- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 48(1); 2024 > Article
-
Original ArticleCardiovascular Risk/Epidemiology Psychotic Disorders and the Risk of Type 2 Diabetes Mellitus, Atherosclerotic Cardiovascular Diseases, and All-Cause Mortality: A Population-Based Matched Cohort Study
-
You-Bin Lee1
 , Hyewon Kim2, Jungkuk Lee3, Dongwoo Kang3, Gyuri Kim1, Sang-Man Jin1, Jae Hyeon Kim1, Hong Jin Jeon4
, Hyewon Kim2, Jungkuk Lee3, Dongwoo Kang3, Gyuri Kim1, Sang-Man Jin1, Jae Hyeon Kim1, Hong Jin Jeon4 , Kyu Yeon Hur1
, Kyu Yeon Hur1
-
Diabetes & Metabolism Journal 2024;48(1):122-133.
DOI: https://doi.org/10.4093/dmj.2022.0431
Published online: January 3, 2024
- 1,089 Views
- 144 Download
1Division of Endocrinology and Metabolism, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
2Department of Psychiatry, Hanyang University Hospital, Seoul, Korea
3Data Science Team, Hanmi Pharm. Co., Ltd., Seoul, Korea
4Department of Psychiatry, Depression Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
-
Corresponding authors: Kyu Yeon Hur
 Division of Endocrinology and Metabolism, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnamgu, Seoul 06351, Korea E-mail: ky.hur@samsung.com
Division of Endocrinology and Metabolism, Department of Internal Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnamgu, Seoul 06351, Korea E-mail: ky.hur@samsung.com - Hong Jin Jeon https://orcid.org/0000-0002-6126-542X Department of Psychiatry, Depression Center, Samsung Medical Center, Sungkyunkwan University School of Medicine, 81 Irwon-ro, Gangnam-gu, Seoul 06351, Korea E-mail: jeonhj@skku.edu
Copyright © 2024 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- The effects of psychotic disorders on cardiometabolic diseases and premature death need to be determined in Asian populations.
-
Methods
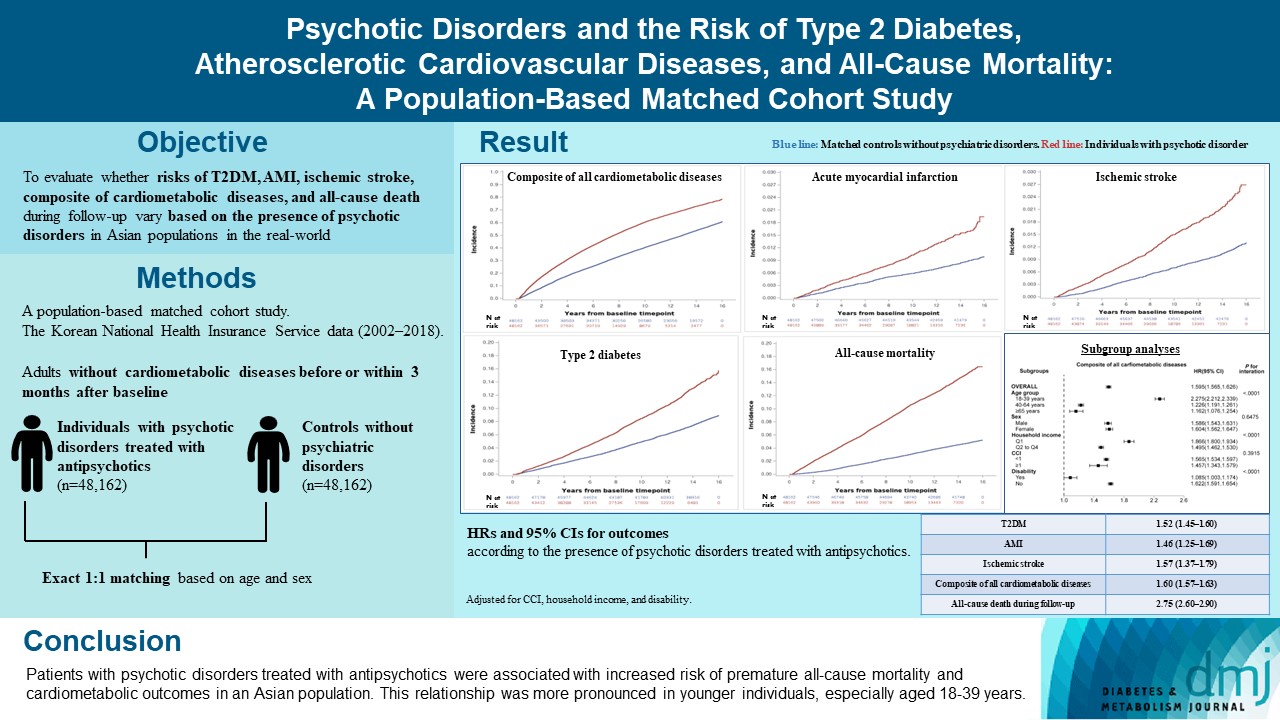
- In this population-based matched cohort study, the Korean National Health Insurance Service database (2002 to 2018) was used. The risk of type 2 diabetes mellitus (T2DM), acute myocardial infarction (AMI), ischemic stroke, composite of all cardiometabolic diseases, and all-cause death during follow-up was compared between individuals with psychotic disorders treated with antipsychotics (n=48,162) and 1:1 matched controls without psychiatric disorders among adults without cardiometabolic diseases before or within 3 months after baseline.
-
Results
- In this cohort, 53,683 composite cases of all cardiometabolic diseases (during median 7.38 years), 899 AMI, and 1,216 ischemic stroke cases (during median 14.14 years), 7,686 T2DM cases (during median 13.26 years), and 7,092 deaths (during median 14.23 years) occurred. The risk of all outcomes was higher in subjects with psychotic disorders than matched controls (adjusted hazard ratios [95% confidence intervals]: 1.522 [1.446 to 1.602] for T2DM; 1.455 [1.251 to 1.693] for AMI; 1.568 [1.373 to 1.790] for ischemic stroke; 1.595 [1.565 to 1.626] for composite of all cardiometabolic diseases; and 2.747 [2.599 to 2.904] for all-cause mortality) during follow-up. Similar patterns of associations were maintained in subgroup analyses but more prominent in younger individuals (P for interaction <0.0001) when categorized as those aged 18–39, 40–64, or ≥65 years.
-
Conclusion
- Patients with psychotic disorders treated with antipsychotics were associated with increased risk of premature allcause mortality and cardiometabolic outcomes in an Asian population. This relationship was more pronounced in younger individuals, especially aged 18 to 39 years.
