ratio [OR], 2.82; 95% confidence interval [CI], 2.01 to 3.96;
P <0.001). This association was observed in both sexes, all age groups, and all subgroups stratified by body mass index, waist circumference, homeostasis model assessments of insulin resistance, and the presence of metabolic syndrome (all,P <0.05). Multiple logistic regression analyses also demonstrated that the lowest LF/TF ratio was independently associated with albuminuria risk (OR, 1.55 to 2.16; all,P <0.05). In addition, the risk of albuminuria was higher in sarcopenic individuals with lower LF/TF ratios than in the highest LF/TF ratio subjects without sarcopenia (OR, 3.73; 95% CI, 2.26 to 6.13).Conclusion A lower LF/TF ratio was associated with an increased risk of albuminuria independent of obesity, insulin resistance, and metabolic syndrome, and when combined with sarcopenia, the albuminuria risk synergistically increased. Hence, our findings may have implications to improve risk stratification and recommendations on body fat distribution in the general population.
-
Citations
Citations to this article as recorded by- Efficacy and safety of evogliptin in patients with type 2 diabetes and non‐alcoholic fatty liver disease: A multicentre, double‐blind, randomized, comparative trial
Eugene Han, Ji Hye Huh, Eun Y. Lee, Ji C. Bae, Sung W. Chun, Sung H. Yu, Soo H. Kwak, Kyong S. Park, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(4): 752. CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef
- Efficacy and safety of evogliptin in patients with type 2 diabetes and non‐alcoholic fatty liver disease: A multicentre, double‐blind, randomized, comparative trial
- Epidemiology
- Are We in the Same Risk of Diabetes Mellitus? Gender- and Age-Specific Epidemiology of Diabetes in 2001 to 2014 in the Korean Population
- Bo Kyung Koo, Min Kyong Moon
- Diabetes Metab J. 2016;40(3):175-181. Published online May 24, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.175
- 4,348 View
- 38 Download
- 19 Web of Science
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader In the early 2000s, the prevalence of diabetes in adults aged ≥30 years in Korea was about 9% to 10%, and it remained stable. However, a nationwide survey showed that this prevalence increased over the past few years. After age-standardization using the Korean population of the year 2010, the prevalence of diabetes in adults aged ≥30 years was 10.0% to 10.8% between 2001 and 2012, which increased to 12.5% in 2013 and 11.6% in 2014. During that period, there have been changes in the gender- and age-specific prevalence of diabetes in Korean adults. The prevalence of diabetes in the elderly population increased significantly, while this prevalence in young adults, especially in young women, did not change significantly. The contribution of each diabetic risk factor, such as obesity, β-cell dysfunction, sarcopenia, and socioeconomic status, in developing diabetes has also changed during that period in each gender and age group. For young women, obesity was the most important risk factor; by contrast, for elderly diabetic patients, sarcopenia was more important than obesity as a risk factor. Considering the economic burden of diabetes and its associated comorbidities, a public health policy targeting the major risk factors in each population might be more effective in preventing diabetes.
-
Citations
Citations to this article as recorded by- Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
Eun-Gyoung Hong, Kyung-Wan Min, Jung Soo Lim, Kyu-Jeung Ahn, Chul Woo Ahn, Jae-Myung Yu, Hye Soon Kim, Hyun Jin Kim, Won Kim, Dong Han Kim, Hak Chul Jang
Advances in Therapy.2024;[Epub] CrossRef - Plasma glucose levels and diabetes are independent predictors for mortality in patients with COVID-19
Hui Long, Jiachen Li, Rui Li, Haiyang Zhang, Honghan Ge, Hui Zeng, Xi Chen, Qingbin Lu, Wanli Jiang, Haolong Zeng, Tianle Che, Xiaolei Ye, Liqun Fang, Ying Qin, Qiang Wang, Qingming Wu, Hao Li, Wei Liu
Epidemiology and Infection.2022;[Epub] CrossRef - Type 2 Diabetes Mellitus with Early Dry Skin Disorder: A Comparison Study Between Primary and Tertiary Care in Indonesia
Lili Legiawati, Kusmarinah Bramono, Wresti Indriatmi, Em Yunir, Aditya Indra Pratama
Current Diabetes Reviews.2022;[Epub] CrossRef - Physical Comorbidity According to Diagnoses and Sex among Psychiatric Inpatients in South Korea
Suin Park, Go-Un Kim, Hyunlye Kim
International Journal of Environmental Research and Public Health.2021; 18(8): 4187. CrossRef - Muscle strength, an independent determinant of glycemic control in older adults with long-standing type 2 diabetes: a prospective cohort study
Bo Kyung Koo, Seoil Moon, Min Kyong Moon
BMC Geriatrics.2021;[Epub] CrossRef - Site-specific cancer risk in patients with type 2 diabetes: a nationwide population-based cohort study in Korea
Suk Kyeong Kim, Ju-Young Jang, Dong-Lim Kim, Young A Rhyu, Suh Eun Lee, Seung-Hyun Ko, Kyungdo Han, Kee-Ho Song
The Korean Journal of Internal Medicine.2020; 35(3): 641. CrossRef - Hypoglycemic efficacy and safety of Momordica charantia (bitter melon) in patients with type 2 diabetes mellitus
Soo Kyoung Kim, Jaehoon Jung, Jung Hwa Jung, NalAe Yoon, Sang Soo Kang, Gu Seob Roh, Jong Ryeal Hahm
Complementary Therapies in Medicine.2020; 52: 102524. CrossRef - Taking metformin and cognitive function change in older patients with diabetes
Bo Kyung Koo, Lee‐Kyung Kim, Jun‐Young Lee, Min Kyong Moon
Geriatrics & Gerontology International.2019; 19(8): 755. CrossRef - Trends in Diabetes Prevalence, Awareness, Treatment and Control in Yangon Region, Myanmar, Between 2004 and 2014, Two Cross-Sectional Studies
Wai Phyo Aung, Espen Bjertness, Aung Soe Htet, Hein Stigum, Marte Karoline Råberg Kjøllesdal
International Journal of Environmental Research and Public Health.2019; 16(18): 3461. CrossRef - Validity of Japanese version of SARC‐F questionnaire in patients with chronic liver disease
Satoshi Ida, Yuji Kojima, Shima Hamaoka, Naohito Urawa, Jun Araki, Ryutaro Kaneko, Kazuya Murata
Journal of Gastroenterology and Hepatology.2019; 34(5): 947. CrossRef - Letter: Projection of Diabetes Prevalence in Korean Adults for the Year 2030 Using Risk Factors Identified from National Data (Diabetes Metab J 2019;43:90–6)
Bo Kyung Koo
Diabetes & Metabolism Journal.2019; 43(2): 242. CrossRef - Antidiabetic Effects of Vigna nakashimae Extract in Humans: A Preliminary Study
Soo Kyoung Kim, Jaehoon Jung, Jung Hwa Jung, Byong Won Lee, Sang Soo Kang, Gu Seob Roh, Jong Ryeal Hahm
The Journal of Alternative and Complementary Medicine.2018; 24(3): 249. CrossRef - Serum Betatrophin Concentrations and the Risk of Incident Diabetes: A Nested Case-Control Study from Chungju Metabolic Disease Cohort
Seung-Hwan Lee, Marie Rhee, Hyuk-Sang Kwon, Yong-Moon Park, Kun-Ho Yoon
Diabetes & Metabolism Journal.2018; 42(1): 53. CrossRef - Relationship between age and cardiometabolic index in Japanese men and women
Ichiro Wakabayashi
Obesity Research & Clinical Practice.2018; 12(4): 372. CrossRef - Kidney transplantation in patients with diabetes: better than nothing
Chang Seong Kim
The Korean Journal of Internal Medicine.2018; 33(2): 293. CrossRef - The Changes of Macular Microvasculature and Related Systemic Parameters in Diabetic Patients without Diabetic Retinopathy
Sang Wook Choi, Joon Hee Cho, Ha Kyung Kim, So Hyun Bae
Journal of the Korean Ophthalmological Society.2017; 58(7): 811. CrossRef - Dietary total, animal, vegetable calcium and type 2 diabetes incidence among Korean adults: The Korean Multi-Rural Communities Cohort (MRCohort)
J.M. Oh, H.W. Woo, M.K. Kim, Y.-H. Lee, D.H. Shin, M.-H. Shin, B.Y. Choi
Nutrition, Metabolism and Cardiovascular Diseases.2017; 27(12): 1152. CrossRef - The Influence of Prenatal Exercise on Offspring Health: A Review
Carmen Moyer, Olga Roldan Reoyo, Linda May
Clinical Medicine Insights: Women's Health.2016; 9: CMWH.S34670. CrossRef
- Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
- Clinical Care/Education
- Sarcopenia, Frailty, and Diabetes in Older Adults
- Hak Chul Jang
- Diabetes Metab J. 2016;40(3):182-189. Published online April 20, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.3.182
- 6,263 View
- 140 Download
- 77 Web of Science
- 75 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Populations are aging and the prevalence of diabetes mellitus is increasing tremendously. The number of older people with diabetes is increasing unexpectedly. Aging and diabetes are both risk factors for functional disability. Thus, increasing numbers of frail or disabled older patients with diabetes will increase both direct and indirect health-related costs. Diabetes has been reported as an important risk factor of developing physical disability in older adults. Older people with diabetes have lower muscle mass and weaker muscle strength. In addition, muscle quality is poorer in diabetic patients. Sarcopenia and frailty have a common soil and may share a similar pathway for multiple pathologic processes in older people. Sarcopenia is thought to be an intermediate step in the development of frailty in patients with diabetes. Thus, early detection of sarcopenia and frailty in older adults with diabetes should be routine clinical practice to prevent frailty or to intervene earlier in frail patients.
-
Citations
Citations to this article as recorded by- Glycemic control and prescription profiles in internal medicine inpatients: The role of frailty
Jose Carlos Arévalo Lorido, Juana Carretero Gomez, Patricia Vazquez Rodriguez, Ricardo Gómez Huelgas, Carmen Marín Silvente, Fernando Javier Sánchez Lora, Elena Isaba Ares, Anna Pardo i Pelegrín, Onán Pérez Hernández, Javier Ena
European Journal of Internal Medicine.2024; 121: 103. CrossRef - Prolonged hospitalization and 1-year mortality are associated with sarcopenia and malnutrition in older patients with type 2 diabetes: A prospective cohort study
Mileni Vanti Beretta, Tatiana Pedroso de Paula, Ticiana da Costa Rodrigues, Thais Steemburgo
Diabetes Research and Clinical Practice.2024; 207: 111063. CrossRef - Effect of Frailty on Depression among Patients with Late-life Depression: A Test of Anger, Anxiety, and Resilience as Mediators
Junhyung Kim, Hyun-Ghang Jeong, Moon-Soo Lee, Chi-Un Pae, Ashwin A. Patkar, Sang Won Jeon, Cheolmin Shin, Changsu Han
Clinical Psychopharmacology and Neuroscience.2024; 22(2): 253. CrossRef - Urgent needs of caregiving in ageing populations with Alzheimer’s disease and other chronic conditions: Support our loved ones
John W. Culberson, Jonathan Kopel, Ujala Sehar, P. Hemachandra Reddy
Ageing Research Reviews.2023; 90: 102001. CrossRef - Hand grip strength: A reliable assessment tool of frailty status on the person with type 2 diabetes mellitus
Diogo Ramalho, Leonor Silva, Catarina Almeida, Luís Rocha, Gustavo Rocha, Rafaela Veríssimo
Nutrition Clinique et Métabolisme.2023; 37(1): 45. CrossRef - Comprehensive review: Frailty in pancreas transplant candidates and recipients
Ronald F. Parsons, Ekamol Tantisattamo, Wisit Cheungpasitporn, Arpita Basu, Yee Lu, Krista L. Lentine, Kenneth J. Woodside, Neeraj Singh, Joseph Scalea, Tarek Alhamad, Ty B. Dunn, Franco H. Cabeza Rivera, Sandesh Parajuli, Martha Pavlakis, Matthew Cooper
Clinical Transplantation.2023;[Epub] CrossRef - Development and validation of a risk prediction model for frailty in patients with diabetes
Fan Bu, Xiao-hui Deng, Na-ni Zhan, Hongtao Cheng, Zi-lin Wang, Li Tang, Yu Zhao, Qi-yuan Lyu
BMC Geriatrics.2023;[Epub] CrossRef - Amino Acid Profiles in Older Adults with Frailty: Secondary Analysis from MetaboFrail and BIOSPHERE Studies
Riccardo Calvani, Anna Picca, Leocadio Rodriguez-Mañas, Matteo Tosato, Hélio José Coelho-Júnior, Alessandra Biancolillo, Olga Laosa, Jacopo Gervasoni, Aniello Primiano, Lavinia Santucci, Ottavia Giampaoli, Isabelle Bourdel-Marchasson, Sophie C. Regueme, A
Metabolites.2023; 13(4): 542. CrossRef - Where to Start? Physical Assessment, Readiness, and Exercise Recommendations for People With Type 1 or Type 2 Diabetes
Marni Armstrong, Sheri R. Colberg, Ronald J. Sigal
Diabetes Spectrum.2023; 36(2): 105. CrossRef - The Association Between Sarcopenia and Diabetes: From Pathophysiology Mechanism to Therapeutic Strategy
Huiling Chen, Xiaojing Huang, Meiyuan Dong, Song Wen, Ligang Zhou, Xinlu Yuan
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 1541. CrossRef - Analysis of Individual Components of Frailty in Simultaneous Pancreas and Kidney, and Solitary Pancreas Transplant Recipients
Sandesh Parajuli, Jon Odorico, Isabel Breyer, Emily Zona, Fahad Aziz, Heather Lorden, Jacqueline Garonzik-Wang, Dixon Kaufman, Didier Mandelbrot
Transplantation Direct.2023; 9(9): e1523. CrossRef - Effects of moderate exercise versus light exercise on fasting blood glucose in obese patients with type 2 diabetes mellitus
Manal Kamel Youssef
Physiotherapy Quarterly.2023; 31(3): 101. CrossRef - Risk factors associated with frailty in older adults with type 2 diabetes: A cross‐sectional study
Chia‐Ling Lin, Neng‐Chun Yu, Hsueh‐Ching Wu, Yuan‐Ching Liu
Journal of Clinical Nursing.2022; 31(7-8): 967. CrossRef - Sarcopenia in patients with multiple sclerosis
Hatice Yuksel, Mehtap Balaban, Ozlem Ozturk Tan, Semra Mungan
Multiple Sclerosis and Related Disorders.2022; 58: 103471. CrossRef - Amino acid profile of skeletal muscle loss in type 2 diabetes: Results from a 7-year longitudinal study in asians
Serena Low, Jiexun Wang, Angela Moh, Su Fen Ang, Keven Ang, Yi-Ming Shao, Jianhong Ching, Hai Ning Wee, Lye Siang Lee, Jean-Paul Kovalik, Wern Ee Tang, Ziliang Lim, Tavintharan Subramaniam, Chee Fang Sum, Su Chi Lim
Diabetes Research and Clinical Practice.2022; 186: 109803. CrossRef - Assessment of Muscle Quantity, Quality and Function
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2022; 31(1): 9. CrossRef - Sarcopenia is associated with cardiovascular risk in men with COPD, independent of adiposity
Ah Young Leem, Young Sam Kim, Kung Soo Chung, Moo Suk Park, Young Ae Kang, Young-Mok Park, Ji Ye Jung
Respiratory Research.2022;[Epub] CrossRef - Decline in skeletal muscle mass is associated with cognitive decline in type 2 diabetes mellitus
Serena Low, Kiat Sern Goh, Tze Pin Ng, Angela Moh, Su Fen Ang, Jonathon Khoo, Keven Ang, Philip Yap, Chin Yee Cheong, Wern Ee Tang, Ziliang Lim, Tavintharan Subramaniam, Chee Fang Sum, Su Chi Lim
Journal of Diabetes and its Complications.2022; 36(9): 108258. CrossRef - Frailty and diabetes in older adults: Overview of current controversies and challenges in clinical practice
Mohd Zaquan Arif Abd.Ghafar, Mark O’Donovan, Duygu Sezgin, Elizabeth Moloney, Ángel Rodríguez-Laso, Aaron Liew, Rónán O’Caoimh
Frontiers in Clinical Diabetes and Healthcare.2022;[Epub] CrossRef - Implications of the Metabolic Control of Diabetes in Patients with Frailty Syndrome
Marta Muszalik, Hubert Stępień, Grażyna Puto, Mateusz Cybulski, Donata Kurpas
International Journal of Environmental Research and Public Health.2022; 19(16): 10327. CrossRef - Protective Effect of Delta-Like 1 Homolog Against Muscular Atrophy in a Mouse Model
Ji Young Lee, Minyoung Lee, Dong-Hee Lee, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha
Endocrinology and Metabolism.2022; 37(4): 684. CrossRef - Diabetes and osteoporosis – Treating two entities: A challenge or cause for concern?
