- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 45(4); 2021 > Article
-
Original ArticleCardiovascular Risk/Epidemiology Metabolic Syndrome Severity Score for Predicting Cardiovascular Events: A Nationwide Population-Based Study from Korea
-
Yo Nam Jang1
 , Jun Hyeok Lee2, Jin Sil Moon2, Dae Ryong Kang3, Seong Yong Park4, Jerim Cho4, Jang-Young Kim5
, Jun Hyeok Lee2, Jin Sil Moon2, Dae Ryong Kang3, Seong Yong Park4, Jerim Cho4, Jang-Young Kim5 , Ji Hye Huh6
, Ji Hye Huh6
-
Diabetes & Metabolism Journal 2021;45(4):569-577.
DOI: https://doi.org/10.4093/dmj.2020.0103
Published online: January 30, 2021
1Yonsei University Wonju College of Medicine, Wonju, Korea
2Department of Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
3Department of Precision Medicine & Biostatistics, Yonsei University Wonju College of Medicine, Wonju, Korea
4Big Data Streering Department, National Health Insurance Service, Wonju, Korea
5Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea
6Division of Endocrinology and Metabolism, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea
-
Corresponding authors: Jang-Young Kim
 Division of Cardiology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, 20 Ilsan-ro, Wonju 26426, Korea E-mail: kimjang713@gmail.com
Division of Cardiology, Department of Internal Medicine, Yonsei University Wonju College of Medicine, 20 Ilsan-ro, Wonju 26426, Korea E-mail: kimjang713@gmail.com -
Ji Hye Huh
 Division of Endocrinology and Metabolism, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, 22 Gwanpyeong-ro 170beon-gil, Dongan-gu, Anyang 14068, Korea E-mail: png1212@hallym.or.kr
Division of Endocrinology and Metabolism, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, 22 Gwanpyeong-ro 170beon-gil, Dongan-gu, Anyang 14068, Korea E-mail: png1212@hallym.or.kr
Copyright © 2021 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/4.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Recently, a metabolic syndrome severity score (MS score) using a dataset of the Korea National Health and Nutrition Examination Surveys has been developed. We aimed to determine whether the newly developed score is a significant predictor of cardiovascular (CV) events among the Korean population.
-
Methods
- From the Korean National Health Insurance System, 2,541,364 (aged 40 to 59 years) subjects with no history of CV events (ischemic stroke or myocardial infarction [MI]), who underwent health examinations from 2009 to 2011 and were followed up until 2014 to 2017, were identified. Cox proportional hazard model was employed to investigate the association between MS score and CV events. Model performance of MS score for predicting CV events was compared to that of conventional metabolic syndrome diagnostic criteria (Adult Treatment Program III [ATP-III]) using the Akaike information criterion and the area under the receiver operating characteristic curve.
-
Results
- Over a median follow-up of 6 years, 15,762 cases of CV events were reported. MS score at baseline showed a linear association with incident CV events. In the multivariable-adjusted model, the hazard ratios (95% confidence intervals) comparing the highest versus lowest quartiles of MS score were 1.48 (1.36 to 1.60) for MI and 1.89 (1.74 to 2.05) for stroke. Model fitness and performance of the MS score in predicting CV events were superior to those of ATP-III.
-
Conclusion
- The newly developed age- and sex-specific continuous MS score for the Korean population is an independent predictor of ischemic stroke and MI in Korean middle-aged adults even after adjusting for confounding factors.
- Metabolic syndrome (MS) refers to a cluster of several interrelated risk factors for cerebro-cardiovascular diseases (CVDs) [1] and is comprises five individual components (central obesity, hypertension, hypertriglyceridemia, low-high density lipoprotein [HDL], and elevated fasting glucose) that are associated with insulin resistance. The underlying processes in MS include cellular dysfunction, systemic inflammation, and oxidative stress, which are well-known pathophysiological mechanisms of CVD [2,3]. Although MS is not a disease in itself, it is associated with incident CVD, diabetes, chronic kidney disease [4], and even an increased risk of cancer. MS also increases the risk of all-cause mortality and burden of healthcare costs [5]. Therefore, it is important to more carefully assess MS status and track MS severity over time. However, the use of the conventional MS diagnostic criteria (Adult Treatment Program III [ATP-III]) have been limited by the dichotomy of the current MS definitions (i.e., present/absent), and minimal changes in the values of the criteria could result in classifying patients as having MS or not [3,6]. The lack of a universal definition of MS and the fact that MS has been defined as a dichotomous variable have ushered in the development of a continuous MS severity score (MS score) that is specific to sex and race/ethnicity [7,8]. For the Western population, several researchers formulated a MS severity Z score that serves as a continuous estimate of metabolic derangement using confirmatory factor analysis [9-12]. Moreover, studies have demonstrated that the continuous MS score could well predict incident CVD or diabetes in the United States population [13]. Recently, our research group also developed a MS severity Z score for the Korean population from a dataset of the Korea National Health and Nutrition Examination Surveys and using statistical methods similar to those used to develop the score for Western countries [7]. However, whether this newly developed MS score works well in disease prediction remains to be confirmed.
- Thus, we aimed to determine whether the newly developed MS score is a significant predictor of overall mortality and CVD in the Korean population. We also aimed to assess the predictive ability of the MS score for overall mortality and incident CVD by comparing it to other traditional MS diagnostic tools, such as ATP-III, using large-scale cohort data from the whole South Korean population.
INTRODUCTION
- Study population
- This study was approved by the Institutional Review Board of Yonsei University Wonju College of Medicine, Republic of Korea (No. CR318352) and this study was conducted in accordance with the provisions of the Declaration of Helsinki. Anonymous and de-identified information was used for analysis and, therefore, informed consent was not obtained.
- In this retrospective study, we used a database provided by the National Health Insurance Services–Health Screening (NHIS-HEALS) Cohort in Korea. The insurance system was established by the Korean government and covers approximately 97.2% of residents. Individuals aged ≥40 years are entitled to undergo a general health screening program every 2 years. The screening includes standardized self-report questionnaires on medical history and lifestyle behaviours, anthropometric and blood pressure measurements, and routine laboratory tests using blood and urine. The cohort profile of the NHIS-HEALS is described elsewhere [14]. Moreover, the NHIS provided a research-specific database from the NHIS-HEALS according to the conditions set by the researcher. This data is only available for researchers who are permitted by NHIS. Our research-specific database included 2009 to 2011 data of subjects aged 19 to 69 years who underwent at least two general health screening programs in 2009 to 2011. To exclude subjects with myocardial infarction (MI) or ischemic stroke, subjects who had the following International Classification of Diseases, 10th Revision (ICD-10) codes (as main diagnosis or sub-diagnosis at baseline) were not included: I21, I22, I23, I63, or I64. We excluded those who were aged <40 years in 2009 and those who did not participate in a general health screening program in 2009. Therefore, 4,709,862 subjects were assessed for eligibility. Subjects aged >60 years in 2009 or who had one or more missing values in the MS components were excluded (n=971,452) because MS scores were not available. Subjects receiving medications for hypertension (n=1,093,687) or diabetes (n=281,126) were also excluded (n=1,197,046) as these medications possibly affect MS score. Medication status was determined by prescriptions or survey responses. A total of 2,541,364 subjects were enrolled in this study (Supplementary Figs. 1).
- Measurements and definitions
- Healthcare institutions for screening are designated according to the Framework Act on Health Examinations and must meet the standards of manpower, facilities, and equipment [14]. To minimize errors in the measurement, average values of all laboratory test data from 2009 to 2011 were used. Values outside the extreme outlier were treated as missing values. Height, weight, and waist circumference were measured, and body mass index (BMI) was calculated as the subject’s weight in kilograms divided by the square of the subject’s height in meters. Blood samples for serum glucose and total cholesterol (TC) level measurement were obtained after an overnight fast [15]. Low-density lipoprotein cholesterol (LDL-C) levels were calculated from TC, HDL-C, and triglyceride (TG) levels or measured directly. Diabetes was defined as fasting glucose level ≥126 mg/dL and hypertension as systolic/diastolic blood pressure ≥140/90 mm Hg in the 2009 to 2011 health screening program. Medication use for dyslipidaemia was defined as the use of statin, fibrates, bile acid sequestrants, nicotinic acid, ezetimibe, niacin derivatives, or a mixture containing them or determined based on survey response. Income level was divided into four categories based on insurance premium calculation. Information on smoking, alcohol consumption, and regular exercise was obtained by questionnaire. Smoking status was dichotomized as current smoker and not; alcohol consumption as heavy drinker (i.e., consumption of 14 and seven units of alcohol per week in men and women, respectively) and not. Regular exercise was defined as moderate to vigorous intensity physical activity for more than 3 days per week.
- Definition of MS and MS score
- Based on the modified NCEP ATP-III criteria, MS was defined as the presence of three or more of the following components [16]: abdominal obesity (waist circumference ≥90 cm for men and ≥85 cm for women, which is according to the Korean Society of Obesity) [17], hypertriglyceridemia (serum TG concentration ≥150 mg/dL), low HDL-C (serum HDL-C <40 mg/dL for men or <50 mg/dL for women), high blood pressure (systolic blood pressure ≥130 mm Hg, diastolic blood pressure ≥85 mm Hg, or treatment with antihypertensive agents), and high fasting glucose (fasting serum glucose ≥100 mg/dL or a previous diagnosis of type 2 diabetes mellitus) [18].
