
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Articles
- Page Path
- HOME > Diabetes Metab J > Volume 36(4); 2012 > Article
-
Original ArticleEpidemiology Total Energy Intake May Be More Associated with Glycemic Control Compared to Each Proportion of Macronutrients in the Korean Diabetic Population
- Hye Mi Kang, Dong-Jun Kim
-
Diabetes & Metabolism Journal 2012;36(4):300-306.
DOI: https://doi.org/10.4093/dmj.2012.36.4.300
Published online: August 20, 2012
Department of Internal Medicine, Ilsan Paik Hospital, Inje University College of Medicine, Goyang, Korea.
- Corresponding author: Dong-Jun Kim. Department of Internal Medicine, Ilsan Paik Hospital, 170 Juhwa-ro, Ilsanseo-gu, Goyang 411-706, Korea. djkim@paik.ac.kr
• Received: October 20, 2011 • Accepted: February 16, 2012
Copyright © 2012 Korean Diabetes Association
This is an Open Access article distributed under the terms of the Creative Commons Attribution Non-Commercial License (http://creativecommons.org/licenses/by-nc/3.0/) which permits unrestricted non-commercial use, distribution, and reproduction in any medium, provided the original work is properly cited.
ABSTRACT
-
Background
- Major macronutrients for energy intake vary among countries and cultures. Carbohydrates, including rice, are the major component of daily energy intake in Korea. The aim of this study was to examine the association of daily energy intake or each proportion of macronutrients, especially carbohydrates, with glycemic control in diabetic Koreans.
-
Methods
- A total of 334 individuals with diabetes (175 men, age 57.4±0.8 years; 159 women, age 60.9±0.9 years) who participated in the 2005 Korean National Health and Nutrition Examination Survey were examined. Glycemic control was categorized based on concentration of glycated hemoglobin (HbA1c; HbA1c ≤6.5%; 6.6% to 8.0%; ≥8.1%). Dietary intake was assessed by using a 24-recall item questionnaire.
-
Results
- High total energy intake was associated with poor glycemic control (HbA1c ≤6.5%, 1,824±75 kcal; 6.6% to 8.0%, 1,990±57 kcal; ≥8.1%, 2,144±73 kcal; P value for trend=0.002). Each proportion of protein, fat, or carbohydrate was not associated with glycemic control. Even after adjusting for several parameters, the association of daily energy intake with glycemic control still persisted.
-
Conclusion
- Total energy intake may be more closely related to glycemic control than each proportionof macronutrients in Korean diabetics.
- The prevalence of type 2 diabetes mellitus (DM) has increased worldwide, and this trend is expected to continue. The prevalence of diabetes in Korea has explosively increased 6- to 7-fold from 1.5% to almost 10% during the past 30 years [1-4]. Furthermore, the numbers of diabetic patients suffering from various diabetic complications and diabetes-related mortality have rapidly increased over the past few decades [1-3]. Although glycemic control is an important determinant in the development of diabetic complications [5-7], two previous studies reported that only 43.5% and 22.9% of Korean diabetic patients had HbA1c levels<7.0% and<6.5%, respectively [8,9].
- Macronutrients including carbohydrate, protein, and fat have varying effects on blood glucose level. Considering that carbohydrate is the single major dietary component affecting the postprandial glucose level compared to protein and fat, carbohydrate intake is much more important in advanced diabetes, which generally shows marked postprandial hyperglycemia [10]. In far-east Asia, rice is the major staple food and the major source of daily energy intake, which is quite different compared to Western countries. An association between macronutrient intake and glycemic control in Western countries has been conclusively established [11-23]. Total energy intake and total fat intake are closely related with glycemic control [11,12,22,23]. However, the association between carbohydrate intake and glycemic control is unclear [13-21]. While most of the latter studies reported that low carbohydrate intake is related to good glycemic control and weight loss [13-18], severe restriction of carbohydrate intake has been linked to poor glycemic control, because it results in an increase of other dietary components such as fat [19-21].
- The aim of the present study was to evaluate the association between daily energy intake or each proportion of macronutrient, especially carbohydrate, and glycemic control in diabetic Koreans.
INTRODUCTION
- Study population
- This study was based on the data obtained from the third Korea National Health and Nutrition Examination Survey (KNHANES III) among non-institutionalized civilians in the Republic of Korea, which was conducted by the Korean Ministry of Health and Welfare in 2005. This survey was a nationwide representative study using a stratified and multistage probability sampling design for the selection of household units. The survey consisted of a health interview, health behavior, health examination, and nutrition components. A total of 34,145 individuals from these sampling frames were included in the health interview survey. Among them, 334 persons with diabetes (fasting glucose concentration ≥126 mg/dL, taking insulin, or oral anti-diabetic medication) were identified as participants, via a laboratory test and nutritional survey data. Glycemic control was categorized based on the concentration of glycated hemoglobin (HbA1c ≤6.5%; 6.6% to 8.0%; ≥8.1%).
