
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
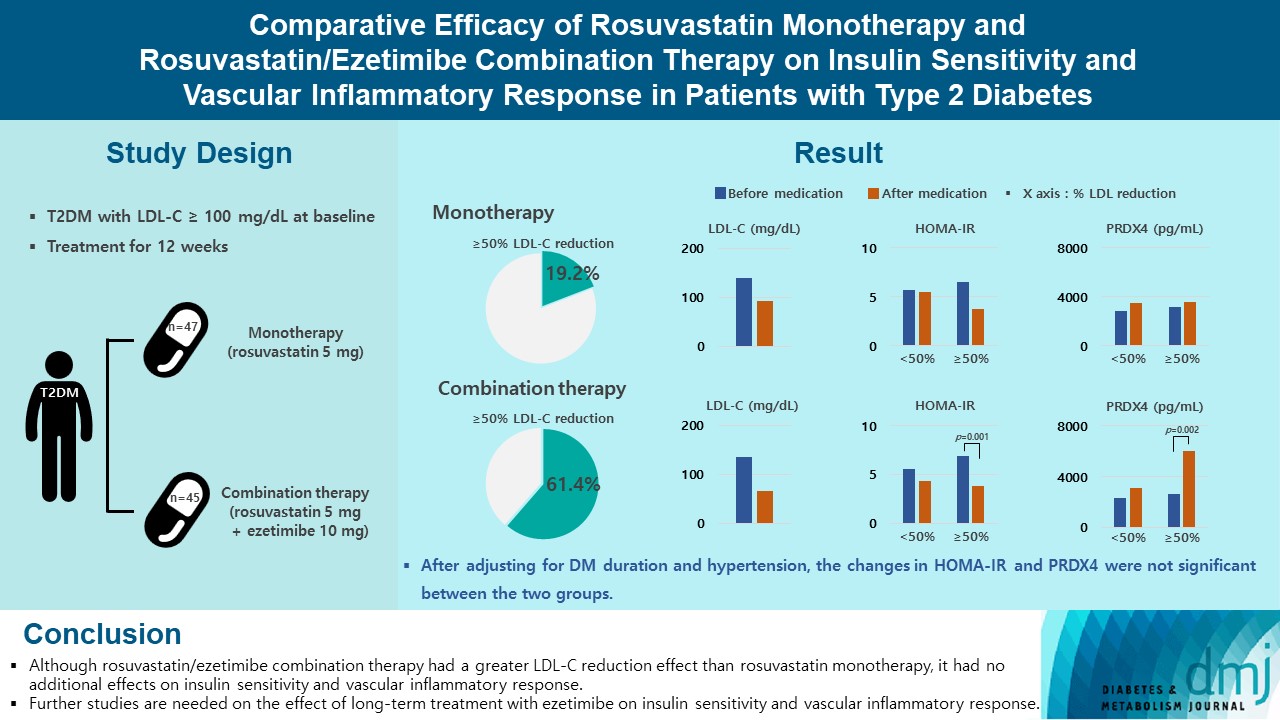
- Comparative Efficacy of Rosuvastatin Monotherapy and Rosuvastatin/Ezetimibe Combination Therapy on Insulin Sensitivity and Vascular Inflammatory Response in Patients with Type 2 Diabetes Mellitus
- Ji Hye Han, Kyong Hye Joung, Jun Choul Lee, Ok Soon Kim, Sorim Choung, Ji Min Kim, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Bon Jeong Ku, Hyun Jin Kim
- Diabetes Metab J. 2024;48(1):112-121. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0402
- 2,145 View
- 226 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Type 2 diabetes mellitus (T2DM) induces endothelial dysfunction and inflammation, which are the main factors for atherosclerosis and cardiovascular disease. The present study aimed to compare the effects of rosuvastatin monotherapy and rosuvastatin/ezetimibe combination therapy on lipid profile, insulin sensitivity, and vascular inflammatory response in patients with T2DM.
Methods
A total of 101 patients with T2DM and dyslipidemia were randomized to either rosuvastatin monotherapy (5 mg/day, n=47) or rosuvastatin/ezetimibe combination therapy (5 mg/10 mg/day, n=45) and treated for 12 weeks. Serum lipids, glucose, insulin, soluble intercellular adhesion molecule-1 (sICAM-1), and peroxiredoxin 4 (PRDX4) levels were determined before and after 12 weeks of treatment.
Results
The reduction in low density lipoprotein cholesterol (LDL-C) by more than 50% from baseline after treatment was more in the combination therapy group. The serum sICAM-1 levels increased significantly in both groups, but there was no difference between the two groups. The significant changes in homeostasis model assessment of insulin resistance (HOMA-IR) and PRDX4 were confirmed only in the subgroup in which LDL-C was reduced by 50% or more in the combination therapy group. However, after adjusting for diabetes mellitus duration and hypertension, the changes in HOMA-IR and PRDX4 were not significant between the two groups.
Conclusion
Although rosuvastatin/ezetimibe combination therapy had a greater LDL-C reduction effect than rosuvastatin monotherapy, it had no additional effects on insulin sensitivity and vascular inflammatory response. Further studies are needed on the effect of long-term treatment with ezetimibe on insulin sensitivity and vascular inflammatory response. -
Citations
Citations to this article as recorded by- Combining Ezetimibe and Rosuvastatin: Impacts on Insulin Sensitivity and Vascular Inflammation in Patients with Type 2 Diabetes Mellitus
Eun Roh
Diabetes & Metabolism Journal.2024; 48(1): 55. CrossRef
- Combining Ezetimibe and Rosuvastatin: Impacts on Insulin Sensitivity and Vascular Inflammation in Patients with Type 2 Diabetes Mellitus
- Drug Regimen
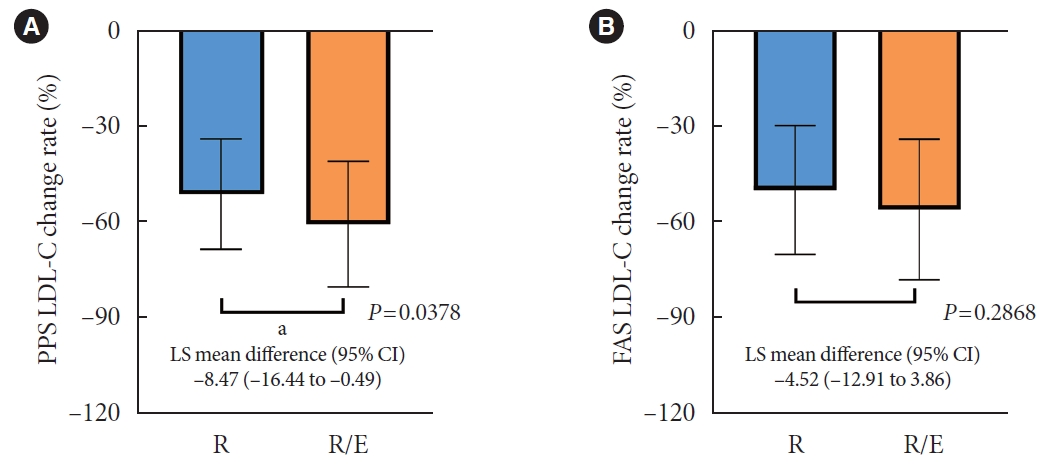
- The Efficacy and Safety of Moderate-Intensity Rosuvastatin with Ezetimibe versus High-Intensity Rosuvastatin in High Atherosclerotic Cardiovascular Disease Risk Patients with Type 2 Diabetes Mellitus: A Randomized, Multicenter, Open, Parallel, Phase 4 Study
- Jun Sung Moon, Il Rae Park, Sang Soo Kim, Hye Soon Kim, Nam Hoon Kim, Sin Gon Kim, Seung Hyun Ko, Ji Hyun Lee, Inkyu Lee, Bo Kyeong Lee, Kyu Chang Won
- Diabetes Metab J. 2023;47(6):818-825. Published online November 24, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0171
- 2,441 View
- 247 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To investigate the efficacy and safety of moderate-intensity rosuvastatin/ezetimibe combination compared to highintensity rosuvastatin in high atherosclerotic cardiovascular disease (ASCVD) risk patients with type 2 diabetes mellitus (T2DM).
Methods
This study was a randomized, multicenter, open, parallel phase 4 study, and enrolled T2DM subjects with an estimated 10-year ASCVD risk ≥7.5%. The primary endpoint was the low-density lipoprotein cholesterol (LDL-C) change rate after 24-week rosuvastatin 10 mg/ezetimibe 10 mg treatment was non-inferior to that of rosuvastatin 20 mg. The achievement proportion of 10-year ASCVD risk <7.5% or comprehensive lipid target (LDL-C <70 mg/dL, non-high-density lipoprotein cholesterol <100 mg/dL, and apolipoprotein B <80 mg/dL) without discontinuation, and several metabolic parameters were explored as secondary endpoints.
Results
A hundred and six participants were assigned to each group. Both groups showed significant reduction in % change of LDL-C from baseline at week 24 (–63.90±6.89 vs. –55.44±6.85, combination vs. monotherapy, p=0.0378; respectively), but the combination treatment was superior to high-intensity monotherapy in LDL-C change (%) from baseline (least square [LS] mean difference, –8.47; 95% confidence interval, –16.44 to –0.49; p=0.0378). The combination treatment showed a higher proportion of achieved comprehensive lipid targets rather than monotherapy (85.36% vs. 62.22% in monotherapy, p=0.015). The ezetimibe combination significantly improved homeostasis model assessment of β-cell function even without A1c changes (LS mean difference, 17.13; p=0.0185).
Conclusion
In high ASCVD risk patients with T2DM, the combination of moderate-intensity rosuvastatin and ezetimibe was not only non-inferior but also superior to improving dyslipidemia with additional benefits compared to high-intensity rosuvastatin monotherapy.
- Cardiovascular Risk/Epidemiology
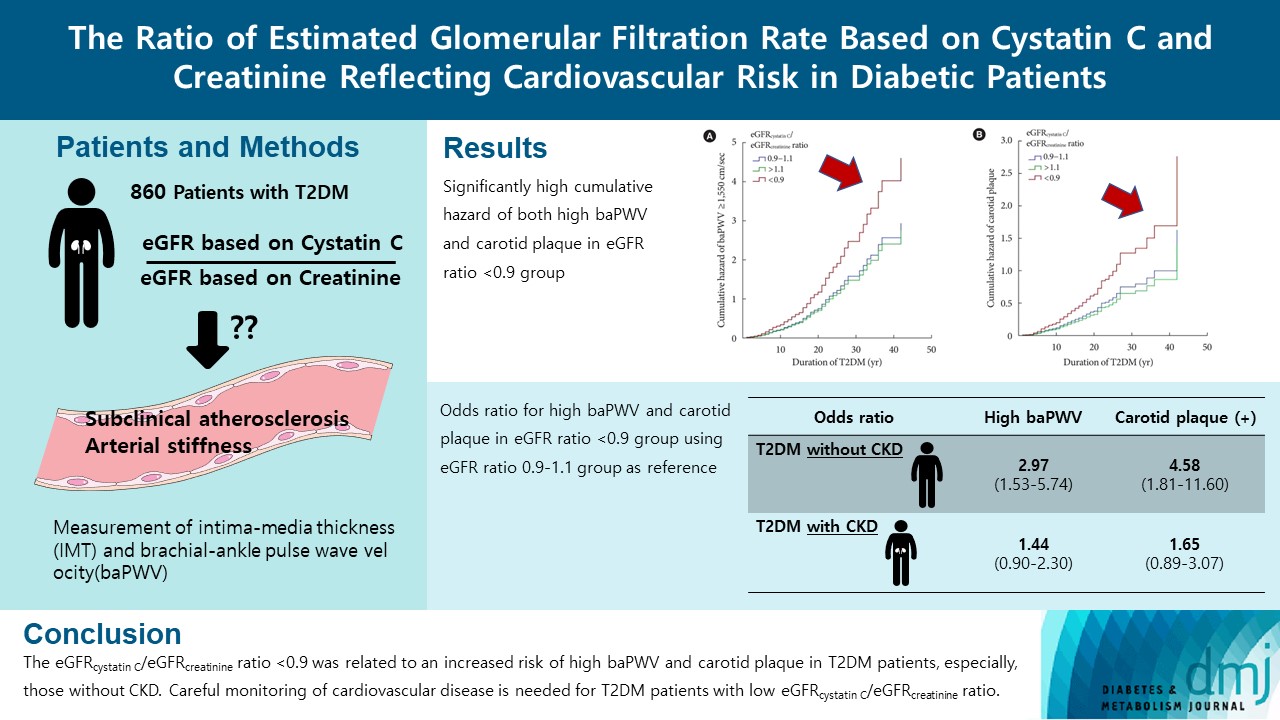
- The Ratio of Estimated Glomerular Filtration Rate Based on Cystatin C and Creatinine Reflecting Cardiovascular Risk in Diabetic Patients
- Ah Reum Khang, Min Jin Lee, Dongwon Yi, Yang Ho Kang
- Diabetes Metab J. 2023;47(3):415-425. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0177
- 1,854 View
- 112 Download
- 2 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The ratio of estimated glomerular filtration rate (eGFR) based on cystatin C and creatinine (eGFRcystatin C/eGFRcreatinine ratio) is related to accumulating atherosclerosis-promoting proteins and increased mortality in several cohorts.
Methods
We assessed whether the eGFRcystatin C/eGFRcreatinine ratio is a predictor of arterial stiffness and sub-clinical atherosclerosis in type 2 diabetes mellitus (T2DM) patients, who were followed up during 2008 to 2016. GFR was estimated using an equation based on cystatin C and creatinine.
Results
A total of 860 patients were stratified according to their eGFRcystatin C/eGFRcreatinine ratio (i.e., <0.9, 0.9–1.1 [a reference group], and >1.1). Intima-media thickness was comparable among the groups; however, presence of carotid plaque was frequent in the <0.9 group (<0.9 group, 38.3%; 0.9–1.1 group, 21.6% vs. >1.1 group, 17.2%, P<0.001). Brachial-ankle pulse wave velocity (baPWV) was faster in the <0.9 group (<0.9 group, 1,656.3±333.0 cm/sec; 0.9–1.1 group, 1,550.5±294.8 cm/sec vs. >1.1 group, 1,494.0±252.2 cm/sec, P<0.001). On comparing the <0.9 group with the 0.9–1.1 group, the multivariate-adjusted odds ratios of prevalence of high baPWV and carotid plaque were 2.54 (P=0.007) and 1.95 (P=0.042), respectively. Cox regression analysis demonstrated near or over 3-fold higher risks of the prevalence of high baPWV and carotid plaque in the <0.9 group without chronic kidney disease (CKD).
Conclusion
We concluded that eGFRcystatin C/eGFRcreatinine ratio <0.9 was related to an increased risk of high baPWV and carotid plaque in T2DM patients, especially, those without CKD. Careful monitoring of cardiovascular disease is needed for T2DM patients with low eGFRcystatin C/eGFRcreatinine ratio. -
Citations
Citations to this article as recorded by- Intraindividual difference in estimated GFR by creatinine and cystatin C, cognitive trajectories and motoric cognitive risk syndrome
Jinqi Wang, Yueruijing Liu, Rui Jin, Xiaoyu Zhao, Zhiyuan Wu, Ze Han, Zongkai Xu, Xiuhua Guo, Lixin Tao
Nephrology Dialysis Transplantation.2024; 39(5): 860. CrossRef - Research Progress of Creatinine, Cystatin C, and Their Ratio in Renal Diseases
广智 杨
Advances in Clinical Medicine.2024; 14(04): 976. CrossRef - Muscle mass, creatinine, cystatin C and selective glomerular hypofiltration syndromes
Linnea Malmgren, Anders Grubb
Clinical Kidney Journal.2023; 16(8): 1206. CrossRef - Investigating kidney function changes in young adults with COVID-19: Serum creatinine level, glomerular filtration rate, and biochemical profile analysis
Nikita Matyushin, Dmitriy Ermakov, Inna Vasileva, Roza Vakolyuk, Anastasiya Spaska
Electronic Journal of General Medicine.2023; 20(6): em547. CrossRef
- Intraindividual difference in estimated GFR by creatinine and cystatin C, cognitive trajectories and motoric cognitive risk syndrome
- Drug/Regimen
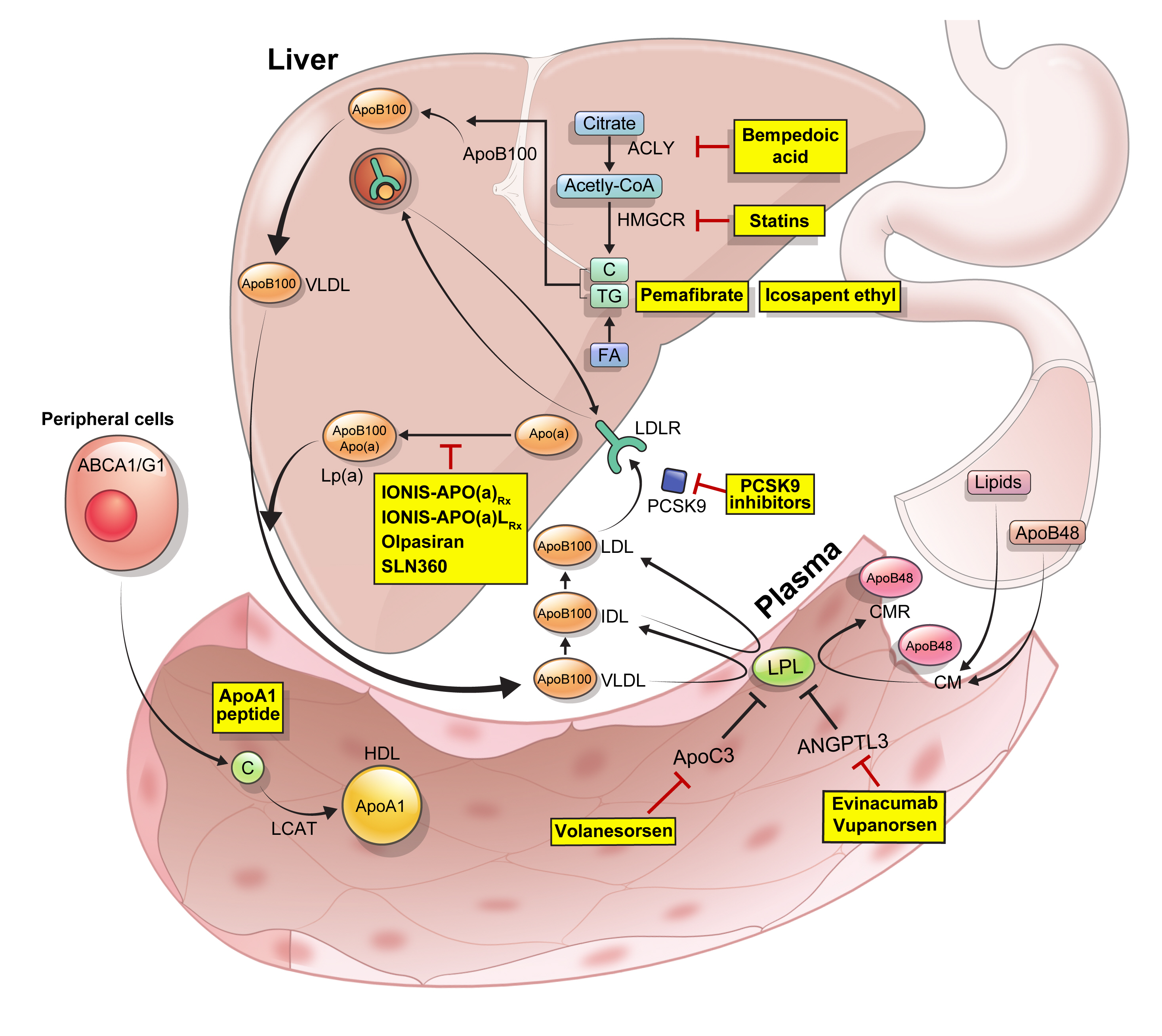
- New, Novel Lipid-Lowering Agents for Reducing Cardiovascular Risk: Beyond Statins
- Kyuho Kim, Henry N. Ginsberg, Sung Hee Choi
- Diabetes Metab J. 2022;46(4):517-532. Published online July 27, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0198
- Correction in: Diabetes Metab J 2022;46(5):817
- 10,063 View
- 865 Download
- 25 Web of Science
- 27 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Statins are the cornerstone of the prevention and treatment of atherosclerotic cardiovascular disease (ASCVD). However, even under optimal statin therapy, a significant residual ASCVD risk remains. Therefore, there has been an unmet clinical need for novel lipid-lowering agents that can target low-density lipoprotein cholesterol (LDL-C) and other atherogenic particles. During the past decade, several drugs have been developed for the treatment of dyslipidemia. Inclisiran, a small interfering RNA that targets proprotein convertase subtilisin/kexin type 9 (PCSK9), shows comparable effects to that of PCSK9 monoclonal antibodies. Bempedoic acid, an ATP citrate lyase inhibitor, is a valuable treatment option for the patients with statin intolerance. Pemafibrate, the first selective peroxisome proliferator-activated receptor alpha modulator, showed a favorable benefit-risk balance in phase 2 trial, but the large clinical phase 3 trial (PROMINENT) was recently stopped for futility based on a late interim analysis. High dose icosapent ethyl, a modified eicosapentaenoic acid preparation, shows cardiovascular benefits. Evinacumab, an angiopoietin-like 3 (ANGPTL3) monoclonal antibody, reduces plasma LDL-C levels in patients with refractory hypercholesterolemia. Novel antisense oligonucleotides targeting apolipoprotein C3 (apoC3), ANGPTL3, and lipoprotein(a) have significantly attenuated the levels of their target molecules with beneficial effects on associated dyslipidemias. Apolipoprotein A1 (apoA1) is considered as a potential treatment to exploit the athero-protective effects of high-density lipoprotein cholesterol (HDL-C), but solid clinical evidence is necessary. In this review, we discuss the mode of action and clinical outcomes of these novel lipid-lowering agents beyond statins.
-
Citations
Citations to this article as recorded by- The role of adherence in patients with chronic diseases
Michel Burnier
European Journal of Internal Medicine.2024; 119: 1. CrossRef - Bempedoic acid: new evidence and recommendations on use
Kristina Paponja, Ivan Pećin, Željko Reiner, Maciej Banach
Current Opinion in Lipidology.2024; 35(1): 41. CrossRef - Genetic insights into repurposing statins for hyperthyroidism prevention: a drug-target Mendelian randomization study
Anqi Huang, Xinyi Wu, Jiaqi Lin, Chiju Wei, Wencan Xu
Frontiers in Endocrinology.2024;[Epub] CrossRef - Targeting host-specific metabolic pathways—opportunities and challenges for anti-infective therapy
Monika I. Konaklieva, Balbina J. Plotkin
Frontiers in Molecular Biosciences.2024;[Epub] CrossRef - Neutrophil Extracellular Traps (NETs) and Atherosclerosis: Does Hypolipidemic Treatment Have an Effect?
