- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 47(3); 2023 > Article
-
Original ArticleDrug/Regimen Risk of Diabetic Retinopathy between Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists
-
Tzu-Yi Lin1,2
 , Eugene Yu-Chuan Kang2,3,4
, Eugene Yu-Chuan Kang2,3,4 , Shih-Chieh Shao5,6, Edward Chia-Cheng Lai6, Sunir J. Garg7, Kuan-Jen Chen2,3, Je-Ho Kang8, Wei-Chi Wu2,3, Chi-Chun Lai2,3, Yih-Shiou Hwang2,3,9
, Shih-Chieh Shao5,6, Edward Chia-Cheng Lai6, Sunir J. Garg7, Kuan-Jen Chen2,3, Je-Ho Kang8, Wei-Chi Wu2,3, Chi-Chun Lai2,3, Yih-Shiou Hwang2,3,9
-
Diabetes & Metabolism Journal 2023;47(3):394-404.
DOI: https://doi.org/10.4093/dmj.2022.0221
Published online: March 6, 2023
1Department of Education, Chang Gung Memorial Hospital, Linkou Medical Center, Taoyuan, Taiwan
2College of Medicine, Chang Gung University, Taoyuan, Taiwan
3Department of Ophthalmology, Chang Gung Memorial Hospital, Linkou Medical Center, Taoyuan, Taiwan
4Graduate Institute of Clinical Medical Sciences, College of Medicine, Chang Gung University, Taoyuan, Taiwan
5Department of Pharmacy, Keelung Chang Gung Memorial Hospital, Keelung, Taiwan
6School of Pharmacy, Institute of Clinical Pharmacy and Pharmaceutical Sciences, College of Medicine, National Cheng Kung University, Tainan, Taiwan
7MidAtlantic Retina, The Retina Service of Wills Eye Hospital, Thomas Jefferson University, Philadelphia, PA, USA
8Department of Nephrology, Yang Ming Hospital, Taoyuan, Taiwan
9Department of Ophthalmology, Jen-Ai Hospital Dali Branch, Taichung, Taiwan
-
Corresponding authors: Eugene Yu-Chuan Kang
 Department of Ophthalmology, Chang Gung Memorial Hospital, Linkou Medical Center, No. 5, Fu Shin St., Kuei-Shan, Taoyuan 333, Taiwan E-mail: yckang0321@gmail.com
Department of Ophthalmology, Chang Gung Memorial Hospital, Linkou Medical Center, No. 5, Fu Shin St., Kuei-Shan, Taoyuan 333, Taiwan E-mail: yckang0321@gmail.com -
Yih-Shiou Hwang
 Department of Ophthalmology, Chang Gung Memorial Hospital, Linkou Medical Center, No. 5, Fu Shin St., Kuei-Shan, Taoyuan 333, Taiwan E-mail: yihshiou.hwang@gmail.com
Department of Ophthalmology, Chang Gung Memorial Hospital, Linkou Medical Center, No. 5, Fu Shin St., Kuei-Shan, Taoyuan 333, Taiwan E-mail: yihshiou.hwang@gmail.com
Copyright © 2023 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (https://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
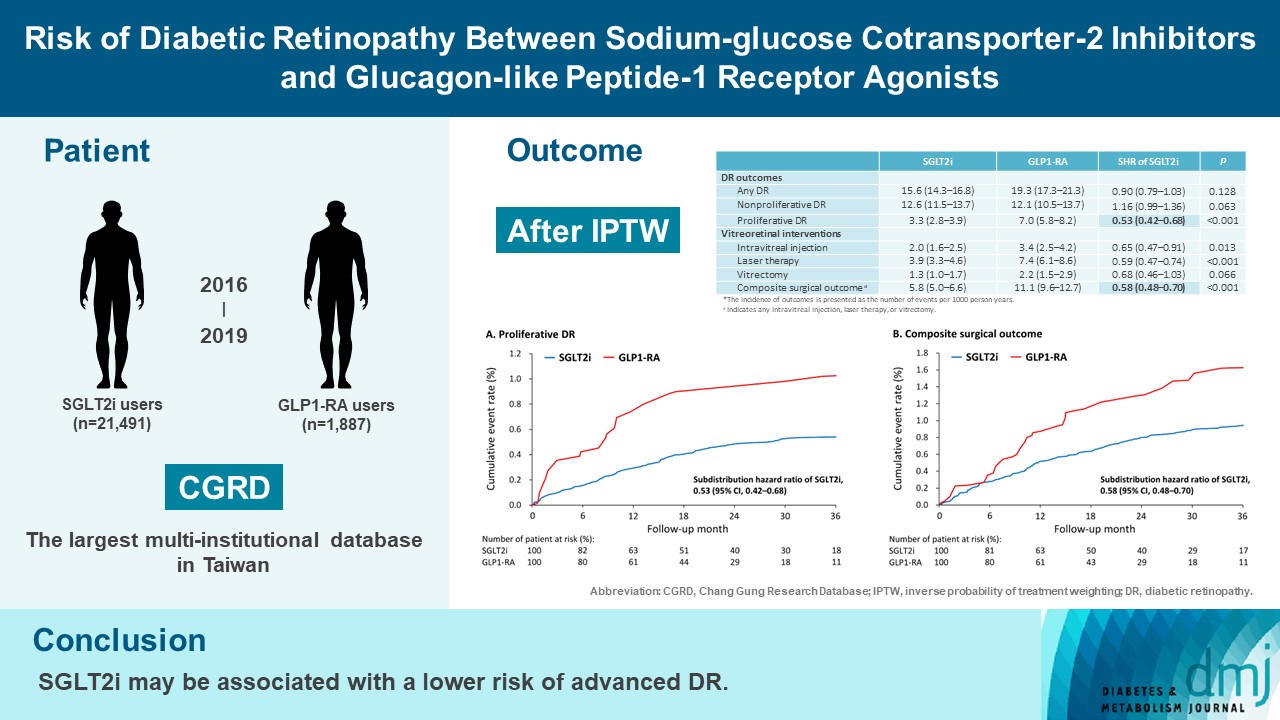
Background
- To compare risk of diabetic retinopathy (DR) between patients taking sodium-glucose cotransporter-2 inhibitors (SGLT2is) and those taking glucagon-like peptide-1 receptor agonists (GLP1-RAs) in routine care.
-
Methods
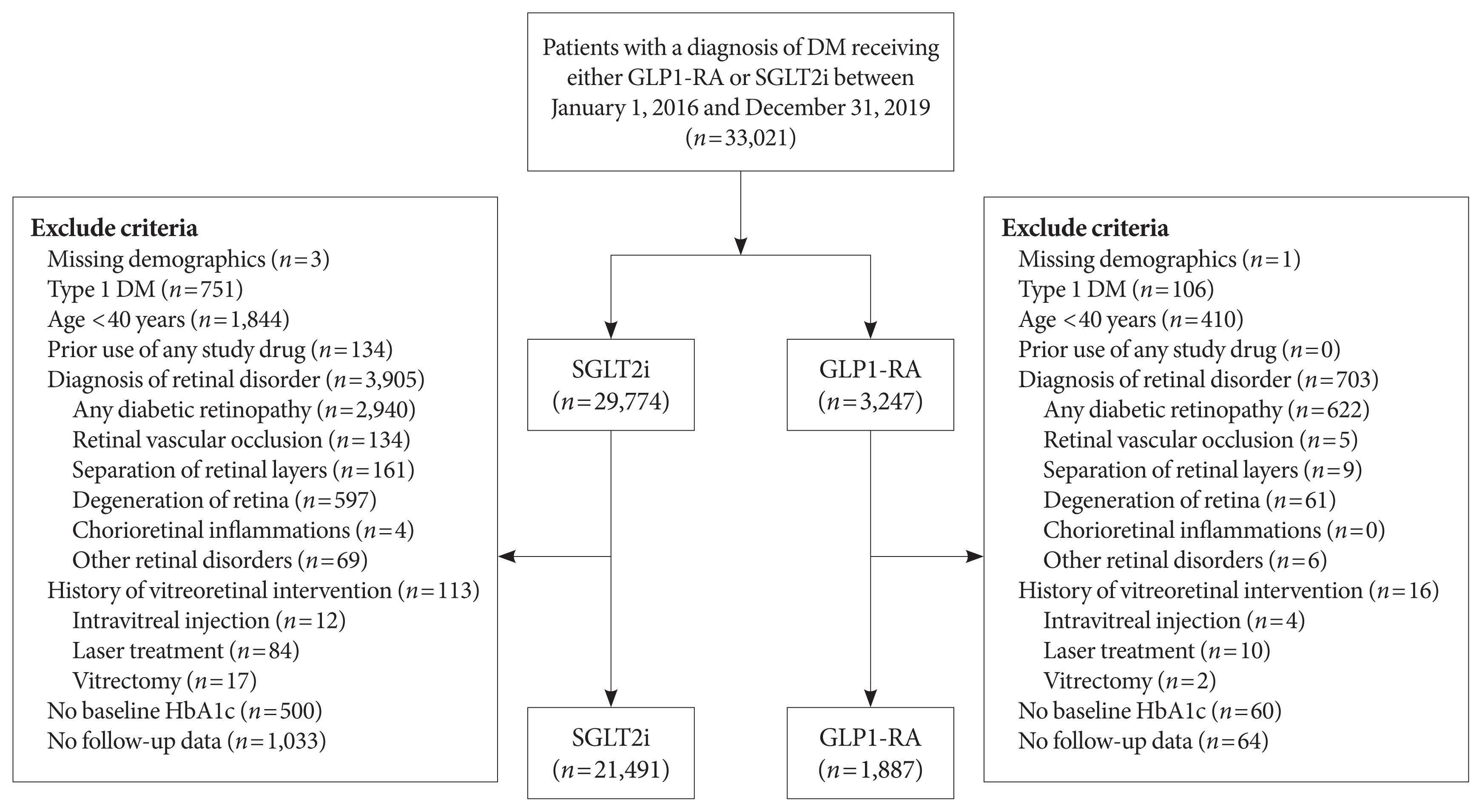
- This retrospective cohort study emulating a target trial included patient data from the multi-institutional Chang Gung Research Database in Taiwan. Totally, 33,021 patients with type 2 diabetes mellitus using SGLT2is and GLP1-RAs between 2016 and 2019 were identified. 3,249 patients were excluded due to missing demographics, age <40 years, prior use of any study drug, a diagnosis of retinal disorders, a history of receiving vitreoretinal procedure, no baseline glycosylated hemoglobin, or no follow-up data. Baseline characteristics were balanced using inverse probability of treatment weighting with propensity scores. DR diagnoses and vitreoretinal interventions served as the primary outcomes. Occurrence of proliferative DR and DR receiving vitreoretinal interventions were regarded as vision-threatening DR.
