
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
- Hepatic Fibrosis and Cancer: The Silent Threats of Metabolic Syndrome
- Scott L. Friedman
- Diabetes Metab J. 2024;48(2):161-169. Published online January 26, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0240
- 2,465 View
- 294 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
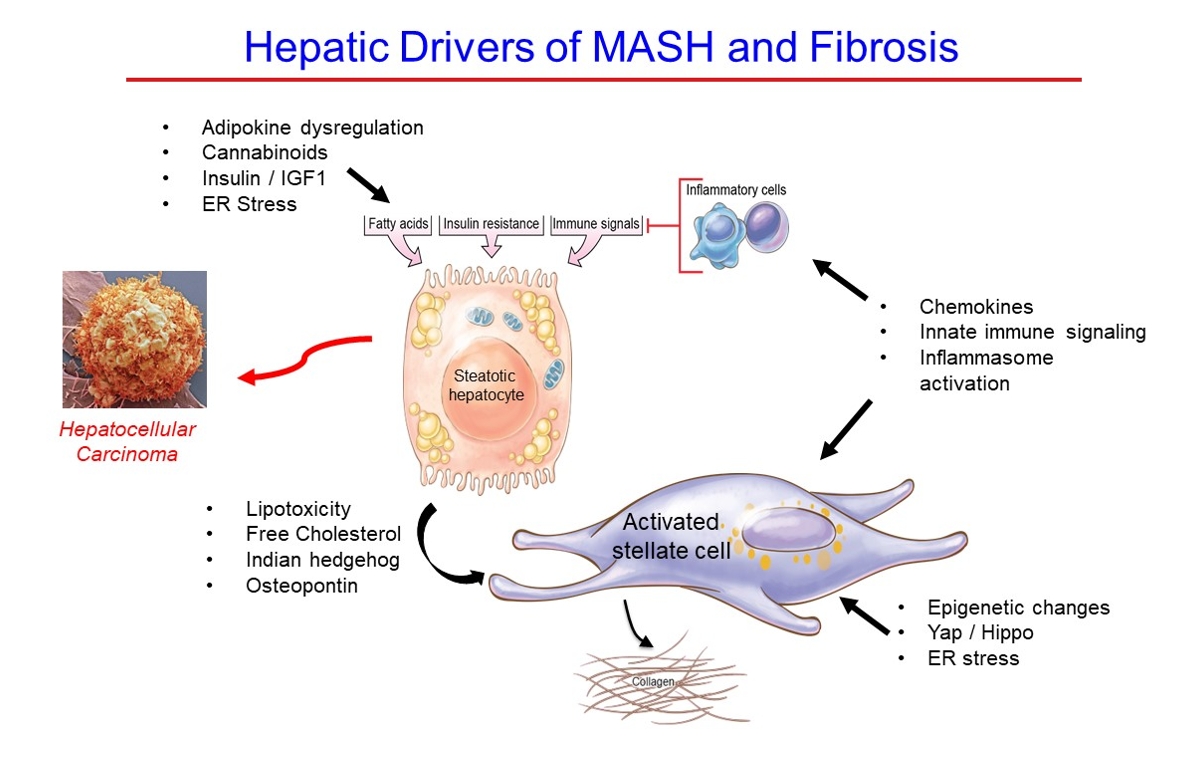
ePub - Metabolic dysfunction-associated steatotic (fatty) liver disease (MASLD), previously termed non-alcoholic fatty liver disease, is a worldwide epidemic that can lead to hepatic inflammation, fibrosis, cirrhosis, and hepatocellular carcinoma (HCC). The disease is typically a component of the metabolic syndrome that accompanies obesity, and is often overlooked because the liver manifestations are clinically silent until late-stage disease is present (i.e., cirrhosis). Moreover, Asian populations, including Koreans, have a higher fraction of patients who are lean, yet their illness has the same prognosis or worse than those who are obese. Nonetheless, ongoing injury can lead to hepatic inflammation and ballooning of hepatocytes as classic features. Over time, fibrosis develops following activation of hepatic stellate cells, the liver’s main fibrogenic cell type. The disease is usually more advanced in patients with type 2 diabetes mellitus, indicating that all diabetic patients should be screened for liver disease. Although there has been substantial progress in clarifying pathways of injury and fibrosis, there no approved therapies yet, but current research seeks to uncover the pathways driving hepatic inflammation and fibrosis, in hopes of identifying new therapeutic targets. Emerging molecular methods, especially single cell sequencing technologies, are revolutionizing our ability to clarify mechanisms underlying MASLD-associated fibrosis and HCC.
- Metabolic Risk/Epidemiology
- Association of Measures of Glucose Metabolism with Colorectal Cancer Risk in Older Chinese: A 13-Year Follow-up of the Guangzhou Biobank Cohort Study-Cardiovascular Disease Substudy and Meta-Analysis
- Shu Yi Wang, Wei Sen Zhang, Chao Qiang Jiang, Ya Li Jin, Tong Zhu, Feng Zhu, Lin Xu
- Diabetes Metab J. 2024;48(1):134-145. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0383

- 1,158 View
- 141 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Abnormal glucose metabolism is a risk factor for colorectal cancer (CRC). However, association of glycosylated hemoglobin (HbA1c) with CRC risk remains under-reported. We examined the association between glycemic indicators (HbA1c, fasting plasma glucose, fasting insulin, 2-hour glucose, 2-hour insulin, and homeostasis model of risk assessment-insulin resistance index) and CRC risk using prospective analysis and meta-analysis.
Methods
Participants (n=1,915) from the Guangzhou Biobank Cohort Study-Cardiovascular Disease Substudy were included. CRC events were identified through record linkage. Cox regression was used to assess the associations of glycemic indicators with CRC risk. A meta-analysis was performed to investigate the association between HbA1c and CRC risk.
Results
During an average of 12.9 years follow-up (standard deviation, 2.8), 42 incident CRC cases occurred. After adjusting for potential confounders, the hazard ratio (95% confidence interval [CI]) of CRC for per % increment in HbA1c was 1.28 (95% CI, 1.01 to 1.63) in overall population, 1.51 (95% CI, 1.13 to 2.02) in women and 1.06 (95% CI, 0.68 to 1.68) in men. No significant association of other measures of glycemic indicators and baseline diabetes with CRC risk was found. Meta-analyses of 523,857 participants including our results showed that per % increment of HbA1c was associated with 13% higher risk of CRC, with the pooled risk ratio being 1.13 (95% CI, 1.01 to 1.27). Subgroupanalyses found stronger associations in women, colon cancer, Asians, and case-control studies.
Conclusion
Higher HbA1c was a significant predictor of CRC in the general population. Our findings shed light on the pathology of glucose metabolism and CRC, which warrants more in-depth investigation.
- Pathophysiology
- Immune-Checkpoint Inhibitors-Induced Type 1 Diabetes Mellitus: From Its Molecular Mechanisms to Clinical Practice
- Yun Kyung Cho, Chang Hee Jung
- Diabetes Metab J. 2023;47(6):757-766. Published online July 24, 2023
- DOI: https://doi.org/10.4093/dmj.2023.0072
- 2,851 View
- 330 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
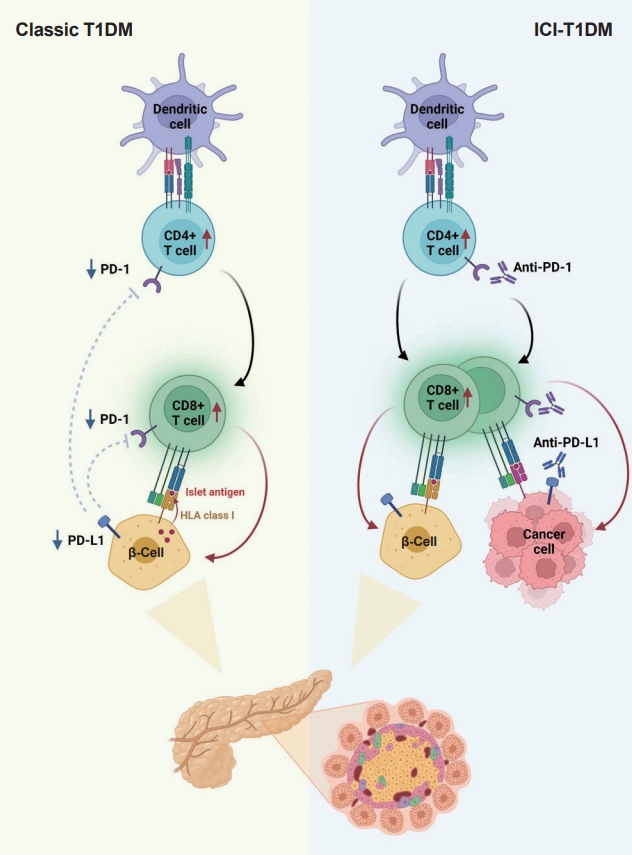
ePub - With the increasing use of immune-checkpoint inhibitors (ICIs), such as anti-cytotoxic T lymphocyte-associated antigen 4 (CTLA-4) and anti-programmed cell death-1 (PD-1), for the treatment of malignancies, cases of ICI-induced type 1 diabetes mellitus (ICI-T1DM) have been reported globally. This review focuses on the features and pathogenesis of this disease. T1DM is an immune-related adverse event that occurs following the administration of anti-PD-1 or anti-programmed death ligand-1 (PDL1) alone or in combination with anti-CTLA-4. More than half of the reported cases presented as abrupt-onset diabetic ketoacidosis. The primary mechanism of ICI-T1DM is T-cell stimulation, which results from the loss of interaction between PD-1 and PD-L1 in pancreatic islet. The similarities and differences between ICI-T1DM and classical T1DM may provide insights into this disease entity. ICI-T1DM is a rare but often life-threatening medical emergency that healthcare professionals and patients need to be aware of. Early detection of and screening for this disease is imperative. At present, the only known treatment for ICI-T1DM is insulin injection. Further research into the mechanisms and risk factors associated with ICI-T1DM development may contribute to a better understanding of this disease entity and the identification of possible preventive strategies.
-
Citations
Citations to this article as recorded by- Research Advances of Immune Checkpoint Inhibitors Related Endocrine Adverse Events
晶晶 王
Advances in Clinical Medicine.2024; 14(02): 2706. CrossRef - Immune checkpoint inhibitor‑associated diabetes mellitus in patients with HCC: Report of three cases and literature review
Gaocheng Wang, Jingjing Wang, Shuilin Dong, Zhanguo Zhang, Wanguang Zhang, Jianping Zhao
Experimental and Therapeutic Medicine.2024;[Epub] CrossRef
- Research Advances of Immune Checkpoint Inhibitors Related Endocrine Adverse Events
- Metabolic risk/Epidemiology
- Obesity, Diabetes, and Increased Cancer Progression
- Dae-Seok Kim, Philipp E. Scherer
- Diabetes Metab J. 2021;45(6):799-812. Published online November 22, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0077

- 14,241 View
- 669 Download
- 71 Web of Science
- 77 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 
- Rates of obesity and diabetes have increased significantly over the past decades and the prevalence is expected to continue to rise further in the coming years. Many observations suggest that obesity and diabetes are associated with an increased risk of developing several types of cancers, including liver, pancreatic, endometrial, colorectal, and post-menopausal breast cancer. The path towards developing obesity and diabetes is affected by multiple factors, including adipokines, inflammatory cytokines, growth hormones, insulin resistance, and hyperlipidemia. The metabolic abnormalities associated with changes in the levels of these factors in obesity and diabetes have the potential to significantly contribute to the development and progression of cancer through the regulation of distinct signaling pathways. Here, we highlight the cellular and molecular pathways that constitute the links between obesity, diabetes, cancer risk and mortality. This includes a description of the existing evidence supporting the obesity-driven morphological and functional alternations of cancer cells and adipocytes through complex interactions within the tumor microenvironment.
