
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Cardiovascular Risk/Epidemiology
- Comparison of on-Statin Lipid and Lipoprotein Levels for the Prediction of First Cardiovascular Event in Type 2 Diabetes Mellitus
- Ji Yoon Kim, Jimi Choi, Sin Gon Kim, Nam Hoon Kim
- Diabetes Metab J. 2023;47(6):837-845. Published online August 23, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0217
- 1,469 View
- 175 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
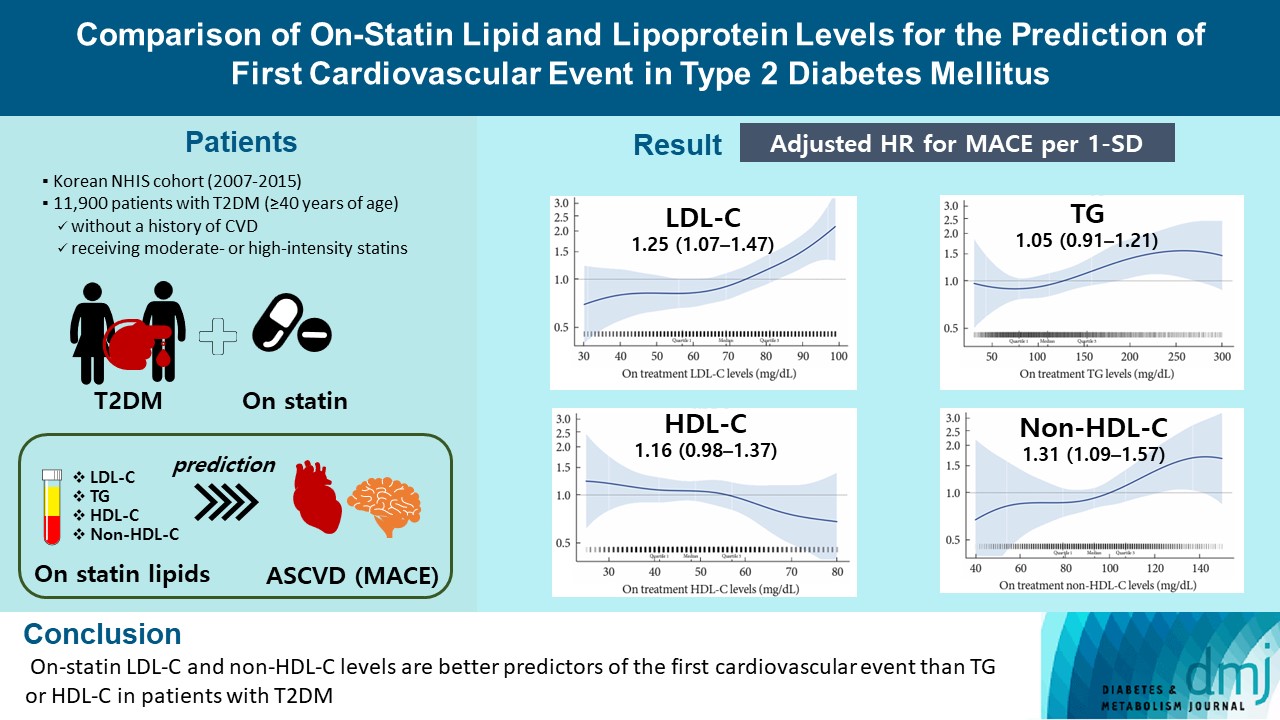
A substantial cardiovascular disease risk remains even after optimal statin therapy. Comparative predictiveness of major lipid and lipoprotein parameters for cardiovascular events in patients with type 2 diabetes mellitus (T2DM) who are treated with statins is not well documented.
Methods
From the Korean Nationwide Cohort, 11,900 patients with T2DM (≥40 years of age) without a history of cardiovascular disease and receiving moderate- or high-intensity statins were included. The primary outcome was the first occurrence of major adverse cardiovascular events (MACE) including ischemic heart disease, ischemic stroke, and cardiovascular death. The risk of MACE was estimated according to on-statin levels of low-density lipoprotein cholesterol (LDL-C), triglyceride (TG), highdensity lipoprotein cholesterol (HDL-C), and non-HDL-C.
Results
MACE occurred in 712 patients during a median follow-up period of 37.9 months (interquartile range, 21.7 to 54.9). Among patients achieving LDL-C levels less than 100 mg/dL, the hazard ratios for MACE per 1-standard deviation change in ontreatment values were 1.25 (95% confidence interval [CI], 1.07 to 1.47) for LDL-C, 1.31 (95% CI, 1.09 to 1.57) for non-HDL-C, 1.05 (95% CI, 0.91 to 1.21) for TG, and 1.16 (95% CI, 0.98 to 1.37) for HDL-C, after adjusting for potential confounders and lipid parameters mutually. The predictive ability of on-statin LDL-C and non-HDL-C for MACE was prominent in patients at high cardiovascular risk or those with LDL-C ≥70 mg/dL.
Conclusion
On-statin LDL-C and non-HDL-C levels are better predictors of the first cardiovascular event than TG or HDL-C in patients with T2DM.
- Cardiovascular Risk/Epidemiology
- Intensified Multifactorial Intervention in Patients with Type 2 Diabetes Mellitus
- Takayoshi Sasako, Toshimasa Yamauchi, Kohjiro Ueki
- Diabetes Metab J. 2023;47(2):185-197. Published online January 12, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0325
- 5,109 View
- 358 Download
- 8 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
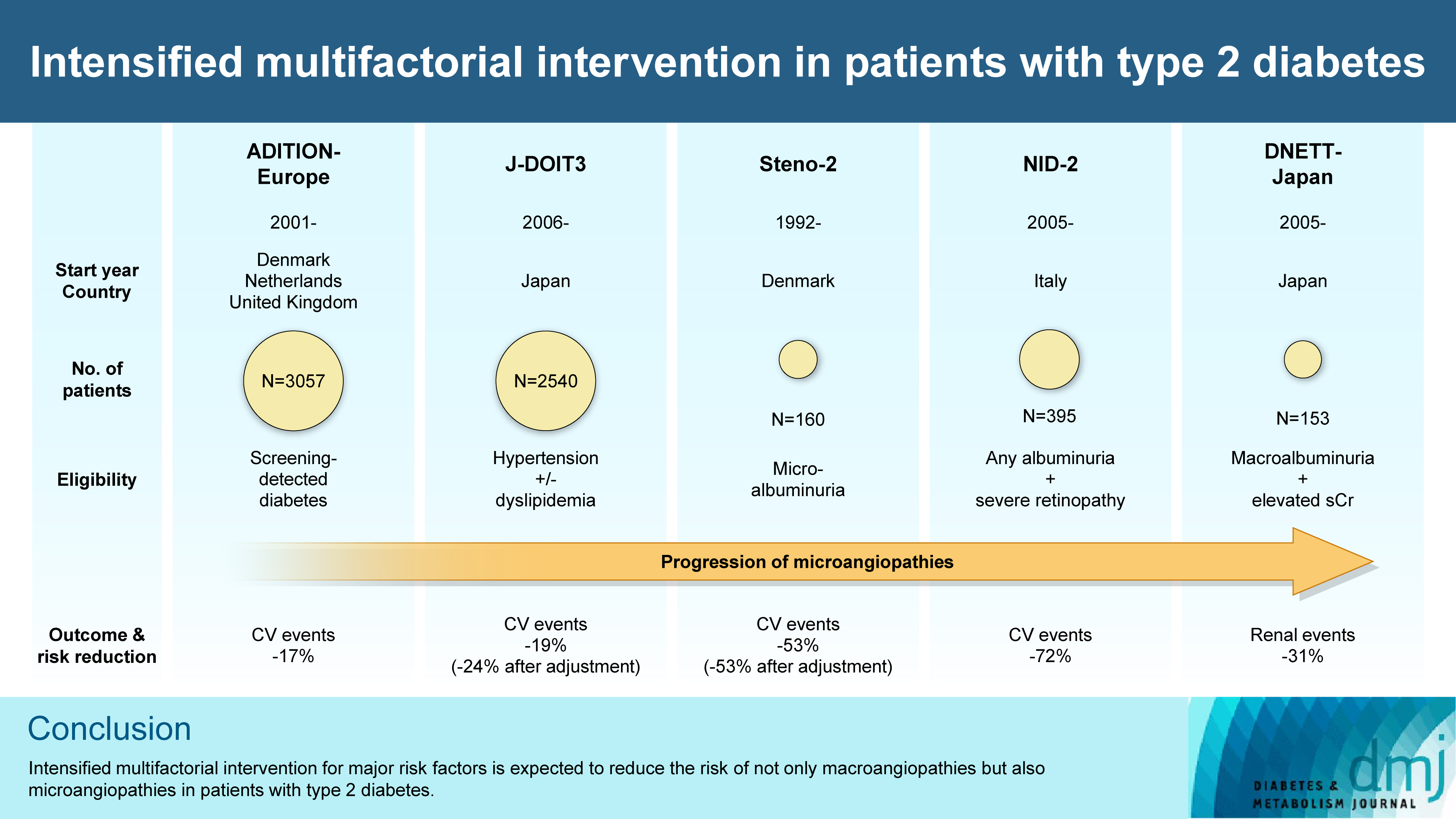
ePub - In the management of diabetes mellitus, one of the most important goals is to prevent its micro- and macrovascular complications, and to that end, multifactorial intervention is widely recommended. Intensified multifactorial intervention with pharmacotherapy for associated risk factors, alongside lifestyle modification, was first shown to be efficacious in patients with microalbuminuria (Steno-2 study), then in those with less advanced microvascular complications (the Anglo-Danish-Dutch Study of Intensive Treatment In People with Screen Detected Diabetes in Primary Care [ADDITION]-Europe and the Japan Diabetes Optimal Treatment study for 3 major risk factors of cardiovascular diseases [J-DOIT3]), and in those with advanced microvascular complications (the Nephropathy In Diabetes-Type 2 [NID-2] study and Diabetic Nephropathy Remission and Regression Team Trial in Japan [DNETT-Japan]). Thus far, multifactorial intervention led to a reduction in cardiovascular and renal events, albeit not necessarily significant. It should be noted that not only baseline characteristics but also the control status of the risk factors and event rates during intervention among the patients widely varied from one trial to the next. Further evidence is needed for the efficacy of multifactorial intervention in a longer duration and in younger or elderly patients. Moreover, now that new classes of antidiabetic drugs are available, it should be addressed whether strict and safe glycemic control, alongside control of other risk factors, could lead to further risk reductions in micro- and macrovascular complications, thereby decreasing all-cause mortality in patients with type 2 diabetes mellitus.
