
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Technology/Device
- Clinical and Lifestyle Determinants of Continuous Glucose Monitoring Metrics in Insulin-Treated Patients with Type 2 Diabetes Mellitus
- Da Young Lee, Namho Kim, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Jihee Kim, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Sung-Min Park, Nan Hee Kim
- Diabetes Metab J. 2023;47(6):826-836. Published online August 24, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0273

- 1,800 View
- 191 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There was limited evidence to evaluate the association between lifestyle habits and continuous glucose monitoring (CGM) metrics. Thus, we aimed to depict the behavioral and metabolic determinants of CGM metrics in insulin-treated patients with type 2 diabetes mellitus (T2DM).
Methods
This is a prospective observational study. We analyzed data from 122 insulin-treated patients with T2DM. Participants wore Dexcom G6 and Fitbit, and diet information was identified for 10 days. Multivariate-adjusted logistic regression analysis was performed for the simultaneous achievement of CGM-based targets, defined by the percentage of time in terms of hyper, hypoglycemia and glycemic variability (GV). Intake of macronutrients and fiber, step counts, sleep, postprandial C-peptide-to-glucose ratio (PCGR), information about glucose lowering medications and metabolic factors were added to the analyses. Additionally, we evaluated the impact of the distribution of energy and macronutrient during a day, and snack consumption on CGM metrics.
Results
Logistic regression analysis revealed that female, participants with high PCGR, low glycosylated hemoglobin (HbA1c) and daytime step count had a higher probability of achieving all targets based on CGM (odds ratios [95% confidence intervals] which were 0.24 [0.09 to 0.65], 1.34 [1.03 to 1.25], 0.95 [0.9 to 0.99], and 1.15 [1.03 to 1.29], respectively). And participants who ate snacks showed a shorter period of hyperglycemia and less GV compared to those without.
Conclusion
We confirmed that residual insulin secretion, daytime step count, HbA1c, and women were the most relevant determinants of adequate glycemic control in insulin-treated patients with T2DM. In addition, individuals with snack consumption were exposed to lower times of hyperglycemia and GV. -
Citations
Citations to this article as recorded by- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
Lotte Bogaert, Iris Willems, Patrick Calders, Eveline Dirinck, Manon Kinaupenne, Marga Decraene, Bruno Lapauw, Boyd Strumane, Margot Van Daele, Vera Verbestel, Marieke De Craemer
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2024; 18(4): 102995. CrossRef
- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
- Metabolic Risk/Epidemiology
- Lifestyle Interventions for Non-Obese Patients Both with, and at Risk, of Non-Alcoholic Fatty Liver Disease
- Xin-Lei Zhang, Ting-Yao Wang, Giovanni Targher, Christopher D. Byrne, Ming-Hua Zheng
- Diabetes Metab J. 2022;46(3):391-401. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0048
- 5,261 View
- 274 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
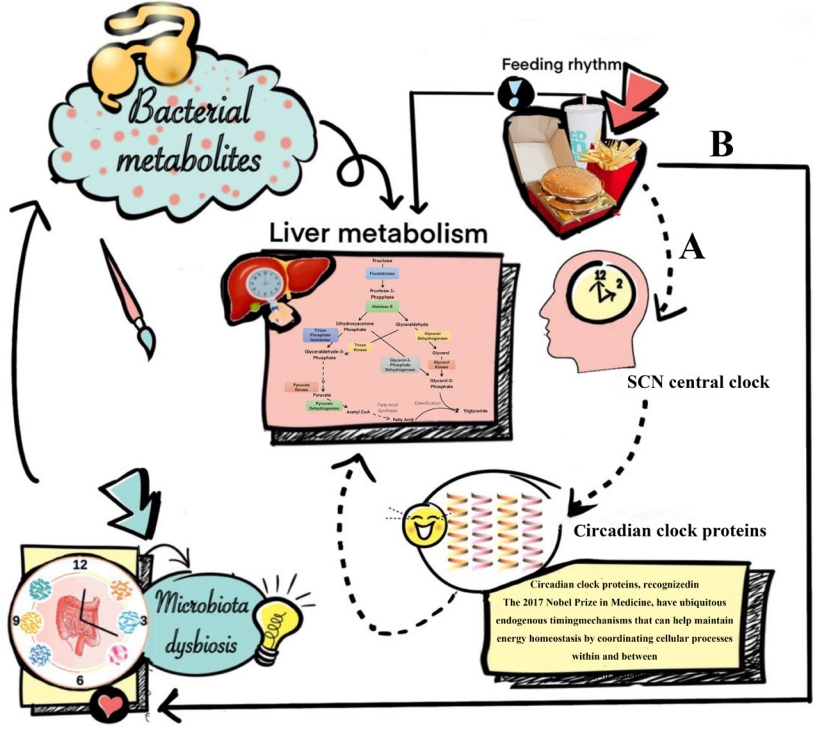
ePub - Non-alcoholic fatty liver disease occurring in non-obese subjects (the so-called non-obese NAFLD) is a highly prevalent but neglected liver condition, which is closely associated with metabolic disorders and suboptimal lifestyles. Landmark studies have shown that lifestyle interventions are potentially beneficial in decreasing the risk of developing non-obese NAFLD and in ameliorating NAFLD in non-obese individuals with pre-existing NAFLD. Lifestyle interventions usually refer to changes in eating habits and physical activity, both of which have a powerful effect on non-obese NAFLD and on risk factors for non-obese NAFLD. However, to date, patients and health-care professionals have a poor awareness and understanding of non-obese NAFLD and the beneficial effects of lifestyle interventions in this patient population. The aim of this narrative review is to briefly discuss the evidence for the effects of lifestyle changes and what changes are needed amongst medical personnel and other stakeholders in order to raise awareness of non-obese NAFLD.