-
Results
- There were 21,491 SGLT2i and 1,887 GLP1-RA users included for the analysis. Patients receiving SGLT2is and GLP-1 RAs exhibited comparable rate of any DR (subdistribution hazard ratio [SHR], 0.90; 95% confidence interval [CI], 0.79 to 1.03), whereas the rate of proliferative DR (SHR, 0.53; 95% CI, 0.42 to 0.68) was significantly lower in the SGLT2i group. Also, SGLT2i users showed significantly reduced risk of composite surgical outcome (SHR, 0.58; 95% CI, 0.48 to 0.70).
-
Conclusion
- Compared to those taking GLP1-RAs, patients receiving SGLT2is had a lower risk of proliferative DR and vitreoretinal interventions, although the rate of any DR was comparable between the SGLT2i and GLP1-RA groups. Thus, SGLT2is may be associated with a lower risk of vision-threatening DR but not DR development.
- The number of people with diabetes mellitus (DM) surpassed 537 million worldwide in 2021 and has been estimated to reach 783 million by 2045 [1]. Patients with DM are at a high risk of macrovascular and microvascular complications [2]. Diabetic retinopathy (DR) is an important ocular microvascular disease and is the leading cause of blindness at working age [3]. With increasing prevalence of DM, the incidence of vision-threatening DR increases [4]. Multiple therapies, including retinal laser coagulation, intravitreal injection of corticosteroids or anti–vascular endothelial growth factor medications, and vitrectomy, are currently used to treat vision-threatening DR. However, visual outcomes may remain suboptimal in advanced DR [5]. Therefore, prevention of DR is important for vision preservation.
- Within the past decade, sodium-glucose cotransporter-2 inhibitors (SGLT2is) and glucagon-like peptide-1 receptor agonists (GLP1-RAs) have been available for the treatment of type 2 diabetes mellitus (T2DM) [6]. In addition to their glucose-lowering effects, other pleiotropic benefits, such as cardiorenal protections, have been noted in both SGLT2is and GLP1-RAs [7,8]. Recently, SGLT2is have been shown to ameliorate apoptosis of endothelial cells in retinal vessels and thinning of retina [9,10]. By contrast, GLP1-RAs not only reduce damage to retinal ganglion cells but also prevent neural degeneration in DR [11,12]. In addition, both of these medications affect vascular remodeling and alleviate oxidative stress, which may improve hemodynamics of capillaries [13]. Theoretically, both SGLT2is and GLP1-RAs could decrease the likelihood in development of DR.
- Currently, the role of SGLT2is and GLP1-RAs in DR remain unclear. A systematic review and meta-analysis randomized controlled trials (RCTs) reported comparable risks of DR outcomes between SGLT2i and placebo groups [14]. However, 2 real-world studies suggested that SGLT2i significantly decreased the risk of DR, compared to dipeptidyl peptidase-4 inhibitor (DPP4i) and sulfonylurea [15,16]. On the contrary, the trial to evaluate cardiovascular and other long-term outcomes with semaglutide in subjects with type 2 diabetes (SUSTAIN-6) trial demonstrated that GLP1-RA significantly increased the risk of DR outcomes, which was inconsistent with the aforementioned biologic mechanism [17]. However, the liraglutide effect and action in diabetes: evaluation of cardiovascular outcome results (LEADER) trial and AngioSafe trial indicated comparable rates of DR outcomes between the GLP1-RA and placebo [18,19]. Because of the similar medical indications, the National Health Insurance reimbursement guideline in Taiwan does not allow combination therapy of SGLT2i and GLP1-RA. RCTs may restrict generalizability in routine care, and observational studies have insufficient power with small population. Therefore, this study adopted a target trial design with a large real-world database to determine the risk of DR between SGLT2is and GLP1-RAs users.
INTRODUCTION
- Data source
- This retrospective cohort study used data from the Chang Gung Research Database (CGRD), the largest multi-institutional electronic medical record database in Taiwan covering over 1.3 million people. This database comprises clinical information of patients, including medication, intervention, and laboratory data. The CGRD has been described in detail previously [20]. Disease diagnosis was made on the basis of International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) diagnostic codes before 2015 and ICD-10-CM after 2016. The comorbidities and outcomes were defined by at least two outpatient diagnoses or one inpatient diagnosis, and the diagnostic codes are listed in Supplementary Table 1. The intervention data were collected from outpatient and inpatient data. The study protocols adhered to the principles of the Declaration of Helsinki. Written informed consent was waived because of the use of de-identified data. This study was approved by the Institutional Review Board of Chang Gung Medical Foundation (IRB No. 202200260B1).
- Study design and patient inclusion
- A target trial design was pursued to emulate an RCT with observational data (Supplementary Table 2) [21]. RCTs may limit generalizability in clinical practice due to exclusion of patients with high risk at baseline. Observational studies with small population were underpowered to identify meaningful difference in rare events. Therefore, target trial design with large-size population was adopted to acquire powerful evidence of safety profile. New-user and active-comparator designs were adopted to minimize potential selection bias [22]. Patients diagnosed of T2DM receiving either SGLT2is (canagliflozin, dapagliflozin, and empagliflozin) or GLP1-RAs (dulaglutide and liraglutide) between January 1, 2016, and December 31, 2019, were identified. The index date was defined as the day of first prescription of SGLT2i or GLP1-RA. Patients with age >40 years, missing demographics, prior use of any study drug, diagnosis of type 1 DM, retinal disorders classified based on the ICD categories (DR, retinal vascular occlusion, separation of retinal layers [including all types of retinal detachment and central serous retinopathy], degeneration of retina, chorioretinal inflammations, and other retinal disorders [including retinal hemorrhage, vitreous hemorrhage, retinal edema, etc.]), history of receiving vitreoretinal interventions (intravitreal injection, laser coagulation, and vitrectomy), no baseline glycosylated hemoglobin (HbA1c), or no follow-up data in the subsequent 6 months after being prescribed the medication, were excluded from this study. Each patient was followed up until occurrence of primary outcomes, switch between SGLT2is and GLP1-RAs, discontinuation of study drugs, death, or December 31, 2019.
- Primary outcomes
- Our primary outcome included DR outcomes (any DR, nonproliferative DR, and proliferative DR) of vitreoretinal interventions (intravitreal injection, retinal laser, vitrectomy, and composite surgical outcome). Composite surgical outcomes indicated any intravitreal injection, laser therapy, or vitrectomy. Vision-threatening implied proliferative DR or vitreoretinal interventions.
- Secondary outcomes
- Our secondary outcomes were microvascular complications (diabetic nephropathy and neuropathy), macrovascular complications (myocardial infarction, ischemic stroke, and major adverse limb events), and cardiovascular death. To determine internal validity, occurrence of diabetic nephropathy and change of estimated glomerular filtration rate (eGFR) were considered positive control outcomes because of the evidence of renoprotective effects of SGLT2is [23]. Major adverse limb events included any peripheral arterial disease, claudication, critical limb ischemia, endovascular therapy, peripheral bypass, and nontraumatic amputation. Details regarding death and its cause were extracted from the Taiwan Death Registry database released by Taiwan Ministry of Health and Welfare. Laboratory data, HbA1c, and eGFR, were extracted every 6 months. Glycemic control plays a crucial role in development of DR, and analysis of change in HbA1c elucidates whether the impact of glucose-lowering drugs on DR was independent of glycemic status.
- Covariate assessment
- General information comprised sex, age, body mass index, smoking habit, and alcoholic consumption. Severity of DM was assessed by disease duration, associated complications (diabetic nephropathy and diabetic neuropathy), and number of outpatient, inpatient, and emergency department visits for DM in the last year. Comorbidities collected within 6 months before the index date included metabolic syndrome (hypertension and dyslipidemia), cardiovascular disorders (heart failure, myocardial infarction, ischemic stroke, peripheral arterial disease, coronary artery disease, cardiovascular disease [CVD]), and chronic kidney disease. CVD indicates any myocardial infarction, ischemic stroke, peripheral artery disease, or coronary artery disease. Charlson comorbidity index scores were calculated to evaluate disease burden [24]. Concurrent medications retrieved 6 months before the index date were classified into three categories, namely antihypertensive, antidiabetic, and other medications. The eGFR and HbA1c measured at the closet day before the index date were considered the baseline (Table 1).
