- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 47(3); 2023 > Article
-
Sulwon Lecture 2022Others Opening the Precision Diabetes Care through Digital Healthcare
-
Joonyub Lee
 , Jin Yu
, Jin Yu , Kun-Ho Yoon
, Kun-Ho Yoon
-
Diabetes & Metabolism Journal 2023;47(3):307-314.
DOI: https://doi.org/10.4093/dmj.2022.0386
Published online: March 29, 2023
- 5,011 Views
- 247 Download
Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
-
Corresponding author: Kun‐Ho Yoon
 Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, 222 Banpodaero, Seocho-gu, Seoul 06591, Korea E-mail: yoonk@catholic.ac.kr
Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, 222 Banpodaero, Seocho-gu, Seoul 06591, Korea E-mail: yoonk@catholic.ac.kr
Copyright © 2023 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- The national healthcare systems of every country in the world cannot sustain the rise in healthcare expenditure caused by chronic diseases and their complications. To sustain the national healthcare system, a novel system should be developed to improve the quality of care and minimize healthcare costs. For 20 years, our team developed patient-communicating digital healthcare platforms and proved their efficacy. National scale randomized control trials are underway to systematically measure the efficacy and economic benefits of this digital health care system. Precision medicine aims to maximize effectiveness of disease management by considering individual variability. Digital health technologies enable precision medicine at a reasonable cost that was not available before. The government launched the “National Integrated Bio-big Data Project” which will collect diverse health data from the participants. Individuals will share their health information to physicians or researchers at their will by gateway named “My-Healthway.’ Taken together, now we stand in front of the evolution of medical care, so-called “Precision medicine.” led by various kinds of technologies and a huge amount of health information exchange. We should lead these new trends as pioneers, not as followers, to establish and implement the best care for our patients that can help them to withstand their devastating diseases.
- The Sulwon Award for Scientific Achievement is the Korean Diabetes Association’s highest scientific award and honors an individual who has excellently contributed to the progress in the field of diabetes and metabolism. The Sulwon Award is named after an emeritus professor, Eung Jin Kim, who founded Korean Diabetes Association. Prof. Kun-Ho Yoon received the 14th Sulwon Award at the 35th Spring Congress of Korean Diabetes Association, May 12 to 14 in 2022 at Gyeongju, Korea.
Key figure
- National healthcare expenditures are increasing rapidly worldwide, causing a substantial economic burden to each country. The national healthcare expenditure in South Korea is estimated to reach 137.2 billion U.S. dollar (USD) in 2020. This number accounts for 8.4% of the gross domestic product (GDP), which more than doubled within 20 years (3.9% in 2000) [1]. Chronic diseases and their related complications are major causes of this rapidly increasing healthcare burden [2]. Diabetes is one of the most prevalent chronic diseases that results in various vascular complications (nephropathy, retinopathy, neuropathy, peripheral artery diseases, and cardiovascular diseases) [3]. Diabetes-related complications can be prevented or delayed when diabetes and the associated metabolic parameters are properly managed [4-6]. Frustratingly, only 24.5% of patients with diabetes reach the optimal glycemic target (glycosylated hemoglobin [HbA1c] ≤6.5%), and only 9.7% meet comprehensive metabolic targets (HbA1c ≤6.5%, blood pressure <140/90 mm Hg, low-density lipoprotein <100 mg/dL) [7]. Therefore, developing an efficient and comprehensive diabetes healthcare system is essential for alleviating the national healthcare burden.
- Patients with diabetes have heterogeneous pathophysiology and phenotypes that require life-long individualized management [8-12]. Current guidelines recommend individualized therapeutic options, depending on the concomitant disease, obesity, and socioeconomic status of patients with diabetes [13-15]. However, inter-individual and intra-individual variations in medical information (genome, epigenome, metabolite, protein, and life-log data) remain largely unknown [16]. Current practice is based on the assumption that most patients in each subcategory of diabetes respond similarly to standardized treatment. Therefore, it is important to develop a novel diabetes care system which minimizes healthcare costs and improves the quality of care to secure future national healthcare systems. In this review, we discuss the current evidence and share our perspectives on how digital technologies can fulfill these unmet needs of diabetes care.
