- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 35(1); 2011 > Article
-
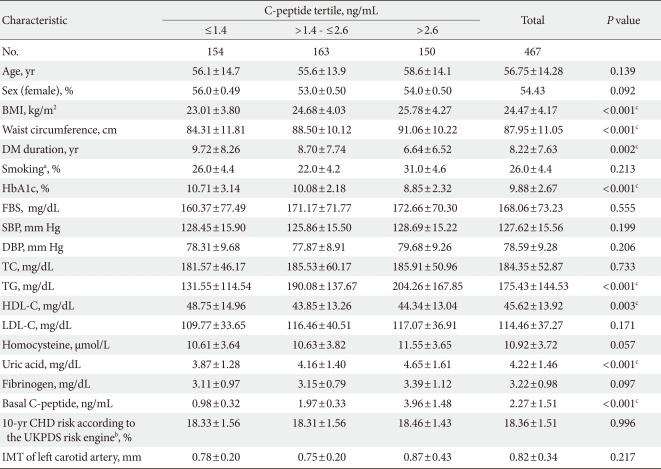
Original ArticleBasal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetic Patients
- Sung-Tae Kim1, Byung-Joon Kim1,2, Dong-Mee Lim1,2, In-Geol Song1, Jang-Han Jung1, Kang-Woo Lee1,2, Keun-Young Park1,2, Youn-Zoo Cho1, Dae-Ho Lee3, Gwan-Pyo Koh3
-
Diabetes & Metabolism Journal 2011;35(1):41-49.
DOI: https://doi.org/10.4093/dmj.2011.35.1.41
Published online: February 28, 2011
1Department of Internal Medicine, Konyang University Hospital, Konyang University School of Medicine, Daejon, Korea.
2Konyang University Myunggok Medical Research Institute, Daejon, Korea.
3Department of Internal Medicine, Jeju National University Hospital, Jeju National University School of Medicine, Jeju, Korea.
- Corresponding author: Dong Mee Lim. Division of Endocrinology and Metabolism, Department of Internal Medicine, Konyang University School of Medicine, 685 Gasuwon-dong, Seo-gu, Daejeon 302-718, Korea. mdldm@hanmail.net
• Received: August 11, 2010 • Accepted: October 11, 2010
Copyright © 2011 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations
Citations to this article as recorded by 

