
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Review
- Page Path
- HOME > Article category > Review
- Others
- Continuous Glucose Monitoring Sensors for Diabetes Management: A Review of Technologies and Applications
- Giacomo Cappon, Martina Vettoretti, Giovanni Sparacino, Andrea Facchinetti
- Diabetes Metab J. 2019;43(4):383-397. Published online July 25, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0121
- 21,074 View
- 973 Download
- 176 Web of Science
- 187 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader By providing blood glucose (BG) concentration measurements in an almost continuous-time fashion for several consecutive days, wearable minimally-invasive continuous glucose monitoring (CGM) sensors are revolutionizing diabetes management, and are becoming an increasingly adopted technology especially for diabetic individuals requiring insulin administrations. Indeed, by providing glucose real-time insights of BG dynamics and trend, and being equipped with visual and acoustic alarms for hypo- and hyperglycemia, CGM devices have been proved to improve safety and effectiveness of diabetes therapy, reduce hypoglycemia incidence and duration, and decrease glycemic variability. Furthermore, the real-time availability of BG values has been stimulating the realization of new tools to provide patients with decision support to improve insulin dosage tuning and infusion. The aim of this paper is to offer an overview of current literature and future possible developments regarding CGM technologies and applications. In particular, first, we outline the technological evolution of CGM devices through the last 20 years. Then, we discuss about the current use of CGM sensors from patients affected by diabetes, and, we report some works proving the beneficial impact provided by the adoption of CGM. Finally, we review some recent advanced applications for diabetes treatment based on CGM sensors.
-
Citations
Citations to this article as recorded by- Continuous glucose monitoring metrics following sub-Tenon’s injection of triamcinolone acetonide for diabetic macular edema
Rei Sotani-Ogawa, Sentaro Kusuhara, Yushi Hirota, Kyung Woo Kim, Wataru Matsumiya, Wataru Ogawa, Makoto Nakamura
Graefe's Archive for Clinical and Experimental Ophthalmology.2024; 262(2): 449. CrossRef - Identifying and mapping measures of medication safety during transfer of care in a digital era: a scoping literature review
Catherine Leon, Helen Hogan, Yogini H Jani
BMJ Quality & Safety.2024; 33(3): 173. CrossRef - Highly sensitive and stable glucose sensing using N-type conducting polymer based organic electrochemical transistor
Gang Zhou, Zhu Cao, Yangxuan Liu, Haoyu Zheng, Kai Xu
Journal of Electroanalytical Chemistry.2024; 952: 117961. CrossRef - Effectiveness and User Perception of an In-Vehicle Voice Warning for Hypoglycemia: Development and Feasibility Trial
Caterina Bérubé, Vera Franziska Lehmann, Martin Maritsch, Mathias Kraus, Stefan Feuerriegel, Felix Wortmann, Thomas Züger, Christoph Stettler, Elgar Fleisch, A Baki Kocaballi, Tobias Kowatsch
JMIR Human Factors.2024; 11: e42823. CrossRef - Can Electrochemical Aptasensors Achieve the Commercial Success of Glucose Biosensors?
Sina Ardalan, Anna Ignaszak
Advanced Sensor Research.2024;[Epub] CrossRef - Digital Health and Machine Learning Technologies for Blood Glucose Monitoring and Management of Gestational Diabetes
Huiqi Y. Lu, Xiaorong Ding, Jane E. Hirst, Yang Yang, Jenny Yang, Lucy Mackillop, David A. Clifton
IEEE Reviews in Biomedical Engineering.2024; 17: 98. CrossRef - Effects of Digitization of Self-Monitoring of Blood Glucose Records Using a Mobile App and the Cloud System on Outpatient Management of Diabetes: Single-Armed Prospective Study
Tomoko Handa, Takeshi Onoue, Tomoko Kobayashi, Ryutaro Maeda, Keigo Mizutani, Ayana Yamagami, Tamaki Kinoshita, Yoshinori Yasuda, Shintaro Iwama, Takashi Miyata, Mariko Sugiyama, Hiroshi Takagi, Daisuke Hagiwara, Hidetaka Suga, Ryoichi Banno, Yoshinori Az
JMIR Diabetes.2024; 9: e48019. CrossRef - The Association of Macronutrient Consumption and BMI to Exhaled Carbon Dioxide in Lumen Users: Retrospective Real-World Study
Shlomo Yeshurun, Tomer Cramer, Daniel Souroujon, Merav Mor
JMIR mHealth and uHealth.2024; 12: e56083. CrossRef - Generative adversarial network-based data augmentation for improving hypoglycemia prediction: A proof-of-concept study
Wonju Seo, Namho Kim, Sung-Woon Park, Sang-Man Jin, Sung-Min Park
Biomedical Signal Processing and Control.2024; 92: 106077. CrossRef - Pre‐dinner walks may be superior to post‐dinner walks for glucose time in range in adults with type 1 diabetes on hybrid closed‐loop insulin delivery systems
Lauren V. Turner, Michael C. Riddell
Diabetes, Obesity and Metabolism.2024;[Epub] CrossRef - Real-world effectiveness of GLP-1 receptor agonist-based treatment strategies on “time in range” in patients with type 2 diabetes
Yongru Chen, Jingxian Chen, Shuo Zhang, Dan Zhu, Feiying Deng, Rui Zuo, Yufei Hu, Yue Zhao, Yale Duan, Benwei Lin, Fengwu Chen, Yun Liang, Jiaxiong Zheng, Barkat Ali Khan, Kaijian Hou
Frontiers in Pharmacology.2024;[Epub] CrossRef - Utility of Flash Glucose Monitoring to Determine Glucose Variation Induced by Different Doughs in Persons with Type 2 Diabetes
Maria Antonietta Taras, Sara Cherchi, Ilaria Campesi, Valentina Margarita, Gavino Carboni, Paola Rappelli, Giancarlo Tonolo
Diabetology.2024; 5(1): 129. CrossRef - Facile chemiresistive biosensor functionalized with PANI/GOx and novel green synthesized silver nanoparticles for glucose sensing
Jitendra B. Zalke, N.P. Narkhede, Dinesh R. Rotake, Shiv Govind Singh
Microchemical Journal.2024; 200: 110339. CrossRef - A novel questionnaire for evaluating digital tool use (DTUQ-D) among individuals with type 2 diabetes: exploring the digital landscape
Ora Peleg, Efrat Hadar, Meyran Boniel-Nissim
Frontiers in Public Health.2024;[Epub] CrossRef - Development of a Novel Insulin Sensor for Clinical Decision-Making
Eva Vargas, Eleonora M. Aiello, Jordan E. Pinsker, Hazhir Teymourian, Farshad Tehrani, Mei Mei Church, Lori M. Laffel, Francis J. Doyle, Mary-Elizabeth Patti, Eyal Dassau, Joseph Wang
Journal of Diabetes Science and Technology.2023; 17(4): 1029. CrossRef - Diabetes technology and sexual health: which role?
V. Zamponi, J. Haxhi, G. Pugliese, A. Faggiano, R. Mazzilli
Journal of Endocrinological Investigation.2023;[Epub] CrossRef - Discordance Between Glycated Hemoglobin A1c and the Glucose Management Indicator in People With Diabetes and Chronic Kidney Disease
Philippe Oriot, Claire Viry, Antoine Vandelaer, Sébastien Grigioni, Malanie Roy, Jean Christophe Philips, Gaëtan Prévost
Journal of Diabetes Science and Technology.2023; 17(6): 1553. CrossRef - Expertenaustausch zum Einsatz von kontinuierlichem Glukosemonitoring (CGM) im Diabetesmanagement: Eine aktuelle Bestandsaufnahme und Blick in die Zukunft
Andreas Thomas, Thomas Haak, Astrid Tombek, Bernhard Kulzer, Dominic Ehrmann, Olga Kordonouri, Jens Kroeger, Oliver Schubert-Olesen, Ralf Kolassa, Thorsten Siegmund, Nicola Haller, Lutz Heinemann
Diabetologie und Stoffwechsel.2023; 18(01): 57. CrossRef - Evaluation of the performance and usability of a novel continuous glucose monitoring system
Li Yan, Qiang Li, Qingbo Guan, Mingsong Han, Yu Zhao, Junfei Fang, Jiajun Zhao
International Journal of Diabetes in Developing Countries.2023; 43(4): 551. CrossRef - Efficacy of intermittent short‐term use of a real‐time continuous glucose monitoring system in non‐insulin–treated patients with type 2 diabetes: A randomized controlled trial
Sun Joon Moon, Kyung‐Soo Kim, Woo Je Lee, Mi Yeon Lee, Robert Vigersky, Cheol‐Young Park
Diabetes, Obesity and Metabolism.2023; 25(1): 110. CrossRef - Intermittent-scanned continuous glucose monitoring with low glucose alarms decreases hypoglycemia incidence in middle-aged adults with type 1 diabetes in real-life setting
Philippe Oriot, Michel P. Hermans
Journal of Diabetes and its Complications.2023; 37(2): 108385. CrossRef - Applications of Microwaves in Medicine
J.-C. Chiao, Changzhi Li, Jenshan Lin, Robert H. Caverly, James C. M. Hwang, Harel Rosen, Arye Rosen
IEEE Journal of Microwaves.2023; 3(1): 134. CrossRef - A Double-Needle Gold-Silver Electrodes Continuous Glucose Monitoring Device
C. Ben Ali Hassine, A. Tekin
IRBM.2023; 44(3): 100752. CrossRef - Accuracy of Flash Glucose Monitoring in Hemodialysis Patients With
and Without Diabetes Mellitus
Michèle R. Weber, Matthias Diebold, Peter Wiesli, Andreas D. Kistler
Experimental and Clinical Endocrinology & Diabetes.2023; 131(03): 132. CrossRef - Minimally invasive electrochemical continuous glucose monitoring sensors: Recent progress and perspective
Yuanyuan Zou, Zhengkang Chu, Jiuchuan Guo, Shan Liu, Xing Ma, Jinhong Guo
Biosensors and Bioelectronics.2023; 225: 115103. CrossRef - Continuous Glucose Monitoring in Enterally Fed Children with Severe Central Nervous System Impairment
Marlena Górska, Joanna Kudzin, Anna Borkowska, Agnieszka Szlagatys-Sidorkiewicz, Agnieszka Szadkowska, Małgorzata Myśliwiec, Ewa Toporowska-Kowalska
Nutrients.2023; 15(3): 513. CrossRef - Prevalence of type 2 diabetes complications and its association with diet knowledge and skills and self‐care barriers in Tabriz, Iran: A cross‐sectional study
Habib Jalilian, Elnaz Javanshir, Leila Torkzadeh, Saeedeh Fehresti, Nazanin Mir, Majid Heidari‐Jamebozorgi, Somayeh Heydari
Health Science Reports.2023;[Epub] CrossRef - Status of continuous glucose monitoring use and management in tertiary hospitals of China: a cross-sectional study
Liping Chen, Xiaoqin Liu, Qin Lin, Hongmei Dai, Yong Zhao, Zumin Shi, Liping Wu
BMJ Open.2023; 13(2): e066801. CrossRef - Diboronic-Acid-Based Electrochemical Sensor for Enzyme-Free Selective and Sensitive Glucose Detection
Joong-Hyun Kim, Hongsik Choi, Chul-Soon Park, Heung-Seop Yim, Dongguk Kim, Sungmin Lee, Yeonkeong Lee
Biosensors.2023; 13(2): 248. CrossRef - Artificial intelligence biosensors for continuous glucose monitoring
Xiaofeng Jin, Andrew Cai, Tailin Xu, Xueji Zhang
Interdisciplinary Materials.2023; 2(2): 290. CrossRef - Continuous Glucose Monitoring in Dogs and Cats
Francesca Del Baldo, Federico Fracassi
Veterinary Clinics of North America: Small Animal Practice.2023; 53(3): 591. CrossRef - Accurate Post-Calibration Predictions for Noninvasive Glucose Measurements in People Using Confocal Raman Spectroscopy
Anders Pors, Kaspar G. Rasmussen, Rune Inglev, Nina Jendrike, Amalie Philipps, Ajenthen G. Ranjan, Vibe Vestergaard, Jan E. Henriksen, Kirsten Nørgaard, Guido Freckmann, Karl D. Hepp, Michael C. Gerstenberg, Anders Weber
ACS Sensors.2023; 8(3): 1272. CrossRef - Diabetes mellitus in der Akut- und Notfallmedizin
Leo Benning, Julian Krehl, Felix Patricius Hans
Notfallmedizin up2date.2023; 18(01): 45. CrossRef - Empowering People with Diabetes: Role of Continuous Glucose Monitor Systems
Sneha B Srivastava
American Journal of Lifestyle Medicine.2023; 17(3): 359. CrossRef - Diabétologie connectée : quelles sont les attentes des médecins et des patients ?
Nicolas Naïditch, Jean-Pierre Riveline
Médecine des Maladies Métaboliques.2023; 17(2): 2S3. CrossRef - Association of Vibrotactile Biofeedback With Reduced Ergonomic Risk for Surgeons During Tonsillectomy
Natalie A. Kelly, Abdulrahman Althubaiti, Aashika D. Katapadi, Adam G. Smith, Sarah C. Nyirjesy, Jane H. Yu, Amanda J. Onwuka, Tendy Chiang
JAMA Otolaryngology–Head & Neck Surgery.2023; 149(5): 397. CrossRef - The Evolution of Diabetes Technology – Options Toward Personalized Care
Maleeha Zahid, Samaneh Dowlatshahi, Abhishek H. Kansara, Archana R. Sadhu
Endocrine Practice.2023; 29(8): 653. CrossRef - A Personalized and Adaptive Insulin Bolus Calculator Based on Double Deep Q- Learning to Improve Type 1 Diabetes Management
Giulia Noaro, Taiyu Zhu, Giacomo Cappon, Andrea Facchinetti, Pantelis Georgiou
IEEE Journal of Biomedical and Health Informatics.2023; 27(5): 2536. CrossRef - Celebrating a Century of Insulin Discovery: A Critical Appraisal of the
Emerging Alternative Insulin Delivery Systems
Ntethelelo Sibiya, Bonisiwe Mbatha, Phikelelani Ngubane, Andile Khathi
Current Drug Delivery.2023; 20(6): 656. CrossRef - Machine Learning–Based Time in Patterns for Blood Glucose Fluctuation Pattern Recognition in Type 1 Diabetes Management: Development and Validation Study
Nicholas Berin Chan, Weizi Li, Theingi Aung, Eghosa Bazuaye, Rosa M Montero
JMIR AI.2023; 2: e45450. CrossRef - Drug Delivery Systems for Personal Healthcare by Smart Wearable Patch System
Bikram Khadka, Byeongmoon Lee, Ki-Taek Kim
Biomolecules.2023; 13(6): 929. CrossRef - Wearable Electrochemical Glucose Sensors in Diabetes Management: A Comprehensive Review
Tamoghna Saha, Rafael Del Caño, Kuldeep Mahato, Ernesto De la Paz, Chuanrui Chen, Shichao Ding, Lu Yin, Joseph Wang
Chemical Reviews.2023; 123(12): 7854. CrossRef - Real-life 24-week changes in glycemic parameters among European users of flash glucose monitoring with type 1 and 2 diabetes and different levels of glycemic control
Annel Lameijer, Julia J. Bakker, Kalvin Kao, Yongjin Xu, Rijk O.B. Gans, Henk J.G. Bilo, Timothy C. Dunn, Peter R. van Dijk
Diabetes Research and Clinical Practice.2023; 201: 110735. CrossRef - Les médicaments anti-diabétiques : ce que le médecin anesthésiste réanimateur doit savoir
Michael Joubert
Anesthésie & Réanimation.2023; 9(3): 251. CrossRef - Glycemia control using remote technologies
L. A. Suplotova, O. O. Alieva
Meditsinskiy sovet = Medical Council.2023; 17(9): 81. CrossRef - Data-enabled learning and control algorithms for intelligent glucose management: The state of the art
Deheng Cai, Wenjing Wu, Marzia Cescon, Wei Liu, Linong Ji, Dawei Shi
Annual Reviews in Control.2023; 56: 100897. CrossRef - A Markov Model of Gap Occurrence in Continuous Glucose Monitoring Data for Realistic in Silico Clinical Trials
Martina Vettoretti, Martina Drecogna, Simone Del Favero, Andrea Facchinetti, Giovanni Sparacino
Computer Methods and Programs in Biomedicine.2023; 240: 107700. CrossRef - Volumetric Electron Transfer from Metabolites to Chemically Doped Polymer Electrodes
Siew Ting Melissa Tan, Gijun Lee, Kalee Rozylowicz, Adam Marks, Alberto Salleo
Advanced Functional Materials.2023;[Epub] CrossRef - Diabetes and hypertension MobileHealth systems: a review of general challenges and advancements
Bliss Utibe-Abasi Stephen, Benedicta C. Uzoewulu, Phillip Michael Asuquo, Simeon Ozuomba
Journal of Engineering and Applied Science.2023;[Epub] CrossRef - THE ASSESSMENT OF COMPENSATION OF CARBOHYDRATE METABOLISM IN PATIENTS WITH TYPE 2 DIABETES MELLITUS WITH METABOLIC SYNDROME BEYOND THE LIMITS OF GLYCATED HEMOGLOBIN
Taras V. Romaniv, Nadiya V. Skrypnyk, Ulyana V. Synko, Nataliia M. Voronych-Semchenko, Oleh V. Melnyk, Anna O. Hryb, Igor B. Boruchok
Wiadomości Lekarskie.2023; 76(6): 1385. CrossRef - Pros and cons of continous glucose monitoring
Marcin Ciechański, Edyta Witkowska, Agnieszka Ostańska, Adrianna Szafran, Klaudia Wiśniewska, Laura Piasek, Grzegorz Godek, Kacper Więcław, Katarzyna Stańko, Wiktor Terelak
Journal of Medical Science.2023;[Epub] CrossRef - Continuous Glucose Monitoring by Insulin-Treated Pilots Flying Commercial Aircraft Within the ARA.MED.330 Diabetes Protocol: A Preliminary Feasibility Study
Gillian L. Garden, Fariba Shojaee-Moradie, Ewan J. Hutchison, Brian M. Frier, Kenneth M. Shaw, Simon R. Heller, Gerd Koehler, Julia K. Mader, Declan Maher, Graham A. Roberts, David L. Russell-Jones
Diabetes Technology & Therapeutics.2023; 25(8): 543. CrossRef - Importance of continuous glucose monitoring in the treatment of diabetes mellitus
Sun Joon Moon, Won-Young Lee
Journal of the Korean Medical Association.2023; 66(7): 432. CrossRef - DiaTrend: A dataset from advanced diabetes technology to enable development of novel analytic solutions
Temiloluwa Prioleau, Abigail Bartolome, Richard Comi, Catherine Stanger
Scientific Data.2023;[Epub] CrossRef - Testing the Real-World Accuracy of the Dexcom G6 Pro CGM During the Insulin-Only Bionic Pancreas Pivotal Trial
Martin Chase Marak, Peter Calhoun, Edward R. Damiano, Steven J. Russell, Katrina J. Ruedy, Roy W. Beck
Diabetes Technology & Therapeutics.2023; 25(11): 817. CrossRef - Use of continuous glucose monitoring in pediatric gastroenterology allows for personalized nutrition support care – Potential for collaboration between pediatric endocrinologists and gastroenterologists
Kathryn Hitchcock, Stephanie Oliveira
Journal of Pediatric Endocrinology and Diabetes.2023; 3: 34. CrossRef - Anti-biofouling strategies for implantable biosensors of continuous glucose monitoring systems
Yan Zheng, Dunyun Shi, Zheng Wang
Frontiers of Chemical Science and Engineering.2023; 17(12): 1866. CrossRef - A novel strategy for therapeutic drug monitoring: application of biosensors to quantify antimicrobials in biological matrices
Quanfang Wang, Sihan Li, Jiaojiao Chen, Luting Yang, Yulan Qiu, Qian Du, Chuhui Wang, Mengmeng Teng, Taotao Wang, Yalin Dong
Journal of Antimicrobial Chemotherapy.2023; 78(11): 2612. CrossRef - Hypoglycemic Effect of an Herbal Decoction (Modified Gangsimtang) in a Patient with Severe Type 2 Diabetes Mellitus Refusing Oral Anti-Diabetic Medication: A Case Report
Sungjun Joo, Hyonjun Chun, Jisu Lee, Seungmin Seo, Jungmin Lee, Jungtae Leem
Medicina.2023; 59(11): 1919. CrossRef - GluGAN: Generating Personalized Glucose Time Series Using Generative Adversarial Networks
Taiyu Zhu, Kezhi Li, Pau Herrero, Pantelis Georgiou
IEEE Journal of Biomedical and Health Informatics.2023; 27(10): 5122. CrossRef - Millifluidic valves and pumps made of tape and plastic
Josue U. Amador-Hernandez, Pablo E. Guevara-Pantoja, Diana F. Cedillo-Alcantar, Gabriel A. Caballero-Robledo, Jose L. Garcia-Cordero
Lab on a Chip.2023; 23(20): 4579. CrossRef - Offline Deep Reinforcement Learning and Off-Policy Evaluation for Personalized Basal Insulin Control in Type 1 Diabetes
Taiyu Zhu, Kezhi Li, Pantelis Georgiou
IEEE Journal of Biomedical and Health Informatics.2023; 27(10): 5087. CrossRef - Flash Glucose Monitoring in Croatia: The Optimal Number of Scans per Day to Achieve Good Glycemic Control in Type 1 Diabetes
Silvija Canecki-Varzic, Ivana Prpic-Krizevac, Maja Cigrovski Berkovic, Dario Rahelic, Ema Schonberger, Marina Gradiser, Ines Bilic-Curcic
Medicina.2023; 59(11): 1893. CrossRef - The importance of interpreting machine learning models for blood glucose prediction in diabetes: an analysis using SHAP
Francesco Prendin, Jacopo Pavan, Giacomo Cappon, Simone Del Favero, Giovanni Sparacino, Andrea Facchinetti
Scientific Reports.2023;[Epub] CrossRef - SHMAD: A Smart Health Care System to Monitor Alzheimer’s Disease Patients
Shabana R. Ziyad, May Altulyan, Meshal Alharbi
Journal of Alzheimer's Disease.2023; 95(4): 1545. CrossRef - Séquelles fonctionnelles après résection pancréatique carcinologique. Un sujet d’actualité pour les patients et les praticiens
Andrea Mulliri, Michael Joubert, Marie-Astrid Piquet, Arnaud Alves, Benoît Dupont
Journal de Chirurgie Viscérale.2023; 160(6): 470. CrossRef - Functional sequelae after pancreatic resection for cancer
Andrea Mulliri, Michael Joubert, Marie-Astrid Piquet, Arnaud Alves, Benoît Dupont
Journal of Visceral Surgery.2023; 160(6): 427. CrossRef - Characteristics of glucose change in diabetes mellitus generalized through continuous wavelet transform processing: A preliminary study
Yoichi Nakamura, Shinya Furukawa
World Journal of Diabetes.2023; 14(10): 1562. CrossRef - Evaluating passive physiological data collection during Spravato treatment
Todd M. Solomon, Matus Hajduk, Martin Majernik, Jamileh Jemison, Alexander Deschamps, Jenna Scoggins, Adam Kolar, Miguel Amável Pinheiro, Peter Dubec, Ondrej Skala, Owen Muir, Amanda Tinkelman, Daniel R. Karlin, Robert Barrow
Frontiers in Digital Health.2023;[Epub] CrossRef - Fabrication of conductive Ag/AgCl/Ag nanorods ink on Laser-induced graphene electrodes on flexible substrates for non-enzymatic glucose detection
Rana Bagheri, Saeid Alikhani, Ebrahim Miri-Moghaddam
Scientific Reports.2023;[Epub] CrossRef - Co-design of Human-centered, Explainable AI for Clinical Decision Support
Cecilia Panigutti, Andrea Beretta, Daniele Fadda, Fosca Giannotti, Dino Pedreschi, Alan Perotti, Salvatore Rinzivillo
ACM Transactions on Interactive Intelligent Systems.2023; 13(4): 1. CrossRef - Analysis of blood glucose monitoring – a review on recent advancements and future prospects
Gayathri Priyadarshini R, Sathiya Narayanan
Multimedia Tools and Applications.2023;[Epub] CrossRef - Nafion based biosensors: a review of recent advances and applications
Roya Mohammadzadeh Kakhki
International Journal of Polymeric Materials and Polymeric Biomaterials.2023; : 1. CrossRef - Overview of modern sensors for continuous glucose monitoring
K. T. Momynaliev, M. V. Prokopiev, I. V. Ivanov
Diabetes mellitus.2023; 26(6): 575. CrossRef - A Prospective Multicenter Clinical Performance Evaluation of the C-CGM System
Mihailo Rebec, Kevin Cai, Ralph Dutt-Ballerstadt, Ellen Anderson
Journal of Diabetes Science and Technology.2022; 16(2): 390. CrossRef - Perceived Burdens and Benefits Associated With Continuous Glucose Monitor Use in Type 1 Diabetes Across the Lifespan
Vidita Divan, Margaret Greenfield, Christopher P. Morley, Ruth S. Weinstock
Journal of Diabetes Science and Technology.2022; 16(1): 88. CrossRef - Technologies for Diabetes Self-Monitoring: A Scoping Review and Assessment Using the REASSURED Criteria
Jessica Hanae Zafra-Tanaka, David Beran, Beatrice Vetter, Rangarajan Sampath, Antonio Bernabe-Ortiz
Journal of Diabetes Science and Technology.2022; 16(4): 962. CrossRef - Temporal Trends for Diabetes Management and Glycemic Control Between 2010 and 2019 in Korean Children and Adolescents with Type 1 Diabetes
Jaewon Choe, Seung Hyun Won, Yunsoo Choe, Sang Hee Park, Yun Jeong Lee, Jieun Lee, Young Ah Lee, Han Hyuk Lim, Jae-Ho Yoo, Seong Yong Lee, Eun Young Kim, Choong Ho Shin, Jae Hyun Kim
Diabetes Technology & Therapeutics.2022; 24(3): 201. CrossRef - International comparison of glycaemic control in people with type 1 diabetes: an update and extension
Regina Prigge, John A. McKnight, Sarah H. Wild, Aveni Haynes, Timothy W. Jones, Elizabeth A. Davis, Birgit Rami‐Merhar, Maria Fritsch, Christine Prchla, Astrid Lavens, Kris Doggen, Suchsia Chao, Ronnie Aronson, Ruth Brown, Else H. Ibfelt, Jannet Svensson,
Diabetic Medicine.2022;[Epub] CrossRef - Artificial intelligence perspective in the future of endocrine diseases
Mandana Hasanzad, Hamid Reza Aghaei Meybodi, Negar Sarhangi, Bagher Larijani
Journal of Diabetes & Metabolic Disorders.2022; 21(1): 971. CrossRef - Telehealth Technologies and Their Benefits to People With Diabetes
Chinenye O. Usoh, Kristine Kilen, Carolyn Keyes, Crystal Paige Johnson, Joseph A. Aloi
Diabetes Spectrum.2022; 35(1): 8. CrossRef - Acetylated Trifluoromethyl Diboronic Acid Anthracene with a Large Stokes Shift and Long Excitation Wavelength as a Glucose-Selective Probe
Hongsik Choi, Inhyeok Song, Chul Soon Park, Heung-seop Yim, Joong Hyun Kim
Applied Sciences.2022; 12(6): 2782. CrossRef - Suitability of the Unified Theory of Acceptance and Use of Technology 2 Model for Predicting mHealth Acceptance Using Diabetes as an Example: Qualitative Methods Triangulation Study
Patrik Schretzlmaier, Achim Hecker, Elske Ammenwerth
JMIR Human Factors.2022; 9(1): e34918. CrossRef - Continuous Glucose Monitoring System Based on Percutaneous Microneedle Array
Ming-Nan Chien, Yu-Jen Chen, Chin-Han Bai, Jung-Tung Huang
Micromachines.2022; 13(3): 478. CrossRef - Impact of COVID-19 Lockdown on the Metabolic Control Parameters in Patients with Diabetes Mellitus: A Systematic Review and Meta-Analysis
Ifan Ali Wafa, Nando Reza Pratama, Nurizzah Farahiyah Sofia, Elsha Stephanie Anastasia, Tiffany Konstantin, Maharani Ayuputeri Wijaya, M. Rifqi Wiyono, Lilik Djuari, Hermina Novida
Diabetes & Metabolism Journal.2022; 46(2): 260. CrossRef - Expert Roundtable on Continuous Glucose Monitoring
Cheryl Rosenfeld, Thomas Blevins, Grazia Aleppo, Gregory Forlenza, Diana Isaacs, Javier Morales, Jane Seley, Jeffrey Unger
Endocrine Practice.2022; 28(6): 622. CrossRef - Glucose variability and predicted cardiovascular risk after gastrectomy
Jun Shibamoto, Takeshi Kubota, Takuma Ohashi, Hirotaka Konishi, Atsushi Shiozaki, Hitoshi Fujiwara, Kazuma Okamoto, Eigo Otsuji
Surgery Today.2022; 52(11): 1634. CrossRef - Efficacy of once-weekly tirzepatide versus once-daily insulin degludec on glycaemic control measured by continuous glucose monitoring in adults with type 2 diabetes (SURPASS-3 CGM): a substudy of the randomised, open-label, parallel-group, phase 3 SURPASS
Tadej Battelino, Richard M Bergenstal, Angel Rodríguez, Laura Fernández Landó, Ross Bray, Zhentao Tong, Katelyn Brown
The Lancet Diabetes & Endocrinology.2022; 10(6): 407. CrossRef - Towards the Integration of an Islet-Based Biosensor in Closed-Loop Therapies for Patients With Type 1 Diabetes
Loïc Olçomendy, Louis Cassany, Antoine Pirog, Roberto Franco, Emilie Puginier, Manon Jaffredo, David Gucik-Derigny, Héctor Ríos, Alejandra Ferreira de Loza, Julien Gaitan, Matthieu Raoux, Yannick Bornat, Bogdan Catargi, Jochen Lang, David Henry, Sylvie Re
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effect of divergent continuous glucose monitoring technologies on glycaemic control in type 1 diabetes mellitus: A systematic review and meta‐analysis of randomised controlled trials
Mona Elbalshy, Jillian Haszard, Hazel Smith, Sarahmarie Kuroko, Barbara Galland, Nick Oliver, Viral Shah, Martin I. de Bock, Benjamin J. Wheeler
Diabetic Medicine.2022;[Epub] CrossRef - Novel Glycemic Index Based on Continuous Glucose Monitoring to Predict Poor Clinical Outcomes in Critically Ill Patients: A Pilot Study
Eun Yeong Ha, Seung Min Chung, Il Rae Park, Yin Young Lee, Eun Young Choi, Jun Sung Moon
Frontiers in Endocrinology.2022;[Epub] CrossRef - Selection of Noninvasive Features in Wrist-Based Wearable Sensors to Predict Blood Glucose Concentrations Using Machine Learning Algorithms
Brian Bogue-Jimenez, Xiaolei Huang, Douglas Powell, Ana Doblas
Sensors.2022; 22(9): 3534. CrossRef - Generation of post-meal insulin correction boluses in type 1 diabetes simulation models for in-silico clinical trials: More realistic scenarios obtained using a decision tree approach
N. Camerlingo, M. Vettoretti, S. Del Favero, A. Facchinetti, P. Choudhary, G. Sparacino
Computer Methods and Programs in Biomedicine.2022; 221: 106862. CrossRef - A Miniaturized Optofluidic Glucose Monitoring System Based on Enzyme Colorimetry
Qingmei Xu, Chongwei Zou, Chengtao Sun, Xingguo Zhang, Haixia Yu, Dachao Li
IEEE Sensors Journal.2022; 22(10): 9246. CrossRef - Use and Trends of Diabetes Self-Management Technologies: A Correlation-Based Study
Jesús Fontecha, Iván González, Alfonso Barragán, Theodore Lim, Dario Pitocco
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Nanotechnology in Diabetes Mellitus: Overview for Nurses
R Priya, Baba Vajrala
Pondicherry Journal of Nursing.2022; 15(1): 22. CrossRef - Effect of Different Glucose Monitoring Methods on Bold Glucose Control: A Systematic Review and Meta-Analysis
Yeling Wang, Congcong Zou, Han Na, Weixin Zeng, Xiaoyan Li, Xi Lou
Computational and Mathematical Methods in Medicine.2022; 2022: 1. CrossRef - Noninvasive Blood Glucose Monitoring Systems Using Near-Infrared Technology—A Review
Aminah Hina, Wala Saadeh
Sensors.2022; 22(13): 4855. CrossRef - Performance of islets of Langerhans conformally coated via an emulsion cross-linking method in diabetic rodents and nonhuman primates
Aaron A. Stock, Grisell C. Gonzalez, Sophia I. Pete, Teresa De Toni, Dora M. Berman, Alexander Rabassa, Waldo Diaz, James C. Geary, Melissa Willman, Joy M. Jackson, Noa H. DeHaseth, Noel M. Ziebarth, Anthony R. Hogan, Camillo Ricordi, Norma S. Kenyon, Ali
Science Advances.2022;[Epub] CrossRef - Review—Electrochemistry and Other Emerging Technologies for Continuous Glucose Monitoring Devices
Saroj Kumar Das, Kavya K. Nayak, P. R. Krishnaswamy, Vinay Kumar, Navakanta Bhat
ECS Sensors Plus.2022; 1(3): 031601. CrossRef - Design Strategies and Prospects in Developing Wearable Glucose Monitoring System Using Printable Organic Transistor and Microneedle: A Review
Fazliyatul Azwa Md Rezali, Norhayati Soin, Sharifah Fatmadiana Wan Muhamad Hatta, Mohamad Hazwan Mohd Daut, Muhammad Hafizuddin Al-Helmy Nouxman, Hanim Hussin
IEEE Sensors Journal.2022; 22(14): 13785. CrossRef - Review of Automated Insulin Delivery Systems for Type 1 Diabetes and Associated Time in Range Outcomes
Armaan Nallicheri, Katherine M Mahoney, Hanna A Gutow, Natalie Bellini, Diana Isaacs
Endocrinology.2022; 18(1): 27. CrossRef - Evaluation of Mesoporous TiO2 Layers as Glucose Optical Sensors
David Ortiz de Zárate, Sara Serna, Salvador Ponce-Alcántara, Jaime García-Rupérez
Sensors.2022; 22(14): 5398. CrossRef - A Prospective Study on Continuous Glucose Monitoring in Glycogen Storage Disease Type Ia: Toward Glycemic Targets
Alessandro Rossi, Annieke Venema, Petra Haarsma, Lude Feldbrugge, Rob Burghard, David Rodriguez-Buritica, Giancarlo Parenti, Maaike H Oosterveer, Terry G J Derks
The Journal of Clinical Endocrinology & Metabolism.2022; 107(9): e3612. CrossRef - Continuous glucose monitoring as a close to real life alternative to meal studies – a pilot study with a functional drink containing amino acids and chromium
Azat Samigullin, Per M. Humpert, Elin Östman
Frontiers in Medical Technology.2022;[Epub] CrossRef - An overview of recent advances in insulin delivery and wearable technology for effective management of diabetes
Sujeet Kumar Raj, M. Ravindra Babu, Sukriti Vishwas, M.V.N.L. Chaitanya, Vancha Harish, Gaurav Gupta, Dinesh Kumar Chellappan, Kamal Dua, Sachin Kumar Singh
Journal of Drug Delivery Science and Technology.2022; 75: 103728. CrossRef - Medical Certification of Pilots Through the Insulin-Treated Diabetes Mellitus Protocol at the FAA
Lynn K. Stanwyck, James R. DeVoll, Joyce Pastore, Zykevise Gamble, Anna Poe, Gabrielle V. Gui
Aerospace Medicine and Human Performance.2022; 93(8): 627. CrossRef - Rate of glycaemic control and associated factors in patients with type 2 diabetes mellitus treated with insulin-based therapy at selected hospitals in Northwest Ethiopia: a multicentre cross-sectional study
Ashenafi Kibret Sendekie, Eyayaw Ashete Belachew, Ephrem Mebratu Dagnew, Adeladlew Kassie Netere
BMJ Open.2022; 12(9): e065250. CrossRef - Glucose Profiles Assessed by Intermittently Scanned Continuous Glucose Monitoring System during the Perioperative Period of Metabolic Surgery
Kyuho Kim, Sung Hee Choi, Hak Chul Jang, Young Suk Park, Tae Jung Oh
Diabetes & Metabolism Journal.2022; 46(5): 713. CrossRef - Hypoglycemic events and glycemic control effects between NPH and premixed insulin in patients with type 2 diabetes mellitus: A real-world experience at a comprehensive specialized hospital in Ethiopia
Ashenafi Kibret Sendekie, Adeladlew Kassie Netere, Eyayaw Ashete Belachew, Rekha Samuel
PLOS ONE.2022; 17(9): e0275032. CrossRef - Continuous Glucose Monitoring for the Diagnosis of Gestational Diabetes Mellitus: A Pilot Study
Daria Di Filippo, Marrwah Ahmadzai, Melissa Han Yiin Chang, Ksana Horgan, Ru Min Ong, Justine Darling, Mahmood Akhtar, Amanda Henry, Alec Welsh, Daniela Foti
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Caring for people with diabetes
Martha M. Funnell, Katherine A. Kloss, Robin B. Nwankwo
Nursing.2022; 52(11): 26. CrossRef - Tackling the challenges of developing microneedle-based electrochemical sensors
Hilmee Abdullah, Tonghathai Phairatana, Itthipon Jeerapan
Microchimica Acta.2022;[Epub] CrossRef - A Concise and Systematic Review on Non-Invasive Glucose Monitoring for Potential Diabetes Management
Soumyasanta Laha, Aditi Rajput, Suvra S. Laha, Rohan Jadhav
Biosensors.2022; 12(11): 965. CrossRef - Assessment of Seasonal Stochastic Local Models for Glucose Prediction without Meal Size Information under Free-Living Conditions
Francesco Prendin, José-Luis Díez, Simone Del Favero, Giovanni Sparacino, Andrea Facchinetti, Jorge Bondia
Sensors.2022; 22(22): 8682. CrossRef - Wearable Sensor-Based Monitoring of Environmental Exposures and the Associated Health Effects: A Review
Xueer Lin, Jiaying Luo, Minyan Liao, Yalan Su, Mo Lv, Qing Li, Shenglan Xiao, Jianbang Xiang
Biosensors.2022; 12(12): 1131. CrossRef - Acceptability and feasibility of continuous glucose monitoring in people with diabetes: protocol for a mixed-methods systematic review of quantitative and qualitative evidence
Jennifer V. E. Brown, Ramzi Ajjan, Najma Siddiqi, Peter A. Coventry
Systematic Reviews.2022;[Epub] CrossRef - Utilization of Personalized Machine-Learning to Screen for Dysglycemia from Ambulatory ECG, toward Noninvasive Blood Glucose Monitoring
I-Min Chiu, Chi-Yung Cheng, Po-Kai Chang, Chao-Jui Li, Fu-Jen Cheng, Chun-Hung Richard Lin
Biosensors.2022; 13(1): 23. CrossRef - Effect of hydroxychloroquine on glycemic variability in type 2 diabetes patients uncontrolled on glimepiride and metformin therapy
Rajesh Rajput, Suyasha Saini, Siddhant Rajput, Parankush Upadhyay
Indian Journal of Endocrinology and Metabolism.2022; 26(6): 537. CrossRef - GESTATIONAL DIABETES MELLITUS: MODERN GLYCEMIA MONITORING SYSTEMS
YU.A. DUDAREVA, V.A. GURYEVA, G.V. NEMTSEVA
AVICENNA BULLETIN.2022; 24(1): 97. CrossRef - Extraction With Sweat-Sebum Emulsion as a New Test Method for Leachables in Patch-Based Medical Devices, Illustrated by Assessment of Isobornylacrylate (IBOA) in Diabetes Products
Herbert Fink, Nuno M. de Barros Fernandes, Jörg Weissmann, Manfred Frey
Journal of Diabetes Science and Technology.2021; 15(4): 792. CrossRef - Mathematical Models of Meal Amount and Timing Variability With Implementation in the Type-1 Diabetes Patient Decision Simulator
Nunzio Camerlingo, Martina Vettoretti, Simone Del Favero, Andrea Facchinetti, Giovanni Sparacino
Journal of Diabetes Science and Technology.2021; 15(2): 346. CrossRef - Fit‐for‐Purpose Biometric Monitoring Technologies: Leveraging the Laboratory Biomarker Experience
Alan Godfrey, Benjamin Vandendriessche, Jessie P. Bakker, Cheryl Fitzer‐Attas, Ninad Gujar, Matthew Hobbs, Qi Liu, Carrie A. Northcott, Virginia Parks, William A. Wood, Vadim Zipunnikov, John A. Wagner, Elena S. Izmailova
Clinical and Translational Science.2021; 14(1): 62. CrossRef - Self-charging wearables for continuous health monitoring
Jiyong Kim, Salman Khan, Peng Wu, Sungjin Park, Hwanjoo Park, Choongho Yu, Woochul Kim
Nano Energy.2021; 79: 105419. CrossRef - Impact of Switching from Intermittently Scanned to Real-Time Continuous Glucose Monitoring Systems in a Type 1 Diabetes Patient French Cohort: An Observational Study of Clinical Practices
Yannis Préau, Martine Armand, Sébastien Galie, Pauline Schaepelynck, Denis Raccah
Diabetes Technology & Therapeutics.2021; 23(4): 259. CrossRef - Individualizing Time-in-Range Goals in Management of Diabetes Mellitus and Role of Insulin: Clinical Insights From a Multinational Panel
Sanjay Kalra, Shehla Shaikh, Gagan Priya, Manas P. Baruah, Abhyudaya Verma, Ashok K. Das, Mona Shah, Sambit Das, Deepak Khandelwal, Debmalya Sanyal, Sujoy Ghosh, Banshi Saboo, Ganapathi Bantwal, Usha Ayyagari, Daphne Gardner, Cecilia Jimeno, Nancy E. Barb
Diabetes Therapy.2021; 12(2): 465. CrossRef - Machine-Learning Based Model to Improve Insulin Bolus Calculation in Type 1 Diabetes Therapy
Giulia Noaro, Giacomo Cappon, Martina Vettoretti, Giovanni Sparacino, Simone Del Favero, Andrea Facchinetti
IEEE Transactions on Biomedical Engineering.2021; 68(1): 247. CrossRef - Efficacy of telemedicine for persons with type 1 diabetes during Covid19 lockdown
Federico Boscari, Sara Ferretto, Ambra Uliana, Angelo Avogaro, Daniela Bruttomesso
Nutrition & Diabetes.2021;[Epub] CrossRef - Technological innovation of Continuous Glucose Monitoring (CGM) as a tool for commercial aviation pilots with insulin-treated diabetes and stakeholders/regulators: A new chance to improve the directives?
F. Strollo, A. Furia, P. Verde, A. Bellia, M. Grussu, A. Mambro, M.D. Petrelli, S. Gentile
Diabetes Research and Clinical Practice.2021; 172: 108638. CrossRef - Machine Learning Techniques for Hypoglycemia Prediction: Trends and Challenges
Omer Mujahid, Ivan Contreras, Josep Vehi
Sensors.2021; 21(2): 546. CrossRef - Time in range–A1c hemoglobin relationship in continuous glucose monitoring of type 1 diabetes: a real-world study
Marina Valenzano, Ivan Cibrario Bertolotti, Adriano Valenzano, Giorgio Grassi
BMJ Open Diabetes Research & Care.2021; 9(1): e001045. CrossRef - Machine learning for the diagnosis of early-stage diabetes using temporal glucose profiles
Woo Seok Lee, Junghyo Jo, Taegeun Song
Journal of the Korean Physical Society.2021; 78(5): 373. CrossRef - Forecasting of Glucose Levels and Hypoglycemic Events: Head-to-Head Comparison of Linear and Nonlinear Data-Driven Algorithms Based on Continuous Glucose Monitoring Data Only
Francesco Prendin, Simone Del Favero, Martina Vettoretti, Giovanni Sparacino, Andrea Facchinetti
Sensors.2021; 21(5): 1647. CrossRef - A “Slide Rule” to Adjust Insulin Dose Using Trend Arrows in Adults with Type 1 Diabetes: Test in Silico and in Real Life
Daniela Bruttomesso, Federico Boscari, Giuseppe Lepore, Giulia Noaro, Giacomo Cappon, Angela Girelli, Lutgarda Bozzetto, Andrea Tumminia, Giorgio Grassi, Giovanni Sparacino, Luigi Laviola, Andrea Facchinetti
Diabetes Therapy.2021; 12(5): 1313. CrossRef - Glycemic variability and cardiovascular disease in patients with type 2 diabetes
Marcela Martinez, Jimena Santamarina, Adrian Pavesi, Carla Musso, Guillermo E Umpierrez
BMJ Open Diabetes Research & Care.2021; 9(1): e002032. CrossRef - Hypoglycaemia detection and prediction techniques: A systematic review on the latest developments
Omar Diouri, Monika Cigler, Martina Vettoretti, Julia K. Mader, Pratik Choudhary, Eric Renard
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Smartphone-based colorimetric detection systems for glucose monitoring in the diagnosis and management of diabetes
Özlem Kap, Volkan Kılıç, John G. Hardy, Nesrin Horzum
The Analyst.2021; 146(9): 2784. CrossRef - The impact of hypoglycaemia on the quality of life of family members of adults with type 1 or type 2 diabetes: A qualitative systematic review
Mette Valdersdorf Jensen, Melanie Broadley, Jane Speight, Alison Scope, Louise Preston, Simon Heller, Bastiaan E. de Galan, Frans Pouwer, Christel Hendrieckx
Diabetic Medicine.2021;[Epub] CrossRef - A review of biosensor technology and algorithms for glucose monitoring
Yaguang Zhang, Jingxue Sun, Liansheng Liu, Hong Qiao
Journal of Diabetes and its Complications.2021; 35(8): 107929. CrossRef - Optical glucose biosensor built-in disposable strips and wearable electronic devices
Abdullah Reda, Sherif A. El-Safty, Mahmoud M. Selim, Mohamed A. Shenashen
Biosensors and Bioelectronics.2021; 185: 113237. CrossRef - Advances, Challenges, and Cost Associated with Continuous Glucose Monitor Use in Adolescents and Young Adults with Type 1 Diabetes
Karishma A. Datye, Daniel R. Tilden, Angelee M. Parmar, Eveline R. Goethals, Sarah S. Jaser
Current Diabetes Reports.2021;[Epub] CrossRef - Is HbA1c an ideal biomarker of well-controlled diabetes?
