
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Metabolic Risk/Epidemiology
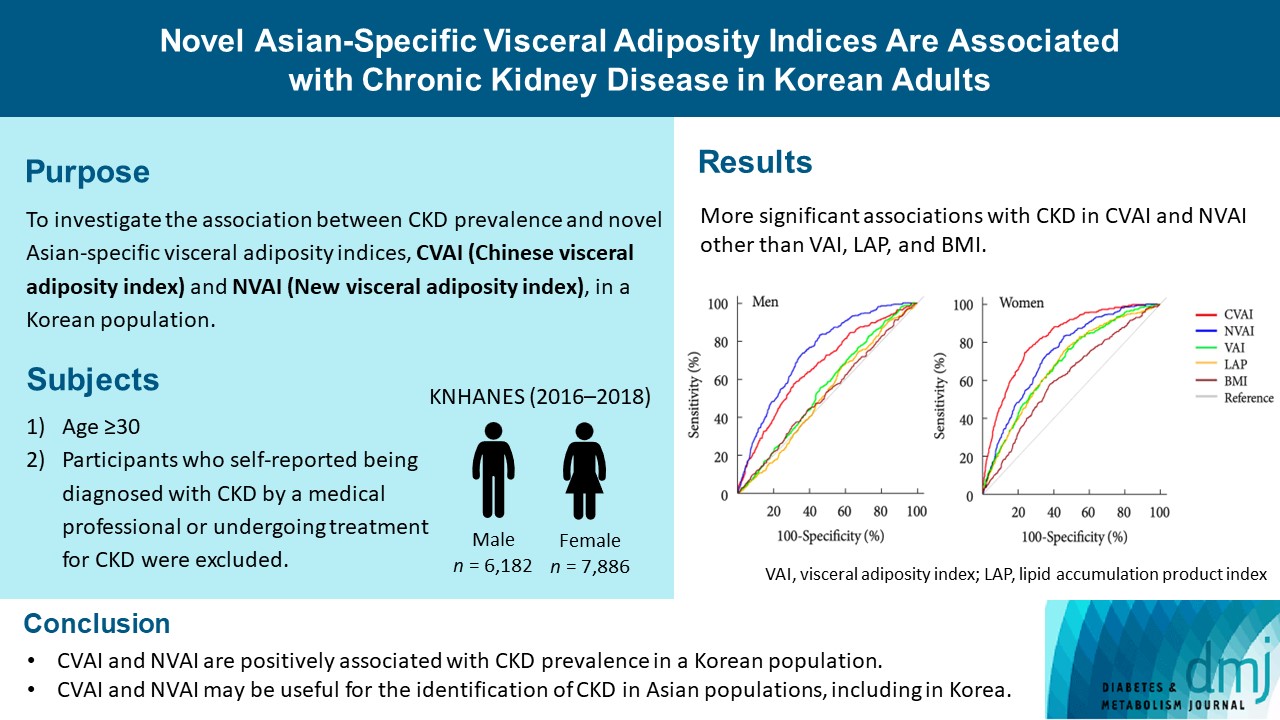
- Novel Asian-Specific Visceral Adiposity Indices Are Associated with Chronic Kidney Disease in Korean Adults
- Jonghwa Jin, Hyein Woo, Youngeun Jang, Won-Ki Lee, Jung-Guk Kim, In-Kyu Lee, Keun-Gyu Park, Yeon-Kyung Choi
- Diabetes Metab J. 2023;47(3):426-436. Published online March 6, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0099
- 2,517 View
- 128 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The Chinese visceral adiposity index (CVAI) and new visceral adiposity index (NVAI) are novel indices of visceral adiposity used to predict metabolic and cardiovascular diseases in Asian populations. However, the relationships of CVAI and NVAI with chronic kidney disease (CKD) have not been investigated. We aimed to characterize the relationships of CVAI and NVAI with the prevalence of CKD in Korean adults.
Methods
A total of 14,068 participants in the 7th Korea National Health and Nutrition Examination Survey (6,182 men and 7,886 women) were included. Receiver operating characteristic (ROC) analyses were employed to compare the associations between indices of adiposity and CKD, and a logistic regression model was used to characterize the relationships of CVAI and NVAI with CKD prevalence.
Results
The areas under the ROC curves for CVAI and NVAI were significantly larger than for the other indices, including the visceral adiposity index and lipid accumulation product, in both men and women (all P<0.001). In addition, high CVAI or NVAI was significantly associated with a high CKD prevalence in both men (odds ratio [OR], 2.14; 95% confidence interval [CI], 1.31 to 3.48 in CVAI and OR, 6.47; 95% CI, 2.91 to 14.38 in NVAI, P<0.05) and women (OR, 4.87; 95% CI, 1.85 to 12.79 in CVAI and OR, 3.03; 95% CI, 1.35 to 6.82 in NVAI, P<0.05); this association remained significant after adjustment for multiple confounding factors in men and women.