-
Citations
Citations to this article as recorded by- Exploring mechanisms underlying diabetes comorbidities and strategies to prevent vascular complications
Takayoshi Sasako
Diabetology International.2024; 15(1): 34. CrossRef - Targeting ERS-mitophagy in hippocampal neurons to explore the improvement of memory by tea polyphenols in aged type 2 diabetic rats
Wenjuan Feng, Chenhui Lv, Le Cheng, Xin Song, Xuemin Li, Haoran Xie, Shuangzhi Chen, Xi Wang, Lushan Xue, Cheng Zhang, Jie Kou, Lili Wang, Haifeng Zhao
Free Radical Biology and Medicine.2024; 213: 293. CrossRef - Risk of Dementia Among Patients With Diabetes in a Multidisciplinary, Primary Care Management Program
Kailu Wang, Shi Zhao, Eric Kam-Pui Lee, Susan Zi-May Yau, Yushan Wu, Chi-Tim Hung, Eng-Kiong Yeoh
JAMA Network Open.2024; 7(2): e2355733. CrossRef - Causes of In-Hospital Death and Pharmaceutical Associations with Age of Death during a 10-Year Period (2011–2020) in Individuals with and without Diabetes at a Japanese Community General Hospital
Minae Hosoki, Taiki Hori, Yousuke Kaneko, Kensuke Mori, Saya Yasui, Seijiro Tsuji, Hiroki Yamagami, Saki Kawata, Tomoyo Hara, Shiho Masuda, Yukari Mitsui, Kiyoe Kurahashi, Takeshi Harada, Shingen Nakamura, Toshiki Otoda, Tomoyuki Yuasa, Akio Kuroda, Itsur
Journal of Clinical Medicine.2024; 13(5): 1283. CrossRef - External validation of a minimal-resource model to predict reduced estimated glomerular filtration rate in people with type 2 diabetes without diagnosis of chronic kidney disease in Mexico: a comparison between country-level and regional performance
Camilla Sammut-Powell, Rose Sisk, Ruben Silva-Tinoco, Gustavo de la Pena, Paloma Almeda-Valdes, Sonia Citlali Juarez Comboni, Susana Goncalves, Rory Cameron
Frontiers in Endocrinology.2024;[Epub] CrossRef - Gut Microbiota Targeted Approach by Natural Products in Diabetes Management: An Overview
Priyanka Sati, Praveen Dhyani, Eshita Sharma, Dharam Chand Attri, Arvind Jantwal, Rajni Devi, Daniela Calina, Javad Sharifi-Rad
Current Nutrition Reports.2024;[Epub] CrossRef - Cardiovascular Risk Reduction in Type 2 Diabetes: Further Insights into the Power of Weight Loss and Exercise
Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(3): 302. CrossRef - Sarcopenia: Loss of mighty armor against frailty and aging
Takayoshi Sasako, Kohjiro Ueki
Journal of Diabetes Investigation.2023; 14(10): 1145. CrossRef
- Exploring mechanisms underlying diabetes comorbidities and strategies to prevent vascular complications
- Metabolic Risk/Epidemiology
- Postprandial Free Fatty Acids at Mid-Pregnancy Increase the Risk of Large-for-Gestational-Age Newborns in Women with Gestational Diabetes Mellitus
- So-Yeon Kim, Young Shin Song, Soo-Kyung Kim, Yong-Wook Cho, Kyung-Soo Kim
- Diabetes Metab J. 2022;46(1):140-148. Published online August 9, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0023
- 5,012 View
- 160 Download
- 3 Web of Science
- 3 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
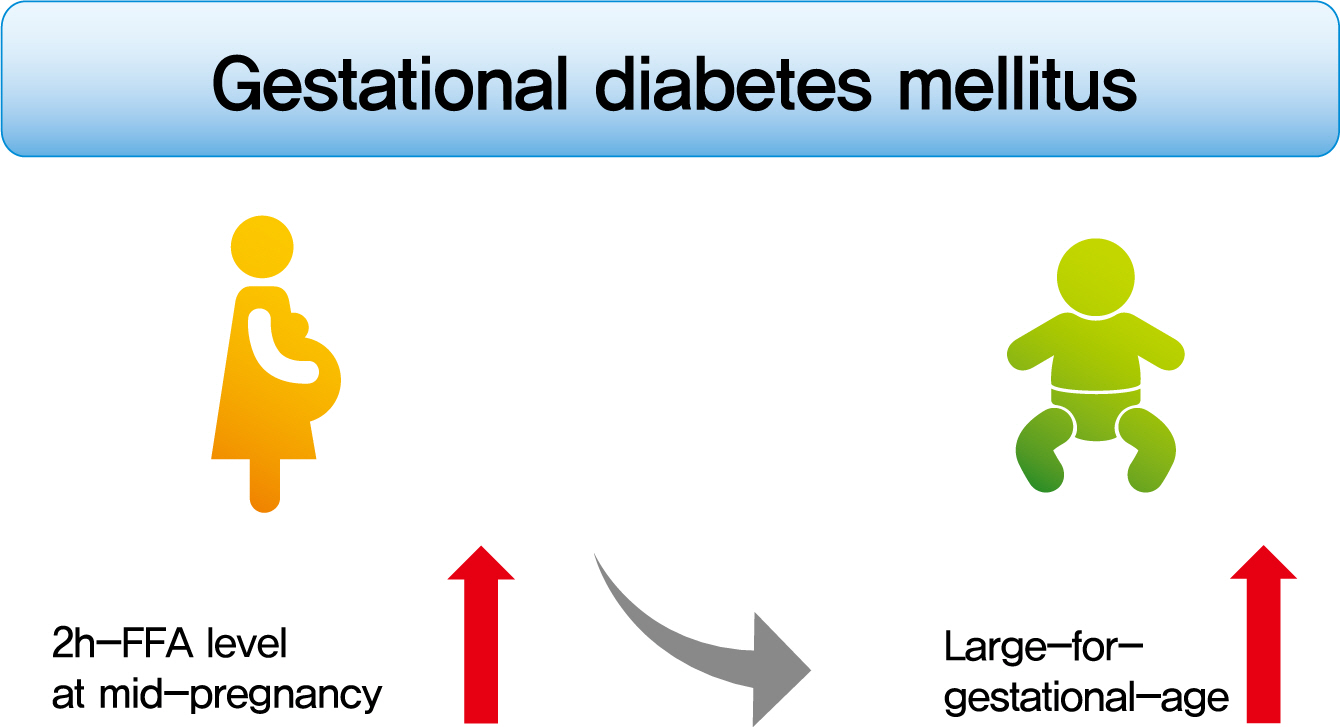
To investigate the association between free fatty acid (FFA) level at mid-pregnancy and large-for-gestational-age (LGA) newborns in women with gestational diabetes mellitus (GDM).