Georgia Kaiafa, Stavroula Veneti, George Polychronopoulos, Dimitrios Pilalas, Stylianos Daios, Ilias Kanellos, Triantafyllos Didangelos, Stamatina Pagoni, Christos Savopoulos
Postgraduate Medical Journal.2021; 97(1148): 380. CrossRef - Technology in the management of type 2 diabetes: Present status and future prospects
Aideen Daly, Roman Hovorka
Diabetes, Obesity and Metabolism.2021; 23(8): 1722. CrossRef - A Non-Invasive Flexible Glucose Monitoring Sensor Using a Broadband Reject Filter
Moussa Bteich, Jessica Hanna, Joseph Costantine, Rouwaida Kanj, Youssef Tawk, Ali H. Ramadan, Assaad A. Eid
IEEE Journal of Electromagnetics, RF and Microwaves in Medicine and Biology.2021; 5(2): 139. CrossRef - Wearable patch delivery system for artificial pancreas health diagnostic-therapeutic application: A review
Nur Farrahain Nadia Ahmad, Nik Nazri Nik Ghazali, Yew Hoong Wong
Biosensors and Bioelectronics.2021; 189: 113384. CrossRef - Technological Ecological Momentary Assessment Tools to Study Type 1 Diabetes in Youth: Viewpoint of Methodologies
Mary Katherine Ray, Alana McMichael, Maria Rivera-Santana, Jacob Noel, Tamara Hershey
JMIR Diabetes.2021; 6(2): e27027. CrossRef - Designing biomaterials for the modulation of allogeneic and autoimmune responses to cellular implants in Type 1 Diabetes
Magdalena M. Samojlik, Cherie L. Stabler
Acta Biomaterialia.2021; 133: 87. CrossRef - Evaluation of a continuous glucose monitoring system in neonatal foals
David Wong, Caitlin Malik, Katarzyna Dembek, Krista Estell, Megan Marchitello, Katie Wilson
Journal of Veterinary Internal Medicine.2021; 35(4): 1995. CrossRef - Flash Glucose Monitoring in the Netherlands: Increased monitoring frequency is associated with improvement of glycemic parameters
Annel Lameijer, Nicole Lommerde, Timothy C. Dunn, Marion J. Fokkert, Mireille A. Edens, Kalvin Kao, Yongjin Xu, R.O.B. Gans, Henk J.G. Bilo, Peter R. van Dijk
Diabetes Research and Clinical Practice.2021; 177: 108897. CrossRef - Utilisation, access and recommendations regarding technologies for people living with type 1 diabetes: consensus statement of the ADS/ADEA/APEG/ADIPS Working Group
Anthony J Pease, Sofianos Andrikopoulos, Mary B Abraham, Maria E Craig, Brett Fenton, Jane Overland, Sarah Price, David Simmons, Glynis P Ross
Medical Journal of Australia.2021; 215(10): 473. CrossRef - Catalytic effects of magnetic and conductive nanoparticles on immobilized glucose oxidase in skin sensors
Lilian C Alarcón-Segovia, Amay J Bandodkar, John A Rogers, Ignacio Rintoul
Nanotechnology.2021; 32(37): 375101. CrossRef - Optical Glucose Sensor Using Pressure Sensitive Paint
Jongwon Park
Sensors.2021; 21(13): 4474. CrossRef - Type 1 diabetes glycemic management: Insulin therapy, glucose monitoring, and automation
Bruce A. Perkins, Jennifer L. Sherr, Chantal Mathieu
Science.2021; 373(6554): 522. CrossRef - Clinical Utilities of Continuous Glucose Monitoring and Insulin Pumps in Pediatric Patients with Type 1 Diabetes
Jieun Lee, Jae Hyun Kim
The Ewha Medical Journal.2021; 44(3): 55. CrossRef - Personalized Postprandial Glucose Response–Targeting Diet Versus Mediterranean Diet for Glycemic Control in Prediabetes
Orly Ben-Yacov, Anastasia Godneva, Michal Rein, Smadar Shilo, Dmitry Kolobkov, Netta Koren, Noa Cohen Dolev, Tamara Travinsky Shmul, Bat Chen Wolf, Noa Kosower, Keren Sagiv, Maya Lotan-Pompan, Niv Zmora, Adina Weinberger, Eran Elinav, Eran Segal
Diabetes Care.2021; 44(9): 1980. CrossRef - Lack of Acceptance of Digital Healthcare in the Medical Market: Addressing Old Problems Raised by Various Clinical Professionals and Developing Possible Solutions
Jong Il Park, Hwa Young Lee, Hyunah Kim, Jisan Lee, Jiwon Shinn, Hun-Sung Kim
Journal of Korean Medical Science.2021;[Epub] CrossRef - Benefits of a Switch from Intermittently Scanned Continuous Glucose Monitoring (isCGM) to Real-Time (rt) CGM in Diabetes Type 1 Suboptimal Controlled Patients in Real-Life: A One-Year Prospective Study §
Yannis Préau, Sébastien Galie, Pauline Schaepelynck, Martine Armand, Denis Raccah
Sensors.2021; 21(18): 6131. CrossRef - A Hybrid Automata Approach for Monitoring the Patient in the Loop in Artificial Pancreas Systems
Aleix Beneyto, Vicenç Puig, B. Wayne Bequette, Josep Vehi
Sensors.2021; 21(21): 7117. CrossRef - Editors’ Choice—Review—From Polarography to Electrochemical Biosensors: The 100-Year Quest for Selectivity and Sensitivity
William R. Heineman, Peter T. Kissinger, Kenneth R. Wehmeyer
Journal of The Electrochemical Society.2021; 168(11): 116504. CrossRef - Digital health and diabetes: experience from India
Jothydev Kesavadev, Gopika Krishnan, Viswanathan Mohan
Therapeutic Advances in Endocrinology and Metabolism.2021; 12: 204201882110546. CrossRef - Current Advances of Artificial Pancreas Systems: A Comprehensive Review of the Clinical Evidence
Sun Joon Moon, Inha Jung, Cheol-Young Park
Diabetes & Metabolism Journal.2021; 45(6): 813. CrossRef - Factors Associated with Adherence to Self-Monitoring of Blood Glucose Among Young People with Type 1 Diabetes in China: A Cross-Sectional Study
Wencong Lv, Jiaxin Luo, Qing Long, Jundi Yang, Xin Wang, Jia Guo
Patient Preference and Adherence.2021; Volume 15: 2809. CrossRef - Continuous glucose monitoring devices: A brief presentation (Review)
Doina Mihai, Diana Stefan, Daniela Stegaru, Georgiana Bernea, Ileana Vacaroiu, Toma Papacocea, Mircea Lupușoru, Adriana Nica, Ovidiu Stiru, Dorin Dragos, Octavian Olaru
Experimental and Therapeutic Medicine.2021;[Epub] CrossRef - Acute glycemic variability on admission predicts the prognosis in hospitalized patients with coronary artery disease: a meta-analysis
Zhaokun Pu, Lihong Lai, Xishan Yang, Yanyu Wang, Pingshuan Dong, Dan Wang, Yingli Xie, Zesen Han
Endocrine.2020; 67(3): 526. CrossRef - Glycemic profile of women with normoglycemia and gestational diabetes mellitus during early pregnancy using continuous glucose monitoring system
Charandeep Singh, Yashdeep Gupta, Alpesh Goyal, Mani Kalaivani, Vineeta Garg, Juhi Bharti, Seema Singhal, Garima Kachhawa, Vidushi Kulshrestha, Rajesh Kumari, Reeta Mahey, Jai B Sharma, Neerja Bhatla, Rajesh Khadgawat, Nandita Gupta, Nikhil Tandon
Diabetes Research and Clinical Practice.2020; 169: 108409. CrossRef - Efficacy of Intermittently Scanned Continuous Glucose Monitoring in the Prevention of Recurrent Severe Hypoglycemia
Timothy M.E. Davis, Penny Dwyer, Michelle England, P. Gerry Fegan, Wendy A. Davis
Diabetes Technology & Therapeutics.2020; 22(5): 367. CrossRef - How was the Diabetes Metabolism Journal added to MEDLINE?
Hye Jin Yoo
Science Editing.2020; 7(2): 201. CrossRef - Applying Nanomaterials to Modern Biomedical Electrochemical Detection of Metabolites, Electrolytes, and Pathogens
Itthipon Jeerapan, Thitaporn Sonsa-ard, Duangjai Nacapricha
Chemosensors.2020; 8(3): 71. CrossRef - Clinical Opportunities for Continuous Biosensing and Closed-Loop Therapies
Jason Li, Jia Y. Liang, Steven J. Laken, Robert Langer, Giovanni Traverso
Trends in Chemistry.2020; 2(4): 319. CrossRef - A single-blind, randomised, crossover study to reduce hypoglycaemia risk during postprandial exercise with closed-loop insulin delivery in adults with type 1 diabetes: announced (with or without bolus reduction) vs unannounced exercise strategies
Sémah Tagougui, Nadine Taleb, Laurent Legault, Corinne Suppère, Virginie Messier, Inès Boukabous, Azadeh Shohoudi, Martin Ladouceur, Rémi Rabasa-Lhoret
Diabetologia.2020; 63(11): 2282. CrossRef - Bimetallic PtAu alloy nanomaterials for nonenzymatic selective glucose sensing at low potential
Lingling Lin, Shaohuang Weng, Yanjie Zheng, Xiyao Liu, Shaoming Ying, Feng Chen, Donghong You
Journal of Electroanalytical Chemistry.2020; 865: 114147. CrossRef - Type 1 Diabetes in Youth and Technology-Based Advances in Management
Christopher Ferber, Catherine S. Mao, Jennifer K. Yee
Advances in Pediatrics.2020; 67: 73. CrossRef - Advanced Diabetes Management Using Artificial Intelligence and Continuous Glucose Monitoring Sensors
Martina Vettoretti, Giacomo Cappon, Andrea Facchinetti, Giovanni Sparacino
Sensors.2020; 20(14): 3870. CrossRef - Efficacy and safety of evogliptin treatment in patients with type 2 diabetes: A multicentre, active‐controlled, randomized, double‐blind study with open‐label extension (the EVERGREEN study)
Gyuri Kim, Soo Lim, Hyuk‐Sang Kwon, Ie B. Park, Kyu J. Ahn, Cheol‐Young Park, Su K. Kwon, Hye S. Kim, Seok W. Park, Sin G. Kim, Min K. Moon, Eun S. Kim, Choon H. Chung, Kang S. Park, Mikyung Kim, Dong J. Chung, Chang B. Lee, Tae H. Kim, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2020; 22(9): 1527. CrossRef - Association Between Continuous Glucose Monitoring-Derived Time in Range, Other Core Metrics, and Albuminuria in Type 2 Diabetes
Jee Hee Yoo, Min Sun Choi, Jiyeon Ahn, Sung Woon Park, Yejin Kim, Kyu Yeon Hur, Sang-Man Jin, Gyuri Kim, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2020; 22(10): 768. CrossRef - A New Approach to Determining Liquid Concentration Using Multiband Annular Ring Microwave Sensor and Polarity Correlator
Waleed Sethi, Ahmed Ibrahim, Khaled Issa, Ali Albishi, Saleh Alshebeili
Electronics.2020; 9(10): 1616. CrossRef - Estrategia terapéutica en el paciente diabético (I). Empoderamiento del paciente y formación. Objetivos terapéuticos. Estilo de vida, alimentación, vacunación y consejos al paciente diabético
F.B. Rivas Sánchez, J. Sanz Cánovas, J. Martín Carmona, S. Jansen Chaparro
Medicine - Programa de Formación Médica Continuada Acreditado.2020; 13(17): 943. CrossRef - Current status of continuous glucose monitoring among Korean children and adolescents with type 1 diabetes mellitus
Jae Hyun Kim
Annals of Pediatric Endocrinology & Metabolism.2020; 25(3): 145. CrossRef - Towards sensor-based calving detection in the rangelands: a systematic review of credible behavioral and physiological indicators
Anita Z Chang, David L Swain, Mark G Trotter
Translational Animal Science.2020;[Epub] CrossRef - Electrochemical glucose sensors in diabetes management: an updated review (2010–2020)
Hazhir Teymourian, Abbas Barfidokht, Joseph Wang
Chemical Society Reviews.2020; 49(21): 7671. CrossRef - An analytical approach to determine the optimal duration of continuous glucose monitoring data required to reliably estimate time in hypoglycemia
Nunzio Camerlingo, Martina Vettoretti, Andrea Facchinetti, Giovanni Sparacino, Julia K. Mader, Pratik Choudhary, Simone Del Favero
Scientific Reports.2020;[Epub] CrossRef - Smartphone-Based Data Collection in Ophthalmology
Florian Philipp Raber, Rokas Gerbutavicius, Armin Wolf, Karsten Kortüm
Klinische Monatsblätter für Augenheilkunde.2020; 237(12): 1420. CrossRef - Glycemic Status Assessment by the Latest Glucose Monitoring Technologies
Ilaria Malandrucco, Benedetta Russo, Fabiana Picconi, Marika Menduni, Simona Frontoni
International Journal of Molecular Sciences.2020; 21(21): 8243. CrossRef - Medical Nutrition Therapy Using Continuous Glucose Monitoring System
Mee Ra Kweon
The Journal of Korean Diabetes.2020; 21(4): 216. CrossRef - Use of Flash Glucose Monitoring in Patients on Intensive Insulin Treatment
Jun Sung Moon
The Journal of Korean Diabetes.2020; 21(4): 184. CrossRef - Data Analysis and Accuracy Evaluation of a Continuous Glucose-Monitoring Device
Lijun Cai, Wancheng Ge, Zhigang Zhu, Xueling Zhao, Zhanhong Li
Journal of Sensors.2019; 2019: 1. CrossRef - Development of an Error Model for a Factory-Calibrated Continuous Glucose Monitoring Sensor with 10-Day Lifetime
Martina Vettoretti, Cristina Battocchio, Giovanni Sparacino, Andrea Facchinetti
Sensors.2019; 19(23): 5320. CrossRef
- Continuous glucose monitoring metrics following sub-Tenon’s injection of triamcinolone acetonide for diabetic macular edema
- Obesity and Metabolic Syndrome
- Understanding Bile Acid Signaling in Diabetes: From Pathophysiology to Therapeutic Targets
- Jessica M. Ferrell, John Y. L. Chiang
- Diabetes Metab J. 2019;43(3):257-272. Published online June 13, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0043
- 8,695 View
- 243 Download
- 64 Web of Science
- 69 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Diabetes and obesity have reached an epidemic status worldwide. Diabetes increases the risk for cardiovascular disease and non-alcoholic fatty liver disease. Primary bile acids are synthesized in hepatocytes and are transformed to secondary bile acids in the intestine by gut bacteria. Bile acids are nutrient sensors and metabolic integrators that regulate lipid, glucose, and energy homeostasis by activating nuclear farnesoid X receptor and membrane Takeda G protein-coupled receptor 5. Bile acids control gut bacteria overgrowth, species population, and protect the integrity of the intestinal barrier. Gut bacteria, in turn, control circulating bile acid composition and pool size. Dysregulation of bile acid homeostasis and dysbiosis causes diabetes and obesity. Targeting bile acid signaling and the gut microbiome have therapeutic potential for treating diabetes, obesity, and non-alcoholic fatty liver disease.
-
Citations
Citations to this article as recorded by- Gut microbiome-derived secondary bile acids: therapeutic targets for reducing cardiovascular disease in type 2 diabetes?
Sarah A. Johnson, Tiffany L. Weir
The American Journal of Clinical Nutrition.2024; 119(2): 241. CrossRef - Current updates on metabolites and its interlinked pathways as biomarkers for diabetic kidney disease: A systematic review
Soumik Das, V Devi Rajeswari, Ganesh Venkatraman, Ramprasad Elumalai, Sivaraman Dhanasekaran, Gnanasambandan Ramanathan
Translational Research.2024; 265: 71. CrossRef - Variant of the lactase LCT gene explains association between milk intake and incident type 2 diabetes
Kai Luo, Guo-Chong Chen, Yanbo Zhang, Jee-Young Moon, Jiaqian Xing, Brandilyn A. Peters, Mykhaylo Usyk, Zheng Wang, Gang Hu, Jun Li, Elizabeth Selvin, Casey M. Rebholz, Tao Wang, Carmen R. Isasi, Bing Yu, Rob Knight, Eric Boerwinkle, Robert D. Burk, Rober
Nature Metabolism.2024; 6(1): 169. CrossRef - Predictive value of serum TBA for 2-year MACEs in ACS patients undergoing PCI: a prospective cohort study
Wen Wen, Qinze Li, Jianqing She, Xiaofang Bai, Lisha Zhang, Ruifeng Li, Yan Wu, Juan Zhou, Zuyi Yuan
Scientific Reports.2024;[Epub] CrossRef - Collaborative Metabolism: Gut Microbes Play a Key Role in Canine and Feline Bile Acid Metabolism
John C. Rowe, Jenessa A. Winston
Veterinary Sciences.2024; 11(2): 94. CrossRef - The paradigm change from reactive medical services to 3PM in ischemic stroke: a holistic approach utilising tear fluid multi-omics, mitochondria as a vital biosensor and AI-based multi-professional data interpretation
Olga Golubnitschaja, Jiri Polivka, Pavel Potuznik, Martin Pesta, Ivana Stetkarova, Alena Mazurakova, Lenka Lackova, Peter Kubatka, Martina Kropp, Gabriele Thumann, Carl Erb, Holger Fröhlich, Wei Wang, Babak Baban, Marko Kapalla, Niva Shapira, Kneginja Ric
EPMA Journal.2024; 15(1): 1. CrossRef - Investigating the mechanism of cornel iridoid glycosides on type 2 diabetes mellitus using serum and urine metabolites in rats
Yadi Hou, Yanmei Huang, Zihui Shang, Shichao Ma, Tianyi Cui, Ali Chen, Yongxia Cui, Suiqing Chen
Journal of Ethnopharmacology.2024; 328: 118065. CrossRef - Improvement of myocardial injury and gut microbiota disturbance in type 2 diabetic mice by inulin with various degrees of polymerization
Siqiang Jia, Jianpeng Li, Bin Yu, Mengjie Li, Bo Cui
Food Bioscience.2023; 51: 102318. CrossRef - Bile acids and their receptors in regulation of gut health and diseases
Sen Lin, Sutian Wang, Peng Wang, Cuiming Tang, Zhenjiang Wang, Lian Chen, Guoqing Luo, Hong Chen, Yuntao Liu, Bin Feng, De Wu, Douglas G. Burrin, Zhengfeng Fang
Progress in Lipid Research.2023; 89: 101210. CrossRef - Effects of dietary oat supplementation on carcass traits, muscle metabolites, amino acid profiles, and its association with meat quality of Small-tail Han sheep
Li-wei Wang, Shao-feng Su, Jie Zhao, Xiao-long He, Shao-yin Fu, Biao Wang, Yun-fei Wang, Da-qing Wang, Na-na Yun, Xin Chen, Damien P Belobrajdic, Terigele, Xiao-dong Li, Li-li Jiang, Jiang-feng He, Yong-bin Liu
Food Chemistry.2023; 411: 135456. CrossRef - Noni (Morinda citrifolia L.) fruit polysaccharide ameliorated high-fat diet-induced obesity by modulating gut microbiota and improving bile acid metabolism
Wenjing Mo, Jiaqi Zou, Ming Wu, Zijun Peng, Wenjiang He, Wenzhi Li, Xiaoyong Wu
Journal of Functional Foods.2023; 101: 105408. CrossRef - Sodium glucose co-transporter 2 (SGLT2) inhibition via dapagliflozin improves diabetic kidney disease (DKD) over time associatied with increasing effect on the gut microbiota in db/db mice
Jiajia Wu, Yan Chen, Huinan Yang, Leyi Gu, Zhaohui Ni, Shan Mou, Jianxiao Shen, Xiajing Che
Frontiers in Endocrinology.2023;[Epub] CrossRef - Short communication: unique metabolic signature of proliferative retinopathy in the tear fluid of diabetic patients with comorbidities — preliminary data for PPPM validation
Martina Kropp, Eline De Clerck, Trong-Tin Kevin Steve Vo, Gabriele Thumann, Vincenzo Costigliola, Olga Golubnitschaja
EPMA Journal.2023; 14(1): 43. CrossRef - Impact of Vancomycin Treatment and Gut Microbiota on Bile Acid Metabolism and the Development of Non-Alcoholic Steatohepatitis in Mice
Kaichi Kasai, Naoya Igarashi, Yuki Tada, Koudai Kani, Shun Takano, Tsutomu Yanagibashi, Fumitake Usui-Kawanishi, Shiho Fujisaka, Shiro Watanabe, Mayuko Ichimura-Shimizu, Kiyoshi Takatsu, Kazuyuki Tobe, Koichi Tsuneyama, Yukihiro Furusawa, Yoshinori Nagai
International Journal of Molecular Sciences.2023; 24(4): 4050. CrossRef - Mitochondrial Cholesterol Metabolites in a Bile Acid Synthetic Pathway Drive Nonalcoholic Fatty Liver Disease: A Revised “Two-Hit” Hypothesis
Genta Kakiyama, Daniel Rodriguez-Agudo, William M. Pandak
Cells.2023; 12(10): 1434. CrossRef - Bile acid metabolism and signaling: Emerging pharmacological targets of dietary polyphenols
Kevin M. Tveter, Esther Mezhibovsky, Yue Wu, Diana E. Roopchand
Pharmacology & Therapeutics.2023; 248: 108457. CrossRef - Role of liver parameters in diabetes mellitus – a narrative review
Sana Rafaqat, Aqsa Sattar, Amber Khalid, Saira Rafaqat
Endocrine Regulations.2023; 57(1): 200. CrossRef - Bile acids induce IL-1α and drive NLRP3 inflammasome-independent production of IL-1β in murine dendritic cells
Ewa Oleszycka, Eoin C. O’Brien, Michael Freeley, Ed C. Lavelle, Aideen Long
Frontiers in Immunology.2023;[Epub] CrossRef - Machine learning for predicting diabetic metabolism in the Indian population using polar metabolomic and lipidomic features
Nikita Jain, Bhaumik Patel, Manjesh Hanawal, Anurag R. Lila, Saba Memon, Tushar Bandgar, Ashutosh Kumar
Metabolomics.2023;[Epub] CrossRef - The mitochondrial translocator protein (TSPO, 18 kDa): A key multifunctional molecule in liver diseases
Yuchang Li, Liting Chen, Vassilios Papadopoulos
Biochimie.2023;[Epub] CrossRef - Sodium+/taurocholate cotransporting polypeptide as target therapy for liver fibrosis
Ahmad Salhab, Johnny Amer, Yinying Lu, Rifaat Safadi
Gut.2022; 71(7): 1373. CrossRef - Comparative Evaluation of the Effect of Metformin and Insulin on Gut Microbiota and Metabolome Profiles of Type 2 Diabetic Rats Induced by the Combination of Streptozotocin and High-Fat Diet
Nan Hu, Qi Zhang, Hui Wang, Xuping Yang, Yan Jiang, Rong Chen, Liying Wang
Frontiers in Pharmacology.2022;[Epub] CrossRef - Immunomodulatory functions of FXR
Stefano Fiorucci, Angela Zampella, Patrizia Ricci, Eleonora Distrutti, Michele Biagioli
Molecular and Cellular Endocrinology.2022; 551: 111650. CrossRef - Production of New Microbially Conjugated Bile Acids by Human Gut Microbiota
Carlos J. Garcia, Vit Kosek, David Beltrán, Francisco A. Tomás-Barberán, Jana Hajslova
Biomolecules.2022; 12(5): 687. CrossRef - Regulation of the intestinal flora: A potential mechanism of natural medicines in the treatment of type 2 diabetes mellitus
liying he, Fang-Qing Yang, Pan Tang, Ting-Hui Gao, Cai-Xia Yang, Li Tan, Pan Yue, Ya-Nan Hua, Si-Jing Liu, Jin-Lin Guo
Biomedicine & Pharmacotherapy.2022; 151: 113091. CrossRef - Acrylamide induced glucose metabolism disorder in rats involves gut microbiota dysbiosis and changed bile acids metabolism
Zonghao Yue, Yanjuan Chen, Qian Dong, Dan Li, Meng Guo, Li Zhang, Yini Shi, Huiting Wu, Lili Li, Zhongke Sun
Food Research International.2022; 157: 111405. CrossRef - Effects of Herbal Therapy on Intestinal Microbiota and Serum Metabolomics in Different Rat Models of Mongolian Medicine
Guniang Jiu, Riao Dao, Dongxing Wu, Wang Hung, Haburi Jin, Li Li, Xiquan Fu, Chula Sa, Eerdunchaolu, Maulidiani .M
Evidence-Based Complementary and Alternative Medicine.2022; 2022: 1. CrossRef - The role of immune cells in the liver tumor microenvironment: an involvement of gut microbiota-derived factors
Tomonori Kamiya, Naoko Ohtani
International Immunology.2022; 34(9): 467. CrossRef - Reduced Cytokine Tumour Necrosis Factor by Pharmacological Intervention in a Preclinical Study
Armin Mooranian, Jacqueline Chester, Edan Johnston, Corina Mihaela Ionescu, Daniel Walker, Melissa Jones, Susbin Raj Wagle, Bozica Kovacevic, Thomas Foster, Momir Mikov, Hani Al-Salami
Biomolecules.2022; 12(7): 877. CrossRef - Crisis of the Asian gut: associations among diet, microbiota, and metabolic diseases
Phatthanaphong THERDTATHA, Akari SHINODA, Jiro NAKAYAMA
Bioscience of Microbiota, Food and Health.2022; 41(3): 83. CrossRef - Valorization of avocado seeds with antioxidant capacity using pressurized hot water extraction
Eng Shi Ong, Janelle Low, Joseph Choon Wee Tan, Su Yi Foo, Chen Huei Leo
Scientific Reports.2022;[Epub] CrossRef - The fungicide prothioconazole and its metabolite prothioconazole-desthio disturbed the liver-gut axis in mice
Lingyu Hu, Xiaofang Wang, Zhiwei Bao, Qihao Xu, Mingrong Qian, Yuanxiang Jin
Chemosphere.2022; 307: 136141. CrossRef - Gut Microbiota and Bile Acids Mediate the Clinical Benefits of YH1 in Male Patients with Type 2 Diabetes Mellitus: A Pilot Observational Study
Yueh-Hsiang Huang, Yi-Hong Wu, Hsiang-Yu Tang, Szu-Tah Chen, Chih-Ching Wang, Wan-Jing Ho, Yi-Hsuan Lin, Geng-Hao Liu, Pei-Yeh Lin, Chi-Jen Lo, Yuan-Ming Yeh, Mei-Ling Cheng
Pharmaceutics.2022; 14(9): 1857. CrossRef - Gut–Liver Axis and Non-Alcoholic Fatty Liver Disease: A Vicious Circle of Dysfunctions Orchestrated by the Gut Microbiome
Salvatore Pezzino, Maria Sofia, Gloria Faletra, Chiara Mazzone, Giorgia Litrico, Gaetano La Greca, Saverio Latteri
Biology.2022; 11(11): 1622. CrossRef - The Role of Bile Acids in Cardiovascular Diseases: from Mechanisms to Clinical Implications
Shuwen Zhang, Junteng Zhou, Wenchao Wu, Ye Zhu, Xiaojing Liu
Aging and disease.2022;[Epub] CrossRef - Role of bile acids in overweight and obese children and adolescents
Cosimo Giannini, Concetta Mastromauro, Serena Scapaticci, Cristina Gentile, Francesco Chiarelli
Frontiers in Endocrinology.2022;[Epub] CrossRef - Bile acids and microbes in metabolic disease
Dhiraj Kumar Sah, Archana Arjunan, Sun Young Park, Young Do Jung
World Journal of Gastroenterology.2022; 28(48): 6846. CrossRef - The Fungicide Prothioconazole and its Metabolite Prothioconazole-Desthio Disturbed the Liver-Gut Axis in Mice
Yuanxiang Jin, Lingyu Hu, Xiaofang Wang, Zhiwei Bao, Qihao Xu, Mingrong Qian
SSRN Electronic Journal .2022;[Epub] CrossRef - The Critical Effect of Bile Acids in Atherosclerosis
Shangwen Qi, Xu Luo, Shuangfang Liu, Bishi Ling, Hua Jin
Journal of Cardiovascular Pharmacology.2022; 80(4): 562. CrossRef - Role of sirtuin-1 (SIRT1) in hypoxic injury in pancreatic β-cells
Ye-Jee Lee, Esder Lee, Young-Hye You, Yu-Bae Ahn, Ki-Ho Song, Ji-Won Kim, Seung-Hyun Ko
Journal of Drug Targeting.2021; 29(1): 88. CrossRef - Impact of gut microbiota: How it could play roles beyond the digestive system on development of cardiovascular and renal diseases
Kanmani Suganya, Taekwon Son, Kyu-Won Kim, Byung-Soo Koo
Microbial Pathogenesis.2021; 152: 104583. CrossRef - Determination of bile acids from human gallbladder by 1H‐MRS—Protocol optimization and estimation of reproducibility
Peter Vermathen, Gaëlle Diserens, Dino Kröll, Philipp Nett, Guido Stirnimann, Reiner Wiest
NMR in Biomedicine.2021;[Epub] CrossRef - The gut microbiome-bile acid axis in hepatocarcinogenesis
Liwei Wu, Jiao Feng, Jingjing Li, Qiang Yu, Jie Ji, Jianye Wu, Weiqi Dai, Chuanyong Guo
Biomedicine & Pharmacotherapy.2021; 133: 111036. CrossRef - Gut microbiome and bile acids in obesity-related diseases
Rumei Li, Sergio Andreu-Sánchez, Folkert Kuipers, Jingyuan Fu
Best Practice & Research Clinical Endocrinology & Metabolism.2021; 35(3): 101493. CrossRef - Gut Microbiome of Indonesian Adults Associated with Obesity and Type 2 Diabetes: A Cross-Sectional Study in an Asian City, Yogyakarta
Phatthanaphong Therdtatha, Yayi Song, Masaru Tanaka, Mariyatun Mariyatun, Maisaroh Almunifah, Nancy Eka Putri Manurung, Siska Indriarsih, Yi Lu, Koji Nagata, Katsuya Fukami, Tetsuo Ikeda, Yuan-Kun Lee, Endang Sutriswati Rahayu, Jiro Nakayama
Microorganisms.2021; 9(5): 897. CrossRef - Microbial Ecosystem in Diabetes Mellitus: Consideration of the Gastrointestinal System
Awgichew Shewasinad Yehualashet, Berhan Begashaw Yikna
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 1841. CrossRef - Role of bile acids in inflammatory liver diseases
Ioannis Evangelakos, Joerg Heeren, Esther Verkade, Folkert Kuipers
Seminars in Immunopathology.2021; 43(4): 577. CrossRef - Plasma Bile Acid Profile in Patients with and without Type 2 Diabetes
Alessandro Mantovani, Andrea Dalbeni, Denise Peserico, Filippo Cattazzo, Michele Bevilacqua, Gian Luca Salvagno, Giuseppe Lippi, Giovanni Targher, Elisa Danese, Cristiano Fava
Metabolites.2021; 11(7): 453. CrossRef - Maternal cecal microbiota transfer rescues early-life antibiotic-induced enhancement of type 1 diabetes in mice
Xue-Song Zhang, Yue Sandra Yin, Jincheng Wang, Thomas Battaglia, Kimberly Krautkramer, Wei Vivian Li, Jackie Li, Mark Brown, Meifan Zhang, Michelle H. Badri, Abigail J.S. Armstrong, Christopher M. Strauch, Zeneng Wang, Ina Nemet, Nicole Altomare, Joseph C
Cell Host & Microbe.2021; 29(8): 1249. CrossRef - Pregnane X receptor exacerbates nonalcoholic fatty liver disease accompanied by obesity- and inflammation-prone gut microbiome signature
Sarah Kim, Sora Choi, Moumita Dutta, Jeffrey O. Asubonteng, Marianne Polunas, Michael Goedken, Frank J. Gonzalez, Julia Yue Cui, Maxwell A. Gyamfi
Biochemical Pharmacology.2021; 193: 114698. CrossRef - Gut microbiota as a target for prevention and treatment of type 2 diabetes: Mechanisms and dietary natural products
Fan Xia, Lu-Ping Wen, Bing-Chen Ge, Yu-Xin Li, Fang-Ping Li, Ben-Jie Zhou
World Journal of Diabetes.2021; 12(8): 1146. CrossRef - Association between circulating bile acid alterations and nonalcoholic steatohepatitis independent of obesity and diabetes mellitus
Youngae Jung, Bo Kyung Koo, Seo Young Jang, Dain Kim, Heeyeon Lee, Dong Hyeon Lee, Sae Kyung Joo, Yong Jin Jung, Jeong Hwan Park, Taekyeong Yoo, Murim Choi, Min Kyung Lee, Sang Won Kang, Mee Soo Chang, Won Kim, Geum‐Sook Hwang
Liver International.2021; 41(12): 2892. CrossRef - Bile acid activated receptors: Integrating immune and metabolic regulation in non-alcoholic fatty liver disease
Michele Biagioli, Stefano Fiorucci
Liver Research.2021; 5(3): 119. CrossRef - Synthesis of 12β-Methyl-18-nor-bile Acids
Andreas Luxenburger, Lawrence D. Harris, Elizabeth M. Ure, Roselis A. Landaeta Aponte, Anthony D. Woolhouse, Scott A. Cameron, Chris D. Ling, Ross O. Piltz, Andrew R. Lewis, Graeme J. Gainsford, Alex Weymouth-Wilson, Richard H. Furneaux
ACS Omega.2021; 6(38): 25019. CrossRef - Serum metabolomic biomarkers of perceptual speed in cognitively normal and mildly impaired subjects with fasting state stratification
Kamil Borkowski, Ameer Y. Taha, Theresa L. Pedersen, Philip L. De Jager, David A. Bennett, Matthias Arnold, Rima Kaddurah-Daouk, John W. Newman
Scientific Reports.2021;[Epub] CrossRef - Myocardial Infarction and Coronary Artery Disease in Menopausal Women With Type 2 Diabetes Mellitus Negatively Correlate With Total Serum Bile Acids
Xunxun Feng, Guangyao Zhai, Jiaqi Yang, Yang Liu, Yujie Zhou, Qianyun Guo
Frontiers in Endocrinology.2021;[Epub] CrossRef - An Integrated Bile Acids Profile Determination by UHPLC-MS/MS to Identify the Effect of Bile Acids Supplement in High Plant Protein Diet on Common Carp (Cyprinus carpio)
Xian Wei, Ting Yao, Fatou Ndoye Fall, Min Xue, Xiaofang Liang, Jie Wang, Wenlong Du, Xu Gu
Foods.2021; 10(10): 2465. CrossRef - Fatty liver index and development of cardiovascular disease in Koreans without pre-existing myocardial infarction and ischemic stroke: a large population-based study
Jun Hyung Kim, Jin Sil Moon, Seok Joon Byun, Jun Hyeok Lee, Dae Ryong Kang, Ki Chul Sung, Jang Young Kim, Ji Hye Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Methionine restriction alleviates high-fat diet-induced obesity: Involvement of diurnal metabolism of lipids and bile acids
Luanfeng Wang, Bo Ren, Qian Zhang, Chuanqi Chu, Zhenting Zhao, Jianbin Wu, Weiyang Zhao, Zhigang Liu, Xuebo Liu
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2020; 1866(11): 165908. CrossRef - Bile Acids: Key Regulators and Novel Treatment Targets for Type 2 Diabetes
Yingjie Wu, An Zhou, Li Tang, Yuanyuan Lei, Bo Tang, Linjing Zhang
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Bile acid receptors FXR and TGR5 signaling in fatty liver diseases and therapy
John Y. L. Chiang, Jessica M. Ferrell
American Journal of Physiology-Gastrointestinal and Liver Physiology.2020; 318(3): G554. CrossRef - Imidacloprid disturbed the gut barrier function and interfered with bile acids metabolism in mice
Guiling Yang, Xianling Yuan, Cuiyuan Jin, Dou Wang, Yanhua Wang, Wenyu Miao, Yuanxiang Jin
Environmental Pollution.2020; 266: 115290. CrossRef - Up to date on cholesterol 7 alpha-hydroxylase (CYP7A1) in bile acid synthesis
John Y.L. Chiang, Jessica M. Ferrell
Liver Research.2020; 4(2): 47. CrossRef -
Diabetes and Metabolism Journal in 2020: Good to Great
In-Kyung Jeong
Diabetes & Metabolism Journal.2020; 44(1): 1. CrossRef - Healthy dietary patterns to reduce obesity-related metabolic disease: polyphenol-microbiome interactions unifying health effects across geography
Camilla Diotallevi, Francesca Fava, Marco Gobbetti, Kieran Tuohy
Current Opinion in Clinical Nutrition & Metabolic Care.2020; 23(6): 437. CrossRef - Metabolic profiling of pre-gestational and gestational diabetes mellitus identifies novel predictors of pre-term delivery
Ilhame Diboun, Manjunath Ramanjaneya, Yasser Majeed, Lina Ahmed, Mohammed Bashir, Alexandra E. Butler, Abdul Badi Abou-Samra, Stephen L. Atkin, Nayef A. Mazloum, Mohamed A. Elrayess
Journal of Translational Medicine.2020;[Epub] CrossRef - Quantification of common and planar bile acids in tissues and cultured cells
Stephanie J. Shiffka, Jace W. Jones, Linhao Li, Ann M. Farese, Thomas J. MacVittie, Hongbing Wang, Peter W. Swaan, Maureen A. Kane
Journal of Lipid Research.2020; 61(11): 1524. CrossRef - Influência da microbiota intestinal na Doença Hepática Gordurosa Não Alcoólica
Isadora Barbosa de Almeida, Wermerson Assunção Barroso, Caroline Amélia Gonçalves
Revista Científica Multidisciplinar Núcleo do Conhecimento.2020; : 14. CrossRef - Ultra-Early and Early Changes in Bile Acids and Insulin after Sleeve Gastrectomy among Obese Patients
Adriana Florinela Cӑtoi, Alina Elena Pârvu, Aurel Mironiuc, Horațiu Silaghi, Ioana Delia Pop, Andra Diana Andreicuț
Medicina.2019; 55(12): 757. CrossRef
- Gut microbiome-derived secondary bile acids: therapeutic targets for reducing cardiovascular disease in type 2 diabetes?
- Clinical Diabetes & Therapeutics
- Nonalcoholic Fatty Liver Disease and Diabetes: Part II: Treatment
- Kyung-Soo Kim, Byung-Wan Lee, Yong Jin Kim, Dae Ho Lee, Bong-Soo Cha, Cheol-Young Park
- Diabetes Metab J. 2019;43(2):127-143. Published online April 15, 2019
- DOI: https://doi.org/10.4093/dmj.2019.0034
- 7,613 View
- 138 Download
- 25 Web of Science
- 35 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Nonalcoholic fatty liver disease (NAFLD) and diabetes are common metabolic disorders that are often comorbid conditions. Among many proposed treatments, weight reduction is the only approved option for NAFLD to date. However, it is not easy to maintain weight loss by lifestyle modification alone; pharmacological treatments are helpful in this regard. Although many drugs have been investigated, pioglitazone could be a first-line therapy in patients with NAFLD and diabetes. Many more drugs are currently being developed and investigated, and it is likely that combination strategies will be used for future treatment of NAFLD and diabetes. Attention should be paid to the management of NAFLD and diabetes and efforts should be made to intervene early and individualize treatment of NAFLD in patients with diabetes.
-
Citations
Citations to this article as recorded by- Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMJ.2024; : e076388. CrossRef - Research Progress of Traditional Chinese Medicine and Western Medicine on Non-Alcoholic Fatty Liver Disease
强江 郭
Advances in Clinical Medicine.2024; 14(03): 561. CrossRef - Liver and cardiovascular disease outcomes in metabolic syndrome and diabetic populations: Bi-directional opportunities to multiply preventive strategies
Alhussain Yasin, Madison Nguyen, Angad Sidhu, Priyanka Majety, Jared Spitz, Amon Asgharpour, Mohammad S. Siddiqui, Laurence S. Sperling, Arshed A. Quyyumi, Anurag Mehta
Diabetes Research and Clinical Practice.2024; 211: 111650. CrossRef - Effect of aerobic training with silymarin consumption on glycemic indices and liver enzymes in men with type 2 diabetes
Keyvan Ghalandari, Mojtaba Shabani, Ali Khajehlandi, Amin Mohammadi
Archives of Physiology and Biochemistry.2023; 129(1): 76. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Mortality: A Population-Based Cohort Study
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(2): 220. CrossRef - Comparative antihypertensive efficacy of combinations of azilsartan medoxomil or olmesartan medoxomil with amlodipine in patients with arterial hypertension, type 2 diabetes mellitus and non-alcoholic fatty liver disease
I. А. Lukonin, V. V. Skibitsky, A. V. Fendrikova, A. V. Skibitsky, I. A. Antipov
South Russian Journal of Therapeutic Practice.2023; 4(1): 68. CrossRef - An Ethyl Acetate Extract of Eryngium carlinae Inflorescences Attenuates Oxidative Stress and Inflammation in the Liver of Streptozotocin-Induced Diabetic Rats
Cristian M. Trejo-Hurtado, Cinthia I. Landa-Moreno, Jenaro Lemus-de la Cruz, Donovan J. Peña-Montes, Rocío Montoya-Pérez, Rafael Salgado-Garciglia, Salvador Manzo-Avalos, Christian Cortés-Rojo, Juan Luis Monribot-Villanueva, José Antonio Guerrero-Analco,
Antioxidants.2023; 12(6): 1235. CrossRef - Pharmacogenetics of glucagon-like peptide-1 agonists in the treatment of type 2 diabetes mellitus
Iu.G. Samoilova, A.E. Stankova, M.V. Matveeva, O.E. Vaizova, D.V. Podchinenova, D.A. Kudlay, T.A. Filippova, I.R. Grishkevich
Profilakticheskaya meditsina.2023; 26(12): 95. CrossRef - Obesity is an important determinant of severity in newly defined metabolic dysfunction-associated fatty liver disease
Ji Hye Huh, Kwang Joon Kim, Seung Up Kim, Bong-Soo Cha, Byung-Wan Lee
Hepatobiliary & Pancreatic Diseases International.2022; 21(3): 241. CrossRef - Triglyceride and glucose index is a simple and easy‐to‐calculate marker associated with nonalcoholic fatty liver disease
Kyung‐Soo Kim, Sangmo Hong, Hong‐Yup Ahn, Cheol‐Young Park
Obesity.2022; 30(6): 1279. CrossRef - Evaluating Triglyceride and Glucose Index as a Simple and Easy-to-Calculate Marker for All-Cause and Cardiovascular Mortality
Kyung-Soo Kim, Sangmo Hong, You-Cheol Hwang, Hong-Yup Ahn, Cheol-Young Park
Journal of General Internal Medicine.2022; 37(16): 4153. CrossRef - Pharmacological Treatment of Nonalcoholic Fatty Liver Disease: Antidiabetic Agents
Kyung-Soo Kim
The Journal of Korean Diabetes.2022; 23(2): 83. CrossRef - Efficacy and mechanism of Jiedu Tongluo Tiaogan Formula in treating type 2 diabetes mellitus combined with non-alcoholic fatty liver disease: Study protocol for a parallel-armed, randomized controlled trial
Jinghan Xu, Chunli Piao, Yue Qu, Tianjiao Liu, Yuting Peng, Qi Li, Xiaohua Zhao, Pei Li, Xuemin Wu, Yawen Fan, Binqin Chen, Jie Yang
Frontiers in Pharmacology.2022;[Epub] CrossRef - Intestinal microbiota in the treatment of metabolically associated fatty liver disease
Ji-Shuai Wang, Jin-Chun Liu
World Journal of Clinical Cases.2022; 10(31): 11240. CrossRef - Efficiency of combined antihypertensive pharmacotherapy in patients with arterial hypertension, combined with type 2 diabetes mellitus and non-alcoholic fatty liver disease
I. A. Lukonin, V. V. Skibitsky, A. V. Fendrikova, I. I. Pavlyuchenko, K. Yu. Lazarev, F. A. Kovalenko
Systemic Hypertension.2022; 19(1): 31. CrossRef - Diosgenin Ameliorated Type II Diabetes-Associated Nonalcoholic Fatty Liver Disease through Inhibiting De Novo Lipogenesis and Improving Fatty Acid Oxidation and Mitochondrial Function in Rats
Yujie Zhong, Zhiman Li, Ruyi Jin, Yanpeng Yao, Silan He, Min Lei, Xin Wang, Chao Shi, Li Gao, Xiaoli Peng
Nutrients.2022; 14(23): 4994. CrossRef - Pluchea indica Leaf Extract Alleviates Dyslipidemia and Hepatic Steatosis by Modifying the Expression of Lipid Metabolism-Related Genes in Rats Fed a High Fat-High Fructose Diet
Patcharin Singdam, Jarinyaporn Naowaboot, Laddawan Senggunprai, Kampeebhorn Boonloh, Patchareewan Pannangpetch
Preventive Nutrition and Food Science.2022; 27(4): 384. CrossRef - NAFLDin type 2 diabetes mellitus: Still many challenging questions
Simona Cernea, Itamar Raz
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - Umbilical Cord-Mesenchymal Stem Cell-Conditioned Medium Improves Insulin Resistance in C2C12 Cell
Kyung-Soo Kim, Yeon Kyung Choi, Mi Jin Kim, Jung Wook Hwang, Kyunghoon Min, Sang Youn Jung, Soo-Kyung Kim, Yong-Soo Choi, Yong-Wook Cho
Diabetes & Metabolism Journal.2021; 45(2): 260. CrossRef - Comparative Efficacy of Lobeglitazone Versus Pioglitazone on Albuminuria in Patients with Type 2 Diabetes Mellitus
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes Therapy.2021; 12(1): 171. CrossRef - Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: Diagnosis and Treatment
Sook Jung Lee, Byung-Wan Lee
The Journal of Korean Diabetes.2021; 22(1): 38. CrossRef - Patient Management in Non-Alcoholic Fatty Liver Disease and Type 2 Diabetes Mellitus
A. E. Bagriy, A. D. Zubov, M. V. Khomenko, E. S. Mikhailichenko, E. A. Pylaeva, N. A. Khaustova, E. V. Bryukhovetskaya
Russian Journal of Gastroenterology, Hepatology, Coloproctology.2021; 31(2): 14. CrossRef - NAFLD and its link with diabetes: Why we should be worried
Louise Cremonesini, Emma Harkin
Independent Nurse.2021; 2021(8): 20. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef - Fatty liver index and development of cardiovascular disease in Koreans without pre-existing myocardial infarction and ischemic stroke: a large population-based study
Jun Hyung Kim, Jin Sil Moon, Seok Joon Byun, Jun Hyeok Lee, Dae Ryong Kang, Ki Chul Sung, Jang Young Kim, Ji Hye Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Novel antisense inhibition of diacylglycerol O-acyltransferase 2 for treatment of non-alcoholic fatty liver disease: a multicentre, double-blind, randomised, placebo-controlled phase 2 trial
Rohit Loomba, Erin Morgan, Lynnetta Watts, Shuting Xia, Lisa A Hannan, Richard S Geary, Brenda F Baker, Sanjay Bhanot
The Lancet Gastroenterology & Hepatology.2020; 5(9): 829. CrossRef - Hepatic fibrosis is associated with total proteinuria in Korean patients with type 2 diabetes
Eugene Han, Yongin Cho, Kyung-won Kim, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-wan Lee
Medicine.2020; 99(33): e21038. CrossRef - Metabolic liver disease in diabetes – From mechanisms to clinical trials
Bedair Dewidar, Sabine Kahl, Kalliopi Pafili, Michael Roden
Metabolism.2020; 111: 154299. CrossRef - Managing NAFLD in Type 2 Diabetes: The Effect of Lifestyle Interventions, a Narrative Review
Siôn A. Parry, Leanne Hodson
Advances in Therapy.2020; 37(4): 1381. CrossRef -
Diabetes and Metabolism Journal in 2020: Good to Great
In-Kyung Jeong
Diabetes & Metabolism Journal.2020; 44(1): 1. CrossRef - Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 382. CrossRef - Molecular mechanisms of hepatic insulin resistance in nonalcoholic fatty liver disease and potential treatment strategies
Chang-hua Zhang, Bu-gao Zhou, Jun-qing Sheng, Yang Chen, Ying-qian Cao, Chen Chen
Pharmacological Research.2020; 159: 104984. CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef - Effects of sodium–glucose cotransporter 2 inhibitors on non‐alcoholic fatty liver disease in patients with type 2 diabetes: A meta‐analysis of randomized controlled trials
Baodi Xing, Yuhang Zhao, Bingzi Dong, Yue Zhou, Wenshan Lv, Wenjuan Zhao
Journal of Diabetes Investigation.2020; 11(5): 1238. CrossRef - Empaglifozin mitigates NAFLD in high-fat-fed mice by alleviating insulin resistance, lipogenesis and ER stress
Tamiris Ingrid Petito-da-Silva, Vanessa Souza-Mello, Sandra Barbosa-da-Silva
Molecular and Cellular Endocrinology.2019; 498: 110539. CrossRef
- Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
- Obesity and Metabolic Syndrome
- Metabolic Consequences of Obstructive Sleep Apnea Especially Pertaining to Diabetes Mellitus and Insulin Sensitivity
- Sun Ok Song, Ken He, Radhika R. Narla, Hyun Goo Kang, Han Uk Ryu, Edward J. Boyko
- Diabetes Metab J. 2019;43(2):144-155. Published online April 15, 2019
- DOI: https://doi.org/10.4093/dmj.2018.0256
- 7,114 View
- 147 Download
- 43 Web of Science
- 42 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Obstructive sleep apnea (OSA) and diabetes has been known to be closely related to each other and both diseases impact highly on the public health. There are many evidence of reports that OSA is associated with diabetes with a bidirectional correlation. A possible causal mechanism of OSA to diabetes is intermittent hypoxemia and diabetes to OSA is microvascular complication. However, OSA and diabetes have a high prevalence rate in public and shares the common overlap characteristic and risk factors such as age, obesity, and metabolic syndrome that make it difficult to establish the exact pathophysiologic mechanism between them. In addition, studies demonstrating that treatment of OSA may help prevent diabetes or improve glycemic control have not shown convincing result but have become a great field of interest research. This review outlines the bidirectional correlation between OSA and diabetes and explore the pathophysiologic mechanisms by approaching their basic etiologies.