- Statistical analysis
- Inverse probability of treatment weighting (IPTW) with propensity scores was performed to obtain homogenous groups with more balanced baseline characteristics for comparison. The propensity score represents the predicted probability that was assigned to the SGLT2i group compared with the GLP1-RA group. The covariates used in the calculation of propensity scores through multivariable logistic regression are listed in Table 1. The IPTW allows a comparison based on the average treatment effect of drugs between groups [25]. To prevent the impact of outlier extreme weight, we used stabilized weight and truncated weight at the 97th percentile [26,27]. Single expectation–maximization was used for imputing missing laboratory data. An absolute standardized difference (STD) <0.1 indicated negligible difference between the two groups. The incidence was presented as the number of events per 1,000 person-years. The risk of non-fatal outcome was compared using the Fine and Gray subdistribution hazard model, which regarded death as a competing risk. The risk of fatal outcome was compared using Cox proportional hazard model. The change in HbA1c and eGFR were compared using a linear mixed model, which contains two random effects, namely intercept and slope. Subgroup analysis was conducted by major risk factors, including sex, age, duration of T2DM, CVD, usage of insulin, HbA1c, hypertension, dyslipidemia, and smoking. A 2-sided P value of <0.05 was considered statistically significant. All analyses were conducted with SAS software version 9.4 (SAS Institute Inc., Cary, NC, USA).
METHODS
- Baseline characteristics
- From January 1, 2016, to December 31, 2019, 33,021 patients with T2DM receiving either SGLT2is or GLP1-RAs were identified. After application of exclusion criteria, 21,491 SGLT2i users and 1,887 GLP1-RA users were included in our analysis (Fig. 1). Before IPTW, SGLT2i group had a greater proportion of male patients than GLP1-RA groups. The age was comparable between the two initiators. Regarding the severity of DM, shorter duration, lower prevalence of diabetic nephropathy and diabetic neuropathy, and fewer outpatient, inpatient, and emergency department visits due to DM were observed in SGLT2i group. The prevalence of most systemic comorbidities was comparable between the two users, but SGLT2i users exhibited a higher prevalence of ischemic stroke and a lower prevalence of chronic kidney disease at baseline. Regarding the medication, more patients receiving SGLT2i used beta-blockers. A higher proportion of SGLT2i users received metformin and DPP4i and a lower proportion of SGLT2i users received sulfonylurea, meglitinide, alpha-glucosidase inhibitor, and insulin. Antiplatelet agents and statins were more often administered in SGLT2i group. Regarding general and laboratory data, SGLT2i initiators had lower body mass index and HbA1c and higher eGFR. After IPTW, most covariates were well balanced (STD <0.1) between the two users, although a nonsubstantial difference was noted in myocardial infarction (STD=0.11) and beta-blocker use (STD=0.10). The duration of follow-up was comparable (1.74±1.13 years vs. 1.83±1.06 years, STD=−0.08) between the SGLT2i and GLP1-RA groups.
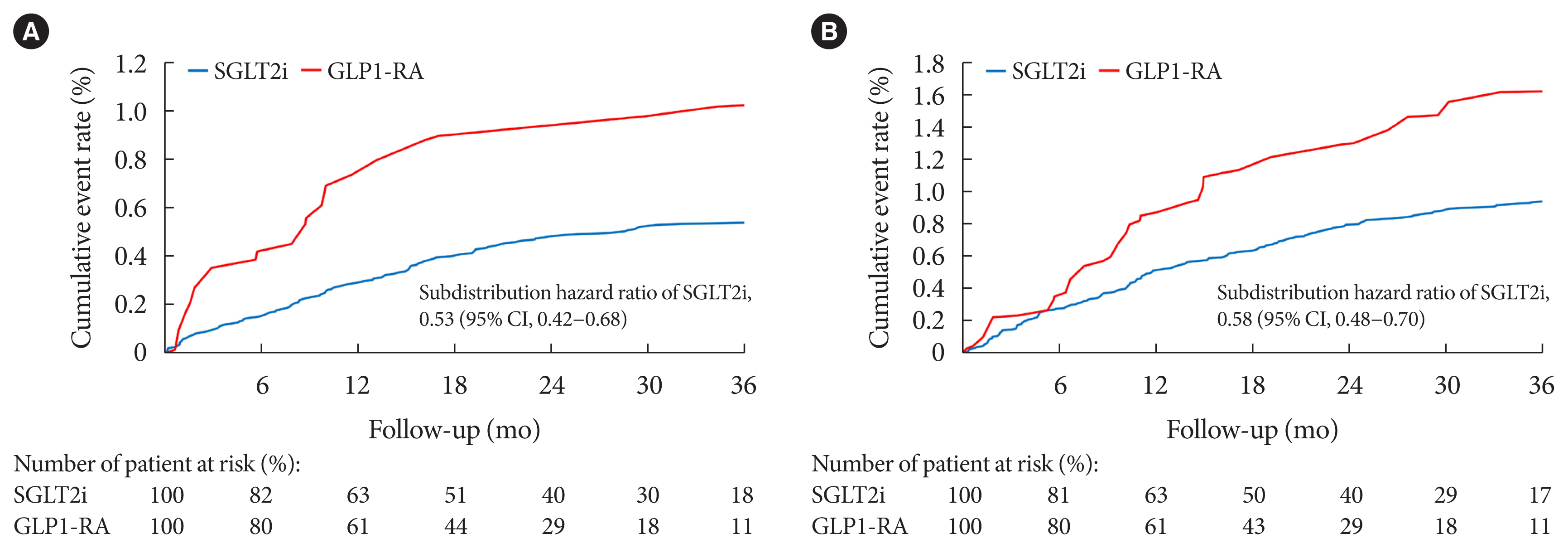
- Primary outcomes
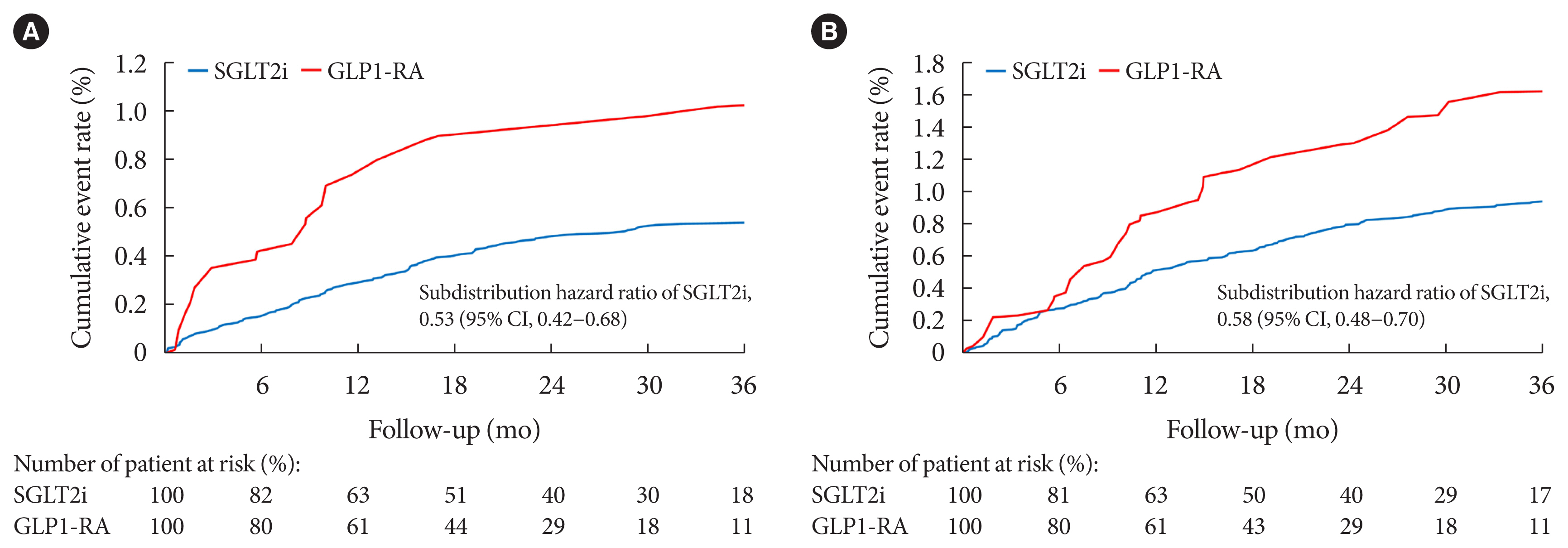
- A comparison of primary outcomes between the SGLT2i to GLP1-RA groups was presented in Table 2. The number of events and incidence data of outcomes before and after IPTW were presented in Supplementary Tables 3 and 4. The incidence of any DR was 15.6 (95% confidence interval [CI], 14.3 to 16.8) events per 1,000 person-years in SGLT2i group and 19.3 (95% CI, 17.3 to 21.3) events per 1,000 person-years in GLP1-RA group, and the rate of any DR (subdistribution hazard ratio [SHR], 0.90; 95% CI, 0.79 to 1.03) was comparable between the two groups. Notably, no significant difference was observed in nonproliferative DR (SHR, 1.16; 95% CI, 0.99 to 1.36) between two users, but SGLT2i users had a significantly lower risk of proliferative DR (SHR, 0.53; 95% CI, 0.42 to 0.68) (Fig. 2A). Furthermore, the SGLT2i group demonstrated a significantly lower risk of composite surgical outcome (SHR, 0.58; 95% CI, 0.48 to 0.70) (Fig. 2B), mainly driven by intravitreal injection (SHR, 0.65; 95% CI, 0.47 to 0.91) and laser therapy (SHR, 0.59; 95% CI, 0.47 to 0.74). In each level of all the subgroup variables, SGLT2i users reported significantly lower incidence of proliferative DR and composite surgical outcome than GLP1 users (Supplementary Tables 5 and 6).