INTRODUCTION
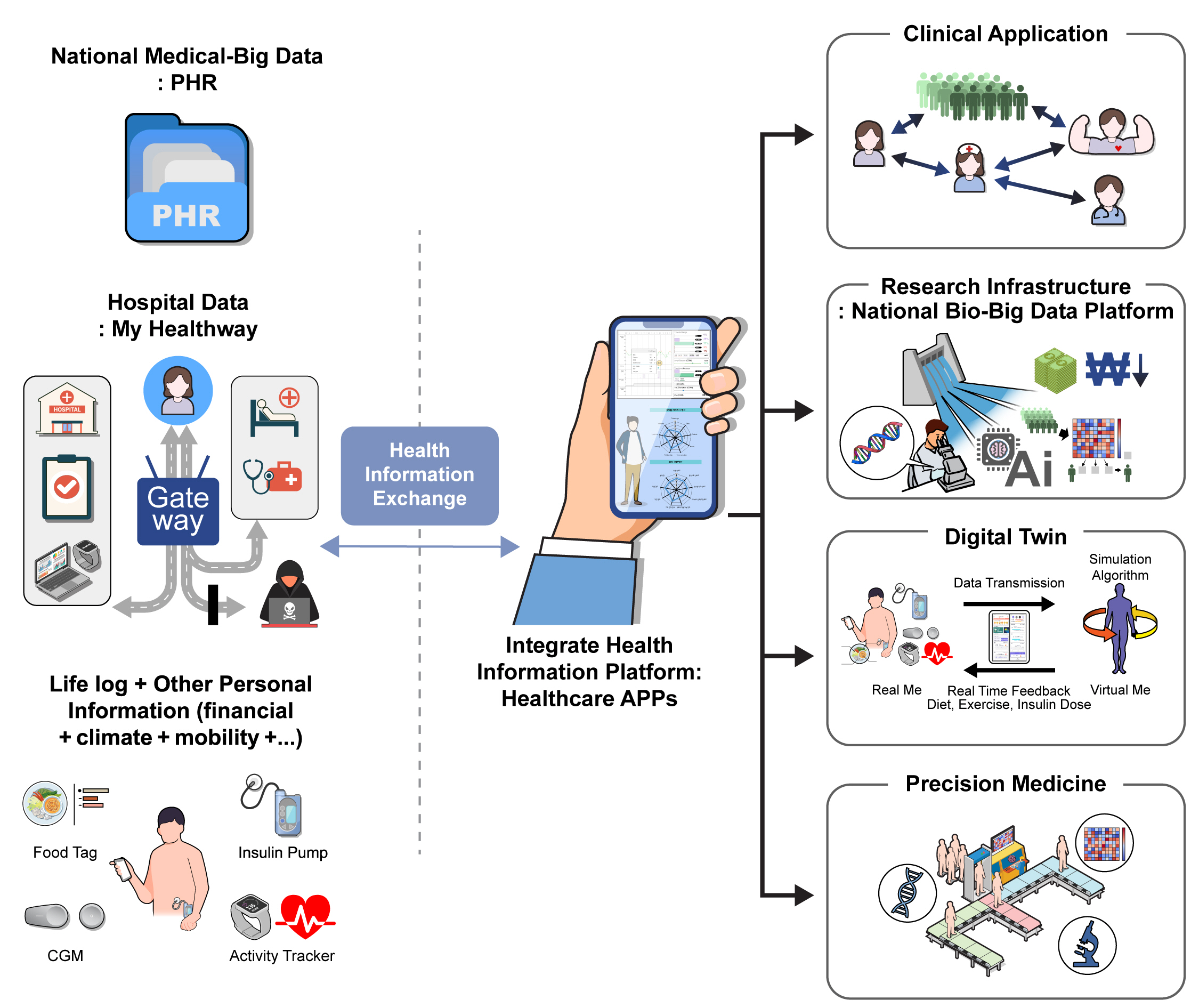
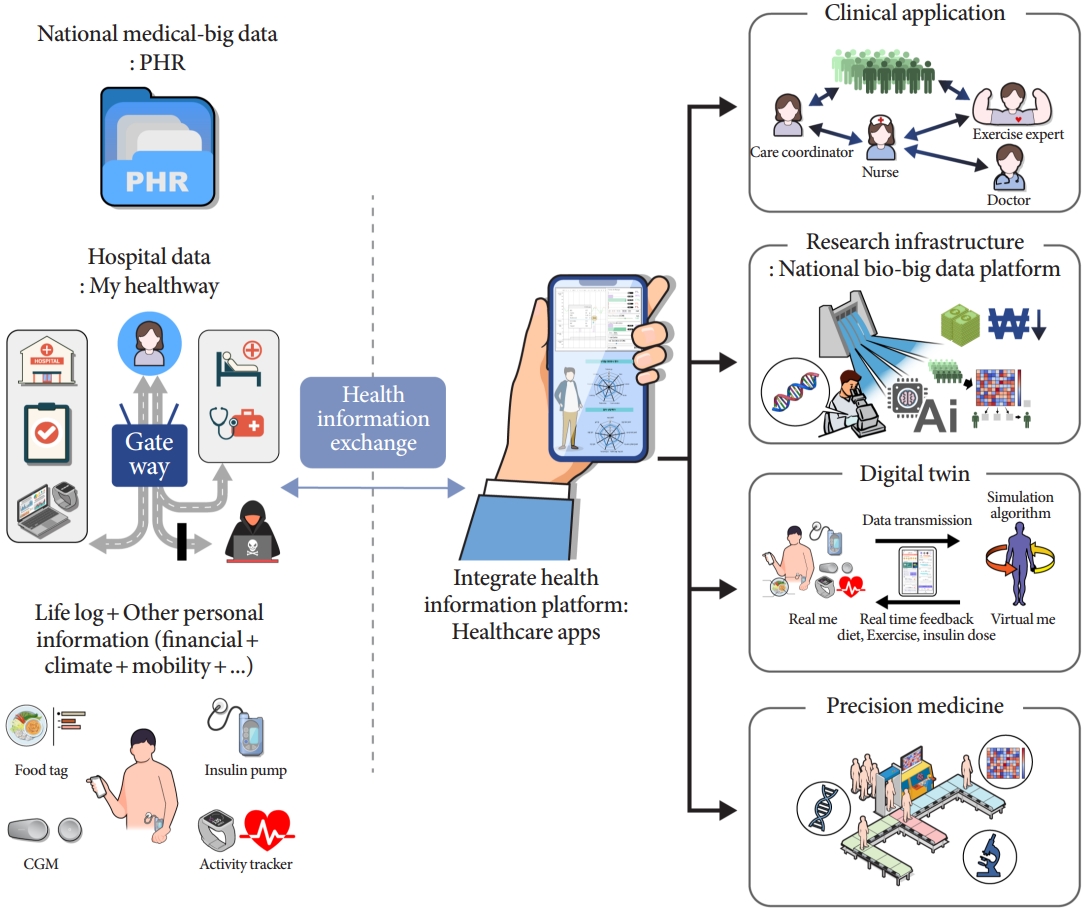
- Digital technology can increase accessibility between patients and healthcare professionals, accelerating the advent of mobile healthcare in diabetes. Previously, we and other groups have demonstrated that digital technology-mediated patient management can improve the outcomes of patients with diabetes. In 2004, when the internet became widely available in Korea, our group demonstrated an Internet-based glucose monitoring (IBGM) system that can improve glycemic outcomes in patients with diabetes [17]. Thus, patients were able to receive feedback from physicians once they uploaded their personal profiles, self-monitored blood glucose levels, medication information, and other diabetes-related questions. After 3 months of follow-up, patients in the IBGM intervention group showed improved HbA1c levels than those in the control group (control vs. intervention HbA1c: 7.62% vs. 6.94%, P<0.001; n=101). The effect of IBGM intervention was still evident even in the long-term (30 months) after the intervention was initiated [18]. This finding was further validated in a large-scale, multicenter clinical trial [19]. In these trial, the frequency of self-blood glucose measurement was similar between the intervention and control groups. Therefore, we speculate the glucose lowering effect of digital communication can be mainly attributed to medical experts’ appropriate response to patients at the right time and constantly encouraging the motivation of patients. For these trials were mainly focused on glucose level, we further explored whether digital healthcare can reduce the incidence of diabetes related complications. By using computer simulation model (CORE diabetes model), we demonstrated that IBGM system can delay the onset and progression of microvascular complications more than a year in patients with diabetes [20]. These findings suggest that digital technology can provide novel opportunity for future healthcare. Since our web-based study, smartphones are being widely used, and mobile app-based communication provides better accessibility to remote health care. Following the results of Internet-based interventions, smartphone-based health care has been shown to be effective in the care of patients with diabetes [21-23]. We developed a mobile app-based patient-physician communication gateway named “iCareD,” in which patients can upload their daily life-log variables (glucose, blood pressure, and activity), and medical experts can provide feedback. Patient-physician communication using “iCareD” system improved glycemic outcomes in patients with type 2 diabetes mellitus at 12 weeks of intervention [23]. Encouraged by these previous results, we participated in a national project called the “Primary health care chronic diseases management pilot program.” “Primary health care chronic diseases management pilot program” was supervised and funded by Ministry of Health and Welfare in Korea with 60 million USD budget. A total of 460,000 patients newly diagnosed with diabetes or hypertension from 3,781 primary care clinics were enrolled in this study. Next, physicians performed comprehensive assessments and set up care plans and goals for the patients. Then, patients received comprehensive disease-related lifestyle education, tele-monitoring, and feedback (smart coaching) conducted by healthcare professionals (dietitians, exercise coaches, and nurses). Physicians then reassess the status twice a year and reset the care plan and goal for each patient [24]. The