
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Lifestyle
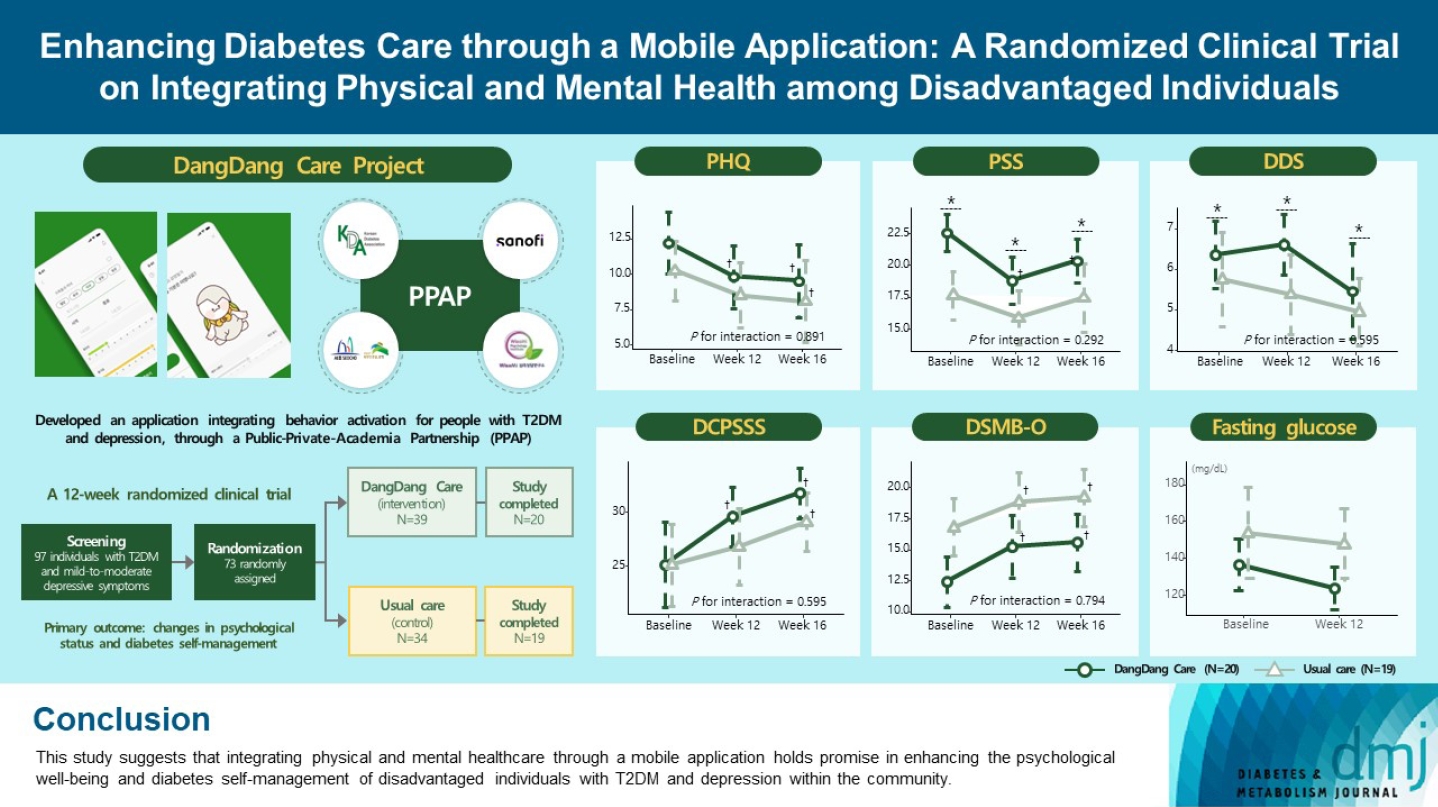
- Enhancing Diabetes Care through a Mobile Application: A Randomized Clinical Trial on Integrating Physical and Mental Health among Disadvantaged Individuals
- Jae Hyun Bae, Eun Hee Park, Hae Kyung Lee, Kun Ho Yoon, Kyu Chang Won, Hyun Mi Kim, Sin Gon Kim
- Received August 24, 2023 Accepted October 16, 2023 Published online February 2, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0298 [Epub ahead of print]
- 716 View
- 98 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study examines integrating physical and mental healthcare for disadvantaged persons with type 2 diabetes mellitus and mild-to-moderate depression in the community, using a mobile application within a public-private-academic partnership.
Methods
The Korean Diabetes Association has developed a mobile application combining behavioral activation for psychological well-being and diabetes self-management, with conventional medical therapy. Participants were randomly assigned to receive the application with usual care or only usual care. Primary outcomes measured changes in psychological status and diabetes selfmanagement through questionnaires at week 12 from the baseline. Secondary outcomes assessed glycemic and lipid control, with psychological assessments at week 16.
Results
Thirty-nine of 73 participants completed the study (20 and 19 in the intervention and control groups, respectively) and were included in the analysis. At week 12, the intervention group showed significant reductions in depression severity and perceived stress compared to the control group. Additionally, they reported increased perceived social support and demonstrated improved diabetes self-care behavior. These positive effects persisted through week 16, with the added benefit of reduced anxiety. While fasting glucose levels in the intervention group tended to improve, no other significant differences were observed in laboratory assessments between the groups.
Conclusion
This study provides compelling evidence for the potential efficacy of a mobile application that integrates physical and mental health components to address depressive symptoms and enhance diabetes self-management in disadvantaged individuals with type 2 diabetes mellitus and depression. Further research involving larger and more diverse populations is warranted to validate these findings and solidify their implications.
- Complications
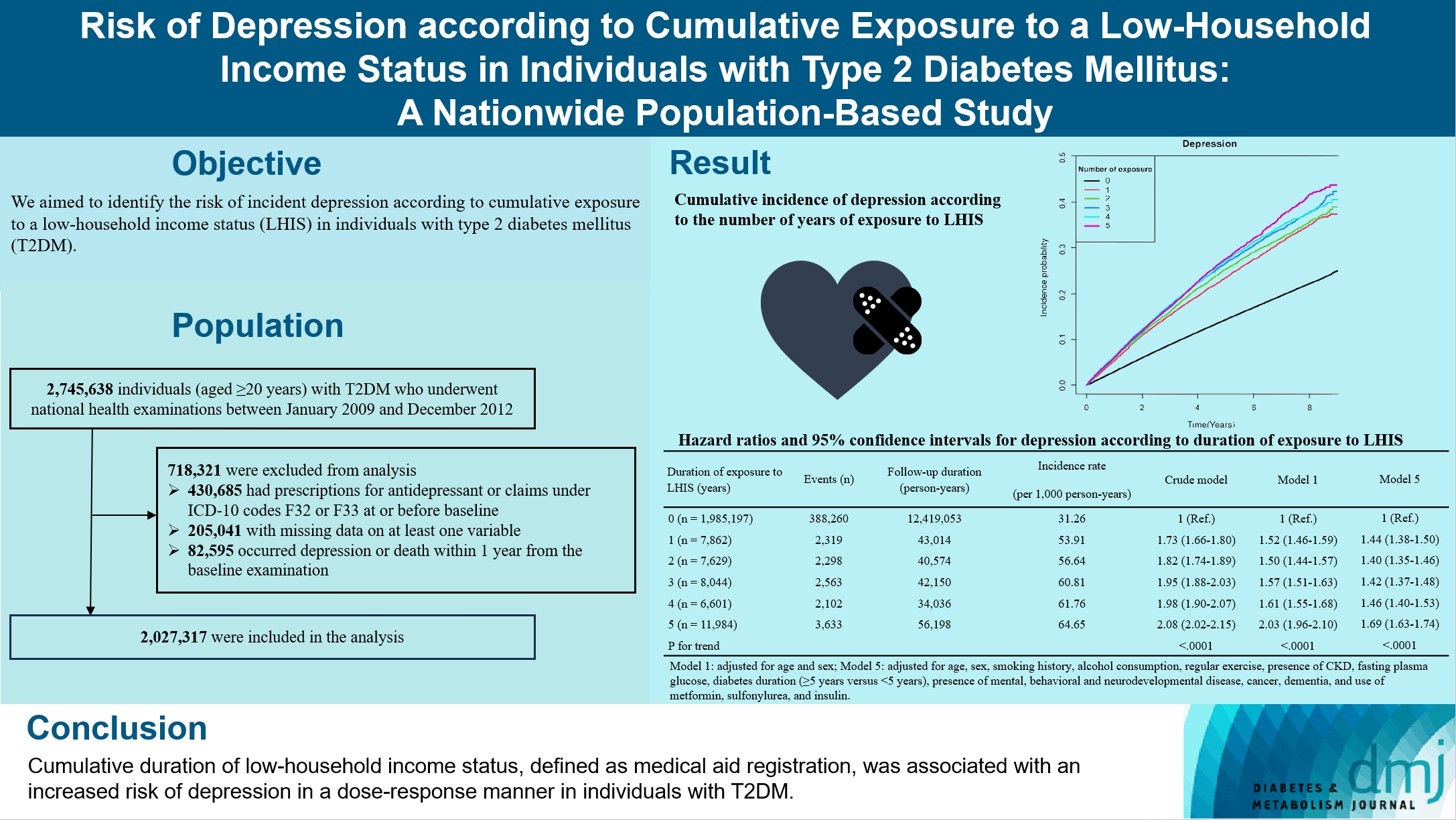
- Risk of Depression according to Cumulative Exposure to a Low-Household Income Status in Individuals with Type 2 Diabetes Mellitus: A Nationwide Population- Based Study
- So Hee Park, You-Bin Lee, Kyu-na Lee, Bongsung Kim, So Hyun Cho, So Yoon Kwon, Jiyun Park, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Kyungdo Han, Jae Hyeon Kim
- Diabetes Metab J. 2024;48(2):290-301. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0299
- 946 View
- 142 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We aimed to identify the risk of incident depression according to cumulative exposure to a low-household income status in individuals with type 2 diabetes mellitus (T2DM).
Methods
For this retrospective longitudinal population-based cohort study, we used Korean National Health Insurance Service data from 2002 to 2018. Risk of depression was assessed according to cumulative exposure to low-household income status (defined as Medical Aid registration) during the previous 5 years among adults (aged ≥20 years) with T2DM and without baseline depression who underwent health examinations from 2009 to 2012 (n=2,027,317).
Results
During an average 6.23 years of follow-up, 401,175 incident depression cases occurred. Advance in cumulative number of years registered for medical aid during the previous 5 years from baseline was associated with an increased risk of depression in a dose-dependent manner (hazard ratio [HR], 1.44 [95% confidence interval (CI), 1.38 to 1.50]; HR, 1.40 [95% CI, 1.35 to 1.46]; HR, 1.42, [95% CI, 1.37 to 1.48]; HR, 1.46, [95% CI, 1.40 to 1.53]; HR, 1.69, [95% CI, 1.63 to 1.74] in groups with 1 to 5 exposed years, respectively). Insulin users exposed for 5 years to a low-household income state had the highest risk of depression among groups categorized by insulin use and duration of low-household income status.
Conclusion
Cumulative duration of low-household income status, defined as medical aid registration, was associated with an increased risk of depression in a dose-response manner in individuals with T2DM.
- Cardiovascular risk/Epidemiology
- Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study
- Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2021;45(3):379-389. Published online December 11, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0008

- 7,522 View
- 236 Download
- 22 Web of Science
- 21 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
Previous studies have suggested that depression in patients with diabetes is associated with worse health outcomes. The aim of this study was to evaluate the risk of cardiovascular disease (CVD) and mortality in patients with diabetes with comorbid depression.
Methods
We examined the general health check-up data and claim database of the Korean National Health Insurance Service (NHIS) of 2,668,615 participants with type 2 diabetes mellitus who had examinations between 2009 and 2012. As NHIS database has been established since 2002, those who had been diagnosed with depression or CVD since 2002 were excluded. The 2,228,443 participants were classified into three groups according to the claim history of depression; normal group (n=2,166,979), transient depression group (one episode of depression, n=42,124) and persistent depression group (at least two episodes of depression, n=19,340). The development of CVD and mortality were analyzed from 2009 to 2017.
Results
Those with depression showed a significantly increased risk for stroke (transient depression group: hazard ratio [HR], 1.20; 95% confidence interval [CI], 1.15 to 1.26) (persistent depression group: HR, 1.54; 95% CI, 1.46 to 1.63). Those with depression had an increased risk for myocardial infarction (transient depression group: HR, 1.25; 95% CI, 1.18 to 1.31) (persistent depression group: HR, 1.38; 95% CI, 1.29 to 1.49). The persistent depression group had an increased risk for all-cause mortality (HR, 1.66; 95% CI, 1.60 to 1.72).
Conclusion
Coexisting depression in patients with diabetes has a deleterious effect on the development of CVD and mortality. We suggest that more attention should be given to patients with diabetes who present with depressive symptoms. -
Citations
Citations to this article as recorded by- Psychological resilience mediates the relationship between diabetes distress and depression among persons with diabetes in a multi-group analysis
Ajele Kenni Wojujutari, Erhabor Sunday Idemudia, Lawrence Ejike Ugwu
Scientific Reports.2024;[Epub] CrossRef - The mediating effect of depression on new-onset stroke in diabetic population: Evidence from the China health and retirement longitudinal study
Gege Jiang, Yaoling Wang, Liping Wang, Minfang Chen, Wei Li
Journal of Affective Disorders.2023; 321: 208. CrossRef - Frailty and outcomes in lacunar stroke
Sima Vazquez, Zehavya Stadlan, Justin M Lapow, Eric Feldstein, Smit Shah, Ankita Das, Alexandria F Naftchi, Eris Spirollari, Akash Thaker, Syed Faraz Kazim, Jose F Dominguez, Neisha Patel, Christeena Kurian, Ji Chong, Stephan A Mayer, Gurmeen Kaur, Chirag
Journal of Stroke and Cerebrovascular Diseases.2023; 32(2): 106942. CrossRef - Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
Jong Ha Baek, Yong-Moon Park, Kyung Do Han, Min Kyong Moon, Jong Han Choi, Seung-Hyun Ko
Diabetes & Metabolism Journal.2023; 47(2): 201. CrossRef - The Association between Dietary Carotenoid Intake and Risk of Depression among Patients with Cardiometabolic Disease
Jie Liang, Yuhao Wang, Min Chen
International Heart Journal.2023; 64(2): 223. CrossRef - Associations of concomitant retinopathy and depression with mortality in a nationally representative population
Zheng Lyu, Yilin Chen, Zhuoting Zhu, Xiaoyang Luo, Ying Cui, Jie Xie, Zhifan Chen, Junbin Liu, Xiyu Wu, Gabrella Bulloch, Qianli Meng
Journal of Affective Disorders.2023; 336: 15. CrossRef - Clinical insights into the cross-link between mood disorders and type 2 diabetes: A review of longitudinal studies and Mendelian randomisation analyses
Chiara Possidente, Giuseppe Fanelli, Alessandro Serretti, Chiara Fabbri
Neuroscience & Biobehavioral Reviews.2023; 152: 105298. CrossRef - Prevalence of depression and association with all-cause and cardiovascular mortality among individuals with type 2 diabetes: a cohort study based on NHANES 2005–2018 data
Zhen Feng, Wai Kei Tong, Xinyue Zhang, Zhijia Tang
BMC Psychiatry.2023;[Epub] CrossRef - Cholecystectomy Increases the Risk of Type 2 Diabetes in the Korean Population
Ji Hye Huh, Kyong Joo Lee, Yun Kyung Cho, Shinje Moon, Yoon Jung Kim, Eun Roh, Kyung-do Han, Dong Hee Koh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Annals of Surgery.2023; 278(2): e264. CrossRef - Risk of depression in patients with acromegaly in Korea (2006-2016): a nationwide population-based study
Shinje Moon, Sangmo Hong, Kyungdo Han, Cheol-Young Park
European Journal of Endocrinology.2023; 189(3): 363. CrossRef - The association between cardiovascular drugs and depression/anxiety in patients with cardiovascular disease: A meta-analysis
Lijun Zhang, Yanping Bao, Shuhui Tao, Yimiao Zhao, Meiyan Liu
Pharmacological Research.2022; 175: 106024. CrossRef - Association of mental health with the risk of coronary artery disease in patients with diabetes: A mendelian randomization study
Teng Hu, Fangkun Yang, Kewan He, Jiajun Ying, Hanbin Cui
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(3): 703. CrossRef - Comorbidity of Type 2 Diabetes Mellitus and Depression: Clinical Evidence and Rationale for the Exacerbation of Cardiovascular Disease
Mengmeng Zhu, Yiwen Li, Binyu Luo, Jing Cui, Yanfei Liu, Yue Liu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Understanding and Utilizing Claim Data from the Korean National Health Insurance Service (NHIS) and Health Insurance Review & Assessment (HIRA) Database for Research
Dae-Sung Kyoung, Hun-Sung Kim
Journal of Lipid and Atherosclerosis.2022; 11(2): 103. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Evaluation of rosmarinic acid against myocardial infarction in maternally separated rats
Himanshu Verma, Anindita Bhattacharjee, Naveen Shivavedi, Prasanta Kumar Nayak
Naunyn-Schmiedeberg's Archives of Pharmacology.2022; 395(10): 1189. CrossRef - Lipid cutoffs for increased cardiovascular disease risk in non-diabetic young people
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Kun-Ho Yoon, Seung-Hwan Lee
European Journal of Preventive Cardiology.2022; 29(14): 1866. CrossRef - Risk factors associated with mortality among individuals with type 2 diabetes and depression across two cohorts
Christopher Rohde, Jens Steen Nielsen, Jakob Schöllhammer Knudsen, Reimar Wernich Thomsen, Søren Dinesen Østergaard
European Journal of Endocrinology.2022; 187(4): 567. CrossRef - Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study (Diabetes Metab J 2021;45:379-89)
Jin Hwa Kim
Diabetes & Metabolism Journal.2021; 45(5): 789. CrossRef - Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study (Diabetes Metab J 2021;45:379-89)
Inha Jung, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2021; 45(5): 793. CrossRef - Affective Temperament and Glycemic Control – The Psychological Aspect of Obesity and Diabetes Mellitus
Natalia Lesiewska, Anna Kamińska, Roman Junik, Magdalena Michalewicz, Bartłomiej Myszkowski, Alina Borkowska, Maciej Bieliński
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4981. CrossRef
- Psychological resilience mediates the relationship between diabetes distress and depression among persons with diabetes in a multi-group analysis
- Lifestyle
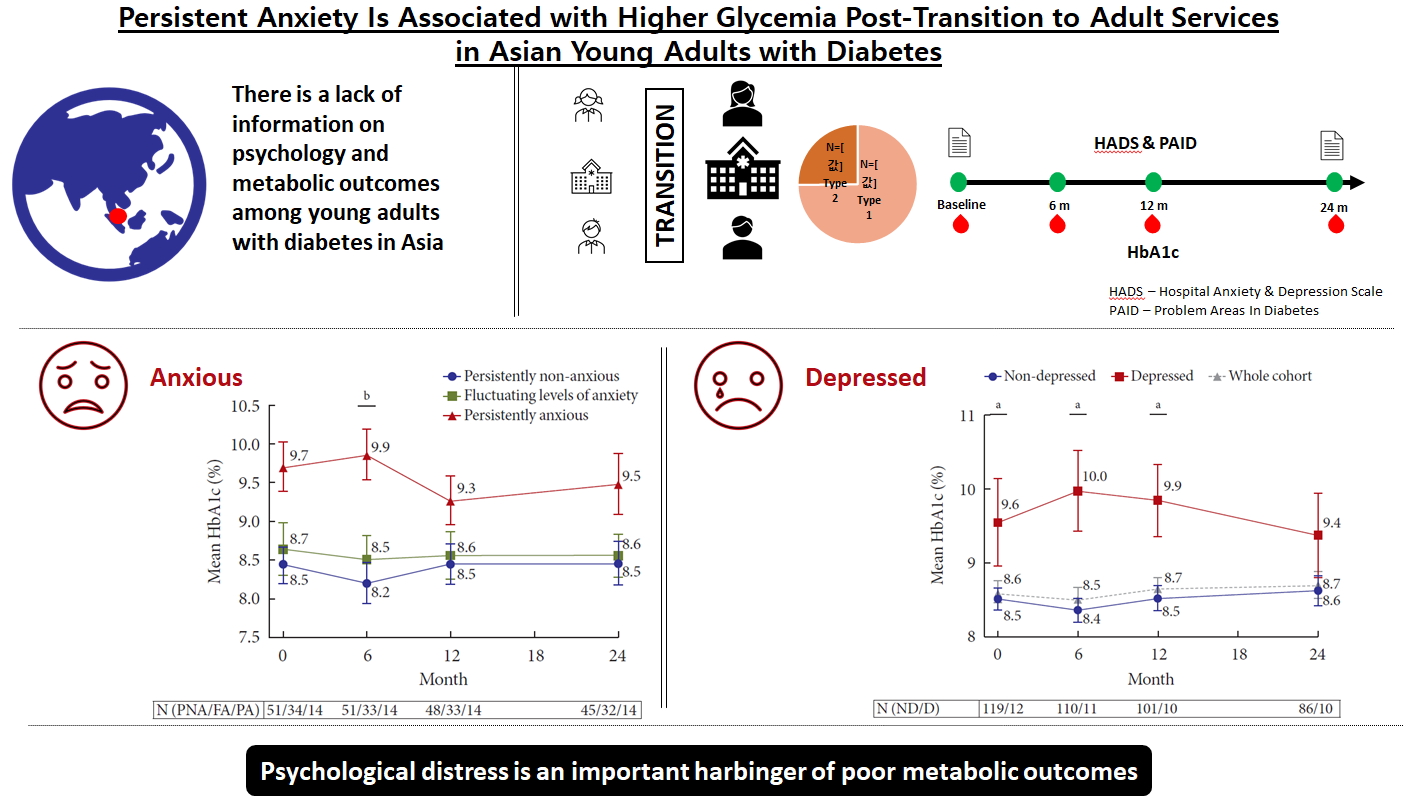
- Persistent Anxiety Is Associated with Higher Glycemia Post-Transition to Adult Services in Asian Young Adults with Diabetes
- Ling Zhu, Suresh Rama Chandran, Wee Boon Tan, Xiaohui Xin, Su-Yen Goh, Daphne Su-Lyn Gardner
- Diabetes Metab J. 2021;45(1):67-76. Published online June 15, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0226
- 5,335 View
- 104 Download
- 5 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
Background There is little longitudinal information on psychological burden and metabolic outcomes in young adults with diabetes (YAD) in Asia. We aimed to evaluate the association between psychological status and glycemia at baseline and 2 years following transition in a cohort of YAD in Singapore.
