
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 38(2); 2014 > Article
-
Original ArticleComplications Prevalence and Determinants of Diabetic Nephropathy in Korea: Korea National Health and Nutrition Examination Survey
- Jae Hee Ahn1, Ji Hee Yu1, Seung-Hyun Ko2, Hyuk-Sang Kwon2, Dae Jung Kim3, Jae Hyeon Kim4, Chul Sik Kim5, Kee-Ho Song6, Jong Chul Won7, Soo Lim8, Sung Hee Choi8, Kyungdo Han9, Bong-Yun Cha2, Nan Hee Kim1, Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association
-
Diabetes & Metabolism Journal 2014;38(2):109-119.
DOI: https://doi.org/10.4093/dmj.2014.38.2.109
Published online: April 18, 2014
1Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University College of Medicine, Ansan, Korea.
2Division of Endocrinology and Metabolism, Department of Internal Medicine, The Catholic University of Korea College of Medicine, Seoul, Korea.
3Department of Endocrinology and Metabolism, Ajou University School of Medicine, Suwon, Korea.
4Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
5Division of Endocrinology and Metabolism, Department of Internal Medicine, Hallym University Sacred Heart Hospital, Hallym University College of Medicine, Anyang, Korea.
6Department of Internal Medicine, Konkuk University School of Medicine, Seoul, Korea.
7Department of Internal Medicine, Mitochondrial Research Group, Inje University Sanggye Paik Hospital, Inje University College of Medicine, Seoul, Korea.
8Department of Internal Medicine, Seoul National University Bundang Hospital, Seoul National University College of Medicine, Seongnam, Korea.
9Department of Biostatistics, The Catholic University of Korea, Seoul, Korea.
- Corresponding author: Nan Hee Kim. Division of Endocrinology and Metabolism, Department of Internal Medicine, Korea University Ansan Hospital, Korea University College of Medicine, 123 Jeokgeum-ro, Danwon-gu, Ansan 425-707, Korea. nhkendo@gmail.com
Copyright © 2014 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Diabetic nephropathy is a leading cause of end stage renal disease and is associated with an increased risk of cardiovascular mortality. It manifests as albuminuria or impaired glomerular filtration rate (GFR), and the prevalence of diabetic nephropathy varies with ethnicity. The prevalence of diabetic nephropathy and its determinants in Korean adults have not previously been studied at the national level. This cross-sectional study was undertaken to ascertain the prevalence and determinants of albuminuria and chronic kidney disease (CKD) in Korean patients with diabetes.
-
Methods
- The Korea National Health and Nutrition Examination Survey (KNHANES) V, conducted in 2011, was used to define albuminuria (n=4,652), and the dataset of KNHANES IV-V (2008-2011) was used to define CKD (n=21,521). Selected samples were weighted to represent the entire civilian population in Korea. Albuminuria was defined as a spot urine albumin/creatinine ratio >30 mg/g. CKD was defined as a GFR <60 mL/min/1.73 m2.
-
Results
- Among subjects with diabetes, 26.7% had albuminuria, and 8.6% had CKD. Diabetes was associated with an approximate 2.5-fold increased risk of albuminuria, with virtually no difference between new-onset and previously diagnosed diabetes. Only systolic blood pressure was significantly associated with albuminuria, and old age, high serum triglyceride levels, and previous cardiovascular disease (CVD) were related with CKD in subjects with diabetes.
-
Conclusion
- Korean subjects with diabetes had a higher prevalence of albuminuria and CKD than those without diabetes. Blood pressure was associated with albuminuria, and age, triglyceride level, and previous CVD were independent determinants of CKD in subjects with diabetes.
- Diabetic nephropathy is the leading cause of end-stage renal disease [1] and is associated with an increased risk of cardiovascular mortality [2,3,4]. Approximately 40% of persons with diabetes develop diabetic nephropathy, which manifests as albuminuria or reduced glomerular filtration rate (GFR) [5,6]. However, the prevalence of albuminuria varies with ethnicity, with higher rates reported in Asian populations than in Caucasian populations [7,8]. In addition, the prevalence of and risk factors for chronic kidney disease (CKD) demonstrate significant interracial disparities [9,10].
- Several studies have reported the incidence and risk factors for diabetic nephropathy in Korean patients with diabetes. In a hospital-based study, Lee et al. [11] and Park et al. [12] reported that 34% of patients with diabetes had albuminuria and that poor glycemic control, high blood pressure, presence of diabetic retinopathy, and duration of diabetes were independently associated with albuminuria. Several studies have also investigated the risk factors for albuminuria, including male sex, hemoglobin A1c (HbA1c), homocysteine, body mass index (BMI), fasting insulin level, and fasting C-peptide level [13,14,15,16]. However, the majority of epidemiologic studies are small single center reports or primary clinic based studies, and did not compare subjects with or without diabetes.
- Recently, the prevalence of CKD in Korean adults in 2009 was reported to be 4.5% in men and 6.3% in women using data from the Korea National Health and Nutrition Examination Survey (KNHANES) IV [17]. However, the authors did not compare the prevalence of CKD by diabetes status, nor did they investigate the determinants of CKD. Furthermore, to the best of our knowledge, there have been no studies regarding albuminuria using data from KNHANES. Albuminuria was measured for the first time in the most recent version of KNHANES (2011); therefore, we were able to use this dataset to investigate the epidemiology of albuminuria, compared between subjects with or without diabetes.
- Therefore, the aim of the present study was to investigate the prevalence and determinants of albuminuria and CKD according to the presence or absence of diabetes using the nationally representative dataset from KNHANES.
INTRODUCTION
- Study population
- KNHANES is a cross-sectional, nationwide survey examining the general health and nutrition status of Korean people. We included subjects aged >30 years and excluded subjects with a missing random urine microalbumin level, fasting plasma glucose level, or previous medical history. Data from KNHANES V, which was conducted in 2011, was used to estimate the prevalence of albuminuria. As a result, the data from 4,652 subjects were used to analyze albuminuria status. The KNHANES IV-V dataset (2008-2011) was used to estimate the prevalence of CKD. Data from 21,521 subjects were used to analyze CKD status.
- Definition of diabetes and glucose tolerance categories
- Diabetes was defined using the following criteria: 1) new onset diabetes, fasting blood glucose ≥126 mg/dL or HbA1c ≥6.5% that was first detected in our survey; or 2) known diabetes, use of medication to decrease blood glucose levels at the time of the interview or self-report of a previous diagnosis by a physician. Impaired fasting glucose (IFG) was defined as fasting plasma glucose levels in the range 100 to 125 mg/dL.
- Definition of albuminuria and CKD
- Diabetic nephropathy was defined as diabetes with the presence of albuminuria or impaired GFR. In KNHANES V, which was conducted in 2011, urine albumin and creatinine concentrations were measured using single urine sampling. Urinary albumin was evaluated by turbidimetric assay using a Hitachi Automatic Analyzer 7600 (Hitachi, Tokyo, Japan). Albuminuria was defined as a spot urine albumin/creatinine ratio (ACR) ≥30 mg/g, and the albuminuria categories were as follows: microalbuminuria, ACR 30 to 299 mg/g and macroalbuminuria, ACR ≥300 mg/g. The level of kidney function was determined by estimating the GFR using an abbreviated equation developed from the Modification of Diet in Renal Disease (MDRD) formula: estimated GFR (mL/min/1.73 m2)=186.3×(serum creatinine-1.154)×(age-0.203)×0.742 (if female) [18]. We defined CKD as eGFR <60 mL/min/1.73 m2. The GFR categories were defined using the following criteria: stage 1, GFR ≥90 mL/min/1.73 m2; stage 2, GFR 60 to 89 mL/min/1.73 m2; stage 3, 30 to 59 mL/min/1.73 m2; stage 4, GFR 15 to 29 mL/min/1.73 m2; and stage 5, GFR <15 mL/min/1.73 m2.
- Other chronic diseases
- Hypertension was defined as the presence of either of the following two criteria: 1) systolic blood pressure (SBP) ≥140 mm Hg or diastolic blood pressure ≥90 mm Hg, or 2) use of an antihypertensive medication at the time of the interview. Dyslipidemia was defined as the presence of any of the following three criteria: 1) serum triglyceride ≥200 mg/dL after 12 hours of fasting, 2) serum total cholesterol ≥240 mg/dL, or 3) use of an antidyslipidemic medication at the time of the interview. Cardiovascular disease (CVD) history was self-reported and included a history of congestive heart failure, coronary heart disease, heart attack, angina, or stroke. Medication history was ascertained using the questionnaire.
- Health-related behavior
- The amount of pure alcohol consumed (g/day) was calculated using the average number of alcoholic beverages consumed and frequency of alcohol consumption. Respondents who drank >30 g/day were considered heavy drinkers. Regular exercise was defined as strenuous physical activity performed for ≥20 minutes at a time ≥3 times a week. A person was considered a smoker when they were currently smoking and had smoked >100 cigarettes in their lifetime.
