
- Current
- Browse
- Collections
-
For contributors
- For Authors
- Instructions to authors
- Article processing charge
- e-submission
- For Reviewers
- Instructions for reviewers
- How to become a reviewer
- Best reviewers
- For Readers
- Readership
- Subscription
- Permission guidelines
- About
- Editorial policy
Article category
- Page Path
- HOME > Article category > Article category
Original Article
- Guideline/Fact Sheet
- Diabetes Fact Sheet in Korea 2021
- Jae Hyun Bae, Kyung-Do Han, Seung-Hyun Ko, Ye Seul Yang, Jong Han Choi, Kyung Mook Choi, Hyuk-Sang Kwon, Kyu Chang Won, on Behalf of the Committee of Media-Public Relation of the Korean Diabetes Association
- Diabetes Metab J. 2022;46(3):417-426. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0106
- 13,518 View
- 1,645 Download
- 74 Web of Science
- 99 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
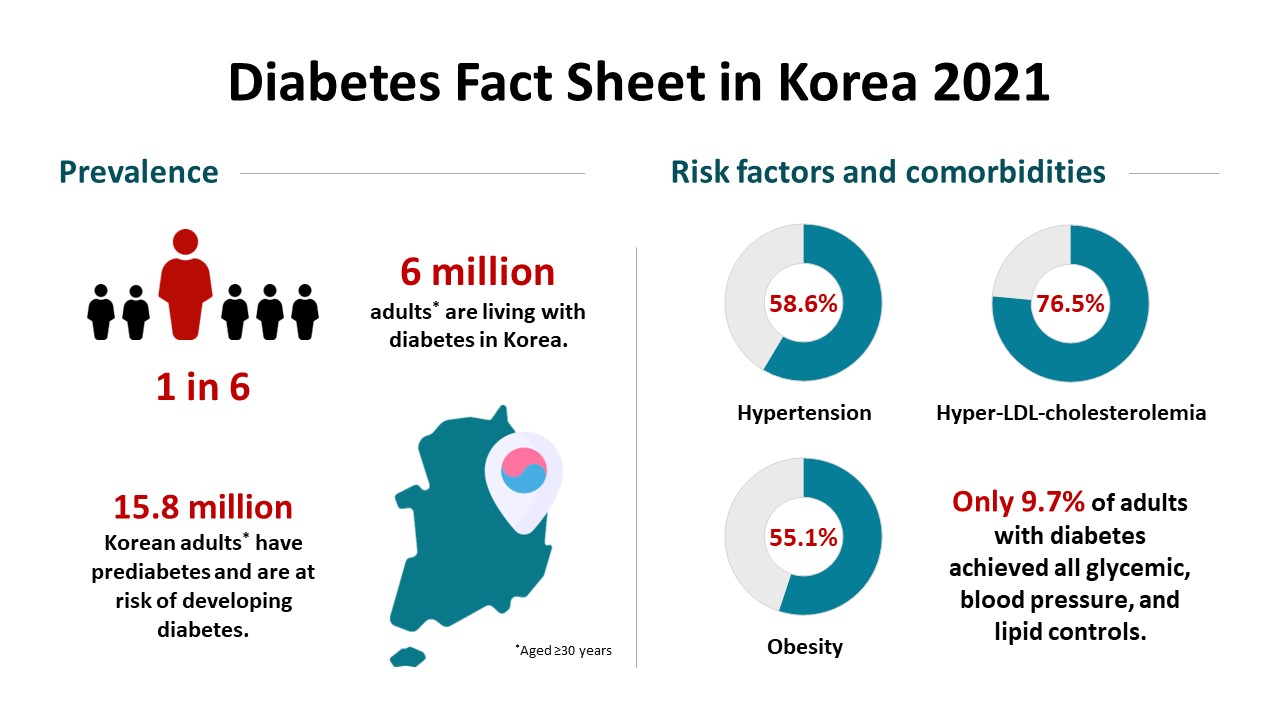
This study aimed to investigate the prevalence and management of diabetes mellitus, risk-factor control, and comorbidities among Korean adults.
Methods
We conducted a cross-sectional analysis of data from the Korea National Health and Nutrition Examination Survey to assess the prevalence, treatment, risk factors, comorbidities, and self-management behaviors of diabetes mellitus from 2019 to 2020. We also analyzed data from the Korean National Health Insurance Service to evaluate the use of antidiabetic medications in people with diabetes mellitus from 2002 through 2018.
