- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 45(6); 2021 > Article
-
Brief ReportMetabolic Risk/Epidemiology Short-Term Effects of the Internet-Based Korea Diabetes Prevention Study: 6-Month Results of a Community-Based Randomized Controlled Trial
-
Jin-Hee Lee1
 , Sun-Young Lim1, Seon-Ah Cha2, Chan-Jung Han1, Ah Reum Jung3, Kook-Rye Kim2, Kun-Ho Yoon4, Seung-Hyun Ko2
, Sun-Young Lim1, Seon-Ah Cha2, Chan-Jung Han1, Ah Reum Jung3, Kook-Rye Kim2, Kun-Ho Yoon4, Seung-Hyun Ko2
-
Diabetes & Metabolism Journal 2021;45(6):960-965.
DOI: https://doi.org/10.4093/dmj.2020.0225
Published online: March 17, 2021
1Catholic Institute of Smart Healthcare Center, Institute of Biomedical Industry, The Catholic University of Korea, Seoul, Korea
2Division of Endocrinology and Metabolism, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, Suwon, Korea
3College of Physical Education, Kookmin University, Seoul, Korea
4Division of Endocrinology and Metabolism, Department of Internal Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
-
Corresponding author: Seung-Hyun Ko
 Division of Endocrinology and Metabolism, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, 93 Jungbu-daero, Paldal-gu, Suwon 16247, Korea E-mail: kosh@catholic.ac.kr
Division of Endocrinology and Metabolism, Department of Internal Medicine, St. Vincent’s Hospital, College of Medicine, The Catholic University of Korea, 93 Jungbu-daero, Paldal-gu, Suwon 16247, Korea E-mail: kosh@catholic.ac.kr
Copyright © 2021 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
- The aims of this study were to determine the short-term effectiveness of an internet-based lifestyle modification (LSM) program in preventing the onset of type 2 diabetes mellitus (T2DM) in prediabetes patients in community settings. A total of 415 subjects who were diagnosed with prediabetes were randomly assigned to the LSM and standard management (SM) groups. After the 6-month intervention, the LSM group had a statistically significant reduction in body weight, body mass index compared to the SM group participants. In the LSM group, blood glucose levels were significantly decreased after intervention and the clinical improvement effect was evident in the group that achieved the target weight loss of 5% or more of the initial weight for 6 months. Internet-based 6-month-intensive LSM programs conducted by public health center personnel are an effective way to provide lifestyle intervention programs and encourage maintenance of healthy behaviors in subjects with a high risk of T2DM in community settings.
- Diabetes is a serious health problem worldwide and continues to increase [1,2]. Several randomized clinical trials (RCTs) have reported that the intensive lifestyle intervention (LSI) can significantly reduce the incidence of diabetes in prediabetes [3-5]. In recent decades, internet-based weight management and LSI programs that can increase the accessibility and effectiveness of healthcare have been developed, and several clinical trials have been conducted to evaluate the effects of weight loss on diabetes onset [6-9]. Unfortunately, there were no RCTs evaluating the effectiveness of diabetes prevention in Korea. To establish evidence for this, the national R&D project for the hospital-based [10] and community-based Korean Diabetes Prevention Study (KDPS) [11] has been in progress since 2016. The aim of this paper was to determine the short-term effectiveness of an internet-based lifestyle modification (LSM) program in the community-based Korean Diabetes Prevention Study (C-KDPS).
INTRODUCTION
- The study design and protocol were described in detail in a preceding paper [11]. This study received ethical approval from the Institutional Review Board of St. Vincent’s (No. VC16MISI0003) and Seoul St. Mary’s Hospital (No. KC16EISI0234), the Catholic University of Korea. All of the participants provided written consent for participation.
- Participants
- Total 415 subjects were randomly assigned to the LSM and the standard management (SM) groups using a stratified blocked randomization strategy [11]. Six months after the core program, the subjects who completed the first follow-up numbered 144 in the LSM group and 142 in the SM group.
- Measurements
- We calculated body mass index (BMI) from body weight and height, which were measured by standard methods. Blood sampling for biochemical assays was drawn in the morning after a 10- to 12-hour overnight fast, and all subjects underwent a 75-g oral glucose tolerance test with glycosylated hemoglobin (HbA1c) level measurement. All laboratory parameters were evaluated in the central laboratory (Seegene Medical Foundation, Seoul, Korea).
