Oral Glucose Tolerance Testing Allows Better Prediction of Diabetes in Women with a History of Gestational Diabetes Mellitus
Article information
Abstract
Background
We aimed to identify the postpartum metabolic factors that were associated with the development of diabetes in women with a history of gestational diabetes mellitus (GDM). In addition, we examined the role of the oral glucose tolerance test (OGTT) in the prediction of future diabetes.
Methods
We conducted a prospective study of 179 subjects who previously had GDM but did not have diabetes at 2 months postpartum. The initial postpartum examination including a 75-g OGTT and the frequently sampled intravenous glucose tolerance test (FSIVGTT) was performed 12 months after delivery, and annual follow-up visits were made thereafter.
Results
The insulinogenic index (IGI30) obtained from the OGTT was significantly correlated with the acute insulin response to glucose (AIRg) obtained from the FSIVGTT. The disposition indices obtained from the OGTT and FSIVGTT were also significantly correlated. Women who progressed to diabetes had a lower insulin secretory capacity including IGI30, AIRg, and disposition indices obtained from the FSIVGTT and OGTT compared with those who did not. However, the insulin sensitivity indices obtained from the OGTT and FSIVGTT did not differ between the two groups. Multivariate logistic regression analysis showed that the 2-hour glucose and disposition index obtained from the FSIVGTT were significant postpartum metabolic risk factors for the development of diabetes.
Conclusion
We identified a crucial role of β-cell dysfunction in the development of diabetes in Korean women with previous GDM. The 2-hour glucose result from the OGTT is an independent predictor of future diabetes. Therefore, the OGTT is crucial for better prediction of future diabetes in Korean women with previous GDM.
INTRODUCTION
It is well known that women with a previous history of gestational diabetes mellitus (GDM) have an increased risk of developing type 2 diabetes mellitus (T2DM) [12]. Although most women with GDM return to normal glucose tolerance when tested several weeks after delivery, increased insulin resistance, and/or impaired insulin secretory function has been reported in women with previous GDM [3]. In addition, a substantial proportion of women with previous GDM eventually develop T2DM [45]. A meta-analysis reported that women with a history of GDM had a 7.4 times higher risk of diabetes than women without a previous history of GDM [6]. Korean women with previous GDM were also at increased risk for postpartum diabetes [25]: compared with Korean women without a history of GDM, their odds ratio (OR) of developing diabetes was 3.7 [7]. Another Korean study showed that approximately 40% of Korean women with GDM developed T2DM over 5 years [5].
Several interventional trials to prevent or delay the development of postpartum diabetes in women with previous GDM have been conducted. The Diabetes Prevention Program Outcomes Study (DPPOS) demonstrated that intensive lifestyle modification and metformin treatment reduced the cumulative incidence of T2DM in women with previous GDM by 35% and 40%, respectively, compared with a placebo group [89]. The Troglitazone in Prevention of Diabetes (TRIPOD) study also showed that troglitazone treatment reduced the risk of diabetes development in these women by 55% [10]. A recent interventional trial comprising advice on diet and exercise included Chinese women with previous GDM who had impaired glucose tolerance (IGT) in a postpartum oral glucose tolerance test (OGTT) [11]. However, lifestyle intervention did not reduce significantly the incidence of postpartum diabetes in a 3-year follow-up. It is unclear why lifestyle modification was not effective in preventing postpartum diabetes in Asian women. Therefore, it is necessary to identify the clinical and metabolic risk factors for predicting future diabetes in Asian women with previous GDM.
Various clinical risk factors for postpartum diabetes in women with GDM have been reported, including maternal age [212], family history of diabetes [213], hyperglycemia during pregnancy [514], early diagnosis of GDM [12], insulin treatment during pregnancy [515], and prepregnancy and postpartum body mass index (BMI) [125]. Several metabolic factors predicting postpartum diabetes have also been identified, including indices of β-cell dysfunction (insulinogenic index [IGI] and disposition index [DI] in pregnancy and postpartum testing) [416] and insulin sensitivity measured by postpartum hyperinsulinemic clamps [17]. In addition, postpartum weight change, breast feeding, additional pregnancy, and physical activity also affect the incidence of T2DM in women with previous GDM [1819].
Postpartum glucose testing has been recommended for women with GDM to identify their postpartum glucose tolerance status. However, clinical guidelines from several health organizations do not agree about when and how to evaluate glucose tolerance in women with previous GDM [20]. Glucose testing in women with GDM has usually been performed at 6 weeks postpartum to coincide with a postpartum visit and to allow the transient increases in insulin resistance seen during pregnancy to return to nonpregnancy levels. After the first postpartum testing, glucose testing is recommended at intervals from 1 to 3 years depending on glucose tolerance status. The OGTT will identify additional women with IGT or diabetes compared with fasting glucose testing alone [2122]. However, postload glucose levels obtained from the OGTT have poorer reproducibility than fasting glucose measurements [23].
In this study, we aimed to identify the postpartum metabolic factors obtained from the OGTT that were associated with the development of diabetes, and evaluated the contribution of β-cell dysfunction and insulin resistance to the incidence of diabetes in women with previous GDM. In addition, we examined the role of the OGTT in the prediction of future diabetes.
METHODS
Study protocol
We conducted a prospective cohort study of subjects who were diagnosed with GDM according to the definition of the 4th International Workshop and Conference on GDM [24], but who did not have diabetes 2 months postpartum. Subjects were diagnosed with GDM at the Seoul National University Bundang Hospital from 2004 to 2006. The baseline postpartum evaluation was performed 12 months after delivery, and annual follow-up visits were made thereafter. This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital (IRB Number: B-0503/018-001). All subjects participated voluntarily, and informed consent was obtained from each subject.
Subjects
We recruited 183 women with previous GDM who were assessed for diabetes at 2 months postpartum using the 75-g OGTT and glutamic acid decarboxylase (GAD) antibody testing. Of these, four had diabetes and 74 had an impaired fasting glucose and/or IGT at the baseline examination. We followed up 179 subjects after excluding the four with diabetes.
Baseline examination
The detailed procedures for baseline and follow-up examinations have been described previously [518]. Briefly, the participants' obstetric history, including their prepregnancy weight, weight at diagnosis of GDM, and weight gain during pregnancy, was retrieved from medical records. Baseline examination 1 year postpartum was conducted using a standardized questionnaire on past medical history and family history of diabetes and anthropometric measurements. To evaluate glucose tolerance status, a 75-g OGTT was performed after an overnight fast. About 1 week later, the frequently sampled intravenous glucose tolerance test (FSIVGTT) was conducted after an overnight fast. An intravenous catheter was placed in each of the subject's forearms: one for bolus injections of glucose and the other for rapid, repeated blood sampling for measurement of glucose and insulin concentrations. After baseline samples (−30, −15, −1 minutes) were obtained, a bolus of glucose (0.3 g/kg body weight) was injected over a 60-second period. Human insulin (0.03 U/kg) was injected 20 minutes later over 30 seconds. Blood was then sampled 29 times over the next 180 minutes, with an initial frequency of 1 sample/minute (1, 2, 3, 4, 5, 6, 7, 8, 10, 12, 14, 16, 19, 22, 23, 24, 25, 27, 30, 40, 50, 60, 70, 80, 90, 100, 120, 160, and 180 minutes).
Follow-up examinations
A standard 75-g OGTT was performed at each follow-up visit. Anthropometric measures including body weight, height, and blood pressure (BP) were measured at each visit. Body weight was measured to the nearest 0.1 kg, and height was measured to the nearest 0.1 cm. Postpartum weight change was calculated as the difference between initial postpartum weight and that at the most recent visit. BP was measured three times to the nearest 2 mm Hg on the left arm by research coordinators using a mercury sphygmomanometer (Baumanometer; Baum, Copiague, NY, USA).
