- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 38(3); 2014 > Article
-
Original ArticleClinical Care/Education Efficacy of the Smartphone-Based Glucose Management Application Stratified by User Satisfaction
- Hun-Sung Kim1,2, Wona Choi2, Eun Kyoung Baek2, Yun A Kim2, So Jung Yang2, In Young Choi3, Kun-Ho Yoon1,2, Jae-Hyoung Cho1,2
-
Diabetes & Metabolism Journal 2014;38(3):204-210.
DOI: https://doi.org/10.4093/dmj.2014.38.3.204
Published online: June 17, 2014
1Division of Endocrinology and Metabolism, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
2Institute of Catholic Ubiquitous Health Care, The Catholic University of Korea, Seoul, Korea.
3Department of Medical Informatics, The Catholic University of Korea College of Medicine, Seoul, Korea.
- Corresponding author: Jae-Hyoung Cho. Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, 222 Banpo-daero, Seocho-gu, Seoul 137-701, Korea. drhopper@catholic.ac.kr
Copyright © 2014 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- We aimed to assess the efficacy of the smartphone-based health application for glucose control and patient satisfaction with the mobile network system used for glucose self-monitoring.
-
Methods
- Thirty-five patients were provided with a smartphone device, and self-measured blood glucose data were automatically transferred to the medical staff through the smartphone application over the course of 12 weeks. The smartphone user group was divided into two subgroups (more satisfied group vs. less satisfied group) based on the results of questionnaire surveys regarding satisfaction, comfort, convenience, and functionality, as well as their willingness to use the smartphone application in the future. The control group was set up via a review of electronic medical records by group matching in terms of age, sex, doctor in charge, and glycated hemoglobin (HbA1c).
-
Results
- Both the smartphone group and the control group showed a tendency towards a decrease in the HbA1c level after 3 months (7.7%±0.7% to 7.5%±0.7%, P=0.077). In the more satisfied group (n=27), the HbA1c level decreased from 7.7%±0.8% to 7.3%±0.6% (P=0.001), whereas in the less satisfied group (n=8), the HbA1c result increased from 7.7%±0.4% to 8.1%±0.5% (P=0.062), showing values much worse than that of the no-smartphone control group (from 7.7%±0.5% to 7.7%±0.7%, P=0.093).
-
Conclusion
- In addition to medical feedback, device and network-related patient satisfaction play a crucial role in blood glucose management. Therefore, for the smartphone app-based blood glucose monitoring to be effective, it is essential to provide the patient with a well-functioning high quality tool capable of increasing patient satisfaction and willingness to use.
- Recently, public healthcare expenditures have been increasing exponentially due to a plethora of chronic diseases such as diabetes and the aging of the population [1,2,3]. Despite the continuing development of pharmaceuticals and therapeutic measures, this tendency appears to be increasing with time. Thus, we are at point where a new type of chronic disease management system should be established. It is against this backdrop that the Ubiquitous-Healthcare (U-Healthcare) has come into existence. The recently commercialized U-Healthcare makes health management possible without temporal and geographical limits by facilitating doctor-patient communication over the internet or via cellular phones [4,5]. This technology is mainly available for patients with chronic diseases, particularly for diabetes mellitus [6,7,8,9,10,11,12,13,14].
- A cellular phone is a suitable device that can be programmed for glucose monitoring without a hospital visit. In addition, it can also be used for receiving diabetes-related educational content. The majority of the previous cellular phone-based research for diabetes management used short message service (SMS) or telephone counseling. This process mainly involves telecommunication with active participation of the medical staff including medical feedback that is based on the blood glucose levels recorded by the patients. Numerous studies have already shown the multiple advantages of telecommunication for patient management and blood-glucose monitoring [15,16,17,18,19,20].
- The requirements for information technology-based blood glucose monitoring are the following: a device for sensing health data, a network for communication, and medical feedback to patients. With the popularization of smart phones, many health applications have been released for these devices. However, most of the applications for chronic disease management have solely focused on self-management without interactive feedback. In contrast, clinical trials thus far have solely focused on medical feedback, thereby largely neglecting aspects pertaining to the convenience of the device or network. Consequently, in this study, we aimed to assess the effectiveness of smartphone applications for blood glucose monitoring and interactive communication between patients and the medical team.
INTRODUCTION
- Study population and design
- This study targeted outpatients with type 2 diabetes mellitus who visited Seoul St. Mary's Hospital from October to November 2012. For the intervention group, the inclusion criteria were men or women aged 20 to 70 years who had type 2 diabetes mellitus for more than 1 year. The baseline glycated hemoglobin (HbA1c) had to be between 7.0% and 10.0%. Patients who had serious concomitant internal diseases, such as heart failure, liver diseases, and kidney disease with a creatinine level >1.5 mg/dL or serious diabetes complications were excluded. Patients who were dependent on an insulin pump, already enrolled in other clinical trials, or otherwise considered unsuitable by the researchers were also excluded from the study.