Petros Adamidis, Despoina Pantazi, Iraklis Moschonas, Evangelos Liberopoulos, Alexandros Tselepis
Journal of Cardiovascular Development and Disease.2024; 11(3): 72. CrossRef - Modulating effects of crocin on lipids and lipoproteins: Mechanisms and potential benefits
Habib Yaribeygi, Mina Maleki, Farin Rashid-Farrokhi, Payman Raise Abdullahi, Mohammad Amin Hemmati, Tannaz Jamialahmadi, Amirhossein Sahebkar
Heliyon.2024; 10(7): e28837. CrossRef - Assessing the Benefits of Lifestyle Influences on Cardiovascu-lar Health After Acute Coronary Syndrome
Marius Rus, Claudia Elena Stanis, Paula Marian, Lilliana Oana Pobirci, Loredana Ioana Banszki, Veronica Huplea, Gheorghe Adrian Osiceanu, Bianca-Maria Pop, Gabriela Dogaru, Felicia Liana Andronie-Cioara
Balneo and PRM Research Journal.2024; 15(Vol.15, no): 660. CrossRef - Comprehensive mendelian randomization analysis of plasma proteomics to identify new therapeutic targets for the treatment of coronary heart disease and myocardial infarction
Ziyi Sun, Zhangjun Yun, Jianguo Lin, Xiaoning Sun, Qingqing Wang, Jinlong Duan, Cheng Li, Xiaoxiao Zhang, Siyu Xu, Zeqi Wang, Xingjiang Xiong, Kuiwu Yao
Journal of Translational Medicine.2024;[Epub] CrossRef - Hypercholesterolemia: a literature review on management using tafolecimab: a novel member of PCSK9 monoclonal antibodies
Zaheer Qureshi, Mikail Khanzada, Adnan Safi, Eeshal Fatima, Faryal Altaf, Timothy J. Vittorio
Annals of Medicine & Surgery.2024; 86(5): 2818. CrossRef - Liver cancer cells as the model for developing liver-targeted RNAi therapeutics
Beibei Hou, Linhui Qin, Linfeng Huang
Biochemical and Biophysical Research Communications.2023; 644: 85. CrossRef - Insights into Causal Cardiovascular Risk Factors from Mendelian Randomization
C. M. Schooling, J. V. Zhao
Current Cardiology Reports.2023; 25(2): 67. CrossRef - Secoisolariciresinol diglucoside and anethole ameliorate lipid abnormalities, oxidative injury, hypercholesterolemia, heart, and liver conditions
Sana Noreen, Habib‐ur Rehman, Tabussam Tufail, Huma Badar Ul Ain, Chinaza Godswill Awuchi
Food Science & Nutrition.2023; 11(6): 2620. CrossRef - Colesterol remanente, riesgo vascular y prevención de la arteriosclerosis
Xavier Pintó, Marta Fanlo, Virginia Esteve, Jesús Millán, Agustín Blanco, Mariano Blasco, José Luís Díaz Díaz, Ángel Díaz Rodríguez, Alipio Mangas, Vicente Pascual, Juan Pedro Botet, Pablo Pérez Martínez
Clínica e Investigación en Arteriosclerosis.2023; 35(4): 206. CrossRef - Evolving Management of Low‐Density Lipoprotein Cholesterol: A Personalized Approach to Preventing Atherosclerotic Cardiovascular Disease Across the Risk Continuum
Michael J. Wilkinson, Norman E. Lepor, Erin D. Michos
Journal of the American Heart Association.2023;[Epub] CrossRef - The cell origins of foam cell and lipid metabolism regulated by mechanical stress in atherosclerosis
Zhi Ouyang, Jian Zhong, Junyi Shen, Ye Zeng
Frontiers in Physiology.2023;[Epub] CrossRef - Triglyceride-Rich Lipoprotein Metabolism: Key Regulators of Their Flux
Alejandro Gugliucci
Journal of Clinical Medicine.2023; 12(13): 4399. CrossRef - Remnant cholesterol, vascular risk, and prevention of atherosclerosis
Xavier Pintó, Marta Fanlo, Virginia Esteve, Jesús Millán
Clínica e Investigación en Arteriosclerosis (English Edition).2023; 35(4): 206. CrossRef - Antibiotics and Lipid-Modifying Agents: Potential Drug–Drug Interactions and Their Clinical Implications
Marios Spanakis, Danny Alon-Ellenbogen, Petros Ioannou, Nikolaos Spernovasilis
Pharmacy.2023; 11(4): 130. CrossRef - Advances in Treatment of Dyslipidemia
Jill Dybiec, Wiktoria Baran, Bartłomiej Dąbek, Piotr Fularski, Ewelina Młynarska, Ewa Radzioch, Jacek Rysz, Beata Franczyk
International Journal of Molecular Sciences.2023; 24(17): 13288. CrossRef - Peroxisome Proliferator-Activated Receptor α in Lipoprotein Metabolism and Atherosclerotic Cardiovascular Disease
Elena Valeria Fuior, Evangelia Zvintzou, Theodosios Filippatos, Katerina Giannatou, Victoria Mparnia, Maya Simionescu, Anca Violeta Gafencu, Kyriakos E. Kypreos
Biomedicines.2023; 11(10): 2696. CrossRef - Preparation, characterization and in vivo pharmacokinetic study of ginsenoside Rb1-PLGA nanoparticles
Lixin Du, Huiling Lu, Yifei Xiao, Zhihua Guo, Ya Li
Scientific Reports.2023;[Epub] CrossRef - Dysregulation of Cholesterol Homeostasis in Ovarian Cancer
Zahraa Qusairy, Anne Gangloff, Shuk On Annie Leung
Current Oncology.2023; 30(9): 8386. CrossRef - Riesgo residual. Conclusiones
Ángel Cequier, José Luis Zamorano
Revista Española de Cardiología Suplementos.2023; 23: 25. CrossRef - Causal effects of circulating lipids and lipid-lowering drugs on the risk of urinary stones: a Mendelian randomization study
Zilong Tan, Jing Hong, Aochuan Sun, Mengdi Ding, Jianwu Shen
Frontiers in Endocrinology.2023;[Epub] CrossRef - Bibliometric analysis of residual cardiovascular risk: trends and frontiers
Lin Wang, Sutong Wang, Chaoyuan Song, Yiding Yu, Yuehua Jiang, Yongcheng Wang, Xiao Li
Journal of Health, Population and Nutrition.2023;[Epub] CrossRef - Current Understanding on the Genetic Basis of Key Metabolic Disorders: A Review
Kenneth Francis Rodrigues, Wilson Thau Lym Yong, Md. Safiul Alam Bhuiyan, Shafiquzzaman Siddiquee, Muhammad Dawood Shah, Balu Alagar Venmathi Maran
Biology.2022; 11(9): 1308. CrossRef - Lipoprotein Lipase: Is It a Magic Target for the Treatment of Hypertriglyceridemia
Joon Ho Moon, Kyuho Kim, Sung Hee Choi
Endocrinology and Metabolism.2022; 37(4): 575. CrossRef
- The role of adherence in patients with chronic diseases
- Metabolic Risk/Epidemiology
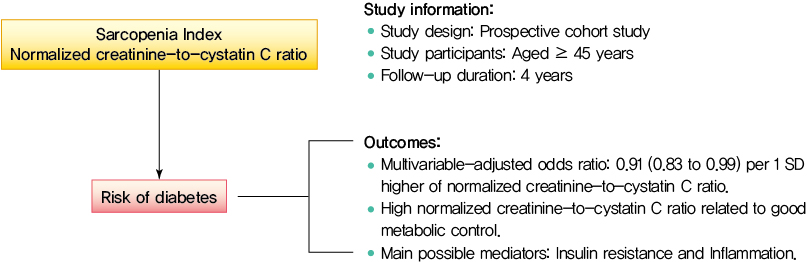
- Normalized Creatinine-to-Cystatin C Ratio and Risk of Diabetes in Middle-Aged and Older Adults: The China Health and Retirement Longitudinal Study
- Shanhu Qiu, Xue Cai, Bo Xie, Yang Yuan, Zilin Sun, Tongzhi Wu
- Diabetes Metab J. 2022;46(3):476-485. Published online March 7, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0074
- 4,755 View
- 205 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Creatinine-to-cystatin C ratio is recently suggested to be a surrogate marker for sarcopenia. However, little is known about its association with diabetes. This study aimed to fill in this gap based on a large-scale prospective cohort.
Methods
A population-based representative sample of 5,055 participants aged ≥45 years from the China Health and Retirement Longitudinal Study was enrolled between 2011 and 2012 and followed at least once during the subsequent surveys at 2013, 2015, or 2018. Creatinine-to-cystatin C ratio was calculated and normalized by body weight. Incident diabetes was ascertained by plasma glucose, glycosylated hemoglobin, self-reported history, or use of anti-diabetic drugs. Logistic regression analysis and mediation analysis were employed.
Results
During follow-up, 634 participants developed diabetes. The risk of diabetes was gradually and significantly decreased with increased normalized creatinine–cystatin C ratio. The multivariable-adjusted odds ratio for diabetes was 0.91 (95% confidence interval, 0.83 to 0.99) per 1 standard deviation higher of normalized creatinine-to-cystatin C ratio, and this relationship remained significant after controlling for muscle strength. The risk reduction in diabetes was significantly larger in participants with normal-weight and high normalized creatinine-to-cystatin C ratio compared with those with overweight/obesity and high normalized creatinine-to-cystatin C ratio (Pinteraction=0.01). Insulin resistance and inflammation appeared to be key mediators accounting for the observed relationship between normalized creatinine-to-cystatin C ratio and risk of diabetes, with their mediating effect being 93.1% and 22.0%, respectively.
Conclusion
High normalized creatinine-to-cystatin C ratio is associated with reduced risk of diabetes in middle-aged and older adults. -
Citations
Citations to this article as recorded by- Muscle Quality in Relation to Prediabetes Phenotypes: A Population-Based Study With Mediation Analysis
Shanhu Qiu, Xue Cai, Xiaoying Zhou, Jinshui Xu, Zilin Sun, Haijian Guo, Tongzhi Wu
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1151. CrossRef - Sex‐specific associations between skeletal muscle mass and incident diabetes: A population‐based cohort study
Dan Liu, Nan Li, Yiling Zhou, Miye Wang, Peige Song, Changzheng Yuan, Qingyang Shi, Hui Chen, Kaixin Zhou, Huan Wang, Tao Li, Xiong‐Fei Pan, Haoming Tian, Sheyu Li
Diabetes, Obesity and Metabolism.2024; 26(3): 820. CrossRef - Diabetes Mellitus Should Be Considered While Analysing Sarcopenia-Related Biomarkers
Justyna Rentflejsz, Zyta Beata Wojszel
Journal of Clinical Medicine.2024; 13(4): 1107. CrossRef - Associations of muscle mass and strength with new-onset diabetes among middle-aged and older adults: evidence from the China health and retirement longitudinal study (CHARLS)
Yun-Yun He, Mei-Ling Jin, Xiang-Yang Fang, Xiao-Juan Wang
Acta Diabetologica.2024;[Epub] CrossRef - The serum creatinine to cystatin C to waist circumference ratios predicts risk for type 2 diabetes: A Chinese cohort study
Yinfei Chen, Weiheng Wen, Zhiliang Mai, Ming Wang, Hong Chen, Jia Sun
Journal of Diabetes.2023; 15(10): 808. CrossRef - Associations of sarcopenia with peak expiratory flow among community-dwelling elderly population: based on the China Health and Retirement Longitudinal Study (CHARLS)
Yun-Yun He, Mei-Ling Jin, Jing Chang, Xiao-Juan Wang
European Geriatric Medicine.2023; 15(1): 95. CrossRef - Additive impact of diabetes and sarcopenia on all-cause and cardiovascular mortality: A longitudinal nationwide population-based study
Eyun Song, Soon Young Hwang, Min Jeong Park, Ahreum Jang, Kyeong Jin Kim, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Metabolism.2023; 148: 155678. CrossRef
- Muscle Quality in Relation to Prediabetes Phenotypes: A Population-Based Study With Mediation Analysis
- Drug/Regimen
- Efficacy and Safety of Omega-3 Fatty Acids in Patients Treated with Statins for Residual Hypertriglyceridemia: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial
- Ji Eun Jun, In-Kyung Jeong, Jae Myung Yu, Sung Rae Kim, In Kye Lee, Kyung-Ah Han, Sung Hee Choi, Soo-Kyung Kim, Hyeong Kyu Park, Ji-Oh Mok, Yong-ho Lee, Hyuk-Sang Kwon, So Hun Kim, Ho-Cheol Kang, Sang Ah Lee, Chang Beom Lee, Kyung Mook Choi, Sung-Ho Her, Won Yong Shin, Mi-Seung Shin, Hyo-Suk Ahn, Seung Ho Kang, Jin-Man Cho, Sang-Ho Jo, Tae-Joon Cha, Seok Yeon Kim, Kyung Heon Won, Dong-Bin Kim, Jae Hyuk Lee, Moon-Kyu Lee
- Diabetes Metab J. 2020;44(1):78-90. Published online June 20, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0265
- 9,365 View
- 190 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Cardiovascular risk remains increased despite optimal low density lipoprotein cholesterol (LDL-C) level induced by intensive statin therapy. Therefore, recent guidelines recommend non-high density lipoprotein cholesterol (non-HDL-C) as a secondary target for preventing cardiovascular events. The aim of this study was to assess the efficacy and tolerability of omega-3 fatty acids (OM3-FAs) in combination with atorvastatin compared to atorvastatin alone in patients with mixed dyslipidemia.
Methods This randomized, double-blind, placebo-controlled, parallel-group, and phase III multicenter study included adults with fasting triglyceride (TG) levels ≥200 and <500 mg/dL and LDL-C levels <110 mg/dL. Eligible subjects were randomized to ATOMEGA (OM3-FAs 4,000 mg plus atorvastatin calcium 20 mg) or atorvastatin 20 mg plus placebo groups. The primary efficacy endpoints were the percent changes in TG and non-HDL-C levels from baseline at the end of treatment.
Results After 8 weeks of treatment, the percent changes from baseline in TG (−29.8% vs. 3.6%,
P <0.001) and non-HDL-C (−10.1% vs. 4.9%,P <0.001) levels were significantly greater in the ATOMEGA group (n =97) than in the atorvastatin group (n =103). Moreover, the proportion of total subjects reaching TG target of <200 mg/dL in the ATOMEGA group was significantly higher than that in the atorvastatin group (62.9% vs. 22.3%,P <0.001). The incidence of adverse events did not differ between the two groups.Conclusion The addition of OM3-FAs to atorvastatin improved TG and non-HDL-C levels to a significant extent compared to atorvastatin alone in subjects with residual hypertriglyceridemia.
-
Citations
Citations to this article as recorded by- Association Between Omega‐3 Fatty Acid Intake and Dyslipidemia: A Continuous Dose–Response Meta‐Analysis of Randomized Controlled Trials
Tianjiao Wang, Xin Zhang, Na Zhou, Yuxuan Shen, Biao Li, Bingshu E. Chen, Xinzhi Li
Journal of the American Heart Association.2023;[Epub] CrossRef - Nutraceutical support in the prevention and treatment of cardiovascular diseases
E. V. Gracheva, E. A. Starovoytova, E. S. Kulikov, N. A. Kirillova, S. V. Fedosenko, M. A. Balaganskaya, D. V. Kromka
Rational Pharmacotherapy in Cardiology.2023; 19(3): 298. CrossRef - Effect of coadministration of omega-3 fatty acids with glimepiride on glycemic control, lipid profile, irisin, and sirtuin-1 in type 2 diabetes mellitus patients: a randomized controlled trial
Rehab H. Werida, Aalaa Ramzy, Youssri Nassief Ebrahim, Maged Wasfy Helmy
BMC Endocrine Disorders.2023;[Epub] CrossRef - The Effect of Dietary Interventions on Hypertriglyceridemia: From Public Health to Molecular Nutrition Evidence
Karla Paulina Luna-Castillo, Xochitl Citlalli Olivares-Ochoa, Rocío Guadalupe Hernández-Ruiz, Iris Monserrat Llamas-Covarrubias, Saraí Citlalic Rodríguez-Reyes, Alejandra Betancourt-Núñez, Barbara Vizmanos, Erika Martínez-López, José Francisco Muñoz-Valle
Nutrients.2022; 14(5): 1104. CrossRef - The effect of omega-3 fatty acids and its combination with statins on lipid profile in patients with hypertriglyceridemia: A systematic review and meta-analysis of randomized controlled trials
Yunjiao Yang, Wen Deng, Yanmei Wang, Tongyi Li, Yiding Chen, Cong Long, Qing Wen, Yue Wu, Qiu Chen
Frontiers in Nutrition.2022;[Epub] CrossRef - Comparison of the Efficacy and Safety of Atorvastatin 40 mg/ω-3 Fatty Acids 4 g Fixed-dose Combination and Atorvastatin 40 mg Monotherapy in Hypertriglyceridemic Patients who Poorly Respond to Atorvastatin 40 mg Monotherapy: An 8-week, Multicenter, Random
Jong Shin Woo, Soon Jun Hong, Dong Hoon Cha, Kee Sik Kim, Moo Hyun Kim, Jun-Won Lee, Myung Ho Jeong, Jin-Ok Jeong, Jun-Hee Lee, Doo Soo Jeon, Eun Joo Cho, Soon Kil Kim, Jun Kwan, Chang Gyu Park, Hae Young Lee, Taek Jong Hong, Jinho Shin, Ho Joong Youn, Do
Clinical Therapeutics.2021; 43(8): 1419. CrossRef - All-Cause Mortality and Cardiovascular Death between Statins and Omega-3 Supplementation: A Meta-Analysis and Network Meta-Analysis from 55 Randomized Controlled Trials
Jeongseon Kim, Tung Hoang, Ji-Myung Kim, So Young Bu, Jeong-Hwa Choi, Eunju Park, Seung-Min Lee, Eunmi Park, Ji Yeon Min, In Seok Lee, So Young Youn, Jee-Young Yeon
Nutrients.2020; 12(10): 3203. CrossRef
- Association Between Omega‐3 Fatty Acid Intake and Dyslipidemia: A Continuous Dose–Response Meta‐Analysis of Randomized Controlled Trials
- Clinical Diabetes & Therapeutics
- Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus
- You-Cheol Hwang, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
- Diabetes Metab J. 2019;43(5):582-589. Published online January 16, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0124
- 6,632 View
- 185 Download
- 14 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The apolipoprotein B/A1 (apoB/A1) ratio is a stronger predictor of future cardiovascular disease than is the level of conventional lipids. Statin and ezetimibe combination therapy have shown additional cardioprotective effects over statin monotherapy.
Methods This was a single-center, randomized, open-label, active-controlled study in Korea. A total of 36 patients with type 2 diabetes mellitus were randomized to either rosuvastatin monotherapy (20 mg/day,
n =20) or rosuvastatin/ezetimibe (5 mg/10 mg/day,n =16) combination therapy for 6 weeks.Results After the 6-week treatment, low density lipoprotein cholesterol (LDL-C) and apoB reduction were comparable between the two groups (−94.3±15.4 and −62.0±20.9 mg/dL in the rosuvastatin group, −89.9±22.7 and −66.8±21.6 mg/dL in the rosuvastatin/ezetimibe group,
P =0.54 andP =0.86, respectively). In addition, change in apoB/A1 ratio (−0.44±0.16 in the rosuvastatin group and −0.47±0.25 in the rosuvastatin/ezetimibe group,P =0.58) did not differ between the two groups. On the other hand, triglyceride and free fatty acid (FFA) reductions were greater in the rosuvastatin/ezetimibe group than in the rosuvastatin group (−10.5 mg/dL [interquartile range (IQR), −37.5 to 29.5] and 0.0 µEq/L [IQR, −136.8 to 146.0] in the rosuvastatin group, −49.5 mg/dL [IQR, −108.5 to −27.5] and −170.5 µEq/L [IQR, −353.0 to 0.8] in the rosuvastatin/ezetimibe group,P =0.010 andP =0.049, respectively). Both treatments were generally well tolerated, and there were no differences in muscle or liver enzyme elevation.Conclusion A 6-week combination therapy of low-dose rosuvastatin and ezetimibe showed LDL-C, apoB, and apoB/A1 ratio reduction comparable to that of high-dose rosuvastatin monotherapy in patients with type 2 diabetes mellitus. Triglyceride and FFA reductions were greater with the combination therapy than with rosuvastatin monotherapy.
-
Citations
Citations to this article as recorded by- Moderate-Intensity Rosuvastatin/Ezetimibe Combination versus Quadruple-Dose Rosuvastatin Monotherapy: A Meta-Analysis and Systemic Review
Yura Kang, Jung Mi Park, Sang-Hak Lee
Yonsei Medical Journal.2024; 65(1): 19. CrossRef - Combination Therapy of Ezetimibe and Rosuvastatin for Dyslipidemia: Current Insights
Maya R Chilbert, Dylan VanDuyn, Sara Salah, Collin M Clark, Qing Ma
Drug Design, Development and Therapy.2022; Volume 16: 2177. CrossRef - Ezetimibe and diabetes mellitus:a new strategy for lowering cholesterol
V.A. Serhiyenko, A.A. Serhiyenko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(5): 302. CrossRef - The Effect of Rosuvastatin on Plasma/Serum Levels of High-Sensitivity C-Reactive Protein, Interleukin-6, and D-Dimer in People Living with Human Immunodeficiency Virus: A Systematic Review and Meta-Analysis
Akililu Alemu Ashuro, Yin-Guang Fan, Yuan-Sheng Fu, Dong-Sheng Di, Napoleon Bellua Sam, Hai-Feng Pan, Dong-Qing Ye
AIDS Research and Human Retroviruses.2021; 37(11): 821. CrossRef - Comparison of the Efficacy and Safety of Rosuvastatin/Ezetimibe Combination Therapy and Rosuvastatin Monotherapy on Lipoprotein in Patients With Type 2 Diabetes: Multicenter Randomized Controlled Study
Jiwoo Lee, You-Cheol Hwang, Woo Je Lee, Jong Chul Won, Kee-Ho Song, Cheol-Young Park, Kyu Jeung Ahn, Joong-Yeol Park
Diabetes Therapy.2020; 11(4): 859. CrossRef - Comparison of Renal Effects of Ezetimibe–Statin Combination versus Statin Monotherapy: A Propensity-Score-Matched Analysis
Jaehyun Bae, Namki Hong, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Yong-ho Lee
Journal of Clinical Medicine.2020; 9(3): 798. CrossRef - Combined use of rosuvastatin and ezetimibe improves hepatic steatosis in patients with dyslipidemia
Won Dong Lee, Beom Kyung Kim, Jun Yong Park, Do Young Kim, Sang Hoon Ahn, Kwang-Hyub Han, Seung Up Kim
European Journal of Gastroenterology & Hepatology.2020; 32(12): 1538. CrossRef - Influence of rosuvastatin dose on total fatty acids and free fatty acids in plasma
Cristian I. Ciucanu, Sonia Olariu, Daliborca C. Vlad, Victor Dumitraşcu
Medicine.2020; 99(48): e23356. CrossRef - The effect of switching from statin-monotherapy to statin/ezetimibe combination therapy on lipid profiles in patients with type 2 diabetes and dyslipidemia: a multicenter open-label study (EUCLID)
Mitsuhide Takeshita, Atsushi Tanaka, Atsushi Kawaguchi, Keiko Sato, Shigeru Toyoda, Teruo Inoue, Koichi Node
Vascular Failure.2020; 4(1): 22. CrossRef - Response: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J 2019;43:582–9)
You-Cheol Hwang
Diabetes & Metabolism Journal.2019; 43(6): 915. CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - Changes in Plasma Free Fatty Acids Associated with Type-2 Diabetes
Amélie I. S. Sobczak, Claudia A. Blindauer, Alan J. Stewart
Nutrients.2019; 11(9): 2022. CrossRef
- Moderate-Intensity Rosuvastatin/Ezetimibe Combination versus Quadruple-Dose Rosuvastatin Monotherapy: A Meta-Analysis and Systemic Review
- Complications
- Association between Serum Cystatin C and Vascular Complications in Type 2 Diabetes Mellitus without Nephropathy
- Hye Jeong Kim, Dong Won Byun, Kyoil Suh, Myung Hi Yoo, Hyeong Kyu Park
- Diabetes Metab J. 2018;42(6):513-518. Published online October 15, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0006
- 3,593 View
- 43 Download
- 12 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recent studies have correlated serum cystatin C (CysC) with vascular complications, but few studies have investigated this correlation in diabetes patients without nephropathy. This study aimed to evaluate if higher serum CysC levels increase the risk for vascular complications in type 2 diabetes mellitus patients with normal renal function or mild renal impairment.
Methods A total of 806 consecutive patients with type 2 diabetes mellitus who were admitted to the diabetes center of Soonchunhyang University Hospital for blood glucose control were retrospectively reviewed. Patients with nephropathy were excluded. Subjects were categorized into quartiles of serum CysC levels (Q1, ≤0.65 mg/L; Q2, 0.66 to 0.79 mg/L; Q3, 0.80 to 0.94 mg/L; and Q4, ≥0.95 mg/L).
Results The proportion of patients with diabetic retinopathy (DR) (
P for trend <0.001), coronary heart disease (CHD) (P for trend <0.001), and stroke (P for trend <0.001) increased across the serum CysC quartiles. After adjustment for confounding factors, the highest serum CysC level remained a significant risk factor for DR (odds ratio [OR], 1.929; 95% confidence interval [CI], 1.007 to 4.144;P =0.040). Compared with Q1, a significant positive association was observed between serum CysC and CHD in Q2 (OR, 7.321; 95% CI, 1.114 to 48.114;P =0.012), Q3 (OR, 6.027; 95% CI, 0.952 to 38.161;P =0.020), and Q4 (OR, 8.122; 95% CI, 1.258 to 52.453;P =0.007). No associations were observed between CysC and stroke after additional adjustment for confounding variables.Conclusion Serum CysC levels are independently associated with DR and CHD, suggesting that CysC may be useful for identifying type 2 diabetes mellitus patients without nephropathy who are at high risk for vascular complications.
-
Citations
Citations to this article as recorded by- A systematic literature review of machine learning based risk prediction models for diabetic retinopathy progression
Tiwalade Modupe Usman, Yakub Kayode Saheed, Augustine Nsang, Abel Ajibesin, Sandip Rakshit
Artificial Intelligence in Medicine.2023; 143: 102617. CrossRef - Serum cystatin C for risk stratification of prediabetes and diabetes populations
Kun Xiong, Shiran Zhang, Pingting Zhong, Zhuoting Zhu, Yanping Chen, Wenyong Huang, Wei Wang
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(11): 102882. CrossRef - Serum VEGF, high-sensitivity CRP, and cystatin-C assist in the diagnosis of type 2 diabetic retinopathy complicated with hyperuricemia
Jing Wei, Jincheng Zhang, Yanan Shi, Huiqin Zhang, Yan Wu
Open Medicine.2023;[Epub] CrossRef - Diagnostic circulating biomarkers to detect vision‐threatening diabetic retinopathy: Potential screening tool of the future?
