
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Search
- Page Path
- HOME > Search
- Technology/Device
- Clinical and Lifestyle Determinants of Continuous Glucose Monitoring Metrics in Insulin-Treated Patients with Type 2 Diabetes Mellitus
- Da Young Lee, Namho Kim, Inha Jung, So Young Park, Ji Hee Yu, Ji A Seo, Jihee Kim, Kyeong Jin Kim, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Sung-Min Park, Nan Hee Kim
- Diabetes Metab J. 2023;47(6):826-836. Published online August 24, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0273

- 1,800 View
- 191 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
There was limited evidence to evaluate the association between lifestyle habits and continuous glucose monitoring (CGM) metrics. Thus, we aimed to depict the behavioral and metabolic determinants of CGM metrics in insulin-treated patients with type 2 diabetes mellitus (T2DM).
Methods
This is a prospective observational study. We analyzed data from 122 insulin-treated patients with T2DM. Participants wore Dexcom G6 and Fitbit, and diet information was identified for 10 days. Multivariate-adjusted logistic regression analysis was performed for the simultaneous achievement of CGM-based targets, defined by the percentage of time in terms of hyper, hypoglycemia and glycemic variability (GV). Intake of macronutrients and fiber, step counts, sleep, postprandial C-peptide-to-glucose ratio (PCGR), information about glucose lowering medications and metabolic factors were added to the analyses. Additionally, we evaluated the impact of the distribution of energy and macronutrient during a day, and snack consumption on CGM metrics.
Results
Logistic regression analysis revealed that female, participants with high PCGR, low glycosylated hemoglobin (HbA1c) and daytime step count had a higher probability of achieving all targets based on CGM (odds ratios [95% confidence intervals] which were 0.24 [0.09 to 0.65], 1.34 [1.03 to 1.25], 0.95 [0.9 to 0.99], and 1.15 [1.03 to 1.29], respectively). And participants who ate snacks showed a shorter period of hyperglycemia and less GV compared to those without.
Conclusion
We confirmed that residual insulin secretion, daytime step count, HbA1c, and women were the most relevant determinants of adequate glycemic control in insulin-treated patients with T2DM. In addition, individuals with snack consumption were exposed to lower times of hyperglycemia and GV. -
Citations
Citations to this article as recorded by- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
Lotte Bogaert, Iris Willems, Patrick Calders, Eveline Dirinck, Manon Kinaupenne, Marga Decraene, Bruno Lapauw, Boyd Strumane, Margot Van Daele, Vera Verbestel, Marieke De Craemer
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2024; 18(4): 102995. CrossRef
- Explanatory variables of objectively measured 24-h movement behaviors in people with prediabetes and type 2 diabetes: A systematic review
- Guideline/Fact Sheet
- Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hypertension
- Jong Han Choi, Jee-Hyun Kang, Suk Chon
- Diabetes Metab J. 2022;46(3):377-390. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0051
- 4,952 View
- 249 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
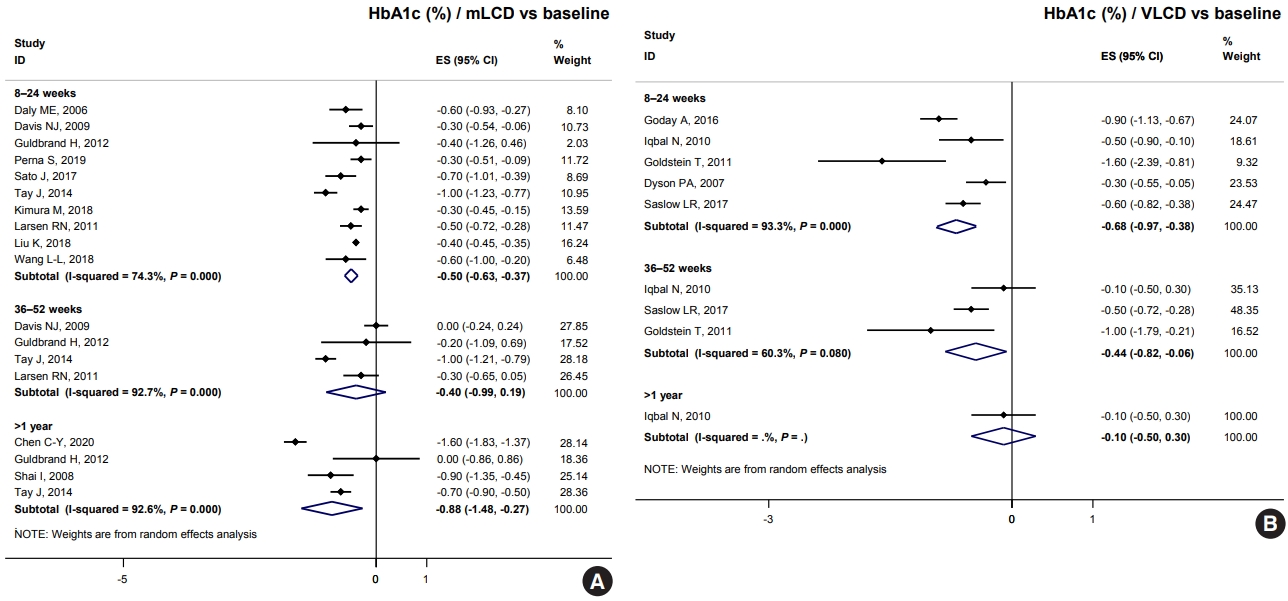
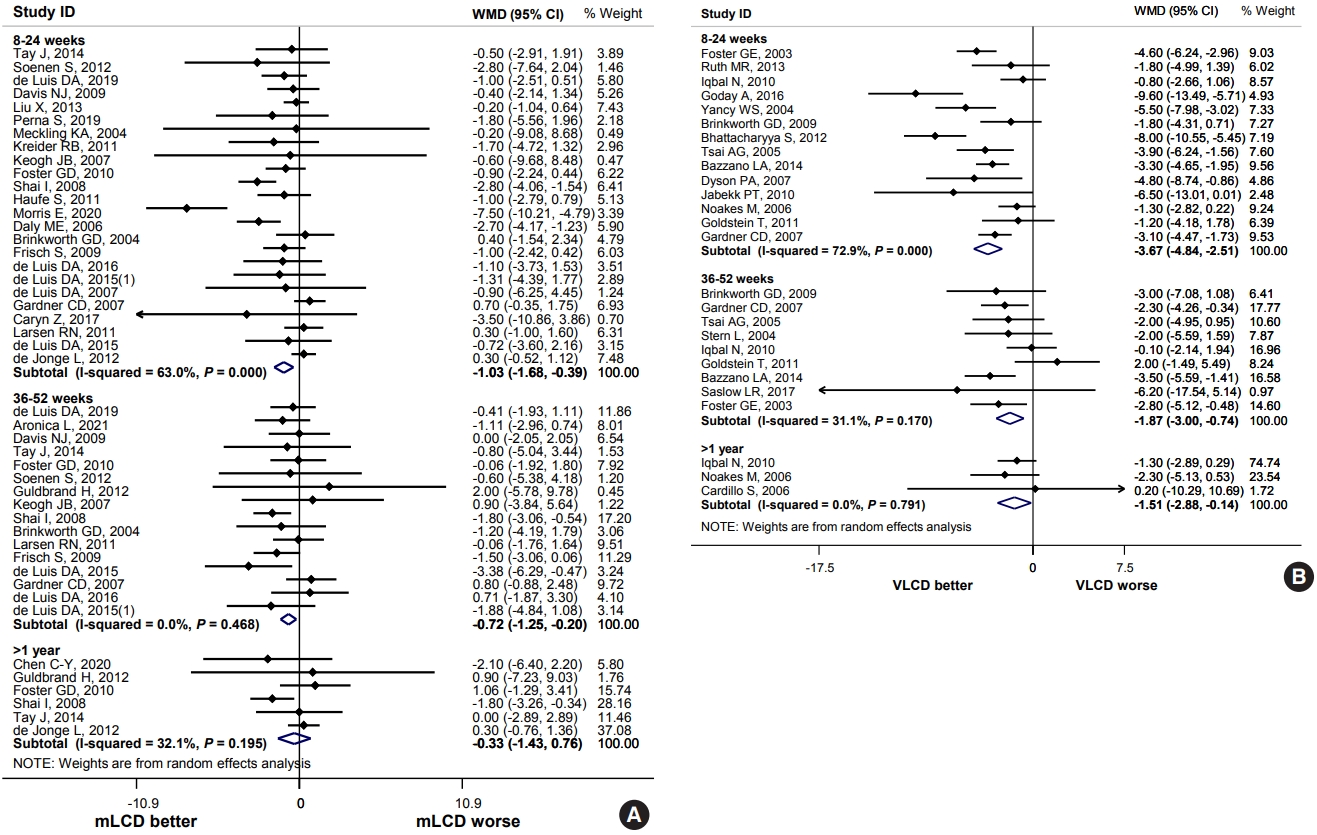
ePub - The Joint Committee of the Korean Diabetes Association, the Korean Society for the Study of Obesity, and the Korean Society of Hypertension announced a consensus statement on carbohydrate-restricted diets and intermittent fasting, representing an emerging and popular dietary pattern. In this statement, we recommend moderately-low-carbohydrate or low-carbohydrate diets, not a very-low-carbohydrate diet, for patients with type 2 diabetes mellitus. These diets can be considered a dietary regimen to improve glycemic control and reduce body weight in adults with type 2 diabetes mellitus. This review provides the detailed results of a meta-analysis and systematic literature review on the potential harms and benefits of carbohydrate-restricted diets in patients with diabetes. We expect that this review will help experts and patients by fostering an in-depth understanding and appropriate application of carbohydrate-restricted diets in the comprehensive management of diabetes.
-
Citations
Citations to this article as recorded by- Efficacy of convenience meal-type foods designed for diabetes in the management of metabolic syndrome based on a 3-week trial
Do Gyeong Lee, In Gyeong Kang, Tae Seok Kim, Yun Ahn, Sang Yun Lee, Hye Jin Ahn, Yoo Kyoung Park
Nutrition.2024; 118: 112287. CrossRef - Long-Term Results of a Digital Diabetes Self-Management and Education Support Program Among Adults With Type 2 Diabetes: A Retrospective Cohort Study
Ashley Berthoumieux, Sarah Linke, Melinda Merry, Alison Megliola, Jessie Juusola, Jenna Napoleone
The Science of Diabetes Self-Management and Care.2024; 50(1): 19. CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef
- Efficacy of convenience meal-type foods designed for diabetes in the management of metabolic syndrome based on a 3-week trial
- Guideline/Fact Sheet
- Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hypertension
- Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim, Committee of Clinical Practice Guidelines, Korean Society for the Study of Obesity (KSSO), Committee of Clinical Practice Guidelines and Committee of Food and Nutrition, Korean Diabetes Association (KDA), Policy Committee of Korean Society of Hypertension (KSH), Policy Development Committee of National Academy of Medicine of Korea (NAMOK)
- Diabetes Metab J. 2022;46(3):355-376. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0038
- 11,020 View
- 588 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Carbohydrate-restricted diets and intermittent fasting (IF) have been rapidly gaining interest among the general population and patients with cardiometabolic disease, such as overweight or obesity, diabetes, and hypertension. However, there are limited expert recommendations for these dietary regimens. This study aimed to evaluate the level of scientific evidence on the benefits and harms of carbohydrate-restricted diets and IF to make responsible recommendations. A meta-analysis and systematic literature review of 66 articles on 50 randomized controlled trials (RCTs) of carbohydrate-restricted diets and 10 articles on eight RCTs of IF was performed. Based on the analysis, the following recommendations are suggested. In adults with overweight or obesity, a moderately-low carbohydrate or low carbohydrate diet (mLCD) can be considered as a dietary regimen for weight reduction. In adults with type 2 diabetes mellitus, mLCD can be considered as a dietary regimen for improving glycemic control and reducing body weight. In contrast, a very-low carbohydrate diet (VLCD) and IF are recommended against in patients with diabetes. Furthermore, no recommendations are suggested for VLCD and IF in adults with overweight or obesity, and carbohydrate-restricted diets and IF in patients with hypertension. Here, we describe the results of our analysis and the evidence for these recommendations.
