
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
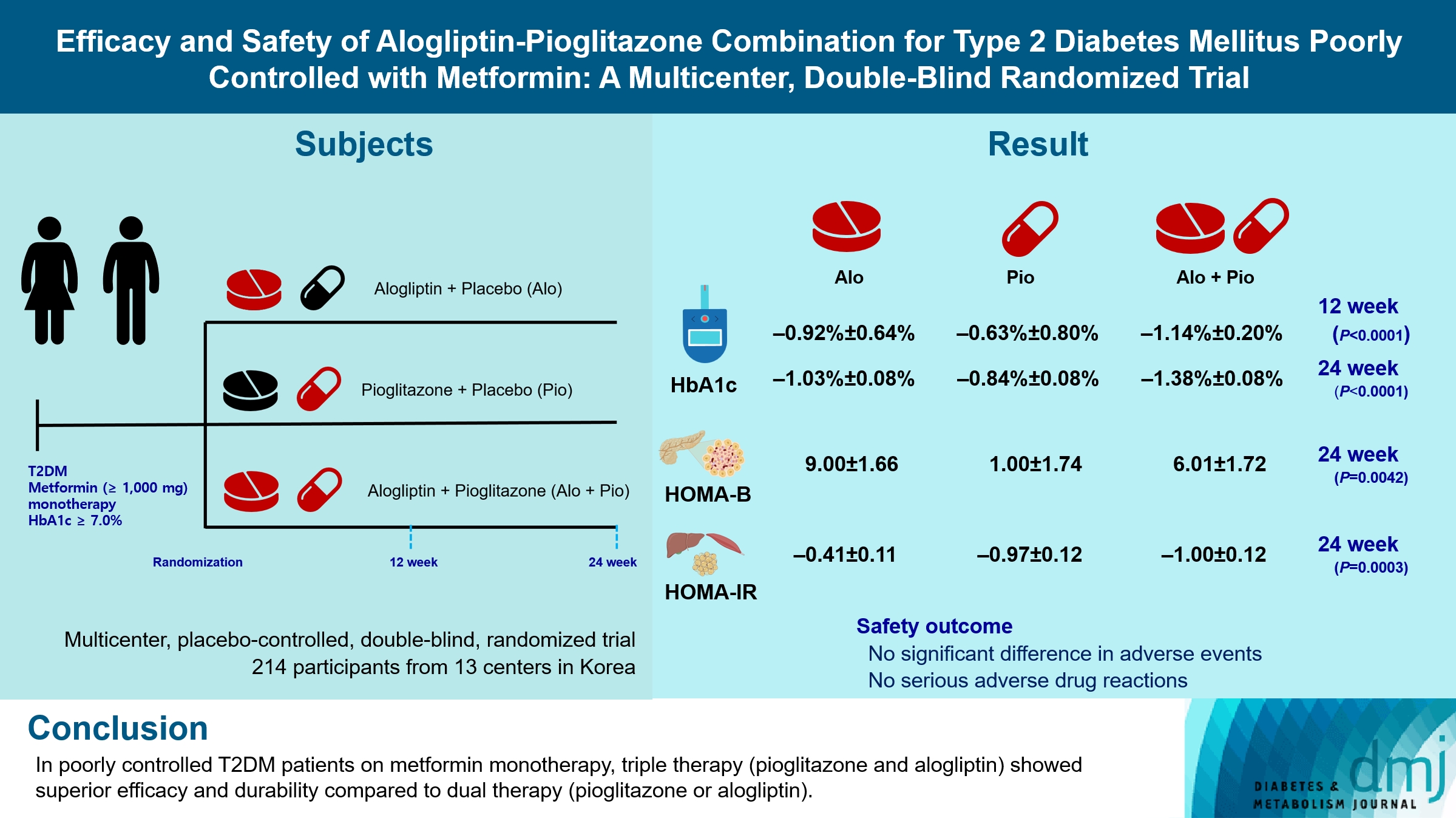
- Efficacy and Safety of Alogliptin-Pioglitazone Combination for Type 2 Diabetes Mellitus Poorly Controlled with Metformin: A Multicenter, Double-Blind Randomized Trial
- Ji-Yeon Park, Joonyub Lee, Yoon-Hee Choi, Kyung Wan Min, Kyung Ah Han, Kyu Jeung Ahn, Soo Lim, Young-Hyun Kim, Chul Woo Ahn, Kyung Mook Choi, Kun-Ho Yoon, the Practical Evidence of Antidiabetic Combination Therapy in Korea (PEAK) study investigators
- Received August 7, 2023 Accepted November 30, 2023 Published online April 23, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0259 [Epub ahead of print]
- 306 View
- 18 Download
-
 Abstract
Abstract
 PDF
PDF - Background
Guidelines for switching to triple combination therapy directly after monotherapy failure are limited. This study investigated the efficacy, long-term sustainability, and safety of either mono or dual add-on therapy using alogliptin and pioglitazone for patients with type 2 diabetes mellitus (T2DM) who did not achieve their target glycemic range with metformin monotherapy.
Methods
The Practical Evidence of Antidiabetic Combination Therapy in Korea (PEAK) was a multicenter, placebo-controlled, double-blind, randomized trial. A total of 214 participants were randomized to receive alogliptin+pioglitazone (Alo+Pio group, n=70), alogliptin (Alo group, n=75), or pioglitazone (Pio group, n=69). The primary outcome was the difference in glycosylated hemoglobin (HbA1c) levels between the three groups at baseline to 24 weeks. For durability, the achievement of HbA1c levels <7% and <6.5% was compared in each group. The number of adverse events was investigated for safety.
Results
After 24 weeks of treatment, the change of HbA1c in the Alo+Pio, Alo, and Pio groups were –1.38%±0.08%, –1.03%±0.08%, and –0.84%±0.08%, respectively. The Alo+Pio group had significantly lower HbA1c levels than the other groups (P=0.0063, P<0.0001) and had a higher proportion of patients with target HbA1c achievement. In addition, insulin sensitivity and β-cell function, lipid profiles, and other metabolic indicators were also improved. There were no significant safety issues in patients treated with triple combination therapy.
Conclusion
Early combination triple therapy showed better efficacy and durability than the single add-on (dual) therapy. Therefore, combination therapy with metformin, alogliptin, and pioglitazone is a valuable early treatment option for T2DM poorly controlled with metformin monotherapy.
- Others
- Comparative Effect of Glucose-Lowering Drugs for Type 2 Diabetes Mellitus on Stroke Prevention: A Systematic Review and Network Meta-Analysis
- Ji Soo Kim, Gyeongsil Lee, Kyung-Il Park, Seung-Won Oh
- Diabetes Metab J. 2024;48(2):312-320. Published online January 26, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0421

- 1,285 View
- 214 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There is still a lack of research on which diabetic drugs are more effective in preventing stroke. Our network metaanalysis aimed to compare cerebrovascular benefits among glucose-lowering treatments.
Methods
We searched MEDLINE, EMBASE, the Cochrane Central Register of Controlled Trials, and the ClinicalTrials.gov registry for clinical trials from inception through May 25, 2021. We included both prespecified cerebrovascular outcomes and cerebrovascular events reported as severe adverse events. Subgroup analyses were conducted by stroke subtype, publication type, age of patients, baseline glycosylated hemoglobin (HbA1c), duration of type 2 diabetes mellitus, and cardiovascular risks.
Results
Of 2,861 reports and 1,779 trials screened, 79 randomized controlled trials comprising 206,387 patients fulfilled the inclusion criteria. In the pairwise meta-analysis, the use of glucagon-like peptide-1 (GLP-1) agonist was associated with a lower risk of total stroke compared with placebo (relative risk [RR], –0.17; 95% confidence interval [CI], –0.27 to –0.07). In the network meta- analysis, only the use of sodium-glucose cotransporter-2 (SGLT-2) inhibitor was associated with a reduction of total stroke, compared with placebo (RR, 0.81; 95% CI, 0.67 to 0.98). In the subgroup analyses, the use of SGLT-2 inhibitor and GLP-1 agonist was associated with a lower risk of stroke in those with high HbA1c (≥8.0) and low-risk of cardiovascular disease, respectively.
Conclusion
SGLT-2 inhibitors and GLP-1 agonists were shown to be beneficial for stroke prevention in patients with type 2 diabetes mellitus. -
Citations
Citations to this article as recorded by- SGLT2 Inhibitors and GLP-1 Agonists: A Beacon of Hope for Stroke Prevention in Diabetes
Jae-Han Jeon
Diabetes & Metabolism Journal.2024; 48(2): 213. CrossRef - Reply to comment on: Association of glucose-lowering drugs with incident stroke and transient ischaemic attacks in primary care patients with type 2 diabetes: disease analyser database
Wolfgang Rathmann, Karel Kostev
Acta Diabetologica.2024;[Epub] CrossRef
- SGLT2 Inhibitors and GLP-1 Agonists: A Beacon of Hope for Stroke Prevention in Diabetes
- Drug Regimen
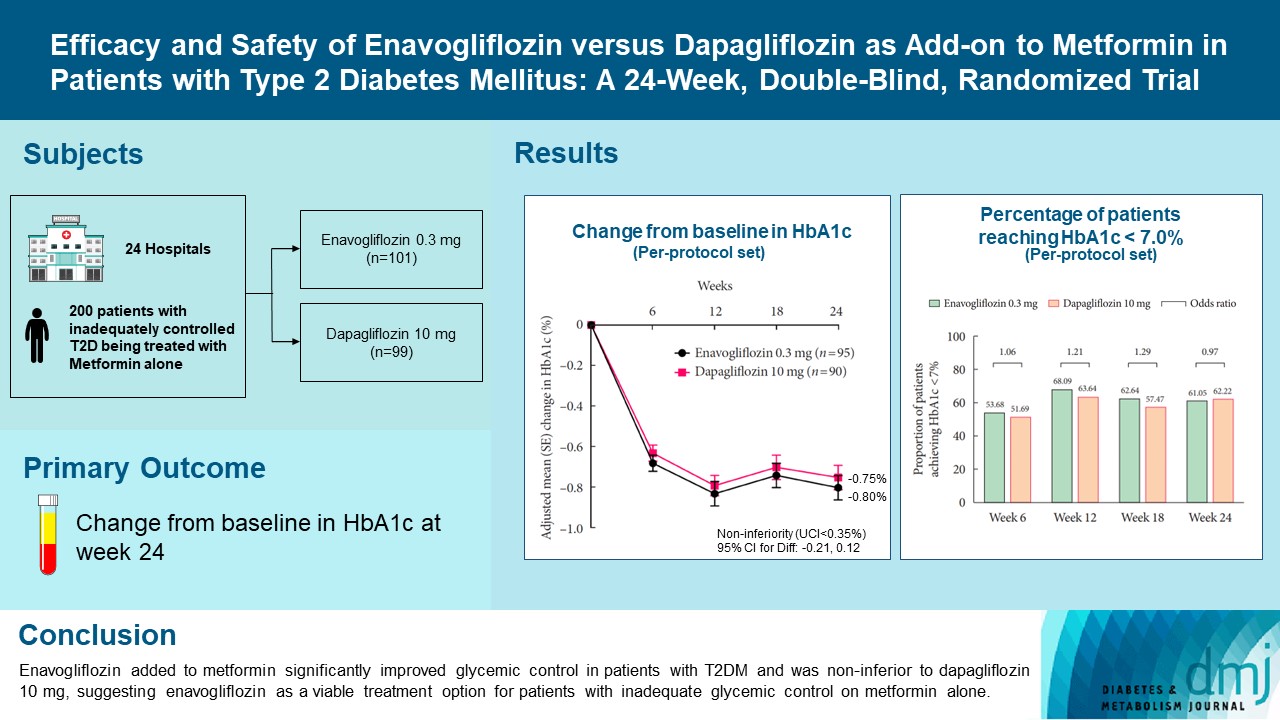
- Efficacy and Safety of Enavogliflozin versus Dapagliflozin as Add-on to Metformin in Patients with Type 2 Diabetes Mellitus: A 24-Week, Double-Blind, Randomized Trial
- Kyung Ah Han, Yong Hyun Kim, Doo Man Kim, Byung Wan Lee, Suk Chon, Tae Seo Sohn, In Kyung Jeong, Eun-Gyoung Hong, Jang Won Son, Jae Jin Nah, Hwa Rang Song, Seong In Cho, Seung-Ah Cho, Kun Ho Yoon
- Diabetes Metab J. 2023;47(6):796-807. Published online February 9, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0315
- 40,109 View
- 576 Download
- 4 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Enavogliflozin is a novel sodium-glucose cotransporter-2 inhibitor currently under clinical development. This study evaluated the efficacy and safety of enavogliflozin as an add-on to metformin in Korean patients with type 2 diabetes mellitus (T2DM) against dapagliflozin.
Methods
In this multicenter, double-blind, randomized, phase 3 study, 200 patients were randomized to receive enavogliflozin 0.3 mg/day (n=101) or dapagliflozin 10 mg/day (n=99) in addition to ongoing metformin therapy for 24 weeks. The primary objective of the study was to prove the non-inferiority of enavogliflozin to dapagliflozin in glycosylated hemoglobin (HbA1c) change at week 24 (non-inferiority margin of 0.35%) (Clinical trial registration number: NCT04634500).
Results
Adjusted mean change of HbA1c at week 24 was –0.80% with enavogliflozin and –0.75% with dapagliflozin (difference, –0.04%; 95% confidence interval, –0.21% to 0.12%). Percentages of patients achieving HbA1c <7.0% were 61% and 62%, respectively. Adjusted mean change of fasting plasma glucose at week 24 was –32.53 and –29.14 mg/dL. An increase in urine glucose-creatinine ratio (60.48 vs. 44.94, P<0.0001) and decrease in homeostasis model assessment of insulin resistance (–1.85 vs. –1.31, P=0.0041) were significantly greater with enavogliflozin than dapagliflozin at week 24. Beneficial effects of enavogliflozin on body weight (–3.77 kg vs. –3.58 kg) and blood pressure (systolic/diastolic, –5.93/–5.41 mm Hg vs. –6.57/–4.26 mm Hg) were comparable with those of dapagliflozin, and both drugs were safe and well-tolerated.