Nicklas H. Rasmussen, Peter Vestergaard
Best Practice & Research Clinical Rheumatology.2022; 36(3): 101779. CrossRef - Predictors associated with prefrailty in older Taiwanese individuals with type 2 diabetes
Shu-Fen Lee, Chih-Ping Li, Yen-Lin Chen, Dee Pei
Medicine.2022; 101(38): e30432. CrossRef - Association of walking speed with cognitive function in Chinese older adults: A nationally representative cohort study
Jianping Liu, Kaiwang Cui, Qian Chen, Zhiteng Li, Jing Fu, Xiangwen Gong, Hui Xu
Frontiers in Aging Neuroscience.2022;[Epub] CrossRef - Lower insulin level is associated with sarcopenia in community-dwelling frail and non-frail older adults
Yanxia Lu, Wee Shiong Lim, Xia Jin, Ma Schwe Zin Nyunt, Tamas Fulop, Qi Gao, Su Chi Lim, Anis Larbi, Tze Pin Ng
Frontiers in Medicine.2022;[Epub] CrossRef - Weight-adjusted waist index reflects fat and muscle mass in the opposite direction in older adults
Nam Hoon Kim, Yousung Park, Nan Hee Kim, Sin Gon Kim
Age and Ageing.2021; 50(3): 780. CrossRef - Examining the links between regular leisure‐time physical activity, sitting time and prefrailty in community‐dwelling older adults
Shu‐Hung Chang, Nai‐Hui Chien, Jackson Pui‐Man Wai, Ching‐Cheng Chiang, Ching‐Yi Yu
Journal of Advanced Nursing.2021; 77(6): 2761. CrossRef - Tale of the Frail: Understanding Frailty in Cirrhosis
Faruq Pradhan, Natasha Narang, Michael Fallon
Southern Medical Journal.2021; 114(3): 186. CrossRef - Type 2 diabetes mellitus in older adults: clinical considerations and management
Srikanth Bellary, Ioannis Kyrou, James E. Brown, Clifford J. Bailey
Nature Reviews Endocrinology.2021; 17(9): 534. CrossRef - Low Protein Intakes and Poor Diet Quality Associate with Functional Limitations in US Adults with Diabetes: A 2005–2016 NHANES Analysis
Stephanie M. Fanelli, Owen J. Kelly, Jessica L. Krok-Schoen, Christopher A. Taylor
Nutrients.2021; 13(8): 2582. CrossRef - Yaşlı Diyabetik Hastalarda Malnutrisyonun Klinik Sonuçları ve Önemi
Saadet KOÇ OKUDUR, Pinar SOYSAL
OSMANGAZİ JOURNAL OF MEDICINE.2021;[Epub] CrossRef - Combined Aerobic and Resistance Exercise Training Reduces Circulating Apolipoprotein J Levels and Improves Insulin Resistance in Postmenopausal Diabetic Women
Yun Kyung Jeon, Sang Soo Kim, Jong Ho Kim, Hyun Jeong Kim, Hyun Jun Kim, Jang Jun Park, Yuen Suk Cho, So Hee Joung, Ji Ryang Kim, Bo Hyun Kim, Sang Heon Song, In Joo Kim, Yong Ki Kim, Young-Bum Kim
Diabetes & Metabolism Journal.2020; 44(1): 103. CrossRef - Effects of elastic band exercise on the frailty states in pre-frail elderly people
Rujie Chen, Qingwen Wu, Dongyan Wang, Zhou Li, Howe Liu, Guangtian Liu, Ying Cui, Linlin Song
Physiotherapy Theory and Practice.2020; 36(9): 1000. CrossRef - Association between Lower Extremity Skeletal Muscle Mass and Impaired Cognitive Function in Type 2 Diabetes
Serena Low, Tze Pin Ng, Chin Leong Lim, Angela Moh, Su Fen Ang, Jiexun Wang, Kiat Sern Goh, Keven Ang, Wern Ee Tang, Pek Yee Kwan, Tavintharan Subramaniam, Chee Fang Sum, Su Chi Lim
Scientific Reports.2020;[Epub] CrossRef - Low free triiodothyronine levels are associated with risk of frailty in older adults with type 2 diabetes mellitus
Shuangling Xiu, Zhijing Mu, Lei Zhao, Lina Sun
Experimental Gerontology.2020; 138: 111013. CrossRef - The Biomechanics of Diabetes Mellitus and Limb Preservation
Jonathan M. Labovitz, Dana Day
Clinics in Podiatric Medicine and Surgery.2020; 37(1): 151. CrossRef - Inorganic Arsenic Exposure Decreases Muscle Mass and Enhances Denervation-Induced Muscle Atrophy in Mice
Chang-Mu Chen, Min-Ni Chung, Chen-Yuan Chiu, Shing-Hwa Liu, Kuo-Cheng Lan
Molecules.2020; 25(13): 3057. CrossRef - Physical Exercise and Myokines: Relationships with Sarcopenia and Cardiovascular Complications
Sandra Maria Barbalho, Uri Adrian Prync Flato, Ricardo José Tofano, Ricardo de Alvares Goulart, Elen Landgraf Guiguer, Cláudia Rucco P. Detregiachi, Daniela Vieira Buchaim, Adriano Cressoni Araújo, Rogério Leone Buchaim, Fábio Tadeu Rodrigues Reina, Piero
International Journal of Molecular Sciences.2020; 21(10): 3607. CrossRef - The relationships between sarcopenic skeletal muscle loss during ageing and macronutrient metabolism, obesity and onset of diabetes
Ailsa A. Welch, Richard P. G. Hayhoe, Donnie Cameron
Proceedings of the Nutrition Society.2020; 79(1): 158. CrossRef - Effects of low skeletal muscle mass and sarcopenic obesity on albuminuria: a 7-year longitudinal study
Jee Hee Yoo, Gyuri Kim, Sung Woon Park, Min Sun Choi, Jiyeon Ahn, Sang-Man Jin, Kyu Yeon Hur, Moon-Kyu Lee, Mira Kang, Jae Hyeon Kim
Scientific Reports.2020;[Epub] CrossRef - Sarcopenia, nutritional status and type 2 diabetes mellitus: A cross‐sectional study in a group of Mexican women residing in a nursing home
María C. Velázquez‐Alva, María E. Irigoyen‐Camacho, Marco A. Zepeda‐Zepeda, Irina Lazarevich, Isabel Arrieta‐Cruz, Carlos D'Hyver
Nutrition & Dietetics.2020; 77(5): 515. CrossRef - Assessing the association between optimal energy intake and all‐cause mortality in older patients with diabetes mellitus using the Japanese Elderly Diabetes Intervention Trial
Takuya Omura, Yoshiaki Tamura, Takuya Yamaoka, Yukio Yoshimura, Takashi Sakurai, Hiroyuki Umegaki, Chiemi Kamada, Satoshi Iimuro, Yasuo Ohashi, Hideki Ito, Atsushi Araki
Geriatrics & Gerontology International.2020; 20(1): 59. CrossRef - Sarkopenie im Kontext von Insulinresistenz und Diabetes mellitus im Alter – Daten aus der Berliner Altersstudie II
Dominik Spira, Nikolaus Buchmann, Knut Mai, Thomas Bobbert, Joachim Spranger, Ilja Demuth, Elisabeth Steinhagen-Thiessen
Diabetologie und Stoffwechsel.2020; 15(05): 400. CrossRef - Effect of Dietary Silk Peptide on Obesity, Hyperglycemia, and Skeletal Muscle Regeneration in High-Fat Diet-Fed Mice
Kippeum Lee, Heegu Jin, Sungwoo Chei, Hyun-Ji Oh, Jeong-Yong Lee, Boo-Yong Lee
Cells.2020; 9(2): 377. CrossRef - Nutrition Management in Older Adults with Diabetes: A Review on the Importance of Shifting Prevention Strategies from Metabolic Syndrome to Frailty
Yoshiaki Tamura, Takuya Omura, Kenji Toyoshima, Atsushi Araki
Nutrients.2020; 12(11): 3367. CrossRef - Mechanical Properties of Single Muscle Fibers: Understanding Poor Muscle Quality in Older Adults with Diabetes
Eun-Jeong Lee, Hak Chul Jang, Kyung-Hoi Koo, Hye-Young Kim, Jae-Young Lim
Annals of Geriatric Medicine and Research.2020; 24(4): 267. CrossRef - Mortality is not increased with Diabetes in hospitalised very old adults: a multi-site review
Peter Smerdely
BMC Geriatrics.2020;[Epub] CrossRef - Falls and Fractures in Diabetes—More than Bone Fragility
Nicklas Højgaard Rasmussen, Jakob Dal
Current Osteoporosis Reports.2019; 17(3): 147. CrossRef - Measuring gait speed to better identify prodromal dementia
Giulia Grande, Federico Triolo, Arturo Nuara, Anna-Karin Welmer, Laura Fratiglioni, Davide L. Vetrano
Experimental Gerontology.2019; 124: 110625. CrossRef - Diabetes and Muscle Dysfunction in Older Adults
Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 160. CrossRef - Association between sarcopenia and diabetes in community dwelling elderly in the Amazon region – Viver Mais Project
Anelza Biene Farias Souza, David Anchieta Costa Nascimento, Isabella Juliana Manfredo Rodrigues, Cynthia Cillene Oliveira Charone, Geovanna Lemos Lopes, Rondinei Silva Lima, Ana Amália Sá, Thiago Xavier Carneiro, Niele Silva Moraes
Archives of Gerontology and Geriatrics.2019; 83: 121. CrossRef - Association between deterioration in muscle strength and peripheral neuropathy in people with diabetes
Tae Jung Oh, Sunyoung Kang, Jie-Eun Lee, Jae Hoon Moon, Sung Hee Choi, Soo Lim, Hak Chul Jang
Journal of Diabetes and its Complications.2019; 33(8): 598. CrossRef - Frailty and Disability in Diabetes
Sol-Ji Yoon, Kwang-il Kim
Annals of Geriatric Medicine and Research.2019; 23(4): 165. CrossRef - Mechanisms Involved in Glycemic Control Promoted by Exercise in Diabetics
Eric Francelino Andrade, Víviam de Oliveira Silva, Débora Ribeiro Orlando, Luciano José Pereira
Current Diabetes Reviews.2019; 15(2): 105. CrossRef - Response: The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity (J Obes Metab Syndr 2019;28:46-52)
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 297. CrossRef - Diabetic Peripheral Neuropathy as a Risk Factor for Sarcopenia
Tae Jung Oh, Yoojung Song, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 170. CrossRef - Sarcopenia and hospital-related outcomes in the old people: a systematic review and meta-analysis
Yunli Zhao, Yunxia Zhang, Qiukui Hao, Meiling Ge, Birong Dong
Aging Clinical and Experimental Research.2019; 31(1): 5. CrossRef - The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(1): 46. CrossRef - Sarcopenia in elderly patients with type 2 diabetes mellitus: prevalence and related clinical factors
Yuko Murata, Yoshiki Kadoya, Shoichi Yamada, Tokio Sanke
Diabetology International.2018; 9(2): 136. CrossRef - Assessment of lower extremity muscle mass, muscle strength, and exercise therapy in elderly patients with diabetes mellitus
Takuo Nomura, Toshihiro Kawae, Hiroaki Kataoka, Yukio Ikeda
Environmental Health and Preventive Medicine.2018;[Epub] CrossRef - Diabetes Treatment in the Elderly: Incorporating Geriatrics, Technology, and Functional Medicine
Willy Marcos Valencia, Diana Botros, Maria Vera-Nunez, Stuti Dang
Current Diabetes Reports.2018;[Epub] CrossRef - Psoas and paraspinous muscle index as a predictor of mortality in African American men with type 2 diabetes mellitus
Mariana Murea, Leon Lenchik, Thomas C. Register, Gregory B. Russell, Jianzhao Xu, S. Carrie Smith, Donald W. Bowden, Jasmin Divers, Barry I. Freedman
Journal of Diabetes and its Complications.2018; 32(6): 558. CrossRef - Presence of Sarcopenia and Its Rate of Change Are Independently Associated with Long-term Mortality in Patients with Liver Cirrhosis
Jae Yoon Jeong, Sanghyeok Lim, Joo Hyun Sohn, Jae Gon Lee, Dae Won Jun, Yongsoo Kim