-
Citations
Citations to this article as recorded by- Metabolic changes with intermittent fasting
Maria G. Lange, Alice A. Coffey, Paul C. Coleman, Thomas M. Barber, Thijs Van Rens, Oyinlola Oyebode, Sally Abbott, Petra Hanson
Journal of Human Nutrition and Dietetics.2024; 37(1): 256. CrossRef - Papel do Jejum Intermitente e da Dieta Restrita em Carboidratos na Prevenção de Doenças Cardiovasculares em Pacientes Pré-Diabéticos
Mohamed Khalfallah, Basma Elnagar, Shaimaa S. Soliman, Ahmad Eissa, Amany Allaithy
Arquivos Brasileiros de Cardiologia.2023;[Epub] CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef - Euglycemic diabetic ketoacidosis development in a patient with type 2 diabetes receiving a sodium-glucose cotransporter-2 inhibitor and a carbohydrate-restricted diet
Gwanpyo Koh, Jisun Bang, Soyeon Yoo, Sang Ah Lee
Journal of Medicine and Life Science.2023; 20(3): 126. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - The Related Metabolic Diseases and Treatments of Obesity
Ming Yang, Shuai Liu, Chunye Zhang
Healthcare.2022; 10(9): 1616. CrossRef - Updated Meta-Analysis of Studies from 2011 to 2021 Comparing the Effectiveness of Intermittent Energy Restriction and Continuous Energy Restriction
Kyoung-Kon Kim, Jee-Hyun Kang, Eun Mi Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(3): 230. CrossRef
- Metabolic changes with intermittent fasting
- Complications
- Peripheral Neuropathy Phenotyping in Rat Models of Type 2 Diabetes Mellitus: Evaluating Uptake of the Neurodiab Guidelines and Identifying Future Directions
- Md Jakir Hossain, Michael D. Kendig, Meg E. Letton, Margaret J. Morris, Ria Arnold
- Diabetes Metab J. 2022;46(2):198-221. Published online March 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0347
- 5,202 View
- 225 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Diabetic peripheral neuropathy (DPN) affects over half of type 2 diabetes mellitus (T2DM) patients, with an urgent need for effective pharmacotherapies. While many rat and mouse models of T2DM exist, the phenotyping of DPN has been challenging with inconsistencies across laboratories. To better characterize DPN in rodents, a consensus guideline was published in 2014 to accelerate the translation of preclinical findings. Here we review DPN phenotyping in rat models of T2DM against the ‘Neurodiab’ criteria to identify uptake of the guidelines and discuss how DPN phenotypes differ between models and according to diabetes duration and sex. A search of PubMed, Scopus and Web of Science databases identified 125 studies, categorised as either diet and/or chemically induced models or transgenic/spontaneous models of T2DM. The use of diet and chemically induced T2DM models has exceeded that of transgenic models in recent years, and the introduction of the Neurodiab guidelines has not appreciably increased the number of studies assessing all key DPN endpoints. Combined high-fat diet and low dose streptozotocin rat models are the most frequently used and well characterised. Overall, we recommend adherence to Neurodiab guidelines for creating better animal models of DPN to accelerate translation and drug development.
-
Citations
Citations to this article as recorded by- SIRT3 alleviates painful diabetic neuropathy by mediating the FoxO3a‐PINK1‐Parkin signaling pathway to activate mitophagy
Jing Yang, Zhuoying Yu, Ye Jiang, Zixian Zhang, Yue Tian, Jie Cai, Min Wei, Yanhan Lyu, Dongsheng Yang, Shixiong Shen, Guo‐Gang Xing, Min Li
CNS Neuroscience & Therapeutics.2024;[Epub] CrossRef - Compound Qiying Granules alleviates diabetic peripheral neuropathy by inhibiting endoplasmic reticulum stress and apoptosis
Yan Hu, Chen Chen, Zhengting Liang, Tao Liu, Xiaoling Hu, Guanying Wang, Jinxia Hu, Xiaolin Xie, Zhiyan Liu
Molecular Medicine.2023;[Epub] CrossRef - HCV affects KATP channels through GnT-IVa-mediated N-glycosylation of GLUT2 on the surface of pancreatic β-cells leading to impaired insulin secretion
Ben Niu, Lijing Ma, Lixuan Yao, Yating Zhang, Heng Su
Endocrine.2023;[Epub] CrossRef - Multimodal Comparison of Diabetic Neuropathy in Aged Streptozotocin-Treated Sprague–Dawley and Zucker Diabetic Fatty Rats
Annalisa Canta, Valentina A. Carozzi, Alessia Chiorazzi, Cristina Meregalli, Norberto Oggioni, Virginia Rodriguez-Menendez, Barbara Sala, Roberto Cosimo Melcangi, Silvia Giatti, Raffaella Lombardi, Roberto Bianchi, Paola Marmiroli, Guido Cavaletti
Biomedicines.2022; 11(1): 20. CrossRef
- SIRT3 alleviates painful diabetic neuropathy by mediating the FoxO3a‐PINK1‐Parkin signaling pathway to activate mitophagy
- Pathophysiology
- Rho-Kinase as a Therapeutic Target for Nonalcoholic Fatty Liver Diseases
- Inês Sousa-Lima, Hyun Jeong Kim, John Jones, Young-Bum Kim
- Diabetes Metab J. 2021;45(5):655-674. Published online September 30, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0197
- 5,782 View
- 171 Download
- 7 Web of Science
- 7 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 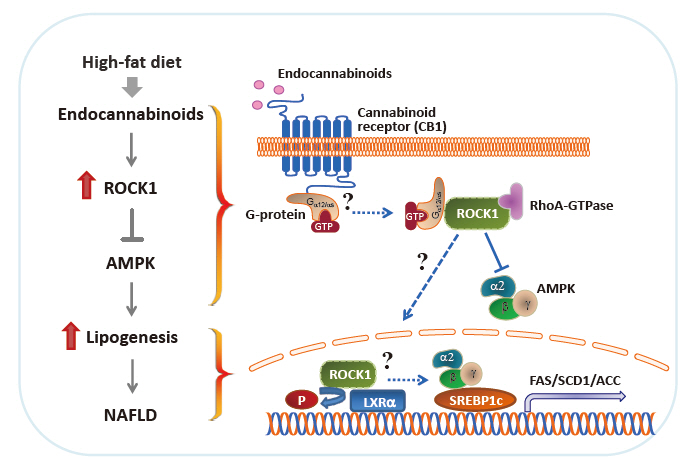
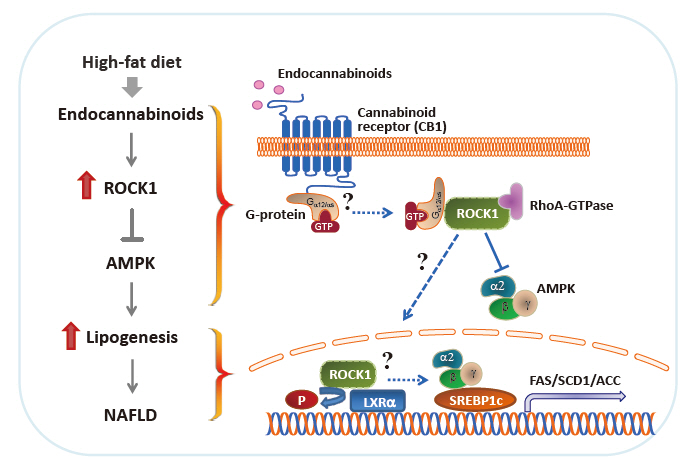
- Nonalcoholic fatty liver disease (NAFLD) is a major public health problem and the most common form of chronic liver disease, affecting 25% of the global population. Although NAFLD is closely linked with obesity, insulin resistance, and type 2 diabetes mellitus, knowledge on its pathogenesis remains incomplete. Emerging data have underscored the importance of Rho-kinase (Rho-associated coiled-coil-containing kinase [ROCK]) action in the maintenance of normal hepatic lipid homeostasis. In particular, pharmacological blockade of ROCK in hepatocytes or hepatic stellate cells prevents the progression of liver diseases such as NAFLD and fibrosis. Moreover, mice lacking hepatic ROCK1 are protected against obesity-induced fatty liver diseases by suppressing hepatic de novo lipogenesis. Here we review the roles of ROCK as an indispensable regulator of obesity-induced fatty liver disease and highlight the key cellular pathway governing hepatic lipid accumulation, with focus on de novo lipogenesis and its impact on therapeutic potential. Consequently, a comprehensive understanding of the metabolic milieu linking to liver dysfunction triggered by ROCK activation may help identify new targets for treating fatty liver diseases such as NAFLD.
