
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Drug/Regimen
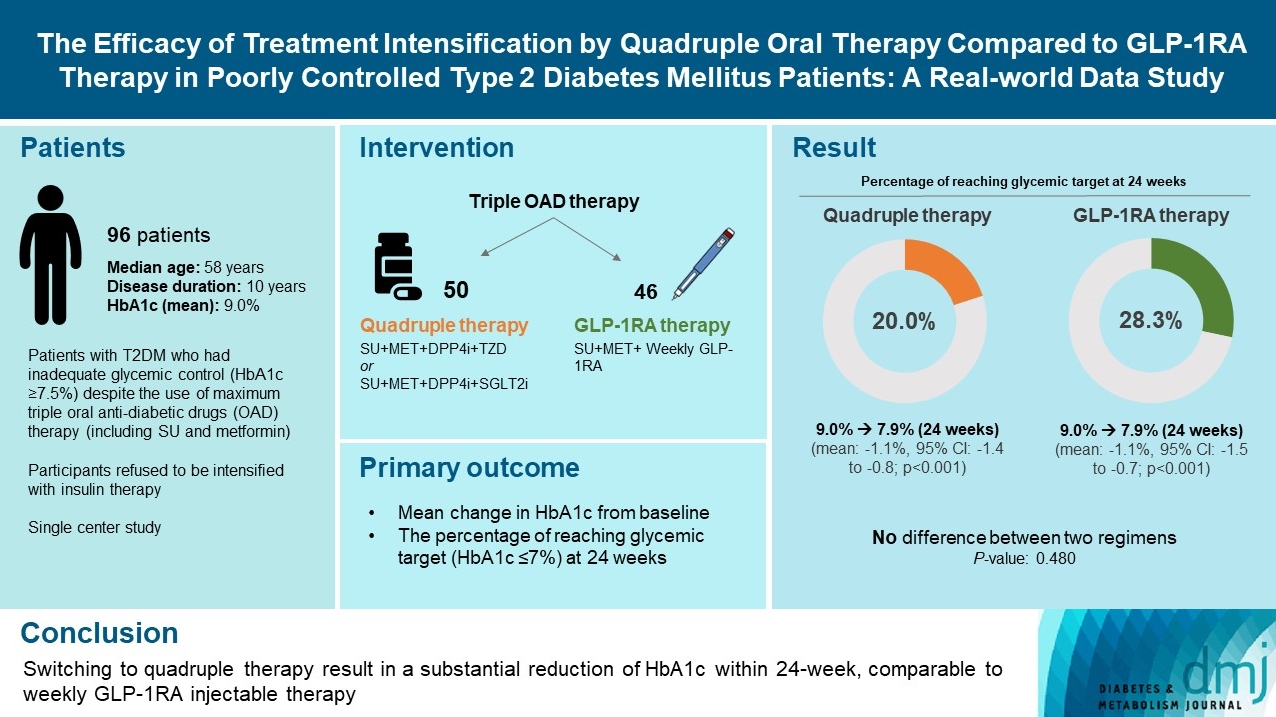
- The Efficacy of Treatment Intensification by Quadruple Oral Therapy Compared to GLP-1RA Therapy in Poorly Controlled Type 2 Diabetes Mellitus Patients: A Real-World Data Study
- Minyoung Kim, Hosu Kim, Kyong Young Kim, Soo Kyoung Kim, Junghwa Jung, Jong Ryeal Hahm, Jaehoon Jung, Jong Ha Baek
- Diabetes Metab J. 2023;47(1):135-139. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0373
- 7,520 View
- 296 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - We compared the glycemic efficacy of treatment intensification between quadruple oral antidiabetic drug therapy and once-weekly glucagon-like peptide-1 receptor agonist (GLP-1RA)-based triple therapy in patients with poorly controlled type 2 diabetes mellitus refractory to triple oral therapy. For 24 weeks, changes in glycosylated hemoglobin (HbA1c) from baseline were compared between the two treatment groups. Of all 96 patients, 50 patients were treated with quadruple therapy, and 46 were treated with GLP-1RA therapy. Reductions in HbA1c for 24 weeks were comparable (in both, 1.1% reduction from baseline; P=0.59). Meanwhile, lower C-peptide level was associated with a lower glucose-lowering response of GLP-1RA therapy (R=0.3, P=0.04) but not with quadruple therapy (R=–0.13, P=0.40). HbA1c reduction by GLP-1RA therapy was inferior to that by quadruple therapy in the low C-peptide subgroup (mean, –0.1% vs. –1.3%; P=0.04). Treatment intensification by switching to quadruple oral therapy showed similar glucose-lowering efficacy to weekly GLP-1RA-based triple therapy. Meanwhile, the therapeutic response was affected by C-peptide levels in the GLP-1RA therapy group but not in the quadruple therapy group.
