2011 Clinical Practice Guidelines for Type 2 Diabetes in Korea
Article information
Abstract
As in other countries, type 2 diabetes is major health concern in Korea. A dramatic increase in the prevalence of type 2 diabetes and its chronic complications has led to an increase in health costs and economic burdens. Early detection of high risk individuals, hidden diabetic patients, and improvement in the quality of care for the disease are the first steps to mitigate the increase in prevalence. The Committee of Clinical Practice Guidelines of the Korean Diabetes Association revised and updated the '3rd Clinical Practice Guidelines' at the end of 2010. In the guidelines, the committee recommended active screening of high risk individuals for early detection and added the hemoglobin A1c level to the diagnostic criteria for type 2 diabetes based on clinical studies performed in Korea. Furthermore, the committee members emphasized that integrating patient education and self-management is an essential part of care. The drug treatment algorithm based on the degree of hyperglycemia and patient characteristics were also updated.
INTRODUCTION
The prevalence of type 2 diabetes mellitus in Korea is estimated to be 7.3% (in those over 20 years of age), according to a report by the Korea National Health and Nutrition Examination Survey (KNHNS III, 2005), an approximately five-fold increase from the value 30 years ago [1-3]. The number of patients with type 2 diabetes is expected to increase dramatically from about 3.5 million in 2010 (7.08% of the total population) to about 5.5 million (10.85%) by 2030 [3,4].
The obese and overweight population is also increasing steadily in Korea; in addition, Korea is becoming one of the aged societies in the world. This increase in societal age has contributed to the dramatic increase in type 2 diabetic patients. Furthermore, diabetes mellitus was the fifth leading cause of death in Korea in 2008 [3]. Therefore, the early detection and prevention of type 2 diabetes are major health concerns for Korean people and the government. The diagnosis and appropriate treatment of type 2 diabetes mellitus are very important issues in establishing and implementing high-priority health policies in Korea.
SCREENING OF TYPE 2 DIABETES MELLITUS
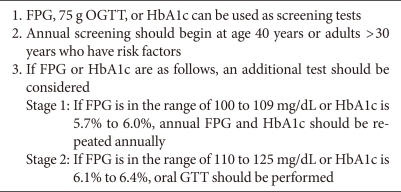
Recently, several hospital-based or community-based cross-sectional and cohort studies undertaken in Korea have been published. In 2007, the Committee of the Korean Diabetes Association (KDA) on the Diagnosis and Classification of Diabetes Mellitus analyzed four of these community-based epidemiological studies performed after 1990, which included 6,234 subjects, to demonstrate the diagnostic equivalence of fasting plasma glucose (FPG) value to a 2-hour plasma glucose (PG) value range of 140 and 200 mg/dL. From a receiver operating characteristic (ROC) analysis, an FPG cutoff of 110 mg/dL corresponded to a 2-hour PG value of 200 mg/dL (sensitivity 76.4%, specificity 92.2%) [5]. The optimal cutoff point for FPG for the diagnosis of impaired glucose tolerance (IGT) in Korean people was 97 mg/dL (sensitivity 57.5%, specificity 71.0%). Another study that compared the FPG criterion for diagnostic screening of diabetes with the 2-hour PG criterion in 1,731 middle-aged Korean adults showed that the level of agreement between the two diagnostic criteria was low (0.268). An ROC analysis determined that an FPG of 100 mg/dL yielded optimal sensitivity and specificity and corresponded to a 2-hour PG result of 200 mg/dL [6]. If these lower cutoff values are applied to the diagnosis of diabetes, the prevalence of diabetes is more than two-fold higher than when the 2-hour PG level of 200 mg/dL is used.
This large discrepancy between the FPG and 2-hour PG criteria in the diagnosis of diabetes and IGT in Koreans is cause for hesitation before changing the diagnostic criteria for diabetes. We also suggest that the FPG level required for a diagnosis of type 2 diabetes mellitus is lower in the Korean and Asian populations than in Western populations [5]. For this reason, Oh et al. [7] analyzed the IFG population according to fasting glucose level, as follows: stage 1 IFG (100 to 109 mg/dL) and stage 2 IFG (110 to 125 mg/dL). For subjects in the stage 2 group, poorer metabolic profiles were detected in terms of total cholesterol, triglyceride, and high blood pressure. Moreover, a greater proportion of people in the stage 2 group were diagnosed with diabetes based on the oral glucose tolerance test (OGTT). From these results, we suggest that Korean individuals with stage 2 IFG should be treated or screened in a different manner from those with stage 1 IFG. To avoid missing further cases of diabetes, the OGTT should be actively recommended for all individuals with stage 2 IFG. However, in patients with stage 1 IFG, additional risk factors for diabetes should be assessed and an annual glucose test be performed (Table 1).
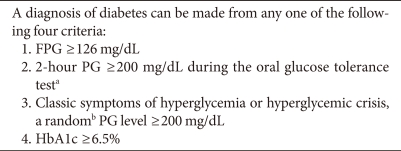
DIAGNOSIS OF TYPE 2 DIABETES MELLITUS
The diagnostic criteria for type 2 diabetes are based on the results of either the fasting or 2-hour 75 g OGTT, according to the observed association between glucose level and the presence of retinopathy. Until now, there have been no cross-sectional epidemiological studies of Koreans to demonstrate an association between PG level and the development of diabetic retinopathy. The KDA has adopted the diagnostic criteria for type 2 diabetes of the American Diabetes Association (ADA) (Table 2). Moreover, the variable association between FPG and 2-hour PG level between populations must be attributed to different genetic or environmental backgrounds across different ethnic groups. Therefore, more large epidemiological studies are required to confirm the suitable cutoff values for the Korean population.
Oral glucose tolerance test (OGTT)
The OGTT has low repeatability, requires more time and blood samples, and is more expensive than the FPG test. It has not been used to screen for type 2 diabetes mellitus and is not recommended for the diagnosis of type 2 diabetes in routine clinical practice in Korea. However, although FPG is a simple and convenient method, a considerable number of type 2 diabetic patients cannot be diagnosed based on FPG results alone, as discussed above. Several previous studies have shown that the FPG criterion is less sensitive for the detection of diabetes in elderly Korean people than the OGTT-based criterion [8-10]. Therefore, the OGTT remains a valuable test in the diagnosis of diabetes and the classification of IGT, especially in elderly Koreans. Moreover, OGTT should particularly be considered if the subject has a history of impaired fasting glucose, is a high-risk individual, is pregnant, or to exclude an IGT state.
Hemoglobin A1c (HbA1c)
HbA1c is the gold standard index for follow-up of glycemic control. In addition to its role in monitoring and targeting glycemic control, HbA1c has received attention as a diagnostic criterion for type 2 diabetes since the ADA included a HbA1c value threshold ≥6.5% as a factor with which to diagnose diabetes [11]. If we are to consider HbA1c level as a diagnostic criterion, priority must be given to standardization of the assay method.
A second consensus meeting on the worldwide standardization of the HbA1c measurement, which included the ADA, the European Association for the Study of Diabetes, the International Diabetes Federation, the International Federation of Clinical Chemistry and Laboratory Medicine (IFCC), and the International Society for Pediatric and Adolescent Diabetes, stated that the IFCC reference system for HbA1c represents the only valid method to standardize the measurement [12]. The ADA recommends that HbA1c should be measured according to the method certified by the National Glycohemoglobin Standardization Program and standardized or traceable to the Diabetes Control and Complication Trial reference assay [11]. Because the HbA1c assay was not standardized throughout the country, HbA1c was not recommended as a diagnostic criterion for diabetes mellitus in Korea until 2007. However, HbA1c standardization has been widely performed since 2007 by the Korean Association of Quality Assurance for Clinical Laboratory, the Metabolic Disorders Subcommittee, the Korean Society of Laboratory Medicine, and the KDA, including a nation-wide survey for the current status of the HbA1c test [13]. Most commercial laboratories in Korea are certified by Designated Comparison Methods, and accuracy-based proficiency tests are underway. Based on this background, we included HbA1c as a diagnostic criterion and renewed our clinical practice guidelines in 2011.
