- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 36(3); 2012 > Article
-
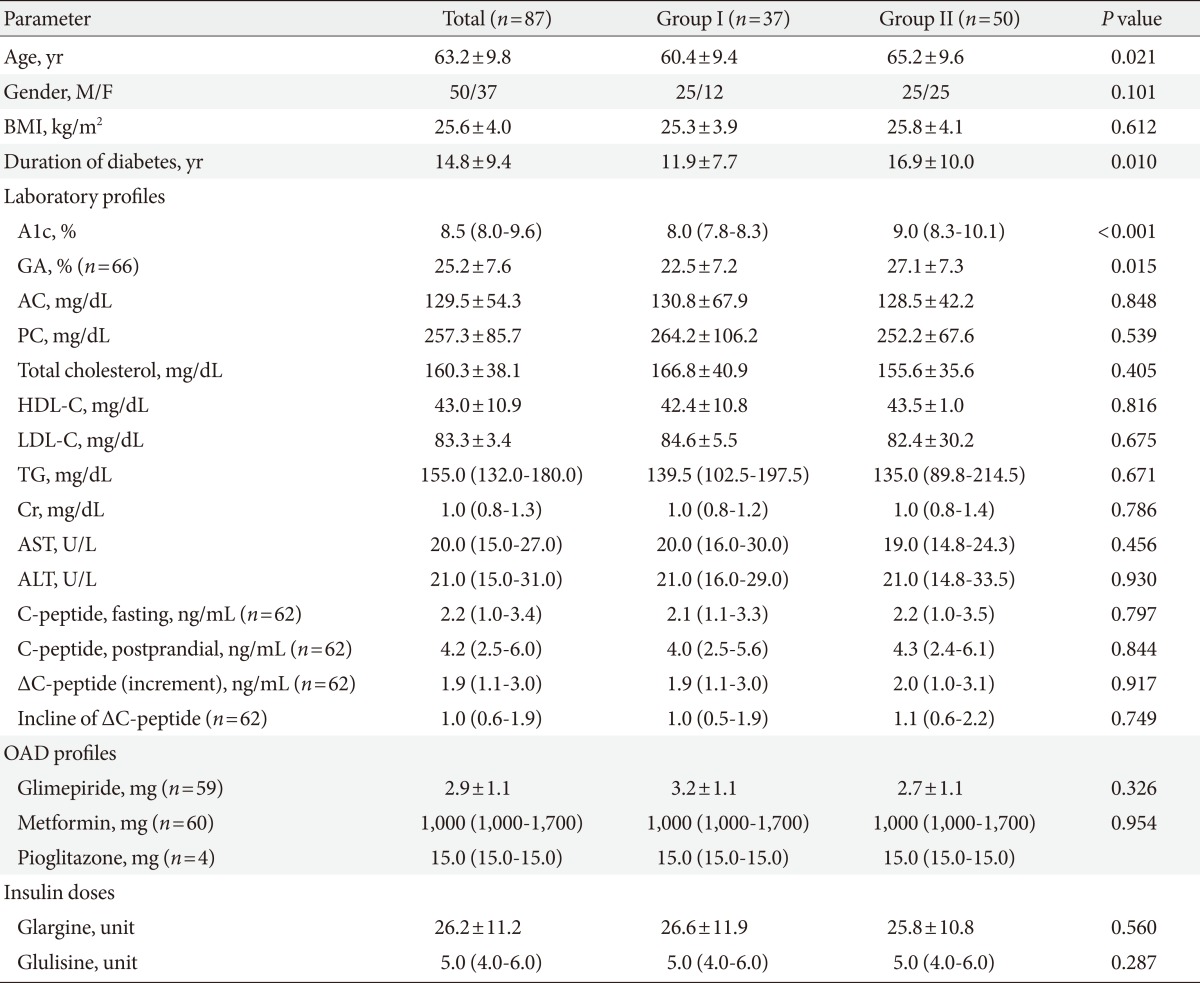
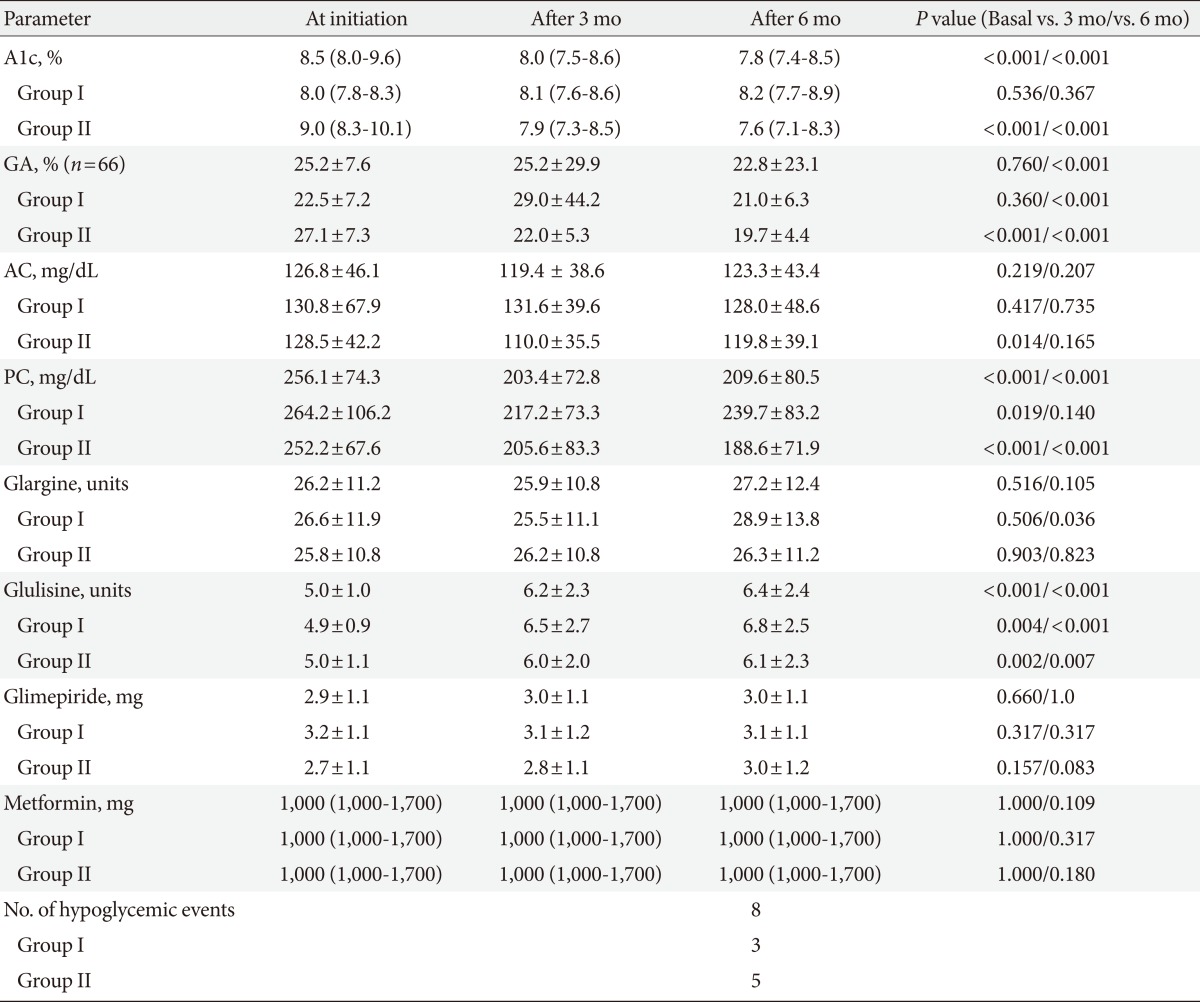
Original ArticleClinical Care/Education Glycemic Effects of Once-a-Day Rapid-Acting Insulin Analogue Addition on a Basal Insulin Analogue in Korean Subjects with Poorly Controlled Type 2 Diabetes Mellitus
- Eun Yeong Choe, Yong-ho Lee, Byung-Wan Lee, Eun-Seok Kang, Bong Soo Cha, Hyun Chul Lee
-
Diabetes & Metabolism Journal 2012;36(3):230-236.
DOI: https://doi.org/10.4093/dmj.2012.36.3.230
Published online: June 14, 2012
Division of Endocrinology and Metabolism, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- Corresponding author: Byung-Wan Lee. Department of Internal Medicine, Yonsei University College of Medicine, 50 Yonsei-ro, Seodaemun-gu, Seoul 120-752, Korea. bwanlee@yuhs.ac
- *Eun Yeong Choe and Yong-ho Lee contributed equally to this study as first authors.
• Received: July 28, 2011 • Accepted: January 16, 2012
Copyright © 2012 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
Figure & Data
References
Citations
Citations to this article as recorded by 

- Titration of basal insulin or immediate addition of rapid acting insulin in patients not at target using basal insulin supported oral antidiabetic treatment – A prospective observational study in 2202 patients
Thorsten Siegmund, Martin Pfohl, Thomas Forst, Stefan Pscherer, Peter Bramlage, Johannes Foersch, Anja Borck, Jochen Seufert
