Small Rice Bowl-Based Meal Plan for Energy and Marcronutrient Intake in Korean Men with Type 2 Diabetes: A Pilot Study
Article information
Abstract
Background
Koreans eat rice, which is usually served in a rice bowl. We investigated the effect of a meal plan using small rice bowls on the total energy intake (TEI) and the marcronutrient intake in Korean men with type 2 diabetes.
Methods
A total of 62 men with type 2 diabetes were divided by body mass index (BMI) (normal weight [NW], BMI<23 kg/m2; overweight [OW], 23≤BMI<25 kg/m2; obese [OB], BMI≥25 kg/m2) and proportions of carbohydrate intake to TEI (PCI) (low carbohydrate intake [LC], <55%; recommended carbohydrate intake [RC], ≥55% and ≤60%; high carbohydrate intake [HC], >60%). The 3-day dietary records were analyzed for TEI and proportions of macronutrients, before and 2 weeks after a small-sized (300 mL) rice bowl based education was given.
Results
There were no significant differences in the age and BMI within the sub-groups by BMI and PCI groups. In baseline, the ratio of TEI to recommended total energy intake (RTR) of OW and OB were higher than that of NW. The PCI of HC was higher than that of LC and alcohol intake of HC was lower than that of LC. After education, the reduction of RTREI in OB was higher than that in OW and NW. The reduction of PCI in HC was higher than that of LC.
Conclusion
A small rice bowl based meal plan was effective for the reduction of energy intake and control of marcronutrient intake in Korean obese men with type 2 diabetes consuming a high carbohydrate diet.
INTRODUCTION
Medical nutritional therapy is an important part of diabetes prevention, management and plays an important role in preventing complications with blood glucose control. In order to achieve these goals, adequate total energy intakes (TEI) and macronutrient compositions are recommended for diabetes patients, and these informations must be presented to patients using the easily understandable methods [1].
Dietary patterns are closely associated with blood glucose control levels in type 2 diabetes patients. Nanri et al. [2] reported that a dietary characterized by frequent intake of white rice was a positively associated with glycated hemoglobin (HbA1c) levels in Japanese men and women. According to the 2008 Korean National Health Statistic and the Korean National Health and Nutritional Examination Survey [3,4], rice as the main source of carbohydrate rich foods in Korean male patients was investigated and proportion of carbohydrate intake to TEI (PCI) was 66.2%, which was higher than the level recommended by the Korean Diabetes Association [5]. These results show that control of rice consumption is important point to reduce the level of carbohydrates consumption in Korean male diabetes patients.
Ahn et al. [6] reported that there was an association between the size of the rice bowl and energy intake from the rice in males, and he investigated the effectiveness of the 380 mL rice bowls to reduce carbohydrate consumption in diabetes patients. It was shown that the size of the rice bowls should be reduced depended on each subject. Additionally, a report of task force team for basic statistical study [7] showed that male diabetes patients eat out more often than female patients, and 61.5% of male diabetes patients consume alcohol more than once a month, while 19.5% of female diabetes patients consume alcohol more than once a month, which denotes a gender based difference in eating out and alcohol consumption.
In order to regulate energy intake and marcronutrient compositions in type 2 diabetes patients, food exchange lists are commonly used [8-10]. However, it is difficult for patients who have low cognitive abilities to understand the contents of the educational information [10-12]. For this reason, a simplified education method is recommended. European countries use this kind of simplified method to convey the message that a medium sized bowl will help control energy intake and marcronutrient composition [1,11,12]. However, research is lacking in how to simplify ways to reduce carbohydrate intake in Korean male type 2 diabetes patients whose consumption patterns are unlike those of individuals from foreign countries.
In this study, the effects of meal plan method using the bowl which is smaller than conventionally used bowl on TEI amd marcronutrient composition according to the body mass index (BMI) and PCI in male type 2 diabetes patients with different dietary patterns from female. This study was a short-term 2 week study that was part of a preliminary study examining male diabetes patients for effective meal planning based on bowl size.
METHODS
Subjects
This study was performed between July 2009 and February 2010 at the Eulji Hospital Diabetes Center on diabetes patients between the ages of 30 to 70. This study analyzed a total of 62 patients, and excluded patients with glycated hemoglobin levels between 7% and 11%, special diets (e.g., vegetarian), type 1 diabetes, cancer, secondary diabetes, patients who were difficult to follow, patients who refused to follow up, patients with indigestion or poor appetites, patients undergoing renal replacement therapy, patients who ordinarily used rice bowls smaller than 300 mL, and patients who consumed foods that were different from their usual diet for three days.
