- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 47(5); 2023 > Article
-
Original ArticleLifestyle Clinical Effects of a Home Care Pilot Program for Patients with Type 1 Diabetes Mellitus: A Retrospective Cohort Study
-
Sejeong Lee1,2*
 , KyungYi Kim3*
, KyungYi Kim3* , Ji Eun Kim4, Yura Hyun5, Minyoung Lee6, Myung-Il Hahm7, Sang Gyu Lee8
, Ji Eun Kim4, Yura Hyun5, Minyoung Lee6, Myung-Il Hahm7, Sang Gyu Lee8 , Eun Seok Kang6
, Eun Seok Kang6
-
Diabetes & Metabolism Journal 2023;47(5):693-702.
DOI: https://doi.org/10.4093/dmj.2022.0170
Published online: June 22, 2023
1Graduate School, Yonsei University College of Medicine, Seoul, Korea
2Division of Endocrinology and Metabolism, Department of Internal Medicine, CHA Gangnam Medical Center, CHA University School of Medicine, Seoul, Korea
3Department of Medical Device Engineering and Management, Yonsei University Graduate School, Seoul, Korea
4Department of Medical Science, Soonchunhyang University Graduate School, Asan, Korea
5Diabetes Center, Severance Hospital, Yonsei University College of Medicine, Seoul, Korea
6Division of Endocrinology and Metabolism, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
7Department of Health Administration and Management, College of Medical Science, Soonchunhyang University, Asan, Korea
8Department of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
-
Corresponding authors: Eun Seok Kang
 Division of Endocrinology and Metabolism, Department of Internal Medicine, Yonsei University College of Medicine, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea E-mail: edgo@yuhs.ac
Division of Endocrinology and Metabolism, Department of Internal Medicine, Yonsei University College of Medicine, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea E-mail: edgo@yuhs.ac -
Sang Gyu Lee
 Department of Preventive Medicine, Yonsei University College of Medicine, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea E-mail: leevan@yuhs.ac
Department of Preventive Medicine, Yonsei University College of Medicine, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea E-mail: leevan@yuhs.ac - *Sejeong Lee and KyungYi Kim contributed equally to this study as first authors.
Copyright © 2023 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Given the importance of continuous self-care for people with type 1 diabetes mellitus (T1DM), the Ministry of Health and Welfare of Korea launched a pilot program for chronic disease management. Herein, we applied a home care pilot program to people with T1DM to investigate its effects.
-
Methods
- This retrospective cohort study was conducted at a single tertiary hospital (January 2019 to October 2021). A multidisciplinary team comprising doctors, nurses, and clinical nutritionists provided specialized education and periodically assessed patients’ health status through phone calls or text messages. A linear mixed model adjusting for age, sex, and body mass index was used to analyze the glycemic control changes before and after implementing the program between the intervention and control groups.
-
Results
- Among 408 people with T1DM, 196 were enrolled in the intervention group and 212 in the control group. The reduction in glycosylated hemoglobin (HbA1c) after the program was significantly greater in the intervention group than in the control group (estimated marginal mean, –0.57% vs. –0.23%, P=0.008); the same trend was confirmed for glycoalbumin (GA) (–3.2% vs. –0.39%, P<0.001). More patients achieved the target values of HbA1c (<7.0%) and GA (<20%) in the intervention group than in the control group at the 9-month follow-up (34.5% vs. 19.6% and 46.7% vs. 28.0%, respectively).
-
Conclusion
- The home care program for T1DM was clinically effective in improving glycemic control and may provide an efficient care option for people with T1DM, and positive outcomes are expected to expand the program to include more patients.
- Type 1 diabetes mellitus (T1DM) is a chronic disease caused by impaired insulin secretion due to the destruction of pancreatic beta cells. Individuals with T1DM require life-long disease management, including insulin administration, and quarterly clinic visits are generally recommended [1]. Although most patients regularly attend outpatient clinics, usually every 3 to 6 months, visiting the outpatient clinic alone is not sufficient to adequately cope with the occasional hypoglycemic or hyperglycemic events of patients, resulting in roughly three-quarters of people with T1DM failing to achieve therapeutic targets [2]. Several studies have reported that a maximally supportive approach from a physician is helpful, as more frequent contact with the clinician is beneficial for glycemic control [3,4]. However, frequent hospital visits are difficult to achieve in clinical practice [5].
- Patient self-care, including intensive insulin therapy and frequent self-monitoring of blood glucose (SMBG), is an important aspect of managing T1DM. Considering that a significant number of people with T1DM may experience worsening glycemic control due to difficulties in adherence to consistent treatment [6], effective methods are needed to enhance self-efficacy and promote intensive insulin therapy. To compensate for the substantial insufficiency of face-to-face care, attempts have been made to improve access to patient care for T1DM from outside the health care facility using interventions such as home nursing and text messaging [7,8]. Several studies have demonstrated that additional support for patient education can help improve glycemic control and encourage routine SMBG rather than simply intensifying treatment [3,9]. Recent guidelines of the American Diabetes Association (ADA) have emphasized the importance of diabetes self-management education and support for people with T1DM to provide them with the knowledge and confidence to manage the disease daily [10].
- Considering the importance of continuous self-care for people with T1DM, the Ministry of Health and Welfare of Korea has commenced a home care pilot program for medical institutions and patients in January 2020. The program has been conducted using a multidisciplinary approach, staffed by experts in each field, including doctors, nurses, and clinical nutritionists, and intended to provide continuous education consultations from experts to people without them visiting the hospital.
- In the present study, the effect of the home care pilot program was evaluated by comparing the glycemic control of the patients enrolled in the home care program with a control group and assessing the clinical significance of the home care program for people with T1DM.
INTRODUCTION
- Ethics statements
- The study procedures were assessed and approved by the Institutional Review Board (IRB) of Severance Hospital, Yonsei University Health System, Seoul, Korea (IRB approval number: 4-2020-1198). The requirement for informed consent was waived because of the retrospective nature of the study.
