
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Lifestyle
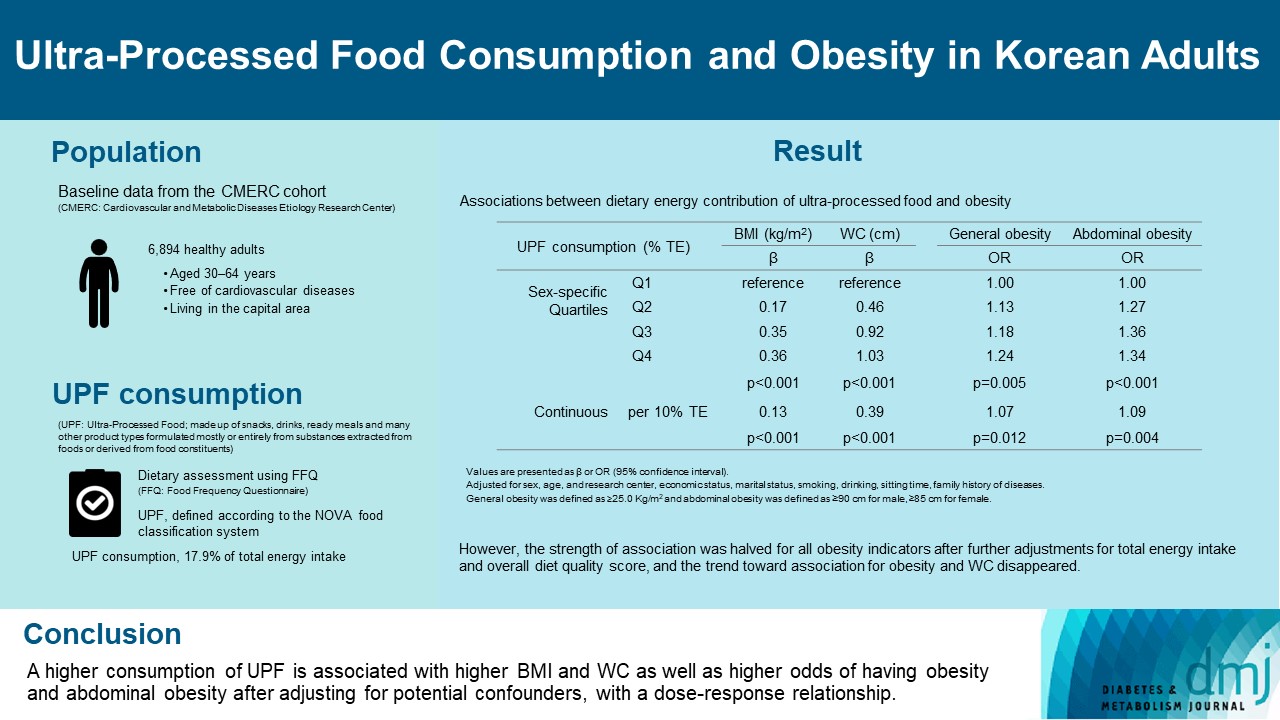
- Ultra-Processed Food Consumption and Obesity in Korean Adults
- Jee-Seon Shim, Kyoung Hwa Ha, Dae Jung Kim, Hyeon Chang Kim
- Diabetes Metab J. 2023;47(4):547-558. Published online April 26, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0026
- 2,854 View
- 139 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
This study aimed to investigate the association between consumption of ultra-processed foods (UPF) and obesity in Korean adults.
Methods
We included the Cardiovascular and Metabolic Diseases Etiology Research Center cohort study baseline data of adults aged 30 to 64 years who completed a validated food frequency questionnaire. UPF was defined using the NOVA food classification. Multivariable linear and logistic regression analyses were performed to assess the association of dietary energy contribution of UPF with obesity indicators (body mass index [BMI], obesity, waist circumference [WC], and abdominal obesity).
