Prevalence and Management of Dyslipidemia in Korea: Korea National Health and Nutrition Examination Survey during 1998 to 2010
Article information
Abstract
Background
Dyslipidemia is a major risk factor of cardiovascular disease. The aim of this study was to investigate the changing trends in the prevalence and management status of dyslipidemia among Korean adults.
Methods
The prevalence of dyslipidemia and the rates of awareness, treatment, and control of dyslipidemia were investigated in adults aged ≥20 years from the Korea National Health and Nutrition Surveys (KNHANES) 1998 to 2010. The updated National Cholesterol Education Program criteria was used, which define dyslipidemia as having one or more of the following lipid abnormalities: hypercholesterolemia (total cholesterol ≥240 mg/dL or diagnosis of dyslipidemia or use of lipid-lowering drugs), hypertriglyceridemia (≥150 mg/dL), hyper-low density lipoprotein (LDL) cholesterolemia (≥160 mg/dL or diagnosis of dyslipidemia or use of lipid-lowering drugs), and hypo-high density lipoprotein (HDL)-cholesterolemia (<40 mg/dL in men and <50 mg/dL in women).
Results
The number of participants was 6,921, 4,894, 5,312, 2,733, 6,295, 6,900, and 5,738 in KNHANES 1998, 2001, 2005, 2007, 2008, 2009, and 2010, respectively. Age-standardized prevalence rates of dyslipidemia were 54.0%, 65.8%, 66.5%, 60.6%, 58.7%, 58.9%, and 59.0% in 1998, 2001, 2005, 2007, 2008, 2009, and 2010, respectively. Hypertriglyceridemia and hypo-HDL-cholesterolemia were the two most frequent lipid abnormalities. The overall prevalence of hypercholesterolemia and hyper-LDL-cholesterolemia increased by 1.36- and 1.35-fold in 2010 compared with 2007, respectively. Awareness, treatment, and control rates of dyslipidemia improved over the period of surveys in both sexes. In 2010, about 30% of dyslipidemic patients who received lipid-lowering treatment reached target levels.
Conclusion
Although the management status of dyslipidemia has improved during recent years, effective strategy is required for achieving better prevention, treatment, and control of dyslipidemia.
INTRODUCTION
Cardiovascular disease is one of main causes of death worldwide [1]. In Korea, cardiovascular disease accounted for approximately 1 of every 10 deaths from 2011 mortality data [2]. Metabolic syndrome is an important risk factor for cardiovascular disease [3,4] and adult Koreans with the metabolic syndrome are more likely to have a history of cardiovascular disease than those without the syndrome [5]. Among the five components of the metabolic syndrome, dyslipidemia, and abdominal obesity were the major factors influencing the increased prevalence of metabolic syndrome in Koreans for the past 10 years [6]. Previous epidemiologic studies revealed that high-carbohydrate diet, abdominal obesity, and physical inactivity were related with greater risk of elevated triglyceride and low high density lipoprotein cholesterol (HDL-C) levels in Korean population [7,8].
Since dyslipidemia has been considered as an important risk factor that contributes to the development of cardiovascular disease, the assessment of the prevalence and management status of dyslipidemia in recent years would be an initial step for planning preventive strategy reducing the development of cardiovascular disease. Studies from the United States using the data from the National Health and Nutrition Examination Surveys (NHANES) 1988 to 2010 reported a decrease in total cholesterol and low density lipoprotein cholesterol (LDL-C), an increase in triglyceride, and an unchanged HDL-C level in United States [9]. Meanwhile, in Japanese general population, the total cholesterol level and triglyceride level (only in men) increased in past 10 years (1990 to 2000) [10]. Lee et al. [11] reported that prevalence of dyslipidemia in Korea gradually increased from 1998 to 2005 through the data from Korea National Health and Nutrition Survey (KNHANES) 1998, 2001, and 2005. However, a relatively short duration of the study, as well as the differences in the definition of dyslipidemia between KNHANES 2005 and 1998/2001 make direct comparisons difficult [11].
In this study, we investigated the recent changes in the prevalence, awareness, treatment, and control rates of dyslipidemia among Korean adults in KNHANES 1998 to 2010 by adopting an updated National Cholesterol Education Program Adult Treatment Panel (NCEP-ATP) III definition [12]. We also investigated the changes in the factors constituting dyslipidemia among Korean adults.
METHODS
Data source and study population
This study was performed using the data from KNHANES I (1998), II (2001), III (2005), and IV (2007 to 2009), V (2010). KNHANES is a nationwide, community-based cross-sectional survey examining the general health and nutrition status of the noninstitutionalized civilians of Korea, conducted by the Division of Health and Nutritional Survey under the Korean Centers for Disease Control and Prevention (KCDCP). It consisted of three distinct surveys: health interview survey, health examination survey, and nutrition survey. Participants were selected from sampling units based on geographical area-, sex-, and age-groups using household registries with a stratified, multistage, clustered, probability sampling design. This sampling method is certified as producing representative statistics by the Korea Department of Statistics. KNHANES was conducted according to the guidelines laid down in the Declaration of Helsinki. All participants in the survey signed an informed consent form. The Institutional Review Board of KCDCP approved the protocol.
In KNHANES I (1998) and II (2001), individuals were not asked about their prior diagnosis and management in the health interview survey because the prevalence of dyslipidemia was considered to be very low in Korea at that time period. Self-reported prior diagnosis of dyslipidemia and current use of lipid-lowering drugs were available since 2005. We analyzed subjects over 20 years old and completed the health examination and health interview survey as well. In the analysis, any measurements that were missing total cholesterol, HDL-C, or triglycerides were excluded. All individuals voluntarily agreed to participate in this survey and informed consent was obtained from all of them. The survey protocol was approved by an Institutional Review Board of KCDCP.