preliminary outcome of this “pilot project” showed that the intervention could improve glycemic outcomes in patients with diabetes. After 3 months of intervention, the difference in HbA1c compared with baseline was significantly lower in the intervention group control (0.27% vs. intervention 0.63%, P<0.05) [25]. Encouraged by this result, a community-based randomized controlled trial is underway to accurately evaluate the efficacy of this new chronic disease primary healthcare platform. Similarly, a pilot digital healthcare program on Medicaid patients were launched during the coronavirus disease 2019 (COVID-19) pandemic in the United States. After 1 year of participating this pilot digital healthcare program, more than half of patients with poorly controlled diabetes improved their glycemic outcome [26]. To establish a mobile app-based primary diabetes care system and evaluate its efficacy, we organized a national scale communitybased randomized control trial in which iCareD is merged into the “Primary health care chronic diseases management program.” The trial was named the “Advanced primary health care chronic diseases management program,” and iCareD was merged with the electronic medical record (EMR) system of the participating primary care clinic. When patients are enrolled, they receive comprehensive assessment and education and sign up to engage in iCareD. Based on the initial assessment, the physicians established individual care goals and plans for each patient. Participants upload individual life log data on iCareD, and physicians provide smart monitoring and feedback based on the uploaded data. Patients can consult physicians and take opinion of medical experts (dietitians, exercise experts, and nurses) when necessary. Subsequently, physicians re-analyze patients during their routine clinic visits and can reset their personal goals. This “Advanced primary health care chronic diseases management program” is an ongoing trial and is planned for 6-month follow-up to evaluate their efficacy (Fig. 1). In 2022, President Yoon Suk-yeol announced the new government’s national goal after he was elected the 20th president of the Republic of Korea. In this announcement, “the expansion of health services based on innovative ICT technology” was included as an important future national goal [27]. The government will increase its investment in developing an Information and communication technology (ICT)-based primary care clinic-centered chronic disease care system to strengthen the management of patients with chronic diseases. In addition, the institutionalization of primary care clinic-based mobile healthcare for patients with chronic diseases will be accelerated to provide constant and proper management to patients in medically vulnerable areas. In summary, ICT increases communication accessibility between patients and healthcare providers, accelerating the advent of mobile healthcare. ICT-based diabetes care has been shown to be effective and cost-efficient. With national support, ICT-based primary care services for diabetes will largely expand.
DIGITAL TECHNOLOGY AND MOBILE HEALTHCARE IN PATIENTS WITH DIABETES