-
Citations
Citations to this article as recorded by- Triglyceride‐glucose index (TyG index) and endometrial carcinoma risk: A retrospective cohort study
Haimeng Shi, Feifei Guo, Kang Zheng, Rong Li, Huaijun Zhou
International Journal of Gynecology & Obstetrics.2024; 164(1): 298. CrossRef - Association between total cholesterol levels and all-cause mortality among newly diagnosed patients with cancer
Seohyun Kim, Gyuri Kim, So Hyun Cho, Rosa Oh, Ji Yoon Kim, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Scientific Reports.2024;[Epub] CrossRef - The Role of Adipokines in Tumor Progression and Its Association with Obesity
Jae Won Kim, Jun Hyeok Kim, Yoon Jae Lee
Biomedicines.2024; 12(1): 97. CrossRef - Triglyceride-glucose index is a risk factor for breast cancer in China: a cross-sectional study
Jinghua Zhang, Binbin Yin, Ya Xi, Yongying Bai
Lipids in Health and Disease.2024;[Epub] CrossRef - Insulin Resistance: The Increased Risk of Cancers
Leszek Szablewski
Current Oncology.2024; 31(2): 998. CrossRef - Epigenetic modifications in obesity‐associated diseases
Yiqian Long, Chao Mao, Shuang Liu, Yongguang Tao, Desheng Xiao
MedComm.2024;[Epub] CrossRef - The Juncture of Diabetes, Cancer, and Observational Population-based Studies: Novel Insights From Canadian Provincial Health Records
Terra Arnason, Kerry Mansell
Canadian Journal of Diabetes.2024; 48(3): 145. CrossRef - The impact of chemotherapy on adipose tissue remodeling: The molecular players involved in this tissue wasting
Samuel Barbosa, Mafalda Barbosa Pedrosa, Rita Ferreira, Daniel Moreira-Gonçalves, Lúcio Lara Santos
Biochimie.2024; 223: 1. CrossRef - Epidemiological and transcriptome data identify shared gene signatures and immune cell infiltration in type 2 diabetes and non-small cell lung cancer
Qian Yuan, Long Li, Liu-shun Wang, Shi-gui Xing
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - THE INFLUENCE OF DIABETES-ASSOCIATED FACTORS OF ONCOGENESIS ON THE RISK OF BREAST AND ENDOMETRIAL CANCER AND ON THE SURVIVAL OF WOMEN WITH THIS CANCER
Tamara S. Vatseba, Liubov K. Sokolova, Vasyl Ye. Neyko, Valentyna V. Dzvonkovska, Oksana V. Muravlova, Volodymyr V. Derpak
Clinical and Preventive Medicine.2024; (2): 99. CrossRef - Associations between diabetes and cancer: A 10-year national population-based retrospective cohort study
Heléna Safadi, Ágnes Balogh, Judit Lám, Attila Nagy, Éva Belicza
Diabetes Research and Clinical Practice.2024; 211: 111665. CrossRef - Colorectal Cancer: Epidemiology, Risk Factors, and Prevention
Gholamreza Roshandel, Fatemeh Ghasemi-Kebria, Reza Malekzadeh
Cancers.2024; 16(8): 1530. CrossRef - Metabolic Alteration Bridging the Prediabetic State and Colorectal Cancer
Antonino Colloca, Isabella Donisi, Camilla Anastasio, Maria Luisa Balestrieri, Nunzia D’Onofrio
Cells.2024; 13(8): 663. CrossRef - Changes in physical activity and diabetes risk after cancer diagnosis: a nationwide cohort study
Wonyoung Jung, In Young Cho, Jinhyung Jung, Mi Hee Cho, Hye Yeon Koo, Yong-Moon Mark Park, Jong-Ha Baek, Kyungdo Han, Dong Wook Shin
Journal of Cancer Survivorship.2024;[Epub] CrossRef - Stratification and prognostic evaluation of breast cancer subtypes defined by obesity-associated genes
Dongjuan Chen, Zilu Xie, Jun Yang, Ting Zhang, Qiliang Xiong, Chen Yi, Shaofeng Jiang
Discover Oncology.2024;[Epub] CrossRef - Ultra‐processed food consumption and the risk of pancreatic cancer in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial
Guo‐Chao Zhong, Qian Zhu, Dong Cai, Jie‐Jun Hu, Xin Dai, Jian‐Ping Gong, Wei‐Ping Sun
International Journal of Cancer.2023; 152(5): 835. CrossRef - Advances in “adiponcosis”: Insights in the inner mechanisms at the base of adipose and tumour tissues interplay
Cristina Pagano, Erika di Zazzo, Giorgio Avilia, Beatrice Savarese, Giovanna Navarra, Maria Chiara Proto, Donatella Fiore, Monica Rienzo, Patrizia Gazzerro, Chiara Laezza, Maurizio Bifulco
International Journal of Cancer.2023; 152(12): 2464. CrossRef - Metabolites as signalling molecules
Steven Andrew Baker, Jared Rutter
Nature Reviews Molecular Cell Biology.2023; 24(5): 355. CrossRef - Characterization of neuroendocrine regulation- and metabolism-associated molecular features and prognostic indicators with aid to clinical chemotherapy and immunotherapy of patients with pancreatic cancer
Biao Zhang, Qihang Yuan, Bolin Zhang, Shuang Li, Zhizhou Wang, Hangyu Liu, Fanyue Meng, Xu Chen, Dong Shang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Concentration of Selected Adipokines and Factors Regulating Carbohydrate Metabolism in Patients with Head and Neck Cancer in Respect to Their Body Mass Index
Jarosław Nuszkiewicz, Jolanta Czuczejko, Wiktor Dróżdż, Alina Woźniak, Bogdan Małkowski, Karolina Szewczyk-Golec
International Journal of Molecular Sciences.2023; 24(4): 3283. CrossRef - Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - A novel five-gene metabolism-related risk signature for predicting prognosis and immune infiltration in endometrial cancer: A TCGA data mining
Huaqing Huang, Xintong Cai, Jiexiang Lin, Qiaoling Wu, Kailin Zhang, Yibin Lin, Bin Liu, Jie Lin
Computers in Biology and Medicine.2023; 155: 106632. CrossRef - Green Antimicrobials as Therapeutic Agents for Diabetic Foot Ulcers
Ines D. Teixeira, Eugenia Carvalho, Ermelindo C. Leal
Antibiotics.2023; 12(3): 467. CrossRef - Impact of abdominal obesity on the risk of glioma development in patients with diabetes: A nationwide population-based cohort study in Korea
Hyunji Sang, Yun Kyung Cho, Kyungdo Han, Eun Hee Koh, Sandar Tin Tin
PLOS ONE.2023; 18(3): e0283023. CrossRef - Relationship Between Physical Exercise and Cognitive Impairment Among Older Adults with Type 2 Diabetes: Chain Mediating Roles of Sleep Quality and Depression
Han Zhang, Yefan Zhang, Sen Sheng, Yang Xing, Zhongchen Mou, Yanqiu Zhang, Zhixue Shi, Zhenjie Yu, Qianqian Gao, Weiqin Cai, Qi Jing
Psychology Research and Behavior Management.2023; Volume 16: 817. CrossRef - The Mediterranean Lifestyle to Contrast Low-Grade Inflammation Behavior in Cancer
Rosa Divella, Graziella Marino, Stefania Infusino, Laura Lanotte, Gaia Gadaleta-Caldarola, Gennaro Gadaleta-Caldarola
Nutrients.2023; 15(7): 1667. CrossRef - Distribution of ABO blood groups and Rh factor in benign and malign thyroid nodules
Muzaffer Serdar DENİZ
Journal of Health Sciences and Medicine.2023; 6(2): 462. CrossRef - The Role of Selected Adipocytokines in Ovarian Cancer and Endometrial Cancer
Sebastian Stępień, Paweł Olczyk, Joanna Gola, Katarzyna Komosińska-Vassev, Aleksandra Mielczarek-Palacz
Cells.2023; 12(8): 1118. CrossRef - Coronary Revascularization in Patients With Cancer
Bala Pushparaji, Teodora Donisan, Dinu Valentin Balanescu, Jong Kun Park, Dominique J. Monlezun, Abdelrahman Ali, Ibrahim Halil Inanc, Jaime Caballero, Mehmet Cilingiroglu, Konstantinos Marmagkiolis, Cezar Iliescu
Current Treatment Options in Cardiovascular Medicine.2023; 25(6): 143. CrossRef - Hepatocellular carcinoma in a large cohort of type 2 diabetes patients
Carlo B. Giorda, Roberta Picariello, Barbara Tartaglino, Elisa Nada, Giuseppe Costa, Roberta Manti, Luca Monge, Roberto Gnavi
Diabetes Research and Clinical Practice.2023; 200: 110684. CrossRef - Prediction of Hypoglycemia in Diabetic Patients During Colonoscopy
Preparation
Xiaohua Lu, Lingqiao Xie, Wane Zhao, Chuangbiao Zhang, Xixi Luo, Yan Zhou
Experimental and Clinical Endocrinology & Diabetes.2023; 131(05): 274. CrossRef - Interplay of skeletal muscle and adipose tissue: sarcopenic obesity
Min Jeong Park, Kyung Mook Choi
Metabolism.2023; 144: 155577. CrossRef - PIK3CA mutation in endometriotic epithelial cells promotes viperin-dependent inflammatory response to insulin
Mike R. Wilson, Shannon Harkins, Jake J. Reske, Rebecca A. Siwicki, Marie Adams, Victoria L. Bae-Jump, Jose M. Teixeira, Ronald L. Chandler
Reproductive Biology and Endocrinology.2023;[Epub] CrossRef - The Function of MondoA and ChREBP Nutrient—Sensing Factors in Metabolic Disease
Byungyong Ahn
International Journal of Molecular Sciences.2023; 24(10): 8811. CrossRef - Mechanism of Cephalophyllum cephalus Intervention in Diabetes Based on Network Pharmacology and Molecular Docking Technology
志梁 范
Hans Journal of Medicinal Chemistry.2023; 11(02): 81. CrossRef - Development and validation of a prognostic model based on metabolic risk score to predict overall survival of endometrial cancer in Chinese patients
Xingchen Li, Xiao Yang, Yuan Cheng, Yangyang Dong, Jingyuan Wang, Jianliu Wang
Journal of Gynecologic Oncology.2023;[Epub] CrossRef - Nε-(1-Carboxymethyl)-L-lysine, an advanced glycation end product, exerts malignancy on chondrosarcoma via the activation of cancer stemness
Ting-Yu Chang, Kuo-Cheng Lan, Chia-Hung Wu, Meei-Ling Sheu, Rong-Sen Yang, Shing-Hwa Liu
Archives of Toxicology.2023; 97(8): 2231. CrossRef - The Link between Diabetes, Pancreatic Tumors, and miRNAs—New Players for Diagnosis and Therapy?
Małgorzata Kozłowska, Agnieszka Śliwińska
International Journal of Molecular Sciences.2023; 24(12): 10252. CrossRef - Obesity, diabetes, and cancer: epidemiology, pathophysiology, and potential interventions
Leonardo de Andrade Mesquita, Laura Fink Wayerbacher, Gilberto Schwartsmann, Fernando Gerchman
Archives of Endocrinology and Metabolism.2023;[Epub] CrossRef - Distinct Lipid Phenotype of Cancer-Associated Fibroblasts (CAFs) Isolated From Overweight/Obese Endometrial Cancer Patients as Assessed Using Raman Spectroscopy
Tze Hua Yeu, Intan Sofia Omar, S.F. Abdul Sani, Dharini Pathmanathan, Boon Tong Goh, Nithyialakshmi Ravindran, Ik Hui Teo, Yogeeta Gunasagran, Noor Azmi Mat Adenan, Ivy Chung, Amira Hajirah Abd Jamil
Applied Spectroscopy.2023; 77(7): 723. CrossRef - Global, Regional, and National Epidemiology of Diabetes in Children From 1990 to 2019
Kexin Zhang, Chengxia Kan, Fang Han, Jingwen Zhang, Chuanhua Ding, Zhentao Guo, Na Huang, Yang Zhang, Ningning Hou, Xiaodong Sun
JAMA Pediatrics.2023; 177(8): 837. CrossRef - The effects of physical exercise therapy on weight control: its regulation of adipocyte physiology and metabolic capacity
Hyun Jung Park, Sung Ja Rhie, Insop Shim
Journal of Exercise Rehabilitation.2023; 19(3): 141. CrossRef - The Ephrin tyrosine kinase a3 (EphA3) is a novel mediator of RAGE-prompted motility of breast cancer cells
Marianna Talia, Francesca Cirillo, Asia Spinelli, Azzurra Zicarelli, Domenica Scordamaglia, Lucia Muglia, Salvatore De Rosis, Damiano Cosimo Rigiracciolo, Gianfranco Filippelli, Ida Daniela Perrotta, Mariano Davoli, Rosanna De Rosa, Rachele Macirella, Elv
Journal of Experimental & Clinical Cancer Research.2023;[Epub] CrossRef - Signal detection in real‐world data and confirmation in clinical trials: Diabetes as a case study for a conversation worth having
Elad Sharon, Megan Othus, Zoe Eloise Quandt
Cancer.2023; 129(18): 2769. CrossRef - Ultra-Processed Food Consumption and Obesity in Korean Adults
Jee-Seon Shim, Kyoung Hwa Ha, Dae Jung Kim, Hyeon Chang Kim
Diabetes & Metabolism Journal.2023; 47(4): 547. CrossRef - Decoding the role of leptin and adiponectin in obesity-related gastrointestinal cancer
Vanda Marques, Fabiola Arella, Marta B. Afonso, André A. Santos, Cecília M.P. Rodrigues
Clinical Science.2023; 137(15): 1095. CrossRef - Diabetes and two kinds of primary tumors in a patient with thalassemia: a case report and literature review
Xiaoyan Yu, Yi Peng, Tingting Nie, Wenjia Sun, Yajuan Zhou
Frontiers in Oncology.2023;[Epub] CrossRef - Additive impact of diabetes and sarcopenia on all-cause and cardiovascular mortality: A longitudinal nationwide population-based study
Eyun Song, Soon Young Hwang, Min Jeong Park, Ahreum Jang, Kyeong Jin Kim, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Metabolism.2023; 148: 155678. CrossRef - Obesity and Colorectal Cancer
Jundeok Lee, Su Young Kim
The Korean Journal of Gastroenterology.2023; 82(2): 63. CrossRef - Cognitive Behavioural Therapies for Weight-Loss in Adults: A Scoping Review Protocol
Laura María Compañ-Gabucio, Diana Mancheño-Bañón, Laura Torres-Collado, Jesús Vioque, Manuela García-de-la-Hera
Healthcare.2023; 11(18): 2473. CrossRef - Saxagliptin, a selective dipeptidyl peptidase-4 inhibitor, alleviates somatic cell aneugenicity and clastogenicity in diabetic mice
Sabry M. Attia, Sheikh F. Ahmad, Ahmed Nadeem, Mohamed S.M. Attia, Mushtaq A. Ansari, Abdelkader E. Ashour, Norah A. Albekairi, Mohammed A. Al-Hamamah, Ali A. Alshamrani, Saleh A. Bakheet
Mutation Research/Genetic Toxicology and Environmental Mutagenesis.2023; 892: 503707. CrossRef - Mechanisms of Linggui Zhugan Decoction in the Treatment of Obesity Based on Network Pharmacology
Chunmei Liu, Li Zhang, Yubin Yang
Science of Advanced Materials.2023; 15(9): 1265. CrossRef - Beyond Body Size: Adiponectin as a Key Player in Obesity-Driven Cancers
Maurizio Capuozzo, Venere Celotto, Loris Landi, Francesco Ferrara, Francesco Sabbatino, Francesco Perri, Marco Cascella, Vincenza Granata, Mariachiara Santorsola, Alessandro Ottaiano
Nutrition and Cancer.2023; 75(10): 1848. CrossRef - Impact of sarcopenic obesity on post-hepatectomy bile leakage for hepatocellular carcinoma
Hikaru Hayashi, Akira Shimizu, Koji Kubota, Tsuyoshi Notake, Hitoshi Masuo, Takahiro Yoshizawa, Kiyotaka Hosoda, Hiroki Sakai, Koya Yasukawa, Yuji Soejima, Ezio Lanza
PLOS ONE.2023; 18(10): e0286353. CrossRef - Colorectal Cancer: From Risk Factors to Oncogenesis
Vlad Alexandru Ionescu, Gina Gheorghe, Nicolae Bacalbasa, Alexandru Laurentiu Chiotoroiu, Camelia Diaconu
Medicina.2023; 59(9): 1646. CrossRef - The impact of poor metabolic health on aggressive breast cancer: adipose tissue and tumor metabolism
Barbara Mensah Sankofi, Estefania Valencia-Rincón, Malika Sekhri, Adriana L. Ponton-Almodovar, Jamie J. Bernard, Elizabeth A. Wellberg
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association of nonalcoholic fatty liver disease and growth hormone deficiency: a systematic review and meta-analysis
Tingting Kong, Yunpeng Gu, Lei Sun, Run Zhou, Jie Li, Junping Shi
Endocrine Journal.2023; 70(10): 959. CrossRef - Impact of Caloric Restriction in Breast Cancer Patients Treated with Neoadjuvant Chemotherapy: A Prospective Case Control Study
Isabella Castellano, Francesco Gallo, Paola Durelli, Taira Monge, Maurizio Fadda, Jasna Metovic, Paola Cassoni, Fulvio Borella, Carlo Raucci, Monica Menischetti, Alessandra Beano, Giuseppe Migliaretti, Concetta Finocchiaro
Nutrients.2023; 15(21): 4677. CrossRef - Metabolomic and lipidomic studies on the intervention of taurochenodeoxycholic acid in mice with hyperlipidemia
Na Cui, Wensen Zhang, Fazhi Su, Zhihong Zhang, Biao Li, Donghui Peng, Yanping Sun, Yuanning Zeng, Bingyou Yang, Haixue Kuang, Qiuhong Wang
Frontiers in Pharmacology.2023;[Epub] CrossRef - Is MG53 a potential therapeutic target for cancer?