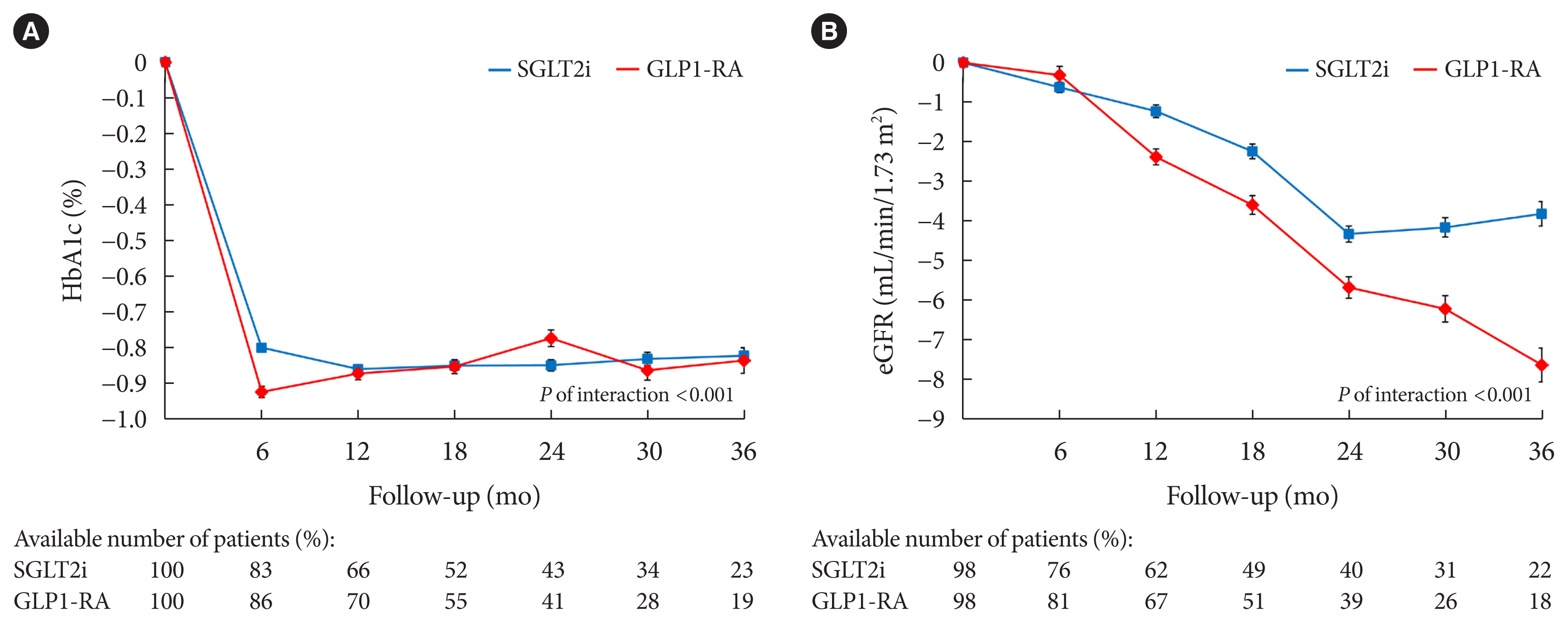
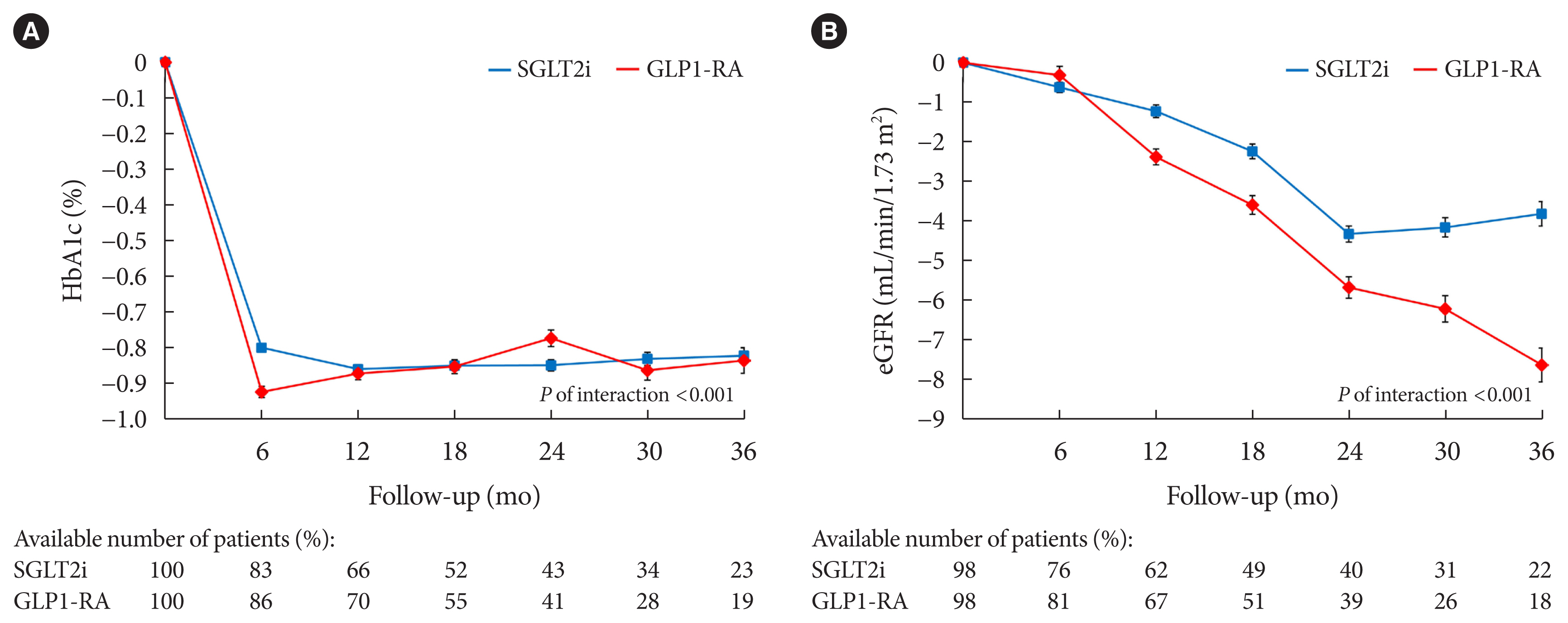
- Secondary outcomes
- A comparison of secondary outcomes between the SGLT2i and GLP1-RA groups was presented in Table 3. The number of events and incidence data of secondary outcomes was presented in Supplementary Tables 3 and 4. Regarding microvascular complications, the SGLT2i group had a significantly lower risk of diabetic nephropathy (SHR, 0.79; 95% CI, 0.71 to 0.88) and neuropathy (SHR, 0.64; 95% CI, 0.53 to 0.76). Concerning macrovascular complications, the rate of myocardial infarction was comparable between the two groups (SHR, 1.03; 95% CI, 0.79 to 1.35), but a significantly higher incidence of ischemic stroke (SHR, 2.53; 95% CI, 1.88 to 3.40) and major adverse limb events (SHR, 1.65; 95% CI, 1.37 to 1.99) were observed in SGLT2i users. Moreover, risk of cardiovascular death was comparable between the two groups (hazard ratio [HR], 0.82; 95% CI, 0.63 to 1.06). Regarding laboratory data, the HbA1c in both user groups swiftly decreased 6 months after drug initiation and became stable subsequently. Notably, the decline in HbA1c was significantly lower in SGLT2i users than in GLP1-RA users at 6th months (−0.80%±1.56% vs. −0.93%±1.63%, P for interaction <0.001) (Fig. 3A). The eGFR in both the groups gradually decreased after drug initiation. However, SGLT2is maintained but GLP1-RAs persistently reduced the eGFR after the 24th month (−4.34±19.75 mL/min/1.73 m2 vs. −5.70±18.81 mL/min/1.73 m2, P for interaction <0.001) (Fig. 3B).
RESULTS
- DR serves as the leading cause of blindness in working-age population. Novel glucose-lowering drugs are proposed to prevent DR, but current studies are underpowered to confirm their safety profile. Therefore, this study compared the risk of DR between patients with T2DM receiving SGLT2is and GLP1-RAs using a real-word database. Regarding our primary outcomes, the two groups had comparable incidence of DR. However, the SGLT2i group exhibited a lower rate of proliferative DR and vitreoretinal interventions. That is, SGLT2is may be associated with a reduced risk of vision-threatening DR. Regarding our secondary outcomes, SGLT2i users had a lower risk of diabetic nephropathy and a more stable eGFR. These positive control outcomes confirmed the internal validity of our study.
