Diabetes Prevention in Australia: 10 Years Results and Experience
Article information
Abstract
Clinical trials have demonstrated the efficacy of lifestyle modification for the prevention of type 2 diabetes mellitus but it was achieved at higher cost than can be sustained in routine health services. The first clinical trial to report was the Finnish Diabetes Prevention Study. This paper describes how Australia worked with Finnish colleagues to adapt the findings of that study to achieve a statewide diabetes prevention program. Small evaluative, effectiveness trials have been conducted in a number of countries to see if the results of the clinical trials can be replicated in routine health services. The Australian evaluative trial, Greater Green Triangle Diabetes Prevention Program is described in detail to demonstrate the ingredients for success in moving a program from one country to another. Few countries have managed to scale up from evaluative trials to statewide or national programs. The Australian experience is described in detail including lessons learned about what reduced the effectiveness, particularly the need for policy makers in government, people from the implementing organisation and researchers to work together from the start of the evaluative trial and throughout the first 5 years of a national program.
INTRODUCTION
It is widely recognised that the incidence of type 2 diabetes mellitus (T2DM) is high and increasing both in Australia [1] and throughout the world [2]. T2DM is a chronic and costly disease associated with premature mortality and high rates of health service utilisation linked with cardiovascular disease (CVD), retinopathy, renal failure and neuropathy [3].
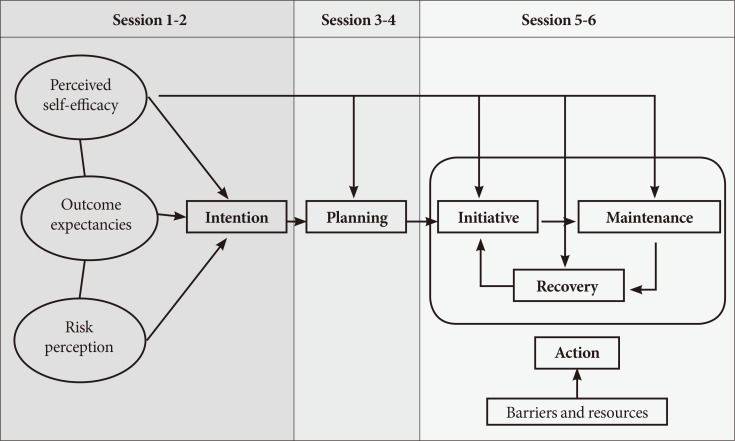
The risk factors associated with T2DM onset are largely preventable. Lifestyle modification, particularly weight loss and physical activity, can significantly reduce the risk of T2DM [4567]. Diabetes prevention trials using lifestyle modification have been proven to be effective in reducing the risk of developing T2DM, and have been shown to be more effective than pharmacological interventions [789]. The Finnish Diabetes Prevention Study (DPS) [45] investigated the role of lifestyle interventions in the progression of T2DM among individuals with impaired glucose tolerance. Results demonstrated that the incidence of T2DM decreased by 58% in the intervention group compared with the control group, a finding which was directly associated with lifestyle modification (Fig. 1). Two other studies have demonstrated similar results [67]. Randomised controlled trials with one-to-one counselling and trials using drugs are expensive [8910]. The lifestyle interventions have all lasted several years [5711] and for example in the Finnish DPS, the median number of counselling sessions during a 3-year intervention was 20 [4]. The aim of this paper is to describe the experience of moving from clinical trials, through evaluative trials to scaling up diabetes prevention at the state or national level.
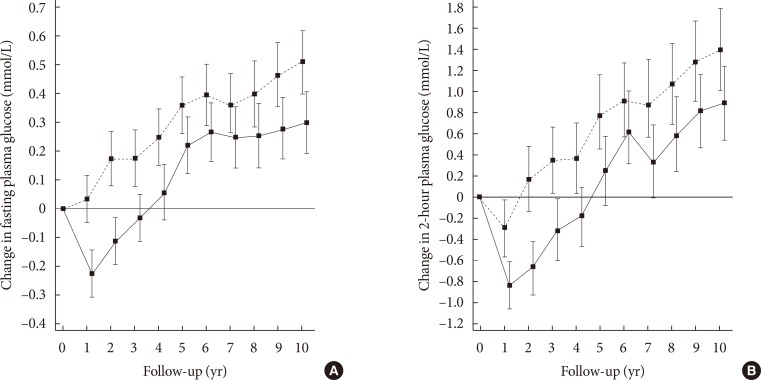
Persistence of the benefit from lifestyle modification over 13 years; 9 years after the randomised control trial ended: comparison of (A) fasting plasma glucose and (B) 2-hour plasma glucose levels among intervention and controls. Adapted from Lindstrom et al. [5], with permission from Springer.