Methods Subjects with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM), aged 17 to 25 years, were recruited from the YAD clinic in Singapore General Hospital. The Hospital Anxiety and Depression and Problem Areas for Diabetes scales were administered at transition (baseline) and at 18 to 24 months. Glycosylated hemoglobin (HbA1c) assessed during routine visits was tracked longitudinally.
Results A total of 98 T1DM (74.8%) and 33 T2DM (25.2%) subjects were recruited between January 2011 and November 2017. At baseline, mean HbA1c was 8.6%±1.7%. Only 26.0% achieved HbA1c of ≤7.5% and 16.8% achieved HbA1c of <7%. At baseline, prevalence of anxiety was 29.8%. At 24 months, 14.1% had persistent anxiety. Those with persistent anxiety had the highest mean HbA1c, particularly at 6 months (persistently anxious vs. persistently non-anxious: 9.9%±1.2% vs. 8.2%±1.9%,
P =0.009). At baseline, 9.2% of subjects had depression. This group also had poorer glycemia at baseline (HbA1c of depressed vs non-depressed: 9.6%±2.1% vs. 8.5%±1.6%,P =0.04), which persisted up to 24 months.Conclusion The majority of YAD in Singapore have suboptimal glycemia. Psychological distress is a critical harbinger of poorer metabolic outcomes.
-
Citations
Citations to this article as recorded by- The Cost-Effectiveness of an Advanced Hybrid Closed-Loop System Compared to Standard Management of Type 1 Diabetes in a Singapore Setting
Daphne Gardner, Mrinmayee Lakkad, Zhiyu Qiu, Yuta Inoue, Suresh Rama Chandran, Kael Wherry
Diabetes Technology & Therapeutics.2024;[Epub] CrossRef - Impact of diabetes distress on glycemic control and diabetic complications in type 2 diabetes mellitus
Hye-Sun Park, Yongin Cho, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, Young Ju Suh, Suk Chon, Jeong-Taek Woo, Sei Hyun Baik, Kwan Woo Lee, So Hun Kim
Scientific Reports.2024;[Epub] CrossRef - The Interaction of Glycemia with Anxiety and Depression Is Related to Altered Cerebellar and Cerebral Functional Correlations
Grace E. Shearrer
Brain Sciences.2023; 13(7): 1086. CrossRef - The prevalence of anxiety in adult endocrinology outpatients: A systematic review and meta–analysis
Kelly Ann Kershaw, Ben Storer, Taylor Braund, Cassandra Chakouch, Matthew Coleshill, Sam Haffar, Samuel Harvey, Jill Newby, Gemma Sicouri, Michael Murphy
Psychoneuroendocrinology.2023; 158: 106357. CrossRef - Increased Levels of Serum Glycosylated Hemoglobin are Associated with Depressive Symptoms in a Population with Cancer (≥49 Years): An Antidepressant-Stratified Analysis
Ying Huang, Yilin Xu, Anwen Liu
Clinical Interventions in Aging.2021; Volume 16: 205. CrossRef - The Burden of Type 2 Diabetes and the Value of Achieving Near Normoglycemia from the Patient Perspective
Heather Gelhorn, Zaneta Balantac, Shraddha Shinde, Vivian Thuyanh Thieu, Kristina S. Boye
Diabetes Therapy.2021; 12(7): 1821. CrossRef
- The Cost-Effectiveness of an Advanced Hybrid Closed-Loop System Compared to Standard Management of Type 1 Diabetes in a Singapore Setting
- Cardiovascular Risk/Epidemiology
- Pre-existing Depression among Newly Diagnosed Dyslipidemia Patients and Cardiovascular Disease Risk
- Jihoon Andrew Kim, Seulggie Choi, Daein Choi, Sang Min Park
- Diabetes Metab J. 2020;44(2):307-315. Published online November 1, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0002
- 5,226 View
- 89 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Whether depression before diagnosis of dyslipidemia is associated with higher cardiovascular disease (CVD) risk among newly diagnosed dyslipidemia patients is yet unclear.
Methods The study population consisted of 72,235 newly diagnosed dyslipidemia patients during 2003 to 2012 from the National Health Insurance Service–Health Screening Cohort of South Korea. Newly diagnosed dyslipidemia patients were then detected for pre-existing depression within 3 years before dyslipidemia diagnosis. Starting from 2 years after the diagnosis date, patients were followed up for CVD until 2015. Adjusted hazard ratios (aHRs) and 95% confidence intervals (CIs) for CVD were calculated by Cox proportional hazards regression.
Results Compared to dyslipidemia patients without depression, those with depression had higher risk for CVD (aHR, 1.24; 95% CI, 1.09 to 1.41). Similarly, pre-existing depression was associated with increased risk for stroke (aHR, 1.27; 95% CI, 1.06 to 1.53). The risk for CVD among depressed dyslipidemia patients for high (aHR, 1.42; 95% CI, 1.06 to 1.90), medium (aHR, 1.17; 95% CI, 0.91 to 1.52), and low (aHR, 1.25; 95% CI, 1.05 to 1.50) statin compliance patients tended to be increased compared to patients without pre-existing dyslipidemia. The risk-elevating effect of depression on CVD tended to be preserved regardless of subgroups of smoking, alcohol consumption, physical activity, and body mass index.
Conclusion Dyslipidemia patients with pre-existing depression had increased risk for CVD. Future studies that determine CVD risk after management of depression among dyslipidemia patients are needed.
-
Citations
Citations to this article as recorded by- Mediating effect of depression on the association between cardiovascular disease and the risk of all‐cause mortality: NHANES in 2005−2018
Xinxin Ma, Huan Zhang, Yuan Tian, Yaping Wang, Ling Liu, Lei Wang
Clinical Cardiology.2023; 46(11): 1380. CrossRef - Associations of sleep duration, daytime napping, and snoring with depression in rural China: a cross-sectional study
Xueyao Zhang, Guangxiao Li, Chuning Shi, Yingxian Sun
BMC Public Health.2023;[Epub] CrossRef - Association between socioeconomic inequality and the global prevalence of anxiety and depressive disorders: an ecological study
Fatemeh Shahbazi, Marjan Shahbazi, Jalal Poorolajal
General Psychiatry.2022; 35(3): e100735. CrossRef - Impact of Alexithymia on the Lipid Profile in Major Depressed Individuals
Camille Point, Benjamin Wacquier, Marjorie Dosogne, Mohammed Al Faker, Hadrien Willame, Gwenolé Loas, Matthieu Hein, Philip W. Wertz
Journal of Lipids.2022; 2022: 1. CrossRef - Association of Depression With Cardiovascular Diseases
Zain I Warriach, Sruti Patel, Fatima Khan, Gerardo F Ferrer
Cureus.2022;[Epub] CrossRef - Fenofibrate add-on to statin treatment is associated with low all-cause death and cardiovascular disease in the general population with high triglyceride levels
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
Metabolism.2022; 137: 155327. CrossRef - Dyslipidemia prevalence and trends among adult mental disorder inpatients in Beijing, 2005–2018: A longitudinal observational study
Fude Yang, Qiuyue Ma, Botao Ma, Wenzhan Jing, Jue Liu, Moning Guo, Juan Li, Zhiren Wang, Min Liu
Asian Journal of Psychiatry.2021; 57: 102583. CrossRef - Non-HDL cholesterol level and depression among Canadian elderly—a cross-sectional analysis of the baseline data from the CLSA
Jian Liu, Surim Son, Mike Giancaterino, Chris P. Verschoor, Miya Narushima, David Moher
FACETS.2020; 5(1): 1006. CrossRef
- Mediating effect of depression on the association between cardiovascular disease and the risk of all‐cause mortality: NHANES in 2005−2018
- Clinical Diabetes & Therapeutics
- Past and Current Status of Adult Type 2 Diabetes Mellitus Management in Korea: A National Health Insurance Service Database Analysis
- Seung-Hyun Ko, Kyungdo Han, Yong-ho Lee, Junghyun Noh, Cheol-Young Park, Dae-Jung Kim, Chang Hee Jung, Ki-Up Lee, Kyung-Soo Ko
- Diabetes Metab J. 2018;42(2):93-100. Published online April 19, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.2.93
- 8,381 View
- 142 Download
- 81 Web of Science
- 82 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Korea's National Healthcare Program, the National Health Insurance Service (NHIS), a government-affiliated agency under the Korean Ministry of Health and Welfare, covers the entire Korean population. The NHIS supervises all medical services in Korea and establishes a systematic National Health Information database (DB). A health information DB system including all of the claims, medications, death information, and health check-ups, both in the general population and in patients with various diseases, is not common worldwide. On June 9, 2014, the NHIS signed a memorandum of understanding with the Korean Diabetes Association (KDA) to provide limited open access to its DB. By October 31, 2017, seven papers had been published through this collaborative research project. These studies were conducted to investigate the past and current status of type 2 diabetes mellitus and its complications and management in Korea. This review is a brief summary of the collaborative projects between the KDA and the NHIS over the last 3 years. According to the analysis, the national health check-up DB or claim DB were used, and the age category or study period were differentially applied.