- Statistical analysis
- We analyzed by intention-to-treat (ITT) as recommended in the consolidated standards of reporting trials (CONSORT) statement [12], and the baseline observation carried forward (BOCF) [13] method was used for the values of subjects who were not followed up. To compare the change within groups, we used the Wilcoxon signed rank test. Six-month changes in the outcomes compared between two groups using a repeated measures analysis of covariance (ANCOVA). In the LSM group, an analysis was also conducted to determine whether the clinical outcomes differed depending on whether the weight loss goal set at the start of the study was achieved. Statistical analyses were performed using SAS version 9.3 (SAS Institute Inc., Cary, NC, USA).
METHODS
- Changes in body composition and blood glucose levels
- Baseline characteristics did not differ significantly between the LSM and SM groups. The mean age of the two groups at randomization was 52.6±7.5 and 53.5±7.4 years in the LSM and SM groups, respectively, with female participation rates of 55.6% and 52.4%, respectively.
- After the 6-month intervention, LSM group participants had a statistically significant reduction in body weight and BMI compared to SM group participants: weight loss was –1.6 kg in the LSM group versus –0.4 kg in the SM group (P<0.001), the change in BMI was –0.6 kg/m2 in the LSM group versus –0.1 kg/m2 in the SM group (P<0.001). Although there was no difference between groups, fasting plasma glucose (FPG) and 2-hour plasma glucose (PG) showed statistically significant decreases after the intervention compared to before the intervention in the LSM group (Table 1).
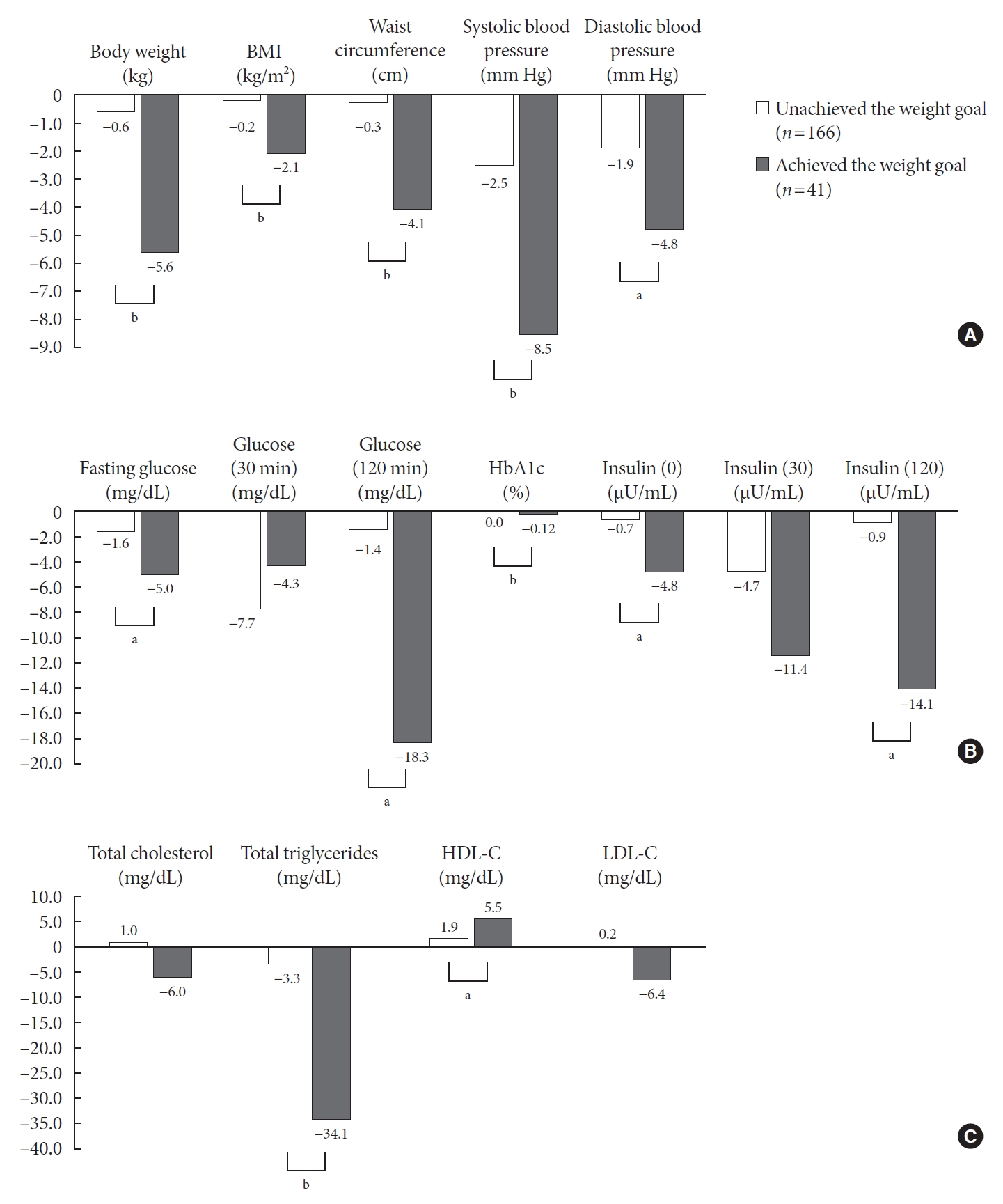
- Differences in clinical outcomes with or without the archiving of the weight loss goals after 6 months in LSM
- One of the major goals of the C-KDPS is a minimum of 5% loss of initial body weight in 6 months and maintenance of this weight loss. Therefore, we analyzed the differences in clinical outcomes with or without achievement of the weight loss goals after 6 months among 207 patients in the LSM group (Fig. 1). After 6 months, 41 (19.8%) of 207 people achieved their weight loss goals, and 166 subjects (80.2%) did not. The positive improvement in anthropometric measures was greater in the group that achieved the weight loss goal. The changes in blood glucose (FPG: –5.0 mg/dL vs. –1.6 mg/dL, P=0.029; 2-hr PG: –18.3 mg/dL vs. –1.4 mg/dL, P=0.001; HbA1c: –0.12 vs. 0.00, P<0.001) were significantly lowed in the group that achieved the weight goal after 6 months.
RESULTS
