
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Most cited
- Page Path
- HOME > Browse > Most cited
From articles published in Diabetes & Metabolism Journal during the past two years (2022 ~ ).
Original Article
- Basic Research
- N6-Methyladenosine Methyltransferase METTL3 Alleviates Diabetes-Induced Testicular Damage through Modulating TUG1/Clusterin Axis
- Yuan Tian, Yue-Hai Xiao, Chao Sun, Bei Liu, Fa Sun
- Diabetes Metab J. 2023;47(2):287-300. Published online January 19, 2023
- DOI: https://doi.org/10.4093/dmj.2021.0306
- 2,138 View
- 153 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
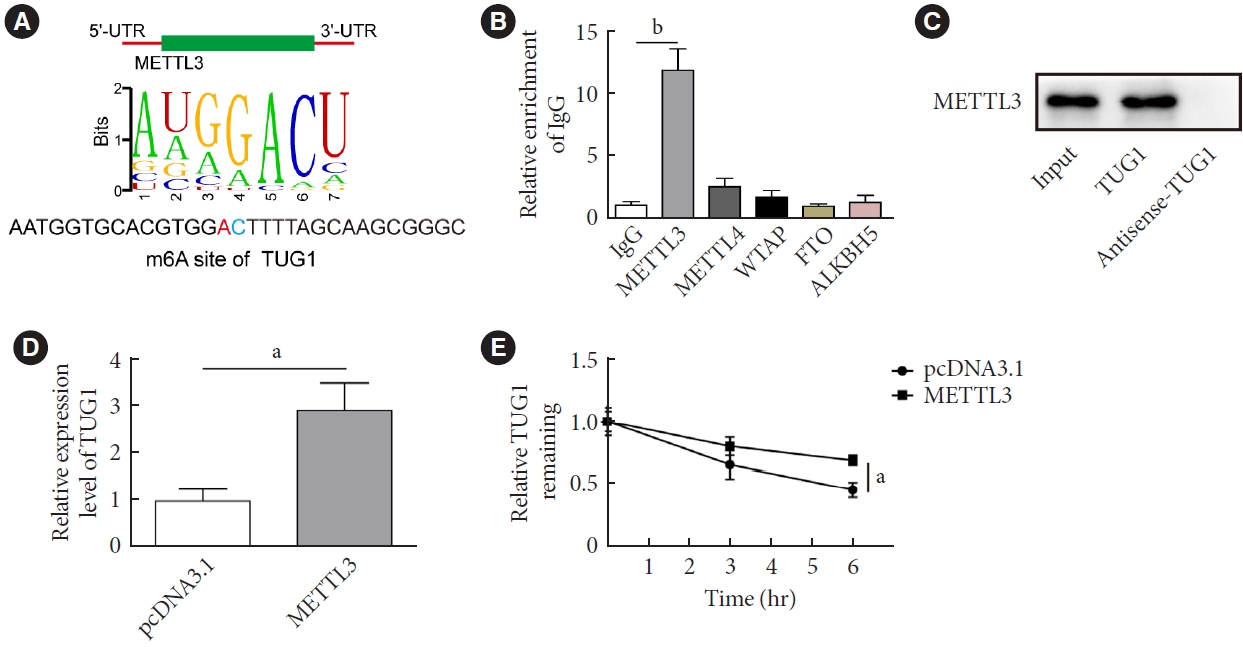
The present study investigated the regulatory effects of N6-methyladenosine (m6A) methyltransferase like-3 (METTL3) in diabetes-induced testicular damage.
Methods
In vivo diabetic mice and high glucose (HG) treated GC-1 spg cells were established. The mRNA and protein expressions were determined by real-time quantitative polymerase chain reaction, Western blot, immunofluorescence and immunohistochemistry staining. Levels of testosterone, blood glucose, cell viability, and apoptosis were detected by enzyme-linked immunosorbent assay, MTT, and flow cytometry, respectively. Molecular interactions were verified by RNA immunoprecipitation and RNA pull-down assay. Histopathological staining was performed to evaluate testicular injury.
Results
METTL3 and long non-coding RNA taurine up-regulated 1 (lncRNA TUG1) were downregulated in testicular tissues of diabetic mice and HG-treated GC-1 spg cells. METTL3 overexpression could reduce the blood glucose level, oxidative stress and testicular damage but enhance testosterone secretion in diabetic mouse model and HG-stimulated GC-1 spg cells. Mechanically, METTL3-mediated m6A methylation enhanced the stability of TUG1, then stabilizing the clusterin mRNA via recruiting serine and arginine rich splicing factor 1. Moreover, inhibition of TUG1/clusterin signaling markedly reversed the protective impacts of METTL3 overexpression on HG-stimulated GC-1 spg cells.
Conclusion
This study demonstrated that METTL3 ameliorated diabetes-induced testicular damage by upregulating the TUG1/clusterin signaling. These data further elucidate the potential regulatory mechanisms of m6A modification on diabetes-induced testicular injury. -
Citations
Citations to this article as recorded by- Negative Regulation of LINC01013 by METTL3 and YTHDF2 Enhances the Osteogenic Differentiation of Senescent Pre‐Osteoblast Cells Induced by Hydrogen Peroxide
Jiaxin Song, Yuejun Wang, Zhao Zhu, Wanqing Wang, Haoqing Yang, Zhaochen Shan
Advanced Biology.2024;[Epub] CrossRef - Diabetes and diabetic associative diseases: An overview of epigenetic regulations of TUG1
Mohammed Ageeli Hakami
Saudi Journal of Biological Sciences.2024; 31(5): 103976. CrossRef
- Negative Regulation of LINC01013 by METTL3 and YTHDF2 Enhances the Osteogenic Differentiation of Senescent Pre‐Osteoblast Cells Induced by Hydrogen Peroxide
Reviews
- Drug/Regimen
- Machine Learning Approach to Drug Treatment Strategy for Diabetes Care
- Kazuya Fujihara, Hirohito Sone
- Diabetes Metab J. 2023;47(3):325-332. Published online January 12, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0349
- 65,535 View
- 241 Download
- 1 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
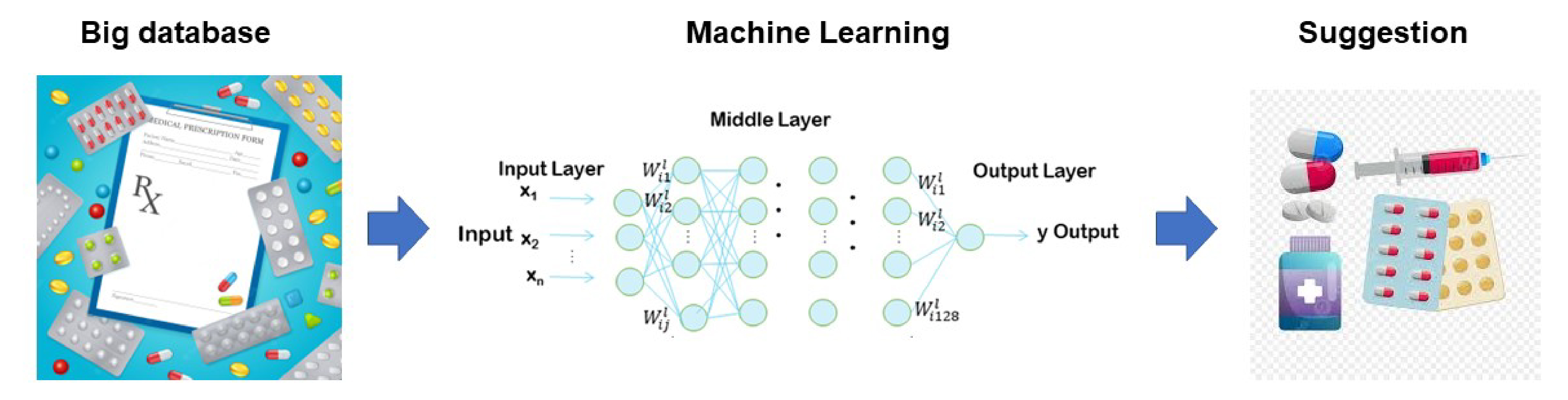
ePub - Globally, the number of people with diabetes mellitus has quadrupled in the past three decades, and approximately one in 11 adults worldwide have diabetes mellitus. Since both microvascular and macrovascular diseases in patients with diabetes predispose them to a lower quality of life as well as higher rates of mortality, managing blood glucose levels is of clinical relevance in diabetes care. Many classes of antihyperglycemic drugs are currently approved to treat hyperglycemia in patients with type 2 diabetes mellitus, with several new drugs having been developed during the last decade. Diabetes-related complications have been reduced substantially worldwide. Prioritization of therapeutic agents varies according to national guidelines. However, since the characteristics of participants in clinical trials differ from patients in actual clinical practice, it is difficult to apply the results of such trials to clinical practice. Machine learning approaches became highly topical issues in medicine along with rapid technological innovations in the fields of information and communication in the 1990s. However, adopting these technologies to support decision-making regarding drug treatment strategies for diabetes care has been slow. This review summarizes data from recent studies on the choice of drugs for type 2 diabetes mellitus focusing on machine learning approaches.
