Intensive Individualized Reinforcement Education Is Important for the Prevention of Hypoglycemia in Patients with Type 2 Diabetes
Article information
Abstract
Background
We investigated whether an intensive individualized reinforcement education program could influence the prevention of hypoglycemic events in patients with type 2 diabetes.
Methods
From March 2013 to September 2013, patients aged 35 to 75 years with type 2 diabetes who had not previously participated in diabetes education, and treated with insulin or a sulfonylurea-containing regimen were included in the study. After structured group education, the patients assigned to the intensive individualized education group (IT) were requested to visit for reinforcement. All subjects in the IT were encouraged to self-manage dose adjustments. Participants in both groups (control group [CG, group education only; n=22] and IT [n=24]) attended follow-up visits at 2, 8, 12, and 24 weeks. At each visit, all patients were asked whether they had experienced hypoglycemia.
Results
The total study population consisted of 20 men (43.5%; mean age and diabetic duration of 55.9±11.0 and 5.1±7.3 years, respectively). At 24 weeks, there were no significant differences in hemoglobin A1c values between the CG and IT. The total number of hypoglycemic events per patient was 5.26±6.5 in the CG and 2.58±2.3 times in the IT (P=0.004). Adherence to lifestyle modification including frequency of exercise, self-monitoring of blood glucose, or dietary habit was not significantly different between the groups. However, adherence to hypoglycemia management, especially the dose adjustment of medication, was significantly higher in the IT compared with the CG.
Conclusion
Compared with the structured group education, additional IT resulted in additional benefits in terms of avoidance of hypoglycemia and treating hypoglycemia in patients with type 2 diabetes.
INTRODUCTION
Glycemic control and treatment of diabetes should start with lifestyle modification (LSM). Because self-care behaviors such as exercise and dietary habits are recognized as important tools for the maintenance of LSM, diabetes self-management education (DSME) needs to be emphasized for patients with diabetes [1]. The benefits of DSME have been demonstrated by a number of successful studies. DSME is associated with improved diabetes knowledge and self-care behavior, improved clinical outcomes, a reduction in body weight, improved quality of life (QOL), healthy coping, and lower health care costs [2,3,4]. Both individual and group approaches have been found effective [5,6]. Diabetic patients must receive standardized DSME at the time of diagnosis and as needed thereafter [1,7]. In addition, clinical practice guidelines recommend that DSME must be provided by a certified educator who has received professional training or by a multidisciplinary care team [8]. Because DSME can result in cost-savings and improved outcomes, its cost should be supported by a third-party payer [1,7].
Hypoglycemia is a major obstacle for patients with type 2 diabetes trying to achieve glycemic targets [9,10,11]. With a steadily growing number of people with type 2 diabetes and the increased use of insulin or hypoglycemic agents for strict glycemic control, the number of diabetics with severe hypoglycemia is also increasing [12]. The fear of hypoglycemia is usually a barrier towards increasing the dosage of medication or initiating insulin treatment for patients with diabetes, although their glycemic status is not adequately controlled [13].
Previously, we investigated the long-term effectiveness of a structured intensive diabetes education program (SIDEP) in patients with type 2 diabetes [4]. We found that the SIDEP encouraged people with type 2 diabetes to attain better glycemic control, as well as better physical activity and dietary and self-monitoring of blood glucose (SMBG) habits. In general, a diabetes education program, including our group-based program, covers the knowledge and coping with hypoglycemia; however, whether our group education program could reduce the incidence of hypoglycemia remains unknown.
Therefore, we investigated the effectiveness of reinforced diabetes education for the prevention of hypoglycemia in patients with type 2 diabetes. After our SIDEP was delivered, patients were randomly assigned to the control group (CG) or the intensive individualized reinforcement education group (IT). The number of symptomatic or asymptomatic hypoglycemic episodes was the primary outcome. Glycemic control status, self-care skills, and adherence to the LSM were also measured.
