- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 41(6); 2017 > Article
-
ReviewObesity and Metabolic Syndrome Non-Alcoholic Fatty Liver Disease: The Emerging Burden in Cardiometabolic and Renal Diseases
-
Eugene Han1,2, Yong-ho Lee2,3

-
Diabetes & Metabolism Journal 2017;41(6):430-437.
DOI: https://doi.org/10.4093/dmj.2017.41.6.430
Published online: November 17, 2017
1Division of Endocrinology and Metabolism, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea.
2Graduate School, Yonsei University College of Medicine, Seoul, Korea.
3Division of Endocrinology and Metabolism, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea.
- Corresponding author: Yong-ho Lee. Division of Endocrinology and Metabolism, Department of Internal Medicine, Yonsei University College of Medicine, 50-1 Yonsei-ro, Seodaemun-gu, Seoul 03722, Korea. yholee@yuhs.ac
Copyright © 2017 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- As the number of individuals with non-alcoholic fatty liver disease (NAFLD) has increased, the influence of NAFLD on other metabolic diseases has been highlighted. Accumulating epidemiologic evidence indicates that NAFLD not only affects the liver but also increases the risk of extra-hepatic diseases such as type 2 diabetes mellitus, metabolic syndrome, dyslipidemia, hypertension, cardiovascular or cerebrovascular diseases, and chronic kidney disease. Non-alcoholic steatohepatitis, an advanced type of NAFLD, can aggravate these inter-organ relationships and lead to poorer outcomes. NAFLD induces insulin resistance and exacerbates systemic chronic inflammation and oxidative stress, which leads to organ dysfunction in extra-hepatic tissues. Although more research is needed to identify the pathophysiological mechanisms and causal relationship between NAFLD and cardiometabolic and renal diseases, screening for heart, brain, and kidney diseases, risk assessment for diabetes, and a multidisciplinary approach for managing these patients should be highly encouraged.
- As the prevalence and incidence of obesity has dramatically increased worldwide, it has had a great impact on the development of obesity-related diseases, including type 2 diabetes mellitus (T2DM) and cardiovascular disease (CVD), which is considered a global health threat to both individuals and societies. The substantial burden of obesity is not only limited to Western nations, but is also occurring in many Asian countries [123]. Recently, non-alcoholic fatty liver disease (NAFLD) has been recognized as the hepatic manifestation of metabolic syndrome [4] and established as a major leading cause of chronic liver disease [5]. Over the past two decades, the reported number of patients with NAFLD has increased, while the number of individuals with hepatitis B virus, hepatitis C virus, or alcohol-related liver disease remained stable [6]. The prevalence of NAFLD in Asia has been reported from 15% to 45% [3], and a quarter of the total Asian population is affected by this disease on average [7]. This high rate is similar to the global NAFLD prevalence [5].
- NAFLD is characterized as the presence of more than 5% of lipid accumulation in the hepatocytes, excluding other liver disease etiologies (virus, autoimmune, alcohol, drugs, and genetics) [5]. NAFLD can progress to an advanced form, non-alcoholic steatohepatitis (NASH), which is defined by histological findings of hepatic steatosis with hepatocyte damage/inflammation [5]. Both NAFLD and NASH can further develop into liver fibrosis, cirrhosis, and eventually hepatocellular carcinoma (HCC). Although the reported incidence of HCC from NAFLD is rare, the number of patients with NAFLD-related HCC or liver transplantation are continuously increasing, which might suggest a significant role of NAFLD in these end-stage hepatic complications [89].
- NAFLD has been regarded as the hepatic phenotype of metabolic impairment [4], indicating one aspect of multisystem disease. In addition to obesity, aging and sarcopenia are also known to be crucial risk factors for NAFLD or NASH [101112]. As aging gradually induces sarcopenia, which is linked to frailty, leading to the development of cardiometabolic and renal diseases as well as NAFLD or NASH, NAFLD can confer significant risks of morbidity and mortality in elderly patients in particular. The current review outlines the recent epidemiologic evidence of the extrahepatic complications of NAFLD and highlights the clinical relevance of NAFLD.
INTRODUCTION
- Prediabetes and type 2 diabetes mellitus in NAFLD
- Traditionally, T2DM has been a well-known risk factor for NAFLD [12]. Although insulin resistance is common for both NAFLD and T2DM [13], several studies support that NAFLD per se can increase the risk of T2DM as well as prediabetes [14151617]. Furthermore, the degree of hepatic steatosis is positively associated with future T2DM risk in a dose-dependent manner [1416]. In a large and healthy cohort study, individuals with NAFLD had a 2-fold higher risk for T2DM and the risk for T2DM was elevated up to 4-fold with an increase in hepatic fibrosis [16]. Even among the non-obese population, the impact of NAFLD on the incidence of impaired fasting glucose (IFG) and T2DM was strong [17]. Moreover, this association remained significant regardless of insulin resistance, obesity, and age [14], suggesting the direct role of NAFLD in the pathogenesis of T2DM. Although the incident risk for T2DM in NAFLD was not as high as that of IFG, the presence of NAFLD had an additive effect on future T2DM risk among subjects with IFG [15]. The severity of NAFLD, NASH, significant hepatic fibrosis, and HCC are all highly linked with diabetes; thus, modalities for screening diabetes should be implemented for individuals diagnosed with NAFLD [18].
- Metabolic syndrome and dyslipidemia in NAFLD
- NAFLD is considered a strong predictor for metabolic syndrome and vice versa. Dyslipidemia can be involved in the development of NAFLD and also occurs as a complication of NAFLD [19]. Currently, 20% to 80% of NAFLD patients have dyslipidemia, mainly characterized as high triglyceride and low high-density lipoprotein cholesterol (HDL-C) [19]. Although the reported findings regarding low density lipoprotein cholesterol (LDL-C) levels are controversial, an increase or no difference in LDL-C levels or a higher proportion of small dense LDL were demonstrated across several studies [202122]. Among the components of the lipid parameters, elevated non-HDL-C is the most frequently observed in the NASH population (low HDL-C in 63%, high triglyceride in 46%, high non-HDL-C in 73%, and high LDL-C in 16%) [23]. An 11-year follow-up study showed that NAFLD increased the incidence of metabolic syndrome by 50%; however, only two components of metabolic syndrome, waist circumference and triglyceride levels, had significant associations after multivariable regression analyses [24]. This evidence might support the possible role of NAFLD in the development of abdominal obesity and excessive levels of very low density lipoprotein (VLDL), which are essential components of insulin resistance, an underlying pathophysiology of metabolic syndrome. Both hepatic over-production of VLDL and impaired lipoprotein clearance contribute to dyslipidemia in NAFLD [22]. According to the previous cross-sectional study, which revealed a strong association among liver fat contents, LDL particle size, and apolipoprotein B/A-I levels, atherogenic dyslipidemia might be driven from liver fat itself, independent of obesity [25]. Although the severity of NASH was not associated with abnormal lipoprotein profiles in this cohort [25], another study demonstrated that NASH can promote LDL-C oxidation [19].