- Forty-two patients expressed their interest in participating in the study, and 38 signed the informed consent form approved by the Investigation Review Board of Seoul St. Mary Hospital. Three patients refused for reasons such as change in cell phone number. Thus, 35 patients were selected to participate in the intervention group.
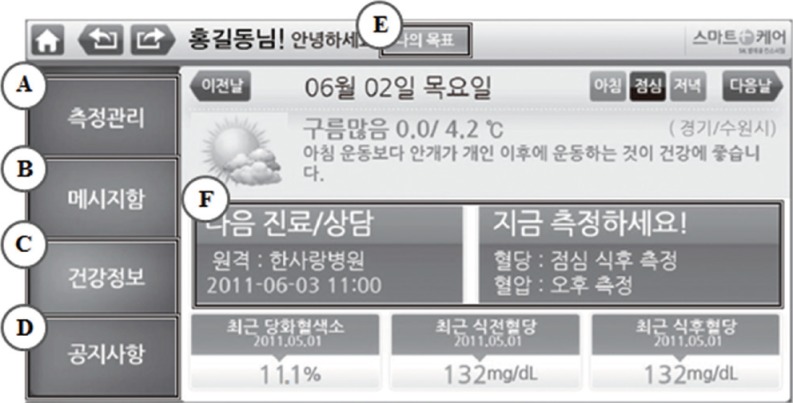
- At the first and the final visit, height, body-weight, waist and hip circumference, and blood pressure were measured. Blood samples were also collected for HbA1c measurement and lipid profile assessment (total cholesterol [TC], triglyceride [TG], low density lipoprotein cholesterol [LDL-C], and high density lipoprotein cholesterol [HDL-C]). The collected data were transferred to the Galaxy S-II Smartphone (Samsung Electronics, Suwon, Korea), CareSens-LINK blood glucose monitor (i-SENS, Wonju, Korea), and S(M)BPM-1 blood pressure monitor (Samsung Electronics) at the first visit. The blood glucose and blood pressure were self-measured by the patients and the recorded data were automatically transferred to the medical staff through the smartphone application (henceforth app) 'Mobile Smartcare, version 1.0.7' (Samsung Electronics). The smartphone users checked their blood glucose level and recorded the data in the smartphone application. The data were then automatically transferred to the hospital. The medical staff analyzed the data and sent recommendations and feedback tailored to the patient an average of once per week (Fig. 1). If the blood glucose level remained high, a warning message and recommendations for exercise and diet were sent to the user. If the user had hypoglycemia (<60 mg/dL) or did not record any blood glucose measurements, the medical team called the user to change the insulin dose or recommend an early visit to the hospital.
- After 3 months, at the second outpatient visit, the same laboratory tests and anthropometric tests were conducted to evaluate the effects of blood glucose monitoring and interactive communication. A questionnaire survey on the smartphone app was also performed at the follow-up visit. The questionnaire made by the Catholic medical team consisted of items pertaining to satisfaction, comfort, convenience, and functionality, as well as the willingness to use the app in the future and recommend to other patients.
- The control group in this study was set up via electronic medical records (EMRs) review. The criteria for the control group were patients who visited the hospital with the same diagnosed disease during the same period as the intervention group. Patients matched to the intervention group in terms of age, sex, doctor in charge, and HbA1c were screened and randomly selected through EMR review. All patients were provided with the written informed consents to participate, and the study was approved by the Ethics Committee and the Review Board of Korea Institution for Social and Health Affairs.
- Statistical analysis
- The baseline characteristics of the two groups were compared using an unpaired t-test for continuous variables and the Mantel-Haenszel chi-square test for categorical variables. To improve the normality, we performed log-transformation for variables with a skewed distribution. We also conducted an analysis of the within-group mean change from baseline to the end of the trial using a paired t-test. Nonparametric tests were performed for subgroup analysis based on compliance. The signed-rank test was used to assess the differences in the variables between baselines and follow-up in the high and low compliance groups and the Kruskal-Wallis test was used to test differences among the three groups (high and low compliance groups, and control). Data were analyzed using a standard package (SAS version 9.1; SAS Institute, Cary, NC, USA).
METHODS
- Of the 38 patients who participated in the study, three patients dropped out due to personal reasons, and 35 patients continued until the end of the 12 week study period.
- Baseline characteristics
- The baseline characteristics are shown in Table 1. The mean age in the intervention group was 51.8±10.3 years, while in the control group the mean age was 53.8±9.0 years. The mean body mass index (BMI) in the intervention group was 25.0±3.3 kg/m2, and the mean duration of diabetes was 11.8±7.3 years. There were no significant differences between the two groups with respect to sex, BMI, glucose control methods and laboratory data, including HbA1c and cholesterol levels.