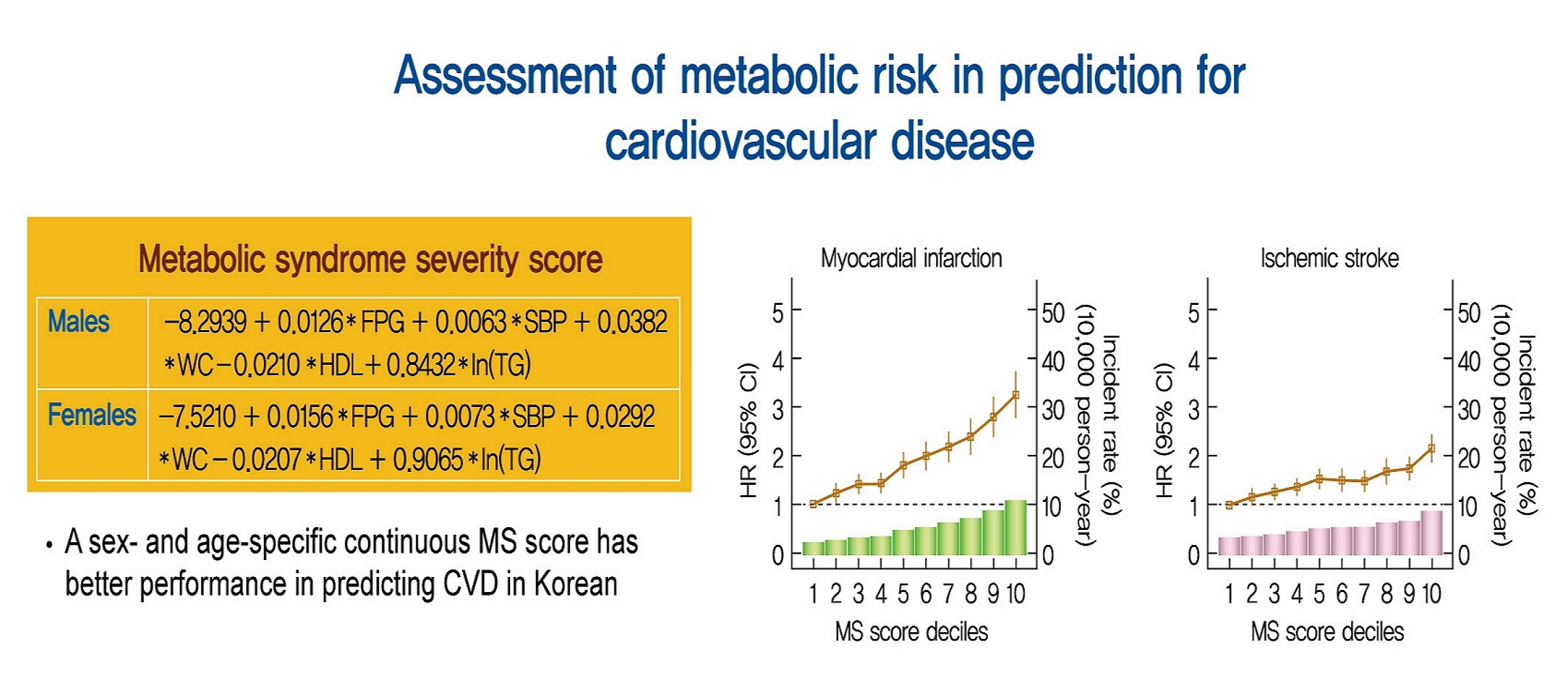
- Our research group previously demonstrated a continuous MS severity Z score based on data from the Korean population. Prior researchers calculated the MS severity Z scores at baseline using sex- and race/ethnicity-based formulas. The MS score was derived from the five traditional MS components (i.e., waist circumference, TG, HDL-C, systolic blood pressure, fasting glucose) using a factor analysis approach. Because of differences in traditional MS criteria by race/ethnicity and in MS-related risk by sex, we performed a confirmatory factor analysis on a sex- and age-specific basis and found differences in the factor loadings of the five MS components between sexes and between age groups among Korean adults [7]. Equations based on the factor coefficients from confirmatory factor analysis results are presented in Supplementary table 1 and Supplementary Figs. 2.
- Study outcome
- We enrolled the population at risk between 2009 and 2011 in this study and investigated the study outcomes in the follow-up period from 2014 to 2017, following a 2-year washout period (2012 to 2013). The primary endpoints of the study were newly diagnosed cardiovascular (CV) events (ischemic stroke or MI) during the follow-up period. MI was determined by either the recording of ICD-10 code I21 or I22 during hospitalization of ≥4 days or the recording of these codes at least twice. Ischemic stroke was described as the recording of the ICD-10 code I63 or I64 during hospitalization of ≥4 days with claims for brain magnetic resonance imaging or brain computed tomography [15]. Subjects were considered to have completed the study at the date of their CV events or at the end of the follow-up, whichever came first (Supplementary table 2).
- Statistical analysis
- Baseline characteristics are presented as mean±standard deviation or number (%). Participants were classified into four groups according to MS score quartiles. The incidence rate of primary and secondary outcomes was calculated by dividing the number of incident cases by the total follow-up duration (person-years). The multivariable-adjusted proportional hazards model was applied: model 1 was adjusted for age, BMI, smoking status, alcohol consumption, regular exercise, and income; model 2 was adjusted for the presence of hypertension, diabetes, medication for dyslipidaemia and TC. Hazard ratios and 95% confidence interval (CI) values of MI and stroke were analyzed using the Cox proportional hazards model for the quartile groups of MS score. Model performance was also analyzed. We compared the model performance of ATP-III-based MS and that of MS score for predicting CVD using the Akaike information criterion (AIC) and area under receiver operating characteristic (AUC) of receiver operating characteristic curve (ROC) analysis. Smaller AIC values indicated a better fit. Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc., Cary, NC, USA), and a P<0.05 was considered statistically significant.
