
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Basic Research
- Hyperglycemia-Suppressed SMARCA5 Disrupts Transcriptional Homeostasis to Facilitate Endothelial Dysfunction in Diabetes
- Ju Wang, Hui Zhou, Jinhua Shao, Shu Zhang, Jing Jin
- Diabetes Metab J. 2023;47(3):366-381. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0179
- 1,704 View
- 98 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
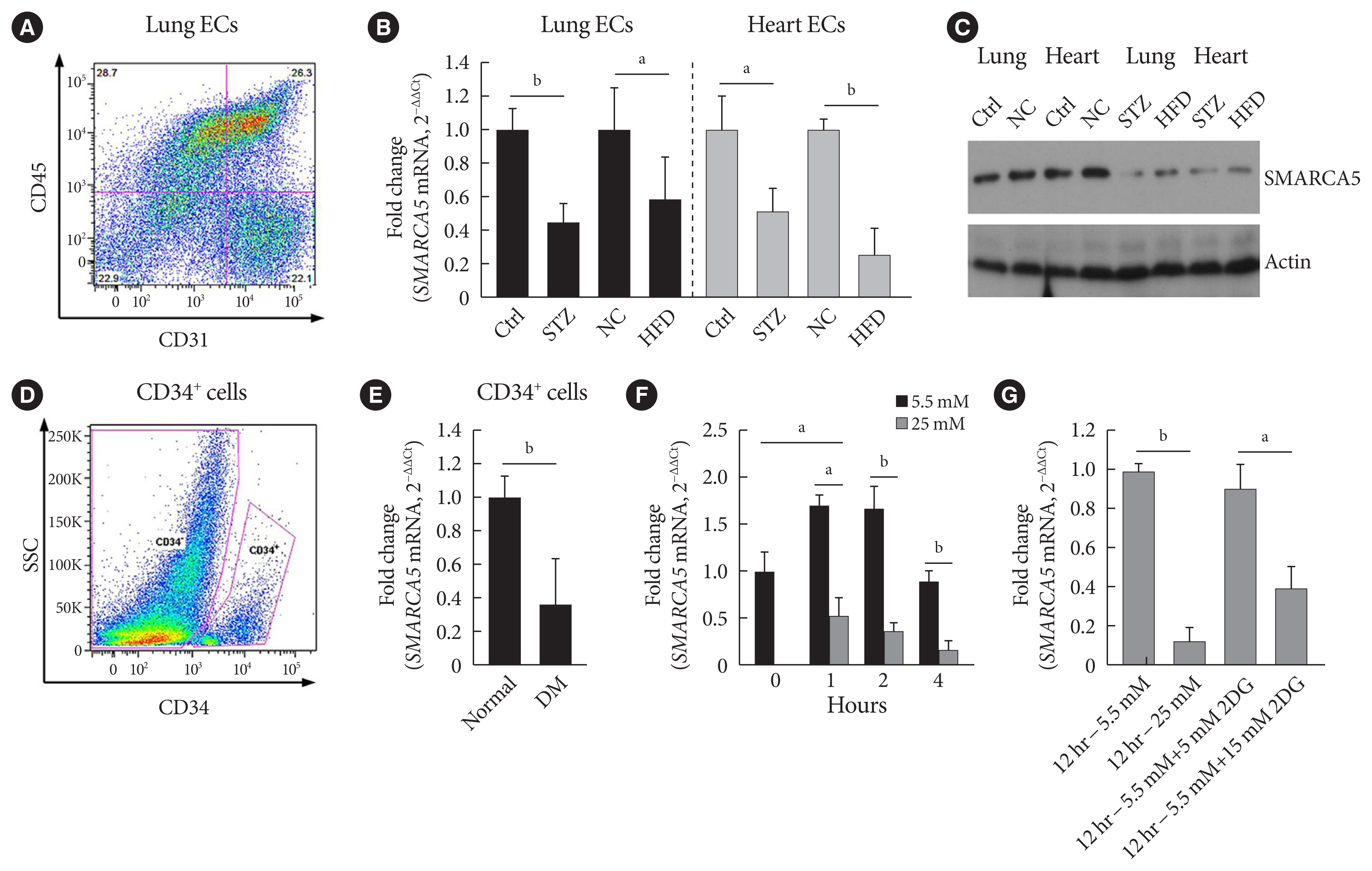
Dysfunction of vascular endothelial cells (ECs) plays a central role in the pathogenesis of cardiovascular complications in diabetes. SWI/SNF-related matrix-associated actin-dependent regulator of chromatin subfamily A member 5 (SMARCA5) is a key regulator of chromatin structure and DNA repair, but its role in ECs remains surprisingly unexplored. The current study was designed to elucidate the regulated expression and function of SMARCA5 in diabetic ECs.
Methods
SMARCA5 expression was evaluated in ECs from diabetic mouse and human circulating CD34+ cells using quantitative reverse transcription polymerase chain reaction and Western blot. Effects of SMARCA5 manipulation on ECs function were evaluated using cell migration, in vitro tube formation and in vivo wound healing assays. Interaction among oxidative stress, SMARCA5 and transcriptional reprogramming was elucidated using luciferase reporter assay, electrophoretic mobility shift assay and chromatin immunoprecipitation.
Results
Endothelial SMARCA5 expression was significantly decreased in diabetic rodents and humans. Hyperglycemia-suppressed SMARCA5 impaired EC migration and tube formation in vitro, and blunted vasculogenesis in vivo. Contrarily, overexpression of SMARCA5 in situ by a SMARCA5 adenovirus-incorporated hydrogel effectively promoted the rate of wound healing in a dorsal skin punch injury model of diabetic mice. Mechanistically, hyperglycemia-elicited oxidative stress suppressed SMARCA5 transactivation in a signal transducer and activator of transcription 3 (STAT3)-dependent manner. Moreover, SMARCA5 maintained transcriptional homeostasis of several pro-angiogenic factors through both direct and indirect chromatin-remodeling mechanisms. In contrast, depletion of SMARCA5 disrupted transcriptional homeostasis to render ECs unresponsive to established angiogenic factors, which ultimately resulted in endothelial dysfunction in diabetes.
Conclusion
Suppression of endothelial SMARCA5 contributes to, at least in part, multiple aspects of endothelial dysfunction, which may thereby exacerbate cardiovascular complications in diabetes.
- Pathophysiology
- Glial and Vascular Cell Regulation of the Blood-Brain Barrier in Diabetes
- Xiaolong Li, Yan Cai, Zuo Zhang, Jiyin Zhou
- Diabetes Metab J. 2022;46(2):222-238. Published online March 18, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0146
- 6,264 View
- 298 Download
- 12 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - As a structural barrier, the blood-brain barrier (BBB) is located at the interface between the brain parenchyma and blood, and modulates communication between the brain and blood microenvironment to maintain homeostasis. The BBB is composed of endothelial cells, basement membrane, pericytes, and astrocytic end feet. BBB impairment is a distinguishing and pathogenic factor in diabetic encephalopathy. Diabetes causes leakage of the BBB through downregulation of tight junction proteins, resulting in impaired functioning of endothelial cells, pericytes, astrocytes, microglia, nerve/glial antigen 2-glia, and oligodendrocytes. However, the temporal regulation, mechanisms of molecular and signaling pathways, and consequences of BBB impairment in diabetes are not well understood. Consequently, the efficacy of therapies diabetes targeting BBB leakage still lags behind the requirements. This review summarizes the recent research on the effects of diabetes on BBB composition and the potential roles of glial and vascular cells as therapeutic targets for BBB disruption in diabetic encephalopathy.