- Effect on blood glucose level
- In the smartphone group, the mean HbA1c decreased after 3 months from the baseline level of 7.7%±0.7% to 7.5%±0.7% (P=0.077). In the control group there was no change from baseline (7.7%±0.5% to 7.7%±0.7%) over the same period thus showing no intergroup difference after 3 months. Both the smartphone group and control group had no difference in the baseline TC, TG, HDL-C, and LDL-C levels after 3 months thus showing no significant intergroup differences (Table 2).
- Analysis of the questionnaire survey
- Of the 35 users, two patients expressed unchanged or increased satisfaction and expectations when compared to the pre-use survey. The remaining eight patients expressed less satisfaction accompanied with complaints. Thirty-six complaints were received during the study period. The majority of these complaints were due to data transfer errors (15/36 cases, 41.7%). Other causes of complaints were mismatch between measured data and uploaded data (6/36 cases, 16.7%), network errors (5/36 cases, 13.9%), and difficulties in using the device (3/36 cases, 8.3%), which led to a decrease in satisfaction (Table 3).
- Subgroup analysis by compliance
- The smartphone user group was divided into two subgroups based on the results of the on the surveys conducted at baseline and after 3 months. The more satisfied group consisted of 27 patients, and the less satisfied group consisted of eight patients. There were no significant difference in age, sex, diabetes mellitus duration, blood pressure, or BMI between the more satisfied group and less satisfied group.
- The change in HbA1c level from baseline to the 3-month follow-up was significantly different once satisfaction was taken into consideration (P for interaction=0.0004). The HbA1c in the more satisfied group decreased significantly from 7.7%±0.8% to 7.3%±0.6% (P<0.001), whereas in the less satisfied group, the HbA1c remained essentially the same (7.7%±0.4% to 8.1%±0.5%, P=0.062) and was actually worse than the control group. TC, TG, HDL-C, and LDL-C levels were not significantly different from the baseline levels (Table 4).
RESULTS
- Of the three major prerequisites for IT-based health management systems, device utility (Sensors), network (Transfer), and medical feedback, existing studies have exclusively focused on medical feedback. The blood glucose monitoring system mostly revolves around active involvement of the medical staff, i.e., medical feedback. A previous study involving the use of SMS for 12 weeks demonstrated a decrease in HbA1c level by 1.01% [15], and another study on type 1 diabetes showed that the application of a cellular phone-based blood glucose monitoring system resulted in a 0.5% decrease of HbA1c levels [16]. Likewise, a number of other similar studies have shown successful reduction in the HbA1c levels [17,18,19]. These study results provide evidence regarding the feasibility of cellular phones as an important tool for blood glucose monitoring. However, it is not easy to commercialize a medical feedback-enabled smartphone, as it involves human-resource (HR) costs for the medical team that provides the medical feedback. This is directly associated with the rise of healthcare costs, thereby limiting commercialization because of low cost-effectiveness. In other words, commercialization must be preceded by economic feasibility. Several ongoing studies focus on economic analyses to investigate the possibilities of reducing medical feedback-related HR costs [19,20]. Cho et al. [20] reported a satisfactory result of a 50% reduction in medical staff by means of a simple algorithm. Methods such as a clinical decision support system and artificial intelligence that can achieve high effectiveness with low HR should be explored [20,21].
- As mentioned above, the studies conducted thus far have not focused on sensor (device utility) and network transfer, which are the mediators for blood glucose monitoring. Meanwhile, this study has shown that, in addition to medical feedback, patient satisfaction with the device or network is important for blood-glucose management.
- In our study, the HbA1c in the more satisfied group significantly decreased from 7.7%±0.8% to 7.3%±0.6% (P<0.001). There were no significant changes in TC, TG, HDL-C, and LDL-C. Because the study was performed over 3 months, it is unlikely that a significant change in lipid values would occur. Dissatisfaction with the use of the smartphone-based blood glucose monitoring system led to an increase in the HbA1c from 7.7%±0.4% to 8.1%±0.5% (P=0.062). The results of this study show the high positive effect on the blood glucose level in the more satisfied group after the use of smartphone compared to the less satisfied group. A notable point, however, is the negative impact on blood glucose level in the less satisfied group when compared to the no-smartphone control group. This appears to be associated with the users' dissatisfaction when an app is difficult to apply or when encountering frequent device breakdowns that affect compliance. This is immediately related to poorly controlled blood glucose. It is obvious that, in addition to medical feedback, device, and network-related patient satisfaction play a crucial role in blood glucose management. Therefore, for the smartphone app-based blood glucose monitoring to be effective, it is essential to provide the patient with a well-functioning high quality tool capable of increasing patient satisfaction and willingness to use the device. A smartphone is an upgraded type of device and network compared to the traditional cellular phone. It is simple, convenient, comfortable to carry, and appropriate for communication with the medical team. A patient who voluntarily downloads the diabetes-related app may be considered to have an interest in their blood glucose management. Nevertheless, if frequent breakdowns and other shortcomings decrease their satisfaction, then they are likely to fail in their blood glucose management. In other words, the results may be worse than if the smartphone app was not used.