- Digital technology provides unprecedented quantity and quality of patient-generated health data (PGHD), accelerating the advent of precision medicine in diabetes care. Patients with diabetes share heterogeneous pathophysiology and phenotypes that require life-long individualized management [8-12]. In 2015, former U.S. President Barack Obama announced the launch of the Precision Medicine Initiative [28]. Since then, large-scale investments and actions have been undertaken to enable precision medicine. Precision medicine aims to predict the individual risk of developing various diseases and provide the most optimal therapy for those who already have diseases [29-31]. To achieve this goal, it is important to understand how environmental and genetic factors and their interactions contribute to the development of diseases and understand the variation in individual responses to medical treatments [30,32]. Each nation has organized large-scale cohorts to collect and analyze medical information and biological samples. National Institutes of Health in the U.S. initiated enrollment of a national cohort (“All of the US”) in 2018 to collect medical information (electronic health record), PGHD, and biological samples (DNA, metabolite, proteome). The cohort aims to engage >1 million participants, and approximately 35% of individuals were enrolled 2 years after the launch of the program [33]. “The Million Veteran Program” directed by the U.S. Department of Veterans Affairs, is also under progress and has already enrolled 0.9 million participants [34]. The U.K. biobank engaged 0.5 million participants, and further plans to pursue their project until the number of participants reaches 5 million [35]. Finland organized “FinnGen” project in 2017 to enroll 0.5 million participants [36]. China has also organized a national precision medicine project aimed at enrolling 1 million participants [37]. One of the main hurdles in collecting data for largescale national cohorts is the integration of EMRs. EMRs were initially developed to efficiently share health information between physicians, patients, insurance companies, and researchers. However, integrating high-throughput EMR data remains challenging because of the diverse number of EMR platforms, the un-unified use of medical terminologies, and the lack of important patient information [38]. Recent advances in artificial intelligence (AI) technologies have enabled us to deal with missing values and systematically analyze high volumes of EMR data [39-41]. In addition, the ontological classification of medical records provides a link between heterogeneously described medical records and biologically meaningful phenotypes [42]. Data security and storage are other important issues in integrating EMR data and adopting them in precision medicine [43]. I have participated in “The digital healthcare special committee belonging to the president committee fourth industrial revolution” in South Korea and organized the “My-Healthway” system. “My-Healthway” enables each individual to store their personal health record (PHR) in a personal cloud or mobile smartphone (Fig. 1) [44]. As a result, each individual can take the initiative for integrating and managing their own medical data and transferring them to others, such as hospitals, government, insurance companies, and researchers, when necessary. The first service of “MyHealthway” was started in January 2021 by the Ministry of Health and Welfare. The national healthcare big data generated by Korea Disease Control and Prevention Agency, Health Insurance Review & Assessment Service, and National Health Insurance Service is already provided through “My-Healthway” mobile application. Seoul St. Mary’s Hospital and Pusan National University Hospital have already finished a national pilot project to adopt “My-Healthway” and shared PHRs between primary care clinics and general hospitals. The use of “My-Healthway” will be expanded to general hospitals and private clinics within 2 to 3 years.