Dyslipidemia was defined entirely based on the blood test results in the health examination performed in 1998 and 2001. The definition of dyslipidemia was made according to the presence of one or more of the following criteria: hypercholesterolemia (total cholesterol ≥240 mg/dL); hypertriglyceridemia (triglyceride ≥150 mg/dL); hyper-LDL-cholesterolemia (LDL-C ≥160 mg/dL); and hypo-HDL-cholesterolemia (HDL-C <40 mg/dL in men and <50 mg/dL in women). Since 2005, dyslipidemia was determined with fasting blood tests as well as health interview survey data. Hypercholesterolemia was defined by previous diagnosis by physician or current use of lipid-lowering drugs or total cholesterol of ≥240 mg/dL. Hyper-LDL-cholesterolemia was defined by previous diagnosis by medical doctor or current use of lipid-lowering medications or LDL-C of ≥160 mg/dL. Hypo-HDL-cholesterolemia and hypertriglyceridemia were defined in the same manner as in 1998 and 2001.
And then, we divided the participants into diabetic and nondiabetic subjects to compare the prevalence and management status of dyslipidemia between the two groups. The diagnostic criteria for diabetes mellitus were obtained from the American Diabetes Association (ADA) guidelines [13]: diabetes was diagnosed in subjects whose level of fasting plasma glucose was over 126 mg/dL or who responded to health interview survey as having had a previous diagnosis of diabetes by physician or treated with antidiabetic agents or insulin. We categorized the lipid-related risks of coronary artery disease in diabetic participants according to the updated NCEP-ATP III and the 2008 ADA/American College of Cardiology Statement [14]. Patients with diabetes alone should be considered to be at high risk, while patients with diabetes and one or more additional risk factors of coronary artery disease are considered to be at very high risk. The major risk factors of coronary artery disease included high LDL-C (≥160 mg/dL), cigarette smoking, hypertension (systolic/diastolic blood pressure ≥140/90 mm Hg or use of antihypertensive medication), low HDL-C (<40 mg/dL), and age (men ≥45 years, women ≥55 years). When HDL-C concentration was ≥60 mg/dL, one risk factor was subtracted from a patient's overall risk profile.
Awareness rate, treatment rate, and control rate of dyslipidemia were defined using the health interview survey and the health examination survey results from KNHANES. Awareness rate was defined as the number of individuals who were identified in the health interview survey as having had a previous diagnosis of dyslipidemia by a physician divided by the number of people with dyslipidemia. Treatment rate was defined as participants whose response to the health interview survey indicated that they have been taking lipid-lowering drugs among those with dyslipidemia. Treatment goal was defined according to the American Association of Clinical Endocrinologists guidelines for management of dyslipidemia [15]. Control rate was defined based on individuals who reached treatment goal (LDL-C levels <160 mg/dL, triglyceride levels <150 mg/dL, HDL-C levels >40 mg/dL in men and >50 mg/dL in women) among who have taken lipid-lowering drugs. For the definition of control rate in diabetic participants, LDL-C target of <100 mg/dL was used. Dyslipidemic patients with a very high risk of coronary artery disease had LDL-C target of <70 mg/dL.
Biochemical measurements
The blood samples were drawn from antecubital vein of each participant in the morning after fasting for at least 8 hours. Samples were properly processed, refrigerated at 2℃ to 8℃, and immediately sent to the Central Testing Institute in Seoul, Korea, where plasma was separated immediately by centrifugation. The fasting plasma concentrations of glucose and lipids were measured enzymatically in a central laboratory; a 747-chemistry analyzer was used (Hitachi, Tokyo, Japan) in the 1998 and 2001 studies, while an Advia 1,650/2,400 was employed (Siemens, New York, NY, USA) in 2005 and 2007, and a Hitachi Automatic Analyzer 7600 (Hitachi) was used in 2008, 2009, and 2010. Because the analysis tool and the method of measuring HDL-C were changed due to changes in clinical laboratory organization, revised HDL-C level was derived since 2007 according to the Lipid Standardization Program [16] made by Centers for Disease Control and Prevention (CDC) in the United States. LDL-C was calculated using Friedewald's formula [17] in individuals with triglycerides ≤400 mg/dL. LDL-C level has been directly measured using automated enzymatic techniques since 2009 in KNHANES IV.
Statistical analysis
Statistical analyses were performed with complex-samples analysis procedures in SPSS version 19.0 (IBM Co., Armonk, NY, USA). We used KNHANES stratification variables and sampling weights designated by KCDCP, which were based on the sample design of each survey year. Data were presented as percentage (standard error) for nominal data or means±standard error for continuous variables. The age-standardized prevalence of dyslipidemia and other lipid abnormalities were calculated by the age- and sex-specific structure of the 2010 Korean population. As the definition of dyslipidemia changed in KNHANES 2005 and revised HDL-C level have been available since the KNHANES 2007, we compared the prevalence of dyslipidemia during 2007 to 2010. In order to compare the prevalence rates of each year, logistic regression analyses were used. Every comparison among the studies was done after age adjustment.
RESULTS
A total of 6,921 (aged 43.2±0.37 years), 4,894 (45.8±0.40), 5,312 (43.5±0.35), 2,733 (44.2±0.48), 6,295 (44.7±0.38), 6,900 (44.9±0.36), and 5,738 (45.0±0.44) respondents were available for analysis from KNHANES in the 1998, 2001, 2005, 2007, 2008, 2009, and 2010, respectively. Table 1 shows the characteristics of participants in KNHANES during 1998 to 2010. Age-standardized prevalence rates of dyslipidemia were 54.0% in 1998, 65.8% in 2001, 66.5% in 2005, 60.6% in 2007, 58.7% in 2008, 58.9% in 2009, and 59.0% in 2010. The prevalence of dyslipidemia was higher in women than in men every year (57.6% in men and 60.4% in women in 2010).