- The role of SGLT2is in DR remained unknown according to previous studies. Certain research synthesized data form RCTs to assess the risk of DR in SGLT2i users. A network meta-analysis reported that the incidence of DR outcomes, including DR, macular edema, vitreous hemorrhage, diabetes-related blindness, and treatment of intravitreal agent, retinal photocoagulation, and vitrectomy, were comparable not only between patients receiving SGLT2i and placebo (odds ratio [OR], 0.79; 95% CI, 0.49 to 1.28) but also between patients receiving SGLT2i and GLP1-RA (OR, 0.66; 95% CI, 0.39 to 1.13) [28]. Also, a systematic review and meta-analysis found no significant difference in DR outcomes, including DR, macular edema, vitreous abnormality, requirement for eye-related surgery, and blindness, between SGLT2i and placebo users (risk ratio, 0.98; 95% CI, 0.84 to 1.16) [14]. That is, SGLT2i seemed not to reduce the risk of DR. These different findings from our results may be derived from the following reasons. First, the definition of DR outcomes in the above meta-analyses included not only DR but also DR-related diseases, blindness, and vitreoretinal interventions. In addition, we respectively retrieved the incidence of nonproliferative and proliferative DR. Second, certain RCTs were designed to apply intention-to-treat analysis which the patients were followed up in their respective groups until the end of follow-up. Our study utilized as-treated analysis which ceased the follow-up until the switch between two drugs. This method could avoid the impact from both SGLT2i and GLP1RA. However, a retrospective cohort study declared that SGLT2i significantly reduced the incidence of DR compared to DPP4i (HR, 0.89; 95% CI, 0.83 to 0.97) [15]. A real-world study between SGLT2i and sulfonylurea, significantly decreased rate of DR was observed in SGLT2i group (OR, 0.152; 95% CI, 0.034 to 0.674) [16]. Another retrospective cohort study showed that SGLT2i users reported significantly lower risk of diabetic macular edema than GLP1-RA users (HR, 0.75; 95% CI, 0.64 to 0.88) [29]. Therefore, SGLT2is were considered to decrease the risk of more advanced DR in routine care. Consequently, we conducted an observational real-world study with large population to realize the association between SGLT2is, GLP1-RAs and DR.
- Our study revealed that SGLT2is were associated with a decreased rate of proliferative DR and vitreoretinal interventions compared with GLP1-RAs. Notably, two groups had a similar incidence of any DR and nonproliferative DR. Nonproliferative and proliferative DR represent the early and advanced stage of DR, respectively [5]. A smaller proportion of patients with proliferative DR indicated that SGLT2i may ameliorate development of advanced DR. SGLT2i was associated a smaller decline in HbA1c in our study. Rapid decline of serum glucose level was proposed to induce DR [30]. Therefore, SGLT2i provide steady glucose-lowering effect which resulted in lower incidence of PDR in the early phase of this study (Fig. 2A). Furthermore, this possible effect may be related to anti-inflammatory activity of SGLT2i [31,32]. Excessive glucose level results in secretion of pro-inflammatory cytokines and swelling of pericytes [33], and subsequent destruction of retinal capillaries causes ischemia and induces neovascularization [34]. SGLT2i has been proposed to alleviate apoptosis in retinal microvascular endothelial cells and attenuate thinning of retina and thereby prevent structural change in DR [9,10]. However, definite mechanisms between these glucose-lowering drugs and DR require further experimental investigations.
- SGLT2i and GLP1-RA may also be associated with a reduction of other diabetic complications. SGLT2i significantly lowered the risk of diabetic nephropathy and maintained the eGFR effectively compared with GLP1-RA in our study, which were similar with the outcomes found in two recent network meta-analyses [35,36]. The consistency between our outcome and the published data confirmed the internal validity of this study. Regarding macrovascular complications, comparable incidence of myocardial infarction was observed between patients receiving SGLT2i and GLP1-RA, which was consistent with a population-based cohort study [37]. Similar with the results in two network meta-analyses, GLP1-RA users exhibited a significantly lower incidence of ischemic stroke than SGLT2i users [38,39]. Moreover, we found that GLP1-RA significantly reduced the rate of major adverse limb events compared with SGLT2i, which was consistent with the conclusions in two retrospective cohort studies [40,41]. Based on our results, SGLT2is were associated with a lower rate of vision-threatening DR, diabetic nephropathy, and diabetic neuropathy, and GLP1-RAs were associated with the reduction of ischemic stroke and major adverse limb events. Thus, SGLT2is and GLP1-RAs may have different mechanisms in microvascular and macrovascular complications of T2DM. Further experimental studies are required to confirm these observations.
- To the best of our knowledge, this is the first study to compare the risk of DR between the patients with T2DM receiving SGLT2i and GLP1-RA with a rea-world database. Our study has a number of strengths. First, target trial, new user, and active comparator designs were adopted to minimize bias. Through IPTW adjustment, the confounding factors were well balanced between the two groups. Second, the validated code of T2DM and the regular administration of glucose-lowering drugs confirmed the diagnosis. Third, the inclusion of a large population provided powerful evidence for our results. Fourth, we assessed the disease status by extracting critical laboratory data, such as HbA1c, which was also a risk factor for DR. Fifth, significantly lower incidence of proliferative DR and composite surgical outcome were observed in SGLT2i users than GLP1 users in all subgroup analysis, which strengthen the power of evidence in this study.
- Our study has some limitations. First, the CGRD does not include data, such as the occurrence of DR outcomes or vitreoretinal interventions, from the hospitals not covered by the CGRD. Therefore, the incidence of DR may have been underestimated. However, this underestimation occurred non-differentially across the two groups, and the relative effect should therefore be unbiased. Second, our findings were only applicable to the studied SGLT2is (canagliflozin, dapagliflozin, and empagliflozin) and GLP1-RAs (dulaglutide and liraglutide). Additional studies should confirm our observations by analyzing newer drugs such as oral semaglutide. Third, although we applied IPTW to balance the baseline characteristics between the two groups, the potential residual confounding effect due to unobserved variables may still exist. Therefore, given the retrospective nature of this study, the conclusions should be taken more conservatively. However, the positive control outcome of diabetic nephropathy confirmed our internal validity. Fourth, experimental evidence for pathophysiological mechanism of SGLT2i in DR is still lacking, which should be clarified by future studies.
- In conclusion, the incidence of any DR was comparable between SGLT2i and GLP1-RA users, but the SGLT2i group exhibited a reduced rate of proliferative DR as well as vitreoretinal surgeries. That is, SGLT2is may be associated a decreased risk of vision-threatening DR.
DISCUSSION
SUPPLEMENTARY MATERIALS
Supplementary Table 1.
Supplementary Table 2.
Supplementary Table 3.
Supplementary Table 4.
Supplementary Table 5.
Supplementary Table 6.
-
Acknowledgements
- The authors thank Alfred Hsing-Fen Lin, Ben Yu-Lin Chou, and Judy Jia-Jheng Wu for their assistance in the statistical analysis during the completion of manuscript. This manuscript was edited by Wallace Academic Editing.
ACKNOWLEDGMENTS
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conception or design: T.Y.L., E.Y.C.K., Y.S.H.
Acquisition, analysis, or interpretation of data: T.Y.L., E.Y.C.K., K.J.C., J.H.K., W.C.W., C.C.L., Y.S.H.
Drafting the work or revising: T.Y.L., E.Y.C.K., S.C.S., E.C.C.L., S.J.G.
Final approval of the manuscript: T.Y.L., E.Y.C.K., S.C.S., E.C.C.L., S.J.G., K.J.C., J.H.K., W.C.W., C.C.L., Y.S.H.
-
FUNDING
This study was supported by Chang Gung Memorial Hospital (CMRPG3K0481 and CMRPG3L0251). The funder had no role in study conduction and result interpretation. All authors declared no conflict of interest regarding this study.