Conclusion
CVAI and NVAI are positively associated with CKD prevalence in a Korean population. CVAI and NVAI may be useful for the identification of CKD in Asian populations, including in Korea. -
Citations
Citations to this article as recorded by- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
Zenglei Zhang, Lin Zhao, Yiting Lu, Xu Meng, Xianliang Zhou
Journal of Translational Medicine.2023;[Epub] CrossRef
- Association between Chinese visceral adiposity index and risk of stroke incidence in middle-aged and elderly Chinese population: evidence from a large national cohort study
- Cardiovascular Risk/Epidemiology
- Clinical Significance of Body Fat Distribution in Coronary Artery Calcification Progression in Korean Population
- Heesun Lee, Hyo Eun Park, Ji Won Yoon, Su-Yeon Choi
- Diabetes Metab J. 2021;45(2):219-230. Published online October 28, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0161
- Correction in: Diabetes Metab J 2021;45(6):974

- 6,520 View
- 257 Download
- 8 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 
- Background
Although obesity differs according to ethnicity, it is globally established as a solid risk factor for cardiovascular disease. However, it is not fully understood how obesity parameters affect the progression of coronary artery calcification (CAC) in Korean population. We sought to evaluate the association of obesity-related parameters including visceral adipose tissue (VAT) measurement and CAC progression.
Methods
This retrospective observational cohort study investigated 1,015 asymptomatic Korean subjects who underwent serial CAC scoring by computed tomography (CT) with at least 1-year interval and adipose tissue measurement using non-contrast CT at baseline for a routine checkup between 2003 and 2015. CAC progression, the main outcome, was defined as a difference of ≥2.5 between the square roots of the baseline and follow-up CAC scores using Agatston units.
Results
During follow-up (median 39 months), 37.5% of subjects showed CAC progression of a total population (56.4 years, 80.6% male). Body mass index (BMI) ≥25 kg/m2, increasing waist circumferences (WC), and higher VAT/subcutaneous adipose tissue (SAT) area ratio were independently associated with CAC progression. Particularly, predominance of VAT over SAT at ≥30% showed the strongest prediction for CAC progression (adjusted hazard ratio, 2.20; P<0.001) and remained of prognostic value regardless of BMI or WC status. Further, it provided improved risk stratification of CAC progression beyond known prognosticators.
Conclusion
Predominant VAT area on CT is the strongest predictor of CAC progression regardless of BMI or WC in apparently healthy Korean population. Assessment of body fat distribution may be helpful to identify subjects at higher risk. -
Citations
Citations to this article as recorded by- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
Xiaoliu Shi, Wanyue Wang, Jiafan Feng, Xiaochun Ma, Mengting Xu, Cui Wang
Environmental Pollution.2024; 349: 123959. CrossRef - The association between C-reactive protein and coronary artery calcification: a systematic review and meta-analysis
Amirhossein Tajani, Masoumeh Sadeghi, Navid Omidkhoda, Amir Hooshang Mohammadpour, Sara Samadi, Vahid Jomehzadeh
BMC Cardiovascular Disorders.2024;[Epub] CrossRef - Visceral adipose tissue is an independent predictor and mediator of the progression of coronary calcification: a prospective sub-analysis of the GEA study
Neftali Eduardo Antonio-Villa, Juan Gabriel Juárez-Rojas, Rosalinda Posadas-Sánchez, Juan Reyes-Barrera, Aida Medina-Urrutia
Cardiovascular Diabetology.2023;[Epub] CrossRef - Deep learning-based prediction for significant coronary artery stenosis on coronary computed tomography angiography in asymptomatic populations
Heesun Lee, Bong Gyun Kang, Jeonghee Jo, Hyo Eun Park, Sungroh Yoon, Su-Yeon Choi, Min Joo Kim
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Relationship between a novel non–insulin-based metabolic score for insulin resistance (METS‐IR) and coronary artery calcification
Zhenwei Wang, Xiaofang Hui, Xu Huang, Jingjie Li, Naifeng Liu
BMC Endocrine Disorders.2022;[Epub] CrossRef - Association Between Abdominal Adipose Tissue Distribution and Risk of Endometrial Cancer: A Case-Control Study
Yuan Cheng, Zhongyu Wang, Xiaoxuan Jia, Rong Zhou, Jianliu Wang
Clinical Medicine Insights: Oncology.2022; 16: 117955492211407. CrossRef - Sex differences in cardiovascular risk may be related to sex differences in diet patterns: a narrative review
A. M. Tindall, V. A. Stallings
Annals of Human Biology.2021; 48(6): 517. CrossRef
- Gender-specific abdominal fat distribution and insulin resistance associated with organophosphate esters and phthalate metabolites exposure
- Lifestyle
- Body Fat Is Related to Sedentary Behavior and Light Physical Activity but Not to Moderate-Vigorous Physical Activity in Type 2 Diabetes Mellitus
- Keun Hee An, Kyung Ah Han, Tae Seo Sohn, Ie Byung Park, Hae Jin Kim, Sung Dae Moon, Kyung Wan Min
- Diabetes Metab J. 2020;44(2):316-325. Published online November 12, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0029
- 5,502 View
- 138 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Sedentary behavior (SB) has emerged as a new risk factor for cardiovascular accidents. We investigated whether physical activity levels or SB were related to percent body fat (%BF) in type 2 diabetes mellitus (T2DM).