- Statistical analysis
- All data are presented as mean±standard error (SE) for continuous variables or as proportion (SE) for categorical variables. Logarithmic transformation was used for variables with skewed distributions. Statistical analyses were performed using SAS statistical software version 9.3 (SAS Institute Inc., Cary, NC, USA) to reflect the complex sampling design and sampling weights of KNHANES and to provide nationally representative prevalence estimates using a complex sampling design. Differences were analyzed using chi-square tests for categorical variables and Student t-tests for the continuous variables. Determinants of albuminuria were analyzed using multivariate logistic regression analysis. The odds ratio (OR) and 95% confidence interval (95% CI) for the factors associated with the presence of albuminuria or CKD were calculated using multivariate logistic regression analysis. A P value <0.05 was considered statistically significant.
METHODS
- Clinical characteristics of the study population
- Table 1 shows the clinical characteristics of the study population. Of the 4,652 subjects, 660 had diabetes. The mean duration of diabetes was 5.1 years. Age, HbA1c level, fasting plasma glucose concentration, BMI, prevalence of hypertension, and prevalence of dyslipidemia were higher in the subjects with diabetes than in those without diabetes. The ACR was higher, and the GFR was lower, in patients with diabetes than in those without diabetes (geometric mean of ACR, 14.1±0.4 mg/g vs. 5.7±0.7 mg/g, P<0.0001; and GFR, 87.4±1.0 mL/min/1.73 m2 vs. 92.8±0.4 mL/min/1.73 m2, P<0.0001). Alcohol consumption, smoking, and exercise status were not different between the two groups.
- Prevalence and determinants of albuminuria according to the diabetes status
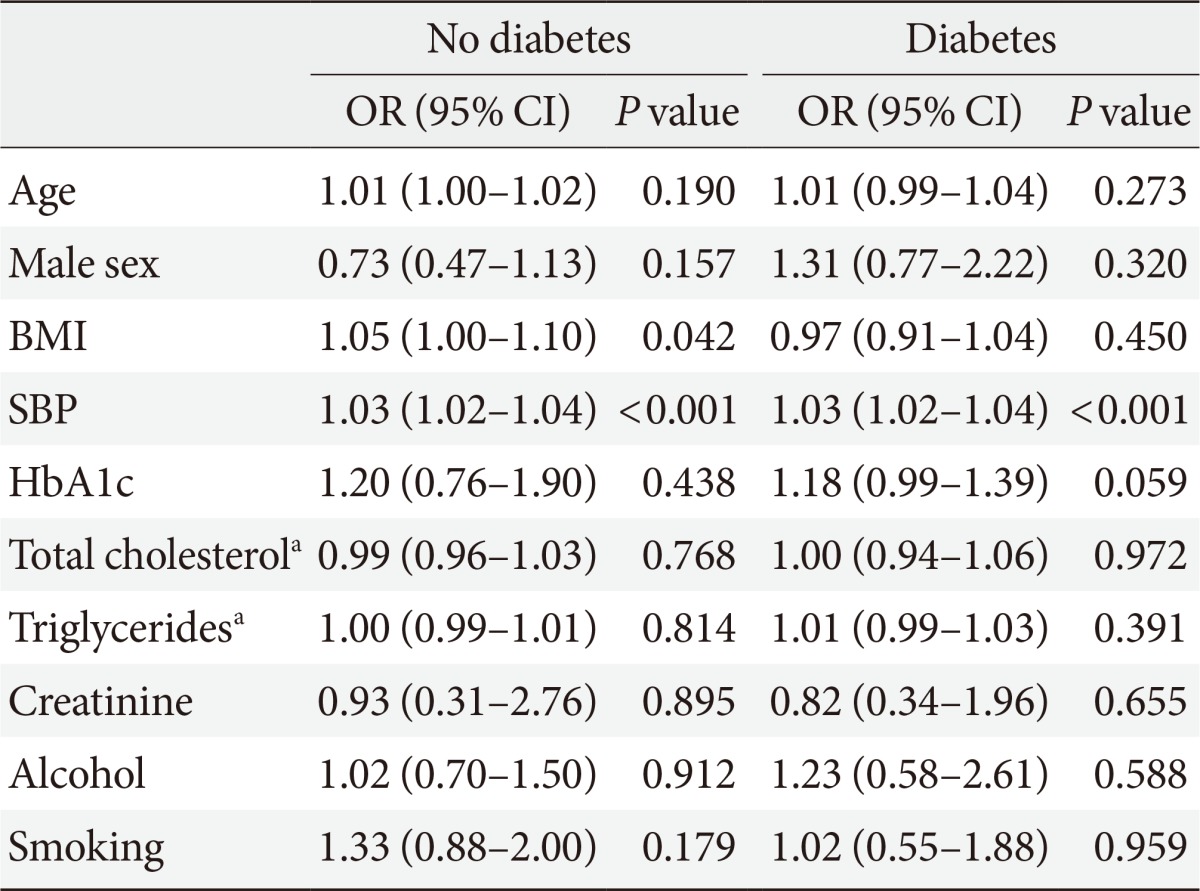
- Albuminuria was more prevalent in subjects with diabetes than in those without (26.7% vs. 10.2%, P<0.0001). The prevalence of microalbuminuria and macroalbuminuria was also higher in subjects with diabetes than in those without (22.0% vs. 9.4% and 4.6% vs. 0.8%, respectively) (Fig. 1). There was a significant trend for increased albuminuria with increasing age in subjects without diabetes (P for trend <0.0001), whereas the trend was not statistically significant in subjects with diabetes (P for trend=0.076) (Fig. 2). Table 2 shows the clinical characteristics of the study population according to the status of albuminuria and diabetes. In the group without diabetes, subjects with albuminuria were older and had higher BMI, waist circumference (WC), fasting plasma glucose concentration, and SBP than those without diabetes. However, in the group with diabetes, subjects with albuminuria had a higher fasting plasma glucose concentration and SBP. In multiple logistic regression analysis, in the nondiabetic group, BMI and SBP were independent risk factors for albuminuria, whereas, in the diabetic group, only SBP was independently associated with albuminuria (Table 3).
- Association between glucose tolerance categories and albuminuria
- In the logistic regression analysis to determine the impact of diabetes on albuminuria, subjects with diabetes had an increased risk of albuminuria, compared to those without diabetes (OR, 2.35; 95% CI, 1.78 to 3.10; P<0.0001) after adjusting for age, sex, BMI, SBP, exercise, smoking status, and alcohol consumption status. When we categorized the subjects into four groups according to glucose tolerance status and duration of diabetes (normal, IFG, new onset diabetes, and known diabetes), IFG, new onset diabetes, and known diabetes were significant risk factors for albuminuria after adjusting for age and sex (Table 4). However, with further adjustment for BMI and SBP, only new onset diabetes and known diabetes were significantly associated with albuminuria (Table 4).