EVIDENCE FROM EVALUATIVE TRIALS
Evaluative trials are effectiveness trials in the real world with a small number of participants usually fewer than 500. If clinical trials show what can be done, evaluative trials show how to do it. To determine whether the results obtained in clinical trials could be replicated in the ‘real world’ of primary health care settings with limited resources and existing personnel, the Good Ageing in Lahti region (GOAL) intervention study, a lifestyle modification trial using a structured group program was designed in Finland [12]. Whilst the implementation of lifestyle modification interventions in routine healthcare posed a greater challenge, the results of this program demonstrated that group lifestyle counselling can be effective and feasible in real-world settings for individuals with an elevated risk of T2DM.
Greater Green Triangle Diabetes Prevention Program
Greater Green Triangle Diabetes Prevention Program (GGT DPP) was based closely on the design of GOAL and established in close collaboration with Finnish colleagues with 237 participants in a pre-test, post-test design. Patients were recruited at local general practices and screened using the Finnish diabetes risk score (FINDRISC).
The intervention consisted of six structured, 90-minute group sessions over 8 months using the Health Action Process Approach (HAPA). The psychological changes resulting from the HAPA approach predicted behaviour changes resulting in 12-month biophysical changes and support the theoretical basis of the intervention (Fig. 2) [1213141516].
The first five sessions occurred within 3 months with 2-week intervals between sessions. The last session took place at 8 months (Fig. 3). The sessions were facilitated by specially trained nurses, dieticians, and physiotherapists. A goal setting approach was used to motivate individuals to progress from intention to actual behaviour change. Regular self-monitoring and feedback was used to empower patients to take responsibility for their own decisions and to make informed choices. Session content for diet and physical activity was based on the dietary guidelines for Australian adults and the national physical activity guidelines. Social support was enhanced by the group setting and by encouraging participants to seek support from their own social networks. Intervention targets followed the lifestyle targets in the Finnish DPS aiming to reduce weight, total and saturated fat intake and increase fibre intake and physical activity. They are (1) no more than 30% of energy consumed from fat; (2) no more than 10% of energy from saturated fat; (3) at least 15 g fibre/1,000 kcal; (4) at least 30 minutes/day of moderate intensity physical exercise; and (5) at least 5% weight reduction. There is a linear relationship between the number of goals achieved and diabetes prevention (Fig. 4).
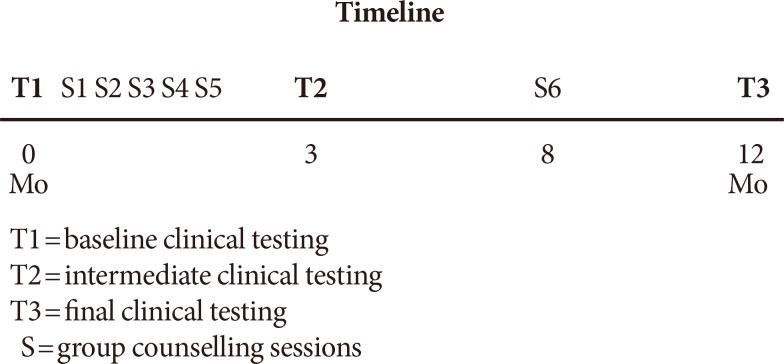
Timeline in months for the Greater Green Triangle Diabetes Prevention Program showing timing of clinical testing and group counselling sessions.
