Increasing Trend in the Number of Severe Hypoglycemia Patients in Korea
Article information
Abstract
Background
To investigate whether the number of subjects with severe hypoglycemia who are brought to a hospital emergency department is increasing and to identify whether there have been changes in the demographic and clinical characteristics of those subjects.
Methods
We analyzed data from the Emergency Departments of two general hospitals in Seoul, Korea. We included data from all adult subjects with type 2 diabetes who presented to an emergency department with severe hypoglycemia between January 1, 2004 and December 30, 2009.
Results
A total of 740 cases of severe hypoglycemia were identified. The mean subject age was 69±12 years, mean duration of diabetes was 13.8±9.3 years, and 53.2% of subjects were receiving insulin therapy. We observed a sharp rise in the number of cases between 2006 and 2007. Stages 3-5 chronic kidney disease was diagnosed in 31.5% of subjects, and low C-peptide levels (<0.6 ng/mL) were found in 25.5%. The mean subject age, duration of diabetes, HbA1c level, and renal and insulin secretory function values did not change significantly during the study period. The proportion of glimepiride use increased, while use of gliclazide decreased among sulfonylurea users. Use of insulin analogues increased, while use of NPH/RI decreased among insulin users.
Conclusion
We identified a sharp increase in the number of subjects with severe hypoglycemia presenting to an emergency room since 2006. The clinical characteristics of these subjects did not change markedly during the study period. Nationwide studies are warranted to further clarify this epidemic of severe hypoglycemia.
INTRODUCTION
The epidemic of diabetes mellitus is a worldwide problem, and Korea is no exception. While proper glucose control is a mainstay for the prevention and management of diabetes-related complications, hypoglycemia remains a major problem associated with this disease [1-3]. Mild cases of hypoglycemia can be managed by the subject; however, severe hypoglycemia is accompanied by change in consciousness and can lead to trauma, injury, and even death in rare cases [4].
Since publication of results from the Diabetes Control and Complications Trial (DCCT) and the United Kingdom Prospective Diabetes Study (UKPDS), glycemic control has been heavily emphasized in diabetes management for prevention of micro- and macrovascular complications [1,2]. However, it has been shown through recent landmark trials, such as Action to Control Cardiovascular Risk in Diabetes (ACCORD), Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE), and Veterans Affairs Diabetes Trial (VADT), that intensive glycemic control does not reduce mortality due to cardiovascular disease (CVD) in subjects with type 2 diabetes mellitus and may actually increase CVD risk, especially in subjects with pre-existing coronary heart disease (CHD) [5-7]. These trials have also shown that achieving rather aggressive HbA1c levels (<6.5%) is associated with a three-fold increased risk of hypoglycemia.
We recently noted that there might be a hypoglycemia epidemic in our community, as we were seeing more hypoglycemic subjects admitted to hospitals via the emergency department. We hypothesized that recent emphasis on glycemic control and changes in anti-diabetic medications may be influencing the incidence of severe hypoglycemia.
The aims of this study were to investigate whether the number of subjects with severe hypoglycemia presenting to an emergency department has increased in recent years and to identify whether there were changes in the demographic and clinical characteristics of those subjects. We also aimed to investigate if there have been changes in sulfonylurea or insulin use in these subjects.
METHODS
Research design and methods
Clinical data from the Emergency Departments of two general hospitals (Seoul National University Hospital and Eulji University Hospital) in Seoul were first obtained from the hospital databases. We included all adult subjects (aged ≥18 years) with type 2 diabetes mellitus who presented to the Emergency Department with severe hypoglycemia between January 1, 2004 and December 30, 2009. We searched for the following International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9CM) codes to identify potential episodes of severe hypoglycemia: 1) hypoglycemic coma in diabetes mellitus (250.3); 2) hypoglycemic coma (251.0); 3) other specified hypoglycemia (251.1); 4) hypoglycemia, unspecified (251.2). We then had three medical doctors (J.T. Kim, T.J. Oh, Y.A. Lee) review the medical records of all subjects for validation of the events and to obtain data on related clinical factors. We only included subjects with severe hypoglycemia, defined as a serum glucose level less than 60 mg/dL and the need for intervention to recover from the hypoglycemic event [8].
Using the subjects' medical records, we obtained data on sex, age, height, weight, duration of diabetes, anti-diabetic treatment, the inciting factor for hypoglycemia, alcohol consumption, co-morbidities, and co-medications. In subjects taking both insulin and anti-diabetic medications, only insulin use was analyzed; for subjects taking multiple anti-diabetic oral medications, only sulfonylurea use was analyzed. The presence of diabetic macro- and microvascular complications were investigated. Data on HbA1c and fasting plasma C-peptide levels, complete blood counts, serum chemistries, and random urine microalbumin/creatinine ratios were obtained. The most recent HbA1c data prior to the hypoglycemic episode was used for analysis. We used an abbreviated MDRD equation for estimating glomerular filtration rate (GFR) [9], as follows: estimated GFR (mL/min/1.73 m2)=186×(creat/88.4)-1.154×(age)-0.203 ×(0.742, if female)×(1.210, if black). Stages 3-5 chronic kidney disease (CKD) was defined when the eGFR was less than 60 mL/min/1.73 m2 [10]. A low C-peptide level was defined as that less than 0.6 ng/dL [11]. The institutional review board for each hospital approved the study protocol.
