Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
Article information
Abstract
Background
Only few studies have shown the efficacy and safety of glucose-control strategies using the quadruple drug combination. Therefore, the aim of the present study was to investigate the usefulness of the quadruple combination therapy with oral hypoglycemic agents (OHAs) in patients with uncontrolled type 2 diabetes mellitus (T2DM).
Methods
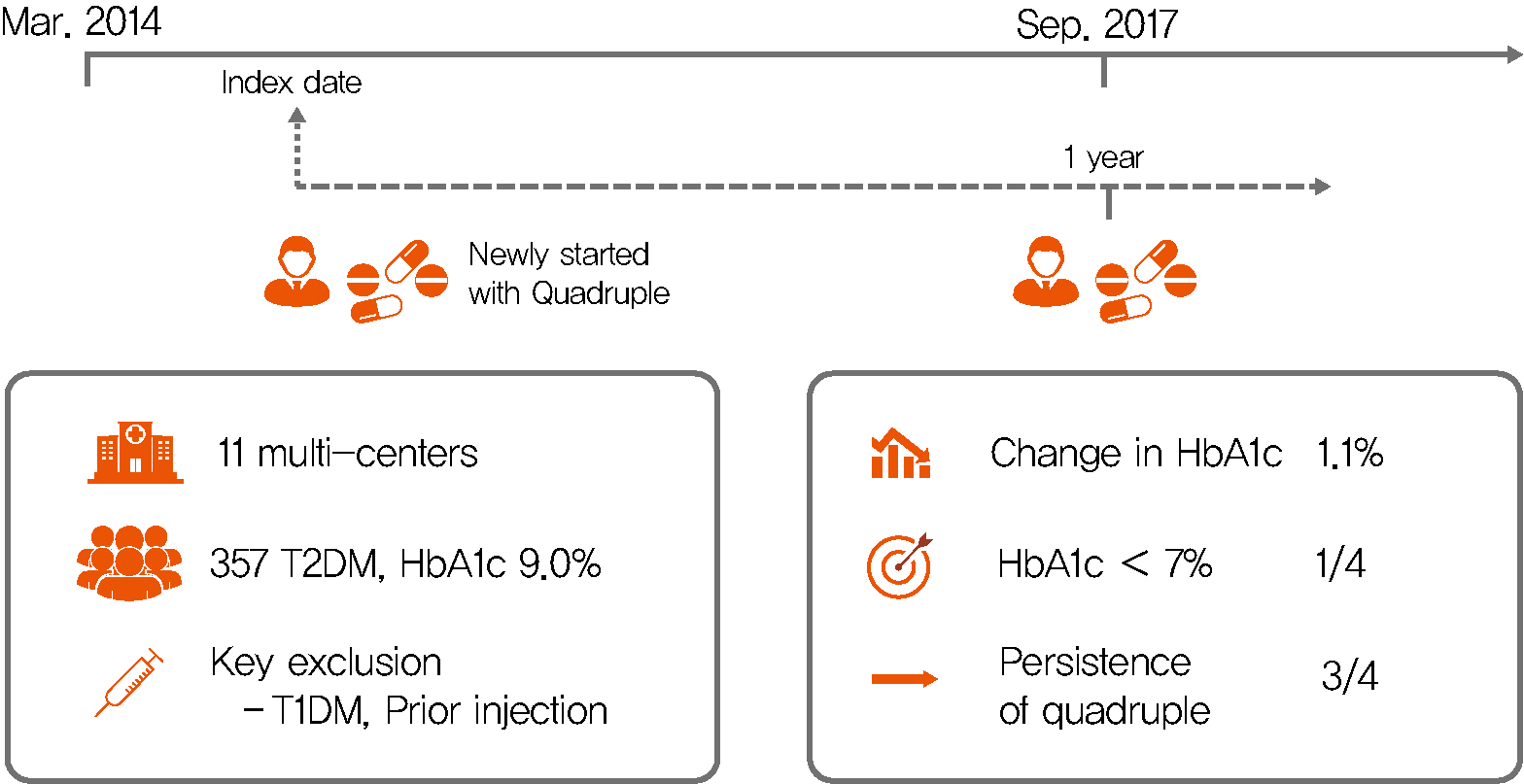
From March 2014 to December 2018, data of patients with T2DM, who were treated with quadruple hypoglycemic medications for over 12 months in 11 hospitals in South Korea, were reviewed retrospectively. We compared glycosylated hemoglobin (HbA1c) levels before and 12 months after quadruple treatment with OHAs. The safety, maintenance rate, and therapeutic patterns after failure of the quadruple therapy were also evaluated.