- Consequently, to increase user satisfaction and involve medical feedback, it is necessary to implement the steps from mobile application development to medical team involvement [22,23]. It is crucial to develop a tool that clearly reflects medical requirements and improvements. Additionally, secondary aspects, such as convenience, low cost, simple- and fun-to-use functions, and orderly design, should be considered to attract active user participation. Further, it is important to continuously upgrade the application based on user feedback. Moreover, the role of medical staff is important for the successful implementation of the fast-developing sensor and transfer app in the medical sector. It is the role of a medical team to select adequate devices, apply them, and earnestly analyze their effectiveness and economic feasibility.
- This study has a few limitations. 1) First, this was not a randomized clinical trial. Nevertheless, the control group was randomly assigned by targeting patients who visited the hospital during the same period. 2) Our result is difficult to generalize because this was a small population and a short-term pilot study. 3) Therefore, additional future studies should be conducted with a larger population and longer duration. Although several blood glucose monitoring applications are available, this study used only one application; therefore, the strengths and weakness of other applications were not assessed. Given the varying functions unique to each application, the study results are likely to differ depending on the app used.
- Despite these limitations, there are a few notable achievements of this study. First, a practical analysis was performed on a program attempting to combine the rapidly developing IT technology with medical needs. Second, the goal of this study was focused on the efficacy of a health management system depending on user satisfaction, which will contribute to further development of a user-friendly system. This study revealed that device utility and network can indirectly influence blood glucose management. This study may be an example of the progress in developing apps for chronic disease management in general, not only for diabetes.
- The rapid development in health technology will continue, and such techniques will obviously be used more intensely in medicine. A large-scale trial investigating the possibility, efficacy, and economic feasibility is necessary to enable the effective grafting of IT to medical needs. Additionally, future efforts will have to focus on constructing a system that is capable of helping patients practically.
DISCUSSION
-
Acknowledgements
- This research was supported by the Technology Innovation Program (No. 10035059, primary care centered Smart Care Service Pilot Project) funded by the Ministry of Trade, Industry & Energy (MOTIE, Korea). The systems and devices used in this research have been provided by the SK Telecom Consortium's Smartcare Service Project. The opinions expressed in this paper are those of the authors and do not necessarily represent those of the SK Telecom Consortium's Smart Care Service Pilot Project. We thank Sun-Young Lim for collecting and inputting all of the data and analysis and Jin-Hee Lee for coordinating the study. The final version of this manuscript was approved by all authors.
ACKNOWLEDGMENTS
- 1. Ong KL, Cheung BM, Wong LY, Wat NM, Tan KC, Lam KS. Prevalence, treatment, and control of diagnosed diabetes in the U.S. National Health and Nutrition Examination Survey 1999-2004. Ann Epidemiol 2008;18:222-229. ArticlePubMed
- 2. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006;368:1681-1688. ArticlePubMed
- 3. Chan JC, Malik V, Jia W, Kadowaki T, Yajnik CS, Yoon KH, Hu FB. Diabetes in Asia: epidemiology, risk factors, and pathophysiology. JAMA 2009;301:2129-2140. ArticlePubMed
- 4. Skrøvseth SO, Arsand E, Godtliebsen F, Joakimsen RM. Model driven mobile care for patients with type 1 diabetes. Stud Health Technol Inform 2012;180:1045-1049. PubMed
- 5. Lund S, Hemed M, Nielsen BB, Said A, Said K, Makungu MH, Rasch V. Mobile phones as a health communication tool to improve skilled attendance at delivery in Zanzibar: a cluster-randomised controlled trial. BJOG 2012;119:1256-1264. ArticlePubMed
- 6. Castaldini M, Saltmarch M, Luck S, Sucher K. The development and pilot testing of a multimedia CD-ROM for diabetes education. Diabetes Educ 1998;24:285-286. 91-92. 95-96. ArticlePubMedPDF
