
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Article category
- Page Path
- HOME > Article category > Article category
Original Articles
- Metabolic Risk/Epidemiology
- Higher Muscle Mass Protects Women with Gestational Diabetes Mellitus from Progression to Type 2 Diabetes Mellitus
- Yujin Shin, Joon Ho Moon, Tae Jung Oh, Chang Ho Ahn, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
- Diabetes Metab J. 2022;46(6):890-900. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0334
- 4,722 View
- 228 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We evaluated whether postpartum muscle mass affects the risk of type 2 diabetes mellitus (T2DM) in Korean women with gestational diabetes mellitus (GDM).
Methods
A total of 305 women with GDM (mean age, 34.9 years) was prospectively evaluated for incident prediabetes and T2DM from 2 months after delivery and annually thereafter. Appendicular skeletal muscle mass (ASM) was assessed with bioelectrical impedance analysis at the initial postpartum visit, and ASM, either divided by body mass index (BMI) or squared height, and the absolute ASM were used as muscle mass indices. The risk of incident prediabetes and T2DM was assessed according to tertiles of these indices using a logistic regression model.
Results
After a mean follow-up duration of 3.3 years, the highest ASM/BMI tertile group had a 61% lower risk of incident prediabetes and T2DM compared to the lowest tertile group, and this remained significant after we adjusted for covariates (adjusted odds ratio, 0.37; 95% confidence interval [CI], 0.15 to 0.92; P=0.032). Equivalent findings were observed in normal weight women (BMI <23 kg/m2), but this association was not significant for overweight women (BMI ≥23 kg/m2). Absolute ASM or ASM/height2 was not associated with the risk of postpartum T2DM.
Conclusion
A higher muscle mass, as defined by the ASM/BMI index, was associated with a lower risk of postpartum prediabetes and T2DM in Korean women with GDM. -
Citations
Citations to this article as recorded by- More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
Melanie S. Haines, Aaron Leong, Bianca C. Porneala, Victor W. Zhong, Cora E. Lewis, Pamela J. Schreiner, Karen K. Miller, James B. Meigs, Mercedes R. Carnethon
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(1): 105. CrossRef - The Association of the Triglyceride and Muscle to Fat Ratio During Early Pregnancy with the Development of Gestational Diabetes Mellitus
Fang Wang, Yuan-Yuan Bao, Kang Yu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3187. CrossRef - Correlation of body composition in early pregnancy on gestational diabetes mellitus under different body weights before pregnancy
Li Xintong, Xu Dongmei, Zhang Li, Cao Ruimin, Hao Yide, Cui Lingling, Chen Tingting, Guo Yingying, Li Jiaxin
Frontiers in Endocrinology.2022;[Epub] CrossRef
- More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
- Drug/Regimen
- Comparison of Serum Ketone Levels and Cardiometabolic Efficacy of Dapagliflozin versus Sitagliptin among Insulin-Treated Chinese Patients with Type 2 Diabetes Mellitus
- Chi-Ho Lee, Mei-Zhen Wu, David Tak-Wai Lui, Darren Shing-Hei Chan, Carol Ho-Yi Fong, Sammy Wing-Ming Shiu, Ying Wong, Alan Chun-Hong Lee, Joanne King-Yan Lam, Yu-Cho Woo, Karen Siu-Ling Lam, Kelvin Kai-Hang Yiu, Kathryn Choon-Beng Tan
- Diabetes Metab J. 2022;46(6):843-854. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0319
- 4,966 View
- 257 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Insulin-treated patients with long duration of type 2 diabetes mellitus (T2DM) are at increased risk of ketoacidosis related to sodium-glucose co-transporter 2 inhibitor (SGLT2i). The extent of circulating ketone elevation in these patients remains unknown. We conducted this study to compare the serum ketone response between dapagliflozin, an SGLT2i, and sitagliptin, a dipeptidyl peptidase-4 inhibitor, among insulin-treated T2DM patients.
Methods
This was a randomized, open-label, active comparator-controlled study involving 60 insulin-treated T2DM patients. Participants were randomized 1:1 for 24-week of dapagliflozin 10 mg daily or sitagliptin 100 mg daily. Serum β-hydroxybutyrate (BHB) levels were measured at baseline, 12 and 24 weeks after intervention. Comprehensive cardiometabolic assessments were performed with measurements of high-density lipoprotein cholesterol (HDL-C) cholesterol efflux capacity (CEC), vibration-controlled transient elastography and echocardiography.
Results
Among these 60 insulin-treated participants (mean age 58.8 years, diabetes duration 18.2 years, glycosylated hemoglobin 8.87%), as compared with sitagliptin, serum BHB levels increased significantly after 24 weeks of dapagliflozin (P=0.045), with a median of 27% increase from baseline. Change in serum BHB levels correlated significantly with change in free fatty acid levels. Despite similar glucose lowering, dapagliflozin led to significant improvements in body weight (P=0.006), waist circumference (P=0.028), HDL-C (P=0.041), CEC (P=0.045), controlled attenuation parameter (P=0.007), and liver stiffness (P=0.022). Average E/e’, an echocardiographic index of left ventricular diastolic dysfunction, was also significantly lower at 24 weeks in participants treated with dapagliflozin (P=0.037).
Conclusion
Among insulin-treated T2DM patients with long diabetes duration, compared to sitagliptin, dapagliflozin modestly increased ketone levels and was associated with cardiometabolic benefits. -
Citations
Citations to this article as recorded by- Serum thrombospondin‐2 level changes with liver stiffness improvement in patients with type 2 diabetes
Jimmy Ho Cheung Mak, David Tak‐Wai Lui, Carol Ho‐Yi Fong, Chloe Yu‐Yan Cheung, Ying Wong, Alan Chun‐Hong Lee, Ruby Lai‐Chong Hoo, Aimin Xu, Kathryn Choon‐Beng Tan, Karen Siu‐Ling Lam, Chi‐Ho Lee
Clinical Endocrinology.2024; 100(3): 230. CrossRef - SGLT-2 inhibitors as novel treatments of multiple organ fibrosis
Junpei Hu, Jianhui Teng, Shan Hui, Lihui Liang
Heliyon.2024; 10(8): e29486. CrossRef - Effect of sodium-glucose cotransporter protein-2 inhibitors on left ventricular hypertrophy in patients with type 2 diabetes: A systematic review and meta-analysis
Yao Wang, Yujie Zhong, Zhehao Zhang, Shuhao Yang, Qianying Zhang, Bingyang Chu, Xulin Hu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Effects of SGLT2 inhibitors on hepatic fibrosis and steatosis: A systematic review and meta-analysis
Peipei Zhou, Ying Tan, Zhenning Hao, Weilong Xu, Xiqiao Zhou, Jiangyi Yu
Frontiers in Endocrinology.2023;[Epub] CrossRef - The impact of sodium-glucose Cotransporter-2 inhibitors on lipid profile: A meta-analysis of 28 randomized controlled trials
Gang Fan, Dian long Guo, Hong Zuo
European Journal of Pharmacology.2023; 959: 176087. CrossRef
- Serum thrombospondin‐2 level changes with liver stiffness improvement in patients with type 2 diabetes
- Complications
- Fatty Acid-Binding Protein 4 in Patients with and without Diabetic Retinopathy
- Ping Huang, Xiaoqin Zhao, Yi Sun, Xinlei Wang, Rong Ouyang, Yanqiu Jiang, Xiaoquan Zhang, Renyue Hu, Zhuqi Tang, Yunjuan Gu
- Diabetes Metab J. 2022;46(4):640-649. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0195
- 3,390 View
- 193 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Background
Fatty acid-binding protein 4 (FABP4) has been demonstrated to be a predictor of early diabetic nephropathy. However, little is known about the relationship between FABP4 and diabetic retinopathy (DR). This study explored the value of FABP4 as a biomarker of DR in patients with type 2 diabetes mellitus (T2DM).
Methods
A total of 238 subjects were enrolled, including 20 healthy controls and 218 T2DM patients. Serum FABP4 levels were measured using a sandwich enzyme-linked immunosorbent assay. The grade of DR was determined using fundus fluorescence angiography. Based on the international classification of DR, all T2DM patients were classified into the following three subgroups: non-DR group, non-proliferative diabetic retinopathy (NPDR) group, and proliferative diabetic retinopathy (PDR) group. Multivariate logistic regression analyses were employed to assess the correlation between FABP4 levels and DR severity.
Results
FABP4 correlated positively with DR severity (r=0.225, P=0.001). Receiver operating characteristic curve analysis was used to assess the diagnostic potential of FABP4 in identifying DR, with an area under the curve of 0.624 (37% sensitivity, 83.6% specificity) and an optimum cut-off value of 76.4 μg/L. Multivariate logistic regression model including FABP4 as a categorized binary variable using the cut-off value of 76.4 μg/L showed that the concentration of FABP4 above the cut-off value increased the risk of NPDR (odds ratio [OR], 3.231; 95% confidence interval [CI], 1.574 to 6.632; P=0.001) and PDR (OR, 3.689; 95% CI, 1.306 to 10.424; P=0.014).