-
Citations
Citations to this article as recorded by- Exploring antioxidant activities and inhibitory effects against α‐amylase and α‐glucosidase of Elaeocarpus braceanus fruits: insights into mechanisms by molecular docking and molecular dynamics
Hong Li, Yuanyue Zhang, Zhijia Liu, Chaofan Guo, Maurizio Battino, Shengbao Cai, Junjie Yi
International Journal of Food Science & Technology.2024; 59(1): 343. CrossRef - 3D Convolutional Neural Networks for Predicting Protein Structure for Improved Drug Recommendation
Pokkuluri Kiran Sree, SSSN Usha Devi N
EAI Endorsed Transactions on Pervasive Health and Technology.2024;[Epub] CrossRef
- Exploring antioxidant activities and inhibitory effects against α‐amylase and α‐glucosidase of Elaeocarpus braceanus fruits: insights into mechanisms by molecular docking and molecular dynamics
- Basic Research
- Multiple Roles of Sirtuin 6 in Adipose Tissue Inflammation
- Eun Ju Bae, Byung-Hyun Park
- Diabetes Metab J. 2023;47(2):164-172. Published online January 12, 2023
- DOI: https://doi.org/10.4093/dmj.2022.0270
- 3,560 View
- 229 Download
- 4 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
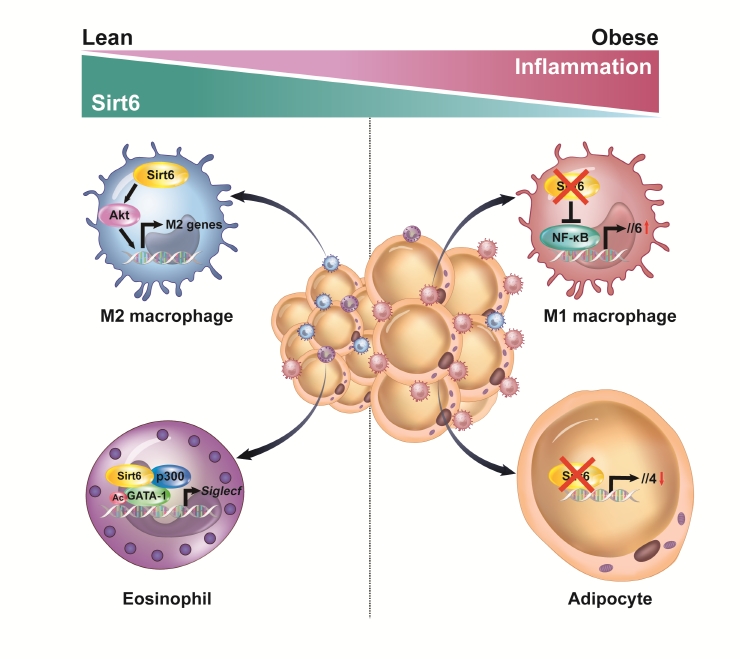
ePub - Adipose tissue (AT) inflammation is strongly associated with obesity-induced insulin resistance. When subjected to metabolic stress, adipocytes become inflamed and secrete a plethora of cytokines and chemokines, which recruit circulating immune cells to AT. Although sirtuin 6 (Sirt6) is known to control genomic stabilization, aging, and cellular metabolism, it is now understood to also play a pivotal role in the regulation of AT inflammation. Sirt6 protein levels are reduced in the AT of obese humans and animals and increased by weight loss. In this review, we summarize the potential mechanism of AT inflammation caused by impaired action of Sirt6 from the immune cells’ point of view. We first describe the properties and functions of immune cells in obese AT, with an emphasis on discrete macrophage subpopulations which are central to AT inflammation. We then highlight data that links Sirt6 to functional phenotypes of AT inflammation. Importantly, we discuss in detail the effects of Sirt6 deficiency in adipocytes, macrophages, and eosinophils on insulin resistance or AT browning. In our closing perspectives, we discuss emerging issues in this field that require further investigation.
-
Citations
Citations to this article as recorded by- The Role of Increased Expression of Sirtuin 6 in the Prevention of Premature Aging Pathomechanisms
Adrianna Dzidek, Olga Czerwińska-Ledwig, Małgorzata Żychowska, Wanda Pilch, Anna Piotrowska
International Journal of Molecular Sciences.2023; 24(11): 9655. CrossRef - Exploring the Influence of Age, Gender and Body Mass Index on Colorectal Cancer Location
Dorel Popovici, Cristian Stanisav, Sorin Saftescu, Serban Negru, Radu Dragomir, Daniel Ciurescu, Razvan Diaconescu
Medicina.2023; 59(8): 1399. CrossRef
- The Role of Increased Expression of Sirtuin 6 in the Prevention of Premature Aging Pathomechanisms
Letter
- Association between Metabolic Syndrome and Microvascular Complications in Chinese Adults with Type 1 Diabetes Mellitus (Diabetes Metab J 2022;46:93-103)
- Gyuri Kim
- Diabetes Metab J. 2022;46(3):512-514. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0134
- 2,637 View
- 119 Download
- 2 Web of Science
- 2 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Receiver Operator Characteristic (ROC) Analysis of Lipids, Proteins, DNA Oxidative Damage, and Antioxidant Defense in Plasma and Erythrocytes of Young Reproductive-Age Men with Early Stages of Type 1 Diabetes Mellitus (T1DM) Nephropathy in the Irkutsk Reg
Marina Darenskaya, Elena Chugunova, Sergey Kolesnikov, Natalya Semenova, Isay Michalevich, Olga Nikitina, Anastasya Lesnaya, Lyubov Kolesnikova
Metabolites.2022; 12(12): 1282. CrossRef - Recent advances and potentiality of postbiotics in the food industry: Composition, inactivation methods, current applications in metabolic syndrome, and future trends
Yujie Zhong, Tao Wang, Ruilin Luo, Jiayu Liu, Ruyi Jin, Xiaoli Peng
Critical Reviews in Food Science and Nutrition.2022; : 1. CrossRef
- Receiver Operator Characteristic (ROC) Analysis of Lipids, Proteins, DNA Oxidative Damage, and Antioxidant Defense in Plasma and Erythrocytes of Young Reproductive-Age Men with Early Stages of Type 1 Diabetes Mellitus (T1DM) Nephropathy in the Irkutsk Reg
Original Articles
- Metabolic Risk/Epidemiology
- Impact of Older Age Adiposity on Incident Diabetes: A Community-Based Cohort Study in China
- Anthony Chen, Weiju Zhou, Jian Hou, Alan Nevill, Yuanlin Ding, Yuhui Wan, Rebecca Jester, Xia Qin, Zhi Hu, Ruoling Chen
- Diabetes Metab J. 2022;46(5):733-746. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0215
- 3,939 View
- 197 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Obesity classifications vary globally and the impact of older age adiposity on incident diabetes has not been well-studied.