- In this study, we found that the application of an Internet-based Diabetes Prevention program (DPP) helped to improve clinical markers related to diabetes onset, such as FPG and homeostatic model assessment for insulin resistance (HOMAIR), in prediabetic subjects. As a result of comparing the effects according to whether the LSM group achieved the target weight, the clinical improvement was greater in the group achieving the target weight.
- Of several studies on the short-term effect of a technology-driven DPP [14-16], only one RCT reported changes in FPG and HbA1c [15]. In Block’s study (mean age 55 years, mean BMI 31.1 kg/m2) [15], diabetes prevention and weight loss with a fully automated behavioral intervention for subjects with prediabetes yielded mean changes in FPG of –7.36 mg/dL in the intervention groups compared with –2.19 mg/dL in the control groups at 6 months (P<0.001). Compared with the Block’s study, our results showed a milder reduction in both FPG and HbA1c in the LSM group. The reason for this is because the FPG of our study was approximately 100 mg/dL at baseline, which was 10 mg/dL lower than that in Block’s study. The baseline FPG among participants was similar to that of subjects of the same age, as reported by the Korea National Health and Nutrition Examination Survey [17]. Our participants had prediabetes, but subjects with a very low risk of developing diabetes.
- Previous technology-driven diabetes prevention studies [15,18,19] reported weight loss in the intervention group, ranging from –2.3 [19] to –6.7 kg [18], over a period of 3 to 6 months. These studies were conducted in prediabetic subjects with BMIs ranging from 31.1 to 38.7 kg/m2 in Western countries. In our study, subjects with a mean BMI of 26.3 kg/m2 were included in the study and losing more than 5% of their initial body weight during the 6 months of the study was recommended. The weight loss after 6 months showed a significant difference between two groups (P<0.001), but the degree of weight loss was less than that in previous studies. It was found that in the intervention group, the weight loss target achievement rate was approximately 20% for 6 months, and 2-hour PG, HbA1c, fasting insulin, and HOMA-IR were significantly improved in the group that archived the target weight compared to the group that did not achieve the target weight. Therefore, this result supports the hypothesis that there is a link between weight and risk factors for diabetes and cardiovascular disease [20].
- The advantage of our research is that it is a well-designed RCT conducted in the community. In addition, the web system was used to effectively apply the DPP to high-risk people with diabetes, and public health manpower is in the people who manage the subjects. These findings could provide an important basis for the development of a model that can effectively disseminate diabetes information to the community in the future.
