
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 39(2); 2015 > Article
-
Original ArticleClinical Care/Education Intensive Individualized Reinforcement Education Is Important for the Prevention of Hypoglycemia in Patients with Type 2 Diabetes
- Yun-Mi Yong1, Kyung-Mi Shin1, Kang-Min Lee2, Jae-Young Cho2, Sun-Hye Ko1,2, Min-Hyang Yoon1, Tae-Won Kim3, Jong-Hyun Jeong3, Yong-Moon Park4, Seung-Hyun Ko1,2, Yu-Bae Ahn1,2
-
Diabetes & Metabolism Journal 2015;39(2):154-163.
DOI: https://doi.org/10.4093/dmj.2015.39.2.154
Published online: March 10, 2015
1Diabetes Care Team, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
2Division of Endocrinology and Metabolism, Department of Internal Medicine, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
3Department of Psychiatry, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea.
4Department of Epidemiology and Biostatistics, Arnold School of Public Health, University of South Carolina, Columbia, SC, USA.
- Corresponding author: Yu-Bae Ahn. Division of Endocrinology and Metabolism, Department of Internal Medicine, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, 93 Jungbu-daero, Paldal-gu, Suwon 442-723, Korea. ybahn@catholic.ac.kr
- Corresponding author: Seung-Hyun Ko. Division of Endocrinology and Metabolism, Department of Internal Medicine, St. Vincent's Hospital, College of Medicine, The Catholic University of Korea, 93 Jungbu-daero, Paldal-gu, Suwon 442-723, Korea. kosh@catholic.ac.kr
Copyright © 2015 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- We investigated whether an intensive individualized reinforcement education program could influence the prevention of hypoglycemic events in patients with type 2 diabetes.
-
Methods
- From March 2013 to September 2013, patients aged 35 to 75 years with type 2 diabetes who had not previously participated in diabetes education, and treated with insulin or a sulfonylurea-containing regimen were included in the study. After structured group education, the patients assigned to the intensive individualized education group (IT) were requested to visit for reinforcement. All subjects in the IT were encouraged to self-manage dose adjustments. Participants in both groups (control group [CG, group education only; n=22] and IT [n=24]) attended follow-up visits at 2, 8, 12, and 24 weeks. At each visit, all patients were asked whether they had experienced hypoglycemia.
-
Results
- The total study population consisted of 20 men (43.5%; mean age and diabetic duration of 55.9±11.0 and 5.1±7.3 years, respectively). At 24 weeks, there were no significant differences in hemoglobin A1c values between the CG and IT. The total number of hypoglycemic events per patient was 5.26±6.5 in the CG and 2.58±2.3 times in the IT (P=0.004). Adherence to lifestyle modification including frequency of exercise, self-monitoring of blood glucose, or dietary habit was not significantly different between the groups. However, adherence to hypoglycemia management, especially the dose adjustment of medication, was significantly higher in the IT compared with the CG.
-
Conclusion
- Compared with the structured group education, additional IT resulted in additional benefits in terms of avoidance of hypoglycemia and treating hypoglycemia in patients with type 2 diabetes.
- Glycemic control and treatment of diabetes should start with lifestyle modification (LSM). Because self-care behaviors such as exercise and dietary habits are recognized as important tools for the maintenance of LSM, diabetes self-management education (DSME) needs to be emphasized for patients with diabetes [1]. The benefits of DSME have been demonstrated by a number of successful studies. DSME is associated with improved diabetes knowledge and self-care behavior, improved clinical outcomes, a reduction in body weight, improved quality of life (QOL), healthy coping, and lower health care costs [2,3,4]. Both individual and group approaches have been found effective [5,6]. Diabetic patients must receive standardized DSME at the time of diagnosis and as needed thereafter [1,7]. In addition, clinical practice guidelines recommend that DSME must be provided by a certified educator who has received professional training or by a multidisciplinary care team [8]. Because DSME can result in cost-savings and improved outcomes, its cost should be supported by a third-party payer [1,7].
- Hypoglycemia is a major obstacle for patients with type 2 diabetes trying to achieve glycemic targets [9,10,11]. With a steadily growing number of people with type 2 diabetes and the increased use of insulin or hypoglycemic agents for strict glycemic control, the number of diabetics with severe hypoglycemia is also increasing [12]. The fear of hypoglycemia is usually a barrier towards increasing the dosage of medication or initiating insulin treatment for patients with diabetes, although their glycemic status is not adequately controlled [13].
- Previously, we investigated the long-term effectiveness of a structured intensive diabetes education program (SIDEP) in patients with type 2 diabetes [4]. We found that the SIDEP encouraged people with type 2 diabetes to attain better glycemic control, as well as better physical activity and dietary and self-monitoring of blood glucose (SMBG) habits. In general, a diabetes education program, including our group-based program, covers the knowledge and coping with hypoglycemia; however, whether our group education program could reduce the incidence of hypoglycemia remains unknown.
- Therefore, we investigated the effectiveness of reinforced diabetes education for the prevention of hypoglycemia in patients with type 2 diabetes. After our SIDEP was delivered, patients were randomly assigned to the control group (CG) or the intensive individualized reinforcement education group (IT). The number of symptomatic or asymptomatic hypoglycemic episodes was the primary outcome. Glycemic control status, self-care skills, and adherence to the LSM were also measured.