-
Citations
Citations to this article as recorded by- THE ROLE OF N6-METHYLADENOSINE METHYLTRANSFERASE RBM15 IN NONALCOHOLIC FATTY LIVER DISEASE
Shiqing Li, Shengyi Lian, Wei Cheng, Tao Zhang, Xiaobing Gong
Shock.2024; 61(2): 311. CrossRef - Exploring the potential of drug repurposing for liver diseases: A comprehensive study
Fares E.M. Ali, Mustafa Ahmed Abdel-Reheim, Emad H.M. Hassanein, Mostafa K. Abd El-Aziz, Hanan S. Althagafy, Khalid S.A. Badran
Life Sciences.2024; : 122642. CrossRef - Targeting of G-protein coupled receptor 40 alleviates airway hyperresponsiveness through RhoA/ROCK1 signaling pathway in obese asthmatic mice
Xixi Lin, Like Wang, Xiaojie Lu, Yuanyuan Zhang, Rongying Zheng, Ruijie Chen, Weixi Zhang
Respiratory Research.2023;[Epub] CrossRef - Selectivity matters: selective ROCK2 inhibitor ameliorates established liver fibrosis via targeting inflammation, fibrosis, and metabolism
Alexandra Zanin-Zhorov, Wei Chen, Julien Moretti, Melanie S. Nyuydzefe, Iris Zhorov, Rashmi Munshi, Malavika Ghosh, Cindy Serdjebi, Kelli MacDonald, Bruce R. Blazar, Melissa Palmer, Samuel D. Waksal
Communications Biology.2023;[Epub] CrossRef - Insight Into Rho Kinase Isoforms in Obesity and Energy Homeostasis
Lei Wei, Jianjian Shi
Frontiers in Endocrinology.2022;[Epub] CrossRef - Paeoniflorin alleviates liver injury in hypercholesterolemic rats through the ROCK/AMPK pathway
Tong Liu, Ning Zhang, Lingya Kong, Sijie Chu, Ting Zhang, Guangdi Yan, Donglai Ma, Jun Dai, Zhihong Ma
Frontiers in Pharmacology.2022;[Epub] CrossRef - Fasudil Increased the Sensitivity to Gefitinib in NSCLC by Decreasing Intracellular Lipid Accumulation
Tingting Liao, Jingjing Deng, Wenjuan Chen, Juanjuan Xu, Guanghai Yang, Mei Zhou, Zhilei Lv, Sufei Wang, Siwei Song, Xueyun Tan, Zhengrong Yin, Yumei Li, Yang Jin
Cancers.2022; 14(19): 4709. CrossRef
- THE ROLE OF N6-METHYLADENOSINE METHYLTRANSFERASE RBM15 IN NONALCOHOLIC FATTY LIVER DISEASE
- Basic Research
- Carnitine Orotate Complex Ameliorates Insulin Resistance and Hepatic Steatosis Through Carnitine Acetyltransferase Pathway
- Jung-Hee Hong, Moon-Kyu Lee
- Diabetes Metab J. 2021;45(6):933-947. Published online August 19, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0223
- 5,790 View
- 167 Download
- 3 Web of Science
- 3 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 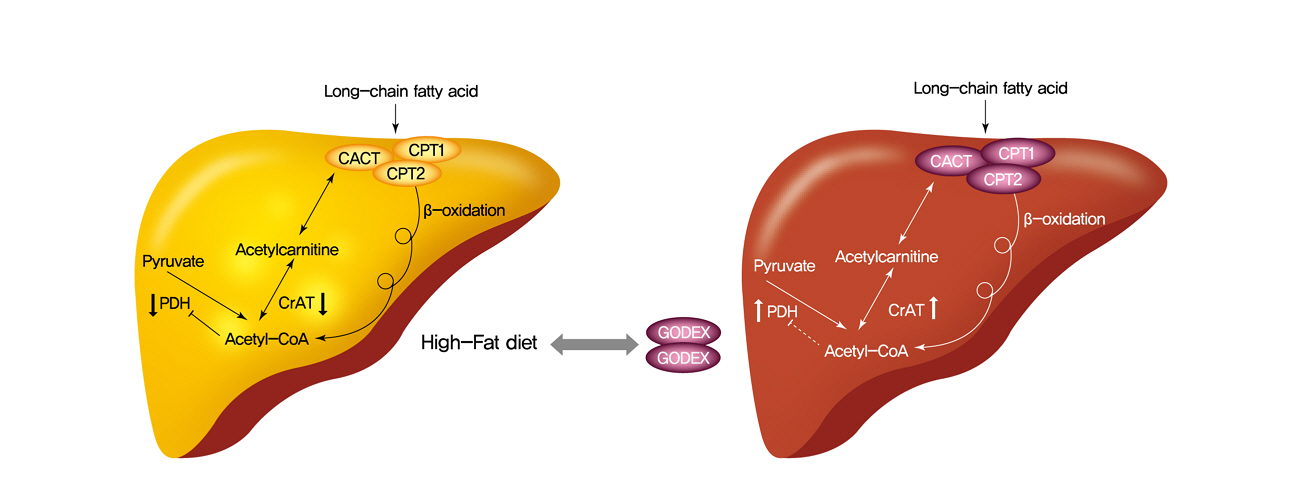
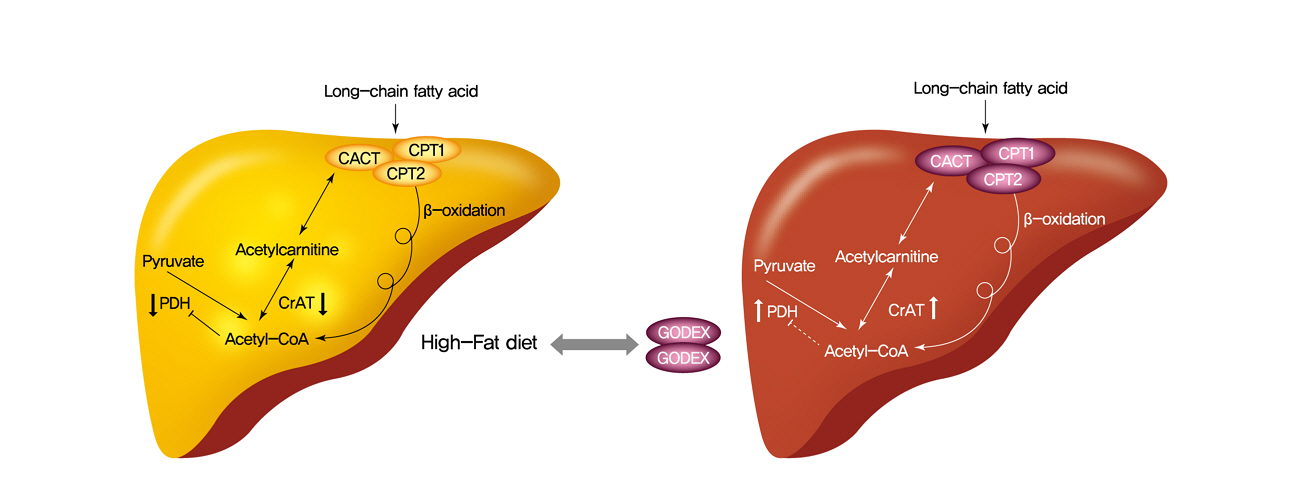
- Background
Carnitine orotate complex (Godex) has been shown to decrease glycated hemoglobin levels and improve steatosis in patients with type 2 diabetes mellitus with non-alcoholic fatty liver disease. However, the mechanisms of Godex in glucose metabolism remain unclear.
Methods
Male C57BL/6J mice were divided into four groups: normal-fat diet, high-fat diet, a high-fat diet supplemented with intraperitoneal injection of (500 mg or 2,000 mg/kg/day) Godex for 8 weeks. Computed tomography, indirect calorimetry, and histological analyses including electron microscopy of the liver were performed, and biochemical profiles and oral glucose tolerance test and insulin tolerance test were undertaken. Expressions of genes in the lipid and glucose metabolism, activities of oxidative phosphorylation enzymes, carnitine acetyltransferase, pyruvate dehydrogenase, and acetyl-coenzyme A (CoA)/CoA ratio were evaluated.
Results
Godex improved insulin sensitivity and significantly decreased fasting plasma glucose, homeostatic model assessment for insulin resistance, steatosis, and gluconeogenesis, with a marked increase in fatty acid oxidation as well as better use of glucose in high-fat diet-fed mice. It preserved mitochondrial function and ultrastructure, restored oxidative phosphorylation enzyme activities, decreased acetyl-CoA/CoA ratio, and increased carnitine acetyltransferase content and pyruvate dehydrogenase activity. Carnitine acetyltransferase knockdown partially reversed the effects of Godex in liver and in vitro.
Conclusion
Godex improved insulin resistance and steatosis by regulating carnitine acetyltransferase in liver in high-fat diet-fed mice. -
Citations
Citations to this article as recorded by- Impact of l-Carnitine Supplementation on Liver Enzyme Normalization in Patients with Chronic Liver Disease: A Meta-Analysis of Randomized Trials
Hyunwoo Oh, Chan Hyuk Park, Dae Won Jun
Journal of Personalized Medicine.2022; 12(7): 1053. CrossRef - Prolonged Use of Carnitine-Orotate Complex (Godex®) Is Associated with Improved Mortality: A Nationwide Cohort Study
Kye-Yeung Park, Sangmo Hong, Kyung-Soo Kim, Kyungdo Han, Cheol-Young Park
Journal of Personalized Medicine.2022; 12(12): 1970. CrossRef - The Role of Carnitine Orotate Complex in Fatty Liver
Hyon-Seung Yi
Diabetes & Metabolism Journal.2021; 45(6): 866. CrossRef
- Impact of l-Carnitine Supplementation on Liver Enzyme Normalization in Patients with Chronic Liver Disease: A Meta-Analysis of Randomized Trials
- Metabolic Risk/Epidemiology
- Trends and Risk Factors of Metabolic Syndrome among Korean Adolescents, 2007 to 2018
- Jiun Chae, Moon Young Seo, Shin-Hye Kim, Mi Jung Park
- Diabetes Metab J. 2021;45(6):880-889. Published online July 6, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0185
- 5,870 View
- 239 Download
- 15 Web of Science
- 16 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub 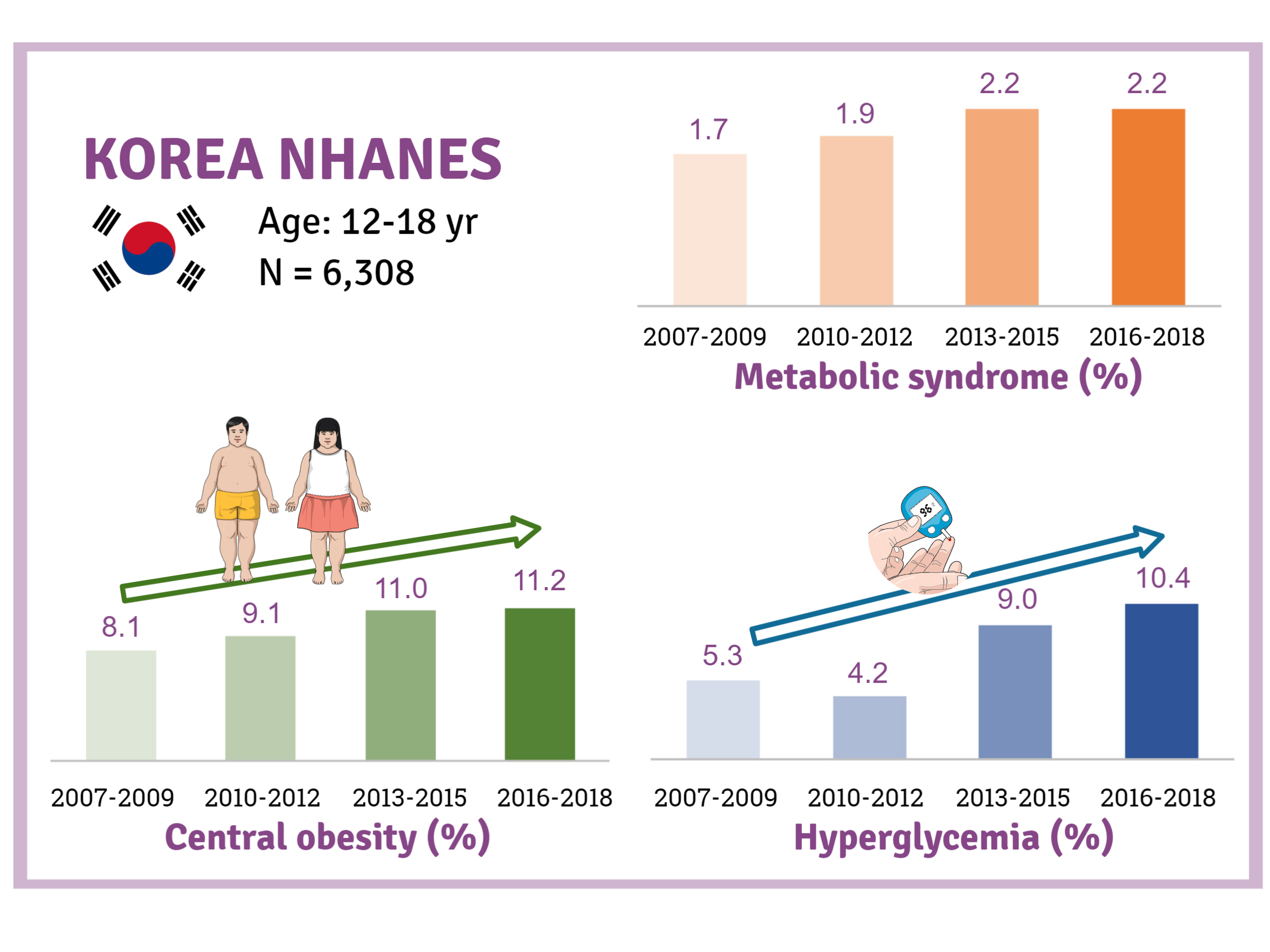
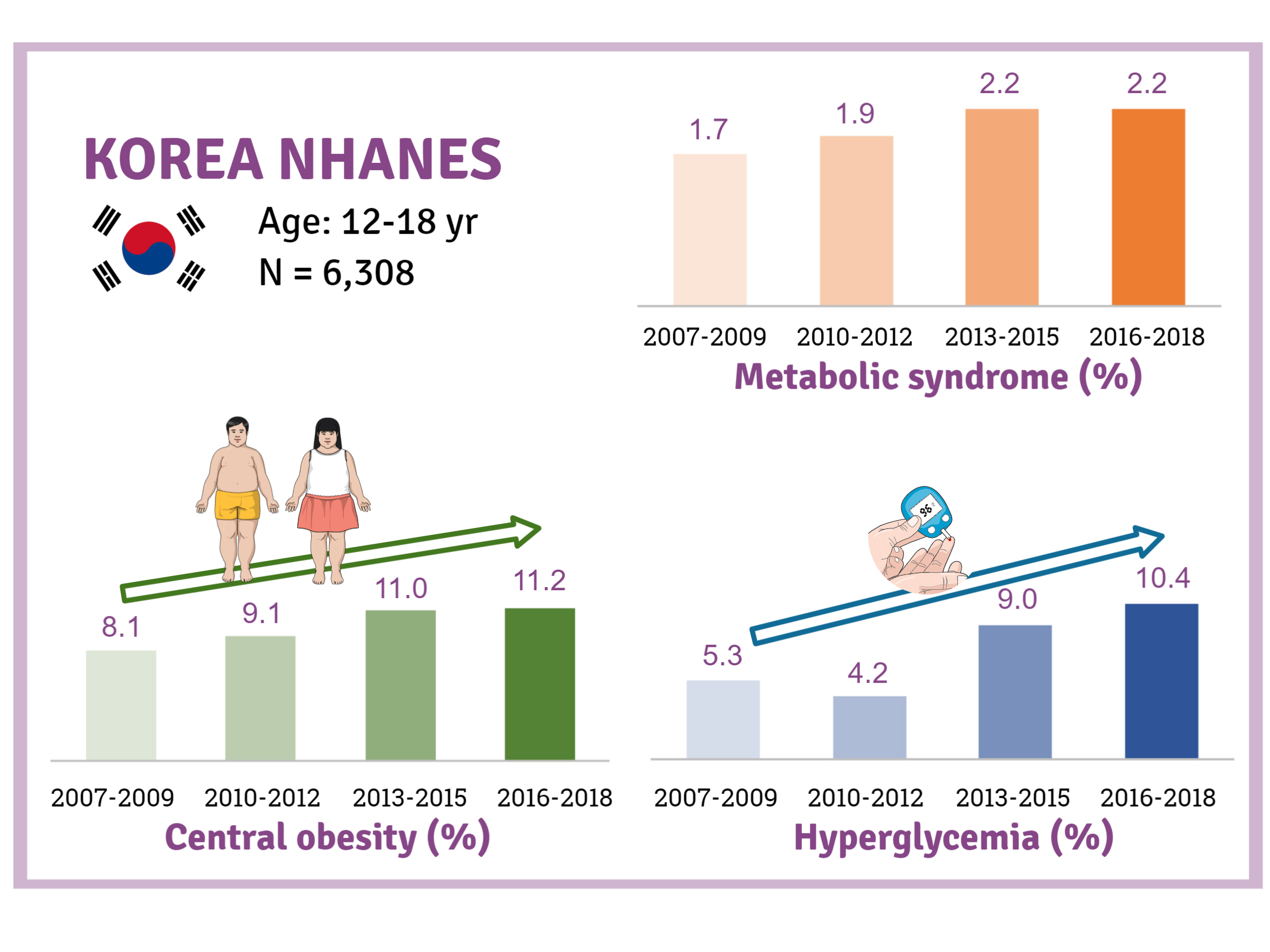
- Background
There is a lack of recent research on the changes in risk factors for metabolic syndrome (MetS) in the Asian pediatric population. We aimed to determine the 12-year trends in the prevalence of MetS and relevant lifestyle factors such as smoking, exercise, and calorie intake among Korean adolescents.
