
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 34(1); 2010 > Article
-
Original ArticleFactors that Affect Medication Adherence in Elderly Patients with Diabetes Mellitus
- Kyung-Ae Park1, Jung-Guk Kim2, Bo-Wan Kim2, Sin Kam3, Keon-Yeop Kim3, Sung-Woo Ha4, Sung-Taek Hyun5
-
Korean Diabetes Journal 2010;34(1):55-65.
DOI: https://doi.org/10.4093/kdj.2010.34.1.55
Published online: February 28, 2010
- 4,478 Views
- 96 Download
- 35 Crossref
1Department of Public Health, Kyungpook National University Graduate School, Daegu, Korea.
2Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu, Korea.
3Department of Preventive Medicine, Kyungpook National University School of Medicine, Daegu, Korea.
4Dr. Ha's Internal Medicine, Daegu, Korea.
5Dr. Hyun's Internal Medicine, Daegu, Korea.
- Corresponding author: Jung-Guk Kim. Department of Internal Medicine, Kyungpook National University School of Medicine, 101, Dongin-dong 2-ga, Jung-gu, Daegu 700-422, Korea. jugkim@knu.ac.kr
• Received: October 19, 2009 • Accepted: February 16, 2010
Copyright © 2010 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- This study was conducted to evaluate the factors affecting medication adherence in geriatric diabetic patients treated at private clinics and tertiary hospitals. We compared the factors affecting medication adherence between these two patient groups.
-
Methods
- We included 108 diabetic patients older than 65 years treated at one tertiary hospital and 157 patients older than 65 years treated at two private clinics. We conducted an interview survey based on the Health Belief Model, and used a questionnaire that included the self-efficacy variable. For the medication adherence, Morisky's self-report was used.
-
Results
- The medication adherence based on Morisky's self-report was significantly higher in tertiary hospital patients (61.1%) compared to private clinic patients (43.2%) (P < 0.01). The results showed that drug storage and self-efficacy were factors affecting adherence to medication in tertiary hospital patients (P < 0.05). The adherence was high in cases of proper drug storage (odds ratio [OR], 5.401) and in cases with high self-efficacy (OR, 13.114). In private clinic patients, financial level (P < 0.05), recognition of the seriousness of diabetes complications (P < 0.05) and self-efficacy (P < 0.01) were associated with medication adherence. The medication adherence was significantly lower in patients whose financial state were moderate than those with lower (OR, 0.410), and medication adherence was significantly higher in patients who had higher perceived severity (OR, 2.936) and in patients with higher self-efficacy (OR, 4.040).
-
Conclusion
- Different strategies should be used to increase medication adherence in geriatric diabetic patients, depending on institutions whether they are treated.
- The elderly population has been rapidly increasing in Korea. In the 1960s, the elderly population older than 65 years was only 2.9% of the general population. Both the absolute number and composition ratio of the elderly population have been continuously increasing, with the estimated elderly population of 11.0% in 2010, 14.9% in 2019, and more than 24% in 2030 [1].
- An increase in the elderly population leads to an increase in the number of elderly patients. According to the National Health Insurance Corporation (2005), diabetes mellitus has the highest treatment amount per elderly patient, and, together with hypertension, diabetes mellitus is considered the representative chronic disease in elderly patients. However, in a study of diabetes patients visiting the tertiary hospitals in Korea, only 36.7% of patients had glycosylated hemoglobin less than 7%, indicating that blood glucose levels are not being controlled at a satisfactory level. Therefore, in order to reduce the number of fatal complications associated with diabetes mellitus, aggressive glycemic control is necessary to achieve target blood glucose levels [2].
- To achieve this goal, it is necessary to encourage therapeutic adherence, so that patients observe the medical recommendations, take their medication, change their life style, and follow the recommendations of the clinicians [3]. Thus, it is necessary to understand the level of therapeutic adherence and factors that affect adherence.
- Medication non-adherence lowers the effectiveness of treatments and raises medical costs. Therefore, non-adherence is an important issue in the management of patients with chronic diseases. In elderly patients, medication adherence is decreased due to multiple prescriptions, the deterioration of recognition and memory, and physical limitations such as visual acuity, hearing, etc. According to some studies, the frequency of medication non-adherence in elderly patients is as high as 55%. Further, about 20% of cases have prescribed drugs that are not being taken [4].
- In other countries, the interest in therapeutic adherence has increased over time; from 1960 to 1995, 11,600 papers on therapeutic adherence have been reported [3]. In Korea, studies on therapeutic adherence have been reported, ranging from systemic studies on the therapeutic adherence in children and therapeutic adherence for hypertension [5,6] to numerous studies on the patients using community health centers or health subcenter [7-13]. In addition, in Korea, numerous studies regarding the survey of the state of medication and the medication guidelines have been conducted in elderly patients [14-18]. Nonetheless, studies on the medication adherence in elderly patients with diabetes mellitus are rare [19,20], and it is difficult to find systemic studies using a model to explain medication adherence in elderly patients with diabetes mellitus.
- In Korea, most elderly diabetes patients use community medical institutions. We assessed the factors that affect medication adherence using a systemic model, and we compared diabetes patients older than 65 years treated at private clinics (primary medical institution) with those treated at university hospital (tertiary medical institution). The data from this study can be used to develop strategies to improve the medication adherence for more effective treatments.