- Type 1 Diabetes
- Real-World Analysis of Therapeutic Outcome in Type 1 Diabetes Mellitus at a Tertiary Care Center
- Antonia Kietaibl, Michaela Riedl, Latife Bozkurt
- Diabetes Metab J. 2022;46(1):149-153. Published online July 6, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0267
- 4,357 View
- 144 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Insulin replacement in type 1 diabetes mellitus (T1DM) needs intensified treatment, which can either be performed by multiple daily injections (MDI) or continuous subcutaneous insulin infusion (CSII). This retrospective analysis of a real-world scenario aimed to evaluate whether glycaemic and cardiovascular risk factors could be controlled with CSII outclass MDI as suggested by recent evidence. Data from patients with either insulin pump (n=68) or injection (n=224) therapy at an Austrian tertiary care centre were analysed between January 2016 and December 2017. There were no significant differences with regard to the latest glycosylated hemoglobin, cardiovascular risk factor control or diabetes-associated late complications. Hypoglycaemia was less frequent (P<0.001), sensor-augmented therapy was more common (P=0.003) and mean body mass index (BMI) was higher (P=0.002) with CSII treatment. This retrospective analysis of real-world data in T1DM did not demonstrate the superiority of insulin pump treatment with regard to glycaemic control or cardiovascular risk factor control.
- Drug/Regimen
- Evaluating the Evidence behind the Novel Strategy of Early Combination from Vision to Implementation
- Päivi Maria Paldánius
- Diabetes Metab J. 2020;44(6):785-801. Published online September 15, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0179
- 7,109 View
- 287 Download
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
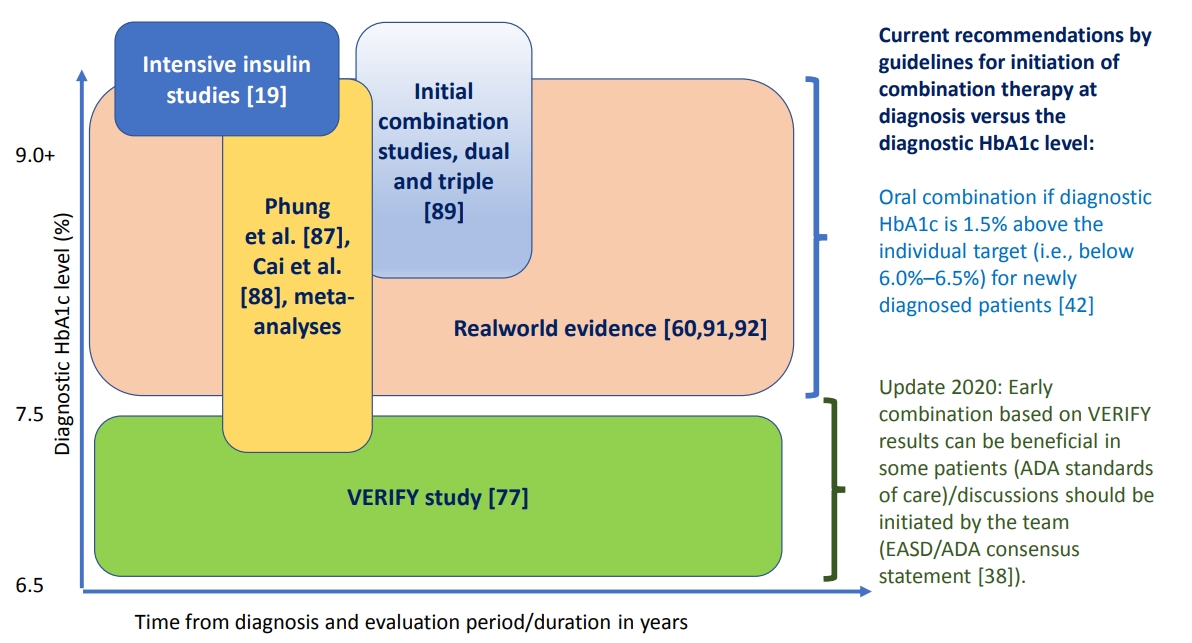
ePub - Type 2 diabetes mellitus (T2DM) is a complex and progressive chronic disease characterised by elevating hyperglycaemia and associated need to gradually intensify therapy in order to achieve and maintain glycaemic control. Treating hyperglycaemia with sequential therapy is proposed to allow holistic assessment of the efficacy and risk-to-benefit ratio of each added component. However, there is an array of evidence supporting the scientific rationale for using synergistic, earlier, modern drug combinations to achieve glycaemic goals, delay the deterioration of glycaemic control, and, therefore, potentially preserve or slow down the declining β-cell function. Additionally, implementation of early combination(s) may lead to opportunities to combat clinical inertia and other hurdles to optimised disease management outcomes. This review aims to discuss the latest empirical evidence for long-term clinical benefits of this novel strategy of early combination in people with newly diagnosed T2DM versus the current widely-implemented treatment paradigm, which focuses on control of hyperglycaemia using lifestyle interventions followed by sequentially intensified (mostly metformin-based) monotherapy. The recent reported Vildagliptin Efficacy in combination with metfoRmin For earlY treatment of T2DM (VERIFY) study results have provided significant new evidence confirming long-term glycaemic durability and tolerability of a specific early combination in the management of newly diagnosed, treatment-naïve patients worldwide. These results have also contributed to changes in clinical treatment guidelines and standards of care while clinical implementation and individualised treatment decisions based on VERIFY results might face barriers beyond the existing scientific evidence.
