Real-World Analysis of Therapeutic Outcome in Type 1 Diabetes Mellitus at a Tertiary Care Center
Article information
Abstract
Insulin replacement in type 1 diabetes mellitus (T1DM) needs intensified treatment, which can either be performed by multiple daily injections (MDI) or continuous subcutaneous insulin infusion (CSII). This retrospective analysis of a real-world scenario aimed to evaluate whether glycaemic and cardiovascular risk factors could be controlled with CSII outclass MDI as suggested by recent evidence. Data from patients with either insulin pump (n=68) or injection (n=224) therapy at an Austrian tertiary care centre were analysed between January 2016 and December 2017. There were no significant differences with regard to the latest glycosylated hemoglobin, cardiovascular risk factor control or diabetes-associated late complications. Hypoglycaemia was less frequent (P<0.001), sensor-augmented therapy was more common (P=0.003) and mean body mass index (BMI) was higher (P=0.002) with CSII treatment. This retrospective analysis of real-world data in T1DM did not demonstrate the superiority of insulin pump treatment with regard to glycaemic control or cardiovascular risk factor control.
Highlights
• Insulin pump treatment did not outclass injection therapy with regard to hemoglobin A1c, cardiovascular risk factor control or diabetes-associated complications in this real-world collective.
• Hypoglycemia and use of sensor-augmented therapy improved within the pump treatment group.
• Future research questions should address hybrid-closed and closed loop systems and incorporate newer target parameters.
• Rapid advancements in diabetic technologies need to be evaluated before implementation in daily diabetes management.
INTRODUCTION
Intensified therapy is the gold standard for lifelong insulin replacement therapy in type 1 diabetes mellitus (T1DM). A stringent glycaemic control targeting a glycosylated hemoglobin (HbA1c) of <7% leads to a decrease in early-stage microvascular [1] as well as later macrovascular complications [2], and thus, metabolic memory [1,3]. Modern diabetes-related technologies, such as insulin pump treatment and sensor-augmented therapy, are meant to improve glycaemic control and ease diabetes management, particularly by providing new target parameters [4-6]. Continuous subcutaneous insulin infusion (CSII) is associated with decreasing the HbA1c level and lowering the rates of severe hypoglycaemia in comparison with multiple daily injections (MDI) [7-9]. In randomized controlled trials (RCTs) and meta-analyses, even in the absence of improvement in glycaemic control, treatment satisfaction [10], and quality of life [11] were found to increase. Regarding complications, less cases of retinopathy and nerve abnormality were observed with pump therapy [12].
This retrospective real-world analysis aimed to investigate whether insulin pump treatment outclass injections therapy helped in achieving the goals for glycaemic and cardiovascular risk factor control (CVRFC) as suggested by recent evidence. Hence, the hypothesis was that glycaemic control is better with CSII when compared with MDI therapy.
METHODS
For this retrospective study of real-world data, we included 292 patients with diabetes (either T1DM or late-autoimmune diabetes in adults), aged 18 to 80 years, who were treated at the Outpatient Department of Endocrinology and Metabolism, Vienna General Hospital. Their data were analysed between January 2016 and December 2017 (extracted from the latest follow-up visit within the observation period for glycaemic control and CVRFC).
Demographic and clinical data, including body mass index (BMI), sex, date of birth, age, lipid profile, and blood pressure (automated-oscillometric-method) were extracted from patient charts.