INTRODUCTION
- Study subjects
- Our study group included diabetes patients older than 65 years treated at either a single tertiary hospital or at two private internal medicine clinics located in the Daegu city. We included patients who had been taking diabetes medication for longer than 6 months and who were treated at the current medical institution for longer than 6 months. Each patient completed a structured questionnaire and an interview survey with a trained examiner who asked questions and recorded the answers. In total, 265 patients were included in the study with 108 patients from the tertiary hospital and 157 patients from the private clinics.
- Data collection
- From June 15 to June 19, 2009, we conducted a preliminary study on 20 diabetes patients using a questionnaire based on the Health Belief Model used to investigate therapeutic adherence. Based on the preliminary results, we revised and supplemented the questionnaire. For one month from June 29, 2009, to July 30, we interviewed diabetes patients older than 65 years who visited the diabetes clinic of one tertiary hospital and two private internal medicine clinics. For patients who agreed to be included in the study, examiners conducted interview surveys using a structured questionnaire. Because the research subjects were elderly patients, direct interview methods were used to help communicate accurate meanings and to ensure the collection of accurate data. To minimize the variance among answers associated with different examiners, the examiners were educated on the questionnaire questions and the questioning skill, and interim assessments were performed thoroughly.
- Analysis model
- To assess factors associated with the therapeutic adherence, it is not sufficient to simply list individual variables or social environmental variables. To obtain systemic research results, a study model is required [21].
- For the investigation of the therapeutic adherence, the Health Belief Model, social learning theory, consumer information processing theory, Fishbein's Theory of reasoned action, Multi-attribute attitude model, etc., are used as research models. Among these, the Health Belief Model was initially developed to investigate preventive health behaviors. Nonetheless, recently, it has been used widely to study the therapeutic adherence associated with illness behavior and sick role behavior, and it has been used most widely as a health-related behavior model in the past 30 years [22].
- Regarding the Health Belief Model, the value-expectancy theory that is the prerequisite of this model has been accepted widely as the theory explaining the motivation of humans. By establishing the belief or attitude that can be altered as the determining factor of the behavior, it is possible to actually utilize research results. In addition, with the Health Belief Model, data can be collected by diverse methods, the data can include as many variables as the investigator desires, and the number of questions required to measure the effect of the major variables is relatively small. Thus the Health Belief Model is an economical model [23].
- In our study, because the study subjects were elderly patients, we kept the number of questions relatively small, and thus made the study economical. Once we selected the Health Belief Model, we could collect data using various methods, including the self-efficacy variable suggested by Bandura [24], which studies the effects on medication drug intake (Fig. 1).
- Therapeutic adherence means that the patient observes the medical recommendations, taking the medication, and maintaining a lifestyle as recommended by clinicians [3]. In our study, we focused on medication adherence.
- The methods typically used to measure medication adherence include measuring serum drug level, measuring pharmacological marker levels, performing pill counts (pill count method), and patient interview, etc. Among these methods, the adherence assessment method by interview involves directly asking the patient whether they take the drugs. The interview approach is simple and thus this approach was not popular among investigators. Nevertheless, since the approach is readily conducted and other methods assessing adherence have the limited usefulness, such method assessing the adherence has drawn attentions gradually. Methods that assess adherence by interview can be broadly classified into two types of methods. The first approach is to lead the response of the patients by using non-critical and non-threatening questions, and the second approach is to assess the adherence using a structured questionnaire, such as the self-report questionnaire. In our study, we evaluated the medication adherence using the Morisky self-report questionnaire, which was previously validated. The questionnaire is designed validate the assessment of the medication adherence, and in addition, to understand and evaluate the adherence barrier, which is advantageous for clinicians supporting patients who have problems with adherence [25]. In other words, by answering "yes" even to one out of 4 questions, the patients are indicating their non-adherence experience. The self-report questionnaire has the advantage that it is simple and can be conducted in any clinical environment rapidly. This method saves time and improves the validity of the medication adherence [26].
- Morisky's self-questionnaire consists of 4 questions: i) Do you ever forget to take your medicine? ii) Are you careless at times about taking your medicine? iii) When you feel better, do you sometimes stop taking your medicine? iv) Sometimes if you feel worse when you take the medicine, do you stop taking it? If the patient answers negatively to just one out of 4 questions, it is defined as 'non-adherence'.
- Analytical methods
- The independent variables to explain the medication adherence of dependent variables include socio-demographic characteristics, lifestyle, the characteristics associated with disease and medication, and variables such as susceptibility, severity, benefit, barrier, cues to action in the Health Belief Model and self-efficacy variable.
- Socio-demographic status and lifestyle variables included age, gender, education level, residence, financial level, the type of health security, person paying treatment fees, marital status and subjective health status, meal habits, exercise state, drinking state, and smoking state.
- The characteristics associated with disease and medication include the number of currently ailing diseases, the number of medical institutions visited for the current ailment, time since diabetes diagnosis, the number of diabetes drugs, the times of diabetes drug medication per day, the status of the insulin injection, and the condition of drug storage. The total current ailing diseases were classified as cases with only diabetes, 2 diseases, and more than 3 diseases. The time since diabetes diagnosis was classified into 3 groups based on less than 5 years, between 5 and 10 years and more than 10 years. The number of current diabetes medications was classified as either one drug or more than two drugs. The frequency of medication was classified as once or more than two times. The drug storage condition was classified as well storage when the patient stored drug according to instructions of doctors or pharmacists or stored at dry room temperature, and bad storage when the patient stored any drug in a refrigerator, or stored anywhere.