- Health examination survey and laboratory test
- Trained interviewers visited each participant's dwelling and administered a standardized questionnaire on smoking, alcohol consumption, regular exercise, and diabetes treatments (e.g., taking insulin or oral hypoglycemic agents). A dietary recall method was used to collect data on food items consumed by participants during the past 24 hours. Height and weight were obtained using standardized techniques and equipment. Height was measured to the nearest 0.1 cm using a portable standiometer (Seriter, Bismarck, ND, USA). Weight was measured to the nearest 0.1 kg using a calibrated balance-beam scale (Giant-150N; Hana, Seoul, Korea). Body mass index (BMI) was calculated by dividing weight by height squared (kg/m2). Waist circumference (WC) was measured on standing participants with a soft tape midway between the lowest rib and the iliac crest. Blood samples were collected on the morning after fasting for at least 8 hours. Fasting plasma glucose (FPG) was measured in a central and certified laboratory; an Advia1650 (Siemens, Tarrytown, NY, USA) was used. HbA1c was measured using a Bio-Rad Varian II (Bio-Rad, Hercules, CA, USA) in all participants.
- Statistical analysis
- Baseline characteristics were summarized for men and women and presented as means±SEM. All statistical techniques were performed using the SPSS for personal computer (SPSS Inc., Chicago, IL, USA). ANCOVA was done to examine age- and sex-adjusted characteristics according to glycemic control. To compare the difference of glycemic control according to daily energy intake or carbohydrate % of energy after adjusting for age, sex, diabetes duration, alcohol intake, exercise, and modality of anti-diabetes treatment, ANCOVA with post hoc analysis (least significant difference [LSD] multiple comparison test) was used. To determine which parameter was associated with glycemic control, logistic regression analysis was done with variables including age, sex, diabetes duration, daily alcohol intake, regular exercise, modality of anti-diabetes treatment, daily energy intake, carbohydrate % of energy, protein % of energy, and fat % of energy. Significance was determined by two-tailed analysis where P<0.05.