- The South Korean government has recently organized the Korea Precision Medicine Initiative (KPMI), in which I have the privilege to participate. The KPMI is planning to establish “a national integrative bio data dam” for engaging 1 million participants and collecting their clinical, genomic, proteome, microbiome, and lifelog data (Fig. 1). The “national integrative bio data dam” will provide valuable information to researchers and physicians for planning individualized therapy or life style guidance and disease prediction/or early detection [45]. Of the various sources of data—exogenous, including behavioral, environmental, and socio-economic status, genomic, and clinical—exogenous data account for approximately 60% of patient health outcomes [46]. Digital sensor devices can provide valuable patient-generated exogenous data, important for understanding an individual’s health status [47]. Therefore, mobile sensor devices are expected to be applied to many national precision medicine cohorts. Furthermore, digital health devices, such as continuous glucose monitoring systems, activity trackers, calorie calculators, and insulin pumps, can provide essential glucose-affecting life-log data to physicians and researchers [48-50]. These digital health devices that generate PGHD will aid physicians in categorizing the heterogeneous phenotypes of patients with diabetes and ultimately enable physicians to provide individualized therapy. We speculate that these advances in technologies and systems will substantially aid in accelerating the advent of precision medicine for diabetes.
DIGITAL TECHNOLOGY AND PRECISION MEDICINE IN PATIENTS WITH DIABETES
- Digital technologies have long influenced the field of diabetes care, accelerating the era of mobile healthcare and precision medicine. Importantly, mobile healthcare and personalized care will not be mutually exclusive in the future diabetes care. The personal ownership of their PHR (“My-Healthway”) will enable distal care providers to understand individuals’ deep phenotyped information. In particular, digital sensor technologies can provide real-time life-log information to medical experts. When combined with a patient-physician communication platform, medical experts can provide individualized realtime feedback to patients. To cope with these changes, our team has recently developed a more evolved diabetes care platform to provide “AI-driven personalized mobile healthcare” to patients with diabetes using digital twin (DT) technology (Fig. 1). A DT is a technology that creates virtual twins with the same characteristics as real objects [51,52]. Simulations can be performed on this virtual object to predict the outcome and provide optimal feedback to the real objects. To apply this technology in diabetes care, we collected continuous life-log variables with digital sensors (continuous glucose monitoring, insulin pump, food tag, and activity tracker) from patients with type 1 diabetes mellitus. We aimed to produce virtual twins from each patient and provide guidance on optimal insulin dosage or lifestyle changes based on AI algorithms. However, this study is still preliminary, and further studies should be conducted. In addition, regulatory problems remain a major hurdle for applying these new diabetes care platforms. Nevertheless, digital technologies have been and will transform future diabetes care and will eventually “minimize healthcare costs” and “improve the quality of care” in patients with diabetes. Therefore, we should not hesitate to implement these technologies that can revolutionize diabetes care.
FUTURE PERSPECTIVES AND CONCLUSION
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
FUNDING
This work was supported by the Institute of Information & Communications Technology Planning & Evaluation (IITP) grant funded by the Korean government (MSIT) (No. 2022-0-00965, Development of diabetes patients’ healthcare digital twin technology based on continuous lifelog variables) and Patient-Centered Clinical Research Coordinating Center (PACEN) funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC19C0341).
NOTES
-
Acknowledgements
- None
- 1. Statista: Health spending as percent of GDP in South Korea 2000-2020. Available from: https://www.statista.com/statistics/647320/health-spending-south-korea/#statisticContainer (cited 2023 Mar 3).
- 2. Centers for Medicare & Medicaid Services: National health expenditure data, historical 2021. Available from: https://www.cms.gov/Research-Statistics-Data-and-Systems/StatisticsTrends-and-Reports/NationalHealthExpendData (cited 2023 Mar 3).