Results
Among Korean adults aged 30 years or older, the estimated prevalence of diabetes mellitus was 16.7% in 2020. From 2019 through 2020, 65.8% of adults with diabetes mellitus were aware of the disease and treated with antidiabetic medications. The percentage of adults with diabetes mellitus who achieved glycosylated hemoglobin (HbA1c) <6.5% was 24.5% despite the increased use of new antidiabetic medications. We found that adults with diabetes mellitus who achieved all three goals of HbA1c <6.5%, blood pressure (BP) <140/85 mm Hg, and low-density lipoprotein cholesterol <100 mg/dL were 9.7%. The percentage of self-management behaviors was lower in men than women. Excess energy intake was observed in 16.7% of adults with diabetes mellitus.
Conclusion
The prevalence of diabetes mellitus among Korean adults remained high. Only 9.7% of adults with diabetes mellitus achieved all glycemic, BP, and lipid controls from 2019 to 2020. Continuous evaluation of national diabetes statistics and a national effort to increase awareness of diabetes mellitus and improve comprehensive diabetes care are needed. -
Citations
Citations to this article as recorded by- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Jinyoung Kim, Bongseong Kim, Mee Kyoung Kim, Ki‐Hyun Baek, Ki‐Ho Song, Kyungdo Han, Hyuk‐Sang Kwon
Diabetes, Obesity and Metabolism.2024; 26(2): 567. CrossRef - Changes in Fatty Liver Disease and Incident Diabetes Mellitus in Young Korean Adults
Kye-Yeung Park, Hwan-Sik Hwang, Kyungdo Han, Hoon-Ki Park
American Journal of Preventive Medicine.2024; 66(4): 717. CrossRef - Widening disparities in the national prevalence of diabetes mellitus for people with disabilities in South Korea
I. Hwang, S.Y. Kim, Y.Y. Kim, J.H. Park
Public Health.2024; 226: 173. CrossRef - Questionnaire-Based Survey of Diabetes Self-Care Activities and Barriers among Young Korean Adults with Early-Onset Diabetes
Ji In Park, Sang-Wook Kim, Il Sung Nam-Goong, Kee-Ho Song, Ji Hee Yu, Ji Yun Jeong, Eun-Hee Cho
Yonsei Medical Journal.2024; 65(1): 42. CrossRef - Patients with diabetes in regions with population decline and likelihood of receiving diabetes management education and screenings for related complications in Korea
Yeong Jun Ju, Woorim Kim, Kyujin Chang, Tae Hoon Lee, Soon Young Lee
Preventive Medicine.2024; 178: 107793. CrossRef - Association between underweight and risk of heart failure in diabetes patients
Tae Kyung Yoo, Kyung‐Do Han, Eun‐Jung Rhee, Won‐Young Lee
Journal of Cachexia, Sarcopenia and Muscle.2024; 15(2): 671. CrossRef - Gastroparesis might not be uncommon in patients with diabetes mellitus in a real-world clinical setting: a cohort study
Jeongmin Lee, Hye Lim Park, Su Young Park, Chul-Hyun Lim, Min-Hee Kim, Jung Min Lee, Sang-Ah Chang, Jung-Hwan Oh
BMC Gastroenterology.2024;[Epub] CrossRef - Cumulative exposure to impaired fasting glucose and gastrointestinal cancer risk: A nationwide cohort study
Byeong Yun Ahn, Bokyung Kim, Sanghyun Park, Sang Gyun Kim, Kyungdo Han, Soo‐Jeong Cho
Cancer.2024;[Epub] CrossRef - Multidimensional behavioral factors for diabetes management among middle-aged adults: a population-based study
Hyerang Kim, Heesook Son
Journal of Public Health.2024;[Epub] CrossRef - Efficacy and Safety of Once-Weekly Semaglutide Versus Once-Daily Sitagliptin as Metformin Add-on in a Korean Population with Type 2 Diabetes
Byung-Wan Lee, Young Min Cho, Sin Gon Kim, Seung-Hyun Ko, Soo Lim, Amine Dahaoui, Jin Sook Jeong, Hyo Jin Lim, Jae Myung Yu