Methods
We enrolled 710 pregnant women diagnosed with GDM from February 2009 to October 2016. GDM was diagnosed by a ‘two-step’ approach with Carpenter and Coustan criteria. We measured plasma lipid profiles including fasting and 2-hour postprandial FFA (2h-FFA) levels at mid-pregnancy. LGA was defined if birthweights of newborns were above the 90th percentile for their gestational age.
Results
Mean age of pregnant women in this study was 33.1 years. Mean pre-pregnancy body mass index (BMI) was 22.4 kg/m2. The prevalence of LGA was 8.3% (n=59). Levels of 2h-FFA were higher in women who delivered LGA newborns than in those who delivered non-LGA newborns (416.7 μEq/L vs. 352.5 μEq/L, P=0.006). However, fasting FFA was not significantly different between the two groups. The prevalence of delivering LGA newborns was increased with increasing tertile of 2h-FFA (T1, 4.3%; T2, 9.8%; T3, 10.7%; P for trend <0.05). After adjustment for maternal age, pre-pregnancy BMI, and fasting plasma glucose, the highest tertile of 2h-FFA was 2.38 times (95% confidence interval, 1.11 to 5.13) more likely to have LGA newborns than the lowest tertile. However, there was no significant difference between groups according to fasting FFA tertiles.
Conclusion
In women with GDM, a high 2h-FFA level (but not fasting FFA) at mid-pregnancy is associated with an increasing risk of delivering LGA newborns. -
Citations
Citations to this article as recorded by- Advances in free fatty acid profiles in gestational diabetes mellitus
Haoyi Du, Danyang Li, Laura Monjowa Molive, Na Wu
Journal of Translational Medicine.2024;[Epub] CrossRef - Modulation of gut microbiota and lipid metabolism in rats fed high-fat diets by Ganoderma lucidum triterpenoids
Aijun Tong, Weihao Wu, Zhengxin Chen, Jiahui Wen, Ruibo Jia, Bin Liu, Hui Cao, Chao Zhao
Current Research in Food Science.2023; 6: 100427. CrossRef - Fetal Abdominal Obesity Detected at 24 to 28 Weeks of Gestation Persists until Delivery Despite Management of Gestational Diabetes Mellitus (Diabetes Metab J 2021;45:547-57)
Wonjin Kim, Soo Kyung Park, Yoo Lee Kim
Diabetes & Metabolism Journal.2021; 45(6): 970. CrossRef
- Advances in free fatty acid profiles in gestational diabetes mellitus
- Obesity and Metabolic Syndrome
- Comparison of Competitive Models of Metabolic Syndrome Using Structural Equation Modeling: A Confirmatory Factor Analysis
- Karimollah Hajian-Tilaki
- Diabetes Metab J. 2018;42(5):433-441. Published online October 22, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0010
- 3,232 View
- 41 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The purpose of this study was to apply the structural equation modeling (SEM) to compare the fitness of different competing models (one, two, and three factors) of the metabolic syndrome (MetS) in Iranian adult population.
Methods Data are given on the cardiometabolic risk factors of 841 individuals with nondiabetic adults from a cross-sectional population-based study of glucose, lipids, and MetS in the north of Iran. The three conceptual hypothesized models (single factor, two correlated factors, and three correlated latent factors) were evaluated by using confirmatory factor analysis with the SEM approach. The summary statistics of correlation coefficients and the model summary fitting indexes were calculated.
Results The findings show that a single-factor model and a two-correlated factor model had a poorer summary fitting index compared with a three-correlated factor model. All fitting criteria met the conceptual hypothesized three-correlated factor model for both sexes. However, the correlation structure between the three underlying constructs designating the MetS was higher in women than in men.
Conclusion These results indicate the plausibility of the pathophysiology and etiology of MetS being multifactorial, rather than a single factor, in a nondiabetic Iranian adult population.
-
Citations
Citations to this article as recorded by- Structural Equation Modelling for Predicting the Relative Contribution of Each Component in the Metabolic Syndrome Status Change
José E. Teixeira, José A. Bragada, João P. Bragada, Joana P. Coelho, Isabel G. Pinto, Luís P. Reis, Paula O. Fernandes, Jorge E. Morais, Pedro M. Magalhães
International Journal of Environmental Research and Public Health.2022; 19(6): 3384. CrossRef - New risk score model for identifying individuals at risk for diabetes in southwest China
Liying Li, Ziqiong Wang, Muxin Zhang, Haiyan Ruan, Linxia Zhou, Xin Wei, Ye Zhu, Jiafu Wei, Sen He
Preventive Medicine Reports.2021; 24: 101618. CrossRef - Definition and early diagnosis of metabolic syndrome in children
Gunter Matthias Christian Flemming, Sarah Bussler, Antje Körner, Wieland Kiess
Journal of Pediatric Endocrinology and Metabolism.2020; 33(7): 821. CrossRef - Calcium-Sensing Receptor in Adipose Tissue: Possible Association with Obesity-Related Elevated Autophagy
Pamela Mattar, Sofía Sanhueza, Gabriela Yuri, Lautaro Briones, Claudio Perez-Leighton, Assaf Rudich, Sergio Lavandero, Mariana Cifuentes
International Journal of Molecular Sciences.2020; 21(20): 7617. CrossRef
- Structural Equation Modelling for Predicting the Relative Contribution of Each Component in the Metabolic Syndrome Status Change
- Pathophysiology
- The Phospholipid Linoleoylglycerophosphocholine as a Biomarker of Directly Measured Insulin Resistance
- Maria Camila Pérez-Matos, Martha Catalina Morales-Álvarez, Freddy Jean Karlo Toloza, Maria Laura Ricardo-Silgado, Jose Oscar Mantilla-Rivas, Jairo Arturo Pinzón-Cortes, Maritza Perez-Mayorga, Elizabeth Jiménez, Edwin Guevara, Carlos O Mendivil
- Diabetes Metab J. 2017;41(6):466-473. Published online November 27, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.6.466
- 4,139 View
- 43 Download
- 9 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Plasma concentrations of some lysophospholipids correlate with metabolic alterations in humans, but their potential as biomarkers of insulin resistance (IR) is insufficiently known. We aimed to explore the association between plasma linoleoylglycerophosphocholine (LGPC) and objective measures of IR in adults with different metabolic profiles.
Methods We studied 62 men and women, ages 30 to 69 years, (29% normal weight, 59% overweight, 12% obese). Participants underwent a 5-point oral glucose tolerance test (5p-OGTT) from which we calculated multiple indices of IR and insulin secretion. Fifteen participants additionally underwent a hyperinsulinemic-euglycemic clamp for estimation of insulin-stimulated glucose disposal. Plasma LGPC was determined using high performance liquid chromatography/time-of-flight mass spectrometry. Plasma LGPC was compared across quartiles defined by the IR indices.
Results Mean LGPC was 15.4±7.6 ng/mL in women and 14.1±7.3 ng/mL in men. LGPC did not correlate with body mass in-dex, percent body fat, waist circumference, blood pressure, glycosylated hemoglobin, log-triglycerides, or high density lipoprotein cholesterol. Plasma LGPC concentrations was not systematically associated with any of the studied 5p-OGTT-derived IR indices. However, LGPC exhibited a significant negative correlation with glucose disposal in the clamp (Spearman
r =−0.56,P =0.029). Despite not being diabetic, participants with higher plasma LGPC exhibited significantly higher post-challenge plasma glucose excursions in the 5p-OGTT (P trend=0.021 for the increase in glucose area under the curve across quartiles of plasma LGPC).Conclusion In our sample of Latino adults without known diabetes, LGPC showed potential as a biomarker of IR and impaired glucose metabolism.