-
Citations
Citations to this article as recorded by- Gut microbiota and type 2 diabetes mellitus: a focus on the gut-brain axis
Yi Pan, Tong Bu, Xia Deng, Jue Jia, Guoyue Yuan
Endocrine.2024; 84(1): 1. CrossRef - Long-Term Exposure of Cultured Astrocytes to High Glucose Impact on Their LPS-Induced Activation
Ayna Abdyeva, Ekaterina Kurtova, Irina Savinkova, Maksim Galkov, Liubov Gorbacheva
International Journal of Molecular Sciences.2024; 25(2): 1122. CrossRef - Role of autophagy in angiogenic potential of vascular pericytes
Soheil Zamen Milani, Aysa Rezabakhsh, Mohammad Karimipour, Leila Salimi, Narges Mardi, Maryam Taghavi Narmi, Fatemeh Sadeghsoltani, Ferzane Valioglu, Reza Rahbarghazi
Frontiers in Cell and Developmental Biology.2024;[Epub] CrossRef - The NG2-glia is a potential target to maintain the integrity of neurovascular unit after acute ischemic stroke
Xiaoyan Hu, Panpan Geng, Xiaoyun Zhao, Qian Wang, Changqing Liu, Chun Guo, Wen Dong, Xinchun Jin
Neurobiology of Disease.2023; 180: 106076. CrossRef - Tight junction disruption and the pathogenesis of the chronic complications of diabetes mellitus: A narrative review
Ma Ludivina Robles-Osorio, Ernesto Sabath
World Journal of Diabetes.2023; 14(7): 1013. CrossRef - Function and therapeutic value of astrocytes in diabetic cognitive impairment
Fanyu Meng, Jiafeng Fu, Lin Zhang, Mengqing Guo, Pengwei Zhuang, Qingsheng Yin, Yanjun Zhang
Neurochemistry International.2023; 169: 105591. CrossRef - Exploring the molecular targets for Type 2 diabetes-induced Alzheimer’s disease through bioinformatics analysis
Lin Gao, Chengyu Huang, Hui Li, Shidi Wu, Xiaoyan Zhou, Changjiang Ying
Epigenomics.2023; 15(11): 619. CrossRef - In vivo retinal imaging is associated with cognitive decline, blood-brain barrier disruption and neuroinflammation in type 2 diabetic mice
May Majimbi, Samuel McLenachan, Michael Nesbit, Fred K. Chen, Virginie Lam, John Mamo, Ryu Takechi
Frontiers in Endocrinology.2023;[Epub] CrossRef - Diabetic microvascular disease in non-classical beds: the hidden impact beyond the retina, the kidney, and the peripheral nerves
Dídac Mauricio, Mònica Gratacòs, Josep Franch-Nadal
Cardiovascular Diabetology.2023;[Epub] CrossRef - Transcranial photobiomodulation improves insulin therapy in diabetic microglial reactivity and the brain drainage system
Shaojun Liu, Dongyu Li, Tingting Yu, Jingtan Zhu, Oxana Semyachkina-Glushkovskaya, Dan Zhu
Communications Biology.2023;[Epub] CrossRef - NG2‐glia crosstalk with microglia in health and disease
Zuo Zhang, Xiaolong Li, Hongli Zhou, Jiyin Zhou
CNS Neuroscience & Therapeutics.2022; 28(11): 1663. CrossRef - Accelerated amyloid angiopathy and related vascular alterations in a mixed murine model of Alzheimer´s disease and type two diabetes
Maria Vargas-Soria, Juan Jose Ramos-Rodriguez, Angel del Marco, Carmen Hierro-Bujalance, Maria Jose Carranza-Naval, Maria Calvo-Rodriguez, Susanne J. van Veluw, Alan W. Stitt, Rafael Simó, Brian J. Bacskai, Carmen Infante-Garcia, Monica Garcia-Alloza
Fluids and Barriers of the CNS.2022;[Epub] CrossRef
- Gut microbiota and type 2 diabetes mellitus: a focus on the gut-brain axis
- Basic Research
- GPR40 Agonism Modulates Inflammatory Reactions in Vascular Endothelial Cells
- Joo Won Kim, Eun Roh, Kyung Mook Choi, Hye Jin Yoo, Hwan-Jin Hwang, Sei Hyun Baik
- Diabetes Metab J. 2022;46(3):506-511. Published online January 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0092
- 4,763 View
- 229 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
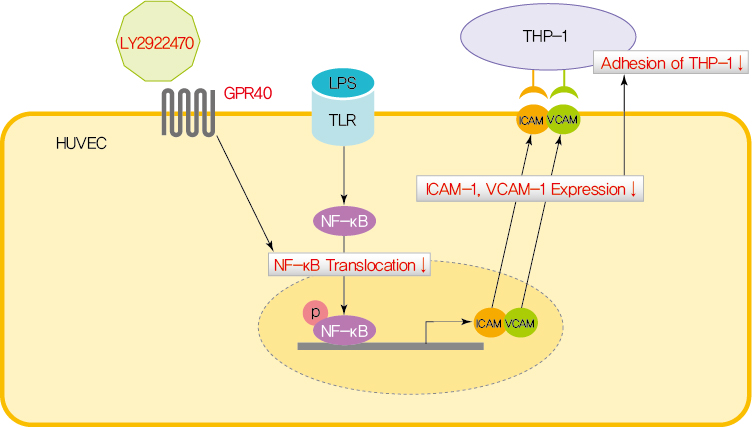
ePub - Endothelial dysfunction is strongly linked with inflammatory responses, which can impact cardiovascular disease. Recently, G protein-coupled receptor 40 (GPR40) has been investigated as a modulator of metabolic stress; however, the function of GPR40 in vascular endothelial cells has not been reported. We analyzed whether treatment of GPR40-specific agonists modulated the inflammatory responses in human umbilical vein endothelial cells (HUVECs). Treatment with LY2922470, a GPR40 agonist, significantly reduced lipopolysaccharide (LPS)-mediated nuclear factor-kappa B (NF-κB) phosphorylation and movement into the nucleus from the cytosol. However, treatment with another GPR40 agonist, TAK875, did not inhibit LPS-induced NF-κB activation. LPS treatment induced expression of adhesion molecules vascular cell adhesion molecule-1 (VCAM-1) and intercellular adhesion molecule-1 (ICAM-1) and attachment of THP-1 cells to HUVECs, which were all decreased by LY2922470 but not TAK875. Our results showed that ligand-dependent agonism of GPR40 is a promising therapeutic target for overcoming inflammatory reactions in the endothelium.
-
Citations
Citations to this article as recorded by- Synthetic GPR40/FFAR1 agonists: An exhaustive survey on the most recent chemical classes and their structure-activity relationships
Abhik Paul, Sourin Nahar, Pankaj Nahata, Arnab Sarkar, Avik Maji, Ajeya Samanta, Sanmoy Karmakar, Tapan Kumar Maity
European Journal of Medicinal Chemistry.2024; 264: 115990. CrossRef - Metabolite-sensing GPCRs in rheumatoid arthritis
Xuezhi Yang, Wankang Zhang, Luping Wang, Yingjie Zhao, Wei Wei
Trends in Pharmacological Sciences.2024; 45(2): 118. CrossRef - GPR40 deficiency worsens metabolic syndrome‐associated periodontitis in mice
Yanchun Li, Zhongyang Lu, Cameron L. Kirkwood, Keith L. Kirkwood, Stephen A. Wank, Ai‐Jun Li, Maria F. Lopes‐Virella, Yan Huang
Journal of Periodontal Research.2023; 58(3): 575. CrossRef - Signaling pathways and intervention for therapy of type 2 diabetes mellitus
Rong Cao, Huimin Tian, Yu Zhang, Geng Liu, Haixia Xu, Guocheng Rao, Yan Tian, Xianghui Fu
MedComm.2023;[Epub] CrossRef - G Protein-Coupled Receptor 40 Agonist LY2922470 Alleviates Ischemic-Stroke-Induced Acute Brain Injury and Functional Alterations in Mice
Yingyu Lu, Wanlu Zhou, Qinghua Cui, Chunmei Cui
International Journal of Molecular Sciences.2023; 24(15): 12244. CrossRef - AM1638, a GPR40-Full Agonist, Inhibited Palmitate- Induced ROS Production and Endoplasmic Reticulum Stress, Enhancing HUVEC Viability in an NRF2-Dependent Manner
Hwan-Jin Hwang, Joo Won Kim, SukHwan Yun, Min Jeong Park, Eyun Song, Sooyeon Jang, Ahreum Jang, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Endocrinology and Metabolism.2023; 38(6): 760. CrossRef - Learn from failures and stay hopeful to GPR40, a GPCR target with robust efficacy, for therapy of metabolic disorders
Hong-Ping Guan, Yusheng Xiong
Frontiers in Pharmacology.2022;[Epub] CrossRef
- Synthetic GPR40/FFAR1 agonists: An exhaustive survey on the most recent chemical classes and their structure-activity relationships
- Complications
- Pathophysiology of Diabetic Retinopathy: The Old and the New
- Sentaro Kusuhara, Yoko Fukushima, Shuntaro Ogura, Naomi Inoue, Akiyoshi Uemura
- Diabetes Metab J. 2018;42(5):364-376. Published online October 22, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0182
- 13,647 View
- 473 Download
- 114 Web of Science
- 108 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Vision loss in diabetic retinopathy (DR) is ascribed primarily to retinal vascular abnormalities—including hyperpermeability, hypoperfusion, and neoangiogenesis—that eventually lead to anatomical and functional alterations in retinal neurons and glial cells. Recent advances in retinal imaging systems using optical coherence tomography technologies and pharmacological treatments using anti-vascular endothelial growth factor drugs and corticosteroids have revolutionized the clinical management of DR. However, the cellular and molecular mechanisms underlying the pathophysiology of DR are not fully determined, largely because hyperglycemic animal models only reproduce limited aspects of subclinical and early DR. Conversely, non-diabetic mouse models that represent the hallmark vascular disorders in DR, such as pericyte deficiency and retinal ischemia, have provided clues toward an understanding of the sequential events that are responsible for vision-impairing conditions. In this review, we summarize the clinical manifestations and treatment modalities of DR, discuss current and emerging concepts with regard to the pathophysiology of DR, and introduce perspectives on the development of new drugs, emphasizing the breakdown of the blood-retina barrier and retinal neovascularization.