INTRODUCTION
- Study subjects
- Type 2 diabetics aged between 35 and 75 years old who had not previously participated in a diabetes education course and been treated with insulin or sulfonylurea-containing drugs were included (n=55). Patients were excluded if they were older than 75 years of age, mentally ill, unable to participate in the recommended exercise program, suffered from alcoholism, had a malignancy, or had any severe medical illness such as sepsis, severe infection, or shock. The study protocol was approved by the Institutional Review Board of The Catholic University of Korea College of Medicine. Written informed consent was obtained from all participants.
- Intensive individualized reinforcement education program
- Previously, we organized our own diabetes education program based on the Dusseldorf study and the Diabetes Prevention Program [14,15]. The program was designed as group education consisting of five to 10 patients. Our education team was composed of a diabetologist, a certified diabetes educator, a psychiatrist, and a dietician. The curriculum consisted of 6, 40 minutes teaching units totaling 4 hours. The curriculum contents were structured to provide an understanding of diabetes and teach the SMBG and injection techniques, meal planning, physical activity, stress management, and sick day care with hypoglycemia management (Supplementary Table 1) [4]. During the hypoglycemia session, a diabetes educator nurse introduced the definition and symptoms of hypoglycemia and how to correct hypoglycemia with a glucose supplement.
- Fifty-five people with type 2 diabetes were enrolled and attended the group program. After the group education, the patients were randomly assigned to a CG (group education only, n=27) or a IT (n=28) using a random number table. The patients assigned to the IT returned after 1 week for intensive individual education. The IT program consisted of hypoglycemia-specific lessons totaling 1 hour taught by a diabetes educator nurse. Key components of the IT program consisted of four parts: (1) detection of hypoglycemia symptoms; (2) correct management and re-checking of blood glucose levels after 15 minutes of hypoglycemia treatment; (3) possible causes as assessed by the patients themselves; and (4) dose adjustment of insulin or oral medication (Supplementary Table 2) [16]. All subjects in the IT were encouraged to self-manage dose adjustments. Their basal insulin dose titration was performed according to the mean fasting glucose level for the previous three consecutive days with the algorithm [17].
- Both groups were followed up at 2, 8, 12, and 24 weeks after education. All participants continued the usual treatment provided by physicians, were scheduled for regular follow-up visits, and could contact our care team anytime by phone. Patients were asked to perform a 4-point SMBG for 14 consecutive days before each visit and whenever they had hypoglycemia symptoms. At each visit, all patients were asked whether they had experienced hypoglycemia (Fig. 1).
- Measurements of clinical parameters and adherence to LSM
- Hypertension was defined as a systolic blood pressure (BP) of at least 140 mm Hg or a diastolic BP of at least 90 mm Hg or having a history of treatment for hypertension. The body mass index (BMI) was calculated by the individual's weight in kilograms divided by the square of the individual's height in meters.
- Blood samples were obtained after a minimum fasting time of 8 hours. Hemoglobin A1c (HbA1c) values were measured using a high-performance liquid chromatography-723 G7 system (Bio-Rad, Montreal, QC, Canada). Serum levels of fasting glucose, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), triglycerides, and low density lipoprotein cholesterol (LDL-C) were measured enzymatically using an automatic analyzer 7600 (Hitachi, Tokyo, Japan). Diabetic nephropathy was defined as an albumin-creatinine ratio≥30 mg/g creatinine using a spot urine sample.
- Adherence to LSM, dietary habits, physical activity, and the frequency of SMBG was evaluated by the subjects completing a questionnaire when they visited the hospital. Each parameter was scored using a 5-point scale based on the average status of the individual during the recent few days [4].
- Measurement of hypoglycemia
- At every visit, we evaluated the SMBG data and the number of episodes of hypoglycemia. Hypoglycemia was defined as a SMBG value<70 mg/dL with or without hypoglycemia symptoms [18]. If the subjects had hypoglycemic symptoms and a glucose level check was not available, the participants were allowed to eat a snack. If the hypoglycemic symptoms were relieved with the snack, the event counted as hypoglycemia [18]. The cause of hypoglycemia was classified as (1) diet (delayed or missed meal, eating less food in a meal than planned); (2) exercise (unexpected or more vigorous exercise than usual); (3) medication (no adjustment of medication in spite of lower than normal glycemic range); and (4) others (concurrent illness, unknown cause).
- Statistical analysis
- Statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA). All values are presented as mean±standard deviation for continuous variables or number (%) for categorical variables. Comparison of the CG and IT was performed using an unpaired t-test, analysis of covariance, or a chi-square test. Comparison within the groups was conducted using a paired t-test. The SAS mixed procedure was used to analyze the repeated measurements of hypoglycemic events for evaluating the educational effects according to different time intervals.
- We used logistic regression analysis to test associations between the outcome (hypoglycemia episodes) and potential explanatory variables after adjustment for the following prognostic factors: sex, age, BMI, duration of diabetes, presence of hypertension, diabetic retinopathy, or nephropathy, HbA1c, and the use of insulin. The results are presented as an odds ratios (ORs) and 95% confidence intervals (CIs). A P value of less than 0.05 was considered statistically significant.
METHODS
- Clinical characteristics
- After randomization, there were no differences between the CG and IT in age (P=0.282), diabetic duration (P=0.125), baseline HbA1c (P=0.824), and sex ratio (P=0.107). Within the total population (n=55), 24 subjects in the IT and 22 subjects in the CG completed the follow-up at 24 weeks (follow-up loss, n=7 [CG, 5; IT, 2]; drop-out, n=2 [IT]). The participants' mean age was 55.9±11.0 years. 43.5% were men, and the mean diabetic duration was 5.1±7.3 years. The average HbA1c level was 10.7%±2.5%. Regarding the baseline clinical characteristics that were determined (n=46), there were no significant differences between the CG and IT, except for fasting plasma glucose and TC levels (Table 1).