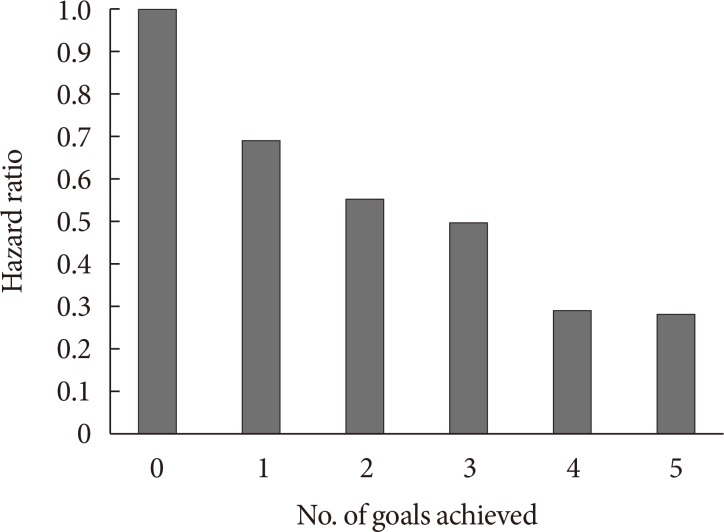
Relationship between the number of goals of the Finnish Diabetes Prevention Study achieved and hazard ratio for progression to type 2 diabetes mellitus after 13 years, adjusted for baseline age, body mass index, 2-hour glucose, and sex. Fig. 4 was drawn by Prof Lindstrom at the National Institute of Health and Welfare, Helsinki. She has advised that permission has been given by the Institute.
At 12 months participants' mean weight was reduced by 2.52 kg and waist circumference by 4.17 cm. Mean fasting glucose reduced by 0.14 mmol/L, plasma glucose 2 hours after oral glucose challenge by 0.5 mmol/L, total cholesterol by 0.29 mmol/L, low density lipoprotein by 0.25 mmol/L, triglycerides were 0.15 mmol/L, and diastolic blood pressure by 2.1 mm Hg.
The study provided evidence that a T2DM prevention program using lifestyle intervention was feasible in primary health care settings, with reductions in risk factors approaching those observed in clinical trials.
Encouraging results from small evaluative efficacy trials conducted in Finland [12], USA [171819], UK [20], GGT DPP [15], and Sydney DPP [21] in Australia, have contributed to evidence in this field. The Diabetes in Europe-Prevention using Lifestyle, Physical Activity and Nutritional Intervention (DE-PLAN study) involved many European countries [22]. A systematic review has shown that many of the evaluative trials have demonstrated positive results but they were on a small scale [23]. Once high-risk individuals attended the interventions, and especially if the intervention dose was large enough and evidence-based protocols adhered to, participants benefited from the lifestyle modification.
FORMATION OF DIABETES PREVENTION POLICY IN AUSTRALIA
The argument that convinced the Australian Government to have a diabetes prevention program arose from the impact on the working population of the growing preventable chronic disease prevalence. At the time, only half of the cases of diabetes were diagnosed and a quarter of the Australian population was at high risk of diabetes. During 2004 to 2006, work was undertaken by the Council of Australian Governments (COAG) on a new economic reform agenda to ensure Australia's prosperity in a global market. COAG subsequently announced a first tranche of human capital reforms include a specific focus on diabetes.
Further in 2006, as part of the work undertaken for COAG, the GGT DPP was identified as the only evidence-based diabetes prevention intervention in Australia. Combined evidence obtained from diabetes prevalence, economic analysis, scientific evidence of diabetes prevention effectiveness from randomised controlled trials, and the GGT DPP results strengthen the case for a national policy on diabetes prevention.
SCALING UP FROM EVALUATIVE TRIALS: IMPLEMENTATION OF LARGE-SCALE DIABETES PREVENTION PROGRAMS
Understanding how to implement interventions on a large-scale is the next step in the process of translating diabetes prevention research into population level strategies which covering a state or nation. Knowledge about the effectiveness of interventions, their acceptability, uptake, reach, cost and how they work in different population subgroups and via which mechanisms, is particularly important for public health research, practice, and policy. Evaluations of this kind can determine program intensity, fidelity, and sustainability in the long term.