- 7. Frost D, Beischer W. Telemedicine in the management of pregnancy in type 1 diabetic women. Diabetes Care 2000;23:863-864. ArticlePubMedPDF
- 8. Levetan CS, Dawn KR, Robbins DC, Ratner RE. Impact of computer-generated personalized goals on HbA(1c). Diabetes Care 2002;25:2-8. ArticlePubMedPDF
- 9. McKay HG, King D, Eakin EG, Seeley JR, Glasgow RE. The diabetes network internet-based physical activity intervention: a randomized pilot study. Diabetes Care 2001;24:1328-1334. PubMed
- 10. Meigs JB, Cagliero E, Dubey A, Murphy-Sheehy P, Gildesgame C, Chueh H, Barry MJ, Singer DE, Nathan DM. A controlled trial of web-based diabetes disease management: the MGH diabetes primary care improvement project. Diabetes Care 2003;26:750-757. PubMed
- 11. Meneghini LF, Albisser AM, Goldberg RB, Mintz DH. An electronic case manager for diabetes control. Diabetes Care 1998;21:591-596. ArticlePubMedPDF
- 12. Smith SA, Murphy ME, Huschka TR, Dinneen SF, Gorman CA, Zimmerman BR, Rizza RA, Naessens JM. Impact of a diabetes electronic management system on the care of patients seen in a subspecialty diabetes clinic. Diabetes Care 1998;21:972-976. ArticlePubMedPDF
- 13. Tomky DM. Developing a computerized diabetes self-management education module for documenting outcomes. Diabetes Educ 1999;25:197-210. ArticlePubMedPDF
- 14. Yoon KH, Kim HS. A short message service by cellular phone in type 2 diabetic patients for 12 months. Diabetes Res Clin Pract 2008;79:256-261. ArticlePubMed
- 15. Zolfaghari M, Mousavifar SA, Pedram S, Haghani H. The impact of nurse short message services and telephone follow-ups on diabetic adherence: which one is more effective? J Clin Nurs 2012;21:1922-1931. PubMed
- 16. Carroll AE, DiMeglio LA, Stein S, Marrero DG. Contracting and monitoring relationships for adolescents with type 1 diabetes: a pilot study. Diabetes Technol Ther 2011;13:543-549. ArticlePubMedPMC
- 17. Kim SI, Kim HS. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Inform 2008;77:399-404. ArticlePubMed
- 18. Istepanian RS, Zitouni K, Harry D, Moutosammy N, Sungoor A, Tang B, Earle KA. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. J Telemed Telecare 2009;15:125-128. ArticlePubMedPDF
- 19. Shearer A, Scuffham P, Gordois A, Oglesby A. Predicted costs and outcomes from reduced vibration detection in people with diabetes in the U.S. Diabetes Care 2003;26:2305-2310. ArticlePubMedPDF
- 20. Cho JH, Choi YH, Kim HS, Lee JH, Yoon KH. Effectiveness and safety of a glucose data-filtering system with automatic response software to reduce the physician workload in managing type 2 diabetes. J Telemed Telecare 2011;17:257-262. ArticlePubMedPDF
- 21. Ali MK, Shah S, Tandon N. Review of electronic decision-support tools for diabetes care: a viable option for low- and middle-income countries? J Diabetes Sci Technol 2011;5:553-570. ArticlePubMedPMCPDF
- 22. Kim HS, Shin JA, Chang JS, Cho JH, Son HY, Yoon KH. Continuous glucose monitoring: current clinical use. Diabetes Metab Res Rev 2012;28(Suppl 2):73-78. ArticlePubMed
- 23. Ko SH, Park SA, Cho JH, Ko SH, Shin KM, Lee SH, Song KH, Park YM, Ahn YB. Influence of the duration of diabetes on the outcome of a diabetes self-management education program. Diabetes Metab J 2012;36:222-229. ArticlePubMedPMC
REFERENCES


Values are presented as mean±standard deviation or number (%).
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HbA1c, glycated hemoglobin; HMG-CoA, 3-hydroxy-3-methylglutaryl-CoA; TC, total cholesterol; TG, triglyceride; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol.
aBased on Mantel-Haenszel chi-square test.

Values are presented as mean±standard deviation. Interaction between group and time about all variables were not significant.
BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HbA1c, glycated hemoglobin; TC, total cholesterol; TG, triglyceride; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol.

Values are presented as mean±standard deviation or number (%).
DM, diabetes mellitus; BMI, body mass index; SBP, systolic blood pressure; DBP, diastolic blood pressure; HbA1c, glycated hemoglobin; TC, total cholesterol; TG, triglyceride; HDL-C, high density lipoprotein cholesterol; LDL-C, low density lipoprotein cholesterol.
aStatistical significance was noticed (P<0.05) for the more satisfied group vs. the less satisfied group at 3 months later.