Karen Frudd, Sobha Sivaprasad, Rajiv Raman, Subramanian Krishnakumar, Yeddula Rebecca Revathy, Patric Turowski
Acta Ophthalmologica.2022;[Epub] CrossRef - Association between circulating cystatin C and hyperuricemia: a cross-sectional study
Yanjun Guo, Hangkai Huang, Yishu Chen, Chao Shen, Chengfu Xu
Clinical Rheumatology.2022; 41(7): 2143. CrossRef - Multicenter Evaluation of Diagnostic Circulating Biomarkers to Detect Sight-Threatening Diabetic Retinopathy
Sarega Gurudas, Karen Frudd, Jayapal Jeya Maheshwari, Yeddula Rebecca Revathy, Sobha Sivaprasad, Shruthi Mahalakshmi Ramanathan, Vignesh Pooleeswaran, A. Toby Prevost, Eleni Karatsai, Sandra Halim, Shruti Chandra, Paul Nderitu, Dolores Conroy, Subramanian
JAMA Ophthalmology.2022; 140(6): 587. CrossRef - A Cross-Sectional Study of Serum and Urine Fluoride in Diabetes in Fluoride Exposed Population
Sai Deepika Ram Mohan, Shashidhar Kurpad Nagaraj, Raveesha Anjanappa, Muninarayana Chandrappa
Journal of Evolution of Medical and Dental Sciences.2021; 10(11): 798. CrossRef - Cystatin C predicts the risk of incident cerebrovascular disease in the elderly
Xin Zheng, Hong-da She, Qiao-xin Zhang, Tong Si, Ku-sheng Wu, Ying-xiu Xiao
Medicine.2021; 100(28): e26617. CrossRef - Proteinuria Is Associated with Carotid Artery Atherosclerosis in Non-Albuminuric Type 2 Diabetes: A Cross-Sectional Study
Jaehyun Bae, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Journal of Clinical Medicine.2020; 9(1): 136. CrossRef
- A systematic literature review of machine learning based risk prediction models for diabetic retinopathy progression
- Clinical Care/Education
- Efficacy of Moderate Intensity Statins in the Treatment of Dyslipidemia in Korean Patients with Type 2 Diabetes Mellitus
- Sung Hye Kong, Bo Kyung Koo, Min Kyong Moon
- Diabetes Metab J. 2017;41(1):23-30. Published online December 16, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.23
- 4,505 View
- 84 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background There has been evidences of ethnic differences in the low density lipoprotein cholesterol (LDL-C) lowering effect of statin. We aimed to evaluate the efficacy of moderate-intensity statins in the treatment of dyslipidemia among Korean patients with type 2 diabetes mellitus (T2DM).
Methods We analyzed a retrospective cohort that consisted of Korean patients with T2DM aged 40 to 75 years who had been prescribed any of the moderate-intensity statins (atorvastatin 10 or 20 mg, rosuvastatin 5 or 10 mg, pitavastatin 2 mg, or pravastatin 40 mg). Among them, only patients with baseline lipid profiles before starting statin treatment were selected, and changes in their lipid profiles before and 6 months after statin therapy were analyzed.
Results Following the first 6 months of therapy, the overall LDL-C reduction was −47.4% (interquartile range, −56.6% to −34.1%). In total, 92.1% of the participants achieved an LDL-C level of <100 mg/dL, 38.3% had a 30% to 50% reduction in their LDL-C levels, and 42.3% had a reduction in their LDL-C levels greater than 50%. The response rates of each drug for achieving a LDL-C level <100 mg/dL were 81.7%, 93.1%, 95.0%, 95.0%, 96.5%, and 91.7% for treatment with atorvastatin doses of 10 or 20 mg, rosuvastatin 5 or 10 mg, pitavastatin 2 mg, and pravastatin 40 mg, respectively.
Conclusion In conclusion, the use of moderate-intensity statins reduced LDL-C levels less than 100 mg/dL in most of the Korean patients studied with T2DM. The efficacies of those statins were higher than expected in about 42% of Korean patients with T2DM.
-
Citations
Citations to this article as recorded by- Effect of combining evolocumab with statin on carotid intraplaque neovascularization in patients with premature coronary artery disease (EPOCH)
Yanyan Han, Ling Ren, Xiang Fei, Jingjing Wang, Tao Chen, Jun Guo, Qi Wang
Atherosclerosis.2024; 391: 117471. CrossRef - Impact of Plasma Exposure of Statins and Their Metabolites With Major Adverse Cardiovascular Events in Chinese Patients With Coronary Artery Disease
Xiao-hong Zhou, Li-yun Cai, Wei-Hua Lai, Xue Bai, Yi-bin Liu, Qian Zhu, Guo-dong He, Ji-Yan Chen, Min Huang, Zhi-ling Zhou, Shi-long Zhong
Frontiers in Pharmacology.2020;[Epub] CrossRef - Efficacy and Safety of High-Dose Atorvastatin in Moderate-to-High Cardiovascular Risk Postmenopausal Korean Women with Dyslipidemia
Jaecheol Moon, Soyeon Yoo, Gwanpyo Koh, Kyung-Wan Min, Hyun Ho Shin
Journal of Lipid and Atherosclerosis.2020; 9(1): 162. CrossRef - Effects of lowest-dose vs. highest-dose pitavastatin on coronary neointimal hyperplasia at 12-month follow-up in type 2 diabetic patients with non-ST elevation acute coronary syndrome: an optical coherence tomography analysis
Jung Wook Lim, Han Saem Jeong, Soon Jun Hong, Hyo Jeong Kim, Young Chan Kim, Bong Gyun Kang, Su Min Jeon, Jae Young Cho, Seung Hoon Lee, Hyung Joon Joo, Jae Hyoung Park, Cheol Woong Yu
Heart and Vessels.2019; 34(1): 62. CrossRef - Effect of Statin Therapy on Outcomes of Patients With Acute Ischemic Stroke and Atrial Fibrillation
Kang‐Ho Choi, Woo‐Keun Seo, Man‐Seok Park, Joon‐Tae Kim, Jong‐Won Chung, Oh Young Bang, Gyeong‐Moon Kim, Tae‐Jin Song, Bum Joon Kim, Sung Hyuk Heo, Jin‐Man Jung, Kyung‐Mi Oh, Chi Kyung Kim, Sungwook Yu, Kwang‐Yeol Park, Jeong‐Min Kim, Jong‐Ho Park, Jay Ch
Journal of the American Heart Association.2019;[Epub] CrossRef - Moderate-intensity versus high-intensity statin therapy in Korean patients with angina undergoing percutaneous coronary intervention with drug-eluting stents: A propensity-score matching analysis
Mahn-Won Park, Gyung-Min Park, Seungbong Han, Yujin Yang, Yong-Giun Kim, Jae-Hyung Roh, Hyun Woo Park, Jon Suh, Young-Rak Cho, Ki-Bum Won, Soe Hee Ann, Shin-Jae Kim, Dae-Won Kim, Sung Ho Her, Sang-Gon Lee, George C.M. Siontis
PLOS ONE.2018; 13(12): e0207889. CrossRef - Letter: Efficacy of Moderate Intensity Statins in the Treatment of Dyslipidemia in Korean Patients with Type 2 Diabetes Mellitus (Diabetes Metab J 2017;41:23-30)
Jae-Han Jeon
Diabetes & Metabolism Journal.2017; 41(2): 150. CrossRef - Response: Efficacy of Moderate Intensity Statins in the Treatment of Dyslipidemia in Korean Patients with Type 2 Diabetes Mellitus (Diabetes Metab J 2017;41:23-30)
Sung Hye Kong, Bo Kyung Koo, Min Kyong Moon
Diabetes & Metabolism Journal.2017; 41(2): 152. CrossRef
- Effect of combining evolocumab with statin on carotid intraplaque neovascularization in patients with premature coronary artery disease (EPOCH)
- Obesity and Metabolic Syndrome
- Statins Increase Mitochondrial and Peroxisomal Fatty Acid Oxidation in the Liver and Prevent Non-Alcoholic Steatohepatitis in Mice
- Han-Sol Park, Jung Eun Jang, Myoung Seok Ko, Sung Hoon Woo, Bum Joong Kim, Hyun Sik Kim, Hye Sun Park, In-Sun Park, Eun Hee Koh, Ki-Up Lee
- Diabetes Metab J. 2016;40(5):376-385. Published online April 5, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.5.376
- 6,299 View
- 85 Download
- 63 Web of Science
- 126 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Non-alcoholic fatty liver disease is the most common form of chronic liver disease in industrialized countries. Recent studies have highlighted the association between peroxisomal dysfunction and hepatic steatosis. Peroxisomes are intracellular organelles that contribute to several crucial metabolic processes, such as facilitation of mitochondrial fatty acid oxidation (FAO) and removal of reactive oxygen species through catalase or plasmalogen synthesis. Statins are known to prevent hepatic steatosis and non-alcoholic steatohepatitis (NASH), but underlying mechanisms of this prevention are largely unknown.
Methods Seven-week-old C57BL/6J mice were given normal chow or a methionine- and choline-deficient diet (MCDD) with or without various statins, fluvastatin, pravastatin, simvastatin, atorvastatin, and rosuvastatin (15 mg/kg/day), for 6 weeks. Histological lesions were analyzed by grading and staging systems of NASH. We also measured mitochondrial and peroxisomal FAO in the liver.
Results Statin treatment prevented the development of MCDD-induced NASH. Both steatosis and inflammation or fibrosis grades were significantly improved by statins compared with MCDD-fed mice. Gene expression levels of peroxisomal proliferator-activated receptor α (PPARα) were decreased by MCDD and recovered by statin treatment. MCDD-induced suppression of mitochondrial and peroxisomal FAO was restored by statins. Each statin's effect on increasing FAO and improving NASH was independent on its effect of decreasing cholesterol levels.
Conclusion Statins prevented NASH and increased mitochondrial and peroxisomal FAO via induction of PPARα. The ability to increase hepatic FAO is likely the major determinant of NASH prevention by statins. Improvement of peroxisomal function by statins may contribute to the prevention of NASH.
-
Citations
Citations to this article as recorded by- Organelle stress and alterations in interorganelle crosstalk during liver fibrosis
Saloni Sinha, Nora Hassan, Robert E. Schwartz
Hepatology.2024; 79(2): 482. CrossRef - Statin therapy: a potential adjuvant to immunotherapies in hepatocellular carcinoma
Jiao Wang, Chengyu Liu, Ronghua Hu, Licheng Wu, Chuanzhou Li
Frontiers in Pharmacology.2024;[Epub] CrossRef - Recent Progress in Anti‐Tumor Nanodrugs Based on Tumor Microenvironment Redox Regulation
Lan Yao, Xiang Zhu, Yunyi Shan, Liang Zhang, Jing Yao, Hui Xiong
Small.2024;[Epub] CrossRef - Exploration of the Key Genes Involved in Non-alcoholic Fatty Liver Disease and Possible MicroRNA Therapeutic Targets
Ali Mahmoudi, Amin Jalili, Alexandra E. Butler, Seyed H. Aghaee-Bakhtiari, Tannaz Jamialahmadi, Amirhossein Sahebkar
Journal of Clinical and Experimental Hepatology.2024; 14(4): 101365. CrossRef - Inflammation drives pathogenesis of early intestinal failure-associated liver disease
Scott C. Fligor, Savas T. Tsikis, Thomas I. Hirsch, Ashish Jain, Liang Sun, Shira Rockowitz, Kathleen M. Gura, Mark Puder
Scientific Reports.2024;[Epub] CrossRef - A Systematic Review of Statins for the Treatment of Nonalcoholic Steatohepatitis: Safety, Efficacy, and Mechanism of Action
Shiqin Zhang, Xiaoling Ren, Bingzheng Zhang, Tian Lan, Bing Liu
Molecules.2024; 29(8): 1859. CrossRef - Effects of metformin and simvastatin treatment on ultrastructural features of liver macrophages in HFD mice
Darko Ciric, Tamara Kravic-Stevovic, Vladimir Bumbasirevic, Sasa Petricevic, Sofija Jovanovic, Vladimir Trajkovic, Tamara Martinovic
Ultrastructural Pathology.2023; 47(1): 1. CrossRef - Statins for the Treatment of Nonalcoholic Fatty Liver Disease and Nonalcoholic Steatohepatitis: A Systematic Review and Meta-Analysis
Weiwei Dai, Baohong Xu, Peng Li, Junhua Weng
American Journal of Therapeutics.2023; 30(1): e17. CrossRef - Atorvastatin Attenuates Diet-Induced Non-Alcoholic Steatohepatitis in APOE*3-Leiden Mice by Reducing Hepatic Inflammation
José A. Inia, Geurt Stokman, Elsbet J. Pieterman, Martine C. Morrison, Aswin L. Menke, Lars Verschuren, Martien P. M. Caspers, Martin Giera, J. Wouter Jukema, Anita M. van den Hoek, Hans M. G. Princen
International Journal of Molecular Sciences.2023; 24(9): 7818. CrossRef - The interplay between nonalcoholic fatty liver disease and atherosclerotic cardiovascular disease
Alexandra C. Finney, Sandeep Das, Dhananjay Kumar, M. Peyton McKinney, Bishuang Cai, Arif Yurdagul, Oren Rom
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Serum metabolomic signatures of fatty acid oxidation defects differentiate host-response subphenotypes of acute respiratory distress syndrome
Tomeka L. Suber, Stacy G. Wendell, Steven J. Mullett, Benjamin Zuchelkowski, William Bain, Georgios D. Kitsios, Bryan J. McVerry, Prabir Ray, Anuradha Ray, Rama K. Mallampalli, Yingze Zhang, Faraaz Shah, Seyed Mehdi Nouraie, Janet S. Lee
Respiratory Research.2023;[Epub] CrossRef - Statins on nonalcoholic fatty liver disease: A systematic review and meta-analysis of 14 RCTs
Haiyan Zhou, Maeda Toshiyoshi,, Wenli Zhao, Ye Zhao, Yan Zhao,
Medicine.2023; 102(26): e33981. CrossRef - Atorvastatin rescues hyperhomocysteinemia-induced cognitive deficits and neuroinflammatory gene changes
Erica M. Weekman, Sherika N. Johnson, Colin B. Rogers, Tiffany L. Sudduth, Kevin Xie, Qi Qiao, David W. Fardo, Teodoro Bottiglieri, Donna M. Wilcock
Journal of Neuroinflammation.2023;[Epub] CrossRef - Crosstalk between Lipids and Non-Alcoholic Fatty Liver Disease
Divyavani Gowda, Chandra Shekhar, Siddabasave Gowda B. Gowda, Yifan Chen, Shu-Ping Hui
Livers.2023; 3(4): 687. CrossRef - Empagliflozin: Potential Protective Effects on Hepatocytes and Liver Outcomes in Streptozotocin -Diabetic Rats.
Alia Khwaldeh, Nour Al-Sawalha, Shefa' Aljabali, Ziad Shraideh, Sokiyna Ababneh, Roba Bdeir
Biomedical and Pharmacology Journal.2023; 16(4): 2123. CrossRef - Is there a role of lipid-lowering therapies in the management of fatty liver disease?
Ismini Tzanaki, Aris P Agouridis, Michael S Kostapanos
World Journal of Hepatology.2022; 14(1): 119. CrossRef - Bifidobacterium animalis subsp. lactis A6 Enhances Fatty Acid β-Oxidation of Adipose Tissue to Ameliorate the Development of Obesity in Mice
Yanxiong Huo, Guoping Zhao, Jinwang Li, Ran Wang, Fazheng Ren, Yixuan Li, Xiaoyu Wang
Nutrients.2022; 14(3): 598. CrossRef - PharmOmics: A species- and tissue-specific drug signature database and gene-network-based drug repositioning tool
Yen-Wei Chen, Graciel Diamante, Jessica Ding, Thien Xuan Nghiem, Jessica Yang, Sung-Min Ha, Peter Cohn, Douglas Arneson, Montgomery Blencowe, Jennifer Garcia, Nima Zaghari, Paul Patel, Xia Yang
iScience.2022; 25(4): 104052. CrossRef - Pleyotropic Effects of Statins Non-Alcoholic Fat Disease of the Liver Non-Alcoholic Steatohepatitis
И.Р. Агабабян, Ш.Ш. Садыкова
Рецепт.2022; (2): 194. CrossRef - PPAR Alpha as a Metabolic Modulator of the Liver: Role in the Pathogenesis of Nonalcoholic Steatohepatitis (NASH)
Simona Todisco, Anna Santarsiero, Paolo Convertini, Giulio De Stefano, Michele Gilio, Vito Iacobazzi, Vittoria Infantino
Biology.2022; 11(5): 792. CrossRef - Association between organochlorine pesticides and nonalcoholic fatty liver disease in the National Health and Nutrition Examination Survey 2003–2004
Hyunji Sang, Kyu-Na Lee, Chang Hee Jung, Kyungdo Han, Eun Hee Koh
Scientific Reports.2022;[Epub] CrossRef - Integrating the contributions of mitochondrial oxidative metabolism to lipotoxicity and inflammation in NAFLD pathogenesis
Curtis C. Hughey, Patrycja Puchalska, Peter A. Crawford
Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids.2022; 1867(11): 159209. CrossRef - Supplementation of Lycium barbarum Polysaccharide Combined with Aerobic Exercise Ameliorates High-Fat-Induced Nonalcoholic Steatohepatitis via AMPK/PPARα/PGC-1α Pathway
Dou-Dou Li, Jia-Min Ma, Ming-Jing Li, Lu-Lu Gao, Yan-Na Fan, Yan-Nan Zhang, Xiu-Juan Tao, Jian-Jun Yang
Nutrients.2022; 14(15): 3247. CrossRef - Targeted therapeutics and novel signaling pathways in non-alcohol-associated fatty liver/steatohepatitis (NAFL/NASH)
Xiaohan Xu, Kyle L. Poulsen, Lijuan Wu, Shan Liu, Tatsunori Miyata, Qiaoling Song, Qingda Wei, Chenyang Zhao, Chunhua Lin, Jinbo Yang
Signal Transduction and Targeted Therapy.2022;[Epub] CrossRef - Regulation of Hepatic Lipid and Glucose Metabolism by INSP3R1
Rachel J. Perry
Diabetes.2022; 71(9): 1834. CrossRef - Effects of SLCO1B1 Genetic Variant on Metabolite Profile in Participants on Simvastatin Treatment
Lilian Fernandes Silva, Rowmika Ravi, Jagadish Vangipurapu, Anniina Oravilahti, Markku Laakso
Metabolites.2022; 12(12): 1159. CrossRef - Acute and chronic effects of environmental realistic concentrations of simvastatin in danio rerio: evidences of oxidative alterations and endocrine disruptive activity
D. Rebelo, A.T. Correia, B. Nunes
Environmental Toxicology and Pharmacology.2021; 81: 103522. CrossRef - Allopurinol ameliorates high fructose diet induced hepatic steatosis in diabetic rats through modulation of lipid metabolism, inflammation, and ER stress pathway
In-Jin Cho, Da-Hee Oh, Jin Yoo, You-Cheol Hwang, Kyu Jeung Ahn, Ho-Yeon Chung, Soung Won Jeong, Ju-Young Moon, Sang-Ho Lee, Sung-Jig Lim, In-Kyung Jeong
Scientific Reports.2021;[Epub] CrossRef - Atorvastatin Modulates Bile Acid Homeostasis in Mice with Diet-Induced Nonalcoholic Steatohepatitis
Hana Lastuvkova, Fatemeh Alaei Faradonbeh, Jolana Schreiberova, Milos Hroch, Jaroslav Mokry, Hana Faistova, Zuzana Nova, Radomír Hyspler, Ivone Cristina Igreja Sa, Petr Nachtigal, Alzbeta Stefela, Petr Pavek, Stanislav Micuda
International Journal of Molecular Sciences.2021; 22(12): 6468. CrossRef - PPARs as Metabolic Sensors and Therapeutic Targets in Liver Diseases
Hugo Christian Monroy-Ramirez, Marina Galicia-Moreno, Ana Sandoval-Rodriguez, Alejandra Meza-Rios, Arturo Santos, Juan Armendariz-Borunda
International Journal of Molecular Sciences.2021; 22(15): 8298. CrossRef - Simvastatin affects the PPARα signaling pathway and causes oxidative stress and embryonic development interference in Mugilogobius abei
Chao Wang, Tianli Tang, Yimeng Wang, Xiangping Nie, Kaibin Li
Aquatic Toxicology.2021; 239: 105951. CrossRef - Impact of statin use on the risk and prognosis of hepatocellular carcinoma: a meta-analysis
Jianfeng Wang, Xiaogang Li
European Journal of Gastroenterology & Hepatology.2021; 33(12): 1603. CrossRef - Statins in Non-alcoholic Steatohepatitis
Jose D. Torres-Peña, Laura Martín-Piedra, Francisco Fuentes-Jiménez
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Comparison of the liver findings after simvastatin-treatment between Spontaneously Diabetic Torii-Leprfa (SDT fatty) rats and Sprague-Dawley rats
Tadakazu Takahashi, Yusuke Suzuki, Naohito Yamada, Kaoru Toyoda, Keisuke Goda, Katsunori Ryoke, Chizuru Matsuura, Akio Kobayashi, Shoichiro Sugai, Kayoko Shimoi
Fundamental Toxicological Sciences.2020; 7(1): 41. CrossRef - Current and emerging pharmacotherapeutic interventions for the treatment of liver fibrosis
Joeri Lambrecht, Leo A. van Grunsven, Frank Tacke
Expert Opinion on Pharmacotherapy.2020; 21(13): 1637. CrossRef - The Influence of Statins on the Aerobic Metabolism of Endothelial Cells
Izabela Broniarek, Karolina Dominiak, Lukasz Galganski, Wieslawa Jarmuszkiewicz
International Journal of Molecular Sciences.2020; 21(4): 1485. CrossRef - NADPH Oxidase Inhibition in Fibrotic Pathologies
Karen Bernard, Victor J. Thannickal
Antioxidants & Redox Signaling.2020; 33(6): 455. CrossRef - Pleiotropic Effects of Statins in the Light of Non-Alcoholic Fatty Liver Disease and Non-Alcoholic Steatohepatitis
Farah Ahsan, Federico Oliveri, Harshit K Goud, Zainab Mehkari, Lubna Mohammed, Moiz Javed, Aldanah Althwanay, Ian H Rutkofsky
Cureus.2020;[Epub] CrossRef - Peroxisomal footprint in the pathogenesis of nonalcoholic steatohepatitis
S.M. Touhidul Islam, Jeseong Won, Mushfiquddin Khan, Kenneth D. Chavin, Inderjit Singh
Annals of Hepatology.2020; 19(5): 466. CrossRef - Structural Basis for Activation of Human Sirtuin 6 by Fluvastatin
Weijie You, Clemens Steegborn
ACS Medicinal Chemistry Letters.2020; 11(11): 2285. CrossRef - Specificity of transaminase activities in the prediction of drug-induced hepatotoxicity
Akio Kobayashi, Yusuke Suzuki, Shoichiro Sugai
The Journal of Toxicological Sciences.2020; 45(9): 515. CrossRef - Disease-associated gut microbiome and metabolome changes in patients with chronic obstructive pulmonary disease
Kate L. Bowerman, Saima Firdous Rehman, Annalicia Vaughan, Nancy Lachner, Kurtis F. Budden, Richard Y. Kim, David L. A. Wood, Shaan L. Gellatly, Shakti D. Shukla, Lisa G. Wood, Ian A. Yang, Peter A. Wark, Philip Hugenholtz, Philip M. Hansbro
Nature Communications.2020;[Epub] CrossRef - Simvastatin Reduces Hepatic Oxidative Stress and Endoplasmic Reticulum Stress in Nonalcoholic Steatohepatitis Experimental Model
Graziella Rodrigues, Andrea Janz Moreira, Silvia Bona, Elizângela Schemitt, Cláudio Augusto Marroni, Fábio Cangeri Di Naso, Alexandre Simões Dias, Thienne Rocha Pires, Jaqueline Nascimento Picada, Norma Possa Marroni
Oxidative Medicine and Cellular Longevity.2019; 2019: 1. CrossRef - Impaired Peroxisomal Fitness in Obese Mice, a Vicious Cycle Exacerbating Adipocyte Dysfunction via Oxidative Stress
Lingjuan Piao, Debra Dorotea, Songling Jiang, Eun Hee Koh, Goo Taeg Oh, Hunjoo Ha
Antioxidants & Redox Signaling.2019; 31(18): 1339. CrossRef - (5R)-5-hydroxytriptolide ameliorates liver lipid accumulation by suppressing lipid synthesis and promoting lipid oxidation in mice
Yunxia Dong, Henglei Lu, Qiang Li, Xinming Qi, Yuanchao Li, Zean Zhang, Jing Chen, Jin Ren
Life Sciences.2019; 232: 116644. CrossRef - Simvastatin alleviates bone resorption in apical periodontitis possibly by inhibition of mitophagy‐related osteoblast apoptosis
C.‐N. Yang, S.‐H. Kok, H.‐W. Wang, J. Z.‐C. Chang, E. H.‐H. Lai, C.‐T. Shun, H. Yang, M.‐H. Chen, C.‐Y. Hong, S.‐K. Lin
International Endodontic Journal.2019; 52(5): 676. CrossRef - Different Effects of Pravastatin on Preeclampsia-like Symptoms in Different Mouse Models
Jing Huai, Zi Yang, Yan-Hong Yi, Guang-Jiao Wang
Chinese Medical Journal.2018; 131(4): 461. CrossRef - Ameliorating effects of D-47, a newly developed compound, on lipid metabolism in an animal model of familial hypercholesterolemia (WHHLMI rabbits)
Shohei Tamura, Yui Koike, Hiroaki Takeda, Tomonari Koike, Yoshihiro Izumi, Ryosuke Nagasaka, Tetsuto Tsunoda, Motoo Tori, Kazuo Ogawa, Takeshi Bamba, Masashi Shiomi
European Journal of Pharmacology.2018; 822: 147. CrossRef - Fluvastatin activates sirtuin 6 to regulate sterol regulatory element-binding proteins and AMP-activated protein kinase in HepG2 cells
Ji-Hye Kim, Jun Mi Lee, Jong-Hoon Kim, Kwang Rok Kim
Biochemical and Biophysical Research Communications.2018; 503(3): 1415. CrossRef - Statin use and the risk of hepatocellular carcinoma in patients at high risk: A nationwide nested case-control study
Gyuri Kim, Suk-Yong Jang, Chung Mo Nam, Eun Seok Kang
Journal of Hepatology.2018; 68(3): 476. CrossRef - Membrane Remodeling as a Key Player of the Hepatotoxicity Induced by Co-Exposure to Benzo[a]pyrene and Ethanol of Obese Zebrafish Larvae
Muhammad Imran, Odile Sergent, Arnaud Tête, Isabelle Gallais, Martine Chevanne, Dominique Lagadic-Gossmann, Normand Podechard
Biomolecules.2018; 8(2): 26. CrossRef - Corticosterone-Induced Lipogenesis Activation and Lipophagy Inhibition in Chicken Liver Are Alleviated by Maternal Betaine Supplementation
Yun Hu, Qinwei Sun, Yan Hu, Zhen Hou, Yibo Zong, Nagmeldin A Omer, Halima Abobaker, Ruqian Zhao