Journal of Korean Medical Science.2018;[Epub] CrossRef - Comparison between Dual-Energy X-ray Absorptiometry and Bioelectrical Impedance Analyses for Accuracy in Measuring Whole Body Muscle Mass and Appendicular Skeletal Muscle Mass
Seo Lee, Soyeon Ahn, Young Kim, Myoung Ji, Kyoung Kim, Sung Choi, Hak Jang, Soo Lim
Nutrients.2018; 10(6): 738. CrossRef - The association of low muscle mass with soluble receptor for advanced glycation end products (sRAGE): The Korean Sarcopenic Obesity Study (KSOS)
Tae Nyun Kim, Man Sik Park, Eun Joo Lee, Hye Soo Chung, Hye Jin Yoo, Hyun Joo Kang, Wook Song, Sei Hyun Baik, Kyung Mook Choi
Diabetes/Metabolism Research and Reviews.2018;[Epub] CrossRef - Obesity paradox on the survival of elderly patients with diabetes: an AHAP-based study
Ali Bijani, Robert G. Cumming, Seyed-Reza Hosseini, Masoumeh Yazdanpour, Mahdis Rahimi, Abbas Sahebian, Reza Ghadimi
Journal of Diabetes & Metabolic Disorders.2018; 17(1): 45. CrossRef - Effects of Seahorse Supplementation on Muscle Mass, Exercise Performance Abilities and the Related Blood Factors in Healthy Elderly Women
Bae-jin LEE, Chan-ho PARK, Byeong-Hwan JEON
JOURNAL OF FISHRIES AND MARINE SCIENCES EDUCATION.2018; 30(2): 409. CrossRef - Frailty risk in hospitalised older adults with and without diabetes mellitus
Deborah A. Lekan, Thomas P. McCoy
Journal of Clinical Nursing.2018; 27(19-20): 3510. CrossRef - Sarcopenia
А.А. Пальцын
ZHurnal «Patologicheskaia fiziologiia i eksperimental`naia terapiia».2018; (2()): 113. CrossRef - Prevention of Falls and Frailty in Older Adults with Diabetes
Helen P. Hazuda, Sara E. Espinoza
Current Geriatrics Reports.2017; 6(3): 158. CrossRef - Patterns and Predictors of Frailty Transitions in Older Men: The Osteoporotic Fractures in Men Study
Lauren R. Pollack, Stephanie Litwack‐Harrison, Peggy M. Cawthon, Kristine Ensrud, Nancy E. Lane, Elizabeth Barrett‐Connor, Thuy‐Tien Dam
Journal of the American Geriatrics Society.2017; 65(11): 2473. CrossRef - Diabetic Neuropathy and Gait: A Review
Uazman Alam, David R. Riley, Ravinder S. Jugdey, Shazli Azmi, Satyan Rajbhandari, Kristiaan D’Août, Rayaz A. Malik
Diabetes Therapy.2017; 8(6): 1253. CrossRef - Care of older people with diabetes
Trisha Dunning
Nursing Standard.2017; 32(3): 50. CrossRef - Decreased Muscle Strength and Quality in Diabetes-Related Dementia
Akito Tsugawa, Yusuke Ogawa, Naoto Takenoshita, Yoshitsugu Kaneko, Hirokuni Hatanaka, Eriko Jaime, Raita Fukasawa, Haruo Hanyu
Dementia and Geriatric Cognitive Disorders Extra.2017; 7(3): 454. CrossRef - Aging of the endocrine system and its potential impact on sarcopenia
Giovanni Vitale, Matteo Cesari, Daniela Mari
European Journal of Internal Medicine.2016; 35: 10. CrossRef
- Glycemic control and prescription profiles in internal medicine inpatients: The role of frailty
- Clinical Care/Education
- Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging
- Ji Won Yoon, Yong-Chan Ha, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Soo Lim, Young Joo Park, Jae Young Lim, Ki Woong Kim, Kyong Soo Park, Hak Chul Jang
- Diabetes Metab J. 2016;40(2):140-146. Published online March 31, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.2.140
- 7,307 View
- 78 Download
- 86 Web of Science
- 89 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The study aimed to investigate the influence of hyperglycemia on muscle quality in older men with type 2 diabetes.
Methods This was a subsidiary study of the Korean Longitudinal Study of Health and Aging. Among 326 older men consenting to tests of body composition and muscle strength, 269 men were ultimately analyzed after the exclusion because of stroke (
n =30) and uncertainty about the diagnosis of diabetes (n =27). Body composition was measured using dual-energy X-ray absorptiometry and computed tomography. Muscle strength for knee extension was measured using an isokinetic dynamometer. Muscle quality was assessed from the ratio of leg strength to the entire corresponding leg muscle mass.Results The muscle mass, strength, and quality in patients with type 2 diabetes did not differ significantly from controls. However, when patients with diabetes were subdivided according to their glycemic control status, patients with a glycosylated hemoglobin (HbA1c) level of ≥8.5% showed significantly decreased leg muscle quality by multivariate analysis (odds ratio, 4.510;
P =0.045) after adjustment for age, body mass index, smoking amount, alcohol consumption, physical activity, and duration of diabetes. Physical performance status was also impaired in subjects with an HbA1c of ≥8.5%.Conclusion Poor glycemic control in these older patients with diabetes was associated with significant risk of decreased muscle quality and performance status. Glycemic control with an HbA1c of <8.5% might be needed to reduce the risk of adverse skeletal and functional outcomes in this population.
-
Citations
Citations to this article as recorded by- Downhill running and caloric restriction attenuate insulin resistance associated skeletal muscle atrophy via the promotion of M2-like macrophages through TRIB3-AKT pathway
Wei Luo, Yue Zhou, Qiang Tang, Yuhang Wang, Yansong Liu, Lei Ai
Free Radical Biology and Medicine.2024; 210: 271. CrossRef - Diabetic Sarcopenia. A proposed muscle screening protocol in people with diabetes
Daniel de Luis Román, Juana Carretero Gómez, José Manuel García-Almeida, Fernando Garrachón Vallo, German Guzmán Rolo, Juan José López Gómez, Francisco José Tarazona-Santabalbina, Alejandro Sanz-Paris
Reviews in Endocrine and Metabolic Disorders.2024;[Epub] CrossRef - Dynapenia and sarcopenia: association with the diagnosis, duration and complication of type 2 diabetes mellitus in ELSA-Brasil
Débora Noara Duarte dos Santos, Carolina Gomes Coelho, Maria de Fátima Haueisen Sander Diniz, Bruce Bartholow Duncan, Maria Inês Schmidt, Isabela Judith Martins Bensenor, Claudia Szlejf, Rosa Weiss Telles, Sandhi Maria Barreto
Cadernos de Saúde Pública.2024;[Epub] CrossRef - Breaking Down Cachexia: A Narrative Review on the Prevalence of Cachexia in Cancer Patients and Its Associated Risk Factors
Mahmathi Karuppannan, Fares M. S. Muthanna, Fazlin Mohd Fauzi
Nutrition and Cancer.2024; 76(5): 404. CrossRef - Mechanism of muscle atrophy in a normal-weight rat model of type 2 diabetes established by using a soft-pellet diet
Sayaka Akieda-Asai, Hao Ma, Wanxin Han, Junko Nagata, Fumitake Yamaguchi, Yukari Date
Scientific Reports.2024;[Epub] CrossRef - Morphological and functional changes in skeletal muscle in type 2 diabetes mellitus: A systematic review and meta-analysis
Jardeson Rocha Filgueiras, Cleudiane Pereira Sales, Ivanilson Gomes da Silva, Cristiana Maria Dos Santos, Elias de Carvalho Magalhães Neto, Rebeca Barbosa da Rocha, Vinicius Saura Cardoso
Physiotherapy Theory and Practice.2023; 39(9): 1789. CrossRef - Hypoglycemic drug liraglutide alleviates low muscle mass by inhibiting the expression of MuRF1 and MAFbx in diabetic muscle atrophy
Dongmei Fan, Yue Wang, Bowei Liu, Fuzai Yin
Journal of the Chinese Medical Association.2023; 86(2): 166. CrossRef - Mechanisms underlying altered neuromuscular function in people with DPN
Antonin Le Corre, Nathan Caron, Nicolas A. Turpin, Georges Dalleau
European Journal of Applied Physiology.2023; 123(7): 1433. CrossRef - Effects of body compositions on the associations between ferritin and diabetes parameters among Japanese community dwellers
Kyi Mar Wai, Rei Akuzawa, Yoko Umeda, Wataru Munakata, Yoshiko Takahashi, Shigeyuki Nakaji, Kazushige Ihara
Journal of Trace Elements in Medicine and Biology.2023; 78: 127174. CrossRef - Effects of glycemic control on frailty: a multidimensional perspective
Ahmed H Abdelhafiz
Hospital Practice.2023; 51(3): 124. CrossRef - Hand grip strength is inversely associated with total daily insulin dose requirement in patients with type 2 diabetes mellitus: a cross-sectional study
Da-shuang Chen, Yun-qing Zhu, Wen-ji Ni, Yu-jiao Li, Guo-ping Yin, Zi-yue Shao, Jian Zhu
PeerJ.2023; 11: e15761. CrossRef - Sarcopenia in Type 2 Diabetes Mellitus: Study of the Modifiable Risk Factors Involved
Surapaneni Lakshmi Sravya, Jayshree Swain, Abhay Kumar Sahoo, Swayamsidha Mangaraj, Jayabhanu Kanwar, Pooja Jadhao, Srijit Das
Journal of Clinical Medicine.2023; 12(17): 5499. CrossRef - Salbutamol ameliorates skeletal muscle wasting and inflammatory markers in streptozotocin (STZ)-induced diabetic rats
Anand Kumar, Priyanka Prajapati, Vinit Raj, Seong-Cheol Kim, Vikas Mishra, Chaitany Jayprakash Raorane, Ritu Raj, Dinesh Kumar, Sapana Kushwaha
International Immunopharmacology.2023; 124: 110883. CrossRef - Decreased serum musclin concentration is independently associated with the high prevalence of sarcopenia in Chinese middle‐elderly patients with type 2 diabetes mellitus
Lei Fu, Qing Zhang, Juan Liu, Xiaoqing Yuan, Xinhua Ye
Journal of Diabetes Investigation.2023; 14(12): 1412. CrossRef - Association between relative muscle strength and hypertension in middle-aged and older Chinese adults
Jin-hua Luo, Tu-ming Zhang, Lin-lin Yang, Yu-ying Cai, Yu Yang
BMC Public Health.2023;[Epub] CrossRef - Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
Diabetes & Metabolism Journal.2023; 47(5): 643. CrossRef - Management of Hyperglycemia in Older Adults with Type 2 Diabetes
Gunjan Y. Gandhi, Arshag D. Mooradian
Drugs & Aging.2022; 39(1): 39. CrossRef - Deleterious Effect of High-Fat Diet on Skeletal Muscle Performance Is Prevented by High-Protein Intake in Adult Rats but Not in Old Rats
Eleonora Poggiogalle, Fanny Rossignon, Aude Carayon, Fréderic Capel, Jean-Paul Rigaudière, Sarah De Saint Vincent, Olivier Le-Bacquer, Jérôme Salles, Christophe Giraudet, Véronique Patrac, Patrice Lebecque, Stéphane Walrand, Yves Boirie, Vincent Martin, C
Frontiers in Physiology.2022;[Epub] CrossRef - Metabolic phenotypes explain the relationship between dysglycaemia and frailty in older people with type 2 diabetes
A.H. Abdelhafiz, A.J. Sinclair