- Hypertension and atherosclerosis in NAFLD
- Prospective studies demonstrated that the incidence of hypertension increases in NAFLD and its rate is gradually elevated according to the degree of NAFLD [262728]. The odds ratio (OR) of incident hypertension in individuals with NAFLD compared to those with normal livers ranges from 1.1 to 2.1, according to previous studies [262729]. Moreover, among NAFLD individuals without incident hypertension, blood pressure tends to increase, and high-normal systolic blood pressure (130 to 139 mm Hg) is more prevalent [29]. In addition, dysregulated flow-mediated vasodilatation, increased thickness of intima-media, and plaques in carotid arteries, which are well-established surrogate markers for subclinical atherosclerosis, are exhibited in patients with NAFLD [20]. The carotid artery intima-medial thickness is increased in a dose-dependent manner with the degree of NAFLD or fibrosis stage of NASH [2030]. In a cohort study conducted at a general health check-up, the risk for coronary artery calcification was 1.8-fold greater in individuals with NAFLD, and concomitant NAFLD and systemic inflammation (high levels of C-reactive protein) elevate its risk by approximately 2.4-fold [31]. Compared to individuals without NAFLD, the annual progression rate of coronary artery calcification was also higher in the NAFLD group and the positive association between NAFLD and coronary artery calcification progression was more evident in NAFLD regardless of subgroup analysis [32]. Although pathophysiologic pathways from NAFLD to atherosclerosis and hypertension remain elusive, a series of studies suggested that systemic inflammation, endothelial dysfunction, hemodynamic alteration, and atherogenic lipid particles including small dense LDL are involved in NAFLD-related atherosclerotic and vascular complications [31333435].
- Cardiovascular disease in NAFLD
- Given the strong association between NAFLD and diabetes, dyslipidemia, hypertension, and atherosclerosis, which are all established risk factors for CVD, it is not surprising that NAFLD subjects have a higher prevalence and incidence of CVD. In particular, CVD accounts for the most common cause of mortality in individuals with NAFLD [36], larger than the number of liver-related deaths [37]. The estimated 10-year CVD risk score is increased in individuals with NAFLD, and multivariable regression analyses demonstrate up to a 3.4-fold increase in CVD risk among advanced stages of hepatic steatosis [38]. In a meta-analysis analyzing 16 observational studies of 34,043 adults followed for 6.9 years, patients with NAFLD had a higher risk of fatal and non-fatal CVD events (OR, 1.64; 95% confidence interval [CI], 1.26 to 2.13) [39]. Furthermore, severe NAFLD, defined either by liver histology or by a combination of radiological imaging evidence and one of three components (high levels of serum γ-glutamyltransferase or NAFLD fibrosis score or high hepatic 18F-fluoro-2-deoxyglucose uptake on positron emission tomography), greatly increase the total incident CVD (OR, 2.58; 95% CI, 1.78 to 3.75) and fatal CVD events (OR, 3.28; 95% CI, 2.26 to 4.77) [39]. Metabolic syndrome, diabetes, hypertension, dyslipidemia, atherosclerosis, and insulin resistance can contribute to the pathophysiologic progression of CVD in individuals with NAFLD. Beyond these traditional CVD risk factors, hyperuricemia, hypoadiponectinemia, and vitamin D deficiency are also involved in the association between NAFLD and CVD [40]. Of note, NAFLD and NASH per se could be regarded as emerging risk factors for CVD. The overall consensus states that screening for CVD is mandatory in all people, including adolescents and children with NAFLD [18].
- Cardiac structure, function, and energy metabolism in NAFLD
- Several limited case-control studies with a small number of participants provided consistent evidence that there are significant changes in cardiac structure, function, and energy metabolism in individuals with NAFLD who did not have a previous history of heart disease. Among subjects who did not have hypertension and diabetes, NAFLD was linked to early alterations in echocardiographic parameters that reflect diastolic function and geometry in the left ventricle of the heart, while no significant difference was found in systolic heart function [4142]. In terms of myocardial metabolic abnormalities, individuals with hepatic steatosis show a reduction in myocardial energy metabolism assessed by 31P-magnetic resonance spectroscopy both in young and non-diabetic men [43] and in patients with T2DM [44]. Among patients with T2DM, those with NAFLD have impairment in myocardial perfusion and glucose uptake, but no difference in cardiac fatty acid metabolism as measured by positron emission tomography [44]. Insulin-resistant condition converts preference in the energy substrate utilization of the myocardium, which might induce oxidative stress, and subsequent hyperinsulinemia accelerates the growth of cardiomyocytes. Furthermore, the dysregulation in the energy metabolism of the myocardium can impair left ventricular contractility, resulting in an aggravation of fibrosis [45], which might lead to diastolic dysfunction.
- Arrhythmias in NAFLD
- Accumulating evidence strengthens the idea that NAFLD is an emerging risk factor for cardiac arrhythmias [4647]. Among various types of arrhythmia, atrial fibrillation, QT prolongation, ventricular arrhythmias, and conduction defects are frequently reported in patients with NAFLD. In a prospective Finnish cohort of middle-aged adults, ultrasonographically defined NAFLD was an independent predictor of atrial fibrillation (OR, 1.88; 95% CI, 1.03 to 3.45) [48]. A recent cross-sectional study of a general population revealed that the mean QT interval increases according to the degree of steatosis in the liver (2.55 ms vs. 6.59 ms vs. 12.13 ms for mild, moderate, and severe steatosis, respectively), and subjects with NAFLD had a 1.87-fold increased risk for QT prolongation [46]. The prevalence of ventricular arrhythmia detected by 24-hour Holter monitoring, including non-sustained ventricular tachycardia and frequent premature ventricular complex (>30 times per hour) was higher in individuals with NAFLD among the T2DM population (27.3% vs. 9.8%) [47]. In this cross-sectional study, NAFLD was associated with a 3-fold increased risk of ventricular arrhythmia after adjusting for history of other underlying cardiac diseases and metabolic covariates [47].
- Stroke in NAFLD
- While ischemic stroke is generally included as a composite endpoint of CVD that is significantly linked to NAFLD based on the previous section, few studies have investigated the direct association between stroke and NAFLD. A case-control study from Canada reported a 3.3-fold higher prevalence for ischemic stroke in patients with elevated alanine aminotransferase, a biomarker for NAFLD [49]. Although confounding factors such as diabetes or obesity are not fully adjusted, patients with biochemically defined NAFLD had more severe forms of stroke and worse functional outcomes compared to those without NAFLD in a prospective cohort of acute ischemic stroke patients [50]. Recently, a propensity-score matched case-control study from Korea revealed a strong association of ischemic stroke risk with liver fibrosis assessed by transient elastography (FibroScan; EchoSens, Paris, France), with the OR for ischemic stroke at 1.80 (95% CI, 1.46 to 2.23) per 1 kPa increase in liver stiffness, but not with liver steatosis per se [51]. This result might indicate the importance of liver fibrosis or NASH on the risk of ischemic stroke. Further prospective research is needed to confirm the complex link between stroke and the severity of NAFLD.