METHODS
Study subjects
Type 2 diabetics aged between 35 and 75 years old who had not previously participated in a diabetes education course and been treated with insulin or sulfonylurea-containing drugs were included (n=55). Patients were excluded if they were older than 75 years of age, mentally ill, unable to participate in the recommended exercise program, suffered from alcoholism, had a malignancy, or had any severe medical illness such as sepsis, severe infection, or shock. The study protocol was approved by the Institutional Review Board of The Catholic University of Korea College of Medicine. Written informed consent was obtained from all participants.
Intensive individualized reinforcement education program
Previously, we organized our own diabetes education program based on the Dusseldorf study and the Diabetes Prevention Program [14,15]. The program was designed as group education consisting of five to 10 patients. Our education team was composed of a diabetologist, a certified diabetes educator, a psychiatrist, and a dietician. The curriculum consisted of 6, 40 minutes teaching units totaling 4 hours. The curriculum contents were structured to provide an understanding of diabetes and teach the SMBG and injection techniques, meal planning, physical activity, stress management, and sick day care with hypoglycemia management (Supplementary Table 1) [4]. During the hypoglycemia session, a diabetes educator nurse introduced the definition and symptoms of hypoglycemia and how to correct hypoglycemia with a glucose supplement.
Fifty-five people with type 2 diabetes were enrolled and attended the group program. After the group education, the patients were randomly assigned to a CG (group education only, n=27) or a IT (n=28) using a random number table. The patients assigned to the IT returned after 1 week for intensive individual education. The IT program consisted of hypoglycemia-specific lessons totaling 1 hour taught by a diabetes educator nurse. Key components of the IT program consisted of four parts: (1) detection of hypoglycemia symptoms; (2) correct management and re-checking of blood glucose levels after 15 minutes of hypoglycemia treatment; (3) possible causes as assessed by the patients themselves; and (4) dose adjustment of insulin or oral medication (Supplementary Table 2) [16]. All subjects in the IT were encouraged to self-manage dose adjustments. Their basal insulin dose titration was performed according to the mean fasting glucose level for the previous three consecutive days with the algorithm [17].
Both groups were followed up at 2, 8, 12, and 24 weeks after education. All participants continued the usual treatment provided by physicians, were scheduled for regular follow-up visits, and could contact our care team anytime by phone. Patients were asked to perform a 4-point SMBG for 14 consecutive days before each visit and whenever they had hypoglycemia symptoms. At each visit, all patients were asked whether they had experienced hypoglycemia (Fig. 1).
Measurements of clinical parameters and adherence to LSM
Hypertension was defined as a systolic blood pressure (BP) of at least 140 mm Hg or a diastolic BP of at least 90 mm Hg or having a history of treatment for hypertension. The body mass index (BMI) was calculated by the individual's weight in kilograms divided by the square of the individual's height in meters.
Blood samples were obtained after a minimum fasting time of 8 hours. Hemoglobin A1c (HbA1c) values were measured using a high-performance liquid chromatography-723 G7 system (Bio-Rad, Montreal, QC, Canada). Serum levels of fasting glucose, total cholesterol (TC), high-density lipoprotein cholesterol (HDL-C), triglycerides, and low density lipoprotein cholesterol (LDL-C) were measured enzymatically using an automatic analyzer 7600 (Hitachi, Tokyo, Japan). Diabetic nephropathy was defined as an albumin-creatinine ratio≥30 mg/g creatinine using a spot urine sample.
Adherence to LSM, dietary habits, physical activity, and the frequency of SMBG was evaluated by the subjects completing a questionnaire when they visited the hospital. Each parameter was scored using a 5-point scale based on the average status of the individual during the recent few days [4].
Measurement of hypoglycemia
At every visit, we evaluated the SMBG data and the number of episodes of hypoglycemia. Hypoglycemia was defined as a SMBG value<70 mg/dL with or without hypoglycemia symptoms [18]. If the subjects had hypoglycemic symptoms and a glucose level check was not available, the participants were allowed to eat a snack. If the hypoglycemic symptoms were relieved with the snack, the event counted as hypoglycemia [18]. The cause of hypoglycemia was classified as (1) diet (delayed or missed meal, eating less food in a meal than planned); (2) exercise (unexpected or more vigorous exercise than usual); (3) medication (no adjustment of medication in spite of lower than normal glycemic range); and (4) others (concurrent illness, unknown cause).