Methods
We examined a random sample of 2,809 participants aged ≥60 years in China, who were free of diabetes at baseline and were followed up for up to 10 years to document diabetes (n=178). The incidence of diabetes was assessed in relation to different cut-off points of body mass index (BMI) and waist circumference (WC) in multiple adjusted Cox regression models.
Results
The diabetic risk in the cohort increased linearly with the continuous and quartile variables of BMI and WC. The BMI-World Health Organization (WHO) and BMI-China criteria analysis did not show such a linear relationship, however, the BMI-Asian/Hong Kong criteria did; adjusted hazards ratio (HR) was 0.42 (95% confidence interval [CI], 0.20 to 0.90) in BMI <20 kg/m2, 1.46 (95% CI, 0.99 to 2.14) in 23–≤26 kg/m2, and 1.63 (95% CI, 1.09 to 2.45) in ≥26 kg/m2. The WC-China criteria revealed a slightly better prediction of diabetes (adjusted HRs were 1.79 [95% CI, 1.21 to 2.66] and 1.87 [95% CI, 1.22 to 2.88] in central obese action levels 1 and 2) than the WC-WHO. The combination of the BMI-Asian/Hong Kong with WC-China demonstrated the strongest prediction. There were no gender differences in the impact of adiposity on diabetes.
Conclusion
In older Chinese, BMI-Asian/Hong Kong criteria is a better predictor of diabetes than other BMI criterion. Its combination with WC-China improved the prediction of adiposity to diabetes, which would help manage bodyweight in older age to reduce the risk of diabetes. -
Citations
Citations to this article as recorded by- Association of air pollution with dementia: a systematic review with meta-analysis including new cohort data from China
Jie Tang, Anthony Chen, Fan He, Martin Shipley, Alan Nevill, Hugh Coe, Zhi Hu, Tao Zhang, Haidong Kan, Eric Brunner, Xuguang Tao, Ruoling Chen
Environmental Research.2023; 223: 115048. CrossRef - Impact of fish consumption on all-cause mortality in older people with and without dementia: a community-based cohort study
Aishat T. Bakre, Anthony Chen, Xuguang Tao, Jian Hou, Yuyou Yao, Alain Nevill, James J. Tang, Sabine Rohrmann, Jindong Ni, Zhi Hu, John Copeland, Ruoling Chen
European Journal of Nutrition.2022; 61(7): 3785. CrossRef
- Association of air pollution with dementia: a systematic review with meta-analysis including new cohort data from China
- Complications
- Fatty Acid-Binding Protein 4 in Patients with and without Diabetic Retinopathy
- Ping Huang, Xiaoqin Zhao, Yi Sun, Xinlei Wang, Rong Ouyang, Yanqiu Jiang, Xiaoquan Zhang, Renyue Hu, Zhuqi Tang, Yunjuan Gu
- Diabetes Metab J. 2022;46(4):640-649. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0195
- 3,338 View
- 192 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Fatty acid-binding protein 4 (FABP4) has been demonstrated to be a predictor of early diabetic nephropathy. However, little is known about the relationship between FABP4 and diabetic retinopathy (DR). This study explored the value of FABP4 as a biomarker of DR in patients with type 2 diabetes mellitus (T2DM).
Methods
A total of 238 subjects were enrolled, including 20 healthy controls and 218 T2DM patients. Serum FABP4 levels were measured using a sandwich enzyme-linked immunosorbent assay. The grade of DR was determined using fundus fluorescence angiography. Based on the international classification of DR, all T2DM patients were classified into the following three subgroups: non-DR group, non-proliferative diabetic retinopathy (NPDR) group, and proliferative diabetic retinopathy (PDR) group. Multivariate logistic regression analyses were employed to assess the correlation between FABP4 levels and DR severity.
Results
FABP4 correlated positively with DR severity (r=0.225, P=0.001). Receiver operating characteristic curve analysis was used to assess the diagnostic potential of FABP4 in identifying DR, with an area under the curve of 0.624 (37% sensitivity, 83.6% specificity) and an optimum cut-off value of 76.4 μg/L. Multivariate logistic regression model including FABP4 as a categorized binary variable using the cut-off value of 76.4 μg/L showed that the concentration of FABP4 above the cut-off value increased the risk of NPDR (odds ratio [OR], 3.231; 95% confidence interval [CI], 1.574 to 6.632; P=0.001) and PDR (OR, 3.689; 95% CI, 1.306 to 10.424; P=0.014).
Conclusion
FABP4 may be used as a serum biomarker for the diagnosis of DR. -
Citations
Citations to this article as recorded by- Circulating AFABP, FGF21, and PEDF Levels as Prognostic Biomarkers of Sight-threatening Diabetic Retinopathy
Chi-Ho Lee, David Tak-Wai Lui, Chloe Yu-Yan Cheung, Carol Ho-Yi Fong, Michele Mae-Ann Yuen, Yu-Cho Woo, Wing-Sun Chow, Ian Yat-Hin Wong, Aimin Xu, Karen Siu-Ling Lam
The Journal of Clinical Endocrinology & Metabolism.2023; 108(9): e799. CrossRef - A Prediction Model for Sight-Threatening Diabetic Retinopathy Based on Plasma Adipokines among Patients with Mild Diabetic Retinopathy
Yaxin An, Bin Cao, Kun Li, Yongsong Xu, Wenying Zhao, Dong Zhao, Jing Ke, Takayuki Masaki
Journal of Diabetes Research.2023; 2023: 1. CrossRef
- Circulating AFABP, FGF21, and PEDF Levels as Prognostic Biomarkers of Sight-threatening Diabetic Retinopathy
Editorial
- Variability of Metabolic Risk Factors: Causative Factor or Epiphenomenon?
- Hye Jin Yoo
- Diabetes Metab J. 2022;46(2):257-259. Published online March 24, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0060
- 3,031 View
- 131 Download
- 2 Web of Science
- 2 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Ji Eun Jun, You-Cheol Hwang, Kyu Jeong Ahn, Ho Yeon Chung, Geon-Ho Jahng, Soonchan Park, In-Kyung Jeong, Chang-Woo Ryu
Diabetes Research and Clinical Practice.2022; 191: 110067. CrossRef - Mean versus variability of lipid measurements over 6 years and incident cardiovascular events: More than a decade follow-up
Soroush Masrouri, Leila Cheraghi, Niloofar Deravi, Neda Cheraghloo, Maryam Tohidi, Fereidoun Azizi, Farzad Hadaegh
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef
- Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Original Article
- Drug/Regimen
- Comparison of Efficacy of Glimepiride, Alogliptin, and Alogliptin-Pioglitazone as the Initial Periods of Therapy in Patients with Poorly Controlled Type 2 Diabetes Mellitus: An Open-Label, Multicenter, Randomized, Controlled Study
- Hae Jin Kim, In Kyung Jeong, Kyu Yeon Hur, Soo-Kyung Kim, Jung Hyun Noh, Sung Wan Chun, Eun Seok Kang, Eun-Jung Rhee, Sung Hee Choi
- Diabetes Metab J. 2022;46(5):689-700. Published online March 17, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0183
- 5,592 View
- 376 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The choice of an optimal oral hypoglycemic agent in the initial treatment periods for type 2 diabetes mellitus (T2DM) patients remains difficult and deliberate. We compared the efficacy and safety of glimepiride (GLIM), alogliptin (ALO), and alogliptin-pioglitazone (ALO-PIO) in poorly controlled T2DM patients with drug-naïve or metformin failure.