- Albuminuria and chronic kidney disease in NAFLD
- Although chronic kidney disease (CKD) is traditionally recognized as a complication of diabetes, obesity, and CVD, recent studies have clearly demonstrated the possibility that NAFLD directly affects kidney outcomes [52535455]. The prevalence of CKD in NAFLD patients ranged from 20% to 55%, an approximately 2-fold increase, compared to those without NAFLD (5% to 30%) [52]. A meta-analysis with individual participant data shows consistent findings that the presence and severity of NAFLD are associated with an increased risk and severity of CKD [55]. The NAFLD group had 2.1-fold and 1.8-fold increased risk of prevalent and incident CKD, respectively, and these risks were potentiated when they had NASH (hazard ratios [HRs] of 2.5 and 2.1 for prevalent and incident CKD, respectively) compared to those with simple steatosis [55]. Advanced fibrosis is associated with a higher prevalence (OR, 5.20; 95% CI, 3.14 to 8.61) and incidence (HR, 3.29; 95% CI, 2.30 to 4.71) of CKD than non-advanced fibrosis [55]. In addition, albuminuria is more prevalent in patients with NAFLD [5354], and the impairment in kidney function is significantly associated with the severity of NASH histology [54]; thus, the presence of NAFLD and the severity of fibrosis can predict the development of CKD regardless of other risk factors. Further studies are warranted to investigate whether improvement in NAFLD can attenuate CKD progression, and efforts are needed for the early screening of renal function and albuminuria in NAFLD patients.
- Mortality in NAFLD
- The impact of NAFLD on overall mortality apparently differs according to its severity. In a community-based cohort study, the overall survival of NAFLD patients was lower than expected in the general population (standardized mortality ratio, 1.34; 95% CI, 1.01 to 1.76) [36]. Among NAFLD's causes of death, CVD was the most common (15.5% to 25%), followed by extrahepatic malignancies, and then liver-related diseases [3637]. In the spectrum of NAFLD, simple steatosis is not associated with increased mortality [3756], whereas NASH or advanced fibrosis, as defined by either biopsy or noninvasive fibrosis panels, showed approximately 1.14-fold and 1.66-fold to 1.85-fold increased risk for overall mortality in Swedish [37] and United States studies, respectively [56]. In addition, this decline in survival seen in advanced fibrosis or NASH is almost certainly from cardiovascular causes [56].
ASSOCIATION AND PROGRESSION TO CARDIOMETABOLIC AND RENAL DISEASES
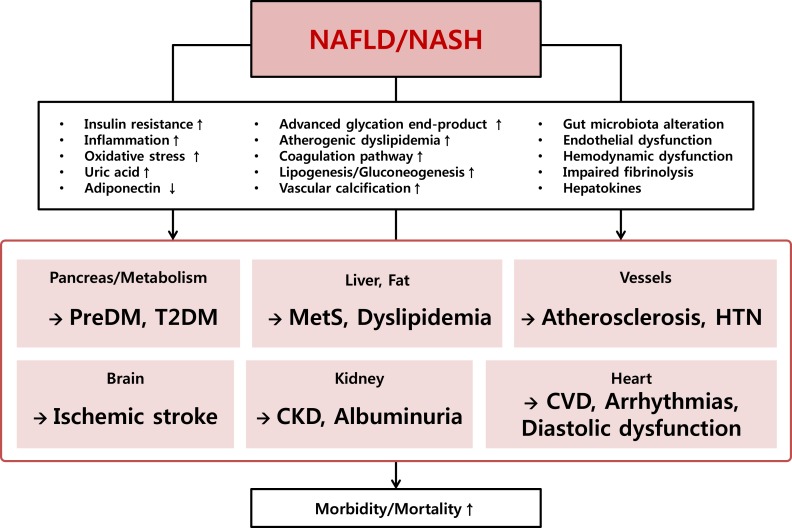
- NAFLD shares a common denominator with cardiometabolic diseases and kidney diseases, such as insulin resistance, oxidative stress, and systemic inflammation. It has been reported that visceral adipose tissue and fat accumulation in the liver alter signals in lipid and glucose metabolism, resulting in inflammation and cellular injury in the liver and other organs [57]. Accelerated free fatty acid flux to the portal circulation induces oxidative stress and accumulated advanced glycation end-products promote vascular and renal damage [58]. In addition, endothelial dysfunction, hemodynamic alteration, and atherogenic dyslipidemia mediate prothrombotic and profibrogenic factors, stimulating organ dysfunction [31333435]. Recent emerging evidence has indicated that the intestinal microbiota and its dysbiosis can both affect the progression of NAFLD [59] and CVD [60] through chronic inflammation in the immune cells and insulin resistance [52]. Moreover, inter-organ communications between the liver and affected organs may exist, which should be further investigated in future research (Fig. 1).
POSSIBLE MECHANISM LINKING NAFLD TO CARDIOMETABOLIC AND RENAL DISEASES
- NAFLD is presently regarded as an emerging risk factor and essential phenotype of chronic metabolic disorder beyond benign liver disease. Accumulating evidence indicates that the presence and severity of NAFLD are strongly associated with the increased prevalence and incidence of other metabolic diseases, including diabetes, hypertension, atherosclerosis, CVD, diastolic heart dysfunction, arrhythmia, and CKD, which have considerable impacts on global healthcare. Taken together, individuals with NAFLD should be screened for these extra-hepatic disorders and early effective intervention on their lifestyle and the future development of a pharmacologic approach to treat NAFLD or NASH is necessary to further prevent future complications.
CONCLUSIONS
-
Acknowledgements
- This research was supported by the grant from the Korea Healthcare Technology R&D Project, Ministry of Health and Welfare, Republic of Korea (HI17C0913).