Conclusion
FABP4 may be used as a serum biomarker for the diagnosis of DR. -
Citations
Citations to this article as recorded by- Circulating AFABP, FGF21, and PEDF Levels as Prognostic Biomarkers of Sight-threatening Diabetic Retinopathy
Chi-Ho Lee, David Tak-Wai Lui, Chloe Yu-Yan Cheung, Carol Ho-Yi Fong, Michele Mae-Ann Yuen, Yu-Cho Woo, Wing-Sun Chow, Ian Yat-Hin Wong, Aimin Xu, Karen Siu-Ling Lam
The Journal of Clinical Endocrinology & Metabolism.2023; 108(9): e799. CrossRef - A Prediction Model for Sight-Threatening Diabetic Retinopathy Based on Plasma Adipokines among Patients with Mild Diabetic Retinopathy
Yaxin An, Bin Cao, Kun Li, Yongsong Xu, Wenying Zhao, Dong Zhao, Jing Ke, Takayuki Masaki
Journal of Diabetes Research.2023; 2023: 1. CrossRef
- Circulating AFABP, FGF21, and PEDF Levels as Prognostic Biomarkers of Sight-threatening Diabetic Retinopathy
- Complications
- Effect of the Glucagon-Like Peptide-1 Receptor Agonists on Autonomic Function in Subjects with Diabetes: A Systematic Review and Meta-Analysis
- Carla Greco, Daniele Santi, Giulia Brigante, Chiara Pacchioni, Manuela Simoni
- Diabetes Metab J. 2022;46(6):901-911. Published online April 12, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0314
- 4,460 View
- 266 Download
- 5 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
In addition to the metabolic effects in diabetes, glucagon-like peptide 1 receptor (GLP-1R) agonists lead to a small but substantial increase in heart rate (HR). However, the GLP-1R actions on the autonomic nervous system (ANS) in diabetes remain debated. Therefore, this meta-analysis evaluates the effect of GLP-1R agonist on measures of ANS function in diabetes.
Methods
According to the Cochrane Collaboration and Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) statement, we conducted a meta-analysis considering clinical trials in which the autonomic function was evaluated in diabetic subjects chronically treated with GLP-1R agonists. The outcomes were the change of ANS function measured by heart rate variability (HRV) and cardiac autonomic reflex tests (CARTs).
Results
In the studies enrolled, HR significantly increased after treatment (P<0.001), whereas low frequency/high frequency ratio did not differ (P=0.410); no changes in other measures of HRV were detected. Considering CARTs, only the 30:15 value derived from lying-to-standing test was significantly lower after treatment (P=0.002), but only two studies reported this measurement. No differences in other CARTs outcome were observed.
Conclusion
The meta-analysis confirms the HR increase but seems to exclude an alteration of the sympatho-vagal balance due to chronic treatment with GLP-1R agonists in diabetes, considering the available measures of ANS function. -
Citations
Citations to this article as recorded by- Liraglutide does not increase heart rate of diabetic patients during acute myocardial infarction
Qianyi Li, Chunxuan Wu, Shiqun Sun, Lingchao Yang, Yanyan Li, Yixin Niu, Li Zhang, Wei Li, Ying Yu
Journal of Diabetes.2024;[Epub] CrossRef - Hormonal Gut–Brain Signaling for the Treatment of Obesity
Eun Roh, Kyung Mook Choi
International Journal of Molecular Sciences.2023; 24(4): 3384. CrossRef - Effects of new hypoglycemic drugs on cardiac remodeling: a systematic review and network meta-analysis
Yi-lin Huang, Xiao-zhuo Xu, Jing Liu, Pin-yao Wang, Xue-li Wang, Hong-lin Feng, Cheng-jiang Liu, Xu Han
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Obesity and hypertension: Obesity medicine association (OMA) clinical practice statement (CPS) 2023
Tiffany Lowe Clayton, Angela Fitch, Harold Edward Bays
Obesity Pillars.2023; 8: 100083. CrossRef - Incretins and microvascular complications of diabetes: neuropathy, nephropathy, retinopathy and microangiopathy
Jonathan Goldney, Jack A. Sargeant, Melanie J. Davies
Diabetologia.2023; 66(10): 1832. CrossRef - Diabetes-Induced Cardiac Autonomic Neuropathy: Impact on Heart Function and Prognosis
Susumu Z. Sudo, Tadeu L. Montagnoli, Bruna de S. Rocha, Aimeé D. Santos, Mauro P. L. de Sá, Gisele Zapata-Sudo
Biomedicines.2022; 10(12): 3258. CrossRef
- Liraglutide does not increase heart rate of diabetic patients during acute myocardial infarction
- Type 1 Diabetes
- Identification of Key Genes and Pathways in Peripheral Blood Mononuclear Cells of Type 1 Diabetes Mellitus by Integrated Bioinformatics Analysis
- Xing Li, Mingyu Liao, Jiangheng Guan, Ling Zhou, Rufei Shen, Min Long, Jiaqing Shao
- Diabetes Metab J. 2022;46(3):451-463. Published online April 1, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0018
- 6,963 View
- 292 Download
- 6 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
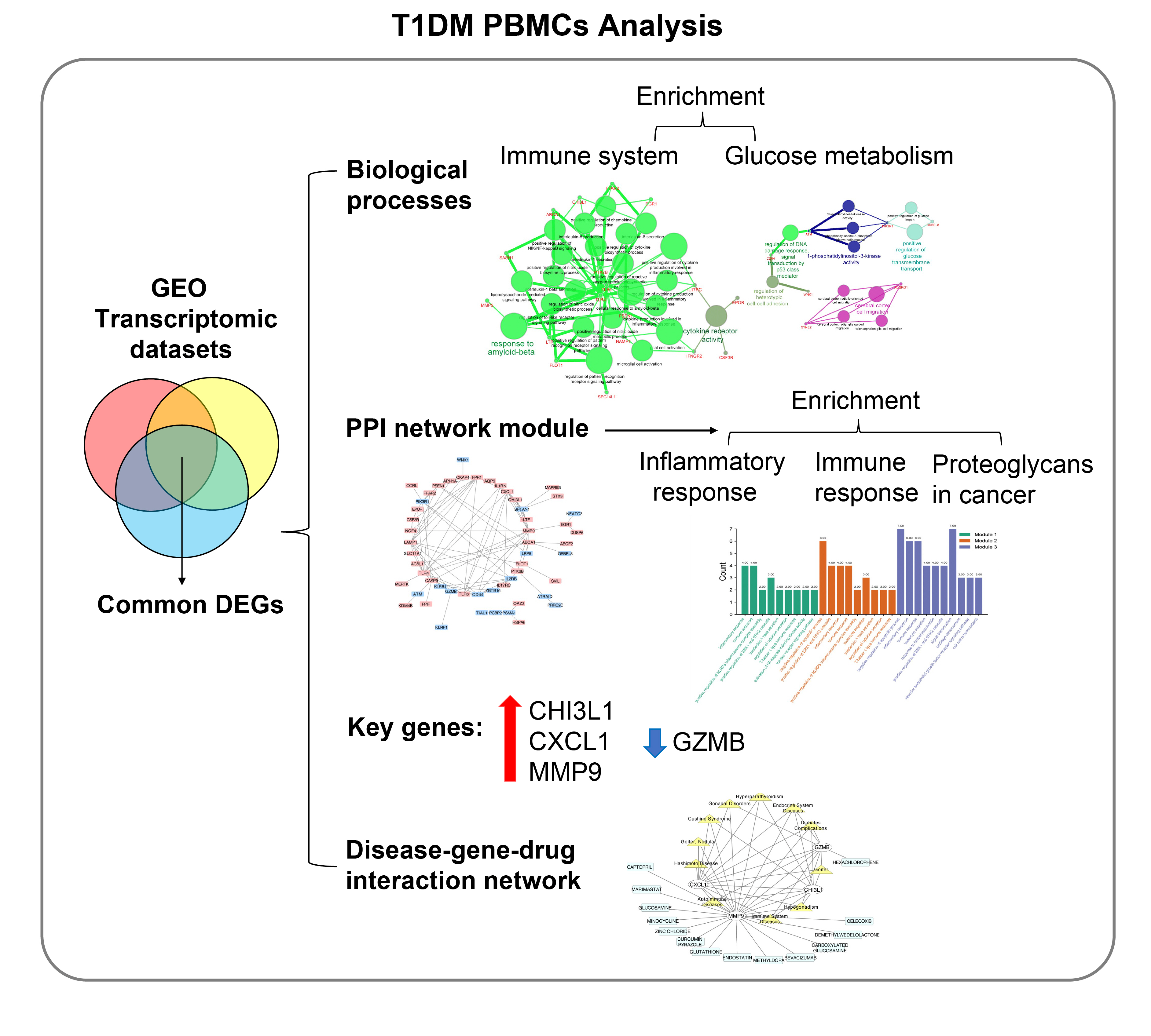
The onset and progression of type 1 diabetes mellitus (T1DM) is closely related to autoimmunity. Effective monitoring of the immune system and developing targeted therapies are frontier fields in T1DM treatment. Currently, the most available tissue that reflects the immune system is peripheral blood mononuclear cells (PBMCs). Thus, the aim of this study was to identify key PBMC biomarkers of T1DM.
Methods
Common differentially expressed genes (DEGs) were screened from the Gene Expression Omnibus (GEO) datasets GSE9006, GSE72377, and GSE55098, and PBMC mRNA expression in T1DM patients was compared with that in healthy participants by GEO2R. Gene Ontology, Kyoto Encyclopedia of Genes and Genomes (KEGG) pathway and protein-protein interaction (PPI) network analyses of DEGs were performed using the Cytoscape, DAVID, and STRING databases. The vital hub genes were validated by reverse transcription-polymerase chain reaction using clinical samples. The disease-gene-drug interaction network was built using the Comparative Toxicogenomics Database (CTD) and Drug Gene Interaction Database (DGIdb).