-
Citations
Citations to this article as recorded by- Identification of potential serum biomarkers associated with HbA1c levels in Indian type 2 diabetic subjects using NMR-based metabolomics
Saleem Yousf, Hitender S. Batra, Rakesh M. Jha, Devika M. Sardesai, Kalyani Ananthamohan, Jeetender Chugh, Shilpy Sharma
Clinica Chimica Acta.2024; 557: 117857. CrossRef - Comparative Metabolomic Profiling of L-Histidine and NEFA Treatments in Bovine Mammary Epithelial Cells
Wenqiang Sun, Mengze Li, Hanjun Ren, Yang Chen, Wei Zeng, Xiong Tan, Xianbo Jia, Shiyi Chen, Jie Wang, Songjia Lai
Animals.2024; 14(7): 1045. CrossRef - Mechanistic Insight of Innovative Biomarkers for Screening of Type II Diabetes
Mellitus
Shubh Deep Yadav, Neelam Singh
Current Indian Science.2024;[Epub] CrossRef - Is insulin resistance tissue-dependent and substrate-specific? The role of white adipose tissue and skeletal muscle
Diana Calderón-DuPont, Ivan Torre-Villalvazo, Andrea Díaz-Villaseñor
Biochimie.2023; 204: 48. CrossRef - Causality of genetically determined metabolites and metabolic pathways on osteoarthritis: a two-sample mendelian randomization study
Yifei Gu, Qianmei Jin, Jinquan Hu, Xinwei Wang, Wenchao Yu, Zhanchao Wang, Chen Wang, Yang Liu, Yu Chen, Wen Yuan
Journal of Translational Medicine.2023;[Epub] CrossRef - Assessing the causal effect of genetically predicted metabolites and metabolic pathways on stroke
Tianlong Zhang, Yina Cao, Jianqiang Zhao, Jiali Yao, Gang Liu
Journal of Translational Medicine.2023;[Epub] CrossRef - Lipidomics in diabetes
Eun Ji Kim, Radha Ramachandran, Anthony S. Wierzbicki
Current Opinion in Endocrinology, Diabetes & Obesity.2022; 29(2): 124. CrossRef - Recent Developments in Biomarkers for Diagnosis and Screening of Type 2 Diabetes Mellitus
Margarita Ortiz-Martínez, Mirna González-González, Alexandro J. Martagón, Victoria Hlavinka, Richard C. Willson, Marco Rito-Palomares
Current Diabetes Reports.2022; 22(3): 95. CrossRef - Discrete Correlation Summation Clustering Reveals Differential Regulation of Liver Metabolism by Thrombospondin-1 in Low-Fat and High-Fat Diet-Fed Mice
Steven M. Bronson, Brian Westwood, Katherine L. Cook, Nancy J. Emenaker, Mark C. Chappell, David D. Roberts, David R. Soto-Pantoja
Metabolites.2022; 12(11): 1036. CrossRef - Metabolic Dysfunction Biomarkers as Predictors of Early Diabetes
Carla Luís, Pilar Baylina, Raquel Soares, Rúben Fernandes
Biomolecules.2021; 11(11): 1589. CrossRef - Serum metabolomics analysis of mice that received repeated airway exposure to a water-soluble PM2.5 extract
Chen Zhao, Mengyuan Niu, Shiyu Song, Jing Li, Zhonglan Su, Yong Wang, Qian Gao, Hongwei Wang
Ecotoxicology and Environmental Safety.2019; 168: 102. CrossRef
- Identification of potential serum biomarkers associated with HbA1c levels in Indian type 2 diabetic subjects using NMR-based metabolomics
- The Effect of DPP-4 Inhibitors on Metabolic Parameters in Patients with Type 2 Diabetes
- Eun Yeong Choe, Yongin Cho, Younjeong Choi, Yujung Yun, Hye Jin Wang, Obin Kwon, Byung-Wan Lee, Chul Woo Ahn, Bong Soo Cha, Hyun Chul Lee, Eun Seok Kang
- Diabetes Metab J. 2014;38(3):211-219. Published online June 17, 2014
- DOI: https://doi.org/10.4093/dmj.2014.38.3.211
- 4,684 View
- 69 Download
- 27 Web of Science
- 25 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background We evaluated the effects of two dipeptidyl peptidase-4 (DPP-4) inhibitors, sitagliptin and vildagliptin, on metabolic parameters in patients with type 2 diabetes mellitus.
Methods A total of 170 type 2 diabetes patients treated with sitagliptin or vildagliptin for more than 24 weeks were selected. The patients were separated into two groups, sitagliptin (100 mg once daily,
n =93) and vildagliptin (50 mg twice daily,n =77). We compared the effect of each DPP-4 inhibitor on metabolic parameters, including the fasting plasma glucose (FPG), postprandial glucose (PPG), glycated hemoglobin (HbA1c), and glycated albumin (GA) levels, and lipid parameters at baseline and after 24 weeks of treatment.Results The HbA1c, FPG, and GA levels were similar between the two groups at baseline, but the sitagliptin group displayed a higher PPG level (
P =0.03). After 24 weeks of treatment, all of the glucose-related parameters were significantly decreased in both groups (P =0.001). The levels of total cholesterol and triglycerides were only reduced in the vildagliptin group (P =0.001), although the sitagliptin group received a larger quantity of statins than the vildagliptin group (P =0.002).The mean change in the glucose- and lipid-related parameters after 24 weeks of treatment were not significantly different between the two groups (P =not significant). Neither sitagliptin nor vildagliptin treatment was associated with a reduction in the high sensitive C-reactive protein level (P =0.714).Conclusion Vildagliptin and sitagliptin exert a similar effect on metabolic parameters, but vildagliptin exerts a more potent beneficial effect on lipid parameters.
-
Citations
Citations to this article as recorded by- Insulin Tregopil: An Ultra-Fast Oral Recombinant Human Insulin Analog: Preclinical and Clinical Development in Diabetes Mellitus
Shashank Joshi, Vathsala Jayanth, Subramanian Loganathan, Vasan K. Sambandamurthy, Sandeep N. Athalye
Drugs.2023; 83(13): 1161. CrossRef - Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
Jun Sung Moon, Sunghwan Suh, Sang Soo Kim, Heung Yong Jin, Jeong Mi Kim, Min Hee Jang, Kyung Ae Lee, Ju Hyung Lee, Seung Min Chung, Young Sang Lyu, Jin Hwa Kim, Sang Yong Kim, Jung Eun Jang, Tae Nyun Kim, Sung Woo Kim, Eonju Jeon, Nan Hee Cho, Mi-Kyung Ki
Diabetes & Metabolism Journal.2021; 45(5): 675. CrossRef - Vasculoprotective Effects of Vildagliptin. Focus on Atherogenesis
Michał Wiciński, Karol Górski, Eryk Wódkiewicz, Maciej Walczak, Magdalena Nowaczewska, Bartosz Malinowski
International Journal of Molecular Sciences.2020; 21(7): 2275. CrossRef - Anti-inflammatory properties of antidiabetic drugs: A “promised land” in the COVID-19 era?
Niki Katsiki, Ele Ferrannini
Journal of Diabetes and its Complications.2020; 34(12): 107723. CrossRef Effect of Switching from Linagliptin to Teneligliptin Dipeptidyl Peptidase-4 Inhibitors in Older Patients with Type 2 Diabetes Mellitus
Eugene Han, Minyoung Lee, Yong-ho Lee, Hye Soon Kim, Byung-wan Lee, Bong-Soo Cha, Eun Seok Kang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4113. CrossRef- Combined vildagliptin and memantine treatment downregulates expression of amyloid precursor protein, and total and phosphorylated tau in a rat model of combined Alzheimer’s disease and type 2 diabetes
Samar S. Khalaf, Mohamed M. Hafez, Eman T. Mehanna, Noha M. Mesbah, Dina M. Abo-Elmatty
Naunyn-Schmiedeberg's Archives of Pharmacology.2019; 392(6): 685. CrossRef - Therapeutic experience of saxagliptin as first add-on after metformin in Indian type 2 diabetes patients: A non-interventional, prospective, observational study (ONTARGET-INDIA)
Sanjay Kalra, Sarita Bajaj, AG Unnikrishnan, ManashP Baruah, Rakesh Sahay, V Hardik, Amit Kumar
Indian Journal of Endocrinology and Metabolism.2019; 23(3): 312. CrossRef - Cardiovascular Outcome Trials of the Incretin-Based Therapies: What Do We Know So Far?