Several studies have been performed in Korea to determine the cutoff point for HbA1c required to predict an abnormal glucose tolerance status in non-diabetic Korean subjects. Bae et al. [14] analyzed 1,482 subjects without diabetes and reported a cutoff point of 5.95% HbA1c to predict diabetes, with a sensitivity of 60.8% and specificity of 85.6%. One study that included 392 subjects with risk factors for diabetes showed that the current guideline of FPG ≥126 mg/dL for diabetes screening detected only 55.7% of diabetic subjects. The optimal cutoff points for HbA1c and FPG for the diagnosis of diabetes were 6.1% (sensitivity 81.8%, specificity 84.9%) and 110 mg/dL (sensitivity 85.2%, specificity 88.5%), respectively [15]. Ku et al. [16] reported a cutoff point for HbA1c derived from the data collected from 19,178 subjects without diabetes. When the FPG criterion was used, the cutoff value was 5.9% (sensitivity 84.6%, specificity 85.9%), and when the 2-hour glucose level after OGTT was used, the cutoff value was 6.1% (sensitivity 86.5%, specificity 85.8%).
Based on these clinical results, we suggest that the HbA1c cutoff level should be lower than the ADA criterion. However, larger epidemiological studies are required to confirm the suitable cutoff values for the Korean population.
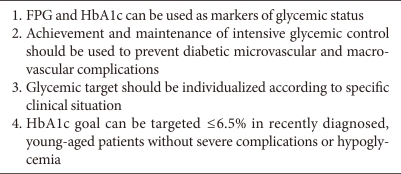
TARGET OF GLYCEMIC CONTROL
Large prospective, randomized controlled clinical trials such as the Kumamoto study [17] and the UK Prospective Diabetes Study (UKPDS) [18,19] have showed that early intensive glycemic control in type 2 diabetic patients significantly reduced microvascular and macrovascular diabetic complications. Based on these results, most of the clinical practice guidelines for glycemic control target of type 2 diabetes since early the 2000s have recommend the achievement of near-normoglycemia to prevent diabetic vascular complications. However, three recently published large RCT studies (ACCORD, ADVANCE, VADT) have demonstrated no significant benefits in cardiovascular outcome with intensive glycemic control in type 2 diabetes [20]. From these findings, we agreed not to overlook the potential risks of very strict glycemic control in specific situations, such as old age with long diabetic duration, combined severe complications, recurrent severe hypoglycemic episodes, or limited life expectancy. However, it should be kept in mind that many meta-analysis consistently provide evidence for the clinical benefits of achieving and maintaining intensive glycemic control to prevent diabetic complications. Therefore, a glycemic goal of HbA1c ≤6.5% should be attained, especially in the recently diagnosed, young type 2 diabetic patients without severe complications or hypoglycemia through lifestyle modification and glucose-lowering agents, including insulin (Table 3, Fig. 1).
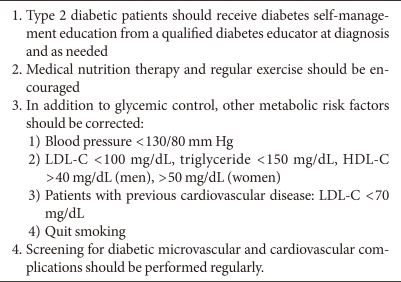
COMPREHENSIVE MANAGEMENT OF METABOLIC RISK FACTORS BEYOND GLYCEMIC CONTROL
In addition to glycemic control within the target range, the comprehensive management of metabolic risk factors is also clinically important. After diagnosis of type 2 diabetes, lifestyle modification, as well as medical treatment, should be emphasized to prevent cardiovascular events. Lifestyle modification could be accomplished by diabetes self-management education, including knowledge, self-care behavior, self monitoring of blood glucose, medical nutrition therapy, exercise, and hypoglycemia. Blood pressure and dyslipidemia should be normalized by lifestyle modification and anti-hypertensive or lipid-lowering agents. Regular screening for diabetic microvascular or macrovascular complications should be performed (Table 4).
CONCLUSION
The dramatic increase in the prevalence of type 2 diabetes and its accompanying acute or chronic complications are major health concerns in Korea. Screening of high risk individuals, early detection, and proper management of type 2 diabetes are urgently needed. Although more evidence and clinical trials should be undertaken, appropriate clinical practice guidelines characterized in Korean people with type 2 diabetes have been developed and updated to provide better glycemic control and favorable clinical outcomes.
Notes
No potential conflict of interest relevant to this article was reported.