Journal of Diabetes and its Complications.2022; 36(4): 108144. CrossRef - Altered features of body composition in older adults with type 2 diabetes and prediabetes compared with matched controls
Kirsten E. Bell, Michael T. Paris, Egor Avrutin, Marina Mourtzakis
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(2): 1087. CrossRef - A modern approach to glucose-lowering therapy in frail older people with type 2 diabetes mellitus
Ahmed H. Abdelhafiz, Daniel Pennells, Alan J. Sinclair
Expert Review of Endocrinology & Metabolism.2022; 17(2): 95. CrossRef - Metabolic syndrome and its association with components of sarcopenia in older community-dwelling Chinese
Qiangwei Tong, Xiao Wang, Yunlu Sheng, Shu Chen, Bin Lai, Rong Lv, Jing Yu
The Journal of Biomedical Research.2022; 36(2): 120. CrossRef - Sarcopenia is associated with the Geriatric Nutritional Risk Index in elderly patients with poorly controlled type 2 diabetes mellitus
Shun Matsuura, Koji Shibazaki, Reiko Uchida, Yukiko Imai, Takuya Mukoyama, Shoko Shibata, Hiroshi Morita
Journal of Diabetes Investigation.2022; 13(8): 1366. CrossRef - Increased serum levels of advanced glycation end products are negatively associated with relative muscle strength in patients with type 2 diabetes mellitus
Tsung-Hui Wu, Shiow-Chwen Tsai, Hsuan-Wei Lin, Chiao-Nan Chen, Chii-Min Hwu
BMC Endocrine Disorders.2022;[Epub] CrossRef - Clinical outcomes of multidimensional association of type 2 diabetes mellitus, COVID-19 and sarcopenia: an algorithm and scoping systematic evaluation
Anmar Al-Taie, Oritsetimeyin Arueyingho, Jalal Khoshnaw, Abdul Hafeez
Archives of Physiology and Biochemistry.2022; : 1. CrossRef - Hypoglycaemic therapy in frail older people with type 2 diabetes mellitus—a choice determined by metabolic phenotype
Alan J. Sinclair, Daniel Pennells, Ahmed H. Abdelhafiz
Aging Clinical and Experimental Research.2022; 34(9): 1949. CrossRef - Insulin in Frail, Older People with Type 2 Diabetes—Low Threshold for Therapy
Ahmed Abdelhafiz, Shail Bisht, Iva Kovacevic, Daniel Pennells, Alan Sinclair
Diabetology.2022; 3(2): 369. CrossRef - Sex-Specific Associations Between Low Muscle Mass and Glucose Fluctuations in Patients With Type 2 Diabetes Mellitus
Xiulin Shi, Wenjuan Liu, Lulu Zhang, Fangsen Xiao, Peiying Huang, Bing Yan, Yiping Zhang, Weijuan Su, Qiuhui Jiang, Mingzhu Lin, Wei Liu, Xuejun Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - Lifestyle factors associated with muscle quality in community‐dwelling older people with type 2 diabetes in Japan and Taiwan: a cross‐sectional study
Yuko Yamaguchi, Chieko Greiner, Shu‐Chun Lee, Hirochika Ryuno, Hsin‐Yen Yen, Chiou‐Fen Lin, Ting‐I Lee, Pi‐Hsia Lee
Psychogeriatrics.2022; 22(5): 736. CrossRef - Relationship between Echo Intensity of Vastus Lateralis and Knee Extension Strength in Patients with Type 2 Diabetes Mellitus
Yoshikazu HIRASAWA, Ryosuke MATSUKI, Hideaki TANINA
Physical Therapy Research.2022; 25(3): 113. CrossRef - Time trends (2012–2020) in glycated hemoglobin and adherence to the glycemic targets recommended for elderly patients by the Japan Diabetes Society/Japan Geriatrics Society Joint Committee among memory clinic patients with diabetes mellitus
Taiki Sugimoto, Hisashi Noma, Yujiro Kuroda, Nanae Matsumoto, Kazuaki Uchida, Yoshinobu Kishino, Naoki Saji, Shumpei Niida, Takashi Sakurai
Journal of Diabetes Investigation.2022; 13(12): 2038. CrossRef - Relationship between Diabetes Status and Sarcopenia in Community-Dwelling Older Adults
Kazuhei Nishimoto, Takehiko Doi, Kota Tsutsumimoto, Sho Nakakubo, Satoshi Kurita, Yuto Kiuchi, Hiroyuki Shimada
Journal of the American Medical Directors Association.2022; 23(10): 1718.e7. CrossRef - Low relative hand grip strength is associated with a higher risk for diabetes and impaired fasting glucose among the Korean population
Min Jin Lee, Ah Reum Khang, Dongwon Yi, Yang Ho Kang, Giacomo Pucci
PLOS ONE.2022; 17(10): e0275746. CrossRef - Association between Lower-to-Upper Ratio of Appendicular Skeletal Muscle and Metabolic Syndrome
Hyun Eui Moon, Tae Sic Lee, Tae-Ha Chung
Journal of Clinical Medicine.2022; 11(21): 6309. CrossRef - Association of plasma brain-derived neurotrophic factor levels and frailty in community-dwelling older adults
Eun Roh, Soon Young Hwang, Eyun Song, Min Jeong Park, Hye Jin Yoo, Sei Hyun Baik, Miji Kim, Chang Won Won, Kyung Mook Choi
Scientific Reports.2022;[Epub] CrossRef - Organokines, Sarcopenia, and Metabolic Repercussions: The Vicious Cycle and the Interplay with Exercise
Giulia Minniti, Letícia Maria Pescinini-Salzedas, Guilherme Almeida dos Santos Minniti, Lucas Fornari Laurindo, Sandra Maria Barbalho, Renata Vargas Sinatora, Lance Alan Sloan, Rafael Santos de Argollo Haber, Adriano Cressoni Araújo, Karina Quesada, Jesse
International Journal of Molecular Sciences.2022; 23(21): 13452. CrossRef - Multimorbidity, Frailty and Diabetes in Older People–Identifying Interrelationships and Outcomes
Alan J. Sinclair, Ahmed H. Abdelhafiz
Journal of Personalized Medicine.2022; 12(11): 1911. CrossRef - Determinants of High-Dose Insulin Usage and Upper Extremity Muscle Strength in Adult Patients With Type 2 Diabetes
Eren Imre, Tugce Apaydin, Hatice Gizem Gunhan, Dilek Gogas Yavuz
Canadian Journal of Diabetes.2021; 45(4): 341. CrossRef - Glycemic Control and Insulin Improve Muscle Mass and Gait Speed in Type 2 Diabetes: The MUSCLES-DM Study
Ken Sugimoto, Hiroshi Ikegami, Yasunori Takata, Tomohiro Katsuya, Masahiro Fukuda, Hiroshi Akasaka, Yasuharu Tabara, Haruhiko Osawa, Yoshihisa Hiromine, Hiromi Rakugi
Journal of the American Medical Directors Association.2021; 22(4): 834. CrossRef - A Narrative Review on Sarcopenia in Type 2 Diabetes Mellitus: Prevalence and Associated Factors
Anna Izzo, Elena Massimino, Gabriele Riccardi, Giuseppe Della Pepa
Nutrients.2021; 13(1): 183. CrossRef - Decreased handgrip strength in patients with type 2 diabetes: A cross-sectional study in a tertiary care hospital in north India
Parjeet Kaur, Ritesh Bansal, Bharti Bhargava, Sunil Mishra, Harmandeep Gill, Ambrish Mithal
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(1): 325. CrossRef - Factors associated with relative muscle strength in patients with type 2 diabetes mellitus
Chiao-Nan Chen, Ting-Chung Chen, Shiow-Chwen Tsai, Chii-Min Hwu
Archives of Gerontology and Geriatrics.2021; 95: 104384. CrossRef - Newer anti-diabetic therapies with low hypoglycemic risk-potential advantages for frail older people
Demelza Emmerton, Ahmed Abdelhafiz
Hospital Practice.2021; 49(3): 164. CrossRef - Influence of glucose, insulin fluctuation, and glycosylated hemoglobin on the outcome of sarcopenia in patients with type 2 diabetes mellitus
Yuxi Lin, Yongze Zhang, Ximei Shen, Lingning Huang, Sunjie Yan
Journal of Diabetes and its Complications.2021; 35(6): 107926. CrossRef - Presence and Implications of Sarcopenia in Non-alcoholic Steatohepatitis
Gregory Habig, Christa Smaltz, Dina Halegoua-DeMarzio
Metabolites.2021; 11(4): 242. CrossRef - Sensory-Motor Mechanisms Increasing Falls Risk in Diabetic Peripheral Neuropathy
Neil D. Reeves, Giorgio Orlando, Steven J. Brown
Medicina.2021; 57(5): 457. CrossRef - Impact of frailty metabolic phenotypes on the management of older people with type 2 diabetes mellitus
Ahmed H Abdelhafiz, Demelza Emmerton, Alan J Sinclair
Geriatrics & Gerontology International.2021; 21(8): 614. CrossRef - Type 2 diabetes mellitus in older adults: clinical considerations and management
Srikanth Bellary, Ioannis Kyrou, James E. Brown, Clifford J. Bailey
Nature Reviews Endocrinology.2021; 17(9): 534. CrossRef - Metabolic Syndrome and Sarcopenia
Hiroki Nishikawa, Akira Asai, Shinya Fukunishi, Shuhei Nishiguchi, Kazuhide Higuchi
Nutrients.2021; 13(10): 3519. CrossRef - Angiotensin II inhibition: a potential treatment to slow the progression of sarcopenia
Jeffrey Kingsley, Keiichi Torimoto, Tomoki Hashimoto, Satoru Eguchi
Clinical Science.2021; 135(21): 2503. CrossRef - Muscle strength, an independent determinant of glycemic control in older adults with long-standing type 2 diabetes: a prospective cohort study
Bo Kyung Koo, Seoil Moon, Min Kyong Moon
BMC Geriatrics.2021;[Epub] CrossRef - Associations between homocysteine, inflammatory cytokines and sarcopenia in Chinese older adults with type 2 diabetes
Zhi-Jing Mu, Jun-Ling Fu, Li-Na Sun, Piu Chan, Shuang-Ling Xiu
BMC Geriatrics.2021;[Epub] CrossRef - The Association Between Diabetes Mellitus and Risk of Sarcopenia: Accumulated Evidences From Observational Studies
Yu-Shun Qiao, Yin-He Chai, Hong-Jian Gong, Zhiyessova Zhuldyz, Coen D. A. Stehouwer, Jian-Bo Zhou, Rafael Simó
Frontiers in Endocrinology.2021;[Epub] CrossRef - The utility of the ultrasonographic assessment of the lower leg muscles to evaluate sarcopenia and muscle quality in older adults
Masaaki Isaka, Ken Sugimoto, Taku Fujimoto, Yukiko Yasunobe, Keyu Xie, Yuri Onishi, Shino Yoshida, Toshimasa Takahashi, Hitomi Kurinami, Hiroshi Akasaka, Yasushi Takeya, Koichi Yamamoto, Hiromi Rakugi
JCSM Clinical Reports.2021; 6(2): 53. CrossRef - Associations between grip strength and glycemic control in type 2 diabetes mellitus: an analysis of data from the 2014-2019 Korea National Health and Nutrition Examination Survey
Harim Choe, Hoyong Sung, Geon Hui Kim, On Lee, Hyo Youl Moon, Yeon Soo Kim
Epidemiology and Health.2021; 43: e2021080. CrossRef - Uncontrolled Diabetes as an Associated Factor with Dynapenia in Adults Aged 50 Years or Older: Sex Differences
Clarice Cavalero Nebuloni, Roberta de Oliveira Máximo, Cesar de Oliveira, Tiago da Silva Alexandre, Anne Newman
The Journals of Gerontology: Series A.2020; 75(6): 1191. CrossRef - Identification and prevalence of frailty in diabetes mellitus and association with clinical outcomes: a systematic review protocol
Peter Hanlon, Isabella Fauré, Neave Corcoran, Elaine Butterly, Jim Lewsey, David A McAllister, Frances S Mair
BMJ Open.2020; 10(9): e037476. CrossRef - Longitudinal association of type 2 diabetes and insulin therapy with muscle parameters in the KORA-Age study