- In the last decades, the relationship between severe mental illness (SMI), including schizophrenia, bipolar disorder, and major depressive disorder, and atherosclerotic cardiovascular disease (ASCVD) has received attention [1]. The American Heart Association recognized major depressive disorder and bipolar disorder among youth as moderate-risk conditions associated with accelerated atherosclerosis and early ASCVD in a scientific statement [2]. However, relatively less attention has been given to the importance of psychotic disorders, including schizophrenia and schizoaffective, schizotypal, and delusional disorders, as risk factors for cardiovascular or metabolic morbidity and mortality. Furthermore, in Asian populations, research regarding the effects of psychotic disorders on the risk of cardiometabolic outcomes or premature mortality has been limited, and it has been even more limited in Korean populations. Although a shorter life expectancy and higher all-cause or cardiovascular mortality has been reported in patients with SMI, including psychotic disorders, than in the general population [3-5], and psychotic disorders were reportedly associated with diabetes and cardiovascular morbidity [6,7], most results were based on analyses from Western populations. Thus, whether this is applicable to Asian populations, especially to Koreans, remains to be determined.
- Therefore, to evaluate whether risk profiles of metabolic disease, ASCVDs, and premature all-cause mortality also vary based on the presence of psychotic disorders in Asian populations in the real-world, the risk of type 2 diabetes mellitus (T2DM), acute myocardial infarction (AMI), ischemic stroke, composite of cardiometabolic diseases, and all-cause death during follow-up were compared between subjects with psychotic disorders treated with antipsychotics and age- and sexmatched controls without psychiatric disorders using a population-based nationwide study cohort in Korea.
INTRODUCTION
- Data sources
- For this population-based matched cohort study, the Korean National Health Insurance Service (KNHIS) database from January 2002 to December 2018 was analyzed. The Korean government operates the single nationwide insurer, KNHIS, and all Korean residents are covered by this system [8,9]. The KNHIS constructed an anonymized public database, the KNHIS database, which contains information on demographics, date of death for the deceased, household income state, disability, primary and all secondary diagnoses summarized according to the International Classification of Diseases-10th Revision (ICD-10), prescriptions, medical or surgical procedures, and dates of hospitalization or hospital visits for the entire population in Korea [8].
- The Institutional Review Board of Samsung Medical Center approved this study (SMC 2019-09-030) and granted informed consent exemption because only anonymous data were provided to the researchers from the KNHIS.
- Patient selection and 1:1 exact matching
- A representative sample cohort of patients with psychotic disorders was constructed using the KNHIS database. From all individuals who had been first diagnosed with a psychotic disorder (schizophrenia, schizoaffective disorder, schizotypal disorder, and/or delusional disorder, ICD-10 codes F20–29) between 2003 and 2017, a representative sample cohort comprised of 20% of the total was randomly selected using systematic stratified random sampling with proportional allocation within each stratum. The strata were established based on sex, age, residential region, and household income level. In this sample population with claims for psychotic disorder, 112,491 individuals who were prescribed antipsychotics between 2003 and 2017 were selected. The incidence date of psychotic disorder was determined as the date when the antipsychotics were prescribed for the first time in individuals with psychotic disorder. For comparison, a representative 20% sample cohort was constructed of healthy controls (n=405,111) who had never been diagnosed for major psychiatric disorders (depression, bipolar disorder, and/or psychotic disorder) between 2002 and 2018 after systematic stratified random sampling based on sex, age, residential region, and household income level. The index date (baseline) was defined as the incidence date of psychotic disorder for individuals with psychotic disorders, and as January 1, 2003 for those without major psychiatric disorders. Among the sample population with psychotic disorders treated with antipsychotics and subjects without any major psychiatric disorder, individuals with missing data in at least one variable, those who died within 90 days after baseline, those who had, before or within 3 months after baseline, claims with codes for diabetes (E10–14), obesity (E66), dyslipidemia (E78), hypertension (I10–15), atherosclerosis (I70), aortic aneurysm and dissection (I71–72), arterial embolism and thrombosis (I74), heart failure (I50), ischemic heart disease (I20–25), or cerebrovascular disease (I61–69), subjects who underwent coronary artery bypass graft operation, percutaneous transluminal coronary angioplasty, percutaneous coronary intervention, or thrombolytic treatment before or within 3 months after baseline, those who had claims for transient ischemic attack (G45) during admission before or within 3 months after baseline, and individuals aged <18 years at baseline were excluded (Supplementary Fig. 1). Finally, 357,382 adults without any metabolic or cardiovascular disease were selected; 48,250 were individuals with psychotic disorders treated with antipsychotics and the remaining 309,132 had never been diagnosed with major psychiatric disorders. Exact 1:1 matching based on age and sex was applied for individuals with psychotic disorders and those without major psychiatric disorders. Finally, 48,162 individuals with psychotic disorders and 48,162 matched control participants without major psychiatric disorders were selected for analysis (Supplementary Fig. 1).
- Included antipsychoticsg
- To define individuals with a psychotic disorder treated with antipsychotics, prescription data for antipsychotics available in Korea were examined. The antipsychotics included amisulpride, aripiprazole, blonanserin, chlorpromazine, clozapine, haloperidol, olanzapine, paliperidone, pimozide, quetiapine, risperidone, sulpiride, and ziprasidone. Among them, chlorpromazine, clozapine, and olanzapine were classified as antipsychotics with substantial weight gain liability [10]. Quetiapine, risperidone, and paliperidone (an active metabolite drug of risperidone) in addition to aforementioned three agents with substantial weight gain liability were considered as antipsychotics with any weight gain liability [10].
- Outcomes and follow-up
- The outcomes of interest were incident T2DM, AMI, ischemic stroke, composite of all cardiometabolic diseases, and all-cause death during follow-up. All-cause mortality included deaths from physical diseases as well as from suicide or accident. T2DM was defined as one or more claims per year for the prescription of anti-diabetes medication with ICD-10 codes E11–14 [11-13] and AMI was defined as at least one claim with ICD-10 codes I21–22 during hospitalization or two or more claims with these codes [13-15]. Ischemic stroke was defined as recorded ICD-10 code I63 during hospitalization with claims for brain magnetic resonance imaging or computed tomography [14,15]. All cardiometabolic diseases included T2DM, obesity, dyslipidemia, hypertension, ischemic heart disease, cerebrovascular disease, atherosclerosis, aortic aneurysm and dissection, arterial embolism and thrombosis, and hospitalization for heart failure. Definitions of each component of cardiometabolic diseases are summarized in Supplementary Table 1. The study population was followed up from baseline until the date of death, development of outcomes, or December 31, 2018, whichever came first.
- Measurements and definitions
- The Charlson comorbidity index (CCI) was calculated according to the established method [16] using the diagnostic codes summarized in a previous report [17]. In Korea, according to the Korean Disability Act, persons with physical, mental, or intellectual disabilities diagnosed by the respective medical specialists are registered in a National Disability Registry System [18]. Presence of disability at baseline was verified using anonymized records in this registry system. Among individuals with psychotic disorders, use of other psychiatric medications (mood stabilizers, benzodiazepines, stimulants, antidepressant, and zolpidem) within 3 months after baseline and history of admission to psychiatry from baseline to the end of the follow-up were examined.