Methods
We investigated trends in MetS and lifestyle factors among 6,308 adolescents aged 12 to 18 years from the Korea National Health and Nutrition Examination Survey, 2007 to 2018.
Results
The prevalence of MetS was stable from 2007 to 2018 (1.7% to 2.2%). There were significant increases in the prevalence of central obesity (from 8.1% to 11.2%, P=0.012) and hyperglycemia (from 5.3% to 10.4%, P<0.001) and decreases in hypo-high-density lipoprotein (HDL)-cholesterolemia (from 22.4% to 14.8%, P<0.001). Total calorie intake and calorie intake from fat significantly increased (P<0.001), whereas calorie intake from carbohydrates significantly decreased (P<0.001) during the study period. The proportions of tobacco smokers and regular walkers significantly decreased from 2007 to 2018. After controlling for all covariates, total calorie intake was positively correlated with waist circumference (P<0.05). HDL-cholesterol was negatively associated with carbohydrate consumption (P<0.01) and positively associated with fat consumption (P<0.001). Regular walking and regular strength training were associated with lower waist circumference (P<0.05). Smoking was associated with lower fasting glucose levels (P<0.01).
Conclusion
Although the prevalence rate of MetS is stable among Korean adolescents, the prevalence of central obesity and hyperglycemia has increased greatly in the recent decade. Public education on proper dietary intake and lifestyle modification is required. -
Citations
Citations to this article as recorded by- Impact of Overseas Deployment on Fatty Liver and Metabolic Diseases Among Korean Soldiers
Chang In Han, Jaejun Lee
Military Medicine.2024;[Epub] CrossRef - The impacts of dietary sphingomyelin supplementation on metabolic parameters of healthy adults: a systematic review and meta-analysis of randomized controlled trials
Chen-Zi Li, Li-Mei Wu, Chen-Xi Zhu, Huan-Yu Du, Guo-Xun Chen, Fang Yang
Frontiers in Nutrition.2024;[Epub] CrossRef - Association between Thyroid Function and Insulin Resistance Indices in Korean Adolescents: Findings from the 2014–2015 Korea National Health and Nutrition Examination Survey
Eunji Mun, Hye Ah Lee, Jung Eun Choi, Rosie Lee, Kyung Hee Kim, Hyesook Park, Hae Soon Kim
Children.2024; 11(3): 370. CrossRef - Ongoing increasing trends in central precocious puberty incidence among Korean boys and girls from 2008 to 2020
Sinyoung Kang, Mi Jung Park, Jung Min Kim, Jin-Sung Yuk, Shin-Hye Kim, Jun Mori
PLOS ONE.2023; 18(3): e0283510. CrossRef - The association between urinary cotinine level and metabolic syndrome profiles among adolescents: findings from the Ewha Birth and growth study
Hyunjin Park, Ui-Jeong Kim, Eun Jeong Choi, Seunghee Jun, Bomi Park, Hye Ah Lee, Hae Soon Kim, Hyesook Park
BMC Public Health.2023;[Epub] CrossRef - Artificial Intelligence-Based Speech Analysis System for Medical Support
Eui-Sun Kim, Dong Jin Shin, Sung Tae Cho, Kyung Jin Chung
International Neurourology Journal.2023; 27(2): 99. CrossRef - The effect of hypothalamic involvement and growth hormone treatment on cardiovascular risk factors during the transition period in patients with childhood-onset craniopharyngioma
Sang Hee Park, Yun Jeong Lee, Jung-Eun Cheon, Choong Ho Shin, Hae Woon Jung, Young Ah Lee
Annals of Pediatric Endocrinology & Metabolism.2023; 28(2): 107. CrossRef - Increase of Prevalence of Obesity and Metabolic Syndrome in Children and Adolescents in Korea during the COVID-19 Pandemic: A Cross-Sectional Study Using the KNHANES
Jung Eun Choi, Hye Ah Lee, Sung Won Park, Jung Won Lee, Ji Hyen Lee, Hyesook Park, Hae Soon Kim
Children.2023; 10(7): 1105. CrossRef - The Prevalence of Abdominal Obesity and Metabolic Syndrome in Korean Children and Adolescents
Ja Hyang Cho
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 103. CrossRef - Temporal Trends of the Prevalence of Abdominal Obesity and Metabolic Syndrome in Korean Children and Adolescents between 2007 and 2020
Jieun Lee, Sung-Chan Kang, Obin Kwon, Seung-sik Hwang, Jin Soo Moon, Hyun Wook Chae, Jaehyun Kim
Journal of Obesity & Metabolic Syndrome.2023; 32(2): 170. CrossRef - Changes in the Number of Children and Adolescents with Complex Chronic Conditions and Medical Spending: Analyzing National Health Insurance Claims Data from 2011 to 2021
Jeong-Yoon Oh, Su-Jin Cho, Jin-Seon Jung, Jin-Suk Cho, Choon-Seon Park
Health Insurance Review & Assessment Service Research.2023; 3(2): 155. CrossRef - Trends and Risk Factors of Metabolic Syndrome among Korean Adolescents, 2007 to 2018 (Diabetes Metab J 2021;45:880-9)
Dae Jung Kim
Diabetes & Metabolism Journal.2022; 46(2): 349. CrossRef - Trends and Risk Factors of Metabolic Syndrome among Korean Adolescents, 2007 to 2018 (Diabetes Metab J 2021;45:880-9)
Jiun Chae, Moon Young Seo, Shin-Hye Kim, Mi Jung Park
Diabetes & Metabolism Journal.2022; 46(2): 351. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - Environmental polycyclic aromatic hydrocarbon exposure in relation to metabolic syndrome in US adults
Xue Yang, Qingping Xue, Ying Wen, Yichao Huang, Yi Wang, Gaga Mahai, Tong Yan, Yanjun Liu, Tao Rong, Yixin Wang, Da Chen, Shuqin Zeng, Chun-Xia Yang, Xiong-Fei Pan
Science of The Total Environment.2022; 840: 156673. CrossRef - Commentary on "Single point insulin sensitivity estimator for predicting type 2 diabetes mellitus in obese adolescents"
Shin-Hye Kim
Annals of Pediatric Endocrinology & Metabolism.2022; 27(3): 155. CrossRef