NOTES

| Variable | Available number | Before IPTW | After IPTW | ||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| SGLT2i (n=21,491) | GLP1-RA (n=1,887) | STD | SGLT2i | GLP1-RA | STD | ||
| Male sex | 23,378 | 13,019 (60.6) | 895 (47.4) | 0.27 | 59.4 | 59.7 | −0.01 |
| Age, yr | 23,378 | 61.0±10.3 | 60.3±11.1 | 0.07 | 61.0±10.3 | 60.3±10.6 | 0.06 |
| Age ≥65 yr | 23,378 | 7,544 (35.1) | 641 (34.0) | 0.02 | 35.1 | 32.8 | 0.05 |
| Body mass index, kg/m2 | 20,942 | 28.0±4.8 | 29.1±5.4 | −0.23 | 28.1±4.6 | 28.4±4.8 | −0.07 |
| Smoking | 23,378 | 3,764 (17.5) | 306 (16.2) | 0.03 | 17.4 | 16.5 | 0.02 |
| Alcohol | 23,378 | 2,106 (9.8) | 151 (8.0) | 0.06 | 9.7 | 9.4 | 0.01 |
|
|
|||||||
| Severity of DM | |||||||
| Duration, yr | 23,378 | 6.98±5.42 | 7.93±5.82 | −0.17 | 7.05±5.43 | 7.15±5.72 | −0.02 |
| Diabetic nephropathy | 23,378 | 4,996 (23.2) | 672 (35.6) | −0.27 | 24.2 | 26.7 | −0.06 |
| Diabetic neuropathy | 23,378 | 2,051 (9.5) | 283 (15.0) | −0.17 | 10.0 | 11.4 | −0.05 |
| OPD visit due to DM last year | 23,378 | 4.85±3.73 | 6.45±4.82 | −0.37 | 5.00±3.89 | 5.37±4.16 | −0.09 |
| IPD visit due to DM last year | 23,378 | 3,347 (15.6) | 393 (20.8) | −0.14 | 16.0 | 14.1 | 0.05 |
| ED visit due to DM last year | 23,378 | 1,710 (8.0) | 245 (13.0) | −0.16 | 8.4 | 10.1 | −0.06 |
|
|
|||||||
| Comorbidity | |||||||
| Hypertension | 23,378 | 15,522 (72.2) | 1,375 (72.9) | −0.01 | 72.3 | 71.9 | 0.01 |
| Dyslipidemia | 23,378 | 16,094 (74.9) | 1,384 (73.3) | 0.04 | 74.7 | 73.5 | 0.03 |
| Heart failure | 23,378 | 1,239 (5.8) | 79 (4.2) | 0.07 | 5.6 | 5.4 | 0.01 |
| Myocardial infarction | 23,378 | 1,663 (7.7) | 79 (4.2) | 0.15 | 7.4 | 4.8 | 0.11 |
| Ischemic stroke | 23,378 | 1,156 (5.4) | 123 (6.5) | −0.05 | 5.5 | 5.6 | <0.01 |
| Peripheral arterial disease | 23,378 | 836 (3.9) | 80 (4.2) | −0.02 | 3.9 | 4.4 | −0.03 |
| Coronary arterial disease | 23,378 | 6,343 (29.5) | 422 (22.4) | −0.16 | 28.9 | 25.1 | −0.09 |
| Cardiovascular diseasea | 23,378 | 7,418 (34.5) | 540 (28.6) | −0.13 | 34.0 | 30.9 | −0.07 |
| Chronic kidney disease | 23,378 | 8,018 (37.3) | 987 (52.3) | −0.31 | 38.5 | 40.6 | −0.04 |
|
|
|||||||
| Charlson comorbidity index score | 23,378 | 3.26±2.20 | 3.96±2.65 | −0.29 | 3.32±2.23 | 3.36±2.32 | −0.02 |
|
|
|||||||
| Anti-hypertensive medication | |||||||
| ACEi/ARB | 23,378 | 11,088 (51.6) | 924 (49.0) | 0.05 | 51.4 | 49.4 | 0.04 |
| Beta-blocker | 23,378 | 7,722 (35.9) | 534 (28.3) | 0.16 | 35.2 | 30.7 | 0.10 |
| Calcium channel blocker | 23,378 | 3,476 (16.2) | 326 (17.3) | −0.03 | 16.4 | 16.5 | <0.01 |
| Diuretic | 23,378 | 2,643 (12.3) | 274 (14.5) | −0.07 | 12.5 | 13.6 | −0.03 |
|
|
|||||||
| Anti-diabetic medication | |||||||
| Metformin | 23,378 | 19,561 (91.0) | 1,390 (73.7) | 0.47 | 89.5 | 88.6 | 0.03 |
| Sulfonylurea | 23,378 | 5,294 (24.6) | 590 (31.3) | −0.15 | 25.2 | 22.9 | 0.05 |
| Meglitinide | 23,378 | 353 (1.6) | 90 (4.8) | −0.18 | 1.9 | 2.0 | <0.01 |
| Thiazolidinedione | 23,378 | 2,846 (13.2) | 240 (12.7) | 0.02 | 13.2 | 13.9 | −0.02 |
| Alpha-glucosidase inhibitor | 23,378 | 3,247 (15.1) | 399 (21.1) | −0.16 | 15.7 | 17.4 | −0.04 |
| Dipeptidyl peptidase-4 inhibitor | 23,378 | 3,458 (16.1) | 199 (10.5) | 0.16 | 15.7 | 14.8 | 0.03 |
| Insulin | 23,378 | 2,926 (13.6) | 860 (45.6) | −0.75 | 16.4 | 17.8 | −0.04 |
|
|
|||||||
| Other medication | |||||||
| Anti-platelet | 23,378 | 7,298 (34.0) | 530 (28.1) | 0.13 | 33.5 | 29.1 | 0.09 |
| Anti-coagulant | 23,378 | 842 (3.9) | 48 (2.5) | 0.08 | 3.8 | 3.5 | 0.02 |
| Statin | 23,378 | 14,084 (65.5) | 1,146 (60.7) | 0.10 | 65.0 | 60.4 | 0.09 |
| Fibrate | 23,378 | 1,994 (9.3) | 213 (11.3) | −0.07 | 9.4 | 10.6 | −0.04 |
|
|
|||||||
| Laboratory data | |||||||
| HbA1c, % | 23,378 | 8.58±1.63 | 9.08±1.75 | −0.30 | 8.62±1.65 | 8.73±1.63 | −0.07 |
| eGFR, mL/min/1.73 m2 | 22,816 | 89.9±28.0 | 79.7±37.3 | 0.31 | 89.0±28.8 | 90.2±29.0 | −0.04 |
|
|
|||||||
| Follow-up, yr | 23,378 | 1.75±1.12 | 1.61±1.03 | 0.13 | 1.74±1.13 | 1.83±1.06 | −0.08 |
Values are presented as number (%) or mean±standard deviation.
T2DM, type 2 diabetes mellitus; SGLT2i, sodium-glucose co-transporter 2 inhibitor; GLP1-RA, glucagon-like peptide-1 receptor agonist; IPTW, inverse probability of treatment weighting; STD, standardized difference; DM, diabetes mellitus; OPD, outpatient department; IPD, inpatient department; ED, emergency department; ACEi, angiotensin converting enzyme inhibitor; ARB, angiotensin receptor blocker; HbA1c, glycosylated hemoglobin; eGFR, estimated glomerular filtration rate.
a Anyone of myocardial infarction, ischemic stroke, peripheral arterial disease, or coronary arterial disease.
| Variable | Before IPTW | After IPTW | P value | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| SGLT2i (n=21,491) | GLP1-RA (n=1,887) | SGLT2i | GLP1-RA | SHR of SGLT2i (95% confidence interval) | ||
| DR outcomes | ||||||
| Any DR | 15.0 (13.8–16.3) | 23.3 (17.5–29.2) | 15.6 (14.3–16.8) | 19.3 (17.3–21.3) | 0.90 (0.79–1.03) | 0.128 |
| Non-proliferative DR | 12.2 (11.0–13.3) | 14.4 (9.8–19.0) | 12.6 (11.5–13.7) | 12.1 (10.5–13.7) | 1.16 (0.99–1.36) | 0.063 |
| Proliferative DR | 3.3 (2.7–3.9) | 8.7 (5.1–12.2) | 3.3 (2.8–3.9) | 7.0 (5.8–8.2) | 0.53 (0.42–0.68) | <0.001 |
|
|
||||||
| Vitreoretinal interventions | ||||||
| Intravitreal injection | 1.9 (1.4–2.3) | 3.7 (1.4–6.1) | 2.0 (1.6–2.5) | 3.4 (2.5–4.2) | 0.65 (0.47–0.91) | 0.013 |
| Laser therapy | 3.8 (3.1–4.4) | 9.4 (5.7–13.1) | 3.9 (3.3–4.6) | 7.4 (6.1–8.6) | 0.59 (0.47–0.74) | <0.001 |
| Vitrectomy | 1.3 (0.9–1.7) | 3.0 (0.9–5.1) | 1.3 (1.0–1.7) | 2.2 (1.5–2.9) | 0.68 (0.46–1.03) | 0.066 |
| Composite surgical outcomea | 5.5 (4.8–6.3) | 13.2 (8.8–17.6) | 5.8 (5.0–6.6) | 11.1 (9.6–12.7) | 0.58 (0.48–0.70) | <0.001 |
Values are presented as the number of events per 1,000 person-years (95% confidence interval).
T2DM, type 2 diabetes mellitus; SGLT2i, sodium-glucose co-transporter 2 inhibitor; GLP1-RA, glucagon-like peptide-1 receptor agonist; IPTW, inverse probability of treatment weighting; SHR, subdistribution hazard ratio; DR, diabetic retinopathy.
a Indicates any intravitreal injection, laser therapy, or vitrectomy.
| Variable | Before IPTW | After IPTW | P value | |||
|---|---|---|---|---|---|---|
|
|
|
|||||
| SGLT2i (n=21,491) | GLP1-RA (n=1,887) | SGLT2i | GLP1-RA | SHR of SGLT2i (95% confidence interval) | ||
| Microvascular complications | ||||||
| Diabetic nephropathy | 20.8 (19.3–22.3) | 35.3 (28.0–42.5) | 22.0 (20.5–23.4) | 31.2 (28.6–33.7) | 0.79 (0.71–0.88) | <0.001 |
| Diabetic neuropathy | 7.02 (6.15–7.88) | 13.7 (9.2–18.1) | 7.27 (6.43–8.12) | 12.8 (11.1–14.4) | 0.64 (0.53–0.76) | <0.001 |
|
|
||||||
| Macrovascular complications | ||||||
| Myocardial infarction | 3.9 (3.3–4.6) | 6.4 (3.3–9.4) | 4.04 (3.41–4.67) | 4.31 (3.37–5.25) | 1.03 (0.79–1.35) | 0.833 |
| Ischemic stroke | 6.1 (5.3–6.9) | 4.1 (1.7–6.5) | 6.27 (5.49–7.06) | 2.80 (2.04–3.56) | 2.53 (1.88–3.40) | <0.001 |
| Major adverse limb eventsa | 6.5 (5.6–7.3) | 5.6 (2.8–8.5) | 6.76 (5.94–7.58) | 4.12 (3.20–5.04) | 1.84 (1.42–2.37) | <0.001 |
| Cardiovascular death | 3.8 (3.1–4.4) | 4.9 (2.2–7.5) | 3.81 (3.20–4.42) | 4.68 (3.70–5.66) | 0.82 (0.63–1.06) | 0.131 |
Values are presented as the number of events per 1,000 person-years (95% confidence interval).