Statistical analysis
Statistical analyses were performed using SAS version 9.2 (SAS Institute, Cary, NC, USA). All values are presented as mean±standard deviation for continuous variables or number (%) for categorical variables. Comparison of the CG and IT was performed using an unpaired t-test, analysis of covariance, or a chi-square test. Comparison within the groups was conducted using a paired t-test. The SAS mixed procedure was used to analyze the repeated measurements of hypoglycemic events for evaluating the educational effects according to different time intervals.
We used logistic regression analysis to test associations between the outcome (hypoglycemia episodes) and potential explanatory variables after adjustment for the following prognostic factors: sex, age, BMI, duration of diabetes, presence of hypertension, diabetic retinopathy, or nephropathy, HbA1c, and the use of insulin. The results are presented as an odds ratios (ORs) and 95% confidence intervals (CIs). A P value of less than 0.05 was considered statistically significant.
RESULTS
Clinical characteristics
After randomization, there were no differences between the CG and IT in age (P=0.282), diabetic duration (P=0.125), baseline HbA1c (P=0.824), and sex ratio (P=0.107). Within the total population (n=55), 24 subjects in the IT and 22 subjects in the CG completed the follow-up at 24 weeks (follow-up loss, n=7 [CG, 5; IT, 2]; drop-out, n=2 [IT]). The participants' mean age was 55.9±11.0 years. 43.5% were men, and the mean diabetic duration was 5.1±7.3 years. The average HbA1c level was 10.7%±2.5%. Regarding the baseline clinical characteristics that were determined (n=46), there were no significant differences between the CG and IT, except for fasting plasma glucose and TC levels (Table 1).
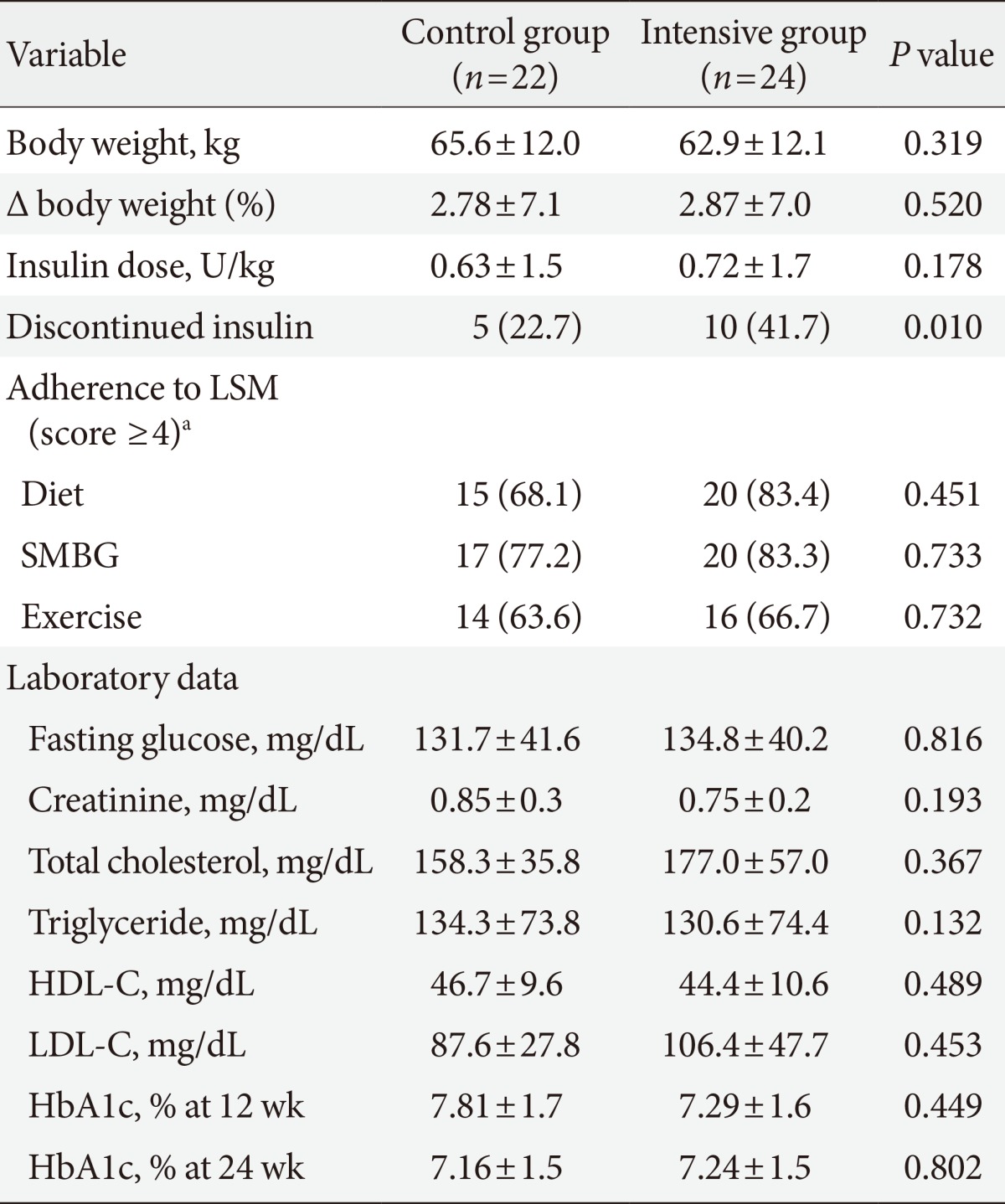
Effect of intensive education on glycemic control and LSM