- Effect of intensive education on glycemic control and LSM
- At the 24 weeks follow-up visit, we observed significant improvements in HbA1c in the CG (0 week vs. 24 weeks, 11.3%±2.3% vs. 7.16%±1.5%, P<0.001) and the IT (0 week vs. 24 weeks, 10.2%±2.5% vs. 7.24%±1.5%, P<0.001). However, no significant difference was found between the CG and IT at 24 weeks (CG vs. IT, P=0.802) (Table 2). In addition, there were no significant differences between the CG and IT in body weight and LDL-C level at 24 weeks (Table 2).
- Adherence to their self-care behavior, including the frequency of SMBG, physical activity, and dietary habits, was investigated using a 5-point scale. At 24 weeks, the scores greater than four were not different between the IT and CG for all three items (Table 2).
- Effect of intensive education on the hypoglycemic events
- At 24 weeks, hypoglycemia developed 121 times in the CG and 62 times in the IT. The 87.0% of patients in the CG and 70.8% of patients in IT experienced hypoglycemia. Total hypoglycemic events per patient during the observation period were 5.26±6.5 events in the CG and 2.58±2.3 events in the IT (P=0.004).
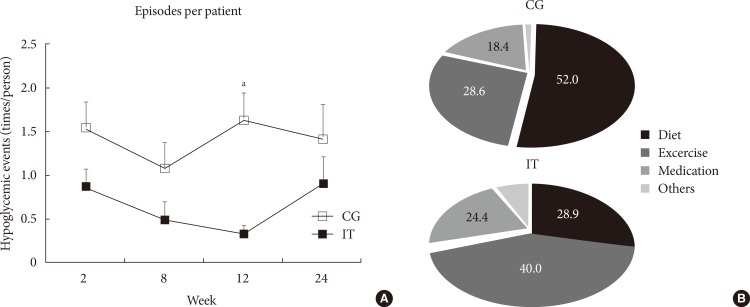
- Overall, the number of hypoglycemic events was significantly higher in the CG compared with the IT (P=0.002), and the difference in the mean number of hypoglycemic events between the two groups was consistent across the four time periods (P for interaction=0.674). At 12 weeks, however, hypoglycemic events per patient were significantly increased in the CG compared with those in the IT (P=0.007) (Fig. 2A). The number of patients who discontinued insulin use was higher in the IT compared with those in the CG (41.7% vs. 22.7%, P=0.010). However, no difference was detected in the daily insulin dose between the groups at follow-up (Table 2). The percentage of patients who were treated with insulin was decreased in both groups (CG vs. IT, 77.3% vs. 54.2% at baseline, P=0.210; 36.4% vs. 12.5% at 24 weeks, P=0.060).
- The cause of hypoglycemia was significantly different between the groups (P=0.029) (Fig. 2B). Approximately half of all hypoglycemic episodes were preceded by meal-related events before breakfast in the CG. However, unexpected or more vigorous exercise than usual was the most common antecedent of hypoglycemia in the IT.
- At 24 weeks, hypoglycemia management skills, such as detection of hypoglycemia symptoms by SMBG, correct management with a snack, re-checking blood glucose levels after 15 minutes, and dose adjustment of insulin or oral medication by schedule, were assessed. The percentage of patients who adhered to hypoglycemia management, especially re-checking blood glucose and adjusting the dose of their medication, was significantly higher in the IT compared with the CG (Fig. 3).
- Effect of intensive reinforcement on frequency of hypoglycemia
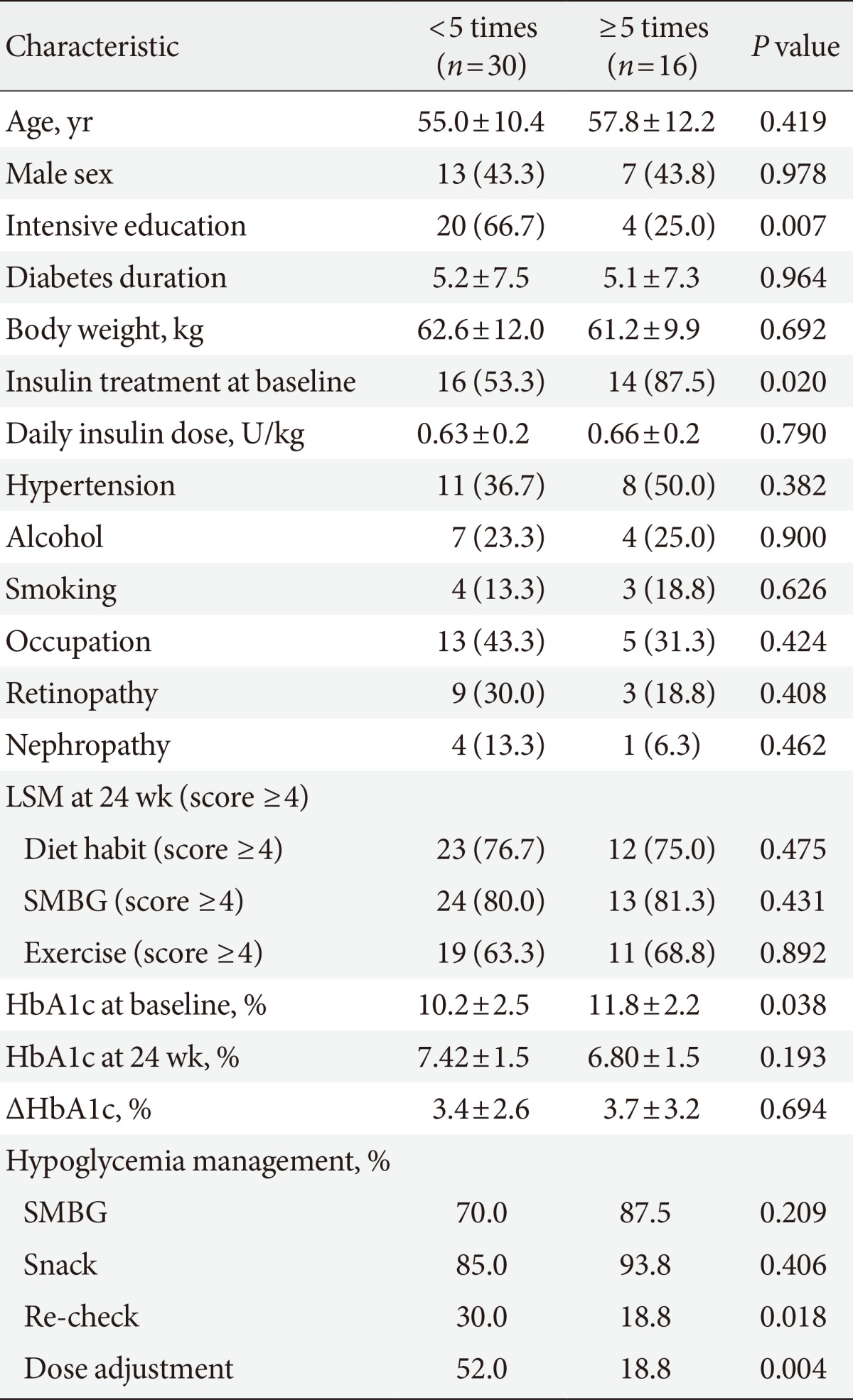
- We divided our patients according to the frequency of hypoglycemia. We compared the clinical characteristics of the subjects who experienced hypoglycemia <5 times and ≥5 times. The patients who experienced hypoglycemia ≥5 times had significantly higher baseline HbA1c levels (P=0.038) and were more frequently treated with insulin (P=0.020). In patients who experienced hypoglycemia <5 times, 66.7% experienced intensive education, but only 25.0% of those who experienced hypoglycemia ≥5 times had intensive education (Table 3). Of note, the percent of patients who adhered to hypoglycemia management, such as re-checking blood glucose and adjusting the dose of medication, was significantly higher in patients who experienced hypoglycemia <5 times compared with those who experienced hypoglycemia ≥5 times (Table 3).