Methods In this cross sectional study, we measured the duration of SB, light physical activity (LPA), moderate to vigorous physical activity (MVPA), total energy expenditure, and step counts using a wireless activity tracker (Fitbit HR; FB) for 7 days in free-living conditions, along with %BF using a bio impedance analyzer (Inbody; Biospace) in 120 smartphone users with T2DM. Subjects were divided into exercise (Exe,
n =68) and non-exercise (nonExe,n =52) groups based on self-reports of whether the recommended exercises (30 min/day, 3 days/week for 3 months) were performed. SBt, LPAt, MVPAt were transformed from SB, LPA, MVPA for normally distributed variables.Results Participants were: female, 59.2%; age, 59.3±8.4 years; body mass index, 25.5±3.4 kg/m2; glycosylated hemoglobin (HbA1c), 7.6%±1.2%; %BF, 30.4%±7.1%. They performed SB for 15.7±3.7 hr/day, LPA for 4.4±1.7 hr/day, and MVPA for 0.9±0.8 hr/day. The %BF was related to SBt and LPAt, but not to MVPA after adjustments for age, gender, and HbA1c. VPA was significantly higher in the Exe group than in the nonExe group, but SB, LPA, and moderate physical activity were not different. Predicted %BF was 89.494 to 0.105 (age), −13.047 (gender), −0.507 (HbA1c), −7.655 (LPAt) (F[4, 64]=62.929,
P <0.001), with anR 2 of 0.785 in multiple linear regression analysis.Conclusion Reduced body fat in elderly diabetic patients might be associated with reduced inactivity and increased LPA.
-
Citations
Citations to this article as recorded by- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
Lotte Bogaert, Iris Willems, Patrick Calders, Eveline Dirinck, Manon Kinaupenne, Marga Decraene, Bruno Lapauw, Boyd Strumane, Margot Van Daele, Vera Verbestel, Marieke De Craemer
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2024; 18(4): 102995. CrossRef - Association between depression, anemia and physical activity using isotemporal substitution analysis
Hee-kyoung Nam, Jungmi Park, Sung-il Cho
BMC Public Health.2023;[Epub] CrossRef - The Impact of Wearable Technologies in Health Research: Scoping Review
Sophie Huhn, Miriam Axt, Hanns-Christian Gunga, Martina Anna Maggioni, Stephen Munga, David Obor, Ali Sié, Valentin Boudo, Aditi Bunker, Rainer Sauerborn, Till Bärnighausen, Sandra Barteit
JMIR mHealth and uHealth.2022; 10(1): e34384. CrossRef - The Correlation of Prediabetes and Type 2 Diabetes With Adiposity in Adults
Juan Sun, Zhen Liu, Zimu Zhang, Ziyang Zeng, Weiming Kang
Frontiers in Nutrition.2022;[Epub] CrossRef - The Physical Activity Assessment of Adults With Type 2 Diabetes Using Accelerometer-Based Cut Points: Scoping Review
Ioana A Moldovan, Alexa Bragg, Anna S Nidhiry, Barbara A De La Cruz, Suzanne E Mitchell
Interactive Journal of Medical Research.2022; 11(2): e34433. CrossRef - Effects of 4 Weeks of a Technique-Specific Protocol with High-Intensity Intervals on General and Specific Physical Fitness in Taekwondo Athletes: An Inter-Individual Analysis
Alex Ojeda-Aravena, Tomás Herrera-Valenzuela, Pablo Valdés-Badilla, Jorge Cancino-López, José Zapata-Bastias, José Manuel García-García
International Journal of Environmental Research and Public Health.2021; 18(7): 3643. CrossRef - Inter-Individual Variability of a High-Intensity Interval Training With Specific Techniques vs. Repeated Sprints Program in Sport-Related Fitness of Taekwondo Athletes
Alex Ojeda-Aravena, Tomás Herrera-Valenzuela, Pablo Valdés-Badilla, Jorge Cancino-López, José Zapata-Bastias, José Manuel García-García
Frontiers in Physiology.2021;[Epub] CrossRef - EFFECT OF SPORTS MEDICINE ON REDUCING BODY FAT PERCENTAGE AND LEAN BODY MASS
Chunyan Fan
Revista Brasileira de Medicina do Esporte.2021; 27(7): 714. CrossRef - Validation of the effectiveness of a digital integrated healthcare platform utilizing an AI-based dietary management solution and a real-time continuous glucose monitoring system for diabetes management: a randomized controlled trial
Sung Woon Park, Gyuri Kim, You-Cheol Hwang, Woo Je Lee, Hyunjin Park, Jae Hyeon Kim