Pablo F. Mora, Eric L. Johnson
Endocrine Practice.2017; 23(1): 89. CrossRef - Treatment of Dyslipidemias to Prevent Cardiovascular Disease in Patients with Type 2 Diabetes
Maryam Khavandi, Francisco Duarte, Henry N. Ginsberg, Gissette Reyes-Soffer
Current Cardiology Reports.2017;[Epub] CrossRef - Sodium butyrate has context-dependent actions on dipeptidyl peptidase-4 and other metabolic parameters
Eun-Sol Lee, Dong-Sung Lee, Prakash Raj Pandeya, Youn-Chul Kim, Dae-Gil Kang, Ho-Sub Lee, Byung-Chul Oh, Dae Ho Lee
The Korean Journal of Physiology & Pharmacology.2017; 21(5): 519. CrossRef - Risk of Myopathy Associated With DPP-4 Inhibitors in Combination With Statins: A Disproportionality Analysis Using Data From the WHO and French Spontaneous Reporting Databases
Vanessa Labat, Mickael Arnaud, Ghada Miremont-Salamé, Francesco Salvo, Bernard Bégaud, Antoine Pariente
Diabetes Care.2017; 40(3): e27. CrossRef - Soluble DPP-4 up-regulates toll-like receptors and augments inflammatory reactions, which are ameliorated by vildagliptin or mannose-6-phosphate
Dong-Sung Lee, Eun-Sol Lee, Md. Morshedul Alam, Jun-Hyeog Jang, Ho-Sub Lee, Hyuncheol Oh, Youn-Chul Kim, Zahid Manzoor, Young-Sang Koh, Dae-Gil Kang, Dae Ho Lee
Metabolism.2016; 65(2): 89. CrossRef - A Multifactorial Approach to Reduce Cardiovascular Disease in Type 2 Diabetes Mellitus: Now More Than Ever
Jan N. Basile
Hospital Practice.2016; 44(1): 9. CrossRef - Association between DPP4 gene polymorphism and serum lipid levels in Chinese type 2 diabetes individuals
Xiaomin Xing, Yi Han, Xiaojun Zhou, Bo Zhang, Yan Li, Zhongsu Wang, Lin Liao, Lequn Su
Neuropeptides.2016; 60: 1. CrossRef - Common medications used by patients with type 2 diabetes mellitus: what are their effects on the lipid profile?
Paul D. Rosenblit
Cardiovascular Diabetology.2016;[Epub] CrossRef - Dipeptidyl peptidase-4 inhibition and narrow-band ultraviolet-B light in psoriasis (DINUP): study protocol for a randomised controlled trial
Maeve Lynch, Tomás B. Ahern, Irene Timoney, Cheryl Sweeney, Genevieve Kelly, Rosalind Hughes, Anne-Marie Tobin, Donal O’Shea, Brian Kirby
Trials.2016;[Epub] CrossRef - Efficacy of different dipeptidyl peptidase-4 (DPP-4) inhibitors on metabolic parameters in patients with type 2 diabetes undergoing dialysis
Se Hee Park, Joo Young Nam, Eugene Han, Yong-ho Lee, Byung-Wan Lee, Beom Seok Kim, Bong-Soo Cha, Chul Sik Kim, Eun Seok Kang
Medicine.2016; 95(32): e4543. CrossRef - Incretin-based therapies for obesity treatment
Aline Haas de Mello, Morgana Prá, Larissa Colonetti Cardoso, Rosiane de Bona Schraiber, Gislaine Tezza Rezin
Metabolism.2015; 64(9): 967. CrossRef - Brain signaling systems in the Type 2 diabetes and metabolic syndrome: promising target to treat and prevent these diseases
Alexander O Shpakov, Kira V Derkach, Lev M Berstein
Future Science OA.2015;[Epub] CrossRef - Comparative analysis of therapeutic efficiency and costs (experience in Bulgaria) of oral antidiabetic therapies based on glitazones and gliptins
Elena Pavlova Filipova, Katya Hristova Uzunova, Toni Yonkov Vekov
Diabetology & Metabolic Syndrome.2015;[Epub] CrossRef - Antidiabetic Effect of Galantamine: Novel Effect for a Known Centrally Acting Drug
Mennatallah A. Ali, Hanan S. El-Abhar, Maher A. Kamel, Ahmed S. Attia, John Calvert
PLOS ONE.2015; 10(8): e0134648. CrossRef - The Nonglycemic Actions of Dipeptidyl Peptidase-4 Inhibitors
Na-Hyung Kim, Taeyang Yu, Dae Ho Lee
BioMed Research International.2014; 2014: 1. CrossRef - A Post Hoc Analysis of HbA1c, Hypoglycemia, and Weight Change Outcomes with Alogliptin vs Glipizide in Older Patients with Type 2 Diabetes
Morgan Bron, Craig Wilson, Penny Fleck
Diabetes Therapy.2014; 5(2): 521. CrossRef - Response: The Effect of DPP-4 Inhibitors on Metabolic Parameters in Patients with Type 2 Diabetes (Diabetes Metab J2014;38:211-9)
EunYeong Choe, Eun Seok Kang
Diabetes & Metabolism Journal.2014; 38(4): 319. CrossRef - Letter: The Effect of DPP-4 Inhibitors on Metabolic Parameters in Patients with Type 2 Diabetes (Diabetes Metab J2014;38:211-9)
Seung-Hwan Lee
Diabetes & Metabolism Journal.2014; 38(4): 317. CrossRef
- Insulin Tregopil: An Ultra-Fast Oral Recombinant Human Insulin Analog: Preclinical and Clinical Development in Diabetes Mellitus
- Prevalence of Dyslipidemia among Korean Adults: Korea National Health and Nutrition Survey 1998-2005
- Myung Ha Lee, Hyeon Chang Kim, Song Vogue Ahn, Nam Wook Hur, Dong Phil Choi, Chang Gyu Park, Il Suh
- Diabetes Metab J. 2012;36(1):43-55. Published online February 17, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.1.43
- 3,886 View
- 38 Download
- 60 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Dyslipidemia is a disorder of lipid metabolism, including elevated total cholesterol, elevated triglyceride, elevated low density lipoprotein cholesterol (LDL-C), and decreased high density lipoprotein cholesterol (HDL-C). The objective of this study was to investigate recent changes in the prevalence of dyslipidemia and also the rates of awareness, treatment, and control of dyslipidemia among Korean adults.
Methods Dyslipidemia is defined according to the National Cholesterol Education Program-Adult Treatment Panel III as total cholesterol ≥240 mg/dL, LDL-C ≥160 mg/dL, HDL-C <40 mg/dL, and triglyceride ≥200 mg/dL. The prevalence of dyslipidemia was estimated for adults aged ≥20 years using the Korea National Health and Nutrition Survey (KNHANES) in 1998 (
n =6,923), 2001 (n =4,882), and 2005 (n =5,323). Rates of awareness, treatment and control of dyslipidemia were calculated for adults aged ≥30 years using the KNHANES in 2005 (n =4,654).Results The prevalence of dyslipidemia (aged ≥20 years) increased from 32.4% in 1998 to 42.6% in 2001 and 44.1% in 2005. Compared with the KNHANES in 1998, the prevalence of dyslipidemia was 47% (95% confidence interval [CI], 35% to 59%) higher in 2001 and 61% (95% CI, 49% to 75%) higher in 2005. In 2005, only 9.5% of people with dyslipidemia were aware of the disease, 5.2% used lipid-lowering medication, and 33.2% of patients with treatment reached treatment goals.
Conclusion The prevalence of dyslipidemia in Korea gradually increased between 1998 and 2005. These findings suggest that more intense efforts for the prevention and treatment of dyslipidemia may lead to further improvement in the management of dyslipidemia.
