Assessment of the Association between Mean Hemoglobin A1c Levels for 5 Years and Coronary Artery Disease by Coronary Angiography in Nondiabetic Patients
Article information
Abstract
Background
The effects of glucose on cardiovascular events or mortality in nondiabetic patients has been recently reported. However, since atherosclerosis can be formed over a long period of time, it is necessary to devote several years to unveil the relationship between the two factors. Here, we attempted to find out the relationship between the mean hemoglobin A1c (HbA1c) level and HbA1c variability for 5 years and coronary artery disease (CAD) by using coronary angiography (CAG) to assess nondiabetic patients.
Methods
We reviewed patients who performed CAG who were followed up for at least 5 years after the initial diagnosis. The fasting blood test was performed annually for glucose and HbA1c level. CAD was defined as more than 50% of luminal narrowing. The severity of CAD was divided into two groups depending on whether no vessels were involved or one more vessel were involved (CAD(-) or CAD(+), respectively).
Results
The patients in CAD(+) group had higher mean HbA1c level for 5 years than CAD(-) group (5.71±0.40 vs. 5.86±0.68; P=0.04). Mean HbA1c was a significant predictor for CAD in multiple regression (odds ratio, 2.224; P=0.028). The percentage of patients with CAD was significantly higher in patients with >6.2% of mean HbA1c levels compared to patients with <6.2% of mean HbA1c levels (P<0.019).
Conclusion
When the mean HbA1c levels were above 6.2%, the risk of CAD was higher. Also this study shows that HbA1c level can be one of the predictors for CAD even if the patients do not have diabetes.
INTRODUCTION
Diabetes is a well-known and an important risk factor for coronary artery disease (CAD) [1-6], but several studies have demonstrated the correlation between blood glucose levels and coronary atherosclerosis even in nondiabetic patients [7-12]. Hemoglobin A1c (HbA1c), which reflects the average plasma glucose level for the several months prior to examination, have been used in many epidemiology studies as a parameter for glycemic control, and those studies reported the relationship between HbA1c and the chronic complications of diabetes [13,14]. Furthermore, increased levels of HbA1c are reported to be associated with the presence of coronary atherosclerosis and atherosclerosis burden [5]. In addition, few other studies have shown the relationship between HbA1c and atherosclerosis in nondiabetic patients [4,15-20].
It is well-known that it takes a long while until vessel changes by diseases such as atherosclerosis eventually cause a CAD. Previous studies that were conducted mainly focused on the HbA1c levels, but it failed to yield comprehensive results regarding the effect of chronic changes of vessels, induced by atherosclerosis, on the glucose level. In addition, observing the fluctuations in the blood glucose level over prolonged periods have been emphasized these days over reading the HbA1c level only once to represent the average glucose level for over several months. The authors of Diabetes Control and Complications Trial study suggested the potential of HbA1c variability in diabetic complications to represent longer duration of glucose control. Their study showed that the possibility of association between HbA1c variability and chronic diabetic complication including cardiovascular events and microvascular complications in type 1 diabetes [21,22].
In normal people, their glucose levels would not be constant even for one day and their glucose levels would be oscillating for several years. Thus, the HbA1c levels that are measured for 5 years and the degree of inconsistency would also be different. In this study, we attempted to reveal the relationship between the mean HbA1c levels for over 5 years and its variability during that time and coronary atherosclerosis in nondiabetic patients.
METHODS
This study was performed in a retrospective manner, based on chart review. The data, collected by the cardiology department of Maryknoll Medical Center, regarding the patients who have conducted coronary angiography (CAG) since 2004 was used in this study. The systolic and diastolic blood pressure of these patients were checked every clinic visit according to the principles for baseline assessment which was set up by the department. The patients underwent fasting blood test including routine complete blood count liver function test, kidney function, and lipid profile at least once a year. Their fasting glucose and HbA1c levels were monitored every year as a screening test for diabetes mellitus. Inclusion criteria of our study was that the subjects must have performed CAG due to chest pain and had been followed up in our institute for at least 5 years before the final CAG. CAG was taken when the patients had typical angina chest pain and also atypical chest pain for differential diagnosis. The subjects with known diabetes and diagnosed as diabetes during follow-up based on fasting blood sugar >126 or HbA1c >6.5% were excluded. The patients who had measured their HbA1c level at least three times during the follow-up period were elected. The final 211 patients who were selected did not have a history of diabetes mellitus or any biochemical evidence. The mean HbA1c was calculated, and the HbA1c variability assessed by standard deviation (SD) of HbA1c levels for 5 years. HbA1c at CAG is the serum HbA1c levels measured at the time CAG was performed. CAD was defined as the presence of one or more lesions of more than 50% luminal narrowing in the coronary artery. Our data were analyzed with the SPSS version 18 (IBM Co., Armonk, NY, USA). Comparison of multiple factors between groups divided by CAD was performed by Student t-tests. Logistic regression analysis of CAD with the variables was performed. The proportion of patients who had CAD among the groups divided by the mean HbA1c were analyzed with the chi-square test. P value less than 0.05 was considered as statistically significant. HbA1c was measured by ion exchange high performance liquid chromatography using Variant II (Bio-Rad, Hercules, CA, USA).