Results
We found that various biological functions or pathways related to the immune system and glucose metabolism changed in PBMCs from T1DM patients. In the PPI network, the DEGs of module 1 were significantly enriched in processes including inflammatory and immune responses and in pathways of proteoglycans in cancer. Moreover, we focused on four vital hub genes, namely, chitinase-3-like protein 1 (CHI3L1), C-X-C motif chemokine ligand 1 (CXCL1), matrix metallopeptidase 9 (MMP9), and granzyme B (GZMB), and confirmed them in clinical PBMC samples. Furthermore, the disease-gene-drug interaction network revealed the potential of key genes as reference markers in T1DM.
Conclusion
These results provide new insight into T1DM pathogenesis and novel biomarkers that could be widely representative reference indicators or potential therapeutic targets for clinical applications. -
Citations
Citations to this article as recorded by- Single-cell and transcriptomic analyses reveal the influence of diabetes on ovarian cancer
Zhihao Zhao, Qilin Wang, Fang Zhao, Junnan Ma, Xue Sui, Hyok Chol Choe, Peng Chen, Xue Gao, Lin Zhang
BMC Genomics.2024;[Epub] CrossRef - Bioinformatics analysis identifies TGF-β signaling pathway-associated molecular subtypes and gene signature in diabetic foot
Guanggang Du, Jie Chen, Xuezhu Zhu, Zongdong Zhu
iScience.2024; 27(3): 109094. CrossRef - Identification of Comorbidities, Genomic Associations, and Molecular Mechanisms for COVID-19 Using Bioinformatics Approaches
Shudeb Babu Sen Omit, Salma Akhter, Humayan Kabir Rana, A. R. M. Mahamudul Hasan Rana, Nitun Kumar Podder, Mahmudul Islam Rakib, Ashadun Nobi, Ali Imran
BioMed Research International.2023; 2023: 1. CrossRef - Advanced Delivery Strategies for Immunotherapy in Type I Diabetes Mellitus
Mingshu Huang, Weixing Chen, Min Wang, Yisheng Huang, Hongyu Liu, Yue Ming, Yuanxin Chen, Zhengming Tang, Bo Jia
BioDrugs.2023; 37(3): 331. CrossRef - Identification of the key genes of tuberculosis and construction of a diagnostic model via weighted gene co-expression network analysis
Baiying Li, Lifang Sun, Yaping Sun, Libo Zhen, Qi Qi, Ting Mo, Huijie Wang, Meihua Qiu, Qingshan Cai
Journal of Infection and Chemotherapy.2023; 29(11): 1046. CrossRef - Probing biological network in concurrent carcinomas and Type-2 diabetes for potential biomarker screening: An advanced computational paradigm
Abdullah Al Marzan, Shatila Shahi, Md Sakil Arman, Md Zafrul Hasan, Ajit Ghosh
Advances in Biomarker Sciences and Technology.2023; 5: 89. CrossRef - Transcriptional analysis of human peripheral blood mononuclear cells stimulated by Mycobacterium tuberculosis antigen
Jing Wei, Fangzheng Guo, Yamin Song, Kun Xu, Feiyang Lin, Kangsheng Li, Baiqing Li, Zhongqing Qian, Xiaojing Wang, Hongtao Wang, Tao Xu
Frontiers in Cellular and Infection Microbiology.2023;[Epub] CrossRef - Combining bioinformatics and machine learning algorithms to identify and analyze shared biomarkers and pathways in COVID-19 convalescence and diabetes mellitus
Jinru Shen, Yaolou Wang, Xijin Deng, Si Ri Gu Leng Sana
Frontiers in Endocrinology.2023;[Epub] CrossRef - Transcriptome analysis of peripheral blood mononuclear cells in patients with type 1 diabetes mellitus
Zhaoxiang Wang, Li Zhang, Fengyan Tang, Zhongming Yang, Mengzhu Wang, Jue Jia, Dong Wang, Ling Yang, Shao Zhong, Guoyue Yuan
Endocrine.2022; 78(2): 270. CrossRef
- Single-cell and transcriptomic analyses reveal the influence of diabetes on ovarian cancer
- Metabolic Risk/Epidemiology
- Associations between Weight-Adjusted Waist Index and Abdominal Fat and Muscle Mass: Multi-Ethnic Study of Atherosclerosis
- Ji Yoon Kim, Jimi Choi, Chantal A. Vella, Michael H. Criqui, Matthew A. Allison, Nam Hoon Kim
- Diabetes Metab J. 2022;46(5):747-755. Published online March 30, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0294
- 5,457 View
- 255 Download
- 29 Web of Science
- 35 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
The weight-adjusted waist index (WWI) reflected body compositional changes with aging. This study was to investigate the association of WWI with abdominal fat and muscle mass in a diverse race/ethnic population.
Methods
Computed tomography (CT) data from 1,946 participants for abdominal fat and muscle areas from the Multi-Ethnic Study of Atherosclerosis (785 Whites, 252 Asians, 406 African American, and 503 Hispanics) were used. Among them, 595 participants underwent repeated CT. The WWI was calculated as waist circumference (cm) divided by the square root of body weight (kg). The associations of WWI with abdominal fat and muscle measures were examined, and longitudinal changes in abdominal composition measures were compared.
Results
In all race/ethnic groups, WWI was positively correlated with total abdominal fat area (TFA), subcutaneous fat area, and visceral fat area, but negatively correlated with total abdominal muscle area (TMA) and abdominal muscle radiodensity (P<0.001 for all). WWI showed a linear increase with aging regardless of race and there were no significant differences in the WWI distribution between Whites, Asians, and African Americans. In longitudinal analyses, over 38.6 months of follow-up, all abdominal fat measures increased but muscle measures decreased, along with increase in WWI. The more the WWI increased, the more the TFA increased and the more the TMA decreased.
Conclusion
WWI showed positive associations with abdominal fat mass and negative associations with abdominal muscle mass, which likely reflects the abdominal compositional changes with aging in a multi-ethnic population. -
Citations
Citations to this article as recorded by- The association between weight-adjusted-waist index and depression: Results from NHANES 2005–2018
Meng Li, Xue Yu, Wenhui Zhang, Jiahui Yin, Lu Zhang, Guoshuai Luo, Yuanxiang Liu, Jiguo Yang
Journal of Affective Disorders.2024; 347: 299. CrossRef - Association between weight-adjusted-waist index and gallstones: an analysis of the National Health and Nutrition Examination Survey
Si-Hua Wen, Xin Tang, Tao Tang, Zheng-Rong Ye
BMC Gastroenterology.2024;[Epub] CrossRef - Association between weight-adjusted waist index and myopia in adolescents and young adults: results from NHANES 1999–2008
Xu Han Shi, Li Dong, Rui Heng Zhang, Wen Bin Wei
BMC Ophthalmology.2024;[Epub] CrossRef - Association between the weight-adjusted waist index and the odds of type 2 diabetes mellitus in United States adults: a cross-sectional study
Dongdong Zheng, Suzhen Zhao, Dan Luo, Feng Lu, Zhishen Ruan, Xiaokang Dong, Wenjing Chen
Frontiers in Endocrinology.2024;[Epub] CrossRef - Association between Weight-Adjusted Waist Index and depressive symptoms: A nationally representative cross-sectional study from NHANES 2005 to 2018
Hangyu Liu, Jin Zhi, Chuzhao Zhang, Shiyi Huang, Yang Ma, Dandan Luo, Lungang Shi
Journal of Affective Disorders.2024; 350: 49. CrossRef - Relationship between cognitive function and weight-adjusted waist index in people ≥ 60 years old in NHANES 2011–2014
Xue-li Wang, Hong-lin Feng, Xiao-zhuo Xu, Jing Liu, Xu Han
Aging Clinical and Experimental Research.2024;[Epub] CrossRef - Association between weight-adjusted waist index and non-alcoholic fatty liver disease: a population-based study
Changhui Yu, Shiming He, Maobin Kuang, Chao Wang, Xin Huang, Guotai Sheng, Yang Zou
BMC Endocrine Disorders.2024;[Epub] CrossRef - Association between weight-adjusted waist index and serum total testosterone in males aged 6–19 years in the United States: Data from NHANES 2013–2016
Zhifei Wu, Lingling Bao, Haiyan Wang, Jiajing Zheng, Yu Chen, Wenjuan Wang, Dongkai Qiu
Heliyon.2024; 10(6): e27520. CrossRef - Associations of weight-adjusted-waist index and depression with secondary infertility
Fei Sun, Min Liu, Shanshan Hu, Ruijie Xie, Huijuan Chen, Zhaona Sun, Huiya Bi
Frontiers in Endocrinology.2024;[Epub] CrossRef - Association between weight-adjusted-waist index and depression in US adults: A cross-sectional study
Yun Shen, Yahui Wu, Panru Luo, Minghan Fu, Kai Zhu, Jinsheng Wang
Journal of Affective Disorders.2024;[Epub] CrossRef - Age differences in the association of body mass index-defined obesity with abdominal aortic calcification