Methods
In this three-arm, multicenter, open-label, randomized, controlled trial, poorly controlled T2DM patients were randomized to receive GLIM (n=35), ALO (n=31), or ALO-PIO (n=33) therapy for 24 weeks. The primary endpoint was change in the mean glycosylated hemoglobin (HbA1c) levels at week 24 from baseline. Secondary endpoints were changes in HbA1c level at week 12 from baseline, fasting plasma glucose (FPG) levels, lipid profiles at weeks 12 and 24, and parameters of glycemic variability, assessed by continuous glucose monitoring for 24 weeks.
Results
At weeks 12 and 24, the ALO-PIO group showed significant reduction in HbA1c levels compared to the ALO group (–0.96%±0.17% vs. –0.37%±0.17% at week 12; –1.13%±0.19% vs. –0.18%±0.2% at week 24). The ALO-PIO therapy caused greater reduction in FPG levels and significant increase in high-density lipoprotein cholesterol levels at weeks 12 and 24 than the ALO therapy. Compared to low-dose GLIM therapy, ALO-PIO therapy showed greater improvement in glycemic variability. The adverse events were similar among the three arms.
Conclusion
ALO-PIO combination therapy during the early period exerts better glycemic control than ALO monotherapy and excellency in glycemic variability than low-dose sulfonylurea therapy in uncontrolled, drug-naïve or metformin failed T2DM patients. -
Citations
Citations to this article as recorded by- A Comprehensive Review on Weight Loss Associated with Anti-Diabetic Medications
Fatma Haddad, Ghadeer Dokmak, Maryam Bader, Rafik Karaman
Life.2023; 13(4): 1012. CrossRef - Role of Dipeptidyl Peptidase 4 Inhibitors in Antidiabetic Treatment
Ruili Yin, Yongsong Xu, Xin Wang, Longyan Yang, Dong Zhao
Molecules.2022; 27(10): 3055. CrossRef
- A Comprehensive Review on Weight Loss Associated with Anti-Diabetic Medications
Short Communications
- Pathophysiology
- Glutamic Acid Decarboxylase and Tyrosine Phosphatase-Related Islet Antigen-2 Positivity among Children and Adolescents with Diabetes in Korea
- Ka Young Kim, Min Seung Kim, Yun Jeong Lee, Young Ah Lee, Seong Yong Lee, Choong Ho Shin, Jae Hyun Kim
- Diabetes Metab J. 2022;46(6):948-952. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0332
- 4,458 View
- 183 Download
- 3 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Autoantibodies against glutamic acid decarboxylase (GADA), tyrosine phosphatase-related islet antigen 2 (IA2A), insulin (INSA), and islet cells (ICA) are critical for determining the type of diabetes and management strategy in new-onset diabetes mellitus (NODM), but there have been few reports of all diabetes-associated autoantibody (DAA) in Korea. We retrospectively analyzed 193 patients with NODM aged 0 to 18 years who were followed at two tertiary centers in Korea (2017 to 2021). Patients with type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) were 93 (48.2%) and 100 (51.8%), respectively. In T1DM patients, the DAA positivity rate was 94.6%; prevalence of GADA, IA2A, INSA, and ICA was 71.0%, 71.0%, 31.2%, and 10.8%, respectively; and IA2A added 10.7% point autoantibody positivity (83.9% for GADA+INSA+ICA and 94.6% for GADA+INSA+ICA+IA2A). Among the patients with T2DM, 12 (12.0%) were positive for DAA, and all were positive for INSA. These findings suggest that DAA at diagnosis, especially GADA and IA2A, is useful for classifying diabetes in Korean children and adolescents.
-
Citations
Citations to this article as recorded by- Immune-Checkpoint Inhibitors-Induced Type 1 Diabetes Mellitus: From Its Molecular Mechanisms to Clinical Practice
Yun Kyung Cho, Chang Hee Jung
Diabetes & Metabolism Journal.2023; 47(6): 757. CrossRef - Diagnostic and Therapeutic Strategies of Type 2 Diabetes Mellitus in Youth
Hwa Young Kim, Jae Hyun Kim
The Ewha Medical Journal.2022;[Epub] CrossRef
- Immune-Checkpoint Inhibitors-Induced Type 1 Diabetes Mellitus: From Its Molecular Mechanisms to Clinical Practice
- Technology/Device
- A 4-Week, Two-Center, Open-Label, Single-Arm Study to Evaluate the Safety and Efficacy of EOPatch in Well-Controlled Type 1 Diabetes Mellitus
- Jiyun Park, Nammi Park, Sangjin Han, You-Bin Lee, Gyuri Kim, Sang-Man Jin, Woo Je Lee, Jae Hyeon Kim
- Diabetes Metab J. 2022;46(6):941-947. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0299
- 5,082 View
- 269 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - This study evaluated the safety and efficacy of tubeless patch pump called EOPatch in patients with well-controlled type 1 diabetes mellitus (T1DM). This 4-week, two-center, open-label, single-arm study enrolled 10 adult patients diagnosed with T1DM with glycosylated hemoglobin less than 7.5%. The co-primary end points were patch pump usage time for one attachment and number of serious adverse events related to the patch pump. The secondary end points were total amount of insulin injected per patch and changes in glycemic parameters including continuous glucose monitoring data compared to those at study entry. The median usage time per patch was 84.00 hours (interquartile range, 64.50 to 92.50). Serious adverse events did not occur during the trial. Four weeks later, time in range 70 to 180 mg/dL was significantly improved (70.71%±17.14 % vs. 82.96%±9.14%, P=0.01). The times spent below range (<54 mg/dL) and above range (>180 mg/dL) also improved (All P<0.05). Four-week treatment with a tubeless patch pump was safe and led to clinical improvement in glycemic control.
-
Citations
Citations to this article as recorded by- Multilayer track‐etched membrane‐based electroosmotic pump for drug delivery
Qian Yang, Zebo Zhang, Junshu Lin, Boyu Zhu, Rongying Yu, Xinru Li, Bin Su, Bo Zhao
ELECTROPHORESIS.2024; 45(5-6): 433. CrossRef - A true continuous healthcare system for type 1 diabetes
Jiyong Kim, Salman Khan, Eun Kyu Kim, Hye-Jun Kil, Bo Min Kang, Hyo Geon Lee, Jin-Woo Park, Jun Young Yoon, Woochul Kim
Nano Energy.2023; 113: 108553. CrossRef
- Multilayer track‐etched membrane‐based electroosmotic pump for drug delivery
Brief Report
- Metabolic Risk/Epidemiology
- Trends in the Prevalence of Obesity and Its Phenotypes Based on the Korea National Health and Nutrition Examination Survey from 2007 to 2017 in Korea
- Sang Ouk Chin, You-Cheol Hwang, Hong-Yup Ahn, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung
- Diabetes Metab J. 2022;46(5):808-812. Published online March 8, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0226
- 3,825 View
- 214 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - This study used data from the Korea National Health and Nutrition Examination Survey IV–VII from 2007 to identify the prevalence of obesity and its phenotypes (metabolically unhealthy obesity [MUO] and metabolically healthy obesity [MHO]) and their secular changes. The prevalence of obesity in Korea increased with significant secular changes observed (β=0.326, P trend <0.01) between 2007 and 2017, and especially in men (β=0.682, P trend <0.001) but not in women. The changes in the prevalence of obesity during the study period were different between men and women (P=0.001). The prevalence of MUO significantly increased only in men (β=0.565, P trend <0.01), while that of MHO increased only in women (β=0.179, P<0.05), especially in the younger age group (β=0.308, P<0.01).