Yunyu Du, Tieying Li, Muqing Yi
Frontiers in Endocrinology.2023;[Epub] CrossRef - Blood Biomarkers Panels for Screening of Colorectal Cancer and Adenoma on a Machine Learning-Assisted Detection Platform
Hui Wang, Zhiwei Zhou, Haijun Li, Weiguang Xiang, Yilin Lan, Xiaowen Dou, Xiuming Zhang
Cancer Control.2023;[Epub] CrossRef - Post-treatment serum triglyceride: An effective biomarker for body fat mass and overall survival in esophageal squamous cell cancer patients treated with chemoradiotherapy
Jiahua Lyu, Ningjing Yang, Wang Guan, Ling Xiao, Xinyu Nie, Long Liang, Hansong Bai, Churong Li, Hao Kuang, Xiao Wang, Tao Li
Frontiers in Nutrition.2022;[Epub] CrossRef - Research Progress of MicroRNA-122 in Obesity and Type 2 Diabetes
路路 潘
Advances in Clinical Medicine.2022; 12(06): 5706. CrossRef - Cancer and Obesity: An Obesity Medicine Association (OMA) Clinical Practice Statement (CPS) 2022
Ethan Lazarus, Harold Edward Bays
Obesity Pillars.2022; 3: 100026. CrossRef - Obesity Fact Sheet in Korea, 2021: Trends in Obesity Prevalence and Obesity-Related Comorbidity Incidence Stratified by Age from 2009 to 2019
Ye Seul Yang, Byoung-Duck Han, Kyungdo Han, Jin-Hyung Jung, Jang Won Son
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 169. CrossRef - Fried food consumption and the risk of pancreatic cancer: A large prospective multicenter study
Guo-Chao Zhong, Qian Zhu, Jian-Ping Gong, Dong Cai, Jie-Jun Hu, Xin Dai, Jun-Hua Gong
Frontiers in Nutrition.2022;[Epub] CrossRef - Intermittent Fasting Is Associated With a Decreased Risk of Age-Related Macular Degeneration
Eun Young Choi, Min Kim, Christopher Seungkyu Lee, Suk Ho Byeon, Sung Soo Kim, Minyoung Lee
American Journal of Ophthalmology.2022; 243: 1. CrossRef - Metformin Mitigated Obesity-Driven Cancer Aggressiveness in Tumor-Bearing Mice
Chun-Jung Chen, Chih-Cheng Wu, Cheng-Yi Chang, Jian-Ri Li, Yen-Chuan Ou, Wen-Ying Chen, Su-Lan Liao, Jiaan-Der Wang
International Journal of Molecular Sciences.2022; 23(16): 9134. CrossRef - Visceral fat area and body fat percentage measured by bioelectrical impedance analysis correlate with glycometabolism
Shuying Li, Shaoping Li, Jie Ding, Weihong Zhou
BMC Endocrine Disorders.2022;[Epub] CrossRef - Insight on the Role of Leptin: A Bridge from Obesity to Breast Cancer
Roberto Buonaiuto, Fabiana Napolitano, Sara Parola, Pietro De Placido, Valeria Forestieri, Giovanna Pecoraro, Alberto Servetto, Luigi Formisano, Pietro Formisano, Mario Giuliano, Grazia Arpino, Sabino De Placido, Carmine De Angelis
Biomolecules.2022; 12(10): 1394. CrossRef - Adipokines as Regulators of Autophagy in Obesity-Linked Cancer
Alin García-Miranda, Alejandra Garcia-Hernandez, Eduardo Castañeda-Saucedo, Napoleon Navarro-Tito, Paola Maycotte
Cells.2022; 11(20): 3230. CrossRef - Roles of hydroxyeicosatetraenoic acids in diabetes (HETEs and diabetes)
Linyue Dong, Heyao Wang, Kaixian Chen, Yiming Li
Biomedicine & Pharmacotherapy.2022; 156: 113981. CrossRef - Changes in the Fecal Metabolome Accompany an Increase in Aberrant Crypt Foci in the Colon of C57BL/6 Mice Fed with a High-Fat Diet
Huawei Zeng, Bryan D. Safratowich, Wen-Hsing Cheng, Andrew D. Magnuson, Matthew J. Picklo
Biomedicines.2022; 10(11): 2891. CrossRef - Targeting Adiponectin in Breast Cancer
Rawan Nehme, Mona Diab-Assaf, Caroline Decombat, Laetitia Delort, Florence Caldefie-Chezet
Biomedicines.2022; 10(11): 2958. CrossRef - Multidisciplinary Progress in Obesity Research
Xiaoqing Lu, Yuxin Jin, Dexin Li, Jingxin Zhang, Jingyan Han, Yin Li
Genes.2022; 13(10): 1772. CrossRef - The association between serum copper and obesity and all-cause mortality: the NHANES 2011–2016
Hongrong Wu, Qingqi Li, Kaifang Zhang, Jianfeng Zhao
Environmental Science and Pollution Research.2022; 30(11): 31395. CrossRef - The crosstalk within the breast tumor microenvironment in type II diabetes: Implications for cancer disparities
Christina S. Ennis, Pablo Llevenes, Yuhan Qiu, Ruben Dries, Gerald V. Denis
Frontiers in Endocrinology.2022;[Epub] CrossRef
- Triglyceride‐glucose index (TyG index) and endometrial carcinoma risk: A retrospective cohort study
- Pathophysiology
- Hyperinsulinemia in Obesity, Inflammation, and Cancer
- Anni M.Y. Zhang, Elizabeth A. Wellberg, Janel L. Kopp, James D. Johnson
- Diabetes Metab J. 2021;45(3):285-311. Published online March 29, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0250
- Correction in: Diabetes Metab J 2021;45(4):622
- 23,327 View
- 904 Download
- 81 Web of Science
- 88 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 
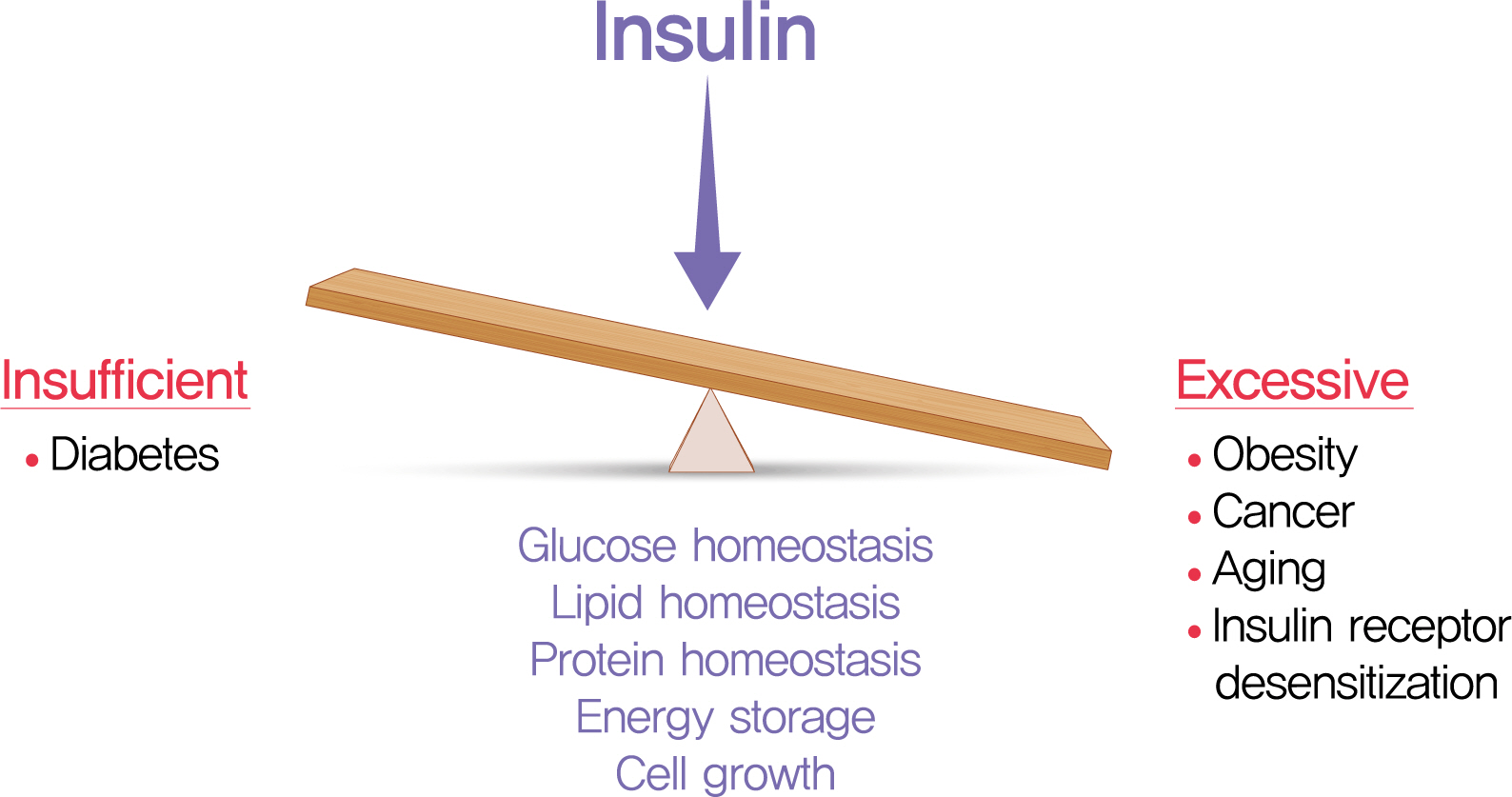
- The relative insufficiency of insulin secretion and/or insulin action causes diabetes. However, obesity and type 2 diabetes mellitus can be associated with an absolute increase in circulating insulin, a state known as hyperinsulinemia. Studies are beginning to elucidate the cause-effect relationships between hyperinsulinemia and numerous consequences of metabolic dysfunctions. Here, we review recent evidence demonstrating that hyperinsulinemia may play a role in inflammation, aging and development of cancers. In this review, we will focus on the consequences and mechanisms of excess insulin production and action, placing recent findings that have challenged dogma in the context of the existing body of literature. Where relevant, we elaborate on the role of specific signal transduction components in the actions of insulin and consequences of chronic hyperinsulinemia. By discussing the involvement of hyperinsulinemia in various metabolic and other chronic diseases, we may identify more effective therapeutics or lifestyle interventions for preventing or treating obesity, diabetes and cancer. We also seek to identify pertinent questions that are ripe for future investigation.
-
Citations
Citations to this article as recorded by- High adherence to Western dietary pattern increases breast cancer risk (an EPIC-Spain study)
Adela Castelló, Miguel Rodríguez-Barranco, Virginia Lope, Marcela Guevara, Sandra Colorado-Yohar, Ane Dorronsoro, José Ramón Quirós, Carlota Castro-Espin, Carmen Sayon-Orea, Carmen Santiuste, Pilar Amiano, Cristina Lasheras, María-José Sanchez, Marina Pol
Maturitas.2024; 179: 107868. CrossRef - Dietary Diabetes Risk Reduction Score (DDRRS) and Breast Cancer Risk: A Case-Control Study in Iran
Milad Mohammadzadeh, Alireza Bahrami, Fatemeh Abdi, Fatemeh Ghafouri-Taleghani, Amin Paydareh, Saba Jalali, Zeinab Heidari, Bahram Rashidkhani
Nutrition and Cancer.2024; 76(1): 106. CrossRef - White adipocyte dysfunction and obesity-associated pathologies in humans
Carolina E. Hagberg, Kirsty L. Spalding
Nature Reviews Molecular Cell Biology.2024; 25(4): 270. CrossRef - Cumulative exposure to impaired fasting glucose and gastrointestinal cancer risk: A nationwide cohort study
Byeong Yun Ahn, Bokyung Kim, Sanghyun Park, Sang Gyun Kim, Kyungdo Han, Soo‐Jeong Cho
Cancer.2024;[Epub] CrossRef - Leptin receptor deficiency impedes metabolic surgery related-weight loss through inhibition of energy expenditure in db/db mice
Dan Tong, Jie Xiang, Wei Liu, Fang Sun, Lijuan Wang, Aidi Mou, Tingbing Cao, Qing Zhou, Mei You, Yingying Liao, Peng Gao, Daoyan Liu, Zongshi Lu, Zhiming Zhu
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - Obesity and Cancer Rehabilitation for Functional Recovery and Quality of Life in Breast Cancer Survivors: A Comprehensive Review
Lorenzo Lippi, Alessandro de Sire, Arianna Folli, Alessio Turco, Stefano Moalli, Marco Marcasciano, Antonio Ammendolia, Marco Invernizzi
Cancers.2024; 16(3): 521. CrossRef - Exploring the Role of Hyperinsulinemia in Obesity-Associated Tumor Development
Ericka Vélez-Bonet, Kristyn Gumpper-Fedus, Zobeida Cruz-Monserrate
Cancer Research.2024; 84(3): 351. CrossRef - Exploring Promising Therapies for Non-Alcoholic Fatty Liver Disease: A ClinicalTrials.gov Analysis
Omar Hegazi, Samer Alalalmeh, Moyad Shahwan, Ammar Jairoun, Mansour Alourfi, Ghfran Bokhari, Abdullah Alkhattabi, Saeed Alsharif, Mohannad Aljehani, Abdulmalik Alsabban, Mohammad Almtrafi, Ysear Zakri, Abdullah AlMahmoud, Khalid Alghamdi, Ahmed Ashour, Na
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 545. CrossRef - Predictors of Cardiac Autonomic Dysfunction in Obesity-Related Hypertension
Aqsa Mujaddadi, Saima Zaki, Majumi M Noohu, Irshad Husain Naqvi, Zubia Veqar
High Blood Pressure & Cardiovascular Prevention.2024; 31(1): 77. CrossRef - The obesity-autophagy-cancer axis: Mechanistic insights and therapeutic perspectives
Amir Barzegar Behrooz, Marco Cordani, Alessandra Fiore, Massimo Donadelli, Joseph W. Gordon, Daniel J. Klionsky, Saeid Ghavami
Seminars in Cancer Biology.2024; 99: 24. CrossRef - Metformin’s role in lowering colorectal cancer risk among individuals with diabetes from the Southern Community Cohort Study
Thomas Lawler, Zoe L. Walts, Lauren Giurini, Mark Steinwandel, Loren Lipworth, Harvey J. Murff, Wei Zheng, Shaneda Warren Andersen
Cancer Epidemiology.2024; 90: 102566. CrossRef - Sex differences in insulin regulation of skeletal muscle glycogen synthase and changes during weight loss and exercise in adults
Alice S. Ryan, Guoyan Li, Shawna McMillin, Heidi K. Ortmeyer
Obesity.2024; 32(4): 667. CrossRef - Therapeutic Repurposing of Antidiabetic Drugs in Diabetes-associated
Comorbidities
Kalyani Pathak, Manash Pratim Pathak, Riya Saikia, Urvashee Gogoi, Ratna Jyoti Das, Pompy Patowary, Partha Pratim Kaishap, Smita Bordoloi, Jyotirmoy Das, Himangshu Sarma, Mohammad Zaki Ahmad, Aparoop Das
Current Drug Therapy.2024; 19(2): 178. CrossRef - The effect of metabolic syndrome on prognosis of diffuse large B-cell lymphoma
Wenjing Xiong, Liru Li, Xue Hui, Yue Liu, Hongbin Li, Yue Zhang, Shu Zhao
Clinical and Translational Oncology.2024;[Epub] CrossRef - Impact of Obesity-Related Endoplasmic Reticulum Stress on Cancer and Associated Molecular Targets
Joud AlBashtawi, Hend Al-Jaber, Sara Ahmed, Layla Al-Mansoori
Biomedicines.2024; 12(4): 793. CrossRef - Healthcare Management of an Obese Person
Syeda Rida Baqir, Shafaque Aslam Khan, Bushra Marium Zaman, Tahira Hamid Ali, Nazish Saeed Bangash, Muhammad Amjad Ali, Fatima Zaidi, Jahan Ara Farooq
DIET FACTOR (Journal of Nutritional and Food Sciences).2024; : 10. CrossRef - Associations between diabetes and cancer: A 10-year national population-based retrospective cohort study
Heléna Safadi, Ágnes Balogh, Judit Lám, Attila Nagy, Éva Belicza
Diabetes Research and Clinical Practice.2024; 211: 111665. CrossRef - Advances in “adiponcosis”: Insights in the inner mechanisms at the base of adipose and tumour tissues interplay
Cristina Pagano, Erika di Zazzo, Giorgio Avilia, Beatrice Savarese, Giovanna Navarra, Maria Chiara Proto, Donatella Fiore, Monica Rienzo, Patrizia Gazzerro, Chiara Laezza, Maurizio Bifulco
International Journal of Cancer.2023; 152(12): 2464. CrossRef - Influence of antidiabetic drugs on glucose metabolism and immune response in patients with metastatic pancreatic ductal adenocarcinoma receiving gemcitabine plus nab-paclitaxel as first-line treatment
Andrea Pretta, Pina Ziranu, Riccardo Giampieri, Clelia Donisi, Erika Cimbro, Dario Spanu, Eleonora Lai, Federica Pecci, Francesca Balconi, Alessio Lupi, Marta Pozzari, Mara Persano, Sara Murgia, Valeria Pusceddu, Marco Puzzoni, Rossana Berardi, Mario Scar
Digestive and Liver Disease.2023; 55(5): 655. CrossRef - Islet amyloid polypeptide does not suppress pancreatic cancer
Austin J. Taylor, Evgeniy Panzhinskiy, Paul C. Orban, Francis C. Lynn, David F. Schaeffer, James D. Johnson, Janel L. Kopp, C. Bruce Verchere
Molecular Metabolism.2023; 68: 101667. CrossRef - Pathophysiology of obesity and its associated diseases
Xin Jin, Tingting Qiu, Li Li, Rilei Yu, Xiguang Chen, Changgui Li, Christopher G. Proud, Tao Jiang
Acta Pharmaceutica Sinica B.2023; 13(6): 2403. CrossRef - Metabolic syndrome as a risk factor for oncogenesis
M.A. Osadchuk, I.N. Vasilieva, V.V. Kozlov, O.I. Mitrokhina
Profilakticheskaya meditsina.2023; 26(1): 70. CrossRef - Polycystic ovary syndrome: Causes, symptoms, pathophysiology, and remedies
Ananya Chaudhuri
Obesity Medicine.2023; 39: 100480. CrossRef - Metformin and long non-coding RNAs in breast cancer
Morteza Gholami, Zeynab Nickhah Klashami, Pirooz Ebrahimi, Amir Ali Mahboobipour, Amir Salehi Farid, Aida Vahidi, Marziyeh Zoughi, Mojgan Asadi, Mahsa M. Amoli
Journal of Translational Medicine.2023;[Epub] CrossRef - Host-Related Factors in the Interplay among Inflammation, Immunity and Dormancy in Breast Cancer Recurrence and Prognosis: An Overview for Clinicians
Lorenzo Ruggieri, Anna Moretti, Rossana Berardi, Maria Silvia Cona, Davide Dalu, Cecilia Villa, Davide Chizzoniti, Sheila Piva, Anna Gambaro, Nicla La Verde
International Journal of Molecular Sciences.2023; 24(5): 4974. CrossRef - Degree of obesity and gastrointestinal adverse reactions influence the weight loss effect of liraglutide in overweight or obese patients with type 2 diabetes
Fang Zhou, Lu Jiang, Jiamei Guo, Yuting Fan, Qin Pan, Tianlian Li, Xiaoshi Sun, Ping Li