Tangmeng Guo, Lili Huang, Zhijian Luo, Huabo Zheng, Shengshuai Shan, Bei Cheng
Frontiers in Endocrinology.2024;[Epub] CrossRef - The relationship between weight-adjusted-waist index and diabetic kidney disease in patients with type 2 diabetes mellitus
Zhaoxiang Wang, Xuejing Shao, Wei Xu, Bingshuang Xue, Shao Zhong, Qichao Yang
Frontiers in Endocrinology.2024;[Epub] CrossRef - Assessment of existing anthropometric indices for screening sarcopenic obesity in older adults
Jin Eui Kim, Jimi Choi, Miji Kim, Chang Won Won
British Journal of Nutrition.2023; 129(5): 875. CrossRef - Relationship Between Weight-Adjusted Waist Index and Osteoporosis in the Senile in the United States from the National Health and Nutrition Examination Survey, 2017-2020
Yuxiang Lin, Zijie Liang, Anxin Zhang, Nuo Xu, Xuewen Pei, Nanbu Wang, Liang Zheng, Danghan Xu
Journal of Clinical Densitometry.2023; 26(2): 101361. CrossRef - The association of asthma duration with body mass index and Weight-Adjusted-Waist index in a nationwide study of the U.S. adults
Xiaoxiao Han, Xiaofang He, Gui Hao, Lifang Cao, Yinliang Qi, Kexing Han
European Journal of Medical Research.2023;[Epub] CrossRef - Relationship between weight-adjusted-waist index and erectile dysfunction in the United State: results from NHANES 2001-2004
Shangqi Cao, Xu Hu, Yanxiang Shao, Yaohui Wang, Yaxiong Tang, Shangqing Ren, Xiang Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - The association between weight-adjusted-waist index and total bone mineral density in adolescents: NHANES 2011–2018
Xiaohua Wang, Shuo Yang, Gansheng He, Lin Xie
Frontiers in Endocrinology.2023;[Epub] CrossRef - Asthma prevalence is increased in patients with high metabolism scores for visceral fat: study reports from the US
Qiushi Liu, Xiaoxiao Han, Yan Chen, Ying Gao, Wei Yang, Lewei Huang
Frontiers in Endocrinology.2023;[Epub] CrossRef - Positive association between weight-adjusted-waist index and dementia in the Chinese population with hypertension: a cross-sectional study
Wei Zhou, Yanyou Xie, Lingling Yu, Chao Yu, Huihui Bao, Xiaoshu Cheng
BMC Psychiatry.2023;[Epub] CrossRef - Associations between weight-adjusted waist index and bone mineral density: results of a nationwide survey
Ya Zhang, Haiyang Wu, Cheng Li, Changxiong Liu, Mingjiang Liu, Xiaozhu Liu, Qiming Yin, Xianzhe Li, Ruijie Xie
BMC Endocrine Disorders.2023;[Epub] CrossRef - Association of weight-adjusted-waist index with non-alcoholic fatty liver disease and liver fibrosis: a cross-sectional study based on NHANES
Qinggang Hu, Kexing Han, Jiapei Shen, Weijie Sun, Long Gao, Yufeng Gao
European Journal of Medical Research.2023;[Epub] CrossRef - Weight‐adjusted waist as an integrated index for fat, muscle and bone health in adults
Kyoung Jin Kim, Serhim Son, Kyeong Jin Kim, Sin Gon Kim, Nam Hoon Kim
Journal of Cachexia, Sarcopenia and Muscle.2023; 14(5): 2196. CrossRef - Association between weight-adjusted-waist index and female infertility: a population-based study
Zujun Wen, Xiang Li
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association between weight-adjusted-waist index and risk of cardiovascular diseases in United States adults: a cross-sectional study
Haiyang Fang, Feng Xie, Kai Li, Meng Li, Yanqing Wu
BMC Cardiovascular Disorders.2023;[Epub] CrossRef - Association between the weight-adjusted waist index and stroke: a cross-sectional study
Jiayi Ye, Yanjie Hu, Xinrong Chen, Zhe Yin, Xingzhu Yuan, Liping Huang, Ka Li
BMC Public Health.2023;[Epub] CrossRef - Association between weight-adjusted-waist index and chronic kidney disease: a cross-sectional study
Xiaowan Li, Lanyu Wang, Hongyi Zhou, Hongyang Xu
BMC Nephrology.2023;[Epub] CrossRef - Sex Differences in the Association of Weight-Adjusted-Waist Index with Sarcopenic Obesity: A Cross-Sectional Study of Hemodialysis Patients
Maolu Tian, Qin Lan, Fangfang Yu, Pinghong He, Shanshan Hu, Yan Zha
Metabolic Syndrome and Related Disorders.2023; 21(10): 596. CrossRef - Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
Eugene Han, Yong-ho Lee
Clinical and Molecular Hepatology.2023; 29(4): 980. CrossRef - The association of body mass index and weight waist adjustment index with serum ferritin in a national study of US adults
Hao Han, Ping Ni, Siqi Zhang, Xiaojuan Ji, Mingli Zhu, Wanyu Ma, Hongfeng Ge, Hailiang Chu
European Journal of Medical Research.2023;[Epub] CrossRef - The weight-adjusted-waist index and cognitive impairment among U.S. older adults: a population-based study
Xiao-tong Huang, Xiang Lv, Hong Jiang
Frontiers in Endocrinology.2023;[Epub] CrossRef - The relationship between weight-adjusted-waist index and total bone mineral density in adults aged 20-59
Meiqian Guo, Yi Lei, Xueqing Liu, Xiang Li, Yong Xu, Donghui Zheng
Frontiers in Endocrinology.2023;[Epub] CrossRef - Associations between weight-adjusted-waist index and infertility: Results from NHANES 2013 to 2020
Huanxin Zhong, Bin Yu, Fen Zhao, Hongyin Cui, Lifang You, Dao Feng, Yi Lu
Medicine.2023; 102(48): e36388. CrossRef - The association between weight-adjusted-waist index and increased urinary albumin excretion in adults: A population-based study
Zheng Qin, Kaixi Chang, Qinbo Yang, Qiao Yu, Ruoxi Liao, Baihai Su
Frontiers in Nutrition.2022;[Epub] CrossRef - Association between the weight-adjusted-waist index and abdominal aortic calcification in United States adults: Results from the national health and nutrition examination survey 2013–2014
Feng Xie, Yuan Xiao, Xiaozhong Li, Yanqing Wu
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef - The association between weight-adjusted-waist index and abdominal aortic calcification in adults aged ≥ 40 years: results from NHANES 2013–2014
Zheng Qin, Dongru Du, Yupei Li, Kaixi Chang, Qinbo Yang, Zhuyun Zhang, Ruoxi Liao, Baihai Su
Scientific Reports.2022;[Epub] CrossRef
- The association between weight-adjusted-waist index and depression: Results from NHANES 2005–2018
Short Communication
- Technology/Device
- Comparison of Laser and Conventional Lancing Devices for Blood Glucose Measurement Conformance and Patient Satisfaction in Diabetes Mellitus
- Jung A Kim, Min Jeong Park, Eyun Song, Eun Roh, So Young Park, Da Young Lee, Jaeyoung Kim, Ji Hee Yu, Ji A Seo, Kyung Mook Choi, Sei Hyun Baik, Hye Jin Yoo, Nan Hee Kim
- Diabetes Metab J. 2022;46(6):936-940. Published online March 30, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0293
- 5,252 View
- 256 Download
- 1 Web of Science
- 1 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Self-monitoring of capillary blood glucose is important for controlling diabetes. Recently, a laser lancing device (LMT-1000) that can collect capillary blood without skin puncture was developed. We enrolled 150 patients with type 1 or 2 diabetes mellitus. Blood sampling was performed on the same finger on each hand using the LMT-1000 or a conventional lancet. The primary outcome was correlation between glucose values using the LMT-1000 and that using a lancet. And we compared the pain and satisfaction of the procedures. The capillary blood sampling success rates with the LMT-1000 and lancet were 99.3% and 100%, respectively. There was a positive correlation (r=0.974, P<0.001) between mean blood glucose levels in the LMT-1000 (175.8±63.0 mg/dL) and conventional lancet samples (172.5±63.6 mg/dL). LMT-1000 reduced puncture pain by 75.0% and increased satisfaction by 80.0% compared to a lancet. We demonstrated considerable consistency in blood glucose measurements between samples from the LMT-1000 and a lancet, but improved satisfaction and clinically significant pain reduction were observed with the LMT-1000 compared to those with a lancet.
-
Citations
Citations to this article as recorded by- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
Chul Kyu Yun, Eui Kyung Choi, Hyung Jin Kim, Jaeyoung Kim, Byung Cheol Park, Kyuhee Park, Byung Min Choi
Journal of Perinatology.2024;[Epub] CrossRef
- Comparison between a laser-lancing device and automatic incision lancet for capillary blood sampling from the heel of newborn infants: a randomized feasibility trial
Editorial
- Variability of Metabolic Risk Factors: Causative Factor or Epiphenomenon?