- Study design
- This retrospective cohort study was conducted on people with T1DM who visited the outpatient clinic at the Division of Endocrinology and Metabolism of Severance Hospital, Seoul, Korea, from January 2019 to October 2021. T1DM was defined according to the ADA Guideline [11]. The inclusion criteria were people with T1DM with follow-up data of glycosylated hemoglobin (HbA1c, %), glycoalbumin (GA, %), fasting blood glucose (FBG, mg/dL), and GA to HbA1c ratio (GA/HbA1c ratio) every 3 months for at least 9 months since the day of recruitment. People with insufficient data and those who did not have a regular follow-up at 3-month intervals were excluded. A total of 408 study patients were divided into the intervention group (people with T1DM enrolled in the home care program between March 2020 and October 2021, n=196) or the control group (people with T1DM not enrolled in the program, n=212). All the patients in the intervention group provided written informed consent regarding enrollment in the home care program. Data were analyzed to compare the following: (1) the percentage of patients achieving the glycemic target range and (2) the clinical outcome trend over the three follow-ups (over a total of 9 months) in the intervention and control groups.
- Data collection and study variables
- All clinical data used in the study were extracted from the electronic medical records at Severance Hospital (Seoul, Korea). Clinical outcomes included HbA1c, GA, and FBG levels, and GA/HbA1c ratio, and the following data were collected as general characteristics: sex; age; duration of diabetes mellitus; height; weight; body mass index (BMI); estimated glomerular filtration rate with modification of diet in renal disease equation; and levels of uric acid, total cholesterol, albumin, aspartate aminotransferase, alanine aminotransferase, gamma-glutamyl transpeptidase, triglyceride, high-density lipoprotein cholesterol, and low-density lipoprotein cholesterol (LDL-C). LDL-C levels were calculated using Friedewald’s formula in the absence of the actual LDL-C measurement [12]. As people with T1DM usually visit the hospital at 3-month intervals, we collected the aforementioned parameters over a 9-month follow-up period.
- Home care program for people with T1DM
- The home care program was designed to provide specialized education to people with T1DM and periodically monitor their health status. Fifty-two hospitals in Korea currently participate in the program, and the program team in each institutions should include at least three professionals: doctors (internal medicine specialists with ≥2 years of experience), nurses (with ≥3 years of experience), and clinical nutritionists. The clinical protocol of the program includes the following: (1) a face-to-face educational consultation when patients visit the hospital and (2) remote care through phone calls or two-way interactive messaging to assess patient status regularly. In detail, face-to-face consultation provides detailed educational information on understanding T1DM, proper insulin dose, diverse complications, and instructions for using a glucometer, insulin pump, and continuous glucose monitoring (CGM). Unlike the control group patients, who continued with their general clinical visits, the intervention group patients were provided with detailed advice regarding issues such as insulin adjustments for specific hypoglycemic/hyperglycemic events that they might have experienced and carbohydrate-based insulin dose calculation for at least 10 minutes by their physician. For remote management, which was usually performed every 2 weeks, medical staff checked whether the patients maintained a regular diet, SMBG, and insulin administration and provided the following information tailored to the patient’s circumstances: diet and exercise management and blood glucose control instructions in specific cases.
- Patient satisfaction survey
- Among the patients in the intervention group, 72 agreed to complete additional surveys. When reimbursed for the home care program at least once (any service among physician education, nurse/clinical nutritionist consultation, or remote care through phone calls/messengers), the patient was included in the study. The survey was administered between April 13, 2021, and April 23, 2021, by four experienced researchers. Three main survey items were selected to analyze the patient satisfaction level: (1) overall satisfaction (“I am satisfied with the home care pilot program.”); (2) effectiveness (“The home care program helped increase the knowledge about managing my disease.”); and (3) behavioral intentions (“I would continue the home care pilot program and recommend it to others.”). A 4-point scale was used to measure each item: (1) strongly disagree; (2) disagree; (3) agree; and (4) strongly agree.
- Statistical analysis
- Data are presented as mean±standard deviation (SD), median with interquartile range (IQR), or number with percentage. Statistical differences between the intervention and control groups were tested using Student’s t-test and the Mann-Whitney U test for continuous variables and the chi-square test for categorical variables. A linear mixed model (LMM) was used to examine regularly measured HbA1c, GA, and FBG levels and the GA/HbA1c ratio to compare the effect of the home care program with that of conventional management.
- Statistical analyses were performed using SPSS Statistics for Windows version 25.0 (IBM Corp., Armonk, NY, USA) and R software version 3.6.3 (R Core Team, Vienna, Austria). Statistical significance was set at a P<0.05.
METHODS
- Baseline characteristics of the study population The baseline characteristics of the patients are presented in Table 1. Among the 408 patients, 42.6% were male, and the mean age of the study patients was 44.4±15.7 years. The median BMI was 22.4 kg/m2 (IQR, 20.4 to 24.6), and the median duration of diabetes was 14.0 years (IQR, 7.0 to 24.0). There were no significant demographic differences in age, sex, BMI, and duration of diabetes between the two groups. In both groups, multiple daily injection insulin therapy was mainly used, and insulin pump users accounted for the smallest proportion, namely, six patients (3.1%) in intervention group and 11 patients (5.2%) in control group; however, there was no significant difference in the type of insulin treatment between the two groups. Severe hypoglycemia requiring an emergency department visit or hospitalization occurred similarly in four (3.2%) patients and seven (3.3%) patients in the two groups, respectively. The proportion of participants who used a CGM during the study period was significantly higher in the intervention group (36.2% vs. 14.6%, P<0.001). As being included in the intervention group entailed the willingness to participate in the home care program, it may be theorized that the intervention group patients would be more motivated and familiarized with T1DM. At baseline, however, the intervention group had significantly higher HbA1c levels than the control group (8.6% vs. 8.1%, P=0.008; respectively), which means that at the baseline, the condition of the intervention group was worse than that of the control group. The mean values of GA (25.7% and 24.2%, P=0.087; respectively), FBG (158.6 and 149.3 mg/dL, P=0.183; respectively), and GA/HbA1c ratio (3.0 and 2.9, P=0.783) were higher in the intervention group than in the control group, with no statistically significant differences. Other variables, including lipid profile and liver function test results, were not significantly different between the two groups.