Group definitions based on BMI and PCI
Male diabetes patients were classified by BMI and PCI, and the details were analyzed. The groups for BMI were separated into the normal weight group (NW; BMI<23 kg/m2, n=13) overweight group (OW; 23 kg/m2≤BMI<25 kg/m2, n=16), and obese group (OB; BMI≥25 kg/m2, n=33), and then comparatilvely analyzed. The groups for PCI by the Korean Diabetes Association (KDA) recommendation [5] were separated into the low carbohydrate intake (LC; <55%, n=18), recommended carbohydrate intake (RC; ≥55% and ≤60%, n=18), and high carbohydrate intake (HC; >60%, n=26)
Diet intervention
After 300 mL rice bowl (Sungwoo, Seoul, Korea) that held approximately 300 kcal was supplied for study participants, a 5-minute 1:1 individual education session was provided regarding tips on how to fill the bowl and methods for utilization. The rice of 300 kcal was calculated below method. First, required daily TEI of the male participants was used on anthropometric data from a multicenter study performed by Sohn et al. [13], and the method recommended by the KDA (ideal body weight×30 kcal). Using this method, daily TEI was calculated to be 1,900 kcal/day, the macronutrient consumption recommended by the KDA was considered, and the serving portion for each meal was set at 300 kcal, and the size of the rice bowl was determined.
We educated to have the participants use the bowl for every meal, and they were educated to fill it with rice so it did not overflow and to use restraint. We offered leaflets containing pictures and tips on how to fill rice bowls to participants so that they could pass the information on to their spouses. Noodles could substitute for rice but any specific amount for that was not suggested. Carbohydrate sources such as bread, rice, potatoes, sweet potatoes, flour pancakes, etc., were limited through the leaflet and fruit consumption was educated regarding the amount that can be consumed daily. Through a preliminary investigation, a leaflet was made about common foods for dieting such as fish and vegetable side dishes. For fish, meat, and vegetables, the subjects were educated with pictures of diet fitting each food exchanges unit and were asked to practice it but that was not emphasized intensively at each visit.
Survey of bowl size and bowl use compliance
The subjects were asked to bring the bowl that they used most often. Because the shape and sizes of the bowls were varied, bowls were filled with water, and the volume of the water from the bowls was measured with 100 mL and 500 mL graduated cylinders. In order to evaluate the compliance of bowl use, subjects were instructed to record whether they used the provided bowls for breakfast, lunch, and dinner, and then patients were instructed to bring those records to their biweekly visits. During each visit, the reported values werea averaged and overall compliance was calculated as:
Compliance of use of bowl (%)=number of using bowl/number of total meals×100
Definitions and analysis of the intake of staple foods, snacks, and alcohol
Staple foods were defined as the meals of consuming at the three regular meal times. Snacks were defined as the fruit and dairy group classified into the food exchange list and the meal of consumed outside of regular meal times (excluding alcohol). Intake of staple foods, snacks, and alcohol were monitored using 3 day dietary record (2 weekdays, 1 weekend day). The subjects were educated on the diet record method simply before writing the record sheet actually and they were asked to write amount and kinds of all foods taken for a meal, nutrition supplementary foods and snack for a day on the dietary record sheet by themselves. To increase accuracy of the record, a registered dietitian reviewed contents of the sheets by using real-sized food models measuring cups, measuring spoons, when the sheets were returned. For a dietary record resource, CAN-Pro (computer-aided nutritional analysis program, version 2.0; Korean Nutrition Society, Seoul, Korea) was used to convert nutrient intake for further analysis [14].
Anthropometric measurement and biochemical tests
The height and body weight of all study participants was measured. Subjects were measured for height and body weight dressed in a thin clothe. BMI was calculated by dividing body weight (kg) with the square of the height (m2). Waist circumference was measured in the narrowest area between the bottom of the ribs to the top of the iliac crest using a tape measure when subjects were relaxed and had exhaled. Venous blood samples were collected following a 10-hour or longer fast. Samples were separated via centrifuge at 3,000 rpm for 15 minutes. Serum was isolated, stored at -70℃, and used for analysis. Fasting plasma glucose was measured using the glucose oxidation method, and glycated hemoglobin (HbA1c) was measured using high performance liquid chromatography. Total cholesterol, triglycerides, high density lipoprotein cholesterol, and low density lipoprotein cholesterol were examined with kit using enzymatic reactions and an automatic biochemical analyzer (Hitachi 7170; Hitachi Co., Tokyo, Japan).