- Safety and Efficacy of Modern Insulin Analogues
- Hye Jin Yoo, Keun Yong Park, Kang Seo Park, Kyu Jeung Ahn, Kyung Wan Min, Jeong Hyun Park, Sang Ah Chang, Bong Soo Cha, Dong-Jun Kim, Yong Seong Kim, Tae Keun Oh, Suk Chon, Il Seong Nam-Goong, Mi Jin Kim, Hye-Soon Kim, Young Sik Choi, You Hern Ahn, Sora Lee, Sei Hyun Baik
- Diabetes Metab J. 2013;37(3):181-189. Published online June 14, 2013
- DOI: https://doi.org/10.4093/dmj.2013.37.3.181
- 4,116 View
- 32 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background A1chieve® was a noninterventional study evaluating the clinical safety and efficacy of biphasic insulin aspart 30, insulin detemir, and insulin aspart.
Methods Korean type 2 diabetes patients who have not been treated with the study insulin or have started it within 4 weeks before enrollment were eligible for the study. The patient selection and the choice of regimen were at the discretion of the physician. The safety and efficacy information was collected from the subjects at baseline, week 12, and week 24. The number of serious adverse drug reactions (SADRs) was the primary endpoint. The changes of clinical diabetic markers at week 12 and/or at week 24 compared to baseline were the secondary endpoints.
Results Out of 4,058 exposed patients, 3,003 completed the study. During the study period, three SADRs were reported in three patients (0.1%). No major hypoglycemic episodes were observed and the rate of minor hypoglycemic episodes marginally decreased during 24 weeks (from 2.77 to 2.42 events per patient-year). The overall quality of life score improved (from 66.7±15.9 to 72.5±13.5) while the mean body weight was slightly increased (0.6±3.0 kg). The 24-week reductions in glycated hemoglobin, fasting plasma glucose and postprandial plasma glucose were 1.6%±2.2%, 2.5±4.7 mmol/L, and 4.0±6.4 mmol/L, respectively.
Conclusion The studied regimens showed improvements in glycemic control with low incidence of SADRs, including no incidence of major hypoglycemic episodes in Korean patients with type 2 diabetes.
-
Citations
Citations to this article as recorded by- Insulin therapy for adult patients with type 2 diabetes mellitus: a position statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
The Korean Journal of Internal Medicine.2017; 32(6): 967. CrossRef - Insulin Therapy for Adult Patients with Type 2 Diabetes Mellitus: A Position Statement of the Korean Diabetes Association, 2017
Byung-Wan Lee, Jin Hwa Kim, Seung-Hyun Ko, Kyu-Yeon Hur, Nan-Hee Kim, Sang Youl Rhee, Hyun Jin Kim, Min Kyong Moon, Seok-O Park, Kyung Mook Choi
Diabetes & Metabolism Journal.2017; 41(5): 367. CrossRef - An information and communication technology-based centralized clinical trial to determine the efficacy and safety of insulin dose adjustment education based on a smartphone personal health record application: a randomized controlled trial
Gyuri Kim, Ji Cheol Bae, Byoung Kee Yi, Kyu Yeon Hur, Dong Kyung Chang, Moon-Kyu Lee, Jae Hyeon Kim, Sang-Man Jin
BMC Medical Informatics and Decision Making.2017;[Epub] CrossRef - Characteristics Predictive for a Successful Switch from Insulin Analogue Therapy to Oral Hypoglycemic Agents in Patients with Type 2 Diabetes
Gyuri Kim, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Hyun Chul Lee, Byung-Wan Lee
Yonsei Medical Journal.2016; 57(6): 1395. CrossRef - Avoiding or coping with severe hypoglycemia in patients with type 2 diabetes
Jae-Seung Yun, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2015; 30(1): 6. CrossRef - Clinical Characteristics of Patients Responding to Once-Daily Basal Insulin Therapy in Korean Subjects with Type 2 Diabetes
Sun Ok Song, You-Cheol Hwang, Kyu-Jeung Ahn, Bong Soo Cha, Young Duk Song, Dae Wook Lee, Byung-Wan Lee
Diabetes Therapy.2015; 6(4): 547. CrossRef - The optimal morning:evening ratio in total dose of twice‐daily biphasic insulin analogue in poorly controlled Type 2 diabetes: a 24‐week multi‐centre prospective, randomized controlled, open‐labelled clinical study
C. H. Jung, J.‐Y. Park, J. H. Cho, K.‐H. Yoon, H. K. Yang, Y.‐H. Lee, B. S. Cha, B.‐W. Lee
Diabetic Medicine.2014; 31(1): 68. CrossRef -
The glycemic efficacies of insulin analogue regimens according to baseline glycemic status in Korean patients with type 2 diabetes: sub‐analysis from the A
1
chieve
®
study
Y.‐C. Hwang, J. G. Kang, K. J. Ahn, B. S. Cha, S.‐H. Ihm, S. Lee, M. Kim, B.‐W. Lee
International Journal of Clinical Practice.2014; 68(11): 1338. CrossRef - Letter: Efficacy and Safety of Biphasic Insulin Aspart 30/70 in Type 2 Diabetes Suboptimally Controlled on Oral Antidiabetic Therapy in Korea: A Multicenter, Open-Label, Single-Arm Study (Diabetes Metab J2013;37:117-24)
