
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Complications
- Glycemic Control and Retinal Microvascular Changes in Type 2 Diabetes Mellitus Patients without Clinical Retinopathy
- Kangmin Lee, Ga Hye Lee, Seung Eun Lee, Jee Myung Yang, Kunho Bae
- Received May 15, 2023 Accepted December 15, 2023 Published online March 13, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0149 [Epub ahead of print]
- 720 View
- 38 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
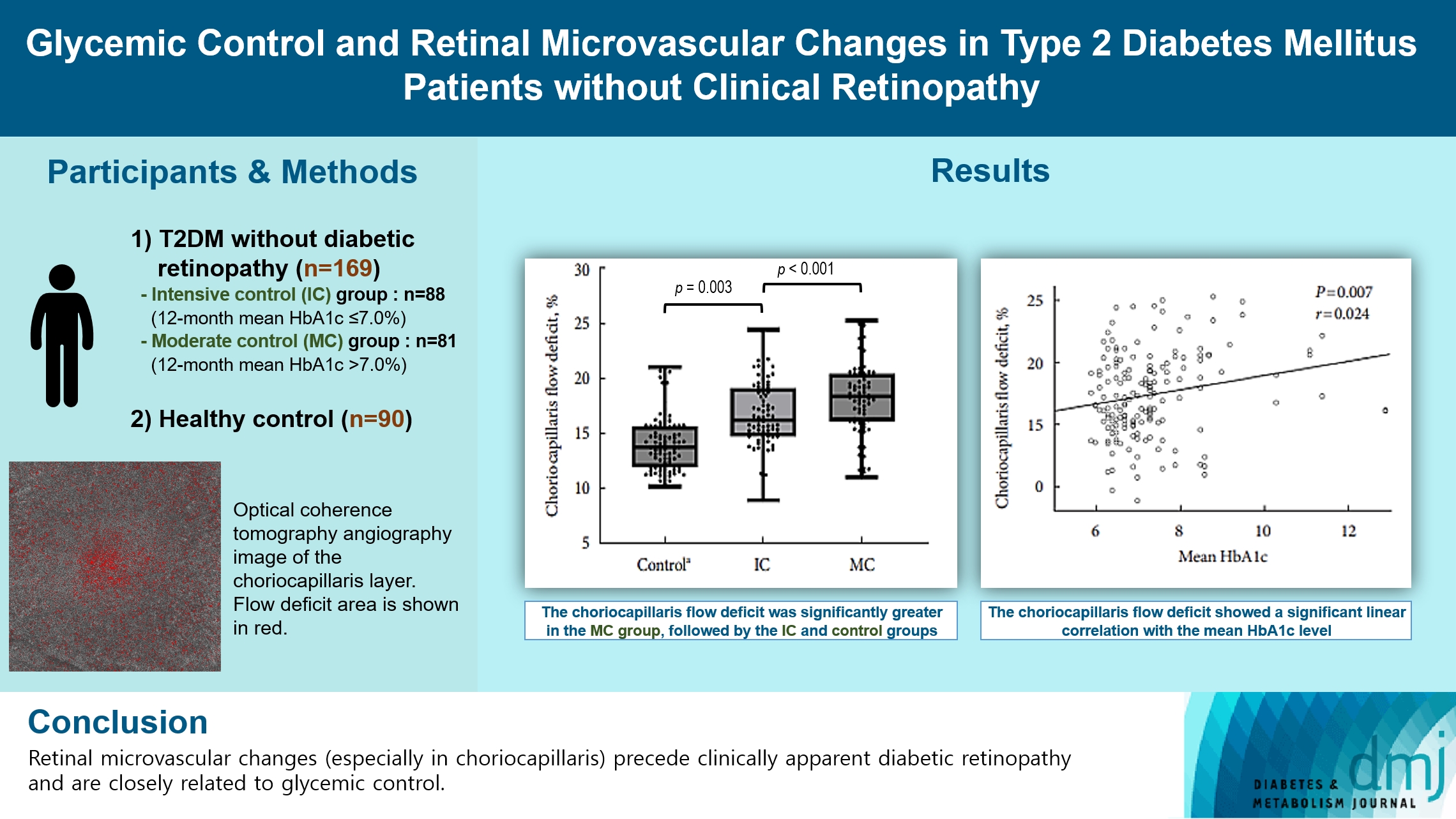
To investigate the association of glycemic control and retinal microvascular changes in patients with type 2 diabetes mellitus (T2DM) without diabetic retinopathy (DR).