At the 24 weeks follow-up visit, we observed significant improvements in HbA1c in the CG (0 week vs. 24 weeks, 11.3%±2.3% vs. 7.16%±1.5%, P<0.001) and the IT (0 week vs. 24 weeks, 10.2%±2.5% vs. 7.24%±1.5%, P<0.001). However, no significant difference was found between the CG and IT at 24 weeks (CG vs. IT, P=0.802) (Table 2). In addition, there were no significant differences between the CG and IT in body weight and LDL-C level at 24 weeks (Table 2).
Adherence to their self-care behavior, including the frequency of SMBG, physical activity, and dietary habits, was investigated using a 5-point scale. At 24 weeks, the scores greater than four were not different between the IT and CG for all three items (Table 2).
Effect of intensive education on the hypoglycemic events
At 24 weeks, hypoglycemia developed 121 times in the CG and 62 times in the IT. The 87.0% of patients in the CG and 70.8% of patients in IT experienced hypoglycemia. Total hypoglycemic events per patient during the observation period were 5.26±6.5 events in the CG and 2.58±2.3 events in the IT (P=0.004).
Overall, the number of hypoglycemic events was significantly higher in the CG compared with the IT (P=0.002), and the difference in the mean number of hypoglycemic events between the two groups was consistent across the four time periods (P for interaction=0.674). At 12 weeks, however, hypoglycemic events per patient were significantly increased in the CG compared with those in the IT (P=0.007) (Fig. 2A). The number of patients who discontinued insulin use was higher in the IT compared with those in the CG (41.7% vs. 22.7%, P=0.010). However, no difference was detected in the daily insulin dose between the groups at follow-up (Table 2). The percentage of patients who were treated with insulin was decreased in both groups (CG vs. IT, 77.3% vs. 54.2% at baseline, P=0.210; 36.4% vs. 12.5% at 24 weeks, P=0.060).