Statistical analysis
All data are presented as mean±standard deviation. Group differences in means were tested by ANOVA or the Kruskall Wallis Test, as appropriate. Group differences in nominal variables were tested using the chi-square test. We analyzed trends over time using the chi-square test for linear trend and linear regression. Two-tailed P values <0.05 were considered statistically significant. Statistical analysis was conducted using commercially available software (SPSS version 15.0; SPSS Inc., Chicago, IL, USA).
RESULTS
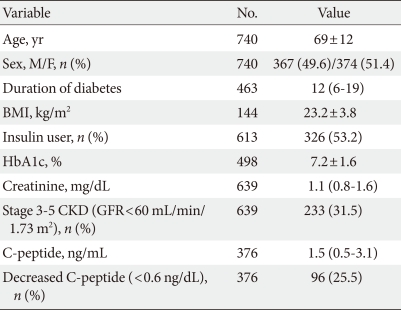
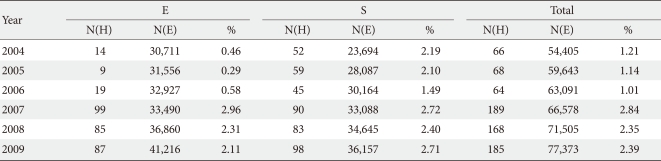
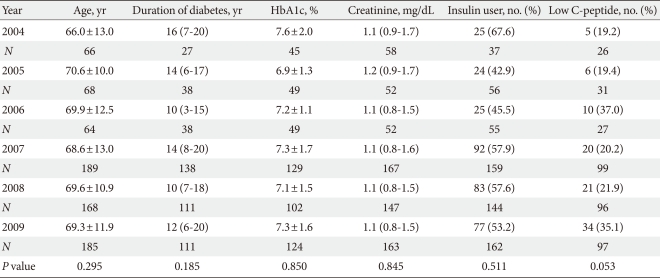
A total of 740 cases of severe hypoglycemia were identified, and the clinical characteristics of the patients are presented in Table 1. The mean subject age was 69±12 years old; 49.6% percent of subjects were male; the mean duration of diabetes was 13.8±9.3 years; mean body mass index was 23.2±3.8; and 53.2% of subjects were receiving insulin therapy. We noted a rather sharp increase in hypoglycemia cases in 2007 in both hospitals, and the level remained high for the remainder of the study period (Table 2). The number of severe hypoglycemia cases in 2009 (n=185) was 2.8-fold higher than the number in 2004 (n=66) (Table 2). During the same period, the total number of subjects who visited the emergency rooms of these hospitals steadily increased by 1.4-fold (2004, n=54, 405; 2009, n=77, 373) (Table 2).
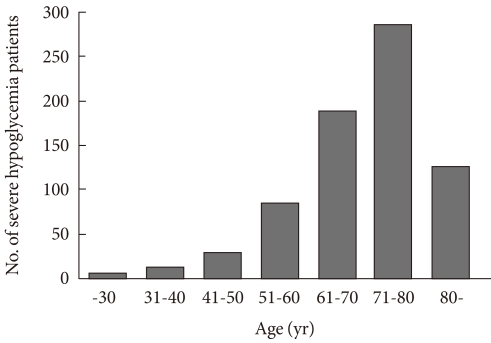
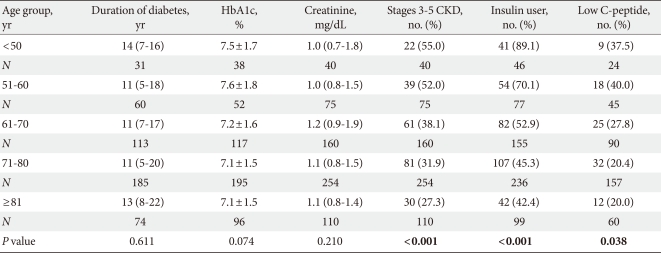
Subjects visiting the emergency room due to severe hypoglycemia were more commonly in their seventies (n=287, 38.8%), sixties (n=191, 25.8%), or eighties (n=121, 16.4%), in order of descending frequency (Fig. 1). When we divided the subjects into five groups according to age (≤50, 51-60, 61-70, 71-80, and ≥81 years), there were no differences in duration of diabetes, HbA1c level, or serum creatinine level (Table 3). Insulin use and insulin secretory defects were more common in the younger age group, and stages 3-5 CKD was more common in the older age group (Table 3).