Figure & Data
References
Citations

- Diverse perspectives on remote collaborative care for chronic disease management
Seo Yeon Baik, Hakyoung Park, Jiwon Shinn, Hun-Sung Kim
Cardiovascular Prevention and Pharmacotherapy.2024; 6(1): 26. CrossRef - Time Efficiency, Reliability, and User Satisfaction of the Tooth Memo App for Recording Oral Health Information: Cross-Sectional Questionnaire Study
Palinee Detsomboonrat, Pagaporn Pantuwadee Pisarnturakit
JMIR Formative Research.2024; 8: e56143. CrossRef - The effect of m-health applications on self-care improvement in older adults: A systematic review
Sharareh Rostam Niakan Kalhori, Meysam Rahmani Katigari, Tahere Talebi Azadboni, Shahrbanoo Pahlevanynejad, Rahil Hosseini Eshpala
Informatics for Health and Social Care.2023; 48(3): 292. CrossRef - Acculturation and Disparities in Telemedicine Readiness: A National Study
Jorge M. Rodríguez-Fernández, Nicolas Hoertel, Hugo Saner, Mukaila Raji
The International Journal of Aging and Human Development.2023;[Epub] CrossRef - The effect of education and mobile health management on improvement of blood glucose with type 2 diabetes mellitus
Sanbao Chai, Danyang Wang, Baoting Yao, Lin Xu, Linong Ji, Xiaomei Zhang
Journal of Public Health.2022; 30(1): 205. CrossRef - Effect of an Integrative Mobile Health Intervention in Patients With Hypertension and Diabetes: Crossover Study
Sang Woo Oh, Kyoung-Kon Kim, Sung Soo Kim, Su Kyung Park, Sangshin Park
JMIR mHealth and uHealth.2022; 10(1): e27192. CrossRef - Evaluation of a Smart After-Care Program for Patients with Lung Cancer: A Prospective, Single-Arm Pilot Study
Hee Chul Yang, Seung Hyun Chung, Ji Sung Yoo, Boram Park, Moon Soo Kim, Jong Mog Lee
Journal of Chest Surgery.2022; 55(2): 108. CrossRef - Effectiveness of Disease-Specific mHealth Apps in Patients With Diabetes Mellitus: Scoping Review
Claudia Eberle, Maxine Löhnert, Stefanie Stichling
JMIR mHealth and uHealth.2021; 9(2): e23477. CrossRef - Mobile Healthcare System Provided by Primary Care Physicians Improves Quality of Diabetes Care
Tae Jung Oh, Jie-Eun Lee, Seok Kim, Sooyoung Yoo, Hak Chul Jang
CardioMetabolic Syndrome Journal.2021; 1(1): 88. CrossRef - Online monitoring system for emergency diabetes mellitus patients
R Kurniawati, S Suryono, S Ismail
IOP Conference Series: Materials Science and Engineering.2021; 1108(1): 012018. CrossRef - Towards Telemedicine Adoption in Korea: 10 Practical Recommendations for Physicians
Hun-Sung Kim
Journal of Korean Medical Science.2021;[Epub] CrossRef - Analysis of Effectiveness and Psychological Techniques Implemented in mHealth Solutions for Middle-Aged and Elderly Adults with Type 2 Diabetes: A Narrative Review of the Literature
Julia Vázquez-de Sebastián, Andreea Ciudin, Carmina Castellano-Tejedor
Journal of Clinical Medicine.2021; 10(12): 2701. CrossRef - Lack of Acceptance of Digital Healthcare in the Medical Market: Addressing Old Problems Raised by Various Clinical Professionals and Developing Possible Solutions
Jong Il Park, Hwa Young Lee, Hyunah Kim, Jisan Lee, Jiwon Shinn, Hun-Sung Kim
Journal of Korean Medical Science.2021;[Epub] CrossRef - Efficacy of Interventions That Incorporate Mobile Apps in Facilitating Weight Loss and Health Behavior Change in the Asian Population: Systematic Review and Meta-analysis
Siew Min Ang, Juliana Chen, Jia Huan Liew, Jolyn Johal, Yock Young Dan, Margaret Allman-Farinelli, Su Lin Lim
Journal of Medical Internet Research.2021; 23(11): e28185. CrossRef - Apprehensions about Excessive Belief in Digital Therapeutics: Points of Concern Excluding Merits
Hun-Sung Kim
Journal of Korean Medical Science.2020;[Epub] CrossRef - Effect of a Mobile Phone–Based Glucose-Monitoring and Feedback System for Type 2 Diabetes Management in Multiple Primary Care Clinic Settings: Cluster Randomized Controlled Trial
Yeoree Yang, Eun Young Lee, Hun-Sung Kim, Seung-Hwan Lee, Kun-Ho Yoon, Jae-Hyoung Cho