- Among variables included in the Health Belief Model, susceptibility was determined by the answer to the question "Do you think that it is possible to develop complications if you do not take diabetes medication as instructed?" Answers were originally ranked on a 5-point scale from "very high" to " not at all". However, there were few answers of "No" and "not at all" so the answers were ultimately divided into 3 scales: "very high", "high", and "lower than moderate". The severity was measured according to answers to the question "Do you think that complications caused by diabetes are very severe?", with the answers graded on a 5-point scale ranging from "very severe" to "not severe at all". These answers were also eventually divided into 3 scales. Benefit was assessed by the question "Do you think that correctly taking your diabetes medication will help to prevent complications?" The answers to this question were divided into 3 scales, as was done with susceptibility. The barrier level was evaluated by the question: "Is it difficult to use hospitals to treat diabetes?" The answers for the barrier level question were divided into 2 categories, either "more than so" or "less than so so". The cue of action was measured by whether the patient knew another patient in the vicinity who had developed diabetic complications. For self-efficacy, the confidence in taking diabetes medication was measured by a 5-point scale, and the answers were classified as "very confident, "confident", and "not so confident".
- As independent variables, for the multivariate analysis, we chose the significant variables among general characteristics such as financial level, meal habits, and the state of drug storage. Health security type was related to financial level, and there were only two cases of medical aid at tertiary hospital, so this variable was excluded from the analysis. For the variables of the Health Belief Model, including the susceptibility, severity, and benefit variable, there were fewer than 10 patients who answered 'lower than moderate'. For self-efficacy, only 6 private clinic patients answered 'very high'. When these variables were considered as the same category at bivariate analysis and multiple logistic regression analysis was performed, the model fitness was significant, and the results were similar to those from the bivariate analysis. Nevertheless, the Hosmer and Lemeshow test showed that the significant probability was low, and thus the model was considered to have some problems. As a result, we repeated the analysis after reclassifying susceptibility, severity and benefit variable as "very high" and "lower than high", and reclassifying self-efficacy as "more than high" and "lower than moderate".
- In the analysis of medication adherence, any patient answering "no" to all 4 questions was considered to be adherent, and any patient answering "yes" to more than one of the 4 questions was considered to be non-adherent. Then, we compared patients from tertiary hospitals with those from the private clinics.
- We performed bivariate and multivariate analysis with medication adherence as the dependent variable, and general characteristics, Health Belief Model variables and the self-efficacy variable as independent variables. For the bivariate analysis, the χ2-test was used. In the multivariate analysis to identify factors that affect the medication adherence, we considered the medication adherence as a dependent variable, and the significant variables among general characteristics, the variables of the Health Belief Model, and self-efficacy as independent variables, and we performed multiple logistic regression analysis.
METHODS
Research frame
Assessment of the medication adherence
Study variables
Analytical method
- Medication adherence according to general characteristics
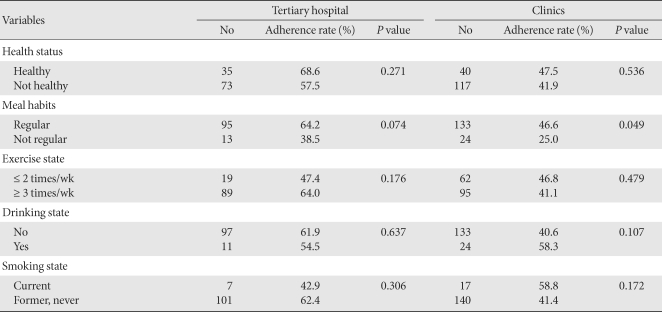
- The medication adherence in patients with diabetes, as measured by the Morisky's tool, was 61.1% for tertiary hospital patients, which was significantly higher than 43.3% for private clinic patients (P < 0.01). The result of the bivariate analysis between the medication adherence and socio-demographic variables showed that in tertiary hospital patients, none of variables showed a significant association, and in private clinic cases, there was a statistically significant association between adherence and financial level and health security type. The medication adherence was significantly high in the cases with a low financial level (P < 0.05). With regard to health security type, the adherence of medical aid cases was higher than that of health insurance cases (P < 0.05) (Table 1).
- In the bivariate analysis of the medication adherence and subjective health state and lifestyle variables, the adherence of the cases with a regular meal habit was higher than that with irregular cases. In the tertiary hospital cases, the association was at the borderline level (P = 0.074). In the private clinic cases, the association was significantly high (P < 0.05) (Table 2).
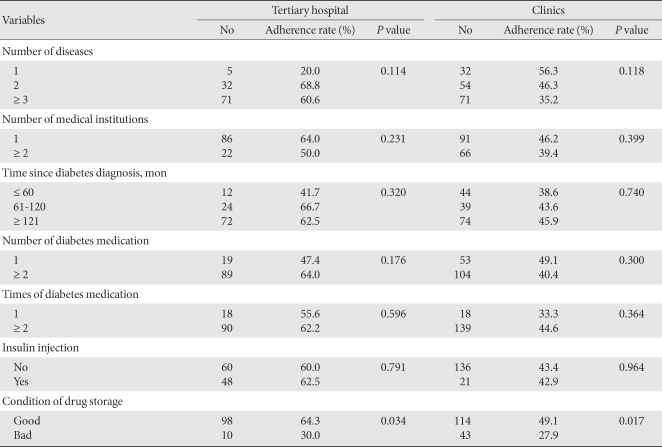
- Between the medication adherence and the variables associated with diseases and medication, the way drugs were stored was significantly associated in both tertiary hospital and private clinic cases, and the adherence of patients using better drug storage was higher (P < 0.05) (Table 3).
