
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
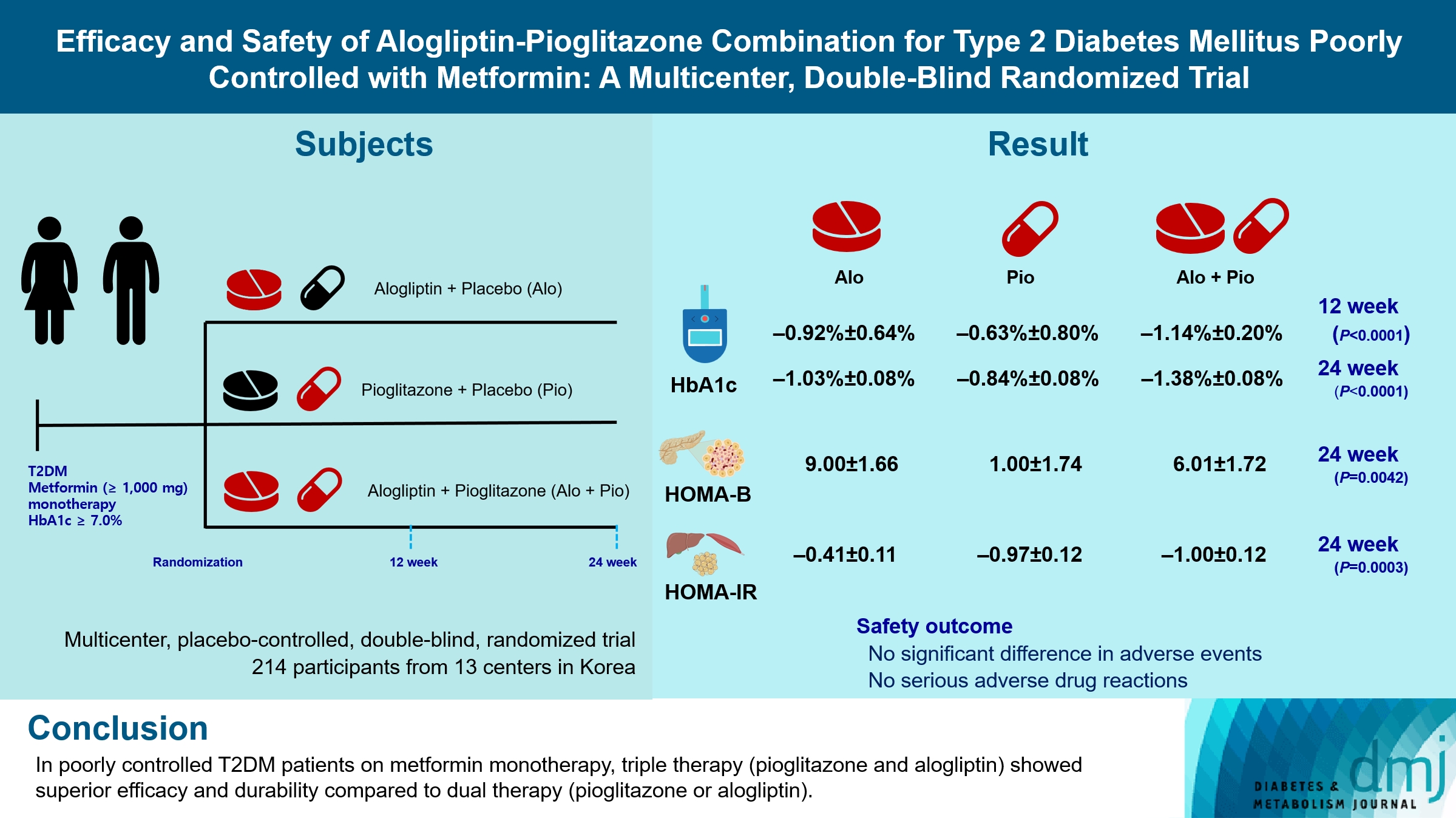
- Efficacy and Safety of Alogliptin-Pioglitazone Combination for Type 2 Diabetes Mellitus Poorly Controlled with Metformin: A Multicenter, Double-Blind Randomized Trial
- Ji-Yeon Park, Joonyub Lee, Yoon-Hee Choi, Kyung Wan Min, Kyung Ah Han, Kyu Jeung Ahn, Soo Lim, Young-Hyun Kim, Chul Woo Ahn, Kyung Mook Choi, Kun-Ho Yoon, the Practical Evidence of Antidiabetic Combination Therapy in Korea (PEAK) study investigators
- Received August 7, 2023 Accepted November 30, 2023 Published online April 23, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0259 [Epub ahead of print]
- 269 View
- 14 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Guidelines for switching to triple combination therapy directly after monotherapy failure are limited. This study investigated the efficacy, long-term sustainability, and safety of either mono or dual add-on therapy using alogliptin and pioglitazone for patients with type 2 diabetes mellitus (T2DM) who did not achieve their target glycemic range with metformin monotherapy.
Methods
The Practical Evidence of Antidiabetic Combination Therapy in Korea (PEAK) was a multicenter, placebo-controlled, double-blind, randomized trial. A total of 214 participants were randomized to receive alogliptin+pioglitazone (Alo+Pio group, n=70), alogliptin (Alo group, n=75), or pioglitazone (Pio group, n=69). The primary outcome was the difference in glycosylated hemoglobin (HbA1c) levels between the three groups at baseline to 24 weeks. For durability, the achievement of HbA1c levels <7% and <6.5% was compared in each group. The number of adverse events was investigated for safety.
Results
After 24 weeks of treatment, the change of HbA1c in the Alo+Pio, Alo, and Pio groups were –1.38%±0.08%, –1.03%±0.08%, and –0.84%±0.08%, respectively. The Alo+Pio group had significantly lower HbA1c levels than the other groups (P=0.0063, P<0.0001) and had a higher proportion of patients with target HbA1c achievement. In addition, insulin sensitivity and β-cell function, lipid profiles, and other metabolic indicators were also improved. There were no significant safety issues in patients treated with triple combination therapy.
Conclusion
Early combination triple therapy showed better efficacy and durability than the single add-on (dual) therapy. Therefore, combination therapy with metformin, alogliptin, and pioglitazone is a valuable early treatment option for T2DM poorly controlled with metformin monotherapy.
- Complications
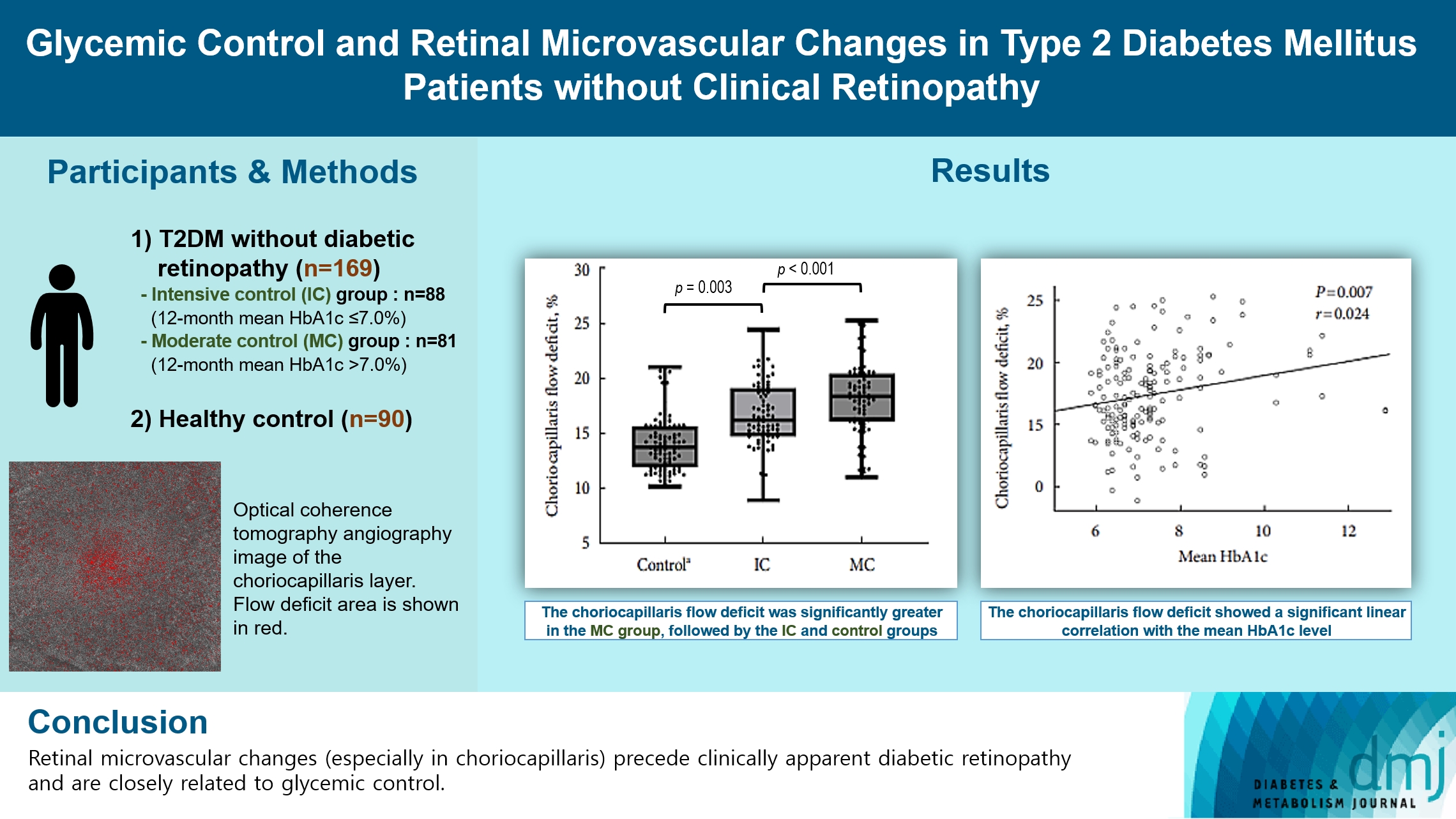
- Glycemic Control and Retinal Microvascular Changes in Type 2 Diabetes Mellitus Patients without Clinical Retinopathy
- Kangmin Lee, Ga Hye Lee, Seung Eun Lee, Jee Myung Yang, Kunho Bae
- Received May 15, 2023 Accepted December 15, 2023 Published online March 13, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0149 [Epub ahead of print]
- 635 View
- 34 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the association of glycemic control and retinal microvascular changes in patients with type 2 diabetes mellitus (T2DM) without diabetic retinopathy (DR).
Methods
This retrospective, observational, cohort study included patients with T2DM without DR. The patients were categorized into intensive control (IC; mean glycosylated hemoglobin [HbA1c] ≤7.0%) and moderate control (MC; mean HbA1c >7.0%) groups. Optical coherence tomography (OCT) and swept-source OCT angiography (OCTA) image parameters were compared between three groups, including healthy controls.
Results
In total, 259 eyes of 259 participants (88 IC, 81 MC, and 90 controls) were included. The foveal avascular zone area was significantly larger in the MC group than IC and control groups (all P<0.05). The IC group had lower vessel density in the superficial retinal layer and deep retinal layer than the controls (all P<0.05). The choriocapillaris (CC) flow deficit (FD) was significantly greater in the MC group than in the IC and control groups (18.2%, 16.7%, and 14.2%, respectively; all P<0.01). In multivariate regression analysis, CC-FD was associated with the mean HbA1c level (P=0.008). There were no significant differences in OCT parameters among the groups.
Conclusion
OCTA revealed that early CC impairment is associated with HbA1c levels; the CC changes precede clinically apparent DR. The OCTA parameters differed among the groups according to the degree of glycemic control. Our results suggest that microvascular changes precede DR and are closely related to glycemic control.
- Metabolic Risk/Epidemiology
- Glycemic Control Is Associated with Histological Findings of Nonalcoholic Fatty Liver Disease
- Teruki Miyake, Shinya Furukawa, Bunzo Matsuura, Osamu Yoshida, Masumi Miyazaki, Akihito Shiomi, Ayumi Kanamoto, Hironobu Nakaguchi, Yoshiko Nakamura, Yusuke Imai, Mitsuhito Koizumi, Takao Watanabe, Yasunori Yamamoto, Yohei Koizumi, Yoshio Tokumoto, Masashi Hirooka, Teru Kumagi, Eiji Takesita, Yoshio Ikeda, Masanori Abe, Yoichi Hiasa
- Received June 24, 2023 Accepted September 21, 2023 Published online February 2, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0200 [Epub ahead of print]

- 935 View
- 40 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Poor lifestyle habits may worsen nonalcoholic fatty liver disease (NAFLD), with progression to nonalcoholic steatohepatitis (NASH) and cirrhosis. This study investigated the association between glycemic control status and hepatic histological findings to elucidate the effect of glycemic control on NAFLD.
Methods
This observational study included 331 patients diagnosed with NAFLD by liver biopsy. Effects of the glycemic control status on histological findings of NAFLD were evaluated by comparing the following four glycemic status groups defined by the glycosylated hemoglobin (HbA1c) level at the time of NAFLD diagnosis: ≤5.4%, 5.5%–6.4%, 6.5%–7.4%, and ≥7.5%.
Results
Compared with the lowest HbA1c group (≤5.4%), the higher HbA1c groups (5.5%–6.4%, 6.5%–7.4%, and ≥7.5%) were associated with advanced liver fibrosis and high NAFLD activity score (NAS). On multivariate analysis, an HbA1c level of 6.5%– 7.4% group was significantly associated with advanced fibrosis compared with the lowest HbA1c group after adjusting for age, sex, hemoglobin, alanine aminotransferase, and creatinine levels. When further controlling for body mass index and uric acid, total cholesterol, and triglyceride levels, the higher HbA1c groups were significantly associated with advanced fibrosis compared with the lowest HbA1c group. On the other hand, compared with the lowest HbA1c group, the higher HbA1c groups were also associated with a high NAS in both multivariate analyses.