Results
Consumption of UPF accounted for 17.9% of total energy intake and obesity and abdominal obesity prevalence was 35.4% and 30.2%, respectively. Compared with those in the lowest quartile of UPF consumption, adults in the highest quartile had greater BMI (β=0.36; 95% confidence interval [CI], 0.15 to 0.56), WC (β=1.03; 95% CI, 0.46 to 1.60), higher odds of having obesity (odds ratio [OR], 1.24; 95% CI, 1.07 to 1.45), and abdominal obesity (OR, 1.34; 95% CI, 1.14 to 1.57), after adjusting for sociodemographic characteristics, health-related behaviors, and family history of diseases. Dose-response associations between UPF consumption and obesity indicators were consistently found (all P trend <0.01). However, the strength of association was halved for all obesity indicators after further adjustments for total energy intake and overall diet quality score, and the trend toward association for obesity and WC disappeared.
Conclusion
Our finding supports the evidence that consumption of UPF is positively associated with obesity among Korean adults. -
Citations
Citations to this article as recorded by- Ultra-processed food consumption and increased risk of metabolic syndrome in Korean adults: A cross-sectional analysis of the KNHANES 2016–2020
Hansol Park, Youngmi Lee, Jinah Hwang, Yujin Lee
Nutrition.2024; 122: 112374. CrossRef - Diet quality partially mediates the association between ultraprocessed food consumption and adiposity indicators
Jee‐Seon Shim, Kyoung Hwa Ha, Dae Jung Kim, Hyeon Chang Kim
Obesity.2023; 31(9): 2430. CrossRef - Development of a Semi-Quantitative Food-Frequency Questionnaire for Korean Adults with Obesity
Jina Chung, Seoeun Ahn, Hyojee Joung, Sangah Shin
Nutrients.2023; 15(22): 4848. CrossRef
- Ultra-processed food consumption and increased risk of metabolic syndrome in Korean adults: A cross-sectional analysis of the KNHANES 2016–2020
- Drug/Regimen
- A Real-World Study of Long-Term Safety and Efficacy of Lobeglitazone in Korean Patients with Type 2 Diabetes Mellitus
- Bo-Yeon Kim, Hyuk-Sang Kwon, Suk Kyeong Kim, Jung-Hyun Noh, Cheol-Young Park, Hyeong-Kyu Park, Kee-Ho Song, Jong Chul Won, Jae Myung Yu, Mi Young Lee, Jae Hyuk Lee, Soo Lim, Sung Wan Chun, In-Kyung Jeong, Choon Hee Chung, Seung Jin Han, Hee-Seok Kim, Ju-Young Min, Sungrae Kim
- Diabetes Metab J. 2022;46(6):855-865. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0264
- 6,696 View
- 296 Download
- 6 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Thiazolidinediones (TZDs) have been associated with various safety concerns including weight gain, bladder cancer, and congestive heart failure (CHF). This study evaluated the efficacy and safety of lobeglitazone, a novel TZD in patients with type 2 diabetes mellitus (T2DM) in real practice.
Methods
In this non-interventional, multi-center, retrospective, and observational study conducted at 15 tertiary or secondary referral hospitals in Korea, a total of 2,228 patients with T2DM who received lobeglitazone 0.5 mg for more than 1 year were enrolled.
Results
Overall adverse events (AEs) occurred in 381 patients (17.10%) including edema in 1.97% (n=44). Cerebrovascular and cardiovascular diseases were identified in 0.81% (n=18) and 0.81% (n=18), respectively. One case of CHF was reported as an AE. Edema occurred in 1.97% (n=44) of patients. Hypoglycemia occurred in 2.47% (n=55) of patients. Fracture occurred in 1.17% (n=26) of all patients. Lobeglitazone significantly decreased HbA1c level, resulting in a mean treatment difference of -1.05%± 1.35% (P<0.001), and decreased total cholesterol, triglyceride, and low-density lipoprotein cholesterol. However, it increased high-density lipoprotein cholesterol, regardless of statin administration. The patients who received lobeglitazone 0.5 mg showed an apparent reduction in glycosylated hemoglobin (HbA1c) from baseline during the first 6 months of treatment. The HbA1c levels remained stable between months 6 and 42.