- Statistical analysis
- SAS Enterprise Guide version 7.1 (SAS Institute, Cary, NC, USA) was used for statistical analyses. Two-sided P-values <0.05 were considered statistically significant. Continuous variables are presented as mean±standard deviation and categorical variables as numbers (percentages). The incidence rates of outcomes were derived as number of incident cases divided by total follow-up duration (person-years). The cumulative incidence rates of outcomes were compared between individuals with psychotic disorders and age- and sex-matched controls without major psychiatric disorders using Kaplan–Meier curves; the difference between groups was evaluated using a log-rank test. The hazard ratios (HRs) and 95% confidence intervals (CIs) for outcomes were compared using multivariable Cox regression analysis for individuals with psychotic disorders and age and sex-matched controls. Model 1 was unadjusted and model 2 adjusted for CCI. Model 3 was adjusted for CCI, household income, and disability.
- The HRs (95% CIs) for outcome incidence were compared between subjects with psychotic disorders and age- and sex-matched controls without major psychiatric disorders (reference) in subgroups. The subgroups were categorized based on age (18–39, 40–64, or ≥65 years), sex, household income quartile (lowest quartile [Q1] vs. Q2–Q4), CCI (<1 vs. ≥1), and presence of disability. The P value for interaction was derived after evaluating the potential effect modification by factors determining the subgroups.
- Sensitivity analyses
- To account for competing risk by all-cause death, a cumulative incidence function for T2DM, AMI, ischemic stroke, and composite of all cardiometabolic diseases was plotted, and the subdistribution HRs based on the Fine and Gray method [19] for the four outcomes were estimated after adjusting for the same potential confounders used in the main analyses. Furthermore, we divided individuals with psychotic disorders according to whether they were constantly treated with antipsychotics or not, and estimated the HRs for outcome incidence in these subpopulations with psychotic disorders compared with controls without major psychiatric disorders. Constant antipsychotics therapy was defined as a total of ≥three prescriptions of antipsychotics and at least one prescription of antipsychotics between 365 and 730 days after the first prescription of antipsychotics. We also conducted sensitivity analyses excluding individuals who had ever treated with antipsychotics with substantial weight gain liability or any weight gain liability. During the latter two sensitivity analyses, models were adjusted for age and sex in addition to the potential confounders used in the main analyses.