- Ethics statement
- This study was approved by the Institutional Review Board of the Ilsan Paik Hospital (IB-3-1106-018).
METHODS
- Table 1 displays data on age and age-adjusted characteristics of the study population. There were 175 diabetic men (mean age, 57.4±0.8 years) and 159 diabetic women (mean age, 60.9±0.9 years) included in the analysis. Mean HbA1c was 7.39±0.13% in men and 7.70±0.13% in women. BMI was 24.6±0.2 kg/m2 in men and 25.1±0.3 kg/m2 in women. DM duration was about 5 years. Total energy intake in men was 2,229±54 kcal, which was higher than that in women (1,724±56 kcal) (P<0.001).
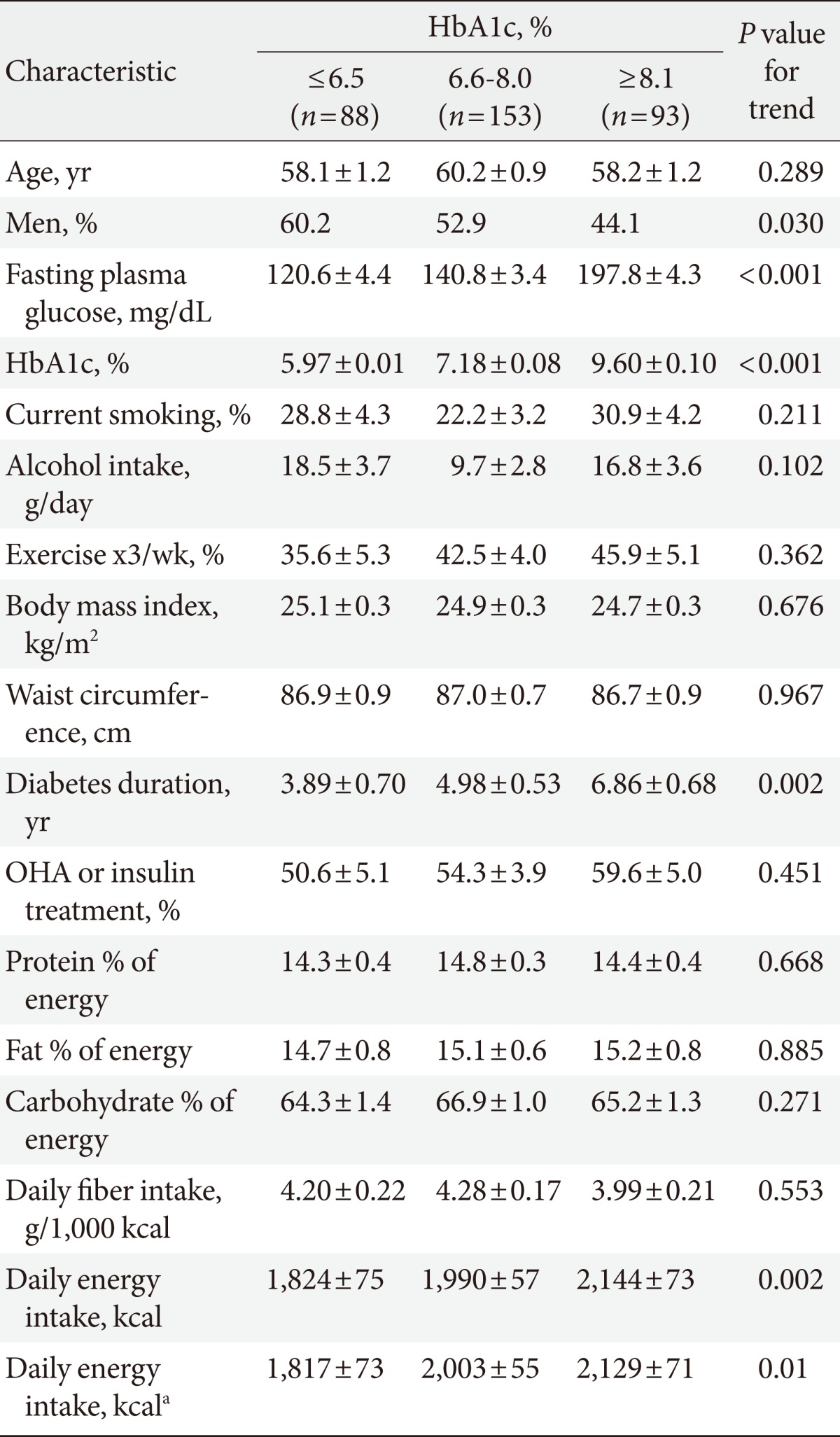
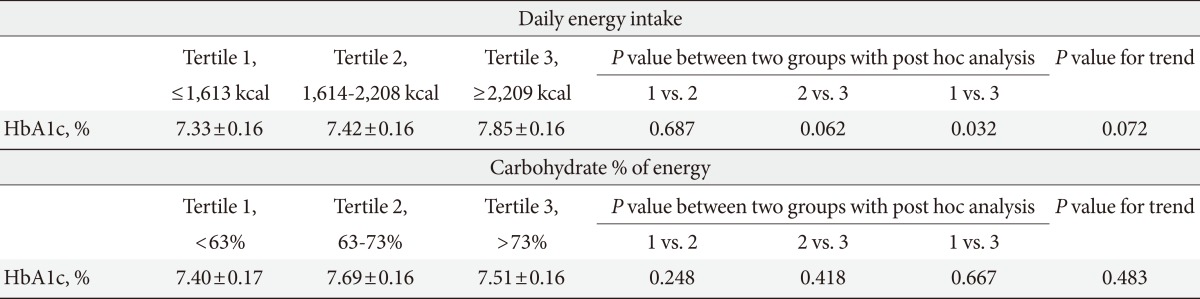
- Table 2 displays data on age, sex, and age- and sex-adjusted characteristics according to glycemic control. Poor glycemic control was associated with a longer duration of diabetes. High total energy intake was associated with poor glycemic control (HbA1c ≤6.5%, 1,824±75 kcal; HbA1c 6.6% to 8.0%, 1,990±57 kcal; HbA1c ≥8.1%, 2,144±73 kcal, P for trend is 0.002). After adjusting for age, sex, alcohol intake, exercise, current smoking, diabetes duration, and oral anti-diabetic medication or insulin treatment, this relationship still persisted. Carbohydrate %, protein %, or fat % of daily energy intake was not associated with glycemic control. In comparison of HbA1c among three equally divided participant groups according to daily energy intake, HbA1c in the highest tertile group was significantly higher than that in the lowest tertile group after adjusting for age, sex, diabetes duration, alcohol intake, exercise, and modality of anti-diabetes treatment (Table 3). There was no difference of HbA1c among three equally divided participant groups according to carbohydrate % of energy intake.