The Journal of Nutrition.2018; 148(3): 316. CrossRef - Simvastatin protects against acetaminophen-induced liver injury in mice
Huan Liang, Yang Feng, Ruixia Cui, Minglong Qiu, Jingyao Zhang, Chang Liu
Biomedicine & Pharmacotherapy.2018; 98: 916. CrossRef - Effects of Pitavastatin on Insulin Sensitivity and Liver Fat: A Randomized Clinical Trial
Laurie R Braun, Meghan N Feldpausch, Natalia Czerwonka, Julian Weiss, Karen Branch, Hang Lee, Edgar L Martinez-Salazar, Martin Torriani, Craig A Sponseller, Steven K Grinspoon, Takara L Stanley
The Journal of Clinical Endocrinology & Metabolism.2018; 103(11): 4176. CrossRef - Inactivation of SREBP-1a Phosphorylation Prevents Fatty Liver Disease in Mice: Identification of Related Signaling Pathways by Gene Expression Profiles in Liver and Proteomes of Peroxisomes
Birgit Knebel, Sonja Hartwig, Sylvia Jacob, Ulrike Kettel, Martina Schiller, Waltraud Passlack, Cornelia Koellmer, Stefan Lehr, Dirk Müller-Wieland, Jorg Kotzka
International Journal of Molecular Sciences.2018; 19(4): 980. CrossRef - MicroRNA-124 Regulates Fatty Acid and Triglyceride Homeostasis
Tyler A. Shaw, Ragunath Singaravelu, Megan H. Powdrill, Jordan Nhan, Nadine Ahmed, Dennis Özcelik, John Paul Pezacki
iScience.2018; 10: 149. CrossRef - Liver Disease in Singapore
Mark Muthiah, Chern H Chong, Seng G Lim
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 66. CrossRef - Accelerating Treatment of Skeletal Class II Malocclusion using Fixed Twin Block Appliances
Snigdha Pattanaik, Navya Puvvula, Noorjahan Mohammad
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 146. CrossRef - Effect of a Papain-based Chemomechanical Agent on Structure of Dentin and Bond Strength: Anin vitroStudy
Veena S Pai, Yashwanth Gowda, Sruthi Nair
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 161. CrossRef - Perception of Indian Dental Surgeons regarding Molar Incisor Hypomineralization
Sumita Upadhyay, Jatinder K Dhillon
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 116. CrossRef - Association between Obesity and Oral Health Status in Schoolchildren: A Survey in Five Districts of West Bengal, India
Rahul Kaul, Paras Angrish, Subrata Saha, Sonali Halder, Bhaswar Bhattacharya, Malay Mitra
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 233. CrossRef - Burden of Alcoholic Liver Disease: Bhutan Scenario
Pelden Wangchuk
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 81. CrossRef - Comparative Evaluation of Effects ofTriphala, Garlic Extracts, and Chlorhexidine Mouthwashes on SalivaryStreptococcus mutansCounts and Oral Hygiene Status
Shweta Gupta, Narendra Padiyar, Bharathi Padiyar
International Journal of Clinical Pediatric Dentistry.2018; 11(4): 299. CrossRef - Evaluation of Dentin–Pulp Complex Response after Conservative Clinical Procedures in Primary Teeth
Thais Marchini Oliveira, Bianca Mello, Tassia C Stafuzza, Luciana Vitor, Daniela Rios, Thiago Silva, Maria Machado
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 188. CrossRef - Nonalcoholic Fatty Liver Disease: Time to Take the Bull by the Horns
Preetam Nath, Shivaram P Singh
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 47. CrossRef - F-18 Fluorodeoxyglucose Positron Emission Tomography/ Computed Tomography Findings of Isolated Gastric Tuberculosis mimicking Gastric Cancer and Lymphoma
Remzi A Akdogan, Halil Rakici, Serkan Güngör, Recep Bedir, Elif Akdogan
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 93. CrossRef - Clinical, Radiological, and Histological Assessment of Magnetic Nanoparticles as Pulpotomy Medicament in Primary Molars
Manoj K Mallela, Harivinder R Konyala, Ajay R Mareddy, N Venugopal Reddy, Keerthi P Susheela
International Journal of Clinical Pediatric Dentistry.2018; 11(4): 283. CrossRef - Determination of ABO Blood Groups and Rh Typing from Dry Salivary Samples
Laxmi Lakade, Priyam R Velani
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 100. CrossRef - Orofacial Manifestations of Leukemic Children on Treatment: A Descriptive Study
Keerthilatha M Pai, Aparna Aggarwal
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 193. CrossRef - Mandibular Regional Odontodysplasia in an 8-year-old Boy showing Teeth Disorders, Gubernaculum Tracts, and Altered Bone Fractal Pattern
Davi de Sá Cavalcante, Cristiane SR Fonteles, Thyciana R Ribeiro, Lúcio M Kurita, Alynne Vde M Pimenta, Francisco SR Carvalho, Fábio WG Costa
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 128. CrossRef - Evaluation of Chemokines in the Gingival Crevicular Fluid of Children with Down Syndrome
Harshini Togaru, Veerakishore Kumar Reddy, Naveen K Kommineni, Prathyusha Padakandla, John P Indupalli, Swapna P Nanga
International Journal of Clinical Pediatric Dentistry.2018; 11(4): 288. CrossRef - Hepatitis B Virus Infection among Health Care Workers in Indonesia
David H Muljono, Teguh Wijayadi, Rizalinda Sjahril
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 88. CrossRef - Comparison of the Effectiveness of Probiotic, Chlorhexidine-based Mouthwashes, and Oil Pulling Therapy on Plaque Accumulation and Gingival Inflammation in 10- to 12-year-old Schoolchildren: A Randomized Controlled Trial
Saravana K Kandaswamy, Asokan Sharath, PR Geetha Priya
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 66. CrossRef - Evaluation of Changes in Salivary pH after Intake of Different Eatables and Beverages in Children at Different Time Intervals
Ankit Pachori, Haalaswamy Kambalimath, Garima Bhambhani, Garima Malhotra
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 177. CrossRef - Customized Hybrid Bluegrass Appliance: An Innovative Technique
Ziauddin Mohammad, Apeksha Bagalkotkar, Ashank Mishra, Gopi Veerala
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 141. CrossRef - Postobstructive Cyst Formation in Pancreatic Duct affecting Surgical Approach
Alper Parlakgumus, Ali Ezer
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 99. CrossRef - Validating the Usage of Cariogram in 5- and 12-year-old School-going Children in Paonta Sahib, Himachal Pradesh, India: A 12-month Prospective Study
Manish Madan, Pallav Singhal, Anu Garg, Akash Dupper
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 110. CrossRef - Epidemiology of Chronic Hepatitis B in Turkey
Hasan Ozkan
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 73. CrossRef - A Comparative Evaluation of Time-dependent Changes on the Surface Hardness of Bulk Cure Composites: Anin vitroStudy
Anindita Sarma
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 183. CrossRef - Management of Hepatocellular Carcinoma: Bangladesh Perspective
Mohammad Noor-E-Alam
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 52. CrossRef - Trichobezoar: Ravenous for Hair
Aman Kamra
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 97. CrossRef - Comparative Evaluation of the Fracture Resistance of Two Different Fiber-reinforced Composite Restorations with Particulate Filler Composite Restorations
Vanga V Narasimha Rao, Srinivas K Chandrabhatla, Vabbala R Rajasekhar
International Journal of Clinical Pediatric Dentistry.2018; 11(4): 277. CrossRef - A Comparative Evaluation of Efficacy ofStreptococcus mutansCounts in Saliva: Anin vivoStudy
Inder K Pandit
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 94. CrossRef - Liver Cancer in Nepal
Ananta Shrestha
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 63. CrossRef - Pre-eruptive Intracoronal Radiolucency in First Permanent Molar
Mariana C Ilha, Paulo F Kramer, Simone H Ferreira, Henrique C Ruschel
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 151. CrossRef - Comparative Evaluation of Various Temperature Changes on Stress Distribution in Class II Mesial-occlusal-distal Preparation restored with Different Restorative Materials: A Finite Element Analysis
Binita Srivastava, Neorem N Devi
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 167. CrossRef - A Survey on the Use of Antibiotics among the Dentists of Kolkata, West Bengal, India
Rahul Kaul, Paras Angrish, Subrata Saha, Ashok V Sengupta, Shantanu Mukherjee
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 122. CrossRef - Changing Etiology in Liver Cirrhosis in Sapporo, Japan
Jong-Hon Kang, Takeshi Matsui
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 77. CrossRef - Epidemiology, Genotype Distribution, Prognosis, Control, and Management of Viral Hepatitis B, C, D, and Hepatocellular Carcinoma in Mongolia
Oidov Baatarkhuu, Tsagaantsooj Gerelchimeg, Dashchirev Munkh-Orshikh, Badamnachin Batsukh, Ganbold Sarangua, Jazag Amarsanaa
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 57. CrossRef - Impact of Diabetes Mellitus Type 1 on Lebanese Families’ Quality of Life
Nahla Nassif, Balsam Noueiri
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 61. CrossRef - Pediatric Dental Appointments No-show: Rates and Reasons
Anup Panda, Rupinder Bhatia, Esha C Vora
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 171. CrossRef - A Case of Painless Excision
Rupinder Bhatia, Ipshita A Suyash
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 135. CrossRef - Manuka Honey: A Potent Cariostatic Agent–Anin vitroStudy
Sapna Konde, Javaregowda P Beena, Punyatoya Sahoo, N Sunil Raj, Narayana C Kumar
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 105. CrossRef - Reviewing of Research Finding of Hepatitis B Virus Infection in Lao People's Democratic Republic
Angkham Ounavong
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 75. CrossRef - Nonalcoholic Fatty Liver Disease: Identifying the Disease Burden in Sri Lanka
Anuradha S Dassanayake
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 69. CrossRef - Comparative Evaluation of Microhardness by Common Drinks on Esthetic Restorative Materials and Enamel: Anin vitroStudy
Manish Madan, Akash Dupper, Roli Gupta, Trilok Kainthla
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 155. CrossRef - Hepatocellular Carcinoma Surveillance: Benefit of Serum Alfa-fetoprotein in Real-world Practice
Patharapan Lersritwimanmaen, Supot Nimanong
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 83. CrossRef - Body Mass Index and Dental Caries: A Systematic Review
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 228. CrossRef - Evaluation of Surgical Options for Supernumerary Teeth in the Anterior Maxilla
Gianluca Porcaro, Luca Mirabelli, Ernesto Amosso
International Journal of Clinical Pediatric Dentistry.2018; 11(4): 294. CrossRef - A Comparative Study to evaluate Parent's Ability to assess Dental Fear in their 6- to 10-year-old Children using Children's Fear Survey Schedule—Dental Subscale
Ritika Malhotra, Anchal Sahni
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 205. CrossRef - Estimation of Salivary Glucose, Calcium, Phosphorus, Alkaline Phosphatase, and Immunoglobulin A among Diabetic and Nondiabetic Children: A Case–Control Study
Kalyani Uppu, Suzan Sahana, Ghanashyam P Madu, Aron AK Vasa, Sowjanya Nalluri
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 71. CrossRef - Pedodontic Considerations in a Child with Attention Deficit Hyperactivity Disorder: Literature Review and a Case Report
Siddhi Sinha, Prasanna Praveen, S Prathibha Rani, Athimuthu Anantharaj
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 254. CrossRef - Salivary Cortisol and Alpha-amylase—Biomarkers of Stress in Children undergoing Extraction: Anin vivoStudy
Neha Agarwal, Shefali Chaturvedy, Saurabh Chaturvedi, Yogita Chaturvedi
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 214. CrossRef - Influence of Storage Media and Duration of Fragment in the Media on the Bond Strength of the Reattached Tooth Fragment
Prashant Jalannavar
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 83. CrossRef - Comparative Evaluation of Mucosal Vibrator with Topical Anesthetic Gel to reduce Pain during Administration of Local Anesthesia in Pediatric Patients: Anin vivoStudy
Mahima Gandhi, Garima Kalia, Khushboo Rathore
International Journal of Clinical Pediatric Dentistry.2018; 11(4): 261. CrossRef - Management of Autistic Patients in Dental Office: A Clinical Update
Jyothi S Bommangoudar
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 219. CrossRef - Foreign Body causing Displacement of Immature Fractured Apical Root Fragment: An Unusual Case Report
Aman Moda, Rajesh Singla, Preeti M Agrawal
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 247. CrossRef - Validity and Reliability of the Hindi Version of the Modified Child Perceptions Questionnaire 11 to 14
Mohit Sharma, Prasanna Kumar, Dempsy CM Mandanna
International Journal of Clinical Pediatric Dentistry.2018; 11(4): 271. CrossRef - Nonsyndromic Gingival Fibromatosis: A Rare Case Report
Mahima Gandhi, Akshat Vijay
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 250. CrossRef - Prevalence of Deleterious Oral Habits among 3- to 5-yearold Preschool Children in Bhubaneswar, Odisha, India
Brahmananda Dutta, Tulika Verma
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 210. CrossRef - Evaluation of Antimicrobial Activity of Two Endodontic Sealers: Zinc Oxide with Thyme Oil and Zinc Oxide Eugenol against Root Canal Microorganisms—Anin vitroStudy
Manoj Chandak, Nilima Thosar, Silpi Basak
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 79. CrossRef - Prevalence and Risk Factors for Dental Caries among Preschool Children: A Cross-sectional Study in Eastern India
Vinay K Chugh, Kushal K Sahu, Ankita Chugh
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 238. CrossRef - Squamous Papilloma on Hard Palate: Case Report and Literature Review
Penmatsa Chaitanya, Satyam Martha, Ramachandran Punithvathy, Madhusudhan Reddy
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 244. CrossRef - Comparison of Vitamin D Level of Children with Severe Early Childhood Caries and Children with No Caries
Anchal Chhonkar, Vishal Arya
International Journal of Clinical Pediatric Dentistry.2018; 11(3): 199. CrossRef - Use of “Surface Analyzer” to evaluate the Effect of Two Polishing Systems on Surface Texture of Four Newer Composites
Shefally Garg, Munish Goel, Shweta Verma, Nanika Mahajan, Bhawna Kaul, Vikas Garg
International Journal of Clinical Pediatric Dentistry.2018; 11(4): 266. CrossRef - Clinical Evaluation of Preventive Effect of Fissure Sealants on Initial Carious Lesion of Permanent Mandibular Molars Pretreated with and without Fluoride Varnish by Fluorescence Camera
Madhagudanahalli S Lakshmi, Kudlapur T Srilatha, Bhojraj Nandlal, Seema Deshmukh
International Journal of Clinical Pediatric Dentistry.2018; 11(2): 89. CrossRef - Hepatocellular Carcinoma in Malaysia and Its Changing Trend
Rosmawati Mohamed, Ruksana Raihan, Amirah Azzeri, Fatiha H Shabaruddin
Euroasian Journal of Hepato-Gastroenterology.2018; 8(1): 54. CrossRef - Advances in the Understanding and Treatment of Mitochondrial Fatty Acid Oxidation Disorders
Eric S. Goetzman
Current Genetic Medicine Reports.2017; 5(3): 132. CrossRef - Hepatokines: linking nonalcoholic fatty liver disease and insulin resistance
Ruth C. R. Meex, Matthew J. Watt
Nature Reviews Endocrinology.2017; 13(9): 509. CrossRef - In ovo injection of betaine alleviates corticosterone-induced fatty liver in chickens through epigenetic modifications
Yun Hu, Qinwei Sun, Jie Liu, Yimin Jia, Demin Cai, Abdulrahman A. Idriss, Nagmeldin A. Omer, Ruqian Zhao
Scientific Reports.2017;[Epub] CrossRef - The therapeutic effect of silymarin in the treatment of nonalcoholic fatty disease
Sheng Zhong, Yuxiang Fan, Qi Yan, Xingyu Fan, Bo Wu, Yujuan Han, Ying Zhang, Yong Chen, Huimao Zhang, Junqi Niu
Medicine.2017; 96(49): e9061. CrossRef - Atorvastatin reduces lipid accumulation in the liver by activating protein kinase A-mediated phosphorylation of perilipin 5
Xing Gao, Yang Nan, Yuanlin Zhao, Yuan Yuan, Bincheng Ren, Chao Sun, Kaiyu Cao, Ming Yu, Xuyang Feng, Jing Ye
Biochimica et Biophysica Acta (BBA) - Molecular and Cell Biology of Lipids.2017; 1862(12): 1512. CrossRef - Aerobic capacity mediates susceptibility for the transition from steatosis to steatohepatitis
E. Matthew Morris, Colin S. McCoin, Julie A. Allen, Michelle L. Gastecki, Lauren G. Koch, Steven L. Britton, Justin A. Fletcher, Xiarong Fu, Wen‐Xing Ding, Shawn C. Burgess, R. Scott Rector, John P. Thyfault
The Journal of Physiology.2017; 595(14): 4909. CrossRef - Use of Statins in Patients with Chronic Liver Disease and Cirrhosis: Current Views and Prospects
Jose Ignacio Vargas, Marco Arrese, Vijay H. Shah, Juan Pablo Arab
Current Gastroenterology Reports.2017;[Epub] CrossRef - Endogenous catalase delays high-fat diet-induced liver injury in mice
Lingjuan Piao, Jiyeon Choi, Guideock Kwon, Hunjoo Ha
The Korean Journal of Physiology & Pharmacology.2017; 21(3): 317. CrossRef - Clinical implications of understanding the association between oxidative stress and pediatric NAFLD
Jake P. Mann, Massimiliano Raponi, Valerio Nobili
Expert Review of Gastroenterology & Hepatology.2017; 11(4): 371. CrossRef
- Organelle stress and alterations in interorganelle crosstalk during liver fibrosis
- Others
- Effect of Atorvastatin on Growth Differentiation Factor-15 in Patients with Type 2 Diabetes Mellitus and Dyslipidemia
- Ji Min Kim, Min Kyung Back, Hyon-Seung Yi, Kyong Hye Joung, Hyun Jin Kim, Bon Jeong Ku
- Diabetes Metab J. 2016;40(1):70-78. Published online February 19, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.1.70
- 4,190 View
- 33 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Elevated serum levels of growth differentiation factor-15 (GDF-15) are associated with type 2 diabetes. Therefore, the effects of atorvastatin on metabolic parameters and GDF-15 levels in patients with type 2 diabetes and dyslipidemia were evaluated.
Methods In this prospective randomized trial from February 2013 to March 2014, 50 consecutive type 2 diabetic patients with a low density lipoprotein cholesterol (LDL-C) levels ≥100 mg/dL were enrolled. The patients were divided into two groups based on the amount of atorvastatin prescribed, 10 mg/day (
n =23) or 40 mg/day (n =27). The effect of atorvastatin on metabolic parameters, including lipid profiles and GDF-15 levels, at baseline and after 8 weeks of treatment were compared.Results The baseline metabolic parameters and GDF-15 levels were not significantly different between the two groups. After 8 weeks of treatment, the total cholesterol (TC) and LDL-C levels were significantly decreased in both groups. The mean changes in TC and LDL-C levels were more significant in the 40 mg atorvastatin group. The GDF-15 level was decreased in the 10 mg atorvastatin group, from 1,460.6±874.8 to 1,451.0±770.8 pg/mL, and was increased in the 40 mg atorvastatin group, from 1,271.6±801.0 to 1,341.4±855.2 pg/mL. However, the change in the GDF-15 level was not statistically significant in the 10 or 40 mg atorvastatin group (
P =0.665 andP =0.745, respectively).Conclusion The GDF-15 levels were not significantly changed after an 8-week treatment with atorvastatin in type 2 diabetic patients.
-
Citations
Citations to this article as recorded by- The relationship of Growth differentiation factor-15 with renal damage and dyslipidemia in non-albuminuric and albuminuric Type-2 Diabetes Mellitus
Hasan Esat Yücel, Bilal İlanbey
Medical Science and Discovery.2022; 9(6): 334. CrossRef - Comparative effectiveness of statins on non-high density lipoprotein cholesterol in people with diabetes and at risk of cardiovascular disease: systematic review and network meta-analysis
Alexander Hodkinson, Dialechti Tsimpida, Evangelos Kontopantelis, Martin K Rutter, Mamas A Mamas, Maria Panagioti
BMJ.2022; : e067731. CrossRef - The Cytokine Growth Differentiation Factor-15 and Skeletal Muscle Health: Portrait of an Emerging Widely Applicable Disease Biomarker
Boel De Paepe
International Journal of Molecular Sciences.2022; 23(21): 13180. CrossRef - Biomarkers of subclinical atherosclerosis in patients with psoriasis
Hannah Kaiser, Xing Wang, Amanda Kvist-Hansen, Martin Krakauer, Peter Michael Gørtz, Benjamin D. McCauley, Lone Skov, Christine Becker, Peter Riis Hansen
Scientific Reports.2021;[Epub] CrossRef - Growth differentiation factor-15 regulates oxLDL-induced lipid homeostasis and autophagy in human macrophages
Kathrin Ackermann, Gabriel A. Bonaterra, Ralf Kinscherf, Anja Schwarz
Atherosclerosis.2019; 281: 128. CrossRef
- The relationship of Growth differentiation factor-15 with renal damage and dyslipidemia in non-albuminuric and albuminuric Type-2 Diabetes Mellitus
- The Association of Serum Cystatin C with Glycosylated Hemoglobin in Korean Adults
- Eun Hee Sim, Hye Won Lee, Hyun Ju Choi, Dong Wook Jeong, Seok Man Son, Yang Ho Kang
- Diabetes Metab J. 2016;40(1):62-69. Published online November 27, 2015
- DOI: https://doi.org/10.4093/dmj.2016.40.1.62
- 3,307 View
- 33 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Cystatin C has been known to be associated not only with early renal impairment but also with the incidence of diabetic conditions (prediabetes plus diabetes). However, it is not clear whether cystatin C levels are associated with the prevalence of diabetic conditions in Asian populations. We evaluated this association using glycosylated hemoglobin (HbA1c) levels as the definition of diabetes in Korean adults.
Methods We analyzed data from 1,559 Korean adults (937 men and 622 women) with available serum cystatin C and HbA1c values.
Results The serum cystatin C levels in subjects with prediabetes and diabetes were significantly increased (0.91±0.14 mg/L in prediabetes and 0.91±0.17 mg/L in diabetes vs. 0.88±0.13 mg/L in patients with normal glucose levels,
P =0.001). At increasing cystatin C levels, the prevalence of subjects with prediabetes (30.2% vs. 14.6%,P <0.001) and those with diabetes (10.6% vs. 8.0%,P <0.001) significantly increased in the group with the highest cystatin C levels. The group with the highest cystatin C levels had a significantly increased odds ratio (OR) for the presence of diabetic conditions compared to the group with the lowest values in total subjects (OR, 2.35; 95% confidence interval [CI], 1.54 to 3.58;P <0.001) and in women (OR, 4.13; 95% CI, 1.97 to 8.65;P <0.001), though there was no significant increase after adjusting for multiple variables.Conclusions Higher levels of serum cystatin C are associated with an increased prevalence of diabetic conditions in Korean adults. Our findings may extend the positive association of cystatin C with diabetes incidence to an Asian population.