- Table 4 shows the association of various risk factors with the frequency of hypoglycemic events. After adjusting for age, sex, diabetic duration, presence of hypertension or diabetic complications, insulin use, and HbA1c level, intensive education for hypoglycemia management was associated with the lower incidence of hypoglycemic events (OR, 0.13; 95% CI, 0.02 to 0.74; P=0.022) (Table 4).
RESULTS
- In this study, we investigated the effectiveness of intensive individualized diabetes education for the prevention of hypoglycemia in patients with type 2 diabetes. Hypoglycemic episodes were significantly decreased in patients with intensive individualized reinforcement compared with those with structured diabetes group education only. Of note, educating individuals about adjusting the dose of their medication after hypoglycemia seems to have been important for the prevention of recurrent hypoglycemia.
- Diabetes education is an initial and essential step for diabetes care. Recently, care of diabetes has shifted to an approach that is more patient centered. In a shared decision-making approach, clinicians, and patients act as partners, and patients are involved in the decision making [19]. In addition, DSME has changed from a didactic approach focused on providing information to a more theoretically based empowerment model that focuses on helping those with diabetes make informed self-management decisions [1]. Therefore, individualized, interactive, and reinforcement of diabetic education would be more helpful for patients with diabetes than simple group lessons.
- Hypoglycemia is a well-known acute complication of diabetes treatment and is considered a main barrier to achieving glycemic goals in patients with type 2 diabetes [20,21,22]. When emphasizing the importance of strict glycemic control for the prevention of diabetic vascular complications, the risk for developing hypoglycemia increased [10,11]. Older age, longer diabetic duration, and the presence of microvascular complications are known risk factors for severe hypoglycemia [23,24]. Detecting high risk populations early and providing specialized diabetic education might reduce the incidence of hypoglycemic events in patients with type 2 diabetes.
- There are some clinical studies, mostly in type 1 diabetics, showing the effect of diabetes education on the development of hypoglycemia. A new education program for treating diabetic patients with hypoglycemia problems (HyPOS) aimed to avoid hypoglycemia by optimizing insulin therapy for type 1 diabetics [16]. When compared with a CG, hypoglycemia awareness significantly improved HyPOS after a 6-month follow-up period. Additionally, blood glucose awareness training (BGAT) was a psychoeducational programmatic intervention designed to improve the accuracy of patients' detection and interpretation of relevant blood glucose symptoms. BGAT led to a significant improvement in the detection of low and high blood glucose levels [25]. The dose adjustment for normal eating (DAFNE) trial was a course that taught flexible intensive insulin treatment combined with dietary freedom and insulin adjustment in type 1 diabetics in the United Kingdom [26]. Despite an increase in the number of insulin injections and encouragement to increase glucose monitoring, HbA1c was significantly improved without an increased risk of hypoglycemia in the DAFNE group compared with the CG. Therefore, diabetic education per se is an effective tool for the treatment of hypoglycemia in patients with type 1 diabetes. However, the effect of structured education on the prevention of hypoglycemia in patients with type 2 diabetes has not been well studied.