BMC Medical Informatics and Decision Making.2020;[Epub] CrossRef - Brain activity during a working memory task in different postures: an EEG study
Ju-Yeon Jung, Hwi-Young Cho, Chang-Ki Kang
Ergonomics.2020; 63(11): 1359. CrossRef
- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
- Epidemiology
- Lower Leg Fat Depots Are Associated with Albuminuria Independently of Obesity, Insulin Resistance, and Metabolic Syndrome (Korea National Health and Nutrition Examination Surveys 2008 to 2011)
- Eugene Han, Nan Hee Cho, Mi Kyung Kim, Hye Soon Kim
- Diabetes Metab J. 2019;43(4):461-473. Published online March 7, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0081
- 5,011 View
- 39 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Although the involvement of obesity in metabolic disorders is well known, leg fat depot influences on albuminuria have not been determined.
Methods This population-based, cross-sectional study used a nationally representative sample of 2,076 subjects aged ≥20 years from the Korea National Health and Nutrition Examination Surveys of 2008 to 2011. The ratio of leg fat to total fat (LF/TF ratio) was assessed by dual X-ray absorptiometry, and albuminuria was defined as more than one positive dipstick test or an albumin-to-creatinine ratio of ≥30 mg/g.
Results Individuals whose LF/TF ratio was in the lowest tertile showed a higher proportion of albuminuria than those in the highest tertile (odds ratio [OR], 2.82; 95% confidence interval [CI], 2.01 to 3.96;
P <0.001). This association was observed in both sexes, all age groups, and all subgroups stratified by body mass index, waist circumference, homeostasis model assessments of insulin resistance, and the presence of metabolic syndrome (all,P <0.05). Multiple logistic regression analyses also demonstrated that the lowest LF/TF ratio was independently associated with albuminuria risk (OR, 1.55 to 2.16; all,P <0.05). In addition, the risk of albuminuria was higher in sarcopenic individuals with lower LF/TF ratios than in the highest LF/TF ratio subjects without sarcopenia (OR, 3.73; 95% CI, 2.26 to 6.13).Conclusion A lower LF/TF ratio was associated with an increased risk of albuminuria independent of obesity, insulin resistance, and metabolic syndrome, and when combined with sarcopenia, the albuminuria risk synergistically increased. Hence, our findings may have implications to improve risk stratification and recommendations on body fat distribution in the general population.
-
Citations
Citations to this article as recorded by- Efficacy and safety of evogliptin in patients with type 2 diabetes and non‐alcoholic fatty liver disease: A multicentre, double‐blind, randomized, comparative trial
Eugene Han, Ji Hye Huh, Eun Y. Lee, Ji C. Bae, Sung W. Chun, Sung H. Yu, Soo H. Kwak, Kyong S. Park, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2022; 24(4): 752. CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef
- Efficacy and safety of evogliptin in patients with type 2 diabetes and non‐alcoholic fatty liver disease: A multicentre, double‐blind, randomized, comparative trial
- Obesity and Metabolic Syndrome
- Relationship between Regional Body Fat Distribution and Diabetes Mellitus: 2008 to 2010 Korean National Health and Nutrition Examination Surveys
- Soo In Choi, Dawn Chung, Jung Soo Lim, Mi Young Lee, Jang Yel Shin, Choon Hee Chung, Ji Hye Huh
- Diabetes Metab J. 2017;41(1):51-59. Published online December 21, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.1.51
- 4,187 View
- 42 Download
- 35 Web of Science
- 36 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The aim of this study was to investigate the association between regional body fat distribution, especially leg fat mass, and the prevalence of diabetes mellitus (DM) in adult populations.
Methods A total of 3,181 men and 3,827 postmenopausal women aged 50 years or older were analyzed based on Korea National Health and Nutrition Examination Surveys (2008 to 2010). Body compositions including muscle mass and regional fat mass were measured using dual-energy X-ray absorptiometry.