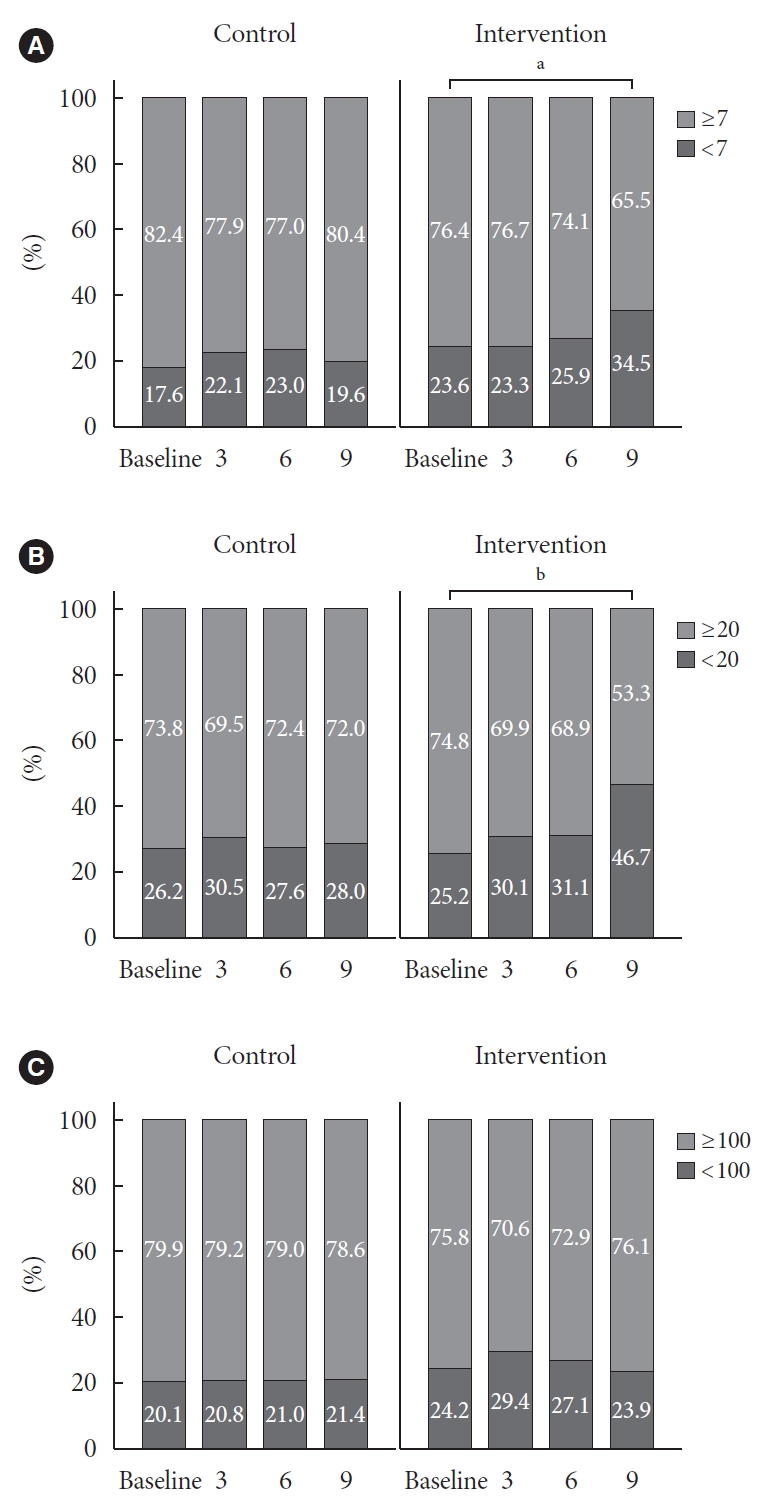
- Proportion of patients who achieved the glycemic target range
- Fig. 1 shows the percentage of the study population that reached the target range according to the ADA guideline [10]. Over the 9-month follow-up period, levels of HbA1c (Fig. 1A) and GA (Fig. 1B) in the intervention group indicated good target control and improved gradually compared to the control group. Specifically, the baseline proportion of achieving the HbA1c goal in the intervention group (23.6%) significantly increased to 34.5% at the 9-month follow-up (P=0.027). Even the levels of HbA1c in the baseline intervention group showed good target control compared to the baseline control group, it showed significant difference in outcomes across the intervention and control group. The GA also improved from baseline (25.2%) to the 9-month follow-up (46.7%) (P<0.001). Other than the aforementioned parameters, the proportion of patients who achieved the FBG goals showed no significant difference over the 9-month follow-up period (Fig. 1C).
