Clinical Characteristics of Diabetic Patients Transferred to Korean Referral Hospitals
Article information
Abstract
Background
We evaluated the disease profile and clinical management, including the status of both glycemic control and complications, in patients with diabetes who were transferred to referral hospitals in Korea.
Methods
Patients referred to 20 referral hospitals in Gyeongsangnam/Gyeongsangbuk-do and Jeollanam/Jeollabuk-do with at least a 1-year history of diabetes between January and June 2011 were retrospectively reviewed using medical records, laboratory tests, and questionnaires.
Results
A total of 654 patients were enrolled in the study. In total, 437 patients (67%) were transferred from clinics and 197 (30%) patients were transferred from hospitals. A total of 279 patients (43%) visited higher medical institutions without a written medical request. The main reason for the referral was glycemic control in 433 patients (66%). Seventy-three patients (11%) had received more than one session of diabetic education. Only 177 patients (27%) had been routinely self-monitoring blood glucose, and 146 patients (22%) were monitoring hemoglobin A1c. In addition, proper evaluations for diabetic complications were performed for 74 patients (11%). The most common complication was neuropathy (32%) followed by nephropathy (31%). In total, 538 patients (82%) had been taking oral hypoglycemic agents. A relatively large number of patients (44%) had been taking antihypertensive medications.
Conclusion
We investigated the clinical characteristics of diabetic patients and identified specific problems in diabetic management prior to the transfer. We also found several problems in the medical system, which were divided into three medical institutions having different roles in Korea. Our findings suggested that the relationships among medical institutions have to be improved, particularly for diabetes.
INTRODUCTION
Diabetes mellitus (DM) is a prevalent and serious global health problem. The number of patients with diabetes worldwide is expected to increase by 11.4% from 366 million in 2011 to 552 million by 2030, affecting one in 10 adults [1]. In particular, the number of people affected in the Asia-Pacific area is expected to increase to 136 million by 2025, and the same trend is expected in Korea [2,3]. The prevalence of diabetes in Korea has increased 6- to 7-fold from 1.5% to 9.9% over the past 40 years [3,4]. The increased prevalence is most likely attributable to rapid economic development, improved living standards, an aging population, and a Westernized lifestyle [2,5].
The global increase in the prevalence of diabetes will inevitably result in increases in the prevalence of diabetic microvascular and macrovascular diseases and, consequently, significantly higher healthcare expenditures [6]. In Korea, diabetes and its complications have become major causes of mortality. The mortality rate of diabetes has doubled from 17.2 per 100,000 persons in 1995 to 24.2 per 100,000 persons in 2005 [4,7]. Although diabetes-related mortality has decreased from 25.1 per 100,000 persons in 2002 to 19.6 per 100,000 persons in 2009, it increased to 21.5 per 100,000 persons in 2011, and diabetes is the fifth leading cause of death in Korea [7]. The rate of death among patients with diabetes is approximately twice the rate among persons without diabetes, and most of the causes of death are complications related to diabetes [8]. Despite the seriousness of diabetic complications, 30% to 70% of patients receive inadequate care and only 40% achieve optimal control, which is defined as a hemoglobin A1c (HbA1c) level <7% in Korea [9,10]. The serious outcomes in patients with diabetes have prompted the need for more aggressive efforts to provide optimal monitoring and care.
Medical institutions in Korea are divided into clinics (primary centers), secondary hospitals, and tertiary hospitals. The clinic as a primary healthcare system is the first line of care for a number of common diseases and serves the basic medical needs of the population, while secondary and tertiary hospitals have roles in treating patients with more severe diseases. Thus, the clinic is considered as an institution mainly for treating outpatients, while the hospital provides mostly inpatient care. There are no restrictions on the use of health care services at each medical institution, but a medical treatment request is required to receive medical insurance benefits in tertiary medical institutions. Additional costs and burden rates are also applied to patients when visiting higher medical institutions to encourage the use of step-by-step medical services. In this system, cooperation with each institution type is particularly important with regard to all diseases, including DM. However, the present imbalance of supply and demand among these institutions has resulted in the ineffective use of healthcare resources and a lower quality of medical care. Thus, we analyzed the clinical characteristics and current medical patterns of patients with diabetes in referral hospitals and discuss several problems in the Korean medical system.