ACKNOWLEDGMENTS
-
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
NOTES
- 1. Yoon KH, Lee JH, Kim JW, Cho JH, Choi YH, Ko SH, Zimmet P, Son HY. Epidemic obesity and type 2 diabetes in Asia. Lancet 2006;368:1681-1688. ArticlePubMed
- 2. Oh SW. Obesity and metabolic syndrome in Korea. Diabetes Metab J 2011;35:561-566. ArticlePubMedPMC
- 3. Farrell GC, Wong VW, Chitturi S. NAFLD in Asia: as common and important as in the West. Nat Rev Gastroenterol Hepatol 2013;10:307-318. ArticlePubMedPDF
- 4. Chalasani N, Younossi Z, Lavine JE, Diehl AM, Brunt EM, Cusi K, Charlton M, Sanyal AJ. The diagnosis and management of non-alcoholic fatty liver disease: practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology, and the American Gastroenterological Association. Hepatology 2012;55:2005-2023. ArticlePubMed
- 5. Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology 2016;64:73-84. ArticlePubMed
- 6. Younossi ZM, Stepanova M, Afendy M, Fang Y, Younossi Y, Mir H, Srishord M. Changes in the prevalence of the most common causes of chronic liver diseases in the United States from 1988 to 2008. Clin Gastroenterol Hepatol 2011;9:524-530. ArticlePubMed
- 7. Fan JG, Kim SU, Wong VW. New trends on obesity and NAFLD in Asia. J Hepatol 2017;67:862-873. ArticlePubMed
- 8. Pais R, Fartoux L, Goumard C, Scatton O, Wendum D, Rosmorduc O, Ratziu V. Temporal trends, clinical patterns and outcomes of NAFLD-related HCC in patients undergoing liver resection over a 20-year period. Aliment Pharmacol Ther 2017;46:856-863. ArticlePubMedPDF
- 9. Goldberg D, Ditah IC, Saeian K, Lalehzari M, Aronsohn A, Gorospe EC, Charlton M. Changes in the prevalence of hepatitis c virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology 2017;152:1090-1099. ArticlePubMedPMC
- 10. Lee YH, Jung KS, Kim SU, Yoon HJ, Yun YJ, Lee BW, Kang ES, Han KH, Lee HC, Cha BS. Sarcopaenia is associated with NAFLD independently of obesity and insulin resistance: Nationwide surveys (KNHANES 2008-2011). J Hepatol 2015;63:486-493. ArticlePubMed
- 11. Lee YH, Kim SU, Song K, Park JY, Kim DY, Ahn SH, Lee BW, Kang ES, Cha BS, Han KH. Sarcopenia is associated with significant liver fibrosis independently of obesity and insulin resistance in nonalcoholic fatty liver disease: nationwide surveys (KNHANES 2008-2011). Hepatology 2016;63:776-786. ArticlePubMedPDF
- 12. Lee YH, Bang H, Park YM, Bae JC, Lee BW, Kang ES, Cha BS, Lee HC, Balkau B, Lee WY, Kim DJ. Non-laboratory-based self-assessment screening score for non-alcoholic fatty liver disease: development, validation and comparison with other scores. PLoS One 2014;9:e107584. ArticlePubMedPMC
- 13. Lee MK, Rhee EJ, Kim MC, Moon BS, Lee JI, Song YS, Han EN, Lee HS, Son Y, Park SE, Park CY, Oh KW, Park SW, Lee WY. Metabolic health is more important than obesity in the development of nonalcoholic fatty liver disease: a 4-year retrospective study. Endocrinol Metab (Seoul) 2015;30:522-530. ArticlePubMedPMC
- 14. Park SK, Seo MH, Shin HC, Ryoo JH. Clinical availability of nonalcoholic fatty liver disease as an early predictor of type 2 diabetes mellitus in Korean men: 5-year prospective cohort study. Hepatology 2013;57:1378-1383. ArticlePubMed
- 15. Bae JC, Rhee EJ, Lee WY, Park SE, Park CY, Oh KW, Park SW, Kim SW. Combined effect of nonalcoholic fatty liver disease and impaired fasting glucose on the development of type 2 diabetes: a 4-year retrospective longitudinal study. Diabetes Care 2011;34:727-729. PubMedPMC
- 16. Chang Y, Jung HS, Yun KE, Cho J, Cho YK, Ryu S. Cohort study of non-alcoholic fatty liver disease, NAFLD fibrosis score, and the risk of incident diabetes in a Korean population. Am J Gastroenterol 2013;108:1861-1868. ArticlePubMedPDF
- 17. Yamada T, Fukatsu M, Suzuki S, Wada T, Yoshida T, Joh T. Fatty liver predicts impaired fasting glucose and type 2 diabetes mellitus in Japanese undergoing a health checkup. J Gastroenterol Hepatol 2010;25:352-356. ArticlePubMed
- 18. European Association for the Study of the Liver (EASL). European Association for the Study of Diabetes (EASD). European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol 2016;64:1388-1402. ArticlePubMed
- 19. Zhang QQ, Lu LG. Nonalcoholic fatty liver disease: dyslipidemia, risk for cardiovascular complications, and treatment strategy. J Clin Transl Hepatol 2015;3:78-84. ArticlePubMedPMC
- 20. Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med 2010;363:1341-1350. ArticlePubMed
- 21. Nseir W, Shalata A, Marmor A, Assy N. Mechanisms linking nonalcoholic fatty liver disease with coronary artery disease. Dig Dis Sci 2011;56:3439-3449. ArticlePubMedPDF
- 22. Chatrath H, Vuppalanchi R, Chalasani N. Dyslipidemia in patients with nonalcoholic fatty liver disease. Semin Liver Dis 2012;32:22-29. ArticlePubMedPMC
- 23. Corey KE, Vuppalanchi R, Wilson LA, Cummings OW, Chalasani N;. NASH resolution is associated with improvements in HDL and triglyceride levels but not improvement in LDL or non-HDL-C levels. Aliment Pharmacol Ther 2015;41:301-309. ArticlePubMedPDF
- 24. Adams LA, Waters OR, Knuiman MW, Elliott RR, Olynyk JK. NAFLD as a risk factor for the development of diabetes and the metabolic syndrome: an eleven-year follow-up study. Am J Gastroenterol 2009;104:861-867. ArticlePubMed
- 25. Bril F, Sninsky JJ, Baca AM, Superko HR, Portillo Sanchez P, Biernacki D, Maximos M, Lomonaco R, Orsak B, Suman A, Weber MH, McPhaul MJ, Cusi K. Hepatic steatosis and insulin resistance, but not steatohepatitis, promote atherogenic dyslipidemia in NAFLD. J Clin Endocrinol Metab 2016;101:644-652. ArticlePubMed
- 26. Ryoo JH, Suh YJ, Shin HC, Cho YK, Choi JM, Park SK. Clinical association between non-alcoholic fatty liver disease and the development of hypertension. J Gastroenterol Hepatol 2014;29:1926-1931. ArticlePubMedPDF
- 27. Huh JH, Ahn SV, Koh SB, Choi E, Kim JY, Sung KC, Kim EJ, Park JB. A prospective study of fatty liver index and incident hypertension: the KoGES-ARIRANG Study. PLoS One 2015;10:e0143560. ArticlePubMedPMC
- 28. Sung KC, Wild SH, Byrne CD. Development of new fatty liver, or resolution of existing fatty liver, over five years of follow-up, and risk of incident hypertension. J Hepatol 2014;60:1040-1045. ArticlePubMed
- 29. Lopez-Suarez A, Guerrero JM, Elvira-Gonzalez J, Beltran-Robles M, Canas-Hormigo F, Bascunana-Quirell A. Nonalcoholic fatty liver disease is associated with blood pressure in hypertensive and nonhypertensive individuals from the general population with normal levels of alanine aminotransferase. Eur J Gastroenterol Hepatol 2011;23:1011-1017. ArticlePubMed
- 30. Targher G, Bertolini L, Padovani R, Rodella S, Zoppini G, Zenari L, Cigolini M, Falezza G, Arcaro G. Relations between carotid artery wall thickness and liver histology in subjects with nonalcoholic fatty liver disease. Diabetes Care 2006;29:1325-1330. ArticlePubMedPDF
- 31. Kim J, Lee DY, Park SE, Park CY, Lee WY, Oh KW, Park SW, Rhee EJ. Increased risk for development of coronary artery calcification in subjects with non-alcoholic fatty liver disease and systemic inflammation. PLoS One 2017;12:e0180118. ArticlePubMedPMC
- 32. Sinn DH, Kang D, Chang Y, Ryu S, Gu S, Kim H, Seong D, Cho SJ, Yi BK, Park HD, Paik SW, Song YB, Lazo M, Lima JA, Guallar E, Cho J, Gwak GY. Non-alcoholic fatty liver disease and progression of coronary artery calcium score: a retrospective cohort study. Gut 2017;66:323-329. ArticlePubMed