METHODS
- Baseline characteristics of the study population
- After 1:1 exact matching based on age and sex, a total of 48,162 individuals with psychotic disorders (cases) and 48,162 matched controls without major psychiatric disorders were included (Supplementary Fig. 1).
- The baseline characteristics of the two groups are presented in Table 1. The mean age was 38.24 years and 49.06% of individuals were males in both groups. Subjects with psychotic disorders were more likely to be in the lowest household income quartile and have a disability. Among individuals with psychotic disorder treated with antipsychotics, use of mood stabilizers, benzodiazepines, stimulants, antidepressant, and zolpidem were identified in 14.05%, 72.80%, 3.68%, 30.12%, and 17.79%, respectively. At least one hospitalization to the psychiatry department was found in 22.67% of individuals with psychotic disorder treated with antipsychotics during the entire follow-up period.
- Psychotic disorders and hazard of outcomesn
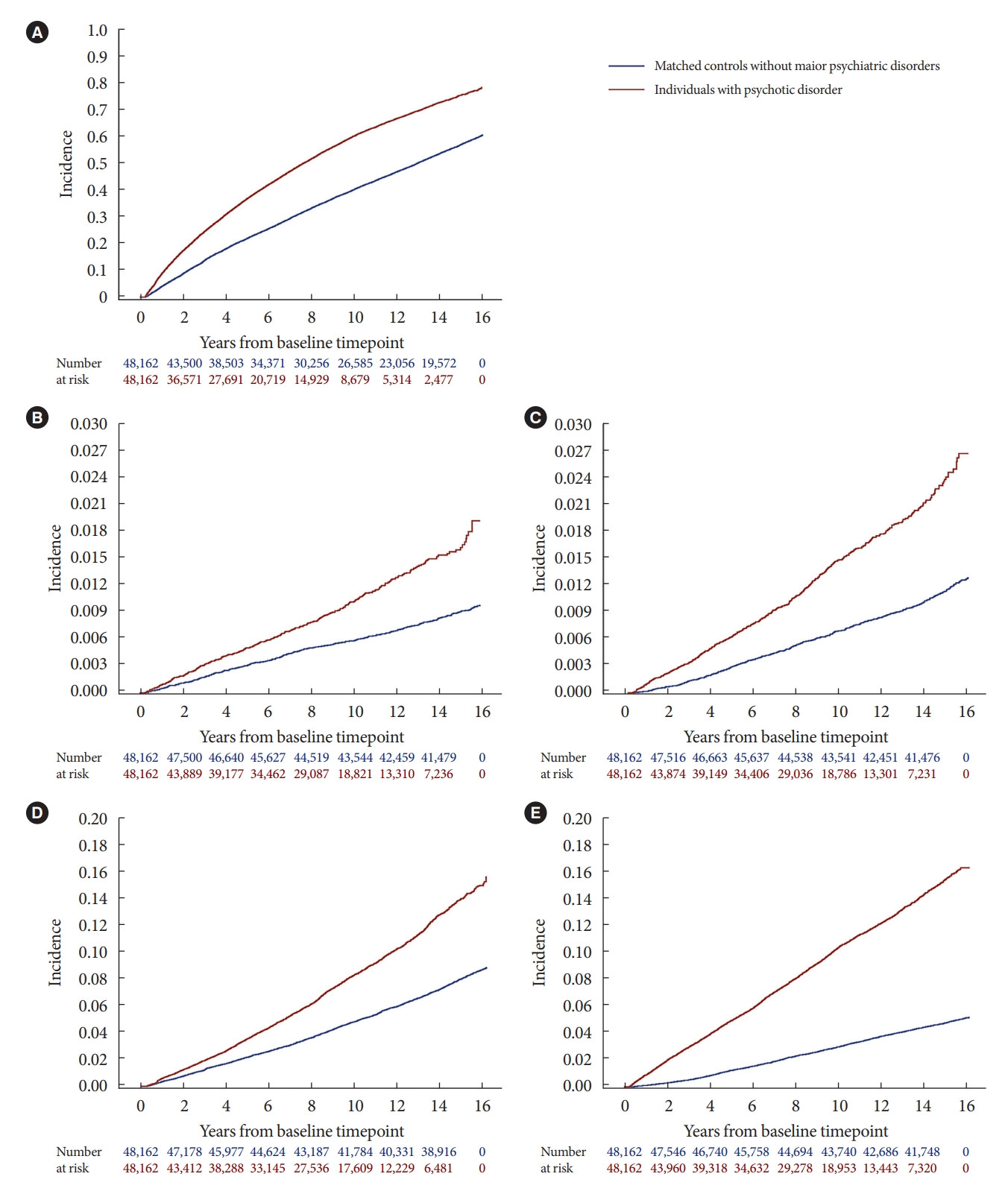
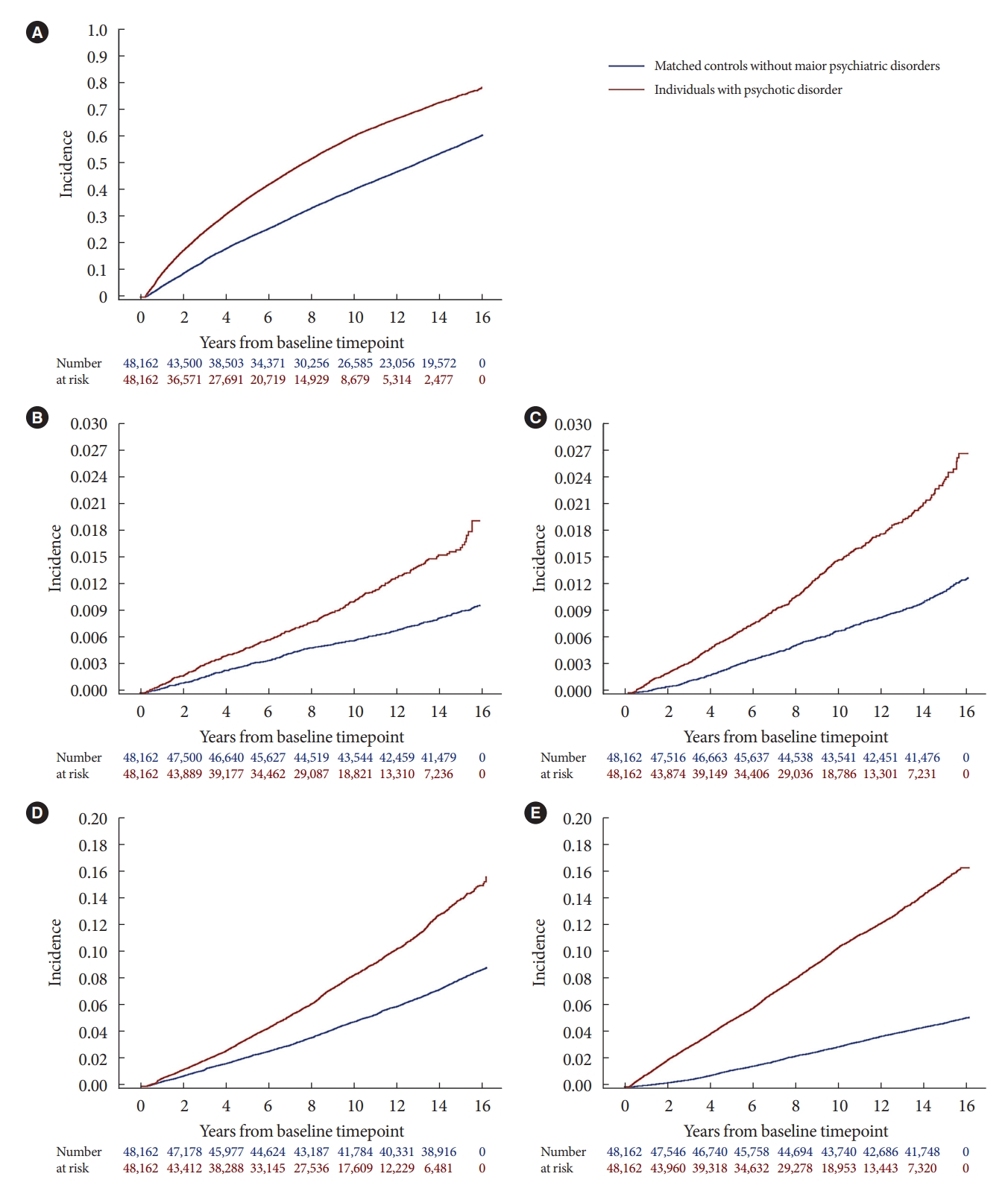
- In the study cohort, 7,686 cases of T2DM were diagnosed during a median 13.26 years (1,102,508.3 person-years) and 899 AMI cases occurred after a median 14.14 years (1,140,531.5 person-years) (Table 2). During a median 14.14 years (1,140,161.0 person-years), 1,216 ischemic stroke cases occurred. After a median 7.38 years (779,755.6 person-years), 53,683 composite cases of all cardiometabolic diseases were detected. A total of 7,092 deaths occurred during a median 14.23 years (1,145,061.4 person-years). The cumulative incidence of all five outcomes was higher in individuals with psychotic disorders than in matched controls without major psychiatric disorders (Fig. 1) The hazards of all outcomes were significantly higher in subjects with psychotic disorders treated with antipsychotics compared with matched controls without major psychiatric disorders (adjusted HR [95% CI]: 1.522 [1.446 to 1.602] for T2DM; 1.455 [1.251 to 1.693] for AMI; 1.568 [1.373 to 1.790] for ischemic stroke; 1.595 [1.565 to 1.626] for composite of all cardiometabolic diseases; and 2.747 [2.599 to 2.904] for all-cause mortality during follow-up) (Table 2).