METHODS
Materials
Patients referred to 20 referral hospitals in Gyeongsangnam/Gyeongsangbuk-do and Jeollanam/Jeollabuk-do with at least a 1-year history of DM between January and June 2011 were reviewed retrospectively using medical records, laboratory tests, and questionnaires. Fifty consecutive patients from each referral hospital were selected for analysis. Patients who were evaluated incompletely after referral, referred from another tertiary hospital, or referred without proper diagnostic evaluations performed at the previous hospital were excluded from the study.
Treatments given and the clinical histories of the patients were analyzed using questionnaires. In addition, the presence of diabetic complications or comorbidities was determined using medical records and the results of the laboratory tests from the visit. When assessing macrovascular complications, coronary artery disease (CAD) was defined as angina pectoris and myocardial infarction and was diagnosed based on medical records or coronary angiography, while stroke was defined based only on medical records. Peripheral artery disease (PAD) was diagnosed using ultrasound or computed tomography angiography. When assessing microvascular complications, retinopathy was diagnosed using fundus photography or ophthalmoscopy, and nephropathy was defined as the presence of microalbuminuria or macroalbuminuria. The reference ranges of the urinary albumin-to-creatinine ratio (ACR) (with albumin measured in milligrams and creatinine measured in grams) used to define microalbuminuria and macroalbuminuria were 30 to 300 µg/mg and >300 µg/mg in random urine samples, respectively. The estimated glomerular filtration rate (eGFR) was calculated using the Modification of Diet in Renal Disease calculation: 186×serum creatinine (mg/dL)-1.154×age-0.203×0.742 (if female) [11]. In addition, diabetic neuropathy was determined based on symptoms and signs evaluated by physicians or medication history related to diabetic neuropathy.
The study was approved by the local ethics committees of each hospital.
Statistical analysis
All results are presented as the mean±standard deviation for normally distributed values, as the median (interquartile range) for nonparametric values, or as percentages. Data were entered and analyzed using SPSS version 17.0 (SPSS Inc., Chicago, IL, USA). In all analyses, P<0.05 indicated statistical significance.
RESULTS
Patient characteristics
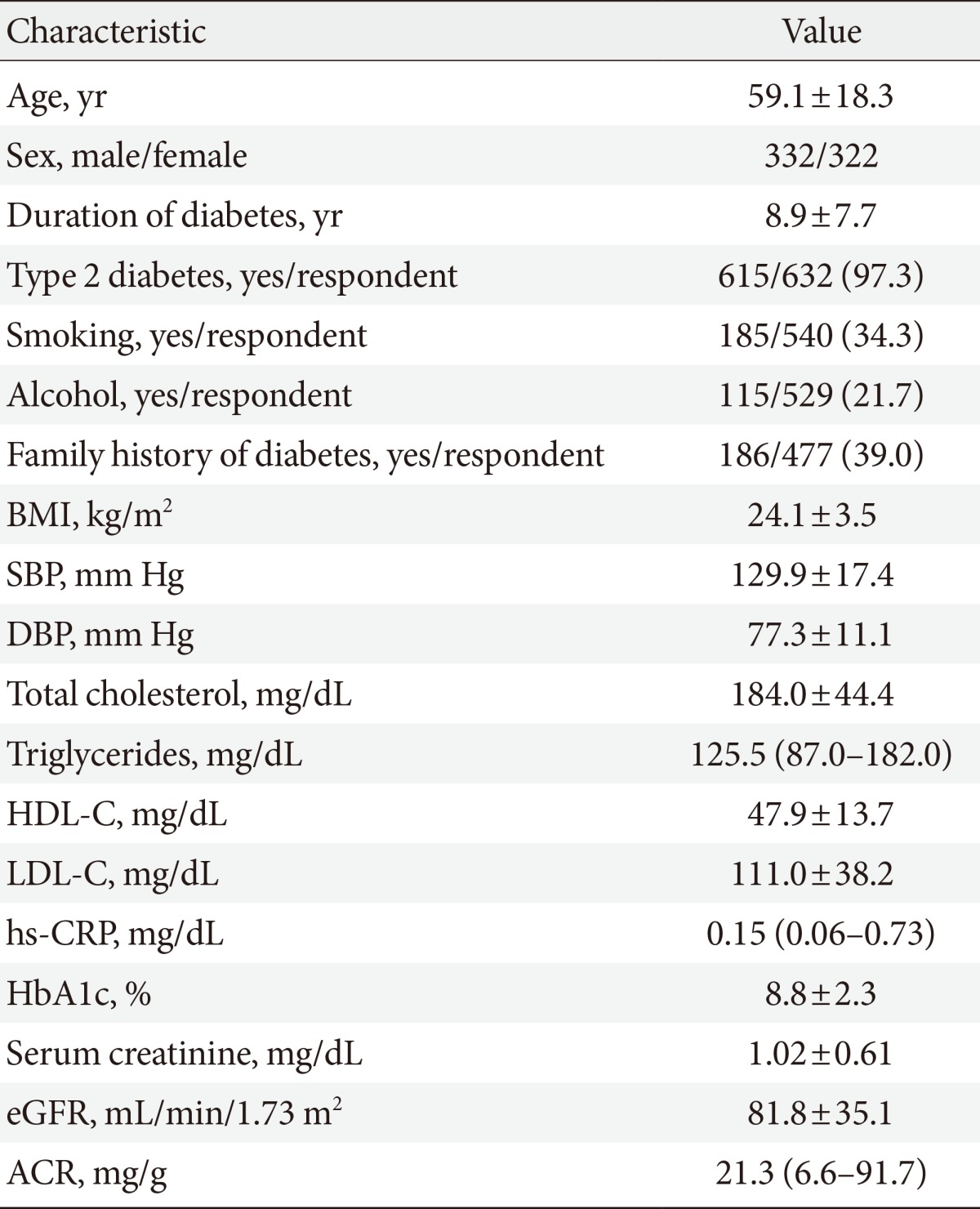
A total of 654 consecutive patients (332 males and 322 females; mean age, 59.1±18.3 years) were enrolled for analysis. The mean duration from diagnosis of DM was 8.9±7.7 years. Other clinical characteristics were as follows: body mass index, 24.1±3.5 kg/m2; systolic blood pressure, 129.9±17.4 mm Hg; diastolic blood pressure, 77.3±11.1 mm Hg; total cholesterol, 184.0±44.4 