Results
In total, 357 patients were enrolled for quadruple OHA therapy, and the baseline HbA1c level was 9.0%±1.3% (74.9±14.1 mmol/mol). After 12 months, 270 patients (75.6%) adhered to the quadruple therapy and HbA1c was significantly reduced from 8.9%±1.2% to 7.8%±1.3% (mean change, −1.1%±1.2%; P<0.001). The number of patients with HbA1c <7% increased significantly from 5 to 68 (P<0.005). In addition, lipid profiles and liver enzyme levels were also improved whereas no changes in body weight. There was no significant safety issue in patients treated with quadruple OHA therapy.
Conclusion
This study shows the therapeutic efficacy of the quadruple OHA regimen T2DM and demonstrates that it can be an option for the management of T2DM patients who cannot use insulin or reject injectable therapy.
INTRODUCTION
Type 2 diabetes mellitus (T2DM) is caused by both decreased secretion of insulin and insulin sensitivity; this pathologic condition is complicated by the associated abnormalities in various organs. Although pancreatic β-cell dysfunction and failure are the key defects in T2DM, recent studies have shown that unexpectedly the intestine, brain, kidney, and immune system are also the new targets for the treatment of diabetes [12]. Several new oral hypoglycemic agents (OHAs) have been developed over the past decades, and unlike the conventional drugs, they have unique mechanisms of action that are targeted toward a specific organ. In addition, most clinical studies have reported that the synergy of combination therapy is more efficacious and safer than monotherapy [3]. Thus, a therapeutic approach targeted toward the diverse pathogenesis of T2DM leads to successful glycemic control.
Insulin injection is the most effective treatment available for managing hyperglycemia [4]. The early start of the insulin treatment provides greater benefits, such as relieving glucotoxicity and delaying or preventing T2DM. However, despite the advantages of insulin therapy, poor adherence is a big challenge for both the physician and patients; over half of the patients for whom the insulin therapy is recommended, fail to continue the therapy and one-third of the insulin-naive patients do not become ongoing users [56]. A study reported that almost 60% of the patients skip the injections intentionally and the regular omission was up to 20%. In addition, the stigma and fear associated with insulin injection is still a big hurdle for adequate diabetes management [3].
Most of the current guidelines recommend the injection therapy after triple combination and do not specify the addition of OHAs [7]. In Korea, OHA add-on to the triple combination is not covered by the health insurance according to these guidelines but there are still clinical unmet needs due to limitations of the injection therapy. If a synergistic effect can be achieved based on the mechanism of action, the quadruple OHA combination may be another option that can delay or replace the use of insulin. However, little is known about the clinical efficacy and safety of the quadruple OHA combination.
The current study aimed to identify the status, glycemic efficacy, and safety of quadruple OHA combinations in Korean patients with uncontrolled T2DM patients who were already using three different OHAs. First, we compared glycosylated hemoglobin (HbA1c) levels before and 12 months after administering different classes of OHAs as add-on to the triple combination regimen. Second, we also evaluated the safety and changing therapeutic patterns after quadruple OHA treatment.
METHODS
Study design
The current study was designed as a multicenter, retrospective study to collect information on the current status of the quadruple combination of OHAs in Korea. This study was conducted at 11 geographically representative centers selected throughout the Yeongnam and Honam regions of South Korea. The study protocol and other related documents were reviewed and approved by the local ethics committee of each hospital (representative IRB No. for Pusan National University Hospital: H-1906-007-079). Written informed consent by the patients was waived due to a retrospective nature of our study.