Conclusion
Glycemic control is associated with NAFLD exacerbation, with even a mild deterioration in glycemic control, especially a HbA1c level of 6.5%–7.4%, contributing to NAFLD progression. -
Citations
Citations to this article as recorded by- Combined effect of histological findings and diabetes mellitus on liver‐related events in patients with metabolic dysfunction‐associated steatotic liver disease
Akihito Shiomi, Teruki Miyake, Shinya Furukawa, Bunzo Matsuura, Osamu Yoshida, Takao Watanabe, Ayumi Kanamoto, Masumi Miyazaki, Hironobu Nakaguchi, Yoshio Tokumoto, Masashi Hirooka, Masanori Abe, Yoichi Hiasa
Hepatology Research.2024;[Epub] CrossRef
- Combined effect of histological findings and diabetes mellitus on liver‐related events in patients with metabolic dysfunction‐associated steatotic liver disease
- Drug/Regimen
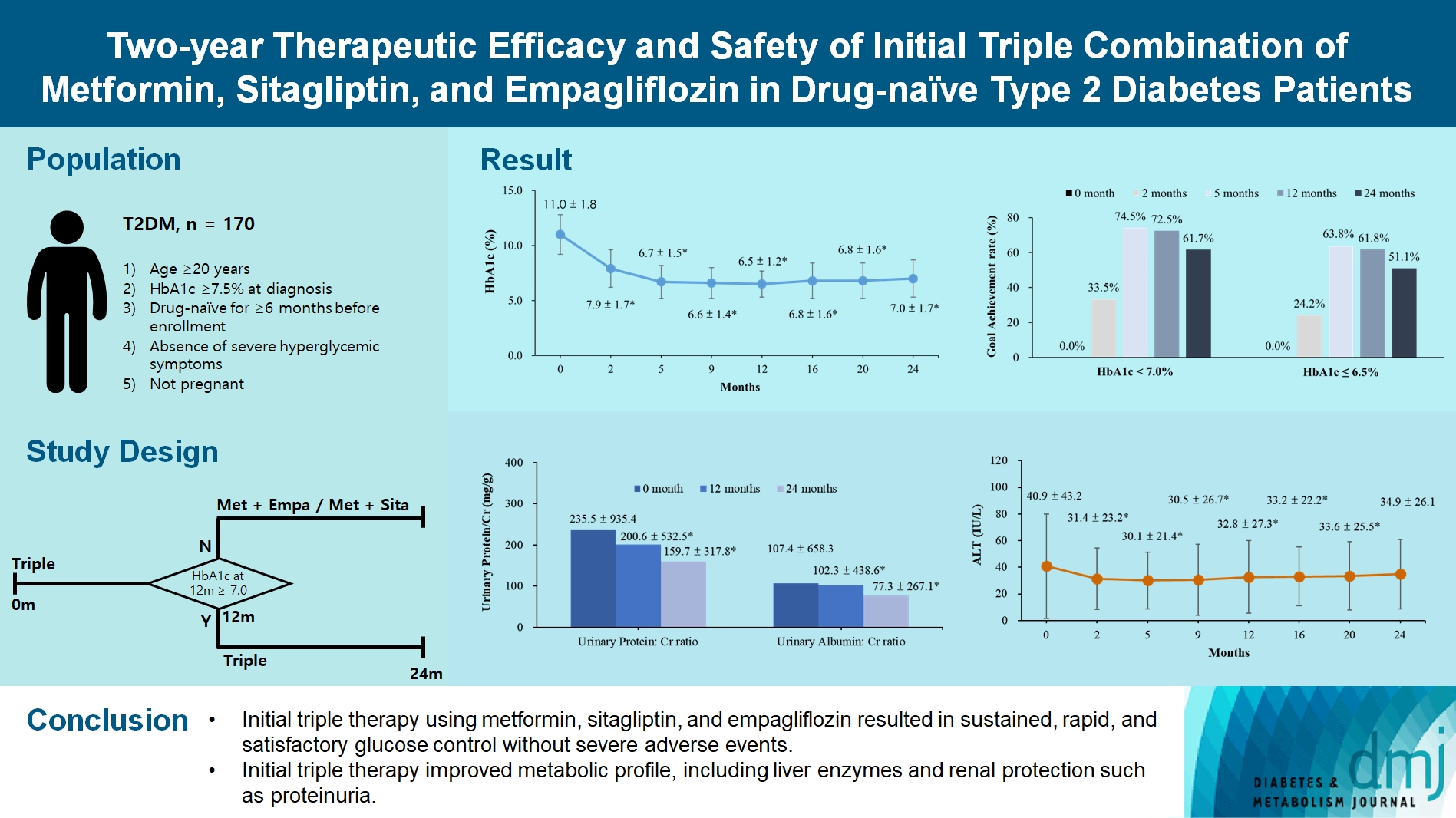
- Two-Year Therapeutic Efficacy and Safety of Initial Triple Combination of Metformin, Sitagliptin, and Empagliflozin in Drug-Naïve Type 2 Diabetes Mellitus Patients
- Young-Hwan Park, Minji Sohn, So Yeon Lee, Soo Lim
- Diabetes Metab J. 2024;48(2):253-264. Published online January 26, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0128
- 1,794 View
- 288 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated the long-term efficacy and safety of initial triple therapy using metformin, a dipeptidyl peptidase-4 inhibitor, and a sodium-glucose cotransporter-2 inhibitor, in patients with type 2 diabetes mellitus.
Methods
We enrolled 170 drug-naïve patients with glycosylated hemoglobin (HbA1c) level >7.5% who had started triple therapy (metformin, sitagliptin, and empagliflozin). Glycemic, metabolic, and urinary parameters were measured for 24 months.
Results
After 24 months, HbA1c level decreased significantly from 11.0%±1.8% to 7.0%±1.7%. At 12 and 24 months, the rates of achievement of the glycemic target goal (HbA1c <7.0%) were 72.5% and 61.7%, respectively, and homeostasis model assessment of β-cell function and insulin resistance indices improved. Whole-body fat percentage decreased by 1.08%, and whole-body muscle percentage increased by 0.97% after 24 months. Fatty liver indices and albuminuria improved significantly. The concentration of ketone bodies was elevated at the baseline but decreased after 24 months. There were no serious adverse events, including ketoacidosis.
Conclusion
Initial triple combination therapy with metformin, sitagliptin, and empagliflozin led to achievement of the glycemic target goal, which was maintained for 24 months without severe hypoglycemia but with improved metabolic function and albuminuria. This combination therapy may be a good strategy for drug-naïve patients with type 2 diabetes mellitus.
- Metabolic Risk/Epidemiology
- Association of Measures of Glucose Metabolism with Colorectal Cancer Risk in Older Chinese: A 13-Year Follow-up of the Guangzhou Biobank Cohort Study-Cardiovascular Disease Substudy and Meta-Analysis
- Shu Yi Wang, Wei Sen Zhang, Chao Qiang Jiang, Ya Li Jin, Tong Zhu, Feng Zhu, Lin Xu
- Diabetes Metab J. 2024;48(1):134-145. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0383

- 1,147 View
- 141 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Abnormal glucose metabolism is a risk factor for colorectal cancer (CRC). However, association of glycosylated hemoglobin (HbA1c) with CRC risk remains under-reported. We examined the association between glycemic indicators (HbA1c, fasting plasma glucose, fasting insulin, 2-hour glucose, 2-hour insulin, and homeostasis model of risk assessment-insulin resistance index) and CRC risk using prospective analysis and meta-analysis.
Methods
Participants (n=1,915) from the Guangzhou Biobank Cohort Study-Cardiovascular Disease Substudy were included. CRC events were identified through record linkage. Cox regression was used to assess the associations of glycemic indicators with CRC risk. A meta-analysis was performed to investigate the association between HbA1c and CRC risk.
Results
During an average of 12.9 years follow-up (standard deviation, 2.8), 42 incident CRC cases occurred. After adjusting for potential confounders, the hazard ratio (95% confidence interval [CI]) of CRC for per % increment in HbA1c was 1.28 (95% CI, 1.01 to 1.63) in overall population, 1.51 (95% CI, 1.13 to 2.02) in women and 1.06 (95% CI, 0.68 to 1.68) in men. No significant association of other measures of glycemic indicators and baseline diabetes with CRC risk was found. Meta-analyses of 523,857 participants including our results showed that per % increment of HbA1c was associated with 13% higher risk of CRC, with the pooled risk ratio being 1.13 (95% CI, 1.01 to 1.27). Subgroupanalyses found stronger associations in women, colon cancer, Asians, and case-control studies.
Conclusion
Higher HbA1c was a significant predictor of CRC in the general population. Our findings shed light on the pathology of glucose metabolism and CRC, which warrants more in-depth investigation.
- Cardiovascular Risk/Epidemiology
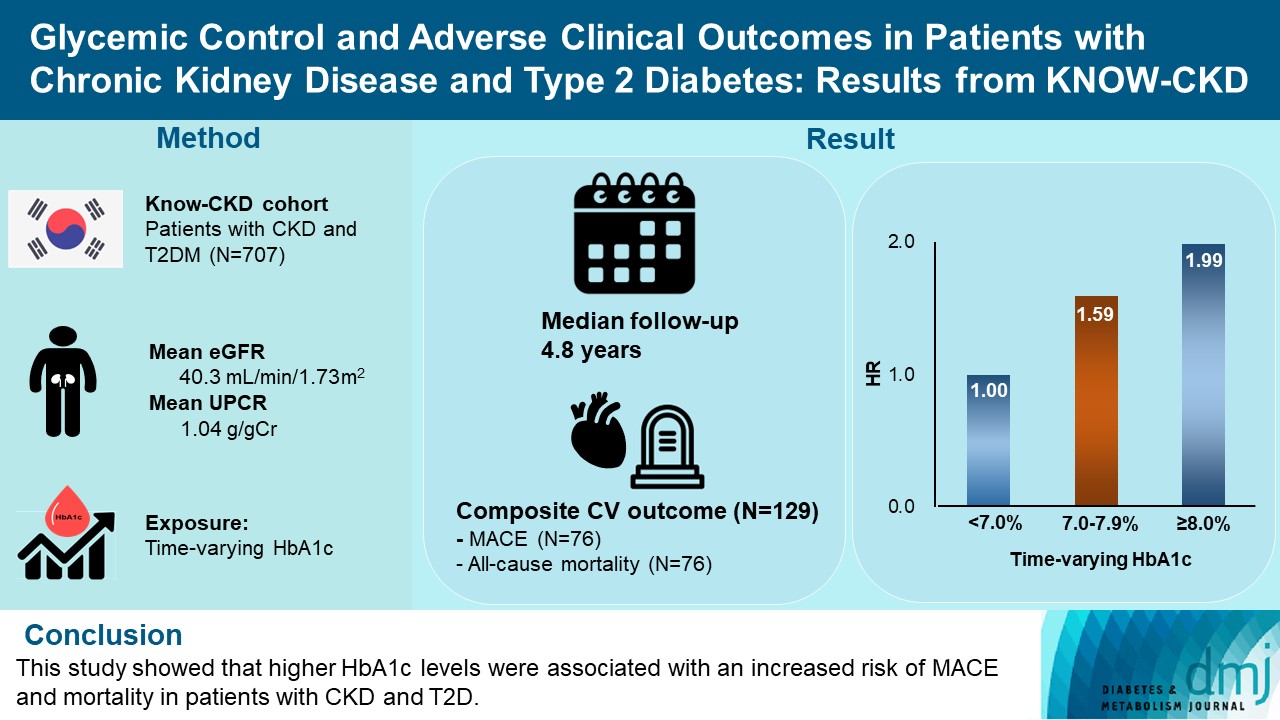
- Glycemic Control and Adverse Clinical Outcomes in Patients with Chronic Kidney Disease and Type 2 Diabetes Mellitus: Results from KNOW-CKD
- Ga Young Heo, Hee Byung Koh, Hyung Woo Kim, Jung Tak Park, Tae-Hyun Yoo, Shin-Wook Kang, Jayoun Kim, Soo Wan Kim, Yeong Hoon Kim, Su Ah Sung, Kook-Hwan Oh, Seung Hyeok Han
- Diabetes Metab J. 2023;47(4):535-546. Published online April 25, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0112
- 2,687 View
- 163 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The optimal level of glycosylated hemoglobin (HbA1c) to prevent adverse clinical outcomes is unknown in patients with chronic kidney disease (CKD) and type 2 diabetes mellitus (T2DM).
Methods
We analyzed 707 patients with CKD G1-G5 without kidney replacement therapy and T2DM from the KoreaN Cohort Study for Outcome in Patients With Chronic Kidney Disease (KNOW-CKD), a nationwide prospective cohort study. The main predictor was time-varying HbA1c level at each visit. The primary outcome was a composite of development of major adverse cardiovascular events (MACEs) or all-cause mortality. Secondary outcomes included the individual endpoint of MACEs, all-cause mortality, and CKD progression. CKD progression was defined as a ≥50% decline in the estimated glomerular filtration rate from baseline or the onset of end-stage kidney disease.
Results
During a median follow-up of 4.8 years, the primary outcome occurred in 129 (18.2%) patients. In time-varying Cox model, the adjusted hazard ratios (aHRs) for the primary outcome were 1.59 (95% confidence interval [CI], 1.01 to 2.49) and 1.99 (95% CI, 1.24 to 3.19) for HbA1c levels of 7.0%–7.9% and ≥8.0%, respectively, compared with <7.0%. Additional analysis of baseline HbA1c levels yielded a similar graded association. In secondary outcome analyses, the aHRs for the corresponding HbA1c categories were 2.17 (95% CI, 1.20 to 3.95) and 2.26 (95% CI, 1.17 to 4.37) for MACE, and 1.36 (95% CI, 0.68 to 2.72) and 2.08 (95% CI, 1.06 to 4.05) for all-cause mortality. However, the risk of CKD progression did not differ between the three groups.