- Hye Jin Yoo
- Diabetes Metab J. 2022;46(2):257-259. Published online March 24, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0060
- 3,060 View
- 131 Download
- 2 Web of Science
- 2 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Ji Eun Jun, You-Cheol Hwang, Kyu Jeong Ahn, Ho Yeon Chung, Geon-Ho Jahng, Soonchan Park, In-Kyung Jeong, Chang-Woo Ryu
Diabetes Research and Clinical Practice.2022; 191: 110067. CrossRef - Mean versus variability of lipid measurements over 6 years and incident cardiovascular events: More than a decade follow-up
Soroush Masrouri, Leila Cheraghi, Niloofar Deravi, Neda Cheraghloo, Maryam Tohidi, Fereidoun Azizi, Farzad Hadaegh
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef
- Association between carotid atherosclerosis and presence of intracranial atherosclerosis using three-dimensional high-resolution vessel wall magnetic resonance imaging in asymptomatic patients with type 2 diabetes
Reviews
- Others
- Links between Thyroid Disorders and Glucose Homeostasis
- Young Sil Eom, Jessica R. Wilson, Victor J. Bernet
- Diabetes Metab J. 2022;46(2):239-256. Published online March 24, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0013
- 10,839 View
- 634 Download
- 22 Web of Science
- 21 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Thyroid disorders and diabetes mellitus often coexist and are closely related. Several studies have shown a higher prevalence of thyroid disorders in patients with diabetes mellitus and vice versa. Thyroid hormone affects glucose homeostasis by impacting pancreatic β-cell development and glucose metabolism through several organs such as the liver, gastrointestinal tract, pancreas, adipose tissue, skeletal muscles, and the central nervous system. The present review discusses the effect of thyroid hormone on glucose homeostasis. We also review the relationship between thyroid disease and diabetes mellitus: type 1, type 2, and gestational diabetes, as well as guidelines for screening thyroid function with each disorder. Finally, we provide an overview of the effects of antidiabetic drugs on thyroid hormone and thyroid disorders.
-
Citations
Citations to this article as recorded by- Linkage and association of rs3110045 and rs28499085 variants in the thyrotropin-releasing hormone receptor (TRHR) gene with the risk of familial type 2 diabetes
Rongling Wu, Claudia Gragnoli
Aspects of Molecular Medicine.2024; 3: 100037. CrossRef - Obesity and Obesity-Related Thyroid Dysfunction: Any Potential Role for the Very Low-Calorie Ketogenic Diet (VLCKD)?
Sebastián Pablo Chapela, Alison Simancas-Racines, Florencia Ceriani, Andrés Luciano Nicolas Martinuzzi, María Paula Russo, Ana Karina Zambrano, Daniel Simancas-Racines, Ludovica Verde, Giovanna Muscogiuri, Christos S. Katsanos, Evelyn Frias-Toral, Luigi B
Current Nutrition Reports.2024;[Epub] CrossRef - View on Metformin: Antidiabetic and Pleiotropic Effects, Pharmacokinetics, Side Effects, and Sex-Related Differences
Guglielmina Froldi
Pharmaceuticals.2024; 17(4): 478. CrossRef - Thyroid Hormones and Diabetes in Euthyroid Hispanic/Latino Adults of Diverse Backgrounds: HCHS/SOL
Victoria Persky, Chibuzor Abasilim, Konstantina Tsintsifas, Tessa Day, Robert M Sargis, Martha Daviglus, Jianwen Cai, Sally Freels, Robert Kaplan, Carmen R Isasi, Amber Pirzada, Michelle L Meyer, Gregory A Talavera, Bharat Thyagarajan, Shivani Agarwal, No
Journal of the Endocrine Society.2024;[Epub] CrossRef - Managing Adults With Hypoglycemia
Christopher James Watson, Jonathan A. Edlow
Annals of Emergency Medicine.2023; 82(6): 705. CrossRef - Relationship of Glucose, C-peptide, Leptin, and BDNF in Maternal and Umbilical Vein Blood in Type-1 Diabetes
Josip Delmis, Slavko Oreskovic, Vesna Elvedji Gasparovic, Mirta Starcevic, Mislav Herman, Nada Dessardo, Vito Starcevic, Marina Ivanisevic
Nutrients.2023; 15(3): 600. CrossRef - Isolated Maternal Hypothyroxinemia May be Associated with Insulin
Requirement in Gestational Diabetes Mellitus
Ömercan Topaloğlu, Mehmet Uzun, Seda Nur Topaloğlu, Ibrahim Sahin
Hormone and Metabolic Research.2023; 55(04): 245. CrossRef - Association of urinary iodine concentration with prediabetes/diabetes in adults: Analysis of the NHANES 2005–2016
Jingmin Chen, Huanzhu Liang, Yuxuan Tan, Lin Wen, Ziang Guo, Jiyu Nie, Xiaoxiao Lin, Feng Huang, Jie Wang, Puyi Xing, Lihong Nie, Lihong Wang, Chunxia Jing
Journal of Trace Elements in Medicine and Biology.2023; 77: 127144. CrossRef - Central sensitivity to thyroid hormones is reduced in youths with overweight or obesity and impaired glucose tolerance
Procolo Di Bonito, Domenico Corica, Maria Rosaria Licenziati, Anna Di Sessa, Emanuele Miraglia del Giudice, Maria Felicia Faienza, Valeria Calcaterra, Francesca Franco, Giulio Maltoni, Giuliana Valerio, Malgorzata Wasniewska
Frontiers in Endocrinology.2023;[Epub] CrossRef - Association of thyroid stimulating hormone and time in range with risk of diabetic retinopathy in euthyroid type 2 diabetes
Yaxin Wang, Jingyi Lu, Jiaying Ni, Ming Wang, Yun Shen, Wei Lu, Wei Zhu, Yuqian Bao, Jian Zhou
Diabetes/Metabolism Research and Reviews.2023;[Epub] CrossRef - The circadian rhythm: an influential soundtrack in the diabetes story
Amirali Hariri, Mina Mirian, Ali Zarrabi, Mohammad Kohandel, Maryam Amini-Pozveh, Amir Reza Aref, Aliye Tabatabaee, Pranav Kumar Prabhakar, Ponnurengam Malliappan Sivakumar
Frontiers in Endocrinology.2023;[Epub] CrossRef - Folate deficiency may increase the risk for elevated TSH in patients with type 2 diabetes mellitus
Lin Lin, Yushan Du, Guanyu Niu, Shuangbo Xia, Jufen Liu
BMC Endocrine Disorders.2023;[Epub] CrossRef - L- Thyroxine ameliorates renal function in thyroidectomized diabetic nephropathy rats through downregulation of TGF- β1, Ang II and ET-1 expression
Zeinab H. El-Said, Sherihan I. Gouda, Hebatallah A. Mahgoub, S El_desouky, Neven A. Ebrahim
Egyptian Journal of Basic and Applied Sciences.2023; 10(1): 632. CrossRef - Thyroid dysfunction in children and adolescents affected by undernourished and overnourished eating disorders
Valeria Calcaterra, Vittoria Carlotta Magenes, Francesca Siccardo, Chiara Hruby, Martina Basso, Veronica Conte, Giulia Maggioni, Valentina Fabiano, Susanna Russo, Pierangelo Veggiotti, Gianvincenzo Zuccotti
Frontiers in Nutrition.2023;[Epub] CrossRef - Preventive Effect of Molecular Iodine in Pancreatic Disorders from Hypothyroid Rabbits
Julia Rodríguez-Castelán, Evangelina Delgado-González, Esteban Rodríguez-Benítez, Francisco Castelán, Estela Cuevas-Romero, Brenda Anguiano, Michael C. Jeziorski, Carmen Aceves
International Journal of Molecular Sciences.2023; 24(19): 14903. CrossRef - Hypothyroidism increases angiotensinogen gene expression associated with vascular smooth muscle cells cholesterol metabolism dysfunction and aorta remodeling in Psammomys obesus
Samia Neggazi, Nadjiba Hamlat, Sihem Berdja, Saliha Boumaza, Leila Smail, Michel Beylot, Souhila Aouichat-Bouguerra
Scientific Reports.2023;[Epub] CrossRef - The Correlation Between Thyroid Parameters and the Ratios of Neutrophil/Lymphocyte and Platelet/Lymphocyte in Euthyroid Type 2 Diabetic Patients
Hui Chen, Jun-Qiang Ju, Xiao-Wu Qian, Zheng-Tai Zhu, Chun-Zhi Zhao, Zhe Liu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3763. CrossRef - Effects of high-intensity interval training program on pituartry function in basketball players: a randomized controlled trial
Recep Soslu, Abdullah Uysal, Meltem Devrilmez, İsmail Can Çuvalcıoğlu, Ali Ahmet Doğan, Sülbiye Karaburgu, Murat Taş
Frontiers in Physiology.2023;[Epub] CrossRef - Selenium and Selenoproteins at the Intersection of Type 2 Diabetes and Thyroid Pathophysiology
Francesca Gorini, Cristina Vassalle
Antioxidants.2022; 11(6): 1188. CrossRef - TSH levels within the normal range and risk of cardiovascular and all-cause mortality among individuals with diabetes
Ping Zhu, Guojuan Lao, Chuping Chen, Lihui Luo, Jing Gu, Jianmin Ran
Cardiovascular Diabetology.2022;[Epub] CrossRef - Metabolite Changes during the Transition from Hyperthyroidism to Euthyroidism in Patients with Graves’ Disease
Ho Yeop Lee, Byeong Chang Sim, Ha Thi Nga, Ji Sun Moon, Jingwen Tian, Nguyen Thi Linh, Sang Hyeon Ju, Dong Wook Choi, Daiki Setoyama, Hyon-Seung Yi
Endocrinology and Metabolism.2022; 37(6): 891. CrossRef
- Linkage and association of rs3110045 and rs28499085 variants in the thyrotropin-releasing hormone receptor (TRHR) gene with the risk of familial type 2 diabetes
- Metabolic Risk/Epidemiology
- Not Control but Conquest: Strategies for the Remission of Type 2 Diabetes Mellitus
- Jinyoung Kim, Hyuk-Sang Kwon
- Diabetes Metab J. 2022;46(2):165-180. Published online March 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0377
- 8,690 View
- 508 Download
- 11 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - A durable normoglycemic state was observed in several studies that treated type 2 diabetes mellitus (T2DM) patients through metabolic surgery, intensive therapeutic intervention, or significant lifestyle modification, and it was confirmed that the functional β-cell mass was also restored to a normal level. Therefore, expert consensus introduced the concept of remission as a common term to express this phenomenon in 2009. Throughout this article, we introduce the recently updated consensus statement on the remission of T2DM in 2021 and share our perspective on the remission of diabetes. There is a need for more research on remission in Korea as well as in Western countries. Remission appears to be prompted by proactive treatment for hyperglycemia and significant weight loss prior to irreversible β-cell changes. T2DM is not a diagnosis for vulnerable individuals to helplessly accept. We attempt to explain how remission of T2DM can be achieved through a personalized approach. It may be necessary to change the concept of T2DM towards that of an urgent condition that requires rapid intervention rather than a chronic, progressive disease. We must grasp this paradigm shift in our understanding of T2DM for the benefit of our patients as endocrine experts.