Diabetes Therapy.2024; 15(2): 547. CrossRef - Association between dietary selenium intake and severe abdominal aortic calcification in the United States: a cross-sectional study
Weiwei Dong, Xiaobai Liu, Lu Ma, Zhiyong Yang, Chunyan Ma
Food & Function.2024; 15(3): 1575. CrossRef - Cumulative exposure to hypertriglyceridemia and risk of type 2 diabetes in young adults
Min-Kyung Lee, Kyungdo Han, Bongsung Kim, Jong-Dai Kim, Moon Jung Kim, Byungpyo Kim, Jung Heo, Jiyeon Ahn, Seo-Young Sohn, Jae-Hyuk Lee
Diabetes Research and Clinical Practice.2024; 208: 111109. CrossRef - Recent evidence on target blood pressure in patients with hypertension
Hack-Lyoung Kim
Cardiovascular Prevention and Pharmacotherapy.2024; 6(1): 17. CrossRef - Status and trends in epidemiologic characteristics of diabetic end-stage renal disease: an analysis of the 2021 Korean Renal Data System
Kyeong Min Kim, Seon A Jeong, Tae Hyun Ban, Yu Ah Hong, Seun Deuk Hwang, Sun Ryoung Choi, Hajeong Lee, Ji Hyun Kim, Su Hyun Kim, Tae Hee Kim, Ho-Seok Koo, Chang-Yun Yoon, Kiwon Kim, Seon Ho Ahn, Yong Kyun Kim, Hye Eun Yoon
Kidney Research and Clinical Practice.2024; 43(1): 20. CrossRef -
In silico
exploration of the potential inhibitory activities of in-house and ZINC database lead compounds against alpha-glucosidase using structure-based virtual screening and molecular dynamics simulation approach
Zuhier A. Awan, Haider Ali Khan, Alam Jamal, Sulaiman Shams, Guojun Zheng, Abdul Wadood, Muhammad Shahab, Mohammad Imran Khan, Abdulaziz A. Kalantan
Journal of Biomolecular Structure and Dynamics.2024; : 1. CrossRef - Evaluation of Mobile Applications for Patients with Diabetes Mellitus: A Scoping Review
Jung Lim Lee, Youngji Kim
Healthcare.2024; 12(3): 368. CrossRef - Current status of remote collaborative care for hypertension in medically underserved areas
Seo Yeon Baik, Kyoung Min Kim, Hakyoung Park, Jiwon Shinn, Hun-Sung Kim
Cardiovascular Prevention and Pharmacotherapy.2024; 6(1): 33. CrossRef - Association of non-alcoholic fatty liver disease with cardiovascular disease and all cause death in patients with type 2 diabetes mellitus: nationwide population based study
Kyung-Soo Kim, Sangmo Hong, Kyungdo Han, Cheol-Young Park
BMJ.2024; : e076388. CrossRef - Comparison of metabolic and neurological comorbidities in Asian patients with psoriasis and atopic dermatitis
Hee Joo Yang, Mi Young Lee, Jeong Hyeon Lee, Chang Jin Jung, Woo Jin Lee, Chong Hyun Won, Mi Woo Lee, Joon Min Jung, Sung Eun Chang
Scientific Reports.2024;[Epub] CrossRef - Cancer risk according to fasting blood glucose trajectories: a population-based cohort study
Thi Minh Thu Khong, Thi Tra Bui, Hee-Yeon Kang, Jinhee Lee, Eunjung Park, Jin-Kyoung Oh
BMJ Open Diabetes Research & Care.2024; 12(1): e003696. CrossRef - Participation experience in self-care program for type 2 diabetes: A mixed-methods study
Mihwan Kim, Haejung Lee, Gaeun Park, Ah Reum Khang
Journal of Korean Gerontological Nursing.2024; 26(1): 31. CrossRef - Fasting GLP-1 Levels and Albuminuria Are Negatively Associated in Patients with Type 2 Diabetes Mellitus
Cheol-Won Jang, Tae Yang Yu, Jin Woo Jeong, Se Eun Ha, Rajan Singh, Moon Young Lee, Seungil Ro
Journal of Personalized Medicine.2024; 14(3): 280. CrossRef - The clinical relevance of a polygenic risk score for type 2 diabetes mellitus in the Korean population
Na Yeon Kim, Haekyung Lee, Sