Trends in the Incidence, Prevalence, and Mortality of End-Stage Kidney Disease in South Korea
Article information
Abstract
Knowledge of the epidemiologic characteristics of end-stage kidney disease (ESKD) patients is essential. The trends in the prevalence, incidence, and mortality rates of ESKD were analyzed retrospectively using the Korean National Health Insurance Service-National Sample Cohort database between 2006 and 2015. From 2006 to 2015, the incidence of ESKD decreased from 28.6 to 24.0 per 100,000 people and showed a decreasing pattern with or without diabetes mellitus. However, the incidence of those aged ≥75 years increased, as did the mean age at the onset of ESKD. From 2007 to 2015, the prevalence of ESKD increased in all age groups, but particularly in those aged ≥75 years. The prevalence of ESKD differed by sex and diabetes mellitus status and this gap widened over time. Mortality rates in ESKD patients remained relatively constant throughout the study period. However, mortality rates in ESKD without diabetes decreased over the same period.
INTRODUCTION
End-stage kidney disease (ESKD) is a global problem and its prevalence is increasing dramatically. An international comparison of ESKD epidemiology showed that Korea ranked fourth in the prevalence of ESKD and sixth in its incidence [1].
Type 2 diabetes mellitus (DM) is the leading causes of ESKD worldwide. The high prevalence of type 2 DM coincides with a high prevalence of diabetic kidney disease (DKD), as shown by data from the National Health and Nutrition Examination Survey [2]. This increase in prevalence of DKD is projected to lead to a significant increase in patients with ESKD requiring renal replacement therapy [3].
Trends in the prevalence and incidence of ESKD are important for health care policy and planning. Although data on patients with ESKD have been collected in the ESKD registry of the Korean Society of Nephrology since 1986 [4,5], this depends on voluntary reports and requires supplementation of unreported data. Therefore, this study evaluated the incidence, prevalence, and mortality of ESKD in a large nationwide population-based cohort in Korea and examined differences in the presence or absence of DM.
METHODS
Data source and study design
We conducted a retrospective population-based cohort study using the National Health Insurance Service–National Sample Cohort (NHIS–NSC) 2006 to 2015. The data comprise a nationally representative sample of 1,021,208 individuals, or approximately 2.2% of the Korean population in 2006. The database contains information on demographic characteristics and medical claims (including diagnostic and treatment codes). Detailed information on NHIS–NSC can be found elsewhere [6]. The study protocol was approved by the Institutional Review Board of Ajou University Hospital, Suwon, Korea (Approval no. AJIRB-MED-EXP-19-347); the requirement for informed consent was waived.
From this cohort, for each calendar year, we identified all individuals, aged ≥20 years, with a diagnosis of ESKD, defined using chronic kidney disease (CKD; International Classification of Disease, 10th edition code N18) or undergoing related procedures for more than 3 months with special exemption codes used in Korea at the same time (Supplementary Table 1).
Statistical analyses
For each calendar year, rates were expressed as crude and age-standardized rates per 100,000 individuals. The crude rate was calculated as the total number of incidence/prevalence/mortality cases divided by the population of that year. The agestandardized rates were directly age–sex standardized against the weighted distribution of the 2011 population across sexes and 5-year age groups from 20–24 to 85 years and above. Annual rates were also stratified by sex, age group, and DM status. All statistical analyses were performed using SAS version 9.4 (SAS Institute, Cary, NC, USA).
RESULTS
Trends in ESKD incidence
The age-and sex-standardized incidence of ESKD decreased slightly from 28.6 per 100,000 people in 2006 to 24.0 per 100,000 people in 2015. This overall decline was consistent across most age groups. However, there was an increase in incidence in the very elderly (≥75 years) that made a meaningful contribution to the overall burden (Fig. 1A, Supplementary Table 2). The mean age of incident ESKD patients at the initiation of dialysis was 56.3 years in 2006, but it increased to 65.3 years in 2015 (Supplementary Table 3). The incidence of ESKD with diabetes was also 13.8 times higher than the incidence of ESKD without DM in 2015. The incidence of ESKD with DM tended to decrease from 168.2 per 100,000 people in 2006 to 109.0 per 100,000 people in 2015, and the ESKD incidence without DM also decreased from 15.4 per 100,000 people in 2006 to 7.9 per 100,000 people in 2015 (Fig. 1C).