-
Citations
Citations to this article as recorded by- Association between weekend catch-up sleep and dyslipidemia among Korean workers
Ye Seul Jang, Yu Shin Park, Kyungduk Hurh, Eun-Cheol Park, Sung-In Jang
Scientific Reports.2023;[Epub] CrossRef - Effects of ambient particulate exposure on blood lipid levels in hypertension inpatients
Yanfang Gao, Chenwei Li, Lei Huang, Kun Huang, Miao Guo, Xingye Zhou, Xiaokang Zhang
Frontiers in Public Health.2023;[Epub] CrossRef - Association between ambient air pollutants and lipid profile: A systematic review and meta-analysis
Chun Wang, Xing-chen Meng, Chao Huang, Jia Wang, Ying-hao Liao, Yang Huang, Ran Liu
Ecotoxicology and Environmental Safety.2023; 262: 115140. CrossRef - Lipoproteins, Cholesterol, and Atherosclerotic Cardiovascular Disease in East Asians and Europeans
Takahito Doi, Anne Langsted, Børge G. Nordestgaard
Journal of Atherosclerosis and Thrombosis.2023; 30(11): 1525. CrossRef - Associations between the Genetic Heritability of Dyslipidemia and Dietary Patterns in Korean Adults Based on Sex Differences
Sei Kim, Hye Kyung Jeon, Gyeonghee Lee, Youbin Kim, Hae Young Yoo
Nutrients.2023; 15(20): 4385. CrossRef - Periodontitis is a factor associated with dyslipidemia
Isaac Suzart Gomes‐Filho, Michelle Teixeira Oliveira, Simone Seixas da Cruz, Eneida de Moraes Marcílio Cerqueira, Soraya Castro Trindade, Graciete Oliveira Vieira, Paulo Henrique Couto Souza, Luis Fernando Fernandes Adan, Alexandre Marcelo Hintz, Johelle
Oral Diseases.2022; 28(3): 813. CrossRef - Association of PM2.5 With blood lipids and dyslipidaemia in a rural population of north-western china
Kairong Wang, Yi Zhao, Qingan Wang, Yajuan Zhang, Yuhong Zhang
Frontiers in Environmental Science.2022;[Epub] CrossRef - The association between ambient air pollution and blood lipids: A longitudinal study in Shijiazhuang, China
Kaihua Zhang, Haoyuan Wang, Weiliang He, Gongbo Chen, Peng Lu, Rongbin Xu, Pei Yu, Tingting Ye, Suying Guo, Shanshan Li, Yinyu Xie, Zhihua Hao, Hebo Wang, Yuming Guo
Science of The Total Environment.2021; 752: 141648. CrossRef - The association between periodontitis and dyslipidemia according to smoking and harmful alcohol use in a representative sample of Korean adults
Su-Jin Han, Yeo Jin Yi, Kwang-Hak Bae
Clinical Oral Investigations.2020; 24(2): 937. CrossRef - Factors Associated with Awareness, Treatment, and Control Rate of Hypertension among Korean Young Adults Aged 30–49 Years
Yong Woo Jeon, Hyeon Chang Kim
Korean Circulation Journal.2020; 50(12): 1077. CrossRef - Efficacy and Safety of Omega-3 Fatty Acids in Patients Treated with Statins for Residual Hypertriglyceridemia: A Randomized, Double-Blind, Placebo-Controlled Clinical Trial
Ji Eun Jun, In-Kyung Jeong, Jae Myung Yu, Sung Rae Kim, In Kye Lee, Kyung-Ah Han, Sung Hee Choi, Soo-Kyung Kim, Hyeong Kyu Park, Ji-Oh Mok, Yong-ho Lee, Hyuk-Sang Kwon, So Hun Kim, Ho-Cheol Kang, Sang Ah Lee, Chang Beom Lee, Kyung Mook Choi, Sung-Ho Her,
Diabetes & Metabolism Journal.2020; 44(1): 78. CrossRef - Prevalencia de hipertrigliceridemia en adultos y factores cardiometabólicos asociados. Estudio SIMETAP-HTG
Antonio Ruiz-García, Ezequiel Arranz-Martínez, Beatriz López-Uriarte, Montserrat Rivera-Teijido, David Palacios-Martínez, Gema M. Dávila-Blázquez, Antonio Rosillo-González, José Antonio González-Posada Delgado, José Enrique Mariño-Suárez, Enrique Revilla-
Clínica e Investigación en Arteriosclerosis.2020; 32(6): 242. CrossRef - Long-term effects of ambient air pollutants to blood lipids and dyslipidemias in a Chinese rural population
Shuyuan Mao, Gongbo Chen, Feifei Liu, Na Li, Chongjian Wang, Yisi Liu, Suyang Liu, Yuanan Lu, Hao Xiang, Yuming Guo, Shanshan Li
Environmental Pollution.2020; 256: 113403. CrossRef - Prevalence of hypertriglyceridemia in adults and related cardiometabolic factors. SIMETAP-HTG study
Antonio Ruiz-García, Ezequiel Arranz-Martínez, Beatriz López-Uriarte, Montserrat Rivera-Teijido, David Palacios-Martínez, Gema M. Dávila-Blázquez, Antonio Rosillo-González, José Antonio González-Posada Delgado, José Enrique Mariño-Suárez, Enrique Revilla-
Clínica e Investigación en Arteriosclerosis (English Edition).2020; 32(6): 242. CrossRef - Long-term effects of various types of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors on changes in glomerular filtration rate in Korea
Seo Yeon Baik, Hyunah Kim, So Jung Yang, Tong Min Kim, Seung-Hwan Lee, Jae Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, Kun-Ho Yoon, Hun-Sung Kim
Frontiers of Medicine.2019; 13(6): 713. CrossRef - The association between low frequency of having breakfast and dyslipidemia in South Korean men and women
Doo Woong Lee, Dong-Woo Choi, Yeong Jun Ju, Sang Ah Lee, Eun-Cheol Park
European Journal of Clinical Nutrition.2019; 73(6): 896. CrossRef - Association between Brachial-Ankle Pulse Wave Velocity and Microalbuminuria and to Predict the Risk for the Development of Microalbuminuria Using Brachial-Ankle Pulse Wave Velocity Measurement in Type 2 Diabetes Mellitus Patients
Byong-Kyu Kim, Dilaram Acharya, Deuk-Young Nah, Moo-Yong Rhee, Seok-Ju Yoo, Kwan Lee
Healthcare.2019; 7(4): 111. CrossRef - A genome-wide search for gene-by-obesity interaction loci of dyslipidemia in Koreans shows diverse genetic risk alleles
Moonil Kang, Joohon Sung
Journal of Lipid Research.2019; 60(12): 2090. CrossRef - Oily Fish Consumption and the Risk of Dyslipidemia in Korean Adults: A Prospective Cohort Study Based on the Health Examinees Gem (HEXA-G) Study
Seong-Ah Kim, Jong-koo Lee, Daehee Kang, Sangah Shin
Nutrients.2019; 11(10): 2506. CrossRef - Dyslipidemia: Genetics, lipoprotein lipase and HindIII polymorphism
Marcos Palacio Rojas, Carem Prieto, Valmore Bermúdez, Carlos Garicano, Trina Núñez Nava, María Sofía Martínez, Juan Salazar, Edward Rojas, Arturo Pérez, Paulo Marca Vicuña, Natalia González Martínez, Santiago Maldonado Parra, Kyle Hoedebecke, Rosanna D’Ad
F1000Research.2018; 6: 2073. CrossRef - Prevalence of dyslipidemia and achievement of low-density lipoprotein cholesterol targets in Chinese adults: A nationally representative survey of 163,641 adults
Mei Zhang, Qian Deng, Linhong Wang, Zhengjing Huang, Maigeng Zhou, Yichong Li, Zhenping Zhao, Yawei Zhang, Limin Wang
International Journal of Cardiology.2018; 260: 196. CrossRef - Change in ALT levels after administration of HMG‐CoA reductase inhibitors to subjects with pretreatment levels three times the upper normal limit in clinical practice
Hyunah Kim, Hyeseon Lee, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung‐Hwan Lee, Jae‐Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun‐Ho Yoon, Hun‐Sung Kim
Cardiovascular Therapeutics.2018;[Epub] CrossRef - Evaluating the prevalence, awareness, and control of hypertension, diabetes, and dyslipidemia in Korea using the NHIS-NSC database
Sunjoo Boo, Young Joo Yoon, Hyunjin Oh
Medicine.2018; 97(51): e13713. CrossRef - Prevalence of Metabolic Syndrome and Associations with Lipid Profiles in Iranian Men: A Population-Based Screening Program
Abolfazl Mohammadbeigi, Hamid Farahani, Esmail Moshiri, Mahbobeh Sajadi, Robabeh Ahmadli, Sima Afrashteh, Salman Khazaei, Hossein Ansari
The World Journal of Men's Health.2018; 36(1): 50. CrossRef - Association of change in waist circumference and dyslipidaemia risk: The rural Chinese cohort study
Junmei Zhou, Yongcheng Ren, Chongjian Wang, Linlin Li, Lu Zhang, Bingyuan Wang, Yang Zhao, Chengyi Han, Hongyan Zhang, Xiangyu Yang, Xinping Luo, Chao Pang, Lei Yin, Tianping Feng, Jingzhi Zhao, Dongsheng Hu, Ming Zhang
Diabetes/Metabolism Research and Reviews.2018;[Epub] CrossRef - Association between triglyceride/high-density lipoprotein ratio and hearing impairment in a Korean population
Da Jung Jung, Jun Young Do, Kyu Hyang Cho, A. Young Kim, Seok Hui Kang