Results The odds ratios (ORs) for DM was higher with increasing truncal fat mass and arm fat mass, while it was lower with increasing leg fat mass. In a partial correlation analysis adjusted for age, leg fat mass was negatively associated with glycosylated hemoglobin in both sexes and fasting glucose in women. Leg fat mass was positively correlated with appendicular skeletal muscle mass and homeostasis model assessment of β cell. In addition, after adjusting for confounding factors, the OR for DM decreased gradually with increasing leg fat mass quartiles in both genders. When we subdivided the participants into four groups based on the median values of leg fat mass and leg muscle mass, higher leg fat mass significantly lowered the risk of DM even though they have smaller leg muscle mass in both genders (
P <0.001).Conclusion The relationship between fat mass and the prevalence of DM is different according to regional body fat distribution. Higher leg fat mass was associated with a lower risk of DM in Korean populations. Maintaining leg fat mass may be important in preventing impaired glucose tolerance.
-
Citations
Citations to this article as recorded by- Effects of chromium supplementation on body composition in patients with type 2 diabetes: A dose-response systematic review and meta-analysis of randomized controlled trials
Mahdi Vajdi, Mahsa khajeh, Ehsan Safaei, Seyedehelham Moeinolsadat, Samin Mousavi, Hooria Seyedhosseini-Ghaheh, Mahdieh Abbasalizad-Farhangi, Gholamreza Askari
Journal of Trace Elements in Medicine and Biology.2024; 81: 127338. CrossRef - Connections between body composition and dysregulation of islet α- and β-cells in type 2 diabetes
Jia-xi Miao, Jia-ping Xu, Rui Wang, Yu-xian Xu, Feng Xu, Chun-hua Wang, Chao Yu, Dong-mei Zhang, Jian-bin Su
Diabetology & Metabolic Syndrome.2024;[Epub] CrossRef - Anthropometric and DXA-derived measures of body composition in relation to pre-diabetes among adults
Anwar Mohammad, Ali H. Ziyab, Talal Mohammad
BMJ Open Diabetes Research & Care.2023; 11(5): e003412. CrossRef - A cohort study on the predictive capability of body composition for diabetes mellitus using machine learning
Mohammad Ali Nematollahi, Amir Askarinejad, Arefeh Asadollahi, Mehdi Bazrafshan, Shirin Sarejloo, Mana Moghadami, Sarvin Sasannia, Mojtaba Farjam, Reza Homayounfar, Babak Pezeshki, Mitra Amini, Mohamad Roshanzamir, Roohallah Alizadehsani, Hanieh Bazrafsha
Journal of Diabetes & Metabolic Disorders.2023;[Epub] CrossRef - Which is the best diet to reduce cardiometabolic risk: dietary counseling or home-delivered diet?
Feray Çağiran Yilmaz, Aysun Atilgan, Günay Saka
Food & Nutrition Research.2023;[Epub] CrossRef - Sedentary lifestyle and body composition in type 2 diabetes
Dan-dan Li, Yang Yang, Zi-yi Gao, Li-hua Zhao, Xue Yang, Feng Xu, Chao Yu, Xiu-lin Zhang, Xue-qin Wang, Li-hua Wang, Jian-bin Su
Diabetology & Metabolic Syndrome.2022;[Epub] CrossRef - Impaired Lung Function and Lung Cancer Incidence: A Nationwide Population-Based Cohort Study
Hye Seon Kang, Yong-Moon Park, Seung-Hyun Ko, Seung Hoon Kim, Shin Young Kim, Chi Hong Kim, Kyungdo Han, Sung Kyoung Kim
Journal of Clinical Medicine.2022; 11(4): 1077. CrossRef - Association between lung function and the risk of atrial fibrillation in a nationwide population cohort study
Su Nam Lee, Seung-Hyun Ko, Sung-Ho Her, Kyungdo Han, Donggyu Moon, Sung Kyoung Kim, Ki-Dong Yoo, Yu-Bae Ahn
Scientific Reports.2022;[Epub] CrossRef - Is imaging-based muscle quantity associated with risk of diabetes? A meta-analysis of cohort studies
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Tongzhi Wu
Diabetes Research and Clinical Practice.2022; 189: 109939. CrossRef - Research Progress of Body Composition Changes in Type 2 Diabetes Patients