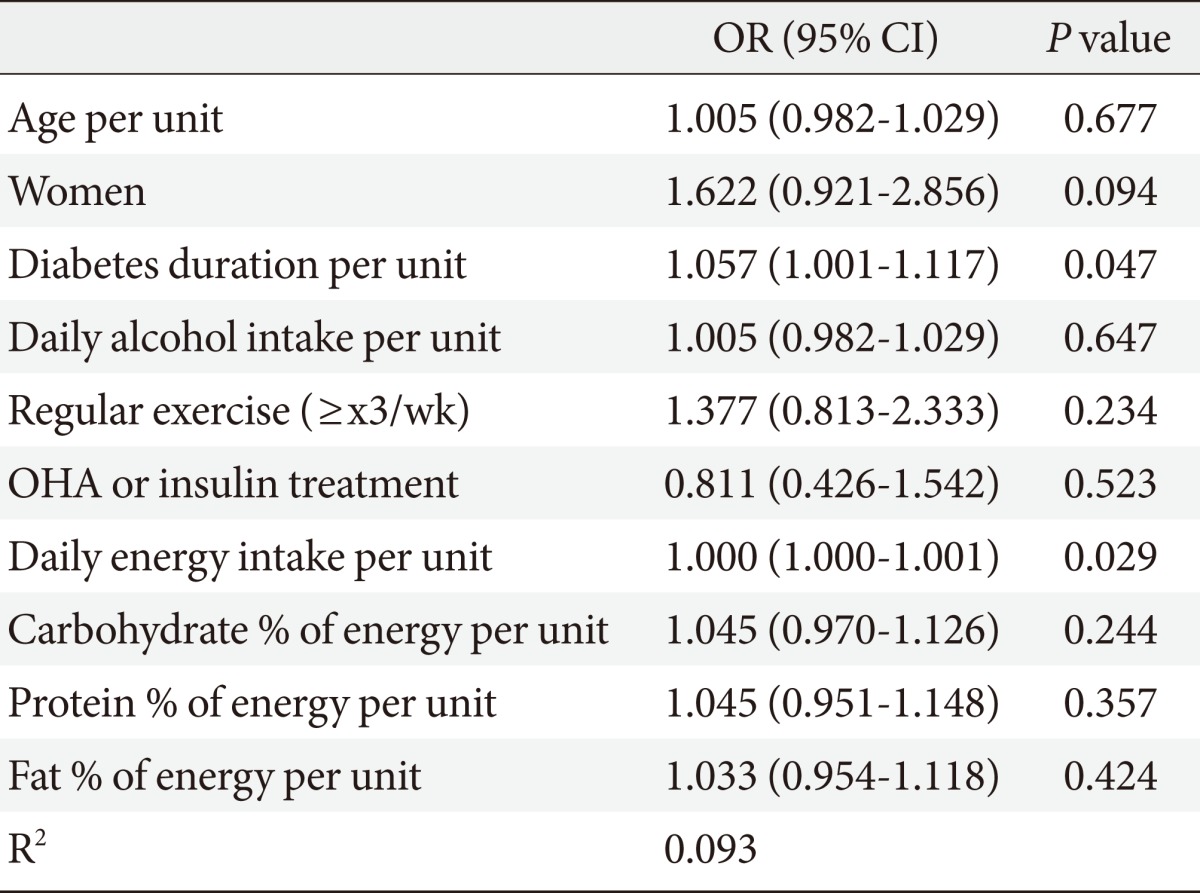
- Logistic regression analysis for HbA1c >6.5% showed that diabetes duration and daily energy intake were associated with glycemic control, respectively, after adjusting for the above mentioned variables. Other parameters, including each proportion of macronutrients, were not significant (Table 4). After dividing the participants into men and women, daily energy intake was associated with glycemic control independently in men (odds ratio [OR], 1.001 [1.000 to 1.001]; P=0.013, per unit of daily energy intake). However, in women there was no significant association (OR, 1.000 [0.999 to 1.001]; P=0.641). In participants with no anti-diabetes medication, daily energy intake was associated with glycemic control independently (OR, 1.001 [1.000 to 1.001]; P=0.032, per unit of daily energy intake). However, there was no significant association in those receiving oral anti-diabetes or insulin treatment (OR, 1.000 [1.000 to 1.001]; P=0.176). In the case of carbohydrate % of energy, there was no significant association with glycemic control in each subgroup (data not shown).
RESULTS
- The present study examined the relationship between glycemic control and macronutrient intake, specifically total daily energy vs. proportion of carbohydrate in daily energy, in a diabetic Korean population. The data suggests that total energy intake is more closely related to glycemic control than the proportion of macronutrients in Korean individuals.
- The staple food of most countries in Asia is carbohydrate. According to KNHANES III [24], the daily total energy intake was 2,016.3 kcal, and the percent of carbohydrate intake of total energy intake was 64.5%. Furthermore, the major component of energy intake was raw rice (38%). Koreans consume more carbohydrate than Americans. In the United States, NHANES 1999-2000 data indicated that carbohydrate intake was 51.9% of total energy intake and fat intake was 32.7% of total energy intake [25].
- Medical nutrition therapy (MNT) is the most important aspect of diabetes treatment including preventing diabetes, managing existing diabetes, and preventing or delaying the rate of development of diabetes complications [26,27]. Optimizing energy intake and macronutrient composition are important in MNT.