Byung-Wan Lee
Diabetes & Metabolism Journal.2013; 37(3): 212. CrossRef
- Insulin therapy for adult patients with type 2 diabetes mellitus: a position statement of the Korean Diabetes Association, 2017
- Effects of a 6-Month Exenatide Therapy on HbA1c and Weight in Korean Patients with Type 2 Diabetes: A Retrospective Cohort Study
- Juyoung Shin, Jin-Sun Chang, Hun-Sung Kim, Sun-Hee Ko, Bong-Yun Cha, Ho-Young Son, Kun-Ho Yoon, Jae-Hyoung Cho
- Diabetes Metab J. 2012;36(5):364-370. Published online October 18, 2012
- DOI: https://doi.org/10.4093/dmj.2012.36.5.364
- 3,507 View
- 37 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background While many studies have shown the good efficacy and safety of exenatide in patients with diabetes, limited information is available about exenatide in clinical practice in Korean populations. Therefore, this retrospective cohort study was designed to analyze the effects of exenatide on blood glucose level and body weight in Korean patients with type 2 diabetes mellitus.
Methods We reviewed the records of the patients with diabetes who visited Seoul St. Mary's Hospital and for whom exenatide was prescribed from June 2009 to October 2011. After excluding subjects based on their race/ethnicity, medical history, whether or not they changed more than 2 kinds of oral hypoglycemic agents with exenatide treatment, loss to follow-up, or whether they stopped exenatide therapy within 6 months, a total of 52 subjects were included in the final analysis.
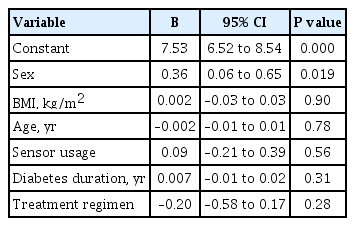
Results The mean glycated hemoglobin (HbA1c) level and weight remarkably decreased from 8.5±1.7% to 6.7±1.0% (
P <0.001) and from 82.3±15.8 kg to 78.6±16.3 kg (P <0.001), respectively. The multiple regression analysis indicated that the reduction in HbA1c level was significantly associated with a shorter duration of diabetes, a higher baseline HbA1c level, and greater weight reduction, whereas weight loss had no significant correlation with other factors. No severe adverse events were observed.Conclusion These results suggest that a 6-month exenatide injection therapy significantly improved patients' HbA1c levels and body weights without causing serious adverse effects in Korean patients with type 2 diabetes.
-
Citations
Citations to this article as recorded by- Clinical and Genetic Predictors of Glycemic Control and Weight Loss Response to Liraglutide in Patients with Type 2 Diabetes
Artemis Kyriakidou, Angeliki V. Kyriazou, Theocharis Koufakis, Yiannis Vasilopoulos, Maria Grammatiki, Xanthippi Tsekmekidou, Iakovos Avramidis, Stefanos Baltagiannis, Dimitrios G. Goulis, Pantelis Zebekakis, Kalliopi Kotsa
Journal of Personalized Medicine.2022; 12(3): 424. CrossRef - Insulin receptor signaling and glucagon-like peptide 1 effects on pancreatic beta cells
Nunzia Caporarello, Cristina Parrino, Vincenzo Trischitta, Lucia Frittitta, Claudia Miele
PLOS ONE.2017; 12(8): e0181190. CrossRef - Exenatide versus Insulin Lispro Added to Basal Insulin in a Subgroup of Korean Patients with Type 2 Diabetes Mellitus
Kun-Ho Yoon, Elise Hardy, Jenny Han
Diabetes & Metabolism Journal.2017; 41(1): 69. CrossRef - Acarbose reduces body weight irrespective of glycemic control in patients with diabetes: results of a worldwide, non-interventional, observational study data pool
Oliver Schnell, Jianping Weng, Wayne H.-H. Sheu, Hirotaka Watada, Sanjay Kalra, Sidartawan Soegondo, Noriyuki Yamamoto, Rahul Rathod, Cheryl Zhang, Wladyslaw Grzeszczak
Journal of Diabetes and its Complications.2016; 30(4): 628. CrossRef - Determining Predictors of Early Response to Exenatide in Patients with Type 2 Diabetes Mellitus
Muhammad Khan, Jing Ouyang, Karen Perkins, Sunil Nair, Franklin Joseph
Journal of Diabetes Research.2015; 2015: 1. CrossRef - The Role of Glucagon-Like Peptide-1 Receptor Agonists in Type 2 Diabetes: Understanding How Data Can Inform Clinical Practice in Korea
Seungjoon Oh, Suk Chon, Kyu Jeong Ahn, In-Kyung Jeong, Byung-Joon Kim, Jun Goo Kang
Diabetes & Metabolism Journal.2015; 39(3): 177. CrossRef - Tolerability, effectiveness and predictive parameters for the therapeutic usefulness of exenatide in obese, Korean patients with type 2 diabetes
Sun Ok Song, Kwang Joon Kim, Byung‐Wan Lee, Eun Seok Kang, Bong Soo Cha, Hyun Chul Lee
Journal of Diabetes Investigation.2014; 5(5): 554. CrossRef - From endocrine to rheumatism: do gut hormones play roles in rheumatoid arthritis?