- Medication adherence by Health Belief Model and self efficacy variable
- In the bivariate analysis between the medication adherence and the variables of the Health Belief Model, in tertiary hospital cases, the barrier to hospital use was lower so the adherence was significantly higher (P < 0.05). In private clinic cases, in the cases recognizing that the complications caused by diabetes are very serious, the adherence was significantly higher (P < 0.01). In the patients who knew a person in the vicinity who had developed diabetes complications, in other words, the patients with a cue to action, the adherence was borderline high (P = 0.092). Between the medication adherence and self-efficacy, in both tertiary hospital and private clinic cases, when self-efficacy was high, the adherence was significantly high (P < 0.01) (Table 4).
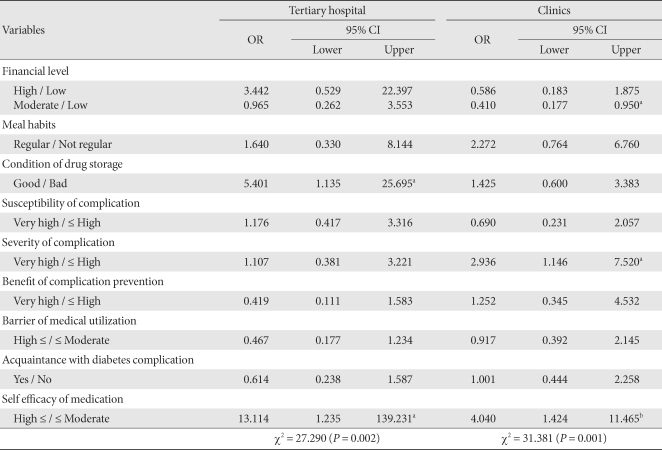
- Factors affecting medication adherence
- To evaluate the factors directly affecting the medication adherence, multiple logistic regression analysis was performed. The result showed that in tertiary hospital cases, the significant variables were the drug storage condition and self-efficacy (P < 0.05). The odds ratio was 5.401 for cases with good storage practice compared to cases with poor storage practice. The odds ratio of cases with high self-efficacy in comparison to cases with low self-efficacy was 13.114. The significant variables in private clinic cases were financial level and severity for diabetes complications and self-efficacy, and the odds ratio for cases with moderate financial state compared to cases with low financial state was 0.410 (P < 0.05) and the odds ratio for cases recognizing the severity of diabetes complications compared to cases not recognizing the severity was 2.936 (P < 0.05). The odds ratio of the cases with high self-efficacy versus low self-efficacy was 4.040 (P < 0.01) (Table 5).
RESULTS
- Medication non-adherence lowers treatment effectiveness, and is thus a very important problem in the management of patients with chronic diseases requiring long-term treatments. Based on the Health Belief Model, we examined the factors that affect the medication adherence and then we compared these factors between patients treated at private clinics versus patients treated at tertiary hospitals. The data from this study can be used to develop strategies to improve the medication adherence for more effective treatments.
- In our study, we applied the Morisky's tool to elderly diabetes patients, and we determined that the medication adherence of was 61.1% for tertiary hospital patients and 43.3% for private clinics. The significant difference between adherence is thought to be due to the fact that patients treated at tertiary hospitals consider the disease to be more severe.
- Based on our bivariate analysis of socio-demographic characteristics, in private clinics cases, adherence was significantly high in the group with a low financial level and in the group with medical aid for health security. In contrast, in the tertiary hospital cases, the group with a high financial level had a high adherence, although the association was not significant. In our study, we used Morisky's tool, so it is difficult to elucidate why financial level and health security type might affect adherence differently in tertiary and private clinic patients.
- In studies from other countries, it has been reported that the higher the education level, the higher the adherence of diabetes patients [27]. Nonetheless, in our study, we did not detect this association.
- In the group with a regular meal routine, the adherence was high, possibly because diabetes medication is usually taken prior to meal or 30 minutes after a meal, and therefore, these patients are not likely to forget their medication. In our study, the proportion of patients with a regular meal routine was 88.0% for tertiary hospital patients and 84.7% for private clinic patients. In comparison, another Korean study of meal habits in type 2 diabetes patients reported that only 39.1% had a regular meal routine [28].
- According to Kim et al. [20], a cause of low medication adherence is having to take multiple medications and taking drugs prescribed by more than 2 medical institutions. Delamater [29] reported that among the factors associated with medication adherence, adherence with a simple prescription is higher than that for a more complex prescription. In our study, both tertiary hospital and private clinic patients had a higher adherence if they were visiting one medical institution for treatment versus more than 2 institutions. In private clinic cases, the adherence with medication of 1 diabetes drug per day was higher than with more than 2 drugs.
- In both tertiary hospital and private clinic patients, when drugs were stored properly, the adherence was significantly higher than when the drugs were improperly stored. This result suggests that adherence is higher in the patients who could understand how drugs should be stored, whether in a refrigerator or at dry room temperature away from sunlight. In our study, the proportion of patients who stored all drugs in the refrigerator was 8.3% for tertiary hospital patients and 5.7% for private clinic patients. Due to humidity within the refrigerator, drugs may become wet, or may become altered if stored for a long time. Thus, it is important to store prepared antibiotics syrups or insulin injection in a refrigerator, and store other drugs as instructed by doctors or pharmacists.