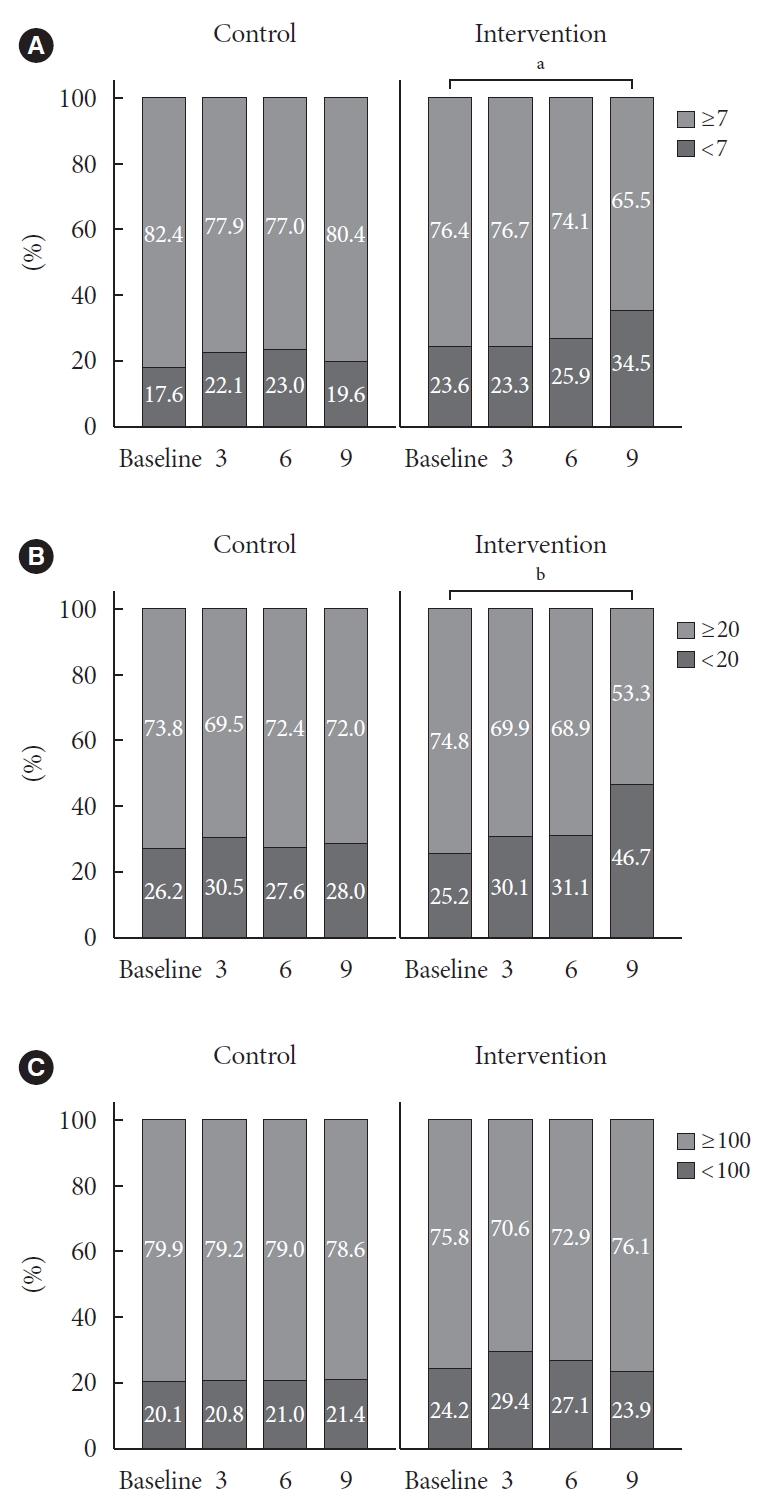
- Change of glycemic parameters after applying the home care program
- The changes in glycemic parameters over the 9-month followup period in the intervention and control groups were analyzed using LMM, and the estimated marginal mean (EMM) after adjusting for age, sex, and BMI are shown in Table 2. The reduction in glycemic parameters was greater in the intervention group than in the control group. There were significantly greater reductions in HbA1c levels in the intervention group than in the control group at the last follow-up (P=0.008). The reduction in HbA1c at the 9-month follow-up was approximately twice as large in the intervention group as that in the control group (EMM, –0.57% vs. –0.23%). This trend was also observed regarding GA and GA/HbA1c ratio. Reductions in GA were significantly larger in the intervention group than the control group at both 6 months (EMM, –2.04% vs. 0.05%, P<0.001) and 9 months (EMM, –3.20% vs. –0.39%, P<0.001). Reductions in GA/HbA1c ratio were significantly larger in the intervention group than the control group at both 6 months (EMM, –0.05 vs. 0.06, P=0.037) and 9 months (EMM, –0.13 vs. 0.04, P=0.008). However, no significant differences in FBG levels were found in all three follow-ups (P>0.05). In the comparison of the differences between the two groups at each time point (Fig. 2), the GA level (P=0.010) and the GA/HbA1c ratio (P=0.027) at follow-up after 9 months showed a significant difference.
- In order to investigate the glycemic effect according to CGM use, subgroup analysis was performed by dividing participants into subgroups accordingly. In the subgroup analysis, the intervention group in both subgroups showed the same trend of decreasing glycemic parameters after the program implementation, similar to all the participants, but in CGM users, only GA at 6 months showed a significant difference (Supplementary Tables 1 and 2). CGM parameters, including time in range (TIR), mean glucose, coefficient of variation, and active usage time percentage of CGM were improved at the 9-month follow-up (Supplementary Table 3). TIR, which is the percentage of the day that blood glucose levels stay within the target range (standard range of 80 to 170 mg/dL), increased from 44% to 57%, indicating improvement in the overall percentage of time with a healthy glucose range. Additionally, active usage time increased from 74% to 89%, meaning blood glucose was monitored more frequently after the intervention.
- Patient satisfaction
- A summary of the patient satisfaction survey results is presented in Table 3. The overall satisfaction (3.42±0.65), effectiveness (3.40±0.66), and behavioral intention (3.50±0.69) were generally positive based on the 4-point scale. Overall satisfaction was higher in subgroups with age >50 years, male sex, high education level, low monthly income, and low subjective health status. In terms of effectiveness, the overall trend was similar to that of overall satisfaction, but age between 30 and 49 years and the mid-level monthly income subgroup were associated with better outcomes. The behavioral intention was especially high in the subgroup with high subjective health status.
RESULTS
- In people with T1DM, the importance of self-care and educational support has been emphasized more compared to many other chronic conditions [13]. Despite its perceived importance, little attention has been paid to specific interventions to optimize self-management in people with T1DM. In this study, we formed a team of health care professionals to establish a system that provides multidisciplinary telemedical services and demonstrated that glycemic control could be improved by supporting the self-management of people with T1DM. After implementing the home care program for 9 months, gradually, over time, more patients who participated in the program reached their glycemic goals. In addition, the absolute value of the glycemic variable in the intervention group gradually decreased over time, indicating improved diabetes control without severe hypoglycemia. However, unlike improvements in HbA1c level, GA level, and GA/HbA1c ratio, the home care program did not significantly affect the FBG level. Similar results were found in studies where a mobile application program focused on women with gestational diabetes was implemented [14,15]. This may be because FBG is a temporary marker of blood glucose on the day of the test with high variability, whereas other indicators are values that represent relatively long-term average values. In addition, the GA/HbA1c ratio is an indicator of glycemic variability [16], and there was no significant difference in HbA1c levels between the two groups at 9 months post-intervention. This indicates that the program mainly improved postprandial glucose levels. Postprandial glucose excursion in people with T1DM contributes significantly to the overall glycemic burden, and achieving optimal postprandial glucose control remains a key component to achieving the recommended glycemic target [17]. These results might indicate that the intervention of multidisciplinary experts affected detailed postprandial glucose control, which is a multifactorial phenomenon affected by factors such as the composition and quantity of meals and the timing and dose of insulin.