METHODS
- Baseline characteristics of the study population
- A total of 2,541,364 subjects who were naïve to antihypertensive and antidiabetic medical treatments and had available MS scores were identified. Baseline characteristics of the subjects according to MS score quartiles are shown in Table 1.
- Mean age was 47.52±5.35 years, 52.75% were male, and MS prevalence was 9.89%. As MS score increased, mean age, waist circumference, systolic/diastolic blood pressure, fasting glucose, TC, LDL-C, and TG tended to increase, and HDL-C tended to decrease. Regarding lifestyle factors, the ratio of heavy drinkers and current smokers was higher in the higher MS score quartile. Subjects who performed regular exercise were more likely to be distributed to the lower MS score quartile. Moreover, hypertension, diabetes, and the use of medications for dyslipidaemia increased as the MS score increased. The higher the MS score, the higher the MS prevalence and the greater the number of MS components.
- Relationship between MS score and cardiovascular outcomes
- A total of 15,762 CV events (7,762 MI and 8,197 ischemic stroke) were recorded during a median follow-up of 6 years. The incidence of CV events during the follow-up period increased with an increase in MS score quartiles (Table 2). The incidence of stroke and MI increased as the MS score quartile increased. Incidence rates of CV events were approximately 2.5 times higher in the fourth MS score quartile group than in the first MS score quartile group. CVD risk was incrementally higher in the higher MS score quartile group than in the lowest MS score quartile group in all models. The risk of MI increased more sharply than that of ischemic stroke as the MS score increased; the fully adjusted hazard ratios of ischemic stroke and MI were 1.89 and 1.48, respectively, in the fourth MS score quartile group.
- To assess the linear trends of the risk, we investigated the risk of CV events (MI or ischemic stroke) by MS score decile groups, with the first decile group as the reference (Fig. 1). The risk of both MI and ischemic stroke increased continuously in the second decile group.
- Predictive ability of MS score for CV events
- With regard to predicting CV events, the AUC of the MS score was 0.720 (95% CI, 0.716 to 0.724), while that of ATP III-diagnosed MS was 0.718 (95% CI, 0.714 to 0.722) (Table 3).
- Similarly, in predicting the incidence of ischemic stroke and MI, the AUC values of MS score were higher than those of ATP III-diagnosed MS. We also compared the model performance of the newly developed MS score and ATP III-diagnosed MS (Table 3). Overall, the MS score plus age, BMI, smoking status, alcohol consumption, regular exercise, and income model had a higher performance than the ATP III-diagnosed MS in terms of AIC values, thereby suggesting that MS score could more properly predict the occurrence of CV events.
RESULTS
- In this large-scale and nationally representative populationbased study, we found that MS score, which is a continuous estimate of MS severity, could well predict CVD risk among the relatively healthy Korean population. The age- and sex-specific continuous MS score is an independent predictor of ischemic stroke and MI even after adjusting for confounding factors, including diabetes, hypertension, and cholesterol levels, which are also individual MS components. Furthermore, we observed that the MS score could predict future CV events better than traditional MS defined using ATP-III criteria could. To the best of our knowledge, this is the first study to demonstrate the potential utility of continuous MS score in identifying Korean adults at a higher risk of CV events.
- In this study, we confirmed that our newly developed continuous MS score could be used as a significant predictor of CVD among the Korean population aged 40 to 59 years. This finding is consistent with the hypothesis that a higher degree of MS severity, which potentially serves as an estimate of the underlying metabolic dysfunction driving the abnormalities of the individual MS components, may contribute to future risk of CVD [19,20]. Our result is also in line with the results of previous studies which demonstrated that MS score is strongly associated with coronary heart disease [21]. Thus, the results of our study suggest that the continuous MS score could provide information on metabolic derangement as well as future CVD risk.
- MS score is distinct from the traditional MS defined using the ATP-III criteria: MS severity could be tracked with a continuous MS score, and any metabolic abnormality slightly below the cut-off value of the ATP-III criteria may be detected with it. Moreover, because the influence of MS components on MS differ between sex and between racial/ethnic groups, MS score could provide a more specialized calculation. Thus, MS score could be clinically useful in predicting CVD risk, especially in relatively healthy adults who are free of chronic diseases such as diabetes or hypertension. Hence, our research group developed an age- and sex-specific MS severity Z score, and in this study we confirmed its usefulness in predicting future CVD occurrence in the Korean population. Nonetheless, calculating MS score may be time-consuming in clinical practice; thus, an automated system (e.g., MS score calculator that automatically uses electronic medical records) is needed.