- In the USA, the Omnibus Budget Reconciliation ACT of 1990 (OBRA 90) was established to require pharmacists to inform patients of the contents and special instructions for medications. The OBRA 90 contains the name of the drug, administration method, administration type, administration duration, special instructions to patients, warning, usage, possible common or severe side effects, contraindication and the action to be taken when such an event occurs or methods to avoid it, the method to self-monitor the efficacy of drug, appropriate storage methods, substitute method when medication is forgotten, etc. In Korea, the importance of medication instruction was also recognized, and the pharmaceutical affairs law defines the medication instruction to provide the information of the name of drug, dosage, efficacy, storage methods, side effects, interaction, and in the obligation. And in observance of article 24, it is clearly stated that when pharmacists prepare drugs, the necessary medication instruction should be provided to patients.
- In chronic diseases such as diabetes mellitus, drugs are generally prescribed for longer than one month, and thus it is important to provide medication instruction to be able to understand and follow directions regarding drug storage.
- In both tertiary hospital and private clinics, in the cases where the diagnosis of diabetes is longer than 5 years, in comparison with the cases of lesser than 5 years, the adherence was higher, but not significantly so. Schatz [30] reported that the longer the illness period in diabetes patients, the higher the adherence in terms of performing the blood glucose test at home, etc. Similarly, in the study reported by Lee et al. [11], in patients with hypertension, which is a representative chronic disease that occurs together with diabetes, a longer diagnosis period was significantly associated with a higher medication adherence.
- Among the variables included in the Health Belief Model, the variables associated with the adherence were the barrier level in tertiary hospital patients and the recognition diabetes complication severity in private clinic patients. In addition, in both tertiary hospital and private clinic cases, a higher patient self-confidence with medication, in other words, a higher self-efficacy, was associated with a significantly higher adherence.
- In our multiple logistic regression analysis, we found a significantly high adherence in tertiary hospital patients who properly stored their drugs (odds ratio [OR], 5.401) and in cases with a high self-efficacy (OR, 13.114). In private clinics, the adherence was significantly high in patients who considered complications more seriously (OR, 2.936) and in patients with high self-efficacy (OR, 4.040), and the adherence was significantly low in patients whose financial state were moderate than those with lower (OR, 0.410).
- In Korea, study conducted on patients with hypertension examined the adherence using the Health Belief Model [12], and found that the benefit and the barrier level affected adherence. In a study conducted by Park et al. [5] on the guardians of pediatric patients, the factors affecting adherence were the susceptibility, severity, barrier level, and self-efficacy. Among these, self-efficacy was reported to mediate the greatest effect, which is partially in agreement with our study.
- The limitation of our study is that it was conducted in patients from diabetes clinic of a tertiary hospital and from 2 private clinics, and that they may not be representative of the diabetes patient population. Nonetheless, with a multi-institutional study, there are characteristics of the institution and its specialists that must be ruled out as having an effect on the adherence of the patients. In the tertiary hospital cases, the subjects were treated all by one specialist who treats most of the elderly patients at that hospital. In the private clinic cases, it was difficult to recruit a sufficient number of patients from 1 clinic, so we recruited from 2 clinics. Since the study was conducted to assess the factors affecting adherence, it wouldn't cause a problem. Another limitation is that the results are dependent on a questionnaire. Medication adherence assessed by questionnaire is higher than the actual value. Nonetheless, it has been shown that such a questionnaire can reliably identify non-adherence [31], and thus, it is a cost-effective method. Another limitation associated with questionnaire survey is that the number of questions is limited. Because our subjects were elderly, a large number of variables can increase the time it takes to answer the questions, which leads to inaccurate or incomplete responses, thus reducing the reliability of the answers [32]. As the result, we limited the number of questions. Despite the above limitations, our study will provide useful results on the factors affecting medication adherence in geriatric diabetes patients treated at private clinics and tertiary hospitals.
- The above results indicate that different strategies are necessary to increase the medication adherence of geriatric diabetes patients, depending on whether they are patients treated at tertiary hospital or patients treated at private clinics. In tertiary hospital patients cases, the illness duration can be very long and there is a higher possibility of severe complications. In this case, the medication adherence may be increased through health education on diabetes and instruction on the proper method for storing drugs. Also, at the time of prescription or distribution, it is important to assess the self-efficacy, and whether the patient takes drugs properly. The patients with low self-efficacy should be instructed to improve their confidence in taking the medication. In clinic patients, it is necessary to educate patients about complications as well as the seriousness of complications that may develop if diabetes is not treated properly. Further, patients should be assessed for self-efficacy and the patients with low confidence should be educated to improve their confidence.
DISCUSSION
- 1. Korea National Statistical Office: Population projection, 2006 Available from: http://www.kostat.go.kr.
- 2. Lim S, Kim DJ, Jeong IK, Son HS, Chung CH, Koh G, Lee DH, Won KC, Park JH, Park TS, Ahn J, Kim J, Park KG, Ko SH, Ahn YB, Lee I. A nationwide survey about the current status of glycemic control and complications in diabetic patients in 2006: The Committee of the Korean Diabetes Association on the Epidemiology of Diabetes Mellitus. Korean Diabetes J 2009;33:48-57.Article
- 3. Gochman DS. Chapter 6. The history and meaning of patient compliance as an ideology. Handbook of health behavior research, II. Provider determinants. 1997. New York: Plenum Press; p. 109-124.
- 4. McElnay JC, McCalion CR, al-Deagi F, Scott M. Self-reported medication non-compliance in the elderly. Eur J Clin Pharmacol 1997;53:171-178. ArticlePubMedPDF
- 5. Park KS, Kam S, Kim HS, Lee JK, Hwang JB. Therapeutic compliance and its related factors in pediatrics patients. Korean J Pediatr 2008;51:584-596.Article
- 6. Park JH. Antihypertensive drug medication adherence of national health insurance beneficiaries and its affecting factors in Korea [dissertation]. 2006. Seoul: Seoul National University.