- Impact of Overseas Deployment on Fatty Liver and Metabolic Diseases Among Korean Soldiers
- Basic Research
-
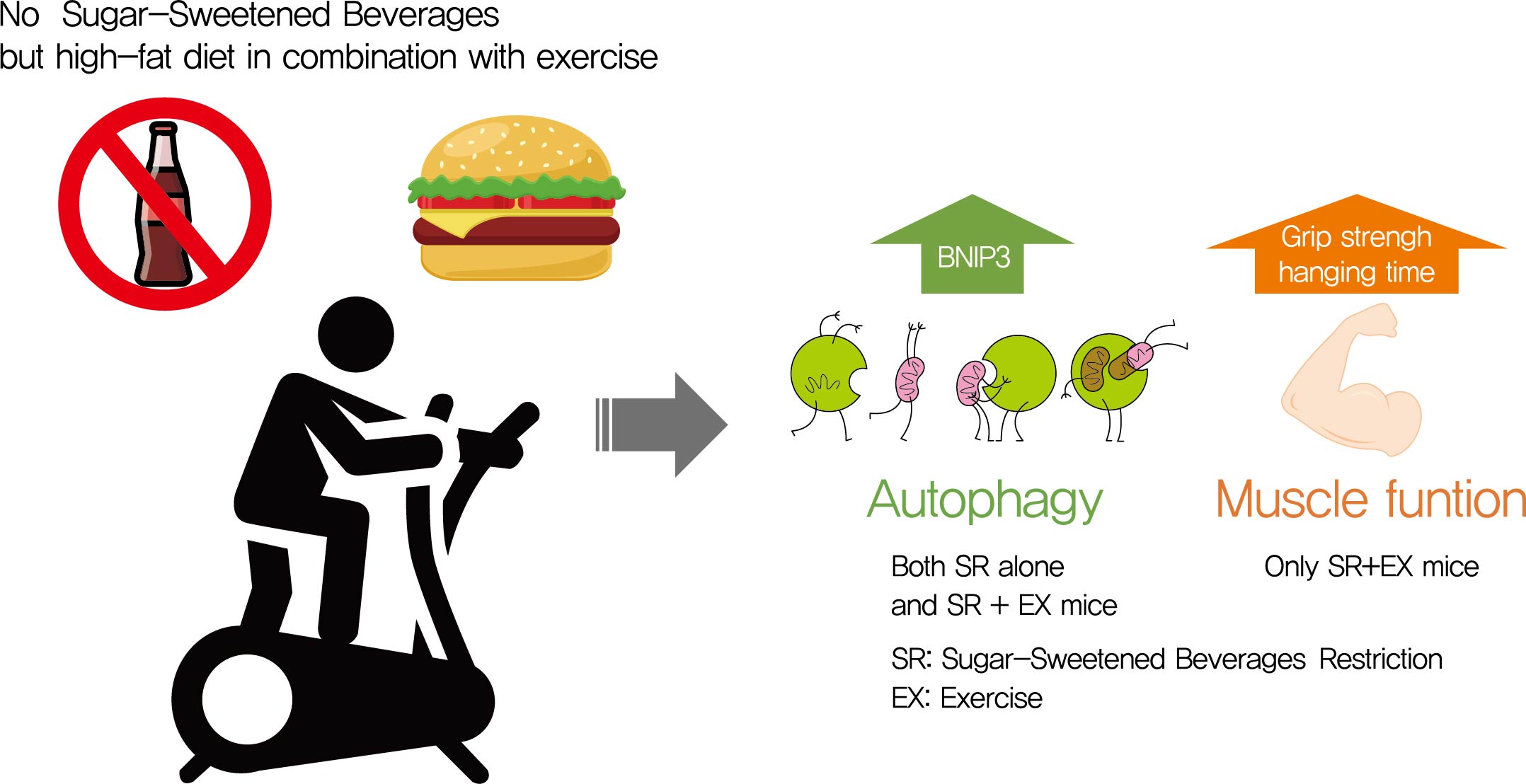
- The Effects of Exercise and Restriction of Sugar-Sweetened Beverages on Muscle Function and Autophagy Regulation in High-Fat High-Sucrose-Fed Obesity Mice
- Didi Zhang, Ji Hyun Lee, Hyung Eun Shin, Seong Eun Kwak, Jun Hyun Bae, Liang Tang, Wook Song
- Diabetes Metab J. 2021;45(5):773-786. Published online March 25, 2021
- DOI: https://doi.org/10.4093/dmj.2020.0157
- 7,091 View
- 252 Download
- 5 Web of Science
- 6 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 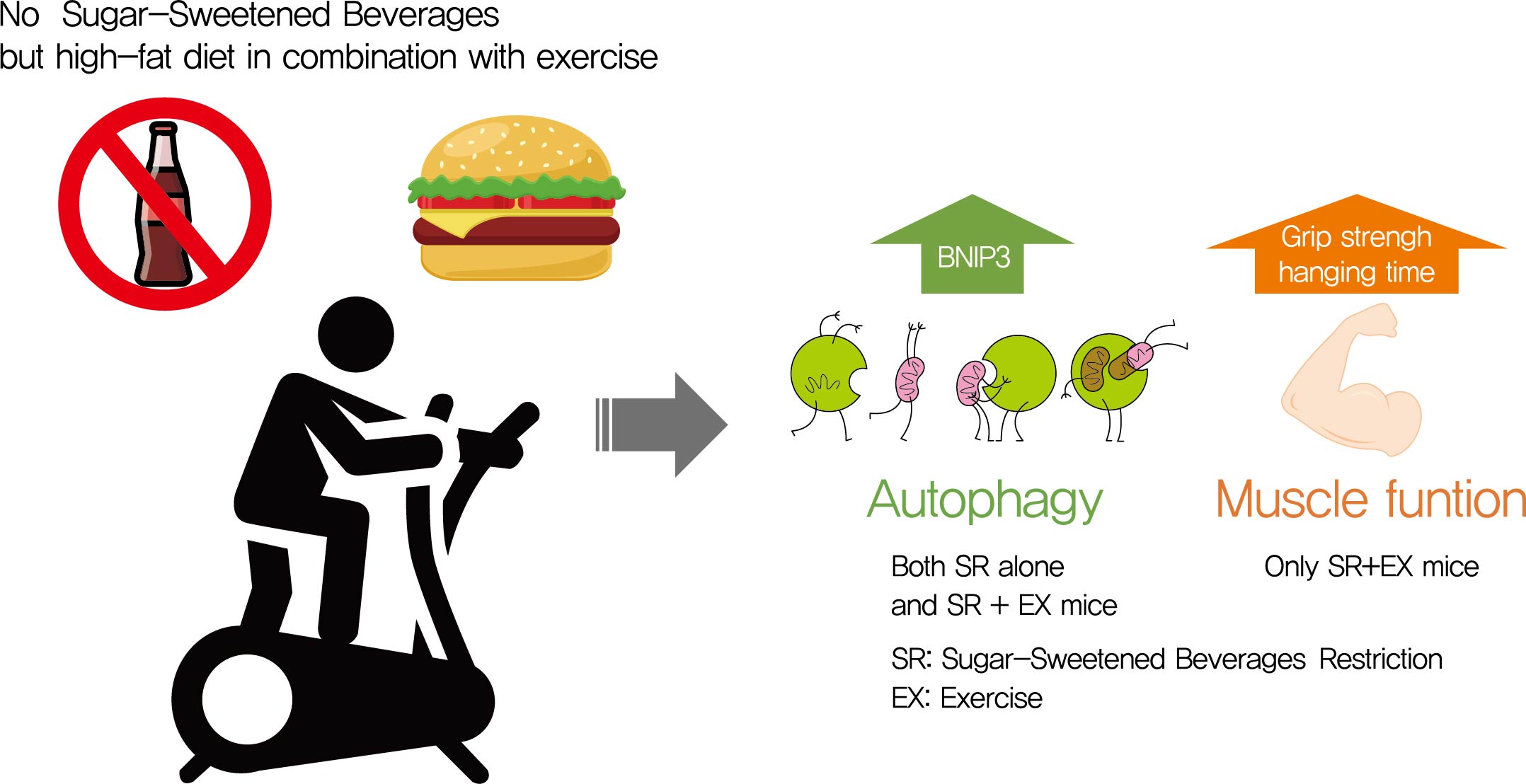
- Background
Autophagy maintains muscle mass and healthy skeletal muscles. Several recent studies have associated sugar-sweetened beverage (SSB) consumption with diseases. We investigated whether muscle dysfunction due to obesity could be restored by SSB restriction (SR) alone or in combination with exercise (EX) training.
Methods
Obese mice were subjected to SR combined with treadmill EX. Intraperitoneal glucose tolerance test, grip strength test, hanging time test, and body composition analysis were performed. Triglyceride (TG) and total cholesterol (TC) serum concentrations and TG concentrations in quadriceps muscles were analyzed. Western blot and reverse transcription-quantitative polymerase chain reaction helped analyze autophagy-related protein and mRNA expression, respectively.
Results
SR alone had no significant effect on fasting blood glucose levels, glucose tolerance, and muscle function. However, it had effect on serum TC, serum TG, and BCL2 interacting protein 3 expression. SR+EX improved glucose tolerance and muscle function and increased serum TC utilization than SR alone. SR+EX reduced P62 levels, increased glucose transporter type 4 and peroxisome proliferator-activated receptor γ coactivator-1α protein expression, and improved grip strength relative to the high-fat and high-sucrose liquid (HFHS) group, and this was not observed in the HFHS+EX group.
Conclusion
SR induced mitophagy-related protein expression in quadriceps, without affecting muscle function. And, the combination of SR and EX activated mitophagy-related proteins and improved muscle function. -
Citations
Citations to this article as recorded by- Mitochondrial Dysfunction, Oxidative Stress, and Inter-Organ Miscommunications in T2D Progression
Rajakrishnan Veluthakal, Diana Esparza, Joseph M. Hoolachan, Rekha Balakrishnan, Miwon Ahn, Eunjin Oh, Chathurani S. Jayasena, Debbie C. Thurmond
International Journal of Molecular Sciences.2024; 25(3): 1504. CrossRef - The association between healthy beverage index and sarcopenia in Iranian older adults: a case-control study
Marzieh Mahmoodi, Zainab Shateri, Mehran Nouri, Mohebat Vali, Nasrin Nasimi, Zahra Sohrabi, Mohammad Hossein Dabbaghmanesh, Maede Makhtoomi
BMC Geriatrics.2024;[Epub] CrossRef - Interplay of skeletal muscle and adipose tissue: sarcopenic obesity
Min Jeong Park, Kyung Mook Choi
Metabolism.2023; 144: 155577. CrossRef - Association between sugar-sweetened beverage consumption frequency and muscle strength: results from a sample of Chinese adolescents
Yunjie Zhang, Pan Xu, Yongjing Song, Nan Ma, Jinkui Lu
BMC Public Health.2023;[Epub] CrossRef - Muscle strength and prediabetes progression and regression in middle‐aged and older adults: a prospective cohort study
Shanhu Qiu, Xue Cai, Yang Yuan, Bo Xie, Zilin Sun, Duolao Wang, Tongzhi Wu
Journal of Cachexia, Sarcopenia and Muscle.2022; 13(2): 909. CrossRef - INTENSITY OF FREE RADICAL PROCESSES IN RAT SKELETAL MUSCLES UNDER THE CONDITIONS OF DIFFERENT DIETARY SUPPLY WITH NUTRIENTS
O.M. Voloshchuk, Н.P. Kopylchuk
Fiziolohichnyĭ zhurnal.2022; 68(4): 48. CrossRef
- Mitochondrial Dysfunction, Oxidative Stress, and Inter-Organ Miscommunications in T2D Progression
- Metabolic Risk/Epidemiology
- A Vegetable Dietary Pattern Is Associated with Lowered Risk of Gestational Diabetes Mellitus in Chinese Women
- Qiong Chen, Weiwei Wu, Hailan Yang, Ping Zhang, Yongliang Feng, Keke Wang, Ying Wang, Suping Wang, Yawei Zhang
- Diabetes Metab J. 2020;44(6):887-896. Published online September 11, 2020
- DOI: https://doi.org/10.4093/dmj.2019.0138
- 6,567 View
- 135 Download
- 10 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Identification of modifiable dietary factors, which are involved in the development of gestational diabetes mellitus (GDM), could inform strategies to prevent GDM.
Methods
We examined the dietary patterns in a Chinese population and evaluated their relationship with GDM risk using a case-control study including 1,464 cases and 8,092 control subjects. Propensity score matching was used to reduce the imbalance of covariates between cases and controls. Dietary patterns were identified using factor analysis while their associations with GDM risk were evaluated using logistic regression models.
Results
A “vegetable” dietary pattern was characterized as the consumption of green leafy vegetables (Chinese little greens and bean seedling), other vegetables (cabbages, carrots, tomatoes, eggplants, potatoes, mushrooms, peppers, bamboo shoots, agarics, and garlic), and bean products (soybean milk, tofu, kidney beans, and cowpea). For every quartile increase in the vegetables factor score during 1 year prior to conception, the first trimester, and the second trimester of pregnancy, the GDM risk lowered by 6% (odds ratio [OR], 0.94; 95% confidence interval [CI], 0.89 to 0.99), 7% (OR, 0.94; 95% CI, 0.88 to 0.99), and 9% (OR, 0.91; 95% CI, 0.86 to 0.96).