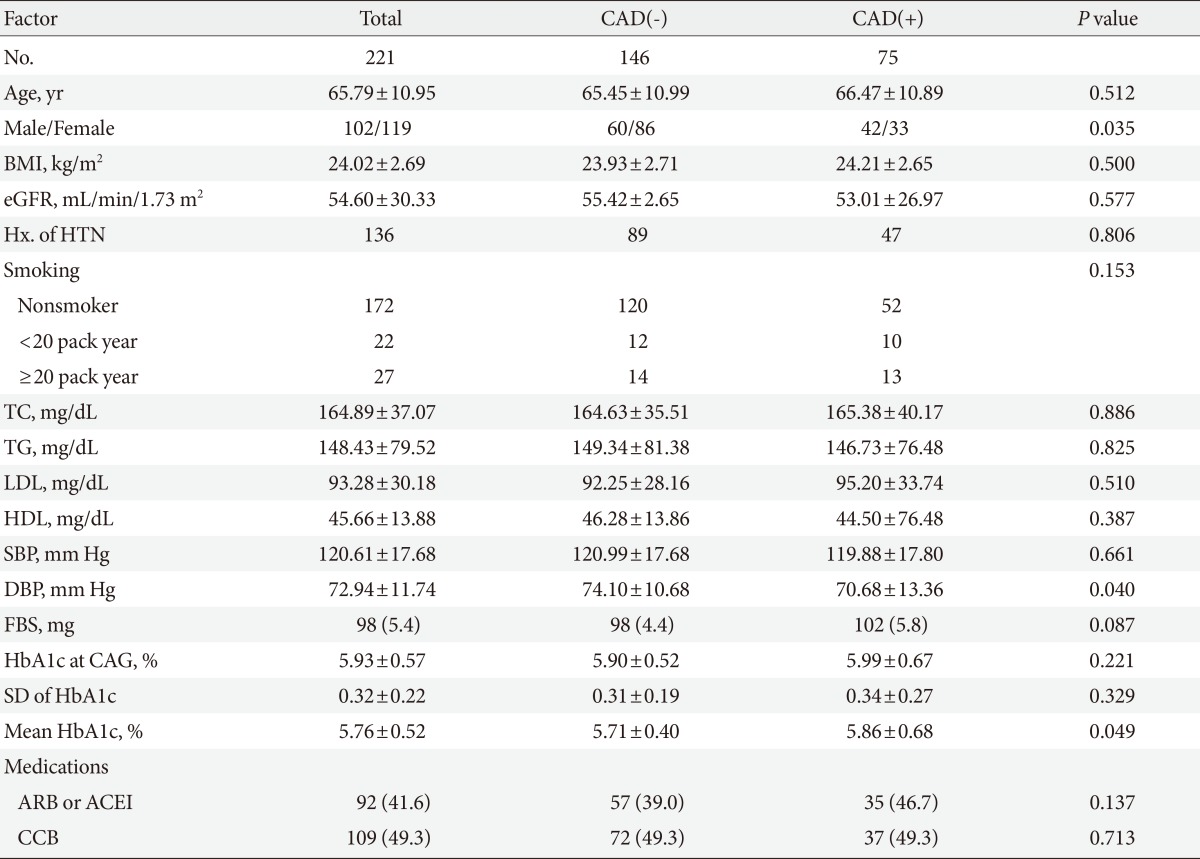
RESULTS
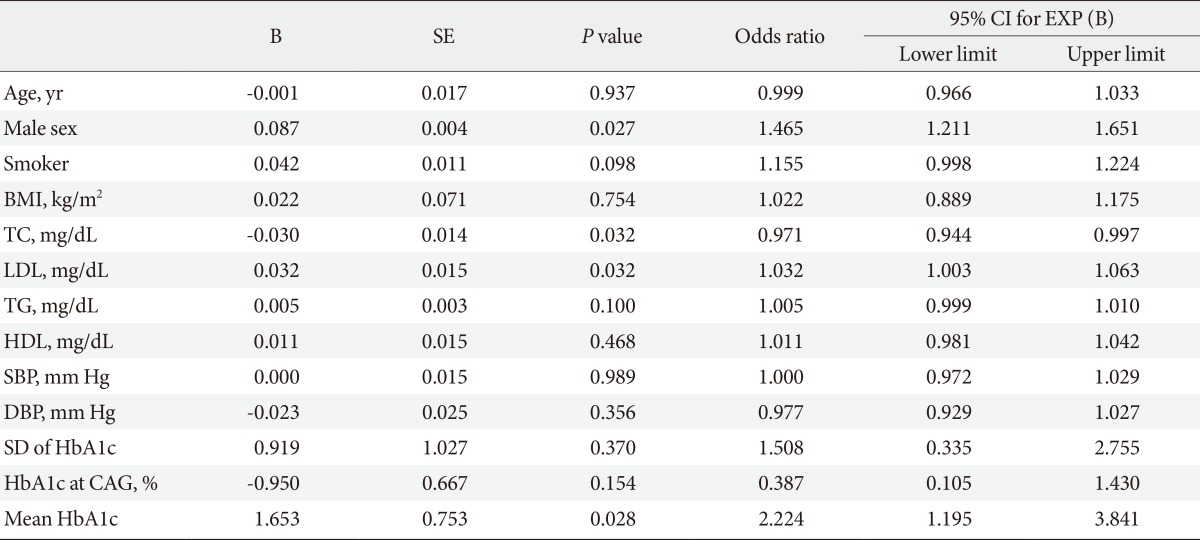
The mean age of our subjects was 65.79±10.95 years, of which 102 of the subjects were male. BMI was 24.02±2.69 kg/m2, and estimated glomerular filtration rate (eGFR) was 54.60±30.33 mL/min/1.73 m2. HbA1c at the time of CAG was 5.93%±0.57%, SD of serial HbA1c level for 5 years was 0.32±0.22, and the mean HbA1c for 5 years was 5.76%±0.52% (Table 1). We divided the subjects into three groups by smoking history. Within these groups, 172 patients were in the nonsmoker group, 22 patients in 1 to 20 pack year group, and 27 patients were in the above 20 pack year group. We also divided the patients into two groups based on the presence or absence of CAD. Interestingly, the percentages of patients in each groups that were divided by smoking history were not different between the CAD(-) and CAD(+) group (Table 1). Between the two groups, the mean systolic blood pressure was not significantly different, but the diastolic blood pressure was significantly lower in the CAD(+) group compared to the CAD(-) group (70.68±13.36 mm Hg vs. 74.10±10.68 mm Hg). Other characteristics including age, percentage of male, BMI, eGFR, and lipid