Conclusion
Enavogliflozin added to metformin significantly improved glycemic control in patients with T2DM and was non-inferior to dapagliflozin 10 mg, suggesting enavogliflozin as a viable treatment option for patients with inadequate glycemic control on metformin alone. -
Citations
Citations to this article as recorded by- Efficacy and safety of enavogliflozin vs. dapagliflozin as add-on therapy in patients with type 2 diabetes mellitus based on renal function: a pooled analysis of two randomized controlled trials
Young Sang Lyu, Sangmo Hong, Si Eun Lee, Bo Young Cho, Cheol-Young Park
Cardiovascular Diabetology.2024;[Epub] CrossRef - A 52‐week efficacy and safety study of enavogliflozin versus dapagliflozin as an add‐on to metformin in patients with type 2 diabetes mellitus: ENHANCE‐M extension study
Tae Seo Sohn, Kyung‐Ah Han, Yonghyun Kim, Byung‐Wan Lee, Suk Chon, In‐Kyung Jeong, Eun‐Gyoung Hong, Jang Won Son, JaeJin Na, Jae Min Cho, Seong In Cho, Wan Huh, Kun‐Ho Yoon
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - The effect of renal function on the pharmacokinetics and pharmacodynamics of enavogliflozin, a potent and selective sodium‐glucose cotransporter‐2 inhibitor, in type 2 diabetes
Sae Im Jeong, Mu Seong Ban, Jun‐Gi Hwang, Min‐Kyu Park, Soo Lim, Sejoong Kim, Soon Kil Kwon, Yoonjin Kim, Jae Min Cho, Jae Jin Na, Wan Huh, Jae‐Yong Chung
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Role of novel sodium glucose co-transporter-2 inhibitor enavogliflozin in type-2 diabetes: A systematic review and meta-analysis
Deep Dutta, B.G. Harish, Beatrice Anne, Lakshmi Nagendra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(8): 102816. CrossRef - Characteristics of the Latest Therapeutic Agent for Diabetes
Nuri Yun
The Journal of Korean Diabetes.2023; 24(3): 148. CrossRef - Prospects of using sodium-glucose co-transporter-2 (SGLT-2) inhibitors in patients with metabolic-associated fatty liver disease (MAFLD)
Iryna Kostitska, Nadia Protas, Liliia Petrovska
Diabetes Obesity Metabolic Syndrome.2023; (5): 8. CrossRef - Navigating the Future of Diabetes Treatment with New Drugs: Focusing on the Possibilities and Prospects of Enavogliflozin
Sang Youl Rhee
Diabetes & Metabolism Journal.2023; 47(6): 769. CrossRef
- Efficacy and safety of enavogliflozin vs. dapagliflozin as add-on therapy in patients with type 2 diabetes mellitus based on renal function: a pooled analysis of two randomized controlled trials
- Guideline/Fact Sheet
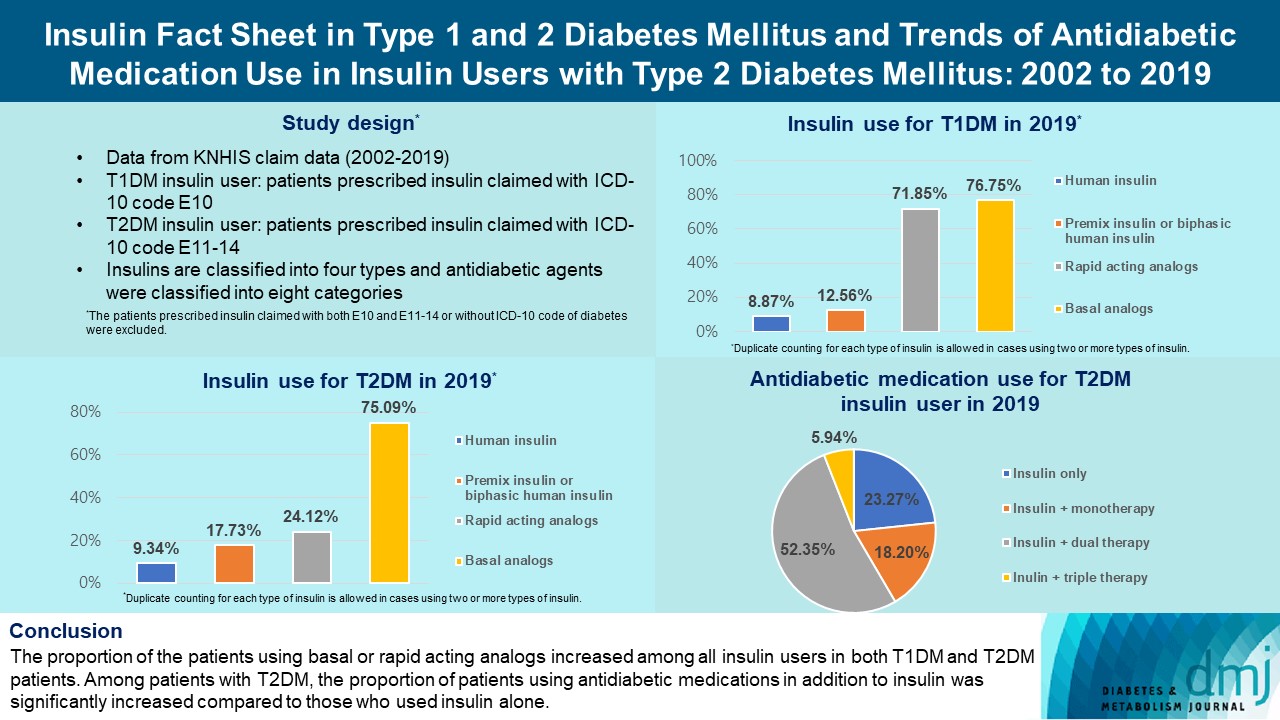
- Insulin Fact Sheet in Type 1 and 2 Diabetes Mellitus and Trends of Antidiabetic Medication Use in Insulin Users with Type 2 Diabetes Mellitus: 2002 to 2019
- Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
- Diabetes Metab J. 2023;47(2):211-219. Published online February 7, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0346
- 3,599 View
- 261 Download
- 1 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study investigated the trends of insulin use among Korean patients with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM). Changes in prescription of antidiabetic medications in T2DM patients taking insulin therapy were evaluated.
Methods
We analyzed data from the National Health Insurance Service database in Korea to evaluate the prevalence of insulin users and trends of insulin use in T1DM and T2DM patients from January 2002 to December 2019. We also investigated numbers and types of antidiabetic medications in insulin users with T2DM.
Results
The overall total number of insulin users increased from 2002 to 2019, reaching 348,254 for T2DM and 20,287 for T1DM in 2019 compared with 109,974 for T2DM and 34,972 for T1DM in 2002. The proportion of patients using basal analogs and short acting analogs have increased and those using human insulin, premixed insulin, or biphasic human insulin have decreased (rapid acting analogs: 71.85% and 24.12% in T1DM and T2DM, respectively, in 2019; basal analogs: 76.75% and 75.09% in T1DM and T2DM, respectively, in 2019). The use of other antidiabetic medication in addition to insulin increased for T2DM, especially in dual therapy, reaching up to 52.35% in 2019 compared with 16.72% in 2002.
Conclusion
The proportion of the patients using basal or rapid acting analogs increased among all insulin users in both T1DM and T2DM patients. Among patients with T2DM, the proportion of patients using antidiabetic medications in addition to insulin was significantly increased compared to those who used insulin alone. -
Citations
Citations to this article as recorded by- Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
Ji Yoon Kim, Sang-Man Jin, Sarah B. Andrade, Boyang Chen, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2024;[Epub] CrossRef - Continuous glucose monitoring for glycaemic control and cardiovascular risk reduction in patients with type 2 diabetes not on insulin therapy: A clinical trial
Joseph Reed, Tony Dong, Elke Eaton, Janice Friswold, Jodie Porges, Sadeer G. Al‐Kindi, Sanjay Rajagopalan, Ian J. Neeland
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Evaluation of pharmacokinetic interactions between lobeglitazone, empagliflozin, and metformin in healthy subjects
Heeyoung Kim, Choon Ok Kim, Hyeonsoo Park, Min Soo Park, Dasohm Kim, Taegon Hong, Yesong Shin, Byung Hak Jin
Translational and Clinical Pharmacology.2023; 31(1): 59. CrossRef - Smart Insulin Pen: Managing Insulin Therapy for People with Diabetes in the Digital Era
Jee Hee Yoo, Jae Hyeon Kim
The Journal of Korean Diabetes.2023; 24(4): 190. CrossRef
- Real-World Continuous Glucose Monitoring Data from a Population with Type 1 Diabetes in South Korea: Nationwide Single-System Analysis
- Drug/Regimen
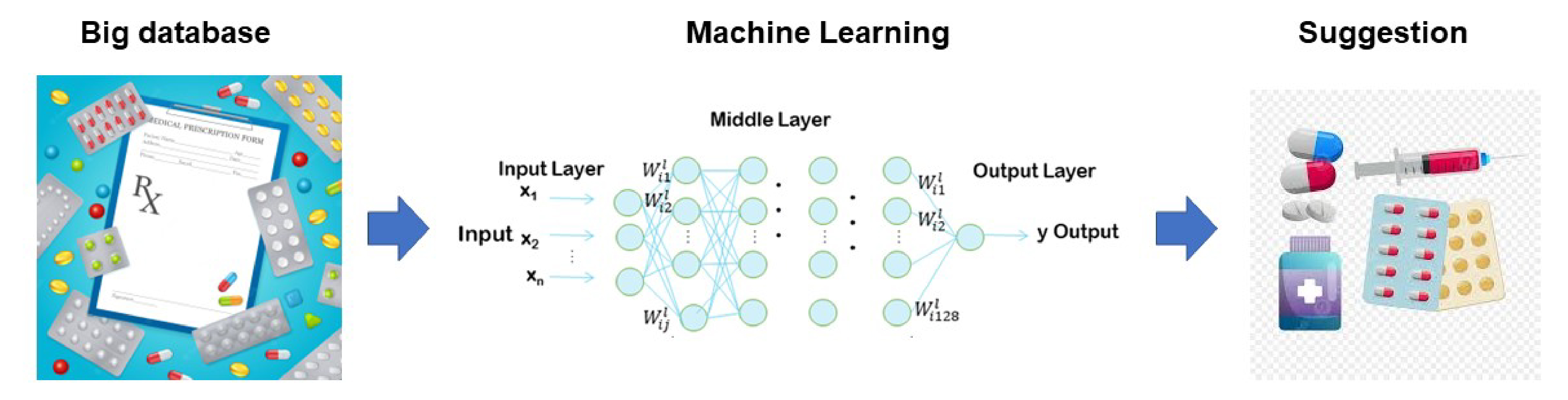
- Machine Learning Approach to Drug Treatment Strategy for Diabetes Care
- Kazuya Fujihara, Hirohito Sone
- Diabetes Metab J. 2023;47(3):325-332. Published online January 12, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0349
- 65,535 View
- 248 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Globally, the number of people with diabetes mellitus has quadrupled in the past three decades, and approximately one in 11 adults worldwide have diabetes mellitus. Since both microvascular and macrovascular diseases in patients with diabetes predispose them to a lower quality of life as well as higher rates of mortality, managing blood glucose levels is of clinical relevance in diabetes care. Many classes of antihyperglycemic drugs are currently approved to treat hyperglycemia in patients with type 2 diabetes mellitus, with several new drugs having been developed during the last decade. Diabetes-related complications have been reduced substantially worldwide. Prioritization of therapeutic agents varies according to national guidelines. However, since the characteristics of participants in clinical trials differ from patients in actual clinical practice, it is difficult to apply the results of such trials to clinical practice. Machine learning approaches became highly topical issues in medicine along with rapid technological innovations in the fields of information and communication in the 1990s. However, adopting these technologies to support decision-making regarding drug treatment strategies for diabetes care has been slow. This review summarizes data from recent studies on the choice of drugs for type 2 diabetes mellitus focusing on machine learning approaches.
-
Citations
Citations to this article as recorded by- Exploring antioxidant activities and inhibitory effects against α‐amylase and α‐glucosidase of Elaeocarpus braceanus fruits: insights into mechanisms by molecular docking and molecular dynamics
Hong Li, Yuanyue Zhang, Zhijia Liu, Chaofan Guo, Maurizio Battino, Shengbao Cai, Junjie Yi
International Journal of Food Science & Technology.2024; 59(1): 343. CrossRef - 3D Convolutional Neural Networks for Predicting Protein Structure for Improved Drug Recommendation
Pokkuluri Kiran Sree, SSSN Usha Devi N
EAI Endorsed Transactions on Pervasive Health and Technology.2024;[Epub] CrossRef
- Exploring antioxidant activities and inhibitory effects against α‐amylase and α‐glucosidase of Elaeocarpus braceanus fruits: insights into mechanisms by molecular docking and molecular dynamics
- Drug/Regimen
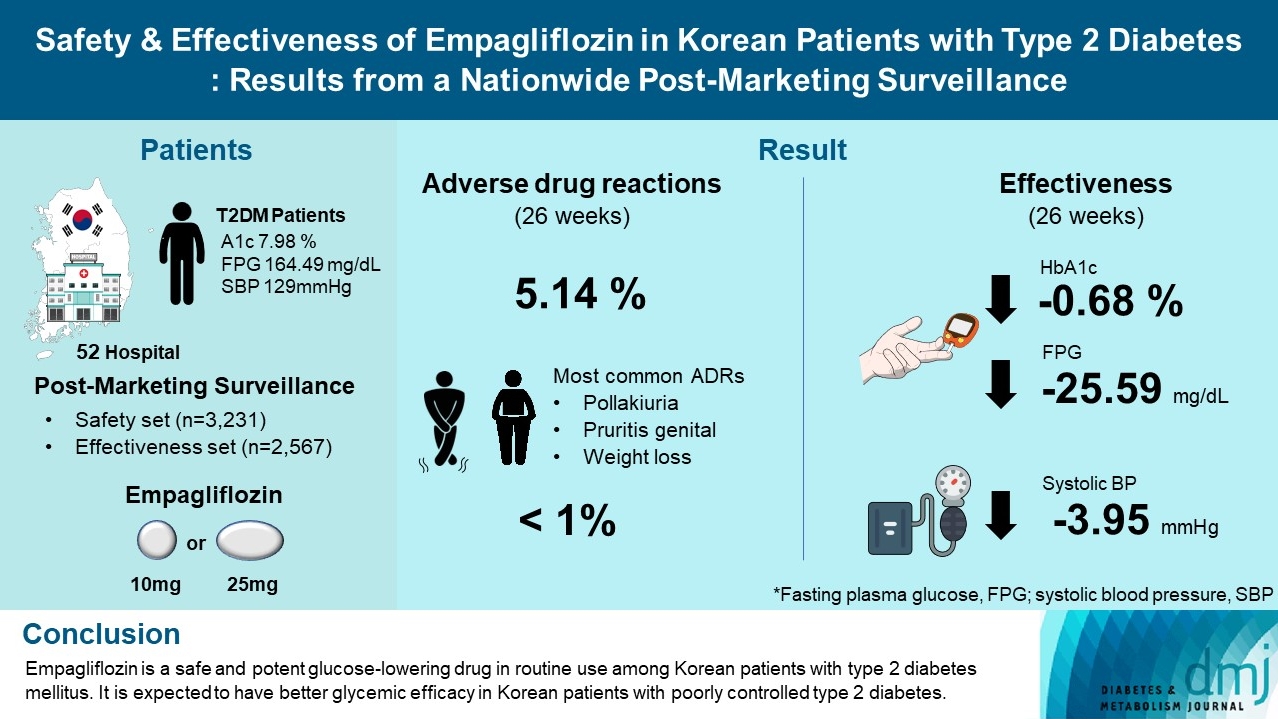
- Safety and Effectiveness of Empagliflozin in Korean Patients with Type 2 Diabetes Mellitus: Results from a Nationwide Post-Marketing Surveillance
- Jun Sung Moon, Nam Hoon Kim, Jin Oh Na, Jae Hyoung Cho, In-Kyung Jeong, Soon Hee Lee, Ji-Oh Mok, Nan Hee Kim, Dong Jin Chung, Jinhong Cho, Dong Woo Lee, Sun Woo Lee, Kyu Chang Won
- Diabetes Metab J. 2023;47(1):82-91. Published online June 20, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0356
- 6,000 View
- 297 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
To evaluate the safety and effectiveness of empagliflozin in routine clinical settings, we collected and assessed the clinical profiles of Korean patients with type 2 diabetes mellitus.
Methods
This was a post-marketing surveillance study of empagliflozin 10 and 25 mg. Information on adverse events and adverse drug reactions (ADRs) was collected as safety data sets. Available effectiveness outcomes, including glycosylated hemoglobin (HbA1c) level, fasting plasma glucose, body weight, and blood pressure, were assessed.