Statistical analysis
Using the statistics program SPSS version 15.0 (SPSS Inc., Chilcago, IL, USA), we calculated means and standard deviations for the measured items. To determine the differences in physical characteristics and nutritional intake between measurements before and after the 2 weeks among the groups was analyzed by one-way ANOVA test and those for each group were by paired t-test, A Kruskal-Wallis test was used to analyze variables from the three group comparison that did not follow normal distribution. P values under 0.05 were considered to be statistically significant.
RESULTS
Characteristics of study participants
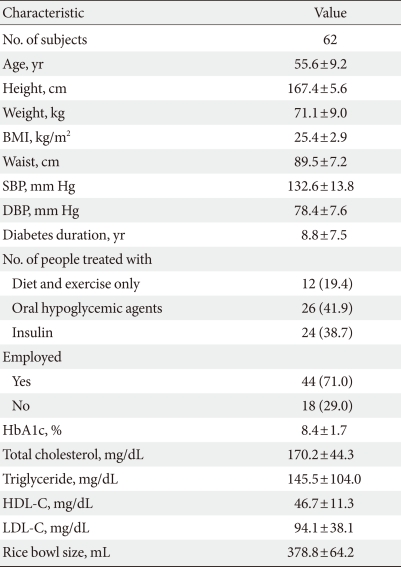
A total of 70 patients were recruited in this study, but among them, patients who ate abnormal foods (n=2), patients who declined to participate (n=3), and patients who used bowls that were under 300 mL (n=3) were exclude. The mean age of subjects was 55.6±9.2, diabetes duration was 8.8±7.5 years, BMI was 25.4±2.9 kg/m2, and HbA1c was 8.4±1.7%. For diabetes treatments, the proportion of insulin, oral hypoglycemic agents and lifestyle modification only were 38.7%, 41.9%, and 19.4%, respectively. A total of 82.3% of the subjects had received diabetes education before participating this study, 71.0% of the subjects had jobs. The mean number of eating out per week was 4.5±4.3, the number of consummimg alcohol per week was 1.3±1.5, and when they consumed alcohol, they consumed 4.5±6.6 servings of alcohol (1 serving=15 g alcohol) (Table 1) [15]. The median surveyed value of the volumes of the rice bowls measured with the graduated cylinders was 378.8 mL. However, the sizes ranged from 310 mL to 740 mL meaning that the largest bowl was 2.4 times larger than the smallest bowl, and there was only a 65.0% compliance with use of the rice bowl provided for the study. When the groups were classified by BMI and PCI, there were no significant differences in the dropout rate, average age, diabetes duration, HbA1c, treatmentmethods, occupation, the number of eating out, and bowl size.
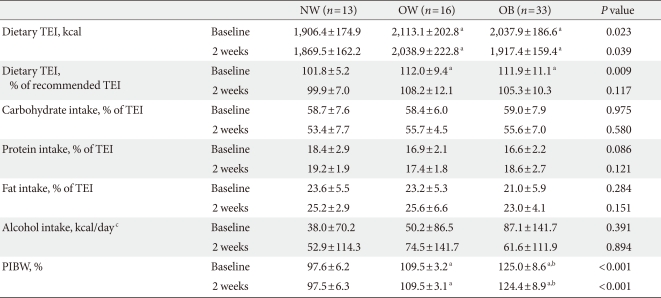
Changes in TEI and marcronutrient composition by BMI
As dietary TEI differed according to BMI, the ratio of TEI to recommended TEI (RTR) was assessed for each patient. The recommended TEI was obtained by multiplying 30 kcal per ideal body weight (IBW).
When the groups were classified by the BMI, the RTR in the OW and OB group was significantly higher than in the NW group (P=0.009) at baseline. However, the reduction of RTR in the OB group was -6.3±4.5%, which was a much larger reduction than in the NW group (P=0.043) (Table 2, Fig. 1). At baseline, the proportions of the carbohydrate, protein and fat to TEI were 58.8%, 17.1%, and 22.1%, which were within the recommednded the KDA (carbohydrate:protein:fat=55-60%: 15-20%:20-25%). The changes in the proportions of carbohydrates, protein, and fat to TEI showed no significant difference between the three groups (Table 2, Fig. 1). At baseline, alcohol consumption was not different between the three groups, and the reduction in alcohol intake among the three groups was also not different (Table 2).

Change in total energy intake (% of recommended TEI) (A), carbohydrate intake (% of TEI) (B), protein intake (% of TEI) (C), and fat intake (% of TEI) (D) according to body mass index after 2 weeks of bowl based education in men with type 2 diabetes mellitus. NW, normal weight (<23 kg/m2); OW, overweight (≥23 kg/m2 and <25 kg/m2); OB, obese (≥25 kg/m2); TEI, total energy intake. aP values<0.05 vs. Baseline, bP values<0.05 vs. NW.