Therapeutic Advances in Chronic Disease.2023; 14: 204062232311615. CrossRef - Both early and late maternal age at childbirth is associated with increasing odds of central obesity in offspring
Hongyun Chen, Yinhua Feng, Changying Chen, Songcheng Yu
American Journal of Human Biology.2023;[Epub] CrossRef - Integrated Physiology of the Exocrine and Endocrine Compartments in Pancreatic Diseases: Workshop Proceedings
Teresa L. Mastracci, Minoti Apte, Laufey T. Amundadottir, Alexandra Alvarsson, Steven Artandi, Melena D. Bellin, Ernesto Bernal-Mizrachi, Alejandro Caicedo, Martha Campbell-Thompson, Zobeida Cruz-Monserrate, Abdelfattah El Ouaamari, Kyle J. Gaulton, Andre
Diabetes.2023; 72(4): 433. CrossRef - Obesity-induced changes in cancer cells and their microenvironment: Mechanisms and therapeutic perspectives to manage dysregulated lipid metabolism
Miriam Lee-Rueckert, Marina Canyelles, Mireia Tondo, Noemi Rotllan, Petri T. Kovanen, Vicenta Llorente-Cortes, Joan Carles Escolà-Gil
Seminars in Cancer Biology.2023; 93: 36. CrossRef - PIK3CA mutation in endometriotic epithelial cells promotes viperin-dependent inflammatory response to insulin
Mike R. Wilson, Shannon Harkins, Jake J. Reske, Rebecca A. Siwicki, Marie Adams, Victoria L. Bae-Jump, Jose M. Teixeira, Ronald L. Chandler
Reproductive Biology and Endocrinology.2023;[Epub] CrossRef - Gut microbiome modified by bariatric surgery improves insulin sensitivity and correlates with increased brown fat activity and energy expenditure
Jitender Yadav, Tao Liang, Tairan Qin, Nayanan Nathan, Katherine J.P. Schwenger, Lauren Pickel, Li Xie, Helena Lei, Daniel A. Winer, Heather Maughan, Susan J. Robertson, Minna Woo, Wendy Lou, Kate Banks, Timothy Jackson, Allan Okrainec, Susy S. Hota, Susa
Cell Reports Medicine.2023; 4(5): 101051. CrossRef - Prevalence of Type 2 Diabetes, Impaired Fasting Glucose, and Diabetes Risk in an Adult and Older North-Eastern Portuguese Population
Pedro M. Magalhães, José E. Teixeira, João P. Bragada, Carlos M. Duarte, José A. Bragada
Healthcare.2023; 11(12): 1712. CrossRef - Hyperinsulinemia Influences the Short-Term Efficiency of Laparoscopic Sleeve Gastrectomy for Patients with Obesity and Insulin Resistance
Zilong Yue, Long Qian, Yan Jin, Yabin Xia, Hui Sha, Qin Wu, Kaifeng Hu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 1745. CrossRef - Acetyl-11-Keto-Beta-Boswellic Acid Has Therapeutic Benefits for NAFLD Rat Models That Were Given a High Fructose Diet by Ameliorating Hepatic Inflammation and Lipid Metabolism
Reza Ataei Kachouei, Alireza Doagoo, Maral Jalilzadeh, Seyyed Hossein Khatami, Shima Rajaei, Ali Jahanbazi Jahan-Abad, Farzaneh Salmani, Roya Pakrad, Somayeh Mahmoodi Baram, Mitra Nourbakhsh, Mohammad-Amin Abdollahifar, Hojjat Allah Abbaszadeh, Shokoofeh
Inflammation.2023; 46(5): 1966. CrossRef - Cancer Risk and its Association With Diabetes Mellitus in Patients With Acromegaly: A Two Center-based Study
Zhe-Hao Xiao, Cheng Wang, Yong Wang, Shang-Kun Yuan, Cheng Huang, Ren-Fang Chen, Yong Li
Endocrine Practice.2023; 29(9): 699. CrossRef - Obesity, diabetes, and cancer: epidemiology, pathophysiology, and potential interventions
Leonardo de Andrade Mesquita, Laura Fink Wayerbacher, Gilberto Schwartsmann, Fernando Gerchman
Archives of Endocrinology and Metabolism.2023;[Epub] CrossRef - Insulin Stimulates IL-23 Expression in Human Adipocytes: A Possible Explanation for the Higher Prevalence of Psoriasis in Obesity
Angelo Di Vincenzo, Marnie Granzotto, Marika Crescenzi, Camilla Costa, Stefano Piaserico, Vincenzo Vindigni, Roberto Vettor, Marco Rossato
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 1885. CrossRef - Immunometabolic aspects of chronic nonspecific inflammation in obesity
O. V. Skvortsova, N. B. Migacheva, E. G. Mikhailova
Meditsinskiy sovet = Medical Council.2023; (12): 75. CrossRef - The Reponic Classification of Insulin
Joshua Moen
Canadian Journal of Diabetes.2023; 47(8): 680. CrossRef - Dietary Acid Load and Cancer Risk: A Review of the Uruguayan Experience
Alvaro Luis Ronco, Maximilian Andreas Storz
Nutrients.2023; 15(14): 3098. CrossRef - Non-alcoholic fatty liver disease and diabetes mellitus as growing aetiologies of hepatocellular carcinoma
Stephanie Talamantes, Michela Lisjak, Eduardo H. Gilglioni, Camilo J. Llamoza-Torres, Bruno Ramos-Molina, Esteban N. Gurzov
JHEP Reports.2023; 5(9): 100811. CrossRef - Alteration of Metabolic Syndrome Is Associated with the Decreased Risk of Colorectal Cancer
Eun Hyo Jin, Yoon Jin Choi, Joo Hyun Lim, Cheol Min Shin, Kyungdo Han, Dong Ho Lee
Journal of Clinical Medicine.2023; 12(15): 4889. CrossRef - Dietary interventions improve diabetic kidney disease, but not peripheral neuropathy, in a db/db mouse model of type 2 diabetes
Stephanie A. Eid, Phillipe D. O'Brien, Katharina H. Kretzler, Dae‐Gyu Jang, Faye E. Mendelson, John M. Hayes, Andrew Carter, Hongyu Zhang, Subramaniam Pennathur, Frank C. Brosius, Emily J. Koubek, Eva L. Feldman
The FASEB Journal.2023;[Epub] CrossRef - Decoding the role of leptin and adiponectin in obesity-related gastrointestinal cancer
Vanda Marques, Fabiola Arella, Marta B. Afonso, André A. Santos, Cecília M.P. Rodrigues
Clinical Science.2023; 137(15): 1095. CrossRef - Metformin Can Attenuate Beta-Cell Hypersecretion—Implications for Treatment of Children with Obesity
Quan Wen, Rasmus Stenlid, Azazul Islam Chowdhury, Iris Ciba, Banu Aydin, Sara Y. Cerenius, Hannes Manell, Anders Forslund, Peter Bergsten
Metabolites.2023; 13(8): 917. CrossRef - The Effectiveness of a Low Glycemic Index/Load Diet on Cardiometabolic, Glucometabolic, and Anthropometric Indices in Children with Overweight or Obesity: A Systematic Review and Meta-Analysis
Ioustini Kalaitzopoulou, Xenophon Theodoridis, Evangelia Kotzakioulafi, Kleo Evripidou, Michail Chourdakis
Children.2023; 10(9): 1481. CrossRef - A review of the last decade: pancreatic cancer and type 2 diabetes
Jiaqi Wu, Liang Tang, Feng Zheng, Xun Chen, Lei Li
Archives of Physiology and Biochemistry.2023; : 1. CrossRef - Characteristics of Children and Adolescents with Hyperinsulinemia Undergoing Oral Glucose Tolerance Test: A Single-Center Retrospective Observational Study
Clelia Cipolla, Ilaria Lazzareschi, Antonietta Curatola, Claudia Lasorella, Lucia Celeste Pane, Linda Sessa, Giulia Rotunno, Donato Rigante, Giorgio Sodero
Diseases.2023; 11(3): 110. CrossRef - Hyperinsulinemia acts via acinar insulin receptors to initiate pancreatic cancer by increasing digestive enzyme production and inflammation
Anni M.Y. Zhang, Yi Han Xia, Jeffrey S.H. Lin, Ken H. Chu, Wei Chuan K. Wang, Titine J.J. Ruiter, Jenny C.C. Yang, Nan Chen, Justin Chhuor, Shilpa Patil, Haoning Howard Cen, Elizabeth J. Rideout, Vincent R. Richard, David F. Schaeffer, Rene P. Zahedi, Chr
Cell Metabolism.2023; 35(12): 2119. CrossRef - Dairy Intake Modifies the Level of the Bile Acid Precursor and Its Correlation with Serum Proteins Associated with Cholesterol Clearance in Subjects with Hyperinsulinemia
Atena Mahdavi, Jocelyn Trottier, Olivier Barbier, Michel Lebel, Iwona Rudkowska
Nutrients.2023; 15(22): 4707. CrossRef - Trapa Bispinosa Roxb. Inhibits the Insulin-Dependent AKT/WNK1 Pathway to Induce Autophagy in Mice with Type 2 Diabetes
Takahiro Suzuki, Takehito Sato, Kaori Masuhara, Mizuki Tokusanai, Hisako Akatsuka, Tomohiro Kashikawa, Yasuyuki Suzuki
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3095. CrossRef - Effects of Functional and Nutraceutical Foods in the Context of the Mediterranean Diet in Patients Diagnosed with Breast Cancer
Giovanna Flore, Andrea Deledda, Mauro Lombardo, Andrea Armani, Fernanda Velluzzi
Antioxidants.2023; 12(10): 1845. CrossRef - A systematic review exploring the mechanisms by which citrus bioflavonoid supplementation benefits blood glucose levels and metabolic complications in type 2 diabetes mellitus
Ankit Gupta, Abdulsatar Jamal, Dina A. Jamil, Hayder A. Al-Aubaidy
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(11): 102884. CrossRef - Diabetes Mellitus and Gastric Cancer: Correlation and Potential Mechanisms
Li Wang, Zhe Zhang, Eusebio Chiefari
Journal of Diabetes Research.2023; 2023: 1. CrossRef - EXPLORATORY ANALYSIS OF DIETARY PATTERNS OF PATIENTS WITH GASTRIC ADENOCARCINOMA: A CASE-CONTROL STUDY IN CENTRAL BRAZIL
Silvana Barbosa SANTIAGO, Gabriela Rodrigues de SOUSA, Amanda Ferreira Paes Landim RAMOS, Gisele Aparecida FERNANDES, Maria Paula CURADO, Mônica Santiago BARBOSA
Arquivos de Gastroenterologia.2023; 60(4): 419. CrossRef - Risk of cancer in acromegaly patients: An updated meta-analysis and systematic review
Zhehao Xiao, Pingping Xiao, Yong Wang, Chen Fang, Yong Li, Alvaro Galli
PLOS ONE.2023; 18(11): e0285335. CrossRef - Long Follow-Up Times Weaken Observational Diet–Cancer Study Outcomes: Evidence from Studies of Meat and Cancer Risk
William B. Grant
Nutrients.2023; 16(1): 26. CrossRef - Serum Lipid Profiles and Cholesterol-Lowering Medication Use in Relation to Subsequent Risk of Colorectal Cancer in the UK Biobank Cohort
Fangcheng Yuan, Wanqing Wen, Guochong Jia, Jirong Long, Xiao-Ou Shu, Wei Zheng
Cancer Epidemiology, Biomarkers & Prevention.2023; 32(4): 524. CrossRef - Prevalence of diabetes mellitus among 80,193 gastrointestinal cancer patients in five European and three Asian countries
Christoph Roderburg, Sven H. Loosen, Laura Hoyer, Tom Luedde, Karel Kostev
Journal of Cancer Research and Clinical Oncology.2022; 148(5): 1057. CrossRef - The Intricate Crosstalk Between Insulin and Pancreatic Ductal Adenocarcinoma: A Review From Clinical to Molecular
Junyuan Deng, Yujie Guo, Jiali Du, Jichun Gu, Lei Kong, Boan Tao, Ji Li, Deliang Fu
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - Effects of hyperinsulinemia on pancreatic cancer development and the immune microenvironment revealed through single-cell transcriptomics
Anni M. Y. Zhang, Ken H. Chu, Brian F. Daly, Titine Ruiter, Yan Dou, Jenny C. C. Yang, Twan J. J. de Winter, Justin Chhuor, Su Wang, Stephane Flibotte, Yiwei Bernie Zhao, Xiaoke Hu, Hong Li, Elizabeth J. Rideout, David F. Schaeffer, James D. Johnson, Jane
Cancer & Metabolism.2022;[Epub] CrossRef - Ghrelin and Cancer: Examining the Roles of the Ghrelin Axis in Tumor Growth and Progression
Anuhya S. Kotta, Abigail S. Kelling, Karen A. Corleto, Yuxiang Sun, Erin D. Giles
Biomolecules.2022; 12(4): 483. CrossRef - Influence of obesity on reproductive health before andduring pregnancy
A. Konwisser, O. Korytko
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(8): 446. CrossRef - Research Status of the Correlation between Type 2 Diabetes Mellitus and the Occurrence and Development of Breast Cancer
聪 李
Advances in Clinical Medicine.2022; 12(04): 3010. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Diabetes & Metabolism Journal.2022; 46(3): 355. CrossRef - Obesity and Pancreatic Cancer: Recent Progress in Epidemiology, Mechanisms and Bariatric Surgery
Shuhei Shinoda, Naohiko Nakamura, Brett Roach, David A. Bernlohr, Sayeed Ikramuddin, Masato Yamamoto
Biomedicines.2022; 10(6): 1284. CrossRef - Effect of carbohydrate-restricted diets and intermittent fasting on obesity, type 2 diabetes mellitus, and hypertension management: consensus statement of the Korean Society for the Study of obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Clinical Hypertension.2022;[Epub] CrossRef - Vitamin D and Risk of Obesity-Related Cancers: Results from the SUN (‘Seguimiento Universidad de Navarra’) Project
Rodrigo Sánchez-Bayona, Maira Bes-Rastrollo, Cesar I. Fernández-Lázaro, Maite Bastyr, Ainhoa Madariaga, Juan J. Pons, Miguel A. Martínez-González, Estefanía Toledo
Nutrients.2022; 14(13): 2561. CrossRef - Metabolically Defined Body Size Phenotypes and Risk of Endometrial Cancer in the European Prospective Investigation into Cancer and Nutrition (EPIC)
Nathalie Kliemann, Romain Ould Ammar, Carine Biessy, Audrey Gicquiau, Verena Katzke, Rudolf Kaaks, Anne Tjønneland, Anja Olsen, Maria-Jose Sánchez, Marta Crous-Bou, Fabrizio Pasanisi, Sandar Tin Tin, Aurora Perez-Cornago, Dagfinn Aune, Sofia Christakoudi,
Cancer Epidemiology, Biomarkers & Prevention.2022; 31(7): 1359. CrossRef - Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hype
Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(2): 100. CrossRef - Detangling the interrelations between MAFLD, insulin resistance, and key hormones
Shreya C. Pal, Mohammed Eslam, Nahum Mendez-Sanchez
Hormones.2022; 21(4): 573. CrossRef - Obesity, cancer risk, and time-restricted eating
Manasi Das, Nicholas J. G. Webster
Cancer and Metastasis Reviews.2022; 41(3): 697. CrossRef - Associations between early-life growth pattern and body size and follicular lymphoma risk and survival: a family-based case-control study
Michael K. Odutola, Marina T. van Leeuwen, Jennifer Turner, Fiona Bruinsma, John F. Seymour, H. Miles Prince, Samuel T. Milliken, Mark Hertzberg, Judith Trotman, Stephen S. Opat, Robert Lindeman, Fernando Roncolato, Emma Verner, Michael Harvey, Campbell T