- Total energy is an important contributor to glycemic control. Several studies focusing on the effects of reducing energy intake have shown improved glycemic control, both in energy restriction and energy balance [11,12]. Among individuals with type 2 DM, significant positive correlations were found between glycemic control and intakes of energy. Modest weight reductions (as little as 5%) confer long-term benefits in patients with type 2 DM due to reductions in FPG [28]. Whereas, it is well-known that caloric restriction is essential for the achievement of good glycemic control, mainly through weight loss, the optimal dietary macronutrient composition for patients with type 2 DM remains controversial.
- A recent meta-analysis compared the effects of a low-fat, high-carbohydrate diet and a high-fat, low-carbohydrate diet on glycemic control [21]. There was no significant difference in the reduction in HbA1c. However, replacing fat with carbohydrate significantly elevated postprandial glucose levels when total energy intake was consistent.
- In a meta-analysis of 13 trials on the influence of restricted carbohydrate diets in individuals with type 2 DM [13], a greater reduction in hyperglycemia was found in the low carbohydrate diet compared to high carbohydrate diets. A 10% increase in caloric intake from carbohydrates was associated with a 3.2±1.2% increase in glucose levels (P=0.047). However, the meta-analysis included a small number of studies and did not evaluate long-term risks or benefits.
- In Korea, according to KNHANES III [29], when percent energy intake from carbohydrates exceeded 70%, the risk of impaired glucose tolerance and diabetes increased. According to another study conducted in elderly diabetic Korean individuals [30], a lower intake of protein or fat was related to higher HbA1c levels, while there was no association between carbohydrate intake and HbA1c levels. In our study, lower total energy intake was related to good glycemic control, whereas the proportion of carbohydrate, protein, and fat were not.
- We hypothesized that the proportion of carbohydrate, which is major energy intake in Korea, could be associated with glycemic control. However, this association was not presently evident. Although our study was done using nationally representative data, the clinical characteristics of the participants should be defined before interpretation of the data. Many participants in the present study exhibited relatively good glycemic control (mean HbA1c, 7.39±0.13% in men and 7.70±0.13% in women) and a shorter duration of diabetes (5.05±0.50 years in men and 5.40±0.53 years in women), which might attenuate the association between the proportion of carbohydrate and glycemic control. Therefore, we cannot rule out the association of carbohydrate percentage with glycemic control in more advanced and more insulin-deficient diabetes patients with prominent postprandial hyperglycemia.
- There were several limitations in the current study. A single day diet is a poor descriptor of a person's usual intake, because of intra-individual variability. Secondly, because the results were obtained from cross-sectional data, we are not able to draw conclusions about the temporal relationship between macronutrient intake and glycemic control. Another limitation might be the lack of information about diabetes treatment, including compliance to treatment and the type of medication. Although the strength of our study was its nationally representative data, there could be some limitation for generalizing these results to the general population in Korea, because we did not account for primary sampling units, stratification, and sampling weights for KNHANES. Moreover, the result could not extend to all diabetics because of the different effects of macronutrients based on age, sex, the duration of diabetes, status of glycemic control, and compliance to treatment. In this study, the association of daily energy intake with glycemic control was observed only in men or participants with no anti-diabetes medication in subgroup analyses. There was no significant association in women or participants with current oral anti-diabetes or insulin treatment. Different health behavior in men compared to that in women or many other related factors for glycemic control, except for diet in the treatment group compared to the no treatment group, potentially explain these finding. However, we could not present a clear explanation due to limitations of this study, including sample size. Further clinical trials are needed to more conclusively establish the relationship between glycemic control and macronutrients in a subgroup of diabetics for optimizing MNT.
- In conclusion, the data suggested that high total energy intake may be more closely related to poor glycemic control in diabetic Koreans, but the proportion of carbohydrate for total energy intake may not. Clinical trials are needed to test the association between carbohydrate and glycemic control in populations with longer diabetic duration and poor glycemic control. Such investigations may be useful in nutritional therapy for diabetic Koreans.
DISCUSSION
- 1. Task Force Team for Basic Statistical Study of Korean Diabetes Mellitus. Report of Task Force Team for Basic Statistical Study of Korean Diabetes Mellitus: diabetes in Korea 2007. 2007. 1st ed. Seoul: Goldfishery.
- 2. Park IB, Baik SH. Epidemiologic characteristics of diabetes mellitus in Korea: current status of diabetic patients using Korean health insurance database. Korean Diabetes J 2009;33:357-362.Article
- 3. Kim SG, Choi DS. Epidemiology and current status of diabetes in Korea. Hanyang Med Rev 2009;29:122-129.