鹏霞 张
Advances in Clinical Medicine.2022; 12(08): 7181. CrossRef - Associations of eating speed with fat distribution and body shape vary in different age groups and obesity status
Saili Ni, Menghan Jia, Xuemiao Wang, Yun Hong, Xueyin Zhao, Liang Zhang, Yuan Ru, Fei Yang, Shankuan Zhu
Nutrition & Metabolism.2022;[Epub] CrossRef - Body composition, trabecular bone score and vertebral fractures in subjects with Klinefelter syndrome
W. Vena, F. Carrone, A. Delbarba, O. Akpojiyovbi, L. C. Pezzaioli, P. Facondo, C. Cappelli, L. Leonardi, L. Balzarini, D. Farina, A. Pizzocaro, A. G. Lania, G. Mazziotti, A. Ferlin
Journal of Endocrinological Investigation.2022; 46(2): 297. CrossRef - Genetically predicted body fat mass and distribution with diabetic kidney disease: A two-sample Mendelian randomization study
Min Wang, Xin Li, Hang Mei, Zhao-Hui Huang, Yue Liu, Yong-Hong Zhu, Tian-Kui Ma, Qiu-Ling Fan
Frontiers in Genetics.2022;[Epub] CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Age- and Sex-Related Differential Associations between Body Composition and Diabetes Mellitus
Eun Roh, Soon Young Hwang, Jung A Kim, You-Bin Lee, So-hyeon Hong, Nam Hoon Kim, Ji A Seo, Sin Gon Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo
Diabetes & Metabolism Journal.2021; 45(2): 183. CrossRef - Neck circumference and metabolic syndrome: A cross-sectional population-based study
Hooman Ebrahimi, Payam Mahmoudi, Farhad Zamani, Sedighe Moradi
Primary Care Diabetes.2021; 15(3): 582. CrossRef - Development of a clinical risk score for incident diabetes: A 10‐year prospective cohort study
Tae Jung Oh, Jae Hoon Moon, Sung Hee Choi, Young Min Cho, Kyong Soo Park, Nam H Cho, Hak Chul Jang
Journal of Diabetes Investigation.2021; 12(4): 610. CrossRef - The association of glucocorticoid receptor polymorphism with metabolic outcomes in menopausal women with adrenal incidentalomas
Sanja Ognjanović, Jadranka Antić, Tatjana Pekmezović, Bojana Popović, Tatjana Isailović, Ivana Božić Antić, Tamara Bogavac, Valentina Elezović Kovačević, Dušan Ilić, Milica Opalić, Djuro Macut
Maturitas.2021; 151: 15. CrossRef - Distinct opposing associations of upper and lower body fat depots with metabolic and cardiovascular disease risk markers
Mahasampath Gowri S, Belavendra Antonisamy, Finney S. Geethanjali, Nihal Thomas, Felix Jebasingh, Thomas V. Paul, Fredrik Karpe, Clive Osmond, Caroline H. D. Fall, Senthil K. Vasan
International Journal of Obesity.2021; 45(11): 2490. CrossRef - Body Roundness Index Is a Superior Obesity Index in Predicting Diabetes Risk Among Hypertensive Patients: A Prospective Cohort Study in China
Yingshan Liu, Xiaocong Liu, Haixia Guan, Shuting Zhang, Qibo Zhu, Xiaoying Fu, Hongmei Chen, Songtao Tang, Yingqing Feng, Jian Kuang
Frontiers in Cardiovascular Medicine.2021;[Epub] CrossRef - Subcutaneous adipose tissue distribution and serum lipid/lipoprotein in unmedicated postmenopausal women: A B-mode ultrasound study
Imaging.2021; 13(2): 119. CrossRef - The Leg Fat to Total Fat Ratio Is Associated with Lower Risks of Non-Alcoholic Fatty Liver Disease and Less Severe Hepatic Fibrosis: Results from Nationwide Surveys (KNHANES 2008–2011)
Hyun Min Kim, Yong-ho Lee
Endocrinology and Metabolism.2021; 36(6): 1232. CrossRef Optimal Cut-Offs of Body Mass Index and Waist Circumference to Identify Obesity in Chinese Type 2 Diabetic Patients
Qinying Zhao, Xiangjun Chen, Jinshan Wu, Lilin Gong, Jinbo Hu, Shumin Yang, Qifu Li, Zhihong Wang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1899. CrossRef- Weight Loss after 12 Weeks of Exercise and/or Nutritional Guidance Is Not Obligatory for Induced Changes in Local Fat/Lean Mass Indexes in Adults with Excess of Adiposity