T2DM, type 2 diabetes mellitus; SGLT2i, sodium-glucose co-transporter 2 inhibitor; GLP1-RA, glucagon-like peptide-1 receptor agonist; IPTW, inverse probability of treatment weighting; SHR, subdistribution hazard ratio.
a Indicates any peripheral arterial disease, claudication, critical limb ischemia, endovascular therapy, peripheral bypass, or nontraumatic amputation.
- 1. Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract 2022;183:109119.ArticlePubMed
- 2. Zoungas S, Woodward M, Li Q, Cooper ME, Hamet P, Harrap S, et al. Impact of age, age at diagnosis and duration of diabetes on the risk of macrovascular and microvascular complications and death in type 2 diabetes. Diabetologia 2014;57:2465-74.ArticlePubMedPDF
- 3. GBD 2019 Blindness and Vision Impairment Collaborators; Vision Loss Expert Group of the Global Burden of Disease Study. Causes of blindness and vision impairment in 2020 and trends over 30 years, and prevalence of avoidable blindness in relation to VISION 2020: the right to sight: an analysis for the Global Burden of Disease Study. Lancet Glob Health 2021;9:e144-60.PubMed
- 4. International Diabetes Federation. IDF Diabetes Atlas. 6th ed. Brussels: International Diabetes Federation; 2015.
- 5. Duh EJ, Sun JK, Stitt AW. Diabetic retinopathy: current understanding, mechanisms, and treatment strategies. JCI Insight 2017;2:e93751.ArticlePubMedPMC
- 6. Lin DS, Lee JK, Hung CS, Chen WJ. The efficacy and safety of novel classes of glucose-lowering drugs for cardiovascular outcomes: a network meta-analysis of randomised clinical trials. Diabetologia 2021;64:2676-86.ArticlePubMedPDF
- 7. Shao SC, Chang KC, Lin SJ, Chien RN, Hung MJ, Chan YY, et al. Favorable pleiotropic effects of sodium glucose cotransporter 2 inhibitors: head-to-head comparisons with dipeptidyl peptidase-4 inhibitors in type 2 diabetes patients. Cardiovasc Diabetol 2020;19:17.ArticlePubMedPMCPDF
- 8. Brown E, Heerspink HJL, Cuthbertson DJ, Wilding JP. SGLT2 inhibitors and GLP-1 receptor agonists: established and emerging indications. Lancet 2021;398:262-76.ArticlePubMed
- 9. Hu Y, Xu Q, Li H, Meng Z, Hao M, Ma X, et al. Dapagliflozin reduces apoptosis of diabetic retina and human retinal microvascular endothelial cells through ERK1/2/cPLA2/AA/ROS pathway independent of hypoglycemic. Front Pharmacol 2022;13:827896.ArticlePubMedPMC
- 10. Fernandes VH, Chaves FR, Soares AA, Breder I, Kimura-Medorima ST, Munhoz DB, et al. Dapagliflozin increases retinal thickness in type 2 diabetic patients as compared with glibenclamide: a randomized controlled trial. Diabetes Metab 2021;47:101280.ArticlePubMed
- 11. Zhou HR, Ma XF, Lin WJ, Hao M, Yu XY, Li HX, et al. Neuroprotective role of GLP-1 analog for retinal ganglion cells via PINK1/Parkin-mediated mitophagy in diabetic retinopathy. Front Pharmacol 2021;11:589114.ArticlePubMedPMC
- 12. Hernandez C, Bogdanov P, Corraliza L, Garcia-Ramirez M, Sola-Adell C, Arranz JA, et al. Topical administration of GLP-1 receptor agonists prevents retinal neurodegeneration in experimental diabetes. Diabetes 2016;65:172-87.ArticlePubMedPDF
- 13. Khat DZ, Husain M. Molecular mechanisms underlying the cardiovascular benefits of SGLT2i and GLP-1RA. Curr Diab Rep 2018;18:45.ArticlePubMedPDF
- 14. Li C, Zhou Z, Neuen BL, Yu J, Huang Y, Young T, et al. Sodium-glucose co-transporter-2 inhibition and ocular outcomes in patients with type 2 diabetes: a systematic review and meta-analysis. Diabetes Obes Metab 2021;23:252-7.ArticlePubMedPDF
- 15. Chung YR, Ha KH, Lee K, Kim DJ. Effects of sodium-glucose cotransporter-2 inhibitors and dipeptidyl peptidase-4 inhibitors on diabetic retinopathy and its progression: a real-world Korean study. PLoS One 2019;14:e0224549.ArticlePubMedPMC
- 16. Cho EH, Park SJ, Han S, Song JH, Lee K, Chung YR. Potent oral hypoglycemic agents for microvascular complication: sodium-glucose cotransporter 2 inhibitors for diabetic retinopathy. J Diabetes Res 2018;2018:6807219.ArticlePubMedPMCPDF
- 17. Marso SP, Bain SC, Consoli A, Eliaschewitz FG, Jodar E, Leiter LA, et al. Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2016;375:1834-44.ArticlePubMed
- 18. Gaborit B, Julla JB, Besbes S, Proust M, Vincentelli C, Alos B, et al. Glucagon-like peptide 1 receptor agonists, diabetic retinopathy and angiogenesis: the AngioSafe Type 2 Diabetes Study. J Clin Endocrinol Metab 2020;105:dgz069.ArticlePubMedPDF
- 19. Marso SP, Daniels GH, Brown-Frandsen K, Kristensen P, Mann JF, Nauck MA, et al. Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 2016;375:311-22.ArticlePubMedPMC
- 20. Shao SC, Chan YY, Kao Yang YH, Lin SJ, Hung MJ, Chien RN, et al. The Chang Gung Research Database: a multi-institutional electronic medical records database for real-world epidemiological studies in Taiwan. Pharmacoepidemiol Drug Saf 2019;28:593-600.ArticlePubMedPDF
- 21. Kutcher SA, Brophy JM, Banack HR, Kaufman JS, Samuel M. Emulating a randomised controlled trial with observational data: an introduction to the target trial framework. Can J Cardiol 2021;37:1365-77.ArticlePubMed
- 22. Lund JL, Richardson DB, Sturmer T. The active comparator, new user study design in pharmacoepidemiology: historical foundations and contemporary application. Curr Epidemiol Rep 2015;2:221-8.ArticlePubMedPMCPDF
- 23. Neuen BL, Young T, Heerspink HJL, Neal B, Perkovic V, Billot L, et al. SGLT2 inhibitors for the prevention of kidney failure in patients with type 2 diabetes: a systematic review and meta-analysis. Lancet Diabetes Endocrinol 2019;7:845-54.ArticlePubMed
- 24. D’Hoore W, Bouckaert A, Tilquin C. Practical considerations on the use of the Charlson comorbidity index with administrative data bases. J Clin Epidemiol 1996;49:1429-33.ArticlePubMed
- 25. Chesnaye NC, Stel VS, Tripepi G, Dekker FW, Fu EL, Zoccali C, et al. An introduction to inverse probability of treatment weighting in observational research. Clin Kidney J 2021;15:14-20.ArticlePubMedPMCPDF
- 26. Hernan MA, Brumback B, Robins JM. Marginal structural models to estimate the causal effect of zidovudine on the survival of HIV-positive men. Epidemiology 2000;11:561-70.ArticlePubMed
- 27. Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med 2015;34:3661-79.ArticlePubMedPMCPDF
- 28. Tang H, Li G, Zhao Y, Wang F, Gower EW, Shi L, et al. Comparisons of diabetic retinopathy events associated with glucose-lowering drugs in patients with type 2 diabetes mellitus: a network meta-analysis. Diabetes Obes Metab 2018;20:1262-79.ArticlePubMedPDF
- 29. Su YC, Shao SC, Lai EC, Lee CN, Hung MJ, Lai CC, et al. Risk of diabetic macular oedema with sodium-glucose cotransporter-2 inhibitors in type 2 diabetes patients: a multi-institutional cohort study in Taiwan. Diabetes Obes Metab 2021;23:2067-76.PubMedPDF