Patients and eligibility
The patients who had T2DM and were 18 years or older age were eligible for the study if they had OHA treatment for at least 6 months and were recommended to the newly introduced 4th OHAs by their physician between March 2014 and December 2018 at each hospital. The key exclusion criteria were as follows: (1) type 1 diabetes mellitus; (2) prior use of insulin over 2 weeks; (3) prior use of glucagon-like peptide-1 receptor agonist (GLP-1 RA); and (4) prior use of prescription of four or more OHAs.
Data collection
The index date was defined as the day when each patient was first prescribed the 4th OHA at each center during the enrollment period. Then, each patient was followed for 12±2 months from the index date. The data included the demographics, anthropometric data, laboratory test, and medical history. These data were collected from the patient's electronic medical records at baseline (the index date) and 12-month post-baseline by the investigators listed on the case report form. The change in HbA1c levels, as well as the safety and changing therapeutic pattern after administration of the 4th OHA were evaluated. Regarding the diabetic complications or comorbidities, coronary artery disease (CAD) was defined as angina pectoris and/or myocardial infarction and was diagnosed based on the medical records or coronary angiography, whereas stroke was defined based only on the medical records. Peripheral artery disease (PAD) was diagnosed using ultrasound or computed tomography angiography. When assessing the microvascular complications, retinopathy was diagnosed using fundus photography or ophthalmoscopy, and diabetic neuropathy was determined based on the symptoms and signs evaluated by the physicians or medication history related to diabetic neuropathy. The safety issues that were collected are as follows: (1) new onset of macrovascular events (CAD, stroke, and PAD); (2) new onset of microvascular complications including end stage kidney disease, dialysis, eye treatment for proliferative diabetic retinopathy (PDR), and amputation; (3) emergency room (ER) visit or hospitalization for hyperglycemia or hypoglycemia.
Statistical analysis
The continuous variables are presented as mean±standard deviation and the categorical variables are presented as numbers and percentages. Paired sampled t-test was used for comparing the baseline and 12 months after quadruple combination therapy, and McNemar test were applied for comparing between-group HbA1c levels (≥7%, <7%). The survival plot was derived from the Kaplan-Meier estimates and the hazard ratio (HR) was calculated by the Cox proportional hazard model for discontinuation of quadruple therapy. All statistical analyses were performed using SPSS version 25.0 for Window (IBM Co., Armonk, NY, USA), and a P value less than 0.05 was considered significant.
RESULTS
Baseline patient demographics
A total of 357 eligible patients (56.3% subjects were men) were consecutively enrolled from multiple centers. The mean age of the study population was 58.9 years, mean HbA1c level was 9.0% (74.9 mmol/mol), and mean duration of diabetes was 13.1 years. Other clinical variables were as follows: body mass index (BMI), 25.1±3.3 kg/m2; systolic blood pressure (SBP), 125.9±14.1 mm Hg; diastolic blood pressure, 73.7±9.5 mm Hg; total cholesterol, 159.3±40.1 mg/dL; low density lipoprotein cholesterol (LDL-C), 91.3±30.5 mg/dL; high density lipoprotein cholesterol, 45.6±11.3 mg/dL; triglyceride (TG), 165.4±98.0 mg/dL; estimated glomerular filtration rate, 90.0±22.8 mL/min/1.73 m2; aspartate aminotransferase (AST), 25.9±13.6 units/L; alanine transferase (ALT), 30.1±17.7 units/L; and gamma-glutamyl transferase (GGT) 45.6±49.8 units/L (Table 1). Many patients (277 patients, 76.6%) had dyslipidemia and approximately half of the subjects (210, 58.8%) had hypertension at baseline. The information regarding habitus was obtained for 196 patients (54.9%). A total of 75 patients (38.3%) were current or ex-smokers. The prevalence of neuropathy, which is classified as a microvascular complication, was the highest (31.7%), followed by retinopathy (24.4%).