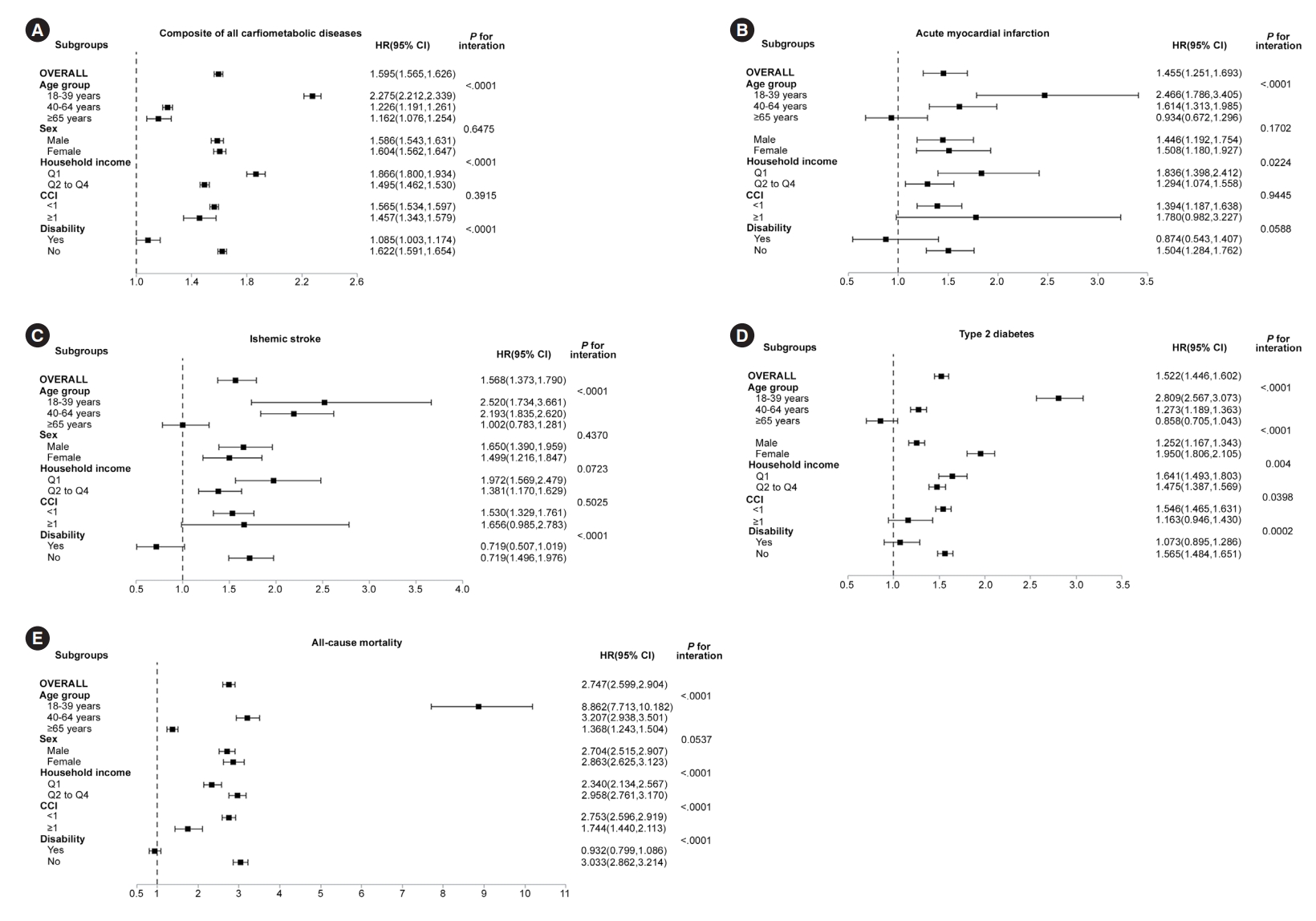
- Subgroup analyses
- The HRs (95% CIs) of outcomes in individuals with psychotic disorders treated with antipsychotics compared with matched controls were estimated in subgroups categorized based on age, sex, household income quartile, CCI, and presence of disability (Fig. 2). Subjects with psychotic disorders treated with antipsychotics exhibited higher hazard of outcomes compared with their matched controls in all subgroups except individuals ≥65 years of age and subjects with CCI ≥1 (for outcomes of T2DM, AMI, and ischemic stroke), as well as individuals with disability (for outcomes of T2DM, AMI, ischemic stroke, and all-cause death).
- The HRs of T2DM, AMI, and ischemic stroke in the psychotic disorder group showed a non-significant increase compared with the control group also in subjects with CCI ≥1. The association between psychotic disorders and hazards of all five outcomes was more prominent in younger individuals and attenuated in the elderly (P for interaction <0.0001). Furthermore, association between psychotic disorders and hazards of other four outcomes except for AMI were more pronounced in subjects without disability and attenuated in disabled individuals (P for interaction ≤0.0002). Although statistical significance was not observed, with respect to the outcome of AMI, the HR tended to be numerically higher in individuals without disability than in subjects with disability (P for interaction= 0.0588). Regarding outcomes of T2DM, AMI, and composite of all cardiometabolic diseases, the association between psychotic disorders and outcomes was more pronounced in subjects with the lowest household income quartile. Furthermore, association between psychotic disorders and the outcomes of T2DM and all-cause death was more prominent in subjects with CCI <1.
- Sensitivity analyses
- When all-cause deaths were considered as competing events, the corresponding cumulative incidence function and subdistribution HRs for T2DM, AMI, ischemic stroke, and composite of all cardiometabolic diseases did not differ from the main findings (Supplementary Table 2, Supplementary Fig. 2).
- Compared to controls without major psychiatric disorders, those with psychotic disorders constantly treated with antipsychotics exhibited higher hazards of all five outcomes while those with psychotic disorders without constant antipsychotics therapy showed significantly higher hazards of ischemic stroke, composite of all cardiometabolic diseases, and all-cause death during follow-up (Supplementary Table 3). In those with psychotic disorders without constant antipsychotics therapy, although hazards of T2DM and AMI were not significantly higher than in controls in model 3, the HR (95% CI) of allcause death during follow-up compared with controls was 5.019 (4.694 to 5.366) whereas that in individuals with psychotic disorders constantly treated with antipsychotics was 2.070 (1.947 to 2.201).
- Additional sensitivity analyses excluding patients who had ever treated with antipsychotics with substantial weight gain liability demonstrated findings consistent to the main analyses (Supplementary Table 4). When patients who had ever treated with antipsychotics with any weight gain liability were excluded, attenuations in HRs were observed throughout all five outcomes (Supplementary Table 5). Nevertheless, people with psychotic disorders exhibited significantly higher hazards of composite of all cardiometabolic diseases and all-cause death during follow-up even in this sensitivity analysis.
RESULTS
- In this large population-based nationwide cohort study including 48,162 adults with psychotic disorders treated with antipsychotics and 1:1 age- and sex-matched healthy controls without psychiatric disorders, presence of psychotic disorders was associated with increased risk of incident T2DM, AMI, ischemic stroke, composite of all cardiometabolic diseases, and all-cause death during the follow-up, although only low-risk individuals without baseline hypertension, dyslipidemia, or any other metabolic or cardiovascular diseases were included. Regarding the outcomes of T2DM, AMI, ischemic stroke, and composite of all cardiometabolic diseases, subdistribution HRs accounting for all-cause death as a competing event also showed consistent results. Similar patterns of associations were maintained in subgroup analyses stratified based on age, sex, household income quartile, and CCI and the association was more pronounced in younger individuals and subjects without disability.
- The results of the present study indicated that psychotic disorders requiring antipsychotic treatment may be associated with higher risk of metabolic and cardiovascular outcomes and premature mortality also in Asian populations. The excess risk of cardiometabolic outcomes and premature all-cause death in subjects with psychotic disorder may be affected by multiple complex factors [3,6]. Antipsychotics may be associated with increased risk of weight gain and metabolic disorders including dyslipidemia and hyperglycemia whereas they mitigate symptom levels of mental illness and might improve lifestyle factors and help-seeking behaviors [3].
- In our sensitivity analyses, although significantly higher hazards compared to controls were more consistently observed throughout all five outcomes in people with psychotic disorders constantly treated with antipsychotics, the excess risk of all-cause mortality during follow-up compared to controls was more prominent in those with psychotic disorders without constant antipsychotics therapy (HR, 5.019) rather than those with constant antipsychotics therapy (HR, 2.070). Similarly, in a recent population-based cohort study, patients with schizophrenia treated with antipsychotics exhibited lower rates of death from ischemic heart disease and stroke than untreated patients [20].