-
Citations
Citations to this article as recorded by- Airway Collapsibility during Drug‐Induced Sleep Endoscopy Relates with Clinical Features of Obstructive Sleep Apnea
Manan Parekh, Vasiliki Triantafillou, Brendan T. Keenan, Everett G. Seay, Eric Thuler, Alan R. Schwartz, Raj C. Dedhia
The Laryngoscope.2024; 134(4): 1978. CrossRef - Clinical features and predictors of metabolic syndrome among obstructive sleep apnea patients
Safy Zahid Kaddah, Merna Hamada Korany, Eman Kamal Ibrahim
The Egyptian Journal of Bronchology.2024;[Epub] CrossRef - Role of Sleep and Sleep Disorders in Cardiometabolic Risk: a Review and Update
Shaden O. Qasrawi, Ahmed S. BaHammam
Current Sleep Medicine Reports.2024; 10(1): 34. CrossRef - Evaluate the Relationship Between Obstructive Sleep Apnea and Metabolic Syndrome in Real-World Data
Renzhe Tang, Chong Li, Dongmei Di, Lin Zhou, Yongxiang Qian, Chaohua Qiang, Chao Ma, Rui Zhou, Bin Wang, Min Wang
Nature and Science of Sleep.2024; Volume 16: 217. CrossRef - Metabolic Crossroads: Unveiling the Complex Interactions between Obstructive Sleep Apnoea and Metabolic Syndrome
Aisling Heffernan, Darko Duplancic, Marko Kumric, Tina Ticinovic Kurir, Josko Bozic
International Journal of Molecular Sciences.2024; 25(6): 3243. CrossRef - The benefits of hypoglycemic therapy for patients with obstructive sleep apnea
Ruihan Lin, Wenjie Yan, Meng He, Bin Liu, Xiaoli Su, Minhan Yi, Yuan Zhang
Sleep and Breathing.2024;[Epub] CrossRef - Endocrine disorders in obstructive sleep apnoea syndrome: A bidirectional relationship
Maud Akset, Kris Gustave Poppe, Pierre Kleynen, Ionela Bold, Marie Bruyneel
Clinical Endocrinology.2023; 98(1): 3. CrossRef - Association between snoring and insulin levels in the US population: a cross-sectional study
Kun Wang, Xuzhong Hu, Ziao Li, Michael Smolinski, Wenjie Xiao, Jinshen He
Sleep and Breathing.2023; 27(3): 1185. CrossRef - Sleep disordered breathing and haemoglobin A1c levels within or over normal range and ageing or sex differences: the Nagahama study
Takeshi Matsumoto, Kimihiko Murase, Yasuharu Tabara, Takuma Minami, Osamu Kanai, Hirofumi Takeyama, Hironobu Sunadome, Tadao Nagasaki, Naomi Takahashi, Yoshinari Nakatsuka, Satoshi Hamada, Tomohiro Handa, Kiminobu Tanizawa, Isuzu Nakamoto, Tomoko Wakamura
Journal of Sleep Research.2023;[Epub] CrossRef - Acceptability, adaptability and adherence to CPAP therapy among Aboriginal Australians with OSA - “The A5 study”
Subash S. Heraganahally, Timothy P. Howarth, Ara J. Perez, Jessie Crespo, Charmain B. Atos, Brian J. Cluney, Linda P. Ford
Sleep Medicine.2023; 102: 147. CrossRef - Comorbid obstructive sleep apnea is associated with adverse cardiovascular outcomes in female patients with acute coronary syndrome complicating metabolic syndrome
Bin Wang, Xiaogang Liu, Wen Hao, Jingyao Fan, Bin Que, Hui Ai, Xiao Wang, Shaoping Nie
Clinical Cardiology.2023; 46(6): 663. CrossRef - Dyslipidemia prevalence in nonobese, nondiabetic patients with obstructive sleep apnea: does sex matter?
Ozen K. Basoglu, Mehmet Sezai Tasbakan, Meral Kayikcioglu
Journal of Clinical Sleep Medicine.2023; 19(5): 889. CrossRef - Plasma tRF-16-79MP9PD and tRF-28-OB1690PQR304 as potential biomarkers for 4- to 7-year-old children with obstructive sleep apnea-hypopnea syndrome
Junhua Wu, Xiaohong Cai, Yanbo Lu, Yijing Shen, Zhisen Shen, Qin Lyv
Frontiers in Pediatrics.2023;[Epub] CrossRef - Association of obstructive sleep apnea with cardiometabolic diseases and cardiovascular mortality
Jia Gao, Licheng Shi, Xuanfeng Zhu, Jiannan Liu
The Clinical Respiratory Journal.2023; 17(8): 764. CrossRef - Comparison of the Patients with Diabetes Mellitus using Either Insulin or Oral Antidiabetic Drug in Terms of Difficult Laryngoscopy: A Randomized Controlled Study
M Win, K Erkalp, S Demirgan, FG Ozcan, MS Sevdi, A Selcan
Nigerian Journal of Clinical Practice.2023; 26(10): 1423. CrossRef - Evaluation of the Continuous Positive Airway Pressure Effect on Neurotrophins’ Gene Expression and Protein Levels
Agata Gabryelska, Szymon Turkiewicz, Marta Ditmer, Adrian Gajewski, Piotr Białasiewicz, Dominik Strzelecki, Maciej Chałubiński, Marcin Sochal
International Journal of Molecular Sciences.2023; 24(23): 16599. CrossRef - Insulin Resistance, but Not Obstructive Sleep Apnea Is Associated with Hepatic Steatosis in Chinese Patients with Severe Obesity
Chonggui Zhu, Shaofang Tang, Jinfeng Xiao, Yang Zhang, Longhao Sun, Jing Zhang, Li Ding, Ming Liu
Obesity Facts.2023; 16(4): 344. CrossRef - The effects of an exercise program on inflammation in adults who differ according to obstructive sleep apnea severity
Devon A. Dobrosielski, Karla A. Kubitz, Mary F. Walter, Hyunjeong Park, Christopher Papandreou, Susheel P. Patil
Sleep and Biological Rhythms.2023;[Epub] CrossRef - Association of Metabolic Syndrome With Long-Term Cardiovascular Risks and All-Cause Mortality in Elderly Patients With Obstructive Sleep Apnea
Lin Liu, Xiaofeng Su, Zhe Zhao, Jiming Han, Jianhua Li, Weihao Xu, Zijun He, Yinghui Gao, Kaibing Chen, Libo Zhao, Yan Gao, Huanhuan Wang, JingJing Guo, Junling Lin, Tianzhi Li, Xiangqun Fang
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Therapeutic effect of laparoscopic sleeve gastrectomy on obstructive sleep apnea and relationship of type 2 diabetes in Japanese patients with severe obesity
Shingo Yanari, Akira Sasaki, Akira Umemura, Yasushi Ishigaki, Haruka Nikai, Tsuguo Nishijima, Shigeru Sakurai
Journal of Diabetes Investigation.2022; 13(6): 1073. CrossRef - Advances in the study of OSA and diabetic foot
Jiayu Lin, Hailing Song, Meihong Liang, Zeqiang Cai, Tan Chen, Zhenyu Lin, Jinying Zhang
Diabetology & Metabolic Syndrome.2022;[Epub] CrossRef - VEGF Receptor 1 Promotes Hypoxia-Induced Hematopoietic Progenitor Proliferation and Differentiation
Jonathan Florentin, Scott P. O’Neil, Lee L. Ohayon, Afaz Uddin, Sathish Babu Vasamsetti, Anagha Arunkumar, Samit Ghosh, Jennifer C. Boatz, Justin Sui, Corrine R. Kliment, Stephen Y. Chan, Partha Dutta
Frontiers in Immunology.2022;[Epub] CrossRef - Sleep Deficiency in Obstructive Sleep Apnea
Olurotimi Adekolu, Andrey Zinchuk
Clinics in Chest Medicine.2022; 43(2): 353. CrossRef - Intermittent Hypoxia Interferes with Autocrine Effects of GABA on Insulin Secretion in Postnatal Rodents—Implications for Pediatric Obstructive Sleep Apnea
Eung-Kwon Pae, Man-Kyo Chung, Ronald M. Harper
Children.2022; 9(9): 1305. CrossRef - CPAP Influence on Readily Available Inflammatory Markers in OSA—A Pilot Study
Ioana Madalina Zota, Cristina Andreea Adam, Dragoș Traian Marius Marcu, Cristian Stătescu, Radu Sascău, Larisa Anghel, Daniela Boișteanu, Mihai Roca, Corina Lucia Dima Cozma, Alexandra Maștaleru, Maria Magdalena Leon Constantin, Elena Andreea Moaleș, Flor
International Journal of Molecular Sciences.2022; 23(20): 12431. CrossRef - Body weight and obstructive sleep apnea: a mathematical relationship between body mass index and apnea-hypopnea index in veterans
Deema Fattal, Stacy Hester, Linder Wendt
Journal of Clinical Sleep Medicine.2022; 18(12): 2723. CrossRef - Hypoxia signaling and cholesterol/steroidogenic acute regulatory protein 1 axis: interplay and role in alcohol and non-alcohol-related liver diseases
Sandra Torres, Jose C. Fernandez-Checa, Carmen Garcia-Ruiz
Exploration of Digestive Diseases.2022; : 170. CrossRef - Obstructive Sleep Apnea, Circadian Clock Disruption, and Metabolic Consequences
Mikołaj Malicki, Filip Franciszek Karuga, Bartosz Szmyd, Marcin Sochal, Agata Gabryelska
Metabolites.2022; 13(1): 60. CrossRef - The relationship between metabolic syndrome and obstructive sleep apnea syndrome: a nationwide population-based study
Do Hyun Kim, Bongseong Kim, Kyungdo Han, Soo Whan Kim
Scientific Reports.2021;[Epub] CrossRef - Triglyceride-Glucose Index in Non-Diabetic, Non-Obese Patients with Obstructive Sleep Apnoea
Andras Bikov, Stefan M. Frent, Martina Meszaros, Laszlo Kunos, Alexander G. Mathioudakis, Alina Gabriela Negru, Laura Gaita, Stefan Mihaicuta
Journal of Clinical Medicine.2021; 10(9): 1932. CrossRef - Evidence of an Association of Obstructive Sleep Apnea with Diabetes and Diabetic Complications
Takeshi Matsumoto, Toyohiro Hirai, Kazuo Chin
Current Sleep Medicine Reports.2021; 7(4): 186. CrossRef - Relationship between obstructive sleep apnea syndrome and functional capacity in patients with diabetes mellitus type 2: an observational transversal study
Moyrane Abreu da Fonseca, Alana Karina Silva Moreira, Railsa Bertilla dos Santos Lima, Marcela de Araújo Oliveira, Aldair Darlan Santos-de-Araújo, Adriana Sousa Rêgo, Ludmilia Rodrigues Lima Neuenschwander Penha, Patrícia Rodrigues Ferreira, Maria Cláudia
Revista da Associação Médica Brasileira.2021; 67(6): 878. CrossRef - Effects of Intermittent Hypoxia on Cytokine Expression Involved in Insulin Resistance
Tomoko Uchiyama, Hiroyo Ota, Chiho Ohbayashi, Shin Takasawa
International Journal of Molecular Sciences.2021; 22(23): 12898. CrossRef - Novel screening model of obstructive sleep apnea for snorers with suspected NAFLD undergoing liver sonography
Yang-Bor Lu, Yu-Chieh Weng, Yung-Ning Huang, Hsiung-Ying Huang, Pei-Ting Cheng, Hui-Shan Hsieh, Ming-Shao Tsai
BMC Pulmonary Medicine.2021;[Epub] CrossRef - Short sleep duration and food intake: an overview and analysis of the influence of the homeostatic and hedonic system
Natálie Brito Gissoni, Marcus Vinicius Lucio dos Santos Quaresma
Nutrire.2020;[Epub] CrossRef - Perioperative implications and prevalence of Obstructive Sleep Apnea risk in a surgical population using the updated STOP-Bang questionnaire
Amr Elkouny, Mohamed AlHarbi, Vassilios Dimitriou, Ali Muzafar, Ali Nawaz, Amel Fayed
Trends in Anaesthesia and Critical Care.2020; 30: 1. CrossRef Obstructive Sleep Apnea Exacerbates Glucose Dysmetabolism and Pancreatic β-Cell Dysfunction in Overweight and Obese Nondiabetic Young Adults
Ning Li, Yun Fan, Jian Ping Zhou, Ocholi Don Maimba, Liu Zhang, Qing Yun Li
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 2465. CrossRef- Sleep disturbances: one of the culprits of obesity-related cardiovascular risk?
Giovanna Muscogiuri, Dario Tuccinardi, Vincenzo Nicastro, Luigi Barrea, Annamaria Colao, Silvia Savastano
International Journal of Obesity Supplements.2020; 10(1): 62. CrossRef - Mild maternal sleep-disordered breathing during pregnancy and offspring growth and adiposity in the first 3 years of life
Avivit Brener, Yael Lebenthal, Sigal Levy, Galit Levi Dunietz, Orna Sever, Riva Tauman
Scientific Reports.2020;[Epub] CrossRef - Association of parameters of nocturnal hypoxemia with diabetic microvascular complications: A cross-sectional study
Pei Xue, Naima Covassin, Xingwu Ran, Junying Zhou, Xiaohan Zhang, Donge Yan, Xiao Li, Yun Gao, Xiangdong Tang
Diabetes Research and Clinical Practice.2020; 170: 108484. CrossRef - Dynamic changes in nocturnal blood glucose levels are associated with sleep-related features in patients with obstructive sleep apnea
Jung-Ick Byun, Kwang Su Cha, Ji Eun Jun, Tae-Joon Kim, Ki-Young Jung, In-Kyung Jeong, Won Chul Shin
Scientific Reports.2020;[Epub] CrossRef - Obstructive Sleep Apnea and Pain
Konstantina Nikolaou, Athanasios Voulgaris, Paschalis Steiropoulos
Current Sleep Medicine Reports.2019; 5(3): 95. CrossRef
- Airway Collapsibility during Drug‐Induced Sleep Endoscopy Relates with Clinical Features of Obstructive Sleep Apnea
- Complications
- Nonalcoholic Fatty Liver Disease in Diabetes. Part I: Epidemiology and Diagnosis
- Yong-ho Lee, Yongin Cho, Byung-Wan Lee, Cheol-Young Park, Dae Ho Lee, Bong-Soo Cha, Eun-Jung Rhee
- Diabetes Metab J. 2019;43(1):31-45. Published online December 17, 2018
- DOI: https://doi.org/10.4093/dmj.2019.0011
- Correction in: Diabetes Metab J 2019;43(5):731
- 8,106 View
- 166 Download
- 106 Web of Science
- 101 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Nonalcoholic fatty liver disease (NAFLD) and diabetes are common metabolic disorders whose prevalence rates are expected to rise worldwide, corresponding to aging and increasingly obese populations. Compared to the general population (around 25%), 50% to 70% of people with diabetes have NAFLD, and NAFLD severity (including fibrosis) tends to be worsened by the presence of diabetes. NAFLD is considered an emerging risk factor for type 2 diabetes mellitus and a contributor to the development of chronic diabetes-related complications. This reciprocal relationship demonstrates the importance of confirming suspected NAFLD in patients with diabetes. Due to the invasive nature of liver biopsy to assess NAFLD status, various alternative non-invasive modalities have been developed and validated. Here, we summarized the epidemiology of NAFLD in patients with diabetes and reviewed currently available imaging modalities and biomarker-based prediction models for their ability to detect liver steatosis and/or fibrosis.
-
Citations
Citations to this article as recorded by- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
Eugene Han, Byung-Wan Lee, Eun Seok Kang, Bong-Soo Cha, Sang Hoon Ahn, Yong-ho Lee, Seung Up Kim
Metabolism.2024; 152: 155789. CrossRef - Intact ketogenesis predicted reduced risk of moderate-severe metabolic-associated fatty liver disease assessed by liver transient elastography in newly diagnosed type 2 diabetes
Sejeong Lee, Jaehyun Bae, Seung Up Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Frontiers in Endocrinology.2024;[Epub] CrossRef - ZJU Index as a Predictive Tool for Diabetes Incidence: Insights from a Population-Based Cohort Study
Chenjiao Wu, Yi Hao Loh, Hangkai Huang, Chengfu Xu
Diabetes, Metabolic Syndrome and Obesity.2024; Volume 17: 715. CrossRef - Sigmoidal relationship between liver fat content and nonalcoholic fatty liver disease in Chinese adults
Pingping Yu, Huachao Yang, Hu Li, Ying Mei, Yuanyuan Wu, Hongfeng Cheng, Huiru Su, Yueling Deng, Tao Jiang, Zhongxiang He, Peng Hu
Postgraduate Medical Journal.2024;[Epub] CrossRef - Safety and Efficacy of Efruxifermin in Combination With a GLP-1 Receptor Agonist in Patients With NASH/MASH and Type 2 Diabetes in a Randomized Phase 2 Study
Stephen A. Harrison, Juan P. Frias, K. Jean Lucas, Gary Reiss, Guy Neff, Sureka Bollepalli, Yan Su, Doreen Chan, Erik J. Tillman, Ali Moulton, Brittany de Temple, Arian Zari, Reshma Shringarpure, Timothy Rolph, Andrew Cheng, Kitty Yale
Clinical Gastroenterology and Hepatology.2024;[Epub] CrossRef - Association between nonalcoholic fatty liver disease and left ventricular diastolic dysfunction: A 7-year retrospective cohort study of 3,496 adults using serial echocardiography
Gyuri Kim, Tae Yang Yu, Jae Hwan Jee, Ji Cheol Bae, Mira Kang, Jae Hyeon Kim
Diabetes & Metabolism.2024; : 101534. CrossRef - Plasma Adiponectin and Its Correlation with Carotid Intima-Media Thickness in Obesity and in Type 2 Diabetes and Nonalcoholic Fatty Liver Disease
Maha Hussein, Aasem Saif, Mona Amin, Osama Khalafallah, Ahmed Hussien, Samar Aboulsoud, Shrook Mousa, S. Razzaque Mohammed
Journal of Nutrition and Metabolism.2023; 2023: 1. CrossRef - Exposure to Bisphenol A, S, and F and its Association with Obesity and Diabetes Mellitus in General Adults of Korea: Korean National Environmental Health Survey (KoNEHS) 2015–2017
Min Kyong Moon, Min Joo Kim, Inae Lee, Sunmi Kim, Sohyeon Choi, Jeongim Park, Yoon Hee Cho, Sooyeon Hong, Jiyoung Yoo, Hyunwoong Park, Gi Jeong Cheon, Young Joo Park, Kyungho Choi
Exposure and Health.2023; 15(1): 53. CrossRef - Liver fat content assessed by conventional B-mode ultrasound and metabolic profile in non-diabetic patients: Implications for clinical practice
Rosanna Villani, Grazia Pia Magnati, Giulia Tuccari, Moris Sangineto, Antonino Davide Romano, Tommaso Cassano, Gaetano Serviddio
Ultrasound.2023; 31(3): 177. CrossRef - Association of cardiovascular health metrics with annual incidence of prediabetes or diabetes: Analysis of a nationwide real‐world database
Akira Okada, Hidehiro Kaneko, Satoshi Matsuoka, Hidetaka Itoh, Yuta Suzuki, Katsuhito Fujiu, Nobuaki Michihata, Taisuke Jo, Norifumi Takeda, Hiroyuki Morita, Satoko Yamaguchi, Koichi Node, Toshimasa Yamauchi, Hideo Yasunaga, Issei Komuro
Journal of Diabetes Investigation.2023; 14(3): 452. CrossRef - Effects of Environmental Cadmium Exposure on the Liver in Korean Adults: Cross-Sectional and Longitudinal Studies
Mi-Na Seo, Sang-Yong Eom, Ji-Ae Lim, Jung-Eum Lee, Byung-Sun Choi, Ho-Jang Kwon, Young-Seoub Hong, Heon Kim, Jung-Duck Park
Archives of Environmental Contamination and Toxicology.2023; 84(2): 237. CrossRef - Newer Glucose-Lowering Therapies in Older Adults with Type 2 Diabetes
Anika Bilal, Richard E. Pratley
Endocrinology and Metabolism Clinics of North America.2023; 52(2): 355. CrossRef - CD24 Gene Expression as a Risk Factor for Non-Alcoholic Fatty Liver Disease
Mona A. Amin, Halla M. Ragab, Nabila Abd El Maksoud, Wafaa Abd Elaziz
Diagnostics.2023; 13(5): 984. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Mortality: A Population-Based Cohort Study
Kyung-Soo Kim, Sangmo Hong, Hong-Yup Ahn, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(2): 220. CrossRef - Non-Alcoholic Fatty Liver Disease with Sarcopenia and Carotid Plaque Progression Risk in Patients with Type 2 Diabetes Mellitus
Yongin Cho, Hye-Sun Park, Byung Wook Huh, Yong-ho Lee, Seong Ha Seo, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, So Hun Kim
Diabetes & Metabolism Journal.2023; 47(2): 232. CrossRef - Nonalcoholic fatty liver disease and type 2 diabetes: an observational and Mendelian randomization study
Yuetian Yu, Yuefeng Yu, Yuying Wang, Yi Chen, Ningjian Wang, Bin Wang, Yingli Lu
Frontiers in Endocrinology.2023;[Epub] CrossRef - β-sitosterol attenuates high- fat diet-induced hepatic steatosis in rats by modulating lipid metabolism, inflammation and ER stress pathway
Omayma AR Abo-Zaid, Fatma SM Moawed, Effet Soliman Ismail, Mostafa A. Farrag
BMC Pharmacology and Toxicology.2023;[Epub] CrossRef - Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(3): 347. CrossRef - Increased expression of sodium-glucose cotransporter 2 and O-GlcNAcylation in hepatocytes drives non-alcoholic steatohepatitis
Hye Jin Chun, Eun Ran Kim, Minyoung Lee, Da Hyun Choi, Soo Hyun Kim, Eugene Shin, Jin-Hong Kim, Jin Won Cho, Dai Hoon Han, Bong-Soo Cha, Yong-ho Lee
Metabolism.2023; 145: 155612. CrossRef - Role of vascular endothelial growth factor B in nonalcoholic fatty liver disease and its potential value
Yu-Qi Li, Lei Xin, Yu-Chi Zhao, Shang-Qi Li, Ya-Nuo Li
World Journal of Hepatology.2023; 15(6): 786. CrossRef - Increased risk of incident diabetes in patients with MAFLD not meeting the criteria for NAFLD
So Hee Park, Jiyun Park, So Yoon Kwon, You-Bin Lee, Gyuri Kim, Kyu Yeon Hur, Janghyun Koh, Jae Hwan Jee, Jae Hyeon Kim, Mira Kang, Sang-Man Jin
Scientific Reports.2023;[Epub] CrossRef - Significance of Diabetic Kidney Disease Biomarkers in Predicting Metabolic-Associated Fatty Liver Disease
Jaehyun Bae, Byung-Wan Lee
Biomedicines.2023; 11(7): 1928. CrossRef - An Evidence-Based Review of Diabetes Care: History, Types, Relationship
to Cancer and Heart Disease, Co-Morbid Factors, and Preventive
Measures
Umesh Chandra Gupta, Subhas Chandra Gupta, Shayle Sugandh Gupta
Current Nutrition & Food Science.2023; 19(4): 399. CrossRef - Associations of serum aminotransferase and the risk of all-cause and cause-specific mortality in Chinese type 2 diabetes: a community-based cohort study
Jian Su, Haoyu Guan, Xikang Fan, Hao Yu, Yu Qin, Jie Yang, Zheng Zhu, Chong Shen, Enchun Pan, Yan Lu, Jin-Yi Zhou, Ming Wu
BMJ Open.2023; 13(7): e068160. CrossRef - Retinoic acid signaling in fatty liver disease
Fathima N. Cassim Bawa, Yanqiao Zhang
Liver Research.2023; 7(3): 189. CrossRef - Pharmaceutical Strategies to Improve Druggability of Potential Drug Candidates in Nonalcoholic Fatty Liver Disease Therapy
Reeju Amatya, Donghee Lee, Kyoung Ah Min, Meong Cheol Shin
Pharmaceutics.2023; 15(7): 1963. CrossRef - Prevalence of Non-Alcoholic Fatty Liver Disease and Its Risk Factors in Korean Population
Sang Gyeong Lee, Songchan Oh, Moon Seong Kim, Jooyeon Kim, Eunjin Jung, Young Jun Kim, Jiyoun Hong
Food Supplements and Biomaterials for Health.2023;[Epub] CrossRef - Low‑dose ionizing radiation attenuates high glucose‑induced hepatic apoptosis and immune factor release via modulation of a miR‑155‑SOCS1 axis
Hongqiong Fan, Shanshan Liu, Benzheng Jiao, Xinyue Liang
Molecular Medicine Reports.2023;[Epub] CrossRef - CT-based measurement of visceral adipose tissue volume as a reliable tool for assessing metabolic risk factors in prediabetes across subtypes
Jihyun Kim, Keunyoung Kim
Scientific Reports.2023;[Epub] CrossRef - The Role of the Fatty Liver Index (FLI) in the Management of Non-Alcoholic Fatty Liver Disease: A Systematic Review
Teodora Biciusca, Sorina Ionelia Stan, Mara Amalia Balteanu, Ramona Cioboata, Alice Elena Ghenea, Suzana Danoiu, Ana-Maria Bumbea, Viorel Biciusca
Diagnostics.2023; 13(21): 3316. CrossRef - Circ_0004535/miR-1827/CASP8 network involved in type 2 diabetes mellitus with nonalcoholic fatty liver disease
Min Li, Ai Zeng, Xinle Tang, Hui Xu, Wei Xiong, Yanying Guo
Scientific Reports.2023;[Epub] CrossRef - Prevalence of High and Moderate Risk of Liver Fibrosis Among Patients With Diabetes at a Noncommunicable Diseases (NCD) Clinic in a Primary Healthcare Center in Northern India
Anubhav Mondal, Aninda Debnath, Ghurumourthy Dhandapani, Abhishek Sharma, Shveta Lukhmana, Geeta Yadav
Cureus.2023;[Epub] CrossRef - Therapeutic outcome of dapagliflozin on various parameters in non-alcoholic fatty liver disease (NAFLD) patients
Mazhar Hussain, Muhammad Zafar Majeed Babar, Saba Tariq, Muhammad Irfan Ahmad, Lubna Akhtar
International Journal of Diabetes in Developing Countries.2022; 42(2): 290. CrossRef - Lead, mercury, and cadmium exposures are associated with obesity but not with diabetes mellitus: Korean National Environmental Health Survey (KoNEHS) 2015–2017
Min Kyong Moon, Inae Lee, Aram Lee, Hyunwoong Park, Min Joo Kim, Sunmi Kim, Yoon Hee Cho, Sooyeon Hong, Jiyoung Yoo, Gi Jeong Cheon, Kyungho Choi, Young Joo Park, Jeongim Park
Environmental Research.2022; 204: 111888. CrossRef - Association of Prenatal Famine Exposure With Inflammatory Markers and Its Impact on Adulthood Liver Function Across Consecutive Generations
Shiwei Yan, Jingqi Ruan, Yu Wang, Jiaxu Xu, Changhao Sun, Yucun Niu
Frontiers in Nutrition.2022;[Epub] CrossRef - Serum Metabolomics in Patients with Coexisting NAFLD and T2DM Using Liquid Chromatography-Mass Spectrometry
Cheng Hu, Xiaoyu Zhuang, Jiaqi Zhang, Tao Wang, Shengnan Du, Jinping Wang, Xuelian Peng, Qin Cao, Mingcai Zhang, Yuanye Jiang
Laboratory Medicine.2022; 53(4): 360. CrossRef - Genistein—Opportunities Related to an Interesting Molecule of Natural Origin
Ewa Garbiec, Judyta Cielecka-Piontek, Magdalena Kowalówka, Magdalena Hołubiec, Przemysław Zalewski
Molecules.2022; 27(3): 815. CrossRef - Renal Tubular Damage Marker, Urinary N-acetyl-β-D-Glucosaminidase, as a Predictive Marker of Hepatic Fibrosis in Type 2 Diabetes Mellitus
Hae Kyung Kim, Minyoung Lee, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-Wan Lee
Diabetes & Metabolism Journal.2022; 46(1): 104. CrossRef - Long-term effects of the changes in hepatic steatosis status on the risk of incident type 2 diabetes mellitus: A 15-year community-based prospective cohort study
Seung Min Chung, Min Kyu Kang, Jinho Jung, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee, Rohit Loomba, Jung Gil Park, Jun Sung Moon
Diabetes Research and Clinical Practice.2022; 184: 109208. CrossRef - Prevalence and Risk Factors of Advanced Liver Fibrosis in a Population‐Based Study in Germany
Yvonne Huber, Andreas Schulz, Irene Schmidtmann, Manfred Beutel, Norbert Pfeiffer, Thomas Münzel, Peter R. Galle, Philipp S. Wild, Karl J. Lackner, Jörn M. Schattenberg
Hepatology Communications.2022; 6(6): 1457. CrossRef - Non-alcoholic fatty liver disease: Epidemiology, pathophysiology and an update on the therapeutic approaches
RehabF Abdel-Rahman
Asian Pacific Journal of Tropical Biomedicine.2022; 12(3): 99. CrossRef - State-of-the-Art Overview of the Pharmacological Treatment of Non-Alcoholic Steatohepatitis
Yongin Cho, Yong-ho Lee
Endocrinology and Metabolism.2022; 37(1): 38. CrossRef - Obesity is an important determinant of severity in newly defined metabolic dysfunction-associated fatty liver disease
Ji Hye Huh, Kwang Joon Kim, Seung Up Kim, Bong-Soo Cha, Byung-Wan Lee
Hepatobiliary & Pancreatic Diseases International.2022; 21(3): 241. CrossRef - The associations of hepatic steatosis and fibrosis using fatty liver index and BARD score with cardiovascular outcomes and mortality in patients with new-onset type 2 diabetes: a nationwide cohort study
Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef - Sociodemographic and genetic determinants of nonalcoholic fatty liver disease in type 2 diabetes mellitus patients
Muhammad Adnan, Abdul Wajid, Wasif Noor, Andleeb Batool, Muhammad Aasim, Kamran Abbas, Quratul Ain
Journal of Genetic Engineering and Biotechnology.2022; 20(1): 68. CrossRef - Concordance between indirect fibrosis and steatosis indices and their predictors in subjects with overweight/obesity
Gaggini Melania, Vigna Luisella, Di Piazza Salvina, Gori Francesca, Tirelli Amedea Silvia, Bamonti Fabrizia, Maltinti Maristella, Napolitano Filomena, Chatzianagnostou Kyriazoula, Cristina Vassalle
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity.2022; 27(7): 2617. CrossRef - Stéatopathie métabolique hépatique évaluée par le FibroScan® avec contrôle des paramètres d’atténuation (CAP) chez la personne diabétique de type 2 en Côte d’Ivoire
Jacko Abodo, Dimitri Kouamé, Jocelyne Danho, Moumouni Léilatou, Pierre Koffi-Dago, Adelaïde Hué, Assita Yao, Franck Kouassi, Anselme N’Guessan, Fulgence Bathaix
Médecine des Maladies Métaboliques.2022; 16(6): 550. CrossRef - Non-invasive diagnosis and staging of non-alcoholic fatty liver disease
Stergios Kechagias, Mattias Ekstedt, Christian Simonsson, Patrik Nasr
Hormones.2022; 21(3): 349. CrossRef - Association between organochlorine pesticides and nonalcoholic fatty liver disease in the National Health and Nutrition Examination Survey 2003–2004
Hyunji Sang, Kyu-Na Lee, Chang Hee Jung, Kyungdo Han, Eun Hee Koh
Scientific Reports.2022;[Epub] CrossRef - Increased Risk of NAFLD in Adults with Glomerular Hyperfiltration: An 8-Year Cohort Study Based on 147,162 Koreans
Dae-Jeong Koo, Mi Yeon Lee, Inha Jung, Sun Joon Moon, Hyemi Kwon, Eun-Jung Rhee, Cheol-Young Park, Won-Young Lee, Ki Won Oh, Se Eun Park
Journal of Personalized Medicine.2022; 12(7): 1142. CrossRef - Advanced Liver Fibrosis Is Associated with Chronic Kidney Disease in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Da Hea Seo, Young Ju Suh, Yongin Cho, Seong Hee Ahn, Seongha Seo, Seongbin Hong, Yong-ho Lee, Young Ju Choi, Eunjig Lee, So Hun Kim
Diabetes & Metabolism Journal.2022; 46(4): 630. CrossRef - New Insights into Non-Alcoholic Fatty Liver Disease and Coronary Artery Disease: The Liver-Heart Axis
Georgiana-Diana Cazac, Cristina-Mihaela Lăcătușu, Cătălina Mihai, Elena-Daniela Grigorescu, Alina Onofriescu, Bogdan-Mircea Mihai
Life.2022; 12(8): 1189. CrossRef - Efficacy and mechanism of Jiedu Tongluo Tiaogan Formula in treating type 2 diabetes mellitus combined with non-alcoholic fatty liver disease: Study protocol for a parallel-armed, randomized controlled trial
Jinghan Xu, Chunli Piao, Yue Qu, Tianjiao Liu, Yuting Peng, Qi Li, Xiaohua Zhao, Pei Li, Xuemin Wu, Yawen Fan, Binqin Chen, Jie Yang
Frontiers in Pharmacology.2022;[Epub] CrossRef - Ultrasound-Based Hepatic Elastography in Non-Alcoholic Fatty Liver Disease: Focus on Patients with Type 2 Diabetes
Georgiana-Diana Cazac, Cristina-Mihaela Lăcătușu, Cătălina Mihai, Elena-Daniela Grigorescu, Alina Onofriescu, Bogdan-Mircea Mihai
Biomedicines.2022; 10(10): 2375. CrossRef - Diosgenin Ameliorated Type II Diabetes-Associated Nonalcoholic Fatty Liver Disease through Inhibiting De Novo Lipogenesis and Improving Fatty Acid Oxidation and Mitochondrial Function in Rats
Yujie Zhong, Zhiman Li, Ruyi Jin, Yanpeng Yao, Silan He, Min Lei, Xin Wang, Chao Shi, Li Gao, Xiaoli Peng
Nutrients.2022; 14(23): 4994. CrossRef - The associations between changes in hepatic steatosis and heart failure and mortality: a nationwide cohort study
Jiyun Park, Gyuri Kim, Hasung Kim, Jungkuk Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef - Recent advances and potentiality of postbiotics in the food industry: Composition, inactivation methods, current applications in metabolic syndrome, and future trends
Yujie Zhong, Tao Wang, Ruilin Luo, Jiayu Liu, Ruyi Jin, Xiaoli Peng
Critical Reviews in Food Science and Nutrition.2022; : 1. CrossRef - Association of nonalcoholic fatty liver disease with coronary artery disease in type 2 diabetes mellitus: A cross-sectional study from a tertiary care medical college hospital
Neelakandan Ramya, Golepu Karthikeya, SethuPrabhu Shankar
Acta Medica International.2022; 9(1): 31. CrossRef - NAFLDin type 2 diabetes mellitus: Still many challenging questions
Simona Cernea, Itamar Raz
Diabetes/Metabolism Research and Reviews.2021;[Epub] CrossRef - The protective effect of shrimp cooked in different methods on high-cholesterol- induced fatty liver in rats
Nora A. AlFaris, Ghedeir M. Alshammari, Jozaa Z. AlTamimi, Lujain A. AlMousa, Nora M. AlKehayez, Dalal H. Aljabryn, Reham I. Alagal, Mohammed A. Yahya
Saudi Journal of Biological Sciences.2021; 28(1): 170. CrossRef - Evolution of liver fibrosis and steatosis markers in patients with type 2 diabetes after metformin treatment for 2 years
Hye Won Lee, Jae Seung Lee, Beom Kyung Kim, Jun Yong Park, Do Young Kim, Sang Hoon Ahn, Seung Up Kim
Journal of Diabetes and its Complications.2021; 35(1): 107747. CrossRef - Prognostic value of non-alcoholic fatty liver disease for predicting cardiovascular events in patients with diabetes mellitus with suspected coronary artery disease: a prospective cohort study
Keishi Ichikawa, Toru Miyoshi, Kazuhiro Osawa, Takashi Miki, Hironobu Toda, Kentaro Ejiri, Masatoki Yoshida, Yusuke Nanba, Masashi Yoshida, Kazufumi Nakamura, Hiroshi Morita, Hiroshi Ito
Cardiovascular Diabetology.2021;[Epub] CrossRef - Implications of Abdominal Adipose Tissue Distribution on Nonalcoholic Fatty Liver Disease and Metabolic Syndrome: A Chinese General Population Study
Chileka Chiyanika, Vincent Wai-Sun Wong, Grace Lai-Hung Wong, Henry Lik-Yuen Chan, Steve C. N. Hui, David K. W. Yeung, Winnie C. W. Chu
Clinical and Translational Gastroenterology.2021; 12(2): e00300. CrossRef - Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: Diagnosis and Treatment
Sook Jung Lee, Byung-Wan Lee
The Journal of Korean Diabetes.2021; 22(1): 38. CrossRef - Pioglitazone for NAFLD Patients With Prediabetes or Type 2 Diabetes Mellitus: A Meta-Analysis
Jingxuan Lian, Jianfang Fu
Frontiers in Endocrinology.2021;[Epub] CrossRef - Allopurinol ameliorates high fructose diet induced hepatic steatosis in diabetic rats through modulation of lipid metabolism, inflammation, and ER stress pathway
In-Jin Cho, Da-Hee Oh, Jin Yoo, You-Cheol Hwang, Kyu Jeung Ahn, Ho-Yeon Chung, Soung Won Jeong, Ju-Young Moon, Sang-Ho Lee, Sung-Jig Lim, In-Kyung Jeong
Scientific Reports.2021;[Epub] CrossRef - Diabetic Kidney Disease, Cardiovascular Disease and Non-Alcoholic Fatty Liver Disease: A New Triumvirate?
Carolina M. Perdomo, Nuria Garcia-Fernandez, Javier Escalada
Journal of Clinical Medicine.2021; 10(9): 2040. CrossRef - Fenofibrate, a PPARα agonist, reduces hepatic fat accumulation through the upregulation of TFEB-mediated lipophagy
Jin Yoo, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung, You-Cheol Hwang
Metabolism.2021; 120: 154798. CrossRef - Association Between Thyroid Hormone Levels and Advanced Liver Fibrosis in Patients with Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease
Jing Du, Sanbao Chai, Xin Zhao, Jianbin Sun, Xiaomei Zhang, Lili Huo
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2021; Volume 14: 2399. CrossRef - Association between toothbrushing and non-alcoholic fatty liver disease
Ji-Youn Kim, Yong-Moon Park, Gyu-Na Lee, Hyun Chul Song, Yu-Bae Ahn, Kyungdo Han, Seung-Hyun Ko, Houkai Li
PLOS ONE.2021; 16(5): e0243686. CrossRef - Non‐alcoholic fatty liver disease and sarcopenia additively increase mortality: a Korean nationwide survey
Joon Ho Moon, Bo Kyung Koo, Won Kim
Journal of Cachexia, Sarcopenia and Muscle.2021; 12(4): 964. CrossRef - Sodium-Glucose Cotransporter-2 Inhibitors Ameliorate Liver Enzyme Abnormalities in Korean Patients With Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Won Euh, Soo Lim, Jin-Wook Kim
Frontiers in Endocrinology.2021;[Epub] CrossRef - Modulation and bioinformatics screening of hepatic mRNA-lncRNAs (HML) network associated with insulin resistance in prediabetic and exercised mice
Fatemeh Kazeminasab, Sayed Mohammad Marandi, Maryam Baharlooie, Mohammad Hossein Nasr-Esfahani, Kamran Ghaedi
Nutrition & Metabolism.2021;[Epub] CrossRef - Liver Fibrosis Indices for the Prediction of Mortality in Korean Subjects: A 16-Year Prospective Cohort Study
Tae Jung Oh, Kyuho Kim, Jae Hoon Moon, Sung Hee Choi, Nam H Cho, Hak Chul Jang
Journal of the Endocrine Society.2021;[Epub] CrossRef - Non-Laboratory-Based Simple Screening Model for Nonalcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Developed Using Multi-Center Cohorts
Jiwon Kim, Minyoung Lee, Soo Yeon Kim, Ji-Hye Kim, Ji Sun Nam, Sung Wan Chun, Se Eun Park, Kwang Joon Kim, Yong-ho Lee, Joo Young Nam, Eun Seok Kang
Endocrinology and Metabolism.2021; 36(4): 823. CrossRef - The association of hepatic steatosis and fibrosis with heart failure and mortality
Jiyun Park, Gyuri Kim, Hasung Kim, Jungkuk Lee, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Cardiovascular Diabetology.2021;[Epub] CrossRef - Magnetic Resonance-Based Assessments Better Capture Pathophysiologic Profiles and Progression in Nonalcoholic Fatty Liver Disease
Seung Joon Choi, Seong Min Kim, Yun Soo Kim, Oh Sang Kwon, Seung Kak Shin, Kyoung Kon Kim, Kiyoung Lee, Ie Byung Park, Cheol Soo Choi, Dong Hae Chung, Jaehun Jung, MunYoung Paek, Dae Ho Lee
Diabetes & Metabolism Journal.2021; 45(5): 739. CrossRef - Albuminuria Is Associated with Steatosis Burden in Patients with Type 2 Diabetes Mellitus and Nonalcoholic Fatty Liver Disease
Eugene Han, Mi Kyung Kim, Byoung Kuk Jang, Hye Soon Kim
Diabetes & Metabolism Journal.2021; 45(5): 698. CrossRef - The potential pathophysiological role of altered lipid metabolism and electronegative low-density lipoprotein (LDL) in non-alcoholic fatty liver disease and cardiovascular diseases
Hüseyin Vural, Ferah Armutcu, Omer Akyol, Ralf Weiskirchen
Clinica Chimica Acta.2021; 523: 374. CrossRef - Increased Visit-to-Visit Liver Enzyme Variability Is Associated with Incident Diabetes: A Community-Based 12-Year Prospective Cohort Study
Kyuhoon Bang, Ji Eun Jun, In-Kyung Jeong, Kyu Jeung Ahn, Ho Yeon Chung, You-Cheol Hwang
Diabetes & Metabolism Journal.2021; 45(6): 890. CrossRef - Efficacy and Safety of GLP-1 Receptor Agonists in Patients With Type 2 Diabetes Mellitus and Non-Alcoholic Fatty Liver Disease: A Systematic Review and Meta-Analysis
Yuan Zhu, Jiao Xu, Dong Zhang, Xingyu Mu, Yi Shi, Shangtao Chen, Zengxiang Wu, Shuangqing Li
Frontiers in Endocrinology.2021;[Epub] CrossRef - Triglyceride Glucose-Waist Circumference Is Superior to the Homeostasis Model Assessment of Insulin Resistance in Identifying Nonalcoholic Fatty Liver Disease in Healthy Subjects
Hwi Seung Kim, Yun Kyung Cho, Eun Hee Kim, Min Jung Lee, Chang Hee Jung, Joong-Yeol Park, Hong-Kyu Kim, Woo Je Lee
Journal of Clinical Medicine.2021; 11(1): 41. CrossRef - The association between nonalcoholic fatty liver disease and esophageal, stomach, or colorectal cancer: National population-based cohort study
Jung-Min Lee, Yong-Moon Park, Jae-Seung Yun, Yu-Bae Ahn, Kang-Moon Lee, Dae Bum Kim, Ji Min Lee, Kyungdo Han, Seung-Hyun Ko, Ming-Lung Yu
PLOS ONE.2020; 15(1): e0226351. CrossRef - Non-alcoholic steatohepatitis and progression of carotid atherosclerosis in patients with type 2 diabetes: a Korean cohort study
Hyeok-Hee Lee, Yongin Cho, Young Ju Choi, Byung Wook Huh, Byung-Wan Lee, Eun Seok Kang, Seok Won Park, Bong-Soo Cha, Eun Jig Lee, Yong-ho Lee, Kap Bum Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Visceral-to-Subcutaneous Abdominal Fat Ratio Is Associated with Nonalcoholic Fatty Liver Disease and Liver Fibrosis
Chan-Hee Jung, Eun-Jung Rhee, Hyemi Kwon, Yoosoo Chang, Seungho Ryu, Won-Young Lee
Endocrinology and Metabolism.2020; 35(1): 165. CrossRef - Fatty liver index and development of cardiovascular disease in Koreans without pre-existing myocardial infarction and ischemic stroke: a large population-based study
Jun Hyung Kim, Jin Sil Moon, Seok Joon Byun, Jun Hyeok Lee, Dae Ryong Kang, Ki Chul Sung, Jang Young Kim, Ji Hye Huh
Cardiovascular Diabetology.2020;[Epub] CrossRef - Non-invasive diagnosis of nonalcoholic fatty liver disease: impact of age and other risk factors
Muharrem Bayrak
The Aging Male.2020; 23(5): 1275. CrossRef - Establishment of a Risk Prediction Model for Non-alcoholic Fatty Liver Disease in Type 2 Diabetes
Yali Zhang, Rong Shi, Liang Yu, Liping Ji, Min Li, Fan Hu
Diabetes Therapy.2020; 11(9): 2057. CrossRef - Noninvasive Evaluation of Nonalcoholic Fatty Liver Disease
Dae Ho Lee
Endocrinology and Metabolism.2020; 35(2): 243. CrossRef - Non-Alcoholic Fatty Liver Disease in Patients with Type 2 Diabetes Mellitus: A Position Statement of the Fatty Liver Research Group of the Korean Diabetes Association
Byung-Wan Lee, Yong-ho Lee, Cheol-Young Park, Eun-Jung Rhee, Won-Young Lee, Nan-Hee Kim, Kyung Mook Choi, Keun-Gyu Park, Yeon-Kyung Choi, Bong-Soo Cha, Dae Ho Lee
Diabetes & Metabolism Journal.2020; 44(3): 382. CrossRef - Sarcopenia is associated with non-alcoholic fatty liver disease in men with type 2 diabetes
D.H. Seo, Y.-h. Lee, S.W. Park, Y.J. Choi, B.W. Huh, E. Lee, K.B. Huh, S.H. Kim, B.-S. Cha
Diabetes & Metabolism.2020; 46(5): 362. CrossRef - Pharmacological Strategies for Insulin Sensitivity in Obesity and Cancer: Thiazolidinediones and Metformin
Luana A. Biondo, Alexandre A. S. Teixeira, Karen C. de O. S. Ferreira, Jose C. R. Neto
Current Pharmaceutical Design.2020; 26(9): 932. CrossRef -
Diabetes and Metabolism Journal in 2020: Good to Great
In-Kyung Jeong
Diabetes & Metabolism Journal.2020; 44(1): 1. CrossRef - Toll-like receptor 9, a possible blocker of non-alcoholic steatohepatitis?
Soung Won Jeong
Clinical and Molecular Hepatology.2020; 26(2): 185. CrossRef - The sex-specific effects of blood lead, mercury, and cadmium levels on hepatic steatosis and fibrosis: Korean nationwide cross-sectional study
Seung Min Chung, Jun Sung Moon, Ji Sung Yoon, Kyu Chang Won, Hyoung Woo Lee
Journal of Trace Elements in Medicine and Biology.2020; 62: 126601. CrossRef - Hepatic fibrosis is associated with total proteinuria in Korean patients with type 2 diabetes
Eugene Han, Yongin Cho, Kyung-won Kim, Yong-ho Lee, Eun Seok Kang, Bong-Soo Cha, Byung-wan Lee
Medicine.2020; 99(33): e21038. CrossRef - Causal relationships between NAFLD, T2D and obesity have implications for disease subphenotyping
Zhipeng Liu, Yang Zhang, Sarah Graham, Xiaokun Wang, Defeng Cai, Menghao Huang, Roger Pique-Regi, Xiaocheng Charlie Dong, Y. Eugene Chen, Cristen Willer, Wanqing Liu
Journal of Hepatology.2020; 73(2): 263. CrossRef - Prevalence of Nonalcoholic Fatty Liver Disease (NAFLD) in Patients With Type 1 Diabetes Mellitus: A Systematic Review and Meta-Analysis
Marieke de Vries, Jan Westerink, Karin H A H Kaasjager, Harold W de Valk
The Journal of Clinical Endocrinology & Metabolism.2020; 105(12): 3842. CrossRef - Beneficial effect of anti-diabetic drugs for nonalcoholic fatty liver disease
Kyung-Soo Kim, Byung-Wan Lee
Clinical and Molecular Hepatology.2020; 26(4): 430. CrossRef - Nonalcoholic Fatty Liver Disease and Diabetes: An Epidemiological Perspective
Eun-Jung Rhee
Endocrinology and Metabolism.2019; 34(3): 226. CrossRef - Role of sodium-glucose co-transporter-2 inhibitors in the management of nonalcoholic fatty liver disease
Anastasia Kontana, Konstantinos Tziomalos
World Journal of Gastroenterology.2019; 25(28): 3664. CrossRef
- Mortality in metabolic dysfunction-associated steatotic liver disease: A nationwide population-based cohort study
- Clinical Diabetes & Therapeutics
- Latent Autoimmune Diabetes in Adults: A Review on Clinical Implications and Management
- Silvia Pieralice, Paolo Pozzilli
- Diabetes Metab J. 2018;42(6):451-464. Published online December 17, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0190
- 12,795 View
- 497 Download
- 51 Web of Science
- 60 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Latent autoimmune diabetes in adults (LADA) is a heterogeneous disease characterized by a less intensive autoimmune process and a broad clinical phenotype compared to classical type 1 diabetes mellitus (T1DM), sharing features with both type 2 diabetes mellitus (T2DM) and T1DM. Since patients affected by LADA are initially insulin independent and recognizable only by testing for islet-cell autoantibodies, it could be difficult to identify LADA in clinical setting and a high misdiagnosis rate still remains among patients with T2DM. Ideally, islet-cell autoantibodies screening should be performed in subjects with newly diagnosed T2DM, ensuring a closer monitoring of those resulted positive and avoiding treatment of hyperglycaemia which might increase the rate of β-cells loss. Thus, since the autoimmune process in LADA seems to be slower than in classical T1DM, there is a wider window for new therapeutic interventions that may slow down β-cell failure. This review summarizes the current understanding of LADA, by evaluating data from most recent studies, the actual gaps in diagnosis and management. Finally, we critically highlight and discuss novel findings and future perspectives on the therapeutic approach in LADA.