-
Citations
Citations to this article as recorded by- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
Kyoung Min Kim, Kyoung Jin Kim, Kyungdo Han, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1194. CrossRef - Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
Eun-Gyoung Hong, Kyung-Wan Min, Jung Soo Lim, Kyu-Jeung Ahn, Chul Woo Ahn, Jae-Myung Yu, Hye Soon Kim, Hyun Jin Kim, Won Kim, Dong Han Kim, Hak Chul Jang
Advances in Therapy.2024;[Epub] CrossRef - Association Between Glycemic Status and the Risk of Kidney Cancer in Men and Women: A Nationwide Cohort Study
Joo-Hyun Park, Jung Yong Hong, Kyungdo Han, Jay J. Shen
Diabetes Care.2023; 46(1): 38. CrossRef - Remnant Cholesterol Is an Independent Predictor of Type 2 Diabetes: A Nationwide Population-Based Cohort Study
Ji Hye Huh, Eun Roh, Seong Jin Lee, Sung-Hee Ihm, Kyung-Do Han, Jun Goo Kang
Diabetes Care.2023; 46(2): 305. CrossRef - Efficacy of acupuncture on cardiovascular complications in patients with diabetes mellitus in Korea: A nationwide retrospective cohort
Hyejin Jung, Tiana Won, Ga-Yeon Kim, Jowon Jang, Sujung Yeo, Sabina Lim
Journal of Integrative Medicine.2023; 21(2): 176. CrossRef - Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
Jong Ha Baek, Yong-Moon Park, Kyung Do Han, Min Kyong Moon, Jong Han Choi, Seung-Hyun Ko
Diabetes & Metabolism Journal.2023; 47(2): 201. CrossRef - Epidemiology of PAH in Korea: An Analysis of the National Health Insurance Data, 2002–2018
Albert Youngwoo Jang, Hyeok-Hee Lee, Hokyou Lee, Hyeon Chang Kim, Wook-Jin Chung
Korean Circulation Journal.2023; 53(5): 313. CrossRef - Increased Risks of Open-Angle Glaucoma in Untreated Hypertension
Jihei Sara Lee, Yong Joon Kim, Sunyeup Kim, Hyoung Won Bae, Sung Soo Kim, Seung Won Lee, Chan Yun Kim
American Journal of Ophthalmology.2023; 252: 111. CrossRef - Lobeglitazone, a novel thiazolidinedione, for secondary prevention in patients with ischemic stroke: a nationwide nested case-control study
Joonsang Yoo, Jimin Jeon, Minyoul Baik, Jinkwon Kim
Cardiovascular Diabetology.2023;[Epub] CrossRef - Association between glycemic status and the risk of acute pancreatitis: a nationwide population-based study
In Rae Cho, Kyung-Do Han, Sang Hyub Lee, Young Hoon Choi, Kwang Hyun Chung, Jin Ho Choi, Namyoung Park, Min Woo Lee, Woo Hyun Paik, Ji Kon Ryu, Yong-Tae Kim
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Type 2 Diabetes and Its Association With Psychiatric Disorders in Young Adults in South Korea
Min-Kyung Lee, Su-Young Lee, Seo-Young Sohn, Jiyeon Ahn, Kyungdo Han, Jae-Hyuk Lee
JAMA Network Open.2023; 6(6): e2319132. CrossRef - Cholecystectomy Increases the Risk of Type 2 Diabetes in the Korean Population
Ji Hye Huh, Kyong Joo Lee, Yun Kyung Cho, Shinje Moon, Yoon Jung Kim, Eun Roh, Kyung-do Han, Dong Hee Koh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Annals of Surgery.2023; 278(2): e264. CrossRef - The Risk of Type 2 Diabetes Mellitus according to Changes in Obesity Status in Late Middle-Aged Adults: A Nationwide Cohort Study of Korea
Joon Ho Moon, Yeonhoon Jang, Tae Jung Oh, Se Young Jung
Diabetes & Metabolism Journal.2023; 47(4): 514. CrossRef - Scalable Infrastructure Supporting Reproducible Nationwide Healthcare Data Analysis toward FAIR Stewardship
Ji-Woo Kim, Chungsoo Kim, Kyoung-Hoon Kim, Yujin Lee, Dong Han Yu, Jeongwon Yun, Hyeran Baek, Rae Woong Park, Seng Chan You
Scientific Data.2023;[Epub] CrossRef - Association between Smoking Status and the Risk of Hip Fracture in Patients with Type 2 Diabetes: A Nationwide Population-Based Study
Se-Won Lee, Jun-Young Heu, Ju-Yeong Kim, Jinyoung Kim, Kyungdo Han, Hyuk-Sang Kwon
Endocrinology and Metabolism.2023; 38(6): 679. CrossRef - Urgensi Kepesertaan BPJS Kesehatan Sebagai Syarat Peralihan Hak Atas Tanah Berdasarkan Instruksi Presiden Nomor 1 Tahun 2022 Tentang Optimalisasi Pelaksanaan Program Jaminan Kesehatan Nasional
Nur Dwi Safitri, Fauziyah Fauziyah
Indonesian Journal of Law and Justice.2023; 1(2): 10. CrossRef - Risk of Incident Dementia According to Glycemic Status and Comorbidities of Hyperglycemia: A Nationwide Population-Based Cohort Study
Woo Jung Kim, Seo Jung Lee, Eun Lee, Eun Y. Lee, Kyungdo Han
Diabetes Care.2022; 45(1): 134. CrossRef - Effects of physical activity on cardiovascular outcomes and mortality in Korean patients with diabetes: a nationwide population-based cohort study
Inha Jung, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2022; 4(1): 42. CrossRef - Increasing Age Associated with Higher Dipeptidyl Peptidase-4 Inhibition Rate Is a Predictive Factor for Efficacy of Dipeptidyl Peptidase-4 Inhibitors
Sangmo Hong, Chang Hee Jung, Song Han, Cheol-Young Park
Diabetes & Metabolism Journal.2022; 46(1): 63. CrossRef - Changes in Patterns of Physical Activity and Risk of Heart Failure in Newly Diagnosed Diabetes Mellitus Patients
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2022; 46(2): 327. CrossRef - Synergistic association between underweight and type 2 diabetes on the development of laryngeal cancer: a national population-based retrospective cohort study
Oh. Hyeong Lee, Yong-Moon Park, Seung-Hyun Ko, Kyuna Lee, Yeonji Kim, Kyungdo Han, Jung-Hae Cho
BMC Cancer.2022;[Epub] CrossRef - Cardiovascular Implications of the 2021 KDIGO Blood Pressure Guideline for Adults With Chronic Kidney Disease
Hyeok-Hee Lee, Hokyou Lee, Raymond R. Townsend, Dong-Wook Kim, Sungha Park, Hyeon Chang Kim
Journal of the American College of Cardiology.2022; 79(17): 1675. CrossRef - Cumulative Exposure to High γ-Glutamyl Transferase Level and Risk of Diabetes: A Nationwide Population-Based Study
Ji-Yeon Park, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Endocrinology and Metabolism.2022; 37(2): 272. CrossRef - Skin accumulation of advanced glycation end products and cardiovascular risk in Korean patients with type 2 diabetes mellitus
Lee-Seoul Choi, Kainat Ahmed, Young-Seol Kim, Jung-Eun Yim
Heliyon.2022; 8(6): e09571. CrossRef - Risk for Behçet’s disease gauged via high-density lipoprotein cholesterol: a nationwide population-based study in Korea
Yeong Ho Kim, Hyun Jee Kim, Jin Woo Park, Kyung Do Han, Yong Gyu Park, Young Bok Lee, Ji Hyun Lee
Scientific Reports.2022;[Epub] CrossRef - Association between the Diabetes Drug Cost and Cardiovascular Events and Death in Korea: A National Health Insurance Service Database Analysis
Seung Min Chung, Ji-In Lee, Eugene Han, Hyun-Ae Seo, Eonju Jeon, Hye Soon Kim, Ji Sung Yoon
Endocrinology and Metabolism.2022; 37(5): 759. CrossRef - Remnant cholesterol and the risk of cardiovascular disease in type 2 diabetes: a nationwide longitudinal cohort study
Ji Hye Huh, Kyung-do Han, Yun Kyung Cho, Eun Roh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Cardiovascular Diabetology.2022;[Epub] CrossRef - Associations between migraine and major cardiovascular events in type 2 diabetes mellitus
Dae Young Cheon, Kyungdo Han, Ye Seul Yang, Yerim Kim, Sang-Hwa Lee, Chulho Kim, Jong-Hee Sohn, Mi Sun Oh, Byung-Chul Lee, Minwoo Lee, Kyung-Ho Yu
Cardiovascular Diabetology.2022;[Epub] CrossRef - Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
Jun Sung Moon, Sunghwan Suh, Sang Soo Kim, Heung Yong Jin, Jeong Mi Kim, Min Hee Jang, Kyung Ae Lee, Ju Hyung Lee, Seung Min Chung, Young Sang Lyu, Jin Hwa Kim, Sang Yong Kim, Jung Eun Jang, Tae Nyun Kim, Sung Woo Kim, Eonju Jeon, Nan Hee Cho, Mi-Kyung Ki
Diabetes & Metabolism Journal.2021; 45(5): 675. CrossRef - Umbilical Cord-Mesenchymal Stem Cell-Conditioned Medium Improves Insulin Resistance in C2C12 Cell
Kyung-Soo Kim, Yeon Kyung Choi, Mi Jin Kim, Jung Wook Hwang, Kyunghoon Min, Sang Youn Jung, Soo-Kyung Kim, Yong-Soo Choi, Yong-Wook Cho
Diabetes & Metabolism Journal.2021; 45(2): 260. CrossRef - Associations of general obesity and central obesity with the risk of hepatocellular carcinoma in a Korean population: A national population‐based cohort study
Seawon Hwang, Yong‐Moon Park, Kyung‐Do Han, Jae‐Seung Yun, Seung‐Hyun Ko, Yu‐Bae Ahn, Jae Hyun Han
International Journal of Cancer.2021; 148(5): 1144. CrossRef - Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
Jaehyun Bae, Ji Hye Huh, Minyoung Lee, Yong‐Ho Lee, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2021; 23(2): 609. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Incident Cardiovascular Disease Risk: A Nationwide Cohort Study
Hokyou Lee, Yong-ho Lee, Seung Up Kim, Hyeon Chang Kim
Clinical Gastroenterology and Hepatology.2021; 19(10): 2138. CrossRef - Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
Soo-Yeon Choi, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 263. CrossRef - Changes in metabolic syndrome status affect the incidence of end-stage renal disease in the general population: a nationwide cohort study