- Prevalence and determinants of CKD according to diabetes status
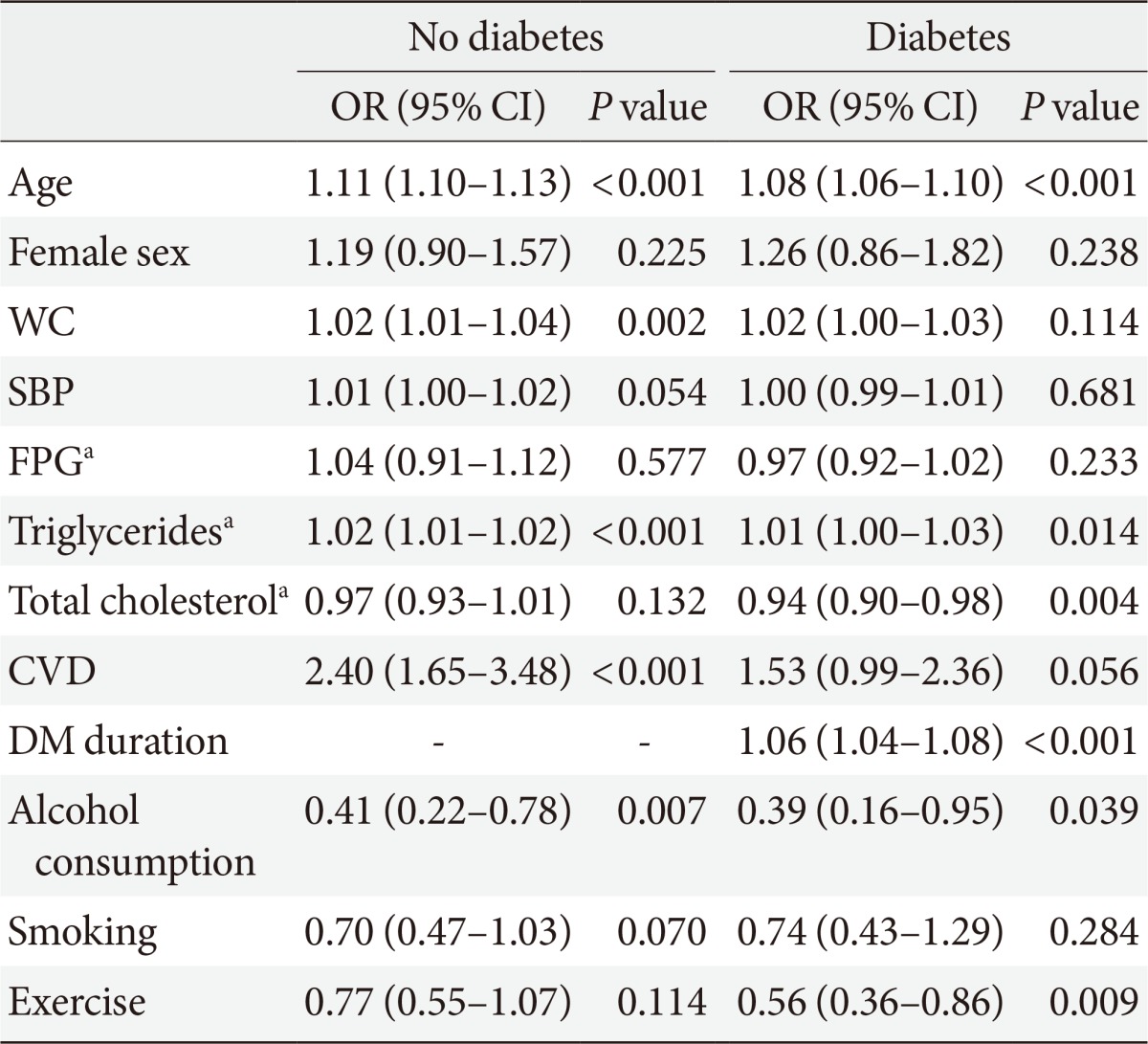
- Table 5 shows the clinical characteristics of the study population according to diabetes status and CKD. Of the 21,521 subjects, 2,436 had diabetes. In subjects without diabetes, 1.7% had CKD with a mean GFR of 51.5±0.6 mL/min/1.73 m2. In those with diabetes, 8.6% had CKD with a mean GFR of 48.1±1.0 mL/min/1.73 m2. Subjects with diabetes had a higher stage of CKD than those without diabetes (P<0.001) (Fig. 3). In both groups, with and without diabetes, the subjects with CKD were older and had a higher fasting plasma glucose level and higher rates of hypertension, dyslipidemia, and CVD than subjects without CKD. However, the percentage of alcohol consumers, smokers, and exercisers was lower in subjects with CKD than that in subjects without CKD in both groups (Table 5). In the multivariate logistic regression analysis, age, WC, triglyceride concentration, and previous CVD events were associated with an increased risk of CKD in the group without diabetes. In the group with diabetes, age, triglyceride concentration, and diabetes duration were risk factors for CKD. However, total cholesterol concentration, heavy alcohol consumption, and exercise were associated with a lower risk of CKD in the group with diabetes (Table 6).
- Association between glucose tolerance categories and CKD
- In the logistic regression analysis to determine the impact of diabetes on CKD, subjects with diabetes had an increased risk of CKD compared to those without diabetes (OR, 1.83; 95% CI, 1.13 to 2.96; P<0.0001) after adjusting for age, sex, BMI, SBP, exercise status, smoking status, and alcohol consumption status. When we categorized the subjects into three groups according to glucose tolerance status and diabetes duration (normal, IFG, and diabetes), IFG and diabetes were significant risk factors for CKD after adjusting for age, sex, BMI, SBP, exercise status, smoking status, and alcohol consumption status (Table 7).
RESULTS
- In this study, using the dataset from KNHANES, we demonstrated that the prevalences of microalbuminuria, macroalbuminuria, and CKD were 22.0%, 4.7%, and 8.6%, respectively, in Korean subjects with diabetes, which were significantly higher than in those without diabetes. In subjects with diabetes, only blood pressure was significantly associated with albuminuria, while older age, higher serum triglyceride levels, and previous CVD events were the determinants of CKD.
- In the United States, a study using data from the Third National Health and Nutrition Examination Survey (NHANES III), which was conducted between 1988 and 1994, reported that the prevalence of microalbuminuria and macroalbuminuria was 35% and 6%, respectively, in adults with type 2 diabetes aged ≥40 years [19]. In 930 subjects with diabetes in the Shanghai Diabetic Complications Study, the prevalence of microalbuminuria was 22.8% and that of macroalbuminuria was 3.4% [20], which were similar to those in the present study. Few studies have evaluated the epidemiology of albuminuria in Korea. The prevalence of albuminuria was 34% (20%, microalbuminuria; 14%, macroalbuminuria) in 631 Korean patients with type 2 diabetes in a single hospital in 1995 [11], and the duration of diabetes was longer than that in the present study. In a multicenter study conducted in a primary care setting, albuminuria was present in 29.4% (23.1%, microalbuminuria; 6.3%, macroalbuminuria) of 3,738 patients with type 2 diabetes and hypertension [16]. Because these two studies were conducted in a hospital or primary care clinic, the prevalence of albuminuria was higher than that in the present study. We believe the present study to be the first to report the prevalence of albuminuria using a nationally representative dataset in Korea, given the use of data from KHANES V, which was the first survey to measure albuminuria.
- Diabetes is considered to be a key risk factor for albuminuria. We also report here that diabetes was associated with an approximate 2.5-fold increased risk of albuminuria. There have been few previous studies investigating the association between prediabetes and albuminuria [21,22]. In our study, IFG was associated with an increased risk of albuminuria after adjusting for age and sex; however, the association was no longer significant after further adjustment for BMI and SBP, which are important risk factors for albuminuria. In a population-based cross-sectional study conducted with 1,791 Korean subjects aged >40 years in the Jungup district, the prevalence of microalbuminuria was higher in subjects with prediabetes than in those with normal glucose tolerance (11.8% vs. 6.0%, P<0.0001), and this relationship was consistent even in hypertensive individuals [23]. However, the authors did not adjust for other potential confounding factors for albuminuria.
- In our study, only SBP was an independent risk factor for albuminuria in subjects with diabetes. However, BMI was a significant risk factor for albuminuria in subjects without diabetes but not in those with diabetes. The positive association between BMI or WC and albuminuria has been reported in previous epidemiological studies [24,25]. In patients with diabetes in the Look AHEAD (Action for Health in Diabetes) Study, higher BMI and abdominal obesity (determined using WC) were found to be associated with albuminuria [26], where the majority of participants had a BMI ≥30 kg/m2. However, there has been some debate in this topic relating to subjects with diabetes. Lee et al. [27] reported that metabolic syndrome was an independent risk factor for albuminuria in 642 nonhypertensive Korean subjects with type 2 diabetes. However, of the various components of metabolic syndrome, abdominal obesity was not significantly related to microalbuminuria. Wentworth et al. [28] also reported that, in people with type 2 diabetes, there was a weaker correlation between BMI and albuminuria than in those without diabetes. We are not currently aware of the mechanism for this finding. BMI can be affected by diabetes treatment, the degree of hyperglycemia, and the insulin secretory capacity in diabetes. Therefore, the association between albuminuria and BMI could be attenuated by the diverse pathophysiology related to obesity in subjects with diabetes. Furthermore, the lower BMI values observed in the present study, than that in studies on Caucasians, may be responsible for the lack of association between albuminuria and BMI.
- Compared to previous studies with Korean patients with diabetes, which reported that male sex, poor glycemic control, high blood pressure, diabetes duration, presence of diabetic retinopathy, homocysteine levels, BMI, and fasting insulin level were associated with an increased risk of microalbuminuria [11,12,13,14,15,16], blood pressure was the only significant variable in the present study, and HbA1c was only a marginally significant determinant. To clarify the causal relationship between these variables, future longitudinal studies in this population are warranted.
- According to the present study conducted in Korea, the prevalence of CKD in subjects with diabetes was 8.6%, lower than in Western populations as well as other East Asian populations [29]. In the United States, the prevalence of CKD increased from 14.9% in NHANES 1988-1994 to 17.7% in NHANES 2005-2008 in patients with diabetes [30]. The prevalence of CKD in patients with type 2 diabetes in Asia was 10.2% in China [31] and 15.3% in Japan [32]. The differences between the two countries might be explained by the different ethnicities and MDRD equations. Following calculation of eGFR in the present study using the different MDRD equations, the prevalence of CKD was 6.8% using the Chinese equation [31] and 38.5% using the Japanese equation [32]. When Kang et al. [17] defined CKD as GFR <60 mL/min/1.73 m2 or proteinuria as ≥1+ using KNHANES IV, which was used in the present study, the prevalence of CKD was 4.5% in men and 6.3% in women among subjects with or without diabetes. However, they did not compare the prevalence of CKD by diabetes status. Therefore, this is the first study to ascertain the status of CKD in Korean subjects with diabetes on a national scale.