-
Citations
Citations to this article as recorded by- A Comprehensive Survey on Diabetes Type-2 (T2D) Forecast Using Machine Learning
Satyanarayana Murthy nimmagadda, Gunnam Suryanarayana, Gangu Bharath Kumar, Ganta Anudeep, Gedela Vinay Sai
Archives of Computational Methods in Engineering.2024;[Epub] CrossRef - Ensemble machine learning reveals key features for diabetes duration from electronic health records
Gabriel Cerono, Davide Chicco
PeerJ Computer Science.2024; 10: e1896. CrossRef - LADA 30th anniversary: A growing form of diabetes with persistent unresolved questions
Ivy Lee Jia Jia, Raffaella Buzzetti, Richard David Leslie, Paolo Pozzilli
Diabetes/Metabolism Research and Reviews.2024;[Epub] CrossRef - A Curious Case of New-Onset Diabetes
Kristina Hernandez, Charity L. Tan
The Journal for Nurse Practitioners.2023; 19(3): 104411. CrossRef - Comprehensive review: Frailty in pancreas transplant candidates and recipients
Ronald F. Parsons, Ekamol Tantisattamo, Wisit Cheungpasitporn, Arpita Basu, Yee Lu, Krista L. Lentine, Kenneth J. Woodside, Neeraj Singh, Joseph Scalea, Tarek Alhamad, Ty B. Dunn, Franco H. Cabeza Rivera, Sandesh Parajuli, Martha Pavlakis, Matthew Cooper
Clinical Transplantation.2023;[Epub] CrossRef - Managing latent autoimmune disease in adults
David Morris
Independent Nurse.2023; 2023(1): 18. CrossRef - Development and validation of a clinical score for identifying patients with high risk of latent autoimmune adult diabetes (LADA): The LADA primary care-protocol study
Pilar Vich-Pérez, Juan Carlos Abánades-Herranz, Gustavo Mora-Navarro, Ángela María Carrasco-Sayalero, Miguel Ángel Salinero-Fort, Ignacio Sevilla-Machuca, Mar Sanz-Pascual, Cristina Álvarez Hernández-Cañizares, Carmen de Burgos-Lunar, Vijayaprakash Suppia
PLOS ONE.2023; 18(2): e0281657. CrossRef - Diagnostic Dilemmas and Current Treatment Approaches in Latent Onset
Autoimmune Diabetes in Adults: A Concise Review
Lakshmi Chandran, Ankul Singh S., Chitra Vellapandian
Current Diabetes Reviews.2023;[Epub] CrossRef - Anti-glutamic Acid Decarboxylase Antibody-Positive Gestational Diabetes Mellitus with Autoimmune Type 1 Diabetes Mellitus in the Early Postpartum Period: A Case Report and Literature Review
Akiko Fujishima, Yohei Onodera, Hiroshi Miura, Yukihiro Terada
The Tohoku Journal of Experimental Medicine.2023; 259(4): 327. CrossRef - Een 54-jarige man met onverklaard gewichtsverlies
N. Mutebi, A. Kharagjitsing
Tijdschrift voor Geneeskunde.2023;[Epub] CrossRef - Effects of Bacillus Calmette-Guérin on immunometabolism, microbiome and liver diseases
Muhammad Umair Ijaz, Farzam Vaziri, Yu-Jui Yvonne Wan
Liver Research.2023; 7(2): 116. CrossRef - The Etiological Diagnosis of Diabetes: Still a Challenge for the Clinician
Danièle Dubois-Laforgue, José Timsit
Endocrines.2023; 4(2): 437. CrossRef - Type 1 diabetes mellitus: features of differential diagnosis
EV Gantsgorn, OV Denisenko, YaO Osipenko, DA Kalmykova, AV Ivanov, SS Gerasyuta, GA Bulguryan, MH Ivanova, DA Saakyan
Bulletin of Russian State Medical University.2023;[Epub] CrossRef - A 1‐year pilot study of intralymphatic injections of GAD‐alum in individuals with latent autoimmune diabetes in adults (LADA) with signs of high immunity: No safety concerns and resemblance to juvenile type 1 diabetes
Ingrid K. Hals, Chandima Balasuriya, Rosaura Casas, Johnny Ludvigsson, Anneli Björklund, Valdemar Grill
Diabetes, Obesity and Metabolism.2023; 25(11): 3400. CrossRef - The relationship between red blood cell distribution width and islet β-cell function indexes in patients with latent autoimmune diabetes in adults
Xiuli Fu, Qin Tan, Wei Wei, Sheng Ding, Zhongjing Wang
BMC Endocrine Disorders.2023;[Epub] CrossRef - A Review on Latent Autoimmune Diabetes in Adults
Vijay Ravikumar, Ariba Ahmed, Ashish Anjankar
Cureus.2023;[Epub] CrossRef - Neutrophils and their role in the aetiopathogenesis of type 1 and type 2 diabetes
Anna Giovenzana, Debora Carnovale, Brett Phillips, Alessandra Petrelli, Nick Giannoukakis
Diabetes/Metabolism Research and Reviews.2022;[Epub] CrossRef - Prevalence of Latent Autoimmune Diabetes in Adult Based on the Presence of GAD 65 Antibodies in North-Eastern Uttar Pradesh, India
Himalina Sangma, Anshul Singh, Anubha Srivastava, Vatsala Misra
Annals of the National Academy of Medical Sciences (India).2022; 58(01): 017. CrossRef - Serum Bile Acid Profiles in Latent Autoimmune Diabetes in Adults and Type 2 Diabetes Patients
Yu Zhou, Deli Ye, Xiaofen Yuan, Yonglie Zhou, Jun Xia, Giuseppe Pugliese
Journal of Diabetes Research.2022; 2022: 1. CrossRef - Early life Bacillus Calmette-Guerin vaccination and incidence of type 1, type 2, and latent autoimmune diabetes in adulthood
Philippe Corsenac, Marie-Élise Parent, Hélène Mansaray, Andrea Benedetti, Hugues Richard, Simona Stäger, Marie-Claude Rousseau
Diabetes & Metabolism.2022; 48(3): 101337. CrossRef - Atypical Diabetes and Management Considerations
Shivajirao Prakash Patil
Primary Care: Clinics in Office Practice.2022; 49(2): 225. CrossRef - Efficacy and safety of sitagliptin and insulin for latent autoimmune diabetes in adults: A systematic review and meta‐analysis
Tong Lin, Yinhe Cai, Liting Tang, Youwei Lian, Min Liu, Chaonan Liu
Journal of Diabetes Investigation.2022; 13(9): 1506. CrossRef - Latent autoimmune diabetes in youth shows greater autoimmunity than latent autoimmune diabetes in adults: Evidence from a nationwide, multicenter, cross‐sectional study
Jin Cheng, Xiaohan Tang, Xiang Yan, Gan Huang, Shuoming Luo, Zhiguang Zhou, Xia Li
Pediatric Diabetes.2022; 23(5): 578. CrossRef - Latent Autoimmune Diabetes in Adults and Metabolic Syndrome—A Mini Review
Niansi Pan, Shimei Yang, Xiaohong Niu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Lifestyle or Environmental Influences and Their Interaction With Genetic Susceptibility on the Risk of LADA
Sofia Carlsson
Frontiers in Endocrinology.2022;[Epub] CrossRef - Antigen-specific immunotherapies in type 1 diabetes
Xuejiao Zhang, Ying Dong, Dianyuan Liu, Liu Yang, Jiayi Xu, Qing Wang
Journal of Trace Elements in Medicine and Biology.2022; 73: 127040. CrossRef - Latent autoimmune diabetes in adults: a focus on β-cell protection and therapy
Wenfeng Yin, Shuoming Luo, Zilin Xiao, Ziwei Zhang, Bingwen Liu, Zhiguang Zhou
Frontiers in Endocrinology.2022;[Epub] CrossRef - Diagnostic camouflage: A case report on Latent autoimmune diabetics of adulthood
Sandhya kiran Neupane, Prakash Paudel Jaishi, Divyaa Koirala, Arjun Kandel, Prabhat Kiran Neupane
Annals of Medicine & Surgery.2022;[Epub] CrossRef - Clinical characteristics and cardiovascular risk profile in children and adolescents with latent autoimmune diabetes: Results from the German/Austrian prospective diabetes follow‐up registry
Alena Welters, Sascha R. Tittel, Thomas Reinehr, Daniel Weghuber, Susanna Wiegand, Wolfram Karges, Clemens Freiberg, Thomas Meissner, Nanette C. Schloot, Reinhard W. Holl
Pediatric Diabetes.2022; 23(8): 1602. CrossRef - The utility of assessing C-peptide in patients with insulin-treated type 2 diabetes: a cross-sectional study
Tuccinardi Dario, Giorgino Riccardo, Pieralice Silvia, Watanabe Mikiko, Maggi Daria, Palermo Andrea, Defeudis Giuseppe, Fioriti Elvira, Pozzilli Paolo, Manfrini Silvia
Acta Diabetologica.2021; 58(4): 411. CrossRef - Cross-reactive peptide epitopes of Enterovirus Coxsackie B4 and human glutamic acid decarboxylase detecting antibodies in latent autoimmune diabetes in adults versus type 1 diabetes
Feliciana Real-Fernández, Alessandra Gallo, Francesca Nuti, Lorenzo Altamore, Gloria Giovanna Del Vescovo, Pietro Traldi, Eugenio Ragazzi, Paolo Rovero, Annunziata Lapolla, Anna Maria Papini
Clinica Chimica Acta.2021; 515: 73. CrossRef - Treating latent autoimmune diabetes in adults in the era of cardiovascular outcomes trials: Old dog should learn new tricks
Theocharis Koufakis, Prashanth Vas, Kalliopi Kotsa
Diabetic Medicine.2021;[Epub] CrossRef - Defining and Classifying New Subgroups of Diabetes
Ashok Balasubramanyam
Annual Review of Medicine.2021; 72(1): 63. CrossRef - Slowly evolving, immune-mediated diabetes in 14-year-old patient: a case report
M. R. Ragimov, D. D. Omelchuk, L. I. Ibragimova, O. S. Derevyanko, T. V. Nikonova
Diabetes mellitus.2021; 24(1): 70. CrossRef - The role of autoimmunity in the pathophysiology of type 2 diabetes: Looking at the other side of the moon
Theocharis Koufakis, George Dimitriadis, Symeon Metallidis, Pantelis Zebekakis, Kalliopi Kotsa
Obesity Reviews.2021;[Epub] CrossRef - Dapagliflozin as an Adjunct Therapy to Insulin in Patients with Type 1 Diabetes Mellitus: Efficacy and Safety of this Combination
Johan H Jendle, Francisco J Ampudia-Blasco, Martin Füchtenbusch, Paolo Pozzilli
European Endocrinology.2021; 1(1): 12. CrossRef - Dapagliflozin as an Adjunct Therapy to Insulin in Patients with Type 1 Diabetes Mellitus: Efficacy and Safety of this Combination
Johan H Jendle, Francisco J Ampudia-Blasco, Martin Füchtenbusch, Paolo Pozzilli
touchREVIEWS in Endocrinology.2021; 17(1): 12. CrossRef - Toward an Improved Classification of Type 2 Diabetes: Lessons From Research into the Heterogeneity of a Complex Disease
Maria J Redondo, Ashok Balasubramanyam
The Journal of Clinical Endocrinology & Metabolism.2021; 106(12): e4822. CrossRef - Bacillus Calmette-Guerin 's beneficial impact on glucose metabolism: Evidence for broad based applications
Gabriella F. Shpilsky, Hiroyuki Takahashi, Anna Aristarkhova, Michele Weil, Nathan Ng, Kacie J. Nelson, Amanda Lee, Hui Zheng, Willem M. Kühtreiber, Denise L. Faustman
iScience.2021; 24(10): 103150. CrossRef - Masqueraders: how to identify atypical diabetes in primary care
Sumera Ahmed, Sana Saeed, Jay H. Shubrook
Journal of Osteopathic Medicine.2021; 121(12): 899. CrossRef - Lada or Type 2 Diabetes Mellitus - A Challenging Diagnosis in Clinical Approach
Lucia Mihaela Custură, Oana Deteşan, Raluca Maria Tilinca, Reka Annamaria Schmiedt, Brigitta Irén Bacso, Mariana Cornelia Tilinca
Acta Medica Transilvanica.2021; 26(3): 55. CrossRef - Antioxidant, Anti-Inflammatory, and Immunomodulatory Properties of Tea—The Positive Impact of Tea Consumption on Patients with Autoimmune Diabetes
Anna Winiarska-Mieczan, Ewa Tomaszewska, Karolina Jachimowicz
Nutrients.2021; 13(11): 3972. CrossRef - A Review of Statistical and Machine Learning Techniques for Microvascular Complications in Type 2 Diabetes
Nitigya Sambyal, Poonam Saini, Rupali Syal
Current Diabetes Reviews.2021; 17(2): 143. CrossRef - Bariatric Surgery Outcomes in Patients with Latent Autoimmune Diabetes of the Adult
Marta Guimarães, Sofia S. Pereira, Mário Nora, Mariana P. Monteiro
Obesity Facts.2021; 14(4): 425. CrossRef - Особливості перебігу діабетичної хвороби нирок у хворих на латентний автоімунний діабет дорослих
I.O. Tsaryk, N.V. Pashkovska
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2021; 17(2): 116. CrossRef - Latenter Autoimmundiabetes im Erwachsenen- und Kindesalter
Alena Welters, Nanette C. Schloot
Der Diabetologe.2020; 16(1): 27. CrossRef - A treatment-based algorithm for identification of diabetes type in the National Health and Nutrition Examination Survey
Mitra Mosslemi, Hannah L. Park, Christine E. McLaren, Nathan D. Wong
Cardiovascular Endocrinology & Metabolism.2020; 9(1): 9. CrossRef - Case 6-2020: A 34-Year-Old Woman with Hyperglycemia
Richard C. Cabot, Eric S. Rosenberg, Virginia M. Pierce, David M. Dudzinski, Meridale V. Baggett, Dennis C. Sgroi, Jo-Anne O. Shepard, Kathy M. Tran, Emily K. McDonald, Tara Corpuz, Miriam S. Udler, Camille E. Powe, Christina A. Austin-Tse
New England Journal of Medicine.2020; 382(8): 745. CrossRef - Therapeutic approaches for latent autoimmune diabetes in adults: One size does not fit all
Theocharis Koufakis, Niki Katsiki, Pantelis Zebekakis, George Dimitriadis, Kalliopi Kotsa
Journal of Diabetes.2020; 12(2): 110. CrossRef - Grenzformen zwischen Typ-1- und Typ-2-Diabetes
Michael Hummel
MMW - Fortschritte der Medizin.2020; 162(11): 60. CrossRef - The Differential Expression of Long Noncoding RNAs in Type 2 Diabetes Mellitus and Latent Autoimmune Diabetes in Adults
Zhang Pengyu, Yan Yan, Fu Xiying, Yang Maoguang, Li Mo, Cheng Yan, Shen Hong, Wang Lijuan, Zhang Xiujuan, Cai Hanqing
International Journal of Endocrinology.2020; 2020: 1. CrossRef - A convenient diagnostic tool for discriminating adult-onset glutamic acid decarboxylase antibody-positive autoimmune diabetes from type 2 diabetes: a retrospective study
Hon-Ke Sia, Shih-Te Tu, Pei-Yung Liao, Kuan-Han Lin, Chew-Teng Kor, Ling-Ling Yeh
PeerJ.2020; 8: e8610. CrossRef - Correct Diabetes Diagnosis and Treatment Allows Sailor to Remain on Active Duty
Andrea R Frazier
Military Medicine.2020; 185(9-10): e1843. CrossRef - Hombre de 28 años con presentación de diabetes
M. Ricci, J. Sanz Cánovas, V. Buonaluto, R. Gómez Huelgas
Medicine - Programa de Formación Médica Continuada Acreditado.2020; 13(16): 942.e1. CrossRef - Uncommon Presentations of Diabetes: Zebras in the Herd
Karen L. Shidler, Lisa R. Letourneau, Lucia M. Novak
Clinical Diabetes.2020; 38(1): 78. CrossRef - Ketogenic Diet as a Trigger for Diabetic Ketoacidosis in a Misdiagnosis of Diabetes: A Case Report
Alexander J. White-Cotsmire, Amber M. Healy
Clinical Diabetes.2020; 38(3): 318. CrossRef - Subphänotypen des Diabetes
Oana Patricia Zaharia, Julia Szendrödi
Der Diabetologe.2019; 15(4): 288. CrossRef - Autoimmunity in latent autoimmune diabetes in adults
Alessandro P. Delitala
AIMS Medical Science.2019; 6(2): 132. CrossRef - Risk of diabetes-associated diseases in subgroups of patients with recent-onset diabetes: a 5-year follow-up study
Oana P Zaharia, Klaus Strassburger, Alexander Strom, Gidon J Bönhof, Yanislava Karusheva, Sofia Antoniou, Kálmán Bódis, Daniel F Markgraf, Volker Burkart, Karsten Müssig, Jong-Hee Hwang, Olof Asplund, Leif Groop, Emma Ahlqvist, Jochen Seissler, Peter Nawr
The Lancet Diabetes & Endocrinology.2019; 7(9): 684. CrossRef - The Influence of Type 2 Diabetes–Associated Factors on Type 1 Diabetes
Maria J. Redondo, Carmella Evans-Molina, Andrea K. Steck, Mark A. Atkinson, Jay Sosenko
Diabetes Care.2019; 42(8): 1357. CrossRef
- A Comprehensive Survey on Diabetes Type-2 (T2D) Forecast Using Machine Learning
- Complications
- Update on the Impact, Diagnosis and Management of Cardiovascular Autonomic Neuropathy in Diabetes: What Is Defined, What Is New, and What Is Unmet
- Vincenza Spallone
- Diabetes Metab J. 2019;43(1):3-30. Published online November 2, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0259
- 15,906 View
- 398 Download
- 151 Web of Science
- 156 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader The burden of diabetic cardiovascular autonomic neuropathy (CAN) is expected to increase due to the diabetes epidemic and its early and widespread appearance. CAN has a definite prognostic role for mortality and cardiovascular morbidity. Putative mechanisms for this are tachycardia, QT interval prolongation, orthostatic hypotension, reverse dipping, and impaired heart rate variability, while emerging mechanisms like inflammation support the pervasiveness of autonomic dysfunction. Efforts to overcome CAN under-diagnosis are on the table: by promoting screening for symptoms and signs; by simplifying cardiovascular reflex tests; and by selecting the candidates for screening. CAN assessment allows for treatment of its manifestations, cardiovascular risk stratification, and tailoring therapeutic targets. Risk factors for CAN are mainly glycaemic control in type 1 diabetes mellitus (T1DM) and, in addition, hypertension, dyslipidaemia, and obesity in type 2 diabetes mellitus (T2DM), while preliminary data regard glycaemic variability, vitamin B12 and D changes, oxidative stress, inflammation, and genetic biomarkers. Glycaemic control prevents CAN in T1DM, whereas multifactorial intervention might be effective in T2DM. Lifestyle intervention improves autonomic function mostly in pre-diabetes. While there is no conclusive evidence for a disease-modifying therapy, treatment of CAN manifestations is available. The modulation of autonomic function by SGLT2i represents a promising research field with possible clinical relevance.
-
Citations
Citations to this article as recorded by- Rectal sensitivity correlated with gastrointestinal‐mediated glucose disposal, but not the incretin effect
Sondre Meling, Erling Tjora, Heike Eichele, Rasmus B. Nedergaard, Filip K. Knop, Niels Ejskjaer, Siri Carlsen, Pål R. Njølstad, Christina Brock, Eirik Søfteland
Endocrinology, Diabetes & Metabolism.2024;[Epub] CrossRef - Glucose metabolism and autonomic function in healthy individuals and patients with type 2 diabetes mellitus at rest and during exercise
Takuto Hamaoka, Urs A. Leuenberger, Rachel C. Drew, Matthew Murray, Cheryl Blaha, Jonathan Carter Luck, Lawrence I. Sinoway, Jian Cui
Experimental Physiology.2024; 109(2): 214. CrossRef - Quantification of lipoproteins by proton nuclear magnetic resonance spectroscopy (1H-NMRS) improves the prediction of cardiac autonomic dysfunction in patients with type 1 diabetes
L. Nattero-Chávez, M. Insenser, N. Amigó, S. Samino, N. Martínez-Micaelo, B. Dorado Avendaño, A. Quintero Tobar, H. F. Escobar-Morreale, M. Luque-Ramírez
Journal of Endocrinological Investigation.2024;[Epub] CrossRef - Predictors of pacemaker requirement in patients with implantable loop recorder and unexplained syncope: A systematic review and meta‐analysis
Moein Zangiabadian, Kiarash Soltani, Yasaman Gholinejad, Reyhane Yahya, Shayan Bastami, Mohammad Ali Akbarzadeh, Mohammad Sharifian Ardestani, Azadeh Aletaha
Clinical Cardiology.2024;[Epub] CrossRef - No clear evidence of neuropathy among patients with high risk for the development of prediabetes/diabetes—a pilot study
Anna E. Körei, Magdolna Békeffy, Adrienn Menyhárt, Karola Osgyán, Ildikó Istenes, Viktor J. Horváth, Péter Kempler
Frontiers in Endocrinology.2024;[Epub] CrossRef - Effects of Physical Cues on Stem Cell-Derived Extracellular Vesicles toward Neuropathy Applications
Danyale Berry, Justice Ene, Aakash Nathani, Mandip Singh, Yan Li, Changchun Zeng
Biomedicines.2024; 12(3): 489. CrossRef - Oxidative stress, endothelial dysfunction, and N-acetylcysteine in type-2 diabetes mellitus
Xin Li, Junyong Zou, Aiping Lin, Jingshu Chi, Hong Hao, Hong Chen, Zhenguo Liu
Antioxidants & Redox Signaling.2024;[Epub] CrossRef - High dose cholecalciferol supplementation causing morning blood pressure reduction in patients with type 1 diabetes mellitus and cardiovascular autonomic neuropathy
João Felício, Lorena Moraes, Gabriela Lemos, Ícaro Souza, Giovana Vieira, Lilian Silva, Natércia Queiroz, Ana Carolina Souza, Franciane Melo, João Felício Abrahão Neto, Hana Britto, Manuela Lemos, Márcia Santos, Priscila Figueiredo, Ana Regina Motta, Meli
Scientific Reports.2024;[Epub] CrossRef - Transcutaneous vagal nerve stimulation for treating gastrointestinal symptoms in individuals with diabetes: a randomised, double-blind, sham-controlled, multicentre trial
Ditte S. Kornum, Davide Bertoli, Huda Kufaishi, Anne-Marie Wegeberg, Tina Okdahl, Esben B. Mark, Katrine L. Høyer, Jens B. Frøkjær, Birgitte Brock, Klaus Krogh, Christian S. Hansen, Filip K. Knop, Christina Brock, Asbjørn M. Drewes
Diabetologia.2024;[Epub] CrossRef - Independent and interactive associations of heart rate and obesity with type 2 diabetes mellites: A population‐based study
Tianxin Zhu, Qingyu Chen, Hongxing Chen, Lili You, Dan Liu, Xiaoyun Zhang, Feng Li, Hongshi Wu, Juying Tang, Diaozhu Lin, Kan Sun, Li Yan, Meng Ren
Journal of Diabetes.2024;[Epub] CrossRef - Mortality risk factors in newly diagnosed diabetic cardiac autonomic neuropathy
Bruce A. Chase, Sylwia Pocica, Roberta Frigerio, Katerina Markopoulou, Demetrius M. Maraganore, Navamon Aunaetitrakul, Alexander Epshteyn, Alexandru C. Barboi
Clinical Autonomic Research.2023; 33(6): 903. CrossRef - Autonomic symptoms and associated factors in patients with chronic heart failure
Hellen Da Silva, Sofie Pardaens, Marc Vanderheyden, Johan De Sutter, Heleen Demeyer, Michel De Pauw, Laurent Demulier, Jan Stautemas, Patrick Calders
Acta Cardiologica.2023; 78(2): 203. CrossRef - Incretins and microvascular complications of diabetes: neuropathy, nephropathy, retinopathy and microangiopathy
Jonathan Goldney, Jack A. Sargeant, Melanie J. Davies
Diabetologia.2023; 66(10): 1832. CrossRef - Functional and morphometric assessment of small-fibre damage in late-onset hereditary transthyretin amyloidosis with polyneuropathy: the controversial relation between small-fibre-related symptoms and diagnostic test findings
Eleonora Galosi, Luca Leonardi, Pietro Falco, Giuseppe Di Pietro, Alessandra Fasolino, Nicoletta Esposito, Caterina Leone, Giulia Di Stefano, Maurizio Inghilleri, Marco Luigetti, Antonini Giovanni, Andrea Truini
Amyloid.2023; 30(1): 59. CrossRef - In vivo molecular imaging of cardiac angiogenesis in persons with and without type 2 diabetes: A cross‐sectional 68 Ga‐RGD‐PET study
Jens Christian Laursen, Ida Kirstine Bull Rasmussen, Emilie Hein Zobel, Philip Hasbak, Lene Holmvang, Christian Stevns Hansen, Bernt Johan von Scholten, Marie Frimodt‐Møller, Peter Rossing, Tine Willum Hansen, Andreas Kjaer, Rasmus Sejersten Ripa
Diabetic Medicine.2023;[Epub] CrossRef - Cardiac innervations in diabetes mellitus—Anatomical evidence of neuropathy
Natalija Filipović, Maja Marinović Guić, Vana Košta, Katarina Vukojević
The Anatomical Record.2023; 306(9): 2345. CrossRef - Clinical Predictors of Pacing Device Implantation in Implantable Cardiac Monitor Recipients for Unexplained Syncope
Reina Tonegawa-Kuji, Yuko Y. Inoue, Michikazu Nakai, Koshiro Kanaoka, Yoko Sumita, Yuichiro Miyazaki, Akinori Wakamiya, Keiko Shimamoto, Nobuhiko Ueda, Kenzaburo Nakajima, Naoya Kataoka, Mitsuru Wada, Kenichiro Yamagata, Kohei Ishibashi, Koji Miyamoto, Sa
CJC Open.2023; 5(4): 259. CrossRef - Cardiovascular autonomic reflex tests using a handheld device in the diagnosis of cardiovascular autonomic neuropathy in patients with schizophrenia
Laura Blok-Husum, Milka Ane Rank Brcelic, Hanin Kawa Farman Kawal Bassi, Svend Eggert Jensen, Rene Ernst Nielsen, Kristian Kragholm, Jesper Fleischer, Esben Laugesen, Christoffer Polcwiartek
American Heart Journal Plus: Cardiology Research and Practice.2023; 26: 100252. CrossRef - Causal association between vitamin D and diabetic neuropathy: a Mendelian randomization analysis
Wei Huang, Lei Gu, Jingwen Wang, Yiqi Wang, Fangzheng Cao, Tianyu Jin, Yifan Cheng
Endocrine.2023; 80(2): 328. CrossRef - Diabetes Mellitus and Heart Failure: Epidemiology, Pathophysiologic Mechanisms, and the Role of SGLT2 Inhibitors
Panagiotis Theofilis, Evangelos Oikonomou, Konstantinos Tsioufis, Dimitris Tousoulis
Life.2023; 13(2): 497. CrossRef - Sex differences and sex steroids influence on the presentation and severity of cardiovascular autonomic neuropathy of patients with type 1 diabetes
Lía Nattero-Chávez, María Insenser, Alejandra Quintero Tobar, Elena Fernández-Durán, Beatriz Dorado Avendaño, Tom Fiers, Jean-Marc Kaufman, Manuel Luque-Ramírez, Héctor F. Escobar-Morreale
Cardiovascular Diabetology.2023;[Epub] CrossRef - Early Gastrointestinal Neuropathy Assessed by Wireless Motility Capsules in Adolescents with Type 1 Diabetes
Vinni Faber Rasmussen, Mathilde Thrysøe, Páll Karlsson, Esben Thyssen Vestergaard, Kurt Kristensen, Ann-Margrethe Rønholt Christensen, Jens Randel Nyengaard, Astrid Juhl Terkelsen, Christina Brock, Klaus Krogh
Journal of Clinical Medicine.2023; 12(5): 1925. CrossRef - Heart rate variability in people with metabolic syndrome
Kostiantyn Apykhtin, Svitlana Drozdovska, Olha Hurenko, Anastasiia Nahorna, Anatoly Pisaruk, Yuliia Panchenko, Olena Andrieieva
Ageing & Longevity.2023; (1 2023): 1. CrossRef - Heart rate variability in people with metabolic syndrome
Kostiantyn Apykhtin, Svitlana Drozdovska, Olha Hurenko, Anastasiia Nahorna, Anatoly Pisaruk, Yuliia Panchenko, Olena Andrieieva
JOURNAL OF THE NATIONAL ACADEMY OF MEDICAL SCIENCES OF UKRAINE.2023; (1 2023): 1. CrossRef - Potential of electronic devices for detection of health problems in older adults at home: A systematic review and meta-analysis
Yu-ting Cao, Xin-xin Zhao, Yi-ting Yang, Shi-jie Zhu, Liang-dong Zheng, Ting Ying, Zhou Sha, Rui Zhu, Tao Wu
Geriatric Nursing.2023; 51: 54. CrossRef - Diabetes mellitus in der Akut- und Notfallmedizin
Leo Benning, Julian Krehl, Felix Patricius Hans
Notfallmedizin up2date.2023; 18(01): 45. CrossRef - Correlation between Heart rate recovery and Left Atrial phasic functions evaluated by 2D speckle-tracking Echocardiography after Acute Myocardial infarction
Behruz Mashayekhi, Reza Mohseni-Badalabadi, Ali Hosseinsabet, Tahereh Ahmadian
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Pancreatic sympathetic innervation disturbance in type 1 diabetes
Senlin Li, Huimin Yuan, Keshan Yang, Qing Li, Ming Xiang
Clinical Immunology.2023; 250: 109319. CrossRef - A Nonrandomized Trial of the Effects of Passive Simulated Jogging on Short-Term Heart Rate Variability in Type 2 Diabetic Subjects
Jose A. Adams, Jose R. Lopez, Veronica Banderas, Marvin A. Sackner, Mark Yorek
Journal of Diabetes Research.2023; 2023: 1. CrossRef - Evaluating treatment options for cardiovascular autonomic neuropathy in patients with diabetes mellitus: a systematic review
Jasmine KaiLi Goh, Leroy Koh
Diabetology International.2023; 14(3): 224. CrossRef - Autonomic neuropathic symptoms in patients with diabetes: practical tools for screening in daily routine
Ana Raquel Souza de Azevedo Vieira, Lara Benigno Porto-Dantas, Flaviene Alves do Prado Romani, Patrícia Souza Carvalho, Rodica Pop-Busui, Hermelinda Cordeiro Pedrosa
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - “Arterial stiffness is not associated with changes in the circadian pattern of blood pressure in patients with type 1 diabetes mellitus and cardiovascular autonomic dysfunction”
Lía Nattero-Chávez, Ane Bayona Cebada, Elena Fernández-Durán, Alejandra Quintero Tobar, Beatriz Dorado Avendaño, Héctor Escobar-Morreale, Manuel Luque-Ramírez
Diabetes and Vascular Disease Research.2023; 20(3): 147916412311736. CrossRef - Frontiers in diagnostic and therapeutic approaches in diabetic sensorimotor neuropathy (DSPN)
Sanjeev Sharma, Gerry Rayman
Frontiers in Endocrinology.2023;[Epub] CrossRef - In Type 2 Diabetes Mellitus, normalization of hemoglobin A1c accompanies reduced sensitivity to pressure at the sternum
Jens Faber, Søren Ballegaard, Nanna Ørsted, Ebbe Eldrup, Benny Karpatschof, Finn Gyntelberg, Sofie Korsgaard Hecquet, Albert Gjedde
Frontiers in Neuroscience.2023;[Epub] CrossRef - Functional status associated with postural dizziness, but not postural hypotension, in older adults: a community-based study
Hsiang-Ju Cheng, Zih-Jie Sun, Feng-Hwa Lu, Yi-Ching Yang, Chih-Jen Chang, Jin-Shang Wu
BMC Geriatrics.2023;[Epub] CrossRef - Effects of baricitinib, empagliflozin, linagliptin and telmisartan on cardiovascular autonomic neuropathy in type 1 diabetes: An exploratory, randomized, open‐label, crossover trial
Jens Christian Laursen, Viktor Rotbain Curovic, Marjolein Y. A. M. Kroonen, Niels Jongs, Emilie H. Zobel, Tine W. Hansen, Marie Frimodt‐Møller, Gozewijn D. Laverman, Adriaan Kooy, Frederik Persson, Hiddo J. L. Heerspink, Christian Stevns Hansen, Peter Ros
Diabetes, Obesity and Metabolism.2023; 25(10): 3064. CrossRef - The Retinal Nerve Fiber Layer Thickness Is Associated with Systemic Neurodegeneration in Long-Term Type 1 Diabetes
Christina Brock, Anne-Marie Wegeberg, Thomas Arendt Nielsen, Bassam Karout, Per M. Hellström, Asbjørn Mohr Drewes, Henrik Vorum
Translational Vision Science & Technology.2023; 12(6): 23. CrossRef - The Use of Empirical Mode Decomposition on Heart Rate Variability Signals to Assess Autonomic Neuropathy Progression in Type 2 Diabetes
Sandra Cossul, Felipe Rettore Andreis, Mateus Andre Favretto, Jefferson Luiz Brum Marques
Applied Sciences.2023; 13(13): 7824. CrossRef - Topical capsaicin for the management of painful diabetic neuropathy: a narrative systematic review
Brandon Goodwin, Maanas Chiplunkar, Ryan Salerno, Kylon Coombs, Umar Sannoh, Vrushank Shah, Nicholas Averell, Usmaan Al-Shebab, Deanna Janora
Pain Management.2023; 13(5): 309. CrossRef - Adynamic response to cold pain reflects dysautonomia in type 1 diabetes and polyneuropathy
Thomas Arendt Nielsen, Søren Lundbye-Christensen, Yoanna Krasimirova Dimitrova, Sam Riahi, Birgitte Brock, Asbjørn Mohr Drewes, Christina Brock
Scientific Reports.2023;[Epub] CrossRef - Autonomic Nerve Function Tests in Patients with Diabetes
Heung Yong Jin, Tae Sun Park
The Journal of Korean Diabetes.2023; 24(2): 71. CrossRef - Understanding the role of hyperglycemia and the molecular mechanism associated with diabetic neuropathy and possible therapeutic strategies
Mandeep Kaur, Sakshi Misra, Priyanka Swarnkar, Preeti Patel, Balak Das Kurmi, Ghanshyam Das Gupta, Amrita Singh
Biochemical Pharmacology.2023; 215: 115723. CrossRef - A three-month physical training program improves cardiovascular autonomic function in patients with metabolic syndrome with and without diabetes – a pilot study
Anna Vágvölgyi, Judit Erzsébet Ábrahám, Éva Máthéné Köteles, Andrea Korom, Mária Barnai, Mónika Szűcs, Andrea Orosz, Péter Kempler, Adrienn Menyhárt, Attila Nemes, Tamás Várkonyi, István Baczkó, István Kósa, Csaba Lengyel
Frontiers in Endocrinology.2023;[Epub] CrossRef - Cardiovascular autonomic neuropathy in patients with type 2 diabetes with and without sensorimotor polyneuropathy
Emil Peters, Mustapha Itani, Alexander G. Kristensen, Astrid Juhl Terkelsen, Thomas Krøigård, Hatice Tankisi, Troels S. Jensen, Nanna B. Finnerup, Sandra Sif Gylfadottir
Journal of the Peripheral Nervous System.2023; 28(3): 450. CrossRef - Cardiac Autonomic Neuropathy in Prediabetes: A Case-Control Study
Pavan Gujjar, Y. S. Ravikumar, Lakshmi Nagendra, Hiya Boro, Saptarshi Bhattacharya
Indian Journal of Endocrinology and Metabolism.2023; 27(4): 325. CrossRef - Diabetic Neuropathies
Melissa A. Elafros, Brian C. Callaghan
CONTINUUM: Lifelong Learning in Neurology.2023; 29(5): 1401. CrossRef - Determinants of the heart rate variability in type 1 diabetes mellitus
Máté Hajdu, Konstandia Garmpis, Vivien Vértes, Noémi Vorobcsuk-Varga, Gergő Attila Molnár, László Hejjel, István Wittmann, Réka Faludi
Frontiers in Endocrinology.2023;[Epub] CrossRef - The Effect of Exercise on Cardiovascular Autonomic Nervous Function in Patients with Diabetes: A Systematic Review
Hidetaka Hamasaki
Healthcare.2023; 11(19): 2668. CrossRef - Influence of Fibrinogen/Albumin Ratio and Fibrinogen/Pre-Albumin Ratio on Cardiac Autonomic Neuropathy in Type 2 Diabetes
Subei Zhao, Zheng Yang, Meng Yu, Linyu Xiang, Yuhuan Lv, Chunyan Tian, Rong Li
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3249. CrossRef - In Ischemic Heart Disease, Reduced Sensitivity to Pressure at the Sternum Accompanies Lower Mortality after Five Years: Evidence from a Randomized Controlled Trial
Søren Ballegaard, Jens Faber, Christian Selmer, Finn Gyntelberg, Svend Kreiner, Benny Karpatschof, Tobias Wirenfeldt Klausen, Åke Hjalmarson, Albert Gjedde
Journal of Clinical Medicine.2023; 12(24): 7585. CrossRef - Assessment of the relationship of systemic vascular dysfunction and cardiac autonomic neuropathy (CAN) with diabetic retinopathy
KJ Hari Prakash, Sucheta Parija, Manisha Kar
Journal of Family Medicine and Primary Care.2023; 12(12): 3236. CrossRef - Autonomic Neuropathy in Ambulatory Type 2 Diabetes Mellitus Patients: A Single-arm Prospective, Observational Study
Kaustav Saha, Shatavisa Mukherjee, Animesh Maiti, Santanu Kumar Tripathi
Journal of the Practice of Cardiovascular Sciences.2023; 9(3): 178. CrossRef - Insomnia and type 2 diabetes: how to help the patient. Modern view of a neurologist
E. S. Akarachkova, O. V. Kotova, V. L. Klimov, D. I. Lebedeva
FOCUS. Endocrinology.2023; 4(4): 12. CrossRef - Impaired Cardiovagal Activity as a Link Between Hyperglycemia and Arterial Stiffness in Adults With Type 2 Diabetes Mellitus Patients Among an Eastern Indian Population: A Cross-sectional Study
Nibedita Priyadarsini, Devineni Likhitha, Madumathy Ramachandran, Kishore Kumar Behera
Canadian Journal of Diabetes.2023;[Epub] CrossRef - Carvedilol improves heart rate variability indices, biomarkers but not cardiac nerve density in streptozotocin-induced T2DM model of diabetic cardiac autonomic neuropathy
Olawale Mathias Akinlade, Bamidele Owoyele, Olufemi Ayodele Soladoye
Journal of Basic and Clinical Physiology and Pharmacology.2022; 33(2): 213. CrossRef - Cardiovascular autonomic responses during head-up tilt test in newly diagnosed type 2 diabetes
Esteban Jorge-Galarza, Margarita Torres-Tamayo, María del Rocío Martínez-Alvarado, Berenice Peña-Aparicio, Carmen González-Salazar, Juan Reyes-Barrera, Manuel Sierra-Beltrán, Erika Fajardo-Flores, Andrey Kostin, J. Antonio González-Hermosillo
Irish Journal of Medical Science (1971 -).2022; 191(5): 2077. CrossRef - Cardiovascular autonomic neuropathy and incident diabetic kidney disease in patients with type 2 diabetes
Ji Eun Jun, Min Sun Choi, Jae Hyeon Kim
Diabetes Research and Clinical Practice.2022; 184: 109181. CrossRef - Kardiovaskuläre Risiken in der 4.–6. Lebensdekade mit Diabetes mellitus Typ 1
Young Hee Lee-Barkey, Bernd Stratmann, Diethelm Tschöpe
Der Diabetologe.2022; 18(2): 131. CrossRef - Mechanisms of cardiac dysfunction in diabetic cardiomyopathy: molecular abnormalities and phenotypical variants
Francesca Romana Prandi, Isabella Evangelista, Domenico Sergi, Alberto Palazzuoli, Francesco Romeo
Heart Failure Reviews.2022; 28(3): 597. CrossRef - Comparison of Risk Assessment Strategies for Patients with Diabetes Mellitus and Stable Chest Pain: A Coronary Computed Tomography Angiography Study
Jia Zhao, Shuo Wang, Pengyu Zhao, Yong Huo, Chunjie Li, Jia Zhou, Pawel Kleczynski
Journal of Diabetes Research.2022; 2022: 1. CrossRef - BOND study: a randomised double-blind, placebo-controlled trial over 12 months to assess the effects of benfotiamine on morphometric, neurophysiological and clinical measures in patients with type 2 diabetes with symptomatic polyneuropathy
Gidon J Bönhof, Gundega Sipola, Alexander Strom, Christian Herder, Klaus Strassburger, Birgit Knebel, Claudia Reule, Jan-Christoph Wollmann, Andrea Icks, Hadi Al-Hasani, Michael Roden, Oliver Kuss, Dan Ziegler
BMJ Open.2022; 12(2): e057142. CrossRef - Pragmatic Clinic-Based Investigation of Glycemic Variability in Patients With Type 1 Diabetes in Routine Clinical Practice and Its Association With Cardiovascular Autonomic Neuropathy: A Pilot Study
Lucianne R.M. Tannus, Marilia B. Gomes
Endocrine Practice.2022; 28(5): 465. CrossRef - Longitudinal effects of one‐leg standing time on neuropathy outcomes in association with glycemic control in non‐elderly patients with type 2 diabetes
Kazuhiro Sugimoto, Takashi Sozu, Takehiko Hoshino, Yuko Watanabe, Akira Tamura, Toshiro Yamazaki, Setsu Ohta, Susumu Suzuki, Takuro Shimbo
Journal of Diabetes Investigation.2022; 13(6): 1039. CrossRef - Thermal quantitative sensory testing as a screening tool for cardiac autonomic neuropathy in patients with diabetes mellitus
Veronika Potockova, Sarka Mala, Lucie Hoskovcova, Vaclav Capek, Tomas Nedelka, Lucie Riedlbauchova, Daniel Baumgartner, Livie Mensova, Radim Mazanec
Brain and Behavior.2022;[Epub] CrossRef - Cardiovascular Autonomic Reflex Tests and 7 Heart Rate Variability Indices for Early Diagnosis of Cardiovascular Autonomic Neuropathy in Type 2 Diabetes Individuals
Yeelen Ballesteros Atala, Mozânia Reis De Matos, Denise Engelbrecht Zantut-Wittmann, Alejandro Rosell Castillo, Daniele P Santos-Bezerra, Maria Lucia Correa-Giannella, Maria Cândida Ribeiro Parisi
Current Diabetes Reviews.2022;[Epub] CrossRef - Design, synthesis, in vitro and in silico studies of naproxen derivatives as dual lipoxygenase and α-glucosidase inhibitors
Asma Sardar, Obaid-ur-Rahman Abid, Saima Daud, M. Fakhar-e-Alam, Muhammad Hussnain Siddique, Muhammad Ashraf, Wardah Shahid, Syeda Abida Ejaz, M. Atif, Shafiq Ahmad, Sulman Shafeeq, Muhammad Afzal
Journal of Saudi Chemical Society.2022; 26(3): 101468. CrossRef - Clinical manifestations and evaluation of cardiac autonomic neuropathy in diabetes mellitus and metabolic syndrome
L. S. Moshkhoeva, A. N. Barinov
Neurology, Neuropsychiatry, Psychosomatics.2022; 14(2): 71. CrossRef - The relationship between vitamin B12 levels and electrocardiographic ventricular repolarization markers
Emre Yılmaz, Devrim Kurt, Aslı Vural, Ertan Aydın, Sencer Çamcı, Ercan Aydın
Nutrición Hospitalaria.2022;[Epub] CrossRef - The effect of liraglutide on cardiac autonomic function in type 2 diabetes: A prespecified secondary analysis from the LIRAFLAME randomized, double‐blinded, placebo‐controlled trial
Suvanjaa Sivalingam, Emilie Hein Zobel, Christian S. Hansen, Rasmus S. Ripa, Bernt J. von Scholten, Viktor Rotbain Curovic, Andreas Kjaer, Jacob K. Jensen, Tine W. Hansen, Peter Rossing
Diabetes, Obesity and Metabolism.2022; 24(8): 1638. CrossRef - Heart Rate Variability and Chronic Kidney Disease in Patients with Type 2 Diabetes
Wei Shi, Jing Zhang, Dan Chen, Xiaolei Chen, Wei Duan, Hongmei Zhang, Fahd Abd Algalil
Applied Bionics and Biomechanics.2022; 2022: 1. CrossRef - Spectrum of cardiac autonomic neuropathy in patients with type 2 diabetes mellitus: A North India perspective
PrativaPriyadarshani Sethi, Basavraj Jatteppanavar, Ravi Kant, Monika Pathania, MukeshChand Bairwa
Journal of Cardio-diabetes and metabolic disorders.2022; 2(1): 23. CrossRef - Cardiac Autonomic Dysfunction Is Associated With Risk of Diabetic Kidney Disease Progression in Type 2 Diabetes Mellitus
Haixia Zeng, Jianmo Liu, Zheng Chen, Peng Yu, Jianping Liu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Diagnostic Tools, Biomarkers, and Treatments in Diabetic polyneuropathy
and Cardiovascular Autonomic Neuropathy
Gidon J. Bönhof, Christian Herder, Dan Ziegler
Current Diabetes Reviews.2022;[Epub] CrossRef - Triglyceride glucose index is related with cardiac autonomic dysfunction in patients with metabolic syndrome
Akif Serhat Balcıoğlu, Ekrem Aksu, Ahmet Çağrı Aykan
Kardiologiia.2022; 62(6): 45. CrossRef - Pathogenesis of Distal Symmetrical Polyneuropathy in Diabetes