- Our study result may not be surprising as MS is known to be associated with CVD [22]. However, the traditional ATP-III MS criteria are limited by identifying risk only when a person exhibits abnormalities beyond the cutoffs for three of the components. In case of an individual with measurements in the MS components just below the threshold for all five components, although they may be at higher risk of CVD than someone who just exceeds the cutoffs in three components but has low or normal levels of the other two, they are considered as subjects with lower CV risk by traditional ATP-III criteria. One of the two major features in which the MS score model differs from the ATP-III model is that each MS component has a different contribution. The second feature is that each MS component contributes linearly to the score. As demonstrated in the preceding study, the effect of each MS component on MS severity varies according to its contributions to the latent MS factor [7]. The MS score reflects the differences in such contributions of each component, which resulted in more sophisticated results than the ATP-III model. Actually, we found that the continuous MS severity Z score model showed improved predictive power for CV events over the traditional ATP-III model in the ROC curve analysis. Furthermore, we are not able to follow metabolic risk change over time in individuals using the binary traditional ATP-III criteria. While, the continuous MS score can follow for the degree of change in metabolic risk over time in individuals. Tracking the change of metabolic risk in population using continuous MS severity score can help to identify specific groups or periods of time of intensive intervention. For these reasons, the newly developed MS score might have more benefit than the traditional ATP-III criteria in predicting CV events and assessing CV risk changes overtime.
- This study has a number of strengths. The continuous MS severity Z score developed in the preceding study is the first MS score for the Korean population; however, it is not to be verified yet by large external data. Our study is the first to verify the MS score for the Korean population. Moreover, we validated the score system with a large, representative population sample, which could increase the reliability of results. Nevertheless, this study has some limitations. Considering the retrospective design, our study was not completely free of potential bias during data collection. Furthermore, although the preceding study suggested Z scores for three age groups, only one was verified in our study. We limited the age of subjects to 40 to 59 years for clarity of results and for obtaining a representative sample considering the eligibility for the general health screening program. Although the proportion was small, lack of data regarding the specific lipid lowering treatment may influence on MS score was the limitation of our study. Another limitation of our study was the short follow-up period. We enrolled the subjects from 2009 to 2011, and CVD incidence and mortality were observed between 2014 and 2017. Thus, the maximum follow-up period from the study enrolment was 6 years, which may not be long enough to investigate chronic diseases, such as CVD, or death. Moreover, the NHIS-HEALS data per se imply the possibility of errors. Owing to the conflict between the health insurance policy and the interests of individual patients, some doctors may have used ICD codes for their patients that do not exactly match. Although such issues could be prevented by a monitoring system, it remains a potential source of bias and may thus affect the study results. However, we adjusted the problem with a careful operational definition of CVD.
- In conclusion, we found that a sex- and age-specific continuous MS score is associated with the risk of future CVD among relatively healthy Korean middle-aged adults based on models that included each MS component. We also confirmed the good predictive ability of the continuous MS score for incident CVD, and MS score had better predictive ability for CVD development than the ATP-III criteria. Thus, our finding provides evidence of the potential utility of MS score tracking in clinical practice to identify those at a higher risk of CVD who would need intervention. Further studies with a long-term follow-up might be warranted to generalize the MS score’s utility in predicting various types of health outcomes in Korean middle-aged adults.
DISCUSSION
Supplementary Materials
Supplementary Table 1.
Supplementary Table 2.
Supplementary Fig. 1.
Supplementary Fig. 2.
-
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
-
AUTHOR CONTRIBUTIONS
Conception or design: J.Y.K., J.H.H.
Acquisition, analysis, or interpretation of data: Y.N.J., J.H.L., J.S.M., D.R.K., S.Y.P., J.C.
Drafting the work or revising: Y.N.J., J.H.H.
Final approval of the manuscript: J.Y.K., J.H.H.
-
FUNDING
This study was supported by a National Research Foundation of Korea (NRF) Grant funded by the Korean government (MSIP) (No. NRF-2019R1G1A109408).
NOTES
-
Acknowledgements
- The authors thank the staff at the Big Data Steering Department at the National Health Insurance Service (NHIS) for providing data and support.

Model 1: adjusted for age, body mass index, current smoking, heavy alcohol consumption, regular exercise, and family income; Model 2: model 1+further adjusted for the presence of hypertension, diabetes, medication for dyslipidemia, and total cholesterol.
MS, metabolic syndrome; HR, hazard ratio; CI, confidence interval.
| Event | Model | MS indicator | AIC | AUC (95% CI) | P valuea |
|---|---|---|---|---|---|
| CV events | |||||
| 1 | ATP-III | 181,473.2 | 0.718 (0.714–0.722) | <0.001 | |
| MS score | 181,292.2 | 0.720 (0.716–0.724) | |||
| 2 | ATP-III | 183,029.2 | 0.704 (0.700–0.708) | <0.001 | |
| MS score | 182,600.6 | 0.708 (0.704–0.712) | |||
| Stroke | |||||
| 1 | ATP-III | 100,892.9 | 0.705 (0.699–0.711) | 0.003 | |
| MS score | 100,828.8 | 0.707 (0.701–0.712) | |||
| 2 | ATP-III | 101,508.2 | 0.693 (0.688–0.699) | 0.003 | |
| MS score | 101,406.9 | 0.696 (0.690–0.702) | |||
| MI | |||||
| 1 | ATP-III | 103,820.7 | 0.741 (0.735–0.746) | <0.001 | |
| MS score | 103,696.9 | 0.743 (0.738–0.748) | |||
| 2 | ATP-III | 105,174.2 | 0.720 (0.714–0.725) | <0.001 | |
| MS score | 104,813.0 | 0.726 (0.721–0.731) |
Model 1: adjusted for age, body mass index, current smoking, heavy alcohol consumption, regular exercise, and family income; Model 2: Model 1+further adjusted presence of hypertension, diabetes, medication for dyslipidemia, and total cholesterol.