Metabolic assessment
The diagnosis of diabetes was based on the criteria of the American Diabetes Association [25]. The homeostasis model assessment of β-cell function (HOMA-β) and insulin resistance (HOMA-IR) were calculated [26]. The IGI30 was defined as (insulin [30 minutes]–insulin [0 minute])/(glucose [30 minutes]–glucose [0 minute]) [27]. The Matsuda index [28] was also calculated as 10,000/√(fasting glucose×fasting insulin×mean glucose×mean insulin). The DI obtained from the OGTT was used to evaluate the composite insulin secretion, taking into consideration the degree of insulin sensitivity, and was calculated as Matsuda index×IGI30.
Parameters obtained from the FSIVGTT were analyzed using the MINMOD Millennium program. The insulin sensitivity index (SI) was defined as the quantitative influence of insulin in enhancing the fractional rate of glucose disappearance [29]. The acute insulin response to glucose (AIRg) was also calculated, which is defined as the mean increment above baseline of the plasma insulin concentration in the first 10 minutes after the administration of glucose. The DI, a measure of acute pancreatic β-cell compensation for insulin resistance, was calculated by multiplying SI by AIRg [1730].
Plasma glucose was measured enzymatically with an automated analyzer (YSI 2300-STAT; Yellow Springs Instrument Co., Yellow Springs, OH, USA) using the glucose oxidase method. Plasma insulin was measured by radioimmunoassay (Linco Research Inc., St. Louis, MO, USA). Total cholesterol, triglycerides, and high density lipoprotein were measured by enzymatic assay (Beckman analyzer; Beckman Instruments, Brea, CA, USA).
Statistical analysis
Statistical analyses were performed using SPSS version 22.0 (IBM Co., Armonk, NY, USA). Data are expressed as mean±standard deviation, % or OR with 95% confidence interval. The metabolic variables for insulin secretion and resistance obtained from the OGTT and FSIVGTT were nonnormally distributed. To analyze the relationship between metabolic variables obtained via the OGTT and FSIVGTT, we used Spearman's ρ correlation test. Subjects were divided into two groups (nondiabetes and diabetes groups) based on the results of the 3-year follow-up examination. Differences between groups were evaluated using Student t-test and Mann-Whitney U test for continuous variables and the chi-square test for categorical variables. We used multiple logistic regression analysis to assess the ability of metabolic variables obtained from the OGTT and FSIVGTT to predict incident diabetes. Differences were considered significant when P<0.05.
RESULTS
Of the 183 women with previous GDM who did not have diabetes at 2 months postpartum, 158 underwent both the 75-g OGTT and the FSIVGTT at the baseline examination. We analyzed the relationship of insulin sensitivity and secretion indices obtained for these subjects from the 75-g OGTT and FSIVGTT.
Correlation of insulin sensitivity and secretion indices obtained from the OGTT and FSIVGTT
The SI calculated from the FSIVGTT correlated significantly with HOMA-IR and the Matsuda index obtained from the OGTT (Table 1). AIRg correlated significantly with IGI30, but not with HOMA-β. However, the DI (Matsuda index×IGI30) obtained from the OGTT correlated significantly with the DI (AIRg×SI) obtained from the FSIVGTT. Fasting and 2-hour glucose levels were negatively correlated with AIRg and DI from the FSIVGTT.
Clinical and metabolic characteristics of women who progress to diabetes
A total of 142 subjects completed follow-up examinations for 3 years but 37 dropped out. There was no significant difference between the subjects who completed follow-up visits and the dropouts for clinical characteristics including age, BMI, systolic and diastolic BP, fasting, and postload glucose during pregnancy and at the baseline examination (data not shown). Of the 142 subjects, 34 (23.9%) were diagnosed with diabetes, 23 of whom had impaired fasting glucose and/or IGT at the baseline examination. Fifty-four women (38%) had impaired fasting glucose and/or IGT.