C.-Y. Chen, C.-Y. Tsai
Rheumatology.2014; 53(2): 205. CrossRef - Early use of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) in Type 2 diabetes
Stuart A. Ross, Jane Ballantine
Current Medical Research and Opinion.2013; 29(12): 1617. CrossRef
- Clinical and Genetic Predictors of Glycemic Control and Weight Loss Response to Liraglutide in Patients with Type 2 Diabetes
- Retrospective Analysis on the Efficacy, Safety and Treatment Failure Group of Sitagliptin for Mean 10-Month Duration
- Won Jun Kim, Cheol-Young Park, Eun Haeng Jeong, Jeong Youn Seo, Ji Soo Seol, Se Eun Park, Eun Jung Rhee, Won Young Lee, Ki Won Oh, Sung Woo Park, Sun Woo Kim
- Diabetes Metab J. 2011;35(3):290-297. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.290
- 4,301 View
- 31 Download
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To investigate the clinical results of sitagliptin (SITA) and the characteristics of the treatment failure group or of low responders to SITA.
Methods A retrospective study of type 2 diabetic patients reviewed 99 cases, including 12 treatment failure cases, who stopped SITA because of worsening patients' condition, and 87 cases, who continued treatment over five visits (total 9.9±10.1 months) after receiving the prescription of SITA from December 2008 to June 2009. Subjects were classified as five groups administered SITA as an initial combination with metformin (MET), add-on to metformin or sulfonylurea, and switching from sulfonylurea or thiazolidinedione. The changes in HbA1c level from the first to last visit (ΔHbA1c) in treatment maintenance group were subanalyzed.
Results The HbA1c level was significantly reduced in four groups, including initial coadministration of SITA with metformin (ΔHbA1c=-1.1%,
P <0.001), add-on to MET (ΔHbA1c=-0.6%,P =0.017), add-on to sulfonylurea (ΔHbA1c=-0.5%,P <0.001), and switching from thiazolidinedione (ΔHbA1c=-0.3%,P =0.013). SITA was noninferior to sulfonlyurea (ΔHbA1c=-0.2%,P =0.63). There was no significant adverse effect. The treatment failure group had a longer diabeties duration (P =0.008), higher HbA1c (P =0.001) and fasting plasma glucose (P =0.003) compared to the maintenance group. Subanalysis on the tertiles of ΔHbA1c showed that low-response to SITA (tertile 1) was associated with a longer diabetes duration (P =0.009) and lower HbA1c (P <0.001).Conclusion SITA was effective and safe for use in Korean type 2 diabetic patients. However, its clinical responses and long-term benefit-harm profile is yet to be established.