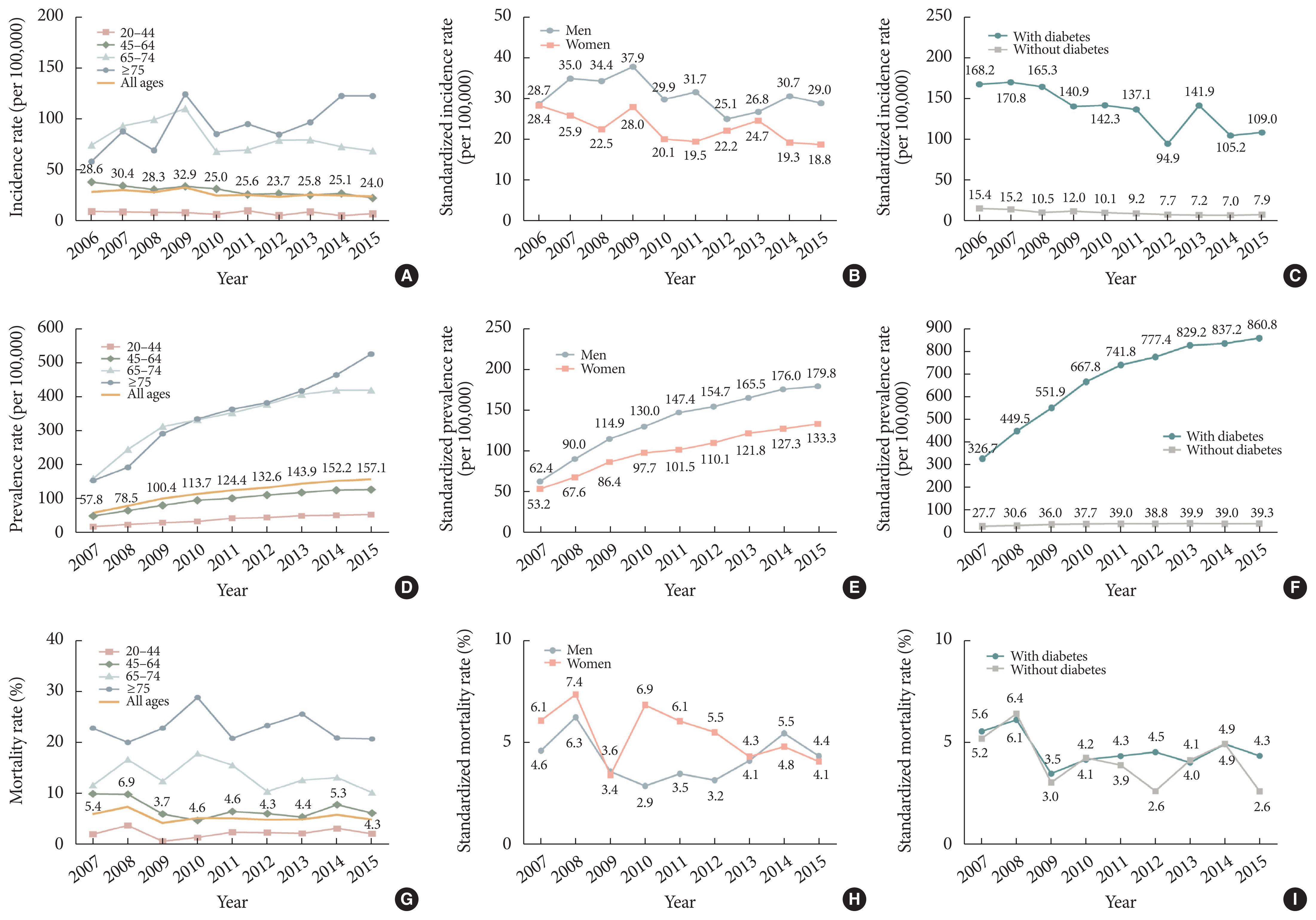
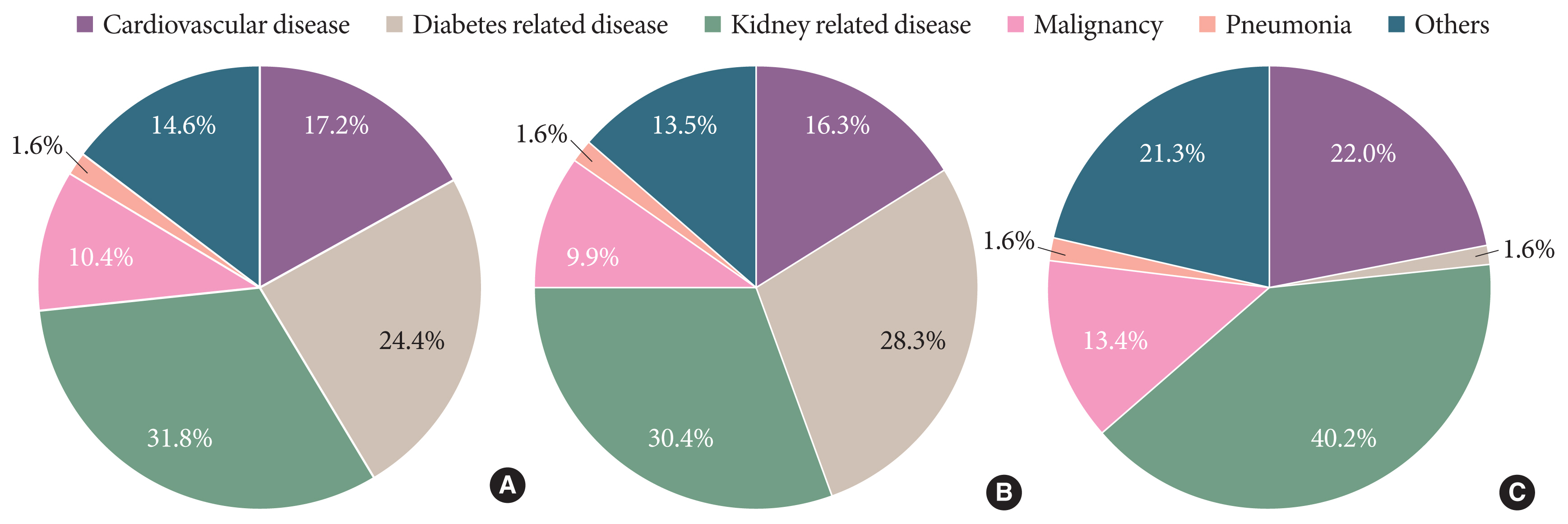
Incidence, prevalence, mortality rates of end-stage kidney disease in South Korea, 2006 to 2015 by age group, sex, and diabetes mellitus status. (A) Incidence rate by age group. (B) Incidence rate by sex. (C) Incidence rate by diabetes mellitus status. (D) Prevalence rate by age group. (E) Prevalence rate by sex. (F) Prevalence rate by diabetes mellitus status. (G) Mortality rate by age group. (H) Mortality rate by sex. (I) Mortality rate by diabetes mellitus status. (A, D, G) ‘All ages’ are shown as standardized values, and the remaining subdivided age groups are shown as crude values.
Trends in ESKD prevalence
The age-and sex-standardized ESKD prevalence increased steadily each year and was approximately 2.7-fold higher at 157.1 per 100,000 in 2015 than 57.8 per 100,000 in 2007. The prevalence in each age group also increased, particularly in the elderly (≥75 years) (3.4-fold) (Fig. 1D, Supplementary Table 2). The increases were greater in men than in women (Fig. 1E). The prevalence of ESKD with DM was higher than that of ESKD without DM, and the prevalence of ESKD with DM increased steeply each year. The prevalence of ESKD with DM increased progressively by 2.6-fold from 326.7 per 100,000 people in 2007 to 860.8 per 100,000 in 2015, and the prevalence of ESKD without DM increased 1.4-fold from 27.7 per 100,000 people in 2007 to 39.3 per 100,000 people in 2015 (Fig. 1F).