Finland was the first country to undertake a large-scale diabetes prevention intervention (DEHKO 2000–2010). A community-based high risk program in primary and occupational care to prevent T2DM, called the National Diabetes Prevention Programme in Finland: FIN-D2D was developed [24]. It achieved an average of 1kg weight loss which represents a 16% reduction in the risk of T2DM.
Implementation of large-scale diabetes prevention programs in Australia
COAG in 2007 agreed to establish a national approach to prevention of T2DM in high risk individuals and the Australian Government funded $217 million from 2007 to 2011 with a number of elements including:
(1) Developing the Australian T2DM Diabetes Risk Assessment tool (AusDRISK)
(2) Establishing national standards for evidence based, intensive lifestyle behaviour change (lifestyle modification programs)
(3) Introducing a new medicare item for T2DM risk assessment in 40 to 49 years age
4) Funding intensive lifestyle behaviour change interventions (lifestyle modification programs) for the 40 to 49 age group through a contract with the peak body for General Practice (Family Medicine).
Some of this was successful but there were major implementation issues with the 40 to 49 age group program and uptake was well below expectations. Funding was discontinued in 2011 (see below).
‘Life!’ Taking Action on Diabetes program
From 2007 to 2011, ‘Life!’ was a Victorian statewide, group based lifestyle intervention targeting 25,000 Victorians over the age of 50 at high risk of T2DM [25]. ‘Life’ consists of predefined protocol of components including a strictly defined intervention based on the GGT DPP, including the HAPA model for behavioural change, standardised facilitator training and manual, and a participant manual to record the lipid, blood pressure, and blood glucose levels plus their individualised goals and outcomes. Payment to facilitators was linked to data returned to use for continuous quality improvement and evaluation. The HAPA behaviour change theories were used to encourage participants to identify the main determinants of intention building and make lifestyle changes associated with healthy diet and active lifestyle; thus, reducing the risk of that T2DM and CVD.
The five goals of the Finnish DPS were retained
Participants were individuals aged 50 years or over with an AusDRisk score of >12- or, aged 18-year-old indigenous Australians with an AusDRisk score of >12, aged 18 years or older with previously diagnosed high-risk conditions such as gestational diabetes or atherosclerosis related CVD.
‘Life!’ provided an opportunity to evaluate the effectiveness of such a large-scale prevention program, and importantly the cost-effectiveness through the Melbourne Diabetes Prevention Study (MDPS) which was an RCT that evaluated the efficacy and effectiveness of ‘Life!’ by monitoring participants' clinical and behavioural outcomes before and after the intervention [26]. Participants were randomly allocated to receive the intervention or receive usual care during the same time period. An economic assessment of ‘Life!’ was also included in the MDPS to determine its ‘value-for-money.’ The MDPS has also provided the opportunity to evaluate implementation of an evidence-based diabetes prevention program in the real world.
PPS analysis demonstrated that intervention participants significantly improved their weight (–1.13 kg), waist circumference (–1.35 cm), systolic blood pressure (–5.2 mm Hg), and diastolic blood pressure (–3.2 mm Hg) compared with controls. Based on observed weight change, estimated risk of developing diabetes reduced by 9.6% in the intervention group and increased by 3.3% in the control participants. Absolute 5-year CVD risk reduced significantly for the intervention participants by 0.97% points. In control participants, the risk increased by 0.11% points. The net effect for the change in CVD was –1.08% points of absolute risk. The MDPS effectively reduced the risk of diabetes and CVD but the intervention effect on weight and waist reduction was modest due to the challenges in recruiting high-risk individuals and the abbreviated intervention (see below).
Four years ago, the Centers for Disease Control and Prevention (CDC) launched the US National Diabetes Prevention Program largely delivered through YMCA. No outcomes have been published yet [27].
This year National Health Service (NHS) England launched the NHS Diabetes Prevention Programme in a pilot phase for 20,000 individuals. It is unclear if the intervention is based on previous English research or whether the intervention has been modified by Public Health England. It will be sometime before the outcomes of the programme are known [28].
In summary, only a small number of countries where evaluative trials have been completed have successfully scaled up programs nationally.