- 33. Loria P, Lonardo A, Targher G. Is liver fat detrimental to vessels?: intersections in the pathogenesis of NAFLD and atherosclerosis. Clin Sci (Lond) 2008;115:1-12. ArticlePubMedPDF
- 34. Luna-Luna M, Medina-Urrutia A, Vargas-Alarcon G, Coss-Rovirosa F, Vargas-Barron J, Perez-Mendez O. Adipose tissue in metabolic syndrome: onset and progression of atherosclerosis. Arch Med Res 2015;46:392-407. ArticlePubMed
- 35. Villanova N, Moscatiello S, Ramilli S, Bugianesi E, Magalotti D, Vanni E, Zoli M, Marchesini G. Endothelial dysfunction and cardiovascular risk profile in nonalcoholic fatty liver disease. Hepatology 2005;42:473-480. ArticlePubMed
- 36. Adams LA, Lymp JF, St Sauver J, Sanderson SO, Lindor KD, Feldstein A, Angulo P. The natural history of nonalcoholic fatty liver disease: a population-based cohort study. Gastroenterology 2005;129:113-121. ArticlePubMed
- 37. Ekstedt M, Franzen LE, Mathiesen UL, Thorelius L, Holmqvist M, Bodemar G, Kechagias S. Long-term follow-up of patients with NAFLD and elevated liver enzymes. Hepatology 2006;44:865-873. ArticlePubMed
- 38. Lee JI, Kim MC, Moon BS, Song YS, Han EN, Lee HS, Son Y, Kim J, Han EJ, Park HJ, Park SE, Park CY, Lee WY, Oh KW, Park SW, Rhee EJ. The relationship between 10-year cardiovascular risk calculated using the pooled cohort equation and the severity of non-alcoholic fatty liver disease. Endocrinol Metab (Seoul) 2016;31:86-92. ArticlePubMedPMCPDF
- 39. Targher G, Byrne CD, Lonardo A, Zoppini G, Barbui C. Non-alcoholic fatty liver disease and risk of incident cardiovascular disease: a meta-analysis. J Hepatol 2016;65:589-600. ArticlePubMed
- 40. Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut 2017;66:1138-1153. ArticlePubMed
- 41. Goland S, Shimoni S, Zornitzki T, Knobler H, Azoulai O, Lutaty G, Melzer E, Orr A, Caspi A, Malnick S. Cardiac abnormalities as a new manifestation of nonalcoholic fatty liver disease: echocardiographic and tissue Doppler imaging assessment. J Clin Gastroenterol 2006;40:949-955. ArticlePubMed
- 42. Hallsworth K, Hollingsworth KG, Thoma C, Jakovljevic D, MacGowan GA, Anstee QM, Taylor R, Day CP, Trenell MI. Cardiac structure and function are altered in adults with non-alcoholic fatty liver disease. J Hepatol 2013;58:757-762. ArticlePubMed
- 43. Perseghin G, Lattuada G, De Cobelli F, Esposito A, Belloni E, Ntali G, Ragogna F, Canu T, Scifo P, Del Maschio A, Luzi L. Increased mediastinal fat and impaired left ventricular energy metabolism in young men with newly found fatty liver. Hepatology 2008;47:51-58. ArticlePubMed
- 44. Rijzewijk LJ, Jonker JT, van der Meer RW, Lubberink M, de Jong HW, Romijn JA, Bax JJ, de Roos A, Heine RJ, Twisk JW, Windhorst AD, Lammertsma AA, Smit JW, Diamant M, Lamb HJ. Effects of hepatic triglyceride content on myocardial metabolism in type 2 diabetes. J Am Coll Cardiol 2010;56:225-233. ArticlePubMed
- 45. Peterson LR, Herrero P, Schechtman KB, Racette SB, Waggoner AD, Kisrieva-Ware Z, Dence C, Klein S, Marsala J, Meyer T, Gropler RJ. Effect of obesity and insulin resistance on myocardial substrate metabolism and efficiency in young women. Circulation 2004;109:2191-2196. ArticlePubMed
- 46. Hung CS, Tseng PH, Tu CH, Chen CC, Liao WC, Lee YC, Chiu HM, Lin HJ, Ho YL, Yang WS, Wu MS, Chen MF. Nonalcoholic fatty liver disease is associated with QT prolongation in the general population. J Am Heart Assoc 2015;4:e001820. ArticlePubMedPMC
- 47. Mantovani A, Rigamonti A, Bonapace S, Bolzan B, Pernigo M, Morani G, Franceschini L, Bergamini C, Bertolini L, Valbusa F, Rigolon R, Pichiri I, Zoppini G, Bonora E, Violi F, Targher G. nonalcoholic fatty liver disease is associated with ventricular arrhythmias in patients with type 2 diabetes referred for clinically indicated 24-hour Holter monitoring. Diabetes Care 2016;39:1416-1423. ArticlePubMedPDF
- 48. Karajamaki AJ, Patsi OP, Savolainen M, Kesaniemi YA, Huikuri H, Ukkola O. Non-alcoholic fatty liver disease as a predictor of atrial fibrillation in middle-aged population (OPERA Study). PLoS One 2015;10:e0142937. ArticlePubMedPMC
- 49. Ying I, Saposnik G, Vermeulen MJ, Leung A, Ray JG. Nonalcoholic fatty liver disease and acute ischemic stroke. Epidemiology 2011;22:129-130. ArticlePubMed
- 50. Abdeldyem SM, Goda T, Khodeir SA, Abou Saif S, Abd-Elsalam S. Nonalcoholic fatty liver disease in patients with acute ischemic stroke is associated with more severe stroke and worse outcome. J Clin Lipidol 2017;11:915-919. ArticlePubMed
- 51. Kim SU, Song D, Heo JH, Yoo J, Kim BK, Park JY, Kim DY, Ahn SH, Kim KJ, Han KH, Kim YD. Liver fibrosis assessed with transient elastography is an independent risk factor for ischemic stroke. Atherosclerosis 2017;260:156-162. ArticlePubMed
- 52. Targher G, Byrne CD. Non-alcoholic fatty liver disease: an emerging driving force in chronic kidney disease. Nat Rev Nephrol 2017;13:297-310. ArticlePubMedPDF
- 53. Yilmaz Y, Alahdab YO, Yonal O, Kurt R, Kedrah AE, Celikel CA, Ozdogan O, Duman D, Imeryuz N, Avsar E, Kalayci C. Microalbuminuria in nondiabetic patients with nonalcoholic fatty liver disease: association with liver fibrosis. Metabolism 2010;59:1327-1330. ArticlePubMed
- 54. Targher G, Bertolini L, Rodella S, Lippi G, Zoppini G, Chonchol M. Relationship between kidney function and liver histology in subjects with nonalcoholic steatohepatitis. Clin J Am Soc Nephrol 2010;5:2166-2171. ArticlePubMedPMC
- 55. Musso G, Gambino R, Tabibian JH, Ekstedt M, Kechagias S, Hamaguchi M, Hultcrantz R, Hagstrom H, Yoon SK, Charatcharoenwitthaya P, George J, Barrera F, Haflithadottir S, Bjornsson ES, Armstrong MJ, Hopkins LJ, Gao X, Francque S, Verrijken A, Yilmaz Y, Lindor KD, Charlton M, Haring R, Lerch MM, Rettig R, Volzke H, Ryu S, Li G, Wong LL, Machado M, Cortez-Pinto H, Yasui K, Cassader M. Association of non-alcoholic fatty liver disease with chronic kidney disease: a systematic review and meta-analysis. PLoS Med 2014;11:e1001680. ArticlePubMedPMC
- 56. Kim D, Kim WR, Kim HJ, Therneau TM. Association between noninvasive fibrosis markers and mortality among adults with nonalcoholic fatty liver disease in the United States. Hepatology 2013;57:1357-1365. ArticlePubMed
- 57. Rinella ME. Nonalcoholic fatty liver disease: a systematic review. JAMA 2015;313:2263-2273. ArticlePubMed
- 58. Tahara N, Yamagishi S, Takeuchi M, Honda A, Tahara A, Nitta Y, Kodama N, Mizoguchi M, Kaida H, Ishibashi M, Hayabuchi N, Matsui T, Imaizumi T. Positive association between serum level of glyceraldehyde-derived advanced glycation end products and vascular inflammation evaluated by [(18)F]fluorode-oxyglucose positron emission tomography. Diabetes Care 2012;35:2618-2625. ArticlePubMedPMCPDF
- 59. Leung C, Rivera L, Furness JB, Angus PW. The role of the gut microbiota in NAFLD. Nat Rev Gastroenterol Hepatol 2016;13:412-425. ArticlePubMedPDF
- 60. Tang WH, Wang Z, Levison BS, Koeth RA, Britt EB, Fu X, Wu Y, Hazen SL. Intestinal microbial metabolism of phosphatidylcholine and cardiovascular risk. N Engl J Med 2013;368:1575-1584. ArticlePubMedPMC
REFERENCES
Putative pathophysiologic mechanisms and associations between non-alcoholic fatty liver disease (NAFLD)/non-alcoholic steatohepatitis (NASH) and cardiometabolic and renal diseases. preDM, prediabetes mellitus; T2DM, type 2 diabetes mellitus; MetS, metabolic syndrome; HTN, hypertension; CKD, chronic kidney disease; CVD, cardiovascular disease.