-
Citations
Citations to this article as recorded by- Recent Insights into the Etiopathogenesis of Diabetic Retinopathy and Its Management
Arpon Biswas, Abhijit Deb Choudhury, Sristi Agrawal, Amol Chhatrapati Bisen, Sachin Nashik Sanap, Sarvesh Kumar Verma, Mukesh Kumar, Anjali Mishra, Shivansh Kumar, Mridula Chauhan, Rabi Sankar Bhatta
Journal of Ocular Pharmacology and Therapeutics.2024; 40(1): 13. CrossRef - GMFB/AKT/TGF‐β3 in Müller cells mediated early retinal degeneration in a streptozotocin‐induced rat diabetes model
Tong Zhu, Yingao Li, Lilin Zhu, Jinyuan Xu, Zijun Feng, Hao Chen, Si Shi, Caiying Liu, Qingjian Ou, Furong Gao, Jieping Zhang, Caixia Jin, Jingying Xu, Jiao Li, Jingfa Zhang, Yanlong Bi, Guo‐tong Xu, Juan Wang, Haibin Tian, Lixia Lu
Glia.2024; 72(3): 504. CrossRef - The significance of glutaredoxins for diabetes mellitus and its complications
Mengmeng Zhou, Eva-Maria Hanschmann, Axel Römer, Thomas Linn, Sebastian Friedrich Petry
Redox Biology.2024; 71: 103043. CrossRef - Proteomic analysis of diabetic retinopathy identifies potential plasma-protein biomarkers for diagnosis and prognosis
Bent Honoré, Javad Nouri Hajari, Tobias Torp Pedersen, Tomas Ilginis, Hajer Ahmad Al-Abaiji, Claes Sepstrup Lønkvist, Jon Peiter Saunte, Dorte Aalund Olsen, Ivan Brandslund, Henrik Vorum, Carina Slidsborg
Clinical Chemistry and Laboratory Medicine (CCLM).2024;[Epub] CrossRef - Next generation therapeutics for retinal neurodegenerative diseases
Matthew B. Appell, Jahnavi Pejavar, Ashwin Pasupathy, Sri Vishnu Kiran Rompicharla, Saed Abbasi, Kiersten Malmberg, Patricia Kolodziejski, Laura M. Ensign
Journal of Controlled Release.2024; 367: 708. CrossRef - Modeling early pathophysiological phenotypes of diabetic retinopathy in a human inner blood-retinal barrier-on-a-chip
Thomas L. Maurissen, Alena J. Spielmann, Gabriella Schellenberg, Marc Bickle, Jose Ricardo Vieira, Si Ying Lai, Georgios Pavlou, Sascha Fauser, Peter D. Westenskow, Roger D. Kamm, Héloïse Ragelle
Nature Communications.2024;[Epub] CrossRef - Emerging role of ferroptosis in diabetic retinopathy: a review
Ruohong Wang, Suyun Rao, Zheng Zhong, Ke Xiao, Xuhui Chen, Xufang Sun
Journal of Drug Targeting.2024; 32(4): 393. CrossRef - Serum vitamin D is substantially reduced and predicts flares in diabetic retinopathy patients
Yong Zhuang, Zihao Zhuang, Qingyan Cai, Xin Hu, Huibin Huang
Journal of Diabetes Investigation.2024;[Epub] CrossRef - Ocular pharmacological and biochemical profiles of 6-thioguanine: a drug repurposing study
Maria Consiglia Trotta, Carlo Gesualdo, Caterina Claudia Lepre, Marina Russo, Franca Ferraraccio, Iacopo Panarese, Ernesto Marano, Paolo Grieco, Francesco Petrillo, Anca Hermenean, Francesca Simonelli, Michele D’Amico, Claudio Bucolo, Francesca Lazzara, F
Frontiers in Pharmacology.2024;[Epub] CrossRef - Pharmacological mechanism and clinical study of Qiming granules in treating diabetic retinopathy based on network pharmacology and literature review
Yuxia Huang, Jia Wang, Yu Wang, Wei Kuang, Mengjun Xie, Mei Zhang
Journal of Ethnopharmacology.2023; 302: 115861. CrossRef - Vitreous humor proteome: unraveling the molecular mechanisms underlying proliferative and neovascular vitreoretinal diseases
Fátima Milhano dos Santos, Sergio Ciordia, Joana Mesquita, João Paulo Castro de Sousa, Alberto Paradela, Cândida Teixeira Tomaz, Luís António Paulino Passarinha
Cellular and Molecular Life Sciences.2023;[Epub] CrossRef - Protective Effects of Human Pericyte-like Adipose-Derived Mesenchymal Stem Cells on Human Retinal Endothelial Cells in an In Vitro Model of Diabetic Retinopathy: Evidence for Autologous Cell Therapy
Gabriella Lupo, Aleksandra Agafonova, Alessia Cosentino, Giovanni Giurdanella, Giuliana Mannino, Debora Lo Furno, Ivana Roberta Romano, Rosario Giuffrida, Floriana D’Angeli, Carmelina Daniela Anfuso
International Journal of Molecular Sciences.2023; 24(2): 913. CrossRef - Predictive factors for microvascular recovery after treatments for diabetic retinopathy
Junyeop Lee, Yoon-Jeon Kim, Joo-Yong Lee, Young Hee Yoon, June-Gone Kim
BMC Ophthalmology.2023;[Epub] CrossRef - Pathophysiology and diagnosis of diabetic retinopathy: a narrative review
Mohadese Estaji, Bita Hosseini, Saeed Bozorg-Qomi, Babak Ebrahimi
Journal of Investigative Medicine.2023; 71(3): 265. CrossRef - Proteomics profiling of vitreous humor reveals complement and coagulation components, adhesion factors, and neurodegeneration markers as discriminatory biomarkers of vitreoretinal eye diseases
Fátima M. Santos, Sergio Ciordia, Joana Mesquita, Carla Cruz, João Paulo Castro e Sousa, Luís A. Passarinha, Cândida T. Tomaz, Alberto Paradela
Frontiers in Immunology.2023;[Epub] CrossRef - Hypoxia-induced transcriptional differences in African and Asian versus European diabetic cybrids
Andrew H. Dolinko, Marilyn Chwa, Kevin Schneider, Mithalesh K. Singh, Shari Atilano, Jie Wu, M. Cristina Kenney
Scientific Reports.2023;[Epub] CrossRef - Downregulation of plasma microRNA-29c-3p expression may be a new risk factor for diabetic retinopathy
Bora TORUS, Hakan KORKMAZ, Kuyaş H. OZTURK, Fevziye B. ŞİRİN, Mehmet ARGUN, Sonmez ŞEVİK, Levent TÖK
Minerva Endocrinology.2023;[Epub] CrossRef - Short-Term Outcomes of Intravitreal Faricimab Injection for Diabetic Macular Edema
Sentaro Kusuhara, Maya Kishimoto-Kishi, Wataru Matsumiya, Akiko Miki, Hisanori Imai, Makoto Nakamura
Medicina.2023; 59(4): 665. CrossRef - L-type calcium channel blocker increases VEGF concentrations in retinal cells and human serum
Anmol Kumar, Stefan Mutter, Erika B. Parente, Valma Harjutsalo, Raija Lithovius, Sinnakaruppan Mathavan, Markku Lehto, Timo P. Hiltunen, Kimmo K. Kontula, Per-Henrik Groop, Satyajit Mohapatra
PLOS ONE.2023; 18(4): e0284364. CrossRef - Efficacy and safety of curcumin in diabetic retinopathy: A protocol for systematic review and meta-analysis