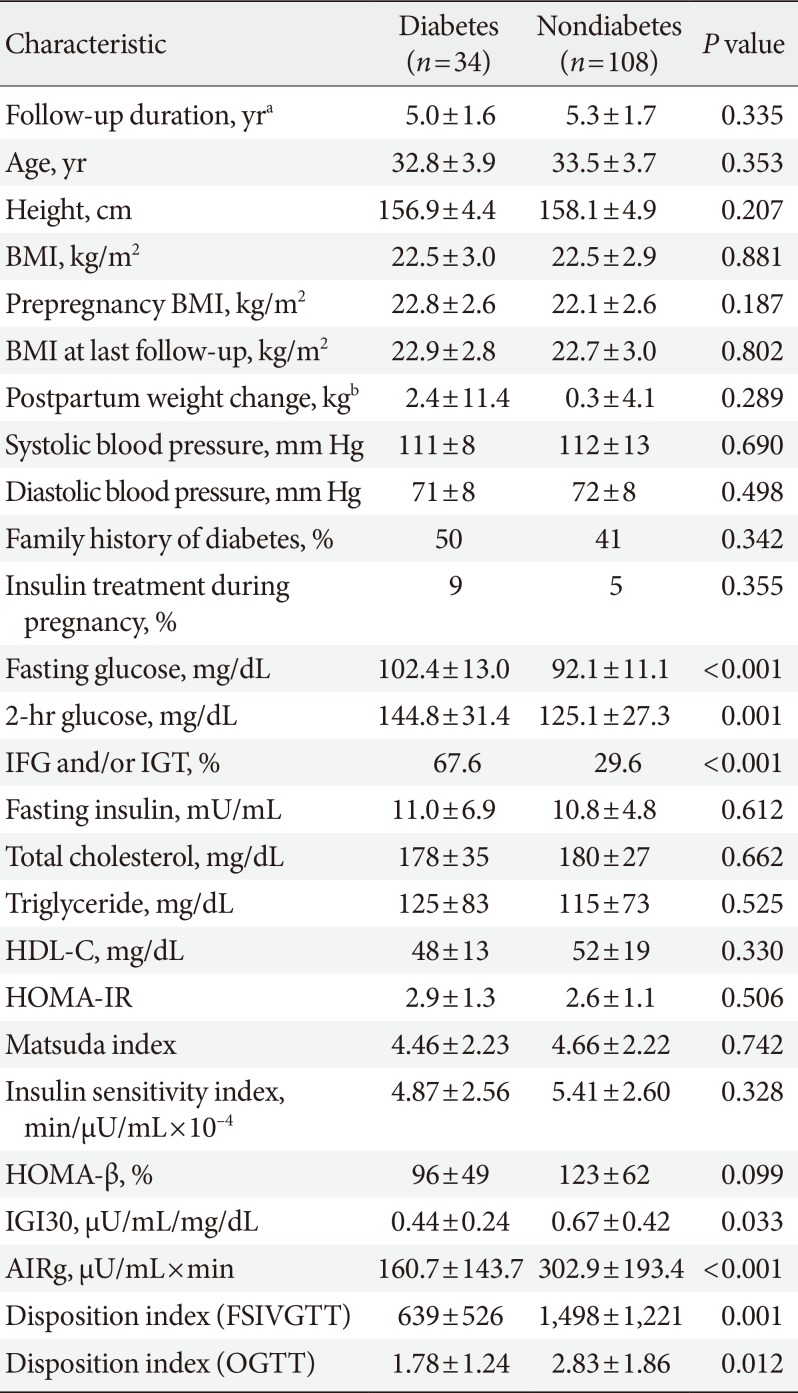
Table 2 shows the clinical and metabolic characteristics of subjects stratified according to the results of 3 years' follow-up examinations. The women who progressed to diabetes did not differ in age, height, BMI prepregnancy, baseline, and last follow-up examinations, duration of follow-up, systolic and diastolic BP, family history of first-degree relatives with diabetes or insulin treatment during pregnancy compared with those who did not develop diabetes. However, women who progressed to diabetes had higher fasting and 2-hour glucose and lower IGI30, AIRg, and DIs for the FSIVGTT and OGTT. Fasting insulin concentration, lipid profile, HOMA-IR, Matsuda index, SI, and HOMA-β did not differ between women who progressed to diabetes and those who did not.