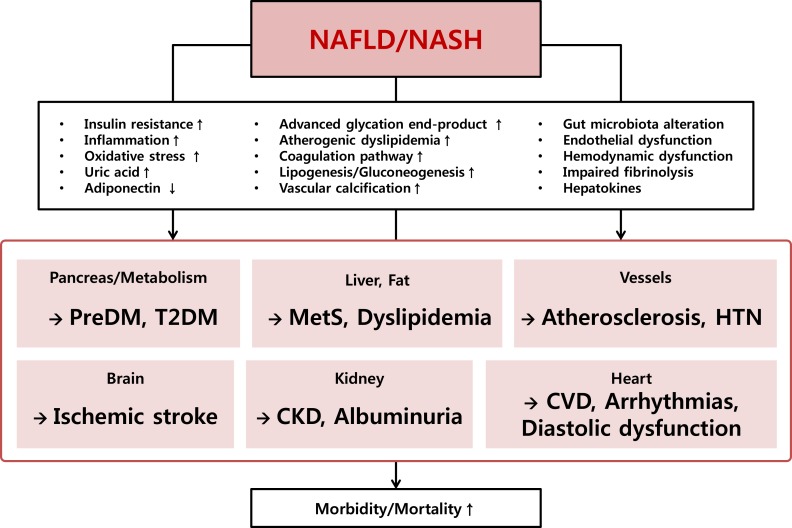
Figure & Data
References
Citations

- Inter‐relationships between cardiovascular, renal and metabolic diseases: Underlying evidence and implications for integrated interdisciplinary care and management
Jiten Vora, David Cherney, Mikhail N. Kosiborod, Jonas Spaak, Naresh Kanumilli, Kamlesh Khunti, Carolyn S. P. Lam, Michael Bachmann, Peter Fenici
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Relationship between Uric Acid to High Density Lipoprotein Cholesterol Ratio and Nonalcoholic Fatty Liver Disease in Nonoverweight/Obese Patients with Type 2 Diabetes
Yuliang Cui, Zhenzhen Qu, Wenmei Hu, Haiyan Shi, Faustino R. Perez-Lopez
International Journal of Endocrinology.2023; 2023: 1. CrossRef - Emerging Role of Protein O-GlcNAcylation in Liver Metabolism: Implications for Diabetes and NAFLD
Ziyan Xie, Ting Xie, Jieying Liu, Qian Zhang, Xinhua Xiao
International Journal of Molecular Sciences.2023; 24(3): 2142. CrossRef - Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
Eugene Han, Yong-ho Lee
Clinical and Molecular Hepatology.2023; 29(4): 980. CrossRef - Factores de riesgo para fibrosis hepática en pacientes diabéticos con enfermedad renal cronica terminal
Ismael Yepes Barreto, Diana Romero Florez, Jorge Coronado Daza
Revista colombiana de Gastroenterología.2023; 38(3): 278. CrossRef - Circ_0004535/miR-1827/CASP8 network involved in type 2 diabetes mellitus with nonalcoholic fatty liver disease
Min Li, Ai Zeng, Xinle Tang, Hui Xu, Wei Xiong, Yanying Guo
Scientific Reports.2023;[Epub] CrossRef - Non-alcoholic fatty liver disease associated with greater herpes zoster risk than alcoholic fatty liver disease
Cheng-Wei Yu, Chia-Hung Chen, Yung-Chi Cheng, Wen-Che Hsieh, Tzu-Ju Hsu, Fuu-Jen Tsai, Chao-Yu Hsu
European Journal of Medical Research.2023;[Epub] CrossRef - A GLP‐1/GLP‐2 receptor dual agonist to treat NASH: Targeting the gut‐liver axis and microbiome
Eun Ran Kim, Jeong Su Park, Jin Hee Kim, Ji Young Oh, In Jeong Oh, Da Hyun Choi, Yu seol Lee, I. Seul Park, SeungWon Kim, Da Hyun Lee, Jae Hee Cheon, Jin‐Woo Bae, Minyoung Lee, Jin Won Cho, In Bok An, Eun Joo Nam, Sang‐In Yang, Myung‐Shik Lee, Soo Han Bae
Hepatology.2022; 75(6): 1523. CrossRef - Analysis of Severe Hypoglycemia Among Adults With Type 2 Diabetes and Nonalcoholic Fatty Liver Disease
Ji-Yeon Lee, Young-eun Kim, Kyungdo Han, Eugene Han, Byung Wan Lee, Eun Seok Kang, Bong-Soo Cha, Seung-Hyun Ko, Yong-ho Lee
JAMA Network Open.2022; 5(2): e220262. CrossRef - State-of-the-Art Overview of the Pharmacological Treatment of Non-Alcoholic Steatohepatitis
Yongin Cho, Yong-ho Lee
Endocrinology and Metabolism.2022; 37(1): 38. CrossRef - Fatty Liver Index is a valid predictor of non-alcoholic fatty liver disease (NAFLD) in pregnancy
Iresha Sandamali Koralegedara, Janith Niwanthaka Warnasekara, Ashani Rathnayake, Korale Gedara Dayaratne, Suneth Buddhika Agampodi
BMJ Open Gastroenterology.2022; 9(1): e000913. CrossRef - A Prediction Model of the Incidence of Nonalcoholic Fatty Liver Disease With Visceral Fatty Obesity: A General Population-Based Study
Yang Zhou, Xiangping Chai, Tuo Guo, Yuting Pu, Mengping Zeng, Aifang Zhong, Guifang Yang, Jiajia Cai
Frontiers in Public Health.2022;[Epub] CrossRef - Non-alcoholic fatty liver disease and sarcopenia is associated with the risk of albuminuria independent of insulin resistance, and obesity
Eugene Han, Mi Kyung Kim, Seung-Soon Im, Byoung Kuk Jang, Hye Soon Kim
Journal of Diabetes and its Complications.2022; 36(8): 108253. CrossRef - Increased Risk of NAFLD in Adults with Glomerular Hyperfiltration: An 8-Year Cohort Study Based on 147,162 Koreans
Dae-Jeong Koo, Mi Yeon Lee, Inha Jung, Sun Joon Moon, Hyemi Kwon, Eun-Jung Rhee, Cheol-Young Park, Won-Young Lee, Ki Won Oh, Se Eun Park
Journal of Personalized Medicine.2022; 12(7): 1142. CrossRef - Effects of Avocado Oil Supplementation on Insulin Sensitivity, Cognition, and Inflammatory and Oxidative Stress Markers in Different Tissues of Diet-Induced Obese Mice
Schérolin de Oliveira Marques, Alexandre Pastoris Muller, Thais Fernandes Luciano, Natália dos Santos Tramontin, Mateus da Silva Caetano, Bruno Luis da Silva Pieri, Tatiane Lima Amorim, Marcone Augusto Leal de Oliveira, Cláudio Teodoro de Souza
Nutrients.2022; 14(14): 2906. CrossRef - Relationship Between Handgrip Strength and Laboratory Values in Adolescents With Non-Alcoholic Fatty Liver Disease