Eun Sil Koh, Kyung Do Han, Mee Kyoung Kim, Eun Sook Kim, Min-Kyung Lee, Ga Eun Nam, Oak-Kee Hong, Hyuk-Sang Kwon
Scientific Reports.2021;[Epub] CrossRef - Status of Diabetic Neuropathy in Korea: A National Health Insurance Service-National Sample Cohort Analysis (2006 to 2015)
Seong-Su Moon, Chong Hwa Kim, Seon Mee Kang, Eun Sook Kim, Tae Jung Oh, Jae-Seung Yun, Ho Chan Cho, Dae Jung Kim, Tae Sun Park
Diabetes & Metabolism Journal.2021; 45(1): 115. CrossRef - Thirty-six Year Trends in Mortality from Diseases of Circulatory System in Korea
Jongmin Baek, Hokyou Lee, Hyeok-Hee Lee, Ji Eun Heo, So Mi Jemma Cho, Hyeon Chang Kim
Korean Circulation Journal.2021; 51(4): 320. CrossRef - Severe hypoglycemia and the risk of end stage renal disease in type 2 diabetes
Jae-Seung Yun, Yong-Moon Park, Kyungdo Han, Hyung-Wook Kim, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Scientific Reports.2021;[Epub] CrossRef - Adherence to Antihypertensive Medication and Incident Cardiovascular Events in Young Adults With Hypertension
Hokyou Lee, Yuichiro Yano, So Mi Jemma Cho, Ji Eun Heo, Dong-Wook Kim, Sungha Park, Donald M. Lloyd-Jones, Hyeon Chang Kim
Hypertension.2021; 77(4): 1341. CrossRef - Cumulative exposure to impaired fasting glucose and future risk of type 2 diabetes mellitus
Mee Kyoung Kim, Kyungdo Han, Eun Sil Koh, Oak-Kee Hong, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Diabetes Research and Clinical Practice.2021; 175: 108799. CrossRef - Association between toothbrushing and non-alcoholic fatty liver disease
Ji-Youn Kim, Yong-Moon Park, Gyu-Na Lee, Hyun Chul Song, Yu-Bae Ahn, Kyungdo Han, Seung-Hyun Ko, Houkai Li
PLOS ONE.2021; 16(5): e0243686. CrossRef - Weight change and microvascular outcomes in patients with new-onset diabetes: a nationwide cohort study
Eun Sil Koh, Kyung Do Han, Mee Kyoung Kim, Eun Sook Kim, Min-Kyung Lee, Ga Eun Nam, Hyuk-Sang Kwon
The Korean Journal of Internal Medicine.2021; 36(4): 932. CrossRef - Current utilization patterns for long-acting insulin analogues including biosimilars among selected Asian countries and the implications for the future
Brian Godman, Mainul Haque, Santosh Kumar, Salequl Islam, Jaykaran Charan, Farhana Akter, Amanj Kurdi, Eleonora Allocati, Muhammed Abu Bakar, Sagir Abdur Rahim, Nusrat Sultana, Farzana Deeba, M. A. Halim Khan, A. B. M Muksudul Alam, Iffat Jahan, Zubair Ma
Current Medical Research and Opinion.2021; 37(9): 1529. CrossRef - Development and Validation of a Deep Learning Based Diabetes Prediction System Using a Nationwide Population-Based Cohort
Sang Youl Rhee, Ji Min Sung, Sunhee Kim, In-Jeong Cho, Sang-Eun Lee, Hyuk-Jae Chang
Diabetes & Metabolism Journal.2021; 45(4): 515. CrossRef - Cardiovascular Safety of Sodium Glucose Cotransporter 2 Inhibitors as Add-on to Metformin Monotherapy in Patients with Type 2 Diabetes Mellitus
Ja Young Jeon, Kyoung Hwa Ha, Dae Jung Kim
Diabetes & Metabolism Journal.2021; 45(4): 505. CrossRef - Nonalcoholic fatty liver disease and the risk of insulin-requiring gestational diabetes
Sang Youn You, Kyungdo Han, Seung-Hawn Lee, Mee Kyoung Kim
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef - On-Treatment Blood Pressure and Cardiovascular Outcomes in Adults With Hypertension and Left Ventricular Hypertrophy
Hyeok-Hee Lee, Hokyou Lee, So Mi Jemma Cho, Dong-Wook Kim, Sungha Park, Hyeon Chang Kim
Journal of the American College of Cardiology.2021; 78(15): 1485. CrossRef - The Effects of Glucose Lowering Agents on the Secondary Prevention of Coronary Artery Disease in Patients with Type 2 Diabetes
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2021; 36(5): 977. CrossRef - Changes in metabolic syndrome and its components and the risk of type 2 diabetes: a nationwide cohort study
Min-Kyung Lee, Kyungdo Han, Mee Kyoung Kim, Eun Sil Koh, Eun Sook Kim, Ga Eun Nam, Hyuk-Sang Kwon
Scientific Reports.2020;[Epub] CrossRef - Obesity and metabolic health status are determinants for the clinical expression of hypertrophic cardiomyopathy
Jun-Bean Park, Da Hye Kim, Heesun Lee, In-Chang Hwang, Yeonyee E Yoon, Hyo Eun Park, Su-Yeon Choi, Yong-Jin Kim, Goo-Yeong Cho, Kyungdo Han, Steve R Ommen, Hyung-Kwan Kim
European Journal of Preventive Cardiology.2020; 27(17): 1849. CrossRef - Clinical Characteristics and Prevalence of Comorbidities according to Metformin Use in Korean Patients with Type 2 Diabetes
Sang Ouk Chin, In Gyoon Ha, Sang Youl Rhee, Su Jin Jeong, Suk Chon, Sung Hoon Kim, Kyu Jeung Ahn, Sei Hyun Baik, Yongsoo Park, Moon Suk Nam, Kwan Woo Lee, Jeong Taek Woo
International Journal of Endocrinology.2020; 2020: 1. CrossRef - Impact of Mean and Variability of High‐Density Lipoprotein‐Cholesterol on the Risk of Myocardial Infarction, Stroke, and Mortality in the General Population
Byung‐Hun Han, Kyungdo Han, Kun‐Ho Yoon, Mee Kyoung Kim, Seung‐Hwan Lee
Journal of the American Heart Association.2020;[Epub] CrossRef - The association between nonalcoholic fatty liver disease and esophageal, stomach, or colorectal cancer: National population-based cohort study
Jung-Min Lee, Yong-Moon Park, Jae-Seung Yun, Yu-Bae Ahn, Kang-Moon Lee, Dae Bum Kim, Ji Min Lee, Kyungdo Han, Seung-Hyun Ko, Ming-Lung Yu
PLOS ONE.2020; 15(1): e0226351. CrossRef - Outcomes for Inappropriate Renal Dose Adjustment of Dipeptidyl Peptidase-4 Inhibitors in Patients With Type 2 Diabetes Mellitus: Population-Based Study
Sangmo Hong, Kyungdo Han, Cheol-Young Park
Mayo Clinic Proceedings.2020; 95(1): 101. CrossRef - Association Between Glycemic Status and the Risk of Parkinson Disease: A Nationwide Population-Based Study
Sang Youl Rhee, Kyung-Do Han, Hyemi Kwon, Se-Eun Park, Yong-Gyu Park, Yang-Hyun Kim, Soon-Jip Yoo, Eun-Jung Rhee, Won-Young Lee
Diabetes Care.2020; 43(9): 2169. CrossRef - A model to predict risk of stroke in middle-aged adults with type 2 diabetes generated from a nationwide population-based cohort study in Korea
Mee-Kyoung Kim, Kyungdo Han, Jae-Hyoung Cho, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
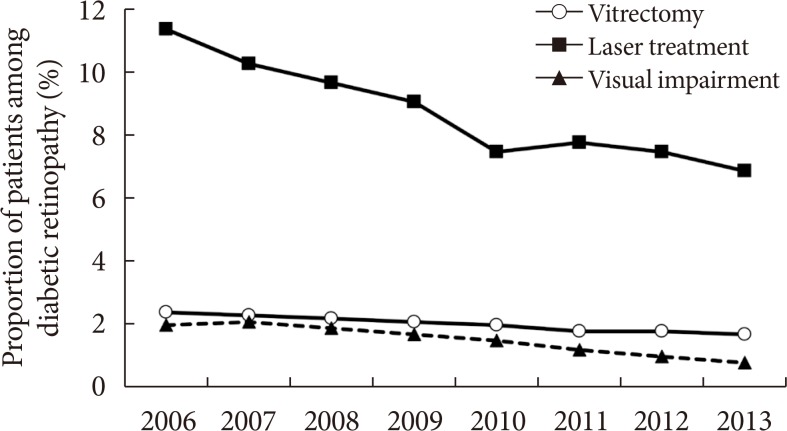
Diabetes Research and Clinical Practice.2020; 163: 108157. CrossRef - Diabetic Retinopathy and Related Clinical Practice for People with Diabetes in Korea: A 10-Year Trend Analysis
Yoo-Ri Chung, Kyoung Hwa Ha, Kihwang Lee, Dae Jung Kim
Diabetes & Metabolism Journal.2020; 44(6): 928. CrossRef - Prepregnancy smoking and the risk of gestational diabetes requiring insulin therapy
Mee Kyoung Kim, Kyungdo Han, Sang Youn You, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Scientific Reports.2020;[Epub] CrossRef - Cardiovascular Risk of Isolated Systolic or Diastolic Hypertension in Young Adults
Hokyou Lee, Yuichiro Yano, So Mi Jemma Cho, Jong Heon Park, Sungha Park, Donald M. Lloyd-Jones, Hyeon Chang Kim
Circulation.2020; 141(22): 1778. CrossRef - Middle-aged men with type 2 diabetes as potential candidates for pancreatic cancer screening: a 10-year nationwide population-based cohort study
Dong-Hoe Koo, Kyung-Do Han, Hong Joo Kim, Cheol-Young Park
Acta Diabetologica.2020; 57(2): 197. CrossRef - Predicting the Development of Myocardial Infarction in Middle-Aged Adults with Type 2 Diabetes: A Risk Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2020; 35(3): 636. CrossRef - Fasting plasma glucose level and the risk of open angle glaucoma: Nationwide population-based cohort study in Korea
Jin A. Choi, Yong-Moon Park, Kyungdo Han, Jiyoung Lee, Jae-Seung Yun, Seung-Hyun Ko, Bang V Bui
PLOS ONE.2020; 15(9): e0239529. CrossRef - Effect of Variability in Blood Pressure, Glucose and Cholesterol Concentrations, and Body Weight on Emergency Hospitalization and 30‐Day Mortality in the General Population
Seung‐Hwan Lee, Kyungdo Han, Hyuk‐Sang Kwon, Kun‐Ho Yoon, Mee Kyoung Kim
Journal of the American Heart Association.2020;[Epub] CrossRef - Does Diabetes Increase the Risk of Contracting COVID-19? A Population-Based Study in Korea
Sung-Youn Chun, Dong Wook Kim, Sang Ah Lee, Su Jung Lee, Jung Hyun Chang, Yoon Jung Choi, Seong Woo Kim, Sun Ok Song
Diabetes & Metabolism Journal.2020; 44(6): 897. CrossRef - Appropriate Medical Technology in the Era of the 4th Industrial Revolution
Sang Youl Rhee
The Korean Journal of Medicine.2019; 94(5): 387. CrossRef - Second-line glucose-lowering drugs added to metformin and the risk of hospitalization for heart failure: A nationwide cohort study
Su Jin Lee, Kyoung Hwa Ha, Jung Hyun Lee, Hokyou Lee, Dae Jung Kim, Hyeon Chang Kim, Tatsuo Shimosawa
PLOS ONE.2019; 14(2): e0211959. CrossRef - 2017 ACC/AHA Blood Pressure Classification and Cardiovascular Disease in 15 Million Adults of Age 20–94 Years
Lee, Cho, Park, Park, Kim
Journal of Clinical Medicine.2019; 8(11): 1832. CrossRef - Management of Cardiovascular Risk Factors in Elderly Diabetes Mellitus Patients
Sung Hoon Yu