Robinson Ramírez-Vélez, Mikel Izquierdo, Karem Castro-Astudillo, Carolina Medrano-Mena, Angela Liliana Monroy-Díaz, Rocío del Pilar Castellanos-Vega, Héctor Reynaldo Triana-Reina, María Correa-Rodríguez
Nutrients.2020; 12(8): 2231. CrossRef - VISCERAL FAT, PHYSICAL FITNESS AND BIOCHEMICAL MARKERS OF BRAZILIAN MILITARY PERSONNEL
Laércio Camilo Rodrigues, Marcos de Sá Rego Fortes, Marco Antônio Muniz Lippert, Samir Ezequiel Da Rosa, José Fernandes Filho
Revista Brasileira de Medicina do Esporte.2020; 26(1): 21. CrossRef - Comparison of 7-site skinfold measurement and dual-energy X-ray absorptiometry for estimating body fat percentage and regional adiposity in Taiwanese diabetic patients
Feng-Chih Kuo, Chieh-Hua Lu, Li-Wei Wu, Tung-Wei Kao, Sheng-Chiang Su, Jhih-Syuan Liu, Kuan-Chan Chen, Chia-Hao Chang, Chih-Chun Kuo, Chien-Hsing Lee, Chang-Hsun Hsieh, Mauro Lombardo
PLOS ONE.2020; 15(7): e0236323. CrossRef - Outcomes specific to patient sex after open ventral hernia repair
Kathryn A. Schlosser, Sean R. Maloney, Otto Thielan, Tanushree Prasad, Kent Kercher, Paul D. Colavita, B Todd Heniford, Vedra A. Augenstein
Surgery.2020; 167(3): 614. CrossRef Age-Related Changes in Body Composition and Bone Mineral Density and Their Relationship with the Duration of Diabetes and Glycaemic Control in Type 2 Diabetes
Ying Tang, Lilin Gong, Xiangjun Chen, Zhipeng Du, Jinbo Hu, Zhixin Xu, Jinshan Wu, Qifu Li, Zhihong Wang
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 4699. CrossRef- Lipodystrophy: A paradigm for understanding the consequences of "overloading" adipose tissue
Koini Lim, Afreen Haider, Claire Adams, Alison Sleigh, David Savage
Physiological Reviews.2020;[Epub] CrossRef - Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals
Chang Ho Ahn, Jae Hyun Bae, Young Min Cho
Diabetes & Metabolism Journal.2019; 43(6): 879. CrossRef - Differences in dietary intakes, body compositions, and biochemical indices between metabolically healthy and metabolically abnormal obese Korean women
Eun Yeong Kang, Jung-Eun Yim
Nutrition Research and Practice.2019; 13(6): 488. CrossRef - The Association between Body Composition using Dual energy X-ray Absorptiometry and Type-2 Diabetes: A Systematic Review and Meta-Analysis of Observational studies
Preeti Gupta, Carla Lanca, Alfred T. L. Gan, Pauline Soh, Sahil Thakur, Yijin Tao, Neelam Kumari, Ryan E. K. Man, Eva K. Fenwick, Ecosse L. Lamoureux
Scientific Reports.2019;[Epub] CrossRef - Genes that make you fat, but keep you healthy
R. J. F. Loos, T. O. Kilpeläinen
Journal of Internal Medicine.2018; 284(5): 450. CrossRef - Overview of Epidemiology and Contribution of Obesity and Body Fat Distribution to Cardiovascular Disease: An Update
Marie-Eve Piché, Paul Poirier, Isabelle Lemieux, Jean-Pierre Després
Progress in Cardiovascular Diseases.2018; 61(2): 103. CrossRef - Relevance of human fat distribution on lipid and lipoprotein metabolism and cardiovascular disease risk
Marie-Eve Piché, Senthil K. Vasan, Leanne Hodson, Fredrik Karpe
Current Opinion in Lipidology.2018; 29(4): 285. CrossRef - Comparison of regional fat measurements by dual-energy X-ray absorptiometry and conventional anthropometry and their association with markers of diabetes and cardiovascular disease risk
S K Vasan, C Osmond, D Canoy, C Christodoulides, M J Neville, C Di Gravio, C H D Fall, F Karpe
International Journal of Obesity.2018; 42(4): 850. CrossRef
- Effects of chromium supplementation on body composition in patients with type 2 diabetes: A dose-response systematic review and meta-analysis of randomized controlled trials
- Effects of Rosiglitazone on Body Fat Mass and Distribution in Type 2 Diabetic Patients.