Cancer Epidemiology.2022; 80: 102241. CrossRef - Differential expression of Ago2‐mediated microRNA signaling in adipose tissue is associated with food‐induced obesity
Hansi Zhang, Liang Qiao, Xiaoxuan Liu, Xiaojing Han, Jing Kang, Yanli Liu, Juntang Lin, Xin Yan
FEBS Open Bio.2022; 12(10): 1828. CrossRef - Proposal for standardizing normal insulin ranges in Brazilian patients and a new classification of metabolic syndrome
Pedro Renato Chocair, Precil Diego Miranda de Menezes Neves, Victor Augusto Hamamoto Sato, Sara Mohrbacher, Érico Souza Oliveira, Leonardo Victor Barbosa Pereira, Alessandra Martins Bales, Fagner Pereira da Silva, John A. Duley, Américo Lourenço Cuvello-N
Frontiers in Medicine.2022;[Epub] CrossRef - Two models of insulin resistance development and the strategy to combat age-related diseases: literature review
A. V. Martyushev-Poklad, D. S. Yankevich, M. V. Petrova, N. G. Savitskaya
Problems of Endocrinology.2022; 68(4): 59. CrossRef - In Vitro Mimicking of Obesity-Induced Biochemical Environment to Study Obesity Impacts on Cells and Tissues
Abdelaziz Ghanemi, Mayumi Yoshioka, Jonny St-Amand
Diseases.2022; 10(4): 76. CrossRef - Long‐term survival analysis of patients with stage IIIB‐IV non‐small cell lung cancer complicated by type 2 diabetes mellitus: A retrospective propensity score matching analysis
Xuejiao Li, Haiyan Fang, Dongwei Zhang, Liming Xia, Xiang Wang, Jingping Yang, Shaohu Zhang, Ya Su, Yongfu Zhu
Thoracic Cancer.2022; 13(23): 3268. CrossRef - Diabetes and skin cancers: Risk factors, molecular mechanisms and impact on prognosis
Elena-Codruta Dobrică, Madalina Laura Banciu, Vincent Kipkorir, Mohammad Amin Khazeei Tabari, Madeleine Jemima Cox, L V Simhachalam Kutikuppala, Mihnea-Alexandru Găman
World Journal of Clinical Cases.2022; 10(31): 11214. CrossRef - The role of the mTOR pathway in diabetic retinopathy
Fabio Casciano, Enrico Zauli, Erika Rimondi, Marco Mura, Maurizio Previati, Massimo Busin, Giorgio Zauli
Frontiers in Medicine.2022;[Epub] CrossRef - Hyperinsulinemia-induced microglial mitochondrial dynamic and metabolic alterations lead to neuroinflammation in vivo and in vitro
Xiaohan Yang, Yuan Xu, Wenting Gao, Li Wang, Xinnan Zhao, Gang Liu, Kai Fan, Shuang Liu, Huimin Hao, Siyan Qu, Renhou Dong, Xiaokai Ma, Jianmei Ma
Frontiers in Neuroscience.2022;[Epub] CrossRef - Integrated Physiology of the Exocrine and Endocrine Compartments in Pancreatic Diseases
Teresa L. Mastracci, Minoti Apte, Laufey T. Amundadottir, Alexandra Alvarsson, Steven Artandi, Melena D. Bellin, Ernesto Bernal-Mizrachi, Alejandro Caicedo, Martha Campbell-Thompson, Zobeida Cruz-Monserrate, Abdelfattah El Ouaamari, Kyle J. Gaulton, Andre
Pancreas.2022; 51(9): 1061. CrossRef - Intestinal Microbiome Modified by Bariatric Surgery Improves Insulin Sensitivity and Correlates with Increased Brown Fat Activity and Energy Expenditure
jitender Yadav, Tao Liang, Tairan Qin, Nayanan N. Nathan, Katherine J.P Schwenger, Lauren Pickel, Li Xie, Helena Lei, Daniel A. Winer, Heather Maughan, Susan J. Robertson, Minna Woo, Wendy Y. W. Lou, Kate Banks, Timothy Jackson, Allan Okrainec, Susy S. Ho
SSRN Electronic Journal .2022;[Epub] CrossRef - Severe hyperglycemia and insulin resistance in patients with SARS-CoV-2 infection: a report of two cases
Alison H. Affinati, Amisha Wallia, Roma Y. Gianchandani
Clinical Diabetes and Endocrinology.2021;[Epub] CrossRef - Promises and pitfalls of beta cell–replacement therapies
Jelena Kolic, James D. Johnson
Nature Metabolism.2021; 3(8): 1036. CrossRef - Hiding unhealthy heart outcomes in a low-fat diet trial: the Women’s Health Initiative Randomized Controlled Dietary Modification Trial finds that postmenopausal women with established coronary heart disease were at increased risk of an adverse outcome if
Timothy David Noakes
Open Heart.2021; 8(2): e001680. CrossRef - On the causal relationships between hyperinsulinaemia, insulin resistance, obesity and dysglycaemia in type 2 diabetes
James D. Johnson
Diabetologia.2021; 64(10): 2138. CrossRef - Diabetes mellitus and cancer: a system of insulin-like growth factors
E. M. Frantsiyants, E. I. Surikova, I. V. Kaplieva, V. A. Bandovkina, I. V. Neskubina, E. A. Sheiko, M. I. Morozova, I. M. Kotieva
Problems of Endocrinology.2021; 67(5): 34. CrossRef
- High adherence to Western dietary pattern increases breast cancer risk (an EPIC-Spain study)
- Basic Research
- Histone Deacetylase 9: Its Role in the Pathogenesis of Diabetes and Other Chronic Diseases
- Siqi Hu, Eun-Hee Cho, Ji-Young Lee
- Diabetes Metab J. 2020;44(2):234-244. Published online March 24, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0243
- 6,396 View
- 161 Download
- 20 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader As a member of the class IIa histone deacetylases (HDACs), HDAC9 catalyzes the deacetylation of histones and transcription factors, commonly leading to the suppression of gene transcription. The activity of HDAC9 is regulated transcriptionally and post-translationally. HDAC9 is known to play an essential role in regulating myocyte and adipocyte differentiation and cardiac muscle development. Also, recent studies have suggested that HDAC9 is involved in the pathogenesis of chronic diseases, including cardiovascular diseases, osteoporosis, autoimmune disease, cancer, obesity, insulin resistance, and liver fibrosis. HDAC9 modulates the expression of genes related to the pathogenesis of chronic diseases by altering chromatin structure in their promotor region or reducing the transcriptional activity of their respective transcription factors. This review summarizes the current knowledge of the regulation of HDAC9 expression and activity. Also, the roles of HDAC9 in the pathogenesis of chronic diseases are discussed, along with potential underlying mechanisms.
-
Citations
Citations to this article as recorded by- Impact of housing temperature on adipose tissue HDAC9 expression and adipogenic differentiation in high fat‐fed mice
Samah Ahmadieh, Brandee Goo, Abdalrahman Zarzour, David Kim, Hong Shi, Praneet Veerapaneni, Ronnie Chouhaita, Nicole K. H. Yiew, Carla Dominguez Gonzalez, Akash Chakravartty, James Pennoyer, Nazeera Hassan, Tyler W. Benson, Mourad Ogbi, David J. Fulton, R
Obesity.2024; 32(1): 107. CrossRef - HDAC9 inhibition reduces skeletal muscle atrophy and enhances regeneration in mice with cigarette smoke-induced COPD
Guixian Zheng, Chao Li, Xiaoli Chen, Zhaohui Deng, Ting Xie, Zengyu Huo, Xinyan Wei, Yanbing Huang, Xia Zeng, Yu Luo, Jing Bai
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2024; 1870(3): 167023. CrossRef - Identification of HDAC9 and ARRDC4 as potential biomarkers and targets for treatment of type 2 diabetes
Jing Liu, Lingzhen Meng, Zhihong Liu, Ming Lu, Ruiying Wang
Scientific Reports.2024;[Epub] CrossRef - HDAC9 as a Privileged Target: Reviewing its Role in Different Diseases
and Structure-activity Relationships (SARs) of its Inhibitors
Totan Das, Samima Khatun, Tarun Jha, Shovanlal Gayen
Mini-Reviews in Medicinal Chemistry.2024; 24(7): 767. CrossRef - Targeting histone deacetylases for cancer therapy: Trends and challenges
Tao Liang, Fengli Wang, Reham M. Elhassan, Yongmei Cheng, Xiaolei Tang, Wengang Chen, Hao Fang, Xuben Hou
Acta Pharmaceutica Sinica B.2023; 13(6): 2425. CrossRef - Therapeutic approach of natural products that treat osteoporosis by targeting epigenetic modulation
Guokai Zhang, Zhenying Liu, Zihan Li, Bing Zhang, Pengyu Yao, Yun Qiao
Frontiers in Genetics.2023;[Epub] CrossRef - Research Progress on Histone Deacetylase Inhibitors
玉姜 汤
Hans Journal of Medicinal Chemistry.2023; 11(02): 116. CrossRef - HDAC9 Inhibition as a Novel Treatment for Stroke
Hugh S. Markus
Stroke.2023; 54(12): 3182. CrossRef - Histone deacetylase 9 exacerbates podocyte injury in hyperhomocysteinemia through epigenetic repression of Klotho
Min Liu, Yang Zhang, Ping Zhan, Wenjuan Sun, Chuanqiao Dong, Xiaohan Liu, Yujie Yang, Xiaojie Wang, Yusheng Xie, Chengjiang Gao, Huili Hu, Benkang Shi, Ziying Wang, Chun Guo, Fan Yi
Pharmacological Research.2023; 198: 107009. CrossRef - Molecular mechanism and therapeutic potential of HDAC9 in intervertebral disc degeneration
Ming Lei, Hui Lin, Deyao Shi, Pan Hong, Hui Song, Bomansaan Herman, Zhiwei Liao, Cao Yang
Cellular & Molecular Biology Letters.2023;[Epub] CrossRef - Interindividual variability in transgene mRNA and protein production following adeno-associated virus gene therapy for hemophilia A
Sylvia Fong, Bridget Yates, Choong-Ryoul Sihn, Aras N. Mattis, Nina Mitchell, Su Liu, Chris B. Russell, Benjamin Kim, Adebayo Lawal, Savita Rangarajan, Will Lester, Stuart Bunting, Glenn F. Pierce, K. John Pasi, Wing Yen Wong
Nature Medicine.2022; 28(4): 789. CrossRef - Active RhoA Exerts an Inhibitory Effect on the Homeostasis and Angiogenic Capacity of Human Endothelial Cells
Michael Hauke, Robert Eckenstaler, Anne Ripperger, Anna Ender, Heike Braun, Ralf A. Benndorf
Journal of the American Heart Association.2022;[Epub] CrossRef - HDAC9 Contributes to Serous Ovarian Cancer Progression through Regulating Epithelial–Mesenchymal Transition
Long Xu, Jian Wang, Buhan Liu, Jiaying Fu, Yuanxin Zhao, Sihang Yu, Luyan Shen, Xiaoyu Yan, Jing Su
Biomedicines.2022; 10(2): 374. CrossRef - Common protein-coding variants influence the racing phenotype in galloping racehorse breeds
Haige Han, Beatrice A. McGivney, Lucy Allen, Dongyi Bai, Leanne R. Corduff, Gantulga Davaakhuu, Jargalsaikhan Davaasambuu, Dulguun Dorjgotov, Thomas J. Hall, Andrew J. Hemmings, Amy R. Holtby, Tuyatsetseg Jambal, Badarch Jargalsaikhan, Uyasakh Jargalsaikh
Communications Biology.2022;[Epub] CrossRef - Proposed minimal essential co-expression and physical interaction networks involved in the development of cognition impairment in human mid and late life
Zahra Salehi, Masoud Arabfard, Omid Sadatpour, Mina Ohadi
Neurological Sciences.2021; 42(3): 951. CrossRef - Emerging roles of SIRT6 in human diseases and its modulators
Gang Liu, Haiying Chen, Hua Liu, Wenbo Zhang, Jia Zhou
Medicinal Research Reviews.2021; 41(2): 1089. CrossRef - Quis Custodiet Ipsos Custodes (Who Controls the Controllers)? Two Decades of Studies on HDAC9
Claudio Brancolini, Eros Di Giorgio, Luigi Formisano, Teresa Gagliano
Life.2021; 11(2): 90. CrossRef - circ_0003204 Regulates Cell Growth, Oxidative Stress, and Inflammation in ox-LDL-Induced Vascular Endothelial Cells via Regulating miR-942-5p/HDAC9 Axis
Huan Wan, Ting You, Wei Luo
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Histone deacetylase (HDAC) 9: versatile biological functions and emerging roles in human cancer
Chun Yang, Stéphane Croteau, Pierre Hardy
Cellular Oncology.2021; 44(5): 997. CrossRef - Dual HDAC/BRD4 inhibitors against cancer
Negar Omidkhah, Farzin Hadizadeh, Razieh Ghodsi
Medicinal Chemistry Research.2021; 30(10): 1822. CrossRef - miR‐211‐5p is down‐regulated and a prognostic marker in bladder cancer
Weisheng Wang, Zhiming Liu, Xuegang Zhang, Junning Liu, Junqing Gui, Maorong Cui, Yong Li
The Journal of Gene Medicine.2020;[Epub] CrossRef
- Impact of housing temperature on adipose tissue HDAC9 expression and adipogenic differentiation in high fat‐fed mice
- Complications
- Diabetes and Cancer: Cancer Should Be Screened in Routine Diabetes Assessment
- Sunghwan Suh, Kwang-Won Kim
- Diabetes Metab J. 2019;43(6):733-743. Published online December 23, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0177
- 8,669 View
- 262 Download
- 83 Web of Science
- 92 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Cancer incidence appears to be increased in both type 1 and type 2 diabetes mellitus (DM). DM represents a risk factor for cancer, particularly hepatocellular, hepatobiliary, pancreas, breast, ovarian, endometrial, and gastrointestinal cancers. In addition, there is evidence showing that DM is associated with increased cancer mortality. Common risk factors such as age, obesity, physical inactivity and smoking may contribute to increased cancer risk in patients with DM. Although the mechanistic process that may link diabetes to cancer is not completely understood yet, biological mechanisms linking DM and cancer are hyperglycemia, hyperinsulinemia, increased bioactivity of insulin-like growth factor 1, oxidative stress, dysregulations of sex hormones, and chronic inflammation. However, cancer screening rate is significantly lower in people with DM than that in people without diabetes. Evidence from previous studies suggests that some medications used to treat DM are associated with either increased or reduced risk of cancer. However, there is no strong evidence supporting the association between the use of anti-hyperglycemic medication and specific cancer. In conclusion, all patients with DM should be undergo recommended age- and sex appropriate cancer screenings to promote primary prevention and early detection. Furthermore, cancer should be screened in routine diabetes assessment.