- The Correlation Between C-Peptide and Severity of Peripheral Atherosclerosis in Type 2 Diabetes Mellitus
Maisa A Wahab, Alshaymaa Alhabibi, Ahmed Khairy Sakr, Mohamed Yahia Zakaria, Ola I Saleh, Inass Hassan Ahmad, Eman Abdelrahman, Randa Taha, Fayka Karem Abdel Azeem Ahmed, Bothayna Ismail, Lamiaa Hosney Azel, Asmaa S Hassan, Hanaa Mohammed Eid El Sayed, Sa
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2617. CrossRef - Blood C‐peptide concentration as a proxy marker of cardiovascular disease: An observational cross‐sectional study
Laurinda Adusu‐Donkor, Emmanuel Kwaku Ofori, Fleischer C. N. Kotey, Francis Kwaku Dogodzi, Wormenor Dziedzorm, Alfred Buabeng, Segla Kwame Bernard, Seth K. Amponsah, Henry Asare‐Anane
Health Science Reports.2023;[Epub] CrossRef - The impact of insulin induced lipohypertrophy on carotid intima-media thickness in patients with type 2 diabetes mellitus
Cem Onur Kirac, Vehbi Sirikci, Huseyin Avni Findikli
Medicine.2023; 102(39): e34696. CrossRef - Effects of Serum C-Peptide Level on Blood Lipid and Cardiovascular and Cerebrovascular Injury in Patients with Type 2 Diabetes Mellitus: A Meta-Analysis
Juan Qin, Rongli Sun, Ding Ding, Yuvaraja Teekaraman
Contrast Media & Molecular Imaging.2022; 2022: 1. CrossRef - Correlation between serum C-peptide-releasing effects and the risk of elevated uric acid in type 2 diabetes mellitus
Yanyan Liu, Xue Zhao, Zequn Yang, Shurui Wang, Cong Han, Huijuan Zhang
Endocrine Journal.2022; 69(7): 773. CrossRef - Human C-peptide is a ligand of the elastin-receptor-complex and therewith central to human vascular remodelling and disease in metabolic syndrome
Gert Wensvoort
Medical Hypotheses.2022; 168: 110964. CrossRef - Influence of blood glucose fluctuation, C-peptide level and conventional risk factors on carotid artery intima–media thickness in Chinese Han patients with type 2 diabetes mellitus
Min Liu, Li Ao, Xinyu Hu, Jianning Ma, Kena Bao, Ye Gu, Jing Zhao, Weiping Huang
European Journal of Medical Research.2019;[Epub] CrossRef - Serum C peptide and carotid intima-medial thickness are independent markers of glucose intolerance among patients with ischemic cerebrovascular stroke
Nearmeen M. Rashad, Ghada M. Samir, Hanan M. Sabry, Nesreen M. Mohy, Shereen M. El Shabrawy
The Egyptian Journal of Internal Medicine.2019; 31(3): 368. CrossRef - Biomarker potential of C-peptide for screening of insulin resistance in diabetic and non-diabetic individuals
Haseeb A. Khan, Samia H. Sobki, Aishah Ekhzaimy, Isra Khan, Mona A. Almusawi
Saudi Journal of Biological Sciences.2018; 25(8): 1729. CrossRef - SERUM C-PEPTIDE LEVEL IN OBESE AND NON-OBESE PATIENTS WITH TYPE 2 DIABETES MELLITUS
Shamha Beegum Mariyam, Saboora Beegum Muthubeevi, Sandhya Chandrasekharan Vasantha
Journal of Evolution of Medical and Dental Sciences.2017; 6(05): 350. CrossRef - Mechanisms of action and therapeutic potential of proinsulin C-peptide
A. O. Shpakov
Journal of Evolutionary Biochemistry and Physiology.2017; 53(3): 180. CrossRef - Hemolysis Affects C‐Peptide Immunoassay
Zhi‐Qi Wu, Ju Lu, Hua‐Guo Xu
Journal of Clinical Laboratory Analysis.2016; 30(6): 1232. CrossRef - Lipid and inflammatory biomarker profiles in early insulin resistance
Itahisa Marcelino Rodríguez, José Oliva García, José Juan Alemán Sánchez, Delia Almeida González, Santiago Domínguez Coello, Buenaventura Brito Díaz, Fadoua Gannar, María del Cristo Rodríguez Pérez, Roberto Elosua, Antonio Cabrera de León
Acta Diabetologica.2016; 53(6): 905. CrossRef - C-Peptide Is Independently Associated with an Increased Risk of Coronary Artery Disease in T2DM Subjects: A Cross-Sectional Study
Lingshu Wang, Peng Lin, Aixia Ma, Huizhen Zheng, Kexin Wang, Wenjuan Li, Chuan Wang, Ruxing Zhao, Kai Liang, Fuqiang Liu, Xinguo Hou, Jun Song, Yiran Lu, Ping Zhu, Yu Sun, Li Chen, Marta Letizia Hribal
PLOS ONE.2015; 10(6): e0127112. CrossRef - C-peptide as a risk factor of coronary artery disease in the general population
Antonio Cabrera de León, José Gregorio Oliva García, Itahisa Marcelino Rodríguez, Delia Almeida González, José Juan Alemán Sánchez, Buenaventura Brito Díaz, Santiago Domínguez Coello, Vicente Bertomeu Martínez, Armando Aguirre Jaime, María del Cristo Rodr
Diabetes and Vascular Disease Research.2015; 12(3): 199. CrossRef - Gender differences in the association of insulin resistance and high-sensitivity c-reactive protein in obese adolescents
Ramin Alemzadeh, Jessica Kichler
Journal of Diabetes & Metabolic Disorders.2014;[Epub] CrossRef - Cytokinome Profile of Patients with Type 2 Diabetes and/or Chronic Hepatitis C Infection
Susan Costantini, Francesca Capone, Eliana Guerriero, Raffaele Marfella, Angela Sorice, Patrizia Maio, Michele Di Stasio, Giuseppe Paolisso, Giuseppe Castello, Giovanni Colonna, Patricia Fitzgerald-Bocarsly
PLoS ONE.2012; 7(6): e39486. CrossRef - Serum glycated albumin predicts the progression of carotid arterial atherosclerosis
Sun Ok Song, Kwang Joon Kim, Byung-Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Atherosclerosis.2012; 225(2): 450. CrossRef - C-Peptide: A New Mediator of Atherosclerosis in Diabetes
Dusica Vasic, Daniel Walcher
Mediators of Inflammation.2012; 2012: 1. CrossRef - Letter: Basal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetes Patients (Diabetes Metab J 2011;35:41-9)
Min Suk Lee, Hae Jin Kim
Diabetes & Metabolism Journal.2011; 35(2): 188. CrossRef - Response: Basal C-peptide Level as a Surrogate Marker of Subclinical Atherosclerosis in Type 2 Diabetic Patients (Diabetes Metab J 2011;35:41-9)
Sung-Tae Kim, Byung-Joon Kim, Dong-Mee Lim, In-Geol Song, Jang-Han Jung, Kang-Woo Lee, Keun-Young Park, Youn-Zoo Cho, Dae-Ho Lee, Gwan-Pyo Koh
Diabetes & Metabolism Journal.2011; 35(2): 190. CrossRef

 KDA
KDA

 PubReader
PubReader Cite
Cite