-
Citations
Citations to this article as recorded by- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Jinyoung Kim, Bongseong Kim, Mee Kyoung Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(2): 567. CrossRef - Mechanisms and the strategy for remission of type 2 diabetes mellitus
Tien‐Jyun Chang
Journal of Diabetes Investigation.2023; 14(3): 351. CrossRef - Remission of type 2 diabetes: A critical appraisal
Michele Ricci, Juan José Mancebo-Sevilla, Lidia Cobos Palacios, Jaime Sanz-Cánovas, Almudena López-Sampalo, Halbert Hernández-Negrin, Miguel Angel Pérez-Velasco, Luis M. Pérez-Belmonte, Maria Rosa Bernal-López, Ricardo Gómez-Huelgas
Frontiers in Endocrinology.2023;[Epub] CrossRef - Incidence and predictors of remission and relapse of type 2 diabetes mellitus in Japan: Analysis of a nationwide patient registry (JDDM73)
Kazuya Fujihara, Laymon Khin, Koshiro Murai, Yurie Yamazaki, Kahori Tsuruoka, Noriko Yagyuda, Katsuya Yamazaki, Hiroshi Maegawa, Shiro Tanaka, Satoru Kodama, Hirohito Sone
Diabetes, Obesity and Metabolism.2023; 25(8): 2227. CrossRef - Use of SGLT2 inhibitors after bariatric/metabolic surgery: Risk/benefit balance
André J. Scheen
Diabetes & Metabolism.2023; 49(4): 101453. CrossRef - Cardiovascular Risk Reduction in Type 2 Diabetes: Further Insights into the Power of Weight Loss and Exercise
Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(3): 302. CrossRef - Unlocking the Potential of Type 2 Diabetes Mellitus Remission
Prakriti Sharma, Swarupa Chakole
Cureus.2023;[Epub] CrossRef - Global research trends of diabetes remission: a bibliometric study
Xue Yang, Zhiwei He, Qilin Chen, Yu Chen, Guofang Chen, Chao Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Gastrointestinal adverse events of tirzepatide in the treatment of type 2 diabetes mellitus: A meta-analysis and trials sequential analysis
Keke Tong, Shuang Yin, Yunfeng Yu, Xinyu Yang, Gang Hu, Fei Zhang, Zhenjie Liu
Medicine.2023; 102(43): e35488. CrossRef - Optimal dose of tirzepatide for type 2 diabetes mellitus: A meta-analysis and trial sequential analysis
Yunfeng Yu, Gang Hu, Shuang Yin, Xinyu Yang, Manli Zhou, Weixiong Jian
Frontiers in Cardiovascular Medicine.2022;[Epub] CrossRef
- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Response
- Trends and Risk Factors of Metabolic Syndrome among Korean Adolescents, 2007 to 2018 (Diabetes Metab J 2021;45:880-9)
- Jiun Chae, Moon Young Seo, Shin-Hye Kim, Mi Jung Park
- Diabetes Metab J. 2022;46(2):351-353. Published online March 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0367
- 2,553 View
- 105 Download
Letter
- Trends and Risk Factors of Metabolic Syndrome among Korean Adolescents, 2007 to 2018 (Diabetes Metab J 2021;45:880-9)
- Dae Jung Kim
- Diabetes Metab J. 2022;46(2):349-350. Published online March 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0353
- 2,572 View
- 124 Download
Reviews
- Complications
- Peripheral Neuropathy Phenotyping in Rat Models of Type 2 Diabetes Mellitus: Evaluating Uptake of the Neurodiab Guidelines and Identifying Future Directions
- Md Jakir Hossain, Michael D. Kendig, Meg E. Letton, Margaret J. Morris, Ria Arnold
- Diabetes Metab J. 2022;46(2):198-221. Published online March 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0347
- 5,186 View
- 225 Download
- 4 Web of Science
- 4 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Diabetic peripheral neuropathy (DPN) affects over half of type 2 diabetes mellitus (T2DM) patients, with an urgent need for effective pharmacotherapies. While many rat and mouse models of T2DM exist, the phenotyping of DPN has been challenging with inconsistencies across laboratories. To better characterize DPN in rodents, a consensus guideline was published in 2014 to accelerate the translation of preclinical findings. Here we review DPN phenotyping in rat models of T2DM against the ‘Neurodiab’ criteria to identify uptake of the guidelines and discuss how DPN phenotypes differ between models and according to diabetes duration and sex. A search of PubMed, Scopus and Web of Science databases identified 125 studies, categorised as either diet and/or chemically induced models or transgenic/spontaneous models of T2DM. The use of diet and chemically induced T2DM models has exceeded that of transgenic models in recent years, and the introduction of the Neurodiab guidelines has not appreciably increased the number of studies assessing all key DPN endpoints. Combined high-fat diet and low dose streptozotocin rat models are the most frequently used and well characterised. Overall, we recommend adherence to Neurodiab guidelines for creating better animal models of DPN to accelerate translation and drug development.
-
Citations
Citations to this article as recorded by- SIRT3 alleviates painful diabetic neuropathy by mediating the FoxO3a‐PINK1‐Parkin signaling pathway to activate mitophagy
Jing Yang, Zhuoying Yu, Ye Jiang, Zixian Zhang, Yue Tian, Jie Cai, Min Wei, Yanhan Lyu, Dongsheng Yang, Shixiong Shen, Guo‐Gang Xing, Min Li
CNS Neuroscience & Therapeutics.2024;[Epub] CrossRef - Compound Qiying Granules alleviates diabetic peripheral neuropathy by inhibiting endoplasmic reticulum stress and apoptosis
Yan Hu, Chen Chen, Zhengting Liang, Tao Liu, Xiaoling Hu, Guanying Wang, Jinxia Hu, Xiaolin Xie, Zhiyan Liu
Molecular Medicine.2023;[Epub] CrossRef - HCV affects KATP channels through GnT-IVa-mediated N-glycosylation of GLUT2 on the surface of pancreatic β-cells leading to impaired insulin secretion
Ben Niu, Lijing Ma, Lixuan Yao, Yating Zhang, Heng Su
Endocrine.2023;[Epub] CrossRef - Multimodal Comparison of Diabetic Neuropathy in Aged Streptozotocin-Treated Sprague–Dawley and Zucker Diabetic Fatty Rats
Annalisa Canta, Valentina A. Carozzi, Alessia Chiorazzi, Cristina Meregalli, Norberto Oggioni, Virginia Rodriguez-Menendez, Barbara Sala, Roberto Cosimo Melcangi, Silvia Giatti, Raffaella Lombardi, Roberto Bianchi, Paola Marmiroli, Guido Cavaletti
Biomedicines.2022; 11(1): 20. CrossRef
- SIRT3 alleviates painful diabetic neuropathy by mediating the FoxO3a‐PINK1‐Parkin signaling pathway to activate mitophagy
- Complications
- Pathophysiologic Mechanisms and Potential Biomarkers in Diabetic Kidney Disease
- Chan-Young Jung, Tae-Hyun Yoo
- Diabetes Metab J. 2022;46(2):181-197. Published online March 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0329
- 11,788 View
- 784 Download
- 41 Web of Science
- 45 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Although diabetic kidney disease (DKD) remains the leading cause of end-stage kidney disease eventually requiring chronic kidney replacement therapy, the prevalence of DKD has failed to decline over the past 30 years. In order to reduce disease prevalence, extensive research has been ongoing to improve prediction of DKD onset and progression. Although the most commonly used markers of DKD are albuminuria and estimated glomerular filtration rate, their limitations have encouraged researchers to search for novel biomarkers that could improve risk stratification. Considering that DKD is a complex disease process that involves several pathophysiologic mechanisms such as hyperglycemia induced inflammation, oxidative stress, tubular damage, eventually leading to kidney damage and fibrosis, many novel biomarkers that capture one specific mechanism of the disease have been developed. Moreover, the increasing use of high-throughput omic approaches to analyze biological samples that include proteomics, metabolomics, and transcriptomics has emerged as a strong tool in biomarker discovery. This review will first describe recent advances in the understanding of the pathophysiology of DKD, and second, describe the current clinical biomarkers for DKD, as well as the current status of multiple potential novel biomarkers with respect to protein biomarkers, proteomics, metabolomics, and transcriptomics.