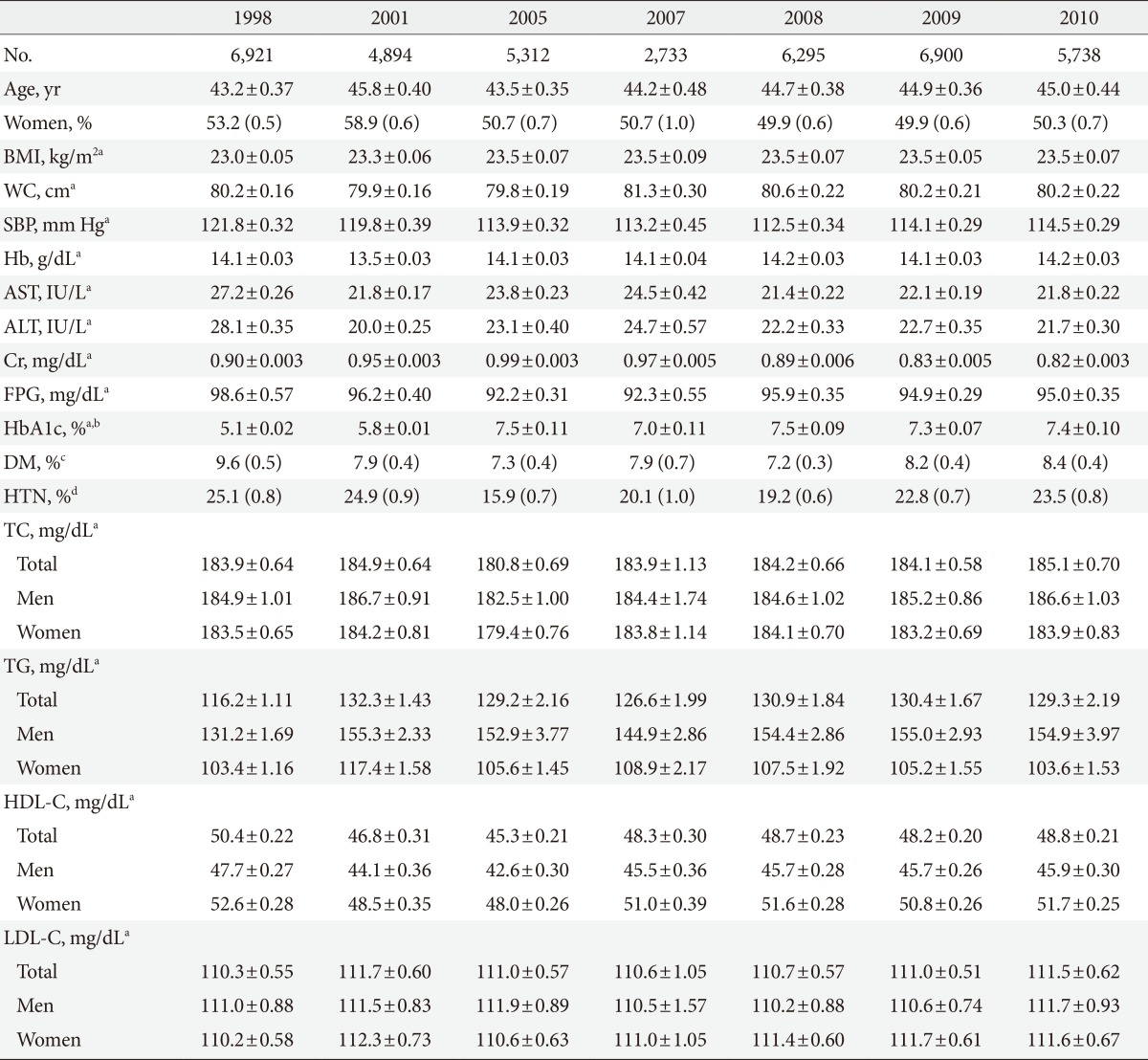
Anthropometric and biochemical parameters in the Korea National Health and Nutrition Survey during 1998 to 2010
Table 2, Fig. 1 show age-standardized prevalence rates of dyslipidemia and each lipid abnormalities of it in KNHANES during 2007 to 2010. In women, the prevalence of hypo-HDL-cholesterolemia tended to decrease and the prevalence in 2010 has decreased by 0.76-fold (95% confidence interval [CI], 0.66 to 0.88) compared with the prevalence reported in 2007. In men, the prevalence of hypo-HDL-cholesterolemia was the second frequent lipid abnormality and accounted for almost one third of all dyslipidemia. In contrast to women, the prevalence of hypo-HDL-cholesterolemia in men tended to increase: prevalence in 2010 had increased by 1.13-fold (95% CI, 0.93 to 1.38) compared with that in 2007. The prevalence of hypertriglyceridemia, most frequent lipid abnormality in men, has not changed significantly in men, while a significantly decreasing tendency was found in women. Compared with the prevalence in 2007, the prevalence in 2010 has decreased by 0.80-fold (95% CI, 0.67 to 0.96) in women. On the other hand, the prevalence of hypercholesterolemia and hyper-LDL-cholesterolemia, the two lowest frequent lipid abnormalities, has significantly increased in both sexes after 2007. In 2010, the overall prevalence of hypercholesterolemia and hyper-LDL-cholesterolemia has increased by 1.36- and 1.35-fold compared with the prevalence in 2007, respectively.