Table 2 shows the prescription status of the study population at baseline. As for the composition of prior triple OHA combination, 97.1% of patients were treated with metformin (MET), 88.8% with insulin secretagogues (sulfonylurea [SU] or glinide), 80.1% with the dipeptidyl peptidase 4 inhibitor (DPP4i), 21.6% with thiazolidinedione (TZD), 7.3% with the sodium-glucose cotransporter 2 inhibitor (SGLT2i), and 5.0% with the α-glucosidase inhibitor, at baseline. Regarding the triple OHA combination, the most frequently prescribed triple combination was MET+SU/glinide+DPP4i (66.9%), followed by MET+SU/glinide+TZD (10.9%), MET+DPP4i+TZD (8.8%) (Supplementary Table 1). When OHA was newly added as the quadruple combination, TZD was most frequently considered as the newly added agent (55.2%), followed by SGLT2i (22.7%), DPP4i (12.8%), and SU/glinide (5.7%) (Table 2). The most frequently prescribed quadruple combination was MET+SU/glinide+DPP4i+TZD (63.3%), followed by MET+SU/glinide+DPP4i+SGLT2i (18.8%) (Supplementary Table 2).
Overall efficacy and safety of quadruple combination therapy
After being prescribed quadruple combination, 270 patients (75.6%) maintained this therapy throughout the 12 months observational period. The mean maintenance period of quadruple combination regimen from the index date was 375.98±55.10 days during the study period (Supplementary Fig. 1). Among the participants who were maintained quadruple therapy, the mean change in the HbA1c level was −1.1%±1.2% (−12.07±13.06 mmol/mol) and HbA1c level was significantly (P<0.001) reduced from 8.9%±1.2% (74±13.0 mmol/mol) to 7.8%±1.3% (63±14.1 mmol/mol) (Table 3, Fig. 1A). The majority of patients (n=235; 87.0%) showed improvement of glycemic control compared to baseline levels. Moreover, the proportion of the patients showing HbA1c <7% (<53 mmol/mol) increased significantly from 1.9% (n=5) at baseline to 25.2% (n=68) at 12 months (P<0.005) (Fig. 1B). Further, 202 patients showed a decrease of about −0.9%±1.2% (−10.05±12.88 mmol/mol) in HbA1c levels as compared to that of the baseline status, although the HbA1c level was not <7.0% at 12 months. After 12 months of treatment with quadruple combination, there were significant changes in the lipid profiles (LDL-C, from 92.3±36.0 to 84.5±30.3 mg/dL, P=0.008; TG, from 162.8±99.4 to 132.7±78.2 mg/dL, P<0.001) (Table 3). In addition, AST, ALT, and GGT levels were significantly decreased at 12 months compared to baseline levels (24.4±13.7 to 22.0±9.3 units/L, P=0.005; 27.5±15.4 to 23.4±11.9 units/L, P=0.001; 49.4±52.1 to 37.8±41.1 mg/dL, P=0.011), respectively. The body weight, BMI, blood pressure, and renal function at 12 months did not change significantly as compared to values at baseline. Similar results were observed when all participants were analyzed, including who failed to maintain quadruple OHA regimens during the study period (Supplementary Table 3).

Changes in anthropometric and laboratory variables of quadruple regimen-maintained participants during study period (n=270)

Efficacy of quadruple combination during study period. (A) Change in glycosylated hemoglobin (HbA1c, %) at baseline and at 12 months. (B) The proportion of subjects achieving HbA1c <7.0% (<53 mmol/mol). aP<0.001.
In this study, three patients (0.8%) had new onset of macrovascular events and only two patients experienced new onset of microvascular events, which comprised PDR (Table 4). There was no visit to ER or hospitalization related to hyperglycemia or hypoglycemia. During this study period, one patient died of aspiration pneumonia.