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2017; 11(1): 51. CrossRef - Characteristics Predictive for a Successful Switch from Insulin Analogue Therapy to Oral Hypoglycemic Agents in Patients with Type 2 Diabetes
Gyuri Kim, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Hyun Chul Lee, Byung-Wan Lee
Yonsei Medical Journal.2016; 57(6): 1395. CrossRef - Clinical Characteristics of Patients Responding to Once-Daily Basal Insulin Therapy in Korean Subjects with Type 2 Diabetes
Sun Ok Song, You-Cheol Hwang, Kyu-Jeung Ahn, Bong Soo Cha, Young Duk Song, Dae Wook Lee, Byung-Wan Lee
Diabetes Therapy.2015; 6(4): 547. CrossRef - The optimal morning:evening ratio in total dose of twice‐daily biphasic insulin analogue in poorly controlled Type 2 diabetes: a 24‐week multi‐centre prospective, randomized controlled, open‐labelled clinical study
C. H. Jung, J.‐Y. Park, J. H. Cho, K.‐H. Yoon, H. K. Yang, Y.‐H. Lee, B. S. Cha, B.‐W. Lee
Diabetic Medicine.2014; 31(1): 68. CrossRef -
The glycemic efficacies of insulin analogue regimens according to baseline glycemic status in Korean patients with type 2 diabetes: sub‐analysis from the A
1
chieve
®
study
Y.‐C. Hwang, J. G. Kang, K. J. Ahn, B. S. Cha, S.‐H. Ihm, S. Lee, M. Kim, B.‐W. Lee
International Journal of Clinical Practice.2014; 68(11): 1338. CrossRef

 KDA
KDA
 PubReader
PubReader Cite
Cite