- 3. Zhang P, Zhang X, Brown J, Vistisen D, Sicree R, Shaw J, et al. Global healthcare expenditure on diabetes for 2010 and 2030. Diabetes Res Clin Pract 2010;87:293-301.ArticlePubMed
- 4. Rawshani A, Rawshani A, Franzen S, Sattar N, Eliasson B, Svensson AM, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 2018;379:633-44.ArticlePubMed
- 5. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837-53.ArticlePubMed
- 6. ADVANCE Collaborative Group; Patel A, MacMahon S, Chalmers J, Neal B, Billot L, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 2008;358:2560-72.ArticlePubMed
- 7. Bae JH, Han KD, Ko SH, Yang YS, Choi JH, Choi KM, et al. Diabetes fact sheet in Korea 2021. Diabetes Metab J 2022;46:417-26.ArticlePubMedPMCPDF
- 8. Ahlqvist E, Storm P, Karajamaki A, Martinell M, Dorkhan M, Carlsson A, et al. Novel subgroups of adult-onset diabetes and their association with outcomes: a data-driven cluster analysis of six variables. Lancet Diabetes Endocrinol 2018;6:361-9.ArticlePubMed
- 9. Chung WK, Erion K, Florez JC, Hattersley AT, Hivert MF, Lee CG, et al. Precision medicine in diabetes: a consensus report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 2020;63:1671-93.ArticlePubMedPMCPDF
- 10. Florez JC, Pearson ER. A roadmap to achieve pharmacological precision medicine in diabetes. Diabetologia 2022;65:1830-8.ArticlePubMedPMCPDF
- 11. McCarthy MI. Painting a new picture of personalised medicine for diabetes. Diabetologia 2017;60:793-9.ArticlePubMedPMCPDF
- 12. Nair ATN, Wesolowska-Andersen A, Brorsson C, Rajendrakumar AL, Hapca S, Gan S, et al. Heterogeneity in phenotype, disease progression and drug response in type 2 diabetes. Nat Med 2022;28:982-8.ArticlePubMedPDF
- 13. Hur KY, Moon MK, Park JS, Kim SK, Lee SH, Yun JS, et al. 2021 Clinical practice guidelines for diabetes mellitus of the Korean Diabetes Association. Diabetes Metab J 2021;45:461-81.ArticlePubMedPMCPDF
- 14. American Diabetes Association. Introduction: standards of medical care in diabetes-2022. Diabetes Care 2022;45(Suppl 1):S1-2.ArticlePubMedPDF
- 15. Davies MJ, Aroda VR, Collins BS, Gabbay RA, Green J, Maruthur NM, et al. Management of hyperglycemia in type 2 diabetes, 2022: a consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care 2022;45:2753-86.ArticlePubMedPMCPDF
- 16. Gloyn AL, Drucker DJ. Precision medicine in the management of type 2 diabetes. Lancet Diabetes Endocrinol 2018;6:891-900.ArticlePubMed
- 17. Kwon HS, Cho JH, Kim HS, Song BR, Ko SH, Lee JM, et al. Establishment of blood glucose monitoring system using the internet. Diabetes Care 2004;27:478-83.ArticlePubMedPDF
- 18. Cho JH, Chang SA, Kwon HS, Choi YH, Ko SH, Moon SD, et al. Long-term effect of the Internet-based glucose monitoring system on HbA1c reduction and glucose stability: a 30-month follow-up study for diabetes management with a ubiquitous medical care system. Diabetes Care 2006;29:2625-31.PubMed
- 19. Cho JH, Kim HS, Yoo SH, Jung CH, Lee WJ, Park CY, et al. An Internet-based health gateway device for interactive communication and automatic data uploading: clinical efficacy for type 2 diabetes in a multi-centre trial. J Telemed Telecare 2017;23:595-604.ArticlePubMedPDF
- 20. Cho JH, Lee JH, Oh JA, Kang MJ, Choi YH, Kwon HS, et al. Complication reducing effect of the information technologybased diabetes management system on subjects with type 2 diabetes. J Diabetes Sci Technol 2008;2:76-81.ArticlePubMedPMCPDF
- 21. Zhang L, He X, Shen Y, Yu H, Pan J, Zhu W, et al. Effectiveness of smartphone app-based interactive management on glycemic control in Chinese patients with poorly controlled diabetes: randomized controlled trial. J Med Internet Res 2019;21:e15401.ArticlePubMedPMC
- 22. Yang Y, Lee EY, Kim HS, Lee SH, Yoon KH, Cho JH. Effect of a mobile phone-based glucose-monitoring and feedback system for type 2 diabetes management in multiple primary care clinic settings: cluster randomized controlled trial. JMIR Mhealth Uhealth 2020;8:e16266.ArticlePubMedPMC
- 23. Lee EY, Cha SA, Yun JS, Lim SY, Lee JH, Ahn YB, et al. Efficacy of personalized diabetes self-care using an electronic medical record-integrated mobile app in patients with type 2 diabetes: 6-month randomized controlled trial. J Med Internet Res 2022;24:e37430.ArticlePubMedPMC
- 24. Ministry of Health and Welfare; Korea Health Promotion Institute. Primary health care chronic diseases management pilot program guide book. 3rd ed. Seoul: KHEPI; 2021.
- 25. Ministry of Health and Welfare, Division of Healthcare and Medicine Policy: Realization of public health care through telemedicine, satisfaction 83-88%, and clinical effectiveness confirmed. Available from: http://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=329739 (cited 2023 Mar 6).