-
Citations
Citations to this article as recorded by- Triglycerides Mediate the Influence of Body Mass Index on Non-Alcoholic Fatty Liver Disease in a Non-Obese Chinese Population with Normal Low-Density Lipoprotein Cholesterol Levels
Xixi Han, Jingwen Kong, Hemin Zhang, Yuan Zhao, Yafeng Zheng, Chao Wei
Obesity Facts.2024; 17(2): 191. CrossRef - Patients with NAFLD exhibit more advanced fibrosis in liver biopsy than patients with other chronic liver diseases
Lydia Rohr, Peter Lemmer, Marie Henning, Andrea Tannapfel, Theodor Baars, Paul Manka, Ali Canbay, Jan-Peter Sowa
Zeitschrift für Gastroenterologie.2023; 61(01): 29. CrossRef - Performance of Simple Fibrosis Score in Non-Alcoholic Fatty Liver Disease with and without Type 2 Diabetes
Seung Min Chung, Min Kyu Kang, Jun Sung Moon, Jung Gil Park
Endocrinology and Metabolism.2023; 38(2): 277. CrossRef - An international multidisciplinary consensus statement on MAFLD and the risk of CVD
Xiao-Dong Zhou, Giovanni Targher, Christopher D. Byrne, Virend Somers, Seung Up Kim, C. Anwar A. Chahal, Vincent Wai-Sun Wong, Jingjing Cai, Michael D. Shapiro, Mohammed Eslam, Philippe Gabriel Steg, Ki-Chul Sung, Anoop Misra, Jian-Jun Li, Carlos Brotons,
Hepatology International.2023; 17(4): 773. CrossRef - Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
Eugene Han, Yong-ho Lee
Clinical and Molecular Hepatology.2023; 29(4): 980. CrossRef - Sex-Based Differences and Risk Factors for Comorbid Nonalcoholic Fatty Liver Disease in Patients with Bipolar Disorder: A Cross-Sectional Retrospective Study
Ying Wang, Yiyi Liu, Xun Zhang, Qing Wu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3533. CrossRef - Benefits of Physical Exercise as Approach to Prevention and Reversion of Non-Alcoholic Fatty Liver Disease in Children and Adolescents with Obesity
Valeria Calcaterra, Vittoria Magenes, Matteo Vandoni, Clarissa Berardo, Luca Marin, Alice Bianchi, Erika Cordaro, Giustino Silvestro, Dario Silvestri, Vittoria Carnevale Pellino, Cristina Cereda, Gianvincenzo Zuccotti
Children.2022; 9(8): 1174. CrossRef - The effects of supplementation of probiotics, prebiotics, or synbiotics on patients with non-alcoholic fatty liver disease: A meta-analysis of randomized controlled trials
Wenmin Xing, Wenyan Gao, Xiaoling Lv, Zhenlei Zhao, Genxiang Mao, Xiaoyan Dong, Zuyong Zhang
Frontiers in Nutrition.2022;[Epub] CrossRef
- Triglycerides Mediate the Influence of Body Mass Index on Non-Alcoholic Fatty Liver Disease in a Non-Obese Chinese Population with Normal Low-Density Lipoprotein Cholesterol Levels
- Metabolic Risk/Epidemiology
- Short-Term Effects of the Internet-Based Korea Diabetes Prevention Study: 6-Month Results of a Community-Based Randomized Controlled Trial
- Jin-Hee Lee, Sun-Young Lim, Seon-Ah Cha, Chan-Jung Han, Ah Reum Jung, Kook-Rye Kim, Kun-Ho Yoon, Seung-Hyun Ko
- Diabetes Metab J. 2021;45(6):960-965. Published online March 17, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0225
- 5,412 View
- 151 Download
- 5 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 
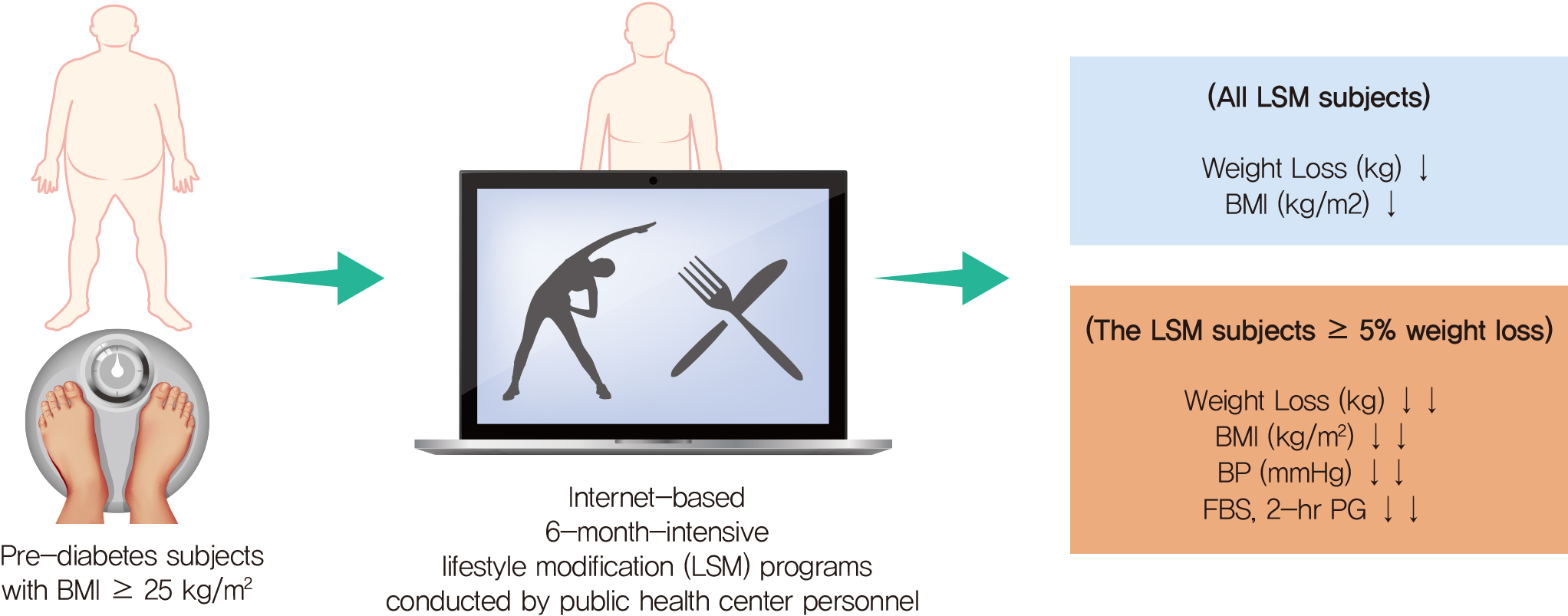
- The aims of this study were to determine the short-term effectiveness of an internet-based lifestyle modification (LSM) program in preventing the onset of type 2 diabetes mellitus (T2DM) in prediabetes patients in community settings. A total of 415 subjects who were diagnosed with prediabetes were randomly assigned to the LSM and standard management (SM) groups. After the 6-month intervention, the LSM group had a statistically significant reduction in body weight, body mass index compared to the SM group participants. In the LSM group, blood glucose levels were significantly decreased after intervention and the clinical improvement effect was evident in the group that achieved the target weight loss of 5% or more of the initial weight for 6 months. Internet-based 6-month-intensive LSM programs conducted by public health center personnel are an effective way to provide lifestyle intervention programs and encourage maintenance of healthy behaviors in subjects with a high risk of T2DM in community settings.