- Furthermore, consistent findings after excluding patients ever treated with antipsychotics with substantial weight gain liability, and higher hazards of composite of all cardiometabolic diseases and all-cause death during follow-up even after excluding patients ever treated with antipsychotics with any weight gain liability in our study indicate the potential association of psychotic disorder itself with increased risks of cardiometabolic disease and early mortality. Accumulating evidence indicates that increased risk of cardiometabolic outcomes is related not only to antipsychotic medications but even more to the overall consequences of psychotic disorder [3].
- Presence of a psychotic disorder may result in unfavorable lifestyles, poor adherence, and subsequently higher rates of cardiovascular risk factors. In individuals with psychotic disorders, lack of awareness to their illness including physical diseases, difficulties in seeking adequate physical care and following health care advice, and poor compliance with treatment may act as barriers to the recognition and adequate care for physical health [21]. In addition, psychotic disorders are frequently associated with low socioeconomic status, social deprivation, and linked to negative attitudes towards these patients when seeking help for physical diseases including cardiometabolic disorders [3].
- Furthermore, predisposition to cardiometabolic diseases due to genetic loading has been proposed as a possible explanation. When polygenic risk scores were used to explore the shared genetic basis of metabolic and cardiovascular influences of schizophrenia, it was suggested that individuals with schizophrenia might be genetically predisposed to cardiovascular and metabolic adverse outcomes [22,23].
- The higher mortality in patients with psychotic disorders treated with antipsychotics compared with controls without psychiatric diseases in the current study may have originated not only from unnatural deaths such as suicide but also from natural deaths including cardiovascular mortality. The rate of unnatural death including suicide has been reported to be higher in patients with psychotic disorders than in the general population [24]. However, the primary cause of death in patients with psychotic disorders is considered a physical condition, representing approximately 70% of all mortality according to a systematic review and meta-analysis although most of the included studies were from Western populations [25]. Similarly, in previous studies in Europe, approximately 25% of patients with schizophrenia die from cardiovascular disease [26] and predominant causes of higher mortality in individuals with schizophrenia were natural causes including cardiovascular disease, prevailing over external causes [27].
- The excess risk of outcomes from psychotic disorders treated with antipsychotics was more prominent in younger individuals and subjects without disability, indicating the effects of psychotic disorders treated with antipsychotics in terms of the risk of metabolic and ASCVDs and premature all-cause mortality may be more pronounced among these subgroups. Although the exact mechanisms could not be clarified in the current study, several explanations are possible. First, regarding the interaction by age, chronologically earlier incipiency of risk factors and physical disease due to accelerated aging [3,28] and genetic predisposition to cardiometabolic adverse outcomes in people with psychotic disorders [22,23] may have contributed. Regarding the increased risk of premature mortality and ASCVD in patients with SMI including psychotic disorders, an older biological age owing to accelerated aging in patients with SMI has been suggested a possibility [3,28], and might have affected the younger individuals more prominently. Furthermore, influence of genetic predisposition might have been more pronounced in younger subjects. Second, regarding the interaction by the presence of disability, social deprivation and disparities in accessing health care, associated with the presence of disability itself, might have reduced the additional effect of psychotic disorders.
- The strength of this study included the use of a large, representative nationwide cohort database managed by the Korean government, 1:1 exact matching for age and sex, and consistent results from various subgroup and sensitivity analyses.
- The study limitations should be acknowledged. First, as an observational study, clarification of causal relationships is inevitably limited. However, to minimize the possibility of reverse causality effect and establish a temporal relationship between exposure and outcomes, individuals with any metabolic or cardiovascular diseases before or within 3 months after baseline were excluded. Second, the possibility of residual confounding may remain despite exact 1:1 matching between groups for age and sex, adjustments for measured potential confounders, and various subgroup analyses. Third, regarding the excess risk of outcomes in people with psychotic disorders treated with antipsychotics, the effect of antipsychotics apart from the psychotic disorder itself cannot be completely discriminated.
- However, considering sensitivity analysis results categorizing individuals with psychotic disorders according to the constant antipsychotics therapy, and excluding patients ever treated with antipsychotics with substantial or any weight gain liability, both antipsychotic medications and psychotic disorder itself may have contributed. Fourth, the specific cause of mortality could not be determined with the KNHIS database used in this study. Lastly, the study population was restricted to Korean adults with low cardiometabolic risk. Therefore, caution should be taken in extrapolating the findings to other populations such as different ethnicities or subjects with multiple cardiometabolic risk factors including baseline hypertension or dyslipidemia.
- In the present large real-world nationwide population-based study with 1:1 exact matching for age and sex, psychotic disorders treated with antipsychotics were associated with an increased risk of premature all-cause mortality and metabolic and ASCVDs including T2DM, AMI, and ischemic stroke. Particularly, this association was more prominent in younger individuals.
- These findings advance the argument that monitoring and screening for early detection of cardiometabolic deterioration and strategies to prevent cardiometabolic disease and premature mortality, including patient education and cardio-protective interventions, should be offered widely and intensively to individuals with psychotic disorders treated with antipsychotics, even from a young age. Multifaceted and collaborative approaches incorporating psychiatric and somatic health care are necessary to optimize outcomes in patients with psychotic disorders requiring antipsychotic treatment.
DISCUSSION
SUPPLEMENTARY MATERIALS
Supplementary Table 1.
Supplementary Table 2.
Supplementary Table 3.
Supplementary Table 4.
Supplementary Table 5.
Supplementary Fig. 2.
-
CONFLICTS OF INTEREST
Sang-Man Jin has been associate editor of the Diabetes & Metabolism Journal since 2022. He was not involved in the review process of this article. Otherwise, there was no conflict of interest.
Two of the authors in this study are affiliated with the Data Science Team at Hanmi Pharm. Co., Ltd., Seoul, Korea, which is a for-profit organization. We hereby declare that there are no potential conflicts of interest arising from this affiliation in relation to the research, methodology, results, and conclusions presented in this article. The authors from Hanmi Pharm. Co., Ltd. have participated in this study solely in the capacity of independent researchers, and their involvement has not been influenced by any financial or proprietary interests of the company.
-
AUTHOR CONTRIBUTIONS
Conception or design: Y.B.L., H.K., H.J.J., K.Y.H.
Acquisition, analysis, or interpretation of data: all authors.
Drafting the work or revising: Y.B.L.
Final approval of the manuscript: all authors.
-
FUNDING
This study was supported by a grant of the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (HR21C0885). This study was also supported by the Samsung Medical Center Grant (SMX123-0041). The funding sources had no role in the design or conduct of the study; collection, management, analysis, or interpretation of the data; preparation, review, or approval of the manuscript; or the decision to submit the manuscript for publication.