- In our present study, we performed a specialized individualized reinforcement education program on hypoglycemia management after structured group education for patients with type 2 diabetes. Subjects in the IT were taught hypoglycemia management skills including frequent SMBG, glucose supplementation, re-checking of blood glucose after hypoglycemic episodes, and adjusting the dose of their medication. There were no differences in the adherence to self-care behaviors and glycemic improvement between the groups; however, hypoglycemic events were remarkably decreased after reinforcement education. We found that our program significantly improved the management skills for hypoglycemic symptoms and dose adjustment according to fasting glucose levels. The percentage of patients with adherence to hypoglycemia management was significantly higher in patients who experienced hypoglycemia less frequently. Therefore, in spite of a significant improvement in glycemic control and LSM with a structured group education program, we found that reinforcement of hypoglycemia management and dose adjustment skills would be additional benefits for the prevention of hypoglycemia in patients with type 2 diabetes.
- There are some limitations in our study. Our study population included a small number of subjects, and the length of follow-up was only 6 months. We did not perform a QOL assessment related to hypoglycemia management. If hypoglycemic events were reduced with a hypoglycemia management program by patients themselves, we believe that the fear or anxiety for hypoglycemia would be decreased, and compliance to their diabetic medication or QOL would be much improved.
- In summary, compared with the control (group education) group, intensive education for hypoglycemia provided additional benefits in terms of avoiding and managing hypoglycemia in patients with type 2 diabetes. Skill training in dose adjustment seemed to be a preferential target. Like an individualized glycemic goal according to one's individual clinical situation, the education curriculum should be individualized, or reinforcement should be focused on particular patient groups for the prevention of hypoglycemia. In the future, practical guidelines for the selection of high risk patients, a specific education program, and reinforcement are needed.
DISCUSSION
-
Acknowledgements
- This study was supported by a grant (KMS, 2012) from the Korean Diabetes Association.
ACKNOWLEDGMENTS
-
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
NOTES
Supplementary Material
Supplementary Table 1
Supplementary Table 2
- 1. American Diabetes Association. Standards of medical care in diabetes: 2014. Diabetes Care 2014;37(Suppl 1):S14-S80. ArticlePubMedPDF
- 2. Rickheim PL, Weaver TW, Flader JL, Kendall DM. Assessment of group versus individual diabetes education: a randomized study. Diabetes Care 2002;25:269-274. PubMed
- 3. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159-1171. PubMed
- 4. Ko SH, Song KH, Kim SR, Lee JM, Kim JS, Shin JH, Cho YK, Park YM, Jeong JH, Yoon KH, Cha BY, Son HY, Ahn YB. Long-term effects of a structured intensive diabetes education programme (SIDEP) in patients with type 2 diabetes mellitus: a 4-year follow-up study. Diabet Med 2007;24:55-62. ArticlePubMed
- 5. Dinneen SF, O'Hara MC, Byrne M, Smith D, Courtney CH, McGurk C, Heller SR, Newell J, Coffey N, Breen C, O'Scannail M, O'Shea D. Irish DAFNE Study Group. Group follow-up compared to individual clinic visits after structured education for type 1 diabetes: a cluster randomised controlled trial. Diabetes Res Clin Pract 2013;100:29-38. ArticlePubMed
- 6. Deakin T, McShane CE, Cade JE, Williams RD. Group based training for self-management strategies in people with type 2 diabetes mellitus. Cochrane Database Syst Rev 2005;2:CD003417Article
- 7. Ko SH, Kim SR, Kim DJ, Oh SJ, Lee HJ, Shim KH, Woo MH, Kim JY, Kim NH, Kim JT, Kim CH, Kim HJ, Jeong IK, Hong EK, Cho JH, Mok JO, Yoon KH. Committee of Clinical Practice Guidelines Korean Diabetes Association. 2011 Clinical practice guidelines for type 2 diabetes in Korea. Diabetes Metab J 2011;35:431-436. ArticlePubMedPMC
- 8. Zwar N, Hasan I, Hermiz O, Vagholkar S, Comino E, Harris M. Multidisciplinary care plans and diabetes: benefits for patients with poor glycaemic control. Aust Fam Physician 2008;37:960-962. PubMed
- 9. Abraira C, Duckworth W, McCarren M, Emanuele N, Arca D, Reda D, Henderson W. VA Cooperative Study of Glycemic Control and Complications in Diabetes Mellitus Type 2. Design of the cooperative study on glycemic control and complications in diabetes mellitus type 2: Veterans Affairs Diabetes Trial. J Diabetes Complications 2003;17:314-322. PubMed
- 10. Action to Control Cardiovascular Risk in Diabetes Study Group. Gerstein HC, Miller ME, Byington RP, Goff DC Jr, Bigger JT, Buse JB, Cushman WC, Genuth S, Ismail-Beigi F, Grimm RH Jr, Probstfield JL, Simons-Morton DG, Friedewald WT. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545-2559. ArticlePubMedPMC