mg/dL; triglycerides, 125.5 mg/dL (range, 87.0 to 182.0 mg/dL); high density lipoprotein cholesterol, 47.9±13.7 mg/dL; low density lipoprotein cholesterol, 111.0±38.2 mg/dL; high-sensitivity C-reactive protein, 0.15 mg/dL (range, 0.06 to 0.73 mg/dL); HbA1c, 8.8%±2.3%; serum creatinine, 1.02±0.61 mg/dL; eGFR, 81.8±35.1 mL/min/1.73 m2; and ACR, 21.3 mg/g (range, 6.6 to 91.7 mg/g) (Table 1).
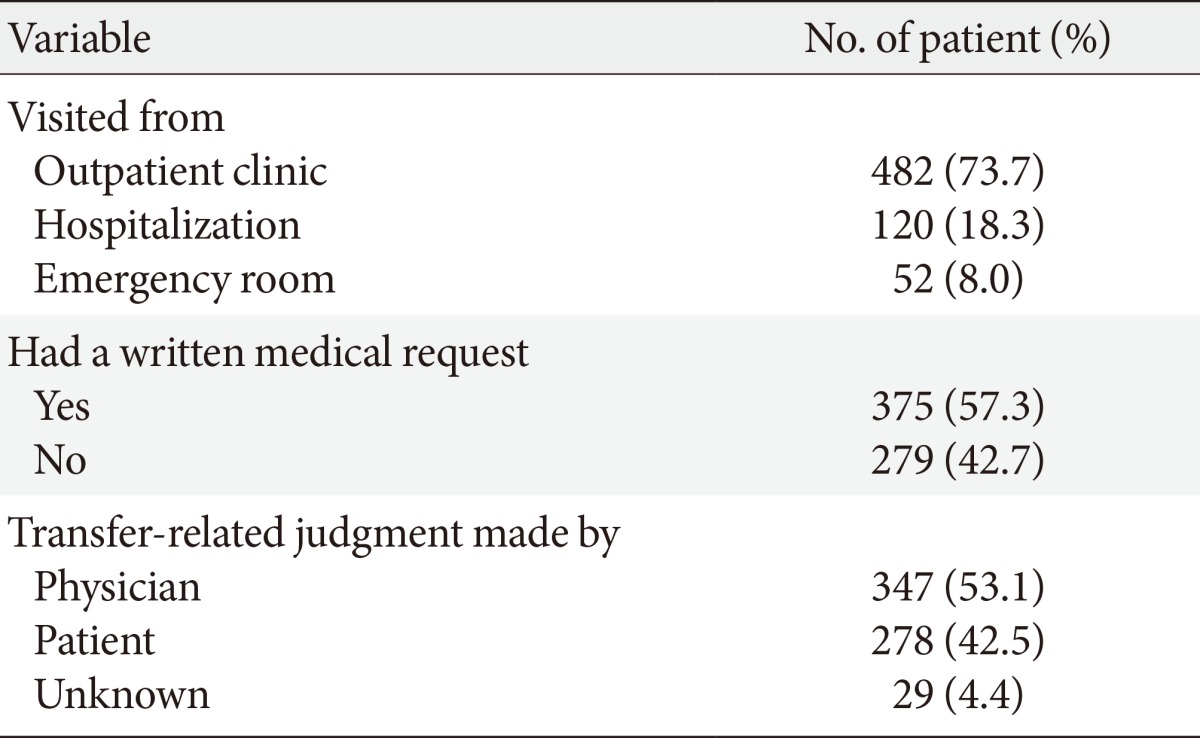
Type of higher medical institution visit
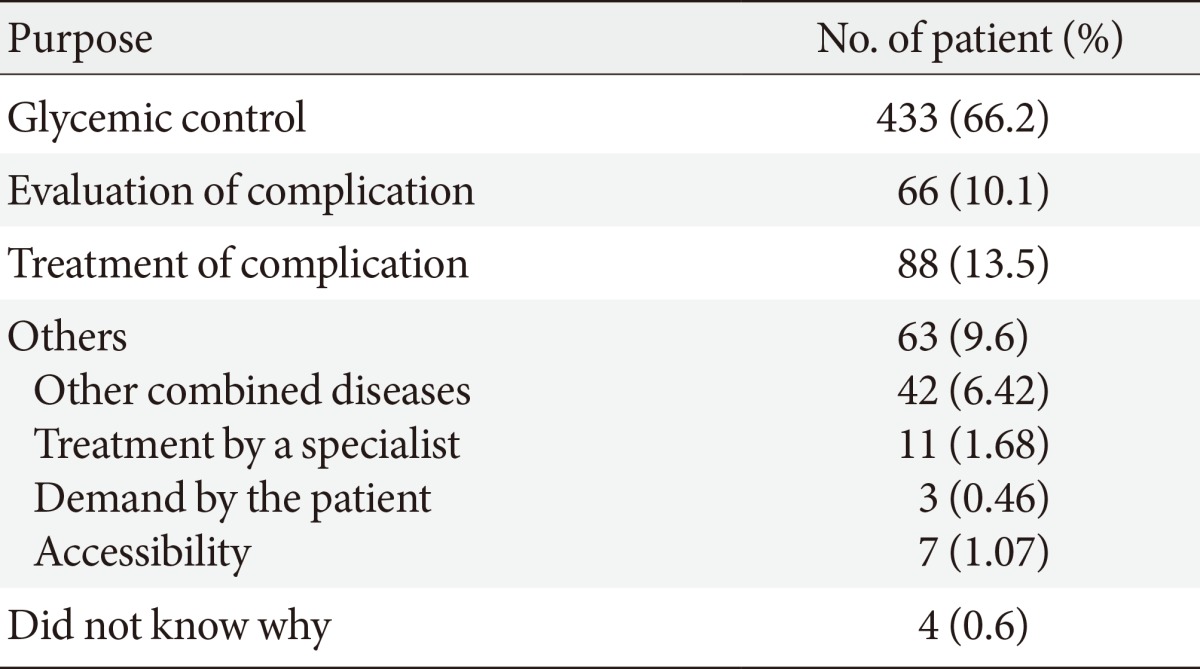
Of the 654 patients, 437 (66.8%) were transferred from clinics and 197 (30.1%) from secondary hospitals. The remaining patients were referred from public health centers or nursing homes (Table 2). A total of 482 patients (73.7%) were initially treated on an outpatient basis, whereas 120 patients (18.3%) and 52 (8.0%) were initially treated during admission or in the emergency department, respectively. In total, 279 patients (42.7%) visited a higher medical institution without a written medical request, and 347 patients (53.1%) responded that a physician made the transfer decision (Table 3). The main reasons for referral were glycemic control in 433 patients (66.2%), management of diabetic complications in 88 patients (13.5%), and evaluation of diabetic complications in 66 patients (10.1%). Other causes included comorbidities of DM (6.42%) and patient preference for place of treatment (1.07%) (Table 4).