-
Citations
Citations to this article as recorded by- U-shaped association between online information exchange and app usage frequency: a large-scale survey of China ‘s online young and middle-aged people with pre diabetes and diabetes
Hanbin Guo, Yibiao Xiao, Canlin Liao, Jiating Sun, Yanchun Xie, Yitong Zheng, Guanhua Fan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Innovation in diabetes prevention research: The 36-year legacy of China Da Qing diabetes prevention study
Xin Chai, Yachen Wang, Jinping Wang, Qiuhong Gong, Juan Zhang, Ruitai Shao
Chinese Science Bulletin.2023; 68(28-29): 3834. CrossRef - Efficacy of Personalized Diabetes Self-care Using an Electronic Medical Record–Integrated Mobile App in Patients With Type 2 Diabetes: 6-Month Randomized Controlled Trial
Eun Young Lee, Seon-Ah Cha, Jae-Seung Yun, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Min Kyung Hyun, Seung-Hyun Ko
Journal of Medical Internet Research.2022; 24(7): e37430. CrossRef - Prevention of type 2 diabetes through remotely administered lifestyle programs: A systematic review
Valaree Villegas, Alisha Shah, JoAnn E. Manson, Deirdre K. Tobias
Contemporary Clinical Trials.2022; 119: 106817. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim,
Diabetes & Metabolism Journal.2021; 45(4): 461. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus in Korea
Seung-Hyun Ko
The Journal of Korean Diabetes.2021; 22(4): 244. CrossRef
- U-shaped association between online information exchange and app usage frequency: a large-scale survey of China ‘s online young and middle-aged people with pre diabetes and diabetes
- Guideline/Fact Sheet
- Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
- Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee, Korean Diabetes Association (KDA) Fatty Liver Research Group
- Diabetes Metab J. 2020;44(3):382-401. Published online May 11, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0010
- 12,347 View
- 337 Download
- 42 Web of Science
- 42 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader This clinical practice position statement, a product of the Fatty Liver Research Group of the Korean Diabetes Association, proposes recommendations for the diagnosis, progression and/or severity assessment, management, and follow-up of non-alcoholic fatty liver disease (NAFLD) in patients with type 2 diabetes mellitus (T2DM). Patients with both T2DM and NAFLD have an increased risk of non-alcoholic steatohepatitis (NASH) and fibrosis and a higher risk of cardiovascular diseases and diabetic complications compared to those without NAFLD. With regards to the evaluation of patients with T2DM and NAFLD, ultrasonography-based stepwise approaches using noninvasive biomarker models such as fibrosis-4 or the NAFLD fibrosis score as well as imaging studies such as vibration-controlled transient elastography with controlled attenuation parameter or magnetic resonance imaging-proton density fat fraction are recommended. After the diagnosis of NAFLD, the stage of fibrosis needs to be assessed appropriately. For management, weight reduction achieved by lifestyle modification has proven beneficial and is recommended in combination with antidiabetic agent(s). Evidence that some antidiabetic agents improve NAFLD/NASH with fibrosis in patients with T2DM is emerging. However, there are currently no definite pharmacologic treatments for NAFLD in patients with T2DM. For specific cases, bariatric surgery may be an option if indicated.
-
Citations
Citations to this article as recorded by- A combined extract containing Schisandra chinensis (SCE) reduced hepatic triglyceride accumulation in rats fed a high-sucrose diet
Haneul Lee, Eun Young Kang, Joowon Lee, Yejin Kim, Sumin Kang, Hayoon Kim, Hyun Kyung Kim, Gyoungok Gang, Sang-gil Lee, Cao Lei, Gwang-woong Go
Food Science and Biotechnology.2024; 33(6): 1449. CrossRef - Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMJ.2024; : e076388. CrossRef - Risk Scores for Prediction of Major Cardiovascular Events in Non-Alcoholic Fatty Liver Disease: A No Man’s Land?
Liliana Gheorghe, Roxana Nemteanu, Andreea Clim, Gina Eosefina Botnariu, Irina Iuliana Costache, Alina Plesa
Life.2023; 13(4): 857. CrossRef - Increased expression of sodium-glucose cotransporter 2 and O-GlcNAcylation in hepatocytes drives non-alcoholic steatohepatitis
Hye Jin Chun, Eun Ran Kim, Minyoung Lee, Da Hyun Choi, Soo Hyun Kim, Eugene Shin, Jin-Hong Kim, Jin Won Cho, Dai Hoon Han, Bong-Soo Cha, Yong-ho Lee
Metabolism.2023; 145: 155612. CrossRef - Association between fatty liver index and risk of end-stage renal disease stratified by kidney function in patients with type 2 diabetes: A nationwide population-based study
Goh Eun Chung, Kyungdo Han, Kyu-Na Lee, Jung Ho Bae, Sun Young Yang, Su-Yeon Choi, Jeong Yoon Yim, Nam Ju Heo
Diabetes & Metabolism.2023; 49(4): 101454. CrossRef - Comparison of glucagon-like peptide-1 receptor agonists and thiazolidinediones on treating nonalcoholic fatty liver disease: A network meta-analysis
Min Jeong Park, Hayeon Kim, Myeong Gyu Kim, Kyungim Kim