Conclusion
In conclusion, our study suggests that the vegetable dietary pattern is associated with lower GDM risk; however, the interpretation of the result should with caution due to the limitations in our study, and additional studies are necessary to explore the underlying mechanism of this relationship. -
Citations
Citations to this article as recorded by- Maternal dietary components in the development of gestational diabetes mellitus: a systematic review of observational studies to timely promotion of health
Victoria Lambert, Sonia Edith Muñoz, Carla Gil, María Dolores Román
Nutrition Journal.2023;[Epub] CrossRef - Fruit, vegetable, and fruit juice consumption and risk of gestational diabetes mellitus: a systematic review and meta-analysis
Yan-Ping Liao, Qing-Xiang Zheng, Xiu-Min Jiang, Xiao-Qian Chen, Xiao-Xia Gao, Yu-Qing Pan
Nutrition Journal.2023;[Epub] CrossRef - The effects of plant-based dietary patterns on the risk of developing gestational diabetes mellitus: A systematic review and meta-analysis
Yu Zhu, QingXiang Zheng, Ling Huang, XiuMin Jiang, XiaoXia Gao, JiaNing Li, RuLin Liu, Kent Lai
PLOS ONE.2023; 18(10): e0291732. CrossRef - Molecular pathways and nutrigenomic review of insulin resistance development in gestational diabetes mellitus
Patricia Guevara-Ramírez, Elius Paz-Cruz, Santiago Cadena-Ullauri, Viviana A. Ruiz-Pozo, Rafael Tamayo-Trujillo, Maria L. Felix, Daniel Simancas-Racines, Ana Karina Zambrano
Frontiers in Nutrition.2023;[Epub] CrossRef - Effectiveness of pre-pregnancy lifestyle in preventing gestational diabetes mellitus—a systematic review and meta-analysis of 257,876 pregnancies
Swetha Sampathkumar, Durga Parkhi, Yonas Ghebremichael-Weldeselassie, Nithya Sukumar, Ponnusamy Saravanan
Nutrition & Diabetes.2023;[Epub] CrossRef - Gestational Diabetes Mellitus: The Crosslink among Inflammation, Nitroxidative Stress, Intestinal Microbiota and Alternative Therapies
Elaine Luiza Santos Soares de Mendonça, Marilene Brandão Tenório Fragoso, Jerusa Maria de Oliveira, Jadriane Almeida Xavier, Marília Oliveira Fonseca Goulart, Alane Cabral Menezes de Oliveira
Antioxidants.2022; 11(1): 129. CrossRef - Ferulic acid targets ACSL1 to ameliorate lipid metabolic disorders in db/db mice
Jie Gao, Xue Gu, Manqian Zhang, Xingwang Zu, Fukui Shen, Xiaotao Hou, Erwei Hao, Gang Bai
Journal of Functional Foods.2022; 91: 105009. CrossRef - Effect of dietary pattern on pregnant women with gestational diabetes mellitus and its clinical significance
Jianping Wang, Zuoliang Xie, Peipei Chen, Yuhuan Wang, Baoqing Li, Fen Dai
Open Life Sciences.2022; 17(1): 202. CrossRef - Dietary Protein Patterns during Pregnancy Are Associated with Risk of Gestational Diabetes Mellitus in Chinese Pregnant Women
Weijia Wu, Nu Tang, Jingjing Zeng, Jin Jing, Li Cai
Nutrients.2022; 14(8): 1623. CrossRef - Dietary Acid Load Is Positively Associated With Risk of Gestational Diabetes Mellitus in a Prospective Cohort of Chinese Pregnant Women
Rui Zhao, Leilei Zhou, Gang Lei, Shanshan Wang, Yan Li, Xuefeng Yang, Guoping Xiong, Liping Hao
Frontiers in Nutrition.2022;[Epub] CrossRef
- Maternal dietary components in the development of gestational diabetes mellitus: a systematic review of observational studies to timely promotion of health
- Lifestyle
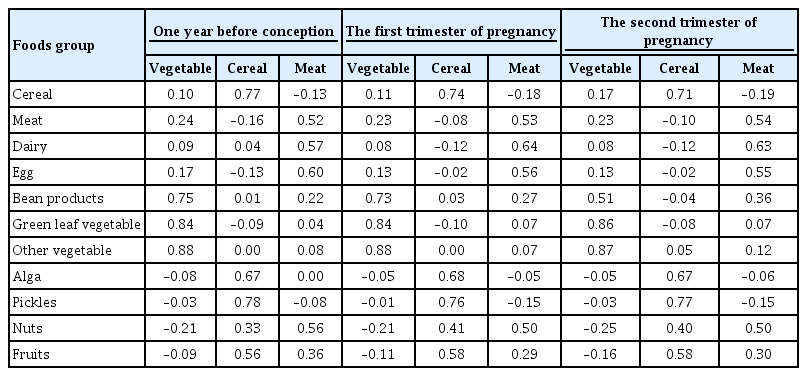
- Reducing Carbohydrate from Individual Sources Has Differential Effects on Glycosylated Hemoglobin in Type 2 Diabetes Mellitus Patients on Moderate Low-Carbohydrate Diets
- Hajime Haimoto, Shiho Watanabe, Keiko Maeda, Takashi Murase, Kenji Wakai
- Diabetes Metab J. 2021;45(3):390-403. Published online July 21, 2020
- DOI: https://doi.org/10.4093/dmj.2020.0033
- 5,791 View
- 160 Download
- 3 Web of Science
- 3 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 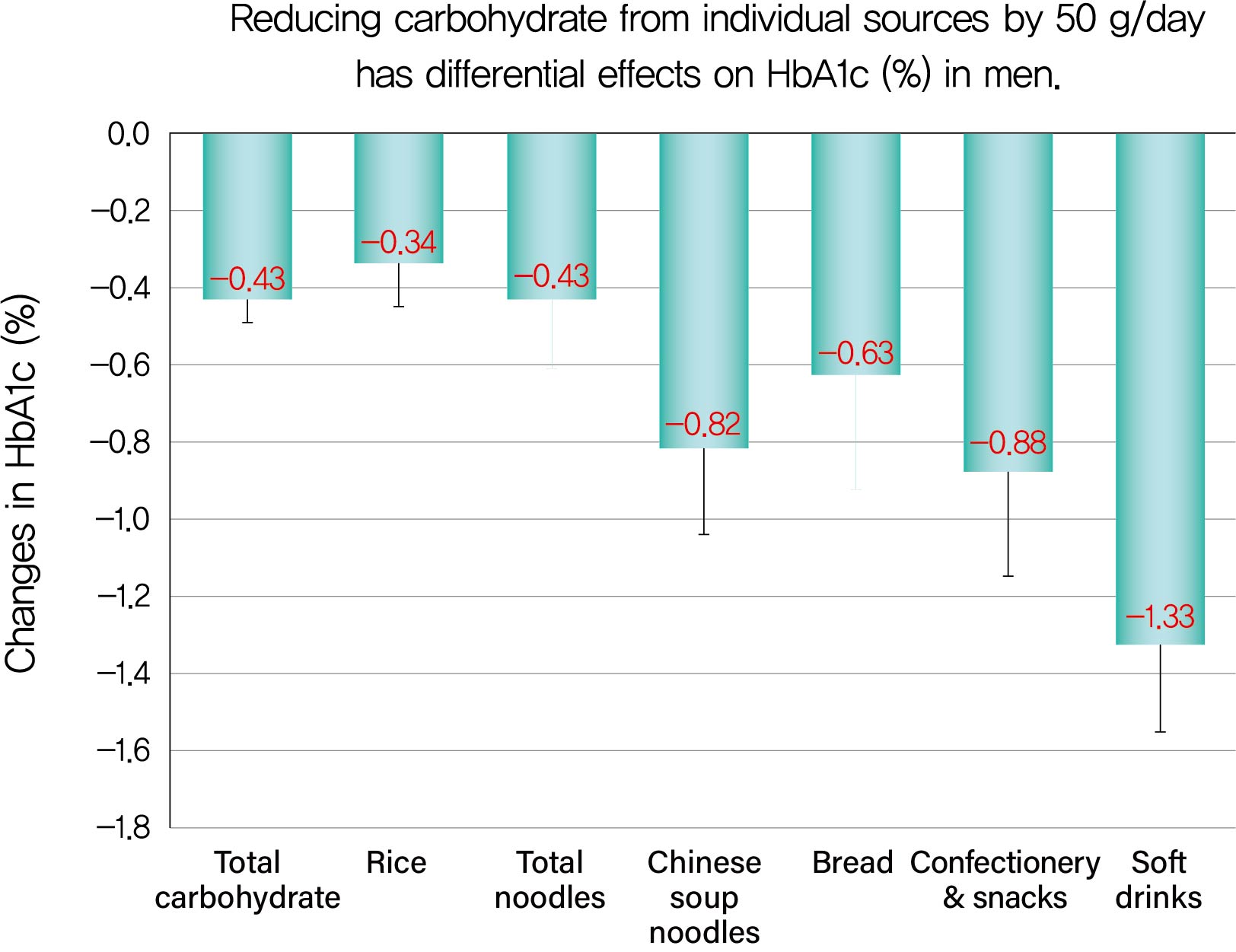
Background We evaluated decreases in glycosylated hemoglobin (HbA1c) achieved by reducing carbohydrate from various sources in type 2 diabetes mellitus patients.
Methods We followed up 138 male and 107 female outpatients on a moderate low-carbohydrate diet without diabetic medication for 6 months. Changes in carbohydrate sources (Δcarbohydrate) were assessed from 3-day dietary records at baseline and 6 months, and associations with changes in HbA1c (ΔHbA1c) were examined with Spearman's correlation coefficients (
r s) and multiple regression analysis.Results ΔHbA1c was −1.5%±1.6% in men and −0.9%±1.3% in women, while Δtotal carbohydrate was −115.3±103.7 g/day in men and −63.6±71.1 g/day in women. Positive associations with ΔHbA1c were found for Δtotal carbohydrate (
r s=0.584), Δcarbohydrate from soft drinks (0.368), confectionery (0.361), rice (0.325), bread (0.221), Chinese soup noodles (0.199) in men, and Δtotal carbohydrate (0.547) and Δcarbohydrate from rice (0.376) and confectionery (0.195) in women. Reducing carbohydrate sources by 50 g achieved decreases in HbA1c of 0.43% for total carbohydrate, 1.33% for soft drinks, 0.88% for confectionery, 0.63% for bread, 0.82% for Chinese soup noodles and 0.34% for rice in men and 0.45% for total carbohydrate, 0.67% for confectionery and 0.34% for rice in women, although mean reductions in carbohydrate from these sources were much smaller than that from rice.Conclusion Decreases in HbA1c achieved by reducing carbohydrate from soft drinks, confectionery, bread and Chinese soup noodles were 2- to 4-fold greater than that for rice. Our results will enable patients to decrease HbA1c efficiently (UMIN000009866).
-
Citations
Citations to this article as recorded by- Exploring diet associations with Covid-19 and other diseases: a Network Analysis–based approach
Rashmeet Toor, Inderveer Chana
Medical & Biological Engineering & Computing.2022; 60(4): 991. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - Associations of Dietary Salt and Its Sources with Hemoglobin A1c in Patients with Type 2 Diabetes Not Taking Anti-Diabetic Medications: Analysis Based on 6-Month Intervention with a Moderate Low-Carbohydrate Diet
Hajime Haimoto, Takashi Murase, Shiho Watanabe, Keiko Maeda, Kenji Wakai
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4569. CrossRef
- Exploring diet associations with Covid-19 and other diseases: a Network Analysis–based approach
- Obesity and Metabolic Syndrome
- Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals
- Chang Ho Ahn, Jae Hyun Bae, Young Min Cho
- Diabetes Metab J. 2019;43(6):879-892. Published online June 25, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0202
- 4,992 View
- 84 Download
- 3 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader Background A premeal load of protein can increase satiety and reduce energy intake. Dietary fiber also conveys metabolic benefits by modulating energy intake. We made a protein-enriched, dietary fiber-fortified bar (PFB) and aimed to investigate its effects on food intake and gut hormone secretion in healthy individuals.