-
Citations
Citations to this article as recorded by- 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Care in Diabetes—2024
Nuha A. ElSayed, Grazia Aleppo, Raveendhara R. Bannuru, Dennis Bruemmer, Billy S. Collins, Kenneth Cusi, Laya Ekhlaspour, Talya K. Fleming, Marisa E. Hilliard, Eric L. Johnson, Kamlesh Khunti, Ildiko Lingvay, Glenn Matfin, Rozalina G. McCoy, Nicola Napoli
Diabetes Care.2024; 47(Supplement): S52. CrossRef - Editorial: The relationship between diabetes and cancers and its underlying mechanisms, volume II
Qiang Huo, Shuo Wang, Ying Hou, Reginald M. Gorczynski, Yining Shen, Bin Wang, Hanyi Ge, Tao Li
Frontiers in Endocrinology.2024;[Epub] CrossRef - Factors associated with gastric and duodenal neuroendocrine tumors: A multicenter case-control study
Kwangwoo Nam, Su Youn Nam, Jun Chul Park, Young Sin Cho, Hyuk Soon Choi, Kyoungwon Jung, Seon-Young Park, Joon Hyun Cho, Hyonho Chun
Digestive and Liver Disease.2024;[Epub] CrossRef - Exploring Perspectives on Cancer Screening in People Aged 30-70: A Comparative Study of Those With and Without Type 2 Diabetes
Yunus GÜR, Egemen TURAL, Akın DAYAN
Konuralp Tıp Dergisi.2024; 16(1): 26. CrossRef - Prognostic significance of glucose‐lipid metabolic index in pancreatic cancer patients with diabetes mellitus
Hailiang Wang, Shiye Ruan, Zelong Wu, Qian Yan, Yubin Chen, Jinwei Cui, Zhongyan Zhang, Shanzhou Huang, Baohua Hou, Chuanzhao Zhang
Cancer Medicine.2024;[Epub] CrossRef - Preoperative glucose-to-lymphocyte ratio predicts survival in cancer
Le Liu, Bei-bei Zhang, Yuan-zhou Li, Wen-juan Huang, Ye Niu, Qing-chun Jia, Wen Wang, Jia-rui Yuan, Shi-di Miao, Rui-tao Wang, Guang-yu Wang
Frontiers in Endocrinology.2024;[Epub] CrossRef - Higher Prevalence of Cancer in Patients with Diabetic Foot Syndrome
Chiara Goretti, Alessandro Prete, Alex Brocchi, Elisabetta Iacopi, Letizia Pieruzzi, Alberto Piaggesi
Journal of Clinical Medicine.2024; 13(5): 1448. CrossRef - Evaluating the Preferences and Willingness-to-Pay for Oral Antidiabetic Drugs Among Patients with Type 2 Diabetes Mellitus in China: A Discrete Choice Experiment
Ling-Hsiang Chuang, Huanlan Zhang, Tianqi Hong, Shitong Xie
The Patient - Patient-Centered Outcomes Research.2024;[Epub] CrossRef - Diabetes and the social, biologic, and behavioral determinants of endometrial cancer in the United States
Nour Massouh, Ayad A. Jaffa, Miran A. Jaffa
BMC Cancer.2024;[Epub] CrossRef - Comorbidity of patients with noncommunicable diseases in general practice. Eurasian guidelines
O. M. Drapkina, A. V. Kontsevaya, A. M. Kalinina, S. N. Avdeev, M. V. Agaltsov, L. I. Alekseeva, I. I. Almazova, E. Yu. Andreenko, D. N. Antipushina, Yu. A. Balanova, S. A. Berns, A. V. Budnevsky, V. V. Gainitdinova, A. A. Garanin, V. M. Gorbunov, A. Yu.
Cardiovascular Therapy and Prevention.2024; 23(3): 3696. CrossRef - Association between glycemic status and the risk of gastric cancer in pre-and postmenopausal women: A nationwide cohort study
Kyung Hee Han, Yoon Jin Choi, Tae Il Kim, Noh Hyun Park, Kyung-do Han, Dong Ho Lee
Annals of Epidemiology.2024;[Epub] CrossRef - Severity of Complications and Duration of Type 2 Diabetes and the Risk of Cancer: A Population-Based Study
Yu-Wen Hu, Chiu-Mei Yeh, Chia-Jen Liu, Tzeng-Ji Chen, Nicole Huang, Yiing-Jenq Chou
Cancer Epidemiology, Biomarkers & Prevention.2024; 33(5): 739. CrossRef - Patterns and Trends in Mortality Associated With and Due to Diabetes Mellitus in a Transitioning Region With 3.17 Million People: Observational Study
Xiaopan Li, Ru Liu, Yichen Chen, Yan Han, Qizhe Wang, Yaxin Xu, Jing Zhou, Sunfang Jiang
JMIR Public Health and Surveillance.2023; 9: e43687. CrossRef - Diabetes and cancer: Optimising glycaemic control
Nalinie Joharatnam‐Hogan, Daniel L. Morganstein
Journal of Human Nutrition and Dietetics.2023; 36(2): 504. CrossRef - Need for improving immunization status and preventive care in diabetes mellitus patients
Teresa Gisinger, Alexandra Kautzky-Willer, Michael Leutner
Wiener klinische Wochenschrift.2023; 135(13-14): 336. CrossRef - Impact of cumulative hyperglycemic burden on the pancreatic cancer risk: A nationwide cohort study
Dong-Hoe Koo, Kyungdo Han, Cheol-Young Park
Diabetes Research and Clinical Practice.2023; 195: 110208. CrossRef - Simultaneous Quantification of Serum Lipids and Their Association with Type 2 Diabetes Mellitus-Positive Hepatocellular Cancer
Zhihong Yue, Lin Pei, Guangyan Meng, Aimin Zhang, Meng Li, Mei Jia, Hui Wang, Linlin Cao
Metabolites.2023; 13(1): 90. CrossRef - Modifiable risk factors for oral cavity cancer in non-smokers: A systematic review and meta-analysis
Margaret A. Heller, Sarah C. Nyirjesy, Robert Balsiger, Nicholas Talbot, Kyle K. VanKoevering, Catherine T. Haring, Matthew O. Old, Stephen Y. Kang, Nolan B. Seim
Oral Oncology.2023; 137: 106300. CrossRef - Hypertension, type 2 diabetes, obesity, and p53 mutations negatively correlate with metastatic colorectal cancer patients’ survival
Alessandro Ottaiano, Mariachiara Santorsola, Luisa Circelli, Francesco Perri, Marco Cascella, Francesco Sabbatino, Maurizio Capuozzo, Vincenza Granata, Silvia Zappavigna, Angela Lombardi, Marianna Scrima, Nadia Petrillo, Monica Ianniello, Marika Casillo,
Frontiers in Medicine.2023;[Epub] CrossRef - The relationship between the CUN-BAE body fatness index and incident diabetes: a longitudinal retrospective study
Qing Peng, Zihao Feng, Zhuojian Cai, Dixing Liu, Jiana Zhong, Hejia Zhao, Xiuwei Zhang, Weikun Chen
Lipids in Health and Disease.2023;[Epub] CrossRef - Association of four lipid-derived indicators with the risk of developing type 2 diabetes: a Chinese population-based cohort study
Linfeng He, Wenbin Zheng, Zeyu Li, Wen Kong, Tianshu Zeng
Lipids in Health and Disease.2023;[Epub] CrossRef - Screening for Coronary Artery Disease in Cancer Survivors
Ragani Velusamy, Mark Nolan, Andrew Murphy, Paaladinesh Thavendiranathan, Thomas H. Marwick
JACC: CardioOncology.2023; 5(1): 22. CrossRef - Diabetes mellitus induces a novel inflammatory network involving cancer progression: Insights from bioinformatic analysis and in vitro validation
Yejun Tan, Jin Kang, Hongli Li, Aifang Zhong, Yaqiong Liu, Zheyu Zhang, Roujie Huang, Xin Cheng, Weijun Peng
Frontiers in Immunology.2023;[Epub] CrossRef - Increased Breast and Colorectal Cancer Risk in Type 2 Diabetes: Awareness Among Adults With and Without Diabetes and Information Provision on Diabetes Websites
Laura Ashley, Kathryn A Robb, Daryl B O’Connor, Rebecca Platt, Mollie Price, Olivia Robinson, Elizabeth Travis, Lorraine Lipscombe, Ramzi Ajjan, Rebecca Birch
Annals of Behavioral Medicine.2023; 57(5): 386. CrossRef - Primary peritoneal serous psammocarcinoma, rare variant: A case report
Srujan Kancharla, Anne Alaniz, Pulin Kothari, Stacy Norton
Gynecologic Oncology Reports.2023; 47: 101176. CrossRef - Association between the Finnish Diabetes Risk Score and cancer in middle-aged and older adults: Involvement of inflammation
Yu Peng, Peng Wang, Jianxiao Gong, Fubin Liu, Yating Qiao, Changyu Si, Xixuan Wang, Huijun Zhou, Fangfang Song
Metabolism.2023; 144: 155586. CrossRef - Interlinking of diabetes mellitus and cancer: An overview
Iftikhar Ahmad, Mohd Suhail, Ausaf Ahmad, Mahmoud Alhosin, Shams Tabrez
Cell Biochemistry and Function.2023; 41(5): 506. CrossRef - High glucose promotes the progression of colorectal cancer by activating the BMP4 signaling and inhibited by glucagon-like peptide-1 receptor agonist
Bingwei Ma, Xingchun Wang, Hui Ren, Yingying Li, Haijiao Zhang, Muqing Yang, Jiyu Li
BMC Cancer.2023;[Epub] CrossRef - Diabetes mellitus and the female reproductive system tumors
K. I. Sharafutdinova, V. S. Shlyapina, A. I. Baeva, A. A. Timurshin, I. E. Sabanaeva, A. G. Nakieva, M. F. Kalashnikova, M. N. Khabibov
Problems of Endocrinology.2023; 69(3): 103. CrossRef - Global estimates of rehabilitation needs and disease burden in tracheal, bronchus, and lung cancer from 1990 to 2019 and projections to 2045 based on the global burden of disease study 2019
Xigui Lai, Conghui Li, Yao Yang, Mingyuan Niu, Yujie Yang, Shanshan Gu, Weiqian Hou, Lili Chen, Yi Zhu
Frontiers in Oncology.2023;[Epub] CrossRef - Social and racial inequalities in diabetes and cancer in the United States
Nour Massouh, Ayad A. Jaffa, Hani Tamim, Miran A. Jaffa
Frontiers in Public Health.2023;[Epub] CrossRef - Lactate in exhaled breath condensate and its correlation to cancer: challenges, promises and a call for data
Veronika Ruzsányi, Miklós Péter Kalapos
Journal of Breath Research.2023; 17(4): 044001. CrossRef - The impact of diabetes status on total and site-specific cancer risk in the elderly population: A nationwide cohort study
Kyuho Kim, Bongseong Kim, Hyunho Kim, Hyung Soon Park, Yu-Bae Ahn, Seung-Hyun Ko, Kyungdo Han, Jae-Seung Yun
Diabetes Research and Clinical Practice.2023; 203: 110866. CrossRef - Team-Based Approach to Reduce Malignancies in People with Diabetes and Obesity
Ziyue Zhu, Samuel Yeung Shan Wong, Joseph Jao Yiu Sung, Thomas Yuen Tung Lam
Current Diabetes Reports.2023; 23(10): 253. CrossRef - PECAM-1 drives β-catenin-mediated EndMT via internalization in colon cancer with diabetes mellitus
Qing Wu, Xingxing Du, Jianing Cheng, Xiuying Qi, Huan Liu, Xiaohong Lv, Xieyang Gong, Changxin Shao, Muhong Wang, Luxiao Yue, Xin Yang, Shiyu Li, Yafang Zhang, Xuemei Li, Huike Yang
Cell Communication and Signaling.2023;[Epub] CrossRef - Saxagliptin, a selective dipeptidyl peptidase-4 inhibitor, alleviates somatic cell aneugenicity and clastogenicity in diabetic mice
Sabry M. Attia, Sheikh F. Ahmad, Ahmed Nadeem, Mohamed S.M. Attia, Mushtaq A. Ansari, Abdelkader E. Ashour, Norah A. Albekairi, Mohammed A. Al-Hamamah, Ali A. Alshamrani, Saleh A. Bakheet
Mutation Research/Genetic Toxicology and Environmental Mutagenesis.2023; 892: 503707. CrossRef - Analysis of differential membrane proteins related to matrix stiffness-mediated metformin resistance in hepatocellular carcinoma cells
Xiangyu Gao, Jiali Qian, Yang Zhang, Heming Wang, Jiefeng Cui, Yehong Yang
Proteome Science.2023;[Epub] CrossRef - Associations of heart failure to prevalence of haematologic- and solid malignancies in southern Sweden: A cross-sectional study
Mia Scholten, Anders Halling, Kathleen Bennett
PLOS ONE.2023; 18(10): e0292853. CrossRef - The interplay between antidiabetic medications and cancer risk
Duaa Durrani, Muhammad Hassan, Aimen Zulfikar
International Journal of Scientific Reports.2023; 9(11): 384. CrossRef - Causal association between inflammatory bowel disease and 32 site-specific extracolonic cancers: a Mendelian randomization study
Hui Gao, Shuhao Zheng, Xin Yuan, Jiarong Xie, Lei Xu
BMC Medicine.2023;[Epub] CrossRef - Association between diabetes at different diagnostic ages and risk of cancer incidence and mortality: a cohort study
Yu Peng, Fubin Liu, Peng Wang, Yating Qiao, Changyu Si, Xixuan Wang, Jianxiao Gong, Huijun Zhou, Fengju Song, Fangfang Song
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Characteristics and Risk of Mortality in the Elderly Korean Population
Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 522. CrossRef - Clinical potentials of metformin in cancer therapy
Nidhi Sharma, Richa Dhingra
Journal of Diabetology.2023; 14(4): 186. CrossRef - High Glucose Induced Upregulation of Cyclin a Associating with a Short Survival of Patients with Cholangiocarcinoma: A Potential Target for Treatment of Patients with Diabetes Mellitus
Charupong Saengboonmee, Marutpong Detarya, Sakkarn Sangkhamanon, Kanlayanee Sawanyawisuth, Wunchana Seubwai, Sopit Wongkham
Nutrition and Cancer.2022; 74(5): 1734. CrossRef - Prevalence of diabetes mellitus among 80,193 gastrointestinal cancer patients in five European and three Asian countries
Christoph Roderburg, Sven H. Loosen, Laura Hoyer, Tom Luedde, Karel Kostev
Journal of Cancer Research and Clinical Oncology.2022; 148(5): 1057. CrossRef - Metformin and survival: Is there benefit in a cohort limited to diabetic women with endometrial, breast, or ovarian cancer?
Lara S. Lemon, Brian Orr, Francesmary Modugno, Ronald J. Buckanovich, Lan Coffman, Robert P. Edwards, Sarah Taylor
Gynecologic Oncology.2022; 165(1): 60. CrossRef - The Relationship Between Diabetes Mellitus and Cancers and Its Underlying Mechanisms
Bing Zhu, Shen Qu
Frontiers in Endocrinology.2022;[Epub] CrossRef - The impact of diabetes mellitus on levels of sex hormones and their receptors in tumor tissues in female rats with Guerin’s carcinoma
E. M. Frantsiyants, V. A. Bandovkina, I. V. Kaplieva, E. I. Surikova, Yu. A. Pogorelova, N. D. Cheryarina, I. M. Kotieva, M. I. Morozova, A. I. Shikhlyarova
Research and Practical Medicine Journal.2022; 9(1): 23. CrossRef - Synergistic association between underweight and type 2 diabetes on the development of laryngeal cancer: a national population-based retrospective cohort study
Oh. Hyeong Lee, Yong-Moon Park, Seung-Hyun Ko, Kyuna Lee, Yeonji Kim, Kyungdo Han, Jung-Hae Cho
BMC Cancer.2022;[Epub] CrossRef - Survival Risk Analysis of Small Cell Lung Cancer Patients with Pre-Existing Type 2 Diabetes Mellitus: A Single-Center Retrospective Cohort Study
Jing Ding, Xudong Li, Jun Ge, Yuanqian Gong, Ya Zhou, Juan Xiao, Qin Yang, Jing Chen, Mian Mao
Cancer Management and Research.2022; Volume 14: 1313. CrossRef - The High Prevalence of Short-Term Elevation of Tumor Markers Due to Hyperglycemia in Diabetic Patients
Xi-yu Liu
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 1113. CrossRef - Stationäre Patienten mit der Nebendiagnose Diabetes mellitus: klinische Relevanz
Christian Jenssen, Cristine Pietsch
Die Diabetologie.2022; 18(4): 379. CrossRef - Utility of Non-High-Density Lipoprotein Cholesterol to High-Density Lipoprotein Cholesterol Ratio in Evaluating Incident Diabetes Risk
Guotai Sheng, Dingyang Liu, Maobin Kuang, Yanjia Zhong, Shuhua Zhang, Yang Zou
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 1677. CrossRef - The Association of Dietary Fiber Intake in Three Meals with All-Cause and Disease-Specific Mortality among Adults: The U.S. National Health and Nutrition Examination Survey, 2003–2014
Jiayue Qi, Jian Gao, Yuntao Zhang, Wanying Hou, Tianshu Han, Changhao Sun
Nutrients.2022; 14(12): 2521. CrossRef - A Serum Metabolite Classifier for the Early Detection of Type 2 Diabetes Mellitus-Positive Hepatocellular Cancer
Lin-Lin Cao, Yi Han, Lin Pei, Zhi-Hong Yue, Bo-Yu Liu, Jing-Wen Cui, Mei Jia, Hui Wang
Metabolites.2022; 12(7): 610. CrossRef - Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(3): 415. CrossRef - Improvement in Age at Mortality and Changes in Causes of Death in the Population with Diabetes: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
Eugene Han, Sun Ok Song, Hye Soon Kim, Kang Ju Son, Sun Ha Jee, Bong-Soo Cha, Byung-Wan Lee
Endocrinology and Metabolism.2022; 37(3): 466. CrossRef - Novel insights into the pathogenic impact of diabetes on the gastrointestinal tract
Piero Portincasa, Leonilde Bonfrate, David Q.‐H. Wang, Gema Frühbeck, Gabriella Garruti, Agostino Di Ciaula
European Journal of Clinical Investigation.2022;[Epub] CrossRef - Editorial: The relationship between diabetes and cancers and its underlying mechanisms
Qiang Huo, Jing Wang, Nannan Zhang, Long Xie, Heshan Yu, Tao Li
Frontiers in Endocrinology.2022;[Epub] CrossRef - Oxidatively Damaged Nucleic Acid: Linking Diabetes and Cancer
Xiujuan Hong, Yiqiu Hu, Zhijun Yuan, Zhihao Fang, Xiaoxiao Zhang, Ying Yuan, Cheng Guo
Antioxidants & Redox Signaling.2022; 37(16-18): 1153. CrossRef - Diabetes mellitus and endometrial carcinoma: Risk factors and etiological links
Ya Wang, Xinling Zeng, Jie Tan, Yi Xu, Cunjian Yi
Medicine.2022; 101(34): e30299. CrossRef - The Good, the Bad and the New about Uric Acid in Cancer
Simone Allegrini, Mercedes Garcia-Gil, Rossana Pesi, Marcella Camici, Maria Grazia Tozzi
Cancers.2022; 14(19): 4959. CrossRef - Family cancer history and smoking habit associated with sarcoma in a Japanese population study
Yoshihiro Araki, Norio Yamamoto, Yoshikazu Tanzawa, Takahiro Higashi, Aya Kuchiba, Katsuhiro Hayashi, Akihiko Takeuchi, Shinji Miwa, Kentaro Igarashi, Makoto Endo, Eisuke Kobayashi, Hiroyuki Tsuchiya, Akira Kawai
Scientific Reports.2022;[Epub] CrossRef - Decreased IGF-1 level is associated with restrained amino acid metabolism in NSCLC with diabetes mellitus
Hehe Lv, Fan Zhang, Can Liang, Xuekui Liu, Yamei Ma, Jiayi Li, Yan Ye, Shanwen Si, Yaran Liu, Hao Heng, Houfa Geng
Frontiers in Endocrinology.2022;[Epub] CrossRef - Acute Pancreatitis Increases the Risk of Gastrointestinal Cancer in Type 2 Diabetic Patients: A Korean Nationwide Cohort Study
Jin Ho Choi, Woo Hyun Paik, Dong Kee Jang, Min Kyu Kim, Ji Kon Ryu, Yong-Tae Kim, Kyungdo Han, Sang Hyub Lee
Cancers.2022; 14(22): 5696. CrossRef - Targets for the prevention of comorbidity of cardiovascular and cancer diseases
M. N. Mamedov, K. K. Badeinikova, A. K. Karimov
Russian Journal of Cardiology.2022; 27(11): 5235. CrossRef - Prevalence and potential risk factors of self-reported diabetes among elderly people in China: A national cross-sectional study of 224,142 adults
Xing Hu, Lingbing Meng, Zhimin Wei, Hongxuan Xu, Jianyi Li, Yingying Li, Na Jia, Hui Li, Xin Qi, Xuezhai Zeng, Qiuxia Zhang, Juan Li, Deping Liu
Frontiers in Public Health.2022;[Epub] CrossRef - Urinary Exosomal Tissue TIMP and Angiopoietin-1 Are Preoperative Novel Biomarkers of Well-Differentiated Thyroid Cancer
Chih-Yuan Wang, Shyang-Rong Shih, Kuen-Yuan Chen, Pei-Jie Huang
Biomedicines.2022; 11(1): 24. CrossRef - Acquired and modifiable cardiovascular risk factors in patients treated for cancer
Gary S. Beasley, Jeffrey A. Towbin
Journal of Thrombosis and Thrombolysis.2021; 51(4): 846. CrossRef - Diabetes and Cancer: Metabolic Association, Therapeutic Challenges, and the Role of Natural Products
Wamidh H. Talib, Asma Ismail Mahmod, Sara Feras. Abuarab, Eliza Hasen, Amer A. Munaim, Shatha Khaled Haif, Amani Marwan Ayyash, Samar Khater, Intisar Hadi AL-Yasari, Lina T. Al Kury
Molecules.2021; 26(8): 2179. CrossRef - Epidemiological link between obesity, type 2 diabetes mellitus and cancer
Cornelius J Fernandez, Annu Susan George, Nikhila A Subrahmanyan, Joseph M Pappachan
World Journal of Methodology.2021; 11(3): 23. CrossRef - Evaluation of the Efficacy of the Hospital Glycemic Management System for Patients with Malignant Tumors and Hyperglycemia
Juan Jiang, Danlan Pu, Renzhi Hu, Mingyang Hu, Qinan Wu
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 2717. CrossRef - Insulin-Like Growth Factor 1 (IGF-1) Signaling in Glucose Metabolism in Colorectal Cancer
Aldona Kasprzak
International Journal of Molecular Sciences.2021; 22(12): 6434. CrossRef - TNBC: Potential Targeting of Multiple Receptors for a Therapeutic Breakthrough, Nanomedicine, and Immunotherapy
Desh Deepak Singh, Dharmendra Kumar Yadav
Biomedicines.2021; 9(8): 876. CrossRef - GLP-1 Receptor Agonists: Beyond Their Pancreatic Effects
Xin Zhao, Minghe Wang, Zhitong Wen, Zhihong Lu, Lijuan Cui, Chao Fu, Huan Xue, Yunfeng Liu, Yi Zhang
Frontiers in Endocrinology.2021;[Epub] CrossRef - The Aneugenicity of Ketone Bodies in Colon Epithelial Cells Is Mediated by Microtubule Hyperacetylation and Is Blocked by Resveratrol
Haruka Sudo, Akira Kubo
International Journal of Molecular Sciences.2021; 22(17): 9397. CrossRef - EFFECT OF DIABETES MELLITUS ON THE LEVEL OF GROWTH FACTORS IN GUERIN CARCINOMA IN RATS OF BOTH SEXES
E.M. Frantsiyants, V.A. Bandovkina, I.V. Kaplieva, E.I. Surikova, I.V. Neskubina, L.K. Trepitaki, N.D. Cheryarina, Yu.A. Pogorelova, L.A. Nemashkalova, A.I. Shikhlyarova, I.M. Kotieva, M.I. Morozova
Ulyanovsk Medico-biological Journal.2021; : 129. CrossRef - Clinical Significance of Screening Differential Metabolites in Ovarian Cancer Tissue and Ascites by LC/MS
Miao Liu, Yu Liu, Hua Feng, Yixin Jing, Shuang Zhao, Shujia Yang, Nan Zhang, Shi Jin, Yafei Li, Mingjiao Weng, Xinzhu Xue, Fuya Wang, Yongheng Yang, Xiaoming Jin, Dan Kong
Frontiers in Pharmacology.2021;[Epub] CrossRef - Diabetes mellitus and cancer: a system of insulin-like growth factors
E. M. Frantsiyants, E. I. Surikova, I. V. Kaplieva, V. A. Bandovkina, I. V. Neskubina, E. A. Sheiko, M. I. Morozova, I. M. Kotieva
Problems of Endocrinology.2021; 67(5): 34. CrossRef - Diabetes and Cancer: Risk, Challenges, Management and Outcomes
Rabia K. Shahid, Shahid Ahmed, Duc Le, Sunil Yadav
Cancers.2021; 13(22): 5735. CrossRef - Obesity, Diabetes, and Increased Cancer Progression
Dae-Seok Kim, Philipp E. Scherer
Diabetes & Metabolism Journal.2021; 45(6): 799. CrossRef - Simple Serum Pancreatic Ductal Adenocarcinoma (PDAC) Protein Biomarkers—Is There Anything in Sight?
Monika Kapszewicz, Ewa Małecka-Wojciesko
Journal of Clinical Medicine.2021; 10(22): 5463. CrossRef - Chronic non-communicable diseases, risk factors, and quality of life in patients with malignancies of various localizations
M.N. Mamedov, V.I. Potievskaya, E.K. Saribekyan, O.V. Pikin, D.V. Sidorov, Z.M. Salimov, V.A. Kutsenko, O.M. Drapkina
Profilakticheskaya meditsina.2021; 24(11): 45. CrossRef - Survival after breast cancer in women with type 2 diabetes using antidiabetic medication and statins: a retrospective cohort study
Mayu Hosio, Elina Urpilainen, Ari Hautakoski, Mikko Marttila, Martti Arffman, Reijo Sund, Anne Ahtikoski, Ulla Puistola, Peeter Karihtala, Arja Jukkola, Esa Läärä
Acta Oncologica.2020; 59(9): 1110. CrossRef - Transcriptional Profiling and Biological Pathway(s) Analysis of Type 2 Diabetes Mellitus in a Pakistani Population
Zarish Noreen, Christopher A. Loffredo, Attya Bhatti, Jyothirmai J. Simhadri, Gail Nunlee-Bland, Thomas Nnanabu, Peter John, Jahangir S. Khan, Somiranjan Ghosh
International Journal of Environmental Research and Public Health.2020; 17(16): 5866. CrossRef - Screening Strategy of Pancreatic Cancer in Patients with Diabetes Mellitus
Suguru Mizuno, Yousuke Nakai, Kazunaga Ishigaki, Kei Saito, Hiroki Oyama, Tsuyoshi Hamada, Yukari Suzuki, Akiyuki Inokuma, Sachiko Kanai, Kensaku Noguchi, Tatsuya Sato, Ryunosuke Hakuta, Tomotaka Saito, Naminatsu Takahara, Hirofumi Kogure, Hiroyuki Isayam
Diagnostics.2020; 10(8): 572. CrossRef - Changes in mortality rates and ratios in people with pharmacologically treated type 2 diabetes mellitus between 2001 and 2016 in Hungary
György Jermendy, Zoltán Kiss, György Rokszin, Ibolya Fábián, István Wittmann, Péter Kempler
Diabetes Research and Clinical Practice.2020; 163: 108134. CrossRef Role of αVβ3 in Prostate Cancer: Metastasis Initiator and Important Therapeutic Target
Lin Tang, Meng Xu, Long Zhang, Lin Qu, Xiaoyan Liu
OncoTargets and Therapy.2020; Volume 13: 7411. CrossRef- Arterial stiffness is an independent predictor for risk of mortality in patients with type 2 diabetes mellitus: the REBOUND study
Jeong Mi Kim, Sang Soo Kim, In Joo Kim, Jong Ho Kim, Bo Hyun Kim, Mi Kyung Kim, Soon Hee Lee, Chang Won Lee, Min Chul Kim, Jun Hyeob Ahn, Jinmi Kim
Cardiovascular Diabetology.2020;[Epub] CrossRef - An Overview of Cancer Prevention: Chemoprevention and Immunoprevention
Kyle J. Gu, Guojun Li
Journal of Cancer Prevention.2020; 25(3): 127. CrossRef - Type 2 diabetes mellitus facilitates endometrial hyperplasia progression by activating the proliferative function of mucin O-glycosylating enzyme GALNT2
Xueyan Zhou, Yinxue Xu, Di Yin, Feng Zhao, Zhixiang Hao, Ya’nan Zhong, Jingbo Zhang, Bei Zhang, Xiaoxing Yin
Biomedicine & Pharmacotherapy.2020; 131: 110764. CrossRef - Diabetes mellitus and the risk of ovarian cancer: a systematic review and meta-analysis of cohort and case–control studies
Lihai Wang, Lei Zhong, Bin Xu, Min Chen, Hongxiao Huang
BMJ Open.2020; 10(12): e040137. CrossRef
- 4. Comprehensive Medical Evaluation and Assessment of Comorbidities: Standards of Care in Diabetes—2024
- The Relationship between Metformin and Cancer in Patients with Type 2 Diabetes
- Hyun Hee Chung, Jun Sung Moon, Ji Sung Yoon, Hyoung Woo Lee, Kyu Chang Won
- Diabetes Metab J. 2013;37(2):125-131. Published online April 16, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.2.125
- 3,563 View
- 29 Download
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Recently, several studies reported that the cancer incidence in type 2 diabetes patients is higher than in the general population. Although a number of risks are shared between cancer and diabetes patients, there have been few studies of its correlation. We evaluated the influences of several factors including low density lipoprotein cholesterol (LDL-C), albuminuria and use of metformin on the risk of cancer in patients with type 2 diabetes.