Results
The incidence rate of ADRs was 5.14% in the safety dataset (n=3,231). Pollakiuria, pruritis genital, and weight loss were the most common ADRs. ADRs of special interest accounted for only 1.18%, and there were no serious events that led to mortality or hospitalization. In the effectiveness data set (n=2,567), empagliflozin significantly reduced the mean HbA1c level and body weight during the study period by –0.68%±1.39% and –1.91±3.37 kg (both P<0.0001), respectively. In addition, shorter disease duration, absence of dyslipidemia, and higher baseline HbA1c levels were identified as the clinical features characteristic of a “responder” to empagliflozin therapy.
Conclusion
Empagliflozin is a safe and potent glucose-lowering drug in routine use among Korean patients with type 2 diabetes mellitus. It is expected to have better glycemic efficacy in Korean patients with poorly controlled type 2 diabetes mellitus. -
Citations
Citations to this article as recorded by- Evaluation of Efficacy and Safety of Empagliflozin in Bangladeshi Patients with Type 2 Diabetes Mellitus (EFFISAEM Study)
Mohammad Saifuddin, Ajit Kumar Paul, Sultana Marufa Shefin, Md. Jahangir Alam, Shahjada Selim, Sunjida Islam, Tanjina Hossain, Sadiqa Tuqan, Nusrat Sultana, Marufa Mustari, Ramen Chandra Basak, Kazi Ali Aftab, Indrajit Prasad, Mohammad Rafiq Uddin, Shoma
Indian Journal of Endocrinology and Metabolism.2024;[Epub] CrossRef - Comparison of the Pharmacokinetics, Safety, and Tolerability of Two Empagliflozin Formulations in Healthy Korean Subjects
Xu Jiang, Sungyeun Bae, Deok Yong Yoon, Shin Jung Park, Jaeseong Oh, Joo-Youn Cho, Kyung-Sang Yu
Drug Design, Development and Therapy.2023; Volume 17: 2137. CrossRef - Comparative safety of different sodium-glucose transporter 2 inhibitors in patients with type 2 diabetes: a systematic review and network meta-analysis of randomized controlled trials
Chun Xing Li, Li Yan Liu, Chen Xiao Zhang, Xu Hua Geng, Si Meng Gu, Yu Qiao Wang, Hua Liu, Qing Xie, Shuo Liang
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Evaluation of Efficacy and Safety of Empagliflozin in Bangladeshi Patients with Type 2 Diabetes Mellitus (EFFISAEM Study)
- Type 1 Diabetes
- Non-Insulin Antidiabetes Treatment in Type 1 Diabetes Mellitus: A Systematic Review and Meta-Analysis
- Xiaoling Cai, Chu Lin, Wenjia Yang, Lin Nie, Linong Ji
- Diabetes Metab J. 2021;45(3):312-325. Published online March 15, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0171

- 6,257 View
- 273 Download
- 5 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- In order to evaluate the efficacy and side effects of the non-insulin antidiabetes medications as an adjunct treatment in type 1 diabetes mellitus (T1DM), we conducted systematic searches in MEDLINE, Embase, and the Cochrane Central Register of Controlled Trials for randomized controlled trials published between the date of inception and March 2020 to produce a systematic review and meta-analysis. Overall, 57 studies were included. Compared with placebo, antidiabetes agents in adjunct to insulin treatment resulted in significant reduction in glycosylated hemoglobin (weighted mean difference [WMD], –0.30%; 95% confidence interval [CI], –0.34 to –0.25%; P<0.01) and body weight (WMD, –2.15 kg; 95% CI, –2.77 to –1.53 kg; P<0.01), and required a significantly lower dosage of insulin (WMD, –5.17 unit/day; 95% CI, –6.77 to –3.57 unit/day; P<0.01). Compared with placebo, antidiabetes agents in adjunct to insulin treatment increased the risk of hypoglycemia (relative risk [RR], 1.04; 95% CI, 1.01 to 1.08; P=0.02) and gastrointestinal side effects (RR, 1.99; 95% CI, 1.61 to 2.46; P<0.01) in patients with T1DM. Compared with placebo, the use of non-insulin antidiabetes agents in addition to insulin could lead to glycemic improvement, weight control and lower insulin dosage, while they might be associated with increased risks of hypoglycemia and gastrointestinal side effects in patients with T1DM.
-
Citations
Citations to this article as recorded by- Dioscin: Therapeutic potential for diabetes and complications
Haoyang Gao, Ze Wang, Danlin Zhu, Linlin Zhao, Weihua Xiao
Biomedicine & Pharmacotherapy.2024; 170: 116051. CrossRef - The Impact of Body Mass Index, Residual Beta Cell Function and Estimated Glucose Disposal Rate on the Development of Double Diabetes and Microvascular Complications in Patients With Type 1 Diabetes Mellitus
Rameez Raja Bhagadurshah, Subbiah Eagappan, Raghavan Kasthuri Santharam, Sridhar Subbiah
Cureus.2023;[Epub] CrossRef - Prescribing patterns of adjunctive therapy for the treatment of type 1 diabetes mellitus among Australian endocrinologists
Patrice Forner, Jennifer Snaith, Jerry R. Greenfield
Internal Medicine Journal.2023;[Epub] CrossRef - Type 1 diabetes glycemic management: Insulin therapy, glucose monitoring, and automation
Bruce A. Perkins, Jennifer L. Sherr, Chantal Mathieu
Science.2021; 373(6554): 522. CrossRef - Current Advances of Artificial Pancreas Systems: A Comprehensive Review of the Clinical Evidence
Sun Joon Moon, Inha Jung, Cheol-Young Park
Diabetes & Metabolism Journal.2021; 45(6): 813. CrossRef
- Dioscin: Therapeutic potential for diabetes and complications
- Drug/Regimen
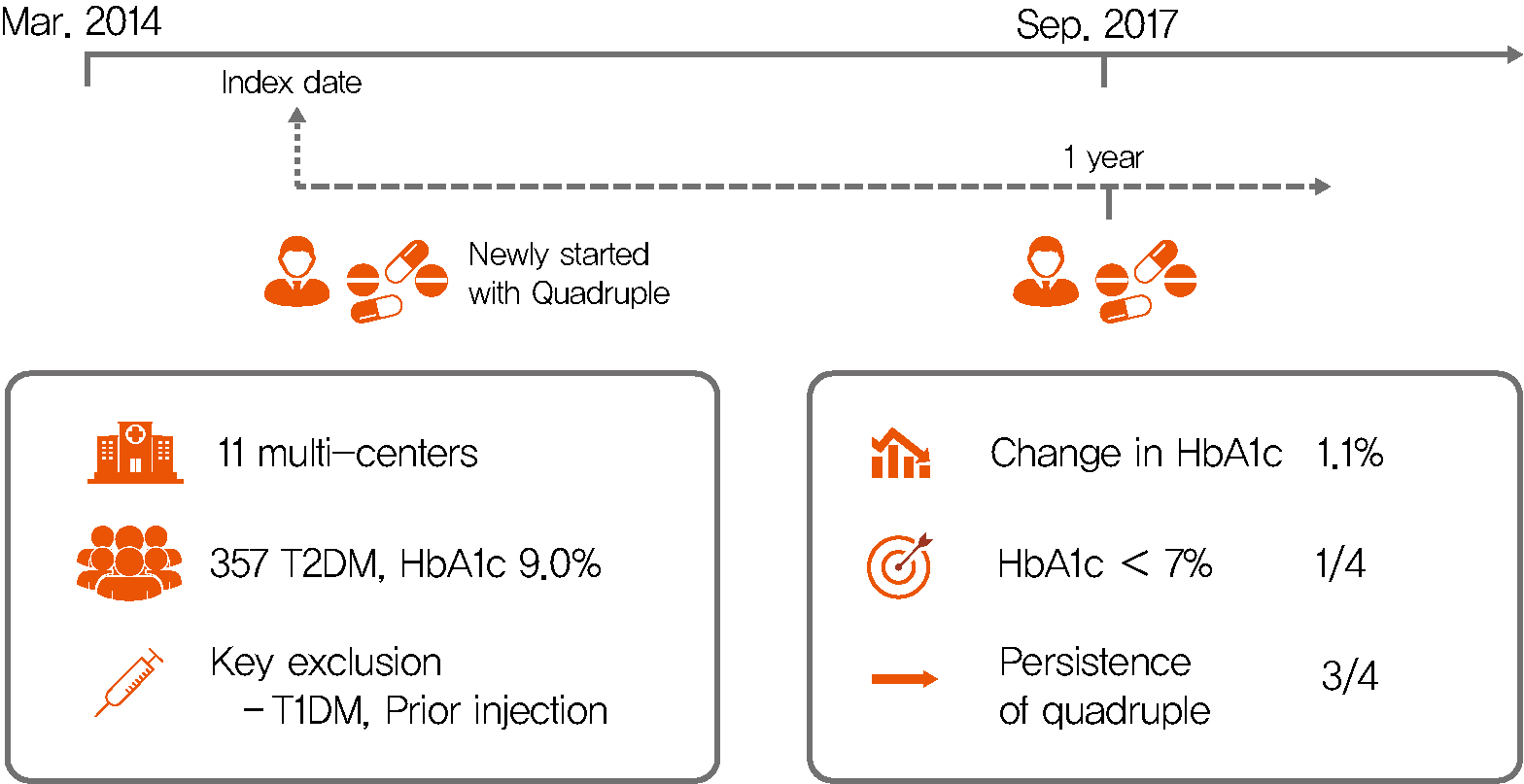
- Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
- Jun Sung Moon, Sunghwan Suh, Sang Soo Kim, Heung Yong Jin, Jeong Mi Kim, Min Hee Jang, Kyung Ae Lee, Ju Hyung Lee, Seung Min Chung, Young Sang Lyu, Jin Hwa Kim, Sang Yong Kim, Jung Eun Jang, Tae Nyun Kim, Sung Woo Kim, Eonju Jeon, Nan Hee Cho, Mi-Kyung Kim, Hye Soon Kim, Il Seong Nam-Goong, Eun Sook Kim, Jin Ook Chung, Dong-Hyeok Cho, Chang Won Lee, Young Il Kim, Dong Jin Chung, Kyu Chang Won, In Joo Kim, Tae Sun Park, Duk Kyu Kim, Hosang Shon
- Diabetes Metab J. 2021;45(5):675-683. Published online August 12, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0107
- 35,389 View
- 367 Download
- 9 Web of Science
- 5 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 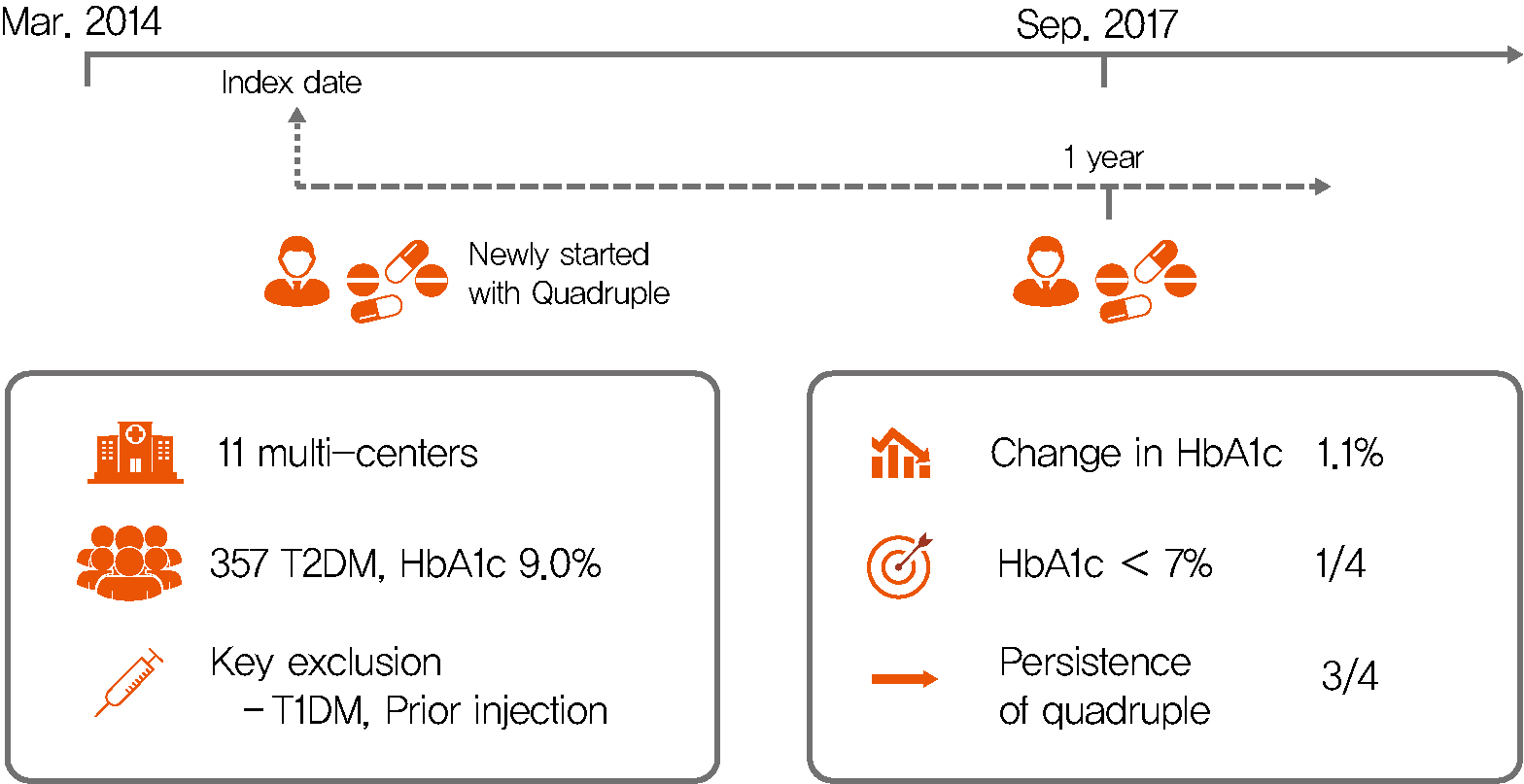
Background Only few studies have shown the efficacy and safety of glucose-control strategies using the quadruple drug combination. Therefore, the aim of the present study was to investigate the usefulness of the quadruple combination therapy with oral hypoglycemic agents (OHAs) in patients with uncontrolled type 2 diabetes mellitus (T2DM).
Methods From March 2014 to December 2018, data of patients with T2DM, who were treated with quadruple hypoglycemic medications for over 12 months in 11 hospitals in South Korea, were reviewed retrospectively. We compared glycosylated hemoglobin (HbA1c) levels before and 12 months after quadruple treatment with OHAs. The safety, maintenance rate, and therapeutic patterns after failure of the quadruple therapy were also evaluated.
Results In total, 357 patients were enrolled for quadruple OHA therapy, and the baseline HbA1c level was 9.0%±1.3% (74.9±14.1 mmol/mol). After 12 months, 270 patients (75.6%) adhered to the quadruple therapy and HbA1c was significantly reduced from 8.9%±1.2% to 7.8%±1.3% (mean change, −1.1%±1.2%;
P <0.001). The number of patients with HbA1c <7% increased significantly from 5 to 68 (P <0.005). In addition, lipid profiles and liver enzyme levels were also improved whereas no changes in body weight. There was no significant safety issue in patients treated with quadruple OHA therapy.Conclusion This study shows the therapeutic efficacy of the quadruple OHA regimen T2DM and demonstrates that it can be an option for the management of T2DM patients who cannot use insulin or reject injectable therapy.
-
Citations
Citations to this article as recorded by- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
Rita Oliveira, Matilde Monteiro-Soares, José Pedro Guerreiro, Rúben Pereira, António Teixeira-Rodrigues
Pharmacy.2024; 12(1): 18. CrossRef - Efficacy and safety of enavogliflozin versus dapagliflozin added to metformin plus gemigliptin treatment in patients with type 2 diabetes: A double-blind, randomized, comparator-active study: ENHANCE-D study
Kyung-Soo Kim, Kyung Ah Han, Tae Nyun Kim, Cheol-Young Park, Jung Hwan Park, Sang Yong Kim, Yong Hyun Kim, Kee Ho Song, Eun Seok Kang, Chul Sik Kim, Gwanpyo Koh, Jun Goo Kang, Mi Kyung Kim, Ji Min Han, Nan Hee Kim, Ji Oh Mok, Jae Hyuk Lee, Soo Lim, Sang S
Diabetes & Metabolism.2023; 49(4): 101440. CrossRef - Effectiveness and safety of teneligliptin added to patients with type 2 diabetes inadequately controlled by oral triple combination therapy: A multicentre, randomized, double‐blind, and placebo‐controlled study
Minyoung Lee, Woo‐je Lee, Jae Hyeon Kim, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(6): 1105. CrossRef - A double‐blind, Randomized controlled trial on glucose‐lowering EFfects and safety of adding 0.25 or 0.5 mg lobeglitazone in type 2 diabetes patients with INadequate control on metformin and dipeptidyl peptidase‐4 inhibitor therapy: REFIND study
Soree Ryang, Sang Soo Kim, Ji Cheol Bae, Ji Min Han, Su Kyoung Kwon, Young Il Kim, Il Seong Nam‐Goong, Eun Sook Kim, Mi‐kyung Kim, Chang Won Lee, Soyeon Yoo, Gwanpyo Koh, Min Jeong Kwon, Jeong Hyun Park, In Joo Kim
Diabetes, Obesity and Metabolism.2022; 24(9): 1800. CrossRef - Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
Jaehyun Bae, Ji Hye Huh, Minyoung Lee, Yong‐Ho Lee, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2021; 23(2): 609. CrossRef
- Estimating Type 2 Diabetes Prevalence: A Model of Drug Consumption Data
- Clinical Diabetes & Therapeutics
- Latent Autoimmune Diabetes in Adults: A Review on Clinical Implications and Management
- Silvia Pieralice, Paolo Pozzilli
- Diabetes Metab J. 2018;42(6):451-464. Published online December 17, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0190
- 12,944 View
- 501 Download
- 51 Web of Science
- 60 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Latent autoimmune diabetes in adults (LADA) is a heterogeneous disease characterized by a less intensive autoimmune process and a broad clinical phenotype compared to classical type 1 diabetes mellitus (T1DM), sharing features with both type 2 diabetes mellitus (T2DM) and T1DM. Since patients affected by LADA are initially insulin independent and recognizable only by testing for islet-cell autoantibodies, it could be difficult to identify LADA in clinical setting and a high misdiagnosis rate still remains among patients with T2DM. Ideally, islet-cell autoantibodies screening should be performed in subjects with newly diagnosed T2DM, ensuring a closer monitoring of those resulted positive and avoiding treatment of hyperglycaemia which might increase the rate of β-cells loss. Thus, since the autoimmune process in LADA seems to be slower than in classical T1DM, there is a wider window for new therapeutic interventions that may slow down β-cell failure. This review summarizes the current understanding of LADA, by evaluating data from most recent studies, the actual gaps in diagnosis and management. Finally, we critically highlight and discuss novel findings and future perspectives on the therapeutic approach in LADA.
-
Citations
Citations to this article as recorded by- A Comprehensive Survey on Diabetes Type-2 (T2D) Forecast Using Machine Learning
Satyanarayana Murthy nimmagadda, Gunnam Suryanarayana, Gangu Bharath Kumar, Ganta Anudeep, Gedela Vinay Sai
Archives of Computational Methods in Engineering.2024;[Epub] CrossRef - Ensemble machine learning reveals key features for diabetes duration from electronic health records
Gabriel Cerono, Davide Chicco
PeerJ Computer Science.2024; 10: e1896. CrossRef - LADA 30th anniversary: A growing form of diabetes with persistent unresolved questions
Ivy Lee Jia Jia, Raffaella Buzzetti, Richard David Leslie, Paolo Pozzilli
Diabetes/Metabolism Research and Reviews.2024;[Epub] CrossRef - A Curious Case of New-Onset Diabetes
Kristina Hernandez, Charity L. Tan
The Journal for Nurse Practitioners.2023; 19(3): 104411. CrossRef - Comprehensive review: Frailty in pancreas transplant candidates and recipients
Ronald F. Parsons, Ekamol Tantisattamo, Wisit Cheungpasitporn, Arpita Basu, Yee Lu, Krista L. Lentine, Kenneth J. Woodside, Neeraj Singh, Joseph Scalea, Tarek Alhamad, Ty B. Dunn, Franco H. Cabeza Rivera, Sandesh Parajuli, Martha Pavlakis, Matthew Cooper
Clinical Transplantation.2023;[Epub] CrossRef - Managing latent autoimmune disease in adults
David Morris
Independent Nurse.2023; 2023(1): 18. CrossRef - Development and validation of a clinical score for identifying patients with high risk of latent autoimmune adult diabetes (LADA): The LADA primary care-protocol study
Pilar Vich-Pérez, Juan Carlos Abánades-Herranz, Gustavo Mora-Navarro, Ángela María Carrasco-Sayalero, Miguel Ángel Salinero-Fort, Ignacio Sevilla-Machuca, Mar Sanz-Pascual, Cristina Álvarez Hernández-Cañizares, Carmen de Burgos-Lunar, Vijayaprakash Suppia
PLOS ONE.2023; 18(2): e0281657. CrossRef - Diagnostic Dilemmas and Current Treatment Approaches in Latent Onset
Autoimmune Diabetes in Adults: A Concise Review
Lakshmi Chandran, Ankul Singh S., Chitra Vellapandian
Current Diabetes Reviews.2023;[Epub] CrossRef - Anti-glutamic Acid Decarboxylase Antibody-Positive Gestational Diabetes Mellitus with Autoimmune Type 1 Diabetes Mellitus in the Early Postpartum Period: A Case Report and Literature Review
Akiko Fujishima, Yohei Onodera, Hiroshi Miura, Yukihiro Terada
The Tohoku Journal of Experimental Medicine.2023; 259(4): 327. CrossRef - Een 54-jarige man met onverklaard gewichtsverlies
N. Mutebi, A. Kharagjitsing
Tijdschrift voor Geneeskunde.2023;[Epub] CrossRef - Effects of Bacillus Calmette-Guérin on immunometabolism, microbiome and liver diseases
Muhammad Umair Ijaz, Farzam Vaziri, Yu-Jui Yvonne Wan
Liver Research.2023; 7(2): 116. CrossRef - The Etiological Diagnosis of Diabetes: Still a Challenge for the Clinician
Danièle Dubois-Laforgue, José Timsit
Endocrines.2023; 4(2): 437. CrossRef - Type 1 diabetes mellitus: features of differential diagnosis
EV Gantsgorn, OV Denisenko, YaO Osipenko, DA Kalmykova, AV Ivanov, SS Gerasyuta, GA Bulguryan, MH Ivanova, DA Saakyan
Bulletin of Russian State Medical University.2023;[Epub] CrossRef - A 1‐year pilot study of intralymphatic injections of GAD‐alum in individuals with latent autoimmune diabetes in adults (LADA) with signs of high immunity: No safety concerns and resemblance to juvenile type 1 diabetes
Ingrid K. Hals, Chandima Balasuriya, Rosaura Casas, Johnny Ludvigsson, Anneli Björklund, Valdemar Grill
Diabetes, Obesity and Metabolism.2023; 25(11): 3400. CrossRef - The relationship between red blood cell distribution width and islet β-cell function indexes in patients with latent autoimmune diabetes in adults
Xiuli Fu, Qin Tan, Wei Wei, Sheng Ding, Zhongjing Wang
BMC Endocrine Disorders.2023;[Epub] CrossRef - A Review on Latent Autoimmune Diabetes in Adults
Vijay Ravikumar, Ariba Ahmed, Ashish Anjankar
Cureus.2023;[Epub] CrossRef - Neutrophils and their role in the aetiopathogenesis of type 1 and type 2 diabetes
Anna Giovenzana, Debora Carnovale, Brett Phillips, Alessandra Petrelli, Nick Giannoukakis
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - Prevalence of Latent Autoimmune Diabetes in Adult Based on the Presence of GAD 65 Antibodies in North-Eastern Uttar Pradesh, India
Himalina Sangma, Anshul Singh, Anubha Srivastava, Vatsala Misra
Annals of the National Academy of Medical Sciences (India).2022; 58(01): 017. CrossRef - Serum Bile Acid Profiles in Latent Autoimmune Diabetes in Adults and Type 2 Diabetes Patients
Yu Zhou, Deli Ye, Xiaofen Yuan, Yonglie Zhou, Jun Xia, Giuseppe Pugliese
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Early life Bacillus Calmette-Guerin vaccination and incidence of type 1, type 2, and latent autoimmune diabetes in adulthood
Philippe Corsenac, Marie-Élise Parent, Hélène Mansaray, Andrea Benedetti, Hugues Richard, Simona Stäger, Marie-Claude Rousseau
Diabetes & Metabolism.2022; 48(3): 101337. CrossRef - Atypical Diabetes and Management Considerations
Shivajirao Prakash Patil
Primary Care: Clinics in Office Practice.2022; 49(2): 225. CrossRef - Efficacy and safety of sitagliptin and insulin for latent autoimmune diabetes in adults: A systematic review and meta‐analysis
Tong Lin, Yinhe Cai, Liting Tang, Youwei Lian, Min Liu, Chaonan Liu
Journal of Diabetes Investigation.2022; 13(9): 1506. CrossRef - Latent autoimmune diabetes in youth shows greater autoimmunity than latent autoimmune diabetes in adults: Evidence from a nationwide, multicenter, cross‐sectional study
Jin Cheng, Xiaohan Tang, Xiang Yan, Gan Huang, Shuoming Luo, Zhiguang Zhou, Xia Li
Pediatric Diabetes.2022; 23(5): 578. CrossRef - Latent Autoimmune Diabetes in Adults and Metabolic Syndrome—A Mini Review
Niansi Pan, Shimei Yang, Xiaohong Niu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Lifestyle or Environmental Influences and Their Interaction With Genetic Susceptibility on the Risk of LADA
Sofia Carlsson
Frontiers in Endocrinology.2022;[Epub] CrossRef - Antigen-specific immunotherapies in type 1 diabetes
Xuejiao Zhang, Ying Dong, Dianyuan Liu, Liu Yang, Jiayi Xu, Qing Wang
Journal of Trace Elements in Medicine and Biology.2022; 73: 127040. CrossRef - Latent autoimmune diabetes in adults: a focus on β-cell protection and therapy
Wenfeng Yin, Shuoming Luo, Zilin Xiao, Ziwei Zhang, Bingwen Liu, Zhiguang Zhou
Frontiers in Endocrinology.2022;[Epub] CrossRef - Diagnostic camouflage: A case report on Latent autoimmune diabetics of adulthood
Sandhya kiran Neupane, Prakash Paudel Jaishi, Divyaa Koirala, Arjun Kandel, Prabhat Kiran Neupane
Annals of Medicine & Surgery.2022;[Epub] CrossRef - Clinical characteristics and cardiovascular risk profile in children and adolescents with latent autoimmune diabetes: Results from the German/Austrian prospective diabetes follow‐up registry
Alena Welters, Sascha R. Tittel, Thomas Reinehr, Daniel Weghuber, Susanna Wiegand, Wolfram Karges, Clemens Freiberg, Thomas Meissner, Nanette C. Schloot, Reinhard W. Holl
Pediatric Diabetes.2022; 23(8): 1602. CrossRef - The utility of assessing C-peptide in patients with insulin-treated type 2 diabetes: a cross-sectional study
Tuccinardi Dario, Giorgino Riccardo, Pieralice Silvia, Watanabe Mikiko, Maggi Daria, Palermo Andrea, Defeudis Giuseppe, Fioriti Elvira, Pozzilli Paolo, Manfrini Silvia
Acta Diabetologica.2021; 58(4): 411. CrossRef - Cross-reactive peptide epitopes of Enterovirus Coxsackie B4 and human glutamic acid decarboxylase detecting antibodies in latent autoimmune diabetes in adults versus type 1 diabetes
Feliciana Real-Fernández, Alessandra Gallo, Francesca Nuti, Lorenzo Altamore, Gloria Giovanna Del Vescovo, Pietro Traldi, Eugenio Ragazzi, Paolo Rovero, Annunziata Lapolla, Anna Maria Papini
Clinica Chimica Acta.2021; 515: 73. CrossRef - Treating latent autoimmune diabetes in adults in the era of cardiovascular outcomes trials: Old dog should learn new tricks
Theocharis Koufakis, Prashanth Vas, Kalliopi Kotsa
Diabetic Medicine.2021;[Epub] CrossRef - Defining and Classifying New Subgroups of Diabetes
Ashok Balasubramanyam
Annual Review of Medicine.2021; 72(1): 63. CrossRef - Slowly evolving, immune-mediated diabetes in 14-year-old patient: a case report
M. R. Ragimov, D. D. Omelchuk, L. I. Ibragimova, O. S. Derevyanko, T. V. Nikonova
Diabetes mellitus.2021; 24(1): 70. CrossRef - The role of autoimmunity in the pathophysiology of type 2 diabetes: Looking at the other side of the moon
Theocharis Koufakis, George Dimitriadis, Symeon Metallidis, Pantelis Zebekakis, Kalliopi Kotsa
Obesity Reviews.2021;[Epub] CrossRef - Dapagliflozin as an Adjunct Therapy to Insulin in Patients with Type 1 Diabetes Mellitus: Efficacy and Safety of this Combination
Johan H Jendle, Francisco J Ampudia-Blasco, Martin Füchtenbusch, Paolo Pozzilli
European Endocrinology.2021; 1(1): 12. CrossRef - Dapagliflozin as an Adjunct Therapy to Insulin in Patients with Type 1 Diabetes Mellitus: Efficacy and Safety of this Combination
Johan H Jendle, Francisco J Ampudia-Blasco, Martin Füchtenbusch, Paolo Pozzilli
touchREVIEWS in Endocrinology.2021; 17(1): 12. CrossRef - Toward an Improved Classification of Type 2 Diabetes: Lessons From Research into the Heterogeneity of a Complex Disease
Maria J Redondo, Ashok Balasubramanyam
The Journal of Clinical Endocrinology & Metabolism.2021; 106(12): e4822. CrossRef - Bacillus Calmette-Guerin 's beneficial impact on glucose metabolism: Evidence for broad based applications
Gabriella F. Shpilsky, Hiroyuki Takahashi, Anna Aristarkhova, Michele Weil, Nathan Ng, Kacie J. Nelson, Amanda Lee, Hui Zheng, Willem M. Kühtreiber, Denise L. Faustman
iScience.2021; 24(10): 103150. CrossRef - Masqueraders: how to identify atypical diabetes in primary care
Sumera Ahmed, Sana Saeed, Jay H. Shubrook
Journal of Osteopathic Medicine.2021; 121(12): 899. CrossRef - Lada or Type 2 Diabetes Mellitus - A Challenging Diagnosis in Clinical Approach
Lucia Mihaela Custură, Oana Deteşan, Raluca Maria Tilinca, Reka Annamaria Schmiedt, Brigitta Irén Bacso, Mariana Cornelia Tilinca
Acta Medica Transilvanica.2021; 26(3): 55. CrossRef - Antioxidant, Anti-Inflammatory, and Immunomodulatory Properties of Tea—The Positive Impact of Tea Consumption on Patients with Autoimmune Diabetes
Anna Winiarska-Mieczan, Ewa Tomaszewska, Karolina Jachimowicz
Nutrients.2021; 13(11): 3972. CrossRef - A Review of Statistical and Machine Learning Techniques for Microvascular Complications in Type 2 Diabetes
Nitigya Sambyal, Poonam Saini, Rupali Syal
Current Diabetes Reviews.2021; 17(2): 143. CrossRef - Bariatric Surgery Outcomes in Patients with Latent Autoimmune Diabetes of the Adult
Marta Guimarães, Sofia S. Pereira, Mário Nora, Mariana P. Monteiro
Obesity Facts.2021; 14(4): 425. CrossRef - Особливості перебігу діабетичної хвороби нирок у хворих на латентний автоімунний діабет дорослих
I.O. Tsaryk, N.V. Pashkovska
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2021; 17(2): 116. CrossRef - Latenter Autoimmundiabetes im Erwachsenen- und Kindesalter
Alena Welters, Nanette C. Schloot
Der Diabetologe.2020; 16(1): 27. CrossRef - A treatment-based algorithm for identification of diabetes type in the National Health and Nutrition Examination Survey
Mitra Mosslemi, Hannah L. Park, Christine E. McLaren, Nathan D. Wong
Cardiovascular Endocrinology & Metabolism.2020; 9(1): 9. CrossRef - Case 6-2020: A 34-Year-Old Woman with Hyperglycemia
Richard C. Cabot, Eric S. Rosenberg, Virginia M. Pierce, David M. Dudzinski, Meridale V. Baggett, Dennis C. Sgroi, Jo-Anne O. Shepard, Kathy M. Tran, Emily K. McDonald, Tara Corpuz, Miriam S. Udler, Camille E. Powe, Christina A. Austin-Tse
New England Journal of Medicine.2020; 382(8): 745. CrossRef - Therapeutic approaches for latent autoimmune diabetes in adults: One size does not fit all
Theocharis Koufakis, Niki Katsiki, Pantelis Zebekakis, George Dimitriadis, Kalliopi Kotsa
Journal of Diabetes.2020; 12(2): 110. CrossRef - Grenzformen zwischen Typ-1- und Typ-2-Diabetes
Michael Hummel
MMW - Fortschritte der Medizin.2020; 162(11): 60. CrossRef - The Differential Expression of Long Noncoding RNAs in Type 2 Diabetes Mellitus and Latent Autoimmune Diabetes in Adults
Zhang Pengyu, Yan Yan, Fu Xiying, Yang Maoguang, Li Mo, Cheng Yan, Shen Hong, Wang Lijuan, Zhang Xiujuan, Cai Hanqing
International Journal of Endocrinology.2020; 2020: 1. CrossRef - A convenient diagnostic tool for discriminating adult-onset glutamic acid decarboxylase antibody-positive autoimmune diabetes from type 2 diabetes: a retrospective study
Hon-Ke Sia, Shih-Te Tu, Pei-Yung Liao, Kuan-Han Lin, Chew-Teng Kor, Ling-Ling Yeh
PeerJ.2020; 8: e8610. CrossRef - Correct Diabetes Diagnosis and Treatment Allows Sailor to Remain on Active Duty
Andrea R Frazier
Military Medicine.2020; 185(9-10): e1843. CrossRef - Hombre de 28 años con presentación de diabetes
M. Ricci, J. Sanz Cánovas, V. Buonaluto, R. Gómez Huelgas
Medicine - Programa de Formación Médica Continuada Acreditado.2020; 13(16): 942.e1. CrossRef - Uncommon Presentations of Diabetes: Zebras in the Herd
Karen L. Shidler, Lisa R. Letourneau, Lucia M. Novak
Clinical Diabetes.2020; 38(1): 78. CrossRef - Ketogenic Diet as a Trigger for Diabetic Ketoacidosis in a Misdiagnosis of Diabetes: A Case Report
Alexander J. White-Cotsmire, Amber M. Healy
Clinical Diabetes.2020; 38(3): 318. CrossRef - Subphänotypen des Diabetes
Oana Patricia Zaharia, Julia Szendrödi
Der Diabetologe.2019; 15(4): 288. CrossRef - Autoimmunity in latent autoimmune diabetes in adults
Alessandro P. Delitala
AIMS Medical Science.2019; 6(2): 132. CrossRef - Risk of diabetes-associated diseases in subgroups of patients with recent-onset diabetes: a 5-year follow-up study
Oana P Zaharia, Klaus Strassburger, Alexander Strom, Gidon J Bönhof, Yanislava Karusheva, Sofia Antoniou, Kálmán Bódis, Daniel F Markgraf, Volker Burkart, Karsten Müssig, Jong-Hee Hwang, Olof Asplund, Leif Groop, Emma Ahlqvist, Jochen Seissler, Peter Nawr
The Lancet Diabetes & Endocrinology.2019; 7(9): 684. CrossRef - The Influence of Type 2 Diabetes–Associated Factors on Type 1 Diabetes
Maria J. Redondo, Carmella Evans-Molina, Andrea K. Steck, Mark A. Atkinson, Jay Sosenko
Diabetes Care.2019; 42(8): 1357. CrossRef
- A Comprehensive Survey on Diabetes Type-2 (T2D) Forecast Using Machine Learning
- Others
- Synthesis of a New Zinc-Mixed Ligand Complex and Evaluation of Its Antidiabetic Properties in High Fat Diet: Low Dose Streptozotocin Induced Diabetic Rats
- Muruganantham Koothappan, Roshana Devi Vellai, Iyyam Pillai Subramanian, Sorimuthu Pillai Subramanian
- Diabetes Metab J. 2018;42(3):244-248. Published online April 24, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0002
- 3,712 View
- 49 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Due to the multifactorial and multisystemic nature of diabetes mellitus, it is often treated with a combination of therapeutic agents having different mode of action. Earlier, we have synthesized several organozinc complexes and evaluated their safety and antidiabetic properties in experimental type 2 diabetes mellitus (T2DM). More recently, we have synthesized a metformin-3-hydroxyflavone complex and studied its antidiabetic efficacy in experimental rats. In the present study, a new zinc-mixed ligand (metformin-3-hydroxyflavone) was synthesized, characterized by spectral studies and its antidiabetic properties was evaluated in HFD fed—low dose streptozotocin induced T2DM in rats. The hypoglycemic efficacy of the complex was evaluated through oral glucose tolerance test, homeostasis model assessment of insulin resistance, quantitative insulin sensitivity check index and by determining the status of important biochemical parameters. Oral administration of the complex at a concentration of 10 mg/kg body weight/rat/day for 30 days significantly improved the glucose homeostasis. The complex possesses significant antidiabetic properties relatively at a less concentration than metformin-3-hydroxyflavone complex in ameliorating hyperglycemia.
-
Citations
Citations to this article as recorded by- Metformin compounds: A review on the importance and the possible applications
A H Ismail, Z S Al-Garawi, K Al-Shamari, A T Salman
Journal of Physics: Conference Series.2021; 1853(1): 012060. CrossRef - A Review on Natural Products and Herbs Used in the Management of Diabetes
Deepshikha Patle, Manish Vyas, Gopal L. Khatik
Current Diabetes Reviews.2021; 17(2): 186. CrossRef - The role of activation of KАTP channels on hydrogen sulfide induced renoprotective effect on diabetic nephropathy
Eman A. Elbassuoni, Neven M. Аziz, Wagdу N. Habeeb
Journal of Cellular Physiology.2020; 235(6): 5223. CrossRef - A comprehensive review on zinc(II) complexes as anti-diabetic agents: The advances, scientific gaps and prospects
Chika Ifeanyi Chukwuma, Samson S. Mashele, Kenneth C. Eze, Godfrey R. Matowane, Shahidul Md. Islam, Susanna L. Bonnet, Anwar E.M. Noreljaleel, Limpho M. Ramorobi
Pharmacological Research.2020; 155: 104744. CrossRef
- Metformin compounds: A review on the importance and the possible applications
- Clinical Diabetes & Therapeutics
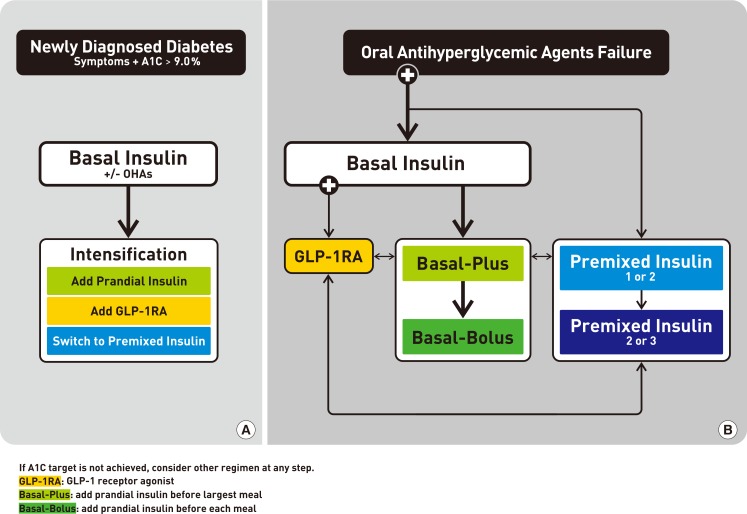
- Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
- Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
- Diabetes Metab J. 2017;41(5):367-373. Published online October 24, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.5.367
- 7,452 View
- 220 Download
- 7 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The Korean Diabetes Association (KDA) has regularly updated its Clinical Practice Guidelines. In 2017, the KDA published a position statement on the use of antihyperglycemic agents for patients with type 2 diabetes mellitus (T2DM). Growing evidence from new multinational clinical trials using novel and traditional insulin analogues has also been accumulated. Following global trends, many results of clinical trials, especially concerning the clinical efficacy and safety of insulin therapy, have been published about Korean patients with T2DM. After a systematic search of recent evidence, the KDA updated and modified its clinical practice recommendations regarding the initiation, choice, and intensification of insulin and created an insulin treatment algorithm for the first time to guide physicians caring for adult Korean patients with T2DM.
-
Citations
Citations to this article as recorded by- Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
Eun-Gyoung Hong, Kyung-Wan Min, Jung Soo Lim, Kyu-Jeung Ahn, Chul Woo Ahn, Jae-Myung Yu, Hye Soon Kim, Hyun Jin Kim, Won Kim, Dong Han Kim, Hak Chul Jang
Advances in Therapy.2024; 41(5): 1967. CrossRef - Tolerability and Effectiveness of Switching to Dulaglutide in Patients With Type 2 Diabetes Inadequately Controlled With Insulin Therapy
Youngsook Kim, Ji Hye Huh, Minyoung Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2022;[Epub] CrossRef - Increasing Individual Target Glucose Levels to Prevent Hypoglycemia in Patients with Diabetes
Juyoung Shin, Hyunah Kim, Hun-Sung Kim, Churlmin Kim, Whan-Seok Choi
Korean Journal of Family Medicine.2021; 42(4): 269. CrossRef - Effects of an actual insulin injection demonstration on insulin acceptance among patients with T2DM: a pragmatic randomized controlled trial
Atthayaporn Choomai, Apichai Wattanapisit, Orathai Tiangtam
Romanian Journal of Internal Medicine.2021; 59(2): 151. CrossRef - Favorable Glycemic Control with Once-Daily Insulin Degludec/Insulin Aspart after Changing from Basal Insulin in Adults with Type 2 Diabetes
Han Na Jang, Ye Seul Yang, Seong Ok Lee, Tae Jung Oh, Bo Kyung Koo, Hye Seung Jung
Endocrinology and Metabolism.2019; 34(4): 382. CrossRef - Capacity and confidence building for general practitioners on optimum insulin use
Sanjay Kalra, Prasun Deb, KalyanK Gangopadhyay, Sunil Gupta, Abhay Ahluwalia
Journal of Family Medicine and Primary Care.2019; 8(10): 3096. CrossRef - Educational Strategies for Insulin Injection Therapy in Elderly Diabetic Patients
Eun Chong Shin
The Journal of Korean Diabetes.2018; 19(2): 101. CrossRef - Summary of Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
Byung-Wan Lee
The Journal of Korean Diabetes.2018; 19(1): 31. CrossRef - New anti-diabetic agents
Doo-Man Kim
Journal of the Korean Medical Association.2017; 60(12): 992. CrossRef
- Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
- Clinical Diabetes & Therapeutics
- Combination Therapy of Oral Hypoglycemic Agents in Patients with Type 2 Diabetes Mellitus
- Min Kyong Moon, Kyu-Yeon Hur, Seung-Hyun Ko, Seok-O Park, Byung-Wan Lee, Jin Hwa Kim, Sang Youl Rhee, Hyun Jin Kim, Kyung Mook Choi, Nan-Hee Kim
- Diabetes Metab J. 2017;41(5):357-366. Published online October 24, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.5.357
- 7,641 View
- 150 Download
- 17 Web of Science
- 15 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
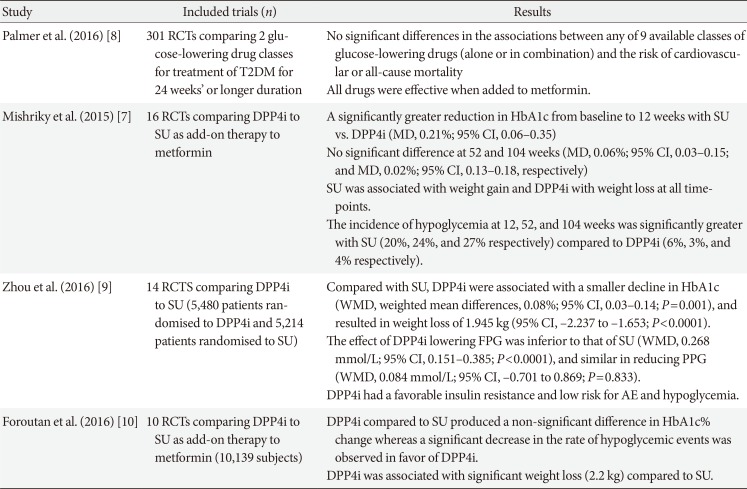
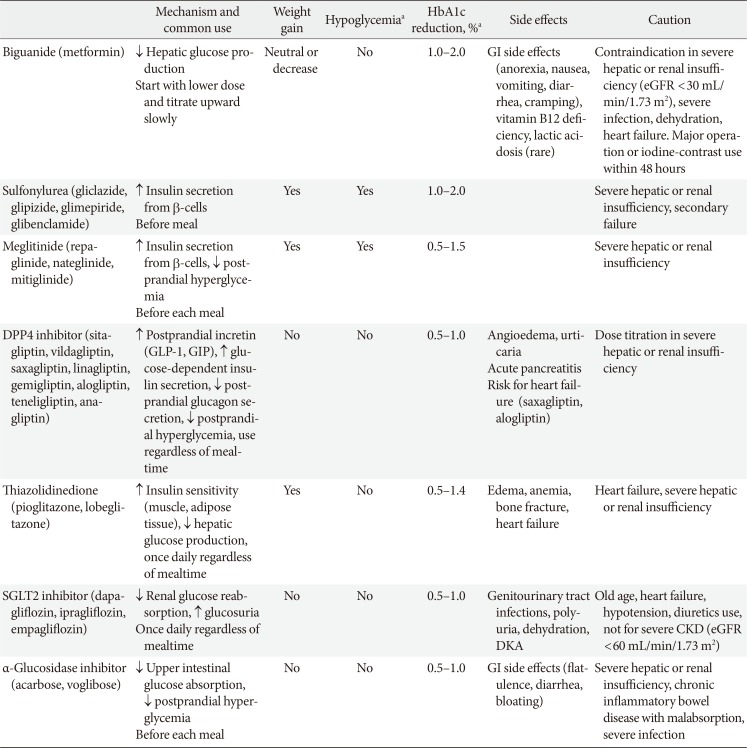
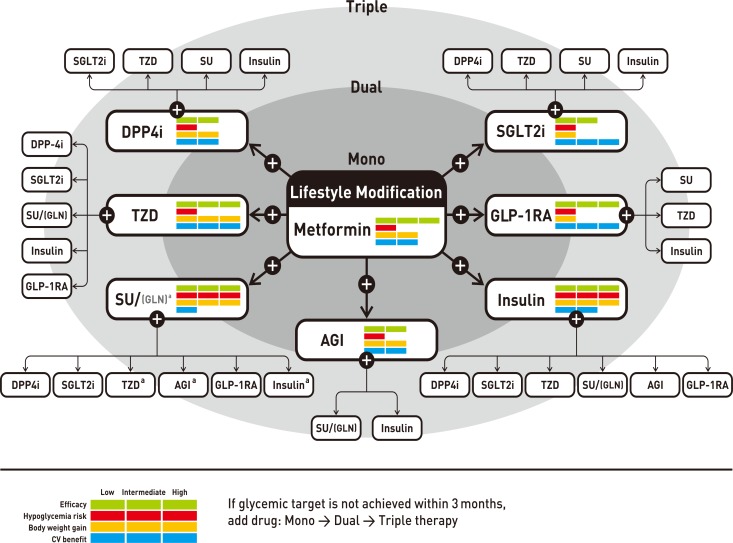
PubReader The Korean Diabetes Association (KDA) recently updated the Clinical Practice Guidelines on antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus (T2DM). In combination therapy of oral hypoglycemic agents (OHAs), general recommendations were not changed from those of the 2015 KDA guidelines. The Committee on Clinical Practice Guidelines of the KDA has extensively reviewed and discussed the results of meta-analyses and systematic reviews of effectiveness and safety of OHAs and many clinical trials on Korean patients with T2DM for the update of guidelines. All OHAs were effective when added to metformin or metformin and sulfonylurea, although the effects of each agent on body weight and hypoglycemia were different. Therefore, selection of a second agent as a metformin add-on therapy or third agent as a metformin and sulfonylurea add-on therapy should be based on the patient's clinical characteristics and the efficacy, side effects, mechanism of action, risk of hypoglycemia, effect on body weight, patient preference, and combined comorbidity. In this review, we address the results of meta-analyses and systematic reviews, comparing the effectiveness and safety among OHAs. It will help to choose the appropriate drug for an individual patient with T2DM.