- 26. Olsen E: Q&A: Ensuring digital health programs work for the Medicaid population. Available from: https://www.mobihealthnews.com/news/qa-ensuring-digital-health-programs-workmedicaid-population (cited 2023 Mar 6).
- 27. Office of the President: One hundred and twenty national tasks of President Yoon Suk-yeol. Available from: https://www.president.go.kr/affairs/gov_project (cited 2023 Mar 6).
- 28. The White House President Barack Obama: The Precision Medicine Initiative. Available from: https://obamawhitehouse.archives.gov/precision-medicine (cited 2023 Mar 6).
- 29. National Research Council (US) Committee on A Framework for Developing a New Taxonomy of Disease. Toward precision medicine: building a knowledge network for biomedical research and a new taxonomy of disease. Washington DC: National Academies Press; 2011.
- 30. Fradkin JE, Hanlon MC, Rodgers GP. NIH Precision Medicine Initiative: implications for diabetes research. Diabetes Care 2016;39:1080-4.ArticlePubMedPMCPDF
- 31. Collins FS, Varmus H. A new initiative on precision medicine. N Engl J Med 2015;372:793-5.ArticlePubMedPMC
- 32. Parikh RB, Schwartz JS, Navathe AS. Beyond genes and molecules: a precision delivery initiative for precision medicine. N Engl J Med 2017;376:1609-12.ArticlePubMed
- 33. Kent J: “All of us” opens precision medicine data platform for beta testing. Available from: https://healthitanalytics.com/news/all-of-us-opens-precision-medicine-data-platform-forbeta-testing (cited 2023 Mar 6).
- 34. Gaziano JM, Concato J, Brophy M, Fiore L, Pyarajan S, Breeling J, et al. Million Veteran Program: a mega-biobank to study genetic influences on health and disease. J Clin Epidemiol 2016;70:214-23.ArticlePubMed
- 35. UK Biobank data on 500,000 people paves way to precision medicine. Nature 2018;562:163-4.ArticlePDF
- 36. University of Helsinki: FinnGen, a global research project focusing on genome data of 500,000 Finns, launched. Available from: https://www.eurekalert.org/news-releases/850739 (cited 2023 Mar 6).
- 37. Ye Y. Unleashing the power of big data to guide precision medicine in China. Nature 2022;606:S49-51.ArticlePubMedPDF
- 38. Reisman M. EHRs: the challenge of making electronic data usable and interoperable. P T 2017;42:572-5.PubMedPMC
- 39. Li J, Yan XS, Chaudhary D, Avula V, Mudiganti S, Husby H, et al. Imputation of missing values for electronic health record laboratory data. NPJ Digit Med 2021;4:147.ArticlePubMedPMCPDF
- 40. Wang H, Tang J, Wu M, Wang X, Zhang T. Application of machine learning missing data imputation techniques in clinical decision making: taking the discharge assessment of patients with spontaneous supratentorial intracerebral hemorrhage as an example. BMC Med Inform Decis Mak 2022;22:13.ArticlePubMedPMCPDF
- 41. Chi EA, Chi G, Tsui CT, Jiang Y, Jarr K, Kulkarni CV, et al. Development and validation of an artificial intelligence system to optimize clinician review of patient records. JAMA Netw Open 2021;4:e2117391.ArticlePubMedPMC
- 42. Haendel MA, Chute CG, Robinson PN. Classification, ontology, and precision medicine. N Engl J Med 2018;379:1452-62.ArticlePubMedPMC
- 43. Thapa C, Camtepe S. Precision health data: requirements, challenges and existing techniques for data security and privacy. Comput Biol Med 2021;129:104130.ArticlePubMed
- 44. The digital healthcare special committee belonging to the president committee fourth industrial revolution: Initiating the establishment of health information highway. Available from: https://www.mohw.go.kr/react/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&page=1&CONT_SEQ=363763 (cited 2023 Mar 18).
- 45. Ministry of Health and Welfare, Ministry of Science and ICT, Ministry of Trade, Industry and Energy, Korea Disease Control and Prevention Agency: National integrated bio big data construction project. Available from: https://bighug.kdca.go.kr/bigdata/ga0010.jsp (cited 2023 Mar 6).