-
Citations
Citations to this article as recorded by- Role of polyphenols in the management of diabetic complications
Jeevika Raina, Atika Firdous, Gurvinder Singh, Rajesh Kumar, Charanjit Kaur
Phytomedicine.2024; 122: 155155. CrossRef - Role of MCP-1 as an inflammatory biomarker in nephropathy
Yanlong Liu, Ke Xu, Yuhua Xiang, Boyan Ma, Hailong Li, Yuan Li, Yue Shi, Shuju Li, Yan Bai
Frontiers in Immunology.2024;[Epub] CrossRef - Urinary podocyte stress marker as a prognostic indicator for diabetic kidney disease
Lingfeng Zeng, Jack Kit-Chung Ng, Winston Wing-Shing Fung, Gordon Chun-Kau Chan, Kai-Ming Chow, Cheuk-Chun Szeto
BMC Nephrology.2024;[Epub] CrossRef - Identification and validation of immune and cuproptosis - related genes for diabetic nephropathy by WGCNA and machine learning
Yubing Chen, Lijuan Liao, Baoju Wang, Zhan Wu
Frontiers in Immunology.2024;[Epub] CrossRef - Specific Alternation of Gut Microbiota and the Role of Ruminococcus gnavus in the Development of Diabetic Nephropathy
Jinni Hong, Tingting Fu, Weizhen Liu, Yu Du, Junmin Bu, Guojian Wei, Miao Yu, Yanshan Lin, Cunyun Min, Datao Lin
Journal of Microbiology and Biotechnology.2024; 34(3): 547. CrossRef - A Narrative Review of New Treatment Options for Diabetic Nephropathy
Aadhira Pillai, Darshna Fulmali
Cureus.2023;[Epub] CrossRef - Bamboo leaf: A review of traditional medicinal property, phytochemistry, pharmacology, and purification technology
Yaqian Cheng, Siqi Wan, Linna Yao, Ding Lin, Tong Wu, Yongjian Chen, Ailian Zhang, Chenfei Lu
Journal of Ethnopharmacology.2023; 306: 116166. CrossRef - Molecular Pathways of Diabetic Kidney Disease Inferred from Proteomics
Lan Wei, Yuanyuan Han, Chao Tu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 117. CrossRef - Omics and Artificial Intelligence in Kidney Diseases
Nadja Grobe, Josef Scheiber, Hanjie Zhang, Christian Garbe, Xiaoling Wang
Advances in Kidney Disease and Health.2023; 30(1): 47. CrossRef - Intestinal microbiome diversity of diabetic and non-diabetic kidney disease: Current status and future perspective
Soumik Das, Ramanathan Gnanasambandan
Life Sciences.2023; 316: 121414. CrossRef - Pediatric Diabetic Nephropathy: Novel Insights from microRNAs
Francesca Lanzaro, Annalisa Barlabà, Angelica De Nigris, Federica Di Domenico, Valentina Verde, Emanuele Miraglia del Giudice, Anna Di Sessa
Journal of Clinical Medicine.2023; 12(4): 1447. CrossRef - Novel Biomarkers of Diabetic Kidney Disease
Jorge Rico-Fontalvo, Gustavo Aroca-Martínez, Rodrigo Daza-Arnedo, José Cabrales, Tomás Rodríguez-Yanez, María Cardona-Blanco, Juan Montejo-Hernández, Dairo Rodelo Barrios, Jhonny Patiño-Patiño, Elber Osorio Rodríguez
Biomolecules.2023; 13(4): 633. CrossRef - Diabetic vascular diseases: molecular mechanisms and therapeutic strategies
Yiwen Li, Yanfei Liu, Shiwei Liu, Mengqi Gao, Wenting Wang, Keji Chen, Luqi Huang, Yue Liu
Signal Transduction and Targeted Therapy.2023;[Epub] CrossRef - Metabolic phenotypes and risk of end-stage kidney disease in patients with type 2 diabetes
Lijun Zhao, Yutong Zou, Yucheng Wu, Linli Cai, Yuancheng Zhao, Yiting Wang, Xiang Xiao, Qing Yang, Jia Yang, Honghong Ren, Nanwei Tong, Fang Liu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Identification of a New RNA and Protein Integrated Biomarker Panel Associated with Kidney Function Impairment in DKD: Translational Implications
Alessandra Scamporrino, Stefania Di Mauro, Agnese Filippello, Grazia Di Marco, Antonino Di Pino, Roberto Scicali, Maurizio Di Marco, Emanuele Martorana, Roberta Malaguarnera, Francesco Purrello, Salvatore Piro
International Journal of Molecular Sciences.2023; 24(11): 9412. CrossRef - Increased serum PCSK9 levels are associated with renal function impairment in patients with type 2 diabetes mellitus
Zhicai Feng, Xiangyu Liao, Hao Zhang, Juan Peng, Zhijun Huang, Bin Yi
Renal Failure.2023;[Epub] CrossRef - Analysis of Serum Pyrodeath Re-lated Proteins and Renal Injury in Patients with Type 2 DKD
茹洁 马
Asian Case Reports in Emergency Medicine.2023; 11(02): 53. CrossRef - Loganin reduces diabetic kidney injury by inhibiting the activation of NLRP3 inflammasome-mediated pyroptosis
Xiangri Kong, Yunyun Zhao, Xingye Wang, Yongjiang Yu, Ying Meng, Guanchi Yan, Miao Yu, Lihong Jiang, Wu Song, Bingmei Wang, Xiuge Wang
Chemico-Biological Interactions.2023; 382: 110640. CrossRef - Machine-learning algorithm-based prediction of a diagnostic model based on oxidative stress-related genes involved in immune infiltration in diabetic nephropathy patients
Heng-Mei Zhu, Na Liu, Dong-Xuan Sun, Liang Luo
Frontiers in Immunology.2023;[Epub] CrossRef - The roles of gut microbiota and its metabolites in diabetic nephropathy
Hui Zhao, Cheng-E Yang, Tian Liu, Ming-Xia Zhang, Yan Niu, Ming Wang, Jun Yu
Frontiers in Microbiology.2023;[Epub] CrossRef - High triglyceride levels increase the risk of diabetic microvascular complications: a cross-sectional study
Jiahang Li, Lei Shi, Guohong Zhao, Fei Sun, Zhenxing Nie, Zhongli Ge, Bin Gao, Yan Yang
Lipids in Health and Disease.2023;[Epub] CrossRef - Correlation of Kidney Injury Molecule-1 and Nephrin Levels in Iraqi Patients with Diabetic Nephropathy
Raghda Hisham Aljorani, Eman Saadi Saleh , Khalaf Gata Hussein Al Mohammadawi
Al-Rafidain Journal of Medical Sciences ( ISSN 2789-3219 ).2023; 5: 99. CrossRef - Diabetic Nephropathy: Significance of Determining Oxidative Stress and Opportunities for Antioxidant Therapies
Marina Darenskaya, Sergey Kolesnikov, Natalya Semenova, Lyubov Kolesnikova
International Journal of Molecular Sciences.2023; 24(15): 12378. CrossRef - Evaluation of Neutrophil/Lymphocyte Ratio, Low-Density Lipoprotein/Albumin Ratio, and Red Cell Distribution Width/Albumin Ratio in the Estimation of Proteinuria in Uncontrolled Diabetic Patients
Duygu Tutan, Murat Doğan
Cureus.2023;[Epub] CrossRef - Hedysarum polybotrys polysaccharide attenuates renal inflammatory infiltration and fibrosis in diabetic mice by inhibiting the HMGB1/RAGE/TLR4 pathway
Changqing Xu, Yanxu Cheng, Zongmei Liu, Xiaoyan Fu
Experimental and Therapeutic Medicine.2023;[Epub] CrossRef - Abdominal adipose tissue and type 2 diabetic kidney disease: adipose radiology assessment, impact, and mechanisms
Fei Lu, Jinlei Fan, Fangxuan Li, Lijing Liu, Zhiyu Chen, Ziyu Tian, Liping Zuo, Dexin Yu