Conclusion
This study showed that higher HbA1c levels were associated with an increased risk of MACE and mortality in patients with CKD and T2DM. -
Citations
Citations to this article as recorded by- The Beneficial Effect of Glycemic Control against Adverse Outcomes in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease
Dong-Hwa Lee
Diabetes & Metabolism Journal.2023; 47(4): 484. CrossRef - Prevalence and predictors of chronic kidney disease among type 2 diabetic patients worldwide, systematic review and meta-analysis
Eneyew Talie Fenta, Habitu Birhan Eshetu, Natnael Kebede, Eyob Ketema Bogale, Amare Zewdie, Tadele Derbew Kassie, Tadele Fentabil Anagaw, Elyas Melaku Mazengia, Sintayehu Shiferaw Gelaw
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Efficacy and safety of teneligliptin in patients with type 2 diabetes mellitus: a Bayesian network meta-analysis
Miao Zhu, Ruifang Guan, Guo Ma
Frontiers in Endocrinology.2023;[Epub] CrossRef
- The Beneficial Effect of Glycemic Control against Adverse Outcomes in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease
- Type 1 Diabetes
- Abnormal Responses in Cognitive Impulsivity Circuits Are Associated with Glycosylated Hemoglobin Trajectories in Type 1 Diabetes Mellitus and Impaired Metabolic Control
- Helena Jorge, Isabel C. Duarte, Sandra Paiva, Ana Paula Relvas, Miguel Castelo-Branco
- Diabetes Metab J. 2022;46(6):866-878. Published online March 22, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0307
- 4,423 View
- 173 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Risky health decisions and impulse control profiles may impact on metabolic control in type 1 diabetes mellitus (T1DM). We hypothesize that the neural correlates of cognitive impulsivity and decision-making in T1DM relate to metabolic control trajectories.
Methods
We combined functional magnetic resonance imaging (fMRI), measures of metabolic trajectories (glycosylated hemoglobin [HbA1c] over multiple time points) and behavioral assessment using a cognitive impulsivity paradigm, the Balloon Analogue Risk Task (BART), in 50 participants (25 T1DM and 25 controls).
Results
Behavioral results showed that T1DM participants followed a rigid conservative risk strategy along the iterative game. Imaging group comparisons showed that patients showed larger activation of reward related, limbic regions (nucleus accumbens, amygdala) and insula (interoceptive saliency network) in initial game stages. Upon game completion differences emerged in relation to error monitoring (anterior cingulate cortex [ACC]) and inhibitory control (inferior frontal gyrus). Importantly, activity in the saliency network (ACC and insula), which monitors interoceptive states, was related with metabolic trajectories, which was also found for limbic/reward networks. Parietal and posterior cingulate regions activated both in controls and patients with adaptive decision-making, and positively associated with metabolic trajectories.
Conclusion
We found triple converging evidence when comparing metabolic trajectories, patients versus controls or risk averse (non-learners) versus patients who learned by trial and error. Dopaminergic reward and saliency (interoceptive and error monitoring) circuits show a tight link with impaired metabolic trajectories and cognitive impulsivity in T1DM. Activity in parietal and posterior cingulate are associated with adaptive trajectories. This link between reward-saliency-inhibition circuits suggests novel strategies for patient management. -
Citations
Citations to this article as recorded by- The usefulness of an intervention with a serious video game as a complementary approach to cognitive behavioural therapy in eating disorders: A pilot randomized clinical trial for impulsivity management
Cristina Vintró‐Alcaraz, Núria Mallorquí‐Bagué, María Lozano‐Madrid, Giulia Testa, Roser Granero, Isabel Sánchez, Janet Treasure, Susana Jiménez‐Murcia, Fernando Fernández‐Aranda
European Eating Disorders Review.2023; 31(6): 781. CrossRef - Adaptations of the balloon analog risk task for neuroimaging settings: a systematic review
Charline Compagne, Juliana Teti Mayer, Damien Gabriel, Alexandre Comte, Eloi Magnin, Djamila Bennabi, Thomas Tannou
Frontiers in Neuroscience.2023;[Epub] CrossRef - Trust-based health decision-making recruits the neural interoceptive saliency network which relates to temporal trajectories of Hemoglobin A1C in Diabetes Type 1
Helena Jorge, Isabel C. Duarte, Miguel Melo, Ana Paula Relvas, Miguel Castelo-Branco
Brain Imaging and Behavior.2023; 18(1): 171. CrossRef
- The usefulness of an intervention with a serious video game as a complementary approach to cognitive behavioural therapy in eating disorders: A pilot randomized clinical trial for impulsivity management
- Technology/Device
- A 4-Week, Two-Center, Open-Label, Single-Arm Study to Evaluate the Safety and Efficacy of EOPatch in Well-Controlled Type 1 Diabetes Mellitus
- Jiyun Park, Nammi Park, Sangjin Han, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Woo Je Lee, Jae Hyeon Kim
- Diabetes Metab J. 2022;46(6):941-947. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0299
- 5,191 View
- 269 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - This study evaluated the safety and efficacy of tubeless patch pump called EOPatch in patients with well-controlled type 1 diabetes mellitus (T1DM). This 4-week, two-center, open-label, single-arm study enrolled 10 adult patients diagnosed with T1DM with glycosylated hemoglobin less than 7.5%. The co-primary end points were patch pump usage time for one attachment and number of serious adverse events related to the patch pump. The secondary end points were total amount of insulin injected per patch and changes in glycemic parameters including continuous glucose monitoring data compared to those at study entry. The median usage time per patch was 84.00 hours (interquartile range, 64.50 to 92.50). Serious adverse events did not occur during the trial. Four weeks later, time in range 70 to 180 mg/dL was significantly improved (70.71%±17.14 % vs. 82.96%±9.14%, P=0.01). The times spent below range (<54 mg/dL) and above range (>180 mg/dL) also improved (All P<0.05). Four-week treatment with a tubeless patch pump was safe and led to clinical improvement in glycemic control.
-
Citations
Citations to this article as recorded by- Multilayer track‐etched membrane‐based electroosmotic pump for drug delivery
Qian Yang, Zebo Zhang, Junshu Lin, Boyu Zhu, Rongying Yu, Xinru Li, Bin Su, Bo Zhao
ELECTROPHORESIS.2024; 45(5-6): 433. CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - A true continuous healthcare system for type 1 diabetes
Jiyong Kim, Salman Khan, Eun Kyu Kim, Hye-Jun Kil, Bo Min Kang, Hyo Geon Lee, Jin-Woo Park, Jun Young Yoon, Woochul Kim
Nano Energy.2023; 113: 108553. CrossRef
- Multilayer track‐etched membrane‐based electroosmotic pump for drug delivery
- Drug/Regimen
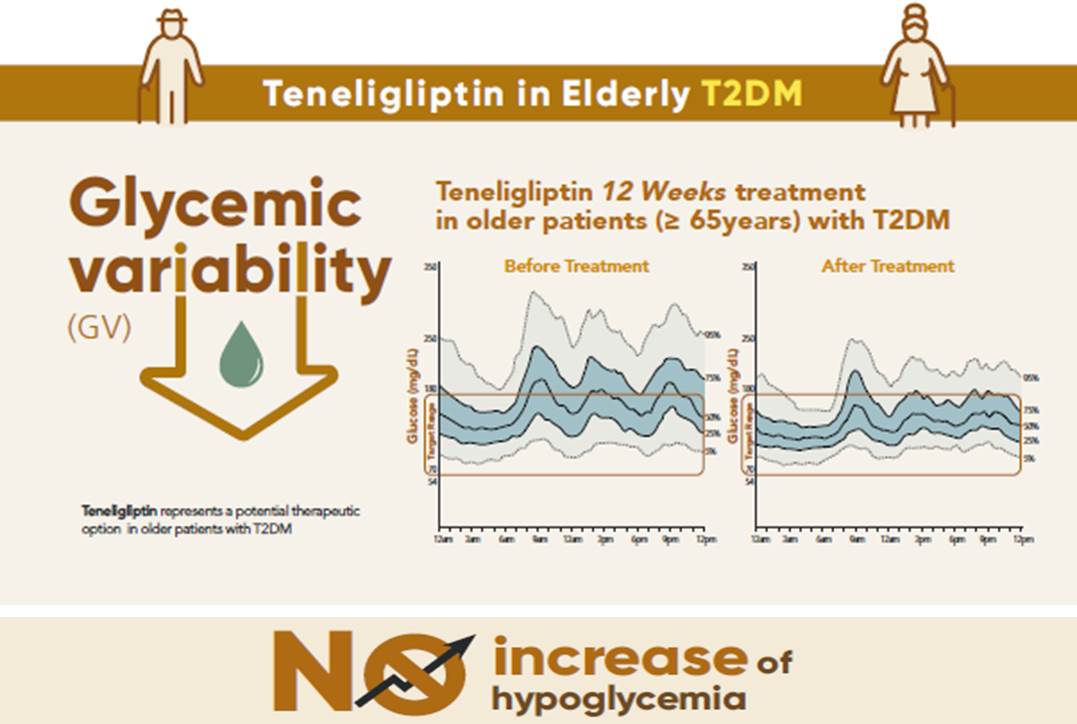
- Effects of Teneligliptin on HbA1c levels, Continuous Glucose Monitoring-Derived Time in Range and Glycemic Variability in Elderly Patients with T2DM (TEDDY Study)
- Ji Cheol Bae, Soo Heon Kwak, Hyun Jin Kim, Sang-Yong Kim, You-Cheol Hwang, Sunghwan Suh, Bok Jin Hyun, Ji Eun Cha, Jong Chul Won, Jae Hyeon Kim
- Diabetes Metab J. 2022;46(1):81-92. Published online June 16, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0016
- 7,577 View
- 431 Download
- 5 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 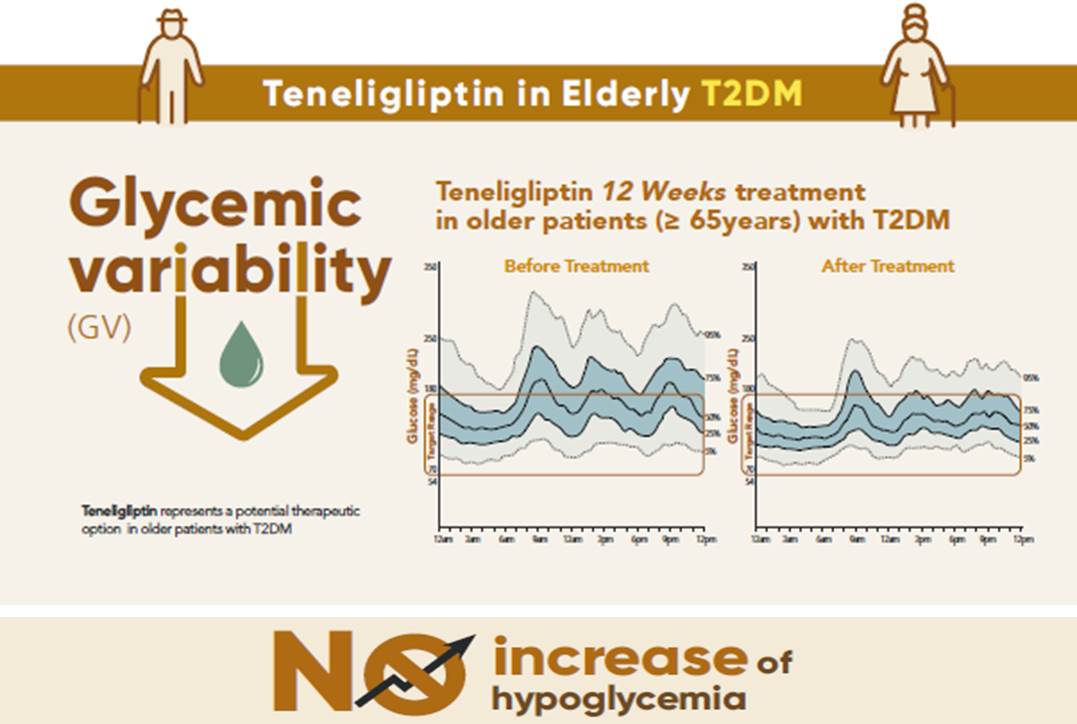
- Background
To evaluate the effects of teneligliptin on glycosylated hemoglobin (HbA1c) levels, continuous glucose monitoring (CGM)-derived time in range, and glycemic variability in elderly type 2 diabetes mellitus patients.
Methods
This randomized, double-blinded, placebo-controlled study was conducted in eight centers in Korea (clinical trial registration number: NCT03508323). Sixty-five participants aged ≥65 years, who were treatment-naïve or had been treated with stable doses of metformin, were randomized at a 1:1 ratio to receive 20 mg of teneligliptin (n=35) or placebo (n=30) for 12 weeks. The main endpoints were the changes in HbA1c levels from baseline to week 12, CGM metrics-derived time in range, and glycemic variability.
Results
After 12 weeks, a significant reduction (by 0.84%) in HbA1c levels was observed in the teneligliptin group compared to that in the placebo group (by 0.08%), with a between-group least squares mean difference of –0.76% (95% confidence interval [CI], –1.08 to –0.44). The coefficient of variation, standard deviation, and mean amplitude of glycemic excursion significantly decreased in participants treated with teneligliptin as compared to those in the placebo group. Teneligliptin treatment significantly decreased the time spent above 180 or 250 mg/dL, respectively, without increasing the time spent below 70 mg/dL. The mean percentage of time for which glucose levels remained in the 70 to 180 mg/dL time in range (TIR70–180) at week 12 was 82.0%±16.0% in the teneligliptin group, and placebo-adjusted change in TIR70–180 from baseline was 13.3% (95% CI, 6.0 to 20.6).