Sasha Smith, Pasha Normahani, Tristan Lane, David Hohenschurz-Schmidt, Nick Oliver, Alun Huw Davies
Life.2022; 12(7): 1074. CrossRef - Correlation between impaired hemodynamic response and cardiopulmonary fitness in middle-aged type 2 diabetes mellitus patients: a case–control study
Jinjin Xie, Lianhua Yin, Jia Huang, Ying Xu, Yannan Chen, Jiawei Qin, Zhizhen Liu, Jing Tao
European Journal of Applied Physiology.2022; 122(10): 2295. CrossRef - Higher frequency of cardiovascular autonomic neuropathy in youth with type 2 compared to type 1 diabetes: Role of cardiometabolic risk factors
Benjamin J. Varley, Megan L. Gow, Yoon Hi Cho, Paul Benitez‐Aguirre, Janine Cusumano, Alison Pryke, Albert Chan, Vallimayil Velayutham, Kim C. Donaghue, Maria E. Craig
Pediatric Diabetes.2022; 23(7): 1073. CrossRef - The role of protein kinase C in diabetic microvascular complications
Deng Pan, Lin Xu, Ming Guo
Frontiers in Endocrinology.2022;[Epub] CrossRef - Effect of SGLT-2 inhibitors on cardiac autonomic function in type 2 diabetes mellitus: a meta-analysis of randomized controlled trials
Dimitrios Patoulias, Alexandra Katsimardou, Nikolaos Fragakis, Christodoulos Papadopoulos, Michael Doumas
Acta Diabetologica.2022; 60(1): 1. CrossRef - Association between blood glucose levels and autonomic symptoms in Peru
Gabriel Angeles-Zurita, Margorie Narro-Fuentes, Antonio Bernabe-Ortiz
Primary Care Diabetes.2022; 16(5): 709. CrossRef - Clinical scoring systems for the risk of cardiovascular autonomic neuropathy in type 1 and type 2 diabetes: A simple tool
Marika Menduni, Cinzia D'Amato, Martina Leoni, Valentina Izzo, Mariateresa Staltari, Carla Greco, Andrea Abbatepassero, Giuseppe Seminara, Ilenia D'Ippolito, Davide Lauro, Vincenza Spallone
Journal of the Peripheral Nervous System.2022; 27(4): 259. CrossRef - Vagus nerve stimulation as a novel treatment for systemic lupus erythematous: study protocol for a randomised, parallel-group, sham-controlled investigator-initiated clinical trial, the SLE-VNS study
Amanda Hempel Zinglersen, Ida Lynghøj Drange, Katrine Aagaard Myhr, Andreas Fuchs, Mogens Pfeiffer-Jensen, Christina Brock, Søren Jacobsen
BMJ Open.2022; 12(9): e064552. CrossRef - To the interpretation of frequency components of the heart rate variability
N. V. Kuzmenko, V. A. Tsyrlin, M. G. Pliss
Translational Medicine.2022; 9(3): 35. CrossRef - Protein pyrrole adducts are associated with elevated glucose indices and clinical features of diabetic diffuse neuropathies
Xiao Chen, Zhuyi Jiang, Lianjing Zhang, Wei Liu, Xiaohu Ren, Luling Nie, Desheng Wu, Zhiwei Guo, Weimin Liu, Xifei Yang, Yan Wu, Zhen Liang, Peter Spencer, Jianjun Liu
Journal of Diabetes.2022; 14(10): 646. CrossRef - Cardiac Autonomic Neuropathy in Type 1 and 2 Diabetes: Epidemiology, Pathophysiology, and Management
Scott Williams, Siddig Abdel Raheim, Muhammad Ilyas Khan, Umme Rubab, Prathap Kanagala, Sizheng Steven Zhao, Anne Marshall, Emily Brown, Uazman Alam
Clinical Therapeutics.2022; 44(10): 1394. CrossRef - Pathophysiological and clinical aspects of the circadian rhythm of arterial stiffness in diabetes mellitus: A minireview
Victoria A. Serhiyenko, Ludmila M. Serhiyenko, Volodymyr B. Sehin, Alexandr A. Serhiyenko
Endocrine Regulations.2022; 56(4): 284. CrossRef - Heart rate-corrected QT interval prolongation is associated with decreased heart rate variability in patients with type 2 diabetes
Seon-Ah Cha
Medicine.2022; 101(45): e31511. CrossRef - Effect of the Glucagon-Like Peptide-1 Receptor Agonists on Autonomic Function in Subjects with Diabetes: A Systematic Review and Meta-Analysis
Carla Greco, Daniele Santi, Giulia Brigante, Chiara Pacchioni, Manuela Simoni
Diabetes & Metabolism Journal.2022; 46(6): 901. CrossRef - Diabetes-Induced Cardiac Autonomic Neuropathy: Impact on Heart Function and Prognosis
Susumu Z. Sudo, Tadeu L. Montagnoli, Bruna de S. Rocha, Aimeé D. Santos, Mauro P. L. de Sá, Gisele Zapata-Sudo
Biomedicines.2022; 10(12): 3258. CrossRef - The Relationship Between Orthostatic Hypotension and Vitamin D Deficiency in Patients with Uncontrolled Type 2 Diabetes Mellitus
Ece YİĞİT, Ridvan SİVRİTEPE, Dilay KARABULUT, Umut KARABULUT
Online Türk Sağlık Bilimleri Dergisi.2022; 7(2): 313. CrossRef - A study of heart rate variability in diabetic mellitus patients
Srinivasa Jayachandra, Satyanath Reddy Kodidala
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 153. CrossRef - The prevalence of cardiac autonomic neuropathy in prediabetes: a systematic review
Aikaterini Eleftheriadou, Scott Williams, Sarah Nevitt, Emily Brown, Rebecca Roylance, John P. H. Wilding, Daniel J. Cuthbertson, Uazman Alam
Diabetologia.2021; 64(2): 288. CrossRef - Risk of cardiac autonomic neuropathy in latent autoimmune diabetes in adults is similar to type 1 diabetes and lower compared to type 2 diabetes: A cross‐sectional study
Ernesto Maddaloni, Chiara Moretti, Rossella Del Toro, Sara Sterpetti, Maria Vittoria Ievolella, Gabriele Arnesano, Rocky Strollo, Silvia Irina Briganti, Luca D'Onofrio, Paolo Pozzilli, Raffaella Buzzetti
Diabetic Medicine.2021;[Epub] CrossRef - Effects of lunar cycle on fasting plasma glucose, heart rate and blood pressure in type 2 diabetic patients
Sutanu Dutta Chowdhury, Subhasish Pramanik, Koena Bhattacharjee, Lakshmi Kanta Mondal
Chronobiology International.2021; 38(2): 270. CrossRef - Intensive Risk Factor Management and Cardiovascular Autonomic Neuropathy in Type 2 Diabetes: The ACCORD Trial
Yaling Tang, Hetal Shah, Carlos Roberto Bueno Junior, Xiuqin Sun, Joanna Mitri, Maria Sambataro, Luisa Sambado, Hertzel C. Gerstein, Vivian Fonseca, Alessandro Doria, Rodica Pop-Busui
Diabetes Care.2021; 44(1): 164. CrossRef - Decreased glomerular filtration rate and increased albuminuria for identification of cardiovascular autonomic neuropathy in subjects with and without diabetes
Ying-Chuen Lai, Hung-Yuan Li, Yi-Dier Jiang, Tien-Jyun Chang, Lee-Ming Chuang
Autonomic Neuroscience.2021; 230: 102757. CrossRef - Exposures influencing the developing central autonomic nervous system
Sarah D. Schlatterer, Adre J. du Plessis
Birth Defects Research.2021; 113(11): 845. CrossRef - Vitamin B12 Supplementation in Diabetic Neuropathy: A 1-Year, Randomized, Double-Blind, Placebo-Controlled Trial
Triantafyllos Didangelos, Eleni Karlafti, Evangelia Kotzakioulafi, Eleni Margariti, Parthena Giannoulaki, Georgios Batanis, Solomon Tesfaye, Kοnstantinos Kantartzis
Nutrients.2021; 13(2): 395. CrossRef - The Association Between Continuous Glucose Monitoring-Derived Metrics and Cardiovascular Autonomic Neuropathy in Outpatients with Type 2 Diabetes
Min Young Kim, Gyuri Kim, Ji Yun Park, Min Sun Choi, Ji Eun Jun, You-Bin Lee, Sang-Man Jin, Kyu Yeon Hur, Jae Hyeon Kim
Diabetes Technology & Therapeutics.2021; 23(6): 434. CrossRef - Insulin resistance is independently associated with cardiovascular autonomic neuropathy in type 2 diabetes
Yingshan Liu, Yu Peng, Jing Jin, Yanshan Chen, Chuna Chen, Zhenguo Chen, Haishan Huang, Lingling Xu
Journal of Diabetes Investigation.2021; 12(9): 1651. CrossRef - SGLT2 inhibitors and the autonomic nervous system in diabetes: A promising challenge to better understand multiple target improvement
Vincenza Spallone, Paul Valensi
Diabetes & Metabolism.2021; 47(4): 101224. CrossRef - Reduction of Pressure Pain Sensitivity as Novel Non-pharmacological Therapeutic Approach to Type 2 Diabetes: A Randomized Trial
Jens Faber, Ebbe Eldrup, Christian Selmer, Caroline Pichat, Sofie Korsgaard Hecquet, Torquil Watt, Svend Kreiner, Benny Karpatschof, Finn Gyntelberg, Søren Ballegaard, Albert Gjedde
Frontiers in Neuroscience.2021;[Epub] CrossRef - Relationship between cardiac autonomic neuropathy and cardio-metabolic risk profile in adults with type 1 diabetes
M. Serdarova, R. Dimova, N. Chakarova, G. Grozeva, A. Todorova, T. Tankova
Diabetes Research and Clinical Practice.2021; 174: 108721. CrossRef - Differences and Similarities in Neuropathy in Type 1 and 2 Diabetes: A Systematic Review
Mar Sempere-Bigorra, Iván Julián-Rochina, Omar Cauli
Journal of Personalized Medicine.2021; 11(3): 230. CrossRef - Assessment of Gastrointestinal Autonomic Dysfunction: Present and Future Perspectives
Ditte S. Kornum, Astrid J. Terkelsen, Davide Bertoli, Mette W. Klinge, Katrine L. Høyer, Huda H. A. Kufaishi, Per Borghammer, Asbjørn M. Drewes, Christina Brock, Klaus Krogh
Journal of Clinical Medicine.2021; 10(7): 1392. CrossRef - Diabetic heart disease: A clinical update
Jake Rajbhandari, Cornelius James Fernandez, Mayuri Agarwal, Beverly Xin Yi Yeap, Joseph M Pappachan
World Journal of Diabetes.2021; 12(4): 383. CrossRef - Novel and Emerging Electrophysiological Biomarkers of Diabetic Neuropathy and Painful Diabetic Neuropathy
Anne Marshall, Uazman Alam, Andreas Themistocleous, Nigel Calcutt, Andrew Marshall
Clinical Therapeutics.2021; 43(9): 1441. CrossRef - Cardiac Autonomic Neuropathy Is Not Reversed by Euglycemia Following Islet Transplantation
Tejas Deshmukh, Peter Emerson, Patricia Anderson, Eddy Kizana, Philip J. O’Connell, D. Jane Holmes-Walker, James J.H. Chong
Transplantation.2021; 105(5): 1125. CrossRef - Attenuation of Muscle Mass and Density Is Associated With Poor Outcomes Among Patients Undergoing Major Gynecologic Surgery: A Retrospective Cohort Study
Lu Che, Yan Zhang, Jiawen Yu, Li Xu, Yuguang Huang
Anesthesia & Analgesia.2021; 132(6): 1692. CrossRef - Association of Urinary N-Acetyl-β-D-Glucosaminidase with Cardiovascular Autonomic Neuropathy in Type 1 Diabetes Mellitus without Nephropathy
Min Sun Choi, Ji Eun Jun, Sung Woon Park, Jee Hee Yoo, Jiyeon Ahn, Gyuri Kim, Sang-Man Jin, Kyu Yeon Hur, Moon-Kyu Lee, Jae Hyeon Kim
Diabetes & Metabolism Journal.2021; 45(3): 349. CrossRef - Pathogenesis, diagnosis and clinical management of diabetic sensorimotor peripheral neuropathy
Gordon Sloan, Dinesh Selvarajah, Solomon Tesfaye
Nature Reviews Endocrinology.2021; 17(7): 400. CrossRef - Heart Rate Variability as a Potential Non-invasive Marker of Blood Glucose Level
L. R. Jarman, J. L. Elliott, T. Lees, R. Clifton-Bligh, A. M. Simpson, N. Nassif, S. Lal
Human Physiology.2021; 47(2): 209. CrossRef - Cardiovascular autonomic neuropathy in diabetes: Pathophysiology, clinical assessment and implications
Alice Duque, Mauro Felippe Felix Mediano, Andrea De Lorenzo, Luiz Fernando Rodrigues Jr
World Journal of Diabetes.2021; 12(6): 855. CrossRef - Gaussian process-based kernel as a diagnostic model for prediction of type 2 diabetes mellitus risk using non-linear heart rate variability features
R. Shashikant, Uttam Chaskar, Leena Phadke, Chetankumar Patil
Biomedical Engineering Letters.2021; 11(3): 273. CrossRef - Possible Preventative/Rehabilitative Role of Gliflozins in OSA and T2DM. A Systematic Literature Review-Based Hypothesis
Vincenzo Maria Monda, Francesca Porcellati, Felice Strollo, Alessandro Fucili, Marcello Monesi, Ersilia Satta, Sandro Gentile
Advances in Therapy.2021; 38(8): 4195. CrossRef - Characteristics of cardiovascular autonomic dysfunction and association with quality of life in patients with systemic lupus erythematosus
Amanda Hempel Zinglersen, Katrine Kjær Iversen, Henrik Christian Bidstrup Leffers, Esben Laugesen, Jesper Fleischer, Søren Jacobsen
Lupus Science & Medicine.2021; 8(1): e000507. CrossRef - Impaired vagal adaptation to an exercise task in women with gestational diabetes mellitus versus women with uncomplicated pregnancies
Marieta P. Theodorakopoulou, Areti Triantafyllou, Andreas Zafeiridis, Afroditi Κ. Boutou, Iris Grigoriadou, Evangelia Kintiraki, Stella Douma, Dimitrios G. Goulis, Konstantina Dipla
Hormones.2021; 20(4): 753. CrossRef - Cardioprotective Effects of Sodium-glucose Cotransporter 2 Inhibitors Regardless of Type 2 Diabetes Mellitus: A Meta-analysis
Lucas Silva Sousa, Felipe de Araújo Nascimento, Juliano Rocha, Michelle Rocha-Parise
International Journal of Cardiovascular Sciences.2021;[Epub] CrossRef - Management of diabetic neuropathy
Simona Cernea, Itamar Raz
Metabolism.2021; 123: 154867. CrossRef - Large fibre, small fibre and autonomic neuropathy in adolescents with type 1 diabetes: A systematic review
Vinni Faber Rasmussen, Troels Staehelin Jensen, Hatice Tankisi, Páll Karlsson, Esben Thyssen Vestergaard, Kurt Kristensen, Jens Randel Nyengaard, Astrid Juhl Terkelsen
Journal of Diabetes and its Complications.2021; 35(11): 108027. CrossRef - Cardiovascular Risk Management in Type 1 Diabetes
I. H. Teoh, P. Elisaus, J. D. Schofield
Current Diabetes Reports.2021;[Epub] CrossRef - Disturbances in the intraventricular conduction system in teenagers with type 1 diabetes. A pilot study
Agnieszka Zubkiewicz-Kucharska, Anna Noczyńska, Małgorzata Sobieszczańska, Małgorzata Poręba, Joanna Chrzanowska, Rafał Poręba, Monika Seifert, Anna Janocha, Krystyna Laszki-Szcząchor
Journal of Diabetes and its Complications.2021; 35(11): 108043. CrossRef - Peripheral and Autonomic Neuropathy Status of Young Patients With Type 1 Diabetes Mellitus at the Time of Transition From Pediatric Care to Adult-Oriented Diabetes Care
Anna Vágvölgyi, Ágnes Maróti, Mónika Szűcs, Csongor Póczik, Dóra Urbán-Pap, István Baczkó, Attila Nemes, Éva Csajbók, Krisztián Sepp, Péter Kempler, Andrea Orosz, Tamás Várkonyi, Csaba Lengyel
Frontiers in Endocrinology.2021;[Epub] CrossRef - Pancreatic exocrine insufficiency in diabetes is associated with autonomic dysfunction
Dag André Sangnes, Elisabeth Sandvik Bergmann, Rose Marie Moss, Trond Engjom, Eirik Søfteland
Scandinavian Journal of Gastroenterology.2021; 56(10): 1222. CrossRef - Dependence of Heart Rate Variability Indices on the Mean Heart Rate in Women with Well-Controlled Type 2 Diabetes
Adriana Robles-Cabrera, José M. Torres-Arellano, Ruben Fossion, Claudia Lerma
Journal of Clinical Medicine.2021; 10(19): 4386. CrossRef - Normative data on cardiovascular autonomic function in Greenlandic Inuit
Marie Mathilde Bjerg Christensen, Christian Stevns Hansen, Jesper Fleischer, Dorte Vistisen, Stine Byberg, Trine Larsen, Jens Christian Laursen, Marit Eika Jørgensen
BMJ Open Diabetes Research & Care.2021; 9(1): e002121. CrossRef - What Is in the Field for Genetics and Epigenetics of Diabetic Neuropathy: The Role of MicroRNAs
V. Spallone, C. Ciccacci, A. Latini, P. Borgiani, Karim Gariani
Journal of Diabetes Research.2021; 2021: 1. CrossRef - Evaluation and treatment of peripheral nervous system dysfunction in patients with prediabetes
O. E. Zinovyeva, T. M. Ostroumova, M. V. Koniashova, N. A. Gorbachev
Neurology, Neuropsychiatry, Psychosomatics.2021; 13(5): 116. CrossRef - Manifestazioni cliniche della neuropatia autonomica diabetica: valutazione dei sintomi
Carla Greco, Chiara Pacchioni, Manuela Simoni
L'Endocrinologo.2021; 22(6): 514. CrossRef - Perspectives of glycemic variability in diabetic neuropathy: a comprehensive review
Xiaochun Zhang, Xue Yang, Bao Sun, Chunsheng Zhu
Communications Biology.2021;[Epub] CrossRef - The Association Between Cardiovascular Autonomic Function and Changes in Kidney and Myocardial Function in Type 2 Diabetes and Healthy Controls
Jens Christian Laursen, Ida Kirstine B. Rasmussen, Emilie H. Zobel, Philip Hasbak, Bernt Johan von Scholten, Lene Holmvang, Rasmus S. Ripa, Christian S. Hansen, Marie Frimodt-Moeller, Andreas Kjaer, Peter Rossing, Tine W. Hansen
Frontiers in Endocrinology.2021;[Epub] CrossRef - Dependence of heart rate variability on indicators of type 1 diabetes mellitus control.
N. O. Pertseva, O. V. Gurzhiy, K. I. Moshenets
Medicni perspektivi (Medical perspectives).2020; 25(1): 88. CrossRef - Efficacy and safety of evogliptin treatment in patients with type 2 diabetes: A multicentre, active‐controlled, randomized, double‐blind study with open‐label extension (the EVERGREEN study)
Gyuri Kim, Soo Lim, Hyuk‐Sang Kwon, Ie B. Park, Kyu J. Ahn, Cheol‐Young Park, Su K. Kwon, Hye S. Kim, Seok W. Park, Sin G. Kim, Min K. Moon, Eun S. Kim, Choon H. Chung, Kang S. Park, Mikyung Kim, Dong J. Chung, Chang B. Lee, Tae H. Kim, Moon‐Kyu Lee
Diabetes, Obesity and Metabolism.2020; 22(9): 1527. CrossRef - Diabetes mellitus and comorbidities: A bad romance
Niki Katsiki, Dimitrios Tousoulis
Hellenic Journal of Cardiology.2020; 61(1): 23. CrossRef - Features of the glucose influence on the heart activity and the changes in the potentials of the stomach and the intestines at the heart insufficiency conditions
V. V. Soltanov, L. M. Komarovskaya
Doklady of the National Academy of Sciences of Belarus.2020; 63(6): 736. CrossRef - Living Day to Day
Gerald Kayingo, Virginia McCoy Hass
Physician Assistant Clinics.2020; 5(2): 213. CrossRef - Source specific PM2.5 associated with heart rate variability in the elderly with coronary heart disease: A community-based panel study
Xi Chen, Bing Qiu, Qinpei Zou, Tian Qiu, Runkui Li, Ashley Truong, Yanmin Qi, Tao Liu, Limin Han, Tiebing Liu, Junrui Chang, Qi Sun, Ying Zhu, Dongqun Xu
Chemosphere.2020; 260: 127399. CrossRef - The Association of Autonomic Nervous System Function With Ischemic Stroke, and Treatment Strategies
Mengxi Zhao, Ling Guan, Yilong Wang
Frontiers in Neurology.2020;[Epub] CrossRef - Cardiac diabetic autonomic neuropathy
L. T. Akhmedzhanova, T. A. Belyakova, Yu. A. Podkovko, Yu. M. Shor
Medical Council.2020; (21): 94. CrossRef - Diabetes, and its treatment, as an effector of autonomic nervous system circuits and its functions
Liliana Espinoza, Carie R Boychuk
Current Opinion in Pharmacology.2020; 54: 18. CrossRef - Morning blood pressure surge is associated with autonomic neuropathy and peripheral vascular disease in patients with diabetes
Federica Di Gennaro, Cinzia D’Amato, Roberto Morganti, Carla Greco, Susanna Longo, Diana Corradini, Davide Lauro, Vincenza Spallone
Journal of Human Hypertension.2020; 34(7): 495. CrossRef - The Compound Expression of HSP90 and INOS in the Testis of Diabetic Rats as Cellular and Pathologic Adverse Effects of Diabetes
Ali Alsarhan, Kawther Faisal Amawi, Inas Saleh Al-Mazari, Hashem Abu Hurirah, Ahed J. Alkhatib
Analytical Cellular Pathology.2020; 2020: 1. CrossRef - Heart rate variability features from nonlinear cardiac dynamics in identification of diabetes using artificial neural network and support vector machine
Yogender Aggarwal, Joyani Das, Papiya Mitra Mazumder, Rohit Kumar, Rakesh Kumar Sinha
Biocybernetics and Biomedical Engineering.2020; 40(3): 1002. CrossRef - Distal Symmetric and Cardiovascular Autonomic Neuropathies in Brazilian Individuals with Type 2 Diabetes Followed in a Primary Health Care Unit: A Cross-Sectional Study
Mozania Reis de Matos, Daniele Pereira Santos-Bezerra, Cristiane das Graças Dias Cavalcante, Jacira Xavier de Carvalho, Juliana Leite, Jose Antonio Januario Neves, Sharon Nina Admoni, Marisa Passarelli, Maria Candida Parisi, Maria Lucia Correa-Giannella
International Journal of Environmental Research and Public Health.2020; 17(9): 3232. CrossRef - Awareness of hypoglycemia and spectral analysis of heart rate variability in type 1 diabetes
Ticiana Paes, L. Clemente Rolim, Celso Sallum Filho, João Roberto de Sa, Sérgio A. Dib
Journal of Diabetes and its Complications.2020; 34(8): 107617. CrossRef - Is there cardiac autonomic neuropathy in prediabetes?
Lindsay A. Zilliox, James W. Russell
Autonomic Neuroscience.2020; 229: 102722. CrossRef - Chronic Microvascular Complications in Prediabetic States—An Overview
Angelika Baranowska-Jurkun, Wojciech Matuszewski, Elżbieta Bandurska-Stankiewicz
Journal of Clinical Medicine.2020; 9(10): 3289. CrossRef - Cardiac vagal tone as a novel screening tool to recognize asymptomatic cardiovascular autonomic neuropathy: Aspects of utility in type 1 diabetes
Anne-Marie Wegeberg, Elin D Lunde, Sam Riahi, Niels Ejskjaer, Asbjørn M Drewes, Birgitte Brock, Rodica Pop-Busui, Christina Brock
Diabetes Research and Clinical Practice.2020; 170: 108517. CrossRef - Assessment of baroreceptor reflex sensitivity in young obese Saudi males at rest and in response to physiological challenges
Abdullah N. AlShahrani, Lubna I. Al‐Asoom, Ahmed A. Alsunni, Nabil S. Elbahai, Talay Yar
Physiological Reports.2020;[Epub] CrossRef - The relationship between QT interval indices with cardiac autonomic neuropathy in diabetic patients: a case control study
Maryam Vasheghani, Farzaneh Sarvghadi, Mohammad Reza Beyranvand, Habib Emami
Diabetology & Metabolic Syndrome.2020;[Epub] CrossRef - Myocardial ischaemia reperfusion injury and cardioprotection in the presence of sensory neuropathy: Therapeutic options
Péter Bencsik, Kamilla Gömöri, Tamara Szabados, Péter Sántha, Zsuzsanna Helyes, Gábor Jancsó, Péter Ferdinandy, Anikó Görbe
British Journal of Pharmacology.2020; 177(23): 5336. CrossRef - Biological Activity of c-Peptide in Microvascular Complications of Type 1 Diabetes—Time for Translational Studies or Back to the Basics?
Aleksandra Ryk, Aleksandra Łosiewicz, Arkadiusz Michalak, Wojciech Fendler
International Journal of Molecular Sciences.2020; 21(24): 9723. CrossRef - Diabetes and cardiovascular disease: inter-relation of risk factors and treatment
Aman Sharma, Shweta Mittal, Rohan Aggarwal, Meenakshi K. Chauhan
Future Journal of Pharmaceutical Sciences.2020;[Epub] CrossRef - Diabetic Autonomic Neuropathy: A Clinical Update
Jugal Kishor Sharma, Anshu Rohatgi, Dinesh Sharma
Journal of the Royal College of Physicians of Edinburgh.2020; 50(3): 269. CrossRef - Obesity, Metabolic Syndrome and the Risk of Microvascular Complications in Patients with Diabetes mellitus
Niki Katsiki, Panagiotis Anagnostis, Kalliopi Kotsa, Dimitrios G. Goulis, Dimitri P. Mikhailidis
Current Pharmaceutical Design.2019; 25(18): 2051. CrossRef - Cardiac Autonomic Neuropathy in Obesity, the Metabolic Syndrome and Prediabetes: A Narrative Review
Scott M. Williams, Aikaterini Eleftheriadou, Uazman Alam, Daniel J. Cuthbertson, John P. H. Wilding
Diabetes Therapy.2019; 10(6): 1995. CrossRef
- Rectal sensitivity correlated with gastrointestinal‐mediated glucose disposal, but not the incretin effect
- Others
- A Journey to Understand Glucose Homeostasis: Starting from Rat Glucose Transporter Type 2 Promoter Cloning to Hyperglycemia
- Yong Ho Ahn
- Diabetes Metab J. 2018;42(6):465-471. Published online November 2, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0116
- 3,906 View
- 49 Download
- 6 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader My professional journey to understand the glucose homeostasis began in the 1990s, starting from cloning of the promoter region of glucose transporter type 2 (
GLUT2 ) gene that led us to establish research foundation of my group. When I was a graduate student, I simply thought that hyperglycemia, a typical clinical manifestation of type 2 diabetes mellitus (T2DM), could be caused by a defect in the glucose transport system in the body. Thus, if a molecular mechanism controlling glucose transport system could be understood, treatment of T2DM could be possible. In the early 70s, hyperglycemia was thought to develop primarily due to a defect in the muscle and adipose tissue; thus, muscle/adipose tissue type glucose transporter (GLUT4) became a major research interest in the diabetology. However, glucose utilization occurs not only in muscle/adipose tissue but also in liver and brain. Thus, I was interested in the hepatic glucose transport system, where glucose storage and release are the most actively occurring.-
Citations
Citations to this article as recorded by- Physiological functions of glucose transporter-2: From cell physiology to links with diabetes mellitus
Zhean Shen, Yingze Hou, Guo Zhao, Libi Tan, Jili Chen, Ziqi Dong, Chunxiao Ni, Longying Pei
Heliyon.2024; 10(3): e25459. CrossRef - Estimation and implications of the genetic architecture of fasting and non-fasting blood glucose
Zhen Qiao, Julia Sidorenko, Joana A. Revez, Angli Xue, Xueling Lu, Katri Pärna, Harold Snieder, Peter M. Visscher, Naomi R. Wray, Loic Yengo
Nature Communications.2023;[Epub] CrossRef - Umbilical Cord-Mesenchymal Stem Cell-Conditioned Medium Improves Insulin Resistance in C2C12 Cell
Kyung-Soo Kim, Yeon Kyung Choi, Mi Jin Kim, Jung Wook Hwang, Kyunghoon Min, Sang Youn Jung, Soo-Kyung Kim, Yong-Soo Choi, Yong-Wook Cho
Diabetes & Metabolism Journal.2021; 45(2): 260. CrossRef - Aging-related modifications to G protein-coupled receptor signaling diversity
Jaana van Gastel, Hanne Leysen, Jan Boddaert, Laura vangenechten, Louis M. Luttrell, Bronwen Martin, Stuart Maudsley
Pharmacology & Therapeutics.2021; 223: 107793. CrossRef - Glucose transporters in the small intestine in health and disease
Hermann Koepsell
Pflügers Archiv - European Journal of Physiology.2020; 472(9): 1207. CrossRef
- Physiological functions of glucose transporter-2: From cell physiology to links with diabetes mellitus
- Complications
- Pathophysiology of Diabetic Retinopathy: The Old and the New
- Sentaro Kusuhara, Yoko Fukushima, Shuntaro Ogura, Naomi Inoue, Akiyoshi Uemura
- Diabetes Metab J. 2018;42(5):364-376. Published online October 22, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0182
- 13,359 View
- 467 Download
- 114 Web of Science
- 108 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Vision loss in diabetic retinopathy (DR) is ascribed primarily to retinal vascular abnormalities—including hyperpermeability, hypoperfusion, and neoangiogenesis—that eventually lead to anatomical and functional alterations in retinal neurons and glial cells. Recent advances in retinal imaging systems using optical coherence tomography technologies and pharmacological treatments using anti-vascular endothelial growth factor drugs and corticosteroids have revolutionized the clinical management of DR. However, the cellular and molecular mechanisms underlying the pathophysiology of DR are not fully determined, largely because hyperglycemic animal models only reproduce limited aspects of subclinical and early DR. Conversely, non-diabetic mouse models that represent the hallmark vascular disorders in DR, such as pericyte deficiency and retinal ischemia, have provided clues toward an understanding of the sequential events that are responsible for vision-impairing conditions. In this review, we summarize the clinical manifestations and treatment modalities of DR, discuss current and emerging concepts with regard to the pathophysiology of DR, and introduce perspectives on the development of new drugs, emphasizing the breakdown of the blood-retina barrier and retinal neovascularization.
-
Citations
Citations to this article as recorded by- Recent Insights into the Etiopathogenesis of Diabetic Retinopathy and Its Management
Arpon Biswas, Abhijit Deb Choudhury, Sristi Agrawal, Amol Chhatrapati Bisen, Sachin Nashik Sanap, Sarvesh Kumar Verma, Mukesh Kumar, Anjali Mishra, Shivansh Kumar, Mridula Chauhan, Rabi Sankar Bhatta
Journal of Ocular Pharmacology and Therapeutics.2024; 40(1): 13. CrossRef - GMFB/AKT/TGF‐β3 in Müller cells mediated early retinal degeneration in a streptozotocin‐induced rat diabetes model
Tong Zhu, Yingao Li, Lilin Zhu, Jinyuan Xu, Zijun Feng, Hao Chen, Si Shi, Caiying Liu, Qingjian Ou, Furong Gao, Jieping Zhang, Caixia Jin, Jingying Xu, Jiao Li, Jingfa Zhang, Yanlong Bi, Guo‐tong Xu, Juan Wang, Haibin Tian, Lixia Lu
Glia.2024; 72(3): 504. CrossRef - The significance of glutaredoxins for diabetes mellitus and its complications
Mengmeng Zhou, Eva-Maria Hanschmann, Axel Römer, Thomas Linn, Sebastian Friedrich Petry
Redox Biology.2024; 71: 103043. CrossRef - Proteomic analysis of diabetic retinopathy identifies potential plasma-protein biomarkers for diagnosis and prognosis
Bent Honoré, Javad Nouri Hajari, Tobias Torp Pedersen, Tomas Ilginis, Hajer Ahmad Al-Abaiji, Claes Sepstrup Lønkvist, Jon Peiter Saunte, Dorte Aalund Olsen, Ivan Brandslund, Henrik Vorum, Carina Slidsborg
Clinical Chemistry and Laboratory Medicine (CCLM).2024;[Epub] CrossRef - Next generation therapeutics for retinal neurodegenerative diseases
Matthew B. Appell, Jahnavi Pejavar, Ashwin Pasupathy, Sri Vishnu Kiran Rompicharla, Saed Abbasi, Kiersten Malmberg, Patricia Kolodziejski, Laura M. Ensign
Journal of Controlled Release.2024; 367: 708. CrossRef - Modeling early pathophysiological phenotypes of diabetic retinopathy in a human inner blood-retinal barrier-on-a-chip
Thomas L. Maurissen, Alena J. Spielmann, Gabriella Schellenberg, Marc Bickle, Jose Ricardo Vieira, Si Ying Lai, Georgios Pavlou, Sascha Fauser, Peter D. Westenskow, Roger D. Kamm, Héloïse Ragelle
Nature Communications.2024;[Epub] CrossRef - Emerging role of ferroptosis in diabetic retinopathy: a review
Ruohong Wang, Suyun Rao, Zheng Zhong, Ke Xiao, Xuhui Chen, Xufang Sun
Journal of Drug Targeting.2024; 32(4): 393. CrossRef - Serum vitamin D is substantially reduced and predicts flares in diabetic retinopathy patients
Yong Zhuang, Zihao Zhuang, Qingyan Cai, Xin Hu, Huibin Huang
Journal of Diabetes Investigation.2024;[Epub] CrossRef - Ocular pharmacological and biochemical profiles of 6-thioguanine: a drug repurposing study
Maria Consiglia Trotta, Carlo Gesualdo, Caterina Claudia Lepre, Marina Russo, Franca Ferraraccio, Iacopo Panarese, Ernesto Marano, Paolo Grieco, Francesco Petrillo, Anca Hermenean, Francesca Simonelli, Michele D’Amico, Claudio Bucolo, Francesca Lazzara, F
Frontiers in Pharmacology.2024;[Epub] CrossRef - Pharmacological mechanism and clinical study of Qiming granules in treating diabetic retinopathy based on network pharmacology and literature review
Yuxia Huang, Jia Wang, Yu Wang, Wei Kuang, Mengjun Xie, Mei Zhang
Journal of Ethnopharmacology.2023; 302: 115861. CrossRef - Vitreous humor proteome: unraveling the molecular mechanisms underlying proliferative and neovascular vitreoretinal diseases
Fátima Milhano dos Santos, Sergio Ciordia, Joana Mesquita, João Paulo Castro de Sousa, Alberto Paradela, Cândida Teixeira Tomaz, Luís António Paulino Passarinha
Cellular and Molecular Life Sciences.2023;[Epub] CrossRef - Protective Effects of Human Pericyte-like Adipose-Derived Mesenchymal Stem Cells on Human Retinal Endothelial Cells in an In Vitro Model of Diabetic Retinopathy: Evidence for Autologous Cell Therapy
Gabriella Lupo, Aleksandra Agafonova, Alessia Cosentino, Giovanni Giurdanella, Giuliana Mannino, Debora Lo Furno, Ivana Roberta Romano, Rosario Giuffrida, Floriana D’Angeli, Carmelina Daniela Anfuso
International Journal of Molecular Sciences.2023; 24(2): 913. CrossRef - Predictive factors for microvascular recovery after treatments for diabetic retinopathy
Junyeop Lee, Yoon-Jeon Kim, Joo-Yong Lee, Young Hee Yoon, June-Gone Kim
BMC Ophthalmology.2023;[Epub] CrossRef - Pathophysiology and diagnosis of diabetic retinopathy: a narrative review
Mohadese Estaji, Bita Hosseini, Saeed Bozorg-Qomi, Babak Ebrahimi
Journal of Investigative Medicine.2023; 71(3): 265. CrossRef - Proteomics profiling of vitreous humor reveals complement and coagulation components, adhesion factors, and neurodegeneration markers as discriminatory biomarkers of vitreoretinal eye diseases
Fátima M. Santos, Sergio Ciordia, Joana Mesquita, Carla Cruz, João Paulo Castro e Sousa, Luís A. Passarinha, Cândida T. Tomaz, Alberto Paradela
Frontiers in Immunology.2023;[Epub] CrossRef - Hypoxia-induced transcriptional differences in African and Asian versus European diabetic cybrids
Andrew H. Dolinko, Marilyn Chwa, Kevin Schneider, Mithalesh K. Singh, Shari Atilano, Jie Wu, M. Cristina Kenney
Scientific Reports.2023;[Epub] CrossRef - Downregulation of plasma microRNA-29c-3p expression may be a new risk factor for diabetic retinopathy
Bora TORUS, Hakan KORKMAZ, Kuyaş H. OZTURK, Fevziye B. ŞİRİN, Mehmet ARGUN, Sonmez ŞEVİK, Levent TÖK
Minerva Endocrinology.2023;[Epub] CrossRef - Short-Term Outcomes of Intravitreal Faricimab Injection for Diabetic Macular Edema
Sentaro Kusuhara, Maya Kishimoto-Kishi, Wataru Matsumiya, Akiko Miki, Hisanori Imai, Makoto Nakamura
Medicina.2023; 59(4): 665. CrossRef - L-type calcium channel blocker increases VEGF concentrations in retinal cells and human serum
Anmol Kumar, Stefan Mutter, Erika B. Parente, Valma Harjutsalo, Raija Lithovius, Sinnakaruppan Mathavan, Markku Lehto, Timo P. Hiltunen, Kimmo K. Kontula, Per-Henrik Groop, Satyajit Mohapatra
PLOS ONE.2023; 18(4): e0284364. CrossRef - Efficacy and safety of curcumin in diabetic retinopathy: A protocol for systematic review and meta-analysis
Liyuan Wang, Jiayu Xu, Tianyang Yu, Hanli Wang, Xiaojun Cai, He Sun, Godwin Ovenseri-Ogbomo
PLOS ONE.2023; 18(4): e0282866. CrossRef - Highly water-soluble diacetyl chrysin ameliorates diabetes-associated renal fibrosis and retinal microvascular abnormality in db/db mice
Young-Hee Kang, Sin-Hye Park, Young Eun Sim, Moon-Sik Oh, Hong Won Suh, Jae-Yong Lee, Soon Sung Lim
Nutrition Research and Practice.2023; 17(3): 421. CrossRef - Preventive and management approach of triptonide, a diterpenoid compound against streptozotocin-induced diabetic retinopathy in Wistar rat model
Chandramohan Govindasamy, Khalid S. Al-Numair, Jun Li, Weibai Chen, Guoqiang Wu
Arabian Journal of Chemistry.2023; 16(9): 105034. CrossRef - New Insights on Dietary Polyphenols for the Management of Oxidative Stress and Neuroinflammation in Diabetic Retinopathy
Gustavo Bernardes Fanaro, Marcelo Rodrigues Marques, Karin da Costa Calaza, Rafael Brito, André Moreira Pessoni, Henrique Rocha Mendonça, Deborah Emanuelle de Albuquerque Lemos, José Luiz de Brito Alves, Evandro Leite de Souza, Marinaldo Pacífico Cavalcan
Antioxidants.2023; 12(6): 1237. CrossRef - Evaluation of Social Platform-Based Continuity of Care in Improving Cognitive and Prognostic Effects of Young Patients with Diabetic Retinopathy
Guo-lan Cao, Ke-jian Chen
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 1931. CrossRef - Role of vascular endothelial growth factor B in nonalcoholic fatty liver disease and its potential value
Yu-Qi Li, Lei Xin, Yu-Chi Zhao, Shang-Qi Li, Ya-Nuo Li
World Journal of Hepatology.2023; 15(6): 786. CrossRef - The rs1800469 T/T and rs1800470 C/C genotypes of the TGFB1 gene confer protection against diabetic retinopathy in a Southern Brazilian population
Aline Rodrigues Costa, Cristine Dieter, Luís Henrique Canani, Taís Silveira Assmann, Daisy Crispim
Genetics and Molecular Biology.2023;[Epub] CrossRef - Evaluation of Self-Care in Patients with Diabetic Retinopathy
Songül BİLTEKİN, Züleyha KILIÇ, Şefika Dilek GÜVEN
Turkish Journal of Diabetes and Obesity.2023; 7(3): 214. CrossRef - Diabetes mellitus and its influence on the incidence and process of diabetic retinopathy
Janka Poráčová, Melinda Nagy, Marta Mydlárová Blaščáková, Mária Konečná, Vincent Sedlák, Mária Zahatňanská, Tatiana Kimáková, Hedviga Vašková, Viktória Rybárová, Mária Majherová, Ivan Uher
Central European Journal of Public Health.2023; 31(Suppl 1): S4. CrossRef - Dysregulation of the NLRP3 Inflammasome in Diabetic Retinopathy and Potential Therapeutic Targets
Karanvir S. Raman, Joanne A. Matsubara
Ocular Immunology and Inflammation.2022; 30(2): 470. CrossRef - Adult-induced genetic ablation distinguishes PDGFB roles in blood-brain barrier maintenance and development
Elisa Vazquez-Liebanas, Khayrun Nahar, Giacomo Bertuzzi, Annika Keller, Christer Betsholtz, Maarja Andaloussi Mäe
Journal of Cerebral Blood Flow & Metabolism.2022; 42(2): 264. CrossRef - Investigation on the Q-markers of Bushen Huoxue Prescriptions for DR treatment based on chemometric methods and spectrum-effect relationship
Yueting Yu, Ziyu Zhu, Mengjun Xie, Liping Deng, Xuejun Xie, Mei Zhang
Journal of Ethnopharmacology.2022; 285: 114800. CrossRef - Corneal Confocal Microscopy in Type 1 Diabetes Mellitus: A Six-Year Longitudinal Study
Stuti L. Misra, James A. Slater, Charles N. J. McGhee, Monika Pradhan, Geoffrey D. Braatvedt
Translational Vision Science & Technology.2022; 11(1): 17. CrossRef - Microphysiological Neurovascular Barriers to Model the Inner Retinal Microvasculature
Thomas L. Maurissen, Georgios Pavlou, Colette Bichsel, Roberto Villaseñor, Roger D. Kamm, Héloïse Ragelle
Journal of Personalized Medicine.2022; 12(2): 148. CrossRef - Long-Term Oral Administration of Salidroside Alleviates Diabetic Retinopathy in db/db Mice
Fei Yao, Xinyi Jiang, Ling Qiu, Zixuan Peng, Wei Zheng, Lexi Ding, Xiaobo Xia
Frontiers in Endocrinology.2022;[Epub] CrossRef - Classification of macular abnormalities using a lightweight CNN-SVM framework
Xuqian Wang, Yu Gu
Measurement Science and Technology.2022; 33(6): 065702. CrossRef - Chorioretinal Hypoxia Detection Using Lipid-Polymer Hybrid Organic Room-Temperature Phosphorescent Nanoparticles
Yingying Zeng, Van Phuc Nguyen, Yanxiu Li, Do Hyun Kang, Yannis M. Paulus, Jinsang Kim
ACS Applied Materials & Interfaces.2022; 14(16): 18182. CrossRef - LncRNA FLG-AS1 Mitigates Diabetic Retinopathy by Regulating Retinal Epithelial Cell Inflammation, Oxidative Stress, and Apoptosis via miR-380-3p/SOCS6 Axis
Rong Luo, Lan Li, Fan Xiao, Jinsong Fu
Inflammation.2022; 45(5): 1936. CrossRef - Correlation between the progression of diabetic retinopathy and inflammasome biomarkers in vitreous and serum – a systematic review
Charisse Y. J. Kuo, Rinki Murphy, Ilva D. Rupenthal, Odunayo O. Mugisho
BMC Ophthalmology.2022;[Epub] CrossRef - The relationship between the neutrophil-to-lymphocyte ratio and diabetic retinopathy in adults from the United States: results from the National Health and nutrition examination survey
Xiaojie He, Shanshan Qi, Xi Zhang, Jiandong Pan
BMC Ophthalmology.2022;[Epub] CrossRef - Th22 cells induce Müller cell activation via the Act1/TRAF6 pathway in diabetic retinopathy
Yufei Wang, Hongdan Yu, Jing Li, Wenqiang Liu, Shengxue Yu, Pan Lv, Lipan Zhao, Xiaobai Wang, Zhongfu Zuo, Xuezheng Liu
Cell and Tissue Research.2022; 390(3): 367. CrossRef - Prevalence and Factors Associated with Diabetic Retinopathy among Adult Diabetes Patients in Southeast Ethiopia: A Hospital-Based Cross-Sectional Study
Biniyam Sahiledengle, Tesfaye Assefa, Wogene Negash, Anwar Tahir, Tadele Regasa, Yohannes Tekalegn, Ayele Mamo, Zinash Teferu, Damtew Solomon, Habtamu Gezahegn, Kebebe Bekele, Demisu Zenbaba, Alelign Tasew, Fikreab Desta, Zegeye Regassa, Zegeye Feleke, Ch
Clinical Ophthalmology.2022; Volume 16: 3527. CrossRef - Diabetic Retinopathy: Are lncRNAs New Molecular Players and Targets?