The Journal of Korean Diabetes.2019; 20(4): 233. CrossRef - Cholesterol levels and development of cardiovascular disease in Koreans with type 2 diabetes mellitus and without pre-existing cardiovascular disease
Mee Kyoung Kim, Kyungdo Han, Han Na Joung, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Cardiovascular Diabetology.2019;[Epub] CrossRef - Comprehensive Efforts Are Needed to Improve the Quality of Primary Diabetes Care in Korea
Chan-Hee Jung
Endocrinology and Metabolism.2019; 34(3): 265. CrossRef - Blood Pressure and Development of Cardiovascular Disease in Koreans With Type 2 Diabetes Mellitus
Mee Kyoung Kim, Kyungdo Han, Eun Sil Koh, Eun Sook Kim, Min-Kyung Lee, Ga Eun Nam, Hyuk-Sang Kwon
Hypertension.2019; 73(2): 319. CrossRef - Weight change and mortality and cardiovascular outcomes in patients with new-onset diabetes mellitus: a nationwide cohort study
Mee Kyoung Kim, Kyungdo Han, Eun Sil Koh, Eun Sook Kim, Min-Kyung Lee, Ga Eun Nam, Hyuk-Sang Kwon
Cardiovascular Diabetology.2019;[Epub] CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study
Yoo-Ri Chung, Kyoung Hwa Ha, Hyeon Chang Kim, Sang Jun Park, Kihwang Lee, Dae Jung Kim
Diabetes & Metabolism Journal.2019; 43(5): 640. CrossRef - The Need to Improve the Quality of Diabetes Care in Korea
Seung Jin Han, Dae Jung Kim
Journal of Korean Medical Science.2019;[Epub] CrossRef - Chasms in Achievement of Recommended Diabetes Care among Geographic Regions in Korea
Sanghyun Cho, Ji-Yeon Shin, Hyun Joo Kim, Sang Jun Eun, Sungchan Kang, Won Mo Jang, Hyemin Jung, Yoon Kim, Jin Yong Lee
Journal of Korean Medical Science.2019;[Epub] CrossRef - An Age of Sodium-Glucose Cotransporter-2 Inhibitor Priority: Are We Ready?
Ji A Seo
Diabetes & Metabolism Journal.2019; 43(5): 578. CrossRef - National trends in metformin-based combination therapy of oral hypoglycaemic agents for type 2 diabetes mellitus
Jisu Kim, Susin Park, Hyunsoo Kim, Nam Kyung Je
European Journal of Clinical Pharmacology.2019; 75(12): 1723. CrossRef - HDL-Cholesterol, Its Variability, and the Risk of Diabetes: A Nationwide Population-Based Study
Seung-Hwan Lee, Hun-Sung Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Kyungdo Han, Mee Kyoung Kim
The Journal of Clinical Endocrinology & Metabolism.2019; 104(11): 5633. CrossRef - Current Management of Type 2 Diabetes Mellitus in Primary Care Clinics in Korea
Da Hea Seo, Shinae Kang, Yong-ho Lee, Jung Yoon Ha, Jong Suk Park, Byoung-Wan Lee, Eun Seok Kang, Chul Woo Ahn, Bong-Soo Cha
Endocrinology and Metabolism.2019; 34(3): 282. CrossRef - Heritability estimation of dichotomous phenotypes using a liability threshold model on ascertained family‐based samples
Wonji Kim, Soo Heon Kwak, Sungho Won
Genetic Epidemiology.2019; 43(7): 761. CrossRef - Letter: Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study (Diabetes Metab J 2019;43:640–8)
Jun Sung Moon
Diabetes & Metabolism Journal.2019; 43(6): 911. CrossRef
- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
- Clinical Care/Education
- Depressive Symptoms Are Negatively Associated with Glucose Testing and Eating Meals on Time among Individuals with Diabetes in Zambia
- Given Hapunda, Amina Abubakar, Frans Pouwer, Fons van de Vijver
- Diabetes Metab J. 2017;41(6):440-448. Published online November 17, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.6.440
- 3,555 View
- 36 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Depression is an established risk factor for cardiovascular diseases and mortality among individuals living with diabetes, and impaired self-care behaviors may play a mediating role. In Africa, this association is not very well known. In this study, we examined the associations between depressive symptoms and different aspects of diabetes self-care in Zambian individuals with diabetes mellitus.
Methods A total of 157 individuals with diabetes mellitus participated. The sample was drawn from four city hospitals in Zambia. Diabetes self-care was assessed using the diabetes self-care inventory, and depression was assessed using the major depression inventory.
Results Fifty-nine percent of the sample had type 1 diabetes mellitus. Variations in self-care activities and behaviors were reported as least adhered to by individuals with type 1 and type 2 diabetes mellitus, in adolescent and adult patients. Regression analysis indicated that there was no association between total diabetes self-care and the depression total score. However, depression was associated with poor glucose testing and not eating meals on time by patients with diabetes.
Conclusion Some variance on poor self-care was explained by demographic characteristics, specifically age, body mass index, and to some extent, socioeconomic status. Recognition and successful treatment of depression in patients with diabetes might help to optimize self-care behaviors, especially glucose testing and eating meals on time. However, this hypothesis needs further testing.
-
Citations
Citations to this article as recorded by- Self-management practices for preventing complications of type II diabetes mellitus in low and middle-income countries: A scoping review
Pauline Muthoni Maina, Melanie Pienaar, Marianne Reid
International Journal of Nursing Studies Advances.2023; 5: 100136. CrossRef - Patient-reported outcomes for diabetes and hypertension care in low- and middle-income countries: A scoping review
Sarah Masyuko, Carrie J. Ngongo, Carole Smith, Rachel Nugent, Cesario Bianchi
PLOS ONE.2021; 16(1): e0245269. CrossRef - Peripheral and Central Metabolites Affecting Depression, Anxiety, Suicidal Ideation, and Anger in Complex Regional Pain Syndrome Patients Using a Magnetic Resonance Spectroscopy: A Pilot Study
Ye-Ha Jung, Hyeonjin Kim, So Yeon Jeon, Jeong Min Kwon, Won Joon Lee, Joon Hwan Jang, Dasom Lee, Yoonji Lee, Do-Hyung Kang
Psychiatry Investigation.2018; 15(9): 891. CrossRef
- Self-management practices for preventing complications of type II diabetes mellitus in low and middle-income countries: A scoping review
- Clinical Care/Education
- The Role of Negative Affect in the Assessment of Quality of Life among Women with Type 1 Diabetes Mellitus
- Nicola R. Gawlik, Malcolm J. Bond
- Diabetes Metab J. 2018;42(2):130-136. Published online November 7, 2017
- DOI: https://doi.org/10.4093/dmj.2018.42.2.130
- 3,444 View
- 33 Download
- 2 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The purpose of this study is to determine the impact of negative affect (defined in terms of lack of optimism, depressogenic attributional style, and hopelessness depression) on the quality of life of women with type 1 diabetes mellitus.
Methods Participants (
n =177) completed either an online or paper questionnaire made available to members of Australian diabetes support groups. Measures of optimism, attributional style, hopelessness depression, disease-specific data, and diabetes-related quality of life were sought. Bivariate correlations informed the construction of a structural equation model.Results Participants were 36.3±11.3 years old, with a disease duration of 18.4±11.2 years. Age and recent glycosylated hemoglobin readings were significant contextual variables in the model. All bivariate associations involving the components of negative affect were as hypothesized. That is, poorer quality of life was associated with a greater depressogenic attributional style, higher hopelessness depression, and lower optimism. The structural equation model demonstrated significant direct effects of depressogenic attributional style and hopelessness depression on quality of life, while (lack of) optimism contributed to quality of life indirectly by way of these variables.
Conclusion The recognition of negative affect presentations among patients, and an understanding of its relevance to diabetes-related quality of life, is a valuable tool for the practitioner.
-
Citations
Citations to this article as recorded by- Menopoz dönemindeki diyabetik kadınlarda yaşanılan semptomların yaşam kalitesi parametreleri üzerindeki etkisinin incelenmesi (Prospektif Tek Grup Çalışma)
Ayşegül KOÇ, Betül ÇAKMAK, Birgül GENÇ
Turkish Journal of Diabetes and Obesity.2021; 5(2): 137. CrossRef - Type 1 Diabetes Home Care Project and Educational Consultation
Eun Chong Shin
The Journal of Korean Diabetes.2020; 21(2): 88. CrossRef - Poorer Quality of Life and Treatment Satisfaction is Associated with Diabetic Retinopathy in Patients with Type 1 Diabetes without Other Advanced Late Complications
Minerva Granado-Casas, Esmeralda Castelblanco, Anna Ramírez-Morros, Mariona Martín, Nuria Alcubierre, Montserrat Martínez-Alonso, Xavier Valldeperas, Alicia Traveset, Esther Rubinat, Ana Lucas-Martin, Marta Hernández, Núria Alonso, Didac Mauricio
Journal of Clinical Medicine.2019; 8(3): 377. CrossRef - Is Diabetes & Metabolism Journal Eligible to Be Indexed in MEDLINE?
