
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Lifestyle
- Reducing Carbohydrate from Individual Sources Has Differential Effects on Glycosylated Hemoglobin in Type 2 Diabetes Mellitus Patients on Moderate Low-Carbohydrate Diets
- Hajime Haimoto, Shiho Watanabe, Keiko Maeda, Takashi Murase, Kenji Wakai
- Diabetes Metab J. 2021;45(3):390-403. Published online July 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0033
- 5,791 View
- 160 Download
- 3 Web of Science
- 3 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 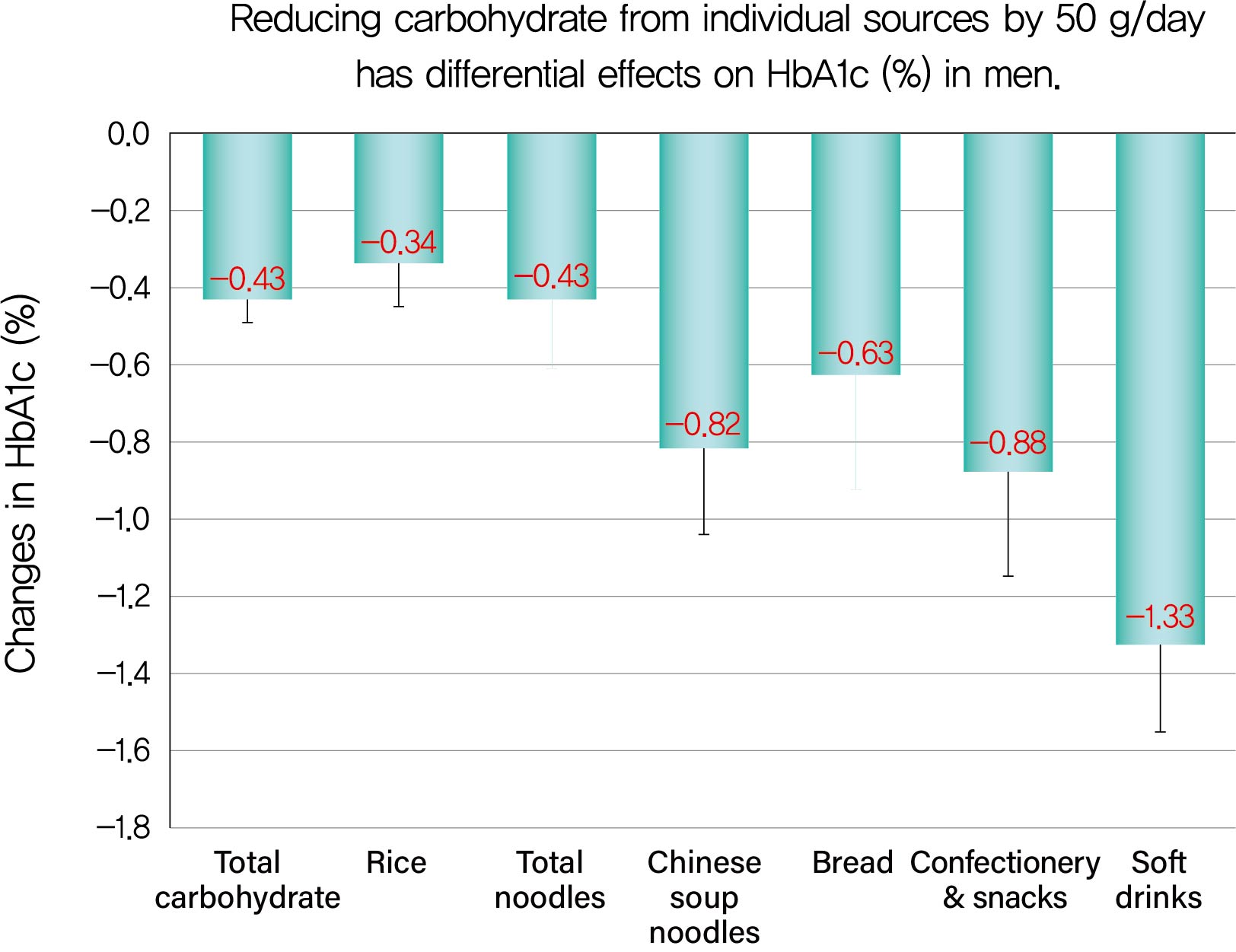
Background We evaluated decreases in glycosylated hemoglobin (HbA1c) achieved by reducing carbohydrate from various sources in type 2 diabetes mellitus patients.