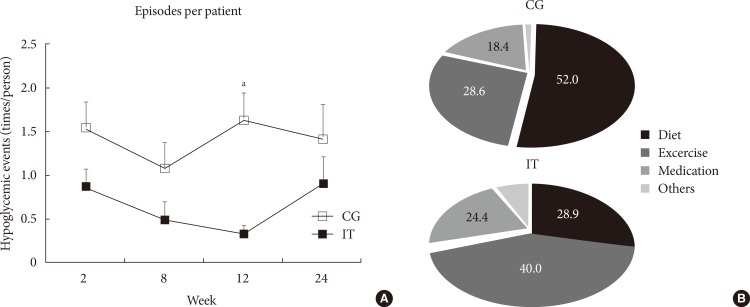
The number of hypoglycemic events per patient at each time point and causes of hypoglycemia. (A) Episodes of hypoglycemia per patient were significantly lower in the intensive group (IT) compared with the control group (CG) (P=0.002), and the difference in the mean number of hypoglycemic events between the two groups was consistent across each time point (P for interaction=0.674). At 12 weeks, however, hypoglycemic events per patient were significantly higher in the CG. (B) The causes of hypoglycemia were significantly different between the groups (P=0.029). The cause of hypoglycemia was classified as (1) diet (delayed or missed meal, eating less food in a meal than planned); (2) exercise (unexpected or more vigorous exercise than usual); (3) medication (no adjustment of medication in spite of lower than normal glycemic range); (4) others (concurrent illness, unknown cause). aP<0.05 vs. IT.
The cause of hypoglycemia was significantly different between the groups (P=0.029) (Fig. 2B). Approximately half of all hypoglycemic episodes were preceded by meal-related events before breakfast in the CG. However, unexpected or more vigorous exercise than usual was the most common antecedent of hypoglycemia in the IT.
At 24 weeks, hypoglycemia management skills, such as detection of hypoglycemia symptoms by SMBG, correct management with a snack, re-checking blood glucose levels after 15 minutes, and dose adjustment of insulin or oral medication by schedule, were assessed. The percentage of patients who adhered to hypoglycemia management, especially re-checking blood glucose and adjusting the dose of their medication, was significantly higher in the IT compared with the CG (Fig. 3).
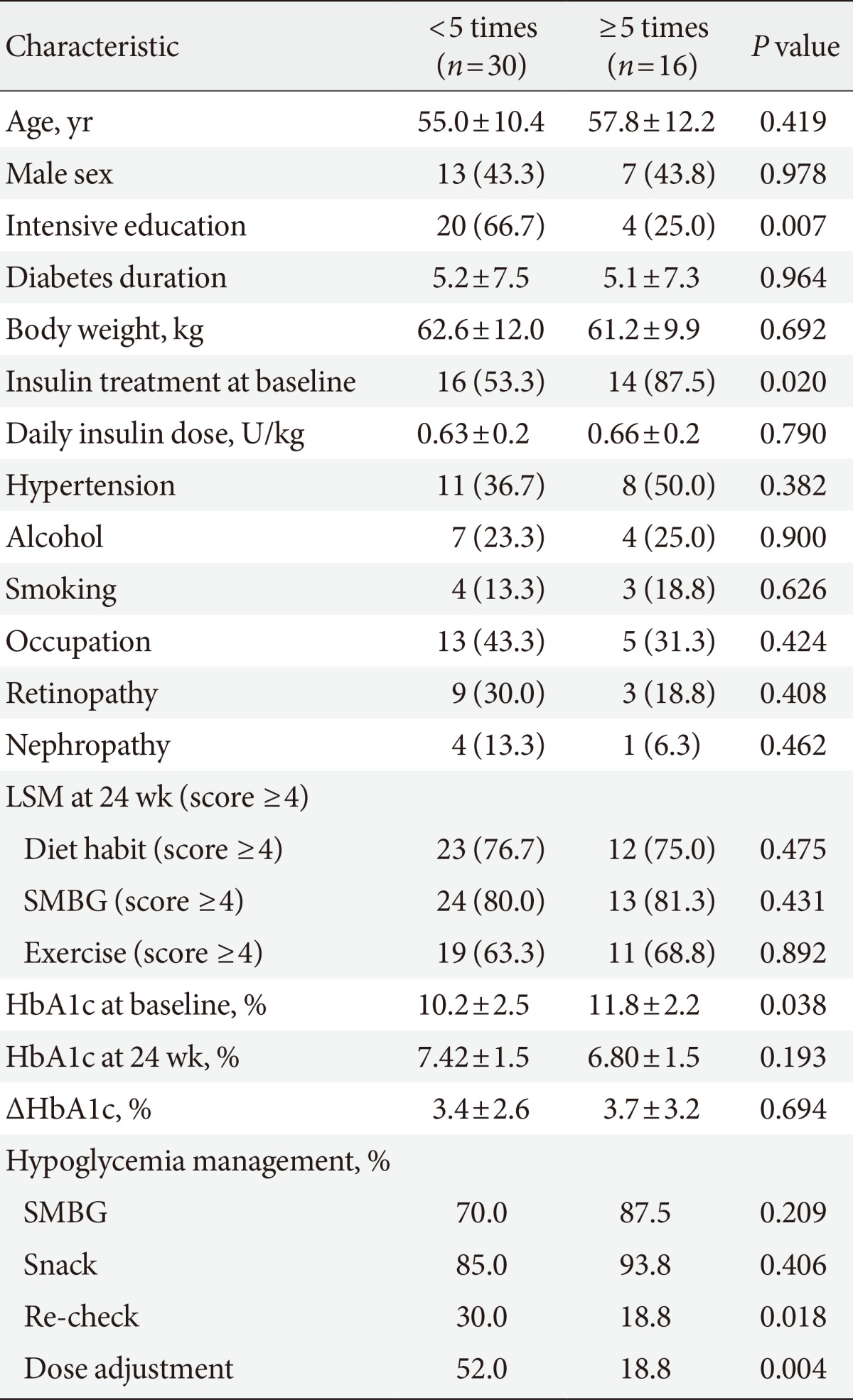
Effect of intensive reinforcement on frequency of hypoglycemia
We divided our patients according to the frequency of hypoglycemia. We compared the clinical characteristics of the subjects who experienced hypoglycemia <5 times and ≥5 times. The patients who experienced hypoglycemia ≥5 times had significantly higher baseline HbA1c levels (P=0.038) and were more frequently treated with insulin (P=0.020). In patients who experienced hypoglycemia <5 times, 66.7% experienced intensive education, but only 25.0% of those who experienced hypoglycemia ≥5 times had intensive education (Table 3). Of note, the percent of patients who adhered to hypoglycemia management, such as re-checking blood glucose and adjusting the dose of medication, was significantly higher in patients who experienced hypoglycemia <5 times compared with those who experienced hypoglycemia ≥5 times (Table 3).
Table 4 shows the association of various risk factors with the frequency of hypoglycemic events. After adjusting for age, sex, diabetic duration, presence of hypertension or diabetic complications, insulin use, and HbA1c level, intensive education for hypoglycemia management was associated with the lower incidence of hypoglycemic events (OR, 0.13; 95% CI, 0.02 to 0.74; P=0.022) (Table 4).
DISCUSSION
In this study, we investigated the effectiveness of intensive individualized diabetes education for the prevention of hypoglycemia in patients with type 2 diabetes. Hypoglycemic episodes were significantly decreased in patients with intensive individualized reinforcement compared with those with structured diabetes group education only. Of note, educating individuals about adjusting the dose of their medication after hypoglycemia seems to have been important for the prevention of recurrent hypoglycemia.
Diabetes education is an initial and essential step for diabetes care. Recently, care of diabetes has shifted to an approach that is more patient centered. In a shared decision-making approach, clinicians, and patients act as partners, and patients are involved in the decision making [19]. In addition, DSME has changed from a didactic approach focused on providing information to a more theoretically based empowerment model that focuses on helping those with diabetes make informed self-management decisions [1]. Therefore, individualized, interactive, and reinforcement of diabetic education would be more helpful for patients with diabetes than simple group lessons.