Clinical and Molecular Hepatology.2023; 29(3): 693. CrossRef - Histological analysis of hypoglycemic agents on liver fibrosis in patients with non-alcoholic fatty liver disease: a systematic review
Qingxing Xie, Xiaohui Pan, Xinyue Zhang, Jinfang Ma, Ge Peng, Nanwei Tong
Chinese Medical Journal.2023; 136(16): 2014. CrossRef - Hepatotropc effects of glucose-lowering drugs: non-alcoholic fatty liver disease in focus
E. V. Uzhakova, Z. E. Zshanko, E. N. Smirnova
Experimental and Clinical Gastroenterology.2023; (6): 121. CrossRef - Complementary effects of dapagliflozin and lobeglitazone on metabolism in a diet-induced obese mouse model
Yun Kyung Lee, Tae Jung Oh, Ji In Lee, Bo Yoon Choi, Hyen Chung Cho, Hak Chul Jang, Sung Hee Choi
European Journal of Pharmacology.2023; 957: 175946. CrossRef - Hepatic T-cell senescence and exhaustion are implicated in the progression of fatty liver disease in patients with type 2 diabetes and mouse model with nonalcoholic steatohepatitis
Byeong Chang Sim, Yea Eun Kang, Sun Kyoung You, Seong Eun Lee, Ha Thi Nga, Ho Yeop Lee, Thi Linh Nguyen, Ji Sun Moon, Jingwen Tian, Hyo Ju Jang, Jeong Eun Lee, Hyon-Seung Yi
Cell Death & Disease.2023;[Epub] CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Circ_0004535/miR-1827/CASP8 network involved in type 2 diabetes mellitus with nonalcoholic fatty liver disease
Min Li, Ai Zeng, Xinle Tang, Hui Xu, Wei Xiong, Yanying Guo
Scientific Reports.2023;[Epub] CrossRef - Stratification by obesity class, rather than age, can identify a higher percent of children at risk for non‐alcoholic fatty liver disease and metabolic dysfunction
Aurelia Radulescu, Adam J. Dugan, Mary Killian, Suzanna L. Attia, Marialena Mouzaki, George J. Fuchs, Rohit Kohli, Henrietta Bada, Philip A. Kern, Samir Softic
Pediatric Obesity.2022;[Epub] CrossRef - Renal Tubular Damage Marker, Urinary N-acetyl-β-D-Glucosaminidase, as a Predictive Marker of Hepatic Fibrosis in Type 2 Diabetes Mellitus
Hae Kyung Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Diabetes & Metabolism Journal.2022; 46(1): 104. CrossRef - Dulaglutide Ameliorates Palmitic Acid-Induced Hepatic Steatosis by Activating FAM3A Signaling Pathway
Jinmi Lee, Seok-Woo Hong, Min-Jeong Kim, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2022; 37(1): 74. CrossRef - State-of-the-Art Overview of the Pharmacological Treatment of Non-Alcoholic Steatohepatitis
Yongin Cho, Yong-ho Lee
Endocrinology and Metabolism.2022; 37(1): 38. CrossRef - Ezetimibe combination therapy with statin for non-alcoholic fatty liver disease: an open-label randomized controlled trial (ESSENTIAL study)
Yongin Cho, Hyungjin Rhee, Young-eun Kim, Minyoung Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Jin-Young Choi, Yong-ho Lee
BMC Medicine.2022;[Epub] CrossRef - Obesity is an important determinant of severity in newly defined metabolic dysfunction-associated fatty liver disease
Ji Hye Huh, Kwang Joon Kim, Seung Up Kim, Bong-Soo Cha, Byung-Wan Lee
Hepatobiliary & Pancreatic Diseases International.2022; 21(3): 241. CrossRef - Anti-Obesity and Anti-Hyperglycemic Effects of Meretrix lusoria Protamex Hydrolysate in ob/ob Mice
Min Ju Kim, Ramakrishna Chilakala, Hee Geun Jo, Seung-Jae Lee, Dong-Sung Lee, Sun Hee Cheong
International Journal of Molecular Sciences.2022; 23(7): 4015. CrossRef - The associations of hepatic steatosis and fibrosis using fatty liver index and BARD score with cardiovascular outcomes and mortality in patients with new-onset type 2 diabetes: a nationwide cohort study
Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef - Cumulative Exposure to High γ-Glutamyl Transferase Level and Risk of Diabetes: A Nationwide Population-Based Study
Ji-Yeon Park, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Endocrinology and Metabolism.2022; 37(2): 272. CrossRef - SGLT-2 inhibitors and GLP-1 receptor agonists in metabolic dysfunction-associated fatty liver disease
Jun Sung Moon, Jun Hwa Hong, Yong Jin Jung, Ele Ferrannini, Michael A. Nauck, Soo Lim
Trends in Endocrinology & Metabolism.2022; 33(6): 424. CrossRef - Plasma Aldo-Keto Reductase Family 1 Member B10 as a Biomarker Performs Well in the Diagnosis of Nonalcoholic Steatohepatitis and Fibrosis
Aron Park, Seung Joon Choi, Sungjin Park, Seong Min Kim, Hye Eun Lee, Minjae Joo, Kyoung Kon Kim, Doojin Kim, Dong Hae Chung, Jae Been Im, Jaehun Jung, Seung Kak Shin, Byung-Chul Oh, Cheolsoo Choi, Seungyoon Nam, Dae Ho Lee
International Journal of Molecular Sciences.2022; 23(9): 5035. CrossRef - Chinese Herbal Medicine for Type 2 Diabetes Mellitus With Nonalcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis
Sihan Peng, Lu Liu, Ziyan Xie, Xiyu Zhang, Chunguang Xie, Sha Ye, Xiangeng Zhang, Xiaoli Liang, Hongyan Wang, Ya Liu
Frontiers in Pharmacology.2022;[Epub] CrossRef - Non-alcoholic fatty liver disease and sarcopenia is associated with the risk of albuminuria independent of insulin resistance, and obesity
Eugene Han, Mi Kyung Kim, Seung-Soon Im, Byoung Kuk Jang, Hye Soon Kim
Journal of Diabetes and its Complications.2022; 36(8): 108253. CrossRef - Extra-Glycemic Effects of Anti-Diabetic Medications: Two Birds with One Stone?
Eun-Jung Rhee
Endocrinology and Metabolism.2022; 37(3): 415. CrossRef - Plasma Metabolomics and Machine Learning-Driven Novel Diagnostic Signature for Non-Alcoholic Steatohepatitis
Moongi Ji, Yunju Jo, Seung Joon Choi, Seong Min Kim, Kyoung Kon Kim, Byung-Chul Oh, Dongryeol Ryu, Man-Jeong Paik, Dae Ho Lee
Biomedicines.2022; 10(7): 1669. CrossRef - Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes
Yewon Na, Soo Wan Kim, Ie Byung Park, Soo Jung Choi, Seungyoon Nam, Jaehun Jung, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(11): 3022. CrossRef - Nonalcoholic fatty liver disease is associated with early left ventricular diastolic dysfunction in patients with type 2 diabeteS
Walaa Sheba, Eman Morsy, Salah Altahan, Mona Ayaad, Sameh A. Lashen
Alexandria Journal of Medicine.2022; 58(1): 117. CrossRef - The association between changes in hepatic steatosis and hepatic fibrosis with cardiovascular outcomes and mortality in patients with New-Onset type 2 Diabetes: A nationwide cohort study
Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
Diabetes Research and Clinical Practice.2022; 194: 110191. CrossRef - Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease (Diabetes Metab J 2022;46:630-9)
Ji Hye Huh
Diabetes & Metabolism Journal.2022; 46(6): 953. CrossRef - The association of fatty liver index and BARD score with all-cause and cause-specific mortality in patients with type 2 diabetes mellitus: a nationwide population-based study
Goh Eun Chung, Su-Min Jeong, Eun Ju Cho, Ji Won Yoon, Jeong-Ju Yoo, Yuri Cho, Kyu-na Lee, Dong Wook Shin, Yoon Jun Kim, Jung-Hwan Yoon, Kyungdo Han, Su Jong Yu
Cardiovascular Diabetology.2022;[Epub] CrossRef - Non-Albumin Proteinuria (NAP) as a Complementary Marker for Diabetic Kidney Disease (DKD)
Jaehyun Bae, Young Jun Won, Byung-Wan Lee
Life.2021; 11(3): 224. CrossRef - Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: Diagnosis and Treatment
Sook Jung Lee, Byung-Wan Lee
The Journal of Korean Diabetes.2021; 22(1): 38. CrossRef - Non-alcoholic fatty liver disease
Elizabeth E Powell, Vincent Wai-Sun Wong, Mary Rinella
The Lancet.2021; 397(10290): 2212. CrossRef - Allopurinol ameliorates high fructose diet induced hepatic steatosis in diabetic rats through modulation of lipid metabolism, inflammation, and ER stress pathway
In-Jin Cho, Da-Hee Oh, Jin Yoo, You-Cheol Hwang, Kyu Jeung Ahn, Ho-Yeon Chung, Soung Won Jeong, Ju-Young Moon, Sang-Ho Lee, Sung-Jig Lim, In-Kyung Jeong
Scientific Reports.2021;[Epub] CrossRef - Patient Management in Non-Alcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus
A. E. Bagriy, A. D. Zubov, M. V. Khomenko, E. S. Mikhailichenko, E. A. Pylaeva, N. A. Khaustova, E. V. Bryukhovetskaya
Russian Journal of Gastroenterology, Hepatology, Coloproctology.2021; 31(2): 14. CrossRef - Liver Fibrosis Indices for the Prediction of Mortality in Korean Subjects: A 16-Year Prospective Cohort Study
Tae Jung Oh, Kyuho Kim, Jae Hoon Moon, Sung Hee Choi, Nam H Cho, Hak Chul Jang
Journal of the Endocrine Society.2021;[Epub] CrossRef - Reduced Rank Regression-Derived Dietary Patterns Related to the Fatty Liver Index and Associations with Type 2 Diabetes Mellitus among Ghanaian Populations under Transition: The RODAM Study
Tracy Bonsu Osei, Anne-Marieke van Dijk, Sjoerd Dingerink, Felix Patience Chilunga, Erik Beune, Karlijn Anna Catharina Meeks, Silver Bahendeka, Matthias Bernd Schulze, Charles Agyemang, Mary Nicolaou, Adriaan Georgius Holleboom, Ina Danquah
Nutrients.2021; 13(11): 3679. CrossRef - Efficacy and Safety of GLP-1 Receptor Agonists in Patients With Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis
Yuan Zhu, Jiao Xu, Dong Zhang, Xingyu Mu, Yi Shi, Shangtao Chen, Zengxiang Wu, Shuangqing Li
Frontiers in Endocrinology.2021;[Epub] CrossRef - Liver fibrosis indices are related to diabetic peripheral neuropathy in individuals with type 2 diabetes
Kyuho Kim, Tae Jung Oh, Hyen Chung Cho, Yun Kyung Lee, Chang Ho Ahn, Bo Kyung Koo, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Scientific Reports.2021;[Epub] CrossRef - Evaluation of Grapefruit Juice in terms of Interleukin 18 Gene Expression in Rats with Fatty Liver and Healthy Rats
Simin Bahmanpoor, Noosha Zia-Jahromi
journal of ilam university of medical sciences.2021; 29(4): 74. CrossRef
- A combined extract containing Schisandra chinensis (SCE) reduced hepatic triglyceride accumulation in rats fed a high-sucrose diet
- Obesity and Metabolic Syndrome
- Impact of Longitudinal Changes in Metabolic Syndrome Status over 2 Years on 10-Year Incident Diabetes Mellitus
- Ji Hye Huh, Sung Gyun Ahn, Young In Kim, Taehwa Go, Ki-Chul Sung, Jae Hyuk Choi, Kwang Kon Koh, Jang Young Kim
- Diabetes Metab J. 2019;43(4):530-538. Published online February 20, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0111
- 5,082 View
- 55 Download
- 20 Web of Science
- 23 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Metabolic syndrome (MetS) is a known predictor of diabetes mellitus (DM), but whether longitudinal changes in MetS status modify the risk for DM remains unclear. We investigated whether changes in MetS status over 2 years modify the 10-year risk of incident DM.
Methods We analyzed data from 7,317 participants aged 40 to 70 years without DM at baseline, who took part in 2001 to 2011 Korean Genome Epidemiology Study. Subjects were categorized into four groups based on repeated longitudinal assessment of MetS status over 2 years: non-MetS, resolved MetS, incident MetS, and persistent MetS. The hazard ratio (HR) of new-onset DM during 10 years was calculated in each group using Cox models.
Results During the 10-year follow-up, 1,099 participants (15.0%) developed DM. Compared to the non-MetS group, the fully adjusted HRs for new-onset DM were 1.28 (95% confidence interval [CI], 0.92 to 1.79) in the resolved MetS group, 1.75 (95% CI, 1.30 to 2.37) in the incident MetS group, and 1.98 (95% CI, 1.50 to 2.61) in the persistent MetS group (
P for trend <0.001). The risk of DM in subjects with resolved MetS was significantly attenuated compared to those with persistent MetS over 2 years. In addition, the adjusted HR for 10-year developing DM gradually increased as the number of MetS components increased 2 years later.Conclusion We found that discrete longitudinal changes pattern in MetS status over 2 years associated with 10-year risk of DM. These findings suggest that monitoring change of MetS status and controlling it in individuals may be important for risk prediction of DM.