- In this study, older age, higher serum triglyceride levels, and longer diabetes duration were associated with an increased risk of CKD, whereas serum total cholesterol level, heavy alcohol drinking, and exercise were associated with a decreased risk of CKD in patients with diabetes. High serum triglyceride levels are considered a risk factor for diabetic nephropathy [33], and this was also true in our study. CKD induces hypertriglyceridemia through impaired clearance of triglyceride-rich lipoproteins [34]. However, we found a negative association between serum cholesterol and CKD, contrary to the findings of previous studies. The reason for this discrepancy is unknown. However, higher doses of lipid lowering medication may be responsible for the lower cholesterol levels in subjects with diabetes and CKD than that in those without CKD. In the previous study using KNHANES data, regular drinking (alcohol consumption ≥1/wk) may have been partly associated with the reduced rates of CKD in men, which is consistent with our study [17]. However, there have been reports that alcohol consumption could be a risk factor for diabetic nephropathy. In the AusDiab study, moderate-to-high alcohol consumption contributed to the development of albuminuria [22]. Subjects with diabetes and CKD in the present study may have led a healthier lifestyle, as evidenced by lower blood glucose and lipid levels, a greater use of medications for diabetes or dyslipidemia, and fewer smokers, although they exercised less. Therefore, the independent relationship between alcohol and CKD may be confounded by the awareness of the diabetes status in subjects with CKD, which led to a better lifestyle.
- Our study has some limitations. The cross-sectional design limits inferences about causality. Second, we could not exclude patients with conditions that could elevate urinary albumin excretion, such as hematuria, pregnancy, urinary tract infection, or other febrile illness, and we could not repeat the random urine sampling for the determination of albuminuria. Instead, the ACR measurement was based on a single random urine sample, not the first morning voided urine. Moreover, the epidemiology of diabetic nephropathy in type 1 diabetes differs from that of type 2 diabetes [35]; however, we could not determine the type of diabetes in our study. Last, we used the KNHANES IV-V dataset from 2008 to 2011 for the assessment of CKD prevalence to obtain a sufficient number of subjects with diabetes and CKD. However, HbA1c was not measured in all participants in KNHANES from 2007 to 2010; therefore, the prevalence of diabetes could be underestimated. Despite these potential limitations, this study has several strengths; for example, the data were based on a nationally representative population, and we adjusted for multiple risk factors in order to evaluate the determinants of diabetic nephropathy.
- In conclusion, Korean subjects with diabetes had a higher prevalence of albuminuria and CKD than those without diabetes. In subjects with diabetes, blood pressure was significantly associated with an increased risk of albuminuria, and older age, higher serum triglyceride levels, and a longer diabetes duration were determinants of CKD. To investigate the causal relationship between the risk factors and the development of albuminuria and CKD, future longitudinal follow-up studies are warranted.
DISCUSSION
- 1. Kidney Disease Improving Global Outcomes. KDIGO 2012 clinical practice guideline for the evaluation and management of chronic kidney disease. Chapter 1: definition and classification of CKD. Kidney Int Suppl 2013;3:19-62.
- 2. Valmadrid CT, Klein R, Moss SE, Klein BE. The risk of cardiovascular disease mortality associated with microalbuminuria and gross proteinuria in persons with older-onset diabetes mellitus. Arch Intern Med 2000;160:1093-1100. ArticlePubMed
- 3. Gerstein HC, Mann JF, Yi Q, Zinman B, Dinneen SF, Hoogwerf B, Halle JP, Young J, Rashkow A, Joyce C, Nawaz S, Yusuf S. HOPE Study Investigators. Albuminuria and risk of cardiovascular events, death, and heart failure in diabetic and nondiabetic individuals. JAMA 2001;286:421-426. ArticlePubMed
- 4. de Boer IH, Katz R, Cao JJ, Fried LF, Kestenbaum B, Mukamal K, Rifkin DE, Sarnak MJ, Shlipak MG, Siscovick DS. Cystatin C, albuminuria, and mortality among older adults with diabetes. Diabetes Care 2009;32:1833-1838. ArticlePubMedPMCPDF
- 5. Viberti GC, Hill RD, Jarrett RJ, Argyropoulos A, Mahmud U, Keen H. Microalbuminuria as a predictor of clinical nephropathy in insulin-dependent diabetes mellitus. Lancet 1982;1:1430-1432. ArticlePubMed
- 6. Eknoyan G, Hostetter T, Bakris GL, Hebert L, Levey AS, Parving HH, Steffes MW, Toto R. Proteinuria and other markers of chronic kidney disease: a position statement of the national kidney foundation (NKF) and the national institute of diabetes and digestive and kidney diseases (NIDDK). Am J Kidney Dis 2003;42:617-622. ArticlePubMed
- 7. Young BA, Katon WJ, Von Korff M, Simon GE, Lin EH, Ciechanowski PS, Bush T, Oliver M, Ludman EJ, Boyko EJ. Racial and ethnic differences in microalbuminuria prevalence in a diabetes population: the pathways study. J Am Soc Nephrol 2005;16:219-228. PubMed
- 8. Parving HH, Lewis JB, Ravid M, Remuzzi G, Hunsicker LG. DEMAND investigators. Prevalence and risk factors for microalbuminuria in a referred cohort of type II diabetic patients: a global perspective. Kidney Int 2006;69:2057-2063. ArticlePubMed
- 9. Buck K, Feehally J. Diabetes and renal failure in Indo-Asians in the UK: a paradigm for the study of disease susceptibility. Nephrol Dial Transplant 1997;12:1555-1557. ArticlePubMed
- 10. Hallan SI, Coresh J, Astor BC, Asberg A, Powe NR, Romundstad S, Hallan HA, Lydersen S, Holmen J. International comparison of the relationship of chronic kidney disease prevalence and ESRD risk. J Am Soc Nephrol 2006;17:2275-2284. ArticlePubMed
- 11. Lee KU, Park JY, Kim SW, Lee MH, Kim GS, Park SK, Park JS. Prevalence and associated features of albuminuria in Koreans with NIDDM. Diabetes Care 1995;18:793-799. ArticlePubMedPDF
- 12. Park JY, Kim HK, Chung YE, Kim SW, Hong SK, Lee KU. Incidence and determinants of microalbuminuria in Koreans with type 2 diabetes. Diabetes Care 1998;21:530-534. ArticlePubMedPDF
- 13. Kim ER, Sung KC, Chon CU, Kwon CH, Koh YL, Lee HJ, Park SK, Lee DY, Yun JH, Kim BJ, Kim BS, Kang JH, Lee MH, Park JR, Ryu SH. Prevalence and clinical characteristics of microalbuminuria in Koreans: a population-based cross-sectional study. Korean J Med 2006;70:617-626.
- 14. Kim DJ, Ryu SJ, Seo YJ, Kim NH, Chung HS, Eun CR, Choi HJ, Kim HS, Yang SJ, Park J, Yoo HJ, Park SY, Lee YJ, Ryu OH, Lee KW, Kim HY, Seo JA, Kim SG, Kim NH, Choi KM, Baik SH, Choi DS. The prevalence of microalbuminuria and associated factors in newly diagnosed type 2 diabetes mellitus in Korea. Korean J Med 2007;73:503-511.
- 15. Cho EH, Kim EH, Kim WG, Jeong EH, Koh EH, Lee WJ, Kim MS, Park JY, Lee KU. Homocysteine as a risk factor for development of microalbuminuria in type 2 diabetes. Korean Diabetes J 2010;34:200-206. ArticlePubMedPMC
- 16. Yang CW, Park JT, Kim YS, Kim YL, Lee YS, Oh YS, Kang SW. Prevalence of diabetic nephropathy in primary care type 2 diabetic patients with hypertension: data from the Korean Epidemiology Study on Hypertension III (KEY III study). Nephrol Dial Transplant 2011;26:3249-3255. ArticlePubMed
- 17. Kang HT, Lee J, Linton JA, Park BJ, Lee YJ. Trends in the prevalence of chronic kidney disease in Korean adults: the Korean National Health and Nutrition Examination Survey from 1998 to 2009. Nephrol Dial Transplant 2013;28:927-936. ArticlePubMed
- 18. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. Modification of Diet in Renal Disease Study Group. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Ann Intern Med 1999;130:461-470. ArticlePubMed
- 19. Kramer HJ, Nguyen QD, Curhan G, Hsu CY. Renal insufficiency in the absence of albuminuria and retinopathy among adults with type 2 diabetes mellitus. JAMA 2003;289:3273-3277. ArticlePubMed
- 20. Jia W, Gao X, Pang C, Hou X, Bao Y, Liu W, Wang W, Zuo Y, Gu H, Xiang K. Prevalence and risk factors of albuminuria and chronic kidney disease in Chinese population with type 2 diabetes and impaired glucose regulation: Shanghai diabetic complications study (SHDCS). Nephrol Dial Transplant 2009;24:3724-3731. ArticlePubMed
- 21. Nelson RG, Kunzelman CL, Pettitt DJ, Saad MF, Bennett PH, Knowler WC. Albuminuria in type 2 (non-insulin-dependent) diabetes mellitus and impaired glucose tolerance in Pima Indians. Diabetologia 1989;32:870-876. ArticlePubMedPDF
- 22. Tapp RJ, Shaw JE, Zimmet PZ, Balkau B, Chadban SJ, Tonkin AM, Welborn TA, Atkins RC. Albuminuria is evident in the early stages of diabetes onset: results from the Australian Diabetes, Obesity, and Lifestyle Study (AusDiab). Am J Kidney Dis 2004;44:792-798. ArticlePubMed
- 23. Kim YI, Chung YE, Kim JY, Kim SW, Kim ES, Lee MS, Park JY, Hong SK, Lee KU. Microalbuminuria in diabetic and non-diabetic subjects: a population based study. J Korean Diabetes Assoc 1999;23:79-86.