For this study, insulin delivery method, data concerning glycaemic control and diabetes-associated-complications were analysed (HbA1c, hypoglycaemia per week, severe hypoglycaemia, sensor-augmented therapy, albuminuria, coronary heart disease [CHD], peripheral artery disease [PAD], ischemic cerebrovascular disease [CBVD], diabetic retinopathy [DRP], and diabetic neuropathy [DNP]). For the analysis of glycaemic control, we used the latest available HbA1c data within the observation period of each individual (the mean follow-up duration was 3.8±12 months). Hypoglycaemia was defined as a measured blood sugar level of ≤70 mg/dL per week (obtained from continuous glucose monitoring [CGM] protocols, handwritten logbooks or the documentation of medical history during the latest outpatient visit) and severe hypoglycaemia, that is, hypoglycaemia requiring external help (extracted from the documentation made during the latest outpatient visit, admission to a hospital and/or documented inpatient stay due to a hypoglycaemic condition). HbA1c was measured using the Haemoglobin Testing System D-10 of BioRad (Hercules, CA, USA; certified method of the National Glycohemoglobin Standardization Program, Diabetes Control and Complications Trial [DCCT] aligned and International Federation of Clinical Chemistry and Laboratory Medicine [IFCC] standardised) [13]. The study was approved by the local ethics committee (EK Nr: 2115/2017) with no informed consent due to retrospective character of the study and was performed in accordance with the Declaration of Helsinki.
Statistical methods
The descriptive characteristics of the demographic and clinical data were stratified according to the insulin delivery method (CSII vs. MDI) and presented in terms of frequency, mean±standard deviation and median (interquartile range). The significance was tested by chi-square test, Mann-Whitney U test (in case of skewed distribution), Fisher’s exact test (expected cell frequency <5) or unpaired t-test. Adjustments for group differences in age, BMI, sex, diabetes duration and the use of real-time continuous glucose monitoring (rtCGM) or intermittently scanning continuous glucose monitoring (iscCGM) systems were performed by using linear models. A two-sided P value of <0.05 was considered statistically significant. The statistical analysis was descriptive and was performed using IBM SPSS version 25 (IBM Co., Armonk, NY, USA).
RESULTS
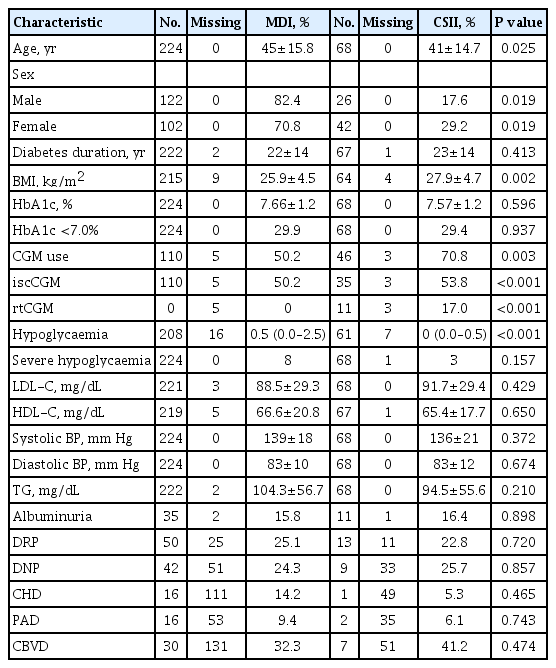
Overall, 68 subjects with CSII and 224 patients with MDI were included. The characteristics of the population, including CVRFC and diabetes-associated complications, are listed in Table 1. Table 2 presents the logistic regression data.
The latest mean HbA1c in the observational period was not significantly different (CSII 7.57%±1.18% vs. MDI 7.66%± 1.18%, P=0.596; 95% confidence interval [CI], –0.24 to 0.41). To adjust the influence of other factors on the achievement of the primary outcome, a linear regression model was performed by including the variables of age, sex, BMI, diabetes duration and use of sensor-augmented therapy. However, only sex had statistically significant values (P=0.019) that influenced the HbA1c. After adjusting for CSII treatment, sex, age, BMI, diabetes duration, and influence of sensor-augmented therapy, there was no significant difference in HbA1c between the groups (∆0.20%, P=0.282; 95% CI, –0.58 to 0.17) (Table 2).
The median number of hypoglycaemic events per week was significantly lower with pump therapy (P<0.001). Adjustment for possible confounders (sex, age, BMI, diabetes duration, and sensor-augmented therapy) was performed by linear regression, and only the insulin delivery method (CSII vs. MDI) and CGM use showed significant values. Results concerning severe hypoglycaemic events were not significant.