-
Citations
Citations to this article as recorded by- Prognostic significance of serum cystatin C in acute brainstem infarctions patients
H. Li, B. Zhang, Z. Huang, H. Wu, B. Qin, L. Zhou, Z. Lu, F. Qin
Revue Neurologique.2024;[Epub] CrossRef - Cardiovascular risk assessment in prediabetic patients in a hypertensive population: The role of cystatin C
Rafael Garcia-Carretero, Luis Vigil-Medina, Inmaculada Mora-Jimenez, Cristina Soguero-Ruiz, Rebeca Goya-Esteban, Javier Ramos-Lopez, Oscar Barquero-Perez
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2018; 12(5): 625. CrossRef - Characteristics of Dapagliflozin Responders: A Longitudinal, Prospective, Nationwide Dapagliflozin Surveillance Study in Korea
Eugene Han, Ari Kim, Sung Jae Lee, Je-Yon Kim, Jae Hyeon Kim, Woo Je Lee, Byung-Wan Lee
Diabetes Therapy.2018; 9(4): 1689. CrossRef - Cystatin C as a Predictor for Diabetes according to Glycosylated Hemoglobin Levels in Korean Patients
Eon Ju Jeon, Ji Hyun Lee
Diabetes & Metabolism Journal.2016; 40(1): 32. CrossRef - Prevalence of Reduced Kidney Function by Estimated Glomerular Filtration Rate Using an Equation Based on Creatinine and Cystatin C in Metabolic Syndrome and Its Components in Korean Adults
Yang Ho Kang, Dong Wook Jeong, Seok Man Son
Endocrinology and Metabolism.2016; 31(3): 446. CrossRef - Letter: The Association of Serum Cystatin C with Glycosylated Hemoglobin in Korean Adults (Diabetes Metab J 2016;40:62-9)
Kyung-Soo Kim
Diabetes & Metabolism Journal.2016; 40(2): 171. CrossRef - Response: The Association of Serum Cystatin C with Glycosylated Hemoglobin in Korean Adults (Diabetes Metab J 2016;40:62-9)
Yang Ho Kang
Diabetes & Metabolism Journal.2016; 40(2): 173. CrossRef
- Prognostic significance of serum cystatin C in acute brainstem infarctions patients
- Interaction between Glucose and Lipid Metabolism: More than Diabetic Dyslipidemia
- Klaus G. Parhofer
- Diabetes Metab J. 2015;39(5):353-362. Published online October 22, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.5.353
- 11,269 View
- 261 Download
- 241 Web of Science
- 237 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Glucose and lipid metabolism are linked to each other in many ways. The most important clinical manifestation of this interaction is diabetic dyslipidemia, characterized by elevated triglycerides, low high density lipoprotein cholesterol (HDL-C), and predominance of small-dense LDL particles. However, in the last decade we have learned that the interaction is much more complex. Hypertriglyceridemia and low HDL-C cannot only be the consequence but also the cause of a disturbed glucose metabolism. Furthermore, it is now well established that statins are associated with a small but significant increase in the risk for new onset diabetes. The underlying mechanisms are not completely understood but modulation of 3-hydroxy-3-methylglutaryl-coenzyme A (HMG CoA)-reductase may play a central role as genetic data indicate that mutations resulting in lower HMG CoA-reductase activity are also associated with obesity, higher glucose concentrations and diabetes. Very interestingly, this statin induced increased risk for new onset type 2 diabetes is not detectable in subjects with familial hypercholesterolemia. Furthermore, patients with familial hypercholesterolemia seem to have a lower risk for type 2 diabetes, a phenomenon which seems to be dose-dependent (the higher the low density lipoprotein cholesterol, the lower the risk). Whether there is also an interaction between lipoprotein(a) and diabetes is still a matter of debate.
-
Citations
Citations to this article as recorded by- Response surface methodology based development of an optimized polyherbal formulation and evaluation of its anti-diabetic and anti-obesity potential in high-fat diet-induced obese mice
Tanisha, Sunil Venkategowda, Mala Majumdar
Journal of Traditional and Complementary Medicine.2024; 14(1): 70. CrossRef - Combined untargeted and targeted lipidomics approaches reveal potential biomarkers in type 2 diabetes mellitus cynomolgus monkeys
Chao‐Yang Tian, Qun‐Hui Yang, Hai‐Zhou Lv, Feng Yue, Fei‐Fan Zhou
Journal of Medical Primatology.2024;[Epub] CrossRef - Aging Hallmarks and Progression and Age-Related Diseases: A Landscape View of Research Advancement
Rumiana Tenchov, Janet M. Sasso, Xinmei Wang, Qiongqiong Angela Zhou
ACS Chemical Neuroscience.2024; 15(1): 1. CrossRef - Premorbid lipid levels and long-term risk of ALS—a population-based cohort study
Anders Myhre Vaage, Jūratė Šaltytė Benth, Haakon E. Meyer, Trygve Holmøy, Ola Nakken
Amyotrophic Lateral Sclerosis and Frontotemporal Degeneration.2024; 25(3-4): 358. CrossRef - Astaxanthin as a metabolic regulator of glucose and lipid homeostasis
Alessandro Medoro, Mariano Intrieri, Daniela Passarella, Donald Craig Willcox, Sergio Davinelli, Giovanni Scapagnini
Journal of Functional Foods.2024; 112: 105937. CrossRef - Gum acacia dietary fiber: Significance in immunomodulation, inflammatory diseases, and cancer
Srikanth Barkeer, Ramesh Pothuraju, Pushkar Malakar, Tatiana Colombo Pimentel, Jawed A. Siddiqui, S. Asha Nair
Phytotherapy Research.2024; 38(3): 1509. CrossRef - Exploring clinical indicator variations in stroke patients with multiple risk factors: focus on hypertension and inflammatory reactions
Jiejie Guo, Mei Tian, Yongang Li, Yitong Guo, Ting Zhang, Xuan Liu, Jinze Shen, Lin Zhang, Yueqi Yu, Ling Cao, Haiyan Gu, Yanfang Li, Shiwei Duan, Qinwen Wang
European Journal of Medical Research.2024;[Epub] CrossRef - Effects of Environmental Enrichments on Welfare and Hepatic Metabolic Regulation of Broiler Chickens
Seong W. Kang, Karen D. Christensen, Michael T. Kidd Jr., Sara K. Orlowski
Animals.2024; 14(4): 557. CrossRef - Serum Glycome as a Diagnostic and Prognostic Factor in Gestational Diabetes Mellitus
Ognjen Radojičić, Lucia Pažitná, Zorana Dobrijević, Paras Kundalia, Kristina Kianičková, Jaroslav Katrlík, Vesna Mandić Marković, Željko Miković, Olgica Nedić, Dragana Robajac
Biochemistry (Moscow).2024; 89(1): 148. CrossRef - Antidiabetic activity of methanolic extract of Hibiscus sabdariffa Linn. fruit in alloxan-induced Swiss albino diabetic mice
Shahida Akter, Hanif Ali, Ali A. Shati, Mohammad Y. Alfaifi, Serag Eldin I. Elbehairi, R. Z. Sayyed, Tanzima Yeasmin
Open Agriculture.2024;[Epub] CrossRef - Probiotic Limosilactobacillus reuteri DSM 17938 Changes Foxp3 Deficiency-Induced Dyslipidemia and Chronic Hepatitis in Mice
Erini Nessim Kostandy, Ji Ho Suh, Xiangjun Tian, Beanna Okeugo, Erin Rubin, Sara Shirai, Meng Luo, Christopher M. Taylor, Kang Ho Kim, J. Marc Rhoads, Yuying Liu
Nutrients.2024; 16(4): 511. CrossRef - Sterol Regulatory Element Binding Protein 1: A Mediator for High-Fat Diet–Induced Hepatic Gluconeogenesis and Glucose Intolerance in Fish
Zengqi Zhao, Xiaojun Xiang, Qiang Chen, Jianlong Du, Si Zhu, Xiang Xu, Yanan Shen, Shunlang Wen, Yueru Li, Wei Xu, Kangsen Mai, Qinghui Ai
The Journal of Nutrition.2024;[Epub] CrossRef - Association of METS-IR index with depressive symptoms in US adults: A cross-sectional study
Qi Huang, Denghong Wang, Shanshan Chen, Lei Tang, Chaoyang Ma
Journal of Affective Disorders.2024; 355: 355. CrossRef - Relationships of apolipoprotein E genotypes with a cluster of seven in persons with type 2 diabetes
Douglas E. Barre, Kazimiera A. Mizier-Barre, Odette Griscti, Kevin Hafez
Endocrine Regulations.2024; 58(1): 40. CrossRef - Normal fat intake with high MUFA content and an appropriate SFA/MUFA/PUFA ratio improved the health of rats
Yuhao Zhou, Ligang Yang, Chu Chu, Shiqing Chen, Danwei Yue, Yoong Jun Hao, Guiju Sun, Hui Xia
European Journal of Lipid Science and Technology.2024;[Epub] CrossRef - A Pueraria lobata root extract alleviates high-fat diet-induced non-alcoholic fatty liver disease by modulating the gut microbiota and associated metabolites
Xin Tang, Yongkang Zhou, Fei Liu, Botao Wang, Bingyong Mao, Qiuxiang Zhang, Jianxin Zhao, Wei Chen, Shumao Cui
Food Bioscience.2024; : 103746. CrossRef - The nutritional profile of chia seeds and sprouts: tailoring germination practices for enhancing health benefits-a comprehensive review
Manting Huang, Hui Xu, Qian Zhou, Jianbo Xiao, Yuting Su, Mingfu Wang
Critical Reviews in Food Science and Nutrition.2024; : 1. CrossRef - Model-Assisted Uniformly Honest Inference for Optimal Treatment Regimes in High Dimension
Yunan Wu, Lan Wang, Haoda Fu
Journal of the American Statistical Association.2023; 118(541): 305. CrossRef - Associations of PFAS-related plasma metabolites with cholesterol and triglyceride concentrations
T. Schillemans, I.A. Bergdahl, K. Hanhineva, L. Shi, C. Donat-Vargas, J. Koponen, H. Kiviranta, R. Landberg, A. Åkesson, C. Brunius
Environmental Research.2023; 216: 114570. CrossRef - Physiological mechanisms of TLR4 in glucolipid metabolism regulation: Potential use in metabolic syndrome prevention
Feng Zeng, Jiawei Zheng, Li Shen, Daniela D. Herrera-Balandrano, Wuyang Huang, Zhongquan Sui
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(1): 38. CrossRef - Ferulic acid improves glucose homeostasis by modulation of key diabetogenic activities and restoration of pancreatic architecture in diabetic rats
Veronica F. Salau, Ochuko L. Erukainure, Kolawole O. Olofinsan, Vishal Bharuth, Omamuyovwi M. Ijomone, Md. Shahidul Islam
Fundamental & Clinical Pharmacology.2023; 37(2): 324. CrossRef - Research Progress of TyG Index and IR in Cognitive Impairment of Type 2 Diabetes Mellitus
艳梅 刘
Advances in Clinical Medicine.2023; 13(01): 415. CrossRef - Potential Therapies Targeting the Metabolic Reprogramming of Diabetes-Associated Breast Cancer
Hang Chee Erin Shum, Ke Wu, Jaydutt Vadgama, Yong Wu
Journal of Personalized Medicine.2023; 13(1): 157. CrossRef - Identification of reversible and druggable pathways to improve beta-cell function and survival in Type 2 diabetes
Smithamol Sithara, Tamsyn Crowley, Ken Walder, Kathryn Aston-Mourney
Islets.2023;[Epub] CrossRef - Metabolic Imaging and Molecular Biology Reveal the Interplay between Lipid Metabolism and DHA-Induced Modulation of Redox Homeostasis in RPE Cells
Giada Bianchetti, Maria Elisabetta Clementi, Beatrice Sampaolese, Cassandra Serantoni, Alessio Abeltino, Marco De Spirito, Shlomo Sasson, Giuseppe Maulucci
Antioxidants.2023; 12(2): 339. CrossRef - Quantitative Assessment of Low-Dose Photodynamic Therapy Effects on Diabetic Wound Healing Using Raman Spectroscopy
Hala Zuhayri, Alice A. Samarinova, Alexey V. Borisov, David A. Lopez Guardado, Houssain Baalbaki, Natalya A. Krivova, Yury V. Kistenev
Pharmaceutics.2023; 15(2): 595. CrossRef - Plasma lipidomic profiling reveals metabolic adaptations to pregnancy and signatures of cardiometabolic risk: a preconception and longitudinal cohort study
Li Chen, Sartaj Ahmad Mir, Anne K. Bendt, Esther W. L. Chua, Kothandaraman Narasimhan, Karen Mei-Ling Tan, See Ling Loy, Kok Hian Tan, Lynette P. Shek, Jerry Chan, Fabian Yap, Michael J. Meaney, Shiao-Yng Chan, Yap Seng Chong, Peter D. Gluckman, Johan G.
BMC Medicine.2023;[Epub] CrossRef - Effect of eugenol on lipid profile, oxidative stress, sex hormone, liver injury, ovarian failure, and expression of COX-2 and PPAR-α genes in a rat model of diabetes
Zahra Kokabiyan, Parichehreh Yaghmaei, Seyed Behnamedin Jameie, Zahra Hajebrahimi
Molecular Biology Reports.2023; 50(4): 3669. CrossRef - Role of ferroptosis in pregnancy related diseases and its therapeutic potential
Jinfeng Xu, Fan Zhou, Xiaodong Wang, Chunheng Mo
Frontiers in Cell and Developmental Biology.2023;[Epub] CrossRef - Impact of Fasting Blood Glucose Levels on Blood Pressure Parameters among Older Adults with Prediabetes
Thapanee Roengrit, Ruchada Sri-Amad, Nawiya Huipao, Suphawadee Phababpha, Piyapong Prasertsri, Francesco Giallauria
The Scientific World Journal.2023; 2023: 1. CrossRef - Effect of saffron and fenugreek on lowering blood glucose: A systematic review with meta‐analysis
Alisson Guilherme da Silva Correia, Matheus Batista Alencar, Alexsia Nunes dos Santos, Dayanne Cristina Barreto da Paixão, Flávia Luryane Ferreira Sandes, Brenda Andrade, Yandra Castro, Joseilze Santos de Andrade
Phytotherapy Research.2023; 37(5): 2092. CrossRef - The roles of dietary lipids and lipidomics in gut-brain axis in type 2 diabetes mellitus
Duygu Ağagündüz, Mehmet Arif Icer, Ozge Yesildemir, Tevfik Koçak, Emine Kocyigit, Raffaele Capasso
Journal of Translational Medicine.2023;[Epub] CrossRef - Canagliflozin protects diabetic cardiomyopathy by mitigating fibrosis and preserving the myocardial integrity with improved mitochondrial function
Deepika Dasari, Srashti Gopal Goyal, Anuhya Penmetsa, Dharmarajan Sriram, Arti Dhar
European Journal of Pharmacology.2023; 949: 175720. CrossRef - Dietary fat intakes, lipid profiles, adiposity, inflammation, and glucose in women and men in the Framingham Offspring Cohort
Ioanna Yiannakou, Mengjie Yuan, Xinyi Zhou, Martha R. Singer, Lynn L. Moore
Frontiers in Physiology.2023;[Epub] CrossRef - Neutrophil-to-high-density-lipoprotein-cholesterol ratio and mortality among patients with hepatocellular carcinoma
Ke Shi, Jie Hou, Qun Zhang, Yufei Bi, Xuanwei Zeng, Xianbo Wang
Frontiers in Nutrition.2023;[Epub] CrossRef - Mitochondrial dysfunction in metabolic disorders induced by per- and polyfluoroalkyl substance mixtures in zebrafish larvae
Yingxin Liu, Shuai Liu, Jing Huang, Yu Liu, Qiyu Wang, Jinyuan Chen, Liwei Sun, Wenqing Tu
Environment International.2023; 176: 107977. CrossRef - Association between the insulin resistance marker TyG index and subsequent adverse long-term cardiovascular events in young and middle-aged US adults based on obesity status
Weihua Chen, Shan Ding, Jiabin Tu, Guitao Xiao, Kaihong Chen, Yanbin Zhang, Rongchong Huang, Ying Liao
Lipids in Health and Disease.2023;[Epub] CrossRef - Uncovering Predictors of Lipid Goal Attainment in Type 2 Diabetes Outpatients Using Logic Learning Machine: Insights from the AMD Annals and AMD Artificial Intelligence Study Group
Davide Masi, Rita Zilich, Riccardo Candido, Annalisa Giancaterini, Giacomo Guaita, Marco Muselli, Paola Ponzani, Pierluigi Santin, Damiano Verda, Nicoletta Musacchio
Journal of Clinical Medicine.2023; 12(12): 4095. CrossRef - Nutritive value, material reduction, biomass conversion rate, and survival of black solider fly larvae reared on palm kernel meal supplemented with fish pellets and fructose
Rudy Agung Nugroho, Retno Aryani, Esti Handayani Hardi, Hetty Manurung, Rudianto Rudianto, Nadhifa Aurellia Wirawan, Nadya Syalsabillah, Wibowo Nugroho Jati
International Journal of Tropical Insect Science.2023; 43(4): 1243. CrossRef - Novel Antidiabetic Agents and Their Effects on Lipid Profile: A Single Shot for Several Cardiovascular Targets
Francesco Piccirillo, Sara Mastroberardino, Annunziata Nusca, Lorenzo Frau, Lorenzo Guarino, Nicola Napoli, Gian Paolo Ussia, Francesco Grigioni
International Journal of Molecular Sciences.2023; 24(12): 10164. CrossRef - Triglyceride-Glucose index as an alternative tool for identifying prediabetes and insulin resistance: A study on Bangladeshi adults
SumonRahman Chowdhury, AmamZonaed Siddiki, AB. M. Kamrul-Hasan
Bangladesh Journal of Endocrinology and Metabolism.2023; 2(2): 73. CrossRef - Inhibitory Investigations of Acyl-CoA Derivatives against Human Lipoxygenase Isozymes
Michelle Tran, Kevin Yang, Alisa Glukhova, Michael Holinstat, Theodore Holman
International Journal of Molecular Sciences.2023; 24(13): 10941. CrossRef - Implications of vitamin D deficiency in systemic inflammation and cardiovascular health
Sanjay Kumar Dey, Shashank Kumar, Diksha Rani, Shashank Kumar Maurya, Pratibha Banerjee, Madhur Verma, Sabyasachi Senapati
Critical Reviews in Food Science and Nutrition.2023; : 1. CrossRef - The effects of pomegranate peel added bread on anthropometric measurements, metabolic and oxidative parameters in individuals with type 2 diabetes: a double-blind, randomized, placebo-controlled study
Özlem Özpak Akkuş, Uğurcan Metin, Zeynep Çamlık
Nutrition Research and Practice.2023; 17(4): 698. CrossRef - Triglyceride glucose index, its modified indices, and triglyceride HDL-C ratio as predictor markers of insulin resistance in prediabetic individuals
RojeenRasheed Suleiman, SherwanFerman Salih, BarhavIssa Abdullah, IbrahimHasan Ibrahim, ZindanAzeez Saeed
Medical Journal of Babylon.2023; 20(2): 268. CrossRef - Differentially Expressed Genes in Response to a Squalene-Supplemented Diet Are Accurate Discriminants of Porcine Non-Alcoholic Steatohepatitis
Roubi Abuobeid, Luis V. Herrera-Marcos, Carmen Arnal, Seyed Hesamoddin Bidooki, Javier Sánchez-Marco, Roberto Lasheras, Joaquín C. Surra, María Jesús Rodríguez-Yoldi, Roberto Martínez-Beamonte, Jesús Osada
International Journal of Molecular Sciences.2023; 24(16): 12552. CrossRef - Do markers of adiposity and glycaemia mediate the association between low carbohydrate diet and cardiovascular risk factors: findings from the UK National Diet and Nutrition Survey (NDNS) 2008–2016
Cláudia Raulino Tramontt, Saad Mouti, Marjorie Lima Do Vale, Xunhan Li, Rajna Golubic, Sumantra Ray
BMJ Nutrition, Prevention & Health.2023; 6(2): 153. CrossRef - Association of HDL Subfraction Profile with the Progression of Insulin Resistance
Peter Piko, Tibor Jenei, Zsigmond Kosa, Janos Sandor, Nora Kovacs, Ildiko Seres, Gyorgy Paragh, Roza Adany
International Journal of Molecular Sciences.2023; 24(17): 13563. CrossRef - The Role of Lipids in the Regulation of Immune Responses
Chelsea Garcia, Catherine J. Andersen, Christopher N. Blesso
Nutrients.2023; 15(18): 3899. CrossRef - The Decrease in Serum Total Cholesterol and Low-Density Lipoprotein (LDL) Concentrations With the Initiation of Hemodialysis Despite a Concomitant Increase in Serum Albumin Concentrations
Ramin Sam, Li Zhang, Delphine S Tuot, Rafia Chaudhry
Cureus.2023;[Epub] CrossRef - Metabolic syndrome: prospects for the use of angiopoetin-like proteins type 3 and 4 for the diagnosis of metabolic disorders
V. A. Aleksandrov
Meditsinskiy sovet = Medical Council.2023; (16): 68. CrossRef - Spectral characterization and binding dynamics of bioactive compounds from Chlorella minutissima against α-glucosidase: An in vitro and in silico approach
Koushalya Selvaraju, Vasantharaja Raguraman, Harlokesh Narayan Yadav, P. Hariprasad, Anushree Malik
Algal Research.2023; 75: 103281. CrossRef - Cholesterol reprograms glucose and lipid metabolism to promote proliferation in colon cancer cells
Shyamananda Singh Mayengbam, Abhijeet Singh, Himanshi Yaduvanshi, Firoz Khan Bhati, Bhavana Deshmukh, Dipti Athavale, Pranay L. Ramteke, Manoj Kumar Bhat
Cancer & Metabolism.2023;[Epub] CrossRef - To Boost or to Reset: The Role of Lactoferrin in Energy Metabolism
Giusi Ianiro, Antonella Niro, Luigi Rosa, Piera Valenti, Giovanni Musci, Antimo Cutone
International Journal of Molecular Sciences.2023; 24(21): 15925. CrossRef - Lipid Profile Paradox: Investigating Improved Lipid Levels in Diabetic Mellitus Patients with Foot Ulcer Infections—A Prospective Descriptive Study
Andrei Ardelean, Andreea-Adriana Neamtu, Diana-Federica Balta, Carmen Neamtu, Dan Goldis, Mihai Rosu, Alexandru Nesiu, Silviu Moldovan, Cristi Tarta, Bogdan Dan Totolici
Diagnostics.2023; 13(23): 3531. CrossRef - Geraniol reverses obesity by improving conversion of WAT to BAT in high fat diet induced obese rats by inhibiting HMGCoA reductase
Shushmita Chand, Alok Shiomurti Tripathi, Tabinda Hasan, Kavitha Ganesh, Mary Anne W. Cordero, Mohammad Yasir, Magdi E. A. Zaki, Pankaj Tripathi, Lucy Mohapatra, Rahul Kumar Maurya
Nutrition & Diabetes.2023;[Epub] CrossRef - Lipidomics Profiling of Metformin-Induced Changes in Obesity and Type 2 Diabetes Mellitus: Insights and Biomarker Potential
Muhammad Mujammami, Shereen M. Aleidi, Adriana Zardini Buzatto, Awad Alshahrani, Reem H. AlMalki, Hicham Benabdelkamel, Mohammed Al Dubayee, Liang Li, Ahmad Aljada, Anas M. Abdel Rahman
Pharmaceuticals.2023; 16(12): 1717. CrossRef - Combined Inositols, α-Lactalbumin, Gymnema Sylvestre and Zinc Improve the Lipid Metabolic Profile of Patients with Type 2 Diabetes Mellitus: A Randomized Clinical Trial
Alessandro Nani, Federico Bertuzzi, Elena Meneghini, Elena Mion, Basilio Pintaudi
Journal of Clinical Medicine.2023; 12(24): 7650. CrossRef - Determination of Diabetes-associated Cardiovascular Autonomic Neuropathy Risk Factors among Insulin and Non-insulin Dependent Diabetics
Ibrahim Abdulsada, Zain Alabdeen Obaid, Farah Almerza, Mays Alwaeli, Anmar Al-Elayawi, Taha Al-Dayyeni, Harir Al-Tuhafy
The Journal of Medical Research.2023; 9(6): 141. CrossRef - Angiopoietin-like protein 8 (betatrophin) inhibits hepatic gluconeogenesis through PI3K/Akt signaling pathway in diabetic mice
Zhicong Zhao, Xia Deng, Jue Jia, Li Zhao, Chenxi Wang, Zhensheng Cai, Chang Guo, Ling Yang, Dong Wang, Suxian Ma, Jialiang Deng, Haoxiang Li, Libin Zhou, Zhigang Tu, Guoyue Yuan
Metabolism.2022; 126: 154921. CrossRef - Clinical significance of controlling nutritional status score (CONUT) in evaluating outcome of postoperative patients with gastric cancer
Qi Xiao, Xiaoqing Li, Baojun Duan, Xiaofan Li, Sida Liu, Boyu Xu, Shuai Shi, Jin Zhang, Haoyuan Qin, Xianglong Duan, Yansong Pu
Scientific Reports.2022;[Epub] CrossRef - Bioactive Compounds from Cardoon as Health Promoters in Metabolic Disorders
Luís R. Silva, Telma A. Jacinto, Paula Coutinho
Foods.2022; 11(3): 336. CrossRef - Protective effect of vanillic acid against diabetes and diabetic nephropathy by attenuating oxidative stress and upregulation of NF‐κB, TNF‐α and COX‐2 proteins in rats
Brahmjot Singh, Ajay Kumar, Hasandeep Singh, Sarabjit Kaur, Saroj Arora, Balbir Singh
Phytotherapy Research.2022; 36(3): 1338. CrossRef - Variability, Mean, and Baseline Values of Metabolic Parameters in Predicting Risk of Type 2 Diabetes
Duong Duc Pham, Jaekyung Song, Yunwan Jeon, Ibrahimi Hajar, Chae Hun Leem
The Journal of Clinical Endocrinology & Metabolism.2022; 107(5): 1270. CrossRef - Glycemic Control and the Heart: The Tale of Diabetic Cardiomyopathy Continues
Miriam Longo, Lorenzo Scappaticcio, Paolo Cirillo, Antonietta Maio, Raffaela Carotenuto, Maria Ida Maiorino, Giuseppe Bellastella, Katherine Esposito
Biomolecules.2022; 12(2): 272. CrossRef - Mechanisms of antidiabetic drugs and cholesterol efflux: A clinical perspective
Ali Ahmadi, Mariam Bagheri Ekta, Amirhossein Sahebkar
Drug Discovery Today.2022; 27(6): 1679. CrossRef - DO‐SRS imaging of diet regulated metabolic activities in Drosophila during aging processes
Yajuan Li, Wenxu Zhang, Anthony A. Fung, Lingyan Shi
Aging Cell.2022;[Epub] CrossRef - The multifaceted role of cytochrome P450-Derived arachidonic acid metabolites in diabetes and diabetic cardiomyopathy
Fadumo Ahmed Isse, Ahmed A. El-Sherbeni, Ayman O. S. El-Kadi
Drug Metabolism Reviews.2022; 54(2): 141. CrossRef - Lipid traits and type 2 diabetes risk in African ancestry individuals: A Mendelian Randomization study
Opeyemi Soremekun, Ville Karhunen, Yiyan He, Skanda Rajasundaram, Bowen Liu, Apostolos Gkatzionis, Chisom Soremekun, Brenda Udosen, Hanan Musa, Sarah Silva, Christopher Kintu, Richard Mayanja, Mariam Nakabuye, Tafadzwa Machipisa, Amy Mason, Marijana Vujko
eBioMedicine.2022; 78: 103953. CrossRef - Poor Glycaemic Control and its Associated Factors among Type 2 Diabetes Mellitus Patients in Southern Part of Peninsular Malaysia: A Registry-based Study
Norizzati Amsah, Zaleha Md Isa, Zaid Kassim
Open Access Macedonian Journal of Medical Sciences.2022; 10(E): 422. CrossRef - The Impact of Metabolic Syndrome and Type 2 Diabetes Mellitus on Prostate Cancer
André P. Sousa, Raquel Costa, Marco G. Alves, Raquel Soares, Pilar Baylina, Rúben Fernandes
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - Maternal lipid profile in pregnancy and embryonic size: a population-based prospective cohort study
Dionne V. Gootjes, Anke G. Posthumus, Deveney F. Wols, Yolanda B. de Rijke, Jeanine E. Roeters Van Lennep, Eric A. P. Steegers
BMC Pregnancy and Childbirth.2022;[Epub] CrossRef - Successful correction of hyperglycemia is critical for weight loss and a decrease in cardiovascular risk in obese patients
Jolanta Zalejska-Fiolka, Anna Birková, Beáta Hubková, Tomasz Wielkoszyński, Beáta Čižmárová, Beata Szlachta, Rafał Fiolka, Urszula Błaszczyk, Adam Wylęgała, Sławomir Kasperczyk, Alicja Grzanka, Mária Mareková, Michal Toborek
The Journal of Nutritional Biochemistry.2022; 106: 109021. CrossRef - Morus alba L. for Blood Sugar Management: A Systematic Review and Meta-Analysis