-
Citations
Citations to this article as recorded by- Development of a 13C Stable Isotope Assay for Dipeptidyl Peptidase-4 Enzyme Activity A New Breath Test for Dipeptidyl Peptidase Activity
Roger Yazbeck, Simone Jaenisch, Michelle Squire, Catherine A. Abbott, Emma Parkinson-Lawrence, Douglas A. Brooks, Ross N. Butler
Scientific Reports.2019;[Epub] CrossRef - Characterization of changes in HbA1c in patients with and without secondary failure after metformin treatments by a population pharmacodynamic analysis using mixture models
Yoko Tamaki, Kunio Maema, Makoto Kakara, Masato Fukae, Ryoko Kinoshita, Yushi Kashihara, Shota Muraki, Takeshi Hirota, Ichiro Ieiri
Drug Metabolism and Pharmacokinetics.2018; 33(6): 264. CrossRef - Effects of 6-Month Sitagliptin Treatment on Insulin and Glucagon Responses in Korean Patients with Type 2 Diabetes Mellitus
Hae Kyung Yang, Borami Kang, Seung-Hwan Lee, Hun-Sung Kim, Kun-Ho Yoon, Bong-Yun Cha, Jae-Hyoung Cho
Diabetes & Metabolism Journal.2015; 39(4): 335. CrossRef - Clinical Characteristics and Metabolic Predictors of Rapid Responders to Dipeptidyl Peptidase-4 Inhibitor as an Add-on Therapy to Sulfonylurea and Metformin
Ye An Kim, Won Sang Yoo, Eun Shil Hong, Eu Jeong Ku, Kyeong Seon Park, Soo Lim, Young Min Cho, Kyong Soo Park, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2015; 39(6): 489. CrossRef - Letter: Predictive Factors for Efficacy of Dipeptidyl Peptidase-4 Inhibitors in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2015;39:342-7)
Ye An Kim
Diabetes & Metabolism Journal.2015; 39(5): 444. CrossRef - Optimal Candidates for the Switch from Glimepiride to Sitagliptin to Reduce Hypoglycemia in Patients with Type 2 Diabetes Mellitus
Hyun Min Kim, Jung Soo Lim, Byung-Wan Lee, Eun-Seok Kang, Hyun Chul Lee, Bong-Soo Cha
Endocrinology and Metabolism.2015; 30(1): 84. CrossRef - One-year real-life efficacy of sitagliptin revealed importance of concomitant pioglitazone use in Japanese patients with type 2 diabetes mellitus
Ayako Suzuki, Nakayuki Yoshimura, Yamato Mashimo, Maiko Numakura, Yuko Fujimaki, Tomomi Maeda, Toshio Ishikawa, Shin Fujimori, Kazuhiro Eto
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2013; 7(3): 143. CrossRef - Clinical Characteristics of the Responders to Dipeptidyl Peptidase-4 Inhibitors in Korean Subjects with Type 2 Diabetes
Tae Jung Oh, Hye Seung Jung, Jae Hyun Bae, Yeong Gi Kim, Kyeong Seon Park, Young Min Cho, Kyong Soo Park, Seong Yeon Kim
Journal of Korean Medical Science.2013; 28(6): 881. CrossRef - Factors predicting therapeutic efficacy of combination treatment with sitagliptin and metformin in type 2 diabetic patients: the COSMETIC study
Soo Lim, Jee Hyun An, Hayley Shin, Ah Reum Khang, Yenna Lee, Hwa Young Ahn, Ji Won Yoon, Seon Mee Kang, Sung Hee Choi, Young Min Cho, Kyong Soo Park, Hak Chul Jang
Clinical Endocrinology.2012; 77(2): 215. CrossRef
- Development of a 13C Stable Isotope Assay for Dipeptidyl Peptidase-4 Enzyme Activity A New Breath Test for Dipeptidyl Peptidase Activity
- Therapeutic Target Achievement in Type 2 Diabetic Patients after Hyperglycemia, Hypertension, Dyslipidemia Management
- Ah Young Kang, Su Kyung Park, So Young Park, Hye Jeong Lee, Ying Han, Sa Ra Lee, Sung Hwan Suh, Duk Kyu Kim, Mi Kyoung Park
- Diabetes Metab J. 2011;35(3):264-272. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.264
- 10,052 View
- 35 Download
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Our study group established "3H care" in 2002. The meaning of "3H care" attain and maintain adequate controls over hypertension, hyperlipidemia, and hyperglycemia in type 2 diabetic patients. This study evaluated the achievement of target goals after one year or more of "3H care" by specialists in our diabetic clinic.
Methods This was a retrospective study of 200 type 2 diabetic patients who received "3H care" for one year or more in our diabetic clinic. We evaluated achievement of target goals for metabolic controls as suggested by the American Diabetes Association.
Results Overall, 200 type 2 diabetes patients were enrolled, of whom 106 were males (53%) and 94 were females (47%). After one year of "3H care," the mean HbA1c was 7.2±1.5% and the percentage of patients achieving glycemic control (HbA1c <7%) was 51.8%. However only 32.2% of hypertensive patients achieved the recommended target. After one year of "3H care," the percentages of those who achieved the target value for dyslipidemia were 80.0% for total cholesterol, 66.3% for low density lipoprotein cholesterol, 57.9% for triglyceride, and 51.8% for high density lipoprotein cholesterol. The percentage that achieved all three targets level was only 4.4% after one year and 14.8% after two years.
Conclusion The results of this study demonstrate that only a minor proportion of patients with type 2 diabetes achieved the recommended goals despite the implementation of "3H care." It is our suggestion that better treatment strategies and methods should be used to control hypertension, hyperlipidemia and hyperglycemia.
