- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 44(2); 2020 > Article
-
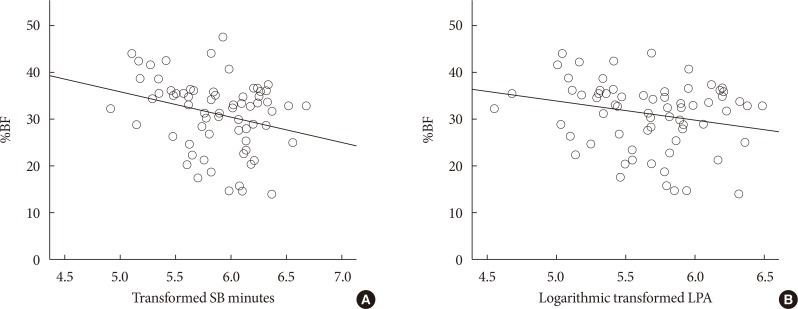
Original ArticleLifestyle Body Fat Is Related to Sedentary Behavior and Light Physical Activity but Not to Moderate-Vigorous Physical Activity in Type 2 Diabetes Mellitus
-
Keun Hee An1
 , Kyung Ah Han2
, Kyung Ah Han2 , Tae Seo Sohn3, Ie Byung Park4, Hae Jin Kim5, Sung Dae Moon6, Kyung Wan Min2
, Tae Seo Sohn3, Ie Byung Park4, Hae Jin Kim5, Sung Dae Moon6, Kyung Wan Min2
-
Diabetes & Metabolism Journal 2020;44(2):316-325.
DOI: https://doi.org/10.4093/dmj.2019.0029
Published online: November 12, 2019
1Department of Sports Science, Daejin University, Pocheon, Korea.
2Department of Internal Medicine, Eulji University School of Medicine, Daejeon, Korea.
3Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
4Department of Endocrinology of Metabolism, Gachon University College of Medicine, Incheon, Korea.
5Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea.
6Division of Endocrinology and Metabolism, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea.
- Corresponding author: Kyung Wan Min. Department of Internal Medicine, Eulji University School of Medicine, 77 Gyeryong-ro 771beon-gil, Jung-gu, Daejeon 34824, Korea. minyungwa@gmail.com
- *Keun Hee An and Kyung Ah Han contributed equally to this study as first authors.
Copyright © 2020 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations

- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
Lotte Bogaert, Iris Willems, Patrick Calders, Eveline Dirinck, Manon Kinaupenne, Marga Decraene, Bruno Lapauw, Boyd Strumane, Margot Van Daele, Vera Verbestel, Marieke De Craemer
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2024; 18(4): 102995. CrossRef - Association between depression, anemia and physical activity using isotemporal substitution analysis
Hee-kyoung Nam, Jungmi Park, Sung-il Cho
BMC Public Health.2023;[Epub] CrossRef - The Impact of Wearable Technologies in Health Research: Scoping Review
Sophie Huhn, Miriam Axt, Hanns-Christian Gunga, Martina Anna Maggioni, Stephen Munga, David Obor, Ali Sié, Valentin Boudo, Aditi Bunker, Rainer Sauerborn, Till Bärnighausen, Sandra Barteit
JMIR mHealth and uHealth.2022; 10(1): e34384. CrossRef - The Correlation of Prediabetes and Type 2 Diabetes With Adiposity in Adults
Juan Sun, Zhen Liu, Zimu Zhang, Ziyang Zeng, Weiming Kang
Frontiers in Nutrition.2022;[Epub] CrossRef - The Physical Activity Assessment of Adults With Type 2 Diabetes Using Accelerometer-Based Cut Points: Scoping Review
Ioana A Moldovan, Alexa Bragg, Anna S Nidhiry, Barbara A De La Cruz, Suzanne E Mitchell
Interactive Journal of Medical Research.2022; 11(2): e34433. CrossRef - Effects of 4 Weeks of a Technique-Specific Protocol with High-Intensity Intervals on General and Specific Physical Fitness in Taekwondo Athletes: An Inter-Individual Analysis
Alex Ojeda-Aravena, Tomás Herrera-Valenzuela, Pablo Valdés-Badilla, Jorge Cancino-López, José Zapata-Bastias, José Manuel García-García
International Journal of Environmental Research and Public Health.2021; 18(7): 3643. CrossRef - Inter-Individual Variability of a High-Intensity Interval Training With Specific Techniques vs. Repeated Sprints Program in Sport-Related Fitness of Taekwondo Athletes
Alex Ojeda-Aravena, Tomás Herrera-Valenzuela, Pablo Valdés-Badilla, Jorge Cancino-López, José Zapata-Bastias, José Manuel García-García
Frontiers in Physiology.2021;[Epub] CrossRef - EFFECT OF SPORTS MEDICINE ON REDUCING BODY FAT PERCENTAGE AND LEAN BODY MASS
Chunyan Fan
Revista Brasileira de Medicina do Esporte.2021; 27(7): 714. CrossRef - Validation of the effectiveness of a digital integrated healthcare platform utilizing an AI-based dietary management solution and a real-time continuous glucose monitoring system for diabetes management: a randomized controlled trial
Sung Woon Park, Gyuri Kim, You-Cheol Hwang, Woo Je Lee, Hyunjin Park, Jae Hyeon Kim
BMC Medical Informatics and Decision Making.2020;[Epub] CrossRef - Brain activity during a working memory task in different postures: an EEG study
Ju-Yeon Jung, Hwi-Young Cho, Chang-Ki Kang
Ergonomics.2020; 63(11): 1359. CrossRef

 KDA
KDA
 PubReader
PubReader Cite
Cite