- The limitations of this study are as follows. First, our study was short-term, so it could not assess effectiveness over the long-term, but we will report on the long-term effects in future studies. Second, the 6-month follow-up rate of subjects enrolled in the study was approximately 70%, slightly lower than the originally planned 75%. Although not presented in the study results, the analysis results showed that there was no characteristic difference depending on whether follow-up was performed in either the LSM group or the SM group, so we think the influence of selection bias will be insignificant. In addition, ITT analysis was conducted, and BOCF [13] was used for the values of subjects who were not followed up. This method is suggested by regulatory agencies when evaluating clinical trials because it seems to be more conservative.
- In conclusion, the present study showed the short-term effectiveness of an internet-based Korean DPP in communities. Future studies will analyze the primary outcome of this study to investigate the effectiveness for prevention of diabetes in prediabetes subjects, and it will serve as a basis for suggesting strategies to effectively prevent diabetes in the community setting.
DISCUSSION
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conception or design: J.H.L., K.H.Y., S.H.K.
Acquisition, analysis, or interpretation of data: J.H.L., S.Y.L., S.A.C., C.J.H., A.R.J., K.R.K., S.H.K.
Drafting the work or revising: J.H.L., K.H.Y., S.H.K.
Final approval of the manuscript: J.H.L., S.Y.L., S.A.C., C.J.H., A.R.J., K.R.K., K.H.Y., S.H.K.
-
FUNDING
This research was supported by a grant of the Korean Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HC15-C3364).
NOTES
-
Acknowledgements
- The research team would like to thank the Korean Diabetes Association, and two healthcare centers of Chungju city and Paldal-Gu, Suwon city.
| Variable |
LSM (n=207) |
SM (n=208) |
P valueb | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | Baseline | 6 Months | Mean change | P valuea | No. | Baseline | 6 Months | Mean change | P valuea | ||
| Body weight, kg | 207 | 71.1±10.9 | 69.4±10.9 | –1.6 | <0.001 | 208 | 69.4±10.1 | 69.0±10.2 | –0.4 | 0.002 | <0.001 |
| BMI, kg/m2 | 207 | 26.5±3.0 | 26.0±3.0 | –0.6 | <0.001 | 208 | 26.0±2.6 | 25.9±2.7 | –0.1 | 0.001 | <0.001 |
| Waist circumference, cm | 206 | 91.4±8.1 | 90.4±8.0 | –1.1 | <0.001 | 208 | 90.7±7.2 | 90.6±7.3 | –0.1 | 0.670 | 0.003 |
| Blood pressure, mm Hg | |||||||||||
| Systolic | 206 | 122.0±11.9 | 118.4±12.6 | –3.7 | <0.001 | 205 | 122.6±11.2 | 120.7±10.7 | –2.0 | 0.001 | 0.051 |
| Diastolic | 206 | 81.9±8.5 | 79.5±9.0 | –2.5 | <0.001 | 205 | 81.9±8.1 | 80.1±8.2 | –1.8 | <0.001 | 0.256 |
| Fasting glucose, mg/dL | 207 | 100.1±8.7 | 97.8±9.9 | –2.3 | <0.001 | 208 | 98.6±8.9 | 97.8±9.6 | –0.9 | 0.077 | 0.102 |
| Glucose, 30 min, mg/dL | 206 | 174.7±24.0 | 167.7±25.6 | –7.0 | <0.001 | 207 | 171.4±25.3 | 169.7±28.5 | –1.7 | 0.305 | 0.021 |
| Glucose, 120 min, mg/dL | 207 | 135.3±31.2 | 130.5±34.2 | –4.8 | 0.026 | 208 | 135.9±29.8 | 135.9±36.1 | 0.0 | 0.990 | 0.140 |
| HbA1c, % | 205 | 5.78±0.30 | 5.76±0.30 | –0.02 | 0.059 | 206 | 5.76±0.30 | 5.77±0.34 | 0.01 | 0.580 | 0.100 |
| Insulin, 0, μU/mL | 191 | 8.8±8.7 | 7.2±4.4 | –1.6 | 0.002 | 194 | 8.1±5.3 | 8.2±4.7 | 0.0 | 0.742 | 0.011 |
| Insulin, 30, μU/mL | 191 | 43.2±36.3 | 37.1±33.6 | –6.1 | 0.001 | 193 | 42.7±26.2 | 43.3±29.5 | 0.6 | 0.937 | 0.015 |
| Insulin, 120, μU/mL | 192 | 43.2±28.5 | 39.6±29.7 | –3.6 | 0.011 | 194 | 46.8±32.8 | 47.9±38.1 | 1.0 | 0.767 | 0.079 |