Liyuan Wang, Jiayu Xu, Tianyang Yu, Hanli Wang, Xiaojun Cai, He Sun, Godwin Ovenseri-Ogbomo
PLOS ONE.2023; 18(4): e0282866. CrossRef - Highly water-soluble diacetyl chrysin ameliorates diabetes-associated renal fibrosis and retinal microvascular abnormality in db/db mice
Young-Hee Kang, Sin-Hye Park, Young Eun Sim, Moon-Sik Oh, Hong Won Suh, Jae-Yong Lee, Soon Sung Lim
Nutrition Research and Practice.2023; 17(3): 421. CrossRef - Preventive and management approach of triptonide, a diterpenoid compound against streptozotocin-induced diabetic retinopathy in Wistar rat model
Chandramohan Govindasamy, Khalid S. Al-Numair, Jun Li, Weibai Chen, Guoqiang Wu
Arabian Journal of Chemistry.2023; 16(9): 105034. CrossRef - New Insights on Dietary Polyphenols for the Management of Oxidative Stress and Neuroinflammation in Diabetic Retinopathy
Gustavo Bernardes Fanaro, Marcelo Rodrigues Marques, Karin da Costa Calaza, Rafael Brito, André Moreira Pessoni, Henrique Rocha Mendonça, Deborah Emanuelle de Albuquerque Lemos, José Luiz de Brito Alves, Evandro Leite de Souza, Marinaldo Pacífico Cavalcan
Antioxidants.2023; 12(6): 1237. CrossRef - Evaluation of Social Platform-Based Continuity of Care in Improving Cognitive and Prognostic Effects of Young Patients with Diabetic Retinopathy
Guo-lan Cao, Ke-jian Chen
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 1931. CrossRef - Role of vascular endothelial growth factor B in nonalcoholic fatty liver disease and its potential value
Yu-Qi Li, Lei Xin, Yu-Chi Zhao, Shang-Qi Li, Ya-Nuo Li
World Journal of Hepatology.2023; 15(6): 786. CrossRef - The rs1800469 T/T and rs1800470 C/C genotypes of the TGFB1 gene confer protection against diabetic retinopathy in a Southern Brazilian population
Aline Rodrigues Costa, Cristine Dieter, Luís Henrique Canani, Taís Silveira Assmann, Daisy Crispim
Genetics and Molecular Biology.2023;[Epub] CrossRef - Evaluation of Self-Care in Patients with Diabetic Retinopathy
Songül BİLTEKİN, Züleyha KILIÇ, Şefika Dilek GÜVEN
Turkish Journal of Diabetes and Obesity.2023; 7(3): 214. CrossRef - Diabetes mellitus and its influence on the incidence and process of diabetic retinopathy
Janka Poráčová, Melinda Nagy, Marta Mydlárová Blaščáková, Mária Konečná, Vincent Sedlák, Mária Zahatňanská, Tatiana Kimáková, Hedviga Vašková, Viktória Rybárová, Mária Majherová, Ivan Uher
Central European Journal of Public Health.2023; 31(Suppl 1): S4. CrossRef - Dysregulation of the NLRP3 Inflammasome in Diabetic Retinopathy and Potential Therapeutic Targets
Karanvir S. Raman, Joanne A. Matsubara
Ocular Immunology and Inflammation.2022; 30(2): 470. CrossRef - Adult-induced genetic ablation distinguishes PDGFB roles in blood-brain barrier maintenance and development
Elisa Vazquez-Liebanas, Khayrun Nahar, Giacomo Bertuzzi, Annika Keller, Christer Betsholtz, Maarja Andaloussi Mäe
Journal of Cerebral Blood Flow & Metabolism.2022; 42(2): 264. CrossRef - Investigation on the Q-markers of Bushen Huoxue Prescriptions for DR treatment based on chemometric methods and spectrum-effect relationship
Yueting Yu, Ziyu Zhu, Mengjun Xie, Liping Deng, Xuejun Xie, Mei Zhang
Journal of Ethnopharmacology.2022; 285: 114800. CrossRef - Corneal Confocal Microscopy in Type 1 Diabetes Mellitus: A Six-Year Longitudinal Study
Stuti L. Misra, James A. Slater, Charles N. J. McGhee, Monika Pradhan, Geoffrey D. Braatvedt
Translational Vision Science & Technology.2022; 11(1): 17. CrossRef - Microphysiological Neurovascular Barriers to Model the Inner Retinal Microvasculature
Thomas L. Maurissen, Georgios Pavlou, Colette Bichsel, Roberto Villaseñor, Roger D. Kamm, Héloïse Ragelle
Journal of Personalized Medicine.2022; 12(2): 148. CrossRef - Long-Term Oral Administration of Salidroside Alleviates Diabetic Retinopathy in db/db Mice
Fei Yao, Xinyi Jiang, Ling Qiu, Zixuan Peng, Wei Zheng, Lexi Ding, Xiaobo Xia
Frontiers in Endocrinology.2022;[Epub] CrossRef - Classification of macular abnormalities using a lightweight CNN-SVM framework
Xuqian Wang, Yu Gu
Measurement Science and Technology.2022; 33(6): 065702. CrossRef - Chorioretinal Hypoxia Detection Using Lipid-Polymer Hybrid Organic Room-Temperature Phosphorescent Nanoparticles
Yingying Zeng, Van Phuc Nguyen, Yanxiu Li, Do Hyun Kang, Yannis M. Paulus, Jinsang Kim
ACS Applied Materials & Interfaces.2022; 14(16): 18182. CrossRef - LncRNA FLG-AS1 Mitigates Diabetic Retinopathy by Regulating Retinal Epithelial Cell Inflammation, Oxidative Stress, and Apoptosis via miR-380-3p/SOCS6 Axis
Rong Luo, Lan Li, Fan Xiao, Jinsong Fu
Inflammation.2022; 45(5): 1936. CrossRef - Correlation between the progression of diabetic retinopathy and inflammasome biomarkers in vitreous and serum – a systematic review
Charisse Y. J. Kuo, Rinki Murphy, Ilva D. Rupenthal, Odunayo O. Mugisho
BMC Ophthalmology.2022;[Epub] CrossRef - The relationship between the neutrophil-to-lymphocyte ratio and diabetic retinopathy in adults from the United States: results from the National Health and nutrition examination survey
Xiaojie He, Shanshan Qi, Xi Zhang, Jiandong Pan
BMC Ophthalmology.2022;[Epub] CrossRef - Th22 cells induce Müller cell activation via the Act1/TRAF6 pathway in diabetic retinopathy
Yufei Wang, Hongdan Yu, Jing Li, Wenqiang Liu, Shengxue Yu, Pan Lv, Lipan Zhao, Xiaobai Wang, Zhongfu Zuo, Xuezheng Liu
Cell and Tissue Research.2022; 390(3): 367. CrossRef - Prevalence and Factors Associated with Diabetic Retinopathy among Adult Diabetes Patients in Southeast Ethiopia: A Hospital-Based Cross-Sectional Study
Biniyam Sahiledengle, Tesfaye Assefa, Wogene Negash, Anwar Tahir, Tadele Regasa, Yohannes Tekalegn, Ayele Mamo, Zinash Teferu, Damtew Solomon, Habtamu Gezahegn, Kebebe Bekele, Demisu Zenbaba, Alelign Tasew, Fikreab Desta, Zegeye Regassa, Zegeye Feleke, Ch
Clinical Ophthalmology.2022; Volume 16: 3527. CrossRef - Diabetic Retinopathy: Are lncRNAs New Molecular Players and Targets?
Simona Cataldi, Mariagiovanna Tramontano, Valerio Costa, Marianna Aprile, Alfredo Ciccodicola
Antioxidants.2022; 11(10): 2021. CrossRef - Diosgenin protects retinal pigment epithelial cells from inflammatory damage and oxidative stress induced by high glucose by activating AMPK/Nrf2/HO‐1 pathway
Yang Hao, Xuefeng Gao
Immunity, Inflammation and Disease.2022;[Epub] CrossRef - Selective Activation of the Wnt-Signaling Pathway as a Novel Therapy for the Treatment of Diabetic Retinopathy and Other Retinal Vascular Diseases
Huy Nguyen, Sung-Jin Lee, Yang Li
Pharmaceutics.2022; 14(11): 2476. CrossRef - Development and validation of a predictive risk model based on retinal geometry for an early assessment of diabetic retinopathy
Minglan Wang, Xiyuan Zhou, Dan Ning Liu, Jieru Chen, Zheng Zheng, Saiguang Ling
Frontiers in Endocrinology.2022;[Epub] CrossRef - Characterization of NLRP3 Inflammasome Activation in the Onset of Diabetic Retinopathy
Charisse Y-J. Kuo, Jack J. Maran, Emma G. Jamieson, Ilva D. Rupenthal, Rinki Murphy, Odunayo O. Mugisho
International Journal of Molecular Sciences.2022; 23(22): 14471. CrossRef - VEGF Gene Polymorphism Among Diabetes Mellitus and Diabetic Retinopathy
Samra Anees, Saima Shareef, Muhammad Roman, Shah Jahan
Futuristic Biotechnology.2022; : 02. CrossRef - Th22 Cells Induce Müller Cells Activation Via the Act1/Traf6 Pathway in Diabetic Retinopathy
YuFei Wang, Hongdan Yu, Jing Li, Wenqiang Liu, Shengxue Yu, Pan Lv, Lipan Zhao, Xiaobai Wang, Zhongfu Zuo, Xuezheng Liu
SSRN Electronic Journal .2022;[Epub] CrossRef - Pathogenesis of diabetic macular edema: the role of pro-inflammatory and vascular factors. Aliterature review
M.L. Kyryliuk, S.A. Suk
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 180. CrossRef - Effects of emixustat hydrochloride in patients with proliferative diabetic retinopathy: a randomized, placebo-controlled phase 2 study
Ryo Kubota, Chirag Jhaveri, John M. Koester, Jeffrey K. Gregory
Graefe's Archive for Clinical and Experimental Ophthalmology.2021; 259(2): 369. CrossRef - Transient receptor potential vanilloid 4 channel deletion regulates pathological but not developmental retinal angiogenesis
Holly C. Cappelli, Brianna D. Guarino, Anantha K. Kanugula, Ravi K. Adapala, Vidushani Perera, Matthew A. Smith, Sailaja Paruchuri, Charles K. Thodeti
Journal of Cellular Physiology.2021; 236(5): 3770. CrossRef - Involvement of miR‐126 rs4636297 and miR‐146a rs2910164 polymorphisms in the susceptibility for diabetic retinopathy: a case–control study in a type 1 diabetes population
Eloísa Toscan Massignam, Cristine Dieter, Felipe Mateus Pellenz, Taís Silveira Assmann, Daisy Crispim
Acta Ophthalmologica.2021;[Epub] CrossRef - Retinal Vascular Endothelial Cell Dysfunction and Neuroretinal Degeneration in Diabetic Patients
Malgorzata Mrugacz, Anna Bryl, Katarzyna Zorena
Journal of Clinical Medicine.2021; 10(3): 458. CrossRef - Factors based on optical coherence tomography correlated with vision impairment in diabetic patients
Hiroaki Endo, Satoru Kase, Hikari Tanaka, Mitsuo Takahashi, Satoshi Katsuta, Yasuo Suzuki, Minako Fujii, Susumu Ishida, Manabu Kase
Scientific Reports.2021;[Epub] CrossRef - Class-3 semaphorins: Potent multifunctional modulators for angiogenesis-associated diseases
Bo Jiao, Shiyang Liu, Xi Tan, Pei Lu, Danning Wang, Hui Xu
Biomedicine & Pharmacotherapy.2021; 137: 111329. CrossRef - Single-Cell Analysis of Blood-Brain Barrier Response to Pericyte Loss
Maarja A. Mäe, Liqun He, Sofia Nordling, Elisa Vazquez-Liebanas, Khayrun Nahar, Bongnam Jung, Xidan Li, Bryan C. Tan, Juat Chin Foo, Amaury Cazenave-Gassiot, Markus R. Wenk, Yvette Zarb, Barbara Lavina, Susan E. Quaggin, Marie Jeansson, Chengua Gu, David
Circulation Research.2021;[Epub] CrossRef - VEGFR1 signaling in retinal angiogenesis and microinflammation
Akiyoshi Uemura, Marcus Fruttiger, Patricia A. D'Amore, Sandro De Falco, Antonia M. Joussen, Florian Sennlaub, Lynne R. Brunck, Kristian T. Johnson, George N. Lambrou, Kay D. Rittenhouse, Thomas Langmann
Progress in Retinal and Eye Research.2021; 84: 100954. CrossRef - Changes in Gene Expression Profiling and Phenotype in Aged Multidrug Resistance Protein 4-Deficient Mouse Retinas
Kyung Woo Kim, Sentaro Kusuhara, Atsuko Katsuyama-Yoshikawa, Sho Nobuyoshi, Megumi Kitamura, Sotaro Mori, Noriyuki Sotani, Kaori Ueda, Wataru Matsumiya, Akiko Miki, Takuji Kurimoto, Hisanori Imai, Makoto Nakamura
Antioxidants.2021; 10(3): 455. CrossRef - Circular RNAs: Novel target of diabetic retinopathy
Huan-ran Zhou, Hong-yu Kuang
Reviews in Endocrine and Metabolic Disorders.2021; 22(2): 205. CrossRef - MicroRNA-431-5p encapsulated in serum extracellular vesicles as a biomarker for proliferative diabetic retinopathy
Bo Yu, Mengran Xiao, Fuhua Yang, Jing Xiao, Hui Zhang, Lin Su, Xiaomin Zhang, Xiaorong Li
The International Journal of Biochemistry & Cell Biology.2021; 135: 105975. CrossRef - EndMT Regulation by Small RNAs in Diabetes-Associated Fibrotic Conditions: Potential Link With Oxidative Stress
Roberta Giordo, Yusra M. A. Ahmed, Hilda Allam, Salah Abusnana, Lucia Pappalardo, Gheyath K. Nasrallah, Arduino Aleksander Mangoni, Gianfranco Pintus
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - Pharmacokinetics of genistein distribution in blood and retinas of diabetic and non-diabetic rats
T. Hakami, M.I. Mahmoud, E. de Juan, M. Cooney
Drug Metabolism and Pharmacokinetics.2021; 39: 100404. CrossRef - Nimbolide ameliorates the streptozotocin-induced diabetic retinopathy in rats through the inhibition of TLR4/NF-κB signaling pathway
Xiangwen Shu, Yali Hu, Chao Huang, Ning Wei
Saudi Journal of Biological Sciences.2021; 28(8): 4255. CrossRef - Basic regulatory effects and clinical value of metalloproteinase-14 and extracellular matrix metalloproteinase inducer in diabetic retinopathy
Shuyan Li, Shiheng Lu, Lei Zhang, Shasha Liu, Lei Wang, Kai Lin, Jialun Du, Meixia Song
Materials Express.2021; 11(6): 873. CrossRef - Reduced Acrolein Detoxification in akr1a1a Zebrafish Mutants Causes Impaired Insulin Receptor Signaling and Microvascular Alterations
Haozhe Qi, Felix Schmöhl, Xiaogang Li, Xin Qian, Christoph T. Tabler, Katrin Bennewitz, Carsten Sticht, Jakob Morgenstern, Thomas Fleming, Nadine Volk, Ingrid Hausser, Elena Heidenreich, Rüdiger Hell, Peter Paul Nawroth, Jens Kroll
Advanced Science.2021;[Epub] CrossRef - The Metaflammatory and Immunometabolic Role of Macrophages and Microglia in Diabetic Retinopathy
Honglian Wu, Mengqi Wang, Xiaorong Li, Yan Shao
Human Cell.2021; 34(6): 1617. CrossRef - Inflammatory resolution and vascular barrier restoration after retinal ischemia reperfusion injury
Steven F. Abcouwer, Sumathi Shanmugam, Arivalagan Muthusamy, Cheng-mao Lin, Dejuan Kong, Heather Hager, Xuwen Liu, David A. Antonetti
Journal of Neuroinflammation.2021;[Epub] CrossRef - Diferenças de mensuração de acuidade visual e velocidade de leitura para perto entre pacientes com retinopatia diabética. Repercussão entre conceitos de deficiência visual parcial e cegueira legal
Roberta Freitas Momenté, Isabella Couto Amaral, Luiz Guilherme Coimbra de Brito, João Gabriel Volpato Ferraresi, Maria Luisa Gois da Fonsêca, Nadyr Antônia Damasceno, Luiz Claudio Santos de Souza Lima, Mauricio Bastos Pereira, Eduardo de França Damasceno
Revista Brasileira de Oftalmologia.2021;[Epub] CrossRef - Maintaining blood retinal barrier homeostasis to attenuate retinal ischemia-reperfusion injury by targeting the KEAP1/NRF2/ARE pathway with lycopene
Hao Huang, Xielan Kuang, Xiaobo Zhu, Hao Cheng, Yuxiu Zou, Han Du, Han Tang, Linbin Zhou, Jingshu Zeng, Huijun Liu, Jianhua Yan, Chongde Long, Huangxuan Shen
Cellular Signalling.2021; 88: 110153. CrossRef - Luteolin, an aryl hydrocarbon receptor antagonist, alleviates diabetic retinopathy by regulating the NLRP/NOX4 signalling pathway: Experimental and molecular docking study
Y. Yang, M. Zhou, H. Liu
Physiology International.2021; 108(2): 172. CrossRef - ALDH2/SIRT1 Contributes to Type 1 and Type 2 Diabetes-Induced Retinopathy through Depressing Oxidative Stress
Mengshan He, Pan Long, Tao Chen, Kaifeng Li, Dongyu Wei, Yufei Zhang, Wenjun Wang, Yonghe Hu, Yi Ding, Aidong Wen, Daniela Ribeiro
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - Looking Ahead: Visual and Anatomical Endpoints in Future Trials of Diabetic Macular Ischemia
Chui Ming Gemmy Cheung, Elizabeth Pearce, Beau Fenner, Piyali Sen, Victor Chong, Sobha Sivaprasad
Ophthalmologica.2021; 244(5): 451. CrossRef - The effect of psychotherapy on anxiety, depression, and quality of life in patients with diabetic retinopathy
Suiping Li, Hong Liu, Xian Zhu
Medicine.2021; 100(51): e28386. CrossRef - Changes in Ocular Blood Flow after Ranibizumab Intravitreal Injection for Diabetic Macular Edema Measured Using Laser Speckle Flowgraphy