Hye In Jeong, Soobin Jang, Kyeong Han Kim, Fernanda Tonelli
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - Correlation between HbA1c and Triglyceride Level with Coronary Stenosis Degree in Type 2 Diabetes Mellitus with Coronary Heart Disease
Laily Adninta, Indranila Samsuria, Edward Kurnia Setiawan Limijadi
Open Access Macedonian Journal of Medical Sciences.2022; 10(B): 944. CrossRef - Growth trajectories in lipid profile and fasting blood sugar in prediabetic people over a 16- year follow-up and future risk of type2 diabetes mellitus: A latent growth modeling approach
Awat Feizi, Fahimeh Haghighatdoost, Parisa Zakeri, Ashraf Aminorroaya, Masoud Amini
Alexandria Journal of Medicine.2022; 58(1): 52. CrossRef - Whole grain rice: Updated understanding of starch digestibility and the regulation of glucose and lipid metabolism
Zihang Cheng, Dongling Qiao, Siming Zhao, Binjia Zhang, Qinlu Lin, Fengwei Xie
Comprehensive Reviews in Food Science and Food Safety.2022; 21(4): 3244. CrossRef - The Role of Triglyceride-HDL Ratio and Triglyceride-glucose Index in Estimating Glycemic Control in Patients with Type 2 Diabetes Mellitus
Özgür Altun, Semih Kalyon
Meandros Medical and Dental Journal.2022; 23(1): 74. CrossRef - Murine Falcor/LL35 lncRNA Contributes to Glucose and Lipid Metabolism In Vitro and In Vivo
Evgeniya Shcherbinina, Tatiana Abakumova, Daniil Bobrovskiy, Ilia Kurochkin, Ksenia Deinichenko, Elena Stekolshchikova, Nickolay Anikanov, Rustam Ziganshin, Pavel Melnikov, Ekaterina Khrameeva, Maria Logacheva, Timofei Zatsepin, Olga Sergeeva
Biomedicines.2022; 10(6): 1397. CrossRef - The Role of Changes in Cumulative Lipid Parameter Burden in the Pathogenesis of Type 2 Diabetes Mellitus: A Cohort Study of People Aged 35–65 Years in Rural China
Qi Wang, Tao Xie, Ting Zhang, Yuanjia Deng, Yuying Zhang, Qingfeng Wu, Minghua Dong, Xiaoting Luo
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 1831. CrossRef - Alternate-day fasting, a high-sucrose/caloric diet and praziquantel treatment influence biochemical and behavioral parameters during Schistosoma mansoni infection in male BALB/c mice
Luis F.C. dos Reis, Cláudio D. Cerdeira, Guilherme S. Gagliano, Ana B.T. de Figueiredo, Juliana H. Ferreira, Aline P. Castro, Raquel L.M. Souza, Marcos J. Marques
Experimental Parasitology.2022; 240: 108316. CrossRef - The value of Genus Acacia in arid and semi-arid environments for the treatment of chronic inflammatory diseases
Akhtar Atiya, Taghreed Majrashi, Safia Akhtar, Arshad Ali Khan, Afnan Mohammad Sultan Asiri, Hanan Jamaan Al-Zahrania, Raghad Sameer Alnami, Sara Abdulrahman Alsharif, Taef Amer, Zainah Abdullah Faiz, Shimaa Ahmad M AlYahya, Shahad Saeedhabtar
Phytomedicine Plus.2022; 2(3): 100315. CrossRef - Beneficial effects of monounsaturated fatty acid‐rich blended oils with an appropriate polyunsaturated/saturated fatty acid ratio and a low n‐6/n‐3 fatty acid ratio on the health of rats
Ligang Yang, Chao Yang, Chu Chu, Min Wan, Dengfeng Xu, Da Pan, Hui Xia, Shao Kang Wang, Guofang Shu, Shiqing Chen, Guiju Sun
Journal of the Science of Food and Agriculture.2022; 102(15): 7172. CrossRef - Hibiscus sabdariffa in Diabetes Prevention and Treatment—Does It Work? An Evidence-Based Review
Daniel Jamrozik, Weronika Borymska, Ilona Kaczmarczyk-Żebrowska
Foods.2022; 11(14): 2134. CrossRef - Statin therapy is not warranted for a person with high LDL-cholesterol on a low-carbohydrate diet
David M. Diamond, Benjamin T. Bikman, Paul Mason
Current Opinion in Endocrinology, Diabetes & Obesity.2022; 29(5): 497. CrossRef - Probiotic therapy, a novel and efficient adjuvant approach to improve glycemic status: An umbrella meta-analysis
Meysam Zarezadeh, Vali Musazadeh, Amir Hossein Faghfouri, Bahareh Sarmadi, Parsa Jamilian, Parmida Jamilian, Helda Tutunchi, Parvin Dehghan
Pharmacological Research.2022; 183: 106397. CrossRef - Amelioration of hyperglycemia and hyperlipidemia in a high-fat diet-fed mice by supplementation of a developed optimized polyherbal formulation
Tanisha, Sunil Venkategowda, Mala Majumdar
3 Biotech.2022;[Epub] CrossRef - Daily Treatment of Mice with Type 2 Diabetes with Adropin for Four Weeks Improves Glucolipid Profile, Reduces Hepatic Lipid Content and Restores Elevated Hepatic Enzymes in Serum
Marek Skrzypski, Paweł A. Kołodziejski, Ewa Pruszyńska-Oszmałek, Tatiana Wojciechowicz, Paulina Janicka, Małgorzata Krążek, Emilian Małek, Mathias Z. Strowski, Krzysztof W. Nowak
International Journal of Molecular Sciences.2022; 23(17): 9807. CrossRef - Comparison of the triglyceride glucose (TyG) index, triglyceride to high-density lipoprotein cholesterol (TG/HDL-C) ratio, and metabolic score for insulin resistance (METS-IR) associated with periodontitis in Korean adults
Yea-Chan Lee, Ji-Won Lee, Yu-Jin Kwon
Therapeutic Advances in Chronic Disease.2022; 13: 204062232211226. CrossRef - Coadministration of L‐alanine and L‐glutamine ameliorate blood glucose levels, biochemical indices and histological features in alloxan‐induced diabetic rats
Ifeanyi J. Ezeonwumelu, Abduljalil M. Mode, Umar F. Magaji, Nnamdi A. Nzoniwu, Muhamad H. Tangaza, Fatima I. Tanimu, Shamsudeen U. Dandare
Journal of Food Biochemistry.2022;[Epub] CrossRef - Laboratory data clustering in defining population cohorts: Case study on metabolic indicators
Ivan Pavicevic, Goran Miljus, Olgica Nedic
Journal of the Serbian Chemical Society.2022; 87(9): 1025. CrossRef - Effects of Psychotropic Medication on Somatic Sterol Biosynthesis of Adult Mice
Marta Balog, Allison C Anderson, Marija Heffer, Zeljka Korade, Karoly Mirnics
Biomolecules.2022; 12(10): 1535. CrossRef - The Correlation Between Angiopoietin-Like 3 and Metabolic Markers of Some Lipid and Glucose in Type 2 Diabetes Mellitus Patients at the First Diagnosis
Minh Hoang Thi, Chung Dang Thanh, Thuan Huynh Quang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 3329. CrossRef - Joint inference of physiological network and survival analysis identifies factors associated with aging rate
Anurag Sethi, Eugene Melamud
Cell Reports Methods.2022; 2(12): 100356. CrossRef - Disease activity and prognosis in Takayasu’s arteritis
Sema Kaymaz Tahra, Fatma Alibaz Öner
Ulusal Romatoloji Dergisi.2022; 14(3): 137. CrossRef - Antihyperlipidemic effect of the hydroalcoholic extract of Basidiomycete Pycnoporus sanguineus (Fr.) Murr. in streptozotocin-induced diabetic rats
Maiza Von Dentz, Gabriela Gambato, Andreza Ferrari, Roselei Claudete Fontana, Eliseu Rodrigues, Mirian Salvador, Marli Camassola, Matheus Parmegiani Jahn
Advances in Traditional Medicine.2021; 21(3): 453. CrossRef - Effect of short-chain chlorinated paraffins on metabolic profiling of male SD rats
Ningbo Geng, Yun Luo, Rong Cao, Xiaoyao Song, Fang Li, Feidi Wang, Yufeng Gong, Liguo Xing, Haijun Zhang, Jiping Chen
Science of The Total Environment.2021; 750: 141404. CrossRef - Dyslipidemia and its associated factors in patients with type 2 diabetes mellitus
Ahmed Tijani Bawah, Richard Darko, Albert Abaka-Yawson, Mohammed Mustapha Seini, Silas Kinanyok, Samuel Adusei
Journal of Public Health.2021; 29(4): 985. CrossRef - The reduction of lipid-sourced energy production caused by ATGL inhibition cannot be compensated by activation of HSL, autophagy, and utilization of other nutrients in fish
Si-Lan Han, Yan Liu, Samwel M. Limbu, Li-Qiao Chen, Mei-Ling Zhang, Zhen-Yu Du
Fish Physiology and Biochemistry.2021; 47(1): 173. CrossRef - Diabetes, Lipids, and CV Risk
Jan Škrha
Current Atherosclerosis Reports.2021;[Epub] CrossRef - Serum soluble epoxide hydrolase related oxylipins and major depression in patients with type 2 diabetes
Natasha Z. Anita, Nubaira Forkan, Radia Kamal, Michelle M. Nguyen, Di Yu, Chelsi Major-Orfao, Sophie K. Wong, Krista L. Lanctôt, Nathan Herrmann, Paul I. Oh, Baiju R. Shah, Jeremy Gilbert, Angela Assal, Ilana J. Halperin, Theresa L. Pedersen, Ameer Y. Tah
Psychoneuroendocrinology.2021; 126: 105149. CrossRef - The controversial role of glucose in the diabetic kidney
Rui Fernandes
Porto Biomedical Journal.2021; 6(1): e113. CrossRef - Effectiveness of the piperine-supplemented Curcuma longa L. in metabolic control of patients with type 2 diabetes: a randomised double-blind placebo-controlled clinical trial
Joana Furtado de Figueiredo Neta, Vivian Saraiva Veras, Danilo Ferreira de Sousa, Maria da Conceição dos Santos Oliveira Cunha, Maria Veraci Oliveira Queiroz, José Claudio Garcia Lira Neto, Marta Maria Coelho Damasceno, Márcio Flávio Moura de Araújo, Robe
International Journal of Food Sciences and Nutrition.2021; 72(7): 968. CrossRef - Mechanisms and Treatment of Dyslipidemia in Diabetes
Ehete Bahiru, Ruth Hsiao, Daniel Phillipson, Karol E. Watson
Current Cardiology Reports.2021;[Epub] CrossRef - The Changes of Cholesterol Profile at the Different Insulin Resistance Range in the Czech Republic
Vladimír Kron, Miroslav Verner, Pavel Smetana, Dagmar Horáková, Jan Šlégr, Filip Studnička, Damián Bušovský, Karel Martiník
Medicina.2021; 57(3): 249. CrossRef - Chronic Intake of Energy Drinks and Their Sugar Free Substitution Similarly Promotes Metabolic Syndrome
Liam T. Graneri, John C. L. Mamo, Zachary D’Alonzo, Virginie Lam, Ryusuke Takechi
Nutrients.2021; 13(4): 1202. CrossRef - Association of maternal lipid profile and gestational diabetes mellitus: A systematic review and meta-analysis of 292 studies and 97,880 women
Jiamiao Hu, Clare L. Gillies, Shaoling Lin, Zoe A. Stewart, Sarah E. Melford, Keith R. Abrams, Philip N. Baker, Kamlesh Khunti, Bee K. Tan
EClinicalMedicine.2021; 34: 100830. CrossRef - THE ROLE OF TRIGLYCERIDE GLUCOSE INDEX AS PREDICTOR OF GLYCEMIC CONTROL IN PATIENTS WITH TYPE 2 DIABETES MELLITUS
Charchit Mehta, Vidyasagar C R, Raveesha A
GLOBAL JOURNAL FOR RESEARCH ANALYSIS.2021; : 106. CrossRef - Interaction of Adiponectin Genotypes and Insulin Resistance on the Occurrence of Taiwanese Metabolic Syndrome
Chun-Chieh Chen, Yu-Hsiang Wei, Chia-Chen Huang, Shin-Hui Hung, Zeng-Wei Wang, Ruey-Hong Wong, Daniel Diaz
BioMed Research International.2021; 2021: 1. CrossRef - Synergistic effects of black ginseng and aged garlic extracts for the amelioration of nonalcoholic fatty liver disease (NAFLD) in mice
Guihun Jiang, Karna Ramachandraiah, Mian Anjum Murtaza, Lili Wang, Shanji Li, Kashif Ameer
Food Science & Nutrition.2021; 9(6): 3091. CrossRef - Does vitamin C supplementation exert profitable effects on serum lipid profile in patients with type 2 diabetes? A systematic review and dose-response meta-analysis
Zahra Namkhah, Damoon Ashtary-Larky, Fatemeh Naeini, Cain C.T. Clark, Omid Asbaghi
Pharmacological Research.2021; 169: 105665. CrossRef - Particulate matter air pollutants and cardiovascular disease: Strategies for intervention
Ankit Aryal, Ashlyn C. Harmon, Tammy R. Dugas
Pharmacology & Therapeutics.2021; 223: 107890. CrossRef - Identification of Docetaxel as a Potential Drug to Promote HDL Biogenesis
Hong Y. Choi, Isabelle Ruel, Jacques Genest
Frontiers in Pharmacology.2021;[Epub] CrossRef - Diet Rich in Lard Promotes a Metabolic Environment Favorable to Trypanosoma cruzi Growth
Débora Maria Soares de Souza, Maria Cláudia Silva, Silvia Elvira Barros Farias, Ana Paula de J. Menezes, Cristiane Maria Milanezi, Karine de P. Lúcio, Nívia Carolina N. Paiva, Paula Melo de Abreu, Daniela Caldeira Costa, Kelerson Mauro de Castro Pinto, Gu
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Association between the triglyceride-glucose index and abdominal aortic calcification in adults: A cross-sectional study
Yuxiong Chen, Zhen'ge Chang, Yakun Zhao, Yanbo Liu, Jia Fu, Yongqiao Zhang, Yijie Liu, Zhongjie Fan
Nutrition, Metabolism and Cardiovascular Diseases.2021; 31(7): 2068. CrossRef - Roles of microRNAs in carbohydrate and lipid metabolism disorders and their therapeutic potential
Sujay Paul, Luis Alberto Bravo Vázquez, Samantha Pérez Uribe, Luis Aarón Manzanero Cárdenas, María Fernanda Ruíz Aguilar, Samik Chakraborty, Ashutosh Sharma
Biochimie.2021; 187: 83. CrossRef - Meal-induced inflammation: postprandial insights from the Personalised REsponses to DIetary Composition Trial (PREDICT) study in 1000 participants
Mohsen Mazidi, Ana M Valdes, Jose M Ordovas, Wendy L Hall, Joan C Pujol, Jonathan Wolf, George Hadjigeorgiou, Nicola Segata, Naveed Sattar, Robert Koivula, Tim D Spector, Paul W Franks, Sarah E Berry
The American Journal of Clinical Nutrition.2021; 114(3): 1028. CrossRef - Daidzein mitigates myocardial injury in streptozotocin-induced diabetes in rats
Ankit P. Laddha, Yogesh A. Kulkarni
Life Sciences.2021; 284: 119664. CrossRef - Impact of triglycerides and waist circumference on insulin resistance and β-cell function in non-diabetic first-degree relatives of type 2 diabetes
Fahd Ahmed, Molham AL-Habori, Ebtesam Al-Zabedi, Riyadh Saif-Ali
BMC Endocrine Disorders.2021;[Epub] CrossRef - Prevalence, prescriptions, outcomes and costs of type 2 diabetes patients with or without prior coronary artery disease or stroke: a longitudinal 5-year claims-data analysis of over 7 million inhabitants
Aldo Pietro Maggioni, Letizia Dondi, Felicita Andreotti, Giulia Ronconi, Silvia Calabria, Carlo Piccinni, Antonella Pedrini, Imma Esposito, Nello Martini
Therapeutic Advances in Chronic Disease.2021; 12: 204062232110263. CrossRef - Fatty acid desaturase 2 (FADS 2) rs174575 (C/G) polymorphism, circulating lipid levels and susceptibility to type-2 diabetes mellitus
Shilpa S. Shetty, N. Suchetha Kumari
Scientific Reports.2021;[Epub] CrossRef - Chitosan Oligosaccharide Alleviates Abnormal Glucose Metabolism without Inhibition of Hepatic Lipid Accumulation in a High-Fat Diet/Streptozotocin-Induced Diabetic Rat Model
Shing-Hwa Liu, Fan-Wen Chen, Meng-Tsan Chiang
Marine Drugs.2021; 19(7): 360. CrossRef - Diabetic dyslipidaemia
Subashini C. Thambiah, Leslie Charles Lai
Practical Laboratory Medicine.2021; 26: e00248. CrossRef - Characterization of PFOS toxicity on in-vivo and ex-vivo mouse pancreatic islets
Hin Ting Wan, Lok Yi Cheung, Ting Fung Chan, Marco Li, Keng Po Lai, Chris Kong Chu Wong
Environmental Pollution.2021; 289: 117857. CrossRef - Prevalence and Metabolic Predictors for Early Diagnosed Prediabetes in Women with Previous Gestational Diabetes: Observational Cohort Study
Aleksandra Z. Jotic, Milica M. Stoiljkovic, Tanja J. Milicic, Katarina S. Lalic, Ljiljana Z. Lukic, Marija V. Macesic, Jelena N. Stanarcic Gajovic, Mina M. Milovancevic, Miroslava G. Gojnic Dugalic, Veljko M. Jeremic, Nebojsa M. Lalic
Diabetes Therapy.2021; 12(10): 2691. CrossRef - PKM2‐TMEM33 axis regulates lipid homeostasis in cancer cells by controlling SCAP stability
Fabao Liu, Min Ma, Ang Gao, Fengfei Ma, Gui Ma, Peng Liu, Chenxi Jia, Yidan Wang, Kristine Donahue, Shengjie Zhang, Irene M Ong, Sunduz Keles, Lingjun Li, Wei Xu
The EMBO Journal.2021;[Epub] CrossRef - Triglyceride/Glucose Index (TyG Index) as a marker of glucose status conversion among reproductive-aged women in Jakarta, Indonesia: The Bogor cohort study (2011–2016)
Iche A. Liberty, Nasrin Kodim, Ratu A.D. Sartika, Indang Trihandini, R.M. Suryadi Tjekyan, Zulkarnain, Masdalina Pane, Livy B. Pratisthita, Dicky L. Tahapary, Pradana Soewondo
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(6): 102280. CrossRef - Novel Serum and Urinary Metabolites Associated with Diabetic Retinopathy in Three Asian Cohorts
Debra Q. Y. Quek, Feng He, Rehena Sultana, Riswana Banu, Miao Li Chee, Simon Nusinovici, Sahil Thakur, Chaoxu Qian, Ching-Yu Cheng, Tien Y. Wong, Charumathi Sabanayagam
Metabolites.2021; 11(9): 614. CrossRef - Lychee Seed as a Potential Hypoglycemic Agent, and Exploration of its Underlying Mechanisms
Yuehong Zhang, De Jin, Xuedong An, Liyun Duan, Yingying Duan, Fengmei Lian
Frontiers in Pharmacology.2021;[Epub] CrossRef - Indole-3-Propionic Acid, a Gut-Derived Tryptophan Metabolite, Associates with Hepatic Fibrosis
Ratika Sehgal, Mariana Ilha, Maija Vaittinen, Dorota Kaminska, Ville Männistö, Vesa Kärjä, Marjo Tuomainen, Kati Hanhineva, Stefano Romeo, Päivi Pajukanta, Jussi Pihlajamäki, Vanessa D. de Mello
Nutrients.2021; 13(10): 3509. CrossRef - Impact of diabetes on the accuracy and speed of accessing information from episodic and working memory
Selene Cansino, Frine Torres-Trejo, Cinthya Estrada-Manilla, Eira Castellanos-Domínguez, Ana Zamora-Olivares, Silvia Ruiz Velasco, Jim Grange
Cogent Psychology.2021;[Epub] CrossRef - Association of the triglyceride-glucose index and major adverse cardiac and cerebrovascular events in female patients undergoing percutaneous coronary intervention with drug-eluting stents: A retrospective study
Su Zou, Yingjia Xu
Diabetes Research and Clinical Practice.2021; 181: 109073. CrossRef - Adherence to Treatment and Glycemic Control in Patients with Type 2 Diabetes Mellitus: A 4-Year Follow-up PTM Bogor Cohort Study, Indonesia
Silma Kaaffah, Pradana Soewondo, Woro Riyadina, Fransiskus Samuel Renaldi, Rani Sauriasari
Patient Preference and Adherence.2021; Volume 15: 2467. CrossRef - Evaluation of secondary electronic cigarette inhalation on lipid metabolism in C57BL/6J mice using indirect calorimetry
Dolly L. Crawford, Alexis R. Phillips, Taylor R. Williams
Metabolism Open.2021; 12: 100150. CrossRef - Momordica charantia leaf extract reduces hepatic lipid accumulation and diet-induced dyslipidemia in zebrafish through lipogenesis and beta-oxidation
Semon Wu, Cheng Huang, You-Ren Chen, Hsiu-Chen Huang, Wen-Cheng Huang, Yu-Heng Lai
Journal of Functional Foods.2021; 87: 104857. CrossRef - Genetic Determinants of Plasma Low-Density Lipoprotein Cholesterol Levels: Monogenicity, Polygenicity, and “Missing” Heritability
Jesús Maria Martín-Campos
Biomedicines.2021; 9(11): 1728. CrossRef - Effect of blood lipid variability on mortality in patients with type 2 diabetes: a large single-center cohort study
Mu-Cyun Wang, Chia-Ing Li, Chiu-Shong Liu, Chih-Hsueh Lin, Shing-Yu Yang, Tsai-Chung Li, Cheng-Chieh Lin
Cardiovascular Diabetology.2021;[Epub] CrossRef - Phenotype correlations reveal the relationships of physiological systems underlying human ageing
Meng Hao, Hui Zhang, Zixin Hu, Xiaoyan Jiang, Qi Song, Xi Wang, Jiucun Wang, Zuyun Liu, Xiaofeng Wang, Yi Li, Li Jin
Aging Cell.2021;[Epub] CrossRef - Association of dyslipidemia, diabetes and metabolic syndrome with serum ferritin levels: a middle eastern population-based cross-sectional study
Neyla S. Al Akl, Olfa Khalifa, Khaoula Errafii, Abdelilah Arredouani
Scientific Reports.2021;[Epub] CrossRef - Antioxidant and Anti-inflammatory Properties of Yttrium Oxide Nanoparticles: New Insights into Alleviating Diabetes
Kim San Tang
Current Diabetes Reviews.2021; 17(4): 496. CrossRef - Evaluation of the Anti-Hypercholesterolemic and Antioxidant Activity of Mentha pulegium (L.) Aqueous Extract in Normal and Streptozotocin- Induced Diabetic Rats
Omar Farid, Mohamed Eddouks
The Natural Products Journal.2020; 10(3): 236. CrossRef - Hyperlipidemias in elderly patients: results from the Berlin Aging Study II (BASEII), a cross-sectional study
Adrian Rosada, Ursula Kassner, Felix Weidemann, Maximilian König, Nikolaus Buchmann, Elisabeth Steinhagen-Thiessen, Dominik Spira
Lipids in Health and Disease.2020;[Epub] CrossRef - Distinct effects of virgin coconut oil supplementation on the glucose and lipid homeostasis in non-diabetic and alloxan-induced diabetic rats
Siniša Đurašević, Gorana Nikolić, Ivan Zaletel, Ilijana Grigorov, Lidija Memon, Dragana Mitić-Ćulafić, Predrag Vujović, Jelena Đorđević, Zoran Todorović
Journal of Functional Foods.2020; 64: 103601. CrossRef - Medium and long-term effects of low doses of Chlorpyrifos during the postnatal, preweaning developmental stage on sociability, dominance, gut microbiota and plasma metabolites
Cristian Perez-Fernandez, Miguel Morales-Navas, Luis Manuel Aguilera-Sáez, Ana Cristina Abreu, Laia Guardia-Escote, Ignacio Fernández, José Antonio Garrido-Cárdenas, María Teresa Colomina, Estela Giménez, Fernando Sánchez-Santed
Environmental Research.2020; 184: 109341. CrossRef - Fatty Acids and Sterol Rich Stem Back Extract of Shorea Roxburghii Attenuates Hyperglycemia, Hyperlipidemia, and Oxidative Stress in Diabetic Rats
Emmanuel Ayobami Makinde, Nisaudah Radenahmad, Raihan Uz Zaman, Opeyemi Joshua Olatunji
European Journal of Lipid Science and Technology.2020;[Epub] CrossRef - Factors Associated with Poor Glycemic and Lipid Levels in Ambulatory Diabetes Mellitus Type 2 Patients in Asmara, Eritrea: A Cross-Sectional Study
Oliver Okoth Achila, Millen Ghebretinsae, Abraham Kidane, Michael Simon, Shewit Makonen, Yohannes Rezene
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Postprandial Metabolism is Impaired in Overweight Normoglycemic Young Adults without Family History of Diabetes
A. Aneesh Kumar, Gopika Satheesh, Gadadharan Vijayakumar, Mahesh Chandran, Priya R. Prabhu, Leena Simon, Vellappillil Raman Kutty, Chandrasekharan C. Kartha, Abdul Jaleel
Scientific Reports.2020;[Epub] CrossRef - HDL inhibits endoplasmic reticulum stress-induced apoptosis of pancreatic β-cells in vitro by activation of Smoothened
Mustafa Yalcinkaya, Anja Kerksiek, Katrin Gebert, Wijtske Annema, Rahel Sibler, Silvija Radosavljevic, Dieter Lütjohann, Lucia Rohrer, Arnold von Eckardstein
Journal of Lipid Research.2020; 61(4): 492. CrossRef - Beneficial effects of pomegranate peel extract on plasma lipid profile, fatty acids levels and blood pressure in patients with diabetes mellitus type-2: A randomized, double-blind, placebo-controlled study
Milkica Grabež, Ranko Škrbić, Miloš P. Stojiljković, Vesna Rudić-Grujić, Marija Paunović, Aleksandra Arsić, Snježana Petrović, Vesna Vučić, Bosa Mirjanić-Azarić, Katarina Šavikin, Nebojša Menković, Teodora Janković, Nađa Vasiljević
Journal of Functional Foods.2020; 64: 103692. CrossRef - Validation of the antidiabetic potential of isolated and nanoemulsified endophytic fungal metabolite 2,4,6-triphenylaniline through AMPK activation pathway
Nathiya Ranganathan, Gayathri Mahalingam
Journal of Molecular Liquids.2020; 316: 113836. CrossRef - Metabolism updates: new directions, techniques, and exciting research that is broadening the horizons
Chrysoula Boutari, Eirini Bouzoni, Aditya Joshi, Konstantinos Stefanakis, Olivia M. Farr, Christos S. Mantzoros
Metabolism.2020; 102: 154009. CrossRef - Anabolic SIRT4 Exerts Retrograde Control over TORC1 Signaling by Glutamine Sparing in the Mitochondria
Eisha Shaw, Manasi Talwadekar, Zeenat Rashida, Nitya Mohan, Aishwarya Acharya, Subhash Khatri, Sunil Laxman, Ullas Kolthur-Seetharam
Molecular and Cellular Biology.2020;[Epub] CrossRef - Inhibition of endoplasmic reticulum stress ameliorates cardiovascular injury in a rat model of metabolic syndrome
Eman Radwan, Marwa H. Bakr, Salma Taha, Sally A. Sayed, Alshaimaa A. Farrag, Maha Ali
Journal of Molecular and Cellular Cardiology.2020; 143: 15. CrossRef - Combination of Exercise and Vegetarian Diet: Relationship with High Density-Lipoprotein Cholesterol in Taiwanese Adults Based on MTHFR rs1801133 Polymorphism
Shu-Lin Chang, Oswald Ndi Nfor, Chien-Chang Ho, Kuan-Jung Lee, Wen-Yu Lu, Chia-Chi Lung, Disline Manli Tantoh, Shu-Yi Hsu, Ming-Chih Chou, Yung-Po Liaw
Nutrients.2020; 12(6): 1564. CrossRef - Relation of Decreased Circulating Sortilin Levels With Unfavorable Metabolic Profiles in Subjects With Newly Diagnosed Type 2 Diabetes Mellitus
İsmail Demir, Ozden Yildirim Akan, Aslı Guler, Giray Bozkaya, Behnaz Aslanipour, Mehmet Calan
The American Journal of the Medical Sciences.2020; 359(1): 8. CrossRef - Antidiabetic effect of Wedelia chinensis leaf extract in alloxan induced Swiss albino diabetic mice
Md. Wasim Bari, Md. Monirul Islam, Mahbuba Khatun, Mst Julia Sultana, Rabbi Ahmed, Ariful Islam, Md. Ismail Hossain, Md. Matiar Rahman, Mohammad Amirul Islam
Clinical Phytoscience.2020;[Epub] CrossRef - iNOS as a metabolic enzyme under stress conditions
Sarit Anavi, Oren Tirosh
Free Radical Biology and Medicine.2020; 146: 16. CrossRef - Ginsenoside Rg5 relieves type 2 diabetes by improving hepatic insulin resistance in db/db mice
Yange Wei, Haixia Yang, Chenhui Zhu, Jianjun Deng, Daidi Fan
Journal of Functional Foods.2020; 71: 104014. CrossRef - High-coverage plasma lipidomics reveals novel sex-specific lipidomic fingerprints of age and BMI: Evidence from two large population cohort studies
Habtamu B. Beyene, Gavriel Olshansky, Adam Alexander T. Smith, Corey Giles, Kevin Huynh, Michelle Cinel, Natalie A. Mellett, Gemma Cadby, Joseph Hung, Jennie Hui, John Beilby, Gerald F. Watts, Jonathan S. Shaw, Eric K. Moses, Dianna J. Magliano, Peter J.
PLOS Biology.2020; 18(9): e3000870. CrossRef - Lack of collagen XVIII leads to lipodystrophy and perturbs hepatic glucose and lipid homeostasis
Tiina Petäistö, David Vicente, Kari A. Mäkelä, Mikko A. Finnilä, Ilkka Miinalainen, Jarkko Koivunen, Valerio Izzi, Mari Aikio, Sanna‐Maria Karppinen, Raman Devarajan, Jerome Thevenot, Karl‐Heinz Herzig, Ritva Heljasvaara, Taina Pihlajaniemi
The Journal of Physiology.2020; 598(16): 3373. CrossRef - Adipose Tissue-Liver Cross Talk in the Control of Whole-Body Metabolism: Implications in Nonalcoholic Fatty Liver Disease
Vian Azzu, Michele Vacca, Samuel Virtue, Michael Allison, Antonio Vidal-Puig
Gastroenterology.2020; 158(7): 1899. CrossRef - Emulsion Droplet Crystallinity Attenuates Short-Term Satiety in Healthy Adult Males: A Randomized, Double-Blinded, Crossover, Acute Meal Study
Samar Hamad, Surangi H Samar, Amanda Cuncins, Melissa Brown, Amanda J Wright
The Journal of Nutrition.2020; 150(9): 2295. CrossRef - Protective effect of hypoglycemic granule against diabetes‐induced liver injury by alleviating glycolipid metabolic disorder and oxidative stress
Xiaosong Yang, Pengjie Zhang, Feixue Zhang, Zhiqiang Ke, Qingjie Chen, Chao Liu
Journal of Cellular Biochemistry.2020; 121(5-6): 3221. CrossRef - Candidate Regulators of Dyslipidemia in Chromosome 1 Substitution Lines Using Liver Co-Expression Profiling Analysis
Fuyi Xu, Maochun Wang, Shixian Hu, Yuxun Zhou, John Collyer, Kai Li, Hongyan Xu, Junhua Xiao
Frontiers in Genetics.2020;[Epub] CrossRef - Early detection of type 2 diabetes mellitus using machine learning-based prediction models
Leon Kopitar, Primoz Kocbek, Leona Cilar, Aziz Sheikh, Gregor Stiglic
Scientific Reports.2020;[Epub] CrossRef - Non-HDL-Cholesterin
Leonie Adam, Thomas Bobbert
Diabetes aktuell.2020; 18(06): 242. CrossRef - Berberine Suppresses Colonic Inflammation in Dextran Sulfate Sodium–Induced Murine Colitis Through Inhibition of Cytosolic Phospholipase A2 Activity
Lixiang Zhai, Tao Huang, Hai-tao Xiao, Pei-gen Wu, Cheng-yuan Lin, Zi-wan Ning, Ling Zhao, Hiu Yee Anna Kwan, Xian-jing Hu, Hoi Leong Xavier Wong, Xian-qian Li, Zhao-xiang Bian
Frontiers in Pharmacology.2020;[Epub] CrossRef - Effects of High-Fiber Biscuits on Lipid and Anthropometric Profile of Patients with Type 2 Diabetes
FATMAH
Journal of Nutritional Science and Vitaminology.2020; 66(Supplement): S391. CrossRef - Acute Myocardial Infarction Hospitalizations between Cold and Hot Seasons in an Island across Tropical and Subtropical Climate Zones—A Population-Based Study
Min-Liang Chu, Chiao-Yu Shih, Tsung-Cheng Hsieh, Han-Lin Chen, Chih-Wei Lee, Jen-Che Hsieh
International Journal of Environmental Research and Public Health.2019; 16(15): 2769. CrossRef - Hydroxyurea alters hematological, biochemical and inflammatory biomarkers in Brazilian children with SCA: Investigating associations with βS haplotype and α-thalassemia
Sètondji Cocou Modeste Alexandre Yahouédéhou, Caroline Conceição da Guarda, Camylla Vilas Boas Figueiredo, Rayra Pereira Santiago, Suellen Pinheiro Carvalho, Luciana Magalhães Fiuza, Uche Samuel Ndidi, Rodrigo Mota Oliveira, Magda Oliveira Seixas Carvalho
PLOS ONE.2019; 14(7): e0218040. CrossRef - Developmental Dioxin Exposure Alters the Methylome of Adult Male Zebrafish Gonads
Camille Akemann, Danielle N. Meyer, Katherine Gurdziel, Tracie R. Baker
Frontiers in Genetics.2019;[Epub] CrossRef - 1H NMR based serum metabolic profiling reveals differentiating biomarkers in patients with diabetes and diabetes-related complication
Atul Rawat, Gunjan Misra, Madhukar Saxena, Sukanya Tripathi, Durgesh Dubey, Sulekha Saxena, Avinash Aggarwal, Varsha Gupta, M.Y. Khan, Anand Prakash
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 290. CrossRef - Dietary calcium affects body composition and lipid metabolism in rats
Haya Alomaim, Philip Griffin, Eleonora Swist, Louise J. Plouffe, Michelle Vandeloo, Isabelle Demonty, Ashok Kumar, Jesse Bertinato, Juan J. Loor
PLOS ONE.2019; 14(1): e0210760. CrossRef - TyG index a promising biomarker for glycemic control in type 2 Diabetes Mellitus
Ekhlas Khalid Hameed
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 560. CrossRef - The association between exposure to different aspects of shift work and metabolic risk factors in health care workers, and the role of chronotype
Bette Loef, Debbie van Baarle, Allard J. van der Beek, Piet K. Beekhof, Linda W. van Kerkhof, Karin I. Proper, David Gatfield
PLOS ONE.2019; 14(2): e0211557. CrossRef - CHANGES IN PENTRAXIN-3 LEVEL AND ITS INTERACTION
WITH METABOLIC INDICES IN PATIENTS WITH CORONARY
ARTERY DISEASE AND TYPE 2 DIABETES MELLITUS
Pavlo G. Kravchun, Olga I. Kadykova, Dmitry G. Molotyagin
Wiadomości Lekarskie.2019; 72(2): 181. CrossRef - Glucose metabolic effects of oat noodles with different processing in type 2 diabetic mice
Lijuan Wang, Lili Wang, Nachuan Zhang, Mengli Li, Zaigui Li
Journal of Cereal Science.2019; 88: 125. CrossRef - Raffia palm (Raphia hookeri G. Mann & H. Wendl) wine modulates glucose homeostasis by enhancing insulin secretion and inhibiting redox imbalance in a rat model of diabetes induced by high fructose diet and streptozotocin
Ochuko L. Erukainure, Olajumoke A. Oyebode, Omamuyovwi M. Ijomone, Chika I. Chukwuma, Neil A. Koorbanally, Md. Shahidul Islam
Journal of Ethnopharmacology.2019; 237: 159. CrossRef - The Relation of Impaired Fasting Glucose and HDL-Cholesterol by Gender and Body Mass Index
Soo-Hee Jin
Journal of Health Informatics and Statistics.2019; 44(1): 8. CrossRef - The Effects of Poncirus fructus on Insulin Resistance and the Macrophage-Mediated Inflammatory Response in High Fat Diet-Induced Obese Mice
Mia Kim, Mi Hyeon Seol, Byung-Cheol Lee
International Journal of Molecular Sciences.2019; 20(12): 2858. CrossRef - HDL-Cholesterol, Its Variability, and the Risk of Diabetes: A Nationwide Population-Based Study
Seung-Hwan Lee, Hun-Sung Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Kyungdo Han, Mee Kyoung Kim
The Journal of Clinical Endocrinology & Metabolism.2019; 104(11): 5633. CrossRef - Cardiovascular organ damage in type 2 diabetes mellitus: the role of lipids and inflammation
Michaela Kozakova, Carmela Morizzo, Isabel Goncalves, Andrea Natali, Jan Nilsson, Carlo Palombo
Cardiovascular Diabetology.2019;[Epub] CrossRef - Determinants of poor glycemic control among adult patients with type 2 diabetes mellitus in Jimma University Medical Center, Jimma zone, south west Ethiopia: a case control study
Yitagesu Mamo, Fekede Bekele, Tadesse Nigussie, Ameha Zewudie
BMC Endocrine Disorders.2019;[Epub] CrossRef - Functional polymorphisms of the APOA1/C3/A4/A5-ZPR1-BUD13 gene cluster are associated with dyslipidemia in a sex-specific pattern
Wei Bai, Changgui Kou, Lili Zhang, Yueyue You, Weiying Yu, Wanqing Hua, Yuanyuan Li, Yaqin Yu, Tiancheng Zhao, Yanhua Wu
PeerJ.2019; 6: e6175. CrossRef - A pre-meal of whey proteins induces differential effects on glucose and lipid metabolism in subjects with the metabolic syndrome: a randomised cross-over trial
Ann Bjørnshave, Jens Juul Holst, Kjeld Hermansen
European Journal of Nutrition.2019; 58(2): 755. CrossRef - Aging and Hyperglycemia Intensify Dyslipidemia-Induced Oxidative Stress and Inflammation in Rats: Assessment of Restorative Potentials of ALA and EPA + DHA
Pooja Acharya, Ramaprasad Ravichandra Talahalli
Inflammation.2019; 42(3): 946. CrossRef - Diabetes Type 2 in Neurologically Impaired Children and Adolescents Without Obesity: A New Emerging Entity?
Valeria Calcaterra, Hellas Cena, Annalisa De Silvestri, Vincenza Girgenti, Denisia Bommarito, Gloria Pelizzo
Frontiers in Neurology.2019;[Epub] CrossRef - Raman spectral signatures of urinary extracellular vesicles from diabetic patients and hyperglycemic endothelial cells as potential biomarkers in diabetes
Maciej Roman, Agnieszka Kamińska, Anna Drożdż, Mark Platt, Marek Kuźniewski, Maciej T. Małecki, Wojciech M. Kwiatek, Czesława Paluszkiewicz, Ewa Ł. Stępień
Nanomedicine: Nanotechnology, Biology and Medicine.2019; 17: 137. CrossRef - Triglycerides and glucose index as an insulin resistance marker in a sample of healthy adults
Carlos J. Toro-Huamanchumo, Diego Urrunaga-Pastor, Mirella Guarnizo-Poma, Herbert Lazaro-Alcantara, Socorro Paico-Palacios, Betzi Pantoja-Torres, Vitalia del Carmen Ranilla-Seguin, Vicente A. Benites-Zapata
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 272. CrossRef - Effects of curcumin on glycemic control and lipid profile in prediabetes and type 2 diabetes mellitus: A systematic review and meta-analysis
Nalinee Poolsup, Naeti Suksomboon, Putu Dian Marani Kurnianta, Kulchalee Deawjaroen, Stephen L. Atkin
PLOS ONE.2019; 14(4): e0215840. CrossRef - Effects of different dietary regimes alone or in combination with standardized Aronia melanocarpa extract supplementation on lipid and fatty acids profiles in rats
Petar Milic, Jovana Jeremic, Vladimir Zivkovic, Ivan Srejovic, Nevena Jeremic, Jovana Bradic, Tamara Nikolic Turnic, Isidora Milosavljevic, Sergey Bolevich, Stefani Bolevich, Milica Labudovic Borovic, Aleksandra Arsic, Miroslav Mitrovic, Vladimir Jakovlje
Molecular and Cellular Biochemistry.2019; 461(1-2): 141. CrossRef - Repression of Transcriptional Activity of Forkhead Box O1 by Histone Deacetylase Inhibitors Ameliorates Hyperglycemia in Type 2 Diabetic Rats
Hyun Cho, Young Seok, Hae Lee, Minji Song, InKyeom Kim
International Journal of Molecular Sciences.2018; 19(11): 3539. CrossRef - Gender and Age Stratified Analyses of Nutrient and Dietary Pattern Associations with Circulating Lipid Levels Identify Novel Gender and Age-Specific Correlations
Huifeng Jin, Jessie Nicodemus-Johnson
Nutrients.2018; 10(11): 1760. CrossRef - Effect of Gum Arabic (Acacia Senegal) supplementation on visceral adiposity index (VAI) and blood pressure in patients with type 2 diabetes mellitus as indicators of cardiovascular disease (CVD): a randomized and placebo-controlled clinical trial
Rasha Babiker, Khalifa Elmusharaf, Michael B. Keogh, Amal M. Saeed
Lipids in Health and Disease.2018;[Epub] CrossRef - Silymarin prevents lipid accumulation in the liver of rats with type 2 diabetes via sirtuin1 and SREBP-1c
Nejat Kheiripour, Jamshid Karimi, Iraj Khodadadi, Heidar Tavilani, Mohammad Taghi Goodarzi, Mohammad Hashemnia
Journal of Basic and Clinical Physiology and Pharmacology.2018; 29(3): 301. CrossRef - Sex-specific relationship between visceral fat index and dyslipidemia in Chinese rural adults: The Henan Rural Cohort Study
Zhongyan Tian, Yuqian Li, Zhenxing Mao, Songcheng Yu, Yanhua Wang, Xiaotian Liu, Runqi Tu, Haiqing Zhang, Xinling Qian, Xia Zhang, Lulu Zhang, Jingzhi Zhao, Lei Yin, Chongjian Wang
Preventive Medicine.2018; 116: 104. CrossRef - The Lipid Side of Bone Marrow Adipocytes: How Tumor Cells Adapt and Survive in Bone
Jonathan D. Diedrich, Mackenzie K. Herroon, Erandi Rajagurubandara, Izabela Podgorski
Current Osteoporosis Reports.2018; 16(4): 443. CrossRef - Revisiting the Diabetes-Heart Failure Connection
Markus Wallner, Deborah M. Eaton, Dirk von Lewinski, Harald Sourij
Current Diabetes Reports.2018;[Epub] CrossRef - DNA methylation markers associated with type 2 diabetes, fasting glucose and HbA1c levels: a systematic review and replication in a case–control sample of the Lifelines study
Eliza Walaszczyk, Mirjam Luijten, Annemieke M. W. Spijkerman, Marc J. Bonder, Helen L. Lutgers, Harold Snieder, Bruce H. R. Wolffenbuttel, Jana V. van Vliet-Ostaptchouk
Diabetologia.2018; 61(2): 354. CrossRef - Ozone modifies the metabolic and endocrine response to glucose: Reproduction of effects with the stress hormone corticosterone
Errol M. Thomson, Shinjini Pilon, Josée Guénette, Andrew Williams, Alison C. Holloway
Toxicology and Applied Pharmacology.2018; 342: 31. CrossRef - Mechanisms and treatment of heart failure in diabetes
Joseph Timmons, Miles Fisher
Practical Diabetes.2018; 35(4): 117. CrossRef - Cyclocarya paliurus Leaves Tea Improves Dyslipidemia in Diabetic Mice: A Lipidomics-Based Network Pharmacology Study
Lixiang Zhai, Zi-wan Ning, Tao Huang, Bo Wen, Cheng-hui Liao, Cheng-yuan Lin, Ling Zhao, Hai-tao Xiao, Zhao-xiang Bian
Frontiers in Pharmacology.2018;[Epub] CrossRef - Actions of metformin and statins on lipid and glucose metabolism and possible benefit of combination therapy
Mariël F. van Stee, Albert A. de Graaf, Albert K. Groen
Cardiovascular Diabetology.2018;[Epub] CrossRef - Body composition analysis, anthropometric indices and lipid profile markers as predictors for prediabetes
Vineetha K. Ramdas Nayak, Kirtana Raghurama Nayak, Sudha Vidyasagar, Asha Kamath, Xiao-Feng Yang
PLOS ONE.2018; 13(8): e0200775. CrossRef - Effect of statins on fasting glucose in non-diabetic individuals: nationwide population-based health examination in Korea
Jinkwon Kim, Hye Sun Lee, Kyung-Yul Lee
Cardiovascular Diabetology.2018;[Epub] CrossRef - Antihyperlipidemic Activity ofArchidendron pauciflorumFruit Peel Extract in Streptozotocin-induced Diabetes Female Wistar Rats
Madihah, A. R Rahim, D. M Malini, W Hermawan
IOP Conference Series: Earth and Environmental Science.2018; 166: 012015. CrossRef - Prolactin regulatory element-binding (PREB) protein regulates hepatic glucose homeostasis
Joo-Man Park, Mi-Young Kim, Tae-Hyun Kim, Dong-Kook Min, Ga Eul Yang, Yong-Ho Ahn
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2018; 1864(6): 2097. CrossRef - Abnormalities in the relationship of paraoxonase 1 with HDL and apolipoprotein A1 and their possible connection to HDL dysfunctionality in type 2 diabetes
Alena Viktorinova, Ingrid Jurkovicova, Lubomira Fabryova, Sona Kinova, Michal Koren, Anna Stecova, Klara Svitekova
Diabetes Research and Clinical Practice.2018; 140: 174. CrossRef - Dietary stearic acid regulates mitochondria in vivo in humans
Deniz Senyilmaz-Tiebe, Daniel H. Pfaff, Sam Virtue, Kathrin V. Schwarz, Thomas Fleming, Sandro Altamura, Martina U. Muckenthaler, Jürgen G. Okun, Antonio Vidal-Puig, Peter Nawroth, Aurelio A. Teleman
Nature Communications.2018;[Epub] CrossRef - Diabetes Update 2017 – Lipide
K. G. Parhofer
Der Diabetologe.2017; 13(5): 313. CrossRef - Adipokines and free fatty acids regulate insulin sensitivity by increasing microRNA-21 expression in human mature adipocytes
Nannan Zhang, Naijian Zhang, Leilei Song, Hui Xie, Chao Zhao, Sujuan Li, Wenxi Zhao, Yaping Zhao, Chunlin Gao, Guangfeng Xu
Molecular Medicine Reports.2017; 16(2): 2254. CrossRef - Efficacy and safety of a combination of red yeast rice and olive extract in hypercholesterolemic patients with and without statin-associated myalgia
Christian Tshongo Muhindo, Sylvie A. Ahn, Michel F. Rousseau, Yvan Dierckxsens, Michel P. Hermans
Complementary Therapies in Medicine.2017; 35: 140. CrossRef - Independent relationship between serum ferritin levels and dyslipidemia in Chinese adults: A population study
Jiang Li, Weimin Bao, Tie Zhang, Yun Zhou, Hui Yang, Hongbing Jia, Rui Wang, Yongtong Cao, Cheng Xiao, Cheng Hu
PLOS ONE.2017; 12(12): e0190310. CrossRef - A Synthetic-Biology-Inspired Therapeutic Strategy for Targeting and Treating Hepatogenous Diabetes
Shuai Xue, Jianli Yin, Jiawei Shao, Yuanhuan Yu, Linfeng Yang, Yidan Wang, Mingqi Xie, Martin Fussenegger, Haifeng Ye
Molecular Therapy.2017; 25(2): 443. CrossRef - Klinische Bedeutung des HDL-Cholesterins
W. März, M. E. Kleber, H. Scharnagl, T. Speer, S. Zewinger, A. Ritsch, K. G. Parhofer, A. von Eckardstein, U. Landmesser, U. Laufs
Herz.2017; 42(1): 58. CrossRef - Increase in resting heart rate over 2 years predicts incidence of diabetes: A 10-year prospective study
G. Kim, Y.-h. Lee, J.Y. Jeon, H. Bang, B.-W. Lee, E.S. Kang, I.-K. Lee, B.-S. Cha, C.S. Kim
Diabetes & Metabolism.2017; 43(1): 25. CrossRef - A Potential of Coleus Tuberosus Crackers Rich in Resistant Starch Type 3 Improves Glucose and Lipid Profile of Alloxan –Induced Diabetic Mice
Mutiara Nugraheni, Siti Hamidah, Rizqie Auliana
Current Research in Nutrition and Food Science Journal.2017; 5(3): 308. CrossRef - Liver-adipose tissue crosstalk: A key player in the pathogenesis of glucolipid metabolic disease
De-wei Ye, Xiang-lu Rong, Ai-min Xu, Jiao Guo
Chinese Journal of Integrative Medicine.2017; 23(6): 410. CrossRef - Dyslipidaemia in type 2 diabetes mellitus
Niki Katsiki, Nikolaos Tentolouris, Dimitri P. Mikhailidis
Current Opinion in Cardiology.2017; 32(4): 422. CrossRef - The PDK1 Inhibitor Dichloroacetate Controls Cholesterol Homeostasis Through the ERK5/MEF2 Pathway
Abrar Ul Haq Khan, Nerea Allende-Vega, Delphine Gitenay, Sabine Gerbal-Chaloin, Claire Gondeau, Dang-Nghiem Vo, Sana Belkahla, Stefania Orecchioni, Giovanna Talarico, Francesco Bertolini, Milica Bozic, Jose M. Valdivielso, Fabienne Bejjani, Isabelle Jarie
Scientific Reports.2017;[Epub] CrossRef - Susceptibility background for type 2 diabetes in eleven Mexican Indigenous populations: HNF4A gene analysis
M. A. Granados-Silvestre, M. G. Ortiz-López, J. Granados, S. Canizales-Quinteros, Rosenda I. Peñaloza-Espinosa, C. Lechuga, V. Acuña-Alonzo, K. Sánchez-Pozos, M. Menjivar
Molecular Genetics and Genomics.2017; 292(6): 1209. CrossRef - Analysis of risk factors and their interactions in type 2 diabetes mellitus: A cross‐sectional survey in Guilin, China
Disha Zou, Yao Ye, Nina Zou, Jian Yu
Journal of Diabetes Investigation.2017; 8(2): 188. CrossRef - A Comparative Study of Metformin alone, in Combination with Insulin or Metformin Plus Insulin in Presence of Simvastatin in Libyan Diabetic Patients
Fathi M Sherif
Pharmacy & Pharmacology International Journal.2017;[Epub] CrossRef - HDL cholesterol: reappraisal of its clinical relevance
Winfried März, Marcus E. Kleber, Hubert Scharnagl, Timotheus Speer, Stephen Zewinger, Andreas Ritsch, Klaus G. Parhofer, Arnold von Eckardstein, Ulf Landmesser, Ulrich Laufs
Clinical Research in Cardiology.2017; 106(9): 663. CrossRef - Glucose and Lipid Dysmetabolism in a Rat Model of Prediabetes Induced by a High-Sucrose Diet
Ana Burgeiro, Manuela Cerqueira, Bárbara Varela-Rodríguez, Sara Nunes, Paula Neto, Frederico Pereira, Flávio Reis, Eugénia Carvalho
Nutrients.2017; 9(6): 638. CrossRef - Longitudinal trends in HbA1c and associations with comorbidity and all-cause mortality in Asian patients with type 2 diabetes: A cohort study
Miyang Luo, Wei Yen Lim, Chuen Seng Tan, Yilin Ning, Kee Seng Chia, Rob M. van Dam, Wern Ee Tang, Ngiap Chuan Tan, Richard Chen, E. Shyong Tai, Kavita Venkataraman
Diabetes Research and Clinical Practice.2017; 133: 69. CrossRef - Plasma Periostin Levels Are Increased in Chinese Subjects with Obesity and Type 2 Diabetes and Are Positively Correlated with Glucose and Lipid Parameters
Yuanyuan Luo, Hua Qu, Hang Wang, Huili Wei, Jing Wu, Yang Duan, Dan Liu, Huacong Deng
Mediators of Inflammation.2016; 2016: 1. CrossRef - Comprehensive assessment of lipoprotein subfraction profiles according to glucose metabolism status, and association with insulin resistance in subjects with early-stage impaired glucose metabolism
Jie-Eun Lee, Se Hee Min, Dong-Hwa Lee, Tae Jung Oh, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Kyong Soo Park, Hak Chul Jang, Soo Lim
International Journal of Cardiology.2016; 225: 327. CrossRef - Clinical benefits of pitavastatin: focus on patients with diabetes or at risk of developing diabetes
Vivencio Barrios, Carlos Escobar
Future Cardiology.2016; 12(4): 449. CrossRef - Triglyceride glucose index, a marker of insulin resistance, is associated with coronary artery stenosis in asymptomatic subjects with type 2 diabetes
Eun Young Lee, Hae Kyung Yang, Joonyub Lee, Borami Kang, Yeoree Yang, Seung-Hwan Lee, Seung-Hyun Ko, Yu-Bae Ahn, Bong Yun Cha, Kun-Ho Yoon, Jae Hyoung Cho
Lipids in Health and Disease.2016;[Epub] CrossRef - Clinical Update: Cardiovascular Disease in Diabetes Mellitus
Cecilia C. Low Wang, Connie N. Hess, William R. Hiatt, Allison B. Goldfine
Circulation.2016; 133(24): 2459. CrossRef - Role of growth hormone-releasing hormone in dyslipidemia associated with experimental type 1 diabetes
Maritza J. Romero, Rudolf Lucas, Huijuan Dou, Supriya Sridhar, Istvan Czikora, Eby M. Mosieri, Ferenc G. Rick, Norman L. Block, Subbaramiah Sridhar, David Fulton, Neal L. Weintraub, Zsolt Bagi, Andrew V. Schally
Proceedings of the National Academy of Sciences.2016; 113(7): 1895. CrossRef - Lipid changes during basal insulin peglispro, insulin glargine, or NPH treatment in six IMAGINE trials
Henry Ginsberg, Bertrand Cariou, Trevor Orchard, Lei Chen, Junxiang Luo, Edward J. Bastyr, Juliana Bue‐Valleskey, Annette M. Chang, Tibor Ivanyi, Scott J. Jacober, Byron J. Hoogwerf
Diabetes, Obesity and Metabolism.2016; 18(11): 1089. CrossRef - PCSK9-Inhibitoren bei Hypercholesterinämie
K. G. Parhofer
Herz.2016; 41(3): 217. CrossRef - Risk assessment and management of post-transplant diabetes mellitus
Eugene Han, Myoung Soo Kim, Yu Seun Kim, Eun Seok Kang
Metabolism.2016; 65(10): 1559. CrossRef - The changes of subtypes in pediatric diabetes and their clinical and laboratory characteristics over the last 20 years
Eun Byul Kwon, Hae Sang Lee, Young Seok Shim, Hwal Rim Jeong, Jin Soon Hwang
Annals of Pediatric Endocrinology & Metabolism.2016; 21(2): 81. CrossRef - 4-Hydroxyisoleucine: A Potential New Treatment for Type 2 Diabetes Mellitus
Mohammad Ishraq Zafar, Feng Gao
BioDrugs.2016; 30(4): 255. CrossRef
- Response surface methodology based development of an optimized polyherbal formulation and evaluation of its anti-diabetic and anti-obesity potential in high-fat diet-induced obese mice
- Clinical Usefulness of Serum Cystatin C as a Marker of Renal Function
- Kwang-Sook Woo, Jae-Lim Choi, Bo-Ram Kim, Ji-Eun Kim, Jin-Yeong Han
- Diabetes Metab J. 2014;38(4):278-284. Published online August 20, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.4.278
- 4,193 View
- 47 Download
- 24 Web of Science
- 26 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Accurate renal function measurements are important in the diagnosis and treatment of kidney diseases. In contrast to creatinine, the production of serum cystatin C has been extensively reported to be unaffected by body muscle mass, age, gender, and nutritional status.
Methods Our study included 37 samples from diabetic chronic kidney disease (CKD) patients for whom serum creatinine tests had been requested and 40 samples from a healthy populations in Dong-A University Hospital between May 2010 and June 2010. The assay precision (i.e., the coefficient of variation) and the reference range of the serum cystatin C test were evaluated. We compared the estimated glomerular filtration rates (GFRs) based on cystatin C with those based on creatinine. Moreover, we investigated the influences of age, gender, weight, and muscle mass on serum creatinine and serum cystatin C.
Results There was a positive correlation between GFR based on creatinine and that based on cystatin C (
r =0.79,P <0.0001) among the diabetic CKD patients. Serum creatinine and cystatin C were significantly correlated with body weight and muscle mass, but the strengths of these correlations were greater for serum creatinine. The precision study revealed excellent results for both the high and low controls. The 95% reference interval of cystatin C in the healthy population was 0.371 to 1.236 mg/L.Conclusion Based on these results, we conclude that, despite the strong correlation between serum creatinine and cystatin C, cystatin C is less affected by weight and muscle mass and might represent a better alternative for the assessment of renal function.
-
Citations
Citations to this article as recorded by- Dyslipidemia and serum cystatin C levels as biomarker of diabetic nephropathy in patients with type 2 diabetes mellitus
Tadesse Asmamaw Dejenie, Endeshaw Chekol Abebe, Misganaw Asmamaw Mengstie, Mohammed Abdu Seid, Natnael Atnafu Gebeyehu, Getachew Asmare Adella, Gizchew Ambaw Kassie, Amanuel Yosef Gebrekidan, Molalegn Mesele Gesese, Kirubel Dagnaw Tegegne, Denekew Tenaw A
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association between serum creatinine and type 2 diabetes in the Chinese population: a retrospective cohort study
Rugang Li, Min He, Qilin Yang, Zezhi Liang, Ying li, Ling Huang, Rong Wu, Jieping Huang
Scientific Reports.2023;[Epub] CrossRef - Significance of Diabetic Kidney Disease Biomarkers in Predicting Metabolic-Associated Fatty Liver Disease
Jaehyun Bae, Byung-Wan Lee
Biomedicines.2023; 11(7): 1928. CrossRef - Reconsideration of the current models of estimated kidney function‐based drug dose adjustment in older adults: The role of biological age
Radin Alikhani, Manjunath P. Pai
Clinical and Translational Science.2023; 16(11): 2095. CrossRef - The Level of Plasma Cystatin C in Patients with Chronic Kidney Disease
Tuan Nguyen Van, Linh Phan Ha, Diep Pham Thao, Minh Nguyen Thi Binh, Minh Hoang Thi, Thuan Huynh Quang, Lan Thi Phuong Dam
Nephro-Urology Monthly.2022;[Epub] CrossRef - Role of cystatin C in urogenital malignancy
Li Ding, Zijie Liu, Junqi Wang
Frontiers in Endocrinology.2022;[Epub] CrossRef - Comparison of cystatin C-based and creatinine-based glomerular filtration rate in the prediction of postoperative residual hypertension in aldosterone-producing adenoma patients after adrenalectomy
Ching-Way Chen, Cheng-Hsuan Tsai, Chi-Sheng Hung, I-Jung Tsai, Yu-Wei Chiu, Chin-Cheng Chang, Kao-Lang Liu, Shih-Cheng Liao, Vin-Cent Wu, Yen-Hung Lin
Clinica Chimica Acta.2021; 520: 147. CrossRef - Harmonizing acute and chronic kidney disease definition and classification: report of a Kidney Disease: Improving Global Outcomes (KDIGO) Consensus Conference
Norbert H. Lameire, Adeera Levin, John A. Kellum, Michael Cheung, Michel Jadoul, Wolfgang C. Winkelmayer, Paul E. Stevens, Fergus J. Caskey, Chris K.T. Farmer, Alejandro Ferreiro Fuentes, Masafumi Fukagawa, Stuart L. Goldstein, Grace Igiraneza, Andreas Kr
Kidney International.2021; 100(3): 516. CrossRef - Correlation of Serum Cystatin C with Renal Function in Gout Patients with Renal Injury
Yanqun Wu, Shunhua Wang, Xiaoqing Xu
Journal of Interferon & Cytokine Research.2021; 41(9): 329. CrossRef - Stressors and Resilience: An Integrative Model for Understanding Chronic Kidney Disease
Jacob Hwang, Arvin Jenab
Alternative and Complementary Therapies.2021; 27(6): 267. CrossRef - The role of serum cystatin C in estimation of renal function in survivors of critical illness
Jirarat Eiamcharoenying, Win Kulvichit, Nuttha Lumlertgul, Tawatchai Chaiwatanarat, Sadudee Peerapornratana, Nattachai Srisawat
Journal of Critical Care.2020; 59: 201. CrossRef - Clinician perspectives on inpatient cystatin C utilization: A qualitative case study at Mayo Clinic
James Roland Markos, Karen S. Schaepe, Hilary R. Teaford, Andrew D. Rule, Kianoush B. Kashani, John C. Lieske, Erin F. Barreto, Pierre Delanaye
PLOS ONE.2020; 15(12): e0243618. CrossRef - Influence of Anthropometric Measurements on Serum Creatinine, Urea and eGFR in Healthy Adolescent Subjects
Kavita Rasalkar, Nagaraju Kashamsetty, Bandi Sai Karthik
Journal of Evidence Based Medicine and Healthcare.2020; 7(36): 1917. CrossRef - Biology and Management of Navel Orangeworm (Lepidoptera: Pyralidae) in California
Houston Wilson, Charles S Burks, Joshua E Reger, Jacob A Wenger, Kelly Tindall
Journal of Integrated Pest Management.2020;[Epub] CrossRef - Low serum creatinine and risk of diabetes: The Japan Epidemiology Collaboration on Occupational Health Study
Huanhuan Hu, Tohru Nakagawa, Toru Honda, Shuichiro Yamamoto, Hiroko Okazaki, Makoto Yamamoto, Toshiaki Miyamoto, Masafumi Eguchi, Takeshi Kochi, Makiko Shimizu, Taizo Murakami, Kentaro Tomita, Takayuki Ogasawara, Naoko Sasaki, Akihiko Uehara, Keisuke Kuwa
Journal of Diabetes Investigation.2019; 10(5): 1209. CrossRef - Comparison of monitoring techniques in and near almonds and pistachios under mating disruption treatment for navel orangeworm
C. Burks, B. Higbee, J. Beck
Acta Horticulturae.2018; (1219): 331. CrossRef - Evaluation of creatinine-based and cystatin C-based equations for estimation of glomerular filtration rate in type 1 diabetic patients
Caroline Pereira Domingueti, Rodrigo Bastos Fóscolo, Ana Cristina Simões e Silva, Luci Maria S. Dusse, Janice Sepúlveda Reis, Maria das Graças Carvalho, Ana Paula Fernandes, Karina Braga Gomes
Archives of Endocrinology and Metabolism.2016; 60(2): 108. CrossRef - Diagnostic Accuracy of Serum Cystatin C for the Evaluation of Renal Dysfunction in Diabetic Patients: A Meta‐Analysis
Shi‐kun Yang, Jun Liu, Xian‐ming Zhang, Chun Hu, Wei Zhang, Lin Sun, Hao Zhang
Therapeutic Apheresis and Dialysis.2016; 20(6): 579. CrossRef - Treatable glomerular hyperfiltration in patients with active acromegaly
Shingo Fujio, Koji Takano, Hiroshi Arimura, Mika Habu, Manoj Bohara, Horofumi Hirano, Ryosuke Hanaya, Yoshihiko Nishio, Chihaya Koriyama, Yasuyuki Kinoshita, Kazunori Arita
European Journal of Endocrinology.2016; 175(4): 325. CrossRef - Glomerular filtration rate assessed by using creatinine and cystatin in patients treated with dabigatran
Gianluca Gessoni, Sara Valverde, Francesca Gessoni, Letizia Valle, Marina Bortolotti, Vincenzo Lidestri, Michele Urso, Roberto Valle
La Rivista Italiana della Medicina di Laboratorio - Italian Journal of Laboratory Medicine.2016; 12(4): 243. CrossRef - СHARACTERISTICS OF THE HEART FATTY ACID-BINDING PROTEIN, INTERLEUKIN-6 AND INTERLEUKIN-8 AS ALTERNATIVE MARKERS OF DIABETIC NEPHROPATHY PROGRESSION IN PATIENTS WITH TYPE 1 DIABETES MELLITUS
Yu. A. Ryzhikova, I. N. Vorozhtsova, T. V. Saprina, V. D. Zavadovskaya, A. B. Merinov, I. V. Kulagina
Bulletin of Siberian Medicine.2015; 14(5): 61. CrossRef - Performance of Cystatin C– and Creatinine-Based Estimated Glomerular Filtration Rate Equations Depends on Patient Characteristics
Jeffrey W Meeusen, Andrew D Rule, Nikolay Voskoboev, Nikola A Baumann, John C Lieske
Clinical Chemistry.2015; 61(10): 1265. CrossRef - Comparison and evaluation of lupus nephritis response criteria in lupus activity indices and clinical trials
Kristin M Corapi, Mary Anne Dooley, William F Pendergraft
Arthritis Research & Therapy.2015;[Epub] CrossRef - Evaluation of Serum Cystatin C as a Marker of Early Renal Impairment in Patients with Liver Cirrhosis
Mahmoud Omar, Wael Abdel-Razek, Gamal Abo-Raia, Medhat Assem, Gasser El-Azab
International Journal of Hepatology.2015; 2015: 1. CrossRef - Efficient expression, purification and characterization of native human cystatin C in Escherichia coli periplasm
Yongjun Zhou, Yan Zhou, Jun Li, Jian Chen, Yuqin Yao, Lin Yu, Desheng Peng, Mingrong Wang, Dan Su, Yong He, Lantu Gou
Protein Expression and Purification.2015; 111: 18. CrossRef - Comparison of Carvedilol and Metoprolol for Preventing Contrast-Induced Nephropathy after Coronary Angiography
Mustafa Yılmaz, Alp Aydınalp, Kaan Okyay, Abdullah Tekin, Uğur Abbas Bal, Nilüfer Bayraktar, Aylin Yıldırır, Haldun Müderrisoğlu
Cardiorenal Medicine.2015; 5(3): 199. CrossRef
- Dyslipidemia and serum cystatin C levels as biomarker of diabetic nephropathy in patients with type 2 diabetes mellitus
- Statin Discontinuation after Achieving a Target Low Density Lipoprotein Cholesterol Level in Type 2 Diabetic Patients without Cardiovascular Disease: A Randomized Controlled Study
- Seung-Hwan Lee, Hyuk-Sang Kwon, Yong-Moon Park, Seung-Hyun Ko, Yoon-Hee Choi, Kun-Ho Yoon, Yu-Bae Ahn
- Diabetes Metab J. 2014;38(1):64-73. Published online February 19, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.1.64
- 3,909 View
- 48 Download
- 16 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background This study investigated the rate of relapse of dyslipidemia and the factors which could predict relapse following a short-term statin discontinuation after achieving a target low density lipoprotein cholesterol (LDL-C) level in type 2 diabetic patients without cardiovascular disease (CVD).
Methods Ninety-nine subjects on rosuvastatin treatment and whose LDL-C level was lower than 100 mg/dL were randomly assigned to discontinue or maintain statin treatment at a 2:1 ratio. The subjects were followed-up after 10 weeks. A relapse of dyslipidemia was defined as a reascent of LDL-C level to greater than 100 mg/dL.
Results The statin discontinuation group had a significant rate of relapse compared to the maintenance group (79% vs. 3%, respectively). Pretreatment and baseline lipid levels, their ratios, and hemoglobin A1c level were significantly different between the relapse and nonrelapse groups. The pretreatment and baseline lipid profiles and their ratios were independently associated with relapse. The pretreatment LDL-C level was the most useful parameter for predicting a relapse, with a cutoff of 123 mg/dL. During the follow-up period, no CVD event was noted.
Conclusion The relapse rate of dyslipidemia was high when statins were discontinued in type 2 diabetic patients without CVD. Statin discontinuation should be considered carefully based on the pretreatment lipid profiles of patients.
-
Citations
Citations to this article as recorded by- Cardiovascular Outcomes and Mortality Associated With Discontinuing Statins in Older Patients Receiving Polypharmacy
Federico Rea, Annalisa Biffi, Raffaella Ronco, Matteo Franchi, Simona Cammarota, Anna Citarella, Valeria Conti, Amelia Filippelli, Carmine Sellitto, Giovanni Corrao
JAMA Network Open.2021; 4(6): e2113186. CrossRef - Visit-to-visit variability of lipid measurements and the risk of myocardial infarction and all-cause mortality: A prospective cohort study
Xiaoxue Liu, Shouling Wu, Qiaofeng Song, Xizhu Wang
Atherosclerosis.2020; 312: 110. CrossRef - 2018 Guidelines for the management of dyslipidemia
Eun-Jung Rhee, Hyeon Chang Kim, Jae Hyeon Kim, Eun Young Lee, Byung Jin Kim, Eun Mi Kim, YoonJu Song, Jeong Hyun Lim, Hae Jin Kim, Seonghoon Choi, Min Kyong Moon, Jin Oh Na, Kwang-Yeol Park, Mi Sun Oh, Sang Youb Han, Junghyun Noh, Kyung Hee Yi, Sang-Hak L
The Korean Journal of Internal Medicine.2019; 34(4): 723. CrossRef - 2018 Guidelines for the Management of Dyslipidemia in Korea
Eun-Jung Rhee, Hyeon Chang Kim, Jae Hyeon Kim, Eun Young Lee, Byung Jin Kim, Eun Mi Kim, YoonJu Song, Jeong Hyun Lim, Hae Jin Kim, Seonghoon Choi, Min Kyong Moon, Jin Oh Na, Kwang-Yeol Park, Mi Sun Oh, Sang Youb Han, Junghyun Noh, Kyung Hee Yi, Sang-Hak L
Journal of Lipid and Atherosclerosis.2019; 8(2): 78. CrossRef - Patterns of statin use and long‐term adherence and persistence among older adults with diabetes
Richard Ofori‐Asenso, Jenni Ilomäki, Mark Tacey, Ella Zomer, Andrea J. Curtis, J. Simon Bell, Sophia Zoungas, Danny Liew
Journal of Diabetes.2018; 10(9): 699. CrossRef - Effect of visit-to-visit LDL-, HDL-, and non-HDL-cholesterol variability on mortality and cardiovascular outcomes after percutaneous coronary intervention
Eun Young Lee, Yeoree Yang, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Wook Sung Chung, Seung-Hwan Lee, Kiyuk Chang
Atherosclerosis.2018; 279: 1. CrossRef - Change in ALT levels after administration of HMG‐CoA reductase inhibitors to subjects with pretreatment levels three times the upper normal limit in clinical practice
Hyunah Kim, Hyeseon Lee, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung‐Hwan Lee, Jae‐Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun‐Ho Yoon, Hun‐Sung Kim
Cardiovascular Therapeutics.2018;[Epub] CrossRef - Orthodox religious fasting as a medical nutrition therapy for dyslipidemia: where do we stand and how far can we go?
Theocharis Koufakis, Spyridon N Karras, Pantelis Zebekakis, Kalliopi Kotsa
European Journal of Clinical Nutrition.2018; 72(4): 474. CrossRef - Phenotyping of Korean patients with better-than-expected efficacy of moderate-intensity statins using tensor factorization
Jingyun Choi, Yejin Kim, Hun-Sung Kim, In Young Choi, Hwanjo Yu, Katriina Aalto-Setala
PLOS ONE.2018; 13(6): e0197518. CrossRef - Impact of educational outreach intervention on enhancing health care providers' knowledge about statin therapy prescribing in Malaysian patients with type 2 diabetes mellitus
Mohamed Hassan Elnaem, Mohamad Haniki Nik Mohamed, Hasniza Zaman Huri, Shah M Azarisman
Journal of Evaluation in Clinical Practice.2018; 24(3): 521. CrossRef - Use of Moderate‐Intensity Statins for Low‐Density Lipoprotein Cholesterol Level above 190 mg/dL at Baseline in Koreans
Hun‐Sung Kim, Hyeseon Lee, Sue Hyun Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Sun Jung Baik, Hyunah Kim, Seung‐Hwan Lee, Jae Hyoung Cho, In‐Young Choi, Kun‐Ho Yoon, Ju Han Kim
Basic & Clinical Pharmacology & Toxicology.2017; 121(4): 272. CrossRef - Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study
Mee Kyoung Kim, Kyungdo Han, Hun-Sung Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
European Heart Journal.2017; 38(48): 3560. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - The differences in the incidence of diabetes mellitus and prediabetes according to the type of HMG-CoA reductase inhibitors prescribed in Korean patients
Tong Min Kim, Hyunah Kim, Yoo Jin Jeong, Sun Jung Baik, So Jung Yang, Seung-Hwan Lee, Jae-Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun-Ho Yoon, Hun-Sung Kim
Pharmacoepidemiology and Drug Safety.2017; 26(10): 1156. CrossRef - Statin for the Primary Prevention of Cardiovascular Disease in Patients with Diabetes Mellitus
Bo Kyung Koo
Diabetes & Metabolism Journal.2014; 38(1): 32. CrossRef
- Cardiovascular Outcomes and Mortality Associated With Discontinuing Statins in Older Patients Receiving Polypharmacy

 KDA
KDA
 First
First Prev
Prev