- 4. Park SW, Kim DJ, Min KW, Baik SH, Choi KM, Park IB, Park JH, Son HS, Ahn CW, Oh JY, Lee J, Chung CH, Kim J, Kim H. Current status of diabetes management in Korea using national health insurance database. J Korean Diabetes Assoc 2007;31:362-367.Article
- 5. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977-986. ArticlePubMed
- 6. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837-853. ArticlePubMed
- 7. Tchobroutsky G. Relation of diabetic control to development of microvascular complications. Diabetologia 1978;15:143-152. ArticlePubMedPDF
- 8. Kim DJ, Kim HM, Park SW, Kim HC, Suh I, Kim HJ, Lee KW. Trends in the prevalence and management status of diabetes in Korea: Korean National Health and Nutrition Examination Survey. Diabetes Res Clin Pract 2008;79(Suppl 1):S21-S22.
- 9. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in Korean adults: Korea National Health and Nutrition Examination Surveys 1998-2005. Diabetes Care 2009;32:2016-2020. PubMedPMC
- 10. Davis N, Forbes B, Wylie-Rosett J. Nutritional strategies in type 2 diabetes mellitus. Mt Sinai J Med 2009;76:257-268. ArticlePubMedPDF
- 11. Bell RA, Summerson JH, Konen JC. Dietary intakes by levels of glycemic control for black and white adults with non-insulin dependent diabetes mellitus (NIDDM). J Am Coll Nutr 1995;14:144-151. ArticlePubMed
- 12. Heilbronn LK, Noakes M, Clifton PM. Effect of energy restriction, weight loss, and diet composition on plasma lipids and glucose in patients with type 2 diabetes. Diabetes Care 1999;22:889-895. ArticlePubMedPDF
- 13. Kirk JK, Graves DE, Craven TE, Lipkin EW, Austin M, Margolis KL. Restricted-carbohydrate diets in patients with type 2 diabetes: a meta-analysis. J Am Diet Assoc 2008;108:91-100. ArticlePubMed
- 14. Dyson PA. A review of low and reduced carbohydrate diets and weight loss in type 2 diabetes. J Hum Nutr Diet 2008;21:530-538. ArticlePubMed
- 15. Ben-Avraham S, Harman-Boehm I, Schwarzfuchs D, Shai I. Dietary strategies for patients with type 2 diabetes in the era of multi-approaches: review and results from the Dietary Intervention Randomized Controlled Trial (DIRECT). Diabetes Res Clin Pract 2009;86(Suppl 1):S41-S48. ArticlePubMed
- 16. Nielsen JV, Joensson EA. Low-carbohydrate diet in type 2 diabetes: stable improvement of bodyweight and glycemic control during 44 months follow-up. Nutr Metab (Lond) 2008;5:14ArticlePubMedPMCPDF
- 17. Gougeon R, Carrington M, Field CJ. The impact of low-carbohydrate diets on glycemic control and weight management in patients with type 2 diabetes. Can J Diabetes 2006;30:269-277.Article
- 18. Boden G, Sargrad K, Homko C, Mozzoli M, Stein TP. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Intern Med 2005;142:403-411. ArticlePubMed
- 19. Xu J, Eilat-Adar S, Loria CM, Howard BV, Fabsitz RR, Begum M, Zephier EM, Lee ET. Macronutrient intake and glycemic control in a population-based sample of American Indians with diabetes: the Strong Heart Study. Am J Clin Nutr 2007;86:480-487. ArticlePubMed
- 20. Ma Y, Olendzki BC, Hafner AR, Chiriboga DE, Culver AL, Andersen VA, Merriam PA, Pagoto SL. Low-carbohydrate and high-fat intake among adult patients with poorly controlled type 2 diabetes mellitus. Nutrition 2006;22:1129-1136. ArticlePubMedPMC
- 21. Kodama S, Saito K, Tanaka S, Maki M, Yachi Y, Sato M, Sugawara A, Totsuka K, Shimano H, Ohashi Y, Yamada N, Sone H. Influence of fat and carbohydrate proportions on the metabolic profile in patients with type 2 diabetes: a meta-analysis. Diabetes Care 2009;32:959-965. ArticlePubMedPMCPDF
- 22. Grylls WK, McKenzie JE, Horwath CC, Mann JI. Lifestyle factors associated with glycaemic control and body mass index in older adults with diabetes. Eur J Clin Nutr 2003;57:1386-1393. ArticlePubMedPDF
- 23. Harding AH, Sargeant LA, Welch A, Oakes S, Luben RN, Bingham S, Day NE, Khaw KT, Wareham NJ. EPIC-Norfolk Study. Fat consumption and HbA(1c) levels: the EPIC-Norfolk study. Diabetes Care 2001;24:1911-1916. PubMed
- 24. Korea Centers for Disease Control and Prevention. The Korea Institute for Health and Social Affairs. In-depth analyses on the Third Korea Health and Nutrition Examination Survey: nutrition survey. 2007. Seoul: Korea Centers for Disease Control and Prevention.