Lisa Toto, Federica Evangelista, Pasquale Viggiano, Emanuele Erroi, Giada D’Onofrio, Daniele Libertini, Annamaria Porreca, Rossella D’Aloisio, Parravano Mariacristina, Luca Di Antonio, Marta Di Nicola, Rodolfo Mastropasqua
BioMed Research International.2020; 2020: 1. CrossRef - microRNA Expression Profile in the Vitreous of Proliferative Diabetic Retinopathy Patients and Differences from Patients Treated with Anti-VEGF Therapy
Julian Friedrich, David H. W. Steel, Reinier O. Schlingemann, Michael J. Koss, Hans-Peter Hammes, Guido Krenning, Ingeborg Klaassen
Translational Vision Science & Technology.2020; 9(6): 16. CrossRef - Update on the Effects of Antioxidants on Diabetic Retinopathy: In Vitro Experiments, Animal Studies and Clinical Trials
Jose Javier Garcia-Medina, Elena Rubio-Velazquez, Elisa Foulquie-Moreno, Ricardo P Casaroli-Marano, Maria Dolores Pinazo-Duran, Vicente Zanon-Moreno, Monica del-Rio-Vellosillo
Antioxidants.2020; 9(6): 561. CrossRef - Methylglyoxal, a Highly Reactive Dicarbonyl Compound, in Diabetes, Its Vascular Complications, and Other Age-Related Diseases
C. G. Schalkwijk, C. D. A. Stehouwer
Physiological Reviews.2020; 100(1): 407. CrossRef - Pericytes, inflammation, and diabetic retinopathy
Benjamin G. Spencer, Jose J. Estevez, Ebony Liu, Jamie E. Craig, John W. Finnie
Inflammopharmacology.2020; 28(3): 697. CrossRef - Eye hemodynamic data and biochemical parameters of the lacrimal fluid of patients with non-proliferative diabetic retinopathy
Guzal Kangilbaeva, Fazilat Bakhritdinova, Iroda Nabieva, Aziza Jurabekova
Data in Brief.2020; 32: 106237. CrossRef - Endocannabinoids in aqueous humour of patients with or without diabetes
Patrick Richardson, Catherine Ortori, Dave Barrett, Saoirse O'Sullivan, Iskandar Idris
BMJ Open Ophthalmology.2020; 5(1): e000425. CrossRef - A pyruvate dehydrogenase kinase inhibitor prevents retinal cell death and improves energy metabolism in rat retinas after ischemia/reperfusion injury
Kota Sato, Seiya Mochida, Daisuke Tomimoto, Takahiro Konuma, Naoki Kiyota, Satoru Tsuda, Yukihiro Shiga, Kazuko Omodaka, Toru Nakazawa
Experimental Eye Research.2020; 193: 107997. CrossRef - The Role of Bone Morphogenetic Proteins in Diabetic Complications
Nimna Perera, Rebecca H. Ritchie, Mitchel Tate
ACS Pharmacology & Translational Science.2020; 3(1): 11. CrossRef - Increased Ephrin-B2 expression in pericytes contributes to retinal vascular death in rodents
Maha Coucha, Amy C. Barrett, Joseph Bailey, Maryam Abdelghani, Mohammed Abdelsaid
Vascular Pharmacology.2020; 131: 106761. CrossRef - Mitochondrial Defects Drive Degenerative Retinal Diseases
Deborah A. Ferrington, Cody R. Fisher, Renu A. Kowluru
Trends in Molecular Medicine.2020; 26(1): 105. CrossRef - Fli1 deficiency induces endothelial adipsin expression, contributing to the onset of pulmonary arterial hypertension in systemic sclerosis
Takuya Miyagawa, Takashi Taniguchi, Ryosuke Saigusa, Maiko Fukayama, Takehiro Takahashi, Takashi Yamashita, Megumi Hirabayashi, Shunsuke Miura, Kouki Nakamura, Ayumi Yoshizaki, Shinichi Sato, Yoshihide Asano
Rheumatology.2020; 59(8): 2005. CrossRef - Natriuretic Peptides Attenuate Retinal Pathological Neovascularization Via Cyclic Guanosine Monophosphate Signaling in Pericytes and Astrocytes
Katarina Špiranec Spes, Sabrina Hupp, Franziska Werner, Franziska Koch, Katharina Völker, Lisa Krebes, Ulrike Kämmerer, Katrin G. Heinze, Barbara M. Braunger, Michaela Kuhn
Arteriosclerosis, Thrombosis, and Vascular Biology.2020; 40(1): 159. CrossRef - Therapeutic investigation of quercetin nanomedicine in a zebrafish model of diabetic retinopathy
Shuai Wang, Shanshan Du, Wenzhan Wang, Fengyan Zhang
Biomedicine & Pharmacotherapy.2020; 130: 110573. CrossRef - The role of CD44 in pathological angiogenesis
Li Chen, Chenying Fu, Qing Zhang, Chengqi He, Feng Zhang, Quan Wei
The FASEB Journal.2020; 34(10): 13125. CrossRef - Associations between alcohol intake and diabetic retinopathy risk: a systematic review and meta-analysis
Chen Chen, Zhaojun Sun, Weigang Xu, Jun Tan, Dan Li, Yiting Wu, Ting Zheng, Derong Peng
BMC Endocrine Disorders.2020;[Epub] CrossRef - Alpha-Smooth Muscle Actin-Positive Perivascular Cells in Diabetic Retina and Choroid
Soo Jin Kim, Sang A. Kim, Yeong A. Choi, Do Young Park, Junyeop Lee
International Journal of Molecular Sciences.2020; 21(6): 2158. CrossRef - The G‐protein‐coupled chemoattractant receptor Fpr2 exacerbates neuroglial dysfunction and angiogenesis in diabetic retinopathy
Ying Yu, Shengding Xue, Keqiang Chen, Yingying Le, Rongrong Zhu, Shiyi Wang, Shuang Liu, Xinliang Cheng, Huaijin Guan, Ji Ming Wang, Hui Chen
FASEB BioAdvances.2020; 2(10): 613. CrossRef - Dual-Acting Antiangiogenic Gene Therapy Reduces Inflammation and Regresses Neovascularization in Diabetic Mouse Retina
Rute S. Araújo, Diogo B. Bitoque, Gabriela A. Silva
Molecular Therapy - Nucleic Acids.2020; 22: 329. CrossRef - The cells involved in the pathological process of diabetic retinopathy
Songtao Yang, Jiaoyue Zhang, Lulu Chen
Biomedicine & Pharmacotherapy.2020; 132: 110818. CrossRef - The Role of Transforming Growth Factor-Beta in Retinal Ganglion Cells with Hyperglycemia and Oxidative Stress
Hsin-Yi Chen, Yi-Jung Ho, Hsiu-Chuan Chou, En-Chi Liao, Yi-Ting Tsai, Yu-Shan Wei, Li-Hsun Lin, Meng-Wei Lin, Yi-Shiuan Wang, Mei-Lan Ko, Hong-Lin Chan
International Journal of Molecular Sciences.2020; 21(18): 6482. CrossRef - Circadian rhythms in diabetic retinopathy: an overview of pathogenesis and investigational drugs
Ashay D. Bhatwadekar, Varun Rameswara
Expert Opinion on Investigational Drugs.2020; 29(12): 1431. CrossRef - Blood-retinal barrier as a converging pivot in understanding the initiation and development of retinal diseases
Xue Yang, Xiao-Wei Yu, Dan-Dan Zhang, Zhi-Gang Fan
Chinese Medical Journal.2020; 133(21): 2586. CrossRef - Immunosubunit β5i Knockout Suppresses Neovascularization and Restores Autophagy in Retinal Neovascularization by Targeting ATG5 for Degradation
Liyang Ji, Li Li, Ying Zhao, Shengqiang Liu, Jingmin Li, Jinsong Zhang, Qi Zhao, Shuai Wang
Investigative Opthalmology & Visual Science.2020; 61(14): 30. CrossRef - Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study
Yoo-Ri Chung, Kyoung Hwa Ha, Hyeon Chang Kim, Sang Jun Park, Kihwang Lee, Dae Jung Kim
Diabetes & Metabolism Journal.2019; 43(5): 640. CrossRef - Age-related changes of the human retinal vessels: Possible involvement of lipid peroxidation
Tapas Chandra Nag, Meenakshi Maurya, Tara Sankar Roy
Annals of Anatomy - Anatomischer Anzeiger.2019; 226: 35. CrossRef - Human iPSCs-Derived Endothelial Cells with Mutation in HNF1A as a Model of Maturity-Onset Diabetes of the Young
Kachamakova-Trojanowska, Stepniewski, Dulak
Cells.2019; 8(11): 1440. CrossRef - Diabetic Retinopathy–An Underdiagnosed and Undertreated Inflammatory, Neuro-Vascular Complication of Diabetes
Stephen H. Sinclair, Stanley S. Schwartz
Frontiers in Endocrinology.2019;[Epub] CrossRef - Identification of Diagnostic and Prognostic microRNAs for Recurrent Vitreous Hemorrhage in Patients with Proliferative Diabetic Retinopathy
Parviz Mammadzada, Juliette Bayle, Johann Gudmundsson, Anders Kvanta, Helder André
Journal of Clinical Medicine.2019; 8(12): 2217. CrossRef - RANKL blockade suppresses pathological angiogenesis and vascular leakage in ischemic retinopathy
Sangmi Ock, Soyoung Park, Junyeop Lee, Jaetaek Kim
Biochemical and Biophysical Research Communications.2019; 516(2): 350. CrossRef - EndogenousClostridium perfringensPanophthalmitis with Potential Entry Port from Diverticulitis Exacerbated by Proliferative Diabetic Retinopathy
Vamsee Neerukonda, Anny M. S. Cheng, Swetha Dhanireddy, Samuel Alpert, Han Y. Yin
Case Reports in Ophthalmological Medicine.2019; 2019: 1. CrossRef - Attenuation of Retinal Endothelial Vasodilator Function in a Rat Model of Retinopathy of Prematurity
Ayuki Nakano, Asami Mori, Shiho Arima, Daiki Asano, Akane Morita, Kenji Sakamoto, Tohru Nagamitsu, Tsutomu Nakahara
Current Eye Research.2019; 44(12): 1360. CrossRef - Efficacy of fenofibrate for diabetic retinopathy
Xing-jie Su, Lin Han, Yan-Xiu Qi, Hong-wei Liu
Medicine.2019; 98(14): e14999. CrossRef - Nutraceuticals for the Treatment of Diabetic Retinopathy
Maria Grazia Rossino, Giovanni Casini
Nutrients.2019; 11(4): 771. CrossRef - Efficacy of ranibizumab for the treatment of diabetic retinopathy
Yong-bo Ren, Xing-jie Su, Yan-xiu Qi, He-qun Luan, Qi Sun
Medicine.2019; 98(17): e15409. CrossRef
- Recent Insights into the Etiopathogenesis of Diabetic Retinopathy and Its Management
- High Glucose and/or Free Fatty Acid Damage Vascular Endothelial Cells via Stimulating of NAD(P)H Oxidase-induced Superoxide Production from Neutrophils.