Status of previous diabetic management
Of the total patients enrolled in the study, only 73 (11.1%) had experience with more than one session of diabetic education, and the rest had never experienced education or did not know. Only 177 patients (27.1%) had been routinely using self-monitoring blood glucose (SMBG), and 146 patients (22.3%) had been monitoring HbA1c according to a disjunctive yes/no question (Table 2). Only 74 patients (11.3%) had undergone proper evaluation of diabetic complications according to the questionnaires; 251 patients (38.4%) had not been advised to undergo assessment, and 44 patients (6.7%) had rejected assessment despite their physician's recommendation. Thus, many of the patients had not been tested for complications of DM (45.1%) or did not know whether they had been evaluated (43.6%). Some patients who had been evaluated did not know whether they had complications. In patients who had been examined for diabetic complications, the most common examination performed was testing for retinopathy (65 patients, 87.8%), and diabetic complications were categorized as cardiovascular disease, retinopathy, nephropathy, and neuropathy (Table 2).
Microvascular complications were more common than macrovascular complications: neuropathy (153 patients, 32.2%), nephropathy (153 patients, 30.5%), followed by retinopathy (112 patients, 26.5%). As expected, the prevalence of CAD, which is classified as a macrovascular disease, was highest (45 patients, 11%), followed by stroke (36 patients, 9.7%) and PAD (26 patients, 6.6%) (Fig. 1).

Prevalence of diabetic complications in referred patients. The prevalence of macrovascular complications, including coronary artery disease (CAD), stroke, and peripheral artery disease (PAD), was lower than that of microvascular complications, including diabetic retinopathy, nephropathy, and neuropathy.
Of 654 patients, 538 patients (82.3%) had been using oral hypoglycemic agents, and information regarding medication was obtained for 385 patients (71.6%). Sulfonylurea (291 patients, 75.6%) and metformin (271 patients, 71.2%) were the most frequently used drugs, and thiazolidinedione (34 patients, 8.8%) was the least frequently used. A total of 122 patients (18.7%) replied that they had injected insulin, and only 107 of these patients (87.7%) knew the type of insulin that they had used. A relatively large number of patients (285 patients, 43.6%) had been taking antihypertensive medication, and approximately half of the patients (149 patients, 69.3%) were using an angiotensin receptor blocker. Few patients had been using lipid-lowering agents, such as statins (124 patients, 19%) or fibrate (10 patients, 1.5%). In addition, some patients (179 patients, 27.4%) had been taking antiplatelet medications (Table 5).
DISCUSSION
The awareness rate of diabetes in Korea increased from 44.1% in 1998 to 57.4% in 2007, as universal health screening has become the norm and diabetes in Korea has evolved into an increasingly developed form [9]. More emphasis should be placed on the education and management of patients with diabetes due to its chronic nature with various complications. However, in this study, based mainly on a survey, a small number of patients had been exposed to diabetic education, and the rate of exposure to diabetes education at a previous medical institution was low (11.1%). In addition, a small proportion of patients were monitored using SMBG and HbA1c (27.1% and 22.3%, respectively), and some patients who were diagnosed with diabetic complications or recommended to undergo evaluation of complications did not receive proper treatment or testing. Only 38% of patients were aware of the need to be evaluated for diabetic complications, and actual testing was performed in only 11% of patients. A similar investigation showed similar results: 34.9% of enrolled patients had been checking SMBG, 39.4% had exposure to diabetic education, and basic evaluation of diabetes was performed in less than 10% of cases [12]. In another questionnaire survey in Korea, the proportions of patients that replied "yes" to the question, "do you have organized management of diabetes?" in each age group were low: 10% in their 40's, 20% in their 50's, and 23% in their 60's or older [13]. In addition, in terms of patients with controlled diabetes, 57% were attending tertiary hospitals, compared to 37% of patients who attended primary centers [13]. This finding suggests that the diagnosis and management of diabetes in Korea is concentrated in tertiary hospitals, unlike other developed countries, and suggests that primary medical institutions have difficulty in diagnosis, management, and education of DM and diabetic complications. In terms of the prevalence of diabetic complications, one nationwide survey on the current status of glycemic control and complications of diabetic patients visiting tertiary hospitals in Korea in 2006 reported similar or slightly higher prevalence rates of microvascular complications (44.6% in neuropathy, 38.3% in retinopathy, 30.4% in nephropathy) and lower prevalence rates of macrovascular complications (8.7% in CAD, 6.7% in cerebral vascular disease, 3.0% in PAD) compared with the present study [10]. In fact, despite the relatively large proportion of patients with macrovascular (6% to 11%) and microvascular (27% to 32%) complications, which are well-known chronic complications of diabetes, most patients do not receive treatment. This causes a rapid increase in disease burden despite early diagnosis. In this study, 43% of the transferred patients decided to visit higher medical institutions by themselves, and 60.4% did not have letters of medical request from previous medical institutions. In addition, the main reason for visiting a higher medical institution, such as a university hospital, is to control blood glucose or to evaluate complications related to diabetes, which could be accomplished at clinics. This is an example of the poor relationship among medical institutions, which are divided into three different roles in Korea.