profiles were not significantly different between the CAD(-) and CAD(+) groups. In addition, neither the HbA1c level at the time when CAG was taken (5.90%±0.52% in CAD(-) group and 5.99%±0.67% in CAD(+) group) nor its SD showed any significant difference. However, the mean of HbA1c for 5 years in CAD(+) group was significantly higher than CAD(-) group (5.86%±0.86% vs. 5.71%±0.40%; P=0.049) (Table 1). With these result, the patients were divided into four groups: <5.7%; ≥5.7% and <6.0%; ≥6.0% and <6.2%; ≥6.2% and <6.5% of HbA1c for 5 years. Further analysis with the new groups showed that the percentage of patients with CAD was significantly higher in patients with mean HbA1c levels between 6.2% and 6.5% compared to other groups (P<0.019). On the other hand, other groups did not show any difference in the percentage of CAD(+) patients (Fig. 1). Male sex, total cholesterol, LDL cholesterol, and mean HbA1c were the independent predictors for CAD in nondiabetic patients who were adjusted by age, BMI, blood pressure, HbA1c at CAG, and SD of HbA1c (Table 2).
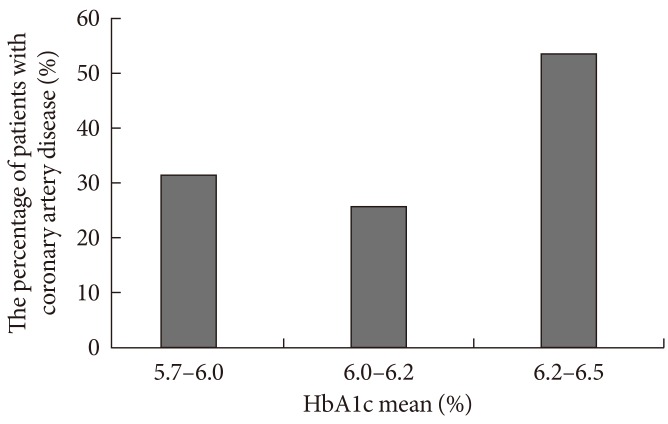
The percentage of patients with coronary artery disease in groups divided by the mean hemoglobin A1c (HbA1c) levels.