Methods
This retrospective, observational, cohort study included patients with T2DM without DR. The patients were categorized into intensive control (IC; mean glycosylated hemoglobin [HbA1c] ≤7.0%) and moderate control (MC; mean HbA1c >7.0%) groups. Optical coherence tomography (OCT) and swept-source OCT angiography (OCTA) image parameters were compared between three groups, including healthy controls.
Results
In total, 259 eyes of 259 participants (88 IC, 81 MC, and 90 controls) were included. The foveal avascular zone area was significantly larger in the MC group than IC and control groups (all P<0.05). The IC group had lower vessel density in the superficial retinal layer and deep retinal layer than the controls (all P<0.05). The choriocapillaris (CC) flow deficit (FD) was significantly greater in the MC group than in the IC and control groups (18.2%, 16.7%, and 14.2%, respectively; all P<0.01). In multivariate regression analysis, CC-FD was associated with the mean HbA1c level (P=0.008). There were no significant differences in OCT parameters among the groups.
Conclusion
OCTA revealed that early CC impairment is associated with HbA1c levels; the CC changes precede clinically apparent DR. The OCTA parameters differed among the groups according to the degree of glycemic control. Our results suggest that microvascular changes precede DR and are closely related to glycemic control.
- Intravitreal Ranibizumab for Subfoveal Choroidal Neovascularization from Age-Related Macular Degeneration with Combined Severe Diabetic Retinopathy
- So Young Han, Jeong Hun Bae, Jaeryung Oh, Hyeong Gon Yu, Su Jeong Song
- Diabetes Metab J. 2015;39(1):46-50. Published online February 16, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.1.46
- 3,118 View
- 34 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background To evaluate the efficacy of intravitreal ranibizumab for subfoveal choroidal neovascularization (CNV) from age-related macular degeneration (AMD) with combined severe diabetic retinopathy (DR).
Methods This retrospective, interventional case series included eleven patients (mean age, 70.09 years; range, 54 to 83 years) with at least severe non-proliferative DR and subfoveal CNV secondary to AMD. Each subject was treated with intravitreal injections of 0.5 mg ranibizumab. The primary outcomes included change in best-corrected visual acuity and central subfield thickness (CST) on optical coherence tomography (OCT).
Results The mean follow-up time was 16.7±14 months (range, 6 to 31 months). Mean visual acuity improved from 1.21±0.80 logarithm of the minimum angle of resolution (logMAR) to 1.0±0.6 logMAR (
P =0.107), 0.95±0.62 logMAR (P =0.044), 1.10±0.68 logMAR (P =0.296), and 1.13±0.66 logMAR (P =0.838) at 1, 3, 6, and 12 months after injection, respectively. Eight patients (72.7%) gained or maintained vision (mean 0.32 logMAR), whereas three patients (27.3%) lost more than one line of vision (mean 0.51 logMAR). The mean OCT CST was 343.9±134.6 µm at baseline, and the mean CST at 1, 3, 6, 12 months after the injection was 367.8±172.1 (P =0.864), 346.2±246.2 (P =0.857), 342±194.1 (P =0.551), and 294.2±108.3 µm (P =0.621), respectively.Conclusion Intravitreal ranibizumab injection can be considered to be a therapy for the stabilization of subfoveal CNV secondary to AMD with combined severe DR. However, these patients might exhibit limited visual improvement after treatment.
-
Citations
Citations to this article as recorded by- Comparative study of widefield swept-source optical coherence tomography angiography in eyes with concomitant age-related macular degeneration and diabetic retinopathy
Matthew Finn, Grace Baldwin, Itika Garg, Hannah E Wescott, Thomas Koch, Filippos Vingopoulos, Rebecca Zeng, Hanna Choi, Diane Sayah, Deeba Husain, Nimesh A Patel, Leo A Kim, Joan W Miller, David M Wu, Demetrios G Vavvas, John B Miller
British Journal of Ophthalmology.2023; : bjo-2023-323792. CrossRef - Outcomes of intravitreal anti-VEGF therapy in eyes with both neovascular age-related macular degeneration and diabetic retinopathy
Francesco Bandello, Federico Corvi, Carlo La Spina, Lucia Benatti, Lea Querques, Vittorio Capuano, Jonathan Naysan, Xuejing Chen, David Sarraf, Maurizio Battaglia Parodi, Eric Souied, K Bailey Freund, Giuseppe Querques
British Journal of Ophthalmology.2016; 100(12): 1611. CrossRef
- Comparative study of widefield swept-source optical coherence tomography angiography in eyes with concomitant age-related macular degeneration and diabetic retinopathy

 KDA
KDA
 First
First Prev
Prev