-
Citations
Citations to this article as recorded by- Unveiling the potential of prodrug and drug-conjugate strategies in treatment of diabetes mellitus and its complications
Neha V. Bhilare, Rushikesh Shedge, Prashant M. Tambe, Ajinkya More
Medicinal Chemistry Research.2024; 33(3): 337. CrossRef - Simultaneous Estimation of Repaglinide and Voglibose in Newly
Approved Fixed-Dose Combination by using UFLC: Application to
ICH Q14 Concept and Comparative Method Greenness Assessment
S.S. Panda, P.C. Rauta, V.S. Pulusu, S. Sahu, B.B. Dash
Asian Journal of Chemistry.2023; 35(4): 887. CrossRef - Time to reposition sulfonylureas in type 2 diabetes management in Indian context: A pragmatic practical approach
Ashok Kumar Das, Banshi Saboo, Rajeev Chawla, S. R. Aravind, Rajesh Rajput, Awadhesh K. Singh, J. J. Mukherjee, Ashok Jhingan, Parag Shah, Vaishali Deshmukh, Shailaja Kale, Shalini Jaggi, G. R. Sridhar, Rajnish Dhediya, Kumar Gaurav
International Journal of Diabetes in Developing Countries.2023; 43(6): 856. CrossRef - The Gut Microbiome, Metformin, and Aging
Sri Nitya Reddy Induri, Payalben Kansara, Scott C. Thomas, Fangxi Xu, Deepak Saxena, Xin Li
Annual Review of Pharmacology and Toxicology.2022; 62(1): 85. CrossRef - Role of resveratrol supplementation in regulation of glucose hemostasis, inflammation and oxidative stress in patients with diabetes mellitus type 2: A randomized, placebo-controlled trial
Wajiha Mahjabeen, Dilshad Ahmed Khan, Shakil Ahmed Mirza
Complementary Therapies in Medicine.2022; 66: 102819. CrossRef - Letrozole: Pharmacology, toxicity and potential therapeutic effects
Anirban Goutam Mukherjee, Uddesh Ramesh Wanjari, Dhanushya Nagarajan, Vibhaa K K, Anagha V, Joshua Paul P, Tharani Priya T, Rituraj Chakraborty, Kaviyarasi Renu, Abhijit Dey, Balachandar Vellingiri, Abilash Valsala Gopalakrishnan
Life Sciences.2022; 310: 121074. CrossRef - Increasing Individual Target Glucose Levels to Prevent Hypoglycemia in Patients with Diabetes
Juyoung Shin, Hyunah Kim, Hun-Sung Kim, Churlmin Kim, Whan-Seok Choi
Korean Journal of Family Medicine.2021; 42(4): 269. CrossRef - Treatment intensification in type 2 diabetes management after the failure of two oral hypoglycemic agents: A non‐interventional comparative study
Sirajudeen Shaik Alavudeen, Sultan M. Alshahrani, Easwaran Vigneshwaran, Noohu Abdulla Khan, Javid I. Mir, Abubakr T. M. Hussein
International Journal of Clinical Practice.2021;[Epub] CrossRef - Aldose reductase and protein tyrosine phosphatase 1B inhibitors as a promising therapeutic approach for diabetes mellitus
Antonios Kousaxidis, Anthi Petrou, Vasiliki Lavrentaki, Maria Fesatidou, Ioannis Nicolaou, Athina Geronikaki
European Journal of Medicinal Chemistry.2020; 207: 112742. CrossRef - Letter: Efficacy and Safety of Voglibose Plus Metformin in Patients with Type 2 Diabetes Mellitus: A Randomized Controlled Trial (Diabetes Metab J 2019;43;276-86)
Hannah Seok, Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(4): 545. CrossRef - A Survey of the Structures of US FDA Approved Combination Drugs
Pradipta Das, Michael D. Delost, Munaum H. Qureshi, David T. Smith, Jon T. Njardarson
Journal of Medicinal Chemistry.2019; 62(9): 4265. CrossRef - Experimental design methodology for optimization and robustness determination in ion pair RP-HPLC method development: Application for the simultaneous determination of metformin hydrochloride, alogliptin benzoate and repaglinide in tablets
Marianne A. Mahrouse, Nesrine T. Lamie
Microchemical Journal.2019; 147: 691. CrossRef - The influence of diabetes and antidiabetic medications on the risk of pancreatic cancer: a nationwide population-based study in Korea
Da Young Lee, Ji Hee Yu, Sanghyun Park, Kyungdo Han, Nam Hoon Kim, Hye Jin Yoo, Kyung Mook Choi, Sei Hyun Baik, Nan Hee Kim, Ji A. Seo
Scientific Reports.2018;[Epub] CrossRef - Effect of Lifestyle Modification and Oral Anti-Diabetic Drugs on Metabolic Parameters in Recently Diagnosed Patientswith Uncomplicated Type 2 Diabetes Mellitus in Eastern India
Nikhilesh Pradhan, Sidhartha Das, Anoj Kumar Baliarsinha, Ashirbad Parhi, Bijan Patnaik, Pramod Kumar Rout
Journal of Diabetes Mellitus.2018; 08(02): 9. CrossRef - Failure of monotherapy in clinical practice in patients with type 2 diabetes: The Korean National Diabetes Program
Ja Young Jeon, Soo Jin Lee, Sieun Lee, Soo Jin Kim, Seung Jin Han, Hae Jin Kim, Dae Jung Kim, Young Seol Kim, Jeong Taek Woo, Kyu Jeung Ahn, Moonsuk Nam, Sei Hyun Baik, Yongsoo Park, Kwan‐Woo Lee
Journal of Diabetes Investigation.2018; 9(5): 1144. CrossRef
- Unveiling the potential of prodrug and drug-conjugate strategies in treatment of diabetes mellitus and its complications
- Clinical Diabetes & Therapeutics
- Monotherapy in Patients with Type 2 Diabetes Mellitus
- Sang Youl Rhee, Hyun Jin Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Kyung Mook Choi, Jin Hwa Kim
- Diabetes Metab J. 2017;41(5):349-356. Published online October 19, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.5.349
- 5,666 View
- 70 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader In order to improve the quality of life and to prevent chronic complications related to diabetes mellitus, intensive lifestyle modification and proper medication are needed from the early stage of diagnosis of type 2 diabetes mellitus (T2DM). When using the first medication for diabetic patients, the appropriate treatment should be selected considering the clinical characteristics of the patient, efficacy of the drug, side effects, and cost. In general, the use of metformin as the first treatment for oral hypoglycemic monotherapy is recommended because of its excellent blood glucose-lowering effect, relatively low side effects, long-term proven safety, low risk of hypoglycemia, and low weight gain. If metformin is difficult to use as a first-line treatment, other appropriate medications should be selected in view of the clinical situation. If the goal of achieving glycemic control is not achieved by monotherapy, a combination therapy with different mechanisms of action should be initiated promptly.
-
Citations
Citations to this article as recorded by- Diabetic Patients with COVID-19 Complications: Insights into Prevalence,
Prognosis, Combination Medications, and Underlying Mechanisms
Pranay Wal, Jyotsana Dwivedi, Ankita Wal, Shivangi Kushwaha
Current Diabetes Reviews.2023;[Epub] CrossRef - Increasing Individual Target Glucose Levels to Prevent Hypoglycemia in Patients with Diabetes
Juyoung Shin, Hyunah Kim, Hun-Sung Kim, Churlmin Kim, Whan-Seok Choi
Korean Journal of Family Medicine.2021; 42(4): 269. CrossRef - Synthesis, antidiabetic activity and molecular docking study of rhodanine-substitued spirooxindole pyrrolidine derivatives as novel α-amylase inhibitors
Amani Toumi, Sarra Boudriga, Khaled Hamden, Mansour Sobeh, Mohammed Cheurfa, Moheddine Askri, Michael Knorr, Carsten Strohmann, Lukas Brieger
Bioorganic Chemistry.2021; 106: 104507. CrossRef - Clinical Impact of Combination Therapy in Diabetic Neuropathy and Nephropathy
Harmeet Kaur, Arvinder Kaur, Pankaj Kumar Prashar, Anamika Gautam, Ankita Sood, Sachin Kumar Singh, Monica Gulati, Narendra Kumar Pandey, Bimlesh Kumar
Research Journal of Pharmacy and Technology.2021; : 3471. CrossRef - Type II diabetes mellitus: a review on recent drug based therapeutics
Santwana Padhi, Amit Kumar Nayak, Anindita Behera
Biomedicine & Pharmacotherapy.2020; 131: 110708. CrossRef - Comparison of the effects of gemigliptin and dapagliflozin on glycaemic variability in type 2 diabetes: A randomized, open‐label, active‐controlled, 12‐week study (STABLE II study)
Soo Heon Kwak, You‐Cheol Hwang, Jong Chul Won, Ji Cheol Bae, Hyun Jin Kim, Sunghwan Suh, Eun Young Lee, Subin Lee, Sang‐Yong Kim, Jae Hyeon Kim
Diabetes, Obesity and Metabolism.2020; 22(2): 173. CrossRef - Metabolomics approach to identify the active substances influencing the antidiabetic activity of Lagerstroemia species
Mun-Ock Kim, Su Ui Lee, Heung Joo Yuk, Hyun-Jae Jang, Jae-Won Lee, Eun-Bin Kwon, Jin-Hyub Paik, SangHo Choi, Adek Nizar, Tran The Bach, Kongmany Sydara, Hang Jin, So-Yeun Woo, Sei-Ryang Oh, Hyung Won Ryu
Journal of Functional Foods.2020; 64: 103684. CrossRef - Cardiometabolic diseases and active aging - polypharmacy in control
Adriana Nancy Medeiros dos Santos, Dulcineia Rebecca Cappelletti Nogueira, Beatriz Aparecida Ozello Gutierrez, Rosa Yuka Sato Chubaci, Caroline Ribeiro de Borja Oliveira
Revista Brasileira de Enfermagem.2020;[Epub] CrossRef - Anti-Diabetic Nephropathy Activities of Polysaccharides Obtained from Termitornyces albuminosus via Regulation of NF-κB Signaling in db/db Mice
Chang Yang, Qi Feng, Huan Liao, Xinlei Yu, Yang Liu, Di Wang
International Journal of Molecular Sciences.2019; 20(20): 5205. CrossRef - Specific PERK inhibitors enhanced glucose-stimulated insulin secretion in a mouse model of type 2 diabetes
Min Joo Kim, Mi Na Kim, Se Hee Min, Dong-Sik Ham, Ji-Won Kim, Kun-Ho Yoon, Kyong Soo Park, Hye Seung Jung
Metabolism.2019; 97: 87. CrossRef - A randomized, open‐label, multicentre, parallel‐controlled study comparing the efficacy and safety of biphasic insulin aspart 30 plus metformin with biphasic insulin aspart 30 monotherapy for type 2 diabetes patients inadequately controlled with oral anti
Lixin Guo, Li Chen, Baocheng Chang, Liyong Yang, Yu Liu, Bo Feng
Diabetes, Obesity and Metabolism.2018; 20(12): 2740. CrossRef - Monotherapy in Type 2 Diabetes Mellitus Patients 2017: A Position Statement of the Korean Diabetes Association
Sang Youl Rhee
The Journal of Korean Diabetes.2018; 19(1): 15. CrossRef
- Diabetic Patients with COVID-19 Complications: Insights into Prevalence,
Prognosis, Combination Medications, and Underlying Mechanisms
- Clinical Diabetes & Therapeutics
- Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
- Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
- Diabetes Metab J. 2017;41(5):337-348. Published online October 17, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.5.337
- 7,127 View
- 64 Download
- 38 Web of Science
- 45 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader In 2017, the Korean Diabetes Association (KDA) published a position statement on the use of antihyperglycemic agents for patients with type 2 diabetes mellitus (T2DM). The KDA regularly updates its Clinical Practice Guidelines, but since the last update in 2015, many results from clinical trials have been introduced, and domestic data from studies performed in Korean patients with T2DM have been published. Recently, evidence from large clinical studies assessing cardiovascular outcomes following the use of sodium-glucose cotransporter 2 inhibitors and glucagon-like peptide 1 receptor agonists in patients with T2DM were incorporated into the recommendations. Additionally, new data from clinical trials using dipeptidyl peptidase 4 inhibitors and thiazolidinediones in Korean patients with T2DM were added. Following a systematic review and assessment of recent evidence, the KDA updated and modified its clinical practice recommendations regarding the use of antihyperglycemic agents and revised the treatment algorithm for Korean adult patients with T2DM.
-
Citations
Citations to this article as recorded by- Comparative Study on Efficacy of Empagliflozin Versus Sitagliptin, as an Add-on Therapy to Metformin in Type 2 Diabetic Patients
Harsh Salankar, Sonali Rode, C. Arjun, Rajeeta Joseph, Gourav B. Deshmane, Radhika P. Vijayan
Journal of Pharmacy and Bioallied Sciences.2024; 16(Suppl 1): S335. CrossRef - Two-Year Therapeutic Efficacy and Safety of Initial Triple Combination of Metformin, Sitagliptin, and Empagliflozin in Drug-Naïve Type 2 Diabetes Mellitus Patients
Young-Hwan Park, Minji Sohn, So Yeon Lee, Soo Lim
Diabetes & Metabolism Journal.2024; 48(2): 253. CrossRef - Association of preoperative blood glucose level with delirium after non-cardiac surgery in diabetic patients
Soo Jung Park, Ah Ran Oh, Jong-Hwan Lee, Kwangmo Yang, Jungchan Park
Korean Journal of Anesthesiology.2024; 77(2): 226. CrossRef - Systematic review and meta-analysis of teneligliptin for treatment of type 2 diabetes
R. Pelluri, S. Kongara, V. R. Nagasubramanian, S. Mahadevan, J. Chimakurthy
Journal of Endocrinological Investigation.2023; 46(5): 855. CrossRef - Effects of dapagliflozin compared with glimepiride on body composition in Asian patients with type 2 diabetes inadequately controlled with metformin: The BEYOND study
Hyeong Kyu Park, Kyoung‐Ah Kim, Kyung‐Wan Min, Tae‐Seo Sohn, In Kyung Jeong, Chul Woo Ahn, Nan‐Hee Kim, Ie Byung Park, Ho Chan Cho, Choon Hee Chung, Sung Hee Choi, Kang Seo Park, Seoung‐Oh Yang, Kwan Woo Lee
Diabetes, Obesity and Metabolism.2023; 25(9): 2743. CrossRef - Paradigm Shift in Management of Hyperglycemia in Patients with Type 2 Diabetes: Glucocentric versus Organ Protection
Jong Chul Won
The Journal of Korean Diabetes.2023; 24(2): 59. CrossRef - A Comparison of the Effects of Empagliflozin and Sitagliptin, When Combined With Metformin, on Lipid Levels in Patients with Type 2 Diabetes: A Clinical Investigation
Mazhar Ahmed, Asjad Saeed, Muhammad Zarar Khan, Sana Z Javaid, Farhan Aslam, Savida Ilyas Dar
Cureus.2023;[Epub] CrossRef - Efficacy and Safety of Evogliptin Add-on Therapy to Dapagliflozin/Metformin Combinations in Patients with Poorly Controlled Type 2 Diabetes Mellitus: A 24-Week Multicenter Randomized Placebo-Controlled Parallel-Design Phase-3 Trial with a 28-Week Extensio
Jun Sung Moon, Il Rae Park, Hae Jin Kim, Choon Hee Chung, Kyu Chang Won, Kyung Ah Han, Cheol-Young Park, Jong Chul Won, Dong Jun Kim, Gwan Pyo Koh, Eun Sook Kim, Jae Myung Yu, Eun-Gyoung Hong, Chang Beom Lee, Kun-Ho Yoon
Diabetes & Metabolism Journal.2023; 47(6): 808. CrossRef - Efficacy and Safety of Mulberry Twig Alkaloids Tablet for Treatment of Type 2 Diabetes: A Randomized, Double-Blind, Placebo-Controlled Multicenter Clinical Study
Ling Qu, Xiao-chun Liang, Guo-qing Tian, Gai-li Zhang, Qun-li Wu, Xiu-mei Huang, Ya-zhong Cui, Yu-ling Liu, Zhu-fang Shen, Guo-qing Ma, Hao Lu, Yi Li, Hong Jiang, Xi-yan Yang, Guang-de Zhang, Chen-hua Yang
Chinese Journal of Integrative Medicine.2022; 28(4): 304. CrossRef - Risk for Imbalanced Blood Glucose Pattern: Construct Analysis and Nursing Diagnosis Proposal
Rafael Oliveira Pitta Lopes, Jéssica de Castro Santos, Hudson Carmo de Oliveira, Juliana Faria Campos, Cândida Caniçali Primo, Camila Takáo Lopes, Marcos Antônio Gomes Brandão
Clinical Nursing Research.2022; 31(7): 1241. CrossRef - Long‐term clinical outcomes of oral antidiabetic drugs as fixed‐dose combinations: A nationwide retrospective cohort study
Sang‐Jun Cho, In‐Sun Oh, Han Eol Jeong, Young Min Cho, Yul Hwangbo, Oriana Hoi Yun Yu, Ju‐Young Shin
Diabetes, Obesity and Metabolism.2022; 24(10): 2051. CrossRef - Randomized Clinical Trial on Efficacy of Empagliflozin Versus Sitagliptin, In Addition to Metformin in Type 2 Diabetic Patients
Muaz Mubashir, Mazhar Ahmed, Hassan Atique, Ahmed Wassan, Mehdi Naqvi, Muneeb Ullah
Cureus.2022;[Epub] CrossRef - The Mediating Effect of Acceptance Action in the Relationship between Diabetes Distress and Self-stigma among Old Adults with Diabetes in South Korea
Hyesun Kim, Kawoun Seo
Journal of Korean Academy of Community Health Nursing.2022; 33(4): 446. CrossRef - Increasing Individual Target Glucose Levels to Prevent Hypoglycemia in Patients with Diabetes
Juyoung Shin, Hyunah Kim, Hun-Sung Kim, Churlmin Kim, Whan-Seok Choi
Korean Journal of Family Medicine.2021; 42(4): 269. CrossRef - Phase III, randomized, double‐blind, placebo‐controlled study to evaluate the efficacy and safety of teneligliptin monotherapy in Chinese patients with type 2 diabetes mellitus inadequately controlled with diet and exercise
Linong Ji, Jianhua Ma, Weiping Lu, Jingdong Liu, Jiao’e Zeng, Jialin Yang, Wei Li, Xiuzhen Zhang, Xinhua Xiao, Gen Takayanagi, Yi Wang
Journal of Diabetes Investigation.2021; 12(4): 537. CrossRef - Umbilical Cord-Mesenchymal Stem Cell-Conditioned Medium Improves Insulin Resistance in C2C12 Cell
Kyung-Soo Kim, Yeon Kyung Choi, Mi Jin Kim, Jung Wook Hwang, Kyunghoon Min, Sang Youn Jung, Soo-Kyung Kim, Yong-Soo Choi, Yong-Wook Cho
Diabetes & Metabolism Journal.2021; 45(2): 260. CrossRef - Blood glucose levels and bodyweight change after dapagliflozin administration
Hyunah Kim, Seung‐Hwan Lee, Hyunyong Lee, Hyeon Woo Yim, Jae‐Hyoung Cho, Kun‐Ho Yoon, Hun‐Sung Kim
Journal of Diabetes Investigation.2021; 12(9): 1594. CrossRef - Effects of liraglutide combined with metformin and Diamicron on glucose–lipid metabolism and islet β-cell function in elderly patients with type 2 diabetes mellitus
Chunzhi Zhao, Xing Li, Jianhua Ma, Zhengtai Zhu, Hua Li, Fangli Lou, Yuefang Zhai, Hui Chen, Shujun Xiao, Qinhui Peng, Huilian Hua, Qing Zhang, Fangyong Lou
All Life.2021; 14(1): 333. CrossRef - Efficacy and Safety of Mulberry Twig Alkaloids Tablet for the Treatment of Type 2 Diabetes: A Multicenter, Randomized, Double-Blind, Double-Dummy, and Parallel Controlled Clinical Trial
Ling Qu, Xiaochun Liang, Guoqing Tian, Gaili Zhang, Qunli Wu, Xiumei Huang, Yazhong Cui, Yuling Liu, Zhufang Shen, Changqing Xiao, Yingfen Qin, Heng Miao, Yongyan Zhang, Ziling Li, Shandong Ye, Xuezhi Zhang, Jing Yang, Guiwen Cao, Yi Li, Gangyi Yang, Ji H
Diabetes Care.2021; 44(6): 1324. CrossRef - Clinical Impact of Combination Therapy in Diabetic Neuropathy and Nephropathy
Harmeet Kaur, Arvinder Kaur, Pankaj Kumar Prashar, Anamika Gautam, Ankita Sood, Sachin Kumar Singh, Monica Gulati, Narendra Kumar Pandey, Bimlesh Kumar
Research Journal of Pharmacy and Technology.2021; : 3471. CrossRef - Effect of Voluntary Participation on Mobile Health Care in Diabetes Management: Randomized Controlled Open-Label Trial
Da Young Lee, Seung-Hyun Yoo, Kyong Pil Min, Cheol-Young Park
JMIR mHealth and uHealth.2020; 8(9): e19153. CrossRef - Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 382. CrossRef - Efficacy and Safety of Pioglitazone versus Glimepiride after Metformin and Alogliptin Combination Therapy: A Randomized, Open-Label, Multicenter, Parallel-Controlled Study
Jeong Mi Kim, Sang Soo Kim, Jong Ho Kim, Mi Kyung Kim, Tae Nyun Kim, Soon Hee Lee, Chang Won Lee, Ja Young Park, Eun Sook Kim, Kwang Jae Lee, Young Sik Choi, Duk Kyu Kim, In Joo Kim
Diabetes & Metabolism Journal.2020; 44(1): 67. CrossRef - Clinical Characteristics and Prevalence of Comorbidities according to Metformin Use in Korean Patients with Type 2 Diabetes
Sang Ouk Chin, In Gyoon Ha, Sang Youl Rhee, Su Jin Jeong, Suk Chon, Sung Hoon Kim, Kyu Jeung Ahn, Sei Hyun Baik, Yongsoo Park, Moon Suk Nam, Kwan Woo Lee, Jeong Taek Woo
International Journal of Endocrinology.2020; 2020: 1. CrossRef - Glucagon-Like Peptide-1 Receptor Agonist Differentially Affects Brain Activation in Response to Visual Food Cues in Lean and Obese Individuals with Type 2 Diabetes Mellitus
Jae Hyun Bae, Hyung Jin Choi, Kang Ik Kevin Cho, Lee Kyung Kim, Jun Soo Kwon, Young Min Cho
Diabetes & Metabolism Journal.2020; 44(2): 248. CrossRef Pharmacokinetic/Pharmacodynamic Interactions Between Evogliptin and Glimepiride in Healthy Male Subjects
Hyounggyoon Yoo, Yun Kim, In-Jin Jang, Kyung-Sang Yu, SeungHwan Lee
Drug Design, Development and Therapy.2020; Volume 14: 5179. CrossRef- Clinical parameters affecting the therapeutic efficacy of empagliflozin in patients with type 2 diabetes
Yun Kyung Cho, Jiwoo Lee, Yu Mi Kang, Jee Hee Yoo, Joong-Yeol Park, Chang Hee Jung, Woo Je Lee, Tatsuo Shimosawa
PLOS ONE.2019; 14(8): e0220667. CrossRef - Teneligliptin versus sitagliptin in Korean patients with type 2 diabetes inadequately controlled with metformin and glimepiride: A randomized, double‐blind, non‐inferiority trial
Yonghyun Kim, Eun Seok Kang, Hak Chul Jang, Dong Jun Kim, Taekeun Oh, Eun Sook Kim, Nan‐Hee Kim, Kyung Mook Choi, Sung‐Rae Kim, JiYoung You, Se‐Jin Kim, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2019; 21(3): 631. CrossRef - Pharmacotherapy of Diabetes Focused on Stroke
Young-Sang Lyu, Jin-Hwa Kim, Sang-Yong Kim
Journal of the Korean Neurological Association.2019; 37(3): 235. CrossRef - Letter: Efficacy and Safety of Voglibose Plus Metformin in Patients with Type 2 Diabetes Mellitus: A Randomized Controlled Trial (Diabetes Metab J 2019;43;276-86)
Hannah Seok, Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(4): 545. CrossRef - Nationwide Trends in Pancreatitis and Pancreatic Cancer Risk Among Patients With Newly Diagnosed Type 2 Diabetes Receiving Dipeptidyl Peptidase 4 Inhibitors
Minyoung Lee, Jiyu Sun, Minkyung Han, Yongin Cho, Ji-Yeon Lee, Chung Mo Nam, Eun Seok Kang
Diabetes Care.2019; 42(11): 2057. CrossRef - Efficacy and Safety of Voglibose Plus Metformin in Patients with Type 2 Diabetes Mellitus: A Randomized Controlled Trial
Tae Jung Oh, Jae Myung Yu, Kyung Wan Min, Hyun Shik Son, Moon Kyu Lee, Kun Ho Yoon, Young Duk Song, Joong Yeol Park, In Kyung Jeong, Bong Soo Cha, Yong Seong Kim, Sei Hyun Baik, In Joo Kim, Doo Man Kim, Sung Rae Kim, Kwan Woo Lee, Jeong Hyung Park, In Kyu
Diabetes & Metabolism Journal.2019; 43(3): 276. CrossRef - 2019 Clinical Practice Guidelines for Type 2 Diabetes Mellitus in Korea
Mee Kyoung Kim, Seung-Hyun Ko, Bo-Yeon Kim, Eun Seok Kang, Junghyun Noh, Soo-Kyung Kim, Seok-O Park, Kyu Yeon Hur, Suk Chon, Min Kyong Moon, Nan-Hee Kim, Sang Yong Kim, Sang Youl Rhee, Kang-Woo Lee, Jae Hyeon Kim, Eun-Jung Rhee, SungWan Chun, Sung Hoon Yu
Diabetes & Metabolism Journal.2019; 43(4): 398. CrossRef - Medical Big Data Is Not Yet Available: Why We Need Realism Rather than Exaggeration
Hun-Sung Kim, Dai-Jin Kim, Kun-Ho Yoon
Endocrinology and Metabolism.2019; 34(4): 349. CrossRef - Monotherapy in Type 2 Diabetes Mellitus Patients 2017: A Position Statement of the Korean Diabetes Association
Sang Youl Rhee
The Journal of Korean Diabetes.2018; 19(1): 15. CrossRef - Glucose Control in Intensive Care Unit Patients: Recent Updates
Sang Youl Rhee
Journal of Neurocritical Care.2018; 11(2): 81. CrossRef - Educational Strategies for Insulin Injection Therapy in Elderly Diabetic Patients
Eun Chong Shin
The Journal of Korean Diabetes.2018; 19(2): 101. CrossRef - Glucagon-Like Peptide-1 Receptor Agonists for the Treatment of Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association
Hyun Jin Kim
The Journal of Korean Diabetes.2018; 19(1): 35. CrossRef - Fifty Years of Compassionate Care and Harmonious Collaboration of the Korean Diabetes Association: The 50th Anniversary of Korean Diabetes Association
Jong Chul Won, Eun-Jung Rhee, Hyung Joon Yoo
Diabetes & Metabolism Journal.2018; 42(6): 475. CrossRef - Efficacy and safety of ipragliflozin as an add‐on therapy to sitagliptin and metformin in Korean patients with inadequately controlled type 2 diabetes mellitus: A randomized controlled trial
Kyung‐Ah Han, Suk Chon, Choon Hee Chung, Soo Lim, Kwan‐Woo Lee, SeiHyun Baik, Chang Hee Jung, Dong‐Sun Kim, Kyong Soo Park, Kun‐Ho Yoon, In‐Kyu Lee, Bong‐Soo Cha, Taishi Sakatani, Sumi Park, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2018; 20(10): 2408. CrossRef - Monotherapy in Patients with Type 2 Diabetes Mellitus
Sang Youl Rhee, Hyun Jin Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 349. CrossRef - Insulin therapy for adult patients with type 2 diabetes mellitus: a position statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
The Korean Journal of Internal Medicine.2017; 32(6): 967. CrossRef - New anti-diabetic agents
Doo-Man Kim
Journal of the Korean Medical Association.2017; 60(12): 992. CrossRef - Glucagon-Like Peptide-1 Receptor Agonists for the Treatment of Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association
Hyun Jin Kim, Seok O Park, Seung-Hyun Ko, Sang Youl Rhee, Kyu-Yeon Hur, Nan-Hee Kim, Min Kyong Moon, Byung-Wan Lee, Jin Hwa Kim, Kyung Mook Choi
Diabetes & Metabolism Journal.2017; 41(6): 423. CrossRef - Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2017; 41(5): 367. CrossRef
- Comparative Study on Efficacy of Empagliflozin Versus Sitagliptin, as an Add-on Therapy to Metformin in Type 2 Diabetic Patients
- Targeting the Peroxisome Proliferator-Activated Receptor-γ to Counter the Inflammatory Milieu in Obesity
- Cesar Corzo, Patrick R. Griffin
- Diabetes Metab J. 2013;37(6):395-403. Published online December 12, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.6.395
- 3,744 View
- 30 Download
- 34 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Adipose tissue, which was once viewed as a simple organ for storage of triglycerides, is now considered an important endocrine organ. Abnormal adipose tissue mass is associated with defects in endocrine and metabolic functions which are the underlying causes of the metabolic syndrome. Many adipokines, hormones secreted by adipose tissue, regulate cells from the immune system. Interestingly, most of these adipokines are proinflammatory mediators, which increase dramatically in the obese state and are believed to be involved in the pathogenesis of insulin resistance. Drugs that target peroxisome proliferator-activated receptor-γ have been shown to possess anti-inflammatory effects in animal models of diabetes. These findings, and the link between inflammation and the metabolic syndrome, will be reviewed here.