- 24. Bonnet F, Marre M, Halimi JM, Stengel B, Lange C, Laville M, Tichet J, Balkau B. DESIR Study Group. Waist circumference and the metabolic syndrome predict the development of elevated albuminuria in non-diabetic subjects: the DESIR Study. J Hypertens 2006;24:1157-1163. ArticlePubMed
- 25. Chandie Shaw PK, Berger SP, Mallat M, Frolich M, Dekker FW, Rabelink TJ. Central obesity is an independent risk factor for albuminuria in nondiabetic South Asian subjects. Diabetes Care 2007;30:1840-1844. ArticlePubMedPDF
- 26. Kramer H, Reboussin D, Bertoni AG, Marcovina S, Lipkin E, Greenway FL 3rd, Brancati FL. Look Ahead Research Group. Obesity and albuminuria among adults with type 2 diabetes: the Look AHEAD (Action for Health in Diabetes) Study. Diabetes Care 2009;32:851-853. PubMedPMC
- 27. Lee JE, Huh W, Son HJ, Kim YG, Kim DJ, Lee MK, Oh HY. Association of metabolic syndrome with microalbuminuria in non-hypertensive type 2 diabetic patients. Nephron Clin Pract 2007;106:c98-c103. ArticlePubMedPDF
- 28. Wentworth JM, Fourlanos S, Colman PG. Body mass index correlates with ischemic heart disease and albuminuria in long-standing type 2 diabetes. Diabetes Res Clin Pract 2012;97:57-62. ArticlePubMed
- 29. Lee SW, Kim YC, Oh SW, Koo HS, Na KY, Chae DW, Kim S, Chin HJ. Trends in the prevalence of chronic kidney disease, other chronic diseases and health-related behaviors in an adult Korean population: data from the Korean National Health and Nutrition Examination Survey (KNHANES). Nephrol Dial Transplant 2011;26:3975-3980. ArticlePubMed
- 30. de Boer IH, Rue TC, Hall YN, Heagerty PJ, Weiss NS, Himmelfarb J. Temporal trends in the prevalence of diabetic kidney disease in the United States. JAMA 2011;305:2532-2539. ArticlePubMedPMC
- 31. Chen W, Chen W, Wang H, Dong X, Liu Q, Mao H, Tan J, Lin J, Zhou F, Luo N, He H, Johnson RJ, Zhou SF, Yu X. Prevalence and risk factors associated with chronic kidney disease in an adult population from southern China. Nephrol Dial Transplant 2009;24:1205-1212. ArticlePubMed
- 32. Yokoyama H, Sone H, Oishi M, Kawai K, Fukumoto Y, Kobayashi M. Japan Diabetes Clinical Data Management Study Group. Prevalence of albuminuria and renal insufficiency and associated clinical factors in type 2 diabetes: the Japan Diabetes Clinical Data Management study (JDDM15). Nephrol Dial Transplant 2009;24:1212-1219. ArticlePubMed
- 33. Mulec H, Johnsen SA, Wiklund O, Bjorck S. Cholesterol: a renal risk factor in diabetic nephropathy? Am J Kidney Dis 1993;22:196-201. ArticlePubMed
- 34. Vaziri ND, Moradi H. Mechanisms of dyslipidemia of chronic renal failure. Hemodial Int 2006;10:1-7. ArticlePubMed
- 35. Reutens AT. Epidemiology of diabetic kidney disease. Med Clin North Am 2013;97:1-18. ArticlePubMed
REFERENCES
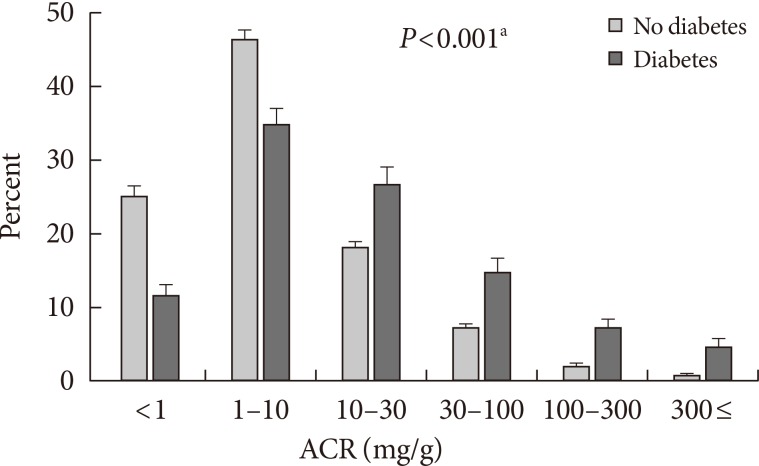

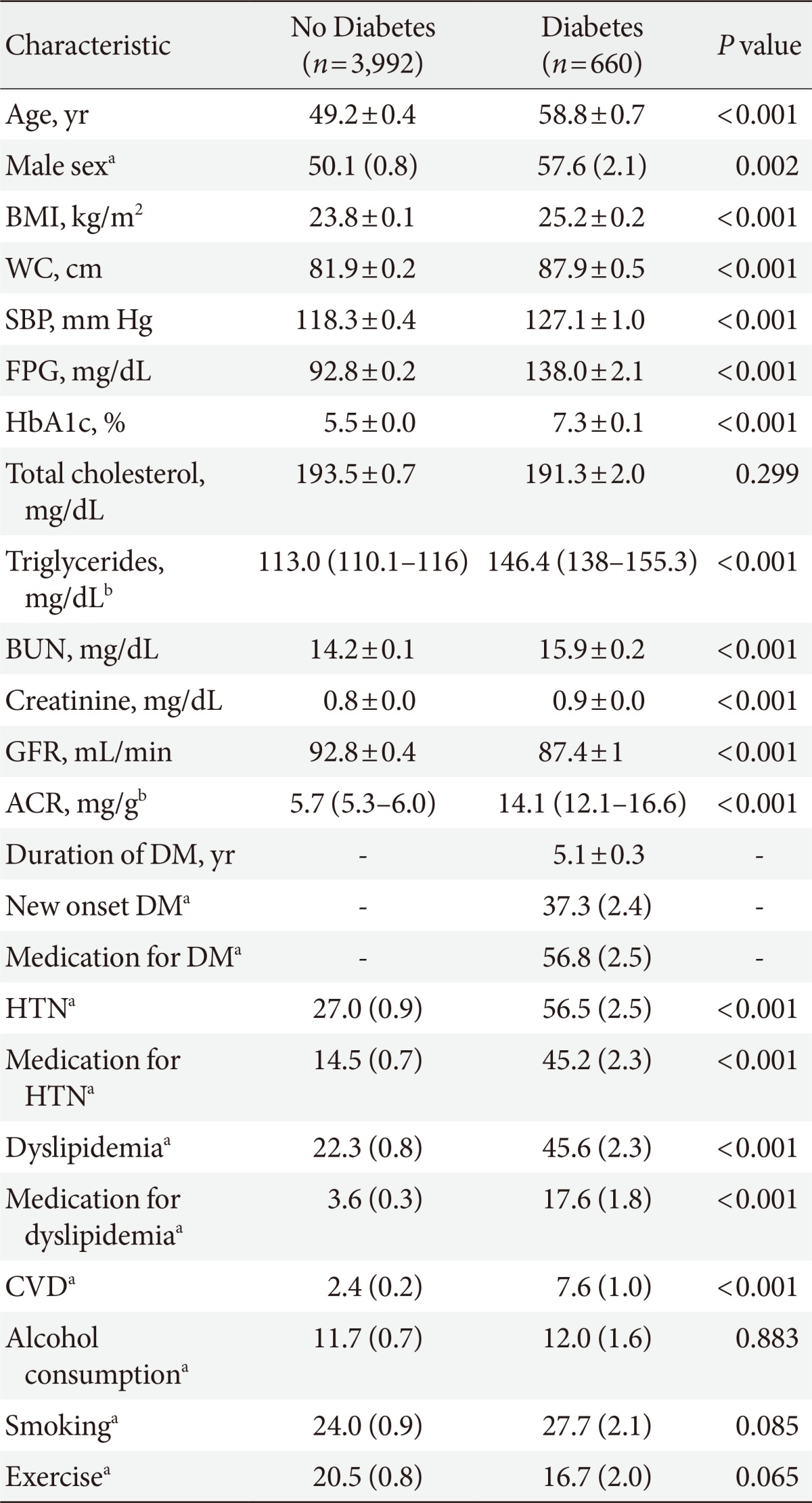
Values are presented as mean±standard error. BMI was defined as body mass (kg) divided by the square of height (m2).
BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; FPG, fasting plasma glucose; HbA1c, hemoglobin A1c; BUN, blood urea nitrogen; GFR, glomerular filtration rate; ACR, albumin creatinine ratio; DM, diabetes mellitus; HTN, hypertension; CVD, cardiovascular disease.
aValues are presented as % (standard error), bACR and triglyceride levels are presented as geometric mean (95% confidence interval).

Values are presented as mean±standard error. BMI was defined as body mass (kg) divided by the square of height (m2).
BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; FPG, fasting plasma glucose; HbA1c, hemoglobin A1c; BUN, blood urea nitrogen; GFR, glomerular filtration rate; ACR, albumin creatinine ratio; DM, diabetes mellitus; HTN, hypertension; CVD, cardiovascular disease.
aValues are presented as % (standard error), bACR and triglyceride levels are presented as geometric mean (95% confidence interval).
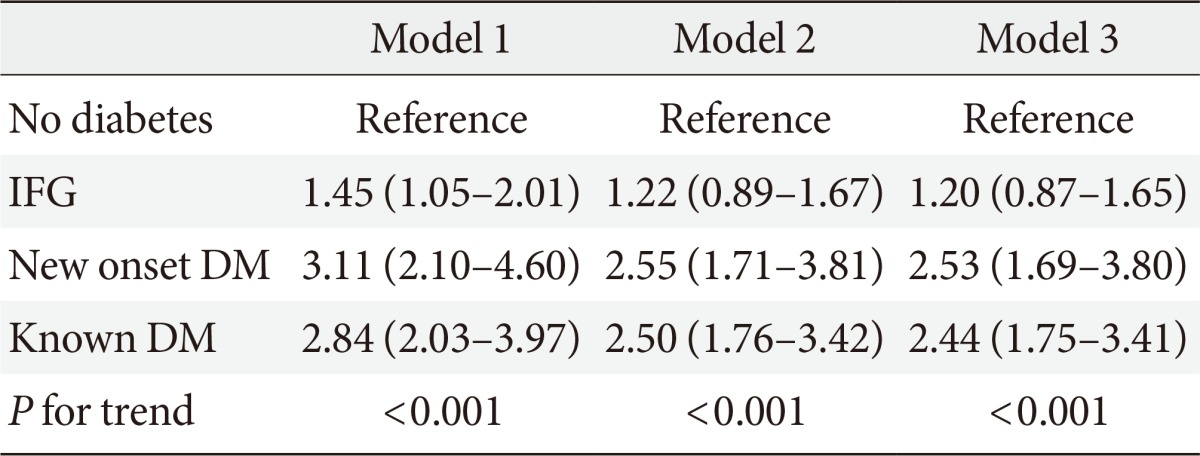
Values are presented as the odds ratio (95% confidence interval). Model 1: adjusted for age and sex; Model 2: adjusted for age, sex, body mass index (BMI), and systolic blood pressure (SBP); Model 3: adjusted for age, sex, BMI, SBP, exercise, drinking, and smoking.
IFG, impaired fasting glucose; DM, diabetes mellitus.

Values are presented as mean±standard error. BMI was defined as body mass (kg) divided by the square of height (m2).
CKD, chronic kidney disease; BMI, body mass index; WC, waist circumference; SBP, systolic blood pressure; FPG, fasting plasma glucose; HbA1c, hemoglobin A1c; BUN, blood urea nitrogen; GFR, glomerular filtration rate; DM, diabetes mellitus; HTN, hypertension; CVD, cardiovascular disease.
aValues are presented as % (standard error), bTriglyceride levels are presented as geometric mean (95% confidence interval).
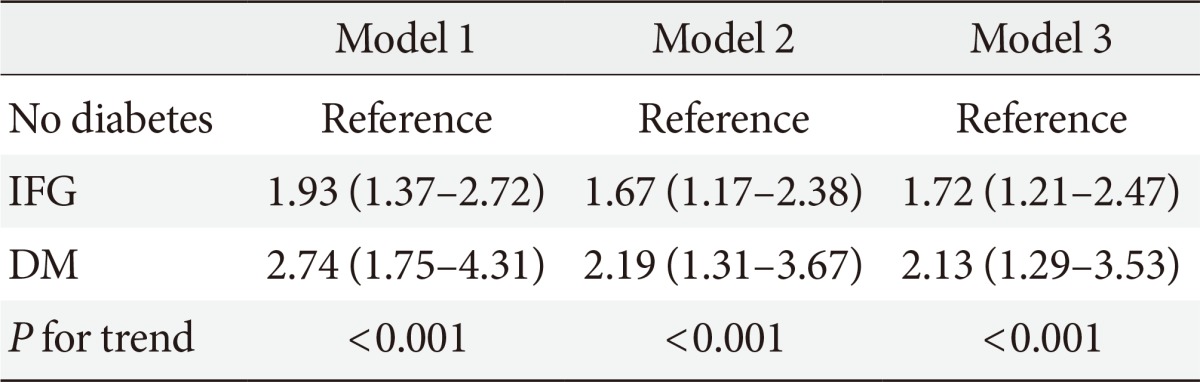
Values are presented as the odds ratio (95% confidence interval).
Model 1: adjusted for age and sex; Model 2: adjusted for age, sex, body mass index (BMI), and systolic blood pressure (SBP); Model 3: adjusted for age, sex, BMI, SBP, exercise, drinking, and smoking.
IFG, impaired fasting glucose; DM, diabetes mellitus.