| HOMA-IR | 191 | 2.2±2.1 | 1.8±1.2 | –0.4 | <0.001 | 194 | 2.0±1.4 | 2.0±1.2 | 0.0 | 0.951 | 0.007 |
| HOMA-β | 191 | 88.1±92.1 | 78.6±49.7 | –9.5 | 0.278 | 194 | 85.1±57.1 | 88.7±57.3 | 3.6 | 0.233 | 0.090 |
| Total cholesterol, mg/dL | 205 | 191.1±31.4 | 190.8±32.7 | –0.4 | 0.853 | 205 | 189.2±36.0 | 190.5±33.2 | 1.2 | 0.352 | 0.541 |
| Total triglycerides, mg/dL | 205 | 155.0±94.9 | 145.7±98.0 | –9.3 | 0.002 | 205 | 153.7±92.8 | 156.8±94.7 | 3.1 | 0.330 | 0.003 |
| HDL-C, mg/dL | 205 | 50.6±12.3 | 53.2±12.7 | 2.6 | <0.001 | 205 | 51.9±13.7 | 52.5±13.9 | 0.5 | 0.260 | 0.001 |
| LDL-C, mg/dL | 203 | 121.5±30.0 | 120.4±32.0 | –1.1 | 0.549 | 204 | 119.1±33.6 | 120.2±30.6 | 1.1 | 0.353 | 0.358 |
Values are presented as mean±standard deviation.
LSM, lifestyle modification; SM, standard management; BMI, body mass index; HbA1c, glycosylated hemoglobin; HOMA-IR, homeostatic model assessment for insulin resistance; HOMA-β, homeostatic model assessment for β-cell function; HDL-C, high-density lipoprotein cholesterol; LDL-C, low-density lipoprotein cholesterol.
a Wilcoxon signed rank test for continues variables was used to compare changes in clinical outcomes between pre- and post-intervention in each group,
b Repeated measures analysis of covariance (ANCOVA) test was used to compare changes in clinical outcomes between two groups.
- 1. International Diabetes Federation. IDF diabetes atlas. 9th ed. Brussels: IDF; 2019.
- 2. Kim BY, Won JC, Lee JH, Kim HS, Park JH, Ha KH, et al. Diabetes fact sheets in Korea, 2018: an appraisal of current status. Diabetes Metab J 2019;43:487-94.ArticlePubMedPMCPDF
- 3. Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, et al. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care 1997;20:537-44.ArticlePubMedPDF
- 4. Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, et al. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med 2002;346:393-403.ArticlePubMedPMC
- 5. Ramachandran A, Snehalatha C, Mary S, Mukesh B, Bhaskar AD, Vijay V, et al. The Indian Diabetes Prevention Programme shows that lifestyle modification and metformin prevent type 2 diabetes in Asian Indian subjects with impaired glucose tolerance (IDPP-1). Diabetologia 2006;49:289-97.ArticlePubMedPDF
- 6. Tate DF, Jackvony EH, Wing RR. Effects of Internet behavioral counseling on weight loss in adults at risk for type 2 diabetes: a randomized trial. JAMA 2003;289:1833-6.ArticlePubMed
- 7. Hunter CM, Peterson AL, Alvarez LM, Poston WC, Brundige AR, Haddock CK, et al. Weight management using the internet a randomized controlled trial. Am J Prev Med 2008;34:119-26.PubMed
- 8. Stewart T, Han H, Allen RH, Bathalon G, Ryan DH, Newton RL Jr, et al. H.E.A.L.T.H.: efficacy of an internet/population-based behavioral weight management program for the U.S. Army. J Diabetes Sci Technol 2011;5:178-87.ArticlePubMedPMCPDF
- 9. Unick JL, Leahey T, Kent K, Wing RR. Examination of whether early weight loss predicts 1-year weight loss among those enrolled in an internet-based weight loss program. Int J Obes (Lond) 2015;39:1558-60.ArticlePubMedPMCPDF
- 10. Rhee SY, Chon S, Ahn KJ, Woo JT; Korean Diabetes Prevention Study Investigators. Hospital-based Korean diabetes prevention study: a prospective, multi-center, randomized, open-label controlled study. Diabetes Metab J 2019;43:49-58.ArticlePubMedPDF
- 11. Cha SA, Lim SY, Kim KR, Lee EY, Kang B, Choi YH, et al. Community-based randomized controlled trial of diabetes prevention study for high-risk individuals of type 2 diabetes: lifestyle intervention using web-based system. BMC Public Health 2017;17:387.ArticlePubMedPMCPDF