Methods Twenty subjects with normal glucose tolerance were enrolled. On three separate visits, the subjects received, in a randomized order, one of the following: a PFB containing 73 kcal with 10.7 g of protein and 12.7 g of dietary fiber; a usual bar (UB) containing the same calories as the PFB but only 0.9 g of protein and no dietary fiber; or water (control). After 15 minutes, the subjects had
ad libitum intake of a test meal. Food consumption, appetite, and plasma gut hormone levels were measured.Results Total energy intake, including the bar and the test meal, was significantly reduced with the PFB preload compared to the water (904.4±534.9 kcal vs. 1,075.0±508.0 kcal,
P =0.016). With the UB preload, only the intake of the test meal was reduced (P =0.044) but not the total energy intake (P =0.471) than the water. Fullness was also significantly increased after the PFB. In addition, postprandial glucose levels decreased and glucagon-like peptide-1 levels increased with the PFB compared with both the UB and water.Conclusion In healthy individuals, a premeal supplementation of PFB reduced total energy intake and decreased postprandial glucose excursion. This finding necessitates long-term studies regarding clinical use in obesity.
-
Citations
Citations to this article as recorded by- Citrus pectin protects mice from burn injury by modulating intestinal microbiota, GLP-1 secretion and immune response
Ji-Wei Hao, Hong-Sheng Liu, Ling-Ying Liu, Qing-Hong Zhang
International Immunopharmacology.2024; 131: 111912. CrossRef - Effect of Two Different Meal Compositions on 1-hour Plasma Ghrelin Levels in Young Men
Brinnell Annette Caszo, Sangeetha Shyam, Purushotham Krishnappa, Justin Vijay Gnanou
Malaysian Journal of Medicine and Health Sciences.2023; 19(5): 185. CrossRef - Intake of Fibre-Associated Foods and Texture Preferences in Relation to Weight Status Among 9–12 Years Old Children in 6 European Countries
Marlies Hörmann-Wallner, Raphaela Krause, Begoña Alfaro, Hannah Jilani, Monica Laureati, Valérie L. Almli, Mari Sandell, Pernilla Sandvik, Gertrude G. Zeinstra, Lisa Methven
Frontiers in Nutrition.2021;[Epub] CrossRef - Response: Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals (Diabetes Metab J 2019;43:879–92)
Chang Ho Ahn, Jae Hyun Bae, Young Min Cho
Diabetes & Metabolism Journal.2020; 44(1): 207. CrossRef - Letter: Premeal Consumption of a Protein-Enriched, Dietary Fiber-Fortified Bar Decreases Total Energy Intake in Healthy Individuals (Diabetes Metab J 2019;43:879–92)
Mi-kyung Kim
Diabetes & Metabolism Journal.2020; 44(1): 203. CrossRef - Spent coffee (Coffea arabicaL.) grounds promote satiety and attenuate energy intake: A pilot study
Rocio Campos‐Vega, Andrea Arreguín‐Campos, Miguel A. Cruz‐Medrano, María Dolores Castillo Bilbao
Journal of Food Biochemistry.2020;[Epub] CrossRef
- Citrus pectin protects mice from burn injury by modulating intestinal microbiota, GLP-1 secretion and immune response
- Clinical Diabetes & Therapeutics
- Additional Effect of Dietary Fiber in Patients with Type 2 Diabetes Mellitus Using Metformin and Sulfonylurea: An Open-Label, Pilot Trial
- Seung-Eun Lee, Yongbin Choi, Ji Eun Jun, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Gwang Pyo Ko, Moon-Kyu Lee
- Diabetes Metab J. 2019;43(4):422-431. Published online April 23, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0090
- 5,796 View
- 77 Download
- 8 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Metformin, sulfonylurea, and dietary fiber are known to affect gut microbiota in patients with type 2 diabetes mellitus (T2DM). This open and single-arm pilot trial investigated the effects of the additional use of fiber on glycemic parameters, insulin, incretins, and microbiota in patients with T2DM who had been treated with metformin and sulfonylurea.
Methods Participants took fiber for 4 weeks and stopped for the next 4 weeks. Glycemic parameters, insulin, incretins during mixed-meal tolerance test (MMTT), lipopolysaccharide (LPS) level, and fecal microbiota were analyzed at weeks 0, 4, and 8. The first tertile of difference in glucose area under the curve during MMTT between weeks 0 and 4 was defined as ‘responders’ and the third as ‘nonresponders,’ respectively.
Results In all 10 participants, the peak incretin levels during MMTT were higher and LPS were lower at week 4 as compared with at baseline. While the insulin sensitivity of the ‘responders’ increased at week 4, that of the ‘nonresponders’ showed opposite results. However, the results were not statistically significant. In all participants, metabolically unfavorable microbiota decreased at week 4 and were restored at week 8. At baseline, metabolically hostile bacteria were more abundant in the ‘nonresponders.’ In ‘responders,’
Roseburia intestinalis increased at week 4.Conclusion While dietary fiber did not induce additional changes in glycemic parameters, it showed a trend of improvement in insulin sensitivity in ‘responders.’ Even if patients are already receiving diabetes treatment, the additional administration of fiber can lead to additional benefits in the treatment of diabetes.
-
Citations
Citations to this article as recorded by- The effects of prebiotics on gastrointestinal side effects of metformin in youth: A pilot randomized control trial in youth-onset type 2 diabetes
Sydney A. Dixon, Sidharth Mishra, Katrina B. Dietsche, Shalini Jain, Lilian Mabundo, Michael Stagliano, Andrea Krenek, Amber Courville, Shanna Yang, Sara A. Turner, Abby G. Meyers, Doris E. Estrada, Hariom Yadav, Stephanie T. Chung
Frontiers in Endocrinology.2023;[Epub] CrossRef - The impact of dietary, surgical, and pharmacological interventions on gut microbiota in individuals with diabetes mellitus: A systematic review
Patricia M. Bock, Andreza F. Martins, Rafaela Ramalho, Gabriela H. Telo, Gabriel Leivas, Clara K. Maraschin, Beatriz D. Schaan
Diabetes Research and Clinical Practice.2022; 189: 109944. CrossRef - Assessment of the safety and probiotic properties of Roseburia intestinalis: A potential “Next Generation Probiotic”
Chao Zhang, Kejia Ma, Kai Nie, Minzi Deng, Weiwei Luo, Xing Wu, Yujun Huang, Xiaoyan Wang
Frontiers in Microbiology.2022;[Epub] CrossRef - The Effect of Prebiotics and Oral Anti-Diabetic Agents on Gut Microbiome in Patients with Type 2 Diabetes: A Systematic Review and Network Meta-Analysis of Randomised Controlled Trials
Omorogieva Ojo, Xiaohua Wang, Osarhumwese Osaretin Ojo, Joanne Brooke, Yiqing Jiang, Qingqing Dong, Trevor Thompson
Nutrients.2022; 14(23): 5139. CrossRef - The Effect of Dietary Interventions on Chronic Inflammatory Diseases in Relation to the Microbiome: A Systematic Review
Carlijn A. Wagenaar, Marieke van de Put, Michelle Bisschops, Wendy Walrabenstein, Catharina S. de Jonge, Hilde Herrema, Dirkjan van Schaardenburg
Nutrients.2021; 13(9): 3208. CrossRef - The Role of Dietary Fibre in Modulating Gut Microbiota Dysbiosis in Patients with Type 2 Diabetes: A Systematic Review and Meta-Analysis of Randomised Controlled Trials
Omorogieva Ojo, Qian-Qian Feng, Osarhumwese Osaretin Ojo, Xiao-Hua Wang
Nutrients.2020; 12(11): 3239. CrossRef - High Fiber and Beta Carotene from Sweet Potatoes and Pumpkin Improve Insulin Resistance by Inhibition of Sterol Regulatory Binding Protein 1c in Liver of Hypertriglyceridemic Rats
Sunarti Sunarti, Umar Santoso, Abrory Agus Cahya Pramana, Emy Huriyati, Dianandha Septiana Rubi
Open Access Macedonian Journal of Medical Sciences.2020; 8(A): 898. CrossRef
- The effects of prebiotics on gastrointestinal side effects of metformin in youth: A pilot randomized control trial in youth-onset type 2 diabetes
- Obesity and Metabolic Syndrome
- Diabetes Prevention in Australia: 10 Years Results and Experience
- James A. Dunbar
- Diabetes Metab J. 2017;41(3):160-167. Published online February 2, 2017
- DOI: https://doi.org/10.4093/dmj.2017.41.3.160
- 4,872 View
- 69 Download
- 12 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Clinical trials have demonstrated the efficacy of lifestyle modification for the prevention of type 2 diabetes mellitus but it was achieved at higher cost than can be sustained in routine health services. The first clinical trial to report was the Finnish Diabetes Prevention Study. This paper describes how Australia worked with Finnish colleagues to adapt the findings of that study to achieve a statewide diabetes prevention program. Small evaluative, effectiveness trials have been conducted in a number of countries to see if the results of the clinical trials can be replicated in routine health services. The Australian evaluative trial, Greater Green Triangle Diabetes Prevention Program is described in detail to demonstrate the ingredients for success in moving a program from one country to another. Few countries have managed to scale up from evaluative trials to statewide or national programs. The Australian experience is described in detail including lessons learned about what reduced the effectiveness, particularly the need for policy makers in government, people from the implementing organisation and researchers to work together from the start of the evaluative trial and throughout the first 5 years of a national program.
-
Citations
Citations to this article as recorded by- Miscarriage, stillbirth and the risk of diabetes in women: A systematic review and meta-analysis
Qiqi You, Qingqing Jiang, Irakoze Shani, Yiling Lou, Shen Huang, Shiqi Wang, Shiyi Cao
Diabetes Research and Clinical Practice.2023; 195: 110224. CrossRef - A multiple case study of pre-diabetes care undertaken by general practice in Aotearoa/New Zealand: de-incentivised and de-prioritised work
Christine Barthow, Jeremy Krebs, Eileen McKinlay
BMC Primary Care.2023;[Epub] CrossRef - Implementation of a diabetes prevention programme in a multi-ethnic community in primary care in England: An evaluation using constructs from the RE-AIM Framework
Helen Dallosso, Kamlesh Khunti, Laura J. Gray, Kerry Hulley, Mel Ghaly, Naina Patel, Joe Kai, Navneet Aujla, Melanie J. Davies, Tom Yates
Primary Care Diabetes.2023; 17(4): 309. CrossRef - A critical realist exploration of factors influencing engagement in diabetes prevention programs in rural settings
Britney McMullen, Kerith Duncanson, David Schmidt, Clare Collins, Lesley MacDonald-Wicks
Australian Journal of Primary Health.2023; 29(5): 510. CrossRef - Characteristics of participants in the first fully online National Diabetes Prevention Programme: A quantitative survey
Clair Haseldine, Gráinne O'Donoghue, Patricia M Kearney, Fiona Riordan, Margaret Humphreys, Liz Kirby, Sheena McHugh
HRB Open Research.2023; 6: 61. CrossRef - Delivering the Diabetes Remission Clinical Trial (DiRECT) in primary care: Experiences of healthcare professionals
Lucia Rehackova, Roy Taylor, Mike Lean, Alison Barnes, Louise McCombie, George Thom, Naomi Brosnahan, Wilma S. Leslie, Falko F. Sniehotta
Diabetic Medicine.2022;[Epub] CrossRef - It is time for a more targeted approach to prediabetes in primary care in Aotearoa New Zealand
Christine Barthow, Sue Pullon, Eileen McKinlay, Jeremy Krebs, Stokes Tim
Journal of Primary Health Care.2022; 14(4): 372. CrossRef - Implementing a national diabetes prevention programme in England: lessons learned
Jonathan Stokes, Judith Gellatly, Peter Bower, Rachel Meacock, Sarah Cotterill, Matt Sutton, Paul Wilson
BMC Health Services Research.2019;[Epub] CrossRef - How do we identify people at high risk of Type 2 diabetes and help prevent the condition from developing?