-
Citations
Citations to this article as recorded by- Achievement of the ABC goal among Canadians with type 2 diabetes and the influence of physical activity: data from the Canadian Health Measures Survey
Alexis Marcotte-Chénard, René Maréchal, Ahmed Ghachem, Alan Cohen, Eléonor Riesco
Applied Physiology, Nutrition, and Metabolism.2023; 48(9): 657. CrossRef - Poor Adherence to Common Recommendations and Associated Factors among Outpatients with Type 2 Diabetes Mellitus in a Police Hospital of Ethiopia
Tariku Shimels, Melesse Abebaw, Gebremedhin Beedemariam Gebretekle
Journal of Social Health and Diabetes.2021; 9(01): e8. CrossRef - Prevalence and correlation of glycemic control achievement in patients with type 2 diabetes in Iraq: A retrospective analysis of a tertiary care database over a 9-year period
Abbas Ali Mansour, Nassar T.Y. Alibrahim, Haider A. Alidrisi, Ali H. Alhamza, Ammar M. Almomin, Ibrahim Abbood Zaboon, Muayad Baheer Kadhim, Rudha Naser Hussein, Hussein Ali Nwayyir, Adel Gassab Mohammed, Dheyaa K.J. Al-Waeli, Ibrahim Hani Hussein
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(3): 265. CrossRef - Notoginsenoside R1 Ameliorates Diabetic Retinopathy through PINK1-Dependent Activation of Mitophagy
Ping Zhou, Weijie Xie, Xiangbao Meng, Yadong Zhai, Xi Dong, Xuelian Zhang, Guibo Sun, Xiaobo Sun
Cells.2019; 8(3): 213. CrossRef - Association of Self-Reported Dietary and Drug Compliance with Optimal Metabolic Control in Patients with Type 2 Diabetes: Clinic-Based Single-Center Study in a Developing Country
Thilak Priyantha Weerarathna, Miyuru Kavinda Weerarathna, Vidarsha Senadheera, Herath Mudiyanselage Meththananda Herath, Gayani Liyanage
Journal of Nutrition and Metabolism.2018; 2018: 1. CrossRef - Prevalence of primary aldosteronism among patients with type 2 diabetes
Mauro Tancredi, Gudmundur Johannsson, Björn Eliasson, Robert Eggertsen, Ulf Lindblad, Sofia Dahlqvist, Henrik Imberg, Marcus Lind
Clinical Endocrinology.2017; 87(3): 233. CrossRef - GS-E3D, a new pectin lyase-modified red ginseng extract, inhibited diabetes-related renal dysfunction in streptozotocin-induced diabetic rats
Chan-Sik Kim, Kyuhyung Jo, Jin Sook Kim, Mi-Kyung Pyo, Junghyun Kim
BMC Complementary and Alternative Medicine.2017;[Epub] CrossRef - Ursodeoxycholic acid and 4-phenylbutyrate prevent endoplasmic reticulum stress-induced podocyte apoptosis in diabetic nephropathy
Ai-Li Cao, Li Wang, Xia Chen, Yun-Man Wang, Heng-Jiang Guo, Shuang Chu, Cheng Liu, Xue-Mei Zhang, Wen Peng
Laboratory Investigation.2016; 96(6): 610. CrossRef - Ursodeoxycholic Acid Ameliorated Diabetic Nephropathy by Attenuating Hyperglycemia-Mediated Oxidative Stress
Aili Cao, Li Wang, Xia Chen, Hengjiang Guo, Shuang Chu, Xuemei Zhang, Wen Peng
Biological & Pharmaceutical Bulletin.2016; 39(8): 1300. CrossRef - Withania coagulansFruit Extract Reduces Oxidative Stress and Inflammation in Kidneys of Streptozotocin-Induced Diabetic Rats
Shreesh Ojha, Juma Alkaabi, Naheed Amir, Azimullah Sheikh, Ahmad Agil, Mohamed Abdelmonem Fahim, Abdu Adem
Oxidative Medicine and Cellular Longevity.2014; 2014: 1. CrossRef - Assessment of cardiometabolic risk and prevalence of meeting treatment guidelines among patients with type 2 diabetes stratified according to their use of insulin and/or other diabetic medications: results from INSPIRE ME IAA
J. Smith, J.‐A. Nazare, A.‐L. Borel, P. Aschner, P. J. Barter, L. Van Gaal, Y. Matsuzawa, T. Kadowaki, R. Ross, C. Brulle‐Wohlhueter, N. Alméras, S. M. Haffner, B. Balkau, J.‐P. Després
Diabetes, Obesity and Metabolism.2013; 15(7): 629. CrossRef - Are PPAR alpha agonists a rational therapeutic strategy for preventing abnormalities of the diabetic kidney?
Pitchai Balakumar, Supriya Kadian, Nanjaian Mahadevan
Pharmacological Research.2012; 65(4): 430. CrossRef
- Achievement of the ABC goal among Canadians with type 2 diabetes and the influence of physical activity: data from the Canadian Health Measures Survey
- The Current Status of Type 2 Diabetes Management at a University Hospital.