Independent metabolic risk factors for development of diabetes
We used multiple logistic regression analysis to identify independent postpartum metabolic risk factors associated with progression to diabetes in women who did not have diabetes 1 year postpartum. Metabolic risk factors that differed significantly between women who progressed to diabetes and those who did not were included in model 1 (Table 3). We also included the two clinical factors (BMI at 2 months postpartum and postpartum weight change) that were identified in previous studies as risk factors in Korean women [518]. The DI obtained from the OGTT, which is derived from IGI30, was included instead of IGI30 in model 2. The 2-hour glucose from the OGTT was the only independent metabolic risk factor for the development of diabetes in Korean women with previous GDM. We included the DI obtained from the FSIVGTT instead of AIRg in model 3, because the DI obtained from the FSIVGTT was derived from AIRg. The introduction of the DI obtained from the FSIVGTT attenuated the association between the 2-hour glucose and the development of diabetes, meaning that the DI obtained from the FSIVGTT was the only significant metabolic risk factor for the development of diabetes.
DISCUSSION
This study showed that IGI30, an insulin secretion index obtained from the OGTT, was significantly correlated with AIRg obtained from the FSIVGTT. The DI obtained from the OGTT was also significantly correlated with the DI obtained from the FSIVGTT. In addition, IGI30 1 year postpartum was significantly correlated with IGI30 measured at 2 months postpartum (ρ=0.644, P<0.001). However, HOMA-β was not correlated with AIRg from the FSIVGTT and did not differ between women who progressed to diabetes and women who did not. Thus, IGI30 is a more reliable and reproducible index of β-cell function than HOMA-β.
Women who progressed to diabetes had lower insulin secretory capacity as measured by IGI30, AIRg, and DIs of the FSIVGTT and OGTT compared with women who did not progress to diabetes. However, the insulin sensitivity indices obtained from the OGTT and FSIVGTT, including HOMA-IR, Matsuda index, and SI, did not differ between women who progressed to diabetes and those who did not. These findings differ from those previously reported for Hispanic women with previous GDM [17]. Xiang et al. [17] reported that both lower insulin sensitivity and lower insulin secretory capacity were independently associated with the development of diabetes in Hispanic women with a median BMI of 30.7 kg/m2 whose body weight increased at rate of 0.69 kg/year during follow-up. However, in our study, the mean BMI of the Korean women with a previous GDM was 22.5 kg/m2 at baseline, and their change in body weight during the 5-year follow-up was 0.8±6.6 kg. Although a direct comparison of SI and AIRg between the Korean and Hispanic women was not possible, the median SI was much higher and AIRg was lower in Korean women compared with Hispanic women (SI and AIRg: 4.95 vs. 1.27 and 226 vs. 509, respectively). Therefore, β-cell failure is more important for the development of diabetes in Korean women with previous GDM. This finding is consistent with the results of Korean Genome and Epidemiology Study by Ohn et al. [31], which showed that decreased β-cell function and impaired β-cell compensation for decreasing insulin sensitivity were crucial factors in the development of prediabetes or diabetes.