- 7. Choi NH, Kim KH, Choi JT, Kim KS. A study of the factors imfluencing the compliance of hypertensive patients to therapy. J Korean Acad Fam Med 1991;12:1-12.
- 8. Joo HG, Choi JS. A study on patient compliance in hypertension and diabetes. J Korean Acad Fam Med 1994;15:446-463.
- 9. Seo SH, Park JY. Status of hypertensive patients' drug-taking in health center and its related factors. Journal J Korean Soc Health Educ Promot 1998;15:23-42.
- 10. Moon JK. Community-based follow up study of compliance and its determinants in hypertension [dissertation]. 1997. Jinju: Gyeongsang National University.
- 11. Lee SW, Kam S, Chun BY, Yeh MH, Kang YS, Kim KY, Lee YS, Park KS, Son JH, Oh HS, Ahn MY, Lim PD. Therapeutic compliance and its related factors of patients with hypertension in rural area. Korean J Prev Med 2000;33:215-225.
- 12. Lee SK. Treatment intention and compliance of newly detected hypertensive patients [dissertation]. 2000. Chuncheon: Hallym University.
- 13. Nam SH, Kam S, Park JY, Chae SC, Bae MS, Shin MC, Yeh MH. Therapeutic compliance and its related factors of lung cancer patients. Korean J Prev Med 2002;35:13-23.
- 14. Choi YS, Sohn UD. Survey on current situations of geriatric patients medication and drug interactions based on prescriptions. J Pharm Soc Korea 2003;47:390-397.
- 15. Yong CS, Kim JA, Choi HG, Yoo BK. Patient counseling of pharmacists to elderly patients. Koreran J Clin Pharm 2004;14:100-105.
- 16. Nam JS, Shin WG, Oh JM. Pattern of medications usage potentially inappropriate medication usage among korean ambulatory elderly patients based on an explicit criterion. Koreran J Clin Pharm 2005;15:149-159.
- 17. Kim KS, Sohn UD, Song HJ. A study of need for medication education and efficient policies for elderly patients in an aging society. J Pharm Soc Korea 2007;51:318-326.
- 18. Lee JS, Lee JE, Jung KY, Ma SH, Kim MY, Yoo SH, Yoon JL. Polypharmcy and inappropriate drug prescription in community dwelling elderly. J Korean Acad Fam Med 2008;29:925-931.
- 19. Kim KC, Kim JT, Kim JS, Cho JS, Shim JY, Lee HR. Medication compliance in the elderly and the factors associated with compliance. J Korean Acad Fam Med 1999;20:1216-1223.
- 20. Kim MO, Kim JH, Kim JE, Park BR, Lee JW, Park HG, Son HJ, Shin KW, Kim DG. Degree of compliance with polypharmacy and its influential factors in rural elderly patients with chronic diseases in South Korea. J Korean Acad Fam Med 2008;29:604-611.
- 21. Counte MA. Interpersonal behavior and health care: behavioral sciences for health care professionals. 1981. Boulder: Westview Press.
- 22. Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q 1984;11:1-47. ArticlePubMedPDF
- 23. Mullen PD, Hersey JC, Iverson DC. Health behavior models compared. Soc Sci Med 1987;24:973-981. ArticlePubMed
- 24. Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 1977;84:191-215. ArticlePubMed
- 25. Kim SW, Kim MY, Yoo TW, Huh BR. Concurrent validity of the Korea version of self-reported questionnaire. J Korean Acad Fam Med 1995;16:172-179.
- 26. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measures of medication adherence. Med Care 1986;24:67-74. PubMed
- 27. Diehl AK, Bauer RL, Sugarek NJ. Correlates of medication compliance in non-insulin-dependent diabetes mellitus. South Med J 1987;80:332-335. ArticlePubMed
- 28. Ahn HJ, Han KA, Koo BK, Kim HJ, Kim HJ, Park KS, Min KW. Analysis of meal habits from the viewpoint of regularity in Korean type 2 diabetes patients. Korean Diabetes J 2008;32:68-76.Article
- 29. Delamater AM. Improving patient adherence. Clin Diabetes 2006;24:71-77.ArticlePDF
- 30. Schatz PE. An evaluation of the components of compliance in patients with diabetes. J Am Assoc 1988;88:708-712.Article
- 31. Eraker SA, Kirscht JP, Becker MH. Understanding and improving patient compliance. Ann Intern Med 1984;100:258-268. ArticlePubMed
- 32. Groves RM. Survey errors and survey costs. 1989. New York: John Wiley and Sons.