Simona Cataldi, Mariagiovanna Tramontano, Valerio Costa, Marianna Aprile, Alfredo Ciccodicola
Antioxidants.2022; 11(10): 2021. CrossRef - Diosgenin protects retinal pigment epithelial cells from inflammatory damage and oxidative stress induced by high glucose by activating AMPK/Nrf2/HO‐1 pathway
Yang Hao, Xuefeng Gao
Immunity, Inflammation and Disease.2022;[Epub] CrossRef - Selective Activation of the Wnt-Signaling Pathway as a Novel Therapy for the Treatment of Diabetic Retinopathy and Other Retinal Vascular Diseases
Huy Nguyen, Sung-Jin Lee, Yang Li
Pharmaceutics.2022; 14(11): 2476. CrossRef - Development and validation of a predictive risk model based on retinal geometry for an early assessment of diabetic retinopathy
Minglan Wang, Xiyuan Zhou, Dan Ning Liu, Jieru Chen, Zheng Zheng, Saiguang Ling
Frontiers in Endocrinology.2022;[Epub] CrossRef - Characterization of NLRP3 Inflammasome Activation in the Onset of Diabetic Retinopathy
Charisse Y-J. Kuo, Jack J. Maran, Emma G. Jamieson, Ilva D. Rupenthal, Rinki Murphy, Odunayo O. Mugisho
International Journal of Molecular Sciences.2022; 23(22): 14471. CrossRef - VEGF Gene Polymorphism Among Diabetes Mellitus and Diabetic Retinopathy
Samra Anees, Saima Shareef, Muhammad Roman, Shah Jahan
Futuristic Biotechnology.2022; : 02. CrossRef - Th22 Cells Induce Müller Cells Activation Via the Act1/Traf6 Pathway in Diabetic Retinopathy
YuFei Wang, Hongdan Yu, Jing Li, Wenqiang Liu, Shengxue Yu, Pan Lv, Lipan Zhao, Xiaobai Wang, Zhongfu Zuo, Xuezheng Liu
SSRN Electronic Journal .2022;[Epub] CrossRef - Pathogenesis of diabetic macular edema: the role of pro-inflammatory and vascular factors. Aliterature review
M.L. Kyryliuk, S.A. Suk
INTERNATIONAL JOURNAL OF ENDOCRINOLOGY (Ukraine).2022; 18(3): 180. CrossRef - Effects of emixustat hydrochloride in patients with proliferative diabetic retinopathy: a randomized, placebo-controlled phase 2 study
Ryo Kubota, Chirag Jhaveri, John M. Koester, Jeffrey K. Gregory
Graefe's Archive for Clinical and Experimental Ophthalmology.2021; 259(2): 369. CrossRef - Transient receptor potential vanilloid 4 channel deletion regulates pathological but not developmental retinal angiogenesis
Holly C. Cappelli, Brianna D. Guarino, Anantha K. Kanugula, Ravi K. Adapala, Vidushani Perera, Matthew A. Smith, Sailaja Paruchuri, Charles K. Thodeti
Journal of Cellular Physiology.2021; 236(5): 3770. CrossRef - Involvement of miR‐126 rs4636297 and miR‐146a rs2910164 polymorphisms in the susceptibility for diabetic retinopathy: a case–control study in a type 1 diabetes population
Eloísa Toscan Massignam, Cristine Dieter, Felipe Mateus Pellenz, Taís Silveira Assmann, Daisy Crispim
Acta Ophthalmologica.2021;[Epub] CrossRef - Retinal Vascular Endothelial Cell Dysfunction and Neuroretinal Degeneration in Diabetic Patients
Malgorzata Mrugacz, Anna Bryl, Katarzyna Zorena
Journal of Clinical Medicine.2021; 10(3): 458. CrossRef - Factors based on optical coherence tomography correlated with vision impairment in diabetic patients
Hiroaki Endo, Satoru Kase, Hikari Tanaka, Mitsuo Takahashi, Satoshi Katsuta, Yasuo Suzuki, Minako Fujii, Susumu Ishida, Manabu Kase
Scientific Reports.2021;[Epub] CrossRef - Class-3 semaphorins: Potent multifunctional modulators for angiogenesis-associated diseases
Bo Jiao, Shiyang Liu, Xi Tan, Pei Lu, Danning Wang, Hui Xu
Biomedicine & Pharmacotherapy.2021; 137: 111329. CrossRef - Single-Cell Analysis of Blood-Brain Barrier Response to Pericyte Loss
Maarja A. Mäe, Liqun He, Sofia Nordling, Elisa Vazquez-Liebanas, Khayrun Nahar, Bongnam Jung, Xidan Li, Bryan C. Tan, Juat Chin Foo, Amaury Cazenave-Gassiot, Markus R. Wenk, Yvette Zarb, Barbara Lavina, Susan E. Quaggin, Marie Jeansson, Chengua Gu, David
Circulation Research.2021;[Epub] CrossRef - VEGFR1 signaling in retinal angiogenesis and microinflammation
Akiyoshi Uemura, Marcus Fruttiger, Patricia A. D'Amore, Sandro De Falco, Antonia M. Joussen, Florian Sennlaub, Lynne R. Brunck, Kristian T. Johnson, George N. Lambrou, Kay D. Rittenhouse, Thomas Langmann
Progress in Retinal and Eye Research.2021; 84: 100954. CrossRef - Changes in Gene Expression Profiling and Phenotype in Aged Multidrug Resistance Protein 4-Deficient Mouse Retinas
Kyung Woo Kim, Sentaro Kusuhara, Atsuko Katsuyama-Yoshikawa, Sho Nobuyoshi, Megumi Kitamura, Sotaro Mori, Noriyuki Sotani, Kaori Ueda, Wataru Matsumiya, Akiko Miki, Takuji Kurimoto, Hisanori Imai, Makoto Nakamura
Antioxidants.2021; 10(3): 455. CrossRef - Circular RNAs: Novel target of diabetic retinopathy
Huan-ran Zhou, Hong-yu Kuang
Reviews in Endocrine and Metabolic Disorders.2021; 22(2): 205. CrossRef - MicroRNA-431-5p encapsulated in serum extracellular vesicles as a biomarker for proliferative diabetic retinopathy
Bo Yu, Mengran Xiao, Fuhua Yang, Jing Xiao, Hui Zhang, Lin Su, Xiaomin Zhang, Xiaorong Li
The International Journal of Biochemistry & Cell Biology.2021; 135: 105975. CrossRef - EndMT Regulation by Small RNAs in Diabetes-Associated Fibrotic Conditions: Potential Link With Oxidative Stress
Roberta Giordo, Yusra M. A. Ahmed, Hilda Allam, Salah Abusnana, Lucia Pappalardo, Gheyath K. Nasrallah, Arduino Aleksander Mangoni, Gianfranco Pintus
Frontiers in Cell and Developmental Biology.2021;[Epub] CrossRef - Pharmacokinetics of genistein distribution in blood and retinas of diabetic and non-diabetic rats
T. Hakami, M.I. Mahmoud, E. de Juan, M. Cooney
Drug Metabolism and Pharmacokinetics.2021; 39: 100404. CrossRef - Nimbolide ameliorates the streptozotocin-induced diabetic retinopathy in rats through the inhibition of TLR4/NF-κB signaling pathway
Xiangwen Shu, Yali Hu, Chao Huang, Ning Wei
Saudi Journal of Biological Sciences.2021; 28(8): 4255. CrossRef - Basic regulatory effects and clinical value of metalloproteinase-14 and extracellular matrix metalloproteinase inducer in diabetic retinopathy
Shuyan Li, Shiheng Lu, Lei Zhang, Shasha Liu, Lei Wang, Kai Lin, Jialun Du, Meixia Song
Materials Express.2021; 11(6): 873. CrossRef - Reduced Acrolein Detoxification in akr1a1a Zebrafish Mutants Causes Impaired Insulin Receptor Signaling and Microvascular Alterations
Haozhe Qi, Felix Schmöhl, Xiaogang Li, Xin Qian, Christoph T. Tabler, Katrin Bennewitz, Carsten Sticht, Jakob Morgenstern, Thomas Fleming, Nadine Volk, Ingrid Hausser, Elena Heidenreich, Rüdiger Hell, Peter Paul Nawroth, Jens Kroll
Advanced Science.2021;[Epub] CrossRef - The Metaflammatory and Immunometabolic Role of Macrophages and Microglia in Diabetic Retinopathy
Honglian Wu, Mengqi Wang, Xiaorong Li, Yan Shao
Human Cell.2021; 34(6): 1617. CrossRef - Inflammatory resolution and vascular barrier restoration after retinal ischemia reperfusion injury
Steven F. Abcouwer, Sumathi Shanmugam, Arivalagan Muthusamy, Cheng-mao Lin, Dejuan Kong, Heather Hager, Xuwen Liu, David A. Antonetti
Journal of Neuroinflammation.2021;[Epub] CrossRef - Diferenças de mensuração de acuidade visual e velocidade de leitura para perto entre pacientes com retinopatia diabética. Repercussão entre conceitos de deficiência visual parcial e cegueira legal
Roberta Freitas Momenté, Isabella Couto Amaral, Luiz Guilherme Coimbra de Brito, João Gabriel Volpato Ferraresi, Maria Luisa Gois da Fonsêca, Nadyr Antônia Damasceno, Luiz Claudio Santos de Souza Lima, Mauricio Bastos Pereira, Eduardo de França Damasceno
Revista Brasileira de Oftalmologia.2021;[Epub] CrossRef - Maintaining blood retinal barrier homeostasis to attenuate retinal ischemia-reperfusion injury by targeting the KEAP1/NRF2/ARE pathway with lycopene
Hao Huang, Xielan Kuang, Xiaobo Zhu, Hao Cheng, Yuxiu Zou, Han Du, Han Tang, Linbin Zhou, Jingshu Zeng, Huijun Liu, Jianhua Yan, Chongde Long, Huangxuan Shen
Cellular Signalling.2021; 88: 110153. CrossRef - Luteolin, an aryl hydrocarbon receptor antagonist, alleviates diabetic retinopathy by regulating the NLRP/NOX4 signalling pathway: Experimental and molecular docking study
Y. Yang, M. Zhou, H. Liu
Physiology International.2021; 108(2): 172. CrossRef - ALDH2/SIRT1 Contributes to Type 1 and Type 2 Diabetes-Induced Retinopathy through Depressing Oxidative Stress
Mengshan He, Pan Long, Tao Chen, Kaifeng Li, Dongyu Wei, Yufei Zhang, Wenjun Wang, Yonghe Hu, Yi Ding, Aidong Wen, Daniela Ribeiro
Oxidative Medicine and Cellular Longevity.2021; 2021: 1. CrossRef - Looking Ahead: Visual and Anatomical Endpoints in Future Trials of Diabetic Macular Ischemia
Chui Ming Gemmy Cheung, Elizabeth Pearce, Beau Fenner, Piyali Sen, Victor Chong, Sobha Sivaprasad
Ophthalmologica.2021; 244(5): 451. CrossRef - The effect of psychotherapy on anxiety, depression, and quality of life in patients with diabetic retinopathy
Suiping Li, Hong Liu, Xian Zhu
Medicine.2021; 100(51): e28386. CrossRef - Changes in Ocular Blood Flow after Ranibizumab Intravitreal Injection for Diabetic Macular Edema Measured Using Laser Speckle Flowgraphy
Lisa Toto, Federica Evangelista, Pasquale Viggiano, Emanuele Erroi, Giada D’Onofrio, Daniele Libertini, Annamaria Porreca, Rossella D’Aloisio, Parravano Mariacristina, Luca Di Antonio, Marta Di Nicola, Rodolfo Mastropasqua
BioMed Research International.2020; 2020: 1. CrossRef - microRNA Expression Profile in the Vitreous of Proliferative Diabetic Retinopathy Patients and Differences from Patients Treated with Anti-VEGF Therapy
Julian Friedrich, David H. W. Steel, Reinier O. Schlingemann, Michael J. Koss, Hans-Peter Hammes, Guido Krenning, Ingeborg Klaassen
Translational Vision Science & Technology.2020; 9(6): 16. CrossRef - Update on the Effects of Antioxidants on Diabetic Retinopathy: In Vitro Experiments, Animal Studies and Clinical Trials
Jose Javier Garcia-Medina, Elena Rubio-Velazquez, Elisa Foulquie-Moreno, Ricardo P Casaroli-Marano, Maria Dolores Pinazo-Duran, Vicente Zanon-Moreno, Monica del-Rio-Vellosillo
Antioxidants.2020; 9(6): 561. CrossRef - Methylglyoxal, a Highly Reactive Dicarbonyl Compound, in Diabetes, Its Vascular Complications, and Other Age-Related Diseases
C. G. Schalkwijk, C. D. A. Stehouwer
Physiological Reviews.2020; 100(1): 407. CrossRef - Pericytes, inflammation, and diabetic retinopathy
Benjamin G. Spencer, Jose J. Estevez, Ebony Liu, Jamie E. Craig, John W. Finnie
Inflammopharmacology.2020; 28(3): 697. CrossRef - Eye hemodynamic data and biochemical parameters of the lacrimal fluid of patients with non-proliferative diabetic retinopathy
Guzal Kangilbaeva, Fazilat Bakhritdinova, Iroda Nabieva, Aziza Jurabekova
Data in Brief.2020; 32: 106237. CrossRef - Endocannabinoids in aqueous humour of patients with or without diabetes
Patrick Richardson, Catherine Ortori, Dave Barrett, Saoirse O'Sullivan, Iskandar Idris
BMJ Open Ophthalmology.2020; 5(1): e000425. CrossRef - A pyruvate dehydrogenase kinase inhibitor prevents retinal cell death and improves energy metabolism in rat retinas after ischemia/reperfusion injury
Kota Sato, Seiya Mochida, Daisuke Tomimoto, Takahiro Konuma, Naoki Kiyota, Satoru Tsuda, Yukihiro Shiga, Kazuko Omodaka, Toru Nakazawa
Experimental Eye Research.2020; 193: 107997. CrossRef - The Role of Bone Morphogenetic Proteins in Diabetic Complications
Nimna Perera, Rebecca H. Ritchie, Mitchel Tate
ACS Pharmacology & Translational Science.2020; 3(1): 11. CrossRef - Increased Ephrin-B2 expression in pericytes contributes to retinal vascular death in rodents
Maha Coucha, Amy C. Barrett, Joseph Bailey, Maryam Abdelghani, Mohammed Abdelsaid
Vascular Pharmacology.2020; 131: 106761. CrossRef - Mitochondrial Defects Drive Degenerative Retinal Diseases
Deborah A. Ferrington, Cody R. Fisher, Renu A. Kowluru
Trends in Molecular Medicine.2020; 26(1): 105. CrossRef - Fli1 deficiency induces endothelial adipsin expression, contributing to the onset of pulmonary arterial hypertension in systemic sclerosis
Takuya Miyagawa, Takashi Taniguchi, Ryosuke Saigusa, Maiko Fukayama, Takehiro Takahashi, Takashi Yamashita, Megumi Hirabayashi, Shunsuke Miura, Kouki Nakamura, Ayumi Yoshizaki, Shinichi Sato, Yoshihide Asano
Rheumatology.2020; 59(8): 2005. CrossRef - Natriuretic Peptides Attenuate Retinal Pathological Neovascularization Via Cyclic Guanosine Monophosphate Signaling in Pericytes and Astrocytes
Katarina Špiranec Spes, Sabrina Hupp, Franziska Werner, Franziska Koch, Katharina Völker, Lisa Krebes, Ulrike Kämmerer, Katrin G. Heinze, Barbara M. Braunger, Michaela Kuhn
Arteriosclerosis, Thrombosis, and Vascular Biology.2020; 40(1): 159. CrossRef - Therapeutic investigation of quercetin nanomedicine in a zebrafish model of diabetic retinopathy
Shuai Wang, Shanshan Du, Wenzhan Wang, Fengyan Zhang
Biomedicine & Pharmacotherapy.2020; 130: 110573. CrossRef - The role of CD44 in pathological angiogenesis
Li Chen, Chenying Fu, Qing Zhang, Chengqi He, Feng Zhang, Quan Wei
The FASEB Journal.2020; 34(10): 13125. CrossRef - Associations between alcohol intake and diabetic retinopathy risk: a systematic review and meta-analysis
Chen Chen, Zhaojun Sun, Weigang Xu, Jun Tan, Dan Li, Yiting Wu, Ting Zheng, Derong Peng
BMC Endocrine Disorders.2020;[Epub] CrossRef - Alpha-Smooth Muscle Actin-Positive Perivascular Cells in Diabetic Retina and Choroid
Soo Jin Kim, Sang A. Kim, Yeong A. Choi, Do Young Park, Junyeop Lee
International Journal of Molecular Sciences.2020; 21(6): 2158. CrossRef - The G‐protein‐coupled chemoattractant receptor Fpr2 exacerbates neuroglial dysfunction and angiogenesis in diabetic retinopathy
Ying Yu, Shengding Xue, Keqiang Chen, Yingying Le, Rongrong Zhu, Shiyi Wang, Shuang Liu, Xinliang Cheng, Huaijin Guan, Ji Ming Wang, Hui Chen
FASEB BioAdvances.2020; 2(10): 613. CrossRef - Dual-Acting Antiangiogenic Gene Therapy Reduces Inflammation and Regresses Neovascularization in Diabetic Mouse Retina
Rute S. Araújo, Diogo B. Bitoque, Gabriela A. Silva
Molecular Therapy - Nucleic Acids.2020; 22: 329. CrossRef - The cells involved in the pathological process of diabetic retinopathy
Songtao Yang, Jiaoyue Zhang, Lulu Chen
Biomedicine & Pharmacotherapy.2020; 132: 110818. CrossRef - The Role of Transforming Growth Factor-Beta in Retinal Ganglion Cells with Hyperglycemia and Oxidative Stress
Hsin-Yi Chen, Yi-Jung Ho, Hsiu-Chuan Chou, En-Chi Liao, Yi-Ting Tsai, Yu-Shan Wei, Li-Hsun Lin, Meng-Wei Lin, Yi-Shiuan Wang, Mei-Lan Ko, Hong-Lin Chan
International Journal of Molecular Sciences.2020; 21(18): 6482. CrossRef - Circadian rhythms in diabetic retinopathy: an overview of pathogenesis and investigational drugs
Ashay D. Bhatwadekar, Varun Rameswara
Expert Opinion on Investigational Drugs.2020; 29(12): 1431. CrossRef - Blood-retinal barrier as a converging pivot in understanding the initiation and development of retinal diseases
Xue Yang, Xiao-Wei Yu, Dan-Dan Zhang, Zhi-Gang Fan
Chinese Medical Journal.2020; 133(21): 2586. CrossRef - Immunosubunit β5i Knockout Suppresses Neovascularization and Restores Autophagy in Retinal Neovascularization by Targeting ATG5 for Degradation
Liyang Ji, Li Li, Ying Zhao, Shengqiang Liu, Jingmin Li, Jinsong Zhang, Qi Zhao, Shuai Wang
Investigative Opthalmology & Visual Science.2020; 61(14): 30. CrossRef - Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study
Yoo-Ri Chung, Kyoung Hwa Ha, Hyeon Chang Kim, Sang Jun Park, Kihwang Lee, Dae Jung Kim
Diabetes & Metabolism Journal.2019; 43(5): 640. CrossRef - Age-related changes of the human retinal vessels: Possible involvement of lipid peroxidation
Tapas Chandra Nag, Meenakshi Maurya, Tara Sankar Roy
Annals of Anatomy - Anatomischer Anzeiger.2019; 226: 35. CrossRef - Human iPSCs-Derived Endothelial Cells with Mutation in HNF1A as a Model of Maturity-Onset Diabetes of the Young
Kachamakova-Trojanowska, Stepniewski, Dulak
Cells.2019; 8(11): 1440. CrossRef - Diabetic Retinopathy–An Underdiagnosed and Undertreated Inflammatory, Neuro-Vascular Complication of Diabetes
Stephen H. Sinclair, Stanley S. Schwartz
Frontiers in Endocrinology.2019;[Epub] CrossRef - Identification of Diagnostic and Prognostic microRNAs for Recurrent Vitreous Hemorrhage in Patients with Proliferative Diabetic Retinopathy
Parviz Mammadzada, Juliette Bayle, Johann Gudmundsson, Anders Kvanta, Helder André
Journal of Clinical Medicine.2019; 8(12): 2217. CrossRef - RANKL blockade suppresses pathological angiogenesis and vascular leakage in ischemic retinopathy
Sangmi Ock, Soyoung Park, Junyeop Lee, Jaetaek Kim
Biochemical and Biophysical Research Communications.2019; 516(2): 350. CrossRef - EndogenousClostridium perfringensPanophthalmitis with Potential Entry Port from Diverticulitis Exacerbated by Proliferative Diabetic Retinopathy
Vamsee Neerukonda, Anny M. S. Cheng, Swetha Dhanireddy, Samuel Alpert, Han Y. Yin
Case Reports in Ophthalmological Medicine.2019; 2019: 1. CrossRef - Attenuation of Retinal Endothelial Vasodilator Function in a Rat Model of Retinopathy of Prematurity
Ayuki Nakano, Asami Mori, Shiho Arima, Daiki Asano, Akane Morita, Kenji Sakamoto, Tohru Nagamitsu, Tsutomu Nakahara
Current Eye Research.2019; 44(12): 1360. CrossRef - Efficacy of fenofibrate for diabetic retinopathy
Xing-jie Su, Lin Han, Yan-Xiu Qi, Hong-wei Liu
Medicine.2019; 98(14): e14999. CrossRef - Nutraceuticals for the Treatment of Diabetic Retinopathy
Maria Grazia Rossino, Giovanni Casini
Nutrients.2019; 11(4): 771. CrossRef - Efficacy of ranibizumab for the treatment of diabetic retinopathy
Yong-bo Ren, Xing-jie Su, Yan-xiu Qi, He-qun Luan, Qi Sun
Medicine.2019; 98(17): e15409. CrossRef
- Recent Insights into the Etiopathogenesis of Diabetic Retinopathy and Its Management
- Clinical Diabetes & Therapeutics
- Diabetes and Subclinical Coronary Atherosclerosis
- Chang Hoon Lee, Seung-Whan Lee, Seong-Wook Park
- Diabetes Metab J. 2018;42(5):355-363. Published online October 22, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0041
- 4,672 View
- 58 Download
- 13 Web of Science
- 11 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader It is well known that diabetic patients have a high risk of cardiovascular events, and although there has been a tremendous effort to reduce these cardiovascular risks, the incidence of cardiovascular morbidity and mortality in diabetic patients remains high. Therefore, the early detection of coronary artery disease (CAD) is necessary in those diabetic patients who are at risk of cardiovascular events. Significant medical and radiological advancements, including coronary computed tomography angiography (CCTA), mean that it is now possible to investigate the characteristics of plaques, instead of solely evaluating the calcium level of the coronary artery. Recently, several studies reported that the prevalence of subclinical coronary atherosclerosis (SCA) is higher than expected, and this could impact on CAD progression in asymptomatic diabetic patients. In addition, several reports suggest the potential benefit of using CCTA for screening for SCA in asymptomatic diabetic patients, which might dramatically decrease the incidence of cardiovascular events. For these reasons, the medical interest in SCA in diabetic patients is increasing. In this article, we sought to review the results of studies on CAD in asymptomatic diabetic patients and discuss the clinical significance and possibility of using CCTA to screen for SCA.
-
Citations
Citations to this article as recorded by- Coronary Artery Calcium Score directed risk stratification of patients with Type-2 diabetes mellitus
Mahmoud Nassar, Nso Nso, Kelechi Emmanuel, Mohsen Alshamam, Most Sirajum Munira, Anoop Misra
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2022; 16(6): 102503. CrossRef - Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Ji Eun Jun, You-Cheol Hwang, Kyu Jeong Ahn, Ho Yeon Chung, Geon-Ho Jahng, Soonchan Park, In-Kyung Jeong, Chang-Woo Ryu
Diabetes Research and Clinical Practice.2022; 191: 110067. CrossRef - Serum metabolic signatures of subclinical atherosclerosis in patients with type 2 diabetes mellitus: a preliminary study
Jiaorong Su, Qing Zhao, Aihua Zhao, Wei Jia, Wei Zhu, Jingyi Lu, Xiaojing Ma
Acta Diabetologica.2021; 58(9): 1217. CrossRef - Atherogenic Index of Plasma, Triglyceride-Glucose Index and Monocyte-to-Lymphocyte Ratio for Predicting Subclinical Coronary Artery Disease
Yueqiao Si, Wenjun Fan, Chao Han, Jingyi Liu, Lixian Sun
The American Journal of the Medical Sciences.2021; 362(3): 285. CrossRef - Cardiologist's approach to the diabetic patient: No further delay for a paradigm shift
Francesco Maranta, Lorenzo Cianfanelli, Carlo Gaspardone, Vincenzo Rizza, Rocco Grippo, Marco Ambrosetti, Domenico Cianflone
International Journal of Cardiology.2021; 338: 248. CrossRef - Co‐expression of glycosylated aquaporin‐1 and transcription factor NFAT5 contributes to aortic stiffness in diabetic and atherosclerosis‐prone mice
Rosalinda Madonna, Vanessa Doria, Anikó Görbe, Nino Cocco, Péter Ferdinandy, Yong‐Jian Geng, Sante Donato Pierdomenico, Raffaele De Caterina
Journal of Cellular and Molecular Medicine.2020; 24(5): 2857. CrossRef - Recent Updates on Vascular Complications in Patients with Type 2 Diabetes Mellitus
Chan-Hee Jung, Ji-Oh Mok
Endocrinology and Metabolism.2020; 35(2): 260. CrossRef - Quantitative measure of asymptomatic cardiovascular disease risk in Type 2 diabetes: Evidence from Indian outpatient setting
Samit Ghosal, Binayak Sinha, Jignesh Ved, Mansij Biswas
Indian Heart Journal.2020; 72(2): 119. CrossRef - Role of pregnancy hormones and hormonal interaction on the maternal cardiovascular system: a literature review
Vitaris Kodogo, Feriel Azibani, Karen Sliwa
Clinical Research in Cardiology.2019; 108(8): 831. CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - Effects of Diabetes on Motor Recovery After Cerebral Infarct: A Diffusion Tensor Imaging Study
Jun Sung Moon, Seung Min Chung, Sung Ho Jang, Kyu Chang Won, Min Cheol Chang
The Journal of Clinical Endocrinology & Metabolism.2019; 104(9): 3851. CrossRef
- Coronary Artery Calcium Score directed risk stratification of patients with Type-2 diabetes mellitus
- Obesity and Metabolic Syndrome
- Role of the Pyruvate Dehydrogenase Complex in Metabolic Remodeling: Differential Pyruvate Dehydrogenase Complex Functions in Metabolism
- Sungmi Park, Jae-Han Jeon, Byong-Keol Min, Chae-Myeong Ha, Themis Thoudam, Bo-Yoon Park, In-Kyu Lee
- Diabetes Metab J. 2018;42(4):270-281. Published online August 21, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0101
- 9,858 View
- 298 Download
- 102 Web of Science
- 101 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Mitochondrial dysfunction is a hallmark of metabolic diseases such as obesity, type 2 diabetes mellitus, neurodegenerative diseases, and cancers. Dysfunction occurs in part because of altered regulation of the mitochondrial pyruvate dehydrogenase complex (PDC), which acts as a central metabolic node that mediates pyruvate oxidation after glycolysis and fuels the Krebs cycle to meet energy demands. Fine-tuning of PDC activity has been mainly attributed to post-translational modifications of its subunits, including the extensively studied phosphorylation and de-phosphorylation of the E1α subunit of pyruvate dehydrogenase (PDH), modulated by kinases (pyruvate dehydrogenase kinase [PDK] 1-4) and phosphatases (pyruvate dehydrogenase phosphatase [PDP] 1-2), respectively. In addition to phosphorylation, other covalent modifications, including acetylation and succinylation, and changes in metabolite levels via metabolic pathways linked to utilization of glucose, fatty acids, and amino acids, have been identified. In this review, we will summarize the roles of PDC in diverse tissues and how regulation of its activity is affected in various metabolic disorders.
-
Citations
Citations to this article as recorded by- Mitochondria dysfunction induced by decyl-TPP mitochondriotropic antioxidant based on caffeic acid AntiOxCIN6 sensitizes cisplatin lung anticancer therapy due to a remodeling of energy metabolism
Ricardo Amorim, Carina C. Magalhães, Sofia Benfeito, Fernando Cagide, Ludgero C. Tavares, Katia Santos, Vilma A. Sardão, Sandipan Datta, Gino A. Cortopassi, Inês Baldeiras, John G. Jones, Fernanda Borges, Paulo J. Oliveira, José Teixeira
Biochemical Pharmacology.2024; 219: 115953. CrossRef - Thiamine analogues featuring amino-oxetanes as potent and selective inhibitors of pyruvate dehydrogenase
Alex H.Y. Chan, Terence C.S. Ho, Finian J. Leeper
Bioorganic & Medicinal Chemistry Letters.2024; 98: 129571. CrossRef - Pyruvate Dehydrogenase Complex in Neonatal Hypoxic–Ischemic Brain Injury
Tao Zhou, Yuangao Zhong, Yong Zhang, Yue Zhou
ACS Pharmacology & Translational Science.2024; 7(1): 42. CrossRef - Biomarkers of heart failure: advances in omics studies
Kuo Chi, Jing Liu, Xinghua Li, He Wang, Yanliang Li, Qingnan Liu, Yabin Zhou, Yuan Ge
Molecular Omics.2024; 20(3): 169. CrossRef - Effects of ambient UVB light on Pacific oyster Crassostrea gigas mantle tissue based on multivariate data
Hongce Song, Chaoyi Xie, Meiyun Dong, Yuxuan Zhang, Haifeng Huang, Yijing Han, Yaqiong Liu, Lei Wei, Xiaotong Wang
Ecotoxicology and Environmental Safety.2024; 274: 116236. CrossRef - Autocrine phosphatase PDP2 inhibits ferroptosis by dephosphorylating ACSL4 in the Luminal A Breast Cancer
Jun-Jie Zhu, Feng-Ying Huang, Hengyu Chen, Yun-long Zhang, Ming-Hui Chen, Ri-Hong Wu, Shu-Zhen Dai, Gui-Sheng He, Guang-Hong Tan, Wu-Ping Zheng, Sreeparna Banerjee
PLOS ONE.2024; 19(3): e0299571. CrossRef - Glutaminase potentiates the glycolysis in esophageal squamous cell carcinoma by interacting with PDK1
Guangzhao Zhu, Fangxia Guan, Shenglei Li, Qing Zhang, Xueying Zhang, Yue Qin, Zhangzhan Sun, Shaohua Peng, Jiexing Cheng, Yiyang Li, Ruili Ren, Tianli Fan, Hongtao Liu
Molecular Carcinogenesis.2024; 63(5): 897. CrossRef - Inhibition of Pyruvate Dehydrogenase Kinase 4 in CD4+ T Cells Ameliorates Intestinal Inflammation
Hoyul Lee, Jae Han Jeon, Yu-Jeong Lee, Mi-Jin Kim, Woong Hee Kwon, Dipanjan Chanda, Themis Thoudam, Haushabhau S. Pagire, Suvarna H. Pagire, Jin Hee Ahn, Robert A. Harris, Eun Soo Kim, In-Kyu Lee
Cellular and Molecular Gastroenterology and Hepatology.2023; 15(2): 439. CrossRef - Nitric oxide regulation of cellular metabolism: Adaptive tuning of cellular energy
Gregory Pappas, Melissa L. Wilkinson, Andrew J. Gow
Nitric Oxide.2023; 131: 8. CrossRef - Furan-based inhibitors of pyruvate dehydrogenase: SAR study, biochemical evaluation and computational analysis
Alex H. Y. Chan, Terence C. S. Ho, Daniel R. Parle, Finian J. Leeper
Organic & Biomolecular Chemistry.2023; 21(8): 1755. CrossRef - The pyruvate dehydrogenase complex: Life’s essential, vulnerable and druggable energy homeostat
Peter W. Stacpoole, Charles E. McCall
Mitochondrion.2023; 70: 59. CrossRef - The Impact of Krebs Cycle Intermediates on the Endocrine System and Immune System: A Comparison
Borros M. Arneth
Endocrines.2023; 4(1): 179. CrossRef - Consequences of reprogramming acetyl-CoA metabolism by 2,3,7,8-tetrachlorodibenzo-p-dioxin in the mouse liver
Giovan N. Cholico, Karina Orlowska, Russell R. Fling, Warren J. Sink, Nicholas A. Zacharewski, Kelly A. Fader, Rance Nault, Tim Zacharewski
Scientific Reports.2023;[Epub] CrossRef - The Link between Mitochondrial Dysfunction and Sarcopenia: An Update Focusing on the Role of Pyruvate Dehydrogenase Kinase 4
Min-Ji Kim, Ibotombi Singh Sinam, Zerwa Siddique, Jae-Han Jeon, In-Kyu Lee
Diabetes & Metabolism Journal.2023; 47(2): 153. CrossRef - Targeting PDK2 rescues stress-induced impaired brain energy metabolism
Changshui Wang, Changmeng Cui, Pengfei Xu, Li Zhu, Hongjia Xue, Beibei Chen, Pei Jiang
Molecular Psychiatry.2023; 28(10): 4138. CrossRef - The Role of Pyruvate Metabolism in Mitochondrial Quality Control and Inflammation
Min-Ji Kim, Hoyul Lee, Dipanjan Chanda, Themis Thoudam, Hyeon-Ji Kang, Robert A. Harris, In-Kyu Lee
Molecules and Cells.2023; 46(5): 259. CrossRef - Inhibition of pyruvate dehydrogenase kinase 4 ameliorates kidney ischemia-reperfusion injury by reducing succinate accumulation during ischemia and preserving mitochondrial function during reperfusion
Chang Joo Oh, Min-Ji Kim, Ji-Min Lee, Dong Hun Kim, Il-Young Kim, Sanghee Park, Yeongmin Kim, Kyung-Bok Lee, Sang-Hee Lee, Chae Won Lim, Myeongjin Kim, Jung-Yi Lee, Haushabhau S. Pagire, Suvarna H. Pagire, Myung Ae Bae, Dipanjan Chanda, Themis Thoudam, Ah
Kidney International.2023; 104(4): 724. CrossRef - PDHA1 hyperacetylation-mediated lactate overproduction promotes sepsis-induced acute kidney injury via Fis1 lactylation
Sheng An, Yi Yao, Hongbin Hu, Junjie Wu, Jiaxin Li, Lulan Li, Jie Wu, Maomao Sun, Zhiya Deng, Yaoyuan Zhang, Shenhai Gong, Qiaobing Huang, Zhongqing Chen, Zhenhua Zeng
Cell Death & Disease.2023;[Epub] CrossRef - Iron promotes glycolysis to drive colon tumorigenesis
Zhaoli Liu, Luke Villareal, Lavanya Goodla, Hyeoncheol Kim, Daniel M. Falcon, Mohammad Haneef, David R. Martin, Li Zhang, Ho-Joon Lee, Daniel Kremer, Costas A. Lyssiotis, Yatrik M. Shah, Henry C. Lin, Hui-kuan Lin, Xiang Xue
Biochimica et Biophysica Acta (BBA) - Molecular Basis of Disease.2023; 1869(8): 166846. CrossRef - Driving force of deteriorated cellular environment in heart failure: Metabolic remodeling
Lu Fan, Chenchen Meng, Xiaoming Wang, Yunjiao Wang, Yanyang Li, Shichao Lv, Junping Zhang
Clinics.2023; 78: 100263. CrossRef - Mitochondrial dysfunctions in T cells: focus on inflammatory bowel disease
Hoyul Lee, Jae-Han Jeon, Eun Soo Kim
Frontiers in Immunology.2023;[Epub] CrossRef - Adrenomedullin induces cisplatin chemoresistance in ovarian cancer through reprogramming of glucose metabolism
Lei Dou, Enting Lu, Dongli Tian, Fangmei Li, Lei Deng, Yi Zhang
Journal of Translational Internal Medicine.2023; 11(2): 169. CrossRef - Metabolic deregulation associated with aging modulates protein aggregation in the yeast model of Huntington’s disease
Sai Sanwid Pradhan, Sai Swaroop R., Sai Phalguna Kanikaram, Datta Darshan V.M., Ashish Pargaonkar, Rajesh Babu Dandamudi, Venketesh Sivaramakrishnan
Journal of Biomolecular Structure and Dynamics.2023; : 1. CrossRef - Unique and generic crossed metabolism in response to four sub-lethal environmental stresses in the oriental fruit fly, Bactrocera dorsalis Hendel
Lili Ren, Hongxia Zhang, Jiao Zhou, Yajing Wu, Bo Liu, Shuping Wang, Xin Liu, Xin Hao, Lilin Zhao
Ecotoxicology and Environmental Safety.2023; 264: 115434. CrossRef - Oxidative stress regulation and related metabolic pathways in epithelial–mesenchymal transition of breast cancer stem cells
Raheleh Farahzadi, Behnaz Valipour, Ezzatollah Fathi, Samaneh Pirmoradi, Ommoleila Molavi, Soheila Montazersaheb, Zohreh Sanaat
Stem Cell Research & Therapy.2023;[Epub] CrossRef - Preclinical Study in Mouse Thymus and Thymocytes: Effects of Treatment with a Combination of Sodium Dichloroacetate and Sodium Valproate on Infectious Inflammation Pathways
Donatas Stakišaitis, Linas Kapočius, Evelina Kilimaitė, Dovydas Gečys, Lina Šlekienė, Ingrida Balnytė, Jolita Palubinskienė, Vaiva Lesauskaitė
Pharmaceutics.2023; 15(12): 2715. CrossRef - Contrasting effects of whole-body and hepatocyte-specific deletion of the RNA polymerase III repressor Maf1 in the mouse
Gilles Willemin, François Mange, Viviane Praz, Séverine Lorrain, Pascal Cousin, Catherine Roger, Ian M. Willis, Nouria Hernandez
Frontiers in Molecular Biosciences.2023;[Epub] CrossRef - Reprogramming of glucose metabolism of cumulus cells and oocytes and its therapeutic significance
Shogo Imanaka, Hiroshi Shigetomi, Hiroshi Kobayashi
Reproductive Sciences.2022; 29(3): 653. CrossRef - Renal denervation ameliorates cardiac metabolic remodeling in diabetic cardiomyopathy rats by suppressing renal SGLT2 expression
Jun-Yu Huo, Wan-Ying Jiang, Shi-Geng Zhang, Yi-Ting Lyu, Jie Geng, Meng Chen, Yuan-Yuan Chen, Zhi-Xin Jiang, Qi-Jun Shan
Laboratory Investigation.2022; 102(4): 341. CrossRef - Alteration in glycolytic/cholesterogenic gene expression is associated with bladder cancer prognosis and immune cell infiltration
Yuying Zhang, Baoyi Zhu, Yi Cai, Sihua Zhu, Hongjun Zhao, Xiaoling Ying, Chonghe Jiang, Jianwen Zeng
BMC Cancer.2022;[Epub] CrossRef - Protein phosphorylation in hemocytes of Fenneropenaeus chinensis in response to white spot syndrome virus infection
Xiaoqian Tang, Ting Liu, Xiaoai Li, Xiuzhen Sheng, Jing Xing, Heng Chi, Wenbin Zhan
Fish & Shellfish Immunology.2022; 122: 106. CrossRef - The Critical Role Played by Mitochondrial MITF Serine 73 Phosphorylation in Immunologically Activated Mast Cells
Lakshmi Bhargavi Paruchuru, Sharmila Govindaraj, Ehud Razin
Cells.2022; 11(3): 589. CrossRef - Glycemic Control and the Heart: The Tale of Diabetic Cardiomyopathy Continues
Miriam Longo, Lorenzo Scappaticcio, Paolo Cirillo, Antonietta Maio, Raffaela Carotenuto, Maria Ida Maiorino, Giuseppe Bellastella, Katherine Esposito
Biomolecules.2022; 12(2): 272. CrossRef - Metabolic Reprogramming in Response to Alterations of Mitochondrial DNA and Mitochondrial Dysfunction in Gastric Adenocarcinoma
Tzu-Ching Chang, Hui-Ting Lee, Siao-Cian Pan, Shih-Han Cho, Chieh Cheng, Liang-Hung Ou, Chia-I Lin, Chen-Sung Lin, Yau-Huei Wei
International Journal of Molecular Sciences.2022; 23(3): 1857. CrossRef - Toxicological effects of tris(1,3-dichloro-2-propyl) phosphate in oyster Crassostrea gigas using proteomic and phosphoproteomic analyses
Chengcheng Yin, Zuodeng Sun, Chenglong Ji, Fei Li, Huifeng Wu
Journal of Hazardous Materials.2022; 434: 128824. CrossRef - Water-Extracted Prunella vulgaris Alleviates Endometriosis by Reducing Aerobic Glycolysis
Min Kyoung Cho, Ling Jin, Jung Ho Han, Jung-Suk Jin, Se-Yun Cheon, Su Shin, Sung-Jin Bae, Jang-Kyung Park, Ki-Tae Ha
Frontiers in Pharmacology.2022;[Epub] CrossRef - Pyruvate Dehydrogenase A1 Phosphorylated by Insulin Associates with Pyruvate Kinase M2 and Induces LINC00273 through Histone Acetylation
Abu Jubayer Hossain, Rokibul Islam, Jae-Gyu Kim, Oyungerel Dogsom, Kim Cuong Cap, Jae-Bong Park
Biomedicines.2022; 10(6): 1256. CrossRef - Celastrol alleviates high-fat diet-induced obesity via enhanced muscle glucose utilization and mitochondrial oxidative metabolism-mediated upregulation of pyruvate dehydrogenase complex
Mohamad Hafizi Abu Bakar, Nor Shafiqah Nor Shahril, Mohamad Shamil Faris Mohamad Khalid, Sharifah Mohammad, Khairul Anuar Shariff, Thiruventhan Karunakaran, Rabeta Mohd Salleh, Mohamad Norisham Mohamad Rosdi
Toxicology and Applied Pharmacology.2022; 449: 116099. CrossRef - Regulation of Metabolism by Mitochondrial MUL1 E3 Ubiquitin Ligase
Lucia Cilenti, Rohit Mahar, Jacopo Di Gregorio, Camilla T. Ambivero, Matthew E. Merritt, Antonis S. Zervos
Frontiers in Cell and Developmental Biology.2022;[Epub] CrossRef - The Pyruvate Dehydrogenase Complex Mitigates LPS-Induced Endothelial Barrier Dysfunction by Metabolic Regulation
Liangfeng Mao, Maomao Sun, Zhenfeng Chen, Zhenhua Zeng, Jie Wu, Zhongqing Chen, Weijin Zhang, Qiaobing Huang
Shock.2022; 57(6): 308. CrossRef - Review: Influence of postabsorptive metabolism on essential amino acid partitioning in lactating dairy cows
J.P. Cant, G.C. Reyes, D.J. Seymour
animal.2022; 16: 100573. CrossRef - T Cells Mediate Kidney Tubular Injury via Impaired PDHA1 and Autophagy in Type 1 Diabetes
Chung-Hsing Wang, Wen-Li Lu, Shang-Lun Chiang, Tsung-Hsun Tsai, Su-Ching Liu, Chia-Hung Hsieh, Pen-Hua Su, Chih-Yang Huang, Fuu-Jen Tsai, Yu-Jung Lin, Yu-Nan Huang
The Journal of Clinical Endocrinology & Metabolism.2022; 107(9): 2556. CrossRef - Pyruvate Dehydrogenase Kinase Protects Dopaminergic Neurons from Oxidative Stress in Drosophila DJ-1 Null Mutants
Yoonjeong Lee, Jaehyeon Kim, Hyunjin Kim, Ji Eun Han, Sohee Kim, Kyong-hwa Kang, Donghoon Kim, Jong-Min Kim, Hyongjong Koh
Molecules and Cells.2022; 45(7): 454. CrossRef - Metabolic regulation of T cell development
Mengdi Zhang, Xiaoxi Lin, Zhou Yang, Xia Li, Zhiguang Zhou, Paul E. Love, Jiaqi Huang, Bin Zhao
Frontiers in Immunology.2022;[Epub] CrossRef - Noncanonical PDK4 action alters mitochondrial dynamics to affect the cellular respiratory status
Themis Thoudam, Dipanjan Chanda, Ibotombi Singh Sinam, Byung-Gyu Kim, Mi-Jin Kim, Chang Joo Oh, Jung Yi Lee, Min-Ji Kim, Soo Yeun Park, Shin Yup Lee, Min-Kyo Jung, Ji Young Mun, Robert A. Harris, Naotada Ishihara, Jae-Han Jeon, In-Kyu Lee
Proceedings of the National Academy of Sciences.2022;[Epub] CrossRef - Frontiers in the enzymology of thiamin diphosphate-dependent enzymes
Sabin Prajapati, Fabian Rabe von Pappenheim, Kai Tittmann
Current Opinion in Structural Biology.2022; 76: 102441. CrossRef - The Role of the Pyruvate Dehydrogenase Complex in the Development of Ischemic-Reperfusion Syndrome
K. A. Popov, Ya. E. Denisova, I. M. Bykov, I. Yu. Tsymbalyuk, G. A. Ermakova, A. G. Zavgorodnyaya, A. S. Shevchenko
Kuban Scientific Medical Bulletin.2022; 29(4): 75. CrossRef - The fragility of liver glycogen from humans with type 2 diabetes: A pilot study
Ziyi Wang, Xiaobo Min, Zhenxia Hu, Mitchell A. Sullivan, Yong Tang, Liang Wang, Robert G. Gilbert, Chen Shi, Bin Deng
International Journal of Biological Macromolecules.2022; 221: 83. CrossRef - Distinct role of mitochondrial function and protein kinase C in intimal and medial calcification in vitro
Marina A. Heuschkel, Anne Babler, Jonas Heyn, Emiel P. C. van der Vorst, Marja Steenman, Maren Gesper, Ben A. Kappel, David Magne, Yann Gouëffic, Rafael Kramann, Willi Jahnen-Dechent, Nikolaus Marx, Thibaut Quillard, Claudia Goettsch
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - Metabolomic responses in livers of female and male zebrafish (Danio rerio) following prolonged exposure to environmental levels of zinc oxide nanoparticles
Xiaohong Wang, Siying Chen, Yingju Qin, Haiqing Wang, Zhenda Liang, Yuanhui Zhao, Li Zhou, Christopher J. Martyniuk
Aquatic Toxicology.2022; 253: 106333. CrossRef - A Missense Variant in PDK1 Associated with Severe Neurodevelopmental Delay and Epilepsy
Raquel Vaz, Josephine Wincent, Najla Elfissi, Kristina Rosengren Forsblad, Maria Pettersson, Karin Naess, Anna Wedell, Anna Wredenberg, Anna Lindstrand, Sofia Ygberg
Biomedicines.2022; 10(12): 3171. CrossRef - Rg3 regulates myocardial pyruvate metabolism via P300-mediated dihydrolipoamide dehydrogenase 2-hydroxyisobutyrylation in TAC-induced cardiac hypertrophy
Jingyu Ni, Hao Zhang, Xiaodan Wang, Zhihao Liu, Tong Nie, Lan Li, Jing Su, Yan Zhu, Chuanrui Ma, Yuting Huang, Jingyuan Mao, Xiumei Gao, Guanwei Fan
Cell Death & Disease.2022;[Epub] CrossRef - Glutamine mitigates murine burn sepsis by supporting macrophage M2 polarization through repressing the SIRT5-mediated desuccinylation of pyruvate dehydrogenase
Yuanfeng Zhu, Xiaoli Chen, Yongling Lu, Lin Xia, Shijun Fan, Qianying Huang, Xin Liu, Xi Peng
Burns & Trauma.2022;[Epub] CrossRef - Loss of metabolic flexibility as a result of overexpression of pyruvate dehydrogenase kinases in muscle, liver and the immune system: Therapeutic targets in metabolic diseases
Jae‐Han Jeon, Themis Thoudam, Eun Jung Choi, Min‐Ji Kim, Robert A Harris, In‐Kyu Lee
Journal of Diabetes Investigation.2021; 12(1): 21. CrossRef - Insulin resistance is mechanistically linked to hepatic mitochondrial remodeling in non-alcoholic fatty liver disease
Chris E. Shannon, Mukundan Ragavan, Juan Pablo Palavicini, Marcel Fourcaudot, Terry M Bakewell, Ivan A. Valdez, Iriscilla Ayala, Eunsook S. Jin, Muniswamy Madesh, Xianlin Han, Matthew E. Merritt, Luke Norton
Molecular Metabolism.2021; 45: 101154. CrossRef - Anti-Warburg Effect of Melatonin: A Proposed Mechanism to Explain its Inhibition of Multiple Diseases
Russel J. Reiter, Ramaswamy Sharma, Sergio Rosales-Corral
International Journal of Molecular Sciences.2021; 22(2): 764. CrossRef - Hyperpolarized magnetic resonance shows that the anti‐ischemic drug meldonium leads to increased flux through pyruvate dehydrogenase in vivo resulting in improved post‐ischemic function in the diabetic heart
Dragana Savic, Vicky Ball, Lorenz Holzner, David Hauton, Kerstin N. Timm, M. Kate Curtis, Lisa C. Heather, Damian J. Tyler
NMR in Biomedicine.2021;[Epub] CrossRef - Beyond the Warburg Effect: Oxidative and Glycolytic Phenotypes Coexist within the Metabolic Heterogeneity of Glioblastoma
Tomás Duraj, Noemí García-Romero, Josefa Carrión-Navarro, Rodrigo Madurga, Ana Ortiz de Mendivil, Ricardo Prat-Acin, Lina Garcia-Cañamaque, Angel Ayuso-Sacido
Cells.2021; 10(2): 202. CrossRef - Detailed evaluation of pyruvate dehydrogenase complex inhibition in simulated exercise conditions
Bodhi A. Jelinek, Michael A. Moxley
Biophysical Journal.2021; 120(5): 936. CrossRef - Proteomics Approach of Rapamycin Anti-Tumoral Effect on Primary and Metastatic Canine Mammary Tumor Cells In Vitro
Patrícia F. Lainetti, Antonio F. Leis-Filho, Priscila E. Kobayashi, Laíza S. de Camargo, Renee Laufer-Amorim, Carlos E. Fonseca-Alves, Fabiana F. Souza
Molecules.2021; 26(5): 1213. CrossRef - Remodeling of Cancer-Specific Metabolism under Hypoxia with Lactate Calcium Salt in Human Colorectal Cancer Cells
Keun-Yeong Jeong, Jae-Jun Sim, Min Hee Park, Hwan Mook Kim
Cancers.2021; 13(7): 1518. CrossRef - The Metabolic Fates of Pyruvate in Normal and Neoplastic Cells
Edward V. Prochownik, Huabo Wang
Cells.2021; 10(4): 762. CrossRef - The Multifaceted Roles of Zinc in Neuronal Mitochondrial Dysfunction
Hilary Y. Liu, Jenna R. Gale, Ian J. Reynolds, John H. Weiss, Elias Aizenman
Biomedicines.2021; 9(5): 489. CrossRef - Melatonin inhibits lung cancer development by reversing the Warburg effect via stimulating the SIRT3/PDH axis
Xiangyun Chen, Bingjie Hao, Dan Li, Russel J. Reiter, Yidong Bai, Baigenzhin Abay, Guojie Chen, Shumeng Lin, Tiansheng Zheng, Yanbei Ren, Xiao Xu, Ming Li, Lihong Fan
Journal of Pineal Research.2021;[Epub] CrossRef - Differential expression of pyruvate dehydrogenase E1A and its inactive phosphorylated form among breast cancer subtypes
Dana M. Zaher, Iman M. Talaat, Amal Hussein, Mahmood Y. Hachim, Hany A. Omar
Life Sciences.2021; 284: 119885. CrossRef - Structure of the native pyruvate dehydrogenase complex reveals the mechanism of substrate insertion
Jana Škerlová, Jens Berndtsson, Hendrik Nolte, Martin Ott, Pål Stenmark
Nature Communications.2021;[Epub] CrossRef - Melatonin: Regulation of Biomolecular Condensates in Neurodegenerative Disorders
Doris Loh, Russel J. Reiter
Antioxidants.2021; 10(9): 1483. CrossRef - Comprehensive Interrogation of Metabolic and Bioenergetic Responses of Early-Staged Zebrafish (Danio rerio) to a Commercial Copper Hydroxide Nanopesticide
Xiaohong Wang, Yingju Qin, Xiaoyu Li, Bing Yan, Christopher J. Martyniuk
Environmental Science & Technology.2021;[Epub] CrossRef - Conditional Knockout of Pdha1 in Mouse Hippocampus Impairs Cognitive Function: The Possible Involvement of Lactate
Wanxin Chen, Xiaoxia Sun, Libin Zhan, Wen Zhou, Tingting Bi
Frontiers in Neuroscience.2021;[Epub] CrossRef - Dihydrolipoamide dehydrogenase, pyruvate oxidation, and acetylation-dependent mechanisms intersecting drug iatrogenesis
I. F. Duarte, J. Caio, M. F. Moedas, L. A. Rodrigues, A. P. Leandro, I. A. Rivera, M. F. B. Silva
Cellular and Molecular Life Sciences.2021; 78(23): 7451. CrossRef - Advanced Bioinformatics Tools in the Pharmacokinetic Profiles of Natural and Synthetic Compounds with Anti-Diabetic Activity
Ana Maria Udrea, Gratiela Gradisteanu Pircalabioru, Anca Andreea Boboc, Catalina Mares, Andra Dinache, Maria Mernea, Speranta Avram
Biomolecules.2021; 11(11): 1692. CrossRef - Obesidade e infecção por SARS-CoV-2: papel da metainflamação
Ana Luísa Silva Albertoni, Luis Gustavo Silva Albertoni, Patricia Elaine de Almeida
HU Revista.2021; 46: 1. CrossRef - Influenza and obesity: its odd relationship and the lessons for COVID-19 pandemic
Livio Luzi, Maria Grazia Radaelli
Acta Diabetologica.2020; 57(6): 759. CrossRef - Acquisition of exogenous fatty acids renders apicoplast-based biosynthesis dispensable in tachyzoites of Toxoplasma
Xiaohan Liang, Jianmin Cui, Xuke Yang, Ningbo Xia, Yaqiong Li, Junlong Zhao, Nishith Gupta, Bang Shen
Journal of Biological Chemistry.2020; 295(22): 7743. CrossRef - Stimulation of glycolysis promotes cardiomyocyte proliferation after injury in adult zebrafish
Ryuichi Fukuda, Rubén Marín‐Juez, Hadil El‐Sammak, Arica Beisaw, Radhan Ramadass, Carsten Kuenne, Stefan Guenther, Anne Konzer, Aditya M Bhagwat, Johannes Graumann, Didier YR Stainier
EMBO reports.2020;[Epub] CrossRef - Fat mass affects nutritional status of ICU COVID-19 patients
Antonino De Lorenzo, Maria Grazia Tarsitano, Carmela Falcone, Laura Di Renzo, Lorenzo Romano, Sebastiano Macheda, Anna Ferrarelli, Demetrio Labate, Marco Tescione, Federico Bilotta, Paola Gualtieri