Conclusion
Teneligliptin effectively reduced HbA1c levels, time spent above the target range, and glycemic variability, without increasing hypoglycemia in our study population. -
Citations
Citations to this article as recorded by- Comparison of teneligliptin and other gliptin-based regimens in addressing insulin resistance and glycemic control in type 2 diabetic patients: a cross-sectional study
Harmanjit Singh, Ravi Rohilla, Shivani Jaswal, Mandeep Singla
Expert Review of Endocrinology & Metabolism.2024; 19(1): 81. CrossRef - Potential approaches using teneligliptin for the treatment of type 2 diabetes mellitus: current status and future prospects
Harmanjit Singh, Jasbir Singh, Ravneet Kaur Bhangu, Mandeep Singla, Jagjit Singh, Farideh Javid
Expert Review of Clinical Pharmacology.2023; 16(1): 49. CrossRef - Mechanism of molecular interaction of sitagliptin with human DPP4 enzyme - New Insights
Michelangelo Bauwelz Gonzatti, José Edvar Monteiro Júnior, Antônio José Rocha, Jonathas Sales de Oliveira, Antônio José de Jesus Evangelista, Fátima Morgana Pio Fonseca, Vânia Marilande Ceccatto, Ariclécio Cunha de Oliveira, José Ednésio da Cruz Freire
Advances in Medical Sciences.2023; 68(2): 402. CrossRef - A prospective multicentre open label study to assess effect of Teneligliptin on glycemic control through parameters of time in range (TIR) Metric using continuous glucose monitoring (TOP-TIR study)
Banshi Saboo, Suhas Erande, A.G. Unnikrishnan
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(2): 102394. CrossRef - Association between Variability of Metabolic Risk Factors and Cardiometabolic Outcomes
Min Jeong Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2022; 46(1): 49. CrossRef
- Comparison of teneligliptin and other gliptin-based regimens in addressing insulin resistance and glycemic control in type 2 diabetic patients: a cross-sectional study
- Drug/Regimen
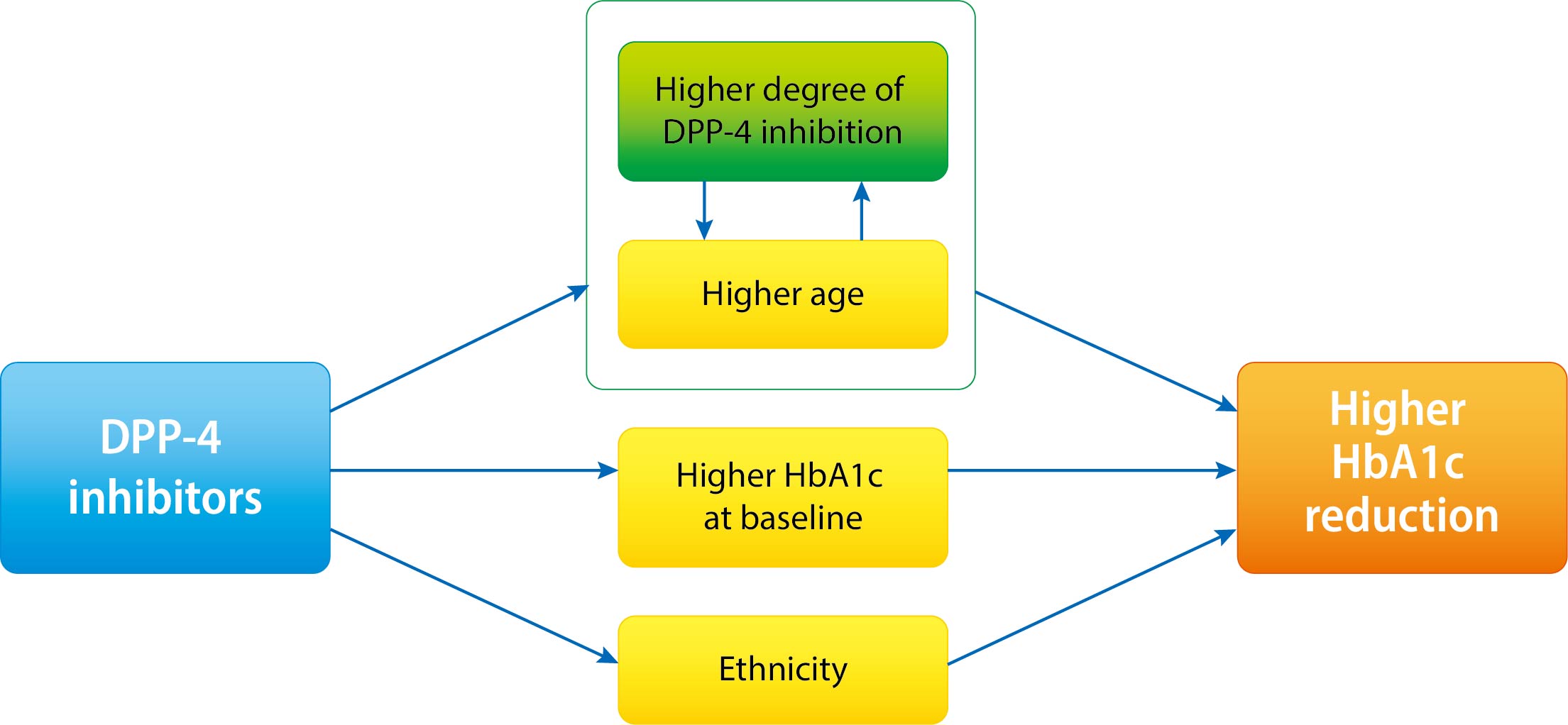
- Increasing Age Associated with Higher Dipeptidyl Peptidase-4 Inhibition Rate Is a Predictive Factor for Efficacy of Dipeptidyl Peptidase-4 Inhibitors
- Sangmo Hong, Chang Hee Jung, Song Han, Cheol-Young Park
- Diabetes Metab J. 2022;46(1):63-70. Published online April 19, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0253
- 65,535 View
- 287 Download
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 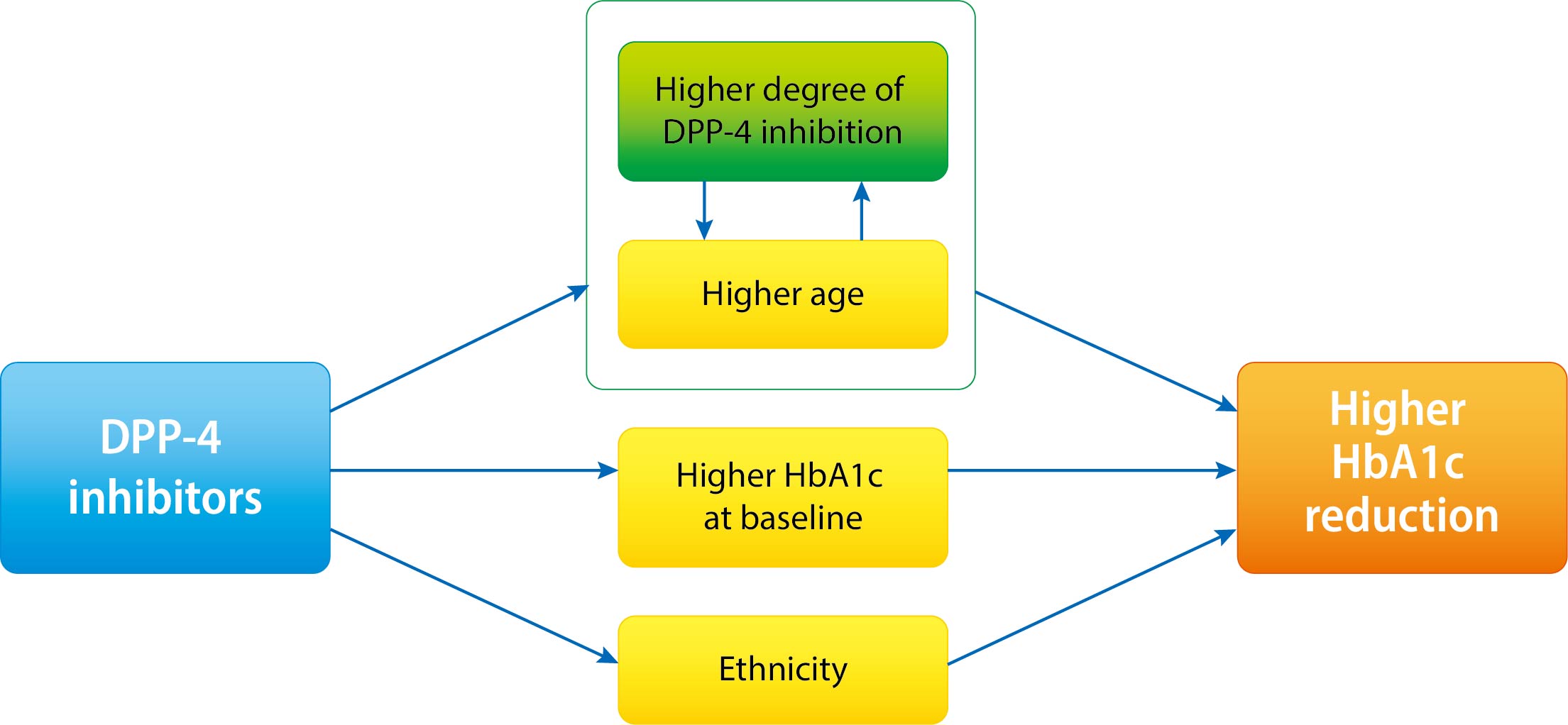
- Background
It is not known which type 2 diabetes mellitus (T2DM) patients would most benefit from dipeptidyl peptidase-4 (DPP-4) inhibitor treatment. We aimed to investigate the predictors of response to DPP-4 inhibitors considering degree of DPP-4 inhibition.
Methods
This study is a post hoc analysis of a 24-week, randomized, double-blind, phase III trial that compared the efficacy and safety of a DPP-4 inhibitor (gemigliptin vs. sitagliptin) in patients with T2DM. Subjects were classified into tertiles of T1 <65.26%, T2=65.26%–76.35%, and T3 ≥76.35% by DPP-4 inhibition. We analyzed the change from baseline in glycosylated hemoglobin (HbA1c) according to DPP-4 inhibition with multiple linear regression adjusting for age, ethnicity, body mass index, baseline HbA1c, and DPP-4 activity at baseline.
Results
The mean age was greater in the high tertile group compared with the low tertile group (T1: 49.8±8.3 vs. T2: 53.1±10.5 vs. T3: 55.3±9.5, P<0.001) of DPP-4 inhibition. Although HbA1c at baseline was not different among tertiles of DPP-4 inhibition (P=0.398), HbA1c after 24-week treatment was lower in the higher tertile compares to the lower tertile (T1: 7.30%±0.88% vs. T2: 7.12%±0.78% vs. T3: 7.00%±0.78%, P=0.021). In multiple regression analysis, DPP-4 enzyme inhibition rate was not a significant determent for HbA1c reduction due to age. In subgroup analysis by tertile of DPP-4 inhibition, age was the only significant predictor and only in the highest tertile (R2=0.281, B=–0.014, P=0.024).
Conclusion
This study showed that HbA1c reduction by DPP-4 inhibitor was associated with increasing age, and this association was linked with higher DPP-4 inhibition.
- Type 1 Diabetes
- Time in Range from Continuous Glucose Monitoring: A Novel Metric for Glycemic Control
- Jee Hee Yoo, Jae Hyeon Kim
- Diabetes Metab J. 2020;44(6):828-839. Published online December 23, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0257
- Correction in: Diabetes Metab J 2021;45(5):795
- 9,860 View
- 469 Download
- 31 Web of Science
- 36 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
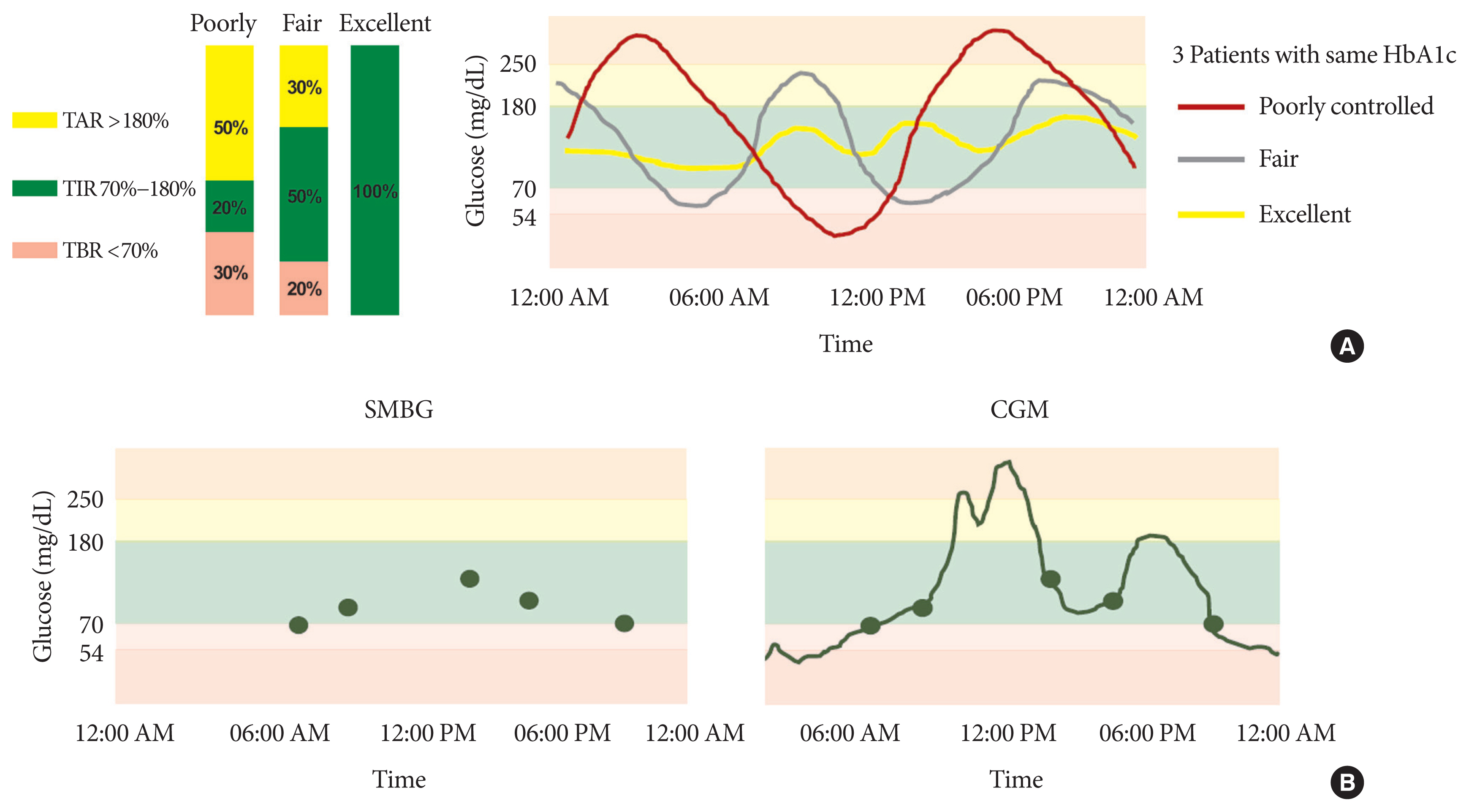
ePub - Glycosylated hemoglobin (HbA1c) has been the sole surrogate marker for assessing diabetic complications. However, consistently reported limitations of HbA1c are that it lacks detailed information on short-term glycemic control and can be easily interfered with by various clinical conditions such as anemia, pregnancy, or liver disease. Thus, HbA1c alone may not represent the real glycemic status of a patient. The advancement of continuous glucose monitoring (CGM) has enabled both patients and healthcare providers to monitor glucose trends for a whole single day, which is not possible with HbA1c. This has allowed for the development of core metrics such as time spent in time in range (TIR), hyperglycemia, or hypoglycemia, and glycemic variability. Among the 10 core metrics, TIR is reported to represent overall glycemic control better than HbA1c alone. Moreover, various evidence supports TIR as a predictive marker of diabetes complications as well as HbA1c, as the inverse relationship between HbA1c and TIR reveals. However, there are more complex relationships between HbA1c, TIR, and other CGM metrics. This article provides information about 10 core metrics with particular focus on TIR and the relationships between the CGM metrics for comprehensive understanding of glycemic status using CGM.
-
Citations
Citations to this article as recorded by- Acute and Chronic Adverse Outcomes of Type 1 Diabetes
Rachel Longendyke, Jody B. Grundman, Shideh Majidi
Endocrinology and Metabolism Clinics of North America.2024; 53(1): 123. CrossRef - La plongée sous-marine en scaphandre autonome avec un diabète de type 1. Une belle histoire du dernier millénaire
Lise Dufaitre Patouraux, Agnès Sola-Gazagnes, Boris Lormeau, Corinne Lormeau
Médecine des Maladies Métaboliques.2024; 18(1): 67. CrossRef - S100A9 exerts insulin-independent antidiabetic and anti-inflammatory effects
Gloria Ursino, Giulia Lucibello, Pryscila D. S. Teixeira, Anna Höfler, Christelle Veyrat-Durebex, Soline Odouard, Florian Visentin, Luca Galgano, Emmanuel Somm, Claudia R. Vianna, Ariane Widmer, François R. Jornayvaz, Andreas Boland, Giorgio Ramadori, Rob
Science Advances.2024;[Epub] CrossRef - Hybrid Closed-Loop Versus Manual Insulin Delivery in Adults With Type 1 Diabetes: A Post Hoc Analysis Using the Glycemia Risk Index
Melissa H. Lee, Sara Vogrin, Timothy W. Jones, David N. O’Neal
Journal of Diabetes Science and Technology.2024;[Epub] CrossRef - Clinically relevant stratification of patients with type 2 diabetes by using continuous glucose monitoring data
Xiaopeng Shao, Jingyi Lu, Rui Tao, Liang Wu, Yaxin Wang, Wei Lu, Hongru Li, Jian Zhou, Xia Yu
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Effects of a 2-Week Kinect-Based Mixed-Reality Exercise Program on Prediabetes: A Pilot Trial during COVID-19
So Young Ahn, Si Woo Lee, Hye Jung Shin, Won Jae Lee, Jun Hyeok Kim, Hyun-Jun Kim, Wook Song
Journal of Obesity & Metabolic Syndrome.2024; 33(1): 54. CrossRef - Continuous glucose monitoring with structured education in adults with type 2 diabetes managed by multiple daily insulin injections: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Kang Hee Sim, Bo-Yeon Kim, Jae Hyoung Cho, Jun Sung Moon, Soo Lim, Eun Seok Kang, Cheol-Young Park, Sin Gon Kim, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - Comparison between a tubeless, on-body automated insulin delivery system and a tubeless, on-body sensor-augmented pump in type 1 diabetes: a multicentre randomised controlled trial
Ji Yoon Kim, Sang-Man Jin, Eun Seok Kang, Soo Heon Kwak, Yeoree Yang, Jee Hee Yoo, Jae Hyun Bae, Jun Sung Moon, Chang Hee Jung, Ji Cheol Bae, Sunghwan Suh, Sun Joon Moon, Sun Ok Song, Suk Chon, Jae Hyeon Kim
Diabetologia.2024;[Epub] CrossRef - Anagliptin twice‐daily regimen improves glycaemic variability in subjects with type 2 diabetes: A double‐blind, randomized controlled trial
Yong‐ho Lee, Doo‐Man Kim, Jae Myung Yu, Kyung Mook Choi, Sin Gon Kim, Kang Seo Park, Hyun‐Shik Son, Choon Hee Chung, Kyu Jeung Ahn, Soon Hee Lee, Ki‐Ho Song, Su Kyoung Kwon, Hyeong Kyu Park, Kyu Chang Won, Hak Chul Jang
Diabetes, Obesity and Metabolism.2023; 25(5): 1174. CrossRef - Advances in Continuous Glucose Monitoring and Integrated Devices for Management of Diabetes with Insulin-Based Therapy: Improvement in Glycemic Control
Jee Hee Yoo, Jae Hyeon Kim
Diabetes & Metabolism Journal.2023; 47(1): 27. CrossRef - Status of continuous glucose monitoring use and management in tertiary hospitals of China: a cross-sectional study
Liping Chen, Xiaoqin Liu, Qin Lin, Hongmei Dai, Yong Zhao, Zumin Shi, Liping Wu
BMJ Open.2023; 13(2): e066801. CrossRef - Real-world outcomes of continuous glucose monitoring in adults with diabetes mellitus attending an Irish tertiary hospital
Aoife Courtney, Diarmuid Smith, Hannah Forde
Irish Journal of Medical Science (1971 -).2023; 192(6): 2763. CrossRef - Insight into continuous glucose monitoring: from medical basics to commercialized devices
Ayman Chmayssem, Małgorzata Nadolska, Emily Tubbs, Kamila Sadowska, Pankaj Vadgma, Isao Shitanda, Seiya Tsujimura, Youssef Lattach, Martin Peacock, Sophie Tingry, Stéphane Marinesco, Pascal Mailley, Sandrine Lablanche, Pierre Yves Benhamou, Abdelkader Zeb
Microchimica Acta.2023;[Epub] CrossRef - Efficacy of polyethylene glycol loxenatide versus insulin glargine on glycemic control in patients with type 2 diabetes: a randomized, open-label, parallel-group trial
Shuo Zhang, Chuanyan Zhang, Jingxian Chen, Feiying Deng, Zezhen Wu, Dan Zhu, Fengwu Chen, Yale Duan, Yue Zhao, Kaijian Hou
Frontiers in Pharmacology.2023;[Epub] CrossRef - Impact of continuous glucose monitoring on glycemic control and its derived metrics in type 1 diabetes: a longitudinal study
So Hyun Cho, Seohyun Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Gyuri Kim, Jae Hyeon Kim
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association Between Continuous Glucose Monitoring-Derived Glycemia Risk Index and Albuminuria in Type 2 Diabetes
Jee Hee Yoo, Ji Yoon Kim, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2023; 25(10): 726. CrossRef - Acute Glycemic Variability and Early Outcomes After Cardiac Surgery:
A Meta-Analysis
Shuo Chang, Mian Xu, Yu Wang, Yanbo Zhang
Hormone and Metabolic Research.2023; 55(11): 771. CrossRef - Comparison of Glycemia Risk Index with Time in Range for Assessing Glycemic Quality
Ji Yoon Kim, Jee Hee Yoo, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2023; 25(12): 883. CrossRef - Correlação entre tempo no alvo e hemoglobina glicada de pessoas com diabetes mellitus: revisão sistemática
Rafael Aparecido Dias Lima, Daiane Rubinato Fernandes, Rute Aparecida Casas Garcia, Lucas Ariel da Rocha Carvalho, Renata Cristina de Campos Pereira Silveira, Carla Regina de Souza Teixeira
Revista Latino-Americana de Enfermagem.2023;[Epub] CrossRef - Correlación entre tiempo en rango y hemoglobina glicosilada en personas con diabetes mellitus: revisión sistemática
Rafael Aparecido Dias Lima, Daiane Rubinato Fernandes, Rute Aparecida Casas Garcia, Lucas Ariel da Rocha Carvalho, Renata Cristina de Campos Pereira Silveira, Carla Regina de Souza Teixeira
Revista Latino-Americana de Enfermagem.2023;[Epub] CrossRef - Correlation between time on target and glycated hemoglobin in people with diabetes mellitus: systematic review
Rafael Aparecido Dias Lima, Daiane Rubinato Fernandes, Rute Aparecida Casas Garcia, Lucas Ariel da Rocha Carvalho, Renata Cristina de Campos Pereira Silveira, Carla Regina de Souza Teixeira
Revista Latino-Americana de Enfermagem.2023;[Epub] CrossRef - Smart Insulin Pen: Managing Insulin Therapy for People with Diabetes in the Digital Era
Jee Hee Yoo, Jae Hyeon Kim
The Journal of Korean Diabetes.2023; 24(4): 190. CrossRef - Novel Glycemic Index Based on Continuous Glucose Monitoring to Predict Poor Clinical Outcomes in Critically Ill Patients: A Pilot Study
Eun Yeong Ha, Seung Min Chung, Il Rae Park, Yin Young Lee, Eun Young Choi, Jun Sung Moon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Hypoglycemic agents and glycemic variability in individuals with type 2 diabetes: A systematic review and network meta-analysis
SuA Oh, Sujata Purja, Hocheol Shin, Minji Kim, Eunyoung Kim
Diabetes and Vascular Disease Research.2022; 19(3): 147916412211068. CrossRef - Advanced Glycation End Products and Their Effect on Vascular Complications in Type 2 Diabetes Mellitus
Jeongmin Lee, Jae-Seung Yun, Seung-Hyun Ko
Nutrients.2022; 14(15): 3086. CrossRef - Influence of dipeptidyl peptidase-4 inhibitors on glycemic variability in patients with type 2 diabetes: A meta-analysis of randomized controlled trials
Shangyu Chai, Ruya Zhang, Ye Zhang, Richard David Carr, Yiman Zheng, Swapnil Rajpathak, Miao Yu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Glucose Profiles Assessed by Intermittently Scanned Continuous Glucose Monitoring System during the Perioperative Period of Metabolic Surgery
Kyuho Kim, Sung Hee Choi, Hak Chul Jang, Young Suk Park, Tae Jung Oh
Diabetes & Metabolism Journal.2022; 46(5): 713. CrossRef - Deterioration in glycemic control on schooldays among children and adolescents with type 1 diabetes: A continuous glucose monitoring-based study
Yu Ding, Wenhao Zhang, Xiumei Wu, Tian Wei, Xulin Wang, Xueying Zheng, Sihui Luo
Frontiers in Pediatrics.2022;[Epub] CrossRef - Effect of repeated bolus and continuous glucose infusion on a panel of circulating biomarkers in healthy volunteers
Roland Feldbauer, Matthias Wolfgang Heinzl, Carmen Klammer, Michael Resl, Johannes Pohlhammer, Klemens Rosenberger, Verena Almesberger, Florian Obendorf, Lukas Schinagl, Thomas Wagner, Margot Egger, Benjamin Dieplinger, Martin Clodi, Stephen L. Atkin
PLOS ONE.2022; 17(12): e0279308. CrossRef - Relationship between glycemic intraday variations evaluated in continuous glucose monitoring and HbA1c variability in type 2 diabetes: pilot study
Akemi Tokutsu, Yosuke Okada, Keiichi Torimoto, Yoshiya Tanaka
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef - Time-in-range for monitoring glucose control: Is it time for a change?
Virginia Bellido, Pedro José Pinés-Corrales, Rocío Villar-Taibo, Francisco Javier Ampudia-Blasco
Diabetes Research and Clinical Practice.2021; 177: 108917. CrossRef - Glucose Management Indicator for People with Type 1 Asian Diabetes Is Different from That of the Published Equation: Differences by Glycated Hemoglobin Distribution
Jee Hee Yoo, Seung Hee Yang, Gyuri Kim, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2021;[Epub] CrossRef - Health-Related Quality of Life, Family Conflicts and Fear of Injecting: Perception Differences between Preadolescents and Adolescents with Type 1 Diabetes and Their Mothers
Marta Tremolada, Maria Cusinato, Sabrina Bonichini, Arianna Fabris, Claudia Gabrielli, Carlo Moretti
Behavioral Sciences.2021; 11(7): 98. CrossRef - Daytime Glycemic Variability and Frailty in Older Patients with Diabetes: a Pilot Study Using Continuous Glucose Monitoring
Seung Min Chung, Yun Hee Lee, Chang Oh Kim, Ji Yeon Lee, Sang-Man Jin, Seung-Hyun Yoo, Jun Sung Moon, Kwang Joon Kim
Journal of Korean Medical Science.2021;[Epub] CrossRef - Benefits of a Switch from Intermittently Scanned Continuous Glucose Monitoring (isCGM) to Real-Time (rt) CGM in Diabetes Type 1 Suboptimal Controlled Patients in Real-Life: A One-Year Prospective Study §
Yannis Préau, Sébastien Galie, Pauline Schaepelynck, Martine Armand, Denis Raccah
Sensors.2021; 21(18): 6131. CrossRef - Recent Advances of Integrative Bio-Omics Technologies to Improve Type 1 Diabetes (T1D) Care
Nisha Karwal, Megan Rodrigues, David D. Williams, Ryan J. McDonough, Diana Ferro
Applied Sciences.2021; 11(24): 11602. CrossRef
- Acute and Chronic Adverse Outcomes of Type 1 Diabetes
- COVID-19
- Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People with Type 2 Diabetes Mellitus
- Sung-Don Park, Sung-Woo Kim, Jun Sung Moon, Yin Young Lee, Nan Hee Cho, Ji-Hyun Lee, Jae-Han Jeon, Yeon-Kyung Choi, Mi Kyung Kim, Keun-Gyu Park
- Diabetes Metab J. 2021;45(1):109-114. Published online December 4, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0226

- 9,444 View
- 307 Download
- 23 Web of Science
- 24 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- This study investigated the impact of social distancing due to coronavirus disease 2019 (COVID-19) on glycemic control in people with type 2 diabetes mellitus (T2DM). We retrospectively analyzed the change in glycosylated hemoglobin level (ΔHbA1c) in people with T2DM who undertook social distancing because of COVID-19. We compared the ΔHbA1c between COVID-19 and non-COVID-19 cohorts that were enrolled at the same time of year. The ΔHbA1c of the COVID-19 cohort was significantly higher than that of two non-COVID-19 cohorts. Subgroup analysis according to age and baseline HbA1c level showed that social distancing significantly increased the mean HbA1c level of participants of <50 years. The ΔHbA1c of participants of <50 years and with HbA1c <7.0% in the COVID-19 cohort showed larger changes than other subgroups. In adjusted model, adjusted ΔHbA1c levels in the COVID-19 cohort remained significantly higher than those in the two other cohorts. Social distancing negatively impacts blood glucose control in people with T2DM, especially those who are younger and have good blood glucose control.