Discontinuation of quadruple combination
When we conducted an analysis of the discontinuation of quadruple therapy with various clinical variables, the baseline glycemic status and drinking status presented relatively high risk ratio of discontinuation, which was not statistically significant (HR, 1.132; 95% confidential interval [CI], 0.979 to 1.310; P=0.095) (HR, 1.895; 95% CI, 0.890 to 4.033; P=0.097, respectively) (Supplementary Table 4). When the quadruple combination was interrupted within the study period, 23% of these patients were initiated into the injection therapy (17 patients for insulin; three patients for GLP-1 RA) (Supplementary Table 5). About half of those who had been discontinued from the quadruple combination therapy stopped taking OHA that was newly added as the initial quadruple combination. The most frequently discontinued agents were TZD (23 patients, 26.4%), followed by SGLT2i (13.8%), and DPP4i (6.9%). The discontinuation of the other agents except OHA, which was newly added as the initial quadruple combination, was also considered for discontinuation during the study period (25.3%). Among these agents, MET was mostly discontinued (seven patients, 8.0%), followed by DPP4i (four patients, 4.6%), and SGLT2i (four patients, 4.6%).
DISCUSSION
In this study, we have demonstrated that the add-on of OHA as the 4th drug achieved significant glycemic control in adequately controlled T2DM patients who were already receiving a regimen containing three different OHAs. In addition, majority of the participants could maintain the quadruple regimen for one year without significant side effects and this combination treatment proved safe. To our best knowledge, this is the first multi-center study investigating the current status, glycemic efficacy, and safety of the quadruple OHA combination in the real-world settings.
Only one of four (25.1%) people with diabetes are reported to have ideal glycemic control (HbA1c <6.5%), and about half of the patients in Korea have suboptimal glycemic control even at a HbA1c of 7% set as the optimal target [89]. When the triple OHA cocktails fail to achieve glycemic control, the guidelines commonly recommend injectables, such as insulin and GLP-1 RA, and many patients with T2DM eventually require and benefit from the insulin therapy [3]. However, many obstacles from both the patients' and physicians' side hinder the achievement. The patients' refusal (33.6%) and physicians' concerns of patients' non-compliance (26.5%) were the major physician-reported reasons for delaying the insulin therapy. The inconvenience associated with insulin therapy (51.6%) and fear of injection (48.2%) were the major reasons for the patient refusal [10]. However, we have had additional OHA options, such as SGLT2i or oral GLP-1 RA in our arsenal for the glycemic control for over the past decade, even before initiating the insulin therapy [11]. From the patient-centric approach, it is time to introduce the new concept of a quadruple OHA combination with guaranteed efficacy and safety, rather than accepting the low compliance resulting from a negative attitude toward the injection therapy.
Recently, a small number of studies revealed the possibility of the quadruple OHA combination therapy. In the T2DM patients using a maximal dose of MET, glimepiride and DPP4i, and SGLT2i (dapagliflozin or empagliflozin) as add-on provided significant benefits in terms of glycemic efficacy, and reduction in body weight and SBP [121314]. Furthermore, these regimens were found to be superior in safety (less hypoglycemic events) and at least non-inferior in glycemic efficacy compared with basal insulin. A study comparing empagliflozin and dapagliflozin as the 4th add-on agent demonstrated that the quadruple regimen could provide glycemic control for up to 52 weeks without any specific regimen related side effects [14]. Thus, MET/SU/DPP4i/SGLT2i combination was suggested to be a reasonable option for patients who want to delay the injection therapy. Similar to these results, the quadruple OHA regimen showed significant glycemic efficacy with 1% reduction in HbA1c and higher proportion of target achievement (<7%), regardless of the combination in our study. Considering that MET/SU/DPP4i/TZD combination was the most frequent prescription in the clinical setting, it suggests that any combination of four drugs may have sufficient glucose-lowering effects unless the mechanisms overlap.