- Hong Kyu Kim, Hyo Joong Yoon, Seung Min You, Ki Young Lee, Hye Young Park, Moon Ho Kang
- Korean Diabetes J. 2003;27(3):272-279. Published online June 1, 2003
- 1,104 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Rosiglitazone, an insulin-sensitizing drug of the thiazolidinediones class, has a high affinity for the ligands of the peroxisome proliferator activated receptor-gamma(PPAR-gamma), is highly expressed in adipose tissue, and plays an important role in the differentiation of adipocyte. The influence of rosiglitazone was investigated on the total fat mass and regional adiposity in type 2 diabetic patients. METHODS: Rosiglitazone (4 mg/day) was administered for 6 months to type 2 diabetic patients (n=20) whose glycemic control was unacceptable with the use of other treatments. Measurements of the total, trunk and leg region body fats (by dual energy X-ray absorptiometry) and abdominal fat distributions (by computed tomography) were compared before and after treatment. RESULTS: Nine patients received rosiglitazone monotherapy and 11 a combined therapy of sulfonylurea and/or metformin. The HbA1C, serum insulin level and homeostasis model assessment insulin resistance index were decreased following the rosiglitazone therapy, but the body weight and BMI were increased. As for the body fat changes, the total (19,382+/-4,786 vs. 22,940+/- 7,300 g, p<0.01), trunk (11,399+/- 2,678 vs. 13,960+/-4,698 g, p<0.01) and leg (4,734+/-1,319 vs. 6,203+/-2,231g, p<0.05) region fat masses were significantly increased. The percentage increase in the total, trunk and leg region fat masses were 20+/-25, 25+/-35 and 58+/-130%, respectively. As for abdominal fat distribution after the treatment, the visceral fat area (225+/-84 vs. 187+/-87 cm2, p<0.05) was significantly decreased, while the subcutaneous fat area tended to increase (178+/-83 vs. 201+/-80 cm2, NS), although these were not statistically significant. The visceral/subcutaneous fat ratio (V/S ratio) was significantly decreased (1.45+/- 0.64 vs. 0.95+/-0.25, p<0.05). CONCLUSION: Although the total body fat mass was increased following the rosiglitazone therapy, a shift in the body fat distribution, from the visceral to the subcutaneous region, was observed, which may be associated with an improvement in insulin resistance. However, a long-term assessment of the consequences of an increasing total fat mass and change in the body fat distribution will be required.
- Dehydroepiandrosterone-Sulfate, Sex Hormone Binding Globulin, Body Fat Distribution Pattern and Insulin Resistance in Women.
- Young Sun Hong, Jee Young Oh, Yeon Ah Sung, Nan Ho Kyung, Yeon Jin Jang
- Korean Diabetes J. 1998;22(3):328-337. Published online January 1, 2001
- 1,094 View
- 16 Download
-
 Abstract
Abstract
 PDF
PDF - BACKGROUND
Sex hormone-binding globulin (SHBG) has been known to be associated with obesity, central fat accumulation and insulin resistance and thought to be a indirect marker for androgenicity in women. The relationships between circulating dehydroepiandrosterone(DHEA). dehydroepiandrosterone sulfate(DHEA-S) levels and body fat accumulation are still controversial. We conducted a cross-sectional study to eva]uate the relationships between serum levels of SHBG, DHEA-S, body fat distribution pattern and insulin sensitivity in women. METHODS: We tested 57 women(age 30~65yr; BMI 18.5~32.8kg/m, 45 premenopausal on the 5~10 day of the menstrual cycle, 12 postmenopausal who were not using hormone replacement therapy) with varying degree of glucose tolerance(32 normal glucose tolerance(NGT), 17 impaired glucose tolerance(IGT) and 8 newly diagnosed diabetes). lnsulin sensitivity was measured as minimal model derived sensitivity index(S) using insulin modified IV glucose tolerance test and fasting serum levels of SHBG and DHEA-S were measured by RIA. Body fat distribution pattern was assessed by waist to hip ratio(WHR),% body fat measured by bioelectrical impedance analyzer, subcutaneous fat area(SFA), visceral fat area(VFA) and VFA to SFA ratio(VSR) at the level of umbilicus using the computed tomography. RESULTS: 1) Measured SHBG and DHEA-S levels were not significantly different among subjects with NGT, IGT and diabetes. 2) SHBG was inversely associated with age, BMI, WHR, diastolic blood pressure, VFA, SFA, VSR,% body fat, fasting insulin and positively associated with S, whereas DHEA-S did not show any significant correlation with above variables except diastolic blood pressure. 3) SHBG level was significantly lower(p<0.05) and DHEA-S level was insignificantly lower (p=0.05) in postmenopausal women than in premenopausal women but the significance disappeared after adjustment for age, BMI, WHR and% body fat. 4) BMI was independently and negatively related to S, WHR and fasting insulin to SHBG by multiple regression analysis. CONCLUSION: We confirmed that SHBG was independently associated with central obesity and fasting hyperinsulinemia. However, S was independently associated with BMI only. It suggested that hyperinsulinemia in insulin resistance might cause the decreased level of SHBG even thaugh the directionality of the association was uncertain because of a cross-sectional nature of this study.

 KDA
KDA
 First
First Prev
Prev