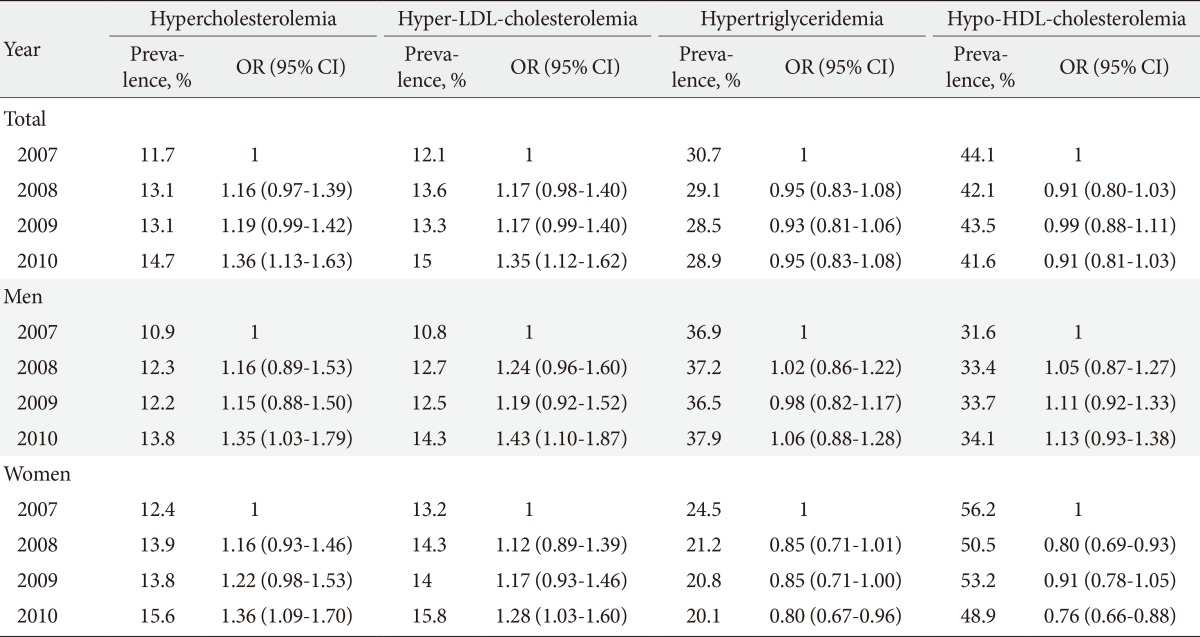
Age-standardized prevalence rates of each lipid abnormalities of dyslipidemia in the Korea National Health and Nutrition Survey during 2007 to 2010
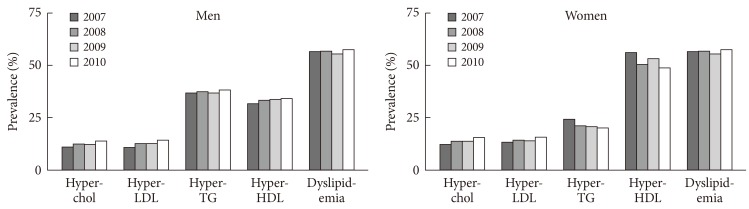
Prevalence rates of dyslipidemia and each factors of it according to sex in the Korea National Health and Nutrition Survey during 2007 to 2010. (A) Men. (B) Women. Hyper-chol, hypercholesterolemia; Hyper-LDL, hyper-low density lipoprotein-cholesterolemia; Hyper-TG, hypertriglyceridemia; Hypo-HDL, hypo-high density lipoprotein-cholesterolemia.
The prevalence of dyslipidemia and its individual lipid abnormalities by sex- and age-category in 2010 are shown in Fig. 2. The prevalence of dyslipidemia peaked in the 50 to 60 year age groups in men and has decreased after age 70 years. In contrast, the prevalence had rapidly increasing trend as age increased in women. In subjects ≥70 years the prevalence of dyslipidemia in women was about 1.5 times higher than that of men. The prevalence of hypercholesterolemia and hyper-LDL-cholesterolemia were higher in men than in women in the 30 to 40 age groups, although the prevalence rate was higher in women after age 50. The prevalence of hypertriglyceridemia was much higher in men in younger age groups. Women had a higher prevalence of hypo-HDL-cholesterolemia in all age groups than men. The percentage of women with HDL-cholesterolemia below 45 mg/dL was similar to that of men with hypo-HDL-cholesterolemia (HDL-C <40 mg/dL) in KNHANES during 1998 to 2010 (data not shown). The prevalence of dyslipidemia and its respective components by sex- and age-category during 1998 to 2010 are described in detail in Appendixes 1-5 (1, prevalence of dyslipidemia; 2, prevalence of hypercholesterolemia; 3, prevalence of hypertriglyceridemia; 4, prevalence of hyper-LDL-cholesteroleamia; 5, prevalence of hypo-HDL-cholesterolemia).

Prevalence rates of dyslipidemia and its individual lipid abnormalities by sex and age-category in the 2010 Korea National Health and Nutrition Survey. LDL, low density lipoprotein; HDL, high density lipoprotein.
Participants with diabetes had a higher prevalence of dyslipidemia and more respective lipid abnormalities than nondiabetic subjects during 1998 to 2010 period (Fig. 3). In 2010, the prevalence of dyslipidemia was 79.6% in diabetic and 56.7% in nondiabetic subjects. The prevalences of hypercholesterolemia and hyper-LDL-cholesterolemia were 36.0% and 35.1% in diabetic and 12.5% and 12.9% in nondiabetic subjects, respectively. The prevalence of hypertriglyceridemia was 49.3% in diabetic and 26.8% in nondiabetic subjects. The prevalence of hypo-HDL-cholesterolemia was 53.7% in diabetic and 40.0% in nondiabetic subjects in 2010.
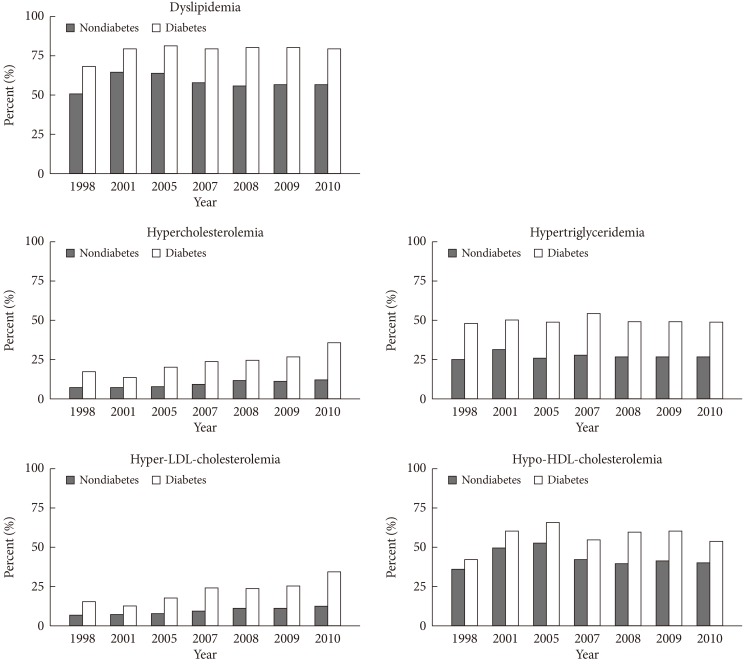
Prevalence rates of dyslipidemia and its individual components according to the presence of diabetes in the Korea National Health and Nutrition Survey during 1998 to 2010. LDL, low density lipoprotein; HDL, high density lipoprotein.