Figure & Data
References
Citations

- Associations between dietary patterns and renal impairment in individuals with diabetes: a cross‐sectional study
Ziling Ding, Xingzhe Wu, Chao Liu, Ruixue Ying, Yi Zhang, Shiqi Zhang, Qiu Zhang, Honglin Hu, Fang Dai
Journal of Human Nutrition and Dietetics.2024; 37(1): 193. CrossRef - Determinants of diabetic nephropathy among adult diabetic patients on follow-up at public hospitals in Addis Ababa, Ethiopia: A case-control study
Diriba Etana Tola, Zenebu Begna Bayissa, Tamene Abera Desissa, Lencho Kajela Solbana, Azeb Haile Tesfaye, Bikila Fufa Eba
SAGE Open Medicine.2024;[Epub] CrossRef - Kidney Health Plan 2033 in Korea: bridging the gap between the present and the future
Do Hyoung Kim, Young Youl Hyun, Jin Joo Cha, Sua Lee, Hyun Kyung Lee, Jong Wook Choi, Su-Hyun Kim, Sang Youb Han, Cheol Whee Park, Eun Young Lee, Dae Ryong Cha, Sung Gyun Kim, Chun Soo Lim, Sun-Hee Park
Kidney Research and Clinical Practice.2024; 43(1): 8. CrossRef - Risk Factors of Microalbuminuria among Patients with Type 2 Diabetes Mellitus in Korea: A Cross-Sectional Study Based on 2019–2020 Korea National Health and Nutrition Examination Survey Data
Eun Sook Bae, Jung Yi Hur, Hyung Soon Jang, Jeong Suk Kim, Hye Seung Kang
International Journal of Environmental Research and Public Health.2023; 20(5): 4169. CrossRef - CORRELATION OF VASCULAR ENDOTHELIAL FUNCTION AND INFLAMMATORY FACTORS WITH RENAL FUNCTION IN PATIENTS WITH DIABETIC NEPHROPATHY
A. Y. Mammadzada, Sh. G. Ismayilova, Sh. S. Ibrahimova, N. I. Huseynova, L. A. Huseyn
World of Medicine and Biology.2023; 19(85): 129. CrossRef - Synopsis of the Korean Society of Nephrology 2023 Practical Recommendations for the Management of Diabetic Kidney Disease
Sungjin Chung
The Korean Journal of Medicine.2023; 98(6): 270. CrossRef - 3-Hydroxybutyrate Ameliorates the Progression of Diabetic Nephropathy
Jeeyoun Jung, Woo Yeong Park, Yun Jin Kim, Mikyung Kim, Misun Choe, Kyubok Jin, Ji Hae Seo, Eunyoung Ha
Antioxidants.2022; 11(2): 381. CrossRef - Development and Validation of a Model That Predicts the Risk of Diabetic Nephropathy in Type 2 Diabetes Mellitus Patients: A Cross-Sectional Study
Jing Yang, Sheng Jiang
International Journal of General Medicine.2022; Volume 15: 5089. CrossRef - Renoprotective Mechanism of Sodium-Glucose Cotransporter 2 Inhibitors: Focusing on Renal Hemodynamics
Nam Hoon Kim, Nan Hee Kim
Diabetes & Metabolism Journal.2022; 46(4): 543. CrossRef - Development and assessment of diabetic nephropathy prediction model using hub genes identified by weighted correlation network analysis
Xuelian Zhang, Yao Wang, Zhaojun Yang, Xiaoping Chen, Jinping Zhang, Xin Wang, Xian Jin, Lili Wu, Xiaoyan Xing, Wenying Yang, Bo Zhang
Aging.2022; 14(19): 8095. CrossRef - Neutrophil–lymphocyte ratio as an inflammatory biomarker of diabetic nephropathy among type 2 diabetes mellitus patients: A comparative cross-sectional study
Mesfin Zewude Gurmu, Solomon Genet, Solomon Tebeje Gizaw, Teka Obsa Feyisa, Natesan Gnanasekaran
SAGE Open Medicine.2022; 10: 205031212211402. CrossRef - Did Sejong the Great have ankylosing spondylitis? The oldest documented case of ankylosing spondylitis
JiHwan Lee
International Journal of Rheumatic Diseases.2021; 24(2): 203. CrossRef - Protective effects of klotho on palmitate-induced podocyte injury in diabetic nephropathy
Jeong Suk Kang, Seung Seob Son, Ji-Hye Lee, Seong Woo Lee, Ah Reum Jeong, Eun Soo Lee, Seung-Kuy Cha, Choon Hee Chung, Eun Young Lee, Partha Mukhopadhyay
PLOS ONE.2021; 16(4): e0250666. CrossRef - Nomogram for the prediction of diabetic nephropathy risk among patients with type 2 diabetes mellitus based on a questionnaire and biochemical indicators: a retrospective study
Yuhong Hu, Rong Shi, Ruohui Mo, Fan Hu
Aging.2020; 12(11): 10317. CrossRef - Differential Urinary Proteome Analysis for Predicting Prognosis in Type 2 Diabetes Patients with and without Renal Dysfunction
Hee-Sung Ahn, Jong Ho Kim, Hwangkyo Jeong, Jiyoung Yu, Jeonghun Yeom, Sang Heon Song, Sang Soo Kim, In Joo Kim, Kyunggon Kim
International Journal of Molecular Sciences.2020; 21(12): 4236. CrossRef - Urine E-cadherin: A Marker for Early Detection of Kidney Injury in Diabetic Patients
Michael Koziolek, Gerhard A. Mueller, Gry H. Dihazi, Klaus Jung, Constanze Altubar, Manuel Wallbach, Ivana Markovic, Dirk Raddatz, Olaf Jahn, Hülya Karaköse, Christof Lenz, Henning Urlaub, Abdelhi Dihazi, Abdellatif El El Meziane, Hassan Dihazi
Journal of Clinical Medicine.2020; 9(3): 639. CrossRef - Study of serum pentraxin 3 level in patients with diabetic nephropathy
Alaaeldin Abdelsalam Dawood, Mai Ashraf Kamel, Thoria Ahmed Omar, Ahmed Ahmed Mohammed Agaba
The Egyptian Journal of Internal Medicine.2020;[Epub] CrossRef - Limitations of Deep Learning Attention Mechanisms in Clinical Research: Empirical Case Study Based on the Korean Diabetic Disease Setting
Junetae Kim, Sangwon Lee, Eugene Hwang, Kwang Sun Ryu, Hanseok Jeong, Jae Wook Lee, Yul Hwangbo, Kui Son Choi, Hyo Soung Cha
Journal of Medical Internet Research.2020; 22(12): e18418. CrossRef - Long-term effects of various types of 3-hydroxy-3-methylglutaryl coenzyme A reductase inhibitors on changes in glomerular filtration rate in Korea
Seo Yeon Baik, Hyunah Kim, So Jung Yang, Tong Min Kim, Seung-Hwan Lee, Jae Hyoung Cho, Hyunyong Lee, Hyeon Woo Yim, Kun-Ho Yoon, Hun-Sung Kim
Frontiers of Medicine.2019; 13(6): 713. CrossRef - Plasma endoglin in Type2 diabetic patients with nephropathy
Ahmed S. Doghish, Atef A. Bassyouni, Mohamed H. Mahfouz, Heba G. Abd El-Aziz, Rania Y. Zakaria
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2019; 13(1): 764. CrossRef - Cigarette smoking as a risk factor for diabetic nephropathy: A systematic review and meta-analysis of prospective cohort studies
Dan Liao, Liang Ma, Jing Liu, Ping Fu, Noël C. Barengo
PLOS ONE.2019; 14(2): e0210213. CrossRef - Risk factors for diabetic nephropathy complications in community patients with type 2 diabetes mellitus in Shanghai: Logistic regression and classification tree model analysis
Jieqiong Lou, Limei Jing, Hui Yang, Fei Qin, Wen Long, Rong Shi
The International Journal of Health Planning and Management.2019; 34(3): 1013. CrossRef - Predictive Factors for Efficacy of AST-120 Treatment in Diabetic Nephropathy: a Prospective Single-Arm, Open-Label, Multi-Center Study
You-Cheol Hwang, Se Won Kim, Kyu Yeon Hur, Bong-Soo Cha, In Joo Kim, Tae Sun Park, Sei Hyun Baik, Kun Ho Yoon, Kwan Woo Lee, In Kyu Lee, Moon-Kyu Lee
Journal of Korean Medical Science.2019;[Epub] CrossRef - Glycated Albumin Is a More Useful Glycation Index than HbA1c for Reflecting Renal Tubulopathy in Subjects with Early Diabetic Kidney Disease
Ji Hye Huh, Minyoung Lee, So Young Park, Jae Hyeon Kim, Byung-Wan Lee
Diabetes & Metabolism Journal.2018; 42(3): 215. CrossRef - Meta‑analysis of the benefit of sitagliptin treatment in patients with type 2 diabetes complicated with incipient nephropathy
Wei Liu, Jiangyi Yu, Qianhua Yan, Lijuan Wang, Nan Li, Wei Xiong
Experimental and Therapeutic Medicine.2018;[Epub] CrossRef - MicroRNA‐326‐3p ameliorates high glucose and ox‐LDL‐IC‐ induced fibrotic injury in renal mesangial cells by targeting FcγRIII
Yiting Wang, Rui Zhang, Junlin Zhang, Fang Liu
Nephrology.2018; 23(11): 1031. CrossRef - The Global Epidemiology of Diabetes and Kidney Disease
Digsu N. Koye, Dianna J. Magliano, Robert G. Nelson, Meda E. Pavkov
Advances in Chronic Kidney Disease.2018; 25(2): 121. CrossRef - Evaluation of the association between the number of natural teeth and anemia among Korean adults using nationally representative data
Kyungdo Han, Jun‐Beom Park
Journal of Periodontology.2018; 89(10): 1184. CrossRef - Correlation of vascular endothelial function and coagulation factors with renal function and inflammatory factors in patients with diabetic nephropathy
Jie Sun, Caiyan Liu
Experimental and Therapeutic Medicine.2018;[Epub] CrossRef - Cigarette smoking and risk of albuminuria in patients with type 2 diabetes: a systematic review and meta-analysis of observational studies
Haili Xu, Jinliu Suo, Jing Lian
International Urology and Nephrology.2018; 50(5): 911. CrossRef - Diabetes Fact Sheet in Korea, 2016: An Appraisal of Current Status
Jong Chul Won, Jae Hyuk Lee, Jae Hyeon Kim, Eun Seok Kang, Kyu Chang Won, Dae Jung Kim, Moon-Kyu Lee
Diabetes & Metabolism Journal.2018; 42(5): 415. CrossRef - Association between the number of natural teeth and diabetic retinopathy among type 2 diabetes mellitus
Su Jeong Song, Kyungdo Han, Seong-su Lee, Jun-Beom Park
Medicine.2017; 96(47): e8694. CrossRef - Arterial Stiffness Is More Associated with Albuminuria than Decreased Glomerular Filtration Rate in Patients with Type 2 Diabetes Mellitus: The REBOUND Study
Jong Ho Kim, Sang Soo Kim, In Joo Kim, Bo Hyun Kim, Ja Young Park, Chang Won Lee, Ji Hye Suk, Sun Hae Shin, Sung Pyo Son, Min Chul Kim, Jun Hyeob Ahn, Kwang Jae Lee, Min Jung Kwon, Soon Hee Lee, Jeong Hyun Park
Journal of Diabetes Research.2017; 2017: 1. CrossRef - Determinants of diabetic nephropathy in Ayder Referral Hospital, Northern Ethiopia: A case-control study
Solomon Hintsa, Lamessa Dube, Mebrahtu Abay, Teklit Angesom, Abdulhalik Workicho, Petter Bjornstad
PLOS ONE.2017; 12(4): e0173566. CrossRef - Comparison between Atorvastatin and Rosuvastatin in Renal Function Decline among Patients with Diabetes
Eugene Han, Gyuri Kim, Ji-Yeon Lee, Yong-ho Lee, Beom Seok Kim, Byung-Wan Lee, Bong-Soo Cha, Eun Seok Kang
Endocrinology and Metabolism.2017; 32(2): 274. CrossRef - Association between underweight and tooth loss among Korean adults
In-Seok Song, Kyungdo Han, Jae-Jun Ryu, Jun-Beom Park
Scientific Reports.2017;[Epub] CrossRef - Variability in glycated albumin levels predicts the progression of diabetic nephropathy
Su Bin Park, Sang Soo Kim, In Joo Kim, Yoon Jeong Nam, Kang Hee Ahn, Jong Ho Kim, Yun Kyung Jeon, Bo Hyun Kim, Sang Heon Song, Ihm Soo Kwak, Eun Kyung Lee, Yong Ki Kim
Journal of Diabetes and its Complications.2017; 31(6): 1041. CrossRef - Low serum bilirubin level predicts the development of chronic kidney disease in patients with type 2 diabetes mellitus
Kang Hee Ahn, Sang Soo Kim, Won Jin Kim, Jong Ho Kim, Yun Jeong Nam, Su Bin Park, Yun Kyung Jeon, Bo Hyun Kim, In Joo Kim, Yong Ki Kim
The Korean Journal of Internal Medicine.2017; 32(5): 875. CrossRef - Periodontitis is associated with diabetic retinopathy in non-obese adults
Su Jeong Song, Seong-su Lee, Kyungdo Han, Jun-Beom Park
Endocrine.2017; 56(1): 82. CrossRef - Baseline Cardiovascular Characteristics of Adult Patients with Chronic Kidney Disease from the KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD)
Hyoungnae Kim, Tae-Hyun Yoo, Kyu Hun Choi, Kook-Hwan Oh, Joongyub Lee, Soo Wan Kim, Tae Hee Kim, Suah Sung, Seung Hyeok Han
Journal of Korean Medical Science.2017; 32(2): 231. CrossRef - Addition of nonalbumin proteinuria to albuminuria improves prediction of type 2 diabetic nephropathy progression
Jong Ho Kim, Seo Young Oh, Eun Heui Kim, Min Jin Lee, Yun Kyung Jeon, Bo Hyun Kim, Jin Mi Kim, Yong Ki Kim, Sang Soo Kim, In Joo Kim
Diabetology & Metabolic Syndrome.2017;[Epub] CrossRef - Smoking and the risk of diabetic nephropathy in patients with type 1 and type 2 diabetes: a meta-analysis of observational studies
Ning Jiang, Feng Huang, Xiurong Zhang
Oncotarget.2017; 8(54): 93209. CrossRef - Treatment of diabetic kidney disease: current and future targets
Mi-Kyung Kim
The Korean Journal of Internal Medicine.2017; 32(4): 622. CrossRef - Analysis and comparison of the cost-effectiveness of statins according to the baseline low-density lipoprotein cholesterol level in Korea
Y. J. Jeong, H. Kim, S. J. Baik, T. M. Kim, S. J. Yang, S.-H. Lee, J.-H. Cho, H. Lee, H. W. Yim, I. Y. Choi, K.-H. Yoon, H.-S. Kim
Journal of Clinical Pharmacy and Therapeutics.2017; 42(3): 292. CrossRef - Mechanistic Insight and Management of Diabetic Nephropathy: Recent Progress and Future Perspective
Rui Xue, Dingkun Gui, Liyang Zheng, Ruonan Zhai, Feng Wang, Niansong Wang
Journal of Diabetes Research.2017; 2017: 1. CrossRef - Nonalbuminuric Renal Insufficiency: Can It Be a Novel Category of Diabetic Nephropathy?
Masami Tanaka, Hiroshi Itoh
Endocrinology and Metabolism.2016; 31(4): 533. CrossRef - Current Challenges in Diabetic Nephropathy: Early Diagnosis and Ways to Improve Outcomes
Sang Soo Kim, Jong Ho Kim, In Joo Kim
Endocrinology and Metabolism.2016; 31(2): 245. CrossRef - Functional mechanisms for diabetic nephropathy-associated genetic variants
Chengxin Gong, Yonghu Xu, Yongfang Fan, Xingzi Liu, Chaopeng Xiong, Luling He, Changle Liu, Shenqiang Rao, Wen Xiao, Lu Ding, Lan Tang, Fangfang Hu, Mengqi Xiong, Mei Yang, Shangdong Liang, Hong Xu
Genes & Genomics.2016; 38(7): 595. CrossRef - Factors Influencing Intention to Receive Examination of Diabetes Complications
Yi-Lin Hsieh, Fang-Hsin Lee, Chien-Liang Chen, Ming-Fong Chang, Pei-Hsuan Han
Asian Nursing Research.2016; 10(4): 289. CrossRef - Associations between the number of natural teeth and renal dysfunction
Hye Min Choi, Kyungdo Han, Yong Gyu Park, Jun-Beom Park
Medicine.2016; 95(34): e4681. CrossRef - Decreased plasma α-Klotho predict progression of nephropathy with type 2 diabetic patients
Sang Soo Kim, Sang Heon Song, In Joo Kim, Eun Young Lee, Su Mi Lee, Choon Hee Chung, Ihm Soo Kwak, Eun Kyung Lee, Yong Ki Kim
Journal of Diabetes and its Complications.2016; 30(5): 887. CrossRef - The Association Between Smoking Tobacco After a Diagnosis of Diabetes and the Prevalence of Diabetic Nephropathy in the Korean Male Population
Hyungseon Yeom, Jung Hyun Lee, Hyeon Chang Kim, Il Suh
Journal of Preventive Medicine and Public Health.2016; 49(2): 108. CrossRef - Effects of Small Dense LDL in Diabetic Nephropathy in Females with Type 2 Diabetes Mellitus
Seongyul Ryu, Youngwoo Kim, Mee Kyoung Kim, Hyuk-Sang Kwon, Ki-Hyun Baek, Ki-Ho Song, Kyung-Jin Yun
Journal of Lipid and Atherosclerosis.2016; 5(1): 11. CrossRef - Translational genomics for human diseases: toward a new era of precision medicine
Yoon Shin Cho, Ki Wha Chung, Nam-Soo Kim
Genes & Genomics.2016; 38(7): 573. CrossRef - Lipoprotein(a) predicts a new onset of chronic kidney disease in people with Type 2 diabetes mellitus
J.‐S. Yun, Y.‐B. Ahn, K.‐H. Song, K.‐D. Yoo, Y.‐M. Park, H.‐W. Kim, S.‐H. Ko
Diabetic Medicine.2016; 33(5): 639. CrossRef - The association between abnormal heart rate variability and new onset of chronic kidney disease in patients with type 2 diabetes: A ten-year follow-up study
Jae-Seung Yun, Yu-Bae Ahn, Ki-Ho Song, Ki-Dong Yoo, Hyung-Wook Kim, Yong-Moon Park, Seung-Hyun Ko
Diabetes Research and Clinical Practice.2015; 108(1): 31. CrossRef - Central obesity is an independent risk factor for microalbuminuria in both the general Korean women and nondiabetic nonhypertensive subpopulation: Association of microalbuminuria and metabolic syndrome from the Korea National Health and Nutrition Examinat
John Hoon Rim, Yong-ho Lee, Bong-Soo Cha, Sang-Guk Lee, Jeong-Ho Kim
Clinica Chimica Acta.2015; 448: 74. CrossRef - Diabetic Kidney Disease: From Epidemiology to Clinical Perspectives
Cheol Whee Park
Diabetes & Metabolism Journal.2014; 38(4): 252. CrossRef
- Figure
- Related articles
-
- Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
- Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
- Trends in the Prevalence of Obesity and Its Phenotypes Based on the Korea National Health and Nutrition Examination Survey from 2007 to 2017 in Korea
- Prevalence of Diabetic Retinopathy in Undiagnosed Diabetic Patients: A Nationwide Population-Based Study

 KDA
KDA
 PubReader
PubReader Cite
Cite