- Sang Soo Kim, Sun Young Kim, Soo Hyung Lee, Yang Ho Kang, In Ju Kim, Yong Ki Kim, Seok Man Son
- Korean Diabetes J. 2009;33(2):94-104. Published online April 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.2.94
- 2,222 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Oxidative stress and inflammation are important factors in the pathogenesis of diabetes and contribute to the development of diabetic complications. To understand the mechanisms that cause vascular complications in diabetes, we examined the effects of high glucose and/or free fatty acids on the production of superoxide from neutrophils and their role in endothelial cell damage. METHODS: Human neutrophils were incubated in the media containing 5.5 mM D-glucose, 30 mM D-glucose, 3 nM oleic acid, or 30 microM oleic acid for 1 hour to evaluate superoxide production through NAD(P)H oxidase activation. Human aortic endothelial cells were co-cultured with neutrophils exposed to high glucose and oleic acid. We then measured neutrophil adhesion to endothelial cells, neutrophil activation and superoxide production, neutrophil-mediated endothelial cell cytotoxicity and subunits of neutrophil NAD(P)H oxidase. RESULTS: After 1 hour of incubation with various concentrations of glucose and oleic acid, neutrophil adherence to high glucose and oleic acid-treated endothelial cells was significantly increased compared with adhesion to low glucose and oleic acid-treated endothelial cells. Incubation of neutrophils with glucose and free fatty acids increased superoxide production in a dose-dependent manner. High glucose and oleic acid treatment significantly increased expression of the membrane components of NAD(P)H oxidase of neutrophil (gp91(phox)). Endothelial cells co-cultured with neutrophils exposed to high glucose and oleic acid showed increased cytolysis, which could be prevented by an antioxidant, N-acetylcysteine. CONCLUSION: These results suggest that high glucose and/orfree fatty acidsincrease injury of endothelial cells via stimulating NAD(P)H oxidase-induced superoxide production from neutrophils.
- Protective Effect of PGC-1 on Lipid Overload-induced Apoptosis in Vascular Endothelial Cell.
- Eun Hee Koh, Youn Mi Kim, Ha Jung Kim, Woo Je Lee, Jong Chul Won, Min Seon Kim, Ki Up Lee, Joong Yeol Park
- Korean Diabetes J. 2006;30(3):151-160. Published online May 1, 2006
- DOI: https://doi.org/10.4093/jkda.2006.30.3.151
- 2,091 View
- 17 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Fatty acids contribute to endothelial cell dysfunction and apoptosis by inducing accumulation of long chain fatty acyl CoA (LCAC), which increases oxidative stress in vascular endothelial cells. Forced expression of PGC-1 was shown to induce mitochondrial biogenesis and to control expression of mitochondrial enzymes involved in fatty acid oxidation. This study was undertaken to test the hypothesis that PGC-1 overexpression could prevent endothelial cell apoptosis by enhancing fatty acid oxidation and relieving oxidative stress in vascular endothelium. METHODS: Adenoviruses containing human PGC-1 (Ad-PGC-1) and beta-galactosidase (Ad-beta-gal) were transfected to confluent human aortic endothelial cells (HAECs). To investigate the effect of adenoviral PGC-1 gene transfer on apoptosis, combined treatment of linoleic acid (LA), an unsaturated fatty acid, was performed. RESULTS: PGC-1 overexpression inhibited the increase in ROS production and apoptosis of HAECs induced by LA. Also, PGC-1 led to a significant increase in fatty acid oxidation and decrease in triglyceride content in HAECs. LA caused the decrease of adenine nucleotide translocase (ANT) activity and transient mitochondrial hyperpolarization, which was followed by depolarization. PGC-1 overexpression prevented these processes. CONCLUSION: In summary, PGC-1 overexpression inhibited mitochondrial dysfunction and apoptosis by facilitating fatty acid oxidation and protecting against the damage from oxidative stress in HAECs. The data collectively suggest that the regulation of intracellular PGC-1 expression might play a critical role in preventing atherosclerosis.
- Effect and Mechanism of High Glucose Level on the Expression of an Adhesion Protein, beta ig-h3, and Cellular Function in Endothelial Cells.
- Sung Woo Ha, Hye Jin Yeo, Jong Sup Bae, Sung Chang Chung, Jung Guk Kim, In San Kim, In Kyu Lee, Bo Wan Kim
- Korean Diabetes J. 2003;27(4):323-331. Published online August 1, 2003
- 998 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Diabetes mellitus is a high risk condition for the development of atherosclerotic and thromboembolic macroangiopathy. There are many factors which are involved in development of these processes. Given the central pathogenic role of endotheliopathy in atherosclerosis, it is likely that this vascular monolayer is the ultimate target of injury in response to many cytokines and growth factors. A dysfunctional endothelium may contribute to the proatherogenic environment. Transforming growth factor (TGF-beta) is a key factor in the development of diabetic angiopathy and atherosclerosis because of its effect on the accumulation of extracellular matrix proteins and endothelial function. The adhesive molecule betaig-h3 is an extracellular matrix protein whose expression is induced by TGF-beta. Considering that TGF-beta plays an important role in diabetic complications and that betaig-h3 is a downstream target gene of TGF-beta, we hypothesized that betaig-h3 may also play a role in the development of diabetic angiopathy through its effect on the endothelial function. Therefore, we examined the effects of high glucose level on the expression of betaig-h3 and endothelial function in human umbilical vein endothelial cells (HUVECs). We also studied the mechanisms of this high glucose-induced betaig-h3 expression. METHODS: Endothelial cells were isolated from human umbilical cord and conditioned with different concentrations of TGF-beta or glucose. We measured TGF-beta and betaig-h3 protein presence/concentration/expression in cell supernatant by ELISA and examined whether TGF-beta is involved in high glucose-induced betaig-h3 expression. Finally, we investigated the biologic function of betaig-h3 in endothelial cells by using adhesion assay. RESULTS: Our study demonstrated that both high glucose level and TGF-beta induced betaig-h3 protein expression in HUVECs. High glucose level also induced TGF-beta protein expression in cells. Anti-TGF-beta antibody almost completely blocked high glucose-induced betaig-h3 expression. betaig-h3 was found to support the adhesion of endothelial cells. CONCLUSION: These results suggest that high glucose level upregulates betaig-h3 protein levels through the induction of TGF-beta and that betaig-h3 may play an important role in diabetic angiopathy by regulating adhesive function of endothelial cells.
- The Effect of Nitric Oxide on Insulin Binding and Insulin Receptor Recycling in Bovine Aortic Endothelial Cells.