Si Yeong Lee, Yong Whi Jeong, Hong Koh, Yunkoo Kang
Journal of Clinical Densitometry.2022; 25(4): 490. CrossRef - Association between non-alcoholic fatty liver disease and metabolically healthy deterioration across different body shape phenotypes at baseline and change patterns
Liu Lei, Wang Changfa, Wang Jiangang, Chen Zhiheng, Yuan Ting, Zhu Xiaoling, Deng Yuling, Wang Yaqin
Scientific Reports.2022;[Epub] CrossRef - Muscle fat contents rather than muscle mass determines nonalcoholic steatohepatitis and liver fibrosis in patients with severe obesity
Eugene Han, Mi Kyung Kim, Hye Won Lee, Seungwan Ryu, Hye Soon Kim, Byoung Kuk Jang, Youngsung Suh
Obesity.2022; 30(12): 2440. CrossRef - Prediction of decreased estimated glomerular filtration rate using liver fibrosis markers: a renal biopsy-based study
Akira Mima
Scientific Reports.2022;[Epub] CrossRef - Therapeutic implications of shared mechanisms in non-alcoholic fatty liver disease and chronic kidney disease
Mehmet Kanbay, Mustafa C. Bulbul, Sidar Copur, Baris Afsar, Alan A. Sag, Dimitrie Siriopol, Masanari Kuwabara, Silvia Badarau, Adrian Covic, Alberto Ortiz
Journal of Nephrology.2021; 34(3): 649. CrossRef - Taxifolin ameliorate high-fat-diet feeding plus acute ethanol binge-induced steatohepatitis through inhibiting inflammatory caspase-1-dependent pyroptosis
Zi-Ying Zhan, Mei Wu, Yue Shang, Min Jiang, Jian Liu, Chun-Ying Qiao, Huan Ye, Yong-Ce Lin, Mei-Hua Piao, Rong-Hui Sun, Zhi-Hong Zhang, Jing-Ya Jiao, Yan-Ling Wu, Ji-Xing Nan, Li-Hua Lian
Food & Function.2021; 12(1): 362. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef - The Leg Fat to Total Fat Ratio Is Associated with Lower Risks of Non-Alcoholic Fatty Liver Disease and Less Severe Hepatic Fibrosis: Results from Nationwide Surveys (KNHANES 2008–2011)
Hyun Min Kim, Yong-ho Lee
Endocrinology and Metabolism.2021; 36(6): 1232. CrossRef - A preliminary report about the detection of ventricular repolarisation in patients with non-alcoholic fatty liver disease
Marwan S. Al-Nimer, Vian A. Esmail, Dler S. Hamid, Mohammad O. Mohammad
Journal of Taibah University Medical Sciences.2020; 15(4): 284. CrossRef - Atorvastatin attenuates obese-induced kidney injury and impaired renal organic anion transporter 3 function through inhibition of oxidative stress and inflammation
Nattavadee Pengrattanachot, Rada Cherngwelling, Krit Jaikumkao, Anchalee Pongchaidecha, Laongdao Thongnak, Myat Theingi Swe, Varanuj Chatsudthipong, Anusorn Lungkaphin
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2020; 1866(6): 165741. CrossRef - Correlation Between Non-Alcoholic Fatty Liver and Chronic Kidney Disease
Hasyim Kasim, St. Rabiul Zatalia, Haerani Rasyid, Syakib Bakri, Muhammad L. Parewangi, Fardah Akil, Arifin Seweng
The Open Urology & Nephrology Journal.2020; 13(1): 1. CrossRef - Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 382. CrossRef - Sarcopenia: an emerging risk factor for non-alcoholic fatty liver disease
Yong-ho Lee, Seung Up Kim
Hepatology International.2020; 14(1): 5. CrossRef - Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus
Hokyou Lee, Gyuri Kim, Young Ju Choi, Byung Wook Huh, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Eun Jig Lee, Yong-ho Lee, Kap Bum Huh
Diabetes & Metabolism Journal.2020; 44(2): 267. CrossRef - Ipragliflozin Additively Ameliorates Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Controlled with Metformin and Pioglitazone: A 24-Week Randomized Controlled Trial
Eugene Han, Yong-ho Lee, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha
Journal of Clinical Medicine.2020; 9(1): 259. CrossRef - Non-alcoholic steatohepatitis and progression of carotid atherosclerosis in patients with type 2 diabetes: a Korean cohort study
Hyeok-Hee Lee, Yongin Cho, Young Ju Choi, Byung Wook Huh, Byung-Wan Lee, Eun Seok Kang, Seok Won Park, Bong-Soo Cha, Eun Jig Lee, Yong-ho Lee, Kap Bum Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Hepatic fibrosis is associated with total proteinuria in Korean patients with type 2 diabetes
Eugene Han, Yongin Cho, Kyung-won Kim, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-wan Lee
Medicine.2020; 99(33): e21038. CrossRef - Association between NAFLD and risk of prevalent chronic kidney disease: why there is a difference between east and west?