DISCUSSION
Our study showed that higher mean HbA1c levels for 5 years might be related to CAD even in nondiabetic subjects. In our study, the mean HbA1c levels taken over the previous 5 years were better predictors for coronary atherosclerosis than the HbA1c levels measured at the time CAG was taken. For several years now, a few reports have studied the relationship between HbA1c and atherosclerosis in nondiabetic patients. Moreover, one study followed up on older, nondiabetic adults for 8 years to elucidate the relations between HbA1c, fasting plasma glucose, postchallenge plasma glucose, and mortality from cardiovascular disease (CVD) and ischemic heart disease (IHD) [4]. The authors concluded that the highest quartile of HbA1c (≥6.7%) is a predictor for CVD and IHD mortality in women without diabetes, but not in men. In addition, another study concluded that increased levels of HbA1c in asymptomatic individuals without diabetes are associated with the presence of coronary atherosclerosis where a burden of mixed coronary plaques gathers [8]. Additionally, accumulating evidence suggested high levels of HbA1c as an indicator of significantly increased risk for ischemic stroke in nondiabetic male adult and presented HbA1c as a potential predictive factor for even those in the nondiabetic range [15,23].
When we divided the patients into four groups according to their mean HbA1c levels for 5 years, the patients with a mean HbA1c value of ≥6.2% showed a significantly increased percentage of CAD(+) patients compared to those with lower HbA1c levels. It has been well known that prediabetes is also a risk factor for cardiovascular pathologies like diabetes [12,24,25]. However, fasting hyperglycemia and postprandial hyperglycemia, so called impaired fasting glucose and impaired glucose tolerance, which are better predictors for cardiovascular event are largely debated [11,12]. More studies suggested that postprandial hyperglycemia is a better predictor or even the only predictor for risk of CVD [4,16]. However, in our study, the postprandial glucose levels were not taken as there are difficulties in measuring the exact postmeal glucose level in clinical practice. Nevertheless, our results indicated that the mean HbA1c levels for 5 years were related to CAD, but not fasting glucose levels. It has been reported that the postprandial glucose level is elevated in earlier stages than fasting glucose levels in the natural course of type 2 diabetes. Although HbA1c is the average glucose levels including fasting and postprandial glucose levels, the contribution of postprandial glucose is bigger than fasting glucose in lower HbA1c levels. Considering such knowledge, our results which demonstrate the correlation between HbA1c and CAD but not with fasting glucose may be consistent to the previous findings in other studies. The reason why the already known risk factors for CAD such as age and blood pressure did not act as predictors in our study is not clear. One possible explanation might be the small numbers of our study subjects due to our selection criteria. As a result, the age was higher in CAD(+), although not significant. Also, the blood pressures were well-controlled in our study, perhaps preventing it from acting as a predictor.
There are some reports that suggest the variability of HbA1c as a risk factor for diabetic complications. Oscillating glucose levels can lead to endothelial dysfunction and more oxidative stress, which can be more deleterious than a constantly high glucose level [26]. Kilpatrick et al. [21] reported that the variability of HbA1c can be used to predict the complications in type 1 diabetes. Furthermore, it is known to be an important risk factor for all cause mortality in type 2 diabetic patients [27]. We also attempted to elucidate the relationship between HbA1c variability and coronary atherosclerosis in nondiabetic patients, but in our study the HbA1c variability did not show any difference between the CAD(+) and CAD(-) groups and was not even a predictor for CAD. We suspect that this could be because HbA1c variability was represented as SD, which was very small in lower HbA1c levels of nondiabetic patients.
Our study has several limitations. First, the subjects in our study were enrolled from a single center. Second, this study is an observational study, not a randomized controlled study. Here, CAD was defined as the presence of one or more lesions of more than 50% luminal narrowing in coronary artery. Yet, the degree of CAD was not separated, and to confirm the diagnosis for diabetes mellitus, we should have performed a 75 g oral glucose tolerance test (OGTT). However, OGTT is not convenient because patients must drink uncomfortable test liquid and wait for 2 hours. So, we used fasting glucose level and HbA1c to screen for diabetes. However, because the cholesterol variability for 5 years was not checked, it is impossible to tell if cholesterol changes may also affect coronary atherosclerosis.
In conclusion, our study showed that the mean HbA1c levels for 5 years may be a significant predictor for CAD even in patients that are not diagnosed with diabetes, but HbA1c levels measured at the time of CAG and the HbA1c variability for 5 years are not suitable.
Notes
No potential conflict of interest relevant to this article was reported.