- 25. Wright JD, Wang CY, Kennedy-Stephenson J, Ervin RB. Dietary intake of ten key nutrients for public health, United States: 1999-2000. Adv Data 2003;1-4.
- 26. American Diabetes Association. Standards of medical care in diabetes: 2011. Diabetes Care 2011;34(Suppl 1):S11-S61. ArticlePubMedPMCPDF
- 27. American Diabetes Association. Bantle JP, Wylie-Rosett J, Albright AL, Apovian CM, Clark NG, Franz MJ, Hoogwerf BJ, Lichtenstein AH, Mayer-Davis E, Mooradian AD, Wheeler ML. Nutrition recommendations and interventions for diabetes: a position statement of the American Diabetes Association. Diabetes Care 2008;31(Suppl 1):S61-S78. PubMed
- 28. Wing RR, Koeske R, Epstein LH, Nowalk MP, Gooding W, Becker D. Long-term effects of modest weight loss in type II diabetic patients. Arch Intern Med 1987;147:1749-1753. ArticlePubMed
- 29. Kim EK, Lee JS, Hong H, Yu CH. Association between glycemic index, glycemic load, dietary carbohydrates and diabetes from Korean National Health and Nutrition Examination Survey 2005. Korean J Nutr 2009;42:622-630.Article
- 30. Woo MH, Park S, Woo JT, Choue R. A comparative study of diet in good and poor glycemic control groups in elderly patients with type 2 diabetes mellitus. Korean Diabetes J 2010;34:303-311. ArticlePubMedPMC
REFERENCES
Figure & Data
References
Citations
Citations to this article as recorded by 

- Association of dietary intake and nutrition knowledge with diabetes self-management behavior among Bangladeshi type 2 diabetes mellitus adults: A multi-center cross-sectional study
Shakil Ahmed, Md Sajjadul Haque Ripon, Mohammad Farhan Islam, Ahmad Ullah, Safayet Sultan, Mohammad Sajid, Tanjina Rahman
Endocrine and Metabolic Science.2024; 14: 100156. CrossRef - The effect of mindful eating on dietary behaviour and fasting blood glucose in type 2 diabetes mellitus patients
Rizki Andriani, Aghnia Kamila, Roofi Asma Putri, Arif Fadhillah, Sabrina Helmi, Delia Septiani
Healthcare in Low-resource Settings.2024;[Epub] CrossRef - Prevalence and the association between clinical factors and Diabetes-Related Distress (DRD) with poor glycemic control in patients with type 2 diabetes: A Northern Thai cross-sectional study