-
Citations
Citations to this article as recorded by- Impact of two COVID-19 lockdowns on HbA1c levels in patients with type 2 diabetes and associations with patient characteristics: a multicentre, observational cohort study over three years
Ingmar Schäfer, Daniel Tajdar, Laura Walther, Lasse Bittner, Dagmar Lühmann, Martin Scherer
Frontiers in Public Health.2024;[Epub] CrossRef - Influence of the COVID-19 pandemic on the achievement of guideline targets for HbA1c, blood pressure, and LDL cholesterol in people with diabetes in Japan
Shingo Kuwajima, Takahito Itoh, Tatsuya Sato, Shoya Ino, Satoru Shibata, Kouhei Ohno, Hiroyuki Hotta, Tomoaki Matsumoto, Hitoshi Ooiwa, Hirofumi Kubo, Takayuki Miki
Diabetology International.2024;[Epub] CrossRef - Socioeconomic status and the effect of prolonged pandemic confinement on anthropometric and glycaemic outcomes in adults with type 2 diabetes mellitus
Chandana Wijeweera, Ummul Muhfaza, Reginald V. Lord, Peter Petocz, Juliana Chen, Veronica Preda
Primary Care Diabetes.2024;[Epub] CrossRef - Physical and Mental Health Characteristics of Hospitalized COVID-19 Patients with and without Type 2 Diabetes Mellitus in Turkey
Abdulbari Bener, Murat Atmaca, Abdulla O. A. A. Al-Hamaq, Antonio Ventriglio
Brain Sciences.2024; 14(4): 377. CrossRef - Self-Care of Adults with Type 2 Diabetes During the COVID-19 Pandemic: A Qualitative Interpretive Description Study
Michela Luciani, Camilla Bigoni, Marta Canesi, Matteo Masotto, Diletta Fabrizi, Stefania Di Mauro, Davide Ausili
Clinical Nursing Research.2023; 32(1): 73. CrossRef - Changes in body weight and glycemic control in association with COVID-19 Shutdown among 23,000 adults with type 2 diabetes
Emily Panza, Kevin E. Kip, Kripa Venkatakrishnan, Oscar C. Marroquin, Rena R. Wing
Acta Diabetologica.2023; 60(6): 787. CrossRef - The Impact of a Lockdown for the COVID-19 Pandemic on Seasonal HbA1c Variation in Patients with Type 2 Diabetes
Yu-Cheng Cheng, Yu-Hsuan Li, Hsiu-Chen Liu, Chiann-Yi Hsu, Wan-Jen Chang, I-Te Lee, Chin-Li Lu
Life.2023; 13(3): 763. CrossRef - Changes in the mean incidence and variance of orthopedic diseases before and during the COVID-19 pandemic in Korea: a retrospective study
Joo-Hee Kim, Mi Jung Kwon, Hyo Geun Choi, Sang Jun Lee, Sangwon Hwang, Jaemin Lee, San-Hui Lee, Jung Woo Lee
BMC Musculoskeletal Disorders.2023;[Epub] CrossRef - Gender differences-based bioinformatics analysis to identify hub genes and key pathways in type 2 diabetes
Md Sojib Hossain, Subrina Islam Rupa, Md Sumon Sarkar, Md Al Amin, Mst Tania Khatun, Md Shamim, Md Zahidul Islam
Informatics in Medicine Unlocked.2023; 40: 101302. CrossRef - Retrospective Study on the Impact of COVID-19 Lockdown on Patients with Type 2 Diabetes in Northern Taiwan
Hsuan Huang, Hsiao-Ling Su, Chih-Hsung Huang, Yi-Hsin Lin
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2539. CrossRef - Understanding impacts of COVID-19 restrictions on glycemic control for patients with diabetes in Japan
Kiyoko Uno-Eder, Noriko Satoh-Asahara, Manabu Hibiya, Kenji Uno, Takuya Uchino, Koji Morita, Toshio Ishikawa, Tetsuji Kaneko, Hajime Yamakage, Yuki Kitaoka, Tomohiro Sawa, Kazuhisa Tsukamoto, Tamio Teramoto
Journal of Diabetes & Metabolic Disorders.2023; 22(2): 1695. CrossRef - Impacts of the COVID-19 pandemic on unmet social needs, self-care, and outcomes among people with diabetes and poor glycemic control
Minal R. Patel, Guanghao Zhang, Cindy Leung, Peter X.K. Song, Michele Heisler, Hae Mi Choe, Roshanak Mehdipanah, Xu Shi, Kenneth Resnicow, Geila Rajaee, John D. Piette
Primary Care Diabetes.2022; 16(1): 57. CrossRef - Impact of the COVID-19 Pandemic on Glycemic Control and Blood Pressure Control in Patients with Diabetes in Japan
Keisuke Endo, Takayuki Miki, Takahito Itoh, Hirofumi Kubo, Ryosuke Ito, Kouhei Ohno, Hiroyuki Hotta, Nobuo Kato, Tomoaki Matsumoto, Aya Kitamura, Mai Tamayama, Takako Wataya, Ayaka Yamaya, Rei Ishikawa, Hitoshi Ooiwa
Internal Medicine.2022; 61(1): 37. CrossRef - The Effects of COVID-19 Lockdown on Glycaemic Control and Lipid Profile in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis
Omorogieva Ojo, Xiao-Hua Wang, Osarhumwese Osaretin Ojo, Edith Orjih, Nivedita Pavithran, Amanda Rodrigues Amorim Adegboye, Qian-Qian Feng, Paul McCrone
International Journal of Environmental Research and Public Health.2022; 19(3): 1095. CrossRef - Lifestyles Under Lockdown: A Scoping Review of International Studies on Type 2 Diabetes Self-Management Behaviors During COVID-19
Caroline Cummings, Kagnica Seng, Ryan Tweet, Julie Wagner
Frontiers in Clinical Diabetes and Healthcare.2022;[Epub] CrossRef - Substitution of telemedicine for clinic visit during the COVID‐19 pandemic of 2020: Comparison of telemedicine and clinic visit
Yukiko Onishi, Rieko Ichihashi, Yoko Yoshida, Tazu Tahara, Takako Kikuchi, Toshiko Kobori, Tetsuya Kubota, Masahiko Iwamoto, Shoko Hamano, Masato Kasuga
Journal of Diabetes Investigation.2022; 13(9): 1617. CrossRef - The impact of the COVID-19 pandemic on the management of patients with chronic diseases in Primary Health Care
Panagiotis Stachteas, Manolis Symvoulakis, Apostolos Tsapas, Emmanouil Smyrnakis
Population Medicine.2022; 4(August): 1. CrossRef - Effects of COVID-19 Pandemic and Lockdown on Monitoring and Treatment Balance of Finnish Coronary Heart Disease and Type 2 Diabetes Patients
Piia Lavikainen, Marja-Leena Lamidi, Teppo Repo, Laura Inglin, Janne Martikainen, Tiina Laatikainen
Clinical Epidemiology.2022; Volume 14: 1363. CrossRef - Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People with Type 2 Diabetes Mellitus (Diabetes Metab J 2021;45:109-14)
Junghyun Noh
Diabetes & Metabolism Journal.2021; 45(2): 275. CrossRef - Impact of Social Distancing Due to Coronavirus Disease 2019 on the Changes in Glycosylated Hemoglobin Level in People with Type 2 Diabetes Mellitus (Diabetes Metab J 2021;45:109-14)
Sung-Don Park, Sung-Woo Kim, Jun Sung Moon, Jae-Han Jeon, Mi Kyung Kim, Keun-Gyu Park
Diabetes & Metabolism Journal.2021; 45(2): 279. CrossRef - Glucose control in diabetes during home confinement for the first pandemic wave of COVID-19: a meta-analysis of observational studies
Giovanni Antonio Silverii, Chiara Delli Poggi, Ilaria Dicembrini, Matteo Monami, Edoardo Mannucci
Acta Diabetologica.2021; 58(12): 1603. CrossRef - The impact of COVID-19 pandemic on glycemic control in patients with diabetes mellitus in Turkey: a multi-center study from Kocaeli
Alev Selek, Emre Gezer, Eda Altun, Mehmet Sözen, Ömercan Topaloğlu, Damla Köksalan, Halil Demirkan, Dilek Karakaya, Berrin Cetinarslan, Zeynep Cantürk, Dilek Taymez
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1461. CrossRef - Effects of Social Distancing on Diabetes Management in Older Adults during COVID-19 Pandemic
Soo Myoung Shin, Tae Jung Oh, Sung Hee Choi, Hak Chul Jang
Diabetes & Metabolism Journal.2021; 45(5): 765. CrossRef - Year-Long Trend in Glycated Hemoglobin Levels in Patients with Type 2 Diabetes during the COVID-19 Pandemic
Jonghwa Jin, Seong Wook Lee, Won-Ki Lee, Jae-Han Jeon, Jung-Guk Kim, In-Kyu Lee, Yeon-Kyung Choi, Keun-Gyu Park
Endocrinology and Metabolism.2021; 36(5): 1142. CrossRef
- Impact of two COVID-19 lockdowns on HbA1c levels in patients with type 2 diabetes and associations with patient characteristics: a multicentre, observational cohort study over three years
- Drug/Regimen
- Long-Term Glycaemic Durability of Early Combination Therapy Strategy versus Metformin Monotherapy in Korean Patients with Newly Diagnosed Type 2 Diabetes Mellitus
- Soon-Jib Yoo, Sang-Ah Chang, Tae Seo Sohn, Hyuk-Sang Kwon, Jong Min Lee, Sungdae Moon, Pieter Proot, Päivi M Paldánius, Kun Ho Yoon
- Diabetes Metab J. 2021;45(6):954-959. Published online November 12, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0173
- 55,086 View
- 368 Download
- 3 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 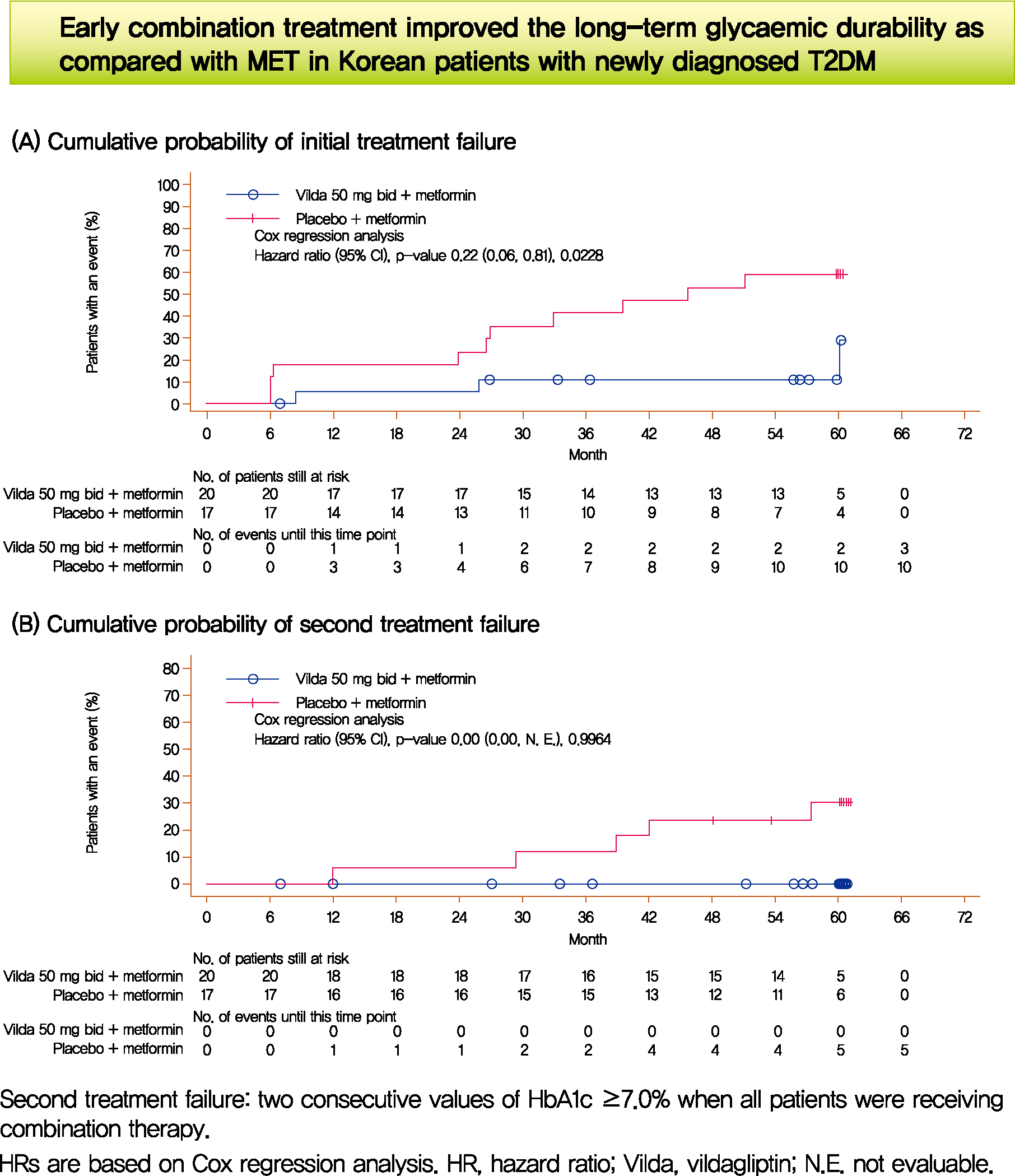
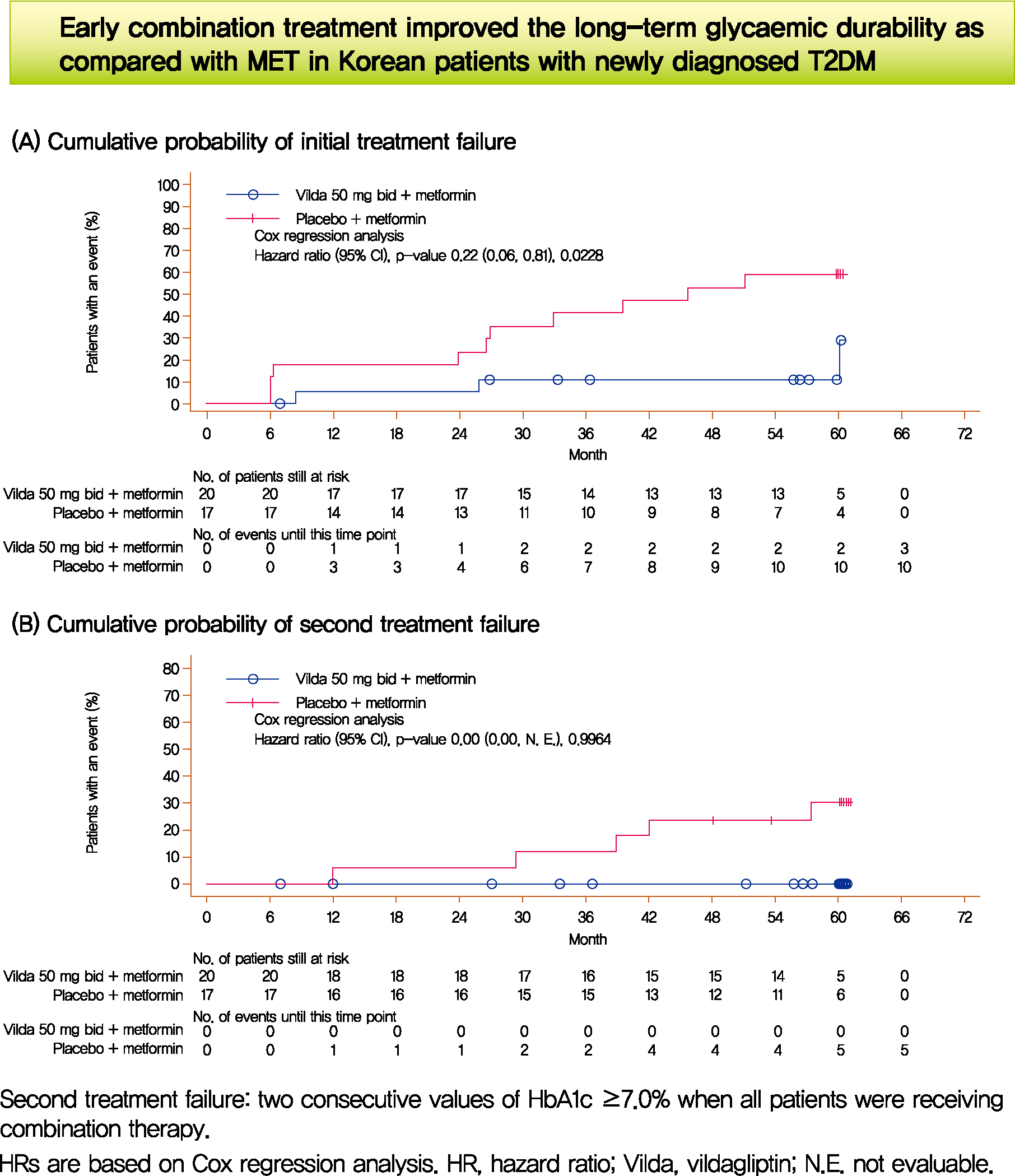
- We assessed the glycaemic durability with early combination (EC; vildagliptin+metformin [MET], n=22) versus MET monotherapy (n=17), among newly-diagnosed type 2 diabetes mellitus (T2DM) enrolled (between 2012 and 2014) in the VERIFY study from Korea (n=39). Primary endpoint was time to initial treatment failure (TF) (glycosylated hemoglobin [HbA1c] ≥7.0% at two consecutive scheduled visits after randomization [end of period 1]). Time to second TF was assessed when both groups were receiving and failing on the combination (end of period 2). With EC the risk of initial TF significantly reduced by 78% compared to MET (n=3 [15%] vs. n=10 [58.7%], P=0.0228). No secondary TF occurred in EC group versus five patients (29.4%) in MET. Patients receiving EC treatment achieved consistently lower HbA1c levels. Both treatment approaches were well tolerated with no hypoglycaemic events. In Korean patients with newly diagnosed T2DM, EC treatment significantly and consistently improved the long-term glycaemic durability as compared with MET.