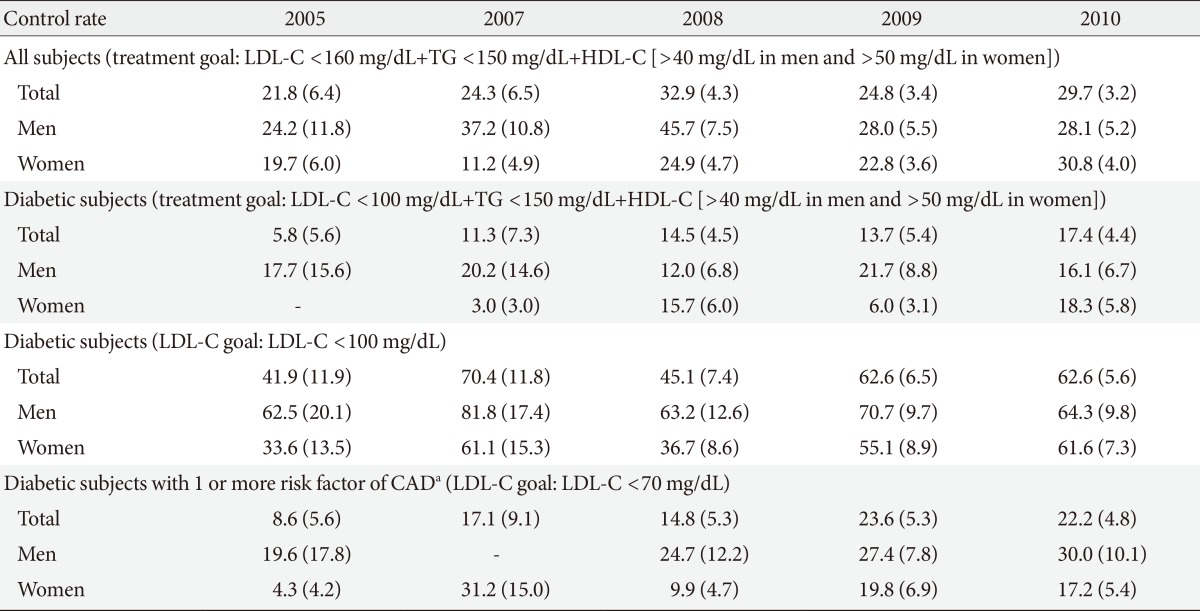
Awareness rate had increased annually during 2005 to 2010 from 6.1% in 2005 to 13.7% in 2010. Treatment rate tended to increase: it was 1.9% in 2005 and 7.4% in 2010 (Table 3). The rates of awareness and treatment in diabetic subjects were much higher than nondiabetic subjects in both sexes. In 2010, awareness rate was 34.6% in diabetic and 11.0% in nondiabetic subjects. Treatment rate in 2010 was 23.6% in diabetic and 5.3% in nondiabetic subjects. Control rate of dyslipidemia among treated patients showed an increasing tendency (Table 4). The rate of dyslipidemic subjects who reached treatment goal (LDL-C levels <160 mg/dL, triglyceride levels <150 mg/dL, HDL-C levels >40 mg/dL in men and >50 mg/dL in women) among who have taken lipid-lowering drugs was 21.8% in 2005 and 29.7% in 2010. The rate of diabetic patients who reached treatment goal (LDL-C levels <100 mg/dL, triglyceride levels <150 mg/dL, HDL-C levels >40 mg/dL in men and >50 mg/dL in women) increased from 5.8% in 2005 to17.4% in 2010. The control rate in LDL-C defined as below 100 mg/dL in diabetic subjects tended to increase from 41.9% in 2005 to 62.6% in 2010. Among diabetic subjects with a very high risk of cardiovascular disease treated with lipid-lowering drug, the rate of subjects who had LDL-C level <70 mg/dL increased from 8.6% in 2005 to 22.2% in 2010.