J. Fagg, J. Valabhji
Diabetic Medicine.2019; 36(3): 316. CrossRef - Associations between physical activity and cataract treated surgically in patients with diabetes: findings from the 45 and Up Study
Changfan Wu, Xiaotong Han, Xixi Yan, Xianwen Shang, Lei Zhang, Mingguang He
British Journal of Ophthalmology.2019; 103(8): 1099. CrossRef - Usefulness of a Novel Mobile Diabetes Prevention Program Delivery Platform With Human Coaching: 65-Week Observational Follow-Up
Andreas Michaelides, Jennifer Major, Edmund Pienkosz Jr, Meghan Wood, Youngin Kim, Tatiana Toro-Ramos
JMIR mHealth and uHealth.2018; 6(5): e93. CrossRef
- Miscarriage, stillbirth and the risk of diabetes in women: A systematic review and meta-analysis
- Obesity and Metabolic Syndrome
- Regulating Hypothalamus Gene Expression in Food Intake: Dietary Composition or Calorie Density?
- Mi Jang, So-Young Park, Yong-Woon Kim, Seung-Pil Jung, Jong-Yeon Kim
- Diabetes Metab J. 2017;41(2):121-127. Published online December 16, 2016
- DOI: https://doi.org/10.4093/dmj.2017.41.2.121
- 3,708 View
- 35 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background The proportion of saturated fatty acids/unsaturated fatty acids in the diet seems to act as a physiological regulation on obesity, cardiovascular diseases, and diabetes. Differently composed fatty acid diets may induce satiety of the hypothalamus in different ways. However, the direct effect of the different fatty acid diets on satiety in the hypothalamus is not clear.
Methods Three experiments in mice were conducted to determine whether: different compositions of fatty acids affects gene mRNA expression of the hypothalamus over time; different types of fatty acids administered into the stomach directly affect gene mRNA expression of the hypothalamus; and fat composition changes in the diet affects gene mRNA expression of the hypothalamus.
Results The type of fat in cases of purified fatty acid administration directly into the stomach may cause changes of gene expressions in the hypothalamus. Gene expression by dietary fat may be regulated by calorie amount ingested rather than weight amount or type of fat.
Conclusion Therefore, the calorie density factor of the diet in regulating hypothalamic gene in food intake may be detrimental, although the possibility of type of fat cannot be ruled out.
-
Citations
Citations to this article as recorded by- Prepartum fatty acid supplementation in sheep. III. Effect of eicosapentaenoic acid and docosahexaenoic acid during finishing on performance, hypothalamus gene expression, and muscle fatty acids composition in lambs1
Ana Cristina Carranza Martin, Danielle Nicole Coleman, Lyda Guadalupe Garcia, Cecilia C Furnus, Alejandro E Relling
Journal of Animal Science.2018; 96(12): 5300. CrossRef - Acute anti‐obesity effects of intracerebroventricular 11β‐HSD1 inhibitor administration in diet‐induced obese mice
M. Seo, S. A. Islam, S.‐S. Moon
Journal of Neuroendocrinology.2018;[Epub] CrossRef - Letter: Regulating Hypothalamus Gene Expression in Food Intake: Dietary Composition or Calorie Density? (Diabetes Metab J 2017;41:121-7)
Bo Kyung Koo
Diabetes & Metabolism Journal.2017; 41(3): 223. CrossRef - Response: Regulating Hypothalamus Gene Expression in Food Intake: Dietary Composition or Calorie Density? (Diabetes Metab J2017;41:121-7)
Mi Jang, So-Young Park, Yong-Woon Kim, Seung-Pil Jung, Jong-Yeon Kim
Diabetes & Metabolism Journal.2017; 41(3): 225. CrossRef
- Prepartum fatty acid supplementation in sheep. III. Effect of eicosapentaenoic acid and docosahexaenoic acid during finishing on performance, hypothalamus gene expression, and muscle fatty acids composition in lambs1
- Epidemiology
- Dietary Sodium Intake in People with Diabetes in Korea: The Korean National Health and Nutrition Examination Survey for 2008 to 2010
- Myung Shin Kang, Chong Hwa Kim, Su Jin Jeong, Tae Sun Park
- Diabetes Metab J. 2016;40(4):290-296. Published online June 23, 2016
- DOI: https://doi.org/10.4093/dmj.2016.40.4.290
- 3,415 View
- 40 Download
- 16 Web of Science
- 18 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Background Diabetics are likely to receive advice from their physicians concerning lifestyle changes. To understand how much sodium is consumed by diabetics in Korea, we compared the average daily sodium intake between diabetics and non-diabetics after controlling for confounding factors.
Methods We obtained the sodium intake data for 13,957 individuals who participated in the Korean National Health and Nutrition Examination Survey (KNHANES), 2008 to 2010, which consisted of a health interview and behavioral and nutritional surveys. The KNHANES uses a stratified, multistage, probability-sampling design, and weighting adjustments were conducted to represent the entire population.
Results Our analysis revealed that, overall, diabetics tended to have lower sodium intake (4,910.2 mg) than healthy individuals (5,188.2 mg). However, both diabetic and healthy individuals reported higher sodium intake than is recommended by the World Health Organization (WHO). Stratified subgroup analyses revealed that the sodium intake (4,314.2 mg) among newly diagnosed diabetics was higher among women when compared to patients with known diabetes (3,812.5 mg,
P =0.035). Female diabetics with cardiovascular disease had lower average sodium intake compared to those without cardiovascular disease after adjusting for sex, age, body mass index, and total energy intake (P =0.058). Sodium intake among male diabetics with hypercholesterolemia (P =0.011) and female diabetics with hypertriglyceridemia (P =0.067) tended to be higher than that among those who without dyslipidemia.Conclusion The average sodium intake of diabetics in Korea was higher than the WHO recommends. Sodium intake in newly diagnosed diabetics was significantly higher than that in non-diabetics and previously diagnosed diabetics among females. Prospective studies are needed to identify the exact sodium intake.
-
Citations
Citations to this article as recorded by- Salt Intake in Adults with Diabetes and Hypertension: The Longitudinal Study of Adult Health-Brasil Study
Natália Gonçalves Ribeiro, Deborah F. Lelis, Rosane H. Griep, Sandhi M. Barreto, Maria del Carmen B Molina, Maria I. Schmidt, Bruce B. Duncan, Isabela Bensenor, Paulo A. Lotufo, José G. Mill, Marcelo Perim Baldo
Metabolic Syndrome and Related Disorders.2024;[Epub] CrossRef - Effects of different diets on glycemic control among patients with type 2 diabetes: A literature review
Maryam E Al-Adwi, Zinab M Al-Haswsa, Karmen M Alhmmadi, Yasmin A Eissa, Aya Hamdan, Hiba Bawadi, Reema F Tayyem
Nutrition and Health.2023; 29(2): 215. CrossRef - Dietary salt intake predicts future development of metabolic syndrome in the general population
Hiroyuki Takase, Kazusa Hayashi, Fumihiko Kin, Suguru Nakano, Masashi Machii, Shin Takayama, Tomonori Sugiura, Yasuaki Dohi
Hypertension Research.2023; 46(1): 236. CrossRef - High Sodium Intake, as Assessed by Urinary Sodium Excretion, Is Associated with Nonalcoholic Fatty Liver Disease or Sarcopenia
Eugene Han, Mi Kyung Kim, Seung-Soon Im, Hye Soon Kim, Taeg Kyu Kwon, Byoung Kuk Jang
Gut and Liver.2023; 17(3): 456. CrossRef - Trends of Dietary Intakes and Metabolic Diseases in Japanese Adults: Assessment of National Health Promotion Policy and National Health and Nutrition Survey 1995–2019
Muhammad Fauzi, Indri Kartiko-Sari, Hemant Poudyal
Journal of Clinical Medicine.2022; 11(9): 2350. CrossRef - Determinants of Type 2 Diabetes Mellitus Among Adults in Dill-Chora Referral Hospital, Dire Dawa, East Ethiopia
Tewodros Getnet Amera, Yibekal Manaye Tefera, Tameru Menberu, Aminu Mohammed Yassin
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2022; Volume 15: 3565. CrossRef - Dietary sodium and cardiovascular morbidity/mortality: a brief commentary on the ‘J-shape hypothesis’
Christiana Tsirimiagkou, Kalliopi Karatzi, Antonios Argyris, Eirini D. Basdeki, Panagiota Kaloudi, Mary Yannakoulia, Athanase D. Protogerou
Journal of Hypertension.2021; 39(12): 2335. CrossRef - Associations of Dietary Salt and Its Sources with Hemoglobin A1c in Patients with Type 2 Diabetes Not Taking Anti-Diabetic Medications: Analysis Based on 6-Month Intervention with a Moderate Low-Carbohydrate Diet
Hajime Haimoto, Takashi Murase, Shiho Watanabe, Keiko Maeda, Kenji Wakai
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 4569. CrossRef - Association of rheumatoid arthritis and high sodium intake with major adverse cardiovascular events: a cross-sectional study from the seventh Korean National Health and Nutrition Examination Survey
Jeong-Hyeon Bae, Min-Young Shin, Eun Ha Kang, Yun Jong Lee, You-Jung Ha
BMJ Open.2021; 11(12): e056255. CrossRef - Nineteen-year trends in fermented food consumption and sodium intake from fermented foods for Korean adults from 1998 to 2016
Sang Young Kim, Jeanne H Freeland-Graves, Hyun Ja Kim
Public Health Nutrition.2020; 23(3): 515. CrossRef - Dietary Sodium Intake and Health Indicators: A Systematic Review of Published Literature between January 2015 and December 2019
Katherine J Overwyk, Zerleen S Quader, Joyce Maalouf, Marlana Bates, Jacqui Webster, Mary G George, Robert K Merritt, Mary E Cogswell
Advances in Nutrition.2020; 11(5): 1174. CrossRef - Lower Leg Fat Depots Are Associated with Albuminuria Independently of Obesity, Insulin Resistance, and Metabolic Syndrome (Korea National Health and Nutrition Examination Surveys 2008 to 2011)
Eugene Han, Nan Hee Cho, Mi Kyung Kim, Hye Soon Kim
Diabetes & Metabolism Journal.2019; 43(4): 461. CrossRef - Factors Predicting Sodium Intake of Korean Americans with Type 2 Diabetes
Jisook Ko, Kim B. Kim, Gayle M. Timmerman, Angela P. Clark, Miyong Kim
Journal of Immigrant and Minority Health.2018; 20(3): 641. CrossRef - Evaluation of the association between the number of natural teeth and anemia among Korean adults using nationally representative data
Kyungdo Han, Jun‐Beom Park
Journal of Periodontology.2018; 89(10): 1184. CrossRef - Clinical implications of age and sex in the prevalence of periodontitis in Korean adults with diabetes
Kyungdo Han, Jun‑Beom Park
Experimental and Therapeutic Medicine.2018;[Epub] CrossRef - Association between underweight and tooth loss among Korean adults
In-Seok Song, Kyungdo Han, Jae-Jun Ryu, Jun-Beom Park
Scientific Reports.2017;[Epub] CrossRef - The Science of Salt: A regularly updated systematic review of the implementation of salt reduction interventions (March–August 2016)
Joseph Alvin Santos, Kathy Trieu, Thout Sudhir Raj, JoAnne Arcand, Claire Johnson, Jacqui Webster, Rachael McLean
The Journal of Clinical Hypertension.2017; 19(4): 439. CrossRef - Salt-sensitive genes and their relation to obesity
Yong-Pil Cheon, Myoungsook Lee
Journal of Nutrition and Health.2017; 50(3): 217. CrossRef
- Salt Intake in Adults with Diabetes and Hypertension: The Longitudinal Study of Adult Health-Brasil Study

 KDA
KDA
 First
First Prev
Prev