MS, metabolic syndrome; AIC, Akaike information criterion; AUC, the area under the receiver operating characteristic curve; CI, confidence interval; CV, cardiovascular; ATP-III, Adult Treatment Program III; MI, myocardial infarction.
a DeLong’s test for receiver operating characteristic (ROC) curves of two metabolic syndrome indicators.
- 1. Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, et al. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 2002;288:2709-16.ArticlePubMed
- 2. Gurka MJ, Guo Y, Filipp SL, DeBoer MD. Metabolic syndrome severity is significantly associated with future coronary heart disease in type 2 diabetes. Cardiovasc Diabetol 2018;17:17.ArticlePubMedPMCPDF
- 3. DeBoer MD, Gurka MJ. Clinical utility of metabolic syndrome severity scores: considerations for practitioners. Diabetes Metab Syndr Obes 2017;10:65-72.ArticlePubMedPMCPDF
- 4. Huh JH, Yadav D, Kim JS, Son JW, Choi E, Kim SH, et al. An association of metabolic syndrome and chronic kidney disease from a 10-year prospective cohort study. Metabolism 2017;67:54-61.ArticlePubMed
- 5. Ford ES. Risks for all-cause mortality, cardiovascular disease, and diabetes associated with the metabolic syndrome: a summary of the evidence. Diabetes Care 2005;28:1769-78.PubMed
- 6. Soldatovic I, Vukovic R, Culafic D, Gajic M, Dimitrijevic-Sreckovic V. siMS score: simple method for quantifying metabolic syndrome. PLoS One 2016;11:e0146143.ArticlePubMedPMC
- 7. Huh JH, Lee JH, Moon JS, Sung KC, Kim JY, Kang DR. Metabolic syndrome severity score in Korean adults: analysis of the 2010-2015 Korea National Health and Nutrition Examination Survey. J Korean Med Sci 2019;34:e48.ArticlePubMedPMCPDF
- 8. Gurka MJ, Lilly CL, Oliver MN, DeBoer MD. An examination of sex and racial/ethnic differences in the metabolic syndrome among adults: a confirmatory factor analysis and a resulting continuous severity score. Metabolism 2014;63:218-25.ArticlePubMed
- 9. Andersen LB, Harro M, Sardinha LB, Froberg K, Ekelund U, Brage S, et al. Physical activity and clustered cardiovascular risk in children: a cross-sectional study (The European Youth Heart Study). Lancet 2006;368:299-304.ArticlePubMed
- 10. Brage S, Wedderkopp N, Ekelund U, Franks PW, Wareham NJ, Andersen LB, et al. Features of the metabolic syndrome are associated with objectively measured physical activity and fitness in Danish children: the European Youth Heart Study (EYHS). Diabetes Care 2004;27:2141-8.PubMed
- 11. Batey LS, Goff DC Jr, Tortolero SR, Nichaman MZ, Chan W, Chan FA, et al. Summary measures of the insulin resistance syndrome are adverse among Mexican-American versus non-Hispanic white children: the Corpus Christi Child Heart Study. Circulation 1997;96:4319-25.ArticlePubMed
- 12. Katzmarzyk PT, Perusse L, Malina RM, Bergeron J, Despres JP, Bouchard C. Stability of indicators of the metabolic syndrome from childhood and adolescence to young adulthood: the Quebec Family Study. J Clin Epidemiol 2001;54:190-5.PubMed
- 13. DeBoer MD, Gurka MJ, Woo JG, Morrison JA. Severity of metabolic syndrome as a predictor of cardiovascular disease between childhood and adulthood: the Princeton Lipid Research Cohort Study. J Am Coll Cardiol 2015;66:755-7.PubMedPMC
- 14. Seong SC, Kim YY, Park SK, Khang YH, Kim HC, Park JH, et al. Cohort profile: the National Health Insurance Service-National Health Screening Cohort (NHIS-HEALS) in Korea. BMJ Open 2017;7:e016640.ArticlePubMedPMC
- 15. Kim MK, Han K, Kim HS, Park YM, Kwon HS, Yoon KH, et al. Cholesterol variability and the risk of mortality, myocardial infarction, and stroke: a nationwide population-based study. Eur Heart J 2017;38:3560-6.ArticlePubMedPMC
- 16. Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation 2005;112:2735-52.ArticlePubMed
- 17. Lee SY, Park HS, Kim DJ, Han JH, Kim SM, Cho GJ, et al. Appropriate waist circumference cutoff points for central obesity in Korean adults. Diabetes Res Clin Pract 2007;75:72-80.ArticlePubMed
- 18. Huh JH, Ahn SG, Kim YI, Go T, Sung KC, Choi JH, et al. Impact of longitudinal changes in metabolic syndrome status over 2 years on 10-year incident diabetes mellitus. Diabetes Metab J 2019;43:530-8.ArticlePubMedPMCPDF
- 19. de Ferranti S, Mozaffarian D. The perfect storm: obesity, adipocyte dysfunction, and metabolic consequences. Clin Chem 2008;54:945-55.ArticlePubMedPDF
- 20. DeBoer MD. Obesity, systemic inflammation, and increased risk for cardiovascular disease and diabetes among adolescents: a need for screening tools to target interventions. Nutrition 2013;29:379-86.ArticlePubMed
- 21. Guo Y, Musani SK, Sims M, Pearson TA, DeBoer MD, Gurka MJ. Assessing the added predictive ability of a metabolic syndrome severity score in predicting incident cardiovascular disease and type 2 diabetes: the Atherosclerosis Risk in Communities Study and Jackson Heart Study. Diabetol Metab Syndr 2018;10:42.ArticlePubMedPMCPDF
- 22. Isomaa B, Almgren P, Tuomi T, Forsen B, Lahti K, Nissen M, et al. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care 2001;24:683-9.ArticlePubMedPDF
REFERENCES
Figure & Data
References
Citations

- Metabolic syndrome awareness in the general Korean population: results from a nationwide survey
Hyun-Jin Kim, Mi-Seung Shin, Kyung-Hee Kim, Mi-Hyang Jung, Dong-Hyuk Cho, Ju-Hee Lee, Kwang Kon Koh
The Korean Journal of Internal Medicine.2024; 39(2): 272. CrossRef - BMI-based metabolic syndrome severity score and arterial stiffness in a cohort Chinese study
Miao Wang, Chi Wang, Maoxiang Zhao, Shouling Wu, Hao Xue, Hongbin Liu
Nutrition, Metabolism and Cardiovascular Diseases.2024;[Epub] CrossRef - Omics biomarkers and an approach for their practical implementation to delineate health status for personalized nutrition strategies
Jaap Keijer, Xavier Escoté, Sebastià Galmés, Andreu Palou-March, Francisca Serra, Mona Adnan Aldubayan, Kristina Pigsborg, Faidon Magkos, Ella J. Baker, Philip C. Calder, Joanna Góralska, Urszula Razny, Malgorzata Malczewska-Malec, David Suñol, Mar Galofr
Critical Reviews in Food Science and Nutrition.2023; : 1. CrossRef - Development and validation of a continuous metabolic syndrome severity score in the Tehran Lipid and Glucose Study
Mohammadjavad Honarvar, Safdar Masoumi, Ladan Mehran, Davood Khalili, Atieh Amouzegar, Fereidoun Azizi