- In subgroup analysis, the overall effectiveness of the home care program was better for non-CGM users than for CGM users. These results may indicate that the effect of the program on improving glycemic control is largely attributed to promoting frequent self-monitoring of glucose in the patients.
- In terms of patient satisfaction, this study showed a positive result, as the patients felt that the home care program was overall effective and were willing to continue participating in the program after the study was completed. A study of smartphone-based diabetes self-management applications found that the higher the user satisfaction, the greater the improvement in diabetes self-management activities [18]. Since T1DM, a chronic disease, is generally associated with high distress, self-reported satisfaction with the program could lead to changes in patient behavior, which may contribute to favorable clinical outcomes [19].
- Previous studies, including several important reviews of diabetes education and its efficacy, have provided evidence of the positive effect of education on people with diabetes [20,21]. As technological innovations become applicable to practical diabetes management, home care has become an attractive option for patient education. A systematic review and meta-analysis of 38 randomized controlled trials on the effects of home care on T1DM noted positive effects on glycemic control, with a mean reduction in HbA1c of 0.18% at the end of the intervention [22]. In contrast, some previous studies on the clinical benefits of telemedical support in people with diabetes have failed to show clear improvements in HbA1c levels or other outcomes [23-25]. In a study of 57 Korean people with T1DM participating in an Internet mentoring program, the program implementation increased the frequency of SMBG, but glycemic control was not demonstrated to be superior to the usual follow-up [25], which was suspected to be due to the small number of patients and the limited follow-up duration. In the Sweet Talk trial [3], which was conducted for a longer period with a large number of participants, the scheduled text messaging system increased self-efficacy and adherence to intensive insulin therapy in young people with T1DM. The study found an effect on emotional or psychological outcomes; however, this did not translate into improvements in glycemic control in all groups and was only effective in the group receiving intensive insulin therapy. Home care services reported in previous studies [3,25] primarily included the automatic delivery of a series of messages consisting of reminders to promote insulin injections and exercise or a web-based protocol provided by volunteer mentors who were patients themselves or a parent of a patient rather than a health care professional. This study, however, differed in that each patient was individually assessed and received personalized care, and bidirectional intervention from certified educators with a multidisciplinary care team was provided.
- The ADA’s HbA1c target of <7% [10] was achieved in only 21% of adult people with T1DM in the United States [26] and in 13.2% of patients in Brazil [27], and ideal glycemic control is achieved in less than a quarter of individuals with T1DM. In the present study, the control group maintained similar outcomes (19.6%), but 34.5% of the patients who participated in the self-care program achieved their goals after 9 months, demonstrating the feasibility of using a home care program in diabetes management. The average HbA1c level in the other study participants was 9% to 10%, whereas that in the patients in the current study was 8%, indicating that it was more difficult for the people with better glycemic control to improve further compared to their counterparts [22]. In addition, considering that the patients of this study exhibited satisfactory compliance to their guided schedule, it is important that there were improvements in achieving the glycemic target without additional hospital visits. On the other hand, satisfactory compliance may have had a positive effect on the outcome of the program by allowing them to follow the expert’s opinion and apply it to their self-care.
- The task of navigating between hyperglycemia and hypoglycemia in daily life can be a significant burden for people with T1DM. However, an increasing number of people with diabetes and an undersupply of diabetes specialists cause time constraints and limit clinic appointments. Because of these limitations, patients have few opportunities to interact with their physicians and often fail to implement the specific medical advice provided by doctors [14]. Most patients do not remember all the medical instruments received at the clinic, and many forget information after leaving the clinic [28]. Therefore, periodic reminders are needed so patients can keep up with their daily regimen. Additionally, the home care program may have enabled patients to discuss medical problems encountered in their daily lives that were not adequately addressed within regular consultation hours. As pointed out in a previous study [15] that demonstrated that the total contact time between patients and educators was an important predictor of improved glycemic control, home care has the advantage of allowing adequate time spent with people within existing health service resources.
- In addition, from the perspective of health care providers, they could immediately respond to patients’ concerns in real time and monitor their actual lifestyle outside the clinic to jointly provide individualized support for behavioral modification. Another major benefit of this home care program is its potential to reduce costs without compromising its clinical effectiveness [29]. It could be cost-effective by reducing hyperglycemic events and minimizing acute complications that lead to emergency department visits or unplanned hospitalizations.
- Home care programs delivered by health care professionals can be an optional strategy to improve patients’ glycemic control within health service resources. Although it cannot replace face-to-face contact with a practitioner, it can provide consistent health care support between visits. The development of standardized materials for education programs and organizational infrastructure is needed to help patients achieve optimal glycemic control and improve their quality of life.
- This study has several limitations. First, there was a short study period of 9 months to determine the effect of the program on the prevention of diabetes complications or mortality. Further research over a longer period is needed in the future. Second, the study was performed in a single tertiary care hospital with sufficient medical staff. Hence, this study’s results probably underrepresent patients in a primary care center, and it is not appropriate to extend the interpretation of our results to all people with T1DM. Because remote patient management may require additional tasks such as phone calls, two-way messaging, or consultation, sufficient human resources are needed in advance. Further multicenter studies with more patients and longer periods would be helpful to demonstrate the effectiveness of the home care program. In addition, this study did not include people with T1DM younger than 19 years, as we targeted people with T1DM older than 20 years. Considering the high incidence rate of T1DM in younger patients, it is recommended to include this age group in the following study. Lastly, as the patient satisfaction survey was conducted only for the intervention group who had participated in the home care program, we could not compare the difference between the two groups but assessed the overall satisfaction levels regarding the program. Despite these limitations, we discovered several meaningful implications of the program.