Uta Ferrari, Cornelia Then, Marietta Rottenkolber, Canan Selte, Jochen Seissler, Romy Conzade, Birgit Linkohr, Annette Peters, Michael Drey, Barbara Thorand
Acta Diabetologica.2020; 57(9): 1057. CrossRef - Triad of impairment in older people with diabetes-reciprocal relations and clinical implications
A.H. Abdelhafiz, P.C. Davies, A.J. Sinclair
Diabetes Research and Clinical Practice.2020; 161: 108065. CrossRef - Physical activity and exercise: Strategies to manage frailty
Javier Angulo, Mariam El Assar, Alejandro Álvarez-Bustos, Leocadio Rodríguez-Mañas
Redox Biology.2020; 35: 101513. CrossRef - Handgrip measurement as a useful benchmark for locomotive syndrome in patients with type 2 diabetes mellitus: A KAMOGAWA‐DM cohort study
Noriyuki Kitagawa, Takuro Okamura, Nobuko Kitagawa, Yoshitaka Hashimoto, Masahide Hamaguchi, Michiaki Fukui
Journal of Diabetes Investigation.2020; 11(6): 1602. CrossRef - Edmonton frail score is associated with diabetic control in elderly type 2 diabetic subjects
Satilmis Bilgin, Gulali Aktas, Ozge Kurtkulagi, Burcin M. Atak, Tuba T. Duman
Journal of Diabetes & Metabolic Disorders.2020; 19(1): 511. CrossRef - Comparison of field- and laboratory-based estimates of muscle quality index between octogenarians and young older adults: an observational study
Dahan da Cunha Nascimento, Jonato Prestes, Joyce de Sousa Diniz, Pedro Rodrigues Beal, Vicente Paulo Alves, Whitley Stone, Fabiani Lage Rodrigues Beal
Journal of Exercise Rehabilitation.2020; 16(5): 458. CrossRef - Tip 2 Diyabetli Hastalarda Kan Glukoz Seviyesi ile Kas Gücü, Propriosepsiyon ve Vücut Kompozisyonu Arasındaki İlişki
Zahide Betül TAYFUR, Esra ATILGAN
Turkish Journal of Diabetes and Obesity.2020; 4(3): 207. CrossRef - Challenges and Strategies for Diabetes Management in Community-Living Older Adults
Alan J. Sinclair, Ahmed H. Abdelhafiz
Diabetes Spectrum.2020; 33(3): 217. CrossRef - Association between deterioration in muscle strength and peripheral neuropathy in people with diabetes
Tae Jung Oh, Sunyoung Kang, Jie-Eun Lee, Jae Hoon Moon, Sung Hee Choi, Soo Lim, Hak Chul Jang
Journal of Diabetes and its Complications.2019; 33(8): 598. CrossRef - The Association between Body Composition using Dual energy X-ray Absorptiometry and Type-2 Diabetes: A Systematic Review and Meta-Analysis of Observational studies
Preeti Gupta, Carla Lanca, Alfred T. L. Gan, Pauline Soh, Sahil Thakur, Yijin Tao, Neelam Kumari, Ryan E. K. Man, Eva K. Fenwick, Ecosse L. Lamoureux
Scientific Reports.2019;[Epub] CrossRef - MECHANISMS OF ENDOCRINE DISEASE: Sarcopenia in endocrine and non-endocrine disorders
Victoria Zeghbi Cochenski Borba, Tatiana Lemos Costa, Carolina Aguiar Moreira, Cesar Luiz Boguszewski
European Journal of Endocrinology.2019; 180(5): R185. CrossRef - Hyperglycemia induces skeletal muscle atrophy via a WWP1/KLF15 axis
Yu Hirata, Kazuhiro Nomura, Yoko Senga, Yuko Okada, Kenta Kobayashi, Shiki Okamoto, Yasuhiko Minokoshi, Michihiro Imamura, Shin’ichi Takeda, Tetsuya Hosooka, Wataru Ogawa
JCI Insight.2019;[Epub] CrossRef - Hyperglycemia in non‐obese patients with type 2 diabetes is associated with low muscle mass: The Multicenter Study for Clarifying Evidence for Sarcopenia in Patients with Diabetes Mellitus
Ken Sugimoto, Yasuharu Tabara, Hiroshi Ikegami, Yasunori Takata, Kei Kamide, Tome Ikezoe, Eri Kiyoshige, Yukako Makutani, Hiroshi Onuma, Yasuyuki Gondo, Kazunori Ikebe, Noriaki Ichihashi, Tadao Tsuboyama, Fumihiko Matsuda, Katsuhiko Kohara, Mai Kabayama,
Journal of Diabetes Investigation.2019; 10(6): 1471. CrossRef - Diabetic Peripheral Neuropathy as a Risk Factor for Sarcopenia
Tae Jung Oh, Yoojung Song, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 170. CrossRef - Diabetes and frailty
Mariam El Assar, Olga Laosa, Leocadio Rodríguez Mañas
Current Opinion in Clinical Nutrition & Metabolic Care.2019; 22(1): 52. CrossRef - Association of Glucose Fluctuations with Sarcopenia in Older Adults with Type 2 Diabetes Mellitus
Noriko Ogama, Takashi Sakurai, Shuji Kawashima, Takahisa Tanikawa, Haruhiko Tokuda, Shosuke Satake, Hisayuki Miura, Atsuya Shimizu, Manabu Kokubo, Shumpei Niida, Kenji Toba, Hiroyuki Umegaki, Masafumi Kuzuya
Journal of Clinical Medicine.2019; 8(3): 319. CrossRef - Diabetes in the elderly
Ahmed H. Abdelhafiz, Alan J. Sinclair
Medicine.2019; 47(2): 119. CrossRef - Diabetes and Muscle Dysfunction in Older Adults
Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 160. CrossRef - Factors influencing safe glucose-lowering in older adults with type 2 diabetes: A PeRsOn-centred ApproaCh To IndiVidualisEd (PROACTIVE) Glycemic Goals for older people
C.E. Hambling, K. Khunti, X. Cos, J. Wens, L. Martinez, P. Topsever, S. Del Prato, A. Sinclair, G. Schernthaner, G. Rutten, S. Seidu
Primary Care Diabetes.2019; 13(4): 330. CrossRef - Effects of resistance training on neuromuscular parameters in elderly with type 2 diabetes mellitus: A randomized clinical trial
Cíntia E. Botton, Daniel Umpierre, Anderson Rech, Lucinéia O. Pfeifer, Carlos L.F. Machado, Juliana L. Teodoro, Alexandre S. Dias, Ronei S. Pinto
Experimental Gerontology.2018; 113: 141. CrossRef - Management of Elderly Diabetes Patients Who Are Unable to Self-Care
Bok Rye Song
The Journal of Korean Diabetes.2018; 19(4): 232. CrossRef - Decreased Muscle Strength and Quality in Diabetes-Related Dementia
Akito Tsugawa, Yusuke Ogawa, Naoto Takenoshita, Yoshitsugu Kaneko, Hirokuni Hatanaka, Eriko Jaime, Raita Fukasawa, Haruo Hanyu
Dementia and Geriatric Cognitive Disorders Extra.2017; 7(3): 454. CrossRef - Diabetes and Sarcopenia
Dong Hyun Kim, Tae Yang Yu
The Journal of Korean Diabetes.2017; 18(4): 239. CrossRef - Frailty and sarcopenia - newly emerging and high impact complications of diabetes
Alan J. Sinclair, Ahmed H. Abdelhafiz, Leocadio Rodríguez-Mañas
Journal of Diabetes and its Complications.2017; 31(9): 1465. CrossRef - Association of diabetic retinopathy with both sarcopenia and muscle quality in patients with type 2 diabetes: a cross-sectional study
Tatsuya Fukuda, Ryotaro Bouchi, Takato Takeuchi, Yujiro Nakano, Masanori Murakami, Isao Minami, Hajime Izumiyama, Koshi Hashimoto, Takanobu Yoshimoto, Yoshihiro Ogawa
BMJ Open Diabetes Research & Care.2017; 5(1): e000404. CrossRef - Practical considerations for managing patients with diabetes and dementia
Michelle L Mair, Rohin Athavale, Ahmed H Abdelhafiz
Expert Review of Endocrinology & Metabolism.2017; 12(6): 429. CrossRef - Sarcopenia: An Endocrine Disorder?
Alexis McKee, John E. Morley, Alvin M. Matsumoto, Aaron Vinik
Endocrine Practice.2017; 23(9): 1143. CrossRef - Response: Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging (Diabetes Metab J 2016;40:140-6)
Ji Won Yoon, Hak Chul Jang
Diabetes & Metabolism Journal.2016; 40(3): 250. CrossRef - Salivary lactate dehydrogenase and aminotransferases in diabetic patients
Barbara Malicka, Katarzyna Skoskiewicz-Malinowska, Urszula Kaczmarek
Medicine.2016; 95(47): e5211. CrossRef - Explanatory models of muscle performance in acromegaly patients evaluated by knee isokinetic dynamometry: Implications for rehabilitation
Agnaldo José Lopes, Arthur Sá Ferreira, Evelyn Mendes Walchan, Mauricio Santos Soares, Priscila Santos Bunn, Fernando Silva Guimarães
Human Movement Science.2016; 49: 160. CrossRef - Letter: Hyperglycemia Is Associated with Impaired Muscle Quality in Older Men with Diabetes: The Korean Longitudinal Study on Health and Aging (Diabetes Metab J 2016;40:140-6)
Jun Sung Moon
Diabetes & Metabolism Journal.2016; 40(3): 248. CrossRef - Sarcopenia, Frailty, and Diabetes in Older Adults
Hak Chul Jang
Diabetes & Metabolism Journal.2016; 40(3): 182. CrossRef
- Downhill running and caloric restriction attenuate insulin resistance associated skeletal muscle atrophy via the promotion of M2-like macrophages through TRIB3-AKT pathway
- Appendicular Skeletal Muscle Mass and Insulin Resistance in an Elderly Korean Population: The Korean Social Life, Health and Aging Project-Health Examination Cohort
- Seung Won Lee, Yoosik Youm, Won Joon Lee, Wungrak Choi, Sang Hui Chu, Yeong-Ran Park, Hyeon Chang Kim
- Diabetes Metab J. 2015;39(1):37-45. Published online February 16, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.1.37
- 4,911 View
- 56 Download
- 89 Web of Science
- 80 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Increasing evidence supports an association between age-related loss of muscle mass and insulin resistance. However, the association has not been fully investigated in the general population. Thus, we investigated the association between appendicular skeletal muscle mass (ASM) and insulin resistance in an elderly Korean population.
Methods This cross-sectional study included 158 men (mean age, 71.8) and 241 women (mean age, 70.6) from the Korean Social Life, Health and Aging Project, which started in 2011. In this study, ASM was measured by bioelectrical impedance analysis and was analyzed in three forms: ASM (kg), ASM/height2 (kg/m2), and ASM/weight (%). The homeostasis model assessment of insulin resistance (HOMA-IR) was used as a measure of insulin resistance. The relationships between the ASM values and the HOMA-IR were investigated by multiple linear regression models.
Results The HOMA-IR was positively associated with ASM (β=0.43,
P <0.0001) and ASM/height2 (β=0.36,P <0.0001) when adjusted for sex and age. However, after additional adjustment for body weight, HOMA-IR was inversely associated with ASM (β=-0.43,P <0.001) and ASM/height2 (β=-0.30,P =0.001). Adjustment for other potential confounders did not change these associations. Conversely, HOMA-IR was consistently and inversely associated with ASM/weight before and after adjustment for other potential confounders.Conclusion Our results support the idea that lower skeletal muscle mass is independently associated with insulin resistance in older adults. When evaluating sarcopenia or muscle-related conditions in older adults, their whole body sizes also need to be considered.