Changes in the PCI and marcronutrient intake
When the groups were classified by the PCI, the RTR was not different among the groups at baseline, and the changes in the RTR were also not different among the groups after intervention.
At baseline, the PCI in the HC group was higher than the LC group (P<0.001), and the proportions of protein (P=0.003) and proportions of fat (P<0.001) was lower. In particular, the PCI froms staple foods in the HC group was higher than the LC group (P=0.005). The PCI from snack was not different among the groups. The decrease in the PCI was significantly higher in the HC group than the LC and RC groups (P=0.001). The increase in the proportions of protein to TEI was significantly higher in the HC group and RC group than in the LC group (P=0.001), and the increase in the proportions of fat to TEI was significantly higher in the HC group than in the RC and LC groups (P=0.001) (Table 3, Fig. 2).
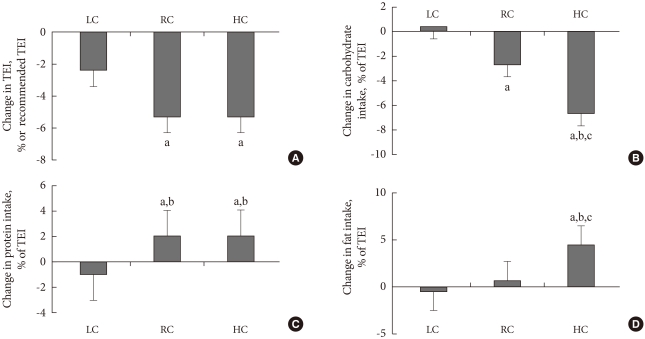
Change in total energy intake (% of recommended TEI) (A), carbohydrate intake (% of TEI) (B), protein intake (% of TEI) (C), and fat intake (% of TEI) (D) according to proportions of carbohydrate intake after 2 weeks of bowl based education in men with type 2 diabetes mellitus. LC, low carbohydrate intake (<55%); RC, recommended carbohydrate intake (≥55% and ≤60%); HC, high carbohydrate intake (>60%); TEI, total energy intake. aP values<0.05 vs. Baseline, bP values<0.05 vs. LC, cP values<0.05 vs. RC.
The results of the analysis of PCI from staple foods and snacks showed that the reduction in PCI from staple foods was significantly higher in the HC group than in the LC group (P=0.005), however, there was no significant difference of the PCI from the snack among the groups. At baseline, the alcohol consumption of the LC group was 157±173 kcal/day, which was significantly higher than in the RC and HC groups (P=0.002), and after intervention, there was no significant difference in the reduction of alcohol consumption between the three groups.
Changes in body weight
As the change in body weight differed according to obesity, the ratio of body weight to ideal body weight (RBI) was assessed for each patient. The RBI was calculated as: current body weight/ideal body weight×100.
When the groups were classified by BMI, the RBI was significantly higher in the OB than in the OW and NW group (P<0.001) at baseline, but the changes in the RBI was not different among the three groups.
When the groups were classified by PCI, the RBI was not different among the groups at baseline, and the change in the RBI was also not different among the groups.
When the groups were classified by BMI, the RBI of the OB group was significantly decreased after 2 weeks (P=0.016). When the groups were classified by PCI, the RBI of the HC group was significantly decreased after 2 weeks and that it was close to the ideal body weight (P=0.028).
DISCUSSION
According to the 2008 Korean National Health Statistics [3], males consume 1.7 times more meat than females, also alcohol and beverage consumption of males was 2.3 times higher than females, therefore, it was reported that males consume more protein and fat rich foods than females. Data from the 2005 Korean National Health and Nutrition Examination Survey [4], demonstrate that the PCI in male type 2 diabetes patients was 66.2%, which was lower than that of females, at 70.3%, and the proportions of fat to TEI in males was reported to be higher than in females. Nevertheless, the PCI in male diabetes patients was still higher than that recommended by the KDA [5], although the proportions of fat to TEI were within the recommended levels. However, the proportions of carbohydrate, protein and fat to TEI in male diabetes patients who participated in this study were 58.8%, 17.1%, and 22.1%, respectively, which are within the values recommended by the KDA [5], but this was lower than the PCI data from the 2005 Korean National Health and Nutrition Examination Survey [4]. However, in studies that examined the relationship between alcohol and marcronutrient composition in male type 2 diabetes patients performed by Chung and Chang [16] and Yoen et al. [17], the proportions of carbohydrate, protein, and fat to TEI were reported to be 58.0% to 60.4%, 16.0% to 17.1%, and 23.6% to 25.0%, respectively. Those results were similar to the results from our study. These variations were considered to result from similarity in marcronutrient composition according to age [18], the availability of diabetes education [19,20], and social classes [21-23].