Min Zhang, Su Lin, Ming-fang Wang, Jiao-feng Huang, Shi-ying Liu, Su-mei Wu, Hao-yang Zhang, Zi-mu Wu, Wen-Yue Liu, Dong-Chu Zhang, Chuan-ming Hao, Yue-yong Zhu, Ming-Hua Zheng, Xiao-zhong Wang
BMC Gastroenterology.2020;[Epub] CrossRef - Association Between Serum Bilirubin and the Progression of Carotid Atherosclerosis in Type 2 Diabetes
Inkuk Lee, Hyeok-Hee Lee, Yongin Cho, Young Ju Choi, Byung Wook Huh, Byung-Wan Lee, Eun Seok Kang, Seok Won Park, Bong-Soo Cha, Eun Jig Lee, Yong-ho Lee, Kap Bum Huh
Journal of Lipid and Atherosclerosis.2020; 9(1): 195. CrossRef - Letter: Sarcopenia Is Significantly Associated with Presence and Severity of Nonalcoholic Fatty Liver Disease (J Obes Metab Syndr 2019;28:129-38)
Chan-Hee Jung
Journal of Obesity & Metabolic Syndrome.2020; 29(2): 158. CrossRef - Metabolic Syndrome and Abnormal Peri-Organ or Intra-Organ Fat (APIFat) Deposition in Chronic Obstructive Pulmonary Disease: An Overview
Niki Katsiki, Anca Pantea Stoian, Paschalis Steiropoulos, Nikolaos Papanas, Andra-Iulia Suceveanu, Dimitri P. Mikhailidis
Metabolites.2020; 10(11): 465. CrossRef - Heart Failure and Liver Disease
Andrew Xanthopoulos, Randall C. Starling, Takeshi Kitai, Filippos Triposkiadis
JACC: Heart Failure.2019; 7(2): 87. CrossRef - Risk factors for non-alcoholic fatty liver disease-associated hepatic fibrosis in type 2 diabetes patients
Asieh Mansour, Mohammad Reza Mohajeri-Tehrani, Majid Samadi, Hadis Gerami, Mostafa Qorbani, Nick Bellissimo, Hossein Poustchi, Azita Hekmatdoost
Acta Diabetologica.2019; 56(11): 1199. CrossRef - Targeting CYP4A attenuates hepatic steatosis in a novel multicellular organotypic liver model
Jae-Sung Ryu, Minji Lee, Seon Ju Mun, Sin-Hyoung Hong, Ho-Joon Lee, Hyo-Suk Ahn, Kyung-Sook Chung, Gun-Hwa Kim, Myung Jin Son
Journal of Biological Engineering.2019;[Epub] CrossRef - Non-alcoholic steatohepatitis and type 2 diabetes mellitus: the effects of weight loss versus drug treatment
Niki Katsiki, Vasilios G Athyros
Current Medical Research and Opinion.2019; 35(7): 1305. CrossRef - Nonalcoholic Fatty Liver Disease in Diabetes. Part I: Epidemiology and Diagnosis
Yong-ho Lee, Yongin Cho, Byung-Wan Lee, Cheol-Young Park, Dae Ho Lee, Bong-Soo Cha, Eun-Jung Rhee
Diabetes & Metabolism Journal.2019; 43(1): 31. CrossRef - Progress in the Study of the Pathogenesis of Chronic Kidney Disease Associated with Nonalcoholic Fatty Liver Disease
清莲 宋
Advances in Clinical Medicine.2019; 09(09): 1073. CrossRef - Association Between Nonalcoholic Fatty Liver Disease and Future Deterioration of Metabolic Health: A Cohort Study
You‐Cheol Hwang, Hong‐Yup Ahn, Cheol‐Young Park
Obesity.2019; 27(8): 1360. CrossRef - Subfornical organ insulin receptors tonically modulate cardiovascular and metabolic function
Jin Kwon Jeong, Julie A. Horwath, Hayk Simonyan, Katherine A. Blackmore, Scott D. Butler, Colin N. Young
Physiological Genomics.2019; 51(8): 333. CrossRef - Nonalcoholic Fatty Liver Disease and Diabetes: Part II: Treatment
Kyung-Soo Kim, Byung-Wan Lee, Yong Jin Kim, Dae Ho Lee, Bong-Soo Cha, Cheol-Young Park
Diabetes & Metabolism Journal.2019; 43(2): 127. CrossRef - Chicken Protein Hydrolysates Have Anti-Inflammatory Effects on High-Fat Diet Induced Obesity in Mice
Thomas Aloysius, Ana Carvajal, Rasa Slizyte, Jon Skorve, Rolf Berge, Bodil Bjørndal
Medicines.2018; 6(1): 5. CrossRef - STK25 Regulates Cardiovascular Disease Progression in a Mouse Model of Hypercholesterolemia
Emmelie Cansby, Elin Magnusson, Esther Nuñez-Durán, Manoj Amrutkar, Matteo Pedrelli, Paolo Parini, Jenny Hoffmann, Marcus Ståhlman, Brian W. Howell, Hanns-Ulrich Marschall, Jan Borén, Margit Mahlapuu
Arteriosclerosis, Thrombosis, and Vascular Biology.2018; 38(8): 1723. CrossRef - Organ-Specific Mechanisms of Transendothelial Neutrophil Migration in the Lung, Liver, Kidney, and Aorta
Sanne L. Maas, Oliver Soehnlein, Joana R. Viola
Frontiers in Immunology.2018;[Epub] CrossRef - Visceral adiposity index as a predictor of NAFLD: A prospective study with 4‐year follow‐up
Chaonan Xu, Zhimin Ma, Yunfeng Wang, Xiangtong Liu, Lixin Tao, Deqiang Zheng, Xiuhua Guo, Xinghua Yang
Liver International.2018; 38(12): 2294. CrossRef - Obesity induced alterations in redox homeostasis and oxidative stress are present from an early age
Alfonso M. Lechuga-Sancho, David Gallego-Andujar, Pablo Ruiz-Ocaña, Francisco M. Visiedo, Ana Saez-Benito, Mónica Schwarz, Carmen Segundo, Rosa M. Mateos, Manuel Portero-Otin
PLOS ONE.2018; 13(1): e0191547. CrossRef - Capybara Oil Improves Hepatic Mitochondrial Dysfunction, Steatosis, and Inflammation in a Murine Model of Nonalcoholic Fatty Liver Disease
Polyana C. Marinho, Aline B. Vieira, Priscila G. Pereira, Kíssila Rabelo, Bianca T. Ciambarella, Ana L. R. Nascimento, Erika Cortez, Aníbal S. Moura, Fernanda V. Guimarães, Marco A. Martins, Gonzalo Barquero, Rodrigo N. Ferreira, Jorge J. de Carvalho
Evidence-Based Complementary and Alternative Medicine.2018; 2018: 1. CrossRef - Persistently Increased Resting Energy Expenditure Predicts Short-Term Mortality in Patients with Acute-on-Chronic Liver Failure
Jia Yao, Xiaoshuang Zhou, Hui Wang, Lili Yuan, Yu Chen, Zhongping Duan
Annals of Nutrition and Metabolism.2018; 73(1): 2. CrossRef - The Sodium-Glucose Cotransporter 2 Inhibitor Dapagliflozin Prevents Renal and Liver Disease in Western Diet Induced Obesity Mice
Dong Wang, Yuhuan Luo, Xiaoxin Wang, David Orlicky, Komuraiah Myakala, Pengyuan Yang, Moshe Levi
International Journal of Molecular Sciences.2018; 19(1): 137. CrossRef - Association of sex hormone-binding globulin with nonalcoholic fatty liver disease in Chinese adults
Jing Luo, Qian Chen, Tianran Shen, Xu Wang, Wanjun Fang, Xiaocai Wu, Zenan Yuan, Gengdong Chen, Wenhua Ling, Yuming Chen
Nutrition & Metabolism.2018;[Epub] CrossRef

 KDA
KDA PubReader
PubReader Cite
Cite