- Hyuk Sang Kwon, Oak Kee Hong, Hee Soo Kim, Jung Min Lee, Sung Rae Kim, Sung Dae Moon, Sang Ah Jang, Hyun Shik Son, Kun Ho Yoon, Moo Il Kang, Bong Yun Cha, Kwang Woo Lee, Ho Young Son, Sung Koo Kang
- Korean Diabetes J. 2003;27(3):213-227. Published online June 1, 2003
- 984 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The coexistence of insulin resistance and endothelial dysfunction is commonly observed in a variety of metabolic and cardiovascular disorders, including athero-sclerosis and type 2 diabetes mellitus. Because nitric oxide (NO), or nitric oxide synthase (NOS), has been suggested as a significant contributing factor in the development of endothelial dysfunction and insulin resistance, reactive NO or NOS were investigated to see if they contribute to the insulin internalization pathway. METHODS: The production of NO (Nitrite), the expression of eNOS (endothelial NOS), insulin binding and the insulin receptor internalization and recycling, following 48 hours of incubation with bradykinin (BK), acetylcholine (Ach), NG-monomethyl- L-arginine (L-NMMA) and N-nitro-L-arginine methylester (L-NAME) in Bovine aortic endothelial cells (BAECs), were examined. RESULTS: The results were as follows: 1. In relation to the time course, the production of eNOS was increased, but was decreased after 8 hours of incubation. The production of eNOS in the L-NMMA and L-NAME treated groups was significantly decreased compared with that of the controls (p<0.05). 2. The specific insulin bindings to the receptors of the endothelial cells were maximized within 20 mins, and then decreased. At 20 mins, the binding rate of the L-NMMA treated group was significantly decreased compared to that of the controls. At a concentration of 0.4ng/ml of unlabelled insulin, the specific insulin binding of the L-NMMA treated group was significantly decreased compared to that of the controls (p<0.05). 3. The internalization of 125I-insulin into the endothelial cells, as assessed by the acid washing dissociation method, occurred rapidly. The internalized radioactivity of 125I-insulin, at 20 mins, was significantly increased in the BK and Ach groups compared with the controls (p<0.05). 4. The recycling of the internalized insulin receptors showed no significant differences between the study groups, but the recycling was slightly delayed compared with controls in the Ach group. CONCLUSION: In conclusion, the NO generating substances, BK and Ach, and the inhibitory substance, L-NMMA, may influence the binding and internalization of insulin-insulin receptors. Our results suggest that NO might contribute to the transcytosis of insulin in BAECs
- Effect of High Glucose Concentration on Expression of Adhesion Molecules in Endothelial Cells.
- In Ju Kim, Seok Man Son, Min Ki Lee, Hee Jeong, Yong Ki Kim
- Korean Diabetes J. 1998;22(3):280-289. Published online January 1, 2001
- 927 View
- 23 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Accelerated atherosclerotic vascular disease is the leading cause of mortality in patients with diabetes mellitus. Endothelial dysfunction, monocytes, and platelets are well known pathogenic factors in atherogenesis. Changes in the neutrophils and endothelial cells, an important early events in all inflammatory process, may contribute to the atherogenesis at early stage, but the significance of this process is not established yet. So we investigated the effects of glucose on the expression of adhesion molecules in endothelial cells, which retlects the change in endothelial-neutrophil adhesive interactions.METHODS: The human umbilical vein endothelial cells(HUVECs) are purchased from American Type Culture Collection. The cells were incubated upto 24 hours to evaluate the expression of E-selectin, PECAM-1, and P-selectin on the cell surface using whole cell ELISA method and soluble P-selectin under different glucose concentration(5.5, 15, and 30 mmol/L). Neutrophil adherence was also measured hy incubation of isolated human neutrophils with monolayers of HUVECs under same different glucose concentration. RESULTS: After 24h incubation with a various concentration of glucose, neutrophil adherence to high concentration of glucose(15 and 30mmol/L)- treated endothelium was significantly increased(5.0 +0.4 and 10.4+0.5%, respectively) compared with adhesion to low concentration of glucose(5.5mmol/ L)-treated endothelium(2.9.+0.4%). Incubation of HUVECs for 24 h in 30mmol/L glucose increased absorbance of E-selectin to 1.36+0.16(P<0.01) and reduced that of P-selectin to 0.56+0.04 compared with the results of respective control culture in 5.5mmol/L glucose(p<0.01), but not changed PECAM-1 expression. In addition, 24 h exposure of HUVECs to 30mmol/L glucose decreased soluble P-selectin concentration to 0.33+0.06ng/mL(P<0.01). CONCLUSION: The results of this study demonstrate that high concentration of glucose stimulates neutrophil adhesion to endothelial cells in association with increased expression of E-selectin. These results suggest that high glucose can directly affect interaction between neutrophil and endothelial cell through a adhesion molecule, especially E-selectin dependent mechanism. Further study should be necessary to investigate the significance of this phenomenon.
- Effects of Free Fatty Acids on Glutathione Redox Status in Cultured Endothelial Cells.
- Joong Yeol Park, Chul Hee Kim, Yun Ey Chung, Hong Kyu Kim, Young Il Kim, Sung Kwan Hong, Jae Dam Lee, Ki Up Lee
- Korean Diabetes J. 1998;22(3):262-270. Published online January 1, 2001
- 855 View
- 19 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Although plasma free fatty acids (FFA) are frequently elevated in diabetes mellitus, its role in the pathogenesis of diabetic vascular complications has not been well investigated. Recent stuclies reported that FFA may cause endothelial dysfunction through an enhancement of oxidative damage by decreasing glutathione redox cycle, an important anti-oxidant defense system in endothelial cells. In this study, we examined the effects of increased availability of FFA on intracellular glutathione redox cycle. METHODS: Bovine pulonary endothelial cells were exposed to 90 umol/L linoleic acid with or without 0.1 mM 2-bromopalmitate, an inhibitor of mitochondrial fatty acid oxidation, for 6hr. Components of the glutathione redox cycle such as total glutathione, reduced glutathione(GSH) and oxidized glutathione(GSSG) concentrations were measured by HPLC. RESULTS: Total glutathione concentration in cultured endothelial cells exposed to linoleic acid was significantly lower than that in control cells (10.8+ 0.5 vs 14.1+0.8 umol/g protein, P<0.05). Linoleic acid significantly decreased GSH concentrations (10.5+0.4 vs. 13.8+0.5 pmol/g protein, P<0.05) and the ratio of GSH/GSSG(26.3+1.3 vs. 47.0+2,1, P<0.05). Compared to cells exposed linoleic acid alone, total glutathione(13.5+0.5umol/g protein, P<0.05) and GSH concentration(13.2+0.4 pmol/g protein, P<0.05) significantly increased in cells treated with 2-bromopalmitate and linoleic acid. The ratio of GSH/GSSG in cells treated with 2-bromopalmitate and linoleic acid was higher th.an that in cells exposed to linoleic acid alone(44.1+1.3, P<0.05). CONCLUSION: Increased provision of FFA resulted in a derangement of glutathione redox cycle in cultured endothelial cells, which appears to be related to an increase in mitochondrial FFA oxidation. These results suggested that FFA can increase the risk of diabetic vascular complications.
- Effect of Glucose on Adherence of Neutrophils to Endothelial Cells.
- Seok Man Son, Seok Dong Yoo, In Ju Kim, Yong Ki Kim, Hee Bag Park, Chi Dae Kim, Ki Whan Hong
- Korean Diabetes J. 1997;21(3):262-270. Published online January 1, 2001
- 881 View
- 20 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Accelerated atherosclerotic vascular disease is the leading cause of mortality in patients with diabetes mellitus. To clarify the mechanisms that cause macrovascular dysfunction in diabetes, we examined the effect of high glucose on the adhesion of neutrophils to the endothelial cells and release of TNF-a from cultured rabbit aortic endotheIial cells. METHODS: Rabbit aortic endothelial cells in primary culture were prepared by the collagenase digestion method. Cells were incubated for various time upto 24 hours to evaluate TNF-a response to different glucose concentrations(0, 5.5, 11, 22mmol/L). Isolated rabbit neutrophils were incubated with monolayers of rabbit aortic endothelial cells under different glucose condition. RESULTS: After 24 hrs incubation with various concentrations of glucose, neutrophil adherence to high concentration of glucose(11 and 22mM)-treated endothelium was significantly increased(46+/-7 and 64 +/-6%, respectively) compared with adhesion to low concentration of glucose(0 or 5.5mM)-treated endothelium(3l +/-5 and 30+/-3%, respectively), In addition, when TNF-a imrnunoreactivity in the culture medium was measured by enzyme-linked immunoassay after 24 hours of incubation with various concentration of glucose, the secretion of TNF-a from endothelial cells was significantly increased in a concentration-dependent manner upon exposure to high concentration of glucose, CONCLUSION: The results of this study ciemonstrate tht high concentration of glucose stimulates neutrophil adhesion to endothelial cells in association with increased production of TNF-a from endothelial cells. These results suggest that glucose directly causes increased interaction between neutrophil and endothelial cell through a TNF-a-dependent mechaniasm,

 KDA
KDA
 First
First Prev
Prev