We found that the quadruple OHA regimen improved the metabolic parameters, such as TG, LDL-C and the liver function as well as hyperglycemia. Previous studies have reported improvements in the blood pressure, lipid profile, and liver function, as well as body weight, as compared to those with basal insulin, and these gains can be attributed to SGLT2i [13]. The changes in SBP and body weight were not identified, and we were not able to determine which agent provided these benefits. TZD was most frequently used as the 4th add-on agent in this study, and it might have led to some differences compared with the previous studies using SGLT2i. TZD is well-known for its cardiovascular benefits [15]. DPP4i has also been reported to improve the metabolic parameters in previous clinical trials [161718], suggesting that a quadruple regimen with a newer OHA class could provide additional benefits beyond the glycemic control. It is not clear the reason for these findings, but a number of studies have suggested the possible mechanisms about these metabolic benefits from each OHAs. Interestingly, inhibition of SGLT2 increased LDL-C in a diabetic mouse model expressing human cholesteryl ester transfer protein and human apolipoprotein B100, and it was associated with increased lipolysis and reduced LDL turnover [19]. Given that SGLT2i also increased LDL-C in clinical studies, the improvement in lipid profile was probably due to the effect of TZD or DPP4i.
Regarding safety issues, we could observe that most participants could maintain the quadruple OHA combinations for 1 year without specific adverse events. It is consistent with the previous studies, the incidence of hypoglycemia and weight gain has been reported more in the insulin use group than the oral combination groups [1213]. In addition, there are now multiple large randomized controlled trials reporting statistically significant reduction in the cardiovascular events in patients with T2DM treated with some of these new class of drugs [20]. Taken together, our findings suggest that any quadruple combinations are, at least, less risky than the injectables, and some OHAs might provide additional cardiovascular benefits over insulin.
An important question to consider is which patients can benefit from the quadruple combination. First, it would be helpful to the patients who cannot inject themselves due to blindness, dementia, motor weakness, or paralysis due to diabetic complications. The oral regimen instead of injection can relieve the need for the caregiver and cost of assisting with the injection treatment. Another target is the elderly T2DM patients. With the aging society, especially in Korea, polypharmacy and inadequate use of injectable therapy are increasingly becoming an unexpectable medical burden for the elderly patients. This leads to a vicious cycle in which the decrease in drug compliance hinders the efficacy of sufficient drug effects, which in turn increases the medical costs [21]. Fortunately, the fixed dose combination formula (even now available as 3-in-1 tablet) is an easily affordable option in Korea and it could significantly reduce the number of pills, which has improved compliance and medical cost [222324].
Our study has limitations. First, our retrospective observational study does not allow superiority compared with the injectables. Second, the long-term effects and safety of more than 1 year cannot be guaranteed. Especially in the safety issues, we could not determine the reason why physicians stopped the quadruple regimens during the study period because this study was an observational study aimed to show the real-world data in Korea. Thus, unfortunately, it is not able to provide information about specific side effects relevant to OHA classes or unexpected drug-drug interactions. Third, the study was not intended to compare the best combinations, so it is not possible to conclude which combinations of OHAs are better. Fourth, we did not investigate the changes in medications other than OHAs during the follow-up period. Some medications such as corticosteroid or statins could directly worse glycemic control, and it might be an important factor to quit the previous regimen or advancing to injectable therapy. Finally, our study has limitations in determining which patient characteristics (depending on the disease duration or insulin secretion capacity) are helpful for the quadruple combination therapy. However, this study was aimed at assessing the current status, effectiveness, and safety of the quadruple regimen in the real world setting rather than demonstrating whether a particular combination of OHAs could replace the injectables. The strength of this study is that it has demonstrated the natural course of the quadruple therapy in clinical practice, and this regimen suggested a new concept, that is, a strategy to consider after a triple combination fails, regardless of the specific OHA. Further larger scale, prospective trials are warranted for these unanswered questions.