Postgraduate Medicine.2017; 129(8): 943. CrossRef - Association of Body Mass Index with Dyslipidemia among the Government Staff of Kermanshah, Iran: A Cross-Sectional Study
Ebrahim Shakiba, Nahid Khademi, Malihe Khoramdad, Yousef Alimohamadi, Neda Izadi
Iranian Red Crescent Medical Journal.2017;[Epub] CrossRef - The differences in the incidence of diabetes mellitus and prediabetes according to the type of HMG-CoA reductase inhibitors prescribed in Korean patients
Tong Min Kim, Hyunah Kim, Yoo Jin Jeong, Sun Jung Baik, So Jung Yang, Seung-Hwan Lee, Jae-Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, In Young Choi, Kun-Ho Yoon, Hun-Sung Kim
Pharmacoepidemiology and Drug Safety.2017; 26(10): 1156. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - Changes over time in the prevalence and treatment of cardiovascular risk factors, and contributions to time trends in coronary mortality over 25 years in the Lille urban area (northern France)
Guillaume Clement, Jonathan Giovannelli, Dominique Cottel, Michele Montaye, Alina Ciuchete, Jean Dallongeville, Philippe Amouyel, Luc Dauchet
Archives of Cardiovascular Diseases.2017; 110(12): 689. CrossRef - Early Postpartum Lipid Profile in Women with and Without Gestational Diabetes Mellitus: Results of a Prospective Cohort Study
Sedigheh Nouhjah, Hajieh Shahbazian, Shayesteh Jahanfar, Nahid Shahbazian, Alireza Jahanshahi, Bahman Cheraghian, Leila Hardanipasand, Mitra Moradi
Iranian Red Crescent Medical Journal.2017;[Epub] CrossRef - Dyslipidemia: Genetics, lipoprotein lipase and HindIII polymorphism
Marcos Palacio Rojas, Carem Prieto, Valmore Bermúdez, Carlos Garicano, Trina Núñez Nava, María Sofía Martínez, Juan Salazar, Edward Rojas, Arturo Pérez, Paulo Marca Vicuña, Natalia González Martínez, Santiago Maldonado Parra, Kyle Hoedebecke, Rosanna D’Ad
F1000Research.2017; 6: 2073. CrossRef - Self‐perceived health versus actual cardiovascular disease risks
Young Ko, Sunjoo Boo
Japan Journal of Nursing Science.2016; 13(1): 65. CrossRef - Hypertriglyceridemia and Cardiovascular Diseases: Revisited
Seung Hwan Han, Stephen J Nicholls, Ichiro Sakuma, Dong Zhao, Kwang Kon Koh
Korean Circulation Journal.2016; 46(2): 135. CrossRef - One-Year Experience Managing a Cancer Survivorship Clinic Using a Shared-Care Model for Gastric Cancer Survivors in Korea
Ji Eun Lee, Dong Wook Shin, Hyejin Lee, Ki Young Son, Warrick Junsuk Kim, Yun-Suhk Suh, Seong-Ho Kong, Hyuk Joon Lee, Belong Cho, Han-Kwang Yang
Journal of Korean Medical Science.2016; 31(6): 859. CrossRef - Relationship Between Dyslipidemia and Albuminuria in Hypertensive Adults
Sung-Ho Lee, Do Hoon Kim, Yang-Hyun Kim, Yong Kyun Roh, Sang Yhun Ju, Hyo-Yun Nam, Ga-Eun Nam, Jun-Seok Choi, Jong-Eun Lee, Jung-Eun Sang, Kyungdo Han, Yong-Gyu Park
Medicine.2016; 95(16): e3224. CrossRef - Epidemiology of dyslipidemia in Korea
Hyeon Chang Kim
Journal of the Korean Medical Association.2016; 59(5): 352. CrossRef - Effects of Age, Sex, and Menopausal Status on Blood Cholesterol Profile in the Korean Population
Ji Hye Park, Myung Ha Lee, Jee-Seon Shim, Dong Phil Choi, Bo Mi Song, Seung Won Lee, Hansol Choi, Hyeon Chang Kim
Korean Circulation Journal.2015; 45(2): 141. CrossRef - Related factors of medication adherence in patients with dyslipidemia: The 2010-2012 Korean National Health and Nutrition Examination Survey
Eun Jung Cho, Kyoung Ja Moon
Korean Journal of Health Education and Promotion.2015; 32(2): 65. CrossRef - Dyslipidemia Prevalence in Iranian Adult Men: The Impact of Population-Based Screening on the Detection of Undiagnosed Patients
Abolfazl Mohammadbeigi, Esamil Moshiri, Narges Mohammadsalehi, Hossein Ansari, Ali Ahmadi
The World Journal of Men's Health.2015; 33(3): 167. CrossRef - Nicotinic acid and derivatives as multifunctional pharmacophores for medical applications
Nujarin Sinthupoom, Veda Prachayasittikul, Supaluk Prachayasittikul, Somsak Ruchirawat, Virapong Prachayasittikul
European Food Research and Technology.2015; 240(1): 1. CrossRef - Relationship between dyslipidemia and albuminuria in prediabetic adults: The Korea National Health and Nutrition Examination Survey 2011–2012
Ga Eun Nam, Kyungdo Han, Do Hoon Kim, Yong Gyu Park, Yeo Joon Yoon, Young Eun Kim, Sangsu Lee, Sungho Lee, Yong Kyun Roh
Endocrine.2015; 48(2): 557. CrossRef - Trends in lipid profiles among South Korean adults: 2005, 2008 and 2010 Korea National Health and Nutrition Examination Survey
Ga Eun Nam, Kyungdo Han, Yong Gyu Park, Youn Seon Choi, Seon Mee Kim, Sang-Yhun Ju, Byung-Joon Ko, Yang Hyun Kim, Eun Hye Kim, Kyung Hwan Cho, Do Hoon Kim
Journal of Public Health.2015; 37(2): 286. CrossRef - Subclinical Hypothyroidism Might Worsen the Effects of Aging on Serum Lipid Profiles: A Population-Based Case-Control Study
Meng Zhao, Tao Yang, Li Chen, Xulei Tang, Qingbo Guan, Bingchang Zhang, Xu Zhang, Haiqing Zhang, Chenggang Wang, Jin Xu, Xinguo Hou, Qiu Li, Chunxiao Yu, Yuanfei Zhao, Li Fang, Zhongshang Yuan, Fuzhong Xue, Guang Ning, Ling Gao, Chao Xu, Jiajun Zhao
Thyroid.2015; 25(5): 485. CrossRef - Serum lipid profiles and glycemic control in adolescents and young adults with type 1 diabetes mellitus
Shin-Hee Kim, In-Ah Jung, Yeon Jin Jeon, Won Kyoung Cho, Kyoung Soon Cho, So Hyun Park, Min Ho Jung, Byoung Kyu Suh
Annals of Pediatric Endocrinology & Metabolism.2014; 19(4): 191. CrossRef - Dyslipidemia in Children and Adolescents: When and How to Diagnose and Treat?
Jung Min Yoon
Pediatric Gastroenterology, Hepatology & Nutrition.2014; 17(2): 85. CrossRef - Sarcopenia and sarcopenic obesity and their association with dyslipidemia in Korean elderly men: the 2008–2010 Korea National Health and Nutrition Examination Survey
S. J. Baek, G. E. Nam, K. D. Han, S. W. Choi, S. W. Jung, A. R. Bok, Y. H. Kim, K. S. Lee, B. D. Han, D. H. Kim
Journal of Endocrinological Investigation.2014; 37(3): 247. CrossRef - Association between Blood Lipid Levels and Personality Traits in Young Korean Women
Seung-Ju Roh, Han-Na Kim, Unjin Shim, Bo-Hye Kim, Su-Jin Kim, Hye Won Chung, Hyejin Lee, Yeon-Ah Sung, Hyung-Lae Kim, Christina Bursill
PLoS ONE.2014; 9(9): e108406. CrossRef - Serum Cholesterol Concentration and Prevalence, Awareness, Treatment, and Control of High Low‐Density Lipoprotein Cholesterol in the Korea National Health and Nutrition Examination Surveys 2008–2010: Beyond the Tip of the Iceberg
Yong‐ho Lee, Sang‐Guk Lee, Myung Ha Lee, Jeong‐Ho Kim, Byung‐Wan Lee, Eun Seok Kang, Hyun Chul Lee, Bong Soo Cha
Journal of the American Heart Association.2014;[Epub] CrossRef - Prevalence of plasma lipid abnormalities and its association with glucose metabolism in Spain: The di@bet.es study
Sergio Martinez-Hervas, Rafael Carmena, Juan F. Ascaso, Jose T. Real, Luis Masana, Miguel Catalá, Joan Vendrell, José Antonio Vázquez, Sergio Valdés, Inés Urrutia, Federico Soriguer, Manuel Serrano-Rios, Gemma Rojo-Martínez, Gemma Pascual-Manich, Emilio O
Clínica e Investigación en Arteriosclerosis.2014; 26(3): 107. CrossRef - The current state of dyslipidemia in Korean children and adolescents and its management in clinical practice
Jung Sub Lim
Annals of Pediatric Endocrinology & Metabolism.2013; 18(1): 1. CrossRef - Prevalence and Management of Dyslipidemia in Korea: Korea National Health and Nutrition Examination Survey during 1998 to 2010
Eun Roh, Seung-Hyun Ko, Hyuk-Sang Kwon, Nan Hee Kim, Jae Hyeon Kim, Chul Sik Kim, Kee-Ho Song, Jong Chul Won, Dae Jung Kim, Sung Hee Choi, Soo Lim, Bong-Yun Cha
Diabetes & Metabolism Journal.2013; 37(6): 433. CrossRef - Socioeconomic status and dyslipidemia in Korean adults: The 2008–2010 Korea National Health and Nutrition Examination Survey
Ga Eun Nam, Kyung Hwan Cho, Yong Gyu Park, Kyung Do Han, Youn Seon Choi, Seon Mee Kim, Kyung Shik Lee, Byung Joon Ko, Yang Hyun Kim, Byoung Duck Han, Do Hoon Kim