JMIR mHealth and uHealth.2020; 8(2): e16266. CrossRef - The development of My Care Hub Mobile-Phone App to Support Self-Management in Australians with Type 1 or Type 2 Diabetes
Mary D. Adu, Usman H. Malabu, Aduli E. O. Malau-Aduli, Bunmi S. Malau-Aduli
Scientific Reports.2020;[Epub] CrossRef - Using the RE-AIM framework to evaluate internal and external validity of mobile phone–based interventions in diabetes self-management education and support
Yilin Yoshida, Sonal J Patil, Ross C Brownson, Suzanne A Boren, Min Kim, Rosie Dobson, Kayo Waki, Deborah A Greenwood, Astrid Torbjørnsen, Ambady Ramachandran, Christopher Masi, Vivian A Fonseca, Eduardo J Simoes
Journal of the American Medical Informatics Association.2020; 27(6): 946. CrossRef - Development and Operation of a Video Teleconsultation System Using Integrated Medical Equipment Gateway: a National Project for Workers in Underserved Areas
Hyun Sang Park, Kwang il Kim, Jae Young Soh, Young Ho Hyun, Bang Eun Lee, Jong Hwa Lee, Jung Gwon Jo, Han Chae Lee, Hwa Sun Kim
Journal of Medical Systems.2020;[Epub] CrossRef - Lessons from Use of Continuous Glucose Monitoring Systems in Digital Healthcare
Hun-Sung Kim, Kun-Ho Yoon
Endocrinology and Metabolism.2020; 35(3): 541. CrossRef - Recent Technology-Driven Advancements in Cardiovascular Disease Prevention in Korea
Jisan Lee, Hun-Sung Kim, Dai-Jin Kim
Cardiovascular Prevention and Pharmacotherapy.2019; 1(2): 43. CrossRef - Development and Evaluation: The Satisfaction of Using an Oral Health Survey Mobile Application
Palinee Detsomboonrat, Pagaporn Pantuwadee Pisarnturakit
Telemedicine and e-Health.2019; 25(1): 55. CrossRef - A Mobile Lifestyle Management Program (GlycoLeap) for People With Type 2 Diabetes: Single-Arm Feasibility Study
David Koot, Paul Soo Chye Goh, Robyn Su May Lim, Yubing Tian, Teng Yan Yau, Ngiap Chuan Tan, Eric Andrew Finkelstein
JMIR mHealth and uHealth.2019; 7(5): e12965. CrossRef - Self-management of Chronic Conditions Using mHealth Interventions in Korea: A Systematic Review
Jae Yoon Yi, Yujin Kim, Yoon-Min Cho, Hongsoo Kim
Healthcare Informatics Research.2018; 24(3): 187. CrossRef - Seamless recording of glucometer measurements among older experienced diabetic patients – A study of perception and usability
Peter Rasche, Alexander Mertens, Talya Miron-Shatz, Corinne Berzon, Christopher M. Schlick, Michael Jahn, Stefan Becker, Clemens Fürnsinn
PLOS ONE.2018; 13(5): e0197455. CrossRef - The efficacy of mobile application use on recall of surgical risks in nasal bone fracture reduction surgery
Choong Hyeon Kim, Ji Seon Cheon, Woo Young Choi, Kyung Min Son
Archives of Craniofacial Surgery.2018; 19(1): 41. CrossRef - Enablers and barriers to using two-way information technology in the management of adults with diabetes: A descriptive systematic review
Emma M Macdonald, Byron M Perrin, Michael IC Kingsley
Journal of Telemedicine and Telecare.2018; 24(5): 319. CrossRef - Considerations for the Development of Mobile Phone Apps to Support Diabetes Self-Management: Systematic Review
Mary D Adu, Usman H Malabu, Emily J Callander, Aduli EO Malau-Aduli, Bunmi S Malau-Aduli
JMIR mHealth and uHealth.2018; 6(6): e10115. CrossRef - The Relationship Between Acceptance Intention Toward a Smartphone Healthcare Application and Health-Promoting Behaviors Among Nursing Students
Eun-Jin Choi, Se-Won Kang
CIN: Computers, Informatics, Nursing.2018; 36(10): 494. CrossRef - Dietary Intake and Micronutrient Supplementation in Youth with Celiac Disease with and without Type 1 Diabetes
Amanda Liu, Margaret Marcon, Esther Assor, Farid H. Mahmud, Justine Turner, Diana Mager
Canadian Journal of Dietetic Practice and Research.2018; 79(3): 118. CrossRef - Determinants of mobile technology use and smartphone application interest in cancer patients
Nirupa Jaya Raghunathan, Deborah Korenstein, Qing S. Li, Emily S. Tonorezos, Jun J. Mao