- In conclusion, this study showed that the home care pilot program resulted in significant improvements in glycemic control over a 9-month period. Additional research is needed to examine the long-term impact of the program and its feasibility in people with T1DM.
DISCUSSION
SUPPLEMENTARY MATERIALS
Supplementary Table 1.
Supplementary Table 2.
Supplementary Table 3.
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conception or design: S.L., K.Y.K., S.G.L., E.S.K.
Acquisition, analysis, or interpretation of data: S.L., K.Y.K., J.E.K., M.L.
Drafting the work or revising: S.L., K.Y.K., Y.H., M.I.H.
Final approval of the manuscript: S.G.L., E.S.K.
-
FUNDING
This study was supported by a Severance Hospital Research fund for Clinical excellence (SHRC) (C-2021-0007).
NOTES
-
Acknowledgements
- None
| Characteristic | Control (n=212) | Intervention (n=196) | P value |
|---|---|---|---|
| Age, yr | 45.4±16.0 | 43.3±15.3 | 0.173 |
| Sex | 0.124 | ||
| Male | 101 (47.6) | 73 (37.2) | |
| Female | 111 (52.4) | 123 (62.8) | |
| DM duration, yr | 15.5 (8.5–24.5) | 14.0 (7.0–23.0) | 0.136 |
| BMI, kg/m2 | 22.5 (20.7–24.6) | 22.0 (20.2–24.7) | 0.219 |
| FBG, mg/dL | 149.3±63.3 | 158.6±75.8 | 0.183 |
| HbA1c, % | 8.1±1.6 | 8.6±1.9 | 0.008 |
| GA, % | 24.2±6.3 | 25.7±8.4 | 0.087 |
| GA/HbA1c ratio | 2.9 (2.6–3.2) | 3.0 (2.7–3.3) | 0.783 |
| eGFR, mL/min/1.73 m2 | 89.7 (71.6–103.5) | 88.6 (74.0–102.3) | 0.990 |
| Uric acid, mg/dL | 4.4 (4.1–4.5) | 4.4 (3.6–5.3) | 0.757 |
| Albumin, g/dL | 4.3 (4.1–4.5) | 4.3 (4.1–4.5) | 0.197 |
| AST, IU/L | 19.0 (15.0–24.0) | 19.0 (16.0–24.0) | 0.583 |
| ALT, IU/L | 16.0 (12.0–23.0) | 16.0 (12.0–23.0) | 0.736 |
| γ-GT, IU/L | 19.5 (15.0–33.0) | 19.5 (13.5–27.5) | 0.395 |
| TC, mg/dL | 171.0 (148.5–191.0) | 171.5 (153.5–196.0) | 0.330 |
| TG, mg/dL | 86.0 (61.5–109.0) | 85.0 (61.5–115.5) | 0.779 |
| HDL-C, mg/dL | 60.0 (47.0–72.0) | 61.0 (51.0–72.0) | 0.396 |
| LDL-C, mg/dL | 90.0 (67.9–106.6) | 89.8 (71.2–112.1) | 0.410 |
| Insulin treatment | |||
| MDI | 175 (82.5) | 176 (89.8) | 0.108 |
| Pre-mixed | 26 (12.3) | 14 (7.1) | |
| Insulin pump | 11 (5.2) | 6 (3.1) | |
| CGM users | |||
| Yes | 31 (14.6) | 71 (36.2) | <0.001 |
| No | 181 (85.4) | 125 (63.8) | |
| Severe hypoglycemiaa | 7 (3.3) | 4 (3.2) | 1.000 |
Values are presented as mean±standard deviation, number (%), or median (interquartile range).
DM, diabetes mellitus; BMI, body mass index; FBG, fasting blood glucose; HbA1c, glycosylated hemoglobin; GA, glycoalbumin; eGFR, estimated glomerular filtration rate; AST, aspartate aminotransferase; ALT, alanine aminotransferase; γ-GT, gamma-glutamyl transpeptidase; TC, total cholesterol; TG, triglyceride; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol; MDI, multiple daily injection; CGM, continuous glucose monitoring system.
a This category included any episode of hypoglycemia that require emergency department visits or hospitalizations.
| Outcomes |
EMM (95% CI) |
P valuea | |
|---|---|---|---|
| Control group | Intervention group | ||
| HbA1c, % | |||
| 3 months | –0.15 (–0.22 to –0.08) | –0.29 (–0.37 to 0.21) | 0.218 |
| 6 months | –0.22 (–0.30 to –0.15) | –0.39 (–0.47 to 0.31) | 0.170 |
| 9 months | –0.23 (–0.32 to –0.15) | –0.57 (–0.66 to –0.49) | 0.008 |
| GA, % | |||
| 3 months | –0.40 (–0.79 to –0.01) | –1.12 (–1.49 to –0.75) | 0.207 |
| 6 months | 0.05 (–0.37 to 0.48) | –2.04 (–2.43 to –1.65) | <0.001 |
| 9 months | –0.39 (–0.84 to 0.08) | –3.20 (–3.60 to –2.79) | <0.001 |
| FBG, mg/dL | |||
| 3 months | –2.60 (–9.17 to 3.97) | –10.44 (–17.28 to –3.60) | 0.345 |
| 6 months | –1.41 (–8.74 to 5.92) | –8.58 (–16.03 to –1.13) | 0.485 |
| 9 months | –10.59 (–19.53 to –1.65) | –7.60 (–19.07 to 3.87) | 0.810 |
| GA/HbA1c ratio | |||
| 3 months | 0.02 (–0.02 to 0.06) | –0.03 (–0.07 to 0.01) | 0.272 |