- 12. Moher D, Schulz KF, Altman D; CONSORT Group (Consolidated Standards of Reporting Trials). The CONSORT statement: revised recommendations for improving the quality of reports of parallel-group randomized trials. JAMA 2001;285:1987-91.ArticlePubMed
- 13. Ware JH. Interpreting incomplete data in studies of diet and weight loss. N Engl J Med 2003;348:2136-7.ArticlePubMed
- 14. Watanabe M, Okayama A, Shimamoto K, Ueshima H. Short-term effectiveness of an individual counseling program for impaired fasting glucose and mild type 2 diabetes in Japan: a multi-center randomized control trial. Asia Pac J Clin Nutr 2007;16:489-97.PubMed
- 15. Block G, Azar KM, Romanelli RJ, Block TJ, Hopkins D, Carpenter HA, et al. Diabetes prevention and weight loss with a fully automated behavioral intervention by email, web, and mobile phone: a randomized controlled trial among persons with prediabetes. J Med Internet Res 2015;17:e240.ArticlePubMedPMC
- 16. Fukuoka Y, Gay CL, Joiner KL, Vittinghoff E. A novel diabetes prevention intervention using a mobile app: a randomized controlled trial with overweight adults at risk. Am J Prev Med 2015;49:223-37.PubMedPMC
- 17. Korea Centers for Disease Control & Prevention; Ministry of Health and Welfare. Korea health statistics 2018: Korea National Health and Nutrition Examination Survey (KNHANES VII-3). Cheongju: KCDC; 2019.
- 18. Vadheim LM, McPherson C, Kassner DR, Vanderwood KK, Hall TO, Butcher MK, et al. Adapted diabetes prevention program lifestyle intervention can be effectively delivered through telehealth. Diabetes Educ 2010;36:651-6.ArticlePubMedPDF
- 19. Bennett GG, Herring SJ, Puleo E, Stein EK, Emmons KM, Gillman MW. Web-based weight loss in primary care: a randomized controlled trial. Obesity (Silver Spring) 2010;18:308-13.ArticlePubMedPDF
- 20. Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature 2006;444:840-6.ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations

- U-shaped association between online information exchange and app usage frequency: a large-scale survey of China ‘s online young and middle-aged people with pre diabetes and diabetes
Hanbin Guo, Yibiao Xiao, Canlin Liao, Jiating Sun, Yanchun Xie, Yitong Zheng, Guanhua Fan
Frontiers in Endocrinology.2023;[Epub] CrossRef - Innovation in diabetes prevention research: The 36-year legacy of China Da Qing diabetes prevention study
Xin Chai, Yachen Wang, Jinping Wang, Qiuhong Gong, Juan Zhang, Ruitai Shao
Chinese Science Bulletin.2023; 68(28-29): 3834. CrossRef - Efficacy of Personalized Diabetes Self-care Using an Electronic Medical Record–Integrated Mobile App in Patients With Type 2 Diabetes: 6-Month Randomized Controlled Trial
Eun Young Lee, Seon-Ah Cha, Jae-Seung Yun, Sun-Young Lim, Jin-Hee Lee, Yu-Bae Ahn, Kun-Ho Yoon, Min Kyung Hyun, Seung-Hyun Ko
Journal of Medical Internet Research.2022; 24(7): e37430. CrossRef - Prevention of type 2 diabetes through remotely administered lifestyle programs: A systematic review
Valaree Villegas, Alisha Shah, JoAnn E. Manson, Deirdre K. Tobias
Contemporary Clinical Trials.2022; 119: 106817. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Kyu Yeon Hur, Min Kyong Moon, Jong Suk Park, Soo-Kyung Kim, Seung-Hwan Lee, Jae-Seung Yun, Jong Ha Baek, Junghyun Noh, Byung-Wan Lee, Tae Jung Oh, Suk Chon, Ye Seul Yang, Jang Won Son, Jong Han Choi, Kee Ho Song, Nam Hoon Kim, Sang Yong Kim, Jin Wha Kim,
Diabetes & Metabolism Journal.2021; 45(4): 461. CrossRef - 2021 Clinical Practice Guidelines for Diabetes Mellitus in Korea
Seung-Hyun Ko
The Journal of Korean Diabetes.2021; 22(4): 244. CrossRef

 KDA
KDA
 PubReader
PubReader ePub Link
ePub Link Cite
Cite