LESSONS LEARNED FROM SCALING UP
‘Program drift’ is the deviation from protocol resulting in reduced effect. ‘Voltage drop’ denotes the reduced benefits of diabetes prevention programs when they move from efficacy trials to the real world [29]. In this section, lessons learned the hard way in Australia are recorded for the benefit of those designing national diabetes prevention programs.
Glasgow argues that there should be no ‘program drift’ or ‘voltage drop’ because programs should be built with quality improvement approaches aiming to achieve the performance levels of randomised controlled trials [29]. Australian experience suggests that effects and benefits could be improved. What is missing is continual measurement of performance in attaining the five goals of the Finnish DPS, and reductions in cholesterol and blood pressure. These are the known predictors of clinical outcomes. The techniques of clinical audit such as ‘Plan-Do-Study-Act’ cycles should be applied to all aspects of program delivery.
The commonest problem is that government plans scaled up programs without taking advice early enough from the researchers who have conducted the evaluative trial. The level of funding and numbers of participants for the ‘Life!’ program were set without reference to the GGT DPP research team. This resulted in one session fewer, and less use of self-monitoring and feedback.
There were other problems. The payments to Life providers did not pay for the last session at 8 months and many of these sessions were not held. There was no check on fidelity of delivery or validation of the data returned by facilitators which was of poor quality. In short, there was no quality improvement program.
Medicare rules did not permit retesting for cholesterol and repeat blood pressure measurements were not taken losing key opportunities for monitoring and feedback to reduce CVD risk.
Too often politics impairs performance. The target of 25,000 participants within 4 years was highly unrealistic and led to a senseless decision to reduce the AusDRISK entry score from >15 to >12. It resulted in a large recruitment of people at low risk both for diabetes and CVD. Indeed, MDPS demonstrated that AusDRISK >15 recruited too many people at low risk [26]. Diabetes prevention programs should only accept participants with AusDRISK scores >15 and impaired fasting glucose, impaired glucose tolerance, or glycosylated hemoglobin 5.7 to 6.4. These criteria also apply to women who have had gestational diabetes [30].
The abbreviated program used in ‘Life!’ has inadequate time for repeated self-monitoring and feedback which is so important for behavioural change. This shows as low attainment of the five goals of the Finnish DPS [26].
When participants leave diabetes prevention programs, the proportion at high cardiovascular risk will have dropped from a third to a quarter. It is important that those continuing at high CVD risk are referred back to their general practitioner (family physician) for medication [31].
In most countries we have seen poor handover from the researchers who have undertaken the evaluative trials to the service providers (implementers) who must scale up across large populations. Usually government processes interrupt the handover. These processes in Australia were so bad that it led to the end of the program for participants aged 40 to 49 years. It happened because the government put the program out to tender without drawing on the experience of the evaluative trial, and the contractor had little relevant experience. Consequently both published and tacit knowledge for implementation were lost. Worse still, the government took the view that the contractor had signed the contract and that all responsibility rested with it. This is exactly contrary to what has been known about effective implementation for over 30 years [32].
Successful implementation requires policymakers, implementers, and researchers to work together to solve the problems which occur when even the best programs are tested the real world [32]. It is not good enough for government to say that it is someone else's problem because they have signed a contract. All too often this approach results in implementation failure and wasted taxpayers' money. This also happens if the implementers do not use to the researchers' advice about how the program needs modified in the light of the research findings.
The implementer also needs to make sure that there is not skills fade in facilitators or mission creep due to external pressures. For instance ‘Life!’ is now promoted as a diabetes and CVD prevention program. It has not been modified in the light of research findings [33].
There remains a paucity of data to assess the long-term clinical and economic impact of diabetes prevention programs [34353637]. While there have been some modelling studies that have determined that lifestyle intervention is cost-effective for those with impaired glucose regulation uncertainties exist about model parameters, real costs and benefits of screening, and practical considerations about the affordability, acceptability, and feasibility of interventions.
CONCLUSIONS
In summary, to develop a national diabetes prevention program in South Korea will require active co-operation between policymakers, implementers, and researchers over several years. This team work should start when plans for the evaluative trial are underway and continue through every stage of scaling up to the national program and its evaluation over the first 5 years.
Notes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.