- 30. Bain SC, Klufas MA, Ho A, Matthews DR. Worsening of diabetic retinopathy with rapid improvement in systemic glucose control: a review. Diabetes Obes Metab 2019;21:454-66.ArticlePubMedPMCPDF
- 31. Bonnet F, Scheen AJ. Effects of SGLT2 inhibitors on systemic and tissue low-grade inflammation: the potential contribution to diabetes complications and cardiovascular disease. Diabetes Metab 2018;44:457-64.ArticlePubMed
- 32. Shao SC, Su YC, Lai EC, Chang KC, Lee CN, Hung MJ, et al. Association between sodium glucose co-transporter 2 inhibitors and incident glaucoma in patients with type 2 diabetes: a multi-institutional cohort study in Taiwan. Diabetes Metab 2022;48:101318.ArticlePubMed
- 33. Corliss BA, Ray HC, Doty RW, Mathews C, Sheybani N, Fitzgerald K, et al. Pericyte bridges in homeostasis and hyperglycemia. Diabetes 2020;69:1503-17.ArticlePubMedPMCPDF
- 34. Gui F, You Z, Fu S, Wu H, Zhang Y. Endothelial dysfunction in diabetic retinopathy. Front Endocrinol (Lausanne) 2020;11:591.ArticlePubMedPMC
- 35. Yamada T, Wakabayashi M, Bhalla A, Chopra N, Miyashita H, Mikami T, et al. Cardiovascular and renal outcomes with SGLT-2 inhibitors versus GLP-1 receptor agonists in patients with type 2 diabetes mellitus and chronic kidney disease: a systematic review and network meta-analysis. Cardiovasc Diabetol 2021;20:14.ArticlePubMedPMCPDF
- 36. Kawai Y, Uneda K, Yamada T, Kinguchi S, Kobayashi K, Azushima K, et al. Comparison of effects of SGLT-2 inhibitors and GLP-1 receptor agonists on cardiovascular and renal outcomes in type 2 diabetes mellitus patients with/without albuminuria: a systematic review and network meta-analysis. Diabetes Res Clin Pract 2022;183:109146.ArticlePubMed
- 37. Dong YH, Chang CH, Lin JW, Yang WS, Wu LC, Toh S. Comparative cardiovascular effectiveness of glucagon-like peptide-1 receptor agonists versus sodium-glucose cotransporter-2 inhibitors in patients with type 2 diabetes: a population-based cohort study. Diabetes Obes Metab 2022;24:1623-37.ArticlePubMedPDF
- 38. Duan XY, Liu SY, Yin DG. Comparative efficacy of 5 sodium glucose cotransporter 2 inhibitor and 7 glucagon-like peptide 1 receptor agonists interventions on cardiorenal outcomes in type 2 diabetes patients: a network meta-analysis based on cardiovascular or renal outcome trials. Medicine (Baltimore) 2021;100:e26431.PubMedPMC
- 39. Palmer SC, Tendal B, Mustafa RA, Vandvik PO, Li S, Hao Q, et al. Sodium-glucose cotransporter protein-2 (SGLT-2) inhibitors and glucagon-like peptide-1 (GLP-1) receptor agonists for type 2 diabetes: systematic review and network meta-analysis of randomised controlled trials. BMJ 2021;372:m4573.ArticlePubMedPMC
- 40. Hsiao FC, Lin CP, Tung YC, Wu CT, Chu PH. Major adverse limb events in type 2 diabetes patients receiving glucagon-like peptide-1 receptor agonists versus sodium-glucose cotransporter 2 inhibitors: a retrospective multi-institutional study. Diabetes Res Clin Pract 2021;180:109076.ArticlePubMed
- 41. Patorno E, Pawar A, Bessette LG, Kim DH, Dave C, Glynn RJ, et al. Comparative effectiveness and safety of sodium-glucose cotransporter 2 inhibitors versus glucagon-like peptide 1 receptor agonists in older adults. Diabetes Care 2021;44:826-35.ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations

- Incretin‐based drugs and the risk of diabetic retinopathy among individuals with type 2 diabetes: A systematic review and meta‐analysis of observational studies
Samuel Igweokpala, Naheemot Olaoluwa Sule, Antonios Douros, Oriana H. Y. Yu, Kristian B. Filion
Diabetes, Obesity and Metabolism.2024; 26(2): 721. CrossRef - Association of sodium–glucose cotransporter‐2 inhibitors and the risk of retinal vascular occlusion: A real‐world retrospective cohort study in Taiwan
Tzu‐Yi Lin, Eugene Yu‐Chuan Kang, Shih‐Chieh Shao, Edward Chia‐Cheng Lai, Nan‐Kai Wang, Sunir J. Garg, Kuan‐Jen Chen, Je‐Ho Kang, Wei‐Chi Wu, Chi‐Chun Lai, Yih‐Shiou Hwang
Diabetes/Metabolism Research and Reviews.2024;[Epub] CrossRef - Risk of rotator cuff tear and rotator cuff repair surgery comparison between sodium-glucose cotransporter 2 inhibitors and glucagon like peptide-1 receptor agonists: A real-world study
Yu-Chi Su, Pei-Chun Hsieh, Edward Chia-Cheng Lai, Yu-Ching Lin
Diabetes & Metabolism.2024; 50(2): 101522. CrossRef - Optimising renal risk parameters in type 2 diabetes mellitus: Perspectives from a retinal viewpoint
Sarita Jacob, George I. Varughese
Clinical Medicine.2024; 24(2): 100031. CrossRef - Risk of diabetic retinopathy and diabetic macular oedema with sodium–glucose cotransporter 2 inhibitors and glucagon-like peptide 1 receptor agonists in type 2 diabetes: a real-world data study from a global federated database
Aikaterini Eleftheriadou, David Riley, Sizheng S. Zhao, Philip Austin, Gema Hernández, Gregory Y. H. Lip, Timothy L. Jackson, John P. H. Wilding, Uazman Alam
Diabetologia.2024;[Epub] CrossRef - Impact of GLP-1 Agonists and SGLT-2 Inhibitors on Diabetic Retinopathy Progression: An Aggregated Electronic Health Record Data Study
Karen M. Wai, Kapil Mishra, Euna Koo, Cassie Ann Ludwig, Ravi Parikh, Prithvi Mruthyunjaya, Ehsan Rahimy
American Journal of Ophthalmology.2024;[Epub] CrossRef - Risk of Diabetic Retinopathy between Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists (Diabetes Metab J 2023;47:394-404)
Tzu-Yi Lin, Eugene Yu-Chuan Kang, Shih-Chieh Shao, Edward Chia-Cheng Lai, Yih-Shiou Hwang
Diabetes & Metabolism Journal.2023; 47(4): 573. CrossRef - Risk of Diabetic Retinopathy between Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists (Diabetes Metab J 2023;47:394-404)
Jihee Ko, Sun Joon Moon
Diabetes & Metabolism Journal.2023; 47(4): 571. CrossRef - Sodium-Glucose Cotransporter 2 Inhibitors and Risk of Retinopathy in Patients With Type 2 Diabetes
Fu-Shun Yen, James Cheng-Chung Wei, Teng-Shun Yu, Yu-Tung Hung, Chih-Cheng Hsu, Chii-Min Hwu
JAMA Network Open.2023; 6(12): e2348431. CrossRef
- Figure
- Related articles
-
- Risk of Diabetic Retinopathy between Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists (Diabetes Metab J 2023;47:394-404)
- Risk of Diabetic Retinopathy between Sodium-Glucose Cotransporter-2 Inhibitors and Glucagon-Like Peptide-1 Receptor Agonists (Diabetes Metab J 2023;47:394-404)
- Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study (Diabetes Metab J 2022;46: 658-62)
- Clinical Efficacy of Sodium-Glucose Cotransporter 2 Inhibitor and Glucagon-Like Peptide-1 Receptor Agonist Combination Therapy in Type 2 Diabetes Mellitus: Real-World Study (Diabetes Metab J 2022;46: 658-62)
- Renoprotective Mechanism of Sodium-Glucose Cotransporter 2 Inhibitors: Focusing on Renal Hemodynamics

 KDA
KDA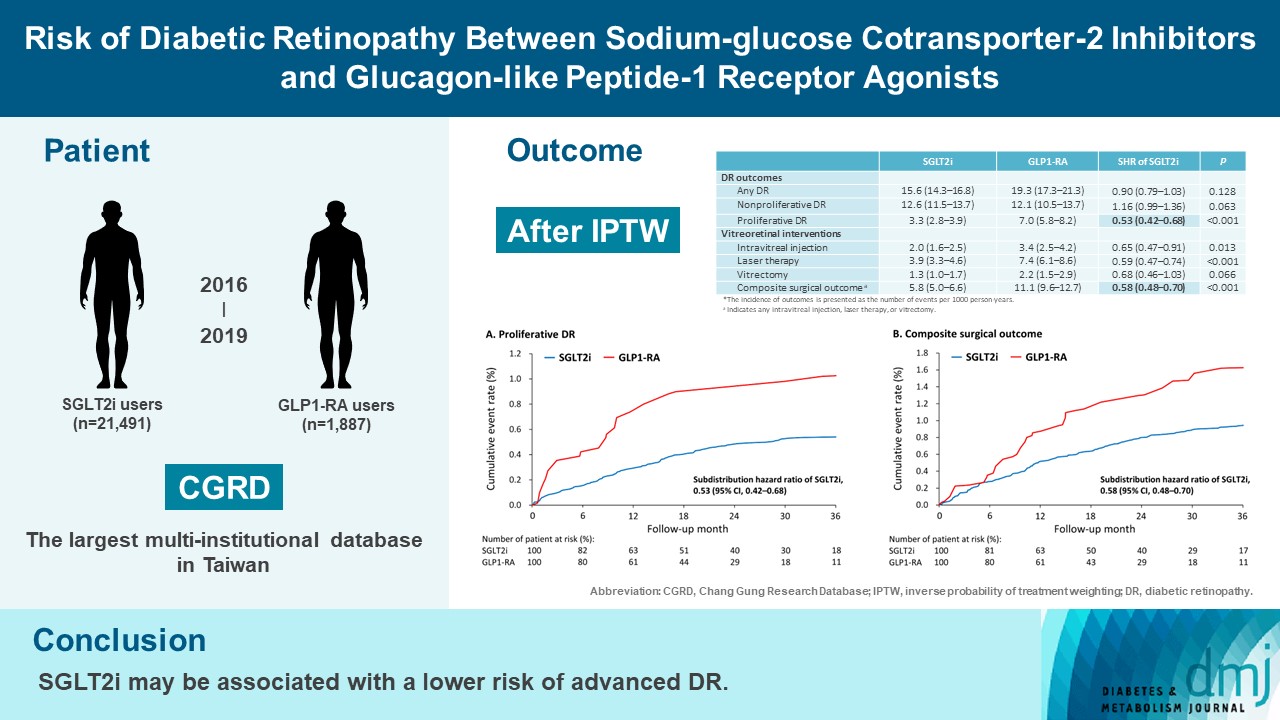
 PubReader
PubReader ePub Link
ePub Link Cite
Cite