Conclusion
Lobeglitazone has long-term safety profile, good glycemic-lowering effect and long-term durability of glycemic control in real-world clinical settings. -
Citations
Citations to this article as recorded by- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
Deep Dutta, Saptarshi Bhattacharya, Manoj Kumar, Priyankar K. Datta, Ritin Mohindra, Meha Sharma
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102697. CrossRef - Efficacy and safety of lobeglitazone, a new Thiazolidinedione, as compared to the standard of care in type 2 diabetes mellitus: A systematic review and meta-analysis
Shashank R. Joshi, Saibal Das, Suja Xaviar, Shambo Samrat Samajdar, Indranil Saha, Sougata Sarkar, Shatavisa Mukherjee, Santanu Kumar Tripathi, Jyotirmoy Pal, Nandini Chatterjee
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(1): 102703. CrossRef - Will lobeglitazone rival pioglitazone? A systematic review and critical appraisal
Kalyan Kumar Gangopadhyay, Awadhesh Kumar Singh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(4): 102747. CrossRef - Lobeglitazone
Reactions Weekly.2023; 1948(1): 262. CrossRef - Lobeglitazone, a novel thiazolidinedione, for secondary prevention in patients with ischemic stroke: a nationwide nested case-control study
Joonsang Yoo, Jimin Jeon, Minyoul Baik, Jinkwon Kim
Cardiovascular Diabetology.2023;[Epub] CrossRef - Lobeglitazone and Its Therapeutic Benefits: A Review
Balamurugan M, Sarumathy S, Robinson R
Cureus.2023;[Epub] CrossRef - Oldies but Goodies: Thiazolidinedione as an Insulin Sensitizer with Cardioprotection
Eun-Hee Cho
Diabetes & Metabolism Journal.2022; 46(6): 827. CrossRef
- Efficacy and safety of novel thiazolidinedione lobeglitazone for managing type-2 diabetes a meta-analysis
- Obesity and Metabolic Syndrome
-
- The Risk of Myocardial Infarction and Ischemic Stroke According to Waist Circumference in 21,749,261 Korean Adults: A Nationwide Population-Based Study
- Jung-Hwan Cho, Eun-Jung Rhee, Se-Eun Park, Hyemi Kwon, Jin-Hyung Jung, Kyung-Do Han, Yong-Gyu Park, Hye Soon Park, Yang-Hyun Kim, Soon-Jib Yoo, Won-Young Lee
- Diabetes Metab J. 2019;43(2):206-221. Published online December 27, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0039
- 5,606 View
- 102 Download
- 22 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background Waist circumference (WC) is a well-known obesity index that predicts cardiovascular disease (CVD). We studied the relationship between baseline WC and development of incident myocardial infarction (MI) and ischemic stroke (IS) using a nationwide population-based cohort, and evaluated if its predictability is better than body mass index (BMI).
Methods Our study included 21,749,261 Koreans over 20 years of age who underwent the Korean National Health Screening between 2009 and 2012. The occurrence of MI or IS was investigated until the end of 2015 using National Health Insurance Service data.
Results A total of 127,289 and 181,637 subjects were newly diagnosed with MI and IS. The incidence rate and hazard ratio of MI and IS increased linearly as the WC level increased, regardless of adjustment for BMI. When the analyses were performed according to 11 groups of WC, the lowest risk of MI was found in subjects with WC of 70 to 74.9 and 65 to 69.9 cm in male and female, and the lowest risk of IS in subjects with WC of 65 to 69.9 and 60 to 64.9 cm in male and female, respectively. WC showed a better ability to predict CVD than BMI with smaller Akaike information criterion. The optimal WC cutoffs were 84/78 cm for male/female for predicting MI, and 85/78 cm for male/female for predicting IS.