-
Citations
Citations to this article as recorded by- 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim,
Diabetes & Metabolism Journal.2021; 45(4): 461. CrossRef
- 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
- Complications
-
- Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study
- Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
- Diabetes Metab J. 2021;45(3):368-378. Published online October 20, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0046
- 9,398 View
- 344 Download
- 19 Web of Science
- 19 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 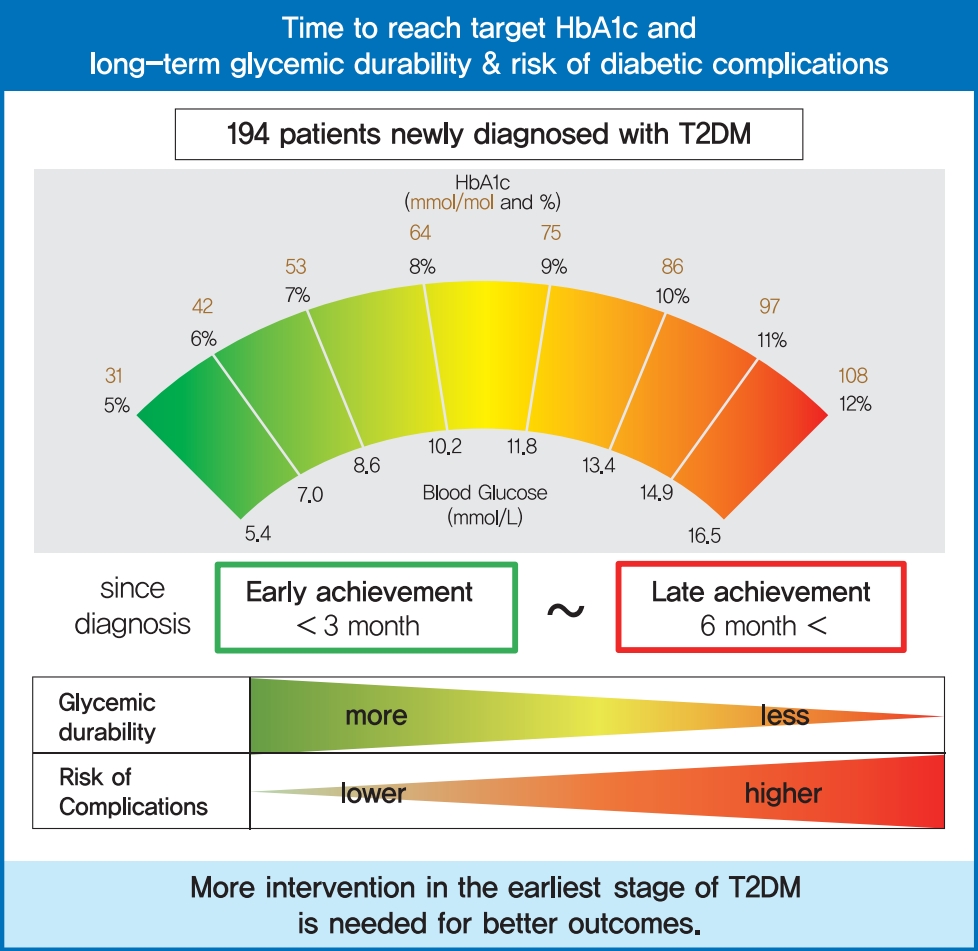
- Background
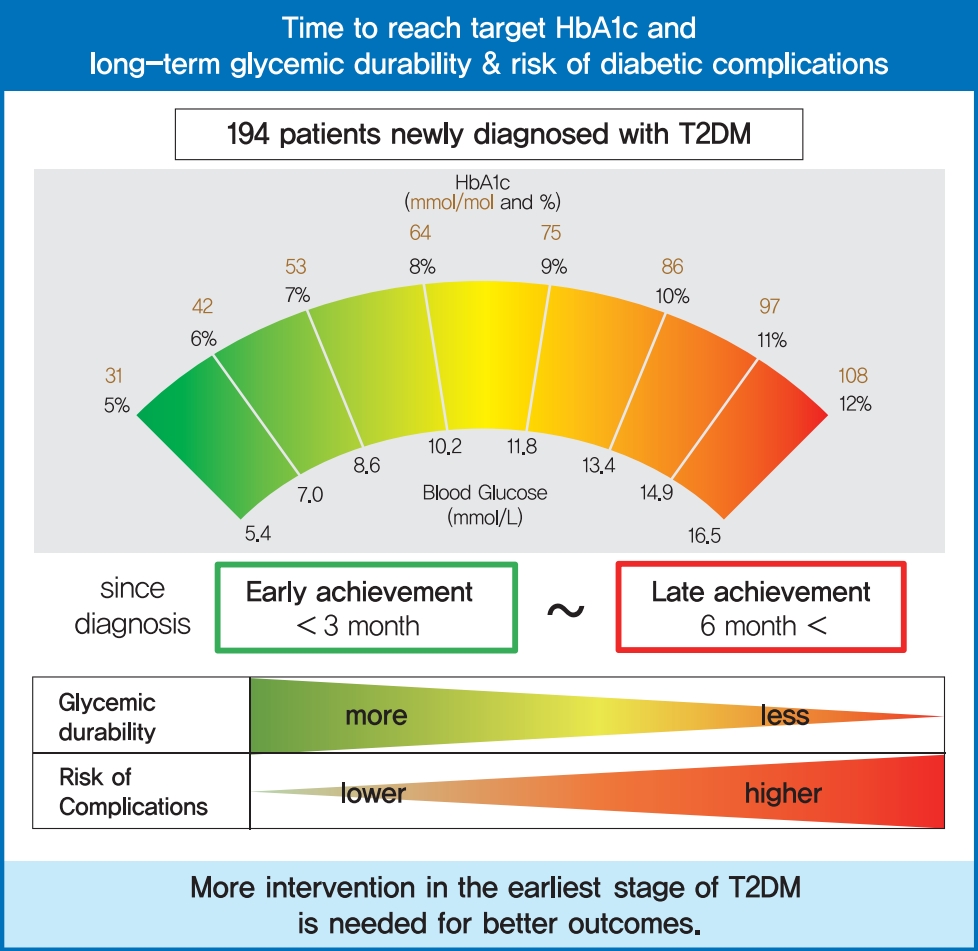
To evaluate the association of time to reach the target glycosylated hemoglobin (HbA1c) level with long-term durable glycemic control and risk of diabetic complications in patients with newly diagnosed type 2 diabetes mellitus (T2DM).
Methods
In a longitudinal observational cohort, 194 patients with T2DM newly diagnosed between January 2011 and March 2013 were followed up over 6 years. Patients were classified according to the time needed to reach the target HbA1c (<7.0%): <3, 3 to 6 (early achievement group), and ≥6 months (late achievement group). Risks of microvascular complications including diabetic retinopathy, nephropathy, and neuropathy as well as macrovascular events including ischemic heart disease, ischemic stroke, and peripheral arterial disease were assessed by multivariable Cox proportional hazards analysis.
Results
During a median follow-up of 6.53 years, 66 microvascular and 14 macrovascular events occurred. Maintenance of durable glycemic control over 6 years was more likely in the early achievement groups than in the late achievement group (34.5%, 30.0%, and 16.1% in <3, 3 to 6, and ≥6 months, respectively, P=0.039). Early target HbA1c achievement was associated with lower risk of composite diabetic complications (adjusted hazard ratio [HR, 0.47; 95% confidence interval [CI], 0.26 to 0.86 in <3 months group) (adjusted HR, 0.50; 95% CI, 0.23 to 1.10 in 3 to 6 months group, in reference to ≥6 months group). Similar trends were maintained for risks of microvascular and macrovascular complications, although statistical significance was not reached for macrovascular complications.