NOTES
-
Acknowledgements
- This work was performed using the database from the Korean National Health Insurance Service (KNHIS).
- The National Health Information Database constructed by the KNHIS was used and the results do not necessarily represent the opinion of the KNHIS.
| Characteristic | Individuals with psychotic disorders treated with antipsychotics | Matcheda controls without major psychiatric disorders | P value |
|---|---|---|---|
| Number | 48,162 | 48,162 | |
| Male sex | 23,630 (49.06) | 23,630 (49.06) | 1.0000 |
| Age, yr | 38.24±13.94 | 38.24±13.94 | 1.0000 |
| Age group, yr | 1.0000 | ||
| 18–39 | 27,256 (56.59) | 27,256 (56.59) | |
| 40–64 | 18,698 (38.82) | 18,698 (38.82) | |
| ≥65 | 2,208 (4.58) | 2,208 (4.58) | |
| Household income quartile | <0.0001 | ||
| Q1 | 20,088 (41.71) | 12,188 (25.31) | |
| Q2 | 9,047 (18.78) | 11,105 (23.06) | |
| Q3 | 8,730 (18.13) | 12,083 (25.09) | |
| Q4 | 10,297 (21.38) | 12,786 (26.55) | |
| CCI | 0.26±0.70 | 0.03±0.21 | <0.0001 |
| CCI categories | <0.0001 | ||
| 0 | 39,184 (81.36) | 47,048 (97.69) | |
| 1 | 6,684 (13.88) | 981 (2.04) | |
| 2 | 1,578 (3.28) | 95 (0.20) | |
| ≥3 | 716 (1.49) | 38 (0.08) | |
| Disability | 10,431 (21.66) | 1,041 (2.16) | <0.0001 |
| Presence of psychotic disorder | No. of subjects | No. of events | Follow-up duration, person-yr | Incidence rate, /1,000 person-yr |
HR (95% CI) |
||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |||||
| Composite of all cardiometabolic disease | |||||||
| Matcheda controls without major psychiatric disorders | 48,162 | 27,698 | 497,846.7 | 55.63560 | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Individuals with psychotic disorders treated with antipsychotics | 48,162 | 25,985 | 281,908.9 | 92.17517 | 1.765 (1.734–1.796) | 1.686 (1.656–1.717) | 1.595 (1.565–1.626) |
| P value | <0.0001 | <0.0001 | <0.0001 | ||||
| Acute myocardial infarction | |||||||
| Matcheda controls without major psychiatric disorders | 48,162 | 444 | 714,608.4 | 0.62132 | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Individuals with psychotic disorders treated with antipsychotics | 48,162 | 455 | 425,923.1 | 1.06827 | 1.820 (1.587–2.088) | 1.721 (1.496–1.980) | 1.455 (1.251–1.693) |
| P value | <0.0001 | <0.0001 | <0.0001 | ||||
| Ischemic stroke | |||||||
| Matcheda controls without major psychiatric disorders | 48,162 | 575 | 714,684.5 | 0.80455 | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Individuals with psychotic disorders treated with antipsychotics | 48,162 | 641 | 425,476.5 | 1.50655 | 2.119 (1.881–2.386) | 1.973 (1.747–2.227) | 1.568 (1.373–1.790) |
| P value | <0.0001 | <0.0001 | <0.0001 | ||||
| Type 2 diabetes mellitus | |||||||
| Matcheda controls without major psychiatric disorders | 48,162 | 3,979 | 691,919.9 | 5.75067 | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Individuals with psychotic disorders treated with antipsychotics | 48,162 | 3,707 | 410,588.4 | 9.02851 | 1.773 (1.692–1.859) | 1.703 (1.623–1.786) | 1.522 (1.446–1.602) |
| P value | <0.0001 | <0.0001 | <0.0001 | ||||
| All-cause mortality | |||||||
| Matcheda controls without major psychiatric disorders | 48,162 | 2,387 | 717,217.0 | 3.32814 | 1 (Ref) | 1 (Ref) | 1 (Ref) |
| Individuals with psychotic disorders treated with antipsychotics | 48,162 | 4,705 | 427,844.4 | 10.99699 | 3.471 (3.297–3.655) | 3.240 (3.075–3.414) | 2.747 (2.599–2.904) |
| P value | <0.0001 | <0.0001 | <0.0001 | ||||
- 1. Newcomer JW, Hennekens CH. Severe mental illness and risk of cardiovascular disease. JAMA 2007;298:1794-6.ArticlePubMed
- 2. Goldstein BI, Carnethon MR, Matthews KA, McIntyre RS, Miller GE, Raghuveer G, et al. Major depressive disorder and bipolar disorder predispose youth to accelerated atherosclerosis and early cardiovascular disease: a scientific statement from the American Heart Association. Circulation 2015;132:965-86.ArticlePubMed
- 3. Nielsen RE, Banner J, Jensen SE. Cardiovascular disease in patients with severe mental illness. Nat Rev Cardiol 2021;18:136-45.ArticlePubMedPDF
- 4. Kugathasan P, Stubbs B, Aagaard J, Jensen SE, Munk Laursen T, Nielsen RE. Increased mortality from somatic multimorbidity in patients with schizophrenia: a Danish nationwide cohort study. Acta Psychiatr Scand 2019;140:340-8.ArticlePubMedPDF
- 5. Ringen PA, Engh JA, Birkenaes AB, Dieset I, Andreassen OA. Increased mortality in schizophrenia due to cardiovascular disease: a non-systematic review of epidemiology, possible causes, and interventions. Front Psychiatry 2014;5:137.ArticlePubMedPMC