- 46. McGovern L, Miller G, Hughes-Cromwick P. Health Policy Brief: the relative contribution of multiple determinants to health outcomes. Health Aff 2014 Aug 21 https://doi.org/10.1377/hpb20140821.404487.Article
- 47. Getting real with wearable data. Nat Biotechnol 2019;37:331.ArticlePubMedPDF
- 48. Rodbard D. Continuous glucose monitoring: a review of successes, challenges, and opportunities. Diabetes Technol Ther 2016;18(Suppl 2):S3-13.ArticlePubMedPMC
- 49. Berget C, Messer LH, Forlenza GP. A clinical overview of insulin pump therapy for the management of diabetes: past, present, and future of intensive therapy. Diabetes Spectr 2019;32:194-204.ArticlePubMedPMCPDF
- 50. Hodgson W, Kirk A, Lennon M, Paxton G. Exploring the use of fitbit consumer activity trackers to support active lifestyles in adults with type 2 diabetes: a mixed-methods study. Int J Environ Res Public Health 2021;18:11598.ArticlePubMedPMC
- 51. Fuller A, Fan Z, Day C, Barlow C. Digital twin: enabling technologies, challenges and open research. IEEE Access 2020;8:108952-71.Article
- 52. Coorey G, Figtree GA, Fletcher DF, Snelson VJ, Vernon ST, Winlaw D, et al. The health digital twin to tackle cardiovascular disease: a review of an emerging interdisciplinary field. NPJ Digit Med 2022;5:126.ArticlePubMedPMCPDF
REFERENCES
Figure & Data
References
Citations


 KDA
KDA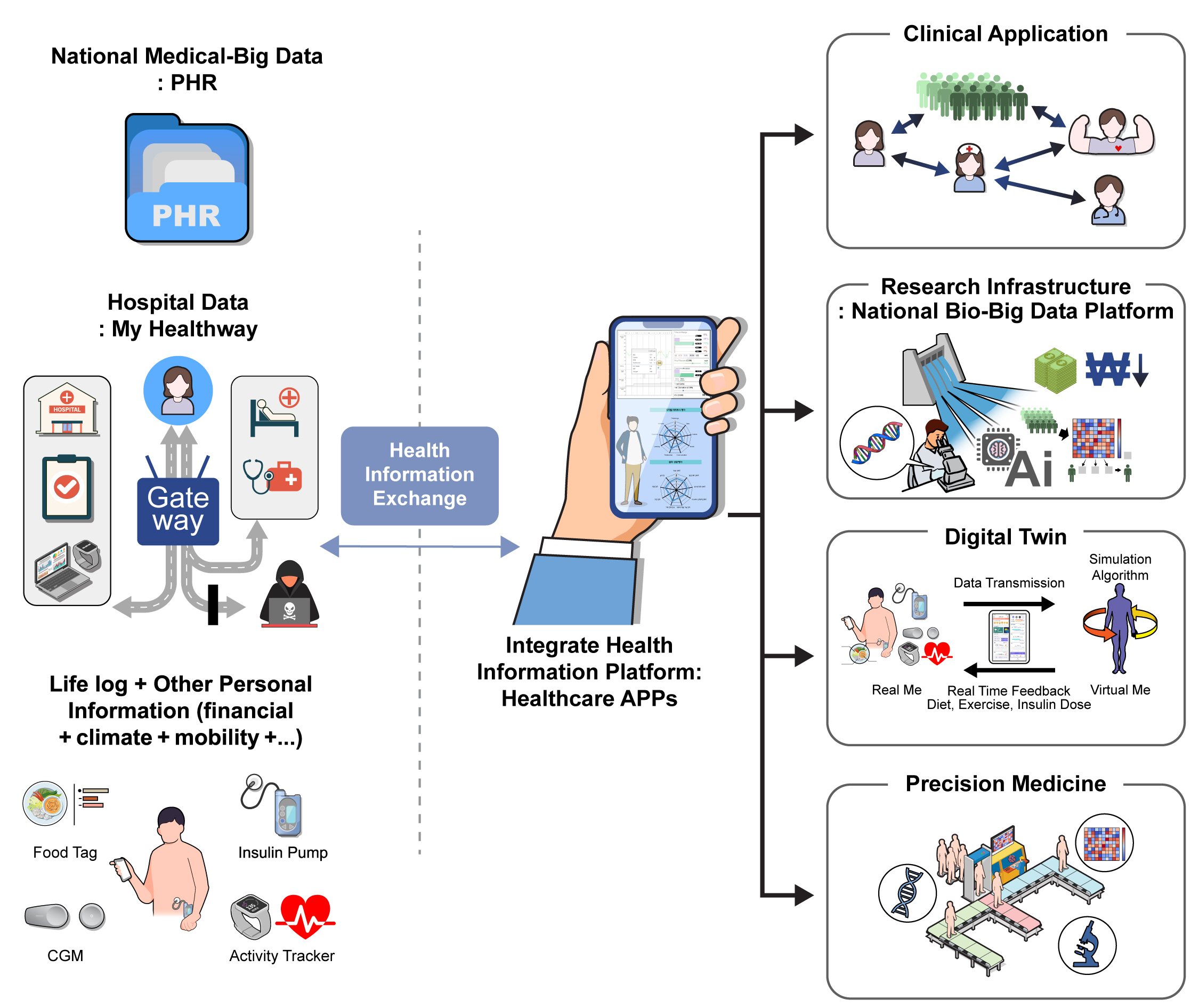
 PubReader
PubReader ePub Link
ePub Link Cite
Cite