- 11. ADVANCE Collaborative Group. Patel A, MacMahon S, Chalmers J, Neal B, Billot L, Woodward M, Marre M, Cooper M, Glasziou P, Grobbee D, Hamet P, Harrap S, Heller S, Liu L, Mancia G, Mogensen CE, Pan C, Poulter N, Rodgers A, Williams B, Bompoint S, de Galan BE, Joshi R, Travert F. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560-2572. ArticlePubMed
- 12. Kim JT, Oh TJ, Lee YA, Bae JH, Kim HJ, Jung HS, Cho YM, Park KS, Lim S, Jang HC, Lee HK. Increasing trend in the number of severe hypoglycemia patients in Korea. Diabetes Metab J 2011;35:166-172. ArticlePubMedPMC
- 13. Wild D, von Maltzahn R, Brohan E, Christensen T, Clauson P, Gonder-Frederick L. A critical review of the literature on fear of hypoglycemia in diabetes: implications for diabetes management and patient education. Patient Educ Couns 2007;68:10-15. ArticlePubMed
- 14. Muhlhauser I, Bruckner I, Berger M, Cheta D, Jorgens V, Ionescu-Tirgoviste C, Scholz V, Mincu I. Evaluation of an intensified insulin treatment and teaching programme as routine management of type 1 (insulin-dependent) diabetes. The Bucharest-Dusseldorf Study. Diabetologia 1987;30:681-690. ArticlePubMedPDF
- 15. The Diabetes Prevention Program. Design and methods for a clinical trial in the prevention of type 2 diabetes. Diabetes Care 1999;22:623-634. ArticlePubMedPMCPDF
- 16. Hermanns N, Kulzer B, Kubiak T, Krichbaum M, Haak T. The effect of an education programme (HyPOS) to treat hypoglycaemia problems in patients with type 1 diabetes. Diabetes Metab Res Rev 2007;23:528-538. ArticlePubMed
- 17. Davies M, Storms F, Shutler S, Bianchi-Biscay M, Gomis R. ATLANTUS Study Group. Improvement of glycemic control in subjects with poorly controlled type 2 diabetes: comparison of two treatment algorithms using insulin glargine. Diabetes Care 2005;28:1282-1288. PubMed
- 18. Workgroup on Hypoglycemia, American Diabetes Association. Defining and reporting hypoglycemia in diabetes: a report from the American Diabetes Association Workgroup on Hypoglycemia. Diabetes Care 2005;28:1245-1249. PubMed
- 19. Inzucchi SE, Bergenstal RM, Buse JB, Diamant M, Ferrannini E, Nauck M, Peters AL, Tsapas A, Wender R, Matthews DR. American Diabetes Association (ADA). European Association for the Study of Diabetes (EASD). European Association for the Study of Diabetes (EASD). Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2012;35:1364-1379. PubMedPMC
- 20. Alsahli M, Gerich JE. Hypoglycemia. Endocrinol Metab Clin North Am 2013;42:657-676. ArticlePubMed
- 21. Cryer PE. Hypoglycaemia: the limiting factor in the glycaemic management of type I and type II diabetes. Diabetologia 2002;45:937-948. ArticlePubMedPDF
- 22. Ha WC, Oh SJ, Kim JH, Lee JM, Chang SA, Sohn TS, Son HS. Severe hypoglycemia is a serious complication and becoming an economic burden in diabetes. Diabetes Metab J 2012;36:280-284. ArticlePubMedPMC
- 23. Akram K, Pedersen-Bjergaard U, Carstensen B, Borch-Johnsen K, Thorsteinsson B. Frequency and risk factors of severe hypoglycaemia in insulin-treated type 2 diabetes: a cross-sectional survey. Diabet Med 2006;23:750-756. ArticlePubMed
- 24. Yun JS, Ko SH, Ko SH, Song KH, Ahn YB, Yoon KH, Park YM, Ko SH. Presence of macroalbuminuria predicts severe hypoglycemia in patients with type 2 diabetes: a 10-year follow-up study. Diabetes Care 2013;36:1283-1289. PubMedPMC
- 25. Cox DJ, Gonder-Frederick L, Polonsky W, Schlundt D, Kovatchev B, Clarke W. Blood glucose awareness training (BGAT-2): long-term benefits. Diabetes Care 2001;24:637-642. PubMed
- 26. Lawton J, Rankin D, Cooke D, Elliott J, Amiel S, Heller S. UKNIHR DAFNE Study Group. Patients' experiences of adjusting insulin doses when implementing flexible intensive insulin therapy: a longitudinal, qualitative investigation. Diabetes Res Clin Pract 2012;98:236-242. ArticlePubMed
REFERENCES
The number of hypoglycemic events per patient at each time point and causes of hypoglycemia. (A) Episodes of hypoglycemia per patient were significantly lower in the intensive group (IT) compared with the control group (CG) (P=0.002), and the difference in the mean number of hypoglycemic events between the two groups was consistent across each time point (P for interaction=0.674). At 12 weeks, however, hypoglycemic events per patient were significantly higher in the CG. (B) The causes of hypoglycemia were significantly different between the groups (P=0.029). The cause of hypoglycemia was classified as (1) diet (delayed or missed meal, eating less food in a meal than planned); (2) exercise (unexpected or more vigorous exercise than usual); (3) medication (no adjustment of medication in spite of lower than normal glycemic range); (4) others (concurrent illness, unknown cause). aP<0.05 vs. IT.
Adherence to hypoglycemia management at 24 weeks. The percentage of patients with good compliance to hypoglycemia management was significantly higher in the intensive group (IT). SMBG, self-monitoring of blood glucose. aP<0.05 vs. control group (CG).