-
Citations
Citations to this article as recorded by- Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - Differences of Regional Fat Distribution Measured by Magnetic Resonance Imaging According to Obese Phenotype in Koreans
Ha-Neul Choi, Hyunjung Lim, Young-Seol Kim, Sang-Youl Rhee, Jung-Eun Yim
Metabolic Syndrome and Related Disorders.2022; 20(10): 551. CrossRef
- Hormonal Gut–Brain Signaling for the Treatment of Obesity
Original Articles
- Cardiovascular Risk/Epidemiology
- Mean and Variability of Lipid Measurements and Risk for Development of Subclinical Left Ventricular Diastolic Dysfunction
- Jiyun Park, Mira Kang, Jiyeon Ahn, Min Young Kim, Min Sun Choi, You-Bin Lee, Gyuri Kim, Kyu Yeon Hur, Jae Hyeon Kim, Jeong Hoon Yang, Sang-Man Jin
- Diabetes Metab J. 2022;46(2):286-296. Published online November 22, 2021
- DOI: https://doi.org/10.4093/dmj.2021.0080
- 5,574 View
- 196 Download
- 1 Web of Science
- 2 Crossref
-
 Graphical Abstract
Graphical Abstract
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub 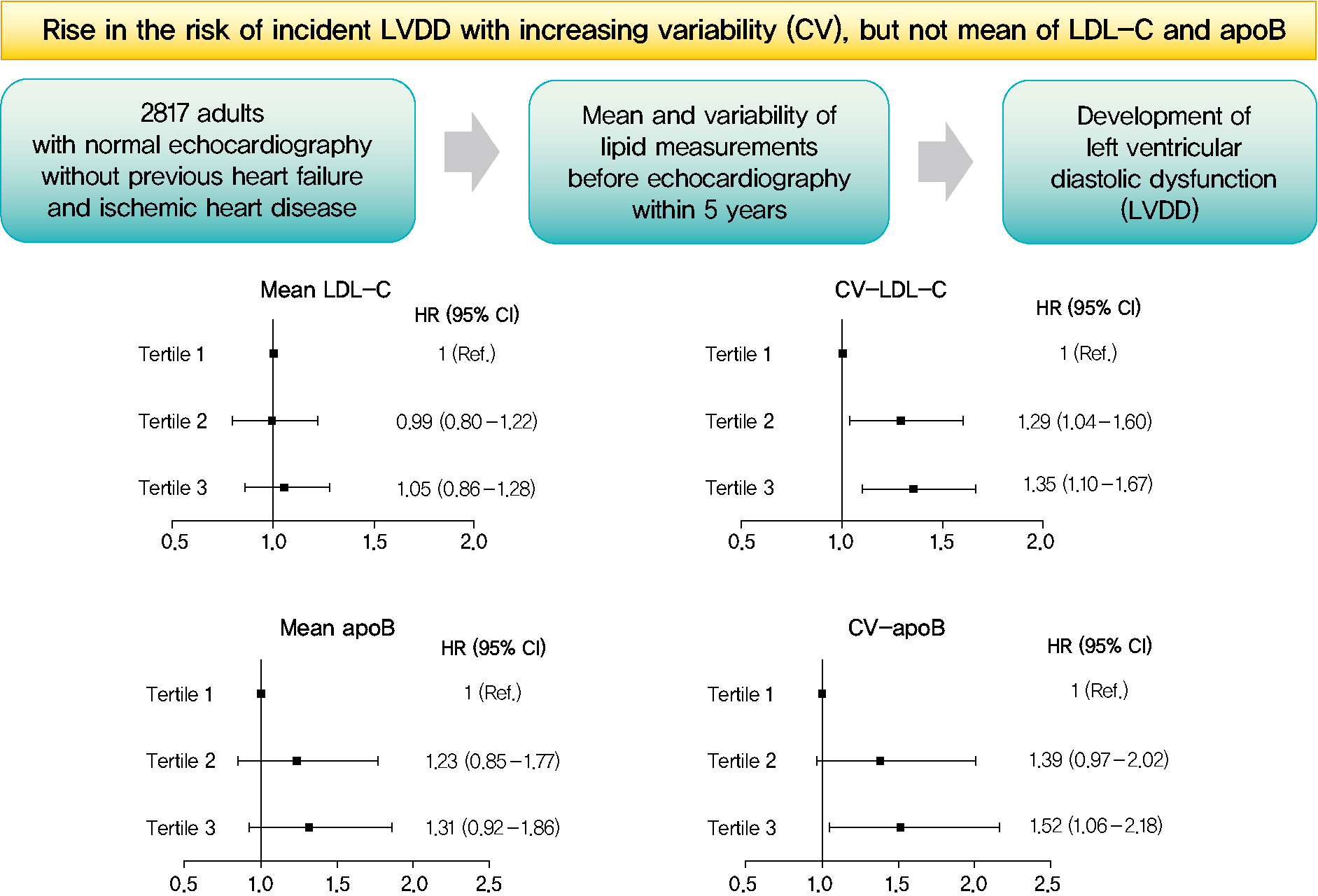
- Background
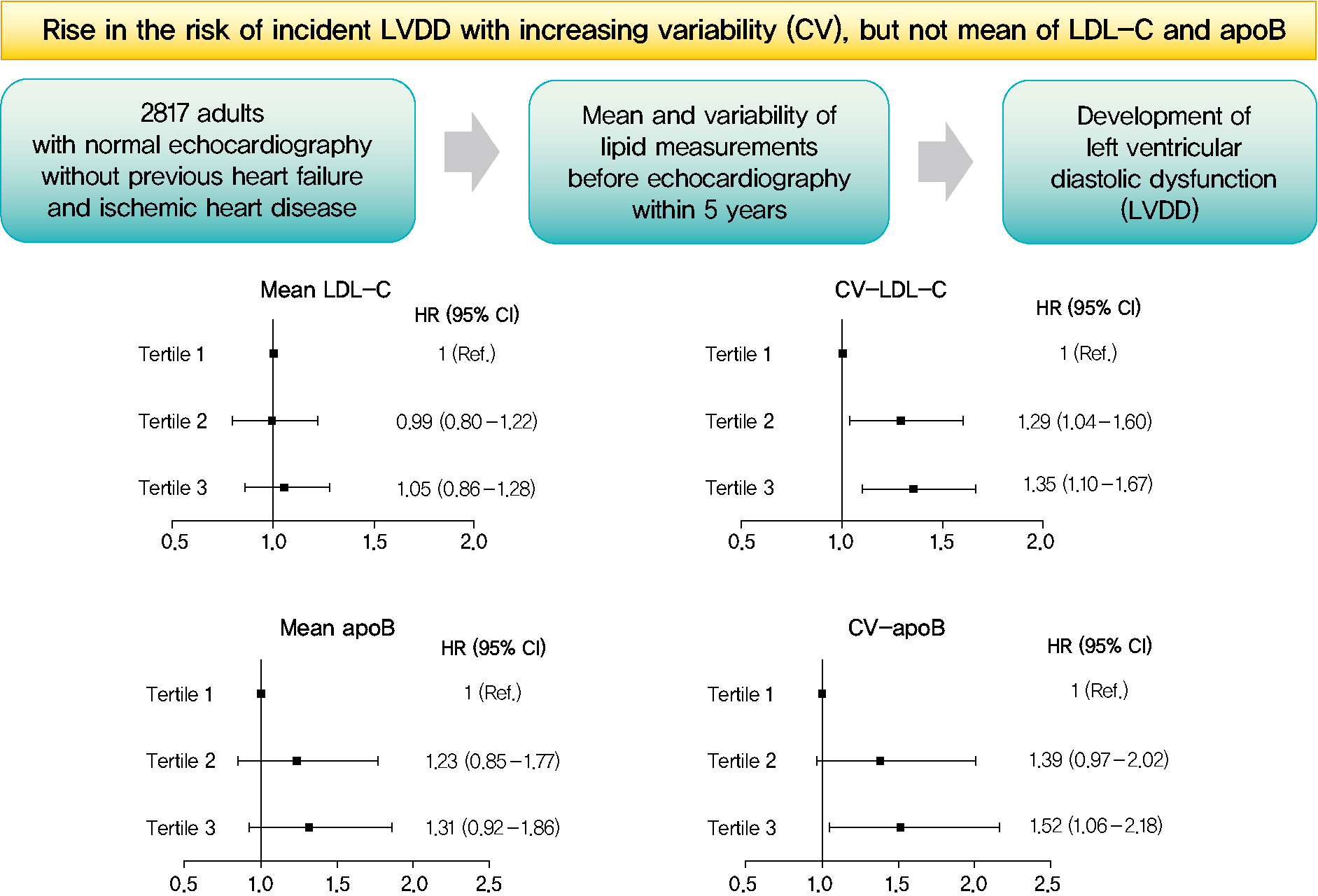
Subclinical left ventricular diastolic dysfunction (LVDD) is an emerging consequence of increased insulin resistance, and dyslipidemia is one of the few correctable risk factors of LVDD. This study evaluated the role of mean and visit-to-visit variability of lipid measurements in risk of LVDD in a healthy population.