In conclusion, this study demonstrated that a regimen comprising four different OHAs was effective and safe as a therapeutic strategy for Korean T2DM patients after triple OHA combination failure. However, this combination should always be prescribed on an individual basis, which should be continuously reviewed for efficacy, side effects, and patient burden [25]. In addition, the physicians should not delay the proper use of injectable therapy, if necessary.
ACKNOWLEDGMENTS
This study was supported by a research grant obtained from the Young-Honam Endocrinology and Metabolism Association in 2018, and clinical research grant from Pusan National University Hospital in 2020. The following investigators and study centers associated with the Young-Honam Endocrinology and Metabolism Association participated in this analysis: Jun Sung Moon, Seung Min Chung, and Kyu Chang Won (Department of Internal Medicine, Yeungnam University College of Medicine, Daegu); Sunghwan Suh and Duk Kyu Kim (Department of Internal Medicine, Dong-A Medical Center, Dong-A University College of Medicine, Busan); Sang Soo Kim, Jeong Mi Kim, Min Hee Jang, and In Joo Kim (Department of Internal Medicine, Pusan National University Hospital, Busan); Heung Yong Jin, Kyung Ae Lee, and Tae Sun Park (Department of Internal Medicine, Chonbuk National University, Medial School, Jeonju); Young Sang Lyu, Jin Hwa Kim, and Sang Yong Kim (Department of Internal Medicine, School of Medicine, Chosun University, Chosun University Hospital, Gwangju); Jung Eun Jang and Tae Nyun Kim (Department of Internal Medicine, College of Medicine, Inje Universtiy, Busan); Sung Woo Kim, Eonju Jeon, and Hosang Shon (Department of Internal Medicine, School of Medicine, Catholic University of Daegu, Daegu); Mi-Kyung Kim and Hye Soo Kim (Department of Internal Medicine, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu); Il Seong Nam-Goong, Eun Sook Kim, and Young Il Kim (Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan); Jin-Ook Chung, Dong-Hyeok Cho, and Dong-Jin Chung (Chonnam National University Medical School Department of Internal Medicine, Gwangju); Chang Won Lee (Department of Internal Medicine, Busan St. Mary's Hospital, Busan, Korea).
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conception or design: J.S.M., S.S., S.S.K., H.Y.J.
Acquisition, analysis, or interpretation of data: J.S.M., S.S., S.S.K., H.Y.J., J.M.K., M.H.J., K.A.L., J.H.L., S.M.C., Y.S.L., J.H.K., S.Y.K., J.E.J., T.N.K., S.W.K., E.J., N.H.C., M.K.K., H.S.K., I.S.N.G., E.S.K., J.O.C., D.H.C., C.W.L., Y.I.K., D.J.C., K.C.W., I.J.K., T.S.P., D.K.K., H.S.
Drafting the work or revising: J.S.M., S.S., S.S.K., H.Y.J.
Final approval of the manuscript: J.S.M., S.S., S.S.K., H.Y.J., J.M.K., M.H.J., K.A.L., J.H.L., S.M.C., Y.S.L., J.H.K., S.Y.K., J.E.J., T.N.K., S.W.K., E.J., M.K.K., H.S.K., I.S.N.G., E.S.K., J.O.C., D.H.C., C.W.L., Y.I.K., D.J.C., K.C.W., I.J.K., T.S.P., D.K.K., H.S.
References
SUPPLEMENTARY MATERIALS
Supplementary materials related to this article can be found online at https://doi.org/10.4093/dmj.2020.0107.
Supplementary Table 1
Prescription status of triple combination of OHAs in study population at baseline
Supplementary Table 2
Prescription status of quadruple combination of OHAs in study population at baseline
Supplementary Table 3
Changes in anthropometric and laboratory variables of all participants during study period (n=357)
Supplementary Table 4
Univariate analyses of the associations of quadruple therapy discontinuation with various clinical parameters
Supplementary Table 5
Prescription pattern after discontinuation of 4th OHA
Supplementary Fig. 1
Persistence of quadruple of oral hypoglycemic agents during study period.