- Young Sil Lee
- Korean Diabetes J. 2009;33(3):241-250. Published online June 1, 2009
- DOI: https://doi.org/10.4093/kdj.2009.33.3.241
- 2,231 View
- 22 Download
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
The prevalence of type 2 diabetes has increased worldwide, as have the incidence and mortality of associated cardiovascular complication. However current status of diabetes management is poor. This study was performed to evaluate the management of care for type 2 diabetes patients at a university hospital. METHODS: This study comprised 926 type 2 diabetes patients, over the age of 30, who were treated at the Dongguk University Gyeongju Hospital between January and December 2008. Medical records were reviewed to collect demographic information, biochemical test results and the pharmacologic agents prescribed. RESULTS: The mean age, duration of diabetes and body mass index were 62.5 +/- 11.8 years, 9.1 +/- 7.2 year and 24.7 +/- 6.3 kg/m2, respectively. There were 251/926 (27.1%) patients with cardiovascular disease. In addition, 49.2% and 27.5% of patients had HbA1c levels < 7% and < 6.5%, respectively. There were 66.3% of the patients with blood pressure < 130/80 mm Hg. Fifty one percent and 47.4% of the patients had an LDL-C < 100 mg/dL and a non-HDL-C < 130 mg/dL, respectively. In addition, 19.7% of the patients with cardiovascular disease had an LDL-C < 70 mg/dL. Antiplatelet agents were used in 81.2% of the patients. The mean number of HbA1c measurements was 1.07 +/- 0.7 /year. HbA1c and lipid profiles were not checked in 21.4% and 23.1% of the patients, respectively. Over the previous six months, 6.9% of the patients had not had their blood pressure monitored. CONCLUSION: Among the patients with type 2 diabetes evaluated, 30~70% received in inadequate level of care. These findings point to the need for more aggressive efforts for optimal metabolic control. -
Citations
Citations to this article as recorded by- Developing a nomogram for predicting depression in diabetic patients after COVID-19 using machine learning
Haewon Byeon
Frontiers in Public Health.2023;[Epub] CrossRef - Factors Influencing the Utilization of Diabetes Complication Tests Under the COVID-19 Pandemic: Machine Learning Approach
Haewon Byeon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Correlation between the Activity of Aldehyde Dehydrogenase and Oxidative Stress Markers in the Saliva of Diabetic Patients
Hina Younus, Sumbul Ahmad, Md. Fazle Alam
Protein & Peptide Letters.2019; 27(1): 67. CrossRef - Current status of treatment of type 2 diabetes mellitus in Ningbo, China
Tianmeng Yang, Rongjiong Zheng, Qingmei Chen, Yushan Mao
Journal of Clinical Laboratory Analysis.2019;[Epub] CrossRef - Current Status of Management in Type 2 Diabetes Mellitus at General Hospitals in South Korea
Jin-Hee Jung, Jung-Hwa Lee, Jin-Won Noh, Jeong-Eun Park, Hee-Sook Kim, Joo-Wha Yoo, Bok-Rye Song, Jeong-rim Lee, Myeong-Hee Hong, Hyang-Mi Jang, Young Na, Hyun-Joo Lee, Jeong-Mi Lee, Yang-Gyo Kang, Sun-Young Kim, Kang-Hee Sim
Diabetes & Metabolism Journal.2015; 39(4): 307. CrossRef - Glucose, Blood Pressure, and Lipid Control in Korean Adults with Diagnosed Diabetes
Sun-Joo Boo
Korean Journal of Adult Nursing.2012; 24(4): 406. CrossRef - Diabetics' Preference in the Design Factors and Performance Requirements of Diabetic Socks
Ji-Eun Lee, Young-Ah Kwon
Journal of the Korean Society of Clothing and Textiles.2011; 35(5): 527. CrossRef - Effect on Glycemic, Blood Pressure, and Lipid Control according to Education Types
Mi-Ju Choi, Seung-Hyun Yoo, Kum-Rae Kim, Yoo-Mi Bae, Sun-Hee Ahn, Seong-Shin Kim, Seong-Ah Min, Jin-Sun Choi, Seung-Eun Lee, Yeo-Jin Moon, Eun Jung Rhee, Cheol-Young Park, Won Young Lee, Ki Won Oh, Sung Woo Park, Sun Woo Kim
Diabetes & Metabolism Journal.2011; 35(6): 580. CrossRef - Therapeutic Target Achievement in Type 2 Diabetic Patients after Hyperglycemia, Hypertension, Dyslipidemia Management
Ah Young Kang, Su Kyung Park, So Young Park, Hye Jeong Lee, Ying Han, Sa Ra Lee, Sung Hwan Suh, Duk Kyu Kim, Mi Kyoung Park
Diabetes & Metabolism Journal.2011; 35(3): 264. CrossRef - A Predictive Model on Self Care Behavior for Patients with Type 2 Diabetes: Based on Self-Determination Theory
Yeong Mi Seo, Won Hee Choi
Journal of Korean Academy of Nursing.2011; 41(4): 491. CrossRef
- Developing a nomogram for predicting depression in diabetic patients after COVID-19 using machine learning

 KDA
KDA
 First
First Prev
Prev