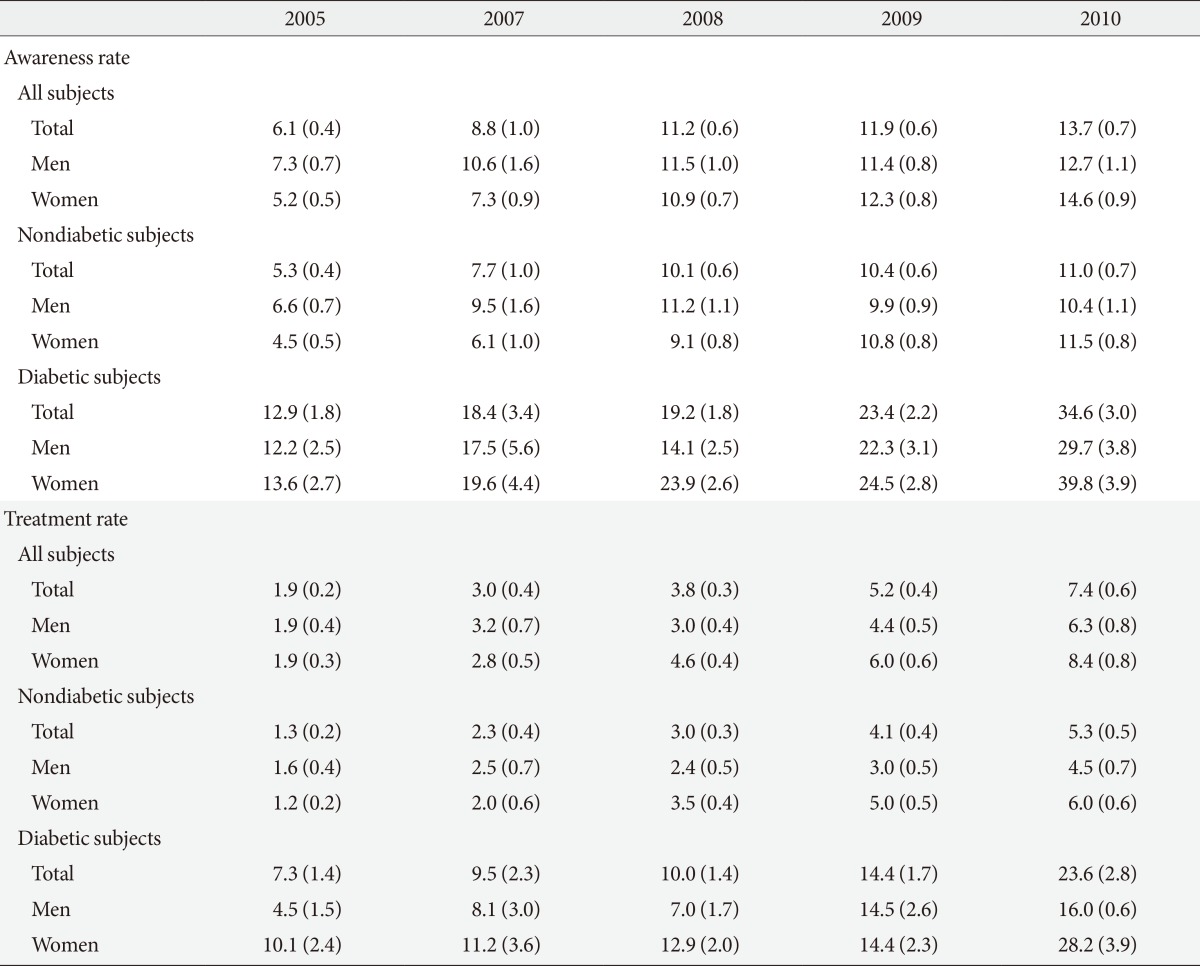
Awareness and treatment rates of dyslipidemia in the Korea National Health and Nutrition Survey during 2005 to 2010
DISCUSSION
This is the first national-scale epidemiologic study to evaluate the changing trends of the prevalence of dyslipidemia and individual components of dyslipidemia including awareness, treatment, and control rates in Korean adults. The prevalence of dyslipidemia was greater than 50% in both men and women during the past 12 years. About one half of the women had a low level of HDL-cholesterolemia. However, the prevalence of hypo-HDL-cholesterolemia has decreased in women, while it showed an increasing tendency in men during recent 4 years. The proportion of adults with elevated levels of triglyceride significantly decreased in women while it has not changed recently in men. The increase in the prevalence of hypercholesterolemia and hyper-LDL-cholesterolemia, the two lowest frequent lipid abnormalities in both sexes, was significant during recent 4 years in Korea. The proportion of dyslipidemic subjects who had been previously diagnosed by a medical doctor and who have been taking lipid-lowering medications and who reached treatment goals after treatment with lipid-lowering drugs increased over the past 5 years.
Elevated total cholesterol and LDL-C levels are independent risk factors of development of cardiovascular disease [18,19]. A 10 mg/dL increase of total cholesterol was associated with 9% increase of death from cardiovascular disease during in a 30-year follow-up study [20]. Reducing plasma LDL-C levels with the use of statins reduced the incidence of death from cardiovascular causes [21,22]. A large-scale epidemiological study in United States observed the decreases in total and LDL-C levels in recent 20 years due to the increase in the percentage of adults taking lipid-lowering drugs [9]. A previous report on trends in total cholesterol worldwide indicated mean cholesterol levels declined in developed countries (North America, Western Europe, Australia, and some Asian regions) [9,23]. A recent increasing trend of the prevalence of hypercholesterolemia and hyper-LDL-cholesterolemia in Korea is consistent with the increasing prevalence of cardiovascular disease [2]. A relatively low proportion of adults taking lipid-lowering drugs (7.4% from KNHANES 2010 vs. 15.5% from NHANES 2007 to 2010 [9]) might have affected the increasing trend of the prevalence of hypercholesterolemia and hyper-LDL-cholesterolemia.
Low-carbohydrate diet contributes to favorable effects on atherogenic dyslipidemia including elevated serum triglyceride and reduced HDL-C [24,25]. The high prevalence of hypertriglyceridemia and hypo-HDL-cholesterolemia in Korean adults could be related with high-carbohydrate diet. A recent Korean study revealed that previous traditional Korean diet with high-carbohydrate content was related with elevated triglyceride and low HDL-C [7]. It is also well-known that body mass index is inversely related to the concentration of HDL-C [26] and positively with triglyceride levels [27]. The recent decreasing trend in the prevalence of hypertriglyceridemia and hypo-HDL-cholesterolemia in Korean women is consistent with a decreased prevalence of obesity in young and middle-aged Korean women [28]. A social preference for thin body image may have affected the decreasing trend of the prevalence of obesity in these female age subgroups [29,30]. Meanwhile, an increasing trend in the prevalence of obesity in Korean men might be one of the reasons of recently increased prevalence of hypo-HDL-cholesterolemia in men [28].
HDL-C is known as an inverse predictor of cardiovascular disease [31-33]. A 1 mg/dL increase of HDL-C is associated with 2% reduction in the relative risk of cardiovascular disease in men and 3% reduction in women [34]. Triglyceride is a risk factor of cardiovascular disease for both men and women in the general population, independent of HDL-C [35]. High body mass index, abdominal obesity, cigarette smoking, and physical inactivity were associated with a greater risk of low HDL-C levels in Korean adults [8]. Thus, smoking cessation, increasing physical activity, and decreasing body weight would all contribute to increasing HDL-C levels in Korean population [36].
The characteristic features of diabetic dyslipidemia are high plasma triglyceride concentration, low HDL-C concentration, and increased concentration of small, dense LDL-C particles [37]. In this study, we found that Korean diabetic patients had a higher prevalence of all lipid abnormalities of dyslipidemia than that of nondiabetic subjects. A higher prevalence of hypercholesterolemia and hyper-LDL-cholesterolemia in diabetic subjects is considered to be affected by a higher rate of self-reported prior diagnosis or current use of lipid-lowering drugs in diabetic participants.