Sun Huh
Diabetes & Metabolism Journal.2018; 42(6): 472. CrossRef
- Menopoz dönemindeki diyabetik kadınlarda yaşanılan semptomların yaşam kalitesi parametreleri üzerindeki etkisinin incelenmesi (Prospektif Tek Grup Çalışma)
- Epidemiology
- Depression and Mortality in People with Type 2 Diabetes Mellitus, 2003 to 2013: A Nationwide Population-Based Cohort Study
- Jong-Hyun Jeong, Yoo Hyun Um, Seung-Hyun Ko, Jong-Heon Park, Joong-Yeol Park, Kyungdo Han, Kyung-Soo Ko
- Diabetes Metab J. 2017;41(4):296-302. Published online August 3, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.4.296
- 4,119 View
- 54 Download
- 23 Web of Science
- 19 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Previous reports have demonstrated a bidirectional relationship between depression and diabetes mellitus (DM), accentuating a need for more intensive depression screening in DM patients. There is a relative paucity of data on the mortality of depressed DM patients in Korea.
Methods Retrospective data from January 2003 to December 2013 were collected for adult type 2 diabetes mellitus (T2DM) patients older than 30 years using the National Health Information database maintained by the Korean National Health Insurance Service (NHIS). Demographic characteristics were analyzed with descriptive statistics, and the annual prevalence of depression was estimated. Mortality rates and hazard ratios for each age group (stratified into six age groups) of patients diagnosed with T2DM in 2003 were estimated using a Cox proportional hazard method, with the Kaplan-Meier cumulative survival curve showing the overall survival rates according to the T2DM status until the given year of 2013.
Results The annual prevalence of depression was consistently higher in T2DM group from 2003 to 2013. The mortality hazard ratio was higher in the depressed in all age groups, and the risk was higher in male groups and in younger-aged groups.
Conclusion Depression was significantly associated with a high mortality risk in T2DM patients; hence, a more systematic surveillance of T2DM patients to identify risk factors for depression might contribute significantly to reducing mortality risk in this group of patients.
-
Citations
Citations to this article as recorded by- An observational study to evaluate the awareness of drug treatment, prescription pattern, adverse drug reactions, and adherence in patients of major depressive disorder
Urwashi Indrakumar Parmar, Pranali Puradkar, Kranti Kadam, Firoz Tadavi, Snehalata Gajbhiye, Shirish Joshi, Amitoj Sohal
Perspectives in Clinical Research.2024; 15(2): 59. CrossRef - Association between type 2 diabetes mellitus and depression among Korean midlife women: a cross-sectional analysis study
You Lee Yang, Eun-Ok Im, Yunmi Kim
BMC Nursing.2023;[Epub] CrossRef - The Effect of Exercise Interventions to Improve Psychosocial Aspects and Glycemic Control in Type 2 Diabetic Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Gholam Rasul Mohammad Rahimi, Reza Aminzadeh, Amin Azimkhani, Vahid Saatchian
Biological Research For Nursing.2022; 24(1): 10. CrossRef - Is it time to consider depression as a major complication of type 2 diabetes? Evidence from a large population-based cohort study
Rossella Messina, Marica Iommi, Paola Rucci, Chiara Reno, Maria Pia Fantini, Carlotta Lunghi, Mattia Altini, Francesca Bravi, Simona Rosa, Antonio Nicolucci, Paolo Di Bartolo
Acta Diabetologica.2022; 59(1): 95. CrossRef - The effects of smoking habit change on the risk of depression–Analysis of data from the Korean National Health Insurance Service
Ga Eun Kim, Min-ho Kim, Weon-Jeon Lim, Soo In Kim
Journal of Affective Disorders.2022; 302: 293. CrossRef - Association Between Diabetic Retinopathy and Insomnia Risk: A Nationwide Population-Based Study
Yoo Hyun Um, Tae-Won Kim, Jong-Hyun Jeong, Seung-Chul Hong, Ho-Jun Seo, Kyung-Do Han
Frontiers in Endocrinology.2022;[Epub] CrossRef - Implication of Melanocortin Receptor Genes in the Familial Comorbidity of Type 2 Diabetes and Depression
Mutaz Amin, Jurg Ott, Rongling Wu, Teodor T. Postolache, Claudia Gragnoli
International Journal of Molecular Sciences.2022; 23(15): 8350. CrossRef - Nutritional importance of tryptophan for improving treatment in depression and diabetes
Darakhshan Jabeen Haleem
Nutrition Reviews.2022; 81(1): 133. CrossRef - Depression but not non-persistence to antidiabetic drugs is associated with mortality in type 2 diabetes: A nested case-control study
Carlotta Lunghi, Arsène Zongo, Isabelle Tardif, Éric Demers, Joël Désiré Relwende Diendéré, Line Guénette
Diabetes Research and Clinical Practice.2021; 171: 108566. CrossRef - Single-session acceptance and commitment therapy (ACT) interventions for patients with chronic health conditions: A systematic review and meta-analysis
Cara Dochat, Jennalee S. Wooldridge, Matthew S. Herbert, Michael W. Lee, Niloofar Afari
Journal of Contextual Behavioral Science.2021; 20: 52. CrossRef - Population segmentation of type 2 diabetes mellitus patients and its clinical applications - a scoping review
Jun Jie Benjamin Seng, Amelia Yuting Monteiro, Yu Heng Kwan, Sueziani Binte Zainudin, Chuen Seng Tan, Julian Thumboo, Lian Leng Low
BMC Medical Research Methodology.2021;[Epub] CrossRef - Increased Risk of Cardiovascular Disease and Mortality in Patients with Diabetes and Coexisting Depression: A Nationwide Population-Based Cohort Study
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Yang-Hyun Kim, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2021; 45(3): 379. CrossRef - Spiritual intelligence, mindfulness, emotional dysregulation, depression relationship with mental well-being among persons with diabetes during COVID-19 pandemic
Wojujutari Kenni Ajele, Teslim Alabi Oladejo, Abimbola A. Akanni, Oyeyemi Bukola Babalola
Journal of Diabetes & Metabolic Disorders.2021; 20(2): 1705. CrossRef - Altered circulatory levels of miR-128, BDNF, cortisol and shortened telomeres in patients with type 2 diabetes and depression
Paramasivam Prabu, Subramani Poongothai, Coimbatore Subramanian Shanthirani, Ranjit Mohan Anjana, Viswanathan Mohan, Muthuswamy Balasubramanyam
Acta Diabetologica.2020; 57(7): 799. CrossRef - Intervention Strategies for Prevention of Comorbid Depression Among Individuals With Type 2 Diabetes: A Scoping Review
Eva Guérin, Hamdi Jaafar, Lisa Amrani, Denis Prud'homme, Céline Aguer
Frontiers in Public Health.2019;[Epub] CrossRef - Association between use of oral hypoglycemic agents in Japanese patients with type 2 diabetes mellitus and risk of depression: A retrospective cohort study
Hayato Akimoto, Kotoe Tezuka, Yayoi Nishida, Tomohiro Nakayama, Yasuo Takahashi, Satoshi Asai
Pharmacology Research & Perspectives.2019;[Epub] CrossRef - Depression and cardiovascular disease in elderly: Current understanding
Yaxin Zhang, Yujing Chen, Lina Ma
Journal of Clinical Neuroscience.2018; 47: 1. CrossRef - Past and Current Status of Adult Type 2 Diabetes Mellitus Management in Korea: A National Health Insurance Service Database Analysis
Seung-Hyun Ko, Kyungdo Han, Yong-ho Lee, Junghyun Noh, Cheol-Young Park, Dae-Jung Kim, Chang Hee Jung, Ki-Up Lee, Kyung-Soo Ko
Diabetes & Metabolism Journal.2018; 42(2): 93. CrossRef - Depression and Mortality in Type 2 Diabetes Mellitus
Seo Young Lee, Sung Hee Choi
Diabetes & Metabolism Journal.2017; 41(4): 263. CrossRef
- An observational study to evaluate the awareness of drug treatment, prescription pattern, adverse drug reactions, and adherence in patients of major depressive disorder
- Prevalence of Depression and Glucose Abnormality in an Urbanizing Rural Population of Bangladesh
- Khurshid Natasha, Akhtar Hussain, A. K. Azad Khan, Bishwajit Bhowmik
- Diabetes Metab J. 2015;39(3):218-229. Published online May 6, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.3.218
- 3,373 View
- 30 Download
- 9 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Depression and glucose abnormality are increasing in Bangladesh including its rural area. This study was designed to determine the prevalence of depression in an urbanizing rural population of Bangladesh with or without glucose abnormality (including diabetes mellitus [DM], and pre-diabetes which combines impaired fasting glucose and impaired glucose tolerance pre-DM).
Methods A total of 2,293 subjects aged ≥20 years were investigated. Sociodemographic and anthropometric details, blood pressure, fasting (fasting plasma glucose) and 2 hours after 75 g plasma glucose (2-hour plasma glucose), were studied. Montgomery-Asberg Depression Rating Scale was used to assess depression.
Results The overall prevalence of DM was 7.9% and pre-DM was 8.6%. Prevalence of depression was 15.31% (n=351; 95% confidence interval [CI], 1.59 to 1.36) with mean depressive score 17.62±3.49. Female were more likely to have depression (17.16%). The 22.35% of male and 29.46% of female with pre-DM and 26.58% male and 36.27% female with DM had depressive symptoms. There was no significant variation in the mean age of different groups (healthy, depressed and with glucose abnormality). Depression was significantly associated with age, marital status, occupation, high physical activity, and low body mass index. The odds ratio (OR) for depression was significantly increased in patients with glucose abnormality compared with those without pre-DM (OR, 2.49; 95% CI, 1.76 to 3.51;
P <0.000) and DM (OR, 3.27; 95% CI, 2.33 to 4.60;P <0.000).Conclusion Prevalence of depression found alarming in our study area though lesser than previous studies and it is significantly related to glucose abnormality. The study reveals that mental health should get more focused specially along with metabolic diseases.