Methods
This was a 3.7-year (interquartile range, 2.1 to 4.9) longitudinal cohort study including 2,817 adults (median age 55 years) with left ventricular ejection fraction >50% who underwent an annual or biannual health screening between January 2008 and July 2016. The mean, standard deviation (SD), coefficient of variation (CV), variability independent of the mean (VIM), and average real variability of total cholesterol, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), apolipoprotein B (apoB), non-HDL-C, and triglycerides were obtained from three to six measurements during the 5 years preceding the first echocardiogram.
Results
Among the 2,817 patients, 560 (19.9%) developed LVDD. The mean of no component of lipid measurements was associated with risk of LVDD. CV (hazard ratio [HR], 1.35; 95% confidence interval [CI], 1.10 to 1.67), SD (HR, 1.27; 95% CI, 1.03 to 1.57), and VIM (HR, 1.26; 95% CI, 1.03 to 1.55) of LDL-C and all the variability parameters of apoB were significantly associated with development of LVDD. The association between CV-LDL and risk of LVDD did not have significant interaction with sex, increasing/decreasing trend at baseline, or use of stain and/or lipid-modifying agents.
Conclusion
The variability of LDL-C and apoB, rather than their mean, was associated with risk for LVDD. -
Citations
Citations to this article as recorded by- Separate and Joint Associations of Remnant Cholesterol Accumulation and Variability With Carotid Atherosclerosis: A Prospective Cohort Study
Jinqi Wang, Rui Jin, Xiaohan Jin, Zhiyuan Wu, Haiping Zhang, Ze Han, Zongkai Xu, Yueruijing Liu, Xiaoyu Zhao, Xiuhua Guo, Lixin Tao
Journal of the American Heart Association.2023;[Epub] CrossRef - Variability of Metabolic Risk Factors: Causative Factor or Epiphenomenon?
Hye Jin Yoo
Diabetes & Metabolism Journal.2022; 46(2): 257. CrossRef
- Separate and Joint Associations of Remnant Cholesterol Accumulation and Variability With Carotid Atherosclerosis: A Prospective Cohort Study
- Cardiovascular Risk/Epidemiology
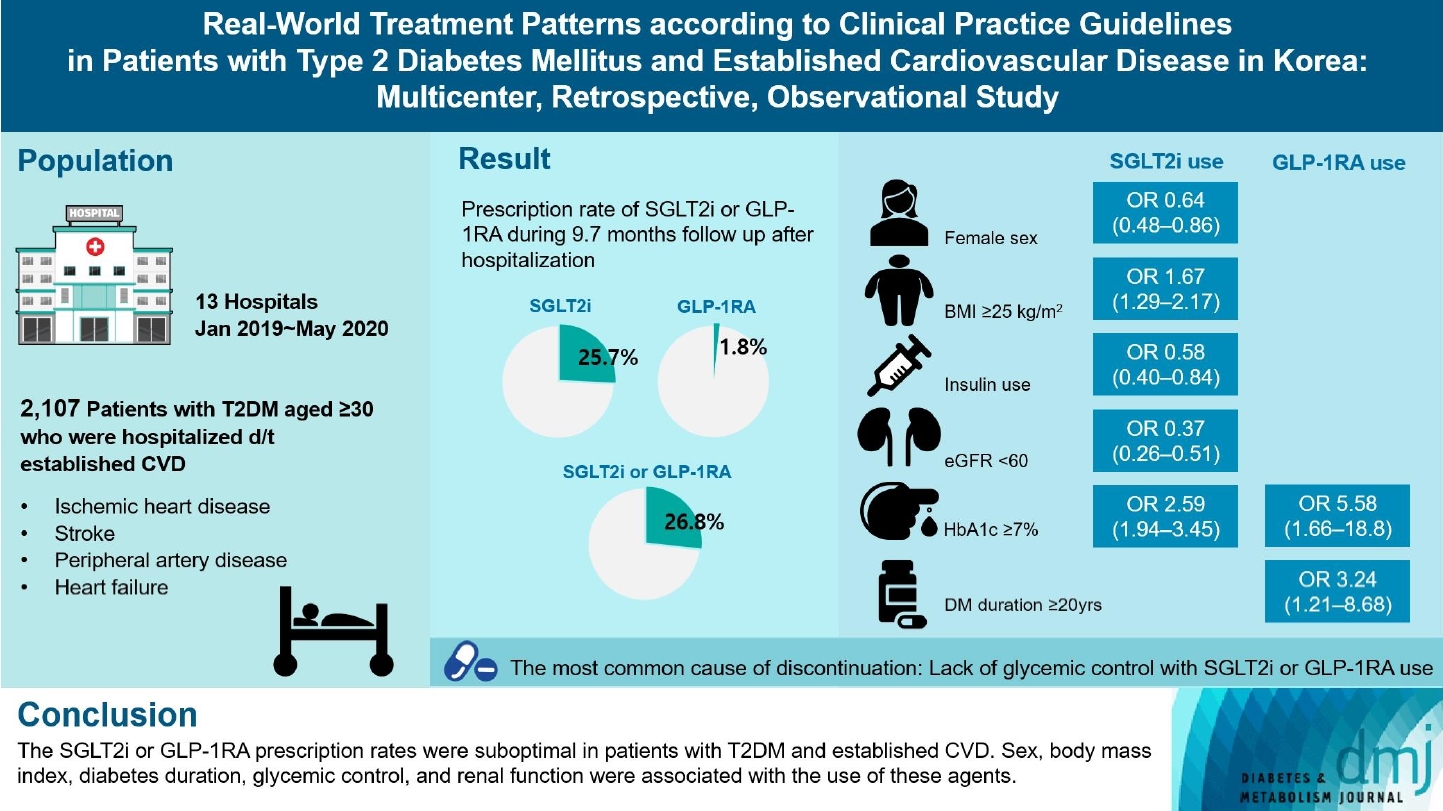
- Real-World Treatment Patterns according to Clinical Practice Guidelines in Patients with Type 2 Diabetes Mellitus and Established Cardiovascular Disease in Korea: Multicenter, Retrospective, Observational Study
- Ye Seul Yang, Nam Hoon Kim, Jong Ha Baek, Seung-Hyun Ko, Jang Won Son, Seung-Hwan Lee, Sang Youl Rhee, Soo-Kyung Kim, Tae Seo Sohn, Ji Eun Jun, In-Kyung Jeong, Chong Hwa Kim, Keeho Song, Eun-Jung Rhee, Junghyun Noh, Kyu Yeon Hur, Committee of Clinical Practice Guidelines, Korean Diabetes Association
- Diabetes Metab J. 2024;48(2):279-289. Published online January 26, 2024
- DOI: https://doi.org/10.4093/dmj.2023.0225
- 891 View
- 120 Download
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Recent diabetes management guidelines recommend that sodium-glucose cotransporter 2 inhibitors (SGLT2is) or glucagon-like peptide 1 receptor agonists (GLP-1RAs) with proven cardiovascular benefits should be prioritized for combination therapy in patients with type 2 diabetes mellitus (T2DM) and established cardiovascular disease (CVD). This study was aimed at evaluating SGLT2i or GLP-1RA usage rates and various related factors in patients with T2DM and established CVD.