| 6 months | 0.06 (0.02 to 0.10) | –0.05 (–0.09 to –0.01) | 0.037 |
| 9 months | 0.04 (–0.01 to 0.09) | –0.13 (–0.17 to –0.09) | 0.008 |
- 1. Phan TL, Hossain J, Lawless S, Werk LN. Quarterly visits with glycated hemoglobin monitoring: the sweet spot for glycemic control in youth with type 1 diabetes. Diabetes Care 2014;37:341-5.ArticlePubMedPDF
- 2. Mannucci E, Monami M, Dicembrini I, Piselli A, Porta M. Achieving HbA1c targets in clinical trials and in the real world: a systematic review and meta-analysis. J Endocrinol Invest 2014;37:477-95.ArticlePubMedPDF
- 3. Franklin VL, Waller A, Pagliari C, Greene SA. A randomized controlled trial of Sweet Talk, a text-messaging system to support young people with diabetes. Diabet Med 2006;23:1332-8.ArticlePubMed
- 4. Lehmkuhl HD, Storch EA, Cammarata C, Meyer K, Rahman O, Silverstein J, et al. Telehealth behavior therapy for the management of type 1 diabetes in adolescents. J Diabetes Sci Technol 2010;4:199-208.ArticlePubMedPMCPDF
- 5. Iqbal A, Novodvorsky P, Heller SR. Recent updates on type 1 diabetes mellitus management for clinicians. Diabetes Metab J 2018;42:3-18.ArticlePubMedPMCPDF
- 6. Cameron FJ, Garvey K, Hood KK, Acerini CL, Codner E. ISPAD Clinical Practice Consensus Guidelines 2018: diabetes in adolescence. Pediatr Diabetes 2018;19 Suppl 27:250-61.ArticlePubMedPDF
- 7. Offringa R, Sheng T, Parks L, Clements M, Kerr D, Greenfield MS. Digital diabetes management application improves glycemic outcomes in people with type 1 and type 2 diabetes. J Diabetes Sci Technol 2018;12:701-8.ArticlePubMedPMCPDF
- 8. Rami B, Popow C, Horn W, Waldhoer T, Schober E. Telemedical support to improve glycemic control in adolescents with type 1 diabetes mellitus. Eur J Pediatr 2006;165:701-5.ArticlePubMedPDF
- 9. McGill DE, Laffel LM, Volkening LK, Butler DA, Levy WL, Wasserman RM, et al. Text message intervention for teens with type 1 diabetes preserves HbA1c: results of a randomized controlled trial. Diabetes Technol Ther 2020;22:374-82.ArticlePubMedPMC
- 10. Holt RI, DeVries JH, Hess-Fischl A, Hirsch IB, Kirkman MS, Klupa T, et al. The management of type 1 diabetes in adults: a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2021;44:2589-625.ArticlePubMedPDF
- 11. American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes-2021. Diabetes Care 2021;44(Suppl 1):S15-33.ArticlePubMedPDF
- 12. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem 1972;18:499-502.ArticlePubMedPDF
- 13. Beck J, Greenwood DA, Blanton L, Bollinger ST, Butcher MK, Condon JE, et al. 2017 National standards for diabetes self-management education and support. Diabetes Care 2017;40:1409-19.ArticlePubMedPDF
- 14. Guo H, Zhang Y, Li P, Zhou P, Chen LM, Li SY. Evaluating the effects of mobile health intervention on weight management, glycemic control and pregnancy outcomes in patients with gestational diabetes mellitus. J Endocrinol Invest 2019;42:709-14.ArticlePubMedPDF
- 15. Norris SL, Lau J, Smith SJ, Schmid CH, Engelgau MM. Self-management education for adults with type 2 diabetes: a meta-analysis of the effect on glycemic control. Diabetes Care 2002;25:1159-71.PubMed
- 16. Imai T, Oikawa Y, Shimada A. Improved monitoring of the hyperglycemic state in type 1 diabetes patients by use of the glycoalbumin/HbA1c ratio. Rev Diabet Stud 2007;4:44-8.ArticlePubMedPMC
- 17. Ceriello A, Hanefeld M, Leiter L, Monnier L, Moses A, Owens D, et al. Postprandial glucose regulation and diabetic complications. Arch Intern Med 2004;164:2090-5.ArticlePubMed
- 18. Kim YJ, Rhee SY, Byun JK, Park SY, Hong SM, Chin SO, et al. A smartphone application significantly improved diabetes self-care activities with high user satisfaction. Diabetes Metab J 2015;39:207-17.ArticlePubMedPMC