This study had some limitations. Although KNHANES collected nationally representative data, it is a cross-sectional evaluation of the health and nutritional status of Koreans. To prevent the potential errors in survey methods, the prevalence estimated in each KNHANES was standardized according to the 2010 Korean population. Each KNHANES was conducted with different subjects and since it was based on self-administered questionnaire, recall bias, confounding factors, and unintentional errors should be considered. The change in the definition of hypercholesterolemia and hyper-LDL-cholesterolemia in 2005 by an introduction of questionnaire for previous diagnosis of dyslipidemia by physician and current use of lipid-lowering drugs made it difficult to analyze trends over time using the 1998 and 2001 KNAHNES data. Also, the change in the protocol of HDL-C measurement could have affected the HDL-C results. For this reason, the values were standardized according to the United States Centers for Disease Control and Prevention Lipid Standardization Program to minimize method effects since 2007.
In conclusion, more than half of Korean adults have had dyslipidemia from KNHANES 1998 to KNHANES 2010. Elevated triglyceride and low HDL-C levels were the two most frequent lipid abnormalities in Korean population. A recent increasing trend of hypercholesterolemia and hyper-LDL-cholesterolemia is associated with an increasing prevalence of cardiovascular mortality in Korea. Although the awareness and treatment rates of dyslipidemia have improved during this period, the low control rate in dyslipidemia suggests a need for a national strategy to prevent increasing trend of atherogenic dyslipidemia. Proper lifestyle management with weight loss, low carbohydrate diet, and regular exercise are recommended to reduce the burden of dyslipidemia and cardiovascular mortality.
Notes
No potential conflict of interest relevant to this article was reported.
Appendix
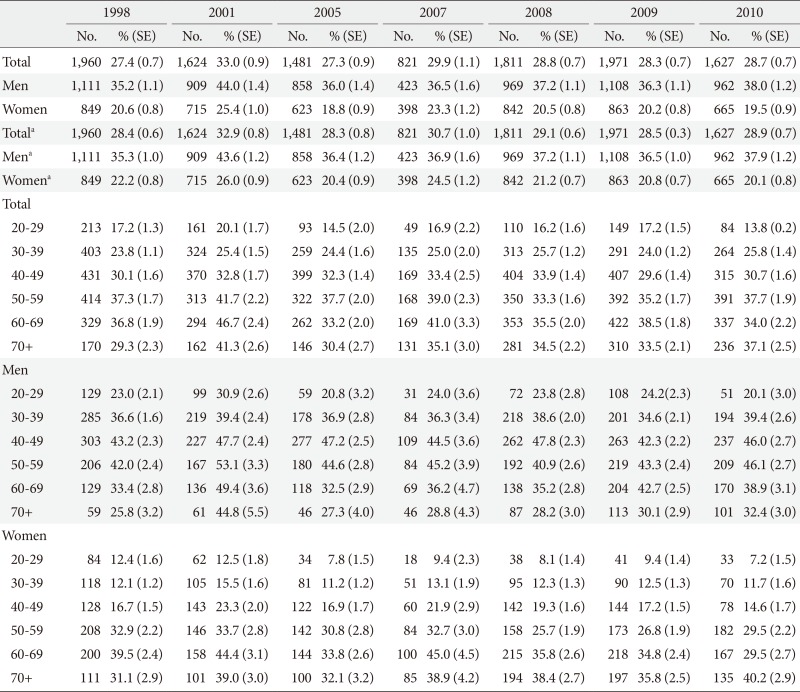
Appendix 1
Prevalence rates of dyslipidemia in the Korea National Health and Nutrition Survey during 1998 to 2010 by sex- and age-category
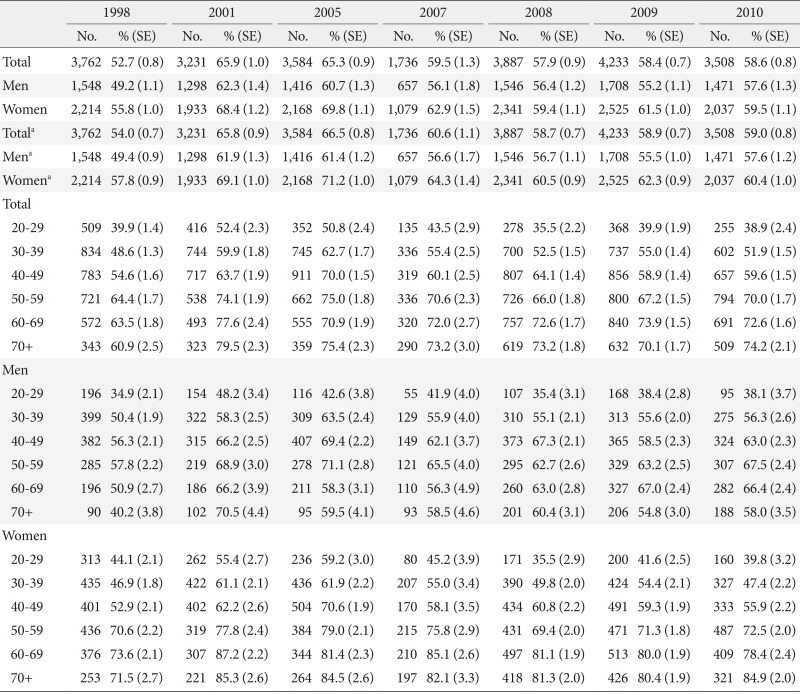
SE, standard error.
aAge-standardized (standard population: 2010 Korean population).