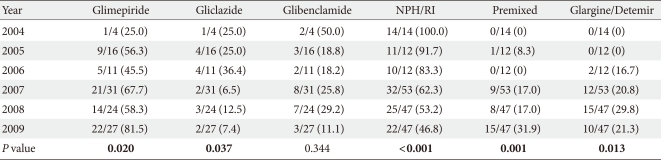
The number of severe hypoglycemia cases increased consistently in the two hospitals over the study period. Mean age, duration of diabetes, creatinine level, HbA1c level, insulin use, and C-peptide level did not change significantly during this period (Table 4). When we analyzed sulfonylurea and insulin use according to year of presentation, we found that the proportion of glimepiride use increased, while gliclazide use decreased among oral drug users; and insulin glargine/detemir use increased, while insulin NPH/RI use decreased among insulin users (Table 5).
DISCUSSION
Hypoglycemia is the principal problem associated with strict glycemic control. Our study indicates that the number of subjects with severe hypoglycemia requiring emergency department visits has increased in recent years. Several previous epidemiologic studies have suggested that the incidence of severe hypoglycemia has also increased [12], while one study indicated that the increasing number may be due to the increased prevalence of type 2 diabetes mellitus, and that the rate of hypoglycemia in the diabetic population has not changed [13]. The prevalence of type 2 diabetes mellitus in Korea has steadily increased over the past 30 years; however, after the late 1990s, the maximum increase per year was estimated to be less than 10% [14-16]. Accordingly, it is inferable from our data that the incidence of severe hypoglycemia in the diabetic population has also increased in Korea.
This trend is particularly problematic since it is prevalent among older adult subjects: those aged 60 years or older comprised the majority (83.2%) of the study population. It is conceivable that severe hypoglycemia may occur more easily in older adult subjects with decreased cognitive function and activity levels. In line with this finding, population-based studies in Scotland and Germany have demonstrated that severe hypoglycemia requiring emergency treatment is common among older adult subjects, and that age was a risk factor for severe hypoglycemia [17,18]. In contrast, a nationwide study in the Uinted States showed that the rate of severe hypoglycemia is higher in younger (age <45 years) and very old (age ≥75 years) subjects [13]. A cohort study in the United States also showed that older subjects experience a lower incidence of hypoglycemia after investigating the frequency of severe hypoglycemia among subjects receiving insulin monotherapy [12]. One explanation for the controversy is that age serves as a marker for the subject's type of diabetes, with the proportion of type 2 diabetes mellitus subjects increasing with age.
Renal insufficiency was common among these subjects: 31.5% of the study population had stages 3-5 CKD (GFR <60 mL/min/1.73 m2). A recent nationwide survey on diabetes complications in Korea showed that 30.3% of diabetics have microalbuminuria [19]. Insulin secretory defects were also common among these subjects; those with decreased C-peptide levels (<0.6 ng/mL) made up 25.5% of the total population. A study investigating C-peptide levels in a large number of Korean subjects with adult onset diabetes showed that 9.1% (922 of 10,172) had low C-peptide levels (<0.6 ng/mL) [20]. However, when we analyzed the clinical characteristics of our study subjects according to year of presentation, the increasing occurrence of severe hypoglycemia did not appear to be associated with known risk factors, such as glycemic control status, duration of diabetes, age, renal function, or insulin secretory function.
The proportion of insulin users decreased during the study period. Use of insulin glargine and premixed insulin increased, while use of insulin NPH and RI decreased. Among sulfonylurea users, the proportion of glimepiride users increased, while that of gliclazide users decreased. These changes in the use of sulfonylureas and insulin in hypoglycemia subjects may or may not be a reflection of changes in medication use due to the introduction of newer-generation drugs. Further investigation into changes in medication use in the type 2 diabetes mellitus population may reveal an association between change in anti-diabetic medication and incidence of hypoglycemia.
Another interesting finding of our study was the sharp increase in severe hypoglycemia after 2007. There is a need for a nationwide survey investigating if there have been changes in glycemic control status, anti-diabetic therapy, and diabetes education in type 2 diabetes mellitus subjects in recent years in order to draw any firm conclusion regarding the cause of this trend. Diabetes educators in Korea should recognize that the most common inciting cause of hypoglycemia reported by our study subjects was decreased or missed food intake. If HbA1c level goals are established, it is essential to educate the subjects about the potential risk of hypoglycemia and methods of avoiding and treating it.
There are several limitations to this study. The major limitation is that we collected data from only two hospitals located in the Korean capital city of Seoul. This limitation makes it difficult to extend the implications of our results throughout Korea and to other countries. Another limitation is the retrospective nature of our analysis. It is quite possible that data may have been missing from the subjects' medical records, thus biasing the results. Since some cases of severe hypoglycemia are treated effectively at home or work by friends, relatives, or colleagues, the results of the current study may not reflect the entire sphere of severe hypoglycemia in our community.
In summary, we identified an increase in the number of severe hypoglycemia subjects presenting to emergency rooms since 2004. Severe hypoglycemia prevails among older adults, and renal insufficiency and decreased endogenous insulin secretion appear to be common conditions in these subjects. We also found that the use of newer generation sulfonylureas and insulin analogues increased during this period among our study subjects. A national survey is urgently needed to verify this epidemic and its implications.
ACKNOWLEDGMENT
The authors have nothing to disclose.