Scientific Reports.2023;[Epub] CrossRef - Associations of metabolic syndrome, its severity with cognitive impairment among hemodialysis patients
Yuqi Yang, Qian Li, Yanjun Long, Jing Yuan, Yan Zha
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Resistin serum levels and its association with clinical profile and carotid intima-media thickness in psoriasis: a cross-sectional study
Sofia Makishi Schlenker, Sofia Inez Munhoz, André Rochinski Busanello, Matheus Guedes Sanches, Barbara Stadler Kahlow, Renato Nisihara, Thelma Larocca Skare
Anais Brasileiros de Dermatologia.2023; 98(6): 799. CrossRef - Cholecystectomy Increases the Risk of Type 2 Diabetes in the Korean Population
Ji Hye Huh, Kyong Joo Lee, Yun Kyung Cho, Shinje Moon, Yoon Jung Kim, Eun Roh, Kyung-do Han, Dong Hee Koh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Annals of Surgery.2023; 278(2): e264. CrossRef - Cardiorespiratory Endurance is Associated with Metabolic Syndrome Severity in Men
V. V. Sverchkov, E. V. Bykov
Journal Biomed.2023; 19(2): 61. CrossRef - Effect of a Wearable Device–Based Physical Activity Intervention in North Korean Refugees: Pilot Randomized Controlled Trial
Ji Yoon Kim, Kyoung Jin Kim, Kyeong Jin Kim, Jimi Choi, Jinhee Seo, Jung-Been Lee, Jae Hyun Bae, Nam Hoon Kim, Hee Young Kim, Soo-Kyung Lee, Sin Gon Kim
Journal of Medical Internet Research.2023; 25: e45975. CrossRef - Independent association between age- and sex-specific metabolic syndrome severity score and cardiovascular disease and mortality
Mohammadjavad Honarvar, Ladan Mehran, Safdar Masoumi, Sadaf Agahi, Shayesteh Khalili, Fereidoun Azizi, Atieh Amouzegar
Scientific Reports.2023;[Epub] CrossRef - Optimal Low-Density Lipoprotein Cholesterol Levels in Adults Without Diabetes Mellitus: A Nationwide Population-Based Study Including More Than 4 Million Individuals From South Korea
Ji Hye Huh, Sang Wook Park, Tae-Hwa Go, Dae Ryong Kang, Sang-Hak Lee, Jang-Young Kim
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Triglyceride-Glucose Index for the Diagnosis of Metabolic Syndrome: A Cross-Sectional Study of 298,652 Individuals Receiving a Health Check-Up in China
Mingfei Jiang, Xiaoran Li, Huan Wu, Fan Su, Lei Cao, Xia Ren, Jian Hu, Grace Tatenda, Mingjia Cheng, Yufeng Wen, Hou De Zhou
International Journal of Endocrinology.2022; 2022: 1. CrossRef - Changes in body composition, body balance, metabolic parameters and eating behavior among overweight and obese women due to adherence to the Pilates exercise program
Hyun Ju Kim, Jihyun Park, Mi Ri Ha, Ye Jin Kim, Chaerin Kim, Oh Yoen Kim
Journal of Nutrition and Health.2022; 55(6): 642. CrossRef - Metabolic Syndrome Severity Score, Comparable to Serum Creatinine, Could Predict the Occurrence of End-Stage Kidney Disease in Patients with Antineutrophil Cytoplasmic Antibody-Associated Vasculitis
Pil Gyu Park, Jung Yoon Pyo, Sung Soo Ahn, Jason Jungsik Song, Yong-Beom Park, Ji Hye Huh, Sang-Won Lee
Journal of Clinical Medicine.2021; 10(24): 5744. CrossRef

 KDA
KDA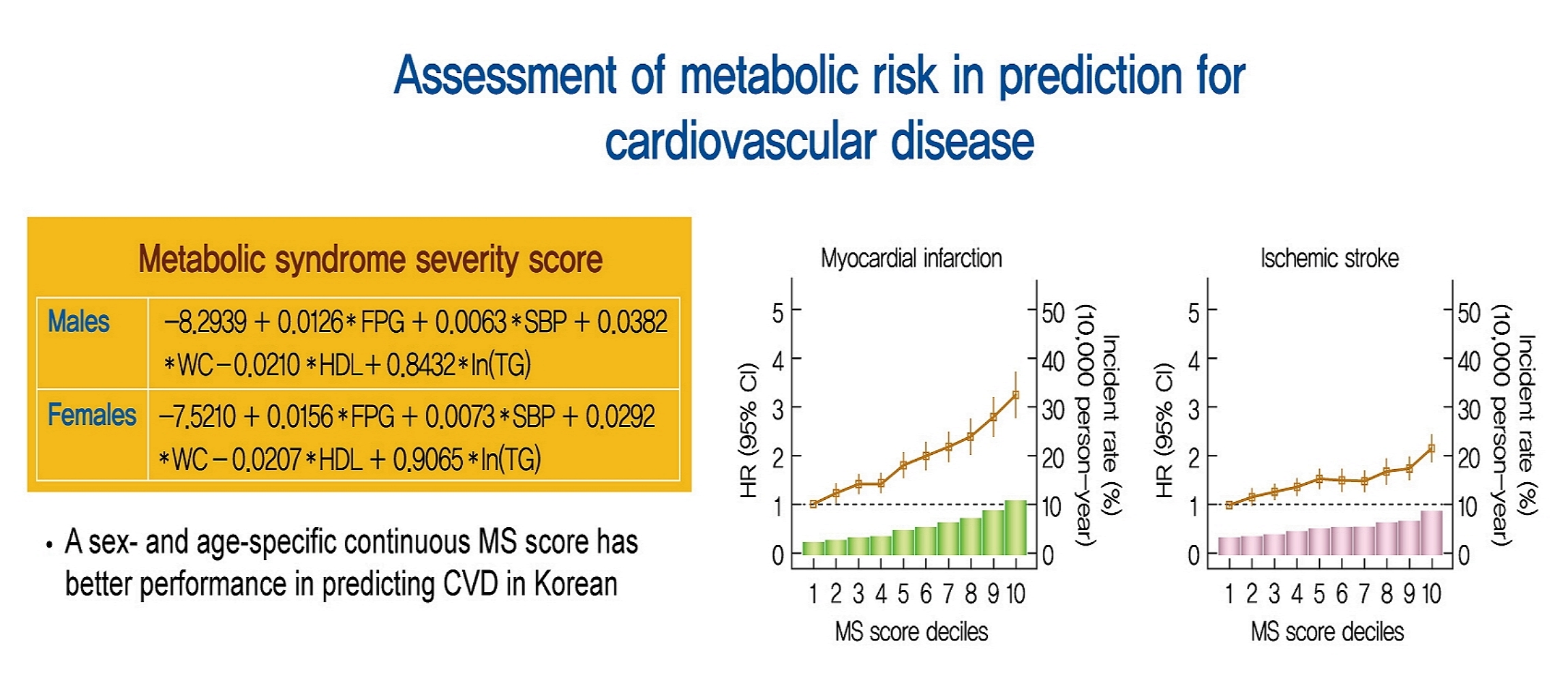
 PubReader
PubReader ePub Link
ePub Link Cite
Cite