Preventive Medicine.2013; 57(4): 304. CrossRef - The association between periodontitis and dyslipidemia based on the fourth Korea National Health and Nutrition Examination Survey
Jun‐Beom Lee, Hee‐Yong Yi, Kwang‐Hak Bae
Journal of Clinical Periodontology.2013; 40(5): 437. CrossRef - Trends in Cardiovascular Health Metrics among Korean Adults
Hae-Joon Lee, Beomseok Suh, Tae-Gon Yoo, Haewon Lee, Dong Wook Shin
Korean Journal of Family Medicine.2013; 34(6): 403. CrossRef - Increasing achievement of the target goals for glycemic, blood pressure and lipid control for adults with diagnosed diabetes in Korea
Sung Hoon Yu, Jun Goo Kang, Yoo‐Cheol Hwang, Kyu Jeung Ahn, Hyung Joon Yoo, Hong Yup Ahn, Sung Woo Park, Cheol‐Young Park
Journal of Diabetes Investigation.2013; 4(5): 460. CrossRef - Low bone mineral density is associated with dyslipidemia in South Korean men: The 2008–2010 Korean National Health and Nutrition Examination Survey
Yang-Hyun Kim, Ga-Eun Nam, Kyung-Hwan Cho, Youn Seon Choi, Seon-Mee Kim, Byung-Duck Han, Kyung Do Han, Kyung-Shik Lee, Chang-Hae Park, Do-Hoon Kim
Endocrine Journal.2013; 60(10): 1179. CrossRef - Response: Prevalence of Dyslipidemia among Korean Adults: Korea National Health and Nutrition Survey 1998-2005 (Diabetes Metab J 2012;36:43-55)
Hyeon Chang Kim
Diabetes & Metabolism Journal.2012; 36(2): 165. CrossRef - Beyond the Shadow: Getting Past the Veil of Nonadherence in the Management of Atherosclerotic Risk Factors
Ross D. Feldman, Tavis S. Campbell
Canadian Journal of Cardiology.2012; 28(5): 531. CrossRef - Letter: Prevalence of Dyslipidemia among Korean Adults: Korea National Health and Nutrition Survey 1998-2005 (Diabetes Metab J 2012;36:43-55)
Bo Kyung Koo
Diabetes & Metabolism Journal.2012; 36(2): 163. CrossRef
- Association between weekend catch-up sleep and dyslipidemia among Korean workers
- Glycosphingolipid Modification: Structural Diversity, Functional and Mechanistic Integration of Diabetes
- Tadashi Yamashita
- Diabetes Metab J. 2011;35(4):309-316. Published online August 31, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.4.309
- 2,927 View
- 34 Download
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Glycosphingolipids (GSLs) are present in all mammalian cell plasma membranes and intracellular membrane structures. They are especially concentrated in plasma membrane lipid domains that are specialized for cell signaling. Plasma membranes have typical structures called rafts and caveola domain structures, with large amounts of sphingolipids, cholesterol, and sphingomyelin. GSLs are usually observed in many organs ubiquitously. However, GSLs, including over 400 derivatives, participate in diverse cellular functions. Several studies indicate that GSLs might have an effect on signal transduction related to insulin receptors and epidermal growth factor receptors. GSLs may modulate immune responses by transmitting signals from the exterior to the interior of the cell. Guillain-Barré syndrome is one of the autoimmune disorders characterized by symmetrical weakness in the muscles of the legs. The targets of the immune response are thought to be gangliosides, which are one group of GSLs. Other GSLs may serve as second messengers in several signaling pathways that are important to cell survival or programmed cell death. In the search for clear evidence that GSLs may play critical roles in various biological functions, many researchers have made genetically engineered mice. Before the era of gene manipulation, spontaneous animal models or chemical-induced disease models were used.
-
Citations
Citations to this article as recorded by- Quantitative proteomics reveals Piccolo as a candidate serological correlate of recovery from Guillain-Barré syndrome
Lourdes Mateos-Hernández, Margarita Villar, Ernesto Doncel-Pérez, Marco Trevisan-Herraz, Ángel García-Forcada, Francisco Romero Ganuza, Jesús Vázquez, José de la Fuente
Oncotarget.2016; 7(46): 74582. CrossRef - Convergence and divergence of genetic and modular networks between diabetes and breast cancer
Xiaoxu Zhang, Yingying Zhang, Yanan Yu, Jun Liu, Ye Yuan, Yijun Zhao, Haixia Li, Jie Wang, Zhong Wang
Journal of Cellular and Molecular Medicine.2015; 19(5): 1094. CrossRef - Profiling over 1500 Lipids in Induced Lung Sputum and the Implications in Studying Lung Diseases
Ruben t’Kindt, Eef D. Telenga, Lucie Jorge, Antoon J. M. Van Oosterhout, Pat Sandra, Nick H. T. Ten Hacken, Koen Sandra
Analytical Chemistry.2015; 87(9): 4957. CrossRef - Untargeted Lipidomic Analysis in Chronic Obstructive Pulmonary Disease. Uncovering Sphingolipids
Eef D. Telenga, Roland F. Hoffmann, Ruben t’Kindt, Susan J. M. Hoonhorst, Brigitte W. M. Willemse, Antoon J. M. van Oosterhout, Irene H. Heijink, Maarten van den Berge, Lucie Jorge, Pat Sandra, Dirkje S. Postma, Koen Sandra, Nick H. T. ten Hacken
American Journal of Respiratory and Critical Care Medicine.2014; 190(2): 155. CrossRef - Immunological cell type characterization and Th1–Th17 cytokine production in a mouse model of Gaucher disease
Manoj Kumar Pandey, Reena Rani, Wujuan Zhang, Kenneth Setchell, Gregory A. Grabowski
Molecular Genetics and Metabolism.2012; 106(3): 310. CrossRef
- Quantitative proteomics reveals Piccolo as a candidate serological correlate of recovery from Guillain-Barré syndrome
- The Relationship Between Coronary Artery Calcification and Serum Apolipoprotein A-1 in Patients with Type 2 Diabetes.
- Hyun Ae Seo, Yeon Kyung Choi, Jae Han Jeon, Jung Eun Lee, Ji Yun Jeong, Seong Su Moon, In Kyu Lee, Bo Wan Kim, Jung Guk Kim
- Korean Diabetes J. 2009;33(6):485-493. Published online December 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.6.485
- 2,432 View
- 20 Download
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The incidence of type 2 diabetes mellitus is increasing annually and patient mortality is high. Coronary artery calcification is a predictor of coronary artery disease. Cardiovascular events, which are the main cause of death in type 2 diabetes patients, may be preventable by addressing risk factors associated with coronary artery calcification. We examined the relationships between coronary artery calcification, lipid profiles, and apolipoprotein levels. METHODS: We calculated the coronary calcium scores (CCS) of 254 subjects with type 2 diabetes (113 males, 141 females) via multi-detector row computed tomography (MDCT). Height, body weight, blood pressure, HbA1c, c-peptide, lipid profile and apolipoprotein were assessed concurrently. RESULTS: In patients with type 2 diabetes, Agatston score and apolipoprotein A-1 were significantly negatively correlated in both males and females (males P = 0.015, females P = 0.021). The negative correlation between Agatston score and apolipoprotein A-1 was retained for the entire patient sample after adjustments for age and sex (P = 0.022). Stepwise multiple regression anaylses with the Agatston score as the dependent variable indicate that apolipoprotein A-1 is a independent predictor (beta coefficient = -0.047, 95%CI = -0.072 ~ -0.021, P < 0.001) of coronary artery calcification. CONCLUSION: The results of our study suggest that apolipoprotein A-1 is a useful independent indicator of coronary artery calcification. -
Citations
Citations to this article as recorded by- The Risk of Coronary Artery Calcification according to Different Lipid Parameters and Average Lipid Parameters
Tae Kyung Yoo, Mi Yeon Lee, Ki-Chul Sung
Journal of Atherosclerosis and Thrombosis.2024;[Epub] CrossRef - Coronary Artery Calcification and Serum Apolipoprotein A-1 in Patients with Type 2 Diabetes
Ki Won Oh
Korean Diabetes Journal.2009; 33(6): 464. CrossRef
- The Risk of Coronary Artery Calcification according to Different Lipid Parameters and Average Lipid Parameters

 KDA
KDA
 First
First Prev
Prev