More patients with CSII used sensor-augmented therapy (P=0.003). The iscCGM was applied in both treatment groups in equal rates, whereas rtCGM was employed in the CSII group (Table 1).
The mean BMI within the CSII treatment group was higher (P=0.002), and more patients with pump therapy tended to suffer from obesity (CSII 28.1% vs. MDI 16.3%, P=0.034). The study does not report further significant results concerning CVRFC. The mean differences in the lipid profile, blood pressure and albumin-creatinine ratio between the two treatment groups were not significantly different. Results concerning complications (DRP, PAD, CHD, DNP, CBVD, and albuminuria) were not significantly different between the groups (Table 1).
DISCUSSION
To sum up the most relevant findings of our study, CSII treatment did not outclass MDI with regard to HbA1c, CVRFC, or diabetes-associated complications in this real-world collective. The number of hypoglycaemic events and the use of sensoraugmented therapy with CSII were superior when compared with MDI.
On the basis of this retrospective analysis, we were not able to demonstrate the superiority of insulin pump therapy in controlling mean HbA1c in our real-world setting although evidence suggests its advantage [7-9,14]. Owing to the retrospective nature of this study, we were not able to reproduce the basis of choice and implications of therapy selection for each of the included patients. Higher insulin needs, worse glycaemic control or higher insulin resistance may be the reasons for patients switching to insulin pump treatment. Moreover, the patients’ preference for either of the treatment options and cost-effectiveness are possible biases to be considered. According to a recently published meta-analysis, there may be a decrease in statistically significant results between CSII and MDI once rapidacting analogues are applied [15]. Our study reports that the number of hypoglycaemic events was significantly lower with CSII treatment, and sensor-augmented therapy was applied more often in this group. Evidence shows that rtCGM is more beneficial in the prevention of hypoglycaemia when compared with iscCGM [16], which might explain the detected difference.
Traditional cardiovascular risk factors in combination with hyperglycaemia increase the risk for diabetes-associated complications in T1DM. Herein, we detected a significant difference in BMI between the two treatment groups. This result may either be explained by the unequal ratio (one-fourth vs. three-fourths) or by the differences in baseline BMI. We do not report further significant results concerning CVRFC and prevention of diabetes-associated complications. Since only few studies are available on this aspect, there is an obvious need for further investigations [17].
RCTs involve powerful and highly methodical approaches [18]. However, this might be disadvantageous for some reasons. There are rapid advancements in diabetic technologies, and the evaluation of these changes and their implementation in daily diabetes management might take longer with the conventional concept of RCTs (complex study design, costs, specific populations). Patients may adjust their behaviour, compliance, and motivation after inclusion in studies, resulting in the improvement of glycaemic control without causality, or the subjects may vary significantly from those seen in daily clinical practice. Therefore, real-world evidence might gain importance in evaluating and converting the possible benefits of diabetic treatment options and settings in a faster manner [18,19]. On the other hand, it may be difficult to interpret and develop reliable conclusions for general populations when analysing data from real-world scenarios. Individual preferences, compliance, cost-effectiveness, and insurance coverage might be some of the possible confounders. This issue might be solved by performing prospective longitudinal analysis with matched pairs from clinical registries or databases. Therefore, the presented results need to take into account the limitations of retrospective real-world data and may not be reproducible in a general population [19].
To conclude, in this retrospective analysis of a real-world scenario, insulin pump treatment did not offer significant benefits in terms of glycated haemoglobin or CVRFC. The available evidence suggesting the superiority of CSII might not be reproducible in this real-world collective because of the retrospective nature and the usage of rapid-acting insulin agents.
Future research questions that exploit the potential of the CSII regimen might address a more recent observation period to evaluate whether hybrid-closed and closed loop systems improve glycaemic control when compared with MDI. Furthermore, newer target parameters (time-in-range and glucose variability) may be incorporated in the analysis.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conception or design: A.K.
Acquisition, analysis, or interpretation of data: A.K., L.B.
Drafting the work or revising: M.R., L.B.
Final approval of the manuscript: M.R., L.B.
FUNDING
None
Acknowledgements
None