Hypoglycemia is a well-known acute complication of diabetes treatment and is considered a main barrier to achieving glycemic goals in patients with type 2 diabetes [20,21,22]. When emphasizing the importance of strict glycemic control for the prevention of diabetic vascular complications, the risk for developing hypoglycemia increased [10,11]. Older age, longer diabetic duration, and the presence of microvascular complications are known risk factors for severe hypoglycemia [23,24]. Detecting high risk populations early and providing specialized diabetic education might reduce the incidence of hypoglycemic events in patients with type 2 diabetes.
There are some clinical studies, mostly in type 1 diabetics, showing the effect of diabetes education on the development of hypoglycemia. A new education program for treating diabetic patients with hypoglycemia problems (HyPOS) aimed to avoid hypoglycemia by optimizing insulin therapy for type 1 diabetics [16]. When compared with a CG, hypoglycemia awareness significantly improved HyPOS after a 6-month follow-up period. Additionally, blood glucose awareness training (BGAT) was a psychoeducational programmatic intervention designed to improve the accuracy of patients' detection and interpretation of relevant blood glucose symptoms. BGAT led to a significant improvement in the detection of low and high blood glucose levels [25]. The dose adjustment for normal eating (DAFNE) trial was a course that taught flexible intensive insulin treatment combined with dietary freedom and insulin adjustment in type 1 diabetics in the United Kingdom [26]. Despite an increase in the number of insulin injections and encouragement to increase glucose monitoring, HbA1c was significantly improved without an increased risk of hypoglycemia in the DAFNE group compared with the CG. Therefore, diabetic education per se is an effective tool for the treatment of hypoglycemia in patients with type 1 diabetes. However, the effect of structured education on the prevention of hypoglycemia in patients with type 2 diabetes has not been well studied.
In our present study, we performed a specialized individualized reinforcement education program on hypoglycemia management after structured group education for patients with type 2 diabetes. Subjects in the IT were taught hypoglycemia management skills including frequent SMBG, glucose supplementation, re-checking of blood glucose after hypoglycemic episodes, and adjusting the dose of their medication. There were no differences in the adherence to self-care behaviors and glycemic improvement between the groups; however, hypoglycemic events were remarkably decreased after reinforcement education. We found that our program significantly improved the management skills for hypoglycemic symptoms and dose adjustment according to fasting glucose levels. The percentage of patients with adherence to hypoglycemia management was significantly higher in patients who experienced hypoglycemia less frequently. Therefore, in spite of a significant improvement in glycemic control and LSM with a structured group education program, we found that reinforcement of hypoglycemia management and dose adjustment skills would be additional benefits for the prevention of hypoglycemia in patients with type 2 diabetes.
There are some limitations in our study. Our study population included a small number of subjects, and the length of follow-up was only 6 months. We did not perform a QOL assessment related to hypoglycemia management. If hypoglycemic events were reduced with a hypoglycemia management program by patients themselves, we believe that the fear or anxiety for hypoglycemia would be decreased, and compliance to their diabetic medication or QOL would be much improved.
In summary, compared with the control (group education) group, intensive education for hypoglycemia provided additional benefits in terms of avoiding and managing hypoglycemia in patients with type 2 diabetes. Skill training in dose adjustment seemed to be a preferential target. Like an individualized glycemic goal according to one's individual clinical situation, the education curriculum should be individualized, or reinforcement should be focused on particular patient groups for the prevention of hypoglycemia. In the future, practical guidelines for the selection of high risk patients, a specific education program, and reinforcement are needed.
ACKNOWLEDGMENTS
This study was supported by a grant (KMS, 2012) from the Korean Diabetes Association.
Notes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
References
Supplementary Material
Supplementary Table 1
Group education program for both the intensive and control groups
Supplementary Table 2
Education program for the intensive individualized education group by educator nurse