We previously reported that 18 single nucleotide polymorphisms associated with T2DM, including CDK5 regulatory subunit associated protein 1-like 1 (CDKAL1), cyclin dependent kinase inhibitor 2A/2B (CDKN2A/2B), hematopoietically expressed homeobox (HHEX), insulin-like growth factor-2 mRNA-binding protein 2 (IGF2BP2), solute carrier family 30, member 8 (SLC30A8), and transcription factor 7-like 2 (TCF7L2), were associated with GDM in Korean women [32]. We also found that genetic variants in CDKN2A/2B and HHEX were associated with diabetes early postpartum (≤8 weeks) and variants in CDKAL1 were associated with late conversion to diabetes (>1 year postpartum) [5]. Most of the genetic variants discovered to be associated with GDM or postpartum diabetes in Korean women were functionally associated with β-cell insulin secretion but not insulin resistance or obesity [532]. These findings support a crucial role for β-cell dysfunction in the development of diabetes in Korean women with previous GDM.
Our findings have clinical implications in terms of prevention of diabetes in women with previous GDM. Lifestyle modification and treatment with insulin sensitizers including metformin and thiazolidinediones may be less effective for preventing diabetes in Korean women than seen in the DPPOS or TRIPOD studies [910]. A lifestyle modification trial [11] conducted in Chinese women with previous GDM and postpartum IGT failed to reduce incident diabetes, which might support our speculation. Glucagon-like peptide-1 (GLP-1) receptor agonists or dipeptidyl peptidase-4 (DPP-4) inhibitors may be more effective for preventing diabetes in Korean women with previous GDM, but further studies are needed to clarify their metabolic benefit in this population.
In this study, the incidence of diabetes in women with a previous history of GDM was 7.9%/year, which is comparable to that reported previously [5]. We found that among the postpartum metabolic and clinical factors we evaluated, the DI obtained from the FSIVGTT was the only independent metabolic risk factor associated with the development of diabetes in Korean women with previous GDM. This finding corroborates the role of β-cell dysfunction in the development of diabetes in this population, and is substantially in agreement with our previous results [5]. Because the FSIVGTT is not easily performed in clinical practice, we added the two clinical risk factors and metabolic risk factors obtained from the OGTT into the multivariate logistic regression model; the 2-hour glucose was the only significant metabolic risk factor for the development of diabetes. The 2-hour glucose was significantly associated with the DI obtained from the FSIVGTT (ρ=−0.397, P<0.001), AIRg (ρ=−0.326, P<0.001), and IGI30 (ρ=−0.334, P<0.001). These findings suggest that the OGTT is crucial for better prediction of future diabetes in Korean women with previous GDM.
This study has certain limitations. Although the clinical characteristics and metabolic variables including fasting and postload glucose and indices of insulin sensitivity and β-cell function at baseline did not differ between the women who completed all follow-up visits and those did not, the dropout rate was 20.7%. We could not compare the SI, AIRg, and DI of the FSIVGTT directly between Hispanic and Korean women, but the protocol used for the FSIVGTT in this study was very similar to that used by Xiang et al. [17]. Annual follow-up examinations may affect the bodyweight changes and health-related behaviors in women with previous GDM. Our findings may not be generalizable to all women with GDM, because we excluded those women who were diagnosed with diabetes early postpartum. Finally, we could not determine the interval at which the OGTT should be performed in Korean women with GDM after the first postpartum test.
In conclusion, we identified a crucial role of β-cell dysfunction in the development of diabetes in Korean women with previous GDM. The 2-hour glucose obtained from the OGTT was the only independent predictor of future diabetes. Thus, the OGTT is crucial for better prediction of future diabetes in Korean women with previous GDM.
ACKNOWLEDGMENTS
This study was supported by a grant from Seoul National University Bundang Hospital (02-2012-009), Korea.
Notes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS:
Conception or design: H.C.J., J.S.H., N.H.C.
Acquisition, analysis, or interpretation of data: T.J.O., Y.G.K., H.C.J.
Drafting the work or revising: T.J.O., Y.G.K., H.C.J.
Final approval of the manuscript: T.J.O., Y.G.K., S.K., J.H.M., S.H.K., S.H.C., S.L., K.S.P., H.C.J., J.S.H., N.H.C.