Conclusion
Early target HbA1c achievement was associated with long-term durable glycemic control and reduced risk of diabetic complications in newly diagnosed T2DM. -
Citations
Citations to this article as recorded by- HbA1c As Diabetes Mellitus Biomarker and Its Methods Evolution
Liong Boy Kurniawan
INDONESIAN JOURNAL OF CLINICAL PATHOLOGY AND MEDICAL LABORATORY.2024; 30(2): 191. CrossRef - Efficacy and safety of enavogliflozin vs. dapagliflozin as add-on therapy in patients with type 2 diabetes mellitus based on renal function: a pooled analysis of two randomized controlled trials
Young Sang Lyu, Sangmo Hong, Si Eun Lee, Bo Young Cho, Cheol-Young Park
Cardiovascular Diabetology.2024;[Epub] CrossRef - The effect of health quotient and time management skills on self-management behavior and glycemic control among individuals with type 2 diabetes mellitus
Mengjie Chen, Man Liu, Ying Pu, Juan Wu, Mingjiao Zhang, Hongxia Tang, Laixi Kong, Maoting Guo, Kexue Zhu, Yuxiu Xie, Zhe Li, Bei Deng, Zhenzhen Xiong
Frontiers in Public Health.2024;[Epub] CrossRef - Glycemic control and cardiovascular complications of type 2 diabetes mellitus
I. V. Druk, S. S. Safronova
Meditsinskiy sovet = Medical Council.2023; (13): 130. CrossRef - Effect of viscous soluble dietary fiber on glucose and lipid metabolism in patients with type 2 diabetes mellitus: a systematic review and meta-analysis on randomized clinical trials
Kun Lu, Tingqing Yu, Xinyi Cao, Hui Xia, Shaokang Wang, Guiju Sun, Liang Chen, Wang Liao
Frontiers in Nutrition.2023;[Epub] CrossRef - Construction and validation of a clinical prediction model for asymptomatic obstructive coronary stenosis in patients with carotid stenosis
Cuijie Qin, Chuang Li, Yunpeng Luo, Zhen Li, Hui Cao
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Risk assessment of rectal anastomotic leakage (RAREAL) after DIXON in non-emergency patients with rectal cancer
Xue-Cong Zheng, Jin-Bo Su, Jin-Jie Zheng
BMC Gastroenterology.2023;[Epub] CrossRef - Evaluation of Left Ventricular Function in Diabetes Patients with Microvascular Disease by Three-Dimensional Speckle Tracking Imaging
青 周
Advances in Clinical Medicine.2023; 13(12): 18908. CrossRef - Validity of the diagnosis of diabetic microvascular complications in Korean national health insurance claim data
Hyung Jun Kim, Moo-Seok Park, Jee-Eun Kim, Tae-Jin Song
Annals of Clinical Neurophysiology.2022; 24(1): 7. CrossRef - Metformin plus a low hypoglycemic risk antidiabetic drug vs. metformin monotherapy for untreated type 2 diabetes mellitus: A meta-analysis of randomized controlled trials
Wei-Tse Hung, Yuan-Jung Chen, Chun-Yu Cheng, Bruce Ovbiagele, Meng Lee, Chia-Yu Hsu
Diabetes Research and Clinical Practice.2022; 189: 109937. CrossRef - Peripheral arterial disease progression and ankle brachial index: a cohort study with newly diagnosed patients with type 2 diabetes
João Soares Felício, Franciane Trindade Cunha de Melo, Giovana Miranda Vieira, Vitória Teixeira de Aquino, Fernanda de Souza Parente, Wanderson Maia da Silva, Nivin Mazen Said, Emanuele Rocha da Silva, Ana Carolina Contente Braga de Souza, Maria Clara Ner
BMC Cardiovascular Disorders.2022;[Epub] CrossRef - Association of long-term visit-to-visit variability of HbA1c and fasting glycemia with hypoglycemia in type 2 diabetes mellitus
Chen Long, Yaling Tang, Jiangsheng Huang, Suo Liu, Zhenhua Xing
Frontiers in Endocrinology.2022;[Epub] CrossRef - The Degree of Glycemic Control for the First Three Months Determines the Next Seven Years
Nami Lee, Dae Jung Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Inhibition of advanced glycation end products and protein oxidation by leaf extracts and phenolics from Chilean bean landraces
Felipe Ávila, Nadia Cruz, Jazmin Alarcon-Espósito, Nélida Nina, Hernán Paillan, Katherine Márquez, Denis Fuentealba, Alberto Burgos-Edwards, Cristina Theoduloz, Carmina Vejar-Vivar, Guillermo Schmeda-Hirschmann
Journal of Functional Foods.2022; 98: 105270. CrossRef - Mediation Effect of Self-Efficacy Between Health Beliefs and Glycated Haemoglobin Levels in Elderly Patients with Type 2 Diabetes Mellitus: A Cross-Sectional Study
Anqi Zhang, Jinsong Wang, Xiaojuan Wan, Jing Zhang, Zihe Guo, Yamin Miao, Shuhan Zhao, Shuo Bai, Ziyi Zhang, Weiwei Yang
Patient Preference and Adherence.2022; Volume 16: 3015. CrossRef - Early Glycosylated Hemoglobin Target Achievement Predicts Clinical Outcomes in Patients with Newly Diagnosed Type 2 Diabetes Mellitus
Joonyub Lee, Jae Hyoung Cho
Diabetes & Metabolism Journal.2021; 45(3): 337. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study (Diabetes Metab J 2021;45:368-78)
Ja Young Jeon
Diabetes & Metabolism Journal.2021; 45(4): 613. CrossRef - Time to Reach Target Glycosylated Hemoglobin Is Associated with Long-Term Durable Glycemic Control and Risk of Diabetic Complications in Patients with Newly Diagnosed Type 2 Diabetes Mellitus: A 6-Year Observational Study (Diabetes Metab J 2021;45:368-78)
Kyoung Jin Kim, Jimi Choi, Jae Hyun Bae, Kyeong Jin Kim, Hye Jin Yoo, Ji A Seo, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Sin Gon Kim, Nam Hoon Kim
Diabetes & Metabolism Journal.2021; 45(4): 617. CrossRef - Plasma Nesfatin-1: Potential Predictor and Diagnostic Biomarker for Cognitive Dysfunction in T2DM Patient
Dandan Xu, Yue Yu, Yayun Xu, Jinfang Ge
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 3555. CrossRef
- HbA1c As Diabetes Mellitus Biomarker and Its Methods Evolution
- Lifestyle
- Reducing Carbohydrate from Individual Sources Has Differential Effects on Glycosylated Hemoglobin in Type 2 Diabetes Mellitus Patients on Moderate Low-Carbohydrate Diets
- Hajime Haimoto, Shiho Watanabe, Keiko Maeda, Takashi Murase, Kenji Wakai
- Diabetes Metab J. 2021;45(3):390-403. Published online July 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0033
- 5,799 View
- 160 Download
- 3 Web of Science
- 3 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 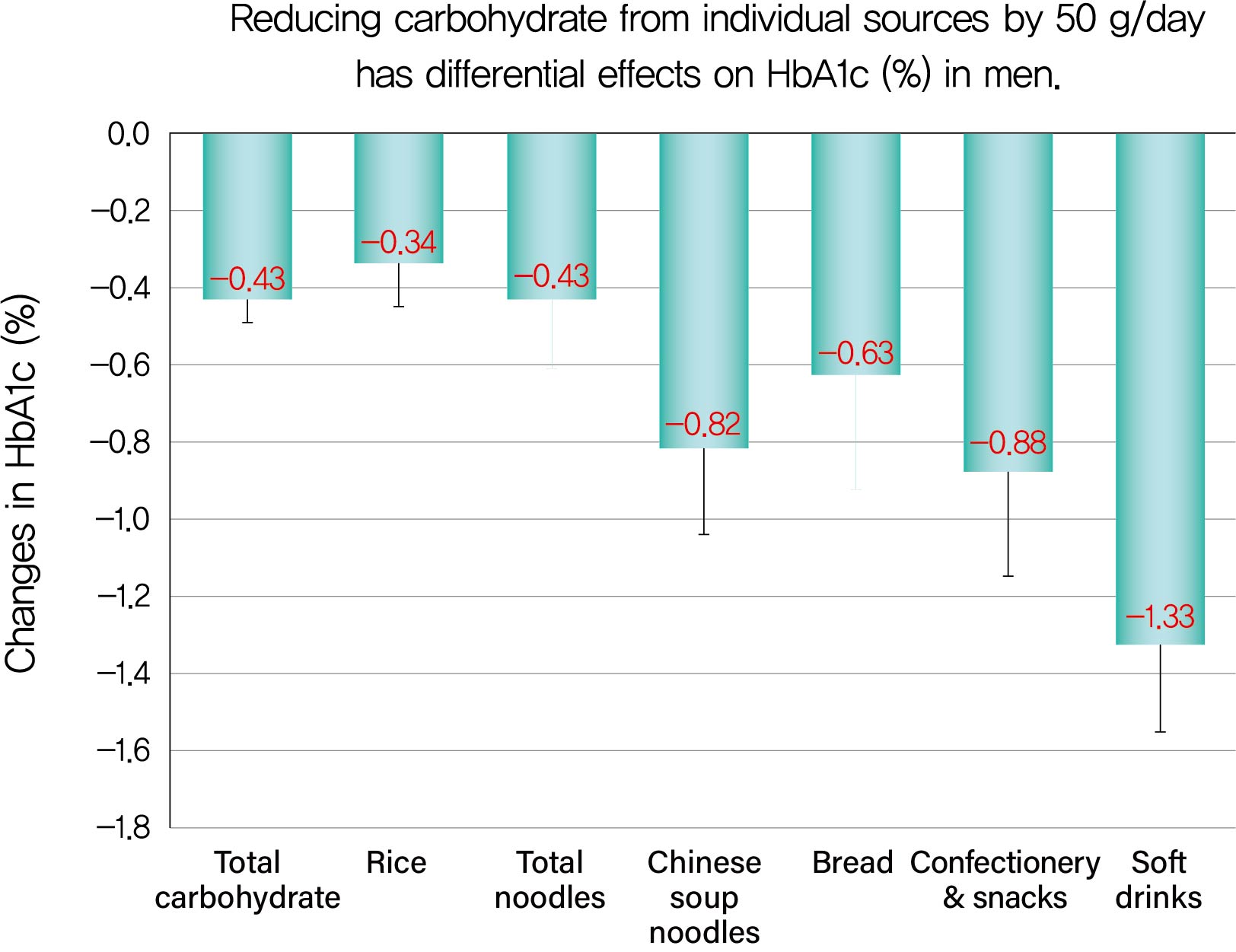
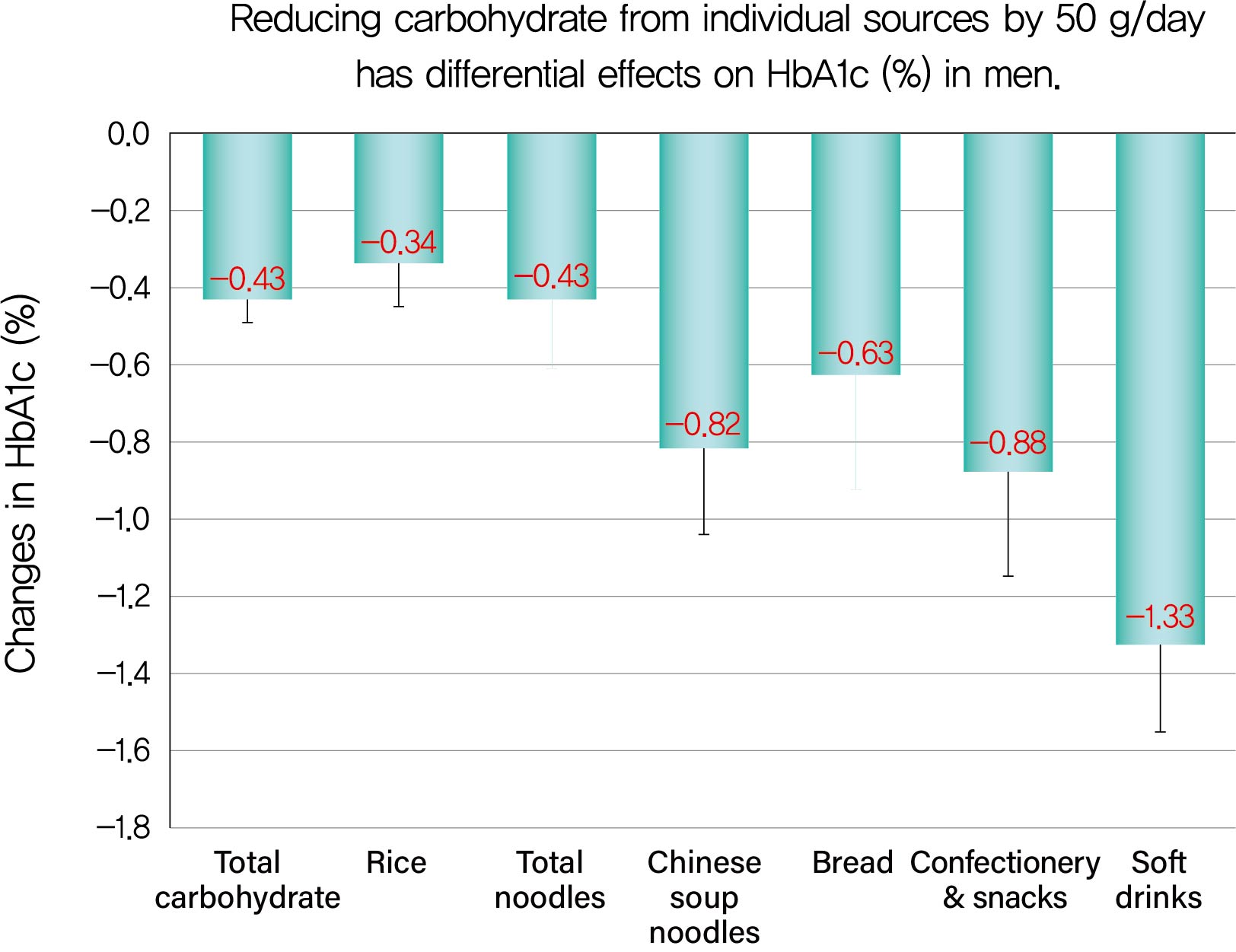
Background We evaluated decreases in glycosylated hemoglobin (HbA1c) achieved by reducing carbohydrate from various sources in type 2 diabetes mellitus patients.
Methods We followed up 138 male and 107 female outpatients on a moderate low-carbohydrate diet without diabetic medication for 6 months. Changes in carbohydrate sources (Δcarbohydrate) were assessed from 3-day dietary records at baseline and 6 months, and associations with changes in HbA1c (ΔHbA1c) were examined with Spearman's correlation coefficients (
r s) and multiple regression analysis.Results ΔHbA1c was −1.5%±1.6% in men and −0.9%±1.3% in women, while Δtotal carbohydrate was −115.3±103.7 g/day in men and −63.6±71.1 g/day in women. Positive associations with ΔHbA1c were found for Δtotal carbohydrate (
r s=0.584), Δcarbohydrate from soft drinks (0.368), confectionery (0.361), rice (0.325), bread (0.221), Chinese soup noodles (0.199) in men, and Δtotal carbohydrate (0.547) and Δcarbohydrate from rice (0.376) and confectionery (0.195) in women. Reducing carbohydrate sources by 50 g achieved decreases in HbA1c of 0.43% for total carbohydrate, 1.33% for soft drinks, 0.88% for confectionery, 0.63% for bread, 0.82% for Chinese soup noodles and 0.34% for rice in men and 0.45% for total carbohydrate, 0.67% for confectionery and 0.34% for rice in women, although mean reductions in carbohydrate from these sources were much smaller than that from rice.Conclusion Decreases in HbA1c achieved by reducing carbohydrate from soft drinks, confectionery, bread and Chinese soup noodles were 2- to 4-fold greater than that for rice. Our results will enable patients to decrease HbA1c efficiently (UMIN000009866).
-
Citations
Citations to this article as recorded by- Exploring diet associations with Covid-19 and other diseases: a Network Analysis–based approach
Rashmeet Toor, Inderveer Chana
Medical & Biological Engineering & Computing.2022; 60(4): 991. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - Associations of Dietary Salt and Its Sources with Hemoglobin A1c in Patients with Type 2 Diabetes Not Taking Anti-Diabetic Medications: Analysis Based on 6-Month Intervention with a Moderate Low-Carbohydrate Diet
Hajime Haimoto, Takashi Murase, Shiho Watanabe, Keiko Maeda, Kenji Wakai
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4569. CrossRef
- Exploring diet associations with Covid-19 and other diseases: a Network Analysis–based approach

 KDA
KDA
 First
First Prev
Prev