-
Citations
Citations to this article as recorded by- Fat Accumulation and Elevated Free Fatty Acid Are Associated With Age-Related Glucose Intolerance: Bunkyo Health Study
Hitoshi Naito, Hideyoshi Kaga, Yuki Someya, Hiroki Tabata, Saori Kakehi, Tsubasa Tajima, Naoaki Ito, Nozomu Yamasaki, Motonori Sato, Satoshi Kadowaki, Daisuke Sugimoto, Yuya Nishida, Ryuzo Kawamori, Hirotaka Watada, Yoshifumi Tamura
Journal of the Endocrine Society.2024;[Epub] CrossRef - Skeletal Muscle Evaluation in Patients With Acromegaly
Angelo Milioto, Giuliana Corica, Federica Nista, Luiz Eduardo Armondi Wildemberg, Federica Rossi, Bianca Bignotti, Mônica R Gadelha, Diego Ferone, Alberto Stefano Tagliafico, Federico Gatto
Journal of the Endocrine Society.2024;[Epub] CrossRef - Muscle attenuation, not skeletal muscle index, is an independent prognostic factor for survival in gastric cancer patients with overweight and obesity
Cheng-Le Zhuang, Hao-Fan Wu, Hao-Jie Jiang, Feng-Min Zhang, Han-Ping Shi, Zhen Yu, Xian Shen, Xiao-Lei Chen, Su-Lin Wang
Nutrition.2024; 122: 112391. CrossRef - Association between soft drink consumption and carotid atherosclerosis in a large-scale adult population: The TCLSIH cohort study
Ge Meng, Tongfeng Liu, Sabina Rayamajhi, Amrish Thapa, Shunming Zhang, Xuena Wang, Hongmei Wu, Yeqing Gu, Qing Zhang, Li Liu, Shaomei Sun, Xing Wang, Ming Zhou, Qiyu Jia, Kun Song, Zhongze Fang, Kaijun Niu
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(11): 2209. CrossRef - Sarcopenia is Associated With Oncological Prognosis and the Incidence of Secondary Cancer in Patients With Middle/Lower Rectal Cancer
Shinya Abe, Hiroaki Nozawa, Kazuhito Sasaki, Koji Murono, Shigenobu Emoto, Yuichiro Yokoyama, Hiroyuki Matsuzaki, Yuzo Nagai, Yuichiro Yoshioka, Takahide Shinagawa, Hirofumi Sonoda, Soichiro Ishihara
Clinical Colorectal Cancer.2023; 22(1): 143. CrossRef - Association between body mass index and reversion to normoglycemia from impaired fasting glucose among Chinese adults: a 5-year cohort study
Yong Han, Haofei Hu, Zhiqiang Huang, Dehong Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Changes in glycemic control and skeletal muscle mass indices after dapagliflozin treatment in individuals with type 1 diabetes mellitus
Yuta Yoshimura, Yoshitaka Hashimoto, Hiroshi Okada, Maya Takegami, Hanako Nakajima, Tomoki Miyoshi, Takashi Yoshimura, Masahiro Yamazaki, Masahide Hamaguchi, Michiaki Fukui
Journal of Diabetes Investigation.2023; 14(10): 1175. CrossRef - Triglyceride Glucose Index is Strongly Associated with a Fragility Fracture in Postmenopausal Elderly Females with Type 2 Diabetes Mellitus Combined with Osteoporosis: A 6-Year Follow-Up Study
Jiangmei Pan, Xiuxian Huang, Qiu Wang, Jingxia Sun, Zhenwei Zhai, Jiacheng Mo, Jianhao Huang, Wensheng Lu
Clinical Interventions in Aging.2023; Volume 18: 1841. CrossRef - Osteocalcin has a muscle-protective effect during weight loss in men without metabolic syndrome: a multicenter, prospective, observational study
Yi Xiang, Wenyi Lu, Xiaomeng Mao, Jing Zou, Jialu Wang, Renying Xu, Qingya Tang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Dual effects of insulin resistance on mortality and function in non-diabetic older adults: findings from the Toledo Study of Healthy Aging
Leocadio Rodríguez-Mañas, Javier Angulo, José A. Carnicero, Mariam El Assar, Francisco J. García-García, Alan J. Sinclair
GeroScience.2022; 44(2): 1095. CrossRef - Metabolically unhealthy individuals, either with obesity or not, have a higher risk of critical coronavirus disease 2019 outcomes than metabolically healthy individuals without obesity
Nam Hoon Kim, Kyeong Jin Kim, Jimi Choi, Sin Gon Kim
Metabolism.2022; 128: 154894. CrossRef - Prevalence and associated risk of advanced colorectal neoplasia in adults with sarcopenia
Min Cheol Kim, Kyeong Ok Kim, Min Kyu Kang
The Korean Journal of Internal Medicine.2022; 37(2): 294. CrossRef - Relationship between creatinine to body weight ratios and diabetes mellitus: A Chinese cohort study
Zhuangsen Chen, Yang Zou, Fan Yang, Xiao han Ding, Changchun Cao, Haofei Hu, Xinyu Wang
Journal of Diabetes.2022; 14(3): 167. CrossRef - Weight Trajectory Since Birth, Current Body Composition, Dietary Intake, and Glucose Tolerance in Young Underweight Japanese Women
Mika Takeuchi, Mari Honda, Ayaka Tsuboi, Satomi Minato-Inokawa, Miki Kurata, Bin Wu, Tsutomu Kazumi, Keisuke Fukuo
Women's Health Reports.2022; 3(1): 215. CrossRef - Advances in Phenotyping Obesity and in Its Dietary and Pharmacological Treatment: A Narrative Review
Roberta Pujia, Maria Grazia Tarsitano, Franco Arturi, Antonino De Lorenzo, Andrea Lenzi, Arturo Pujia, Tiziana Montalcini
Frontiers in Nutrition.2022;[Epub] CrossRef - Can Biological Drugs Diminish the Risk of Sarcopenia in Psoriatic Patients? A Systematic Review
Zuzanna Piętowska, Danuta Nowicka, Jacek Szepietowski
Life.2022; 12(3): 435. CrossRef - Association between total protein intake and low muscle mass in Korean adults
Youn Huh, Ki Young Son
BMC Geriatrics.2022;[Epub] CrossRef - Association between height-corrected appendicular and regional skeletal muscle mass and insulin resistance in patients with type 2 diabetes
Yoshikazu Hirasawa, Yoshiyuki Hamamoto
Journal of Physical Therapy Science.2022; 34(5): 353. CrossRef - Association between dietary inflammatory index score and muscle mass and strength in older adults: a study from National Health and Nutrition Examination Survey (NHANES) 1999–2002
Lingzhi Chen, Jingjing Ming, Tianyi Chen, James R. Hébert, Peng Sun, Li Zhang, Hongya Wang, Qingkuo Wu, Cancan Zhang, Nitin Shivappa, Bo Ban
European Journal of Nutrition.2022; 61(8): 4077. CrossRef - Effect of low skeletal muscle mass and sarcopenic obesity on chronic kidney disease in patients with type 2 diabetes
Da Hea Seo, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongha Seo, Seongbin Hong, Yong‐ho Lee, Young Ju Choi, Eunjig Lee, So Hun Kim
Obesity.2022; 30(10): 2034. CrossRef - Sex‐specific associations between gut microbiota and skeletal muscle mass in a population‐based study
Chul‐Hyun Park, Eun‐Ju Lee, Hyung‐Lae Kim, Yong‐Taek Lee, Kyung Jae Yoon, Han‐Na Kim
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(6): 2908. CrossRef - Impact of Low Skeletal Muscle Mass and Obesity on Hearing Loss in Asymptomatic Individuals: A Population-Based Study
Chul-Hyun Park, Kyung Jae Yoon, Yong-Taek Lee, Sung Min Jin, Sang Hyuk Lee, Tae Hwan Kim
Healthcare.2022; 10(10): 2022. CrossRef - Lower insulin level is associated with sarcopenia in community-dwelling frail and non-frail older adults
Yanxia Lu, Wee Shiong Lim, Xia Jin, Ma Schwe Zin Nyunt, Tamas Fulop, Qi Gao, Su Chi Lim, Anis Larbi, Tze Pin Ng
Frontiers in Medicine.2022;[Epub] CrossRef - Muscle alterations are independently associated with significant fibrosis in patients with nonalcoholic fatty liver disease
Yun‐Cheng Hsieh, Sae Kyung Joo, Bo Kyung Koo, Han‐Chieh Lin, Won Kim
Liver International.2021; 41(3): 494. CrossRef - A high lean body mass is not protecting from type 2 diabetes in the presence of a high body fat mass
Simo K.J. Rehunen, Hannu Kautiainen, Päivi E. Korhonen, Johan G. Eriksson
Diabetes & Metabolism.2021; 47(6): 101219. CrossRef - Abdominal aortic calcification is associated with decline in handgrip strength in the U.S. adult population ≥40 years of age
Robinson Ramírez-Vélez, Antonio García-Hermoso, María Correa-Rodríguez, Felipe Lobelo, Katherine González-Ruiz, Mikel Izquierdo
Nutrition, Metabolism and Cardiovascular Diseases.2021; 31(4): 1035. CrossRef - Association of metabolic syndrome with mobility in the older adults: a Korean nationwide representative cross-sectional study
Ki Young Son, Dong Wook Shin, Ji Eun Lee, Sang Hyuck Kim, Jae Moon Yun, Belong Cho
Scientific Reports.2021;[Epub] CrossRef - Low skeletal muscle mass is associated with liver fibrosis in individuals with type 2 diabetes and nonalcoholic fatty liver disease
Mohammad Shafi Kuchay, Narendra Singh Choudhary, Sakshi Gagneja, Anu Mathew, Tarannum Bano, Parjeet Kaur, Bajarang Bahadur, Manish Kumar Singh, Harmandeep Kaur Gill, Jasjeet Singh Wasir, Randhir Sud, Sunil Kumar Mishra
Journal of Gastroenterology and Hepatology.2021; 36(11): 3204. CrossRef - Association of obesity, visceral adiposity, and sarcopenia with an increased risk of metabolic syndrome: A retrospective study
Su Hwan Kim, Hyoun Woo Kang, Ji Bong Jeong, Dong Seok Lee, Dong-Won Ahn, Ji Won Kim, Byeong Gwan Kim, Kook Lae Lee, Sohee Oh, Soon Ho Yoon, Sang Joon Park, Mauro Lombardo
PLOS ONE.2021; 16(8): e0256083. CrossRef - Paradigm shift in gastrointestinal surgery − combating sarcopenia with prehabilitation: Multimodal review of clinical and scientific data
Frederick H Koh, Jason MW Chua, Joselyn LJ Tan, Fung-Joon Foo, Winson J Tan, Sharmini S Sivarajah, Leonard Ming Li Ho, Bin-Tean Teh, Min-Hoe Chew
World Journal of Gastrointestinal Surgery.2021; 13(8): 734. CrossRef - Concurrent Chemoradiotherapy Induces Body Composition Changes in Locally Advanced Head and Neck Squamous Cell Carcinoma: Comparison between Oral Cavity and Non-Oral Cavity Cancer
Yu-Ching Lin, Hang Huong Ling, Pei-Hung Chang, Yi-Ping Pan, Cheng-Hsu Wang, Wen-Chi Chou, Fang-Ping Chen, Kun-Yun Yeh
Nutrients.2021; 13(9): 2969. CrossRef - Low Skeletal Muscle Mass Is Associated With the Presence, Incidence, and Progression of Coronary Artery Calcification
Ji Eun Jun, Min Sun Choi, Sung Woon Park, Gyuri Kim, Sang-Man Jin, Kyunga Kim, You-Cheol Hwang, Kyu Jeung Ahn, Ho Yeon Chung, In-Kyung Jeong, Mira Kang, Jae Hyeon Kim
Canadian Journal of Cardiology.2021; 37(9): 1480. CrossRef - Association between Adjusted Handgrip Strength and Metabolic Syndrome in Arab Men
Shaea Alkahtani
International Journal of Environmental Research and Public Health.2021; 18(20): 10898. CrossRef - Association Between Low Muscle Mass and Non-alcoholic Fatty Liver Disease Diagnosed Using Ultrasonography, Magnetic Resonance Imaging Derived Proton Density Fat Fraction, and Comprehensive NAFLD Score in Korea
Hun Ju Lee, Jae Seung Chang, Jhii Hyun Ahn, Moon Young Kim, Kyu-Sang Park, Yeon-Soon Ahn, Sang Baek Koh
Journal of Preventive Medicine and Public Health.2021; 54(6): 412. CrossRef - Impact of Sarcopenia on the Risk of Erosive Esophagitis
Chan Mi Heo, Tae Jun Kim, Hyuk Lee, Jeung Hui Pyo, Yang Won Min, Byung-Hoon Min, Jun Haeng Lee, Hee Jung Son, Sun-Young Baek, Kyunga Kim, Seungho Ryu, Poong-Lyul Rhee, Jae J. Kim
The Korean Journal of Gastroenterology.2020; 75(3): 132. CrossRef - Handgrip Strength Among Korean Adolescents With Metabolic Syndrome in 2014–2015
Yunkoo Kang, Sowon Park, Seung Kim, Hong Koh
Journal of Clinical Densitometry.2020; 23(2): 271. CrossRef - Creatinine‐to‐bodyweight ratio is a predictor of incident non‐alcoholic fatty liver disease: A population‐based longitudinal study
Takuro Okamura, Yoshitaka Hashimoto, Masahide Hamaguchi, Akihiro Obora, Takao Kojima, Michiaki Fukui
Hepatology Research.2020; 50(1): 57. CrossRef - Physical performance and chronic kidney disease development in elderly adults: results from a nationwide cohort study
Young Su Joo, Jong Hyun Jhee, Hyung-Woo Kim, Seung Hyeok Han, Tae-Hyun Yoo, Shin-Wook Kang, Jung Tak Park
Aging.2020; 12(17): 17393. CrossRef - Decreased Appendicular Skeletal Muscle Mass is Associated with Poor Outcomes after ST-Segment Elevation Myocardial Infarction
Ryosuke Sato, Eiichi Akiyama, Masaaki Konishi, Yasushi Matsuzawa, Hiroyuki Suzuki, Chika Kawashima, Yuichiro Kimura, Kozo Okada, Nobuhiko Maejima, Noriaki Iwahashi, Kiyoshi Hibi, Masami Kosuge, Toshiaki Ebina, Stephan von Haehling, Stefan D. Anker, Kouich
Journal of Atherosclerosis and Thrombosis.2020; 27(12): 1278. CrossRef - Sarcopenia is associated with non-alcoholic fatty liver disease in men with type 2 diabetes
D.H. Seo, Y.-h. Lee, S.W. Park, Y.J. Choi, B.W. Huh, E. Lee, K.B. Huh, S.H. Kim, B.-S. Cha
Diabetes & Metabolism.2020; 46(5): 362. CrossRef - Associations of skeletal muscle mass with atherosclerosis and inflammatory markers in Korean adults
Soon-Kyu Yoon, Ha-Na Kim, Sang-Wook Song
Archives of Gerontology and Geriatrics.2020; 90: 104163. CrossRef - Lean body mass is not beneficial, but may be detrimental for glucose tolerance – Splitting body mass index according to body composition
Simo KJ Rehunen, Hannu Kautiainen, Päivi E Korhonen, Johan G Eriksson
Primary Care Diabetes.2020; 14(6): 747. CrossRef - Association between the Thigh Muscle and Insulin Resistance According to Body Mass Index in Middle-Aged Korean Adults
Ji Eun Heo, Jee-Seon Shim, Hokyou Lee, Hyeon Chang Kim
Diabetes & Metabolism Journal.2020; 44(3): 446. CrossRef - Independent and combined associations of cardiorespiratory fitness and muscle strength with metabolic syndrome in older adults: A cross-sectional study
Marcyo Câmara, Rodrigo Alberto Vieira Browne, Gabriel Costa Souto, Daniel Schwade, Ludmila Pereira Lucena Cabral, Geovani Araújo Dantas Macêdo, Luiz Fernando Farias-Junior, Fabíola Leite Gouveia, Telma Maria Araújo Moura Lemos, Kenio Costa Lima, Todd A. D
Experimental Gerontology.2020; 135: 110923. CrossRef - Sarcopenia and adverse health‐related outcomes: An umbrella review of meta‐analyses of observational studies
Lin Xia, Rui Zhao, Qianyi Wan, Yutao Wu, Yong Zhou, Yong Wang, Yaping Cui, Xiaoding Shen, Xiaoting Wu
Cancer Medicine.2020; 9(21): 7964. CrossRef - Impact of sarcopenia on the risk of advanced colorectal neoplasia
Ji Taek Hong, Tae Jun Kim, Jeung Hui Pyo, Eun Ran Kim, Sung Noh Hong, Young‐Ho Kim, Hyeon Seon Ahn, Insuk Sohn, Dong Kyung Chang
Journal of Gastroenterology and Hepatology.2019; 34(1): 162. CrossRef - Evaluation of muscle mass in obesity, prediabetes and diabetes mellitus by different equations used for the measurement of muscle mass
Mustafa Reşat Dabak, Elif Sevinç, Sabah Tüzün, Emine Özel Gün
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(3): 2148. CrossRef - Effect of Insulin Resistance on BMD and Fracture Risk in Older Adults
Nicola Napoli, Caterina Conte, Claudio Pedone, Elsa S Strotmeyer, Kamil E Barbour, Dennis M Black, Elizabeth J Samelson, Ann V Schwartz
The Journal of Clinical Endocrinology & Metabolism.2019; 104(8): 3303. CrossRef - Can 24 weeks strength training reduce feelings of depression and increase neurotransmitter in elderly females?