Abdominal Radiology.2023; 49(2): 560. CrossRef - Inhibition of MD2 by natural product-drived JM-9 attenuates renal inflammation and diabetic nephropathy in mice
Minxiu Wang, Qianhui Zhang, Shuaijie Lou, Leiming Jin, Gaojun Wu, Wenqi Wu, Qidong Tang, Yi Wang, Xiaohong Long, Ping Huang, Wu Luo, Guang Liang
Biomedicine & Pharmacotherapy.2023; 168: 115660. CrossRef - Multifaceted relationship between diabetes and kidney diseases: Beyond diabetes
Pasquale Esposito, Daniela Picciotto, Francesca Cappadona, Francesca Costigliolo, Elisa Russo, Lucia Macciò, Francesca Viazzi
World Journal of Diabetes.2023; 14(10): 1450. CrossRef - Mitochondrial antiviral signaling protein: a potential therapeutic target in renal disease
Meng Wu, Zhiyin Pei, Guangfeng Long, Hongbing Chen, Zhanjun Jia, Weiwei Xia
Frontiers in Immunology.2023;[Epub] CrossRef - Research progress on multiple cell death pathways of podocytes in diabetic kidney disease
Can Yang, Zhen Zhang, Jieting Liu, Peijian Chen, Jialing Li, Haiying Shu, Yanhui Chu, Luxin Li
Molecular Medicine.2023;[Epub] CrossRef - Quantitative profiling of carboxylic compounds by gas chromatography-mass spectrometry for revealing biomarkers of diabetic kidney disease
Rongrong Zhu, Yan Yuan, Rourou Qi, Jianying Liang, Yan Shi, Hongbo Weng
Journal of Chromatography B.2023; 1231: 123930. CrossRef - Jiangtang Decoction Ameliorates Diabetic Kidney Disease Through the Modulation of the Gut Microbiota
Jinni Hong, Tingting Fu, Weizhen Liu, Yu Du, Junmin Bu, Guojian Wei, Miao Yu, Yanshan Lin, Cunyun Min, Datao Lin
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3707. CrossRef - GLP-1RA Combined with SGLT2 Inhibitors for the Treatment of Diabetic Kidney Disease: A Meta Analysis
莹 郭
Advances in Clinical Medicine.2023; 13(11): 18117. CrossRef - Potential application of Klotho as a prognostic biomarker for patients with diabetic kidney disease: a meta-analysis of clinical studies
Li Xia Yu, Min Yue Sha, Yue Chen, Fang Tan, Xi Liu, Shasha Li, Qi-Feng Liu
Therapeutic Advances in Chronic Disease.2023;[Epub] CrossRef - Single-Cell RNA Sequencing Reveals RAC1 Involvement in Macrophages Efferocytosis in Diabetic Kidney Disease
Yi Song, Yifan Liu, Feng Guo, Lin Zhao, Guijun Qin
Inflammation.2023;[Epub] CrossRef - Research progress of natural active compounds on improving podocyte function to reduce proteinuria in diabetic kidney disease
Le Gong, Rui Wang, Xinyu Wang, Jing Liu, Zhaodi Han, Qian Li, Yi Jin, Hui Liao
Renal Failure.2023;[Epub] CrossRef - Identification of potential crosstalk genes and mechanisms between periodontitis and diabetic nephropathy through bioinformatic analysis
Huijuan Lu, Jia Sun, Jieqiong Sun
Medicine.2023; 102(52): e36802. CrossRef - Mitochondrial RNAs as Potential Biomarkers of Functional Impairment in Diabetic Kidney Disease
Stefania Di Mauro, Alessandra Scamporrino, Agnese Filippello, Maurizio Di Marco, Maria Teresa Di Martino, Francesca Scionti, Antonino Di Pino, Roberto Scicali, Roberta Malaguarnera, Francesco Purrello, Salvatore Piro
International Journal of Molecular Sciences.2022; 23(15): 8198. CrossRef - Renoprotective Mechanism of Sodium-Glucose Cotransporter 2 Inhibitors: Focusing on Renal Hemodynamics
Nam Hoon Kim, Nan Hee Kim
Diabetes & Metabolism Journal.2022; 46(4): 543. CrossRef - Partial Synthetic PPARƳ Derivative Ameliorates Aorta Injury in Experimental Diabetic Rats Mediated by Activation of miR-126-5p Pi3k/AKT/PDK 1/mTOR Expression
Yasmin M. Ahmed, Raha Orfali, Nada S. Abdelwahab, Hossam M. Hassan, Mostafa E. Rateb, Asmaa M. AboulMagd
Pharmaceuticals.2022; 15(10): 1175. CrossRef - Polydatin attenuates tubulointerstitial fibrosis in diabetic kidney disease by inhibiting YAP expression and nuclear translocation
Manlin He, Lan Feng, Yang Chen, Bin Gao, Yiwei Du, Lu Zhou, Fei Li, Hongbao Liu
Frontiers in Physiology.2022;[Epub] CrossRef - Prevalence of diabetic nephropathy in the diabetes mellitus population: A protocol for systematic review and meta-analysis
Sicheng Li, Huidi Xie, Yang Shi, Hongfang Liu
Medicine.2022; 101(42): e31232. CrossRef - Stratification of diabetic kidney diseases via data-independent acquisition proteomics–based analysis of human kidney tissue specimens
Qinghua Huang, Xianming Fei, Zhaoxian Zhong, Jieru Zhou, Jianguang Gong, Yuan Chen, Yiwen Li, Xiaohong Wu
Frontiers in Endocrinology.2022;[Epub] CrossRef - Novel biomarkers and therapeutic approaches for diabetic retinopathy and nephropathy: Recent progress and future perspectives
Ziyan Xie, Xinhua Xiao
Frontiers in Endocrinology.2022;[Epub] CrossRef - Diabetic Kidney Disease
Susanne B. Nicholas, Amy K. Mottl
Nephrology Self-Assessment Program.2022; 21(5): 394. CrossRef
- Role of polyphenols in the management of diabetic complications
Short Communication
- Others
- Comparison of Insulin-Treated Patients with Ambiguous Diabetes Type with Definite Type 1 and Type 2 Diabetes Mellitus Subjects: A Clinical Perspective
- Insa Laspe, Juris J. Meier, Michael A. Nauck
- Diabetes Metab J. 2023;47(1):140-146. Published online March 22, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0322
- 65,535 View
- 183 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
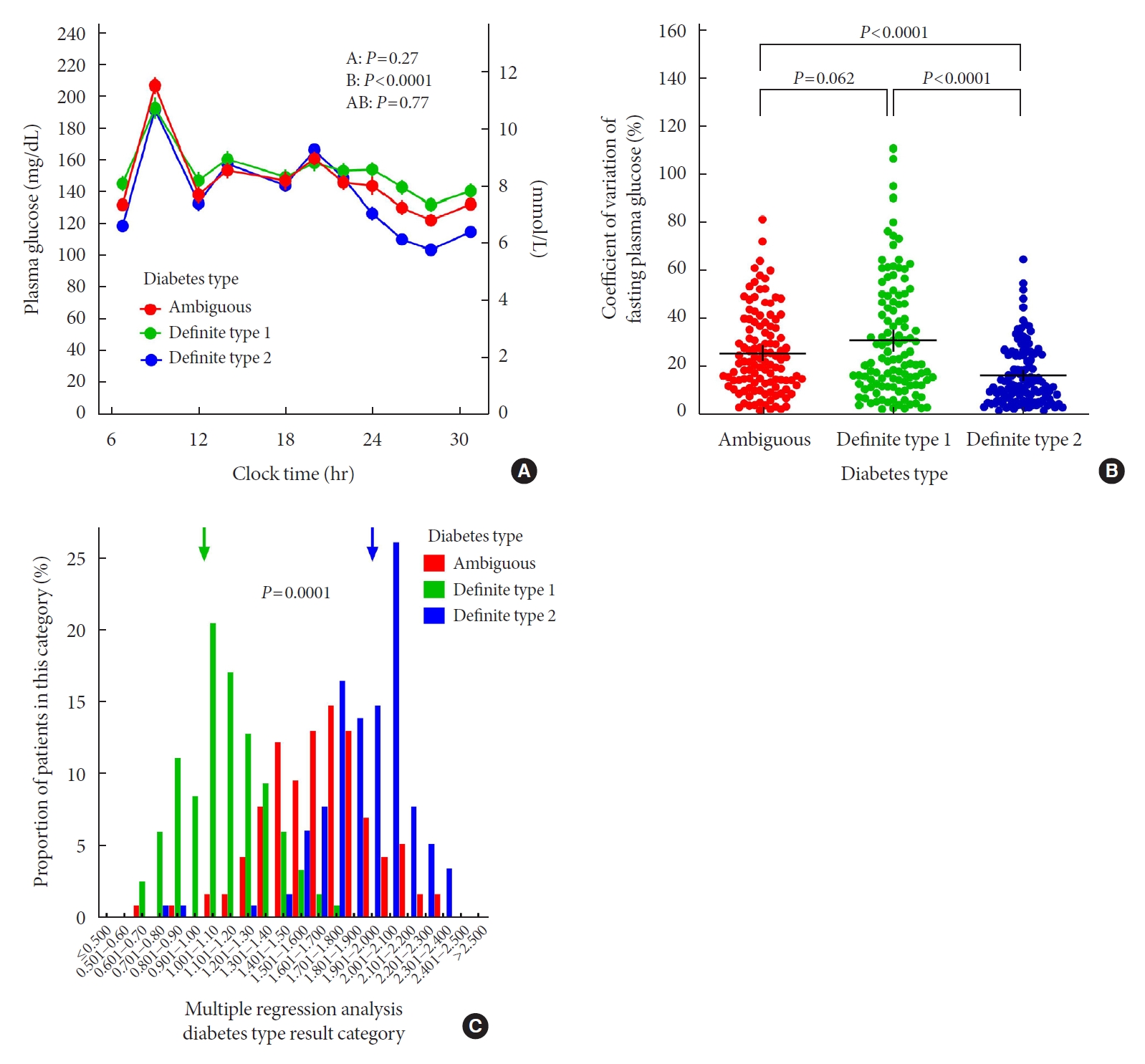
ePub - In clinical practice, the distinction between type 1 diabetes mellitus (T1DM) and type 2 diabetes mellitus (T2DM) can be challenging, leaving patients with “ambiguous” diabetes type. Insulin-treated patients (n=115) previously diagnosed with T2DM had to be re-classified based on clinical phenotype and laboratory results, and were operationally defined as having an ambiguous diabetes type. They were compared against patients with definite T1DM and T2DM regarding 12 clinical and laboratory features typically different between diabetes types. Characteristics of patients with ambiguous diabetes type, representing approximately 6% of all patients with T1DM or T2DM seen at our specialized clinic, fell in between those of patients with definite T1DM and T2DM, both regarding individual features and with respect to a novel classification based on multi-variable regression analysis (P<0.0001). In conclusion, a substantial proportion of diabetes patients in a tertiary care centre presented with an “ambiguous” diabetes type. Their clinical characteristics fall in between those of definite T1DM or T2DM patients.

 KDA
KDA
 First
First Prev
Prev