Methods We enrolled 1,320 patients with at least 5 years of follow-up and 73 patients were diagnosed with cancer during this period. The associations of the risk factors with cancer incidence were evaluated by multiple regression analysis. The subjects were placed into two subgroups based on metformin dosage (<1,000 mg/day, ≥1,000 mg/day) and we compared cancer incidence using analysis of covariance.
Results LDL-C and albuminuria were not significantly correlated with cancer risk. In contrast, metformin showed a reverse correlation with cancer risk (
P =0.006; relative risk, 0.574). In the metformin nonadministration group, smoking, male gender, and high triglyceride levels tended to be contributing factors without statistical significance. Cancer occurence was lower in the low dose metformin group (less than 1,000 mg/day) (P =0.00).Conclusion These results suggest that the administration of low dose metformin in patients with type 2 diabetes may be associated with a reduced risk of cancer.
-
Citations
Citations to this article as recorded by- Metformin Reduces Tumor Growth in a Murine Flank Schwannoma Model
Sudhir Manickavel, Yolanda Hartman, Andrew Burns, Manuel A. Lora Gonzalez, Jason Warram, Erika Walsh, Jacob B. Hunter, Daniel E. Killeen
Otology & Neurotology.2023; 44(9): 941. CrossRef - Metformin induces TPC-1 cell apoptosis through endoplasmic reticulum stress-associated pathways in vitro and in vivo
Jianwen Ye, Lei Qi, Kunlun Chen, Renfeng Li, Shengping Song, Chuang Zhou, Wenlong Zhai
International Journal of Oncology.2019;[Epub] CrossRef - Metformin Promotes Apoptosis but Suppresses Autophagy in Glucose-Deprived H4IIE Hepatocellular Carcinoma Cells
Deok-Bae Park
Diabetes & Metabolism Journal.2015; 39(6): 518. CrossRef - Combination Therapy of Metformin and Statin May Decrease Hepatocellular Carcinoma Among Diabetic Patients in Asia
Hsin-Hung Chen, Ming-Chia Lin, Chih-Hsin Muo, Su-Yin Yeh, Fung-Chang Sung, Chia-Hung Kao
Medicine.2015; 94(24): e1013. CrossRef - mitoNEET as a novel drug target for mitochondrial dysfunction
Werner J. Geldenhuys, Thomas C. Leeper, Richard T. Carroll
Drug Discovery Today.2014; 19(10): 1601. CrossRef - Diabetes - Increased Risk for Cancers through Chromosomal Aberrations?
Sudhaa Anand, Badari Nath, Radha Saraswathy
Asian Pacific Journal of Cancer Prevention.2014; 15(11): 4571. CrossRef - Oleanolic Acid Induces Metabolic Adaptation in Cancer Cells by Activating the AMP-Activated Protein Kinase Pathway
Jia Liu, Lanhong Zheng, Ning Wu, Leina Ma, Jiateng Zhong, Ge Liu, Xiukun Lin
Journal of Agricultural and Food Chemistry.2014; 62(24): 5528. CrossRef - Association of Vitamin B12Deficiency and Metformin Use in Patients with Type 2 Diabetes
Sun-Hye Ko, Sun-Hee Ko, Yu-Bae Ahn, Ki-Ho Song, Kyung-Do Han, Yong-Moon Park, Seung-Hyun Ko, Hye-Soo Kim
Journal of Korean Medical Science.2014; 29(7): 965. CrossRef - Metformin and Cancer Risk and Mortality: A Systematic Review and Meta-analysis Taking into Account Biases and Confounders
Sara Gandini, Matteo Puntoni, Brandy M. Heckman-Stoddard, Barbara K. Dunn, Leslie Ford, Andrea DeCensi, Eva Szabo
Cancer Prevention Research.2014; 7(9): 867. CrossRef - Effects of Metformin on CD133+ Colorectal Cancer Cells in Diabetic Patients
Yanfei Zhang, Meiping Guan, Zongji Zheng, Qian Zhang, Fang Gao, Yaoming Xue, Chunming Liu
PLoS ONE.2013; 8(11): e81264. CrossRef - AACE Comprehensive Diabetes Management Algorithm 2013 Endocrine Practice
Héctor Eloy Tamez-Pérez, Stephanie Lissette Proskauer-Peña, Mayra Ivonne Hernández-Coria
Endocrine Practice.2013; 19(4): 736. CrossRef - Complications of Diabetes Therapy
Sarah D. Corathers, Shawn Peavie, Marzieh Salehi
Endocrinology and Metabolism Clinics of North America.2013; 42(4): 947. CrossRef - Metformin and Cancer in Type 2 Diabetes
Hyeong Kyu Park
Diabetes & Metabolism Journal.2013; 37(2): 113. CrossRef
- Metformin Reduces Tumor Growth in a Murine Flank Schwannoma Model
- The Risk of Bladder Cancer in Korean Diabetic Subjects Treated with Pioglitazone
- Sun Ok Song, Kwang Joon Kim, Byung-Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
- Diabetes Metab J. 2012;36(5):371-378. Published online October 18, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.5.371
- 4,152 View
- 30 Download
- 30 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background There is growing concern regarding the increased incidence of bladder cancer in diabetic patients using pioglitazone. This study aimed to investigate the association between bladder cancer and the use of pioglitazone in Korean diabetics.
Methods This retrospective, matched case-control study included a case group (
n =329) of diabetic patients with bladder cancer who presented at the Severance Hospital from November 2005 to June 2011. The control group consisted of patients without bladder cancer (1:2 ratio matching for sex and age,n =658) who were listed on the Severance Hospital diabetes registry.Results The percentage of subjects who had ever used pioglitazone was significantly lower in the case group than in the control group (6.4% vs. 15.0%,
P <0.001). Multivariate conditional logistic analysis revealed that independent factors affecting bladder cancer were smoking (odds ratio [OR], 11.64; 95% confidence interval [CI], 6.56 to 20.66;P <0.001), coexisting cancer (OR, 6.11; 95% CI, 2.25 to 16.63;P <0.001), and hemoglobin levels (OR, 0.78; 95% CI, 0.69 to 0.88;P <0.001). The OR of the history of pioglitazone use was 2.09 and was not significantly different between the two groups (95% CI, 0.26 to 16.81;P =0.488).Conclusion A relationship between pioglitazone use and incidence of bladder cancer was not observed in Korean diabetic patients. This suggests that the risk for bladder cancer in Korean diabetic subjects treated with pioglitazone might be different from that of Caucasian populations. Large-scale, well-designed and multi-center studies are needed to further evaluate this relationship.
-
Citations
Citations to this article as recorded by- Cancer biology in diabetes update: Focusing on antidiabetic drugs
Emi Kawakita, Keizo Kanasaki
Journal of Diabetes Investigation.2024;[Epub] CrossRef - Pioglitazone, Bladder Cancer, and the Presumption of Innocence
Georgios S. Papaetis
Current Drug Safety.2022; 17(4): 294. CrossRef - A systematic review of observational studies of the association between pioglitazone use and bladder cancer
E. Ripamonti, L. Azoulay, M. Abrahamowicz, R.W. Platt, S. Suissa
Diabetic Medicine.2019; 36(1): 22. CrossRef - Study design choices for evaluating the comparative safety of diabetes medications: An evaluation of pioglitazone use and risk of bladder cancer in older US adults with type‐2 diabetes
Elizabeth M. Garry, John B. Buse, Mugdha Gokhale, Jennifer L. Lund, Matthew E. Nielsen, Virginia Pate, Til Stürmer
Diabetes, Obesity and Metabolism.2019; 21(9): 2096. CrossRef - Pioglitazone use and risk of bladder cancer: a systematic literature review and meta-analysis of observational studies
Juha Mehtälä, Houssem Khanfir, Dimitri Bennett, Yizhou Ye, Pasi Korhonen, Fabian Hoti
Diabetology International.2019; 10(1): 24. CrossRef - Thiazolidinedione drugs in the treatment of type 2 diabetes mellitus: past, present and future
Melissa A. Davidson, Donald R. Mattison, Laurent Azoulay, Daniel Krewski
Critical Reviews in Toxicology.2018; 48(1): 52. CrossRef - An updated meta-analysis of pioglitazone exposure and bladder cancer and comparison to the drug’s effect on cardiovascular disease and non-alcoholic steatohepatitis
Mayer B. Davidson, Deyu Pan
Diabetes Research and Clinical Practice.2018; 135: 102. CrossRef - Pioglitazone and risk of bladder cancer in type 2 diabetes mellitus patients: A systematic literature review and meta-analysis of observational studies using real-world data
Mohammad Adil, Rashid Ali Khan, Pinaki Ghosh, Shiva Kumar Venkata, Amit Dattatraya Kandhare, Manju Sharma
Clinical Epidemiology and Global Health.2018; 6(2): 61. CrossRef - Pioglitazone and bladder cancer risk: a systematic review and meta‐analysis
Huilin Tang, Weilong Shi, Shuangshuang Fu, Tiansheng Wang, Suodi Zhai, Yiqing Song, Jiali Han
Cancer Medicine.2018; 7(4): 1070. CrossRef - Global and Regional Effects of Bladder Cancer Risk Associated with Pioglitazone Therapy in Patients with Diabetes
Hua Qu, Yi Zheng, Yuren Wang, Rui Zhang, Xiongzhong Ruan, Gangyi Yang, Zhenqi Liu, Hongting Zheng
Scientific Reports.2017;[Epub] CrossRef - Pioglitazone and the Risk of Bladder Cancer: A Meta-Analysis
Elena Filipova, Katya Uzunova, Krassimir Kalinov, Toni Vekov
Diabetes Therapy.2017; 8(4): 705. CrossRef - Pioglitazone does not increase the risk of type II diabetes in patients with bladder cancer: A retrospective study
YOUHONG DONG, ANPING WANG
Oncology Letters.2016; 12(1): 89. CrossRef - Ten‐year observational follow‐up of PROactive: a randomized cardiovascular outcomes trial evaluating pioglitazone in type 2 diabetes
E. Erdmann, S. Harding, H. Lam, A. Perez
Diabetes, Obesity and Metabolism.2016; 18(3): 266. CrossRef - Pioglitazone (Actos) and bladder cancer: Legal system triumphs over the evidence
Mayer B. Davidson
Journal of Diabetes and its Complications.2016; 30(6): 981. CrossRef - The current role of thiazolidinediones in diabetes management
Christos V. Rizos, Anastazia Kei, Moses S. Elisaf
Archives of Toxicology.2016; 90(8): 1861. CrossRef - Development of vascular complications and bladder carcinoma in diabetics using pioglitazone: A five-year Indian review
Saarwaani Vallabhajosyula, Shashaank Vallabhajosyula, Saraschandra Vallabhajosyula, Suma Nair, Asha Kamath, Karthik N. Rao
Medical Journal Armed Forces India.2016; 72(3): 253. CrossRef - Baseline glycemic status and mortality in 241,499 Korean metropolitan subjects: A Kangbuk Samsung Health Study
Eun-Jung Rhee, Se Eun Park, Yoosoo Chang, Seungho Ryu, Won-Young Lee
Metabolism.2016; 65(2): 68. CrossRef - Rosiglitazone Use and the Risk of Bladder Cancer in Patients With Type 2 Diabetes
Eugene Han, Suk-Yong Jang, Gyuri Kim, Yong-ho Lee, Eun Yeong Choe, Chung Mo Nam, Eun Seok Kang
Medicine.2016; 95(6): e2786. CrossRef - Polemics of pioglitazone: an appraisal in 2015
Awadhesh Kumar Singh
Expert Review of Endocrinology & Metabolism.2015; 10(4): 447. CrossRef - Pioglitazone and bladder cancer risk: a multipopulation pooled, cumulative exposure analysis
Daniel Levin, Samira Bell, Reijo Sund, Sirpa A. Hartikainen, Jaakko Tuomilehto, Eero Pukkala, Ilmo Keskimäki, Ellena Badrick, Andrew G. Renehan, Iain E. Buchan, Samantha L. Bowker, Jasjeet K. Minhas-Sandhu, Zafar Zafari, Carlo Marra, Jeffrey A. Johnson, B
Diabetologia.2015; 58(3): 493. CrossRef - Thiazolidinediones and associated risk of bladder cancer: a systematic review and meta‐analysis
Richard M. Turner, Chun S. Kwok, Chen Chen‐Turner, Chinedu A. Maduakor, Sonal Singh, Yoon K. Loke
British Journal of Clinical Pharmacology.2014; 78(2): 258. CrossRef - A Review on Thiazolidinediones and Bladder Cancer in Human Studies
Chin-Hsiao Tseng
Journal of Environmental Science and Health, Part C.2014; 32(1): 1. CrossRef - Physiological Functions of Peroxisome Proliferator-Activated Receptor β
Jaap G. Neels, Paul A. Grimaldi
Physiological Reviews.2014; 94(3): 795. CrossRef - Risk of Bladder Cancer among Patients with Diabetes Treated with a 15 mg Pioglitazone Dose in Korea: A Multi-Center Retrospective Cohort Study
Sang-Man Jin, Sun Ok Song, Chang Hee Jung, Jin-Sun Chang, Sunghwan Suh, Seung Min Kang, Inkyung Jung, Cheol-Young Park, Jae Hyeon Kim, Jae Hyoung Cho, Byung-Wan Lee
Journal of Korean Medical Science.2014; 29(2): 238. CrossRef - Pioglitazone
SS Jadhav, VK Shivane, AR Lila, TR Bandgar, NS Shah
Journal of Postgraduate Medicine.2014; 60(3): 293. CrossRef - Refocusing Peroxisome Proliferator Activated Receptor-α: A New Insight for Therapeutic Roles in Diabetes
Hannah Seok, Bong Soo Cha
Diabetes & Metabolism Journal.2013; 37(5): 326. CrossRef - Effects of co-administration of candesartan with pioglitazone on inflammatory parameters in hypertensive patients with type 2 diabetes mellitus: a preliminary report
Hirofumi Suzuki, Masaya Sakamoto, Takeshi Hayashi, Hiroyuki Iuchi, Kennosuke Ohashi, Tsuyoshi Isaka, Noriko Sakamoto, Yosuke Kayama, Katsuyoshi Tojo, Michihiro Yoshimura, Kazunori Utsunomiya
Cardiovascular Diabetology.2013;[Epub] CrossRef - The Future of Thiazolidinedione Therapy in the Management of Type 2 Diabetes Mellitus
Hanford Yau, Kathya Rivera, Romina Lomonaco, Kenneth Cusi
Current Diabetes Reports.2013; 13(3): 329. CrossRef - Letter: The Risk of Bladder Cancer in Korean Diabetic Subjects Treated with Pioglitazone (Diabetes Metab J2012;36:371-8)
Sheyu Li, Haoming Tian
Diabetes & Metabolism Journal.2013; 37(1): 81. CrossRef - Metabolic Surgery for Type 2 Diabetes in Patients with a BMI of <35 kg/m2: A Surgeon’s Perspective
Ricardo Cohen, Pedro Paulo Caravatto, Tarissa Petry
Obesity Surgery.2013; 23(6): 809. CrossRef
- Cancer biology in diabetes update: Focusing on antidiabetic drugs

 KDA
KDA
 First
First Prev
Prev