Yun-Sik Kim, David Michael O'Sullivan, Sang-Keun Shin
Experimental Gerontology.2019; 115: 62. CrossRef - The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(1): 46. CrossRef - Sarcopenic obesity and overall mortality: Results from the application of novel models of body composition phenotypes to the National Health and Nutrition Examination Survey 1999–2004
Carla Van Aller, Jose Lara, Blossom C.M. Stephan, Lorenzo Maria Donini, Steven Heymsfield, Peter T. Katzmarzyk, Jonathan C.K. Wells, Carla M. Prado, Mario Siervo
Clinical Nutrition.2019; 38(1): 264. CrossRef - Carbohydrate oxidation and glucose utilisation under hyperglycaemia in aged and young males during exercise at the same relative exercise intensity
James J. Malone, Minoo Bassami, Sarah C. Waldron, Iain T. Campbell, Andrew Hulton, Dominic Doran, Don P. MacLaren
European Journal of Applied Physiology.2019; 119(1): 235. CrossRef - Association of the muscle/fat mass ratio with insulin resistance in gestational diabetes mellitus
Shin Kawanabe, Yoshio Nagai, Yuta Nakamura, Ami Nishine, Tomoko Nakagawa, Yasushi Tanaka
Endocrine Journal.2019; 66(1): 75. CrossRef - Low muscle mass and inflammation among patients with type 2 diabetes mellitus in Indonesia
Perdana Samekto Tyasnugroho Suyoto, Bianda Aulia
Diabetology International.2019; 10(3): 219. CrossRef - Association of low skeletal muscle mass with advanced liver fibrosis in patients with non‐alcoholic fatty liver disease
Min Kyu Kang, Jung Gil Park, Heon Ju Lee, Min Cheol Kim
Journal of Gastroenterology and Hepatology.2019; 34(9): 1633. CrossRef - Evaluation of skeletal muscle mass indices, assessed by bioelectrical impedance, as indicators of insulin resistance in patients with type 2 diabetes
Yoshikazu Hirasawa, Ryosuke Matsuki, Toshihiko Ebisu, Takeshi Kurose, Yoshiyuki Hamamoto, Yutaka Seino
Journal of Physical Therapy Science.2019; 31(2): 190. CrossRef - Polycystic ovary syndrome is a risk factor for sarcopenic obesity: a case control study
Laura E. McBreairty, Philip D. Chilibeck, Julianne J. Gordon, Donna R. Chizen, Gordon A. Zello
BMC Endocrine Disorders.2019;[Epub] CrossRef - Role of hyperglycaemia in the relationship between serum osteocalcin levels and relative skeletal muscle index
Yiting Xu, Xiaojing Ma, Yun Shen, Chengchen Gu, Junling Tang, Yuqian Bao
Clinical Nutrition.2019; 38(6): 2704. CrossRef - Relationship Between Relative Skeletal Muscle Mass and Nonalcoholic Fatty Liver Disease: A 7‐Year Longitudinal Study
Gyuri Kim, Seung‐Eun Lee, You‐Bin Lee, Ji Eun Jun, Jiyeon Ahn, Ji Cheol Bae, Sang‐Man Jin, Kyu Yeon Hur, Jae Hwan Jee, Moon‐Kyu Lee, Jae Hyeon Kim
Hepatology.2018; 68(5): 1755. CrossRef - Relationships between 25(OH)D concentration, sarcopenia and HOMA-IR in postmenopausal Korean women
J. H. Lee, S. Kim, M. K. Kim, B. H. Yun, S. Cho, Y. S. Choi, B. S. Lee, S. K. Seo
Climacteric.2018; 21(1): 40. CrossRef - Is the Relationship between Depression and C Reactive Protein Level Moderated by Social Support in Elderly?-Korean Social Life, Health, and Aging Project (KSHAP)
Nam Wook Hur, Hyeon Chang Kim, Linda Waite, Yoosik Youm
Psychiatry Investigation.2018; 15(1): 24. CrossRef - Challenges in Treatment of Obesity in the Elderly
Ignacio Sajoux
Endocrinology&Metabolism International Journal.2017;[Epub] CrossRef - Mediterranean diet, Dietary Approaches to Stop Hypertension (DASH) style diet, and metabolic health in U.S. adults
Yong-Moon Mark Park, Susan E. Steck, Teresa T. Fung, Jiajia Zhang, Linda J. Hazlett, Kyungdo Han, Seung-Hwan Lee, Hyuk-Sang Kwon, Anwar T. Merchant
Clinical Nutrition.2017; 36(5): 1301. CrossRef - Sarcopenia is an independent risk factor for non-alcoholic steatohepatitis and significant fibrosis
Bo Kyung Koo, Donghee Kim, Sae Kyung Joo, Jung Ho Kim, Mee Soo Chang, Byeong Gwan Kim, Kook Lae Lee, Won Kim
Journal of Hepatology.2017; 66(1): 123. CrossRef - Low muscle mass and risk of type 2 diabetes in middle-aged and older adults: findings from the KoGES
Jang Won Son, Seong Su Lee, Sung Rae Kim, Soon Jib Yoo, Bong Yun Cha, Ho Young Son, Nam H. Cho
Diabetologia.2017; 60(5): 865. CrossRef - Factors Associated with Insomnia among the Elderly in a Korean Rural Community
Woo Jung Kim, Won-tak Joo, Jiwon Baek, Sung Yun Sohn, Kee Namkoong, Yoosik Youm, Hyeon Chang Kim, Yeong-Ran Park, Sang Hui Chu, Eun Lee
Psychiatry Investigation.2017; 14(4): 400. CrossRef - Differential association between sarcopenia and metabolic phenotype in Korean young and older adults with and without obesity
You‐Cheol Hwang, In‐Jin Cho, In‐Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
Obesity.2017; 25(1): 244. CrossRef - Association of physical activity on body composition, cardiometabolic risk factors, and prevalence of cardiovascular disease in the Korean population (from the fifth Korea national health and nutrition examination survey, 2008–2011)
Gwang-Sil Kim, Eui Im, Ji-Hyuck Rhee
BMC Public Health.2017;[Epub] CrossRef - Low skeletal muscle mass is associated with non-alcoholic fatty liver disease in Korean adults: the Fifth Korea National Health and Nutrition Examination Survey
Hee Yeon Kim, Chang Wook Kim, Chung-Hwa Park, Jong Young Choi, Kyungdo Han, Anwar T Merchant, Yong-Moon Park
Hepatobiliary & Pancreatic Diseases International.2016; 15(1): 39. CrossRef - Frailty and sarcopenia as the basis for the phenotypic manifestation of chronic diseases in older adults
Javier Angulo, Mariam El Assar, Leocadio Rodríguez-Mañas
Molecular Aspects of Medicine.2016; 50: 1. CrossRef - Importance of Lean Muscle Maintenance to Improve Insulin Resistance by Body Weight Reduction in Female Patients with Obesity
Yaeko Fukushima, Satoshi Kurose, Hiromi Shinno, Ha Cao Thu, Nana Takao, Hiromi Tsutsumi, Yutaka Kimura
Diabetes & Metabolism Journal.2016; 40(2): 147. CrossRef - Difference between old and young adults in contribution of β‐cell function and sarcopenia in developing diabetes mellitus
Bo Kyung Koo, Eun Roh, Ye Seul Yang, Min Kyong Moon
Journal of Diabetes Investigation.2016; 7(2): 233. CrossRef - Association between serum triglyceride to high-density lipoprotein cholesterol ratio and sarcopenia in elderly Korean males: The Korean National Health and Nutrition Examination Survey
Tae-Ha Chung, Yu-Jin Kwon, Jae-Yong Shim, Yong-Jae Lee
Clinica Chimica Acta.2016; 463: 165. CrossRef - Association between leukocyte count and sarcopenia in postmenopausal women: The Korean National Health and Nutrition Examination Survey
Tae-Ha Chung, Jae-Yong Shim, Yong-Jae Lee
Maturitas.2016; 84: 89. CrossRef - Low Relative Lean Mass is Associated with Increased Likelihood of Abdominal Aortic Calcification in Community-Dwelling Older Australians
Alexander J. Rodríguez, David Scott, Belal Khan, Nayab Khan, Allison Hodge, Dallas R. English, Graham G. Giles, Peter R. Ebeling
Calcified Tissue International.2016; 99(4): 340. CrossRef - Sarcopenia and the cardiometabolic syndrome: A narrative review
G. Bahat, B. İlhan
European Geriatric Medicine.2016; 7(3): 220. CrossRef - Decreased β-Cell Function Is Associated with Reduced Skeletal Muscle Mass in Japanese Subjects without Diabetes
Satoshi Sakai, Keiji Tanimoto, Ayumi Imbe, Yuiko Inaba, Kanako Shishikura, Yoshimi Tanimoto, Takahisa Ushiroyama, Jungo Terasaki, Toshiaki Hanafusa, Marta Letizia Hribal
PLOS ONE.2016; 11(9): e0162603. CrossRef - Differences among skeletal muscle mass indices derived from height-, weight-, and body mass index-adjusted models in assessing sarcopenia
Kyoung Min Kim, Hak Chul Jang, Soo Lim
The Korean Journal of Internal Medicine.2016; 31(4): 643. CrossRef - Low muscle mass is associated with metabolic syndrome only in nonobese young adults: the Korea National Health and Nutrition Examination Survey 2008-2010
Byung Chul Kim, Mee Kyoung Kim, Kyungdo Han, Sae-Young Lee, Seung-Hwan Lee, Seung-Hyun Ko, Hyuk-Sang Kwon, Anwar T. Merchant, Hyeon Woo Yim, Won-Chul Lee, Yong Gyu Park, Yong-Moon Park
Nutrition Research.2015; 35(12): 1070. CrossRef - Insulin Resistance Is Associated with Prevalence of Physician-Diagnosed Urinary Incontinence in Postmenopausal Non-Diabetic Adult Women: Data from the Fourth Korea National Health and Nutrition Examination Survey
Byung Il Yoon, Kyung-Do Han, Kyu Won Lee, Hyuk Sang Kwon, Sun Wook Kim, Dong Wan Sohn, Yong-Hyun Cho, U-Syn Ha, Tatsuo Shimosawa
PLOS ONE.2015; 10(11): e0141720. CrossRef
- Fat Accumulation and Elevated Free Fatty Acid Are Associated With Age-Related Glucose Intolerance: Bunkyo Health Study
- Management of Type 2 Diabetes Mellitus in Older Adults
- Kyung Soo Kim, Soo Kyung Kim, Kyung Mi Sung, Yong Wook Cho, Seok Won Park
- Diabetes Metab J. 2012;36(5):336-344. Published online October 18, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.5.336
- 5,794 View
- 71 Download
- 42 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader In the near future, the majority of patients with diabetes will be adults aged 65 or older. Unlike young adults with diabetes, elderly diabetic people may be affected by a variety of comorbid conditions such as depression, cognitive impairment, muscle weakness (sarcopenia), falls and fractures, and physical frailty. These geriatric syndromes should be considered in the establishment of treatment goals in older adults with diabetes. Although there are several guidelines for the management of diabetes, only a few are specifically designed for the elderly with diabetes. In this review, we present specific conditions of elderly diabetes which should be taken into account in the management of diabetes in older adults. We also present advantages and disadvantages of various glucose-lowering agents that should be considered when choosing a proper regimen for older adults with diabetes.