-
Citations
Citations to this article as recorded by- 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association
Seth S. Martin, Aaron W. Aday, Zaid I. Almarzooq, Cheryl A.M. Anderson, Pankaj Arora, Christy L. Avery, Carissa M. Baker-Smith, Bethany Barone Gibbs, Andrea Z. Beaton, Amelia K. Boehme, Yvonne Commodore-Mensah, Maria E. Currie, Mitchell S.V. Elkind, Kelly
Circulation.2024;[Epub] CrossRef - Transitioning from having no metabolic abnormality nor obesity to metabolic impairment in a cohort of apparently healthy adults
Hadas Ben-Assayag, Rafael Y. Brzezinski, Shlomo Berliner, David Zeltser, Itzhak Shapira, Ori Rogowski, Sharon Toker, Roy Eldor, Shani Shenhar-Tsarfaty
Cardiovascular Diabetology.2023;[Epub] CrossRef - Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association
Connie W. Tsao, Aaron W. Aday, Zaid I. Almarzooq, Cheryl A.M. Anderson, Pankaj Arora, Christy L. Avery, Carissa M. Baker-Smith, Andrea Z. Beaton, Amelia K. Boehme, Alfred E. Buxton, Yvonne Commodore-Mensah, Mitchell S.V. Elkind, Kelly R. Evenson, Chete Ez
Circulation.2023;[Epub] CrossRef - The Unique Role of Self-Rated Health in Metabolic Syndrome and its Diagnostic Cardiometabolic Abnormalities: An Analysis of Population-Based Data
K. Umeh, S. Adaji, L. Graham
Journal of Medical Psychology.2023; 25(1): 7. CrossRef - Gender differences in the impact of 3-year status changes of metabolic syndrome and its components on incident type 2 diabetes mellitus: a decade of follow-up in the Tehran Lipid and Glucose Study
Farzad Hadaegh, Amir Abdi, Karim Kohansal, Parto Hadaegh, Fereidoun Azizi, Maryam Tohidi
Frontiers in Endocrinology.2023;[Epub] CrossRef - Clinical implications of changes in metabolic syndrome status after kidney transplantation: a nationwide prospective cohort study
Yu Ho Lee, Sang Heon Song, Seung Hwan Song, Ho Sik Shin, Jaeseok Yang, Myoung Soo Kim, Hyeon Seok Hwang, Curie Ahn, Jaeseok Yang, Jin Min Kong, Oh Jung Kwon, Deok Gie Kim, Cheol-Woong Jung, Yeong Hoon Kim, Joong Kyung Kim, Chan-Duck Kim, Ji Won Min, Sung
Nephrology Dialysis Transplantation.2023; 38(12): 2743. CrossRef - Trajectory patterns of metabolic syndrome severity score and risk of type 2 diabetes
Atieh Amouzegar, Mohammadjavad Honarvar, Safdar Masoumi, Davood Khalili, Fereidoun Azizi, Ladan Mehran
Journal of Translational Medicine.2023;[Epub] CrossRef -
Differential association of metabolic syndrome and low-density lipoprotein cholesterol with incident cardiovascular disease according to sex among Koreans: a national population-based study
Su Yong Kim, Tae-Hwa Go, Jun Hyeok Lee, Jin Sil Moon, Dae Ryong Kang, Se Jin Bae, Se-Eun Kim, Sang Jun Lee, Dong-Hyuk Cho, Young Jun Park, Young Jin Youn, Jang Young Kim, Sung Gyun Ahn
European Journal of Preventive Cardiology.2022; 28(18): 2021. CrossRef - The efficacy and safety of Dendropanax morbifera leaf extract on the metabolic syndrome: a 12-week, placebo controlled, double blind, and randomized controlled trial
Ji Eun Jun, You-Cheol Hwang, Kyu Jeung Ahn, Ho Yeon Chung, Se Young Choung, In-Kyung Jeong
Nutrition Research and Practice.2022; 16(1): 60. CrossRef - Stability and Transformation of Metabolic Syndrome in Adolescents: A Prospective Assessment in Relation to the Change of Cardiometabolic Risk Factors
Pei-Wen Wu, Yi-Wen Lai, Yu-Ting Chin, Sharon Tsai, Tun-Min Yang, Wei-Ting Lin, Chun-Ying Lee, Wei-Chung Tsai, Hsiao-Ling Huang, David W. Seal, Tsai-Hui Duh, Chien-Hung Lee
Nutrients.2022; 14(4): 744. CrossRef - Heart Disease and Stroke Statistics—2022 Update: A Report From the American Heart Association
Connie W. Tsao, Aaron W. Aday, Zaid I. Almarzooq, Alvaro Alonso, Andrea Z. Beaton, Marcio S. Bittencourt, Amelia K. Boehme, Alfred E. Buxton, April P. Carson, Yvonne Commodore-Mensah, Mitchell S.V. Elkind, Kelly R. Evenson, Chete Eze-Nliam, Jane F. Fergus
Circulation.2022;[Epub] CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Nonlinear association between changes in fasting plasma glucose and the incidence of diabetes in a nondiabetic Chinese cohort
Chenghu Huang, Chenhong Ren, Xiuping Xuan, Yi Luo, Caibi Peng
BMC Endocrine Disorders.2022;[Epub] CrossRef - The dynamics of metabolic syndrome development from its isolated components among iranian children and adolescents: Findings from 17 Years of the Tehran Lipid and Glucose Study (TLGS)
Pezhman Bagheri, Davood Khalil, Mozhgan Seif, Esmaeil Khedmati Morasae, Ehsan Bahramali, Fereidoun Azizi, Abbas Rezaianzadeh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2021; 15(1): 99. CrossRef - Heart Disease and Stroke Statistics—2021 Update
Salim S. Virani, Alvaro Alonso, Hugo J. Aparicio, Emelia J. Benjamin, Marcio S. Bittencourt, Clifton W. Callaway, April P. Carson, Alanna M. Chamberlain, Susan Cheng, Francesca N. Delling, Mitchell S.V. Elkind, Kelly R. Evenson, Jane F. Ferguson, Deepak K
Circulation.2021;[Epub] CrossRef - The dynamics of metabolic syndrome development from its isolated components among Iranian adults: findings from 17 years of the Tehran lipid and glucose study (TLGS)
Davood Khalili, Pezhman Bagheri, Mozhgan Seif, Abbas Rezaianzadeh, Esmaeil Khedmati Morasae, Ehsan Bahramali, Fereidoun Azizi
Journal of Diabetes & Metabolic Disorders.2021; 20(1): 95. CrossRef - Metabolic Syndrome Fact Sheet 2021: Executive Report
Ji Hye Huh, Dae Ryong Kang, Jang Young Kim, Kwang Kon Koh
CardioMetabolic Syndrome Journal.2021; 1(2): 125. CrossRef - The Incidence of Metabolic Syndrome and the Valid Blood Pressure Cutoff Value for Predicting Metabolic Syndrome Within the Normal Blood Pressure Range in the Population Over 40 Years Old in Guiyang, China
Li Ma, Hong Li, Huijun Zhuang, Qiao Zhang, Nianchun Peng, Ying Hu, Na Han, Yuxing Yang, Lixin Shi
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 2973. CrossRef - Metabolic Syndrome Severity Score for Predicting Cardiovascular Events: A Nationwide Population-Based Study from Korea
Yo Nam Jang, Jun Hyeok Lee, Jin Sil Moon, Dae Ryong Kang, Seong Yong Park, Jerim Cho, Jang-Young Kim, Ji Hye Huh
Diabetes & Metabolism Journal.2021; 45(4): 569. CrossRef - Hospitalization for heart failure incidence according to the transition in metabolic health and obesity status: a nationwide population-based study
You-Bin Lee, Da Hye Kim, Seon Mee Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Yong Gyu Park, Kyungdo Han, Hye Jin Yoo
Cardiovascular Diabetology.2020;[Epub] CrossRef - Effects of tea consumption on metabolic syndrome: A systematic review and meta‐analysis of randomized clinical trials
Wei Liu, Chunpeng Wan, Yingjie Huang, Mingxi Li
Phytotherapy Research.2020; 34(11): 2857. CrossRef - Exposure-weighted scoring for metabolic syndrome and the risk of myocardial infarction and stroke: a nationwide population-based study
Eun Young Lee, Kyungdo Han, Da Hye Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Cardiovascular Diabetology.2020;[Epub] CrossRef - Changes in Metabolic Profile Over Time: Impact on the Risk of Diabetes
Yunjung Cho, Seung-Hwan Lee
Diabetes & Metabolism Journal.2019; 43(4): 407. CrossRef
- 2024 Heart Disease and Stroke Statistics: A Report of US and Global Data From the American Heart Association
- Clinical Diabetes and Therapeutics
- Hospital-Based Korean Diabetes Prevention Study: A Prospective, Multi-Center, Randomized, Open-Label Controlled Study
- Sang Youl Rhee, Suk Chon, Kyu Jeung Ahn, Jeong-Taek Woo
- Diabetes Metab J. 2019;43(1):49-58. Published online November 2, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0033
- 5,307 View
- 131 Download
- 10 Web of Science
- 13 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The prevalence of diabetes mellitus (DM) continues to increase, and the disease burden is the highest of any medical condition in Korea. However, large-scale clinical studies have not yet conducted to establish the basis for diabetes prevention in Korea.
Methods The hospital-based Korean Diabetes Prevention Study (H-KDPS) is a prospective, multi-center, randomized, open-label controlled study conducted at university hospitals for the purpose of gathering data to help in efforts to prevent type 2 DM. Ten university hospitals are participating, and 744 subjects will be recruited. The subjects are randomly assigned to the standard care group, lifestyle modification group, or metformin group, and their clinical course will be observed for 36 months.
Results All intervention methodologies were developed, validated, and approved by Korean Diabetes Association (KDA) multi-disciplinary team members. The standard control group will engage in individual education based on the current KDA guidelines, and the lifestyle modification group will participate in a professionally guided healthcare intervention aiming for ≥5% weight loss. The metformin group will begin dosing at 250 mg/day, increasing to a maximum of 1,000 mg/day. The primary endpoint of this study is the cumulative incidence of DM during the 3 years after randomization.
Conclusion The H-KDPS study is the first large-scale clinical study to establish evidence-based interventions for the prevention of type 2 DM in Koreans. The evidence gathered by this study will be useful for enhancing the health of Koreans and improving the stability of the Korean healthcare system (Trial registration: CRIS KCT0002260, NCT02981121).
-
Citations
Citations to this article as recorded by- Estimating insulin sensitivity and β-cell function from the oral glucose tolerance test: validation of a new insulin sensitivity and secretion (ISS) model
Joon Ha, Stephanie T. Chung, Max Springer, Joon Young Kim, Phil Chen, Aaryan Chhabra, Melanie G. Cree, Cecilia Diniz Behn, Anne E. Sumner, Silva A. Arslanian, Arthur S. Sherman
American Journal of Physiology-Endocrinology and Metabolism.2024; 326(4): E454. CrossRef - Development and Adaptability of Smartphone-based Dietary Coaching Program for Patients Undergoing Diabetes and Prediabetes with Continuous Glucose Monitoring Device
Myoung Soo Kim, Jung Mi Ryu, Minkyeong Kang, Jiwon Park, Yeh Chan Ahn, Yang Seok Kim
Journal of Health Informatics and Statistics.2023; 48(1): 36. CrossRef - Improving Machine Learning Diabetes Prediction Models for the Utmost Clinical Effectiveness
Juyoung Shin, Joonyub Lee, Taehoon Ko, Kanghyuck Lee, Yera Choi, Hun-Sung Kim
Journal of Personalized Medicine.2022; 12(11): 1899. CrossRef - Impaired fasting glucose levels in overweight or obese subjects for screening of type 2 diabetes in Korea
Jin-Hee Lee, Suk Chon, Seon-Ah Cha, Sun-Young Lim, Kook-Rye Kim, Jae-Seung Yun, Sang Youl Rhee, Kun-Ho Yoon, Yu-Bae Ahn, Jeong-Taek Woo, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 382. CrossRef - Development and Validation of a Deep Learning Based Diabetes Prediction System Using a Nationwide Population-Based Cohort
Sang Youl Rhee, Ji Min Sung, Sunhee Kim, In-Jeong Cho, Sang-Eun Lee, Hyuk-Jae Chang
Diabetes & Metabolism Journal.2021; 45(4): 515. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim,
Diabetes & Metabolism Journal.2021; 45(4): 461. CrossRef - Short-Term Effects of the Internet-Based Korea Diabetes Prevention Study: 6-Month Results of a Community-Based Randomized Controlled Trial
Jin-Hee Lee, Sun-Young Lim, Seon-Ah Cha, Chan-Jung Han, Ah Reum Jung, Kook-Rye Kim, Kun-Ho Yoon, Seung-Hyun Ko
Diabetes & Metabolism Journal.2021; 45(6): 960. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus in Korea
Seung-Hyun Ko
The Journal of Korean Diabetes.2021; 22(4): 244. CrossRef - Optimal fasting plasma glucose and haemoglobin A1c levels for screening of prediabetes and diabetes according to 2‐hour plasma glucose in a high‐risk population: The Korean Diabetes Prevention Study
Seon‐Ah Cha, Suk Chon, Jae‐Seung Yun, Sang Youl Rhee, Sun‐Young Lim, Kun‐Ho Yoon, Yu‐Bae Ahn, Seung‐Hyun Ko, Jeong‐Taek Woo, Jin‐Hee Lee
Diabetes/Metabolism Research and Reviews.2020;[Epub] CrossRef - How was the Diabetes Metabolism Journal added to MEDLINE?