Journal of Translational Medicine.2020;[Epub] CrossRef - Conditional knockout of pyruvate dehydrogenase in mouse pancreatic β‑cells causes morphological and functional changes
Xiao Wang, Shuchang Lai, Yanshi Ye, Yuanyuan Hu, Daoyan Pan, Xiaochun Bai, Jie Shen
Molecular Medicine Reports.2020;[Epub] CrossRef - Beneficial Effects of Acetyl-DL-Leucine (ADLL) in a Mouse Model of Sandhoff Disease
Ecem Kaya, David A. Smith, Claire Smith, Barry Boland, Michael Strupp, Frances M. Platt
Journal of Clinical Medicine.2020; 9(4): 1050. CrossRef - Fetal circulating human resistin increases in diabetes during pregnancy and impairs placental mitochondrial biogenesis
Shaoning Jiang, April M. Teague, Jeanie B. Tryggestad, Timothy J. Lyons, Steven D. Chernausek
Molecular Medicine.2020;[Epub] CrossRef - SARS-CoV-2-host dynamics: Increased risk of adverse outcomes of COVID-19 in obesity
Rakhee Yadav, Sandeep Aggarwal, Archna Singh
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2020; 14(5): 1355. CrossRef - Effect of flaxseed oil on muscle protein loss and carbohydrate oxidation impairment in a pig model after lipopolysaccharide challenge
Ping Kang, Yang Wang, Xiangen Li, Zhicheng Wan, Xiuying Wang, Huiling Zhu, Chunwei Wang, Shengjun Zhao, Huifu Chen, Yulan Liu
British Journal of Nutrition.2020; 123(8): 859. CrossRef - Arrangement and symmetry of the fungal E3BP-containing core of the pyruvate dehydrogenase complex
B. O. Forsberg, S. Aibara, R. J. Howard, N. Mortezaei, E. Lindahl
Nature Communications.2020;[Epub] CrossRef - The potential impacts of obesity on COVID-19
Ahmed Abdalazim Dafallah Albashir
Clinical Medicine.2020; 20(4): e109. CrossRef - Selective dietary polyphenols induce differentiation of human osteoblasts by adiponectin receptor 1-mediated reprogramming of mitochondrial energy metabolism
Subhashis Pal, Konica Porwal, Sangam Rajak, Rohit A. Sinha, Naibedya Chattopadhyay
Biomedicine & Pharmacotherapy.2020; 127: 110207. CrossRef - Factors Associated with Increased Morbidity and Mortality of Obese and Overweight COVID-19 Patients
Amany Magdy Beshbishy, Helal F. Hetta, Diaa E. Hussein, Abdullah A. Saati, Christian C. Uba, Nallely Rivero-Perez, Adrian Zaragoza-Bastida, Muhammad Ajmal Shah, Tapan Behl, Gaber El-Saber Batiha
Biology.2020; 9(9): 280. CrossRef - Increased Glucose Availability Attenuates Myocardial Ketone Body Utilization
Manoja K. Brahma, Chae‐Myeong Ha, Mark E. Pepin, Sobuj Mia, Zhihuan Sun, John C. Chatham, Kirk M. Habegger, Evan Dale Abel, Andrew J. Paterson, Martin E. Young, Adam R. Wende
Journal of the American Heart Association.2020;[Epub] CrossRef - Stimulating pyruvate dehydrogenase complex reduces itaconate levels and enhances TCA cycle anabolic bioenergetics in acutely inflamed monocytes
Xuewei Zhu, David Long, Manal Zabalawi, Brian Ingram, Barbara K. Yoza, Peter W. Stacpoole, Charles E. McCall
Journal of Leukocyte Biology.2020; 107(3): 467. CrossRef - Short-term high-fat diet intake leads to exacerbation of concanavalin A-induced liver injury through the induction of procoagulation state
Eri Nanizawa, Yuki Tamaki, Reika Sono, Rintaro Miyashita, Yumi Hayashi, Ayumu Kanbe, Hiroyasu Ito, Tetsuya Ishikawa
Biochemistry and Biophysics Reports.2020; 22: 100736. CrossRef - Role of the Mitochondrial Pyruvate Carrier in the Occurrence of Metabolic Inflexibility in Drosophila melanogaster Exposed to Dietary Sucrose
Chloé J. Simard, Mohamed Touaibia, Eric Pierre Allain, Etienne Hebert-Chatelain, Nicolas Pichaud
Metabolites.2020; 10(10): 411. CrossRef - Metabolic shift underlies recovery in reversible infantile respiratory chain deficiency
Denisa Hathazi, Helen Griffin, Matthew J Jennings, Michele Giunta, Christopher Powell, Sarah F Pearce, Benjamin Munro, Wei Wei, Veronika Boczonadi, Joanna Poulton, Angela Pyle, Claudia Calabrese, Aurora Gomez‐Duran, Ulrike Schara, Robert D S Pitceathly, M
The EMBO Journal.2020;[Epub] CrossRef - Increased pyruvate dehydrogenase activity in skeletal muscle of growth-restricted ovine fetuses
Alexander L. Pendleton, Laurel R. Humphreys, Melissa A. Davis, Leticia E. Camacho, Miranda J. Anderson, Sean W. Limesand
American Journal of Physiology-Regulatory, Integrative and Comparative Physiology.2019; 317(4): R513. CrossRef - Recent advances in the pathogenesis of microvascular complications in diabetes
Sungmi Park, Hyeon-Ji Kang, Jae-Han Jeon, Min-Ji Kim, In-Kyu Lee
Archives of Pharmacal Research.2019; 42(3): 252. CrossRef - Secondary Metabolites of The Endophytic Fungus Alternaria alternata JS0515 Isolated from Vitex rotundifolia and Their Effects on Pyruvate Dehydrogenase activity
Changyeol Lee, Wei Li, Sunghee Bang, Sun Joo Lee, Nam-young Kang, Soonok Kim, Tae In Kim, Younghoon Go, Sang Hee Shim
Molecules.2019; 24(24): 4450. CrossRef - Adaptations in Protein Expression and Regulated Activity of Pyruvate Dehydrogenase Multienzyme Complex in Human Systolic Heart Failure
Freya L. Sheeran, Julie Angerosa, Norman Y. Liaw, Michael M. Cheung, Salvatore Pepe
Oxidative Medicine and Cellular Longevity.2019; 2019: 1. CrossRef - Progression of Multifaceted Immune Cells in Atherosclerotic Development
Sungmi Park, In-Kyu Lee
Journal of Lipid and Atherosclerosis.2019; 8(1): 15. CrossRef - SIRT3 elicited an anti‐Warburg effect through HIF1α/PDK1/PDHA1 to inhibit cholangiocarcinoma tumorigenesis
Lei Xu, Yang Li, Lixing Zhou, Robert Gregory Dorfman, Li Liu, Rui Cai, Chenfei Jiang, Dehua Tang, Yuming Wang, Xiaoping Zou, Lei Wang, Mingming Zhang
Cancer Medicine.2019; 8(5): 2380. CrossRef - Differential Mechanism of ATP Production Occurs in Response to Succinylacetone in Colon Cancer Cells
Lee, Woo, Yoo, Cho, Kim
Molecules.2019; 24(19): 3575. CrossRef - Myocardial Adaptation in Pseudohypoxia: Signaling and Regulation of mPTP via Mitochondrial Connexin 43 and Cardiolipin
Miroslav Ferko, Natália Andelová, Barbara Szeiffová Bačová, Magdaléna Jašová
Cells.2019; 8(11): 1449. CrossRef - NDUFAB1 protects against obesity and insulin resistance by enhancing mitochondrial metabolism
Rufeng Zhang, Tingting Hou, Heping Cheng, Xianhua Wang
The FASEB Journal.2019; 33(12): 13310. CrossRef - Mitochondrial Flexibility of Breast Cancers: A Growth Advantage and a Therapeutic Opportunity
Angelica Avagliano, Maria Rosaria Ruocco, Federica Aliotta, Immacolata Belviso, Antonello Accurso, Stefania Masone, Stefania Montagnani, Alessandro Arcucci
Cells.2019; 8(5): 401. CrossRef - Effects of intermittent hypoxia training on leukocyte pyruvate dehydrogenase kinase 1 (PDK-1) mRNA expression and blood insulin level in prediabetes patients
Tetiana V. Serebrovska, Alla G. Portnychenko, Vladimir I. Portnichenko, Lei Xi, Egor Egorov, Ivanna Antoniuk-Shcheglova, Svitlana Naskalova, Valeriy B. Shatylo
European Journal of Applied Physiology.2019; 119(3): 813. CrossRef
- Mitochondria dysfunction induced by decyl-TPP mitochondriotropic antioxidant based on caffeic acid AntiOxCIN6 sensitizes cisplatin lung anticancer therapy due to a remodeling of energy metabolism
- Complications
- Diagnosing Diabetic Neuropathy: Something Old, Something New
- Ioannis N. Petropoulos, Georgios Ponirakis, Adnan Khan, Hamad Almuhannadi, Hoda Gad, Rayaz A. Malik
- Diabetes Metab J. 2018;42(4):255-269. Published online August 21, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0056
- 8,227 View
- 116 Download
- 68 Web of Science
- 72 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader There are potentially many ways of assessing diabetic peripheral neuropathy (DPN). However, they do not fulfill U.S. Food and Drug Administration (FDA) requirements in relation to their capacity to assess therapeutic benefit in clinical trials of DPN. Over the past several decades symptoms and signs, quantitative sensory and electrodiagnostic testing have been strongly endorsed, but have consistently failed as surrogate end points in clinical trials. Therefore, there is an unmet need for reliable biomarkers to capture the onset and progression and to facilitate drug discovery in DPN. Corneal confocal microscopy (CCM) is a non-invasive ophthalmic imaging modality for
in vivo evaluation of sensory C-fibers. An increasing body of evidence from multiple centers worldwide suggests that CCM fulfills the FDA criteria as a surrogate endpoint of DPN.-
Citations
Citations to this article as recorded by- Painful Diabetic Neuropathy: The Need for New Approaches
Andrea M. Yeung, Jingtong Huang, Kevin T. Nguyen, Nicole Y. Xu, Lorenzo T. Hughes, Brajesh K. Agrawal, Niels Ejskjaer, David C. Klonoff
Journal of Diabetes Science and Technology.2024; 18(1): 159. CrossRef - COMMENT ON: Diabetic peripheral neuropathy is associated with diabetic kidney disease and cardiovascular disease: The silesia diabetes-heart project
Laksh Kumar, Syed Ali Arsal
Current Problems in Cardiology.2024; 49(4): 102227. CrossRef - Risk factors for peripheral artery disease and diabetic peripheral neuropathy among patients with type 2 diabetes
Tian Chen, Shengjue Xiao, Zhengdong Chen, Yiqing Yang, Bingquan Yang, Naifeng Liu
Diabetes Research and Clinical Practice.2024; 207: 111079. CrossRef - Laser-Induced Graphene-Based Smart Insole to Measure Plantar Temperature
Amith Khandakar, Md. Ahasan Atick Faisal, Muhammad E. H. Chowdhury, Mamun Bin Ibne Reaz, Sawal Hamid Md Ali, Mohd Ibrahim bin Shapiai Abd. Razak, Ahmad Ashrif A. Bakar, Sakib Mahmud, Rayaz A. Malik
IEEE Sensors Journal.2024; 24(2): 1190. CrossRef - Morphometry of the sural nerve in diabetic neuropathy: a systematic review
Zhang Ludi, Matthias Yi Quan Liau, Bryan Song Jun Yong, Amanda Sze Yen Auyong, Quah Hui Ting Lynette, Samuel Jianjie Yeo, Khin Swee Elizabeth Tan, Sreenivasulu Reddy Mogali, Ramya Chandrasekaran, Vivek Perumal, Ranganath Vallabhajosyula
Journal of Ultrasound.2024;[Epub] CrossRef - Understanding the Clinical Relationship Between Diabetic Retinopathy, Nephropathy, and Neuropathy: A Comprehensive Review
Aditi Kulkarni, Archana R Thool, Sachin Daigavane
Cureus.2024;[Epub] CrossRef - Development and validation of risk prediction model for diabetic neuropathy among diabetes mellitus patients at selected referral hospitals, in Amhara regional state Northwest Ethiopia, 2005–2021
Negalgn Byadgie Gelaw, Achenef Asmamaw Muche, Adugnaw Zeleke Alem, Nebiyu Bekele Gebi, Yazachew Moges Chekol, Tigabu Kidie Tesfie, Tsion Mulat Tebeje, Jacopo Sabbatinelli
PLOS ONE.2023; 18(8): e0276472. CrossRef - Biomarkers in diabetic neuropathy
Kaveri M. Adki, Yogesh A. Kulkarni
Archives of Physiology and Biochemistry.2023; 129(2): 460. CrossRef - Early detection and treatment device for diabetic foot neuropathy
Hunduma Tolossa Kumsa, Lelisa Getaneh Abdisa, Lelisa Tesema Tolessa, Sosina Ayele Wubneh, Wadajo Feyisa Kusa, Shimelis Nigusu Hordofa, Hundessa Daba Nemomssa
Irish Journal of Medical Science (1971 -).2023; 192(1): 143. CrossRef - Differences in motor unit behavior during isometric contractions in patients with diabetic peripheral neuropathy at various disease severities
Mateus André Favretto, Felipe Rettore Andreis, Sandra Cossul, Francesco Negro, Anderson Souza Oliveira, Jefferson Luiz Brum Marques
Journal of Electromyography and Kinesiology.2023; 68: 102725. CrossRef - Association of peripheral neuropathy with subclinical left ventricular dysfunction in patients with type 2 diabetes
Yanyan Chen, Yi Wang, Ying Zhang, Mengying Li, Weiqing Zhang, Yingni Zhou, Xiangyang Liu, Jianfang Fu, Zuowei Lu, Qian Xu, Tao Liu, Zeping Li, Xiaomiao Li, Jie Zhou
Journal of Diabetes and its Complications.2023; 37(2): 108406. CrossRef - Quantifying gait intralimb coordination patterns in individuals with different levels of diabetic neuropathy: a vector coding analysis
Michelle Bazilio Milan, Guilherme Augusto Gomes De Villa, Eneida Yuri Suda, Isabel de Camargo Neves Sacco, Marcus Fraga Vieira
Research on Biomedical Engineering.2023; 39(1): 311. CrossRef - Mechanisms underlying altered neuromuscular function in people with DPN
Antonin Le Corre, Nathan Caron, Nicolas A. Turpin, Georges Dalleau
European Journal of Applied Physiology.2023; 123(7): 1433. CrossRef - Peripheral Neuropathy in Diabetes Mellitus: Pathogenetic Mechanisms and Diagnostic Options
Raffaele Galiero, Alfredo Caturano, Erica Vetrano, Domenico Beccia, Chiara Brin, Maria Alfano, Jessica Di Salvo, Raffaella Epifani, Alessia Piacevole, Giuseppina Tagliaferri, Maria Rocco, Ilaria Iadicicco, Giovanni Docimo, Luca Rinaldi, Celestino Sardu, T
International Journal of Molecular Sciences.2023; 24(4): 3554. CrossRef - Nerve conduction velocity is independently associated with bone mineral density in type 2 diabetes mellitus
Xiao-jing Chen, Xiao-feng Wang, Zheng-can Pan, Deng Zhang, Ke-cheng Zhu, Tao Jiang, Xiao-ke Kong, Rui Xie, Li-hao Sun, Bei Tao, Jian-min Liu, Hong-yan Zhao
Frontiers in Endocrinology.2023;[Epub] CrossRef - Precision of Michigan Neuropathy Screening Instrument (MNSI) Tool for the Diagnosis of Diabetic Peripheral Neuropathy Among People with Type 2 Diabetes—A Study from South India
Vijay Viswanathan, Balkhiwala Ahmed Khan, Sukanya Nachimuthu, Satyavani Kumpatla
The International Journal of Lower Extremity Wounds.2023; : 153473462311632. CrossRef - Ankle Fractures in Diabetic Patients
Ellen M. Goldberg, William S. Polachek, Kelly Hynes
JBJS Reviews.2023;[Epub] CrossRef - Comparing the Ipswich Touch Test (IpTT) and 10gm-SMWF (10-gm Semmes–Weinstein mono-filament) in Indian population subset with type 2 diabetes mellitus to detect diabetes neuropathy
Sivasubramaniyam Senthilkumar, Ramesh Dasarathan, Pushkar Pazhani, Archana Gaur, Varatharajan Sakthivadivel
Irish Journal of Medical Science (1971 -).2023; 192(6): 2793. CrossRef - Diabetic neuropathy: Pathogenesis and evolving principles of management
Basem Zaino, Rashika Goel, Sanjana Devaragudi, Ananya Prakash, Yogeshkumar Vaghamashi, Yashendra Sethi, Neil Patel, Nirja Kaka
Disease-a-Month.2023; 69(9): 101582. CrossRef - Association between Diabetic Peripheral Neuropathy as Measured Using a Point-of-Care Sural Nerve Conduction Device and Urinary Albumin Excretion in Patients with Type 2 Diabetes
Tatsuya Fukuda, Akiko Fujii, Taro Akihisa, Naoya Otsubo, Masanori Murakami, Tetsuya Yamada, Chisato Maki
Journal of Clinical Medicine.2023; 12(12): 4089. CrossRef - Sudomotor dysfunction in diabetic peripheral neuropathy (DPN) and its testing modalities: A literature review
Muhammad Akbar, Alvian Wandy, Gita Vita Soraya, Yudy Goysal, Mimi Lotisna, Muhammad Iqbal Basri
Heliyon.2023; 9(7): e18184. CrossRef - Novel insights into the nervous system affected by prolonged hyperglycemia
Kamila Zglejc-Waszak, Konark Mukherjee, Agnieszka Korytko, Bogdan Lewczuk, Andrzej Pomianowski, Joanna Wojtkiewicz, Marta Banach, Michał Załęcki, Natalia Nowicka, Julia Jarosławska, Bernard Kordas, Krzysztof Wąsowicz, Judyta K. Juranek
Journal of Molecular Medicine.2023; 101(8): 1015. CrossRef - (Pre)diabetes and a higher level of glycaemic measures are continuously associated with corneal neurodegeneration assessed by corneal confocal microscopy: the Maastricht Study
Sara B. A. Mokhtar, Frank C. T. van der Heide, Karel A. M. Oyaert, Carla J. H. van der Kallen, Tos T. J. M. Berendschot, Fabio Scarpa, Alessia Colonna, Bastiaan E. de Galan, Marleen M. J. van Greevenbroek, Pieter C. Dagnelie, Casper G. Schalkwijk, Rudy M.
Diabetologia.2023; 66(11): 2030. CrossRef - Potential Retinal Biomarkers in Alzheimer’s Disease
Mariana Yolotzin García-Bermúdez, Rupali Vohra, Kristine Freude, Peter van Wijngaarden, Keith Martin, Maj Schneider Thomsen, Blanca Irene Aldana, Miriam Kolko
International Journal of Molecular Sciences.2023; 24(21): 15834. CrossRef - The effect of polyneuropathy severity on nerve conduction and pain syndrome in patients with type 2 diabetes
A.Ya. Sabovchyk, M.M. Oros
INTERNATIONAL NEUROLOGICAL JOURNAL.2023; 19(6): 161. CrossRef - Artificial intelligence utilising corneal confocal microscopy for the diagnosis of peripheral neuropathy in diabetes mellitus and prediabetes
Frank G. Preston, Yanda Meng, Jamie Burgess, Maryam Ferdousi, Shazli Azmi, Ioannis N. Petropoulos, Stephen Kaye, Rayaz A. Malik, Yalin Zheng, Uazman Alam
Diabetologia.2022; 65(3): 457. CrossRef - 10.6-μm infrared laser as adjuvant therapy for diabetic peripheral neuropathy: study protocol for a double-blind, randomized controlled trial
Lin Lin, Yi Chen, Yuxia Li, Ke Cheng, Haiping Deng, Jianping Lu, Ling Zhao, Xueyong Shen
Trials.2022;[Epub] CrossRef - Diabetic corneal neuropathy as a surrogate marker for diabetic peripheral neuropathy
WeiZheng So, NatalieShi Qi Wong, HongChang Tan, MollyTzu Yu Lin, IsabelleXin Yu Lee, JodhbirS Mehta, Yu-Chi Liu
Neural Regeneration Research.2022; 17(10): 2172. CrossRef - SUDOSCAN in Combination with the Michigan Neuropathy Screening Instrument Is an Effective Tool for Screening Diabetic Peripheral Neuropathy
Tae Jung Oh, Yoojung Song, Hak Chul Jang, Sung Hee Choi
Diabetes & Metabolism Journal.2022; 46(2): 319. CrossRef - Performance Analysis of Conventional Machine Learning Algorithms for Diabetic Sensorimotor Polyneuropathy Severity Classification Using Nerve Conduction Studies
Fahmida Haque, Mamun B. I. Reaz, Muhammad E. H. Chowdhury, Serkan Kiranyaz, Sawal H. M. Ali, Mohammed Alhatou, Rumana Habib, Ahmad A. A. Bakar, Norhana Arsad, Geetika Srivastava, Paolo Crippa
Computational Intelligence and Neuroscience.2022; 2022: 1. CrossRef - The Presence of Clonal Hematopoiesis Is Negatively Associated with Diabetic Peripheral Neuropathy in Type 2 Diabetes
Tae Jung Oh, Han Song, Youngil Koh, Sung Hee Choi
Endocrinology and Metabolism.2022; 37(2): 243. CrossRef - An overview of painful diabetic peripheral neuropathy: Diagnosis and treatment advancements
Jonathan M. Hagedorn, Alyson M. Engle, Tony K. George, Jay Karri, Newaj Abdullah, Erik Ovrom, Jhon E. Bocanegra-Becerra, Ryan S. D'Souza
Diabetes Research and Clinical Practice.2022; 188: 109928. CrossRef - Prevalence and risk of diabetic complications in young-onset versus late-onset type 2 diabetes mellitus
Yongin Cho, Hye-Sun Park, Byung Wook Huh, Seong Ha Seo, Da Hea Seo, Seong Hee Ahn, Seongbin Hong, Young Ju Suh, So Hun Kim
Diabetes & Metabolism.2022; 48(6): 101389. CrossRef - Artificial Intelligence and Corneal Confocal Microscopy: The Start of a Beautiful Relationship
Uazman Alam, Matthew Anson, Yanda Meng, Frank Preston, Varo Kirthi, Timothy L. Jackson, Paul Nderitu, Daniel J. Cuthbertson, Rayaz A. Malik, Yalin Zheng, Ioannis N. Petropoulos
Journal of Clinical Medicine.2022; 11(20): 6199. CrossRef - INvesTigating the Abnormality of detrusor ConTractility by uroflowmetry in diabetic children (INTACT Trial): protocol of a prospective, observational study
Ágnes Rita Martonosi, Piroska Pázmány, Szabolcs Kiss, Annamária Zsákai, László Szabó
BMJ Open.2022; 12(11): e062198. CrossRef - Diabetic foot ulcers: A devastating complication of diabetes mellitus continues non-stop in spite of new medical treatment modalities
Gamze Akkus, Murat Sert
World Journal of Diabetes.2022; 13(12): 1106. CrossRef - Corneal nerves in diabetes—The role of the in vivo corneal confocal microscopy of the subbasal nerve plexus in the assessment of peripheral small fiber neuropathy
Anna M. Roszkowska, Carmelo Licitra, Giuseppe Tumminello, Elisa I. Postorino, Michele R. Colonna, Pasquale Aragona
Survey of Ophthalmology.2021; 66(3): 493. CrossRef - Association between Sleep Quality and Painless Diabetic Peripheral Neuropathy Assessed by Current Perception Threshold in Type 2 Diabetes Mellitus
Dughyun Choi, Bo-Yeon Kim, Chan-Hee Jung, Chul-Hee Kim, Ji-Oh Mok
Diabetes & Metabolism Journal.2021; 45(3): 358. CrossRef - Glycaemic control for painful diabetic peripheral neuropathy is more than fasting plasma glucose and glycated haemoglobin
Y.-W. Pai, C.-L. Tang, C.-H. Lin, S.-Y. Lin, I.-T. Lee, M.-H. Chang
Diabetes & Metabolism.2021; 47(1): 101158. CrossRef - Diagnosis of Neuropathy and Risk Factors for Corneal Nerve Loss in Type 1 and Type 2 Diabetes: A Corneal Confocal Microscopy Study
Maryam Ferdousi, Alise Kalteniece, Shazli Azmi, Ioannis N. Petropoulos, Georgios Ponirakis, Uazman Alam, Omar Asghar, Andrew Marshall, Catherine Fullwood, Maria Jeziorska, Caroline Abbott, Giuseppe Lauria, Catharina G. Faber, Handrean Soran, Nathan Efron,
Diabetes Care.2021; 44(1): 150. CrossRef - Widespread sensory neuropathy in diabetic patients hospitalized with severe COVID-19 infection
Ariel Odriozola, Lucía Ortega, Lidia Martinez, Samantha Odriozola, Ainhoa Torrens, David Corroleu, Silvia Martínez, Meritxell Ponce, Yolanda Meije, Mercedes Presas, Alejandra Duarte, M. Belén Odriozola, Rayaz A. Malik
Diabetes Research and Clinical Practice.2021; 172: 108631. CrossRef - Lost in Translation? Measuring Diabetic Neuropathy in Humans and Animals
Heung Yong Jin, Seong-Su Moon, Nigel A. Calcutt
Diabetes & Metabolism Journal.2021; 45(1): 27. CrossRef - Early Detection of Diabetic Peripheral Neuropathy: A Focus on Small Nerve Fibres
Jamie Burgess, Bernhard Frank, Andrew Marshall, Rashaad S. Khalil, Georgios Ponirakis, Ioannis N. Petropoulos, Daniel J. Cuthbertson, Rayaz A. Malik, Uazman Alam
Diagnostics.2021; 11(2): 165. CrossRef - Role of interdigital sensory nerve conduction study as a noninvasive approach for early diagnosis of diabetic peripheral neuropathy
Hamid R. Fateh, Seyed Pezhman Madani
Journal of Diabetes & Metabolic Disorders.2021; 20(1): 71. CrossRef - Performance Analysis of Conventional Machine Learning Algorithms for Diabetic Sensorimotor Polyneuropathy Severity Classification
Fahmida Haque, Mamun Bin Ibne Reaz, Muhammad Enamul Hoque Chowdhury, Geetika Srivastava, Sawal Hamid Md Ali, Ahmad Ashrif A. Bakar, Mohammad Arif Sobhan Bhuiyan
Diagnostics.2021; 11(5): 801. CrossRef - Advances in Screening, Early Diagnosis and Accurate Staging of Diabetic Neuropathy
Josie Carmichael, Hassan Fadavi, Fukashi Ishibashi, Angela C. Shore, Mitra Tavakoli
Frontiers in Endocrinology.2021;[Epub] CrossRef - Vibration Perception Threshold and Related Factors for Balance Assessment in Patients with Type 2 Diabetes Mellitus
Jisang Jung, Min-Gyu Kim, Youn-Joo Kang, Kyungwan Min, Kyung-Ah Han, Hyoseon Choi
International Journal of Environmental Research and Public Health.2021; 18(11): 6046. CrossRef - Diabetic Peripheral Neuropathy Affects Pinch Strength and Hand Dexterity in Elderly Patients
Qi Zhang, Yifang Lin, Xinhua Liu, Li Zhang, Yan Zhang, Dong Zhao, Qi Lu, Jie Jia, Jia-Jia Wu
Neural Plasticity.2021; 2021: 1. CrossRef - Association of Combined TCF7L2 and KCNQ1 Gene Polymorphisms with Diabetic Micro- and Macrovascular Complications in Type 2 Diabetes Mellitus
Rujikorn Rattanatham, Nongnuch Settasatian, Nantarat Komanasin, Upa Kukongviriyapan, Kittisak Sawanyawisuth, Phongsak Intharaphet, Vichai Senthong, Chatri Settasatian
Diabetes & Metabolism Journal.2021; 45(4): 578. CrossRef - Neuropeptide Y: a potential theranostic biomarker for diabetic peripheral neuropathy in patients with type-2 diabetes
Noo Ree Cho, Yeuni Yu, Chang-Kyu Oh, Dai Sik Ko, Kyungjae Myung, Yoonsung Lee, Hee Sam Na, Yun Hak Kim
Therapeutic Advances in Chronic Disease.2021; 12: 204062232110419. CrossRef - Prediction of Diabetic Sensorimotor Polyneuropathy Using Machine Learning Techniques
Dae Youp Shin, Bora Lee, Won Sang Yoo, Joo Won Park, Jung Keun Hyun
Journal of Clinical Medicine.2021; 10(19): 4576. CrossRef - Reduced association between dendritic cells and corneal sub‐basal nerve fibers in patients with fibromyalgia syndrome
Alexander Klitsch, Dimitar Evdokimov, Johanna Frank, Dominique Thomas, Nadine Saffer, Caren Meyer zu Altenschildesche, Marco Sisignano, Daniel Kampik, Rayaz A. Malik, Claudia Sommer, Nurcan Üçeyler
Journal of the Peripheral Nervous System.2020; 25(1): 9. CrossRef - Diet-Induced Rodent Models of Diabetic Peripheral Neuropathy, Retinopathy and Nephropathy
Inês Preguiça, André Alves, Sara Nunes, Pedro Gomes, Rosa Fernandes, Sofia D. Viana, Flávio Reis
Nutrients.2020; 12(1): 250. CrossRef - Diabetic Distal Symmetrical Polyneuropathy: Correlation of Clinical, Laboratory, and Electrophysiologic Studies in Patients with Type 2 Diabetes Mellitus
Yi-Ching Weng, Sung-Sheng Tsai, Rong-Kuo Lyu, Chun-Che Chu, Long-Sun Ro, Ming-Feng Liao, Hong-Shiu Chang, Chiung-Mei Chen, Jawl-Shan Hwang, Hung-Chou Kuo
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Diabetic Peripheral Neuropathy: Is it Underdiagnosed?
Rizaldy T. Pinzon, M. Kes, Rosa De Lima R. Sa
Asian Journal of Biological Sciences.2020; 13(2): 168. CrossRef - Deterioration of Sleep Quality According to Glycemic Status
Myung Haeng Hur, Mi-Kyoung Lee, Kayeon Seong, Jun Hwa Hong
Diabetes & Metabolism Journal.2020; 44(5): 679. CrossRef - Microvascular Complications of Type 2 Diabetes Mellitus
Charles Faselis, Alexandra Katsimardou, Konstantinos Imprialos, Pavlos Deligkaris, Manolis Kallistratos, Kiriakos Dimitriadis
Current Vascular Pharmacology.2020; 18(2): 117. CrossRef - Computational methods for automated analysis of corneal nerve images: Lessons learned from retinal fundus image analysis
Tooba Salahuddin, Uvais Qidwai
Computers in Biology and Medicine.2020; 119: 103666. CrossRef - TIR generated by continuous glucose monitoring is associated with peripheral nerve function in type 2 diabetes
Fengwen Li, Yinan Zhang, Huizhi Li, Jingyi Lu, Lan Jiang, Robert A. Vigersky, Jian Zhou, Congrong Wang, Yuqian Bao, Weiping Jia
Diabetes Research and Clinical Practice.2020; 166: 108289. CrossRef - A Phase 2 Clinical Trial on the Use of Cibinetide for the Treatment of Diabetic Macular Edema
Noemi Lois, Evie Gardner, Margaret McFarland, David Armstrong, Christine McNally, Nuala Jane Lavery, Christina Campbell, Rita I Kirk, Daiva Bajorunas, Ann Dunne, Anthony Cerami, Michael Brines
Journal of Clinical Medicine.2020; 9(7): 2225. CrossRef - Diabetic neuropathy and neuropathic pain: a (con)fusion of pathogenic mechanisms?
Nigel A. Calcutt
Pain.2020; 161(Supplement): S65. CrossRef - Lumos for the long trail: Strategies for clinical diagnosis and severity staging for diabetic polyneuropathy and future directions
Tatsuhito Himeno, Hideki Kamiya, Jiro Nakamura
Journal of Diabetes Investigation.2020; 11(1): 5. CrossRef - Corneal confocal microscopy detects small nerve fibre damage in patients with painful diabetic neuropathy
Alise Kalteniece, Maryam Ferdousi, Shazli Azmi, Womba M. Mubita, Andrew Marshall, Giuseppe Lauria, Catharina G. Faber, Handrean Soran, Rayaz A. Malik
Scientific Reports.2020;[Epub] CrossRef - The Association of Fasting C-peptide with Corneal Neuropathy in Patients with Type 2 Diabetes
Anju Zuo, Chuan Wang, Lili Li, Jingru Qu, Juan Cao, Li Chen, Solomon Tesfaye, Wenjuan Li, Xinguo Hou, Vincenza Spallone
Journal of Diabetes Research.2020; 2020: 1. CrossRef - Performance analysis of noninvasive electrophysiological methods for the assessment of diabetic sensorimotor polyneuropathy in clinical research: a systematic review and meta-analysis with trial sequential analysis
Fahmida Haque, Mamun Bin Ibne Reaz, Sawal Hamid Md Ali, Norhana Arsad, Muhammad Enamul Hoque Chowdhury
Scientific Reports.2020;[Epub] CrossRef - Tear film substance P: A potential biomarker for diabetic peripheral neuropathy
Shyam Sunder Tummanapalli, Mark D.P. Willcox, Tushar Issar, Aimy Yan, Jana Pisarcikova, Natalie Kwai, Ann M. Poynten, Arun V. Krishnan, Maria Markoulli
The Ocular Surface.2019; 17(4): 690. CrossRef - Characterizing distal peripheral neuropathy in type 2 diabetes mellitus in a semi-urban community setting in Peru
Meera F Iyengar, Antonio Bernabe-Ortiz
Journal of Global Health Reports.2019;[Epub] CrossRef - Diabetic peripheral neuropathy: advances in diagnosis and strategies for screening and early intervention
Dinesh Selvarajah, Debasish Kar, Kamlesh Khunti, Melanie J Davies, Adrian R Scott, Jeremy Walker, Solomon Tesfaye
The Lancet Diabetes & Endocrinology.2019; 7(12): 938. CrossRef - Diabetic Peripheral Neuropathy as a Risk Factor for Sarcopenia
Tae Jung Oh, Yoojung Song, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
Annals of Geriatric Medicine and Research.2019; 23(4): 170. CrossRef - Diabetic Neuropathy: New Insights to Early Diagnosis and Treatments
Mark Yorek, Rayaz A. Malik, Nigel A. Calcutt, Aaron Vinik, Soroku Yagihashi
Journal of Diabetes Research.2018; 2018: 1. CrossRef - Use of parenteral vitamin B complexes in treatment of polyneuropathy
O. V. Kurushina, A. E. Barulin, O. I. Agarkova
Medical Council.2018; (18): 62. CrossRef - Circulating microRNAs as biomarkers for diabetic neuropathy: A novel approach
Eleni Xourgia, Athanasia Papazafiropoulou, Andreas Melidonis
World Journal of Experimental Medicine.2018; 8(3): 18. CrossRef
- Painful Diabetic Neuropathy: The Need for New Approaches
- Epidemiology
- The Evidence for an Obesity Paradox in Type 2 Diabetes Mellitus
- Seung Jin Han, Edward J. Boyko
- Diabetes Metab J. 2018;42(3):179-187. Published online May 31, 2018
- DOI: https://doi.org/10.4093/dmj.2018.0055
- 6,274 View
- 122 Download
- 61 Web of Science
- 61 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Although overweight/obesity is a major risk factor for the development of type 2 diabetes mellitus, there is increasing evidence that overweight or obese patients with type 2 diabetes mellitus experience lower mortality compared with patients of normal weight. This paradoxical finding, known as the “obesity paradox,” occurs in other chronic diseases, and in type 2 diabetes mellitus is particularly perplexing given that lifestyle intervention with one goal being weight reduction is an important feature of the management of this condition. We summarize in this review the findings from clinical and epidemiologic studies that have investigated the association between overweight and obesity (usually assessed using body mass index [BMI]) and mortality in type 2 diabetes mellitus and discuss potential causes of the obesity paradox. We conclude that most studies show evidence of an obesity paradox, but important conflicting findings still exist. We also evaluate if potential bias might explain the obesity paradox in diabetes, including, for example, the presence of confounding factors, measurement error due to use of BMI as an index of obesity, and reverse causation.
-
Citations
Citations to this article as recorded by- Association between the weight-adjusted waist index and the odds of type 2 diabetes mellitus in United States adults: a cross-sectional study
Dongdong Zheng, Suzhen Zhao, Dan Luo, Feng Lu, Zhishen Ruan, Xiaokang Dong, Wenjing Chen
Frontiers in Endocrinology.2024;[Epub] CrossRef - Racial and ethnic disparities in primary prevention of cardiovascular disease
Mohammad R. Ali, Hadjer Nacer, Claire A. Lawson, Kamlesh Khunti
Canadian Journal of Cardiology.2024;[Epub] CrossRef - Independent and interactive associations of heart rate and obesity with type 2 diabetes mellites: A population‐based study
Tianxin Zhu, Qingyu Chen, Hongxing Chen, Lili You, Dan Liu, Xiaoyun Zhang, Feng Li, Hongshi Wu, Juying Tang, Diaozhu Lin, Kan Sun, Li Yan, Meng Ren
Journal of Diabetes.2024;[Epub] CrossRef - Two‐sided roles of adipose tissue: Rethinking the obesity paradox in various human diseases from a new perspective
Jing Pan, Jianqiong Yin, Lu Gan, Jianxin Xue
Obesity Reviews.2023;[Epub] CrossRef - Lean or diabetic subtypes predict increased all-cause and disease-specific mortality in metabolic-associated fatty liver disease
Goh Eun Chung, Su Jong Yu, Jeong-Ju Yoo, Yuri Cho, Kyu-na Lee, Dong Wook Shin, Donghee Kim, Yoon Jun Kim, Jung-Hwan Yoon, Kyungdo Han, Eun Ju Cho
BMC Medicine.2023;[Epub] CrossRef - Dynamic changes in prevalence of type 2 diabetes along with associated factors in Bangladesh: Evidence from two national cross-sectional surveys (BDHS 2011 and BDHS 2017–18)
Sabiha Shirin Sara, Ashis Talukder, Ka Yiu Lee, Nayan Basak, Shaharior Rahman Razu, Iqramul Haq, Chuton Deb Nath
Diabetes & Metabolic Syndrome: Clinical Research & Reviews.2023; 17(2): 102706. CrossRef - Association of dietary intake with body mass index and glycemic profile among newly diagnosed patients with type 2 diabetes mellitus
Keddagoda Gamage Piyumi Wasana, Anoja Priyadarshani Attanayake, Thilak Priyantha Weerarathna, Devpura Arachchige Bandumalee Nimalshanthi Amarasekera, Kamani Ayoma Perera Wijewardana Jayatilaka
American Journal of Human Biology.2023;[Epub] CrossRef - Can lipophilic pollutants in adipose tissue explain weight change‐related risk in type 2 diabetes mellitus?
Duk‐Hee Lee, In‐Kyu Lee
Journal of Diabetes Investigation.2023; 14(4): 528. CrossRef - Visceral fat and attribute-based medicine in chronic kidney disease
Hiroshi Kataoka, Kosaku Nitta, Junichi Hoshino
Frontiers in Endocrinology.2023;[Epub] CrossRef - A primary care delivered, technology supported lifestyle program for Type 2 Diabetes Management: An evaluation of changes in metabolic health, feasibility, and acceptability – A pilot interventional study protocol
Pennie J. Taylor, Campbell H. Thompson, Thomas P. Wycherley, Grant D. Brinkworth
Contemporary Clinical Trials Communications.2023; 33: 101152. CrossRef - The medical model of “obesity” and the values behind the guise of health
Kayla R. Mehl
Synthese.2023;[Epub] CrossRef - Elevated MMP-8 levels, inversely associated with BMI, predict mortality in mechanically ventilated patients: an observational multicenter study
Hang Ruan, Shu-sheng Li, Qin Zhang, Xiao Ran
Critical Care.2023;[Epub] CrossRef - Obesity and 30-day case fatality after hyperglycemic crisis hospitalizations in Korea: a national cohort study
Hojun Yoon, Hyun Ho Choi, Giwoong Choi, Sun Ok Song, Kyoung Hwa Ha, Dae Jung Kim
Cardiovascular Prevention and Pharmacotherapy.2023; 5(3): 74. CrossRef - Normal‐weight central obesity and risk of cardiovascular and microvascular events in adults with prediabetes or diabetes: Chinese and British cohorts
Pingting Zhong, Shaoying Tan, Zhuoting Zhu, Ziyu Zhu, Yi Liang, Wenyong Huang, Wei Wang
Diabetes/Metabolism Research and Reviews.2023;[Epub] CrossRef - Overweight and obesity are associated with better survival in STEMI patients with diabetes
Hamza Chaudhry, Ramez Bodair, Ziyad Mahfoud, Soha Dargham, Jassim Al Suwaidi, Hani Jneid, Charbel Abi Khalil
Obesity.2023; 31(11): 2834. CrossRef - Influence of diabetes and obesity on ten-year outcomes after coronary artery bypass grafting in the arterial revascularisation trial
Maria Stefil, Mario Gaudino, Umberto Benedetto, Stephen Gerry, Alastair Gray, Belinda Lees, Bruno Podesser, Lukasz Krzych, Lokeswara Rao Sajja, David Taggart, Marcus Flather
Clinical Research in Cardiology.2023;[Epub] CrossRef - Poor glycaemic control: prevalence, factors and implications for the care of patients with type 2 diabetes in Kinshasa, Democratic Republic of the Congo: a cross-sectional study
Jean-Pierre Fina Lubaki, Olufemi Babatunde Omole, Joel Msafiri Francis
Frontiers in Clinical Diabetes and Healthcare.2023;[Epub] CrossRef - Comparison of obesity indices and triglyceride glucose-related parameters to predict type 2 diabetes mellitus among normal-weight elderly in China
Pan Ke, Xia Wu, Minzhi Xu, Jie Feng, Hongbin Xu, Yong Gan, Chao Wang, Zhenyu Deng, Xiang Liu, Wenning Fu, Qingfeng Tian, Yan He, Lirong Zhong, Heng Jiang, Zuxun Lu
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity.2022; 27(3): 1181. CrossRef - Association Between Obesity and Cardiovascular Disease in Elderly Patients With Diabetes: A Retrospective Cohort Study
Sangmo Hong, Jung Hwan Park, Kyungdo Han, Chang Beom Lee, Dong Sun Kim, Sung Hoon Yu
The Journal of Clinical Endocrinology & Metabolism.2022; 107(2): e515. CrossRef - The Relationship between the Lipid Accumulation Product and Beta-cell Function in Korean Adults with or without Type 2 Diabetes Mellitus: The 2015 Korea National Health and Nutrition Examination Survey
Hye Eun Cho, Seung Bum Yang, Mi Young Gi, Ju Ae Cha, so Young Park, Hyun Yoon
Endocrine Research.2022; 47(2): 80. CrossRef - Body mass index and all-cause mortality in patients with newly diagnosed type 2 diabetes mellitus in South Korea: a retrospective cohort study
Jae-Seok Hong, Hee-Chung Kang
BMJ Open.2022; 12(4): e048784. CrossRef - Social determinants of obesity in American Indian and Alaska Native peoples aged ≥ 50 years
R Turner Goins, Cheryl Conway, Margaret Reid, Luohua Jiang, Jenny Chang, Kimberly R Huyser, Angela G Brega, John F Steiner, Amber L Fyfe-Johnson, Michelle Johnson-Jennings, Vanessa Hiratsuka, Spero M Manson, Joan O’Connell
Public Health Nutrition.2022; 25(8): 2064. CrossRef - Cardiorespiratory Fitness, BMI, Mortality, and Cardiovascular Disease in Adults with Overweight/Obesity and Type 2 Diabetes
ANDREW C. WILLS, ELSA VAZQUEZ ARREOLA, MUIDEEN T. OLAIYA, JEFFREY M. CURTIS, MARGARETA I. HELLGREN, ROBERT L. HANSON, WILLIAM C. KNOWLER
Medicine & Science in Sports & Exercise.2022; 54(6): 994. CrossRef - Spline Longitudinal Multi-response Model for the Detection of Lifestyle-
Based Changes in Blood Glucose of Diabetic Patients
Anna Islamiyati
Current Diabetes Reviews.2022;[Epub] CrossRef - The obesity paradox: Retinopathy, obesity, and circulating risk markers in youth with type 2 diabetes in the TODAY Study
Lynne L. Levitsky, Kimberly L. Drews, Morey Haymond, Rose A. Glubitosi-Klug, Lorraine E. Levitt Katz, Mihai Mititelu, William Tamborlane, Jeanie B. Tryggestad, Ruth S. Weinstock
Journal of Diabetes and its Complications.2022; 36(11): 108259. CrossRef - Distribution of lean mass and mortality risk in patients with type 2 diabetes
Li Ding, Yuxin Fan, Jingting Qiao, Jing He, Ruodan Wang, Qing He, Jingqiu Cui, Zhongshu Ma, Fangqiu Zheng, Hua Gao, Chenlin Dai, Hongyan Wei, Jun Li, Yuming Cao, Gang Hu, Ming Liu
Primary Care Diabetes.2022; 16(6): 824. CrossRef - Current Knowledge on the Pathophysiology of Lean/Normal-Weight Type 2 Diabetes
Teresa Salvatore, Raffaele Galiero, Alfredo Caturano, Luca Rinaldi, Livio Criscuolo, Anna Di Martino, Gaetana Albanese, Erica Vetrano, Christian Catalini, Celestino Sardu, Giovanni Docimo, Raffaele Marfella, Ferdinando Carlo Sasso
International Journal of Molecular Sciences.2022; 24(1): 658. CrossRef - The obesity paradox and diabetes
Giovanni Gravina, Federica Ferrari, Grazia Nebbiai
Eating and Weight Disorders - Studies on Anorexia, Bulimia and Obesity.2021; 26(4): 1057. CrossRef - Implicating the effect of ketogenic diet as a preventive measure to obesity and diabetes mellitus
Sachin Kumar, Tapan Behl, Monika Sachdeva, Aayush Sehgal, Shilpa Kumari, Arun Kumar, Gagandeep Kaur, Harlokesh Narayan Yadav, Simona Bungau
Life Sciences.2021; 264: 118661. CrossRef - Diagnosis of obesity based on body composition‐associated health risks—Time for a change in paradigm
Anja Bosy‐Westphal, Manfred J. Müller
Obesity Reviews.2021;[Epub] CrossRef - Body mass index and clinical outcomes in patients with intracerebral haemorrhage: results from the China Stroke Center Alliance
Zhentang Cao, Xinmin Liu, Zixiao Li, Hongqiu Gu, Yingyu Jiang, Xingquan Zhao, Yongjun Wang
Stroke and Vascular Neurology.2021; 6(3): 424. CrossRef - Obesity and Overweight Are Associated with Minimal Extrathyroidal Extension, Multifocality and Bilaterality of Papillary Thyroid Cancer
Krzysztof Kaliszewski, Dorota Diakowska, Marta Rzeszutko, Jerzy Rudnicki
Journal of Clinical Medicine.2021; 10(5): 970. CrossRef - Obesity paradox in patients with cardiovascular diseases and diabetes mellitus type 2 (analytical review)
Margarita P. Zaikina, Valentina A. Kapustina, Stanislav I. Savel'ev
HEALTH CARE OF THE RUSSIAN FEDERATION.2021; 65(2): 135. CrossRef - Risk factors for adverse outcomes among 35 879 veterans with and without diabetes after diagnosis with COVID-19
Pandora L Wander, Elliott Lowy, Lauren A Beste, Luis Tulloch-Palomino, Anna Korpak, Alexander C Peterson, Bessie A Young, Edward J Boyko
BMJ Open Diabetes Research & Care.2021; 9(1): e002252. CrossRef - Obesity and glycemic control among people with type 2 diabetes in the United States: A retrospective cohort study using insurance claims data
Kristina S. Boye, Maureen J. Lage, Vivian Thieu, Shraddha Shinde, Shivanie Dhamija, Jay Patrick Bae
Journal of Diabetes and its Complications.2021; 35(9): 107975. CrossRef - Differential effects of body mass index on domain-specific cognitive outcomes after stroke
Minwoo Lee, Mi Sun Oh, San Jung, Ju-Hun Lee, Chul-Ho Kim, Min Uk Jang, Young Eun Kim, Hee-Joon Bae, Jaeseol Park, Yeonwook Kang, Byung-Chul Lee, Jae-Sung Lim, Kyung-Ho Yu
Scientific Reports.2021;[Epub] CrossRef - Associations between traditional and non-traditional anthropometric indices and cardiometabolic risk factors among inpatients with type 2 diabetes mellitus: a cross-sectional study
Sahar Golabi, Sajad Ajloo, Fatemeh Maghsoudi, Maryam Adelipour, Mahshid Naghashpour
Journal of International Medical Research.2021; 49(10): 030006052110499. CrossRef - Impact of preexisting type 2 diabetes mellitus and antidiabetic drugs on all-cause and cause-specific mortality among Medicaid-insured women diagnosed with breast cancer
Wayne R. Lawrence, Akiko S. Hosler, Margaret Gates Kuliszewski, Matthew C. Leinung, Xiuling Zhang, Maria J. Schymura, Francis P. Boscoe
Cancer Epidemiology.2020; 66: 101710. CrossRef - Serum Adiponectin and Progranulin Level in Patients with Benign Thyroid Nodule or Papillary Thyroid Cancer
Hyemi Kwon, Se Eun Park, Ji-Sup Yun, Cheol-Young Park
Endocrinology and Metabolism.2020; 35(2): 396. CrossRef - Obesity, sleep apnea, and cancer
Isaac Almendros, Miguel A. Martinez-Garcia, Ramon Farré, David Gozal
International Journal of Obesity.2020; 44(8): 1653. CrossRef - Association of Body Mass Index With Clinical Outcomes in Patients With Atrial Fibrillation: A Report From the FANTASIIA Registry
Vicente Bertomeu‐Gonzalez, José Moreno‐Arribas, María Asunción Esteve‐Pastor, Inmaculada Roldán‐Rabadán, Javier Muñiz, Paula Raña‐Míguez, Martín Ruiz‐Ortiz, Ángel Cequier, Vicente Bertomeu‐Martínez, Lina Badimón, Manuel Anguita, Gregory Y. H. Lip, Francis
Journal of the American Heart Association.2020;[Epub] CrossRef - Risk of type 2 diabetes according to the cumulative exposure to metabolic syndrome or obesity: A nationwide population‐based study
You‐Bin Lee, Da Hye Kim, Seon Mee Kim, Nan Hee Kim, Kyung Mook Choi, Sei Hyun Baik, Yong Gyu Park, Kyungdo Han, Hye Jin Yoo
Journal of Diabetes Investigation.2020; 11(6): 1583. CrossRef - Gut microbiota of obese and diabetic Thai subjects and interplay with dietary habits and blood profiles
Lucsame Gruneck, Niwed Kullawong, Kongkiat Kespechara, Siam Popluechai
PeerJ.2020; 8: e9622. CrossRef Multistate Models to Predict Development of Late Complications of Type 2 Diabetes in an Open Cohort Study
Roqayeh Aliyari, Ebrahim Hajizadeh, Ashraf Aminorroaya, Farshad Sharifi, Iraj Kazemi, Ahmad-Reza Baghestani
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1863. CrossRef- Early weaning induces short‐ and long‐term effects on pancreatic islets in Wistar rats of both sexes
Carla Bruna Pietrobon, Rosiane Aparecida Miranda, Iala Milene Bertasso, Paulo Cezar de Freitas Mathias, Maria Lúcia Bonfleur, Sandra Lucinei Balbo, Marise Auxiliadora de Barros Reis, Márcia Queiroz Latorraca, Vanessa Cristina Arantes, Elaine de Oliveira,
The Journal of Physiology.2020; 598(3): 489. CrossRef - A negative impact of recent weight loss on in-hospital mortality is not modified by overweight and obesity
Rocco Barazzoni, Isabella Sulz, Karin Schindler, Stephan C. Bischoff, Gianluca Gortan Cappellari, Michael Hiesmayr
Clinical Nutrition.2020; 39(8): 2510. CrossRef - Body mass index and mortality among middle-aged Japanese individuals with diagnosed diabetes: The Japan Public Health Center-based prospective study (JPHC study)
Chiho Yamazaki, Atsushi Goto, Motoki Iwasaki, Norie Sawada, Shino Oba, Mitsuhiko Noda, Hiroyasu Iso, Hiroshi Koyama, Shoichiro Tsugane
Diabetes Research and Clinical Practice.2020; 164: 108198. CrossRef Is the Obesity Paradox in Type 2 Diabetes Due to Artefacts of Biases? An Analysis of Pooled Cohort Data from the Heinz Nixdorf Recall Study and the Study of Health in Pomerania
Bernd Kowall, Andreas Stang, Raimund Erbel, Susanne Moebus, Astrid Petersmann, Antje Steveling, Karl-Heinz Jöckel, Henry Völzke
Diabetes, Metabolic Syndrome and Obesity: Targets and Therapy.2020; Volume 13: 1989. CrossRef- Associations between BMI, waist circumference, central obesity and outcomes in type II diabetes mellitus: The ACCORD Trial
Charles A. German, Brian Laughey, Alain G. Bertoni, Joseph Yeboah
Journal of Diabetes and its Complications.2020; 34(3): 107499. CrossRef - Trends in mechanical ventilation use and mortality over time in patients receiving mechanical ventilation in Spain from 2001 to 2015.