Methods We followed up 138 male and 107 female outpatients on a moderate low-carbohydrate diet without diabetic medication for 6 months. Changes in carbohydrate sources (Δcarbohydrate) were assessed from 3-day dietary records at baseline and 6 months, and associations with changes in HbA1c (ΔHbA1c) were examined with Spearman's correlation coefficients (
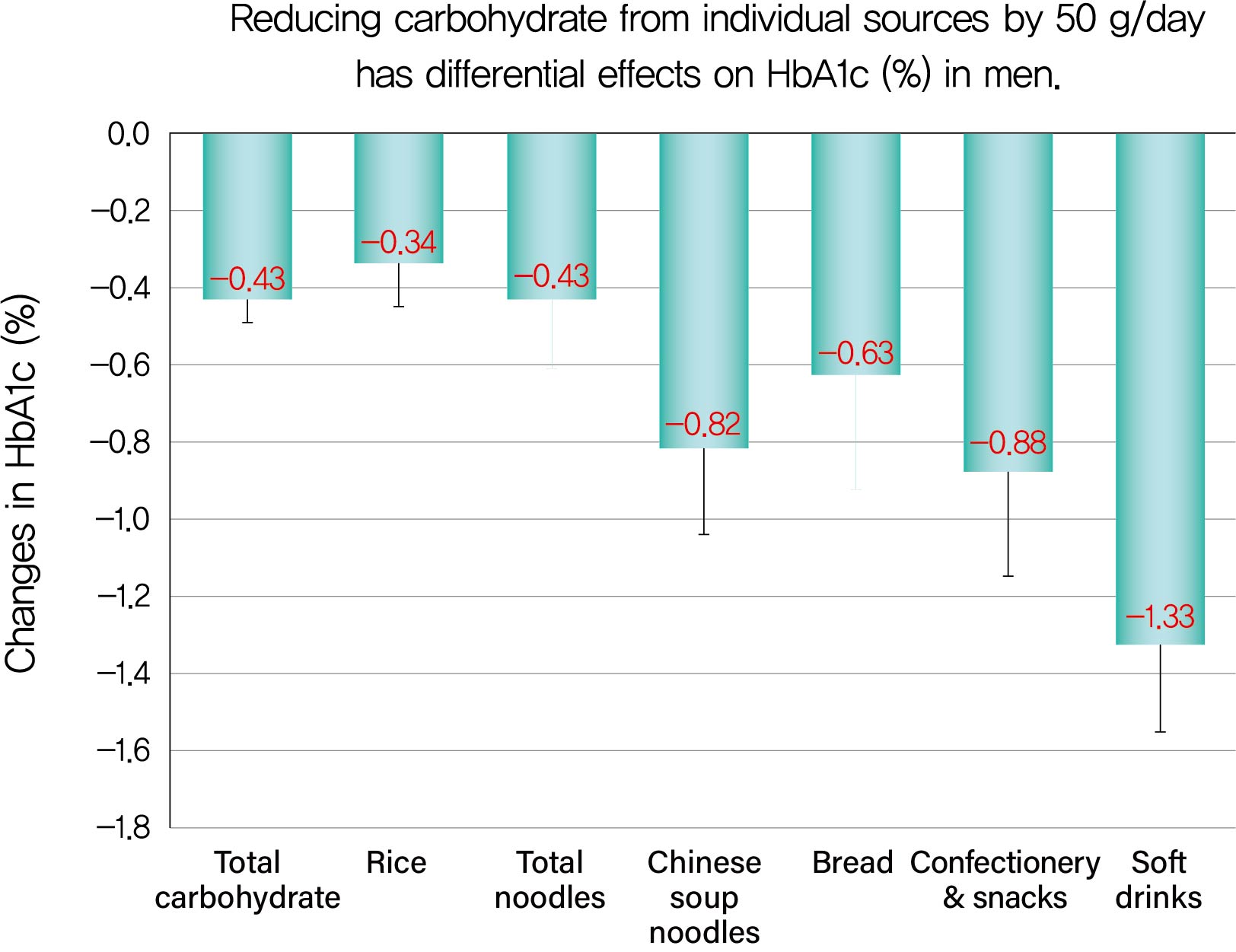
r s) and multiple regression analysis.Results ΔHbA1c was −1.5%±1.6% in men and −0.9%±1.3% in women, while Δtotal carbohydrate was −115.3±103.7 g/day in men and −63.6±71.1 g/day in women. Positive associations with ΔHbA1c were found for Δtotal carbohydrate (
r s=0.584), Δcarbohydrate from soft drinks (0.368), confectionery (0.361), rice (0.325), bread (0.221), Chinese soup noodles (0.199) in men, and Δtotal carbohydrate (0.547) and Δcarbohydrate from rice (0.376) and confectionery (0.195) in women. Reducing carbohydrate sources by 50 g achieved decreases in HbA1c of 0.43% for total carbohydrate, 1.33% for soft drinks, 0.88% for confectionery, 0.63% for bread, 0.82% for Chinese soup noodles and 0.34% for rice in men and 0.45% for total carbohydrate, 0.67% for confectionery and 0.34% for rice in women, although mean reductions in carbohydrate from these sources were much smaller than that from rice.Conclusion Decreases in HbA1c achieved by reducing carbohydrate from soft drinks, confectionery, bread and Chinese soup noodles were 2- to 4-fold greater than that for rice. Our results will enable patients to decrease HbA1c efficiently (UMIN000009866).
-
Citations
Citations to this article as recorded by- Exploring diet associations with Covid-19 and other diseases: a Network Analysis–based approach
Rashmeet Toor, Inderveer Chana
Medical & Biological Engineering & Computing.2022; 60(4): 991. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - Associations of Dietary Salt and Its Sources with Hemoglobin A1c in Patients with Type 2 Diabetes Not Taking Anti-Diabetic Medications: Analysis Based on 6-Month Intervention with a Moderate Low-Carbohydrate Diet
Hajime Haimoto, Takashi Murase, Shiho Watanabe, Keiko Maeda, Kenji Wakai
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4569. CrossRef
- Exploring diet associations with Covid-19 and other diseases: a Network Analysis–based approach
- Small Rice Bowl-Based Meal Plan for Energy and Marcronutrient Intake in Korean Men with Type 2 Diabetes: A Pilot Study
- Hee Jung Ahn, Kyung Ah Han, Jin Young Jang, Jae Hyuk Lee, Kang Seo Park, Kyung Wan Min
- Diabetes Metab J. 2011;35(3):273-281. Published online June 30, 2011
- DOI: https://doi.org/10.4093/dmj.2011.35.3.273
- 65,535 View
- 37 Download
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Koreans eat rice, which is usually served in a rice bowl. We investigated the effect of a meal plan using small rice bowls on the total energy intake (TEI) and the marcronutrient intake in Korean men with type 2 diabetes.
Methods A total of 62 men with type 2 diabetes were divided by body mass index (BMI) (normal weight [NW], BMI<23 kg/m2; overweight [OW], 23≤BMI<25 kg/m2; obese [OB], BMI≥25 kg/m2) and proportions of carbohydrate intake to TEI (PCI) (low carbohydrate intake [LC], <55%; recommended carbohydrate intake [RC], ≥55% and ≤60%; high carbohydrate intake [HC], >60%). The 3-day dietary records were analyzed for TEI and proportions of macronutrients, before and 2 weeks after a small-sized (300 mL) rice bowl based education was given.
Results There were no significant differences in the age and BMI within the sub-groups by BMI and PCI groups. In baseline, the ratio of TEI to recommended total energy intake (RTR) of OW and OB were higher than that of NW. The PCI of HC was higher than that of LC and alcohol intake of HC was lower than that of LC. After education, the reduction of RTREI in OB was higher than that in OW and NW. The reduction of PCI in HC was higher than that of LC.
Conclusion A small rice bowl based meal plan was effective for the reduction of energy intake and control of marcronutrient intake in Korean obese men with type 2 diabetes consuming a high carbohydrate diet.
-
Citations
Citations to this article as recorded by- Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - The association between measurement sites of visceral adipose tissue and cardiovascular risk factors after caloric restriction in obese Korean women
Hye-Ok Lee, Jung-Eun Yim, Jeong-Sook Lee, Young-Seol Kim, Ryowon Choue
Nutrition Research and Practice.2013; 7(1): 43. CrossRef - Daily Rice Intake Strongly Influences the Incidence of Metabolic Syndrome in Japanese Men Aged 40-59 Years
Yoko Watanabe, Isao Saito, Yasuhiko Asada, Taro Kishida, Tatsuhiro Matsuo, Masamitsu Yamaizumi, Tadahiro Kato
Journal of Rural Medicine.2013; 8(1): 161. CrossRef
- Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte

 KDA
KDA
 First
First Prev
Prev