Hye Jin Yoo
Science Editing.2020; 7(2): 201. CrossRef - Commercial Postural Devices: A Review
Nicole Kah Mun Yoong, Jordan Perring, Ralph Jasper Mobbs
Sensors.2019; 19(23): 5128. CrossRef - Changes in Metabolic Profile Over Time: Impact on the Risk of Diabetes
Yunjung Cho, Seung-Hwan Lee
Diabetes & Metabolism Journal.2019; 43(4): 407. CrossRef - Metformin for prevention or delay of type 2 diabetes mellitus and its associated complications in persons at increased risk for the development of type 2 diabetes mellitus
Kasper S Madsen, Yuan Chi, Maria-Inti Metzendorf, Bernd Richter, Bianca Hemmingsen
Cochrane Database of Systematic Reviews.2019;[Epub] CrossRef
- Estimating insulin sensitivity and β-cell function from the oral glucose tolerance test: validation of a new insulin sensitivity and secretion (ISS) model
- Obesity and Metabolic Syndrome
- Diabetes Prevention in Australia: 10 Years Results and Experience
- James A. Dunbar
- Diabetes Metab J. 2017;41(3):160-167. Published online February 2, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.3.160
- 4,871 View
- 69 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Clinical trials have demonstrated the efficacy of lifestyle modification for the prevention of type 2 diabetes mellitus but it was achieved at higher cost than can be sustained in routine health services. The first clinical trial to report was the Finnish Diabetes Prevention Study. This paper describes how Australia worked with Finnish colleagues to adapt the findings of that study to achieve a statewide diabetes prevention program. Small evaluative, effectiveness trials have been conducted in a number of countries to see if the results of the clinical trials can be replicated in routine health services. The Australian evaluative trial, Greater Green Triangle Diabetes Prevention Program is described in detail to demonstrate the ingredients for success in moving a program from one country to another. Few countries have managed to scale up from evaluative trials to statewide or national programs. The Australian experience is described in detail including lessons learned about what reduced the effectiveness, particularly the need for policy makers in government, people from the implementing organisation and researchers to work together from the start of the evaluative trial and throughout the first 5 years of a national program.
-
Citations
Citations to this article as recorded by- Miscarriage, stillbirth and the risk of diabetes in women: A systematic review and meta-analysis
Qiqi You, Qingqing Jiang, Irakoze Shani, Yiling Lou, Shen Huang, Shiqi Wang, Shiyi Cao
Diabetes Research and Clinical Practice.2023; 195: 110224. CrossRef - A multiple case study of pre-diabetes care undertaken by general practice in Aotearoa/New Zealand: de-incentivised and de-prioritised work
Christine Barthow, Jeremy Krebs, Eileen McKinlay
BMC Primary Care.2023;[Epub] CrossRef - Implementation of a diabetes prevention programme in a multi-ethnic community in primary care in England: An evaluation using constructs from the RE-AIM Framework
Helen Dallosso, Kamlesh Khunti, Laura J. Gray, Kerry Hulley, Mel Ghaly, Naina Patel, Joe Kai, Navneet Aujla, Melanie J. Davies, Tom Yates
Primary Care Diabetes.2023; 17(4): 309. CrossRef - A critical realist exploration of factors influencing engagement in diabetes prevention programs in rural settings
Britney McMullen, Kerith Duncanson, David Schmidt, Clare Collins, Lesley MacDonald-Wicks
Australian Journal of Primary Health.2023; 29(5): 510. CrossRef - Characteristics of participants in the first fully online National Diabetes Prevention Programme: A quantitative survey
Clair Haseldine, Gráinne O'Donoghue, Patricia M Kearney, Fiona Riordan, Margaret Humphreys, Liz Kirby, Sheena McHugh
HRB Open Research.2023; 6: 61. CrossRef - Delivering the Diabetes Remission Clinical Trial (DiRECT) in primary care: Experiences of healthcare professionals
Lucia Rehackova, Roy Taylor, Mike Lean, Alison Barnes, Louise McCombie, George Thom, Naomi Brosnahan, Wilma S. Leslie, Falko F. Sniehotta
Diabetic Medicine.2022;[Epub] CrossRef - It is time for a more targeted approach to prediabetes in primary care in Aotearoa New Zealand
Christine Barthow, Sue Pullon, Eileen McKinlay, Jeremy Krebs, Stokes Tim
Journal of Primary Health Care.2022; 14(4): 372. CrossRef - Implementing a national diabetes prevention programme in England: lessons learned
Jonathan Stokes, Judith Gellatly, Peter Bower, Rachel Meacock, Sarah Cotterill, Matt Sutton, Paul Wilson
BMC Health Services Research.2019;[Epub] CrossRef - How do we identify people at high risk of Type 2 diabetes and help prevent the condition from developing?
J. Fagg, J. Valabhji
Diabetic Medicine.2019; 36(3): 316. CrossRef - Associations between physical activity and cataract treated surgically in patients with diabetes: findings from the 45 and Up Study
Changfan Wu, Xiaotong Han, Xixi Yan, Xianwen Shang, Lei Zhang, Mingguang He
British Journal of Ophthalmology.2019; 103(8): 1099. CrossRef - Usefulness of a Novel Mobile Diabetes Prevention Program Delivery Platform With Human Coaching: 65-Week Observational Follow-Up
Andreas Michaelides, Jennifer Major, Edmund Pienkosz Jr, Meghan Wood, Youngin Kim, Tatiana Toro-Ramos
JMIR mHealth and uHealth.2018; 6(5): e93. CrossRef
- Miscarriage, stillbirth and the risk of diabetes in women: A systematic review and meta-analysis
- Epidemiology
- Relationship between Biological Markers, Metabolic Components, Lifestyles, and Impaired Fasting Glucose in Male Workers
- Tomoyuki Kawada
- Diabetes Metab J. 2015;39(5):434-438. Published online October 22, 2015
- DOI: https://doi.org/10.4093/dmj.2015.39.5.434
- 2,799 View
- 26 Download
- 1 Web of Science
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Confirmation regarding the association between impaired fasting glucose (IFG) and biomarkers in addition to metabolic components and lifestyle factors are required in the occupational filed for preventing diabetes mellitus.
Methods The study was performed in working men aged 30 to 60 years old, who were not taking medication for any metabolic diseases. The author measured the serum levels of high-sensitivity C-reactive protein (CRP), uric acid, and plasma fibrinogen as potential biomarkers of IFG.
Results The mean serum uric acid, log-transformed serum CRP, and plasma fibrinogen levels were higher in the subjects with IFG than in those without IFG. Multivariate analysis revealed significant associations between the presence of IFG and age, log-transformed value of serum CRP, increased waist circumference, hypertension, and hypertriglyceridemia, with odds ratios of 1.1 (95% confidence interval [CI], 1.08 to 1.1;
P <0.001), 1.8 (95% CI, 1.4 to 2.3;P <0.001), 1.3 (95% CI, 1.09 to 1.7;P <0.01), 1.9 (95% CI, 1.6 to 2.3;P <0.001), and 1.3 (95% CI, 1.04 to 1.6;P <0.05), respectively, for the presence of IFG.Conclusion Serum CRP, age, and three metabolic components were associated with IFG. In contrast, there were no significant associations between IFG and lifestyle factors, serum uric acid or plasma fibrinogen.

 KDA
KDA
 First
First Prev
Prev