Effect of intensive education at follow-up
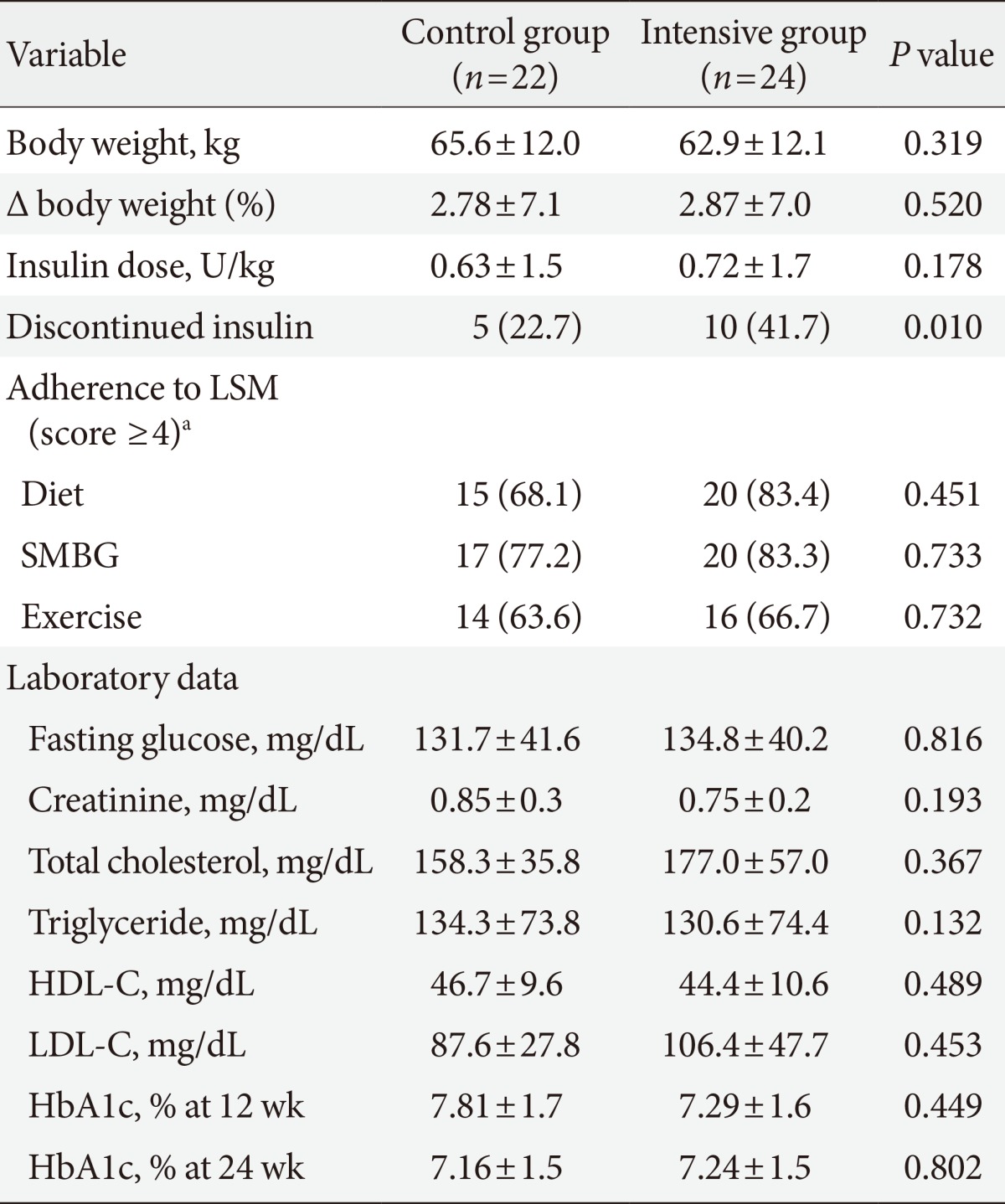
Values are presented as mean±standard deviation or number (%). The differences of body weight, insulin dose, fasting glucose, creatinine, lipid profile, and HbA1c between the control group (CG) and intensive (IT) groups at 24 weeks were analyzed by analysis of covariance (age, diabetic duration, fasting glucose, and total cholesterol were adjusted).
LSM, lifestyle modification; SMBG, self-monitoring of blood glucose; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol; HbA1c, hemoglobin A1c.
aThe scoring system was as followings: dietary habits ("How well do you follow your recommended meal plan?") (1) irregular diet with unlimited snacks; (2) irregular with intermittent snacks; (3) appropriate calories, regular diet with some snacks; (4) regular accurate calories, but few snacks; (5) tightly controlled, with no intermittent snacks. Physical activity ("How often do you undertake at least 20 minutes of physical activity, equivalent in intensity to brisk walking?") (1) never; (2) <30 minutes per week (weekly); (3) <60 minutes per week (1 to 2 times per week); (4) <120 minutes per week (3 to 4 times per week); (5) daily, >150 minutes per week. SMBG frequency ("How often do you check your glucose levels?") (1) never; (2) monthly; (3) weekly; (4) 3 to 4 times per week; (5) daily.