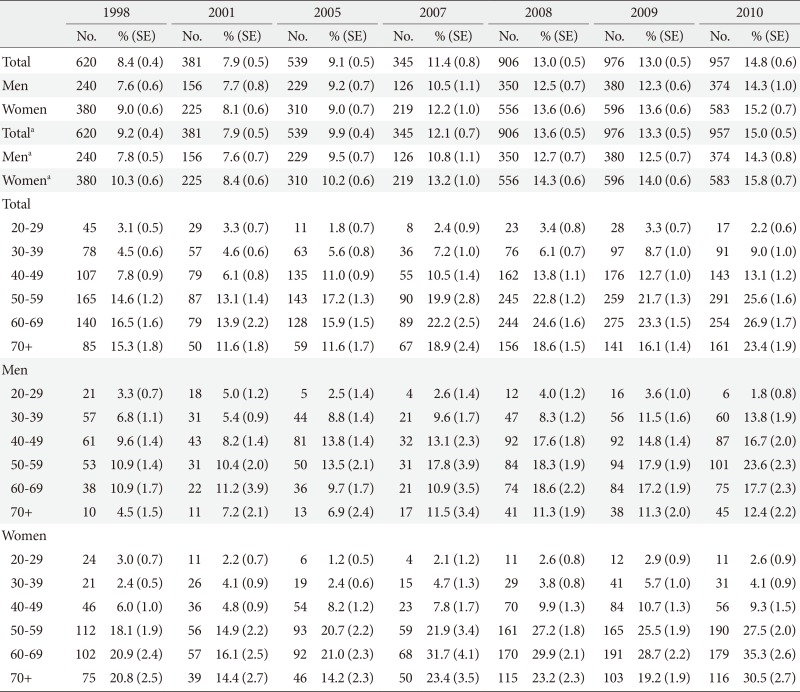
Appendix 2
Prevalence rates of hypercholesterolemia in the Korea National Health and Nutrition Survey during 1998 to 2010 by sex- and age-category
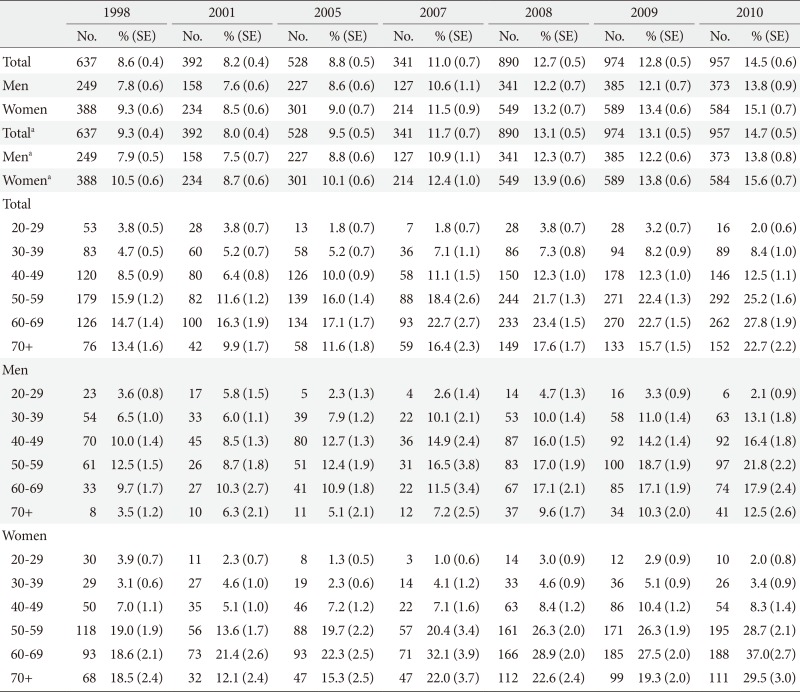
SE, standard error.
aAge-standardized (standard population: 2010 Korean population).
Appendix 3
Prevalence rates of hypertriglyceridemia in the Korea National Health and Nutrition Survey during 1998 to 2010 by sex- and age-category
SE, standard error.
aAge-standardized (standard population: 2010 Korean population).
Appendix 4
Prevalence rates of hyper-low density lipoprotein cholesterolemia in the Korea National Health and Nutrition Survey during 1998 to 2010 by sex- and age-category
SE, standard error.
aAge-standardized (standard population: 2010 Korean population).
Appendix 5
Prevalence rates of hypo-high density lipoprotein cholesterolemia in the Korea National Health and Nutrition Survey during 1998 to 2010 by sex- and age-category
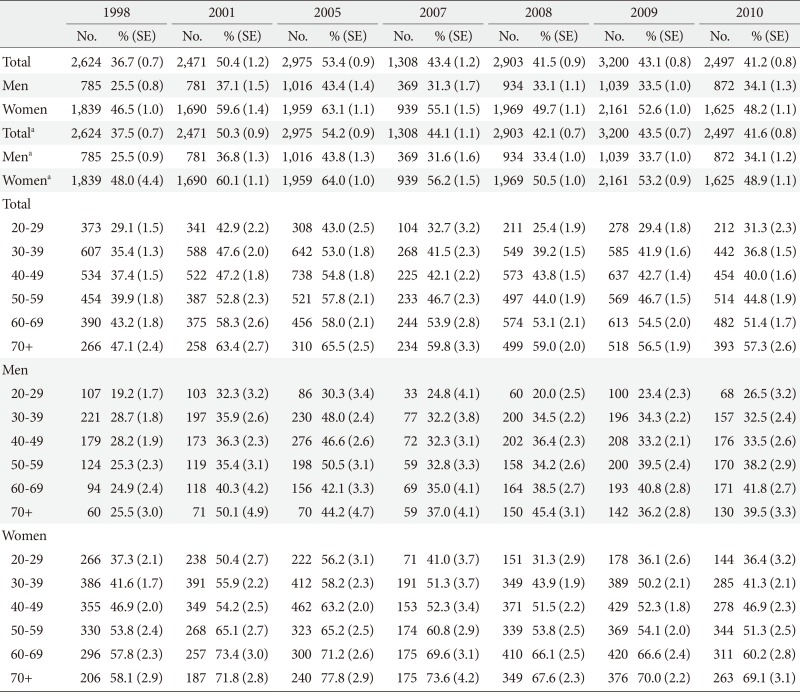
SE, standard error.
aAge-standardized (standard population: 2010 Korean population).