Conclusion WC had a significant linear relationship with the risk of MI and IS and the risk began to increase from a WC that was lower than expected.
-
Citations
Citations to this article as recorded by- Usefulness of New Criteria for Metabolic Syndrome Optimized for Prediction of Cardiovascular Diseases in Japanese
Yurie Yamazaki, Kazuya Fujihara, Takaaki Sato, Mayuko Harada Yamada, Yuta Yaguchi, Yasuhiro Matsubayashi, Takaho Yamada, Satoru Kodama, Kiminori Kato, Hitoshi Shimano, Hirohito Sone
Journal of Atherosclerosis and Thrombosis.2024; 31(4): 382. CrossRef - Association between body composition and subsequent cardiovascular diseases among 5-year breast cancer survivors
Ji Soo Kim, Jihun Song, Seulggie Choi, Sung Min Kim, Young Jun Park, Sun Jae Park, Yoosun Cho, Yun Hwan Oh, Seogsong Jeong, Kyae Hyung Kim, Sang Min Park
Nutrition, Metabolism and Cardiovascular Diseases.2024;[Epub] CrossRef - Body mass index, waist circumference and cardiovascular diseases in transitional ages (40 and 66 years)
Jung Eun Yoo, Kyungdo Han, Jin‐Hyung Jung, Yang‐Im Hur, Yang Hyun Kim, Eun Sook Kim, Jang Won Son, Eun‐Jung Rhee, Won‐Young Lee, Ga Eun Nam
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(1): 369. CrossRef - Risk factors for stroke among anthropometric indices and lipid profiles in the Korean population: a large-scale cross-sectional study
Mi Hong Yim, Young Ju Jeon, Bum Ju Lee
Scientific Reports.2023;[Epub] CrossRef - Big Data Research in the Field of Endocrine Diseases Using the Korean National Health Information Database
Sun Wook Cho, Jung Hee Kim, Han Seok Choi, Hwa Young Ahn, Mee Kyoung Kim, Eun Jung Rhee
Endocrinology and Metabolism.2023; 38(1): 10. CrossRef - Research on obesity using the National Health Information Database: recent trends
Eun-Jung Rhee
Cardiovascular Prevention and Pharmacotherapy.2023; 5(2): 35. CrossRef - Association between the weight-adjusted waist index and stroke: a cross-sectional study
Jiayi Ye, Yanjie Hu, Xinrong Chen, Zhe Yin, Xingzhu Yuan, Liping Huang, Ka Li
BMC Public Health.2023;[Epub] CrossRef - Increased risk of ischemic stroke associated with elevated gamma-glutamyl transferase level in adult cancer survivors: a population-based cohort study
Kyuwoong Kim, Hyeyun Jung, Edvige Di Giovanna, Tae Joon Jun, Young-Hak Kim
Scientific Reports.2023;[Epub] CrossRef - Changes in body composition and subsequent cardiovascular disease risk among 5-year breast cancer survivors
Ji Soo Kim, Jihun Song, Seulggie Choi, Sang Min Park
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Association between Stroke and Abdominal Obesity in the Middle-Aged and Elderly Korean Population: KNHANES Data from 2011–2019
Jong Yeon Kim, Sung Min Cho, Youngmin Yoo, Taesic Lee, Jong Koo Kim
International Journal of Environmental Research and Public Health.2022; 19(10): 6140. CrossRef - Prevalence of metabolic syndrome and related factors in a large sample of antipsychotic naïve patients with first-episode psychosis: Baseline results from the PAFIP cohort
Nathalia Garrido-Torres, Miguel Ruiz-Veguilla, Luis Alameda, Manuel Canal-Rivero, María Juncal Ruiz, Marcos Gómez-Revuelta, Rosa Ayesa-Arriola, Ana Rubio-García, Benedicto Crespo-Facorro, Javier Vázquez-Bourgon