Figure & Data
References
Citations

- Effectiveness of the SUGAR intervention on hypoglycaemia in elderly patients with type 2 diabetes: A pragmatic randomised controlled trial
Huda Y. Almomani, Carlos Rodriguez Pascual, Paul Grassby, Keivan Ahmadi
Research in Social and Administrative Pharmacy.2023; 19(2): 322. CrossRef - A Cross-Sectional study on risk factors for severe hypoglycemia among Insulin-Treated elderly type 2 diabetes Mellitus (T2DM) patients in Singapore
Michelle Shi Min Ko, Wai Kit Lee, Li Chang Ang, Su-Yen Goh, Yong Mong Bee, Ming Ming Teh
Diabetes Research and Clinical Practice.2022; 185: 109236. CrossRef - Management Status of Patients with Type 2 Diabetes Mellitus at General Hospitals in Korea: A 5-Year Follow-Up Study
Jin Hee Jung, Jung Hwa Lee, Hyang Mi Jang, Young Na, Hee Sun Choi, Yeon Hee Lee, Yang Gyo Kang, Na Rae Kim, Jeong Rim Lee, Bok Rye Song, Kang Hee Sim
The Journal of Korean Diabetes.2022; 23(1): 64. CrossRef - Anti-hyperglycemic Medication Compliance: A Quality Assurance Project
Rayan Mamoon, Md Y Mamoon, Debbie Hermanstyne, Issac Sachmechi
Cureus.2022;[Epub] CrossRef - Randomised controlled trial of pharmacist-led patient counselling in controlling hypoglycaemic attacks in older adults with type 2 diabetes mellitus (ROSE-ADAM): A study protocol of the SUGAR intervention
Huda Y. Almomani, Carlos Rodriguez Pascual, Sayer I. Al-Azzam, Keivan Ahmadi
Research in Social and Administrative Pharmacy.2021; 17(5): 885. CrossRef - Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
Soo-Yeon Choi, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 263. CrossRef - Type 2 diabetes patients’ views on prevention of hypoglycaemia – a mixed methods study investigating self-management issues and self-identified causes of hypoglycaemia
Stijn Crutzen, Tessa van den Born-Bondt, Petra Denig, Katja Taxis
BMC Family Practice.2021;[Epub] CrossRef - Cross‐sectional analysis of emergency hypoglycaemia and outcome predictors among people with diabetes in an urban population
Chukwuma Uduku, Valentina Pendolino, Ian Godsland, Nick Oliver, Monika Reddy, Rachael T. Fothergill
Diabetic Medicine.2021;[Epub] CrossRef - Short-term efficacy of high intensity group and individual education in patients with type 2 diabetes: a randomized single-center trial
R. Reale, A. Tumminia, L. Romeo, N. La Spina, R. Baratta, G. Padova, L. Tomaselli, L. Frittitta
Journal of Endocrinological Investigation.2019; 42(4): 403. CrossRef - The role of structured education in the management of hypoglycaemia
Ahmed Iqbal, Simon R. Heller
Diabetologia.2018; 61(4): 751. CrossRef - Association of diabetes therapy-related quality of life and physical activity levels in patients with type 2 diabetes receiving medication therapy: the Diabetes Distress and Care Registry at Tenri (DDCRT 17)
Yasuaki Hayashino, Satoru Tsujii, Hitoshi Ishii
Acta Diabetologica.2018; 55(2): 165. CrossRef - Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2017; 41(5): 367. CrossRef - Antihyperglycemic Agent Therapy for Adult Patients with Type 2 Diabetes Mellitus 2017: A Position Statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
Diabetes & Metabolism Journal.2017; 41(5): 337. CrossRef - Insulin therapy for adult patients with type 2 diabetes mellitus: a position statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
The Korean Journal of Internal Medicine.2017; 32(6): 967. CrossRef - Physician-Directed Diabetes Education without a Medication Change and Associated Patient Outcomes
Hun-Sung Kim, Hyunah Kim, Hae-Kyung Yang, Eun Young Lee, Yoo Jin Jeong, Tong Min Kim, So Jung Yang, Seo Yeon Baik, Seung-Hwan Lee, Jae Hyoung Cho, In Young Choi, Hyeon Woo Yim, Bong-Yun Cha
Diabetes & Metabolism Journal.2017; 41(3): 187. CrossRef - Antihyperglycemic agent therapy for adult patients with type 2 diabetes mellitus 2017: a position statement of the Korean Diabetes Association
Seung-Hyun Ko, Kyu-Yeon Hur, Sang Youl Rhee, Nan-Hee Kim, Min Kyong Moon, Seok-O Park, Byung-Wan Lee, Hyun Jin Kim, Kyung Mook Choi, Jin Hwa Kim
The Korean Journal of Internal Medicine.2017; 32(6): 947. CrossRef - Hypoglycemia and Health Costs
Yong-ho Lee, Gyuri Kim, Eun Seok Kang
The Journal of Korean Diabetes.2016; 17(1): 11. CrossRef - Association between estimated blood glucose levels and glycated hemoglobin levels
Seon-Ah Cha, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2016; 31(3): 457. CrossRef - Characteristics of Hypoglycemia Pateints Visiting the Emergency Department of a University Hospital
Sang-Hyeon Choi, Deok-Ki Youn, Moon-Gi Choi, Ohk-Hyun Ryu
The Journal of Korean Diabetes.2016; 17(3): 202. CrossRef - Experiences of Diabetes Education among Educators of Diabetes : a content analysis approach
Soo Jin Kang, Soo Jung Chang
Journal of Korean Public Health Nursing.2016; 30(2): 221. CrossRef

 KDA
KDA


 PubReader
PubReader Cite
Cite