Methods
We enrolled adults with T2DM aged ≥30 years who were hospitalized due to established CVD from January 2019 to May 2020 at 13 secondary and tertiary hospitals in Korea in this retrospective observational study.
Results
Overall, 2,050 patients were eligible for analysis among 2,107 enrolled patients. The mean patient age, diabetes duration, and glycosylated hemoglobin level were 70.0 years, 12.0 years, and 7.5%, respectively. During the mean follow-up duration of 9.7 months, 25.7% of the patients were prescribed SGLT2is after CVD events. However, only 1.8% were prescribed GLP-1RAs. Compared with SGLT2i non-users, SGLT2i users were more frequently male and obese. Furthermore, they had a shorter diabetes duration but showed worse glycemic control and better renal function at the time of the event. GLP-1RA users had a longer duration of diabetes and worse glycemic control at the time of the event than GLP-1RA non-users.
Conclusion
The SGLT2i or GLP-1RA prescription rates were suboptimal in patients with T2DM and established CVD. Sex, body mass index, diabetes duration, glycemic control, and renal function were associated with the use of these agents. -
Citations
Citations to this article as recorded by- Enhancing Patient Outcomes: Prioritizing SGLT2is and GLP-1RAs in Diabetes with CVD
Gwanpyo Koh
Diabetes & Metabolism Journal.2024; 48(2): 208. CrossRef
- Enhancing Patient Outcomes: Prioritizing SGLT2is and GLP-1RAs in Diabetes with CVD
- Drug/Regimen
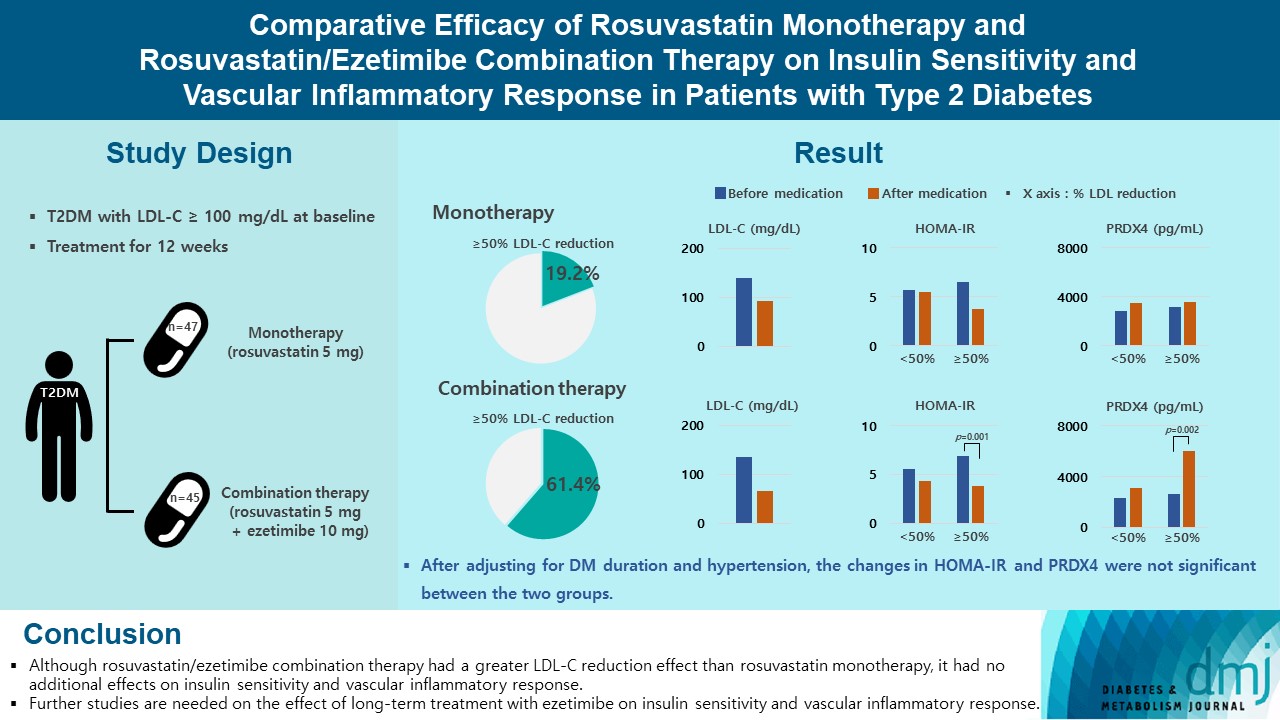
- Comparative Efficacy of Rosuvastatin Monotherapy and Rosuvastatin/Ezetimibe Combination Therapy on Insulin Sensitivity and Vascular Inflammatory Response in Patients with Type 2 Diabetes Mellitus
- Ji Hye Han, Kyong Hye Joung, Jun Choul Lee, Ok Soon Kim, Sorim Choung, Ji Min Kim, Yea Eun Kang, Hyon-Seung Yi, Ju Hee Lee, Bon Jeong Ku, Hyun Jin Kim
- Diabetes Metab J. 2024;48(1):112-121. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0402
- 1,788 View
- 209 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Type 2 diabetes mellitus (T2DM) induces endothelial dysfunction and inflammation, which are the main factors for atherosclerosis and cardiovascular disease. The present study aimed to compare the effects of rosuvastatin monotherapy and rosuvastatin/ezetimibe combination therapy on lipid profile, insulin sensitivity, and vascular inflammatory response in patients with T2DM.
Methods
A total of 101 patients with T2DM and dyslipidemia were randomized to either rosuvastatin monotherapy (5 mg/day, n=47) or rosuvastatin/ezetimibe combination therapy (5 mg/10 mg/day, n=45) and treated for 12 weeks. Serum lipids, glucose, insulin, soluble intercellular adhesion molecule-1 (sICAM-1), and peroxiredoxin 4 (PRDX4) levels were determined before and after 12 weeks of treatment.