Schizophrenia Research.2022; 246: 277. CrossRef - Development and validation of risk prediction models for stroke and mortality among patients with type 2 diabetes in northern China
X. Shao, H. Liu, F. Hou, Y. Bai, Z. Cui, Y. Lin, X. Jiang, P. Bai, Y. Wang, Y. Zhang, C. Lu, H. Liu, S. Zhou, P. Yu
Journal of Endocrinological Investigation.2022; 46(2): 271. CrossRef - Neck circumference for predicting the occurrence of future cardiovascular events: A 7.6-year longitudinal study
Tingting Hu, Yun Shen, Weijie Cao, Yiting Xu, Yufei Wang, Xiaojing Ma, Yuqian Bao
Nutrition, Metabolism and Cardiovascular Diseases.2022; 32(12): 2830. CrossRef - A prospective study of waist circumference trajectories and incident cardiovascular disease in China: the Kailuan Cohort Study
Liang Wang, Yujin Lee, Yuntao Wu, Xinyuan Zhang, Cheng Jin, Zhe Huang, Yixin Wang, Zhiyi Wang, Penny Kris-Etherton, Shouling Wu, Xiang Gao
The American Journal of Clinical Nutrition.2021; 113(2): 338. CrossRef - The Repeatedly Elevated Fatty Liver Index Is Associated With Increased Mortality: A Population-Based Cohort Study
Chang-Hoon Lee, Kyung-Do Han, Da Hye Kim, Min-Sun Kwak
Frontiers in Endocrinology.2021;[Epub] CrossRef - Obesity Degree and Glycemic Status: Factors That Should Be Considered in Heart Failure
Hye Soon Kim
Diabetes & Metabolism Journal.2020; 44(4): 529. CrossRef - Exposure-weighted scoring for metabolic syndrome and the risk of myocardial infarction and stroke: a nationwide population-based study
Eun Young Lee, Kyungdo Han, Da Hye Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Cardiovascular Diabetology.2020;[Epub] CrossRef - Predicting the Development of Myocardial Infarction in Middle-Aged Adults with Type 2 Diabetes: A Risk Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2020; 35(3): 636. CrossRef - Obesity Fact Sheet in Korea, 2018: Data Focusing on Waist Circumference and Obesity-Related Comorbidities
Ga Eun Nam, Yang-Hyun Kim, Kyungdo Han, Jin-Hyung Jung, Yong Gyu Park, Kwan-Woo Lee, Eun-Jung Rhee, Jang Won Son, Seong-Su Lee, Hyuk-Sang Kwon, Won-Young Lee, Soon Jib Yoo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 236. CrossRef - Simply the Best: Anthropometric Indices for Predicting Cardiovascular Disease
Jie-Eun Lee
Diabetes & Metabolism Journal.2019; 43(2): 156. CrossRef - Association and Interaction Analysis of Lipid Accumulation Product with Impaired Fasting Glucose Risk: A Cross-Sectional Survey
Jian Song, Xue Chen, Yuhong Jiang, Jing Mi, Yuyuan Zhang, Yingying Zhao, Xuesen Wu, Huaiquan Gao
Journal of Diabetes Research.2019; 2019: 1. CrossRef - Letter: Association of Z-Score of the Log-Transformed A Body Shape Index with Cardiovascular Disease in People Who Are Obese but Metabolically Healthy: The Korea National Health and Nutrition Examination Survey 2007-2010 (J Obes Metab Syndr 2018;27:158-65
Eun-Jung Rhee
Journal of Obesity & Metabolic Syndrome.2019; 28(2): 139. CrossRef - Response: The Differential Association between Muscle Strength and Diabetes Mellitus According to the Presence or Absence of Obesity (J Obes Metab Syndr 2019;28:46-52)
Bo Kyung Koo
Journal of Obesity & Metabolic Syndrome.2019; 28(4): 297. CrossRef
- Usefulness of New Criteria for Metabolic Syndrome Optimized for Prediction of Cardiovascular Diseases in Japanese

 KDA
KDA
 First
First Prev
Prev