- 19. Jalil S, Myers T, Atkinson I. A meta-synthesis of behavioral outcomes from telemedicine clinical trials for type 2 diabetes and the Clinical User-Experience Evaluation (CUE). J Med Syst 2015;39:28.ArticlePubMedPDF
- 20. Kim MY, Suh S, Jin SM, Kim SW, Bae JC, Hur KY, et al. Education as prescription for patients with type 2 diabetes mellitus: compliance and efficacy in clinical practice. Diabetes Metab J 2012;36:452-9.ArticlePubMedPMC
- 21. Shiferaw WS, Akalu TY, Desta M, Kassie AM, Petrucka PM, Aynalem YA. Effect of educational interventions on knowledge of the disease and glycaemic control in patients with type 2 diabetes mellitus: a systematic review and meta-analysis of randomised controlled trials. BMJ Open 2021;11:e049806.ArticlePubMedPMC
- 22. Lee SW, Ooi L, Lai YK. Telemedicine for the management of glycemic control and clinical outcomes of type 1 diabetes mellitus: a systematic review and meta-analysis of randomized controlled studies. Front Pharmacol 2017;8:330.ArticlePubMedPMC
- 23. Whittemore R, Jaser SS, Jeon S, Liberti L, Delamater A, Murphy K, et al. An internet coping skills training program for youth with type 1 diabetes: six-month outcomes. Nurs Res 2012;61:395-404.PubMedPMC
- 24. Gay CL, Chapuis F, Bendelac N, Tixier F, Treppoz S, Nicolino M. Reinforced follow-up for children and adolescents with type 1 diabetes and inadequate glycaemic control: a randomized controlled trial intervention via the local pharmacist and telecare. Diabetes Metab 2006;32:159-65.ArticlePubMed
- 25. Suh S, Jean C, Koo M, Lee SY, Cho MJ, Sim KH, et al. A randomized controlled trial of an internet-based mentoring program for type 1 diabetes patients with inadequate glycemic control. Diabetes Metab J 2014;38:134-42.ArticlePubMedPMC
- 26. Foster NC, Beck RW, Miller KM, Clements MA, Rickels MR, DiMeglio LA, et al. State of type 1 diabetes management and outcomes from the T1D exchange in 2016-2018. Diabetes Technol Ther 2019;21:66-72.ArticlePubMedPMC
- 27. Gomes MB, Coral M, Cobas RA, Dib SA, Canani LH, Nery M, et al. Prevalence of adults with type 1 diabetes who meet the goals of care in daily clinical practice: a nationwide multicenter study in Brazil. Diabetes Res Clin Pract 2012;97:63-70.ArticlePubMed
- 28. Shankar J. Patients’ memory for medical information. J R Soc Med 2003;96:520.ArticlePDF
- 29. McCarroll Z, Townson J, Pickles T, Gregory JW, Playle R, Robling M, et al. Cost-effectiveness of home versus hospital management of children at onset of type 1 diabetes: the DECIDE randomised controlled trial. BMJ Open 2021;11:e043523.ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations

- Glycemic outcomes and patient satisfaction and self-management improves in transition from standard to virtual multidisciplinary care
Noga Minsky, Liat Arnon Klug, Tatyana Kolobov, Elizabeth Tarshish, Yuval Shalev Many, Aviva Lipsitz, Amna Jabarin, Nicole Morozov, Dania Halperin, Moshe Shalom, Rachel Nissanholtz-Gannot, Genya Aharon-Hananel, Amir Tirosh, Orly Tamir
Diabetes Research and Clinical Practice.2024; 209: 111587. CrossRef
- Figure
- Related articles
-
- The Beneficial Effect of Glycemic Control against Adverse Outcomes in Patients with Type 2 Diabetes Mellitus and Chronic Kidney Disease
- Low Household Income Status and Death from Pneumonia in People with Type 2 Diabetes Mellitus: A Nationwide Study
- Safety of COVID-19 Vaccines among Patients with Type 2 Diabetes Mellitus: Real-World Data Analysis
- Glycemia according to the Use of Continuous Glucose Monitoring among Adults with Type 1 Diabetes Mellitus in Korea: A Real-World Study
- Safety and Effectiveness of Empagliflozin in Korean Patients with Type 2 Diabetes Mellitus: Results from a Nationwide Post-Marketing Surveillance

 KDA
KDA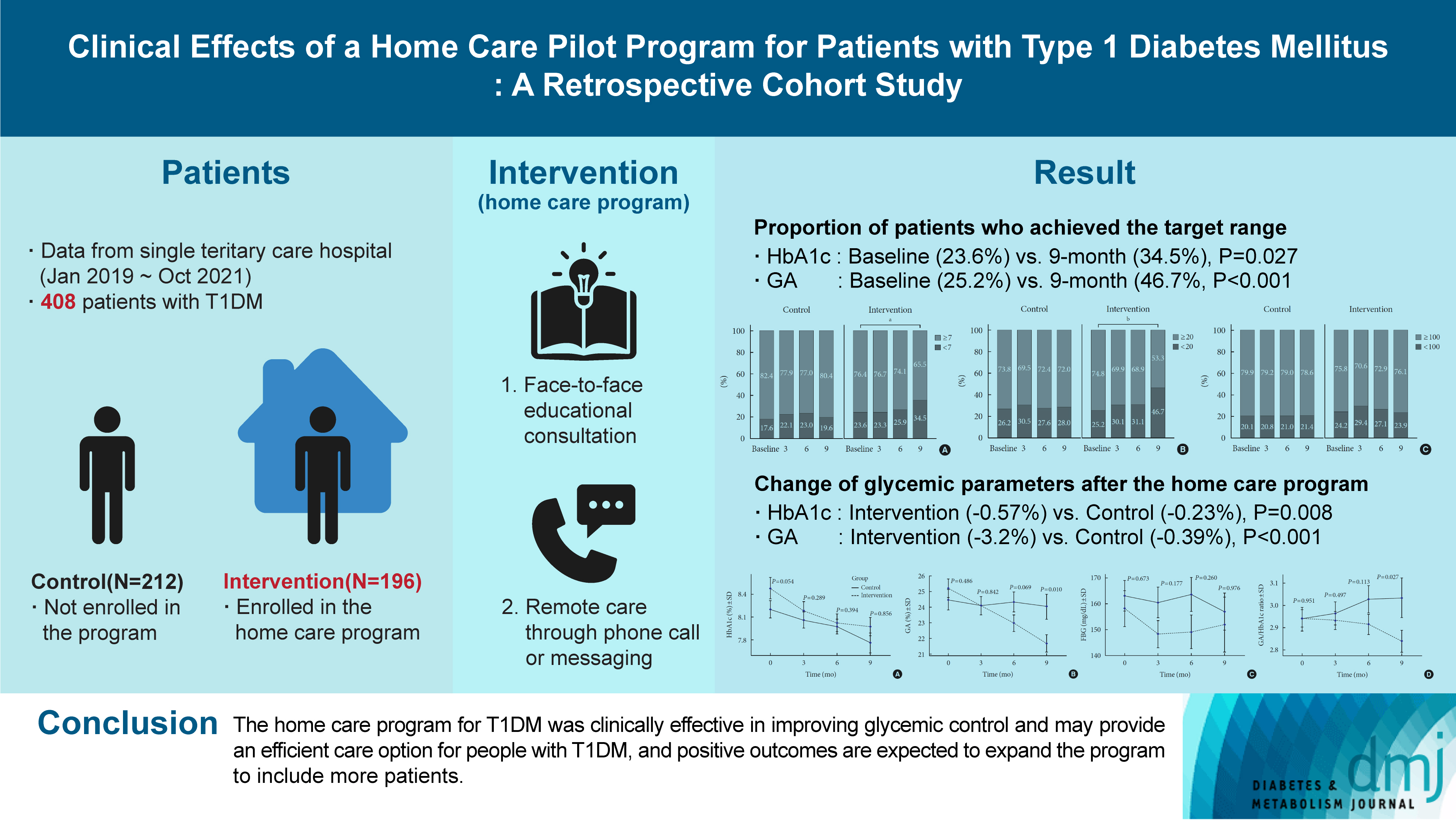
 PubReader
PubReader ePub Link
ePub Link Cite
Cite