Cancer Medicine.2018; 7(11): 5812. CrossRef - Usability and clinical efficacy of diabetes mobile applications for adults with type 2 diabetes: A systematic review
Helen Fu, Siobhan K. McMahon, Cynthia R. Gross, Terrence J. Adam, Jean F. Wyman
Diabetes Research and Clinical Practice.2017; 131: 70. CrossRef - Expectancy, usage and acceptance by general practitioners and patients: exploratory results from a study in the German outpatient sector
Urs-Vito Albrecht, Kambiz Afshar, Kristin Illiger, Stefan Becker, Tobias Hartz, Bernhard Breil, Daniel Wichelhaus, Ute von Jan
DIGITAL HEALTH.2017; 3: 205520761769513. CrossRef - Satisfaction Survey on Information Technology-Based Glucose Monitoring System Targeting Diabetes Mellitus in Private Local Clinics in Korea
Hun-Sung Kim, So Jung Yang, Yoo Jin Jeong, Young-Eun Kim, Seok-Won Hong, Jae Hyoung Cho
Diabetes & Metabolism Journal.2017; 41(3): 213. CrossRef - Tailored Communication Within Mobile Apps for Diabetes Self-Management: A Systematic Review
Heidi Holmen, Astrid Klopstad Wahl, Milada Cvancarova Småstuen, Lis Ribu
Journal of Medical Internet Research.2017; 19(6): e227. CrossRef - Smart Devices for Older Adults Managing Chronic Disease: A Scoping Review
Ben YB Kim, Joon Lee
JMIR mHealth and uHealth.2017; 5(5): e69. CrossRef - What do we know about mobile applications for diabetes self-management? A review of reviews
Megan Hood, Rebecca Wilson, Joyce Corsica, Lauren Bradley, Diana Chirinos, Amanda Vivo
Journal of Behavioral Medicine.2016; 39(6): 981. CrossRef - Randomized, Open-Label, Parallel Group Study to Evaluate the Effect of Internet-Based Glucose Management System on Subjects with Diabetes in China
Hun-Sung Kim, Chenglin Sun, So Jung Yang, Lin Sun, Fei Li, In Young Choi, Jae-Hyoung Cho, Guixia Wang, Kun-Ho Yoon
Telemedicine and e-Health.2016; 22(8): 666. CrossRef - Characterization of Apps and Other e-Tools for Medication Use: Insights Into Possible Benefits and Risks
Linda Wilhelmina Maria van Kerkhof, Catharina Walthera Egbertha van der Laar, Charlie de Jong, Marjolein Weda, Ingrid Hegger
JMIR mHealth and uHealth.2016; 4(2): e34. CrossRef - Social Networking Services-Based Communicative Care for Patients with Diabetes Mellitus in Korea
Hun-Sung Kim, Yoo Jeong, Sun Baik, So Yang, Tong Kim, Hyunah Kim, Hyunyong Lee, Seung-Hwan Lee, Jae Cho, In-Young Choi, Kun-Ho Yoon
Applied Clinical Informatics.2016; 07(03): 899. CrossRef - Use of Mobile Health Technology in the Prevention and Management of Diabetes Mellitus
Jacob Hartz, Leah Yingling, Tiffany M. Powell-Wiley
Current Cardiology Reports.2016;[Epub] CrossRef - Nurses’ experiences of using a smart mobile device application to assist home care for patients with chronic disease: a qualitative study
Kuei‐Feng Chiang, Hsiu‐Hung Wang
Journal of Clinical Nursing.2016; 25(13-14): 2008. CrossRef - Does nutritional counseling in telemedicine improve treatment outcomes for diabetes? A systematic review and meta-analysis of results from 92 studies
Dejun Su, Chelsea McBride, Junmin Zhou, Megan S Kelley
Journal of Telemedicine and Telecare.2016; 22(6): 333. CrossRef - A Smartphone Application Significantly Improved Diabetes Self-Care Activities with High User Satisfaction
Yu Jin Kim, Sang Youl Rhee, Jong Kyu Byun, So Young Park, Soo Min Hong, Sang Ouk Chin, Suk Chon, Seungjoon Oh, Jeong-taek Woo, Sung Woon Kim, Young Seol Kim
Diabetes & Metabolism Journal.2015; 39(3): 207. CrossRef - New Directions in Chronic Disease Management
Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon
Endocrinology and Metabolism.2015; 30(2): 159. CrossRef - Current Clinical Status of Telehealth in Korea: Categories, Scientific Basis, and Obstacles
Hun-Sung Kim, Hyunah Kim, Suehyun Lee, Kye Hwa Lee, Ju Han Kim
Healthcare Informatics Research.2015; 21(4): 244. CrossRef - Using mobile phones in healthcare management for the elderly
Hun-Sung Kim, Kye-Hwa Lee, Hyunah Kim, Ju Han Kim
Maturitas.2014; 79(4): 381. CrossRef

 KDA
KDA
 PubReader
PubReader Cite
Cite