Trend in mortality of patients with ESKD
The mortality rate of patients with ESKD, standardized by age and sex, remained relatively stable during the study period, ranging from 5.4% in 2007 to 4.3% in 2015 (Fig. 1G, Supplementary Table 2). The differences in mortality rates between men and women was up to two to three times higher in men during 2010 to 2012, but was similar between 2013 and 2015 (Fig. 1H). The mortality rate of ESKD patients with DM did not change significantly during the study, from 5.6% in 2007 to 4.3% in 2015, while for ESKD patients without DM, the death rate tended to decrease from 5.2% in 2007 to 2.6% in 2015 (Fig. 1I).
During 2007 to 2015, the five leading causes of death in patients with ESKD accounted for 85.4% of all deaths and were kidney-related disease (31.8%), DM-related disease (24.4%), cardiovascular disease (17.2%), malignancy (10.4%), and pneumonia (1.6%) (Fig. 2).
DISCUSSION
This study examined the trends in the incidence, prevalence, and mortality rate of ESKD in Korea. The prevalence of ESKD has increased rapidly in the last decade, particularly in the elderly and patients with DM. The annual incidence of ESKD has increased slightly in the elderly but has decreased slightly in other age groups. This is the first study to investigate the epidemiology of ESKD in Korea using the nationwide NHIS-NHS claims database.
Annually increasing percentages of the aged and patients with DM were the main causes of increases in the ESKD prevalence in Korea (Fig. 1). With aging, the human kidney becomes much more vulnerable to some insults, which are already more prevalent in some patients, such as those with hypertension or DM [7,8]. Therefore, CKD is a substantial concern in the elderly. In Korea, the CKD prevalence was 30.3% in patients with DM aged ≥30 years and 39.0% in those aged ≥65 years [9]. In our study, the prevalence of ESKD with diabetes in 2015 was 865.24 per 100,000 in patients aged ≥20 years and 947.29 per 100,000 in those aged ≥65 years. In patients with diabetes aged ≥30 years, the prevalence of DKD increased from 8.4% to 12.4% between 2006 and 2015 (Supplementary Table 4).
ESKD incidence decreased slightly during the study period despite the increased prevalence. Possible reasons for the decline in ESKD incidence include improved management of risk factors for kidney failure (e.g., hypertension, glycated haemoglobin, and albuminuria) in diabetics or better treatment of kidney disease, including the use of angiotensin-converting enzyme inhibitors or angiotensin-receptor blockers, which slow the decline in kidney function in addition to lowering blood pressure, thereby delaying the onset of ESKD [10,11].
In, conclusion, from 2006 to 2015, the incidence of ESKD in Korea decreased slightly, while the prevalence of ESKD increased, particularly in diabetic and elderly patients. Given the large burden associated with ESKD, more effort is needed to prevent and treat ESKD.
Supplementary Information
Supplementary materials related to this article can be found online at https://doi.org/10.4093/dmj.2020.0156.
Notes
CONFLICTS OF INTEREST
No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS
Conception or design: D.J.K., I.P.
Acquisition, analysis, or interpretation of data: K.H.H.
Drafting the work or revising: M.J.L., K.H.H., D.J.K., I.P.
Final approval of the manuscript: M.J.L., K.H.H., D.J.K., I.P.
ACKNOWLEDGMENTS
This study was supported by research grants from the National Research Foundation of Korea (2019R1G1A1100671). The study sponsor had no role in study design, analysis, or interpretation of data.
This study used NHIS data (NHIS-2020-2-051) made by NHIS. The authors declare no conflict of interest with NHIS. The authors declare no conflict of interest with NHIS. Some of the data was released in October 2019 in the form of ‘Diabetes & Complications in Korea’ from the Korean Diabetes Association.
We would like to thank the Committee of Public Relation, Korean Diabetes Association for helping with the work.