Providing quality services to enhance the level of public health is a national goal. An appropriate scale and function of each medical institution is required to reach this goal. However, the Korean healthcare system does not share functions or roles among institutions, and it induces duplication of treatments and direct competition among institutions. That is, the role of the clinic as the keeper of national health care has declined, which causes inefficient use of time and energy as well as an overburden of medical costs. Thus, redefining the role of the medical institution is required to ensure the sustainability of the healthcare system.
This study had limitations in that it was not a case-controlled study but rather a simple survey. Thus, we have a strategy to compare data obtained from a single tertiary hospital with other data obtained from other hospitals among our research groups, but unfortunately, it was not analyzed at this time. However, it was meaningful to investigate the clinical characteristics and medical status of diabetic patients referred to referral hospitals in Gyeongsangnam/Gyeongsangbuk-do and Jeollanam/Jeollabuk-do, although it was not designed well. In addition, we found similar prevalence rates of diabetic complications compared with another study based on a nationwide survey performed only in tertiary hospitals, and similar problems of diabetic management have been described in many previous studies.
Strict treatment of diabetes at an early stage is important to prevent chronic complications. However, when we investigated the clinical characteristics and medical status of diabetic patients, we identified some problems in diabetes management, such as diagnosis, evaluation of complications, education, and treatment before transfer, and we concluded that the relationships among medical institutions must be improved with a redefinition of the roles of medical institutions, particularly for diabetes.
ACKNOWLEDGMENTS
This study was supported by a research grant obtained from the Young-Honam Endocrinology and Metabolism Association (2011). Investigators and study centers included in this analysis. In Joo Kim and Sang Soo Kim (Department of Internal Medicine, Pusan National University Hospital, Pusan National University School of Medicine, Busan); In Kyu Lee (Department of Internal Medicine, Kyungpook National University School of Medicine, Daegu); Tae Hyun Kim (Department of Internal Medicine, Kwangju Christian Hospital, Gwangju); Duk Kyu Kim (Departments of Internal Medicine, Dong-A University College of Medicine, Busan); Seong Pyo Son (Department of Internal Medicine, Bongseng Memorial Hospital, Busan); Young Sil Lee (Department of Internal Medicine, Dongguk University Gyeongju Hospital, Dongguk University College of Medicine, Gyeongju); Young Sik Choi (Department of Internal Medicine, Kosin University College of Medicine, Busan); Tae Sun Park (Department of Internal Medicine, Chonbuk National University Hospital, Chonbuk National University Medical School, Jeonju); Ho Sang Sohn (Department of Internal Medicine, Daegu Catholic University Medical Center, Catholic University of Daegu School of Medicine, Daegu); Young Il Kim (Department of Internal Medicine, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan); Hyoung Woo Lee (Department of Internal Medicine, Yeungnam University Medical Center, Yeungnam University College of Medicine, Daegu); Jong Ryeal Hahm (Department of Internal Medicine, Gyeongsang National University Hospital, Gyeongsang National University School of Medicine, Jinju); Jeong Hyun Park (Department of Internal Medicine, Inje University Busan Paik Hospital, Inje University College of Medicine, Busan); Hye Soon Kim (Department of Internal Medicine, Keimyung University Dongsan Medical Center, Keimyung University School of Medicine, Daegu); Chang Won Lee (Department of Internal Medicine, Busan St. Mary's Medical Center, Busan); Ji Hye Kim (Department of Internal Medicine, Presbyterian Medical Center, Jeonju); Min Young Chung (Department of Internal Medicine, Chonnam National University Medical School, Gwangju); Hak Yeon Bae (Department of Internal Medicine, Chosun University Hospital, Chosun University School of Medicine, Gwangju); Sung Rae Cho (Department of Internal Medicine, Changwon Fatima Hospital, Changwon); Mi Kyung Kim (Department of Internal Medicine, Inje University Haeundae Paik Hospital, Inje University College of Medicine, Busan).
Notes
No potential conflict of interest relevant to this article was reported.