-
Citations
Citations to this article as recorded by- Circulating sestrins and force velocity profiling in older adults with type 2 diabetes
Raquel González‐Martos, Raquel Aparicio‐Ugarriza, Julian Alcazar, Carmen Ramirez‐Castillejo, Dace Reihmane, Adrian Menéndez‐Rey, Marcela González‐Gross, Amelia Guadalupe‐Grau
European Journal of Sport Science.2023; 23(8): 1710. CrossRef - Glucose Sensors Based on Chitosan Capped ZnS Doped Mn Nanomaterials
Son Hai Nguyen, Phan Kim Thi Vu, Mai Thi Tran
IEEE Sensors Letters.2023; 7(2): 1. CrossRef - Inhibitory Potential of α-Amylase, α-Glucosidase, and Pancreatic Lipase by a Formulation of Five Plant Extracts: TOTUM-63
Quentin Haguet, Florian Le Joubioux, Vivien Chavanelle, Hugo Groult, Nathan Schoonjans, Cédric Langhi, Arnaud Michaux, Yolanda F. Otero, Nathalie Boisseau, Sébastien L. Peltier, Pascal Sirvent, Thierry Maugard
International Journal of Molecular Sciences.2023; 24(4): 3652. CrossRef - Optical Glucose Sensors Based on Chitosan-Capped ZnS-Doped Mn Nanomaterials
Son Hai Nguyen, Phan Kim Thi Vu, Hung Manh Nguyen, Mai Thi Tran
Sensors.2023; 23(5): 2841. CrossRef - Meta‐analysis of factors associated with antidiabetic drug prescribing for type 2 diabetes mellitus
Fatema Mahmoud, Alexander Mullen, Chris Sainsbury, Gordon F. Rushworth, Haya Yasin, Nouf Abutheraa, Tanja Mueller, Amanj Kurdi
European Journal of Clinical Investigation.2023;[Epub] CrossRef - Efficacy and safety of oral semaglutide by baseline age in Japanese patients with type 2 diabetes: A subgroup analysis of the PIONEER 9 and 10 Japan trials
Yuichiro Yamada, Daisuke Yabe, Christin Løth Hertz, Hiroshi Horio, Jiro Nakamura, Anne Møller Nielsen, Yutaka Seino
Diabetes, Obesity and Metabolism.2022; 24(2): 321. CrossRef - A Low Free T3 to Free T4 Ratio Is Associated with Sarcopenia in Euthyroid Patients with Type 2 Diabetes Mellitus
Kewei Wang, Di Zhang, Guanglei Cao, Chuan Wang, Lingshu Wang, Ruxing Zhao, Qin He, Xinguo Hou, Lei Gong, Li Chen, Antonio Brunetti
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Relationship between Nutrition-Related Problems and Falls in Hemodialysis Patients: A Narrative Review
Nobuyuki Shirai, Tatsuro Inoue, Masato Ogawa, Masatsugu Okamura, Shinichiro Morishita, Yamamoto Suguru, Atsuhiro Tsubaki
Nutrients.2022; 14(15): 3225. CrossRef - Education for Insulin Injection in Elderly Diabetic Patients
Gi Yeon Lee
The Journal of Korean Diabetes.2022; 23(3): 201. CrossRef - Diabetes Mellitus: Insights from Epidemiology, Biochemistry, Risk Factors, Diagnosis, Complications and Comprehensive Management
Saruar Alam, Md. Kamrul Hasan, Sharif Neaz, Nazmul Hussain, Md. Faruk Hossain, Tania Rahman
Diabetology.2021; 2(2): 36. CrossRef - Characteristics of the clinical treatment of Brazilian and French older adults with diabetes
Carina Bandeira Bezerra, Claudio de Brito Ramos Pinto Pinho, Maria Vieira de Lima Saintrain, Ana Karina de Melo Bezerra Sodré, Carlos Antonio Bruno da Silva, Jean Doucet
Diabetes Research and Clinical Practice.2021; 181: 109088. CrossRef - Changes in treatment for NSTEMI in women and the elderly over the past 16 years in a large real-world population
Leonhard Riehle, Birga Maier, Steffen Behrens, Leonhard Bruch, Ralph Schoeller, Helmut Schühlen, Martin Stockburger, Heinz Theres, David M. Leistner, Ulf Landmesser, Georg M. Fröhlich
International Journal of Cardiology.2020; 316: 7. CrossRef - Association of traditional and novel measures of central obesity with cognitive performance in older multi‐ethnic Asians with type 2 diabetes
Mei Chung Moh, Serena Low, Tze Pin Ng, Jiexun Wang, Su Fen Ang, Clara Tan, Keven Ang, Subramaniam Tavintharan, Chee Fang Sum, Pek Yee Kwan, Simon Biing Ming Lee, Wern Ee Tang, Su Chi Lim
Clinical Obesity.2020;[Epub] CrossRef - Potentially Inappropriate Medication Use in Older Hospitalized Patients with Type 2 Diabetes: A Cross-Sectional Study
Rishabh Sharma, Manik Chhabra, Kota Vidyasagar, Muhammed Rashid, Daniela Fialova, Akshaya S. Bhagavathula
Pharmacy.2020; 8(4): 219. CrossRef - A Study of Fall Risk Assessment in Elderly Patients Based on Diabetes and its Significance
Tanuka Mandal, Sanjit Mal, Purbasha Biswas
Bengal Physician Journal.2020; 7(2): 26. CrossRef - De-Intensification of Diabetes Treatment in Elderly Patients with Type 2 Diabetes Mellitus
Daniela V. Pirela, Rajesh Garg
Endocrine Practice.2019; 25(12): 1317. CrossRef - Cognitive Function and Falls in Older Adults With Type 2 Diabetes Mellitus
Jennifer Blackwood
Journal of Geriatric Physical Therapy.2019; 42(4): E91. CrossRef - Managing the Elderly Emergency Department Patient
Christina L. Shenvi, Timothy F. Platts-Mills
Annals of Emergency Medicine.2019; 73(3): 302. CrossRef - Diabetes Management in Older Adults With Chronic Kidney Disease
Kristin K. Clemens, Niamh O’Regan, Jinnie J. Rhee
Current Diabetes Reports.2019;[Epub] CrossRef - Higher Prevalence and Progression Rate of Chronic Kidney Disease in Elderly Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Seok Won Park, Yong-Wook Cho, Soo-Kyung Kim
Diabetes & Metabolism Journal.2018; 42(3): 224. CrossRef - Goal Attainment Rate for Parameters of Metabolic Adjustment in Elderly Patients with Type 2 Diabetes Taking a Hypoglycemic Agent
Kang Hee Shim, Moon Sook Hwang, Jeong Eun Park, Jin Hee Jung, Jung Hwa Lee, Bok Rye Song
The Journal of Korean Diabetes.2018; 19(1): 58. CrossRef - Similar Efficacy and Safety of Basaglar® and Lantus® in Patients with Type 2 Diabetes in Age Groups (< 65 Years, ≥ 65 Years): A Post Hoc Analysis from the ELEMENT-2 Study
Robyn K. Pollom, Timothy Costigan, Lyndon B. Lacaya, Liza L. Ilag, Priscilla A. Hollander
Diabetes Therapy.2018; 9(2): 827. CrossRef - Association of metabolic syndrome and 25‐hydroxyvitamin D with cognitive impairment among elderly Koreans
Eun Young Lee, Su Jin Lee, Kyoung Min Kim, Young Mi Yun, Bo Mi Song, Jong Eun Kim, Hyeon Chang Kim, Yumie Rhee, Yoosik Youm, Chang Oh Kim
Geriatrics & Gerontology International.2017; 17(7): 1069. CrossRef - Satisfaction Survey on Information Technology-Based Glucose Monitoring System Targeting Diabetes Mellitus in Private Local Clinics in Korea
Hun-Sung Kim, So Jung Yang, Yoo Jin Jeong, Young-Eun Kim, Seok-Won Hong, Jae Hyoung Cho
Diabetes & Metabolism Journal.2017; 41(3): 213. CrossRef - Self-managing type 2 diabetes is a unique challenge for older patients. A systematic review and thematic synthesis of barriers and facilitators
Julia Menichetti, Pietro Cipresso, Elena Vegni, Guendalina Graffigna
PSICOLOGIA DELLA SALUTE.2017; (2): 97. CrossRef - Prevalence and treatment of diabetes mellitus and hypertension among older adults with intellectual disability in comparison with the general population
Anna Axmon, Gerd Ahlström, Peter Höglund
BMC Geriatrics.2017;[Epub] CrossRef - Self-care competence in the administration of insulin in older people aged 70 or over
Mayara Sousa Vianna, Patrícia Aparecida Barbosa Silva, Cíntia Vieira do Nascimento, Sônia Maria Soares
Revista Latino-Americana de Enfermagem.2017;[Epub] CrossRef - Prevention of Falls and Frailty in Older Adults with Diabetes
Helen P. Hazuda, Sara E. Espinoza
Current Geriatrics Reports.2017; 6(3): 158. CrossRef - Inadequate glycaemic control and therapeutic management of adults over 65 years old with type 2 diabetes mellitus in Spain
Francesc Formiga, J. Franch-Nadal, L. Rodriguez, L. Ávila, E. Fuster
The Journal of nutrition, health and aging.2017; 21(10): 1365. CrossRef - Insulin provision therapy and mortality in older adults with diabetes mellitus and stable ischemic heart disease: Insights from BARI-2D trial
Abdulla A. Damluji, Erin R. Cohen, Mauro Moscucci, Robert J. Myerburg, Mauricio G. Cohen, Maria M. Brooks, Michael W. Rich, Daniel E. Forman
International Journal of Cardiology.2017; 241: 35. CrossRef - Comparison of Age of Onset and Frequency of Diabetic Complications in the Very Elderly Patients with Type 2 Diabetes
Bong-Ki Lee, Sang-Wook Kim, Daehee Choi, Eun-Hee Cho
Endocrinology and Metabolism.2016; 31(3): 416. CrossRef - Efficacy and safety of teneligliptin, a novel dipeptidyl peptidase‐4 inhibitor, in Korean patients with type 2 diabetes mellitus: a 24‐week multicentre, randomized, double‐blind, placebo‐controlled phase III trial
S. Hong, C.‐Y. Park, K. A. Han, C. H. Chung, B. J. Ku, H. C. Jang, C. W. Ahn, M.‐K. Lee, M. K. Moon, H. S. Son, C. B. Lee, Y.‐W. Cho, S.‐W. Park
Diabetes, Obesity and Metabolism.2016; 18(5): 528. CrossRef - Diabetes mellitus and risk of falls in older adults: a systematic review and meta-analysis
Yu Yang, Xinhua Hu, Qiang Zhang, Rui Zou
Age and Ageing.2016; 45(6): 761. CrossRef - Prevalence and risk factors of chronic complications of type 2 diabetic inpatients in Hubei Province of central China: results from a multiple-hospital study
Hu Xiao, Ai-Ming Du, Peng Yun, Hui-Fang Zhang, Yuan Tian, Fang-Xi Xiao
International Journal of Diabetes in Developing Countries.2016; 36(2): 242. CrossRef - Transcultural Diabetes Nutrition Algorithm: Brazilian Application
Fabio Moura, João Salles, Osama Hamdy, Walmir Coutinho, Deise Baptista, Alexander Benchimol, Albert Marchetti, Refaat Hegazi, Jeffrey Mechanick
Nutrients.2015; 7(9): 7358. CrossRef - Relationship between sarcopenia and nonalcoholic fatty liver disease: The Korean Sarcopenic Obesity Study
Ho Cheol Hong, Soon Young Hwang, Hae Yoon Choi, Hye Jin Yoo, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Dong Seop Choi, Kyung Mook Choi
Hepatology.2014; 59(5): 1772. CrossRef - Relationship between Serum Ferritin Levels and Sarcopenia in Korean Females Aged 60 Years and Older Using the Fourth Korea National Health and Nutrition Examination Survey (KNHANES IV-2, 3), 2008–2009
Tae Ho Kim, Hee-Jin Hwang, Sang-Hwan Kim, Stefan Kiechl
PLoS ONE.2014; 9(2): e90105. CrossRef - Using mobile phones in healthcare management for the elderly
Hun-Sung Kim, Kye-Hwa Lee, Hyunah Kim, Ju Han Kim
Maturitas.2014; 79(4): 381. CrossRef - Type 2 diabetes is associated with low muscle mass in older adults
Kyung‐Soo Kim, Kyung‐Sun Park, Moon‐Jong Kim, Soo‐Kyung Kim, Yong‐Wook Cho, Seok Won Park
Geriatrics & Gerontology International.2014; 14(S1): 115. CrossRef - The Appropriateness of the Length of Insulin Needles Based on Determination of Skin and Subcutaneous Fat Thickness in the Abdomen and Upper Arm in Patients with Type 2 Diabetes
Kang Hee Sim, Moon Sook Hwang, Sun Young Kim, Hye Mi Lee, Ji Yeun Chang, Moon Kyu Lee
Diabetes & Metabolism Journal.2014; 38(2): 120. CrossRef - Nutrición y enfermedades metabólicas en el anciano. Estrategias alimentarias
L. Guardado Fuentes, I. Carmona Álvarez, F. Cuesta Triana
Medicine - Programa de Formación Médica Continuada Acreditado.2014; 11(62): 3691. CrossRef - A Growing Troubling Triad: Diabetes, Aging, and Falls
Ryan T. Crews, Sai V. Yalla, Adam E. Fleischer, Stephanie C. Wu
Journal of Aging Research.2013; 2013: 1. CrossRef
- Circulating sestrins and force velocity profiling in older adults with type 2 diabetes

 KDA
KDA
 First
First Prev
Prev