-
Citations
Citations to this article as recorded by- Early-diagnosis of major depressive disorder: From biomarkers to point-of-care testing
Xin Zhang, Zhiheng Zhang, Weize Diao, Chuangxin Zhou, Yetong Song, Renzhi Wang, Xiaoguang Luo, Guozhen Liu
TrAC Trends in Analytical Chemistry.2023; 159: 116904. CrossRef - Differences and correlations of biochemical index levels in patients with bipolar disorder and major depressive disorder during a stable period
Yukang Tan, Chunguo Zhang, Chaohua Tang, Zhijian Li, Wensheng Chen, Huan Jing, Wenting Liang, Xiaoling Li, Guojun Xie, Jiaquan Liang, Huagui Guo
Medicine.2023; 102(25): e34172. CrossRef - Evidence of gut enteropathy and factors associated with undernutrition among slum-dwelling adults in Bangladesh
Shah Mohammad Fahim, Subhasish Das, Md Amran Gazi, Md Ashraful Alam, Mustafa Mahfuz, Tahmeed Ahmed
The American Journal of Clinical Nutrition.2020; 111(3): 657. CrossRef - Elevated depressive symptoms and risk of all-cause and cardiovascular mortality among adults with and without diabetes: The REasons for Geographic And Racial Differences in Stroke (REGARDS) study
Amandiy N.N. Liwo, Virginia J. Howard, Sha Zhu, Michelle Y. Martin, Monika M. Safford, Joshua S. Richman, Doyle M. Cummings, April P. Carson
Journal of Diabetes and its Complications.2020; 34(10): 107672. CrossRef - Impact of prediabetes on poststroke depression in Chinese patients with acute ischemic stroke
Meijuan Xiao, Qiongzhang Wang, Wenwei Ren, Zheng Zhang, Xujie Wu, Zhen Wang, Liang Feng, Siyan Chen, Jincai He
International Journal of Geriatric Psychiatry.2018; 33(7): 956. CrossRef - Response: Prevalence of Depression and Glucose Abnormality in an Urbanizing Rural Population of Bangladesh (Diabetes Metab J2015;39:218-29)
Khurshid Natasha, Akhtar Hussain, A. K. Azad Khan, Bishwajit Bhowmik
Diabetes & Metabolism Journal.2015; 39(6): 530. CrossRef - Letter: Prevalence of Depression and Glucose Abnormality in an Urbanizing Rural Population of Bangladesh (Diabetes Metab J2015;39:218-29)
Tomoyuki Kawada
Diabetes & Metabolism Journal.2015; 39(6): 528. CrossRef
- Early-diagnosis of major depressive disorder: From biomarkers to point-of-care testing
- Relationship between Opium Abuse and Severity of Depression in Type 2 Diabetic Patients
- Sepehrmanesh Zahra, Sarmast Hossein, Kord Valeshabad Ali
- Diabetes Metab J. 2012;36(2):157-162. Published online April 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.2.157
- 2,947 View
- 27 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Opium use in diabetic populations is associated with major depressive disorder (MDD). This study was designed to investigate the relationship between opium use and severity of depression in Iranian diabetic patients.
Methods In this case-control study, 642 type 2 diabetic patients were recruited from those presenting at two outpatient clinics at the Akhavan Hospital in Kashan, Iran; of them, 600 diabetic patients were included in the study and divided into two groups: opium-abusers (150 patients) and non-opium-abusers (450 patients). Clinical and demographic information was obtained through a detailed questionnaire. Depression symptomalogy and severity were assessed with the Beck Depression Inventory (BDI), and a corresponding diagnosis was made based on the Diagnostic and Statistical Manual of Mental Disorders-IV, Text Revision, 2000 (DSM-IV TR) criteria.
Results The mean depression score was higher in the opium abuse group than in the non-abuser group (29.27±1.44 vs. 18.29±1.31,
P <0.001). In general, a significant association was found between opium abuse and depression among patients (odds ratio [OR], 4.54; 95% confidence interval [CI], 2.87 to 7.44;P =0.001). No significant relationship was found between dysthymia and opium abuse (OR, 0.68; 95% CI, 0.18 to 1.192;P =0.155), while MDD was significantly higher in the opium abuser group (OR, 7.32; 95% CI, 5.20 to 12.01;P <0.001).Conclusion Depression is more frequent in opium-dependent diabetic patients, and its severity is also greater. Given these findings, opium-dependent diabetic patients should be advised about the increased risks of depression and related comorbidities.
-
Citations
Citations to this article as recorded by- Prevalence of and factors associated with depression among hill tribe individuals aged 30 years and over in Thailand
Chalitar Chomchoei, Tawatchai Apidechkul, Vivat Keawdounglek, Chanyanut Wongfu, Siriyaporn Khunthason, Niwed Kullawong, Ratipark Tamornpark, Panupong Upala, Fartima Yeemard
Heliyon.2020; 6(6): e04273. CrossRef - The prevalence of comorbid depression in patients with type 2 diabetes: an updated systematic review and meta-analysis on huge number of observational studies
Mohammad Khaledi, Fahimeh Haghighatdoost, Awat Feizi, Ashraf Aminorroaya
Acta Diabetologica.2019; 56(6): 631. CrossRef - Psychometrics of the PHQ-9 as a measure of depressive symptoms in patients with heart failure
Muna H Hammash, Lynne A Hall, Terry A Lennie, Seongkum Heo, Misook L Chung, Kyoung Suk Lee, Debra K Moser
European Journal of Cardiovascular Nursing.2013; 12(5): 446. CrossRef
- Prevalence of and factors associated with depression among hill tribe individuals aged 30 years and over in Thailand
- Depression and Self-care Behavior in Patients with Diabetes Mellitus.
- Su Yoen Kim, Jae Ho Lee, Ha Neul Kim, Dong Kyu Kim, Young Na, Guil Sun Kim, Mee Kyoung Kim, Ki Hyun Baek, Moo IL Kang, Kwang Woo Lee, Ki Ho Song
- Korean Diabetes J. 2009;33(5):432-438. Published online October 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.5.432
- 2,553 View
- 46 Download
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Depression is known to be a risk factor for type 2 diabetes mellitus. Conversely, diabetes is also a risk factor for depression, and patients with diabetes have nearly twice the risk of comorbid depression as the general population. Depression in patients with diabetes may cause poor clinical outcomes through lower adherence to self-care activities such as exercise, diet control, and glucose monitoring. Furthermore, diabetic patients with depression are more likely to suffer from microvascular or macrovascular complications. We explored the prevalence of major depressive disorder in Korean diabetic patients and its impact on self-care activities and glucose control. METHODS: We surveyed depressive symptoms and self-care activities in 191 type 2 diabetic patients from the outpatient clinic of the St. Mary's hospital. Two questionnaires were used for assessment, the Harvard Department of Psychiatry/National Depression Screening Day Scale (HANDS) and the Summary of Diabetes Self-Care Activities (SDSCA). RESULTS: Of the 191 respondents who completed questionnaires, 39 (20.4%) patients were categorized as having major depressive disorder. Among the depressed patients, only six (15.3%) had been previously evaluated and managed for their psychiatric problems. The incidence of depression was significantly higher in female diabetic patients compared to patients without depression (74.4% vs. 45.4%, P<0.001). Patients with depression showed significantly poorer diet control (18.5 vs. 15.9, P = 0.046) and less glucose monitoring (4.1 vs. 2.7, P = 0.047). However, there were no differences in exercise, foot care, or smoking status between the two groups. Additionally, metabolic parameters such as HbA1C and lipid profile were not significantly different between the two groups. CONCLUSION: Many diabetic patients are suffering from depression and exhibit poorer self-care activities than patients without depression. Identifying and managing depressed diabetic patients may help improve their self-care activities. -
Citations
Citations to this article as recorded by- The Effects of the 2030 Diabetes Camp Program on Depression, Anxiety, and Stress in Diabetic Patients
Jin Hee Jung, Jung Hwa Lee
The Journal of Korean Diabetes.2019; 20(3): 194. CrossRef - Association of Resilience and Depression with Self-care Competence in Adult Patients with Diabetes Mellitus
Youngrye Park, Eun Hee Jang, Ji Ok Kim
Korean Journal of Adult Nursing.2018; 30(5): 555. CrossRef - Health-Related Quality-of-Life and Diabetes Self-Care Activity in Elderly Patients with Diabetes in Korea
Hacksun Kim, Kisook Kim
Journal of Community Health.2017; 42(5): 998. CrossRef - Associations between Smoking, Drinking and Depression among Korean Adults: The 5th Korea National Health and Nutrition Examination Survey
Sun Mi Park, Mi Ah Han, Jong Park, So Yeon Ryu, Seong Woo Choi, Hwan Ho Shin, Mi Hyun Joo
Korean Journal of Health Promotion.2016; 16(2): 111. CrossRef - Diabetes and Depressive Symptoms in Korean Women: The Fifth Korean National Health and Nutrition Examination Survey (2010-2011)
Han Na Sung, Hong Seok Chae, Eung Soo Kim, Jong Sung Kim
Korean Journal of Family Medicine.2014; 35(3): 127. CrossRef - Effects of Abdominal Circumference, Blood Lipids and Blood Pressure according to Diabetes with VO2peak
Sang-Nam Nam, Jung-Beom Park, Hyoung-Ju Lee
The Journal of the Korea Contents Association.2012; 12(12): 363. CrossRef - Effects of a Cardiovascular Risk Reduction Intervention With Psychobehavioral Strategies for Korean Adults With Type 2 Diabetes and Metabolic Syndrome
Chun-Ja Kim, Dae-Jung Kim, Hyung-Ran Park
Journal of Cardiovascular Nursing.2011; 26(2): 117. CrossRef
- The Effects of the 2030 Diabetes Camp Program on Depression, Anxiety, and Stress in Diabetic Patients
- Diabetes, Depression and Doctor-Patient Relationship.
- Hong seock Lee, Joong seo Lee, Heung pyo Lee, Chul eun Jeon
- Korean Diabetes J. 2009;33(3):178-182. Published online June 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.3.178
- 1,923 View
- 17 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF - Although diabetes mellitus (DM) is treatable, it is still not curable. Its chronicity is associated with a high prevalence of psychiatric disorders, especially depression in type 2 DM and learned helplessness in type 1 DM. In turn, this depression and helplessness may affect a patient's adherence to medical appointments, compliance to treatment, and effective doctor-patient relationships, which are vital to promising outcomes. This study reviews the existing literature regarding the interactional relationships between depression, DM and the doctor/patient relationship, and also suggests certain aspects of the doctor/patient relationship which can contribute to more successful treatment outcomes.
-
Citations
Citations to this article as recorded by- Diabetes and depression
Eon-Ju Jeon
Yeungnam University Journal of Medicine.2018; 35(1): 27. CrossRef - Comparative Study on HbA1C, Self-care Behavior, and Quality of Life by Depression Status in Type II Diabetic Patients
Young-Min Jeong, Mi-Young Kim
Journal of Korean Academy of Fundamentals of Nursing.2012; 19(3): 353. CrossRef - Perception and Use of Complementary and Alternative Medicine in Diabetic Patients in Busan Area
Hyeryung Kim, Eunjoo Son, Mikyung Kim, Eunsoon Lyu
Korean Journal of Community Nutrition.2011; 16(4): 488. CrossRef
- Diabetes and depression

 KDA
KDA
 First
First Prev
Prev