-
Citations
Citations to this article as recorded by- Lysine 222 in PPAR γ1 functions as the key site of MuRF2-mediated ubiquitination modification
Yucheng Fan, Fangjing Xu, Rui Wang, Jun He
Scientific Reports.2023;[Epub] CrossRef - Heart failure and diabetes: Clinical significance and epidemiology of this two‐way association
Terri Jerkins, Janet B. McGill, David S. H. Bell
Diabetes, Obesity and Metabolism.2023; 25(S3): 3. CrossRef - The pleiotropic peroxisome proliferator activated receptors: Regulation and therapeutics
Gargi Dixit, Arati Prabhu
Experimental and Molecular Pathology.2022; 124: 104723. CrossRef - The Effect of PPARγ rs1801282 Variant on Mortality Risk Among Asians With Chronic Kidney Disease: A Cohort Study and Meta-Analysis
Wei-Teing Chen, Chih-Chien Chiu, Dung-Jang Tsai, Pi-Shao Ko, Meng-Chang Lee, Hsiao-Ting Lin, Ying-Kai Chen, Wen Su, Yuh-Feng Lin, Sui-Lung Su
Frontiers in Genetics.2022;[Epub] CrossRef - Metabolic Spectrum of Liver Failure in Type 2 Diabetes and Obesity: From NAFLD to NASH to HCC
Hyunmi Kim, Da Som Lee, Tae Hyeon An, Hyun-Ju Park, Won Kon Kim, Kwang-Hee Bae, Kyoung-Jin Oh
International Journal of Molecular Sciences.2021; 22(9): 4495. CrossRef - Associations between obesity-related gene expression in maternal and cord blood and newborn adiposity: findings from the Araraquara Cohort study
P. Nakandakare, C. F. Nicoletti, N. Y. Noronha, C. B. Nonino, P. P. Argentato, N. N. Dejani, L. A. Luzia, M. M. Rogero, P. H. C. Rondó
International Journal of Obesity.2021; 45(9): 1958. CrossRef - PPARG Pro12Ala Polymorphism with CKD in Asians: A Meta-Analysis Combined with a Case-Control Study—A Key for Reaching Null Association
Hsiang-Cheng Chen, Wei-Teing Chen, Tzu-Ling Sung, Dung-Jang Tsai, Chin Lin, Hao Su, Yuh-Feng Lin, Hung-Yi Chiu, Sui-Lung Su
Genes.2020; 11(6): 705. CrossRef - Induction of peroxisome proliferator activated receptor γ (PPARγ) mediated gene expression and inhibition of induced nitric oxide production by Maerua subcordata (Gilg) DeWolf
Mebrahtom Gebrelibanos Hiben, Laura de Haan, Bert Spenkelink, Sebastiaan Wesseling, Jacques Vervoort, Ivonne M. C. M. Rietjens
BMC Complementary Medicine and Therapies.2020;[Epub] CrossRef - UPR modulation of host immunity by Pseudomonas aeruginosa in cystic fibrosis
Brahmchetna Bedi, Kuo-Chuan. Lin, Nicholas M. Maurice, Zhihong Yuan, Kaiser Bijli, Michael Koval, C. Michael Hart, Joanna B. Goldberg, Arlene Stecenko, Ruxana T. Sadikot
Clinical Science.2020; 134(14): 1911. CrossRef - Sepsis Immunometabolism: From Defining Sepsis to Understanding How Energy Production Affects Immune Response
Ioannis Koutroulis, Rachael Batabyal, Brittany McNamara, Matthew Ledda, Claire Hoptay, Robert J. Freishtat
Critical Care Explorations.2019; 1(11): e0061. CrossRef - Combining SGLT2 Inhibition With a Thiazolidinedione Additively Attenuate the Very Early Phase of Diabetic Nephropathy Progression in Type 2 Diabetes Mellitus
Eugene Han, Eugene Shin, Gyuri Kim, Ji-Yeon Lee, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha
Frontiers in Endocrinology.2018;[Epub] CrossRef - Role of oral hypoglycemic drugs on inflammatory condition associated with type 2 diabetes mellitus
Shamim Shaikh Mohiuddin
Journal of Diabetes, Metabolic Disorders & Control.2018; 5(2): 78. CrossRef - Effects of lobeglitazone on insulin resistance and hepatic steatosis in high-fat diet-fed mice
Bong-Hoi Choi, Zhen Jin, Chin-ok Yi, Juhong Oh, Eun Ae Jeong, Jong Youl Lee, Kyung-ah Park, Kyung Eun Kim, Jung Eun Lee, Hyun-Jin Kim, Jong Ryeal Hahm, Gu Seob Roh, Jonathan M Peterson
PLOS ONE.2018; 13(7): e0200336. CrossRef - Cucurbita ficifolia (Cucurbitaceae) modulates inflammatory cytokines and IFN-γ in obese mice
Á. Fortis-Barrera, R. García-Macedo, J.C. Almanza-Perez, G. Blancas-Flores, A. Zamilpa-Alvarez, J.L. Flores-Sáenz, M. Cruz, R. Román-Ramos, F.J. Alarcón-Aguilar
Canadian Journal of Physiology and Pharmacology.2017; 95(2): 170. CrossRef - Lobeglitazone, a Novel Thiazolidinedione, Improves Non-Alcoholic Fatty Liver Disease in Type 2 Diabetes: Its Efficacy and Predictive Factors Related to Responsiveness
Yong-ho Lee, Jae Hyeon Kim, So Ra Kim, Heung Yong Jin, Eun-Jung Rhee, Young Min Cho, Byung-Wan Lee
Journal of Korean Medical Science.2017; 32(1): 60. CrossRef -
Peroxisome proliferator‐activated receptor‐γ agonists attenuate biofilm formation by
Pseudomonas aeruginosa
Brahmchetna Bedi, Nicholas M. Maurice, Vincent T. Ciavatta, K. Sabrina Lynn, Zhihong Yuan, Samuel A. Molina, Myungsoo Joo, William R. Tyor, Joanna B. Goldberg, Michael Koval, C. Michael Hart, Ruxana T. Sadikot
The FASEB Journal.2017; 31(8): 3608. CrossRef - Pioglitazone and the secondary prevention of cardiovascular disease. A meta-analysis of randomized-controlled trials
Marit de Jong, H. Bart van der Worp, Yolanda van der Graaf, Frank L. J. Visseren, Jan Westerink
Cardiovascular Diabetology.2017;[Epub] CrossRef - Gestational diabetes mellitus was related to ambient air pollutant nitric oxide during early gestation
Shih-Chun Pan, Ching-Chun Huang, Shio-Jean Lin, Bing-Yu Chen, Chang-Chuan Chan, Yue-Liang Leon Guo
Environmental Research.2017; 158: 318. CrossRef - The Multifaceted Haptoglobin in the Context of Adipose Tissue and Metabolism
Margherita Maffei, Ilaria Barone, Gaia Scabia, Ferruccio Santini
Endocrine Reviews.2016; 37(4): 403. CrossRef - Enhanced Clearance of Pseudomonas aeruginosa by Peroxisome Proliferator-Activated Receptor Gamma
Brahmchetna Bedi, Zhihong Yuan, Myungsoo Joo, Susu M. Zughaier, Joanna B. Goldberg, Jack L. Arbiser, C. Michael Hart, Ruxana T. Sadikot, B. A. McCormick
Infection and Immunity.2016; 84(7): 1975. CrossRef - F-box only protein 9 is an E3 ubiquitin ligase of PPARγ
Kyeong Won Lee, Soo Heon Kwak, Young Do Koo, Yun-Kyung Cho, Hak Mo Lee, Hye Seung Jung, Young Min Cho, Young Joo Park, Sung Soo Chung, Kyong Soo Park
Experimental & Molecular Medicine.2016; 48(5): e234. CrossRef - The Resin fromProtium heptaphyllumPrevents High-Fat Diet-Induced Obesity in Mice: Scientific Evidence and Potential Mechanisms
Karine Maria Martins Bezerra Carvalho, José Delano Barreto Marinho Filho, Tiago Sousa de Melo, Ana Jérsia Araújo, Josiane da Silva Quetz, Maria do Perpétuo Socorro Saldanha da Cunha, Karina Moura de Melo, Armenio Andre de Carvalho Almeida da Silva, Adrian
Evidence-Based Complementary and Alternative Medicine.2015; 2015: 1. CrossRef - Lobeglitazone and pioglitazone as add‐ons to metformin for patients with type 2 diabetes: a 24‐week, multicentre, randomized, double‐blind, parallel‐group, active‐controlled, phase III clinical trial with a 28‐week extension
S.‐M. Jin, C.‐Y. Park, Y. M. Cho, B. J. Ku, C. W. Ahn, B.‐S. Cha, K. W. Min, Y. A. Sung, S. H. Baik, K. W. Lee, K.‐H. Yoon, M.‐K. Lee, S. W. Park
Diabetes, Obesity and Metabolism.2015; 17(6): 599. CrossRef - Deconvolution of Complex 1D NMR Spectra Using Objective Model Selection
Travis S. Hughes, Henry D. Wilson, Ian Mitchelle S. de Vera, Douglas J. Kojetin, Paul C. Driscoll
PLOS ONE.2015; 10(8): e0134474. CrossRef - PPARγ partial agonist GQ-16 strongly represses a subset of genes in 3T3-L1 adipocytes
Flora Aparecida Milton, Aleksandra Cvoro, Angelica A. Amato, Douglas H. Sieglaff, Carly S. Filgueira, Anithachristy Sigamani Arumanayagam, Maria do Carmo Alves de Lima, Ivan Rocha Pitta, Francisco de Assis Rocha Neves, Paul Webb
Biochemical and Biophysical Research Communications.2015; 464(3): 718. CrossRef - Voluntary exercise prevents colonic inflammation in high-fat diet-induced obese mice by up-regulating PPAR-γ activity
Wei-Xin Liu, Ting Wang, Feng Zhou, Ying Wang, Jun-Wei Xing, Shen Zhang, Shou-Zhi Gu, Li-Xuan Sang, Cong Dai, Hai-Lan Wang
Biochemical and Biophysical Research Communications.2015; 459(3): 475. CrossRef - Effect of a new PPAR-gamma agonist, lobeglitazone, on neointimal formation after balloon injury in rats and the development of atherosclerosis
Soo Lim, Kuy-Sook Lee, Jie Eun Lee, Ho Seon Park, Kyoung Min Kim, Jae Hoon Moon, Sung Hee Choi, Kyong Soo Park, Young Bum Kim, Hak Chul Jang
Atherosclerosis.2015; 243(1): 107. CrossRef - Antidiabetic agents: Potential anti-inflammatory activity beyond glucose control
A.J. Scheen, N. Esser, N. Paquot
Diabetes & Metabolism.2015; 41(3): 183. CrossRef - Genomic binding and regulation of gene expression by the thyroid carcinoma-associated PAX8-PPARG fusion protein
Yanxiao Zhang, Jingcheng Yu, Chee Lee, Bin Xu, Maureen A. Sartor, Ronald J. Koenig
Oncotarget.2015; 6(38): 40418. CrossRef - Peroxisome Proliferator-Activated Receptor γ (PPARγ) and Ligand Choreography: Newcomers Take the Stage
Santiago Garcia-Vallvé, Laura Guasch, Sarah Tomas-Hernández, Josep Maria del Bas, Vincent Ollendorff, Lluís Arola, Gerard Pujadas, Miquel Mulero
Journal of Medicinal Chemistry.2015; 58(14): 5381. CrossRef - Pathway Analysis of Metabolic Syndrome Using a Genome-Wide Association Study of Korea Associated Resource (KARE) Cohorts
Unjin Shim, Han-Na Kim, Yeon-Ah Sung, Hyung-Lae Kim
Genomics & Informatics.2014; 12(4): 195. CrossRef - Pax-8–PPAR-γ fusion protein in thyroid carcinoma
Priyadarshini Raman, Ronald J. Koenig
Nature Reviews Endocrinology.2014; 10(10): 616. CrossRef - Insulin therapy and colorectal cancer risk among type 2 diabetes mellitus patients: a systemic review and meta-analysis
Shinan Yin, Hua Bai, Danqing Jing
Diagnostic Pathology.2014;[Epub] CrossRef - Common biological mechanisms between bipolar disorder and type 2 diabetes: Focus on inflammation
Ajaykumar N. Sharma, Isabelle E. Bauer, Marsal Sanches, Juan F. Galvez, Giovana B. Zunta-Soares, Joao Quevedo, Flavio Kapczinski, Jair C. Soares
Progress in Neuro-Psychopharmacology and Biological Psychiatry.2014; 54: 289. CrossRef
- Lysine 222 in PPAR γ1 functions as the key site of MuRF2-mediated ubiquitination modification

 KDA
KDA
 First
First Prev
Prev