When the groups were classified by BMI, the 300 mL bowl based meal plan was more effective for reduction of TEI in OB group than the NW group. However, in female diabetes patients, these results showed that reduction of TEI was more effective in both the OW and OB groups than the NW group. When the groups were classified by BMI, there were no significant differences in changes on macronutrient composition in men and women.
The TEI for Korean diabetes patients who eat a rice-based diet is dependent on the absolute amount of rice consumed and it has been shown that the energy intake from the rice has an influence on the energy intake from side dishes as well [24]. For these reasons, although there was a large reduction in TEI in the OB group, it is likely that there will be no change in marcronutrient composition.
When the groups were classified by PCI, at baseline, the PCI was higher in the HC group than in the LC group, and the proportions of protein and the proportions of fat were lower. The proportions of carbohydrate from staple foods were especially high, and the proportions of fat and alcohol consumption were lower. Alcohol only provides energy (kcal), and was listed as an empty calorie food. Nevertheless, the reason there is a difference in marcronutrient composition for those who consume alcohol is that foods served with alcohol has an increased the proportions of fat. Chung and Chang [16] reported that the proportions of carbohydrate, protein, and fat from foods consumed with alcohol was 10.4%, 25.9%, and 62.3%, respectively, but these results demonstrated that this is caused by a high proportions of fat intake in the high alcohol consumption group. After the planned meals using the small 300 mL rice bowls, the PCI decreased in the HC group significantly more than in the LC group, and the proportions of protein and fat to TEI increased. These results show that male diabetes patients who comume small amount of alcohol and high carbohydrate meals of over 60% from staple foods had a decreased the proportions of carbohydrate from staple foods, which changes marconutrient composion; this was effective at reducing total energy intake.
According to the Kang et al. [25], there was no difference in TEI and marcronutrient composition between education group who was educated for 1 year via individual and e-mail with regular meal, limited snacks and alcohol, increased consuming of fruits and vegetables and control group.
Although comparing the results directly and drawing conclusion are difficult because of a difference in the study period and education method of each study, making changes in long term dietary energy and marcronutrient composition was challenging in male diabetes patients.
In the study performed by Kang et al. [25], even when education was performed continuously for 1 year, and daily alcohol consumption changed from 232 kcal to 266 kcal after 1 year, which was a very small change in consumption, these results were consistent with the results from our study. There was no significant decrease in the alcohol consumption of male diabetes patients who were using the planned meals with the 300 mL bowls provided in this study, even though we had expeceted that using education regarding the smaller bowl would have a positive effect. Therefore, this shows that a different educational approach is required.
When the groups were classified by BMI or PCI, there was no significant difference in body weight loss wtihin both groups. However, in the before and after 2 weeks comparion, the OB group and HC group showed a decrease in body weight. In which, the result may indicate to the possibility of long term weight loss.
Our study period was a two-week to examine changes of TEI after using a smaller rice bowl, but this short perid made it difficult to determine the effect a reducing body weight, lipid and blood glucose level. In this study, the sizes of bowls regularly used were between 310 mL and 740 mL, and when the patients were educated on using the 300 mL rice bowl, they complained about hunger. However, before and after education, the visual analogue scale measurement results for hunger and satiety levels exhibited no statistical differences (data not presented). This reduced the amount of rice consumed from the rice bowl method in the OB group, which greatly reduced total energy consumption, along with the increase in side dish consumption, demonstrated this expected result as well. In addition, 71% of study subjects had jobs, so there were difficulties with using the bowl during restaurant meals. Nevertheless, the rice bowl consistency expectancy was set at 65% compliance, and excluding dining out, bowl compliance was over 90% (data not presented).
A previous study that analyzed the obstacles and the compliance of using a rice bowl indicated that patients who have experienced in using bowls before developed a sense for correct volumes [6]. Thus, patients with that experience could control the amount of food consumed even without using the bowls, which might have worked positively in controlling the amount of their food intake.
A small rice bowl based meal plan was an effective education method for the reduction of energy intake in obese men with type 2 diabetes and reduction of PCI as staple foods in men with type 2 diabetes consuming more than 60% PCI as staple foods. In order to generalize the effect of using the small rice bowl for planned meals in male diabetes patients, more study subjects and more observation in long-term energy consumption, marcronutrient composition, and clinical changes are needed.
Notes
No potential conflict of interest relevant to this article was reported.