Javier de-Miguel-Díez, Rodrigo Jiménez-García, Valentín Hernández-Barrera, Jose J Zamorano-Leon, Rosa Villanueva-Orbaiz, Romana Albaladejo-Vicente, Ana López-de-Andrés
European Journal of Internal Medicine.2020; 74: 67. CrossRef - Type 2 diabetes mellitus: pathogenesis and genetic diagnosis
D. Himanshu, Wahid Ali, Mohd Wamique
Journal of Diabetes & Metabolic Disorders.2020; 19(2): 1959. CrossRef - Prevalence and factors associated with overweight and obesity among patients with type 2 diabetes mellitus in Uganda—a descriptive retrospective study
Salome Tino, Billy N Mayanja, Michael Charles Mubiru, Emmanuel Eling, Edward Ddumba, Pontiano Kaleebu, Moffat Nyirenda
BMJ Open.2020; 10(11): e039258. CrossRef - Nutrition Therapy in Critically Ill Overweight Elderly Patient with Heart Failure, Myocardial Infarction, Pneumonia, and Chronic Kidney Disease
Christina RUSLI, Agussalim BUKHARI, Nurpudji A. TASLIM, Suryani AS’AD, Haerani RASYID
Journal of Nutritional Science and Vitaminology.2020; 66(Supplement): S25. CrossRef - Obesity and childhood asthma
Jason E. Lang
Current Opinion in Pulmonary Medicine.2019; 25(1): 34. CrossRef - Why primary obesity is a disease?
Antonino De Lorenzo, Santo Gratteri, Paola Gualtieri, Andrea Cammarano, Pierfrancesco Bertucci, Laura Di Renzo
Journal of Translational Medicine.2019;[Epub] CrossRef - Impaired compensatory hyperinsulinemia among nonobese type 2 diabetes patients: a cross-sectional study
Jit Sarkar, Sujay Krishna Maity, Abhishek Sen, Titli Nargis, Dipika Ray, Partha Chakrabarti
Therapeutic Advances in Endocrinology and Metabolism.2019; 10: 204201881988902. CrossRef - Sedentary behaviour is associated with diabetes mellitus in adults: findings of a cross-sectional analysis from the Brazilian National Health System
Ítalo Ribeiro Lemes, Xuemei Sui, Bruna Camilo Turi-Lynch, Duck-chul Lee, Steven N Blair, Rômulo Araújo Fernandes, Jamile Sanches Codogno, Henrique Luiz Monteiro
Journal of Public Health.2019; 41(4): 742. CrossRef - Obesity Paradox in Chronic Liver Diseases: Product of Bias or a Real Thing?
Ines Bilic Curcic, Maja Cigrovski Berkovic, Lucija Kuna, Hrvoje Roguljic, Robert Smolic, Silvija Canecki Varzic, Lucija Virovic Jukic, Martina Smolic
Journal of Clinical and Translational Hepatology.2019; 7(3): 1. CrossRef - From the Obesity Tsunami to the Diabetes Avalanche: Primordial Prevention of the Diabesity-Related Cardiovascular Epidemic by Diabeto-Cardiologists
Mustafa Karakurt, Burak Acar, Ozcan Ozeke, Mustafa Bilal Ozbay, Yasin Ozen, Sefa Unal, Mustafa Karanfil, Cagri Yayla, Serkan Cay, Orhan Maden, Dursun Aras, Serkan Topaloglu, Sinan Aydogdu, Zehra Golbasi
Angiology.2019; 70(4): 371. CrossRef - Increased Plasma Dipeptidyl Peptidase-4 (DPP4) Activity Is an Obesity-Independent Parameter for Glycemic Deregulation in Type 2 Diabetes Patients
Jit Sarkar, Titli Nargis, Om Tantia, Sujoy Ghosh, Partha Chakrabarti
Frontiers in Endocrinology.2019;[Epub] CrossRef - INVESTIGATING INDIVIDUAL FACTORS RELATED TO READMISSION OF PATIENTS WITH TYPE 2 DIABETES- A CROSS-SECTIONAL STUDY
Valiallah Dashtpour, Mehran Hesaraki, Mahnaz Abavisani, Mahdieh Sari, Sudabeh Ahmadidarrehsima
Journal of Evolution of Medical and Dental Sciences.2018; 7(53): 5604. CrossRef
- Association between the weight-adjusted waist index and the odds of type 2 diabetes mellitus in United States adults: a cross-sectional study
- Clinical Diabetes & Therapeutics
- Past and Current Status of Adult Type 2 Diabetes Mellitus Management in Korea: A National Health Insurance Service Database Analysis
- Seung-Hyun Ko, Kyungdo Han, Yong-ho Lee, Junghyun Noh, Cheol-Young Park, Dae-Jung Kim, Chang Hee Jung, Ki-Up Lee, Kyung-Soo Ko
- Diabetes Metab J. 2018;42(2):93-100. Published online April 19, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.2.93
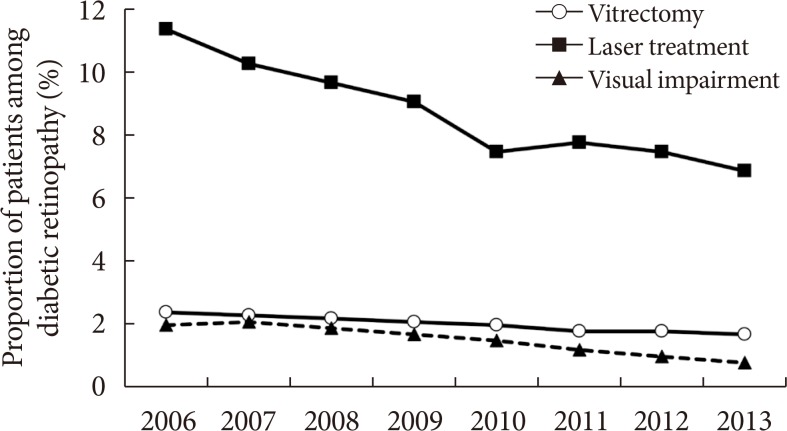
- 8,320 View
- 142 Download
- 81 Web of Science
- 82 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Korea's National Healthcare Program, the National Health Insurance Service (NHIS), a government-affiliated agency under the Korean Ministry of Health and Welfare, covers the entire Korean population. The NHIS supervises all medical services in Korea and establishes a systematic National Health Information database (DB). A health information DB system including all of the claims, medications, death information, and health check-ups, both in the general population and in patients with various diseases, is not common worldwide. On June 9, 2014, the NHIS signed a memorandum of understanding with the Korean Diabetes Association (KDA) to provide limited open access to its DB. By October 31, 2017, seven papers had been published through this collaborative research project. These studies were conducted to investigate the past and current status of type 2 diabetes mellitus and its complications and management in Korea. This review is a brief summary of the collaborative projects between the KDA and the NHIS over the last 3 years. According to the analysis, the national health check-up DB or claim DB were used, and the age category or study period were differentially applied.
-
Citations
Citations to this article as recorded by- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
Kyoung Min Kim, Kyoung Jin Kim, Kyungdo Han, Yumie Rhee
The Journal of Clinical Endocrinology & Metabolism.2024; 109(3): e1194. CrossRef - Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
Eun-Gyoung Hong, Kyung-Wan Min, Jung Soo Lim, Kyu-Jeung Ahn, Chul Woo Ahn, Jae-Myung Yu, Hye Soon Kim, Hyun Jin Kim, Won Kim, Dong Han Kim, Hak Chul Jang
Advances in Therapy.2024;[Epub] CrossRef - Association Between Glycemic Status and the Risk of Kidney Cancer in Men and Women: A Nationwide Cohort Study
Joo-Hyun Park, Jung Yong Hong, Kyungdo Han, Jay J. Shen
Diabetes Care.2023; 46(1): 38. CrossRef - Remnant Cholesterol Is an Independent Predictor of Type 2 Diabetes: A Nationwide Population-Based Cohort Study
Ji Hye Huh, Eun Roh, Seong Jin Lee, Sung-Hee Ihm, Kyung-Do Han, Jun Goo Kang
Diabetes Care.2023; 46(2): 305. CrossRef - Efficacy of acupuncture on cardiovascular complications in patients with diabetes mellitus in Korea: A nationwide retrospective cohort
Hyejin Jung, Tiana Won, Ga-Yeon Kim, Jowon Jang, Sujung Yeo, Sabina Lim
Journal of Integrative Medicine.2023; 21(2): 176. CrossRef - Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
Jong Ha Baek, Yong-Moon Park, Kyung Do Han, Min Kyong Moon, Jong Han Choi, Seung-Hyun Ko
Diabetes & Metabolism Journal.2023; 47(2): 201. CrossRef - Epidemiology of PAH in Korea: An Analysis of the National Health Insurance Data, 2002–2018
Albert Youngwoo Jang, Hyeok-Hee Lee, Hokyou Lee, Hyeon Chang Kim, Wook-Jin Chung
Korean Circulation Journal.2023; 53(5): 313. CrossRef - Increased Risks of Open-Angle Glaucoma in Untreated Hypertension
Jihei Sara Lee, Yong Joon Kim, Sunyeup Kim, Hyoung Won Bae, Sung Soo Kim, Seung Won Lee, Chan Yun Kim
American Journal of Ophthalmology.2023; 252: 111. CrossRef - Lobeglitazone, a novel thiazolidinedione, for secondary prevention in patients with ischemic stroke: a nationwide nested case-control study
Joonsang Yoo, Jimin Jeon, Minyoul Baik, Jinkwon Kim
Cardiovascular Diabetology.2023;[Epub] CrossRef - Association between glycemic status and the risk of acute pancreatitis: a nationwide population-based study
In Rae Cho, Kyung-Do Han, Sang Hyub Lee, Young Hoon Choi, Kwang Hyun Chung, Jin Ho Choi, Namyoung Park, Min Woo Lee, Woo Hyun Paik, Ji Kon Ryu, Yong-Tae Kim
Diabetology & Metabolic Syndrome.2023;[Epub] CrossRef - Type 2 Diabetes and Its Association With Psychiatric Disorders in Young Adults in South Korea
Min-Kyung Lee, Su-Young Lee, Seo-Young Sohn, Jiyeon Ahn, Kyungdo Han, Jae-Hyuk Lee
JAMA Network Open.2023; 6(6): e2319132. CrossRef - Cholecystectomy Increases the Risk of Type 2 Diabetes in the Korean Population
Ji Hye Huh, Kyong Joo Lee, Yun Kyung Cho, Shinje Moon, Yoon Jung Kim, Eun Roh, Kyung-do Han, Dong Hee Koh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Annals of Surgery.2023; 278(2): e264. CrossRef - The Risk of Type 2 Diabetes Mellitus according to Changes in Obesity Status in Late Middle-Aged Adults: A Nationwide Cohort Study of Korea
Joon Ho Moon, Yeonhoon Jang, Tae Jung Oh, Se Young Jung
Diabetes & Metabolism Journal.2023; 47(4): 514. CrossRef - Scalable Infrastructure Supporting Reproducible Nationwide Healthcare Data Analysis toward FAIR Stewardship
Ji-Woo Kim, Chungsoo Kim, Kyoung-Hoon Kim, Yujin Lee, Dong Han Yu, Jeongwon Yun, Hyeran Baek, Rae Woong Park, Seng Chan You
Scientific Data.2023;[Epub] CrossRef - Association between Smoking Status and the Risk of Hip Fracture in Patients with Type 2 Diabetes: A Nationwide Population-Based Study
Se-Won Lee, Jun-Young Heu, Ju-Yeong Kim, Jinyoung Kim, Kyungdo Han, Hyuk-Sang Kwon
Endocrinology and Metabolism.2023; 38(6): 679. CrossRef - Urgensi Kepesertaan BPJS Kesehatan Sebagai Syarat Peralihan Hak Atas Tanah Berdasarkan Instruksi Presiden Nomor 1 Tahun 2022 Tentang Optimalisasi Pelaksanaan Program Jaminan Kesehatan Nasional
Nur Dwi Safitri, Fauziyah Fauziyah
Indonesian Journal of Law and Justice.2023; 1(2): 10. CrossRef - Risk of Incident Dementia According to Glycemic Status and Comorbidities of Hyperglycemia: A Nationwide Population-Based Cohort Study
Woo Jung Kim, Seo Jung Lee, Eun Lee, Eun Y. Lee, Kyungdo Han
Diabetes Care.2022; 45(1): 134. CrossRef - Effects of physical activity on cardiovascular outcomes and mortality in Korean patients with diabetes: a nationwide population-based cohort study
Inha Jung, Sun Joon Moon, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Eun-Jung Rhee, Won-Young Lee
Cardiovascular Prevention and Pharmacotherapy.2022; 4(1): 42. CrossRef - Increasing Age Associated with Higher Dipeptidyl Peptidase-4 Inhibition Rate Is a Predictive Factor for Efficacy of Dipeptidyl Peptidase-4 Inhibitors
Sangmo Hong, Chang Hee Jung, Song Han, Cheol-Young Park
Diabetes & Metabolism Journal.2022; 46(1): 63. CrossRef - Changes in Patterns of Physical Activity and Risk of Heart Failure in Newly Diagnosed Diabetes Mellitus Patients
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Diabetes & Metabolism Journal.2022; 46(2): 327. CrossRef - Synergistic association between underweight and type 2 diabetes on the development of laryngeal cancer: a national population-based retrospective cohort study
Oh. Hyeong Lee, Yong-Moon Park, Seung-Hyun Ko, Kyuna Lee, Yeonji Kim, Kyungdo Han, Jung-Hae Cho
BMC Cancer.2022;[Epub] CrossRef - Cardiovascular Implications of the 2021 KDIGO Blood Pressure Guideline for Adults With Chronic Kidney Disease
Hyeok-Hee Lee, Hokyou Lee, Raymond R. Townsend, Dong-Wook Kim, Sungha Park, Hyeon Chang Kim
Journal of the American College of Cardiology.2022; 79(17): 1675. CrossRef - Cumulative Exposure to High γ-Glutamyl Transferase Level and Risk of Diabetes: A Nationwide Population-Based Study
Ji-Yeon Park, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim, Seung-Hwan Lee
Endocrinology and Metabolism.2022; 37(2): 272. CrossRef - Skin accumulation of advanced glycation end products and cardiovascular risk in Korean patients with type 2 diabetes mellitus
Lee-Seoul Choi, Kainat Ahmed, Young-Seol Kim, Jung-Eun Yim
Heliyon.2022; 8(6): e09571. CrossRef - Risk for Behçet’s disease gauged via high-density lipoprotein cholesterol: a nationwide population-based study in Korea
Yeong Ho Kim, Hyun Jee Kim, Jin Woo Park, Kyung Do Han, Yong Gyu Park, Young Bok Lee, Ji Hyun Lee
Scientific Reports.2022;[Epub] CrossRef - Association between the Diabetes Drug Cost and Cardiovascular Events and Death in Korea: A National Health Insurance Service Database Analysis
Seung Min Chung, Ji-In Lee, Eugene Han, Hyun-Ae Seo, Eonju Jeon, Hye Soon Kim, Ji Sung Yoon
Endocrinology and Metabolism.2022; 37(5): 759. CrossRef - Remnant cholesterol and the risk of cardiovascular disease in type 2 diabetes: a nationwide longitudinal cohort study
Ji Hye Huh, Kyung-do Han, Yun Kyung Cho, Eun Roh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm
Cardiovascular Diabetology.2022;[Epub] CrossRef - Associations between migraine and major cardiovascular events in type 2 diabetes mellitus
Dae Young Cheon, Kyungdo Han, Ye Seul Yang, Yerim Kim, Sang-Hwa Lee, Chulho Kim, Jong-Hee Sohn, Mi Sun Oh, Byung-Chul Lee, Minwoo Lee, Kyung-Ho Yu
Cardiovascular Diabetology.2022;[Epub] CrossRef - Efficacy and Safety of Treatment with Quadruple Oral Hypoglycemic Agents in Uncontrolled Type 2 Diabetes Mellitus: A Multi-Center, Retrospective, Observational Study
Jun Sung Moon, Sunghwan Suh, Sang Soo Kim, Heung Yong Jin, Jeong Mi Kim, Min Hee Jang, Kyung Ae Lee, Ju Hyung Lee, Seung Min Chung, Young Sang Lyu, Jin Hwa Kim, Sang Yong Kim, Jung Eun Jang, Tae Nyun Kim, Sung Woo Kim, Eonju Jeon, Nan Hee Cho, Mi-Kyung Ki
Diabetes & Metabolism Journal.2021; 45(5): 675. CrossRef - Umbilical Cord-Mesenchymal Stem Cell-Conditioned Medium Improves Insulin Resistance in C2C12 Cell
Kyung-Soo Kim, Yeon Kyung Choi, Mi Jin Kim, Jung Wook Hwang, Kyunghoon Min, Sang Youn Jung, Soo-Kyung Kim, Yong-Soo Choi, Yong-Wook Cho
Diabetes & Metabolism Journal.2021; 45(2): 260. CrossRef - Associations of general obesity and central obesity with the risk of hepatocellular carcinoma in a Korean population: A national population‐based cohort study
Seawon Hwang, Yong‐Moon Park, Kyung‐Do Han, Jae‐Seung Yun, Seung‐Hyun Ko, Yu‐Bae Ahn, Jae Hyun Han
International Journal of Cancer.2021; 148(5): 1144. CrossRef - Glycaemic control with add‐on thiazolidinedione or a sodium‐glucose co‐transporter‐2 inhibitor in patients with type 2 diabetes after the failure of an oral triple antidiabetic regimen: A 24‐week, randomized controlled trial
Jaehyun Bae, Ji Hye Huh, Minyoung Lee, Yong‐Ho Lee, Byung‐Wan Lee
Diabetes, Obesity and Metabolism.2021; 23(2): 609. CrossRef - Metabolic Dysfunction-Associated Fatty Liver Disease and Incident Cardiovascular Disease Risk: A Nationwide Cohort Study
Hokyou Lee, Yong-ho Lee, Seung Up Kim, Hyeon Chang Kim
Clinical Gastroenterology and Hepatology.2021; 19(10): 2138. CrossRef - Severe hypoglycemia as a preventable risk factor for cardiovascular disease in patients with type 2 diabetes mellitus
Soo-Yeon Choi, Seung-Hyun Ko
The Korean Journal of Internal Medicine.2021; 36(2): 263. CrossRef - Changes in metabolic syndrome status affect the incidence of end-stage renal disease in the general population: a nationwide cohort study
Eun Sil Koh, Kyung Do Han, Mee Kyoung Kim, Eun Sook Kim, Min-Kyung Lee, Ga Eun Nam, Oak-Kee Hong, Hyuk-Sang Kwon
Scientific Reports.2021;[Epub] CrossRef - Status of Diabetic Neuropathy in Korea: A National Health Insurance Service-National Sample Cohort Analysis (2006 to 2015)
Seong-Su Moon, Chong Hwa Kim, Seon Mee Kang, Eun Sook Kim, Tae Jung Oh, Jae-Seung Yun, Ho Chan Cho, Dae Jung Kim, Tae Sun Park
Diabetes & Metabolism Journal.2021; 45(1): 115. CrossRef - Thirty-six Year Trends in Mortality from Diseases of Circulatory System in Korea
Jongmin Baek, Hokyou Lee, Hyeok-Hee Lee, Ji Eun Heo, So Mi Jemma Cho, Hyeon Chang Kim
Korean Circulation Journal.2021; 51(4): 320. CrossRef - Severe hypoglycemia and the risk of end stage renal disease in type 2 diabetes
Jae-Seung Yun, Yong-Moon Park, Kyungdo Han, Hyung-Wook Kim, Seon-Ah Cha, Yu-Bae Ahn, Seung-Hyun Ko
Scientific Reports.2021;[Epub] CrossRef - Adherence to Antihypertensive Medication and Incident Cardiovascular Events in Young Adults With Hypertension
Hokyou Lee, Yuichiro Yano, So Mi Jemma Cho, Ji Eun Heo, Dong-Wook Kim, Sungha Park, Donald M. Lloyd-Jones, Hyeon Chang Kim
Hypertension.2021; 77(4): 1341. CrossRef - Cumulative exposure to impaired fasting glucose and future risk of type 2 diabetes mellitus
Mee Kyoung Kim, Kyungdo Han, Eun Sil Koh, Oak-Kee Hong, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Diabetes Research and Clinical Practice.2021; 175: 108799. CrossRef - Association between toothbrushing and non-alcoholic fatty liver disease
Ji-Youn Kim, Yong-Moon Park, Gyu-Na Lee, Hyun Chul Song, Yu-Bae Ahn, Kyungdo Han, Seung-Hyun Ko, Houkai Li
PLOS ONE.2021; 16(5): e0243686. CrossRef - Weight change and microvascular outcomes in patients with new-onset diabetes: a nationwide cohort study
Eun Sil Koh, Kyung Do Han, Mee Kyoung Kim, Eun Sook Kim, Min-Kyung Lee, Ga Eun Nam, Hyuk-Sang Kwon
The Korean Journal of Internal Medicine.2021; 36(4): 932. CrossRef - Current utilization patterns for long-acting insulin analogues including biosimilars among selected Asian countries and the implications for the future
Brian Godman, Mainul Haque, Santosh Kumar, Salequl Islam, Jaykaran Charan, Farhana Akter, Amanj Kurdi, Eleonora Allocati, Muhammed Abu Bakar, Sagir Abdur Rahim, Nusrat Sultana, Farzana Deeba, M. A. Halim Khan, A. B. M Muksudul Alam, Iffat Jahan, Zubair Ma
Current Medical Research and Opinion.2021; 37(9): 1529. CrossRef - Development and Validation of a Deep Learning Based Diabetes Prediction System Using a Nationwide Population-Based Cohort
Sang Youl Rhee, Ji Min Sung, Sunhee Kim, In-Jeong Cho, Sang-Eun Lee, Hyuk-Jae Chang
Diabetes & Metabolism Journal.2021; 45(4): 515. CrossRef - Cardiovascular Safety of Sodium Glucose Cotransporter 2 Inhibitors as Add-on to Metformin Monotherapy in Patients with Type 2 Diabetes Mellitus
Ja Young Jeon, Kyoung Hwa Ha, Dae Jung Kim
Diabetes & Metabolism Journal.2021; 45(4): 505. CrossRef - Nonalcoholic fatty liver disease and the risk of insulin-requiring gestational diabetes
Sang Youn You, Kyungdo Han, Seung-Hawn Lee, Mee Kyoung Kim
Diabetology & Metabolic Syndrome.2021;[Epub] CrossRef - On-Treatment Blood Pressure and Cardiovascular Outcomes in Adults With Hypertension and Left Ventricular Hypertrophy
Hyeok-Hee Lee, Hokyou Lee, So Mi Jemma Cho, Dong-Wook Kim, Sungha Park, Hyeon Chang Kim
Journal of the American College of Cardiology.2021; 78(15): 1485. CrossRef - The Effects of Glucose Lowering Agents on the Secondary Prevention of Coronary Artery Disease in Patients with Type 2 Diabetes
Inha Jung, Hyemi Kwon, Se Eun Park, Kyung-Do Han, Yong-Gyu Park, Eun-Jung Rhee, Won-Young Lee
Endocrinology and Metabolism.2021; 36(5): 977. CrossRef - Changes in metabolic syndrome and its components and the risk of type 2 diabetes: a nationwide cohort study
Min-Kyung Lee, Kyungdo Han, Mee Kyoung Kim, Eun Sil Koh, Eun Sook Kim, Ga Eun Nam, Hyuk-Sang Kwon
Scientific Reports.2020;[Epub] CrossRef - Obesity and metabolic health status are determinants for the clinical expression of hypertrophic cardiomyopathy
Jun-Bean Park, Da Hye Kim, Heesun Lee, In-Chang Hwang, Yeonyee E Yoon, Hyo Eun Park, Su-Yeon Choi, Yong-Jin Kim, Goo-Yeong Cho, Kyungdo Han, Steve R Ommen, Hyung-Kwan Kim
European Journal of Preventive Cardiology.2020; 27(17): 1849. CrossRef - Clinical Characteristics and Prevalence of Comorbidities according to Metformin Use in Korean Patients with Type 2 Diabetes
Sang Ouk Chin, In Gyoon Ha, Sang Youl Rhee, Su Jin Jeong, Suk Chon, Sung Hoon Kim, Kyu Jeung Ahn, Sei Hyun Baik, Yongsoo Park, Moon Suk Nam, Kwan Woo Lee, Jeong Taek Woo
International Journal of Endocrinology.2020; 2020: 1. CrossRef - Impact of Mean and Variability of High‐Density Lipoprotein‐Cholesterol on the Risk of Myocardial Infarction, Stroke, and Mortality in the General Population
Byung‐Hun Han, Kyungdo Han, Kun‐Ho Yoon, Mee Kyoung Kim, Seung‐Hwan Lee
Journal of the American Heart Association.2020;[Epub] CrossRef - The association between nonalcoholic fatty liver disease and esophageal, stomach, or colorectal cancer: National population-based cohort study
Jung-Min Lee, Yong-Moon Park, Jae-Seung Yun, Yu-Bae Ahn, Kang-Moon Lee, Dae Bum Kim, Ji Min Lee, Kyungdo Han, Seung-Hyun Ko, Ming-Lung Yu
PLOS ONE.2020; 15(1): e0226351. CrossRef - Outcomes for Inappropriate Renal Dose Adjustment of Dipeptidyl Peptidase-4 Inhibitors in Patients With Type 2 Diabetes Mellitus: Population-Based Study
Sangmo Hong, Kyungdo Han, Cheol-Young Park
Mayo Clinic Proceedings.2020; 95(1): 101. CrossRef - Association Between Glycemic Status and the Risk of Parkinson Disease: A Nationwide Population-Based Study
Sang Youl Rhee, Kyung-Do Han, Hyemi Kwon, Se-Eun Park, Yong-Gyu Park, Yang-Hyun Kim, Soon-Jip Yoo, Eun-Jung Rhee, Won-Young Lee
Diabetes Care.2020; 43(9): 2169. CrossRef - A model to predict risk of stroke in middle-aged adults with type 2 diabetes generated from a nationwide population-based cohort study in Korea
Mee-Kyoung Kim, Kyungdo Han, Jae-Hyoung Cho, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Diabetes Research and Clinical Practice.2020; 163: 108157. CrossRef - Diabetic Retinopathy and Related Clinical Practice for People with Diabetes in Korea: A 10-Year Trend Analysis
Yoo-Ri Chung, Kyoung Hwa Ha, Kihwang Lee, Dae Jung Kim
Diabetes & Metabolism Journal.2020; 44(6): 928. CrossRef - Prepregnancy smoking and the risk of gestational diabetes requiring insulin therapy
Mee Kyoung Kim, Kyungdo Han, Sang Youn You, Hyuk-Sang Kwon, Kun-Ho Yoon, Seung-Hwan Lee
Scientific Reports.2020;[Epub] CrossRef - Cardiovascular Risk of Isolated Systolic or Diastolic Hypertension in Young Adults
Hokyou Lee, Yuichiro Yano, So Mi Jemma Cho, Jong Heon Park, Sungha Park, Donald M. Lloyd-Jones, Hyeon Chang Kim
Circulation.2020; 141(22): 1778. CrossRef - Middle-aged men with type 2 diabetes as potential candidates for pancreatic cancer screening: a 10-year nationwide population-based cohort study
Dong-Hoe Koo, Kyung-Do Han, Hong Joo Kim, Cheol-Young Park
Acta Diabetologica.2020; 57(2): 197. CrossRef - Predicting the Development of Myocardial Infarction in Middle-Aged Adults with Type 2 Diabetes: A Risk Model Generated from a Nationwide Population-Based Cohort Study in Korea
Seung-Hwan Lee, Kyungdo Han, Hun-Sung Kim, Jae-Hyoung Cho, Kun-Ho Yoon, Mee Kyoung Kim
Endocrinology and Metabolism.2020; 35(3): 636. CrossRef - Fasting plasma glucose level and the risk of open angle glaucoma: Nationwide population-based cohort study in Korea
Jin A. Choi, Yong-Moon Park, Kyungdo Han, Jiyoung Lee, Jae-Seung Yun, Seung-Hyun Ko, Bang V Bui
PLOS ONE.2020; 15(9): e0239529. CrossRef - Effect of Variability in Blood Pressure, Glucose and Cholesterol Concentrations, and Body Weight on Emergency Hospitalization and 30‐Day Mortality in the General Population
Seung‐Hwan Lee, Kyungdo Han, Hyuk‐Sang Kwon, Kun‐Ho Yoon, Mee Kyoung Kim
Journal of the American Heart Association.2020;[Epub] CrossRef - Does Diabetes Increase the Risk of Contracting COVID-19? A Population-Based Study in Korea
Sung-Youn Chun, Dong Wook Kim, Sang Ah Lee, Su Jung Lee, Jung Hyun Chang, Yoon Jung Choi, Seong Woo Kim, Sun Ok Song
Diabetes & Metabolism Journal.2020; 44(6): 897. CrossRef - Appropriate Medical Technology in the Era of the 4th Industrial Revolution
Sang Youl Rhee
The Korean Journal of Medicine.2019; 94(5): 387. CrossRef - Second-line glucose-lowering drugs added to metformin and the risk of hospitalization for heart failure: A nationwide cohort study
Su Jin Lee, Kyoung Hwa Ha, Jung Hyun Lee, Hokyou Lee, Dae Jung Kim, Hyeon Chang Kim, Tatsuo Shimosawa
PLOS ONE.2019; 14(2): e0211959. CrossRef - 2017 ACC/AHA Blood Pressure Classification and Cardiovascular Disease in 15 Million Adults of Age 20–94 Years
Lee, Cho, Park, Park, Kim
Journal of Clinical Medicine.2019; 8(11): 1832. CrossRef - Management of Cardiovascular Risk Factors in Elderly Diabetes Mellitus Patients
Sung Hoon Yu
The Journal of Korean Diabetes.2019; 20(4): 233. CrossRef - Cholesterol levels and development of cardiovascular disease in Koreans with type 2 diabetes mellitus and without pre-existing cardiovascular disease
Mee Kyoung Kim, Kyungdo Han, Han Na Joung, Ki-Hyun Baek, Ki-Ho Song, Hyuk-Sang Kwon
Cardiovascular Diabetology.2019;[Epub] CrossRef - Comprehensive Efforts Are Needed to Improve the Quality of Primary Diabetes Care in Korea
Chan-Hee Jung
Endocrinology and Metabolism.2019; 34(3): 265. CrossRef - Blood Pressure and Development of Cardiovascular Disease in Koreans With Type 2 Diabetes Mellitus
Mee Kyoung Kim, Kyungdo Han, Eun Sil Koh, Eun Sook Kim, Min-Kyung Lee, Ga Eun Nam, Hyuk-Sang Kwon
Hypertension.2019; 73(2): 319. CrossRef - Weight change and mortality and cardiovascular outcomes in patients with new-onset diabetes mellitus: a nationwide cohort study
Mee Kyoung Kim, Kyungdo Han, Eun Sil Koh, Eun Sook Kim, Min-Kyung Lee, Ga Eun Nam, Hyuk-Sang Kwon
Cardiovascular Diabetology.2019;[Epub] CrossRef - Letter: Comparison of the Efficacy of Rosuvastatin Monotherapy 20 mg with Rosuvastatin 5 mg and Ezetimibe 10 mg Combination Therapy on Lipid Parameters in Patients with Type 2 Diabetes Mellitus (Diabetes Metab J2019;43:582–9)
Tae Seo Sohn
Diabetes & Metabolism Journal.2019; 43(6): 909. CrossRef - Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study
Yoo-Ri Chung, Kyoung Hwa Ha, Hyeon Chang Kim, Sang Jun Park, Kihwang Lee, Dae Jung Kim
Diabetes & Metabolism Journal.2019; 43(5): 640. CrossRef - The Need to Improve the Quality of Diabetes Care in Korea
Seung Jin Han, Dae Jung Kim
Journal of Korean Medical Science.2019;[Epub] CrossRef - Chasms in Achievement of Recommended Diabetes Care among Geographic Regions in Korea
Sanghyun Cho, Ji-Yeon Shin, Hyun Joo Kim, Sang Jun Eun, Sungchan Kang, Won Mo Jang, Hyemin Jung, Yoon Kim, Jin Yong Lee
Journal of Korean Medical Science.2019;[Epub] CrossRef - An Age of Sodium-Glucose Cotransporter-2 Inhibitor Priority: Are We Ready?
Ji A Seo
Diabetes & Metabolism Journal.2019; 43(5): 578. CrossRef - National trends in metformin-based combination therapy of oral hypoglycaemic agents for type 2 diabetes mellitus
Jisu Kim, Susin Park, Hyunsoo Kim, Nam Kyung Je
European Journal of Clinical Pharmacology.2019; 75(12): 1723. CrossRef - HDL-Cholesterol, Its Variability, and the Risk of Diabetes: A Nationwide Population-Based Study
Seung-Hwan Lee, Hun-Sung Kim, Yong-Moon Park, Hyuk-Sang Kwon, Kun-Ho Yoon, Kyungdo Han, Mee Kyoung Kim
The Journal of Clinical Endocrinology & Metabolism.2019; 104(11): 5633. CrossRef - Current Management of Type 2 Diabetes Mellitus in Primary Care Clinics in Korea
Da Hea Seo, Shinae Kang, Yong-ho Lee, Jung Yoon Ha, Jong Suk Park, Byoung-Wan Lee, Eun Seok Kang, Chul Woo Ahn, Bong-Soo Cha
Endocrinology and Metabolism.2019; 34(3): 282. CrossRef - Heritability estimation of dichotomous phenotypes using a liability threshold model on ascertained family‐based samples
Wonji Kim, Soo Heon Kwak, Sungho Won
Genetic Epidemiology.2019; 43(7): 761. CrossRef - Letter: Dipeptidyl Peptidase-4 Inhibitors versus Other Antidiabetic Drugs Added to Metformin Monotherapy in Diabetic Retinopathy Progression: A Real World-Based Cohort Study (Diabetes Metab J 2019;43:640–8)
Jun Sung Moon
Diabetes & Metabolism Journal.2019; 43(6): 911. CrossRef
- Associations Between Physical Activity and the Risk of Hip Fracture Depending on Glycemic Status: A Nationwide Cohort Study
- Pathophysiology
- Primary Cilia as a Signaling Platform for Control of Energy Metabolism
- Do Kyeong Song, Jong Han Choi, Min-Seon Kim
- Diabetes Metab J. 2018;42(2):117-127. Published online April 19, 2018
- DOI: https://doi.org/10.4093/dmj.2018.42.2.117
- 7,888 View
- 124 Download
- 26 Web of Science
- 24 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader Obesity has become a common healthcare problem worldwide. Cilia are tiny hair-like organelles on the cell surface that are generated and anchored by the basal body. Non-motile primary cilia have been considered to be evolutionary rudiments until a few decades, but they are now considered as important signaling organelles because many receptors, channels, and signaling molecules are highly expressed in primary cilia. A potential role of primary cilia in metabolic regulation and body weight maintenance has been suspected based on rare genetic disorders termed as ciliopathy, such as Bardet-Biedl syndrome and Alström syndrome, which manifest as obesity. Recent studies have demonstrated involvement of cilia-related cellular signaling pathways in transducing metabolic information in hypothalamic neurons and in determining cellular fate during adipose tissue development. In this review, we summarize the current knowledge about cilia and cilia-associated signaling pathways in the regulation of body metabolism.
-
Citations
Citations to this article as recorded by- MRAP2 regulates energy homeostasis by promoting primary cilia localization of MC4R
Adelaide Bernard, Irene Ojeda Naharros, Xinyu Yue, Francois Mifsud, Abbey Blake, Florence Bourgain-Guglielmetti, Jordi Ciprin, Sumei Zhang, Erin McDaid, Kellan Kim, Maxence V. Nachury, Jeremy F. Reiter, Christian Vaisse
JCI Insight.2023;[Epub] CrossRef - A high‐confidence Physcomitrium patens plasmodesmata proteome by iterative scoring and validation reveals diversification of cell wall proteins during evolution
Sven Gombos, Manuel Miras, Vicky Howe, Lin Xi, Mathieu Pottier, Neda S. Kazemein Jasemi, Moritz Schladt, J. Obinna Ejike, Ulla Neumann, Sebastian Hänsch, Franziska Kuttig, Zhaoxia Zhang, Marcel Dickmanns, Peng Xu, Thorsten Stefan, Wolfgang Baumeister, Wol
New Phytologist.2023; 238(2): 637. CrossRef - Primary cilia shape hallmarks of health and aging
Diana Filipa Silva, Cláudia Cavadas
Trends in Molecular Medicine.2023; 29(7): 567. CrossRef - Therapeutic implications of sonic hedgehog pathway in metabolic disorders: Novel target for effective treatment
Chahat Garg, Heena khan, Amarjot Kaur, Thakur Gurjeet Singh, Vivek Kumar Sharma, Sachin Kumar Singh
Pharmacological Research.2022; 179: 106194. CrossRef - Mechanisms of Weight Control by Primary Cilia
Chan Hee Lee, Gil Myoung Kang, Min-Seon Kim
Molecules and Cells.2022; 45(4): 169. CrossRef - Cilia-localized GID/CTLH ubiquitin ligase complex regulates protein homeostasis of sonic hedgehog signaling components
Friederike Hantel, Huaize Liu, Lisa Fechtner, Herbert Neuhaus, Jie Ding, Danilo Arlt, Peter Walentek, Pablo Villavicencio-Lorini, Christoph Gerhardt, Thomas Hollemann, Thorsten Pfirrmann
Journal of Cell Science.2022;[Epub] CrossRef - IFT20 governs mesenchymal stem cell fate through positively regulating TGF-β-Smad2/3-Glut1 signaling mediated glucose metabolism
Yang Li, Shuting Yang, Yang Liu, Ling Qin, Shuying Yang
Redox Biology.2022; 54: 102373. CrossRef - Primary Cilia in Pancreatic β- and α-Cells: Time to Revisit the Role of Insulin-Degrading Enzyme
Marta Pablos, Elena Casanueva-Álvarez, Carlos M. González-Casimiro, Beatriz Merino, Germán Perdomo, Irene Cózar-Castellano
Frontiers in Endocrinology.2022;[Epub] CrossRef - Palmitic acid control of ciliogenesis modulates insulin signaling in hypothalamic neurons through an autophagy-dependent mechanism
Yenniffer Ávalos, María Paz Hernández-Cáceres, Pablo Lagos, Daniela Pinto-Nuñez, Patricia Rivera, Paulina Burgos, Francisco Díaz-Castro, Michelle Joy-Immediato, Leslye Venegas-Zamora, Erik Lopez-Gallardo, Catalina Kretschmar, Ana Batista-Gonzalez, Flavia
Cell Death & Disease.2022;[Epub] CrossRef - Shedding of ciliary vesicles at a glance
Irene Ojeda Naharros, Maxence V. Nachury
Journal of Cell Science.2022;[Epub] CrossRef - Oligodendroglial primary cilium heterogeneity during development and demyelination/remyelination
Giada Delfino, Karelle Bénardais, Julien Graff, Brigitte Samama, Maria Cristina Antal, M. Said Ghandour, Nelly Boehm
Frontiers in Cellular Neuroscience.2022;[Epub] CrossRef - Proteomic and Transcriptomic Landscapes of Alström and Bardet–Biedl Syndromes
Urszula Smyczynska, Marcin Stanczak, Miljan Kuljanin, Aneta Włodarczyk, Ewelina Stoczynska-Fidelus, Joanna Taha, Bartłomiej Pawlik, Maciej Borowiec, Joseph D. Mancias, Wojciech Mlynarski, Piotr Rieske, Wojciech Fendler, Agnieszka Zmysłowska
Genes.2022; 13(12): 2370. CrossRef - A role for primary cilia in coral calcification?
Eric Tambutté, Philippe Ganot, Alexander A Venn, Sylvie Tambutté
Cell and Tissue Research.2021; 383(3): 1093. CrossRef - Myocardin-related transcription factor and serum response factor regulate cilium turnover by both transcriptional and local mechanisms
Pam Speight, Matthew Rozycki, Shruthi Venugopal, Katalin Szászi, Michael Kofler, András Kapus
iScience.2021; 24(7): 102739. CrossRef - Hypothalamic primary cilium: A hub for metabolic homeostasis
Dong Joo Yang, Jessica Hong, Ki Woo Kim
Experimental & Molecular Medicine.2021; 53(7): 1109. CrossRef - Low fluid shear stress promoted ciliogenesis via Dvl2 in hUVECs
Xin Sheng, Yan Sheng, Shuanglin Gao, Fang Fan, Junhua Wang
Histochemistry and Cell Biology.2020; 154(6): 639. CrossRef - Primary cilia mediate early life programming of adiposity through lysosomal regulation in the developing mouse hypothalamus
Chan Hee Lee, Do Kyeong Song, Chae Beom Park, Jeewon Choi, Gil Myoung Kang, Sung Hoon Shin, Ijoo Kwon, Soyoung Park, Seongjun Kim, Ji Ye Kim, Hong Dugu, Jae Woo Park, Jong Han Choi, Se Hee Min, Jong-Woo Sohn, Min-Seon Kim
Nature Communications.2020;[Epub] CrossRef - Evidences of a Direct Relationship between Cellular Fuel Supply and Ciliogenesis Regulated by Hypoxic VDAC1-ΔC
Monique Meyenberg Cunha-de Padua, Lucilla Fabbri, Maeva Dufies, Sandra Lacas-Gervais, Julie Contenti, Charles Voyton, Sofia Fazio, Marie Irondelle, Baharia Mograbi, Matthieu Rouleau, Nirvana Sadaghianloo, Amandine Rovini, Catherine Brenner, William J. Cra
Cancers.2020; 12(11): 3484. CrossRef - High-resolution characterization of centriole distal appendage morphology and dynamics by correlative STORM and electron microscopy
Mathew Bowler, Dong Kong, Shufeng Sun, Rashmi Nanjundappa, Lauren Evans, Veronica Farmer, Andrew Holland, Moe R. Mahjoub, Haixin Sui, Jadranka Loncarek
Nature Communications.2019;[Epub] CrossRef - Sonic hedgehog signaling instigates high-fat diet–induced insulin resistance by targeting PPARγ stability
Qinyu Yao, Jia Liu, Lei Xiao, Nanping Wang
Journal of Biological Chemistry.2019; 294(9): 3284. CrossRef - Cellular signalling by primary cilia in development, organ function and disease
Zeinab Anvarian, Kirk Mykytyn, Saikat Mukhopadhyay, Lotte Bang Pedersen, Søren Tvorup Christensen
Nature Reviews Nephrology.2019; 15(4): 199. CrossRef - O-GlcNAcylation Regulates Primary Ciliary Length by Promoting Microtubule Disassembly
Jie L. Tian, Hongmin Qin
iScience.2019; 12: 379. CrossRef - Interplay Between Primary Cilia and Autophagy and Its Controversial Roles in Cancer
Je Yeong Ko, Eun Ji Lee, Jong Hoon Park
Biomolecules & Therapeutics.2019; 27(4): 337. CrossRef - Neuronal and astrocytic primary cilia in the mature brain
Ashley Sterpka, Xuanmao Chen
Pharmacological Research.2018; 137: 114. CrossRef
- MRAP2 regulates energy homeostasis by promoting primary cilia localization of MC4R

 KDA
KDA
 First
First Prev
Prev