- 6. Ward M, Druss B. The epidemiology of diabetes in psychotic disorders. Lancet Psychiatry 2015;2:431-51.ArticlePubMed
- 7. Curkendall SM, Mo J, Glasser DB, Rose Stang M, Jones JK. Cardiovascular disease in patients with schizophrenia in Saskatchewan, Canada. J Clin Psychiatry 2004;65:715-20.ArticlePubMed
- 8. Seong SC, Kim YY, Khang YH, Park JH, Kang HJ, Lee H, et al. Data resource profile: the National Health Information Database of the National Health Insurance Service in South Korea. Int J Epidemiol 2017;46:799-800.PubMed
- 9. Lee YH, Han K, Ko SH, Ko KS, Lee KU; Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Data analytic process of a nationwide population-based study using National Health Information Database established by National Health Insurance Service. Diabetes Metab J 2016;40:79-82.ArticlePubMedPMCPDF
- 10. De Hert M, Correll CU, Bobes J, Cetkovich-Bakmas M, Cohen D, Asai I, et al. Physical illness in patients with severe mental disorders. I. Prevalence, impact of medications and disparities in health care. World Psychiatry 2011;10:52-77.ArticlePubMedPMC
- 11. Noh J, Han KD, Ko SH, Ko KS, Park CY. Trends in the pervasiveness of type 2 diabetes, impaired fasting glucose and comorbidities during an 8-year-follow-up of nationwide Korean population. Sci Rep 2017;7:46656.ArticlePubMedPMCPDF
- 12. Lee YB, Kim DH, Kim SM, Kim NH, Choi KM, Baik SH, et al. Risk of type 2 diabetes according to the cumulative exposure to metabolic syndrome or obesity: a nationwide populationbased study. J Diabetes Investig 2020;11:1583-93.ArticlePubMedPMCPDF
- 13. Lee YB, Han K, Kim B, Lee SE, Jun JE, Ahn J, et al. Risk of early mortality and cardiovascular disease in type 1 diabetes: a comparison with type 2 diabetes, a nationwide study. Cardiovasc Diabetol 2019;18:157.ArticlePubMedPMCPDF
- 14. Kim MK, Han K, Kim HS, Park YM, Kwon HS, Yoon KH, et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study. Eur Heart J 2017;38:3560-6.ArticlePubMedPMC
- 15. Kim MK, Han K, Koh ES, Kim ES, Lee MK, Nam GE, et al. Blood pressure and development of cardiovascular disease in Koreans with type 2 diabetes mellitus. Hypertension 2019;73:319-26.ArticlePubMed
- 16. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83.ArticlePubMed
- 17. Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol 2004;57:1288-94.ArticlePubMed
- 18. Jung I, Kwon H, Park SE, Han KD, Park YG, Rhee EJ, et al. The prevalence and risk of type 2 diabetes in adults with disabilities in Korea. Endocrinol Metab (Seoul) 2020;35:552-61.ArticlePubMedPMCPDF
- 19. Fine JP, Gray RJ. A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999;94:496-509.Article
- 20. Oh J, Nam H, Park S, Chae JH, Kim TS. Decreased cardiovascular death in schizophrenia patients treated with antipsychotics: a Korean national cohort study. Schizophr Res 2021;228:417-24.ArticlePubMed
- 21. De Hert M, Cohen D, Bobes J, Cetkovich-Bakmas M, Leucht S, Ndetei DM, et al. Physical illness in patients with severe mental disorders. II. Barriers to care, monitoring and treatment guidelines, plus recommendations at the system and individual level. World Psychiatry 2011;10:138-51.ArticlePubMedPMC
- 22. So HC, Chau KL, Ao FK, Mo CH, Sham PC. Exploring shared genetic bases and causal relationships of schizophrenia and bipolar disorder with 28 cardiovascular and metabolic traits. Psychol Med 2019;49:1286-98.ArticlePubMed
- 23. Malan-Muller S, Kilian S, van den Heuvel LL, Bardien S, Asmal L, Warnich L, et al. A systematic review of genetic variants associated with metabolic syndrome in patients with schizophrenia. Schizophr Res 2016;170:1-17.ArticlePubMed
- 24. Laursen TM, Nordentoft M, Mortensen PB. Excess early mortality in schizophrenia. Annu Rev Clin Psychol 2014;10:425-48.ArticlePubMed
- 25. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta-analysis. JAMA Psychiatry 2015;72:334-41.ArticlePubMedPMC
- 26. Nielsen RE, Uggerby AS, Jensen SO, McGrath JJ. Increasing mortality gap for patients diagnosed with schizophrenia over the last three decades: a Danish nationwide study from 1980 to 2010. Schizophr Res 2013;146:22-7.ArticlePubMed
- 27. Piotrowski P, Gondek TM, Krolicka-Deregowska A, Misiak B, Adamowski T, Kiejna A. Causes of mortality in schizophrenia: an updated review of European studies. Psychiatr Danub 2017;29:108-20.ArticlePubMed
- 28. Kirkpatrick B, Kennedy BK. Accelerated aging in schizophrenia and related disorders: future research. Schizophr Res 2018;196:4-8.ArticlePubMed
REFERENCES
Figure & Data
References
Citations


 KDA
KDA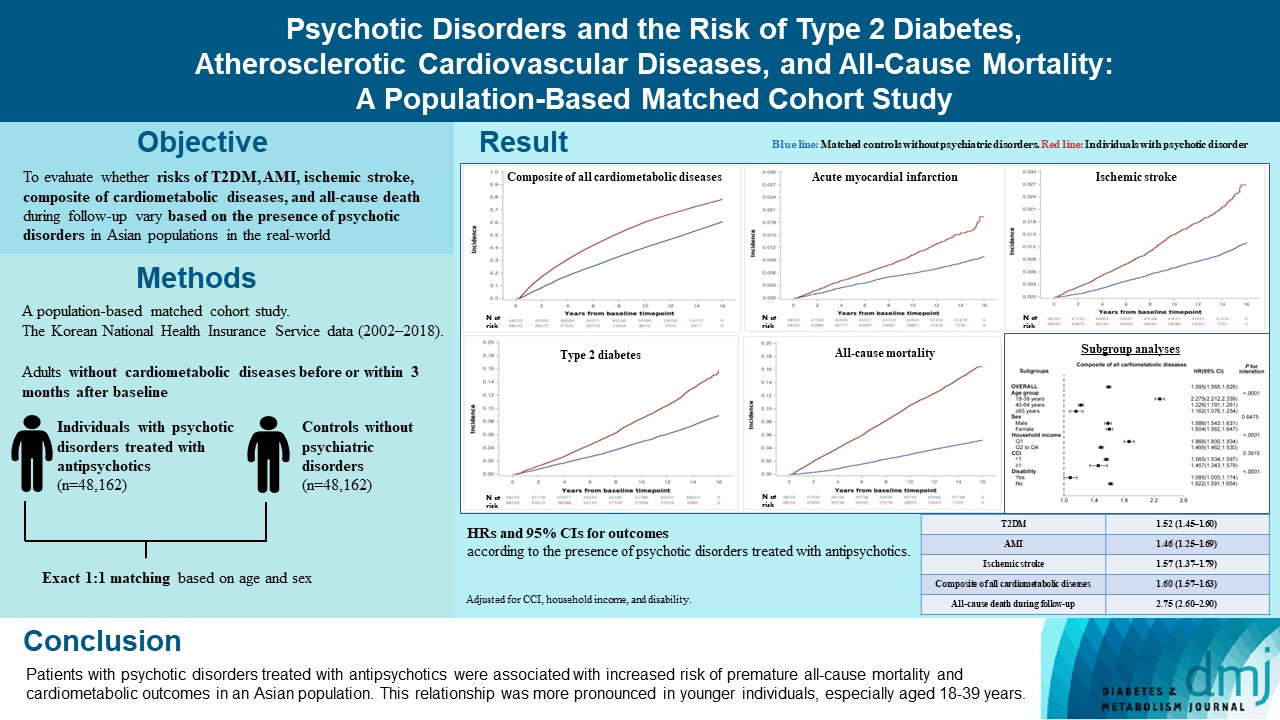
 PubReader
PubReader ePub Link
ePub Link Cite
Cite