Achiraya Ruangchaisiwawet, Narumit Bankhum, Krittai Tanasombatkul, Phichayut Phinyo, Nalinee Yingchankul, Shairyzah Ahmad Hisham
PLOS ONE.2023; 18(11): e0294810. CrossRef - Different Interactive Effects of Metformin and Acarbose With Dietary Macronutrient Intakes on Patients With Type 2 Diabetes Mellitus: Novel Findings From the MARCH Randomized Trial in China
Yu An, Yinhui Li, Nannan Bian, Xiaoyu Ding, Xiaona Chang, Jia Liu, Guang Wang
Frontiers in Nutrition.2022;[Epub] CrossRef - FAKTOR YANG MEMPENGARUHI KADAR GLUKOSA DARAH PENDERITA DIABETES MELITUS TIPE II USIA 46-65 TAHUN DI KABUPATEN WAKATOBI
Ekasari Ekasari, Devieka Rhama Dhanny
Journal of Nutrition College.2022; 11(2): 154. CrossRef - The Effects of Dietary Nutrition Intake on Glycemic Variability in Type 1 Diabetes Mellitus Adults
Liyuan Zhou, Mingqun Deng, Xiao Zhai, Ruiqi Yu, Jieying Liu, Miao Yu, Yuxiu Li, Xinhua Xiao
Diabetes Therapy.2021; 12(4): 1055. CrossRef - Habitual Miso (Fermented Soybean Paste) Consumption Is Associated with Glycemic Variability in Patients with Type 2 Diabetes: A Cross-Sectional Study
Fuyuko Takahashi, Yoshitaka Hashimoto, Ayumi Kaji, Ryosuke Sakai, Akane Miki, Takuro Okamura, Noriyuki Kitagawa, Hiroshi Okada, Naoko Nakanishi, Saori Majima, Takafumi Senmaru, Emi Ushigome, Masahide Hamaguchi, Mai Asano, Masahiro Yamazaki, Michiaki Fukui
Nutrients.2021; 13(5): 1488. CrossRef - Dietary Macronutrient Intakes and Mortality among Patients with Type 2 Diabetes
Cheng-Chieh Lin, Chiu-Shong Liu, Chia-Ing Li, Chih-Hsueh Lin, Wen-Yuan Lin, Mu-Cyun Wang, Shing-Yu Yang, Tsai-Chung Li
Nutrients.2020; 12(6): 1665. CrossRef - Impact of ENPP1 K121Q on Change of Insulin Resistance after Web-Based Intervention in Korean Men with Diabetes and Impaired Fasting Glucose
Ji Yeon Kang, Sook Hee Sung, Yeon Ju Lee, Tae In Choi, Seung Jin Choi
Journal of Korean Medical Science.2014; 29(10): 1353. CrossRef

 KDA
KDA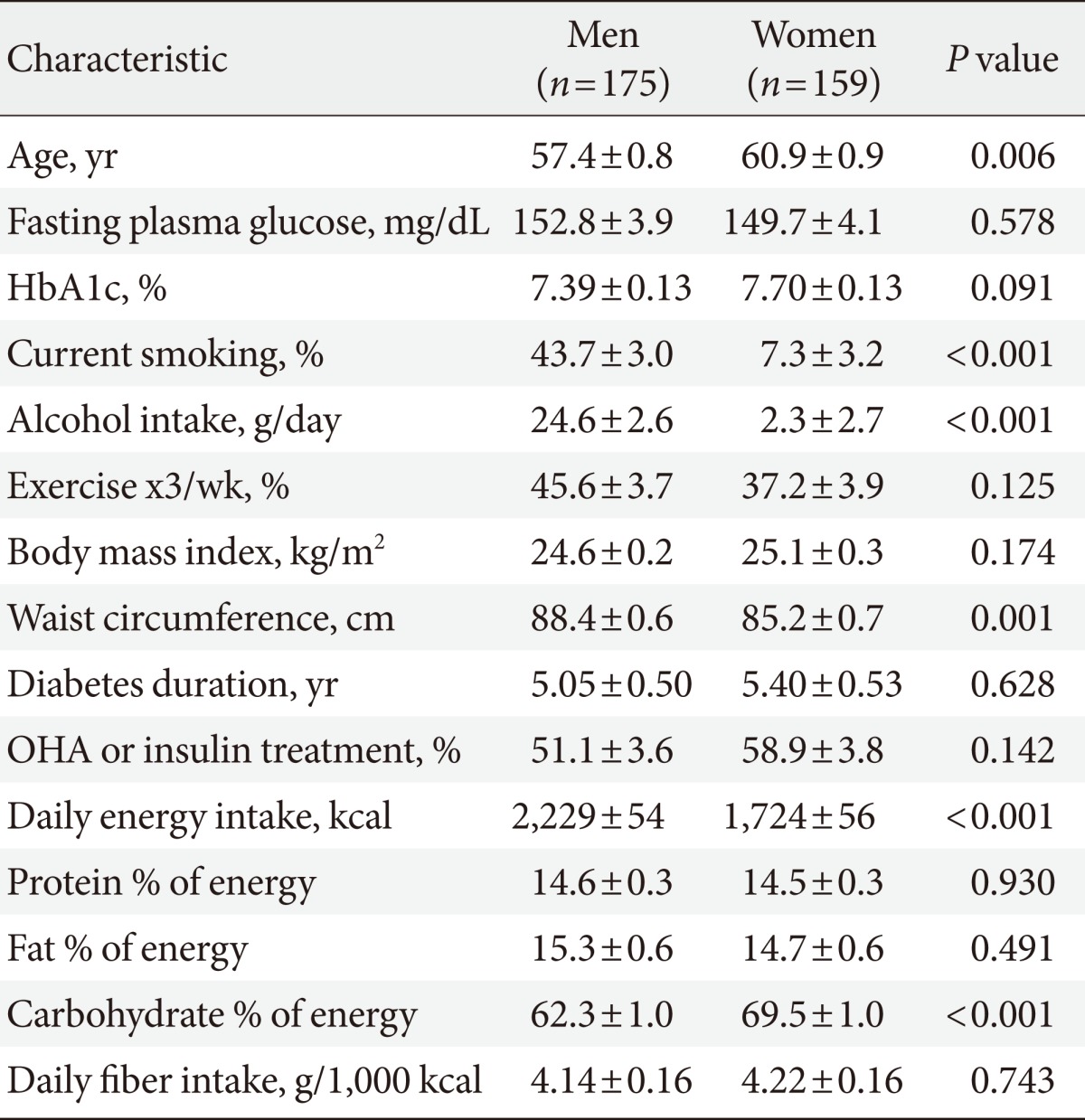
 PubReader
PubReader Cite
Cite