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Medication use problems among older adults at a primary care: A narrative of literature review
Christina Christopher, Bhuvan KC, Sunil Shrestha, Ali Qais Blebil, Deepa Alex, Mohamed Izham Mohamed Ibrahim, Norhasimah Ismail
AGING MEDICINE.2022; 5(2): 126. CrossRef - Changes in Treatment Satisfaction Over 3 Years in Patients With Type 2 Diabetes After Initiating Second-line Treatment
Tomoya Mita, Naoto Katakami, Mitsuyoshi Takahara, Masaru Kawashima, Fumitaka Wada, Hiroki Akiyama, Naru Morita, Yoko Kidani, Toshitaka Yajima, Iichiro Shimomura, Hirotaka Watada
The Journal of Clinical Endocrinology & Metabolism.2022; 107(9): 2424. CrossRef - Associated factors with treatment adherence of patients diagnosed with chronic disease: Relationship with health literacy
Sabahat Coskun, Gulcan Bagcivan
Applied Nursing Research.2021; 57: 151368. CrossRef - The relationships among self-efficacy, health literacy, self-care and glycemic control in older people with type 2 diabetes mellitus
Ariyanti Saleh, Wirda Wirda, Andi Masyitha Irwan, Aulia Insani Latif
Working with Older People.2021; 25(2): 164. CrossRef - Tip 2 Diyabetli Bireylerin Hastalık Yönetiminde Karşılaştıkları Engellerin Değerlendirilmesi
Şuheda ÜSTÜNDAĞ, Nuray DAYAPOĞLU
Adnan Menderes Üniversitesi Sağlık Bilimleri Fakültesi Dergisi.2021; 5(3): 514. CrossRef - Influence of Health Literacy on Medication Adherence Among Elderly Females With Type 2 Diabetes in Pakistan
Nadia Hussain, Amira S. A. Said, Zainab Khan
International Quarterly of Community Health Education.2020; 41(1): 35. CrossRef - Elucidating factors associated with non-adherence among Type 1 diabetes patients in primary care setting in Southeastern Brazil
Heverton Alves Peres, Leonardo Régis Leira Pereira, Edson Zangiacomine Martinez, Carlos Manuel Viana, Maria Cristina Foss de Freitas
Primary Care Diabetes.2020; 14(1): 85. CrossRef - Predictors of poor adherence to antidiabetic therapy in patients with type 2 diabetes: a cross-sectional study insight from Ethiopia
Gebre Teklemariam Demoz, Shishay Wahdey, Degena Bahrey, Halefom Kahsay, Gebremariam Woldu, Yirga Legesse Niriayo, Andrew Collier
Diabetology & Metabolic Syndrome.2020;[Epub] CrossRef - Association of medication storage with diabetes control: A cross-sectional study from Saudi Arabia
Ali F. Altebainawi, Mubarak N. Alrashidi, Moaath K. Aljbreen, Muhammad Majid Aziz, Abdullah A. Alhifany, Mohamad Aljofan, Thamir M. Alshammari
Saudi Pharmaceutical Journal.2020; 28(4): 452. CrossRef - Facteurs associés à la non-observance thérapeutique chez les diabétiques de type 2 : première enquête algérienne
M.Y. Achouri, M. Mammeri, Y. Sehanine, M.A. Selka, W.I. Ghomari, A. Lahmer, M. Hadj Habib
Annales Pharmaceutiques Françaises.2019; 77(6): 506. CrossRef - Heart failure is associated with non-adherence to pharmacotherapy in elderly with type 2 diabetes mellitus in public health system Brazilians
Heverton Alves Peres, Leonardo Régis Leira Pereira, Edson Zangiacomini Martinez, Carlos Manuel Viana, Maria Cristina Foss-Freitas
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(2): 939. CrossRef - Medication Adherence and its Predictors in Type 2 Diabetic Patients Referring to Urban Primary Health Care Centers in Kerman City, Southeastern Iran
Lila Benrazavy, Ali Khalooei
Shiraz E-Medical Journal.2019;[Epub] CrossRef - Adherence to Bisphosphonates among People Admitted to an Orthopaedic and Geriatric Ward at a University Hospital in Sweden
Linnea Abramsson, Maria Gustafsson
Pharmacy.2018; 6(1): 20. CrossRef - Evaluation of factors for therapeutic adherence in diabetic patients
G. Belhabib, M. Lahyani, A. Mhiri, O. Gloulou, J. Sahli, N. Chouchane
Le Pharmacien Hospitalier et Clinicien.2018; 53(2): 159. CrossRef - Évaluation des facteurs conditionnant l’observance thérapeutique chez le patient diabétique
G. Belhabib, M. Lahyani, A. Mhiri, O. Gloulou, J. Sahli, N. Chouchane
Le Pharmacien Hospitalier et Clinicien.2018; 53(2): 87. CrossRef - Factors associated with antidiabetic medication non-adherence in patients with incident comorbid depression
Carlotta Lunghi, Arsène Zongo, Jocelyne Moisan, Jean-Pierre Grégoire, Line Guénette
Journal of Diabetes and its Complications.2017; 31(7): 1200. CrossRef - Psychosocial factors associated with adherence to non-insulin antidiabetes treatments
Line Guénette, Marie-Claude Breton, Laurence Guillaumie, Sophie Lauzier, Jean-Pierre Grégoire, Jocelyne Moisan
Journal of Diabetes and its Complications.2016; 30(2): 335. CrossRef - Effects of pharmacist-led patient education on diabetes-related knowledge and medication adherence: A home-based study
Ee Pin Chow, Mohamed Azmi Hassali, Fahad Saleem, Hisham Aljadhey
Health Education Journal.2016; 75(4): 421. CrossRef - Adherence to diabetes medication: a systematic review
I. Krass, P. Schieback, T. Dhippayom
Diabetic Medicine.2015; 32(6): 725. CrossRef - Study on prevalence and factors influencing patient’s adherence to anti-diabetic medications in Urban Pondicherry
P. Stalin, Zile Singh, Anil J. Purty, Yogesh Sharma, Sherin Billy Abraham
International Journal of Diabetes in Developing Countries.2015; 35(S2): 128. CrossRef - Adherence to anti diabetic medication among patients with diabetes in eastern Uganda; a cross sectional study
James Bagonza, Elizeus Rutebemberwa, William Bazeyo
BMC Health Services Research.2015;[Epub] CrossRef - The role of social support on the relationship of depressive symptoms to medication adherence and self‐care activities in adults with type 2 diabetes
Chun‐Ja Kim, Elizabeth A. Schlenk, Dae Jung Kim, Moonsun Kim, Judith A. Erlen, Se‐Eun Kim
Journal of Advanced Nursing.2015; 71(9): 2164. CrossRef - Adesão ao tratamento do diabetes mellitus e variáveis sociodemográficas, clinicas e de controle metabólico
Clarissa Cordeiro Alves Arrelias, Heloisa Turcatto Gimenes Faria, Carla Regina de Souza Teixeira, Manoel Antônio dos Santos, Maria Lucia Zanetti
Acta Paulista de Enfermagem.2015; 28(4): 315. CrossRef - The Effectiveness of Short Term Mobile Phone Text Reminders in Improving Compliance among Hypertensive Patients
Jung Ah Lee, Woo Sang Kim, Moon Jung Bae, Young-Sik Kim, Han Jin Oh, Sang Yeoup Lee, Chul-Min Kim, Dong Hyeok Shin, Seong-Ho Han, Kyung-Hwan Cho
Korean Journal of Health Promotion.2014; 14(1): 1. CrossRef - Role of depressive symptoms and self‐efficacy of medication adherence in Korean patients after successful percutaneous coronary intervention
Youn‐Jung Son, Sun‐Hee Kim, Jin‐Hee Park
International Journal of Nursing Practice.2014; 20(6): 564. CrossRef - Non-adherence and Associated Factors among Type 2 Diabetic Patients at Jimma University Specialized Hospital, Southwest Ethiopia
Gebrehiwot Teklay, Jemal Hussien, Dawit Tesfaye
Journal of Medical Sciences.2013; 13(7): 578. CrossRef - Conocimientos, percepciones y actitudes que intervienen en la adherencia al tratamiento en pacientes ancianos polimedicados desde una perspectiva cualitativa
E. Crespillo-García, F. Rivas-Ruiz, E. Contreras Fernández, P. Castellano Muñoz, G. Suárez Alemán, E. Pérez-Trueba
Revista de Calidad Asistencial.2013; 28(1): 56. CrossRef - Positive Psychological Characteristics in Diabetes: A Review
Christopher M. Celano, Eleanor E. Beale, Shannon V. Moore, Deborah J. Wexler, Jeff C. Huffman
Current Diabetes Reports.2013; 13(6): 917. CrossRef - The Effect of a Clinic Based Incentive Program on Medication Adherence among Patients with Hypertension or Diabetes Mellitus in Incheon
Won Cheong, Jun Yim, Dae-Kyu Oh, Jeong-Soo Im, Kwang Pil Ko, Ie Byung Park
Health Policy and Management.2013; 23(4): 427. CrossRef - Difficulty adhering to antidiabetic treatment: Factors associated with persistence and compliance
L. Guénette, J. Moisan, M.-C. Breton, C. Sirois, J.-P. Grégoire
Diabetes & Metabolism.2013; 39(3): 250. CrossRef - Impact of Cognitive Function and Self-efficacy on Medication Adherence of Elderly Patients with Chronic Disease
Kyung-Hee Ryu, Youn-Jung Son
Journal of Korean Biological Nursing Science.2013; 15(3): 107. CrossRef - Prevalence and correlates of self-reported medication non-adherence among older adults with coronary heart disease, diabetes mellitus, and/or hypertension
Zachary A. Marcum, Yan Zheng, Subashan Perera, Elsa Strotmeyer, Anne B. Newman, Eleanor M. Simonsick, Ronald I. Shorr, Douglas C. Bauer, Julie M. Donohue, Joseph T. Hanlon
Research in Social and Administrative Pharmacy.2013; 9(6): 817. CrossRef - Medication Adherence in Type 2 Diabetes: The ENTRED Study 2007, a French Population-Based Study
Michel Tiv, Jean-François Viel, Frédéric Mauny, Eveline Eschwège, Alain Weill, Cécile Fournier, Anne Fagot-Campagna, Alfred Penfornis, German Malaga
PLoS ONE.2012; 7(3): e32412. CrossRef - Construction of Explanatory Model for Medication Adherence in Older People with Chronic disease
Shin Hong Min, Jong Im Kim
Journal of Korean Academy of Fundamentals of Nursing.2012; 19(4): 463. CrossRef - The Effects of Tele-care Case Management Services for Medical Aid Beneficiaries
Yang Heui Ahn, Eui Sook Kim, Il Sun Ko
Journal of Korean Academy of Community Health Nursing.2010; 21(3): 351. CrossRef
- Figure
- Related articles
-
- Risk Prediction and Management of Chronic Kidney Disease in People Living with Type 2 Diabetes Mellitus
- The Beneficial Effect of Glycemic Control against Adverse Outcomes in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease
- Non-Alcoholic Fatty Liver Disease with Sarcopenia and Carotid Plaque Progression Risk in Patients with Type 2 Diabetes Mellitus
- Intensified Multifactorial Intervention in Patients with Type 2 Diabetes Mellitus
- A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus

 KDA
KDA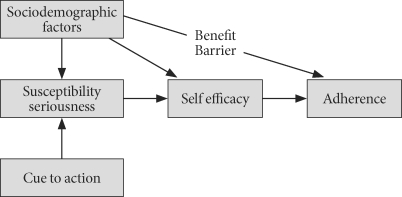


 PubReader
PubReader Cite
Cite