Results
The reduction in low density lipoprotein cholesterol (LDL-C) by more than 50% from baseline after treatment was more in the combination therapy group. The serum sICAM-1 levels increased significantly in both groups, but there was no difference between the two groups. The significant changes in homeostasis model assessment of insulin resistance (HOMA-IR) and PRDX4 were confirmed only in the subgroup in which LDL-C was reduced by 50% or more in the combination therapy group. However, after adjusting for diabetes mellitus duration and hypertension, the changes in HOMA-IR and PRDX4 were not significant between the two groups.
Conclusion
Although rosuvastatin/ezetimibe combination therapy had a greater LDL-C reduction effect than rosuvastatin monotherapy, it had no additional effects on insulin sensitivity and vascular inflammatory response. Further studies are needed on the effect of long-term treatment with ezetimibe on insulin sensitivity and vascular inflammatory response. -
Citations
Citations to this article as recorded by- Combining Ezetimibe and Rosuvastatin: Impacts on Insulin Sensitivity and Vascular Inflammation in Patients with Type 2 Diabetes Mellitus
Eun Roh
Diabetes & Metabolism Journal.2024; 48(1): 55. CrossRef
- Combining Ezetimibe and Rosuvastatin: Impacts on Insulin Sensitivity and Vascular Inflammation in Patients with Type 2 Diabetes Mellitus
- Basic Research
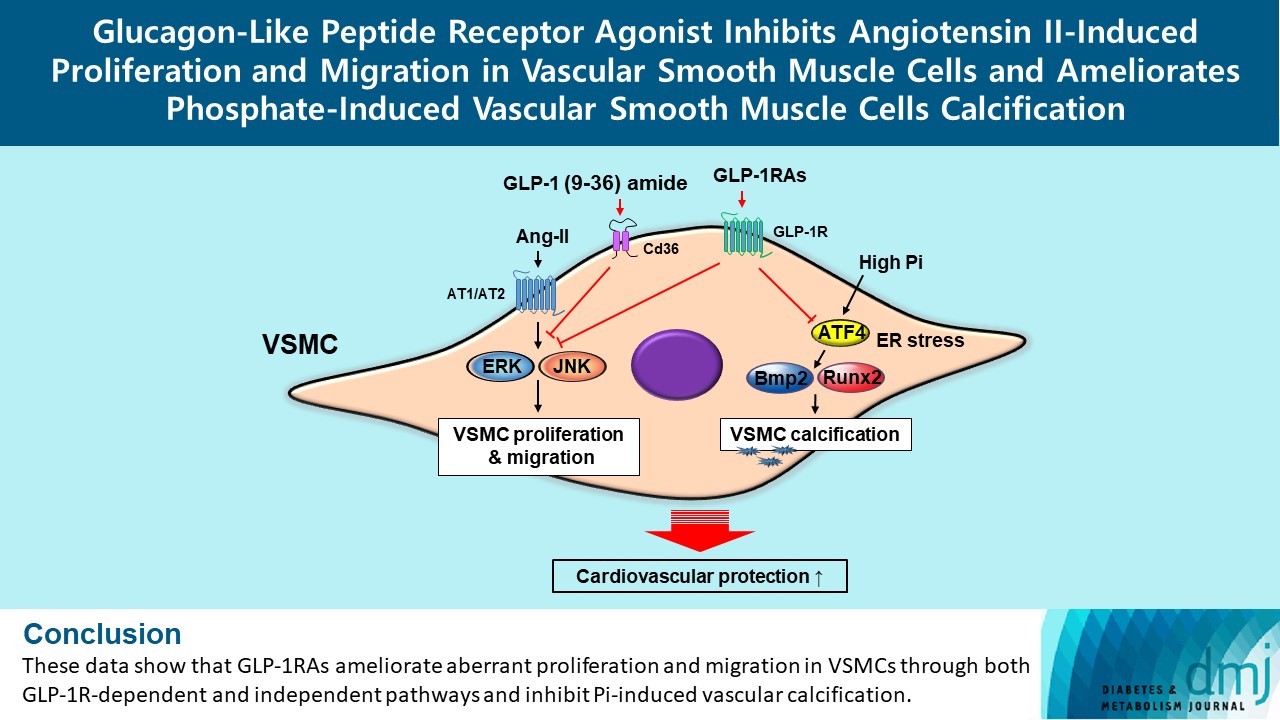
- Glucagon-Like Peptide Receptor Agonist Inhibits Angiotensin II-Induced Proliferation and Migration in Vascular Smooth Muscle Cells and Ameliorates Phosphate-Induced Vascular Smooth Muscle Cells Calcification
- Jinmi Lee, Seok-Woo Hong, Min-Jeong Kim, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Eun-Jung Rhee, Won-Young Lee
- Diabetes Metab J. 2024;48(1):83-96. Published online January 3, 2024
- DOI: https://doi.org/10.4093/dmj.2022.0363
- 1,560 View
- 164 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Glucagon-like peptide-1 receptor agonist (GLP-1RA), which is a therapeutic agent for the treatment of type 2 diabetes mellitus, has a beneficial effect on the cardiovascular system.
Methods
To examine the protective effects of GLP-1RAs on proliferation and migration of vascular smooth muscle cells (VSMCs), A-10 cells exposed to angiotensin II (Ang II) were treated with either exendin-4, liraglutide, or dulaglutide. To examine the effects of GLP-1RAs on vascular calcification, cells exposed to high concentration of inorganic phosphate (Pi) were treated with exendin-4, liraglutide, or dulaglutide.
Results
Ang II increased proliferation and migration of VSMCs, gene expression levels of Ang II receptors AT1 and AT2, proliferation marker of proliferation Ki-67 (Mki-67), proliferating cell nuclear antigen (Pcna), and cyclin D1 (Ccnd1), and the protein expression levels of phospho-extracellular signal-regulated kinase (p-Erk), phospho-c-JUN N-terminal kinase (p-JNK), and phospho-phosphatidylinositol 3-kinase (p-Pi3k). Exendin-4, liraglutide, and dulaglutide significantly decreased the proliferation and migration of VSMCs, the gene expression levels of Pcna, and the protein expression levels of p-Erk and p-JNK in the Ang II-treated VSMCs. Erk inhibitor PD98059 and JNK inhibitor SP600125 decreased the protein expression levels of Pcna and Ccnd1 and proliferation of VSMCs. Inhibition of GLP-1R by siRNA reversed the reduction of the protein expression levels of p-Erk and p-JNK by exendin-4, liraglutide, and dulaglutide in the Ang II-treated VSMCs. Moreover, GLP-1 (9-36) amide also decreased the proliferation and migration of the Ang II-treated VSMCs. In addition, these GLP-1RAs decreased calcium deposition by inhibiting activating transcription factor 4 (Atf4) in Pi-treated VSMCs.
Conclusion
These data show that GLP-1RAs ameliorate aberrant proliferation and migration in VSMCs through both GLP-1Rdependent and independent pathways and inhibit Pi-induced vascular calcification. -
Citations
Citations to this article as recorded by- Incretin Hormone Secretion in Women with Polycystic Ovary Syndrome: Roles of Obesity, Insulin Sensitivity and Treatment with Metformin and GLP-1s
Andrea Etrusco, Mislav Mikuš, Antonio D’Amato, Fabio Barra, Petar Planinić, Trpimir Goluža, Giovanni Buzzaccarini, Jelena Marušić, Mara Tešanović, Antonio Simone Laganà
Biomedicines.2024; 12(3): 653. CrossRef
- Incretin Hormone Secretion in Women with Polycystic Ovary Syndrome: Roles of Obesity, Insulin Sensitivity and Treatment with Metformin and GLP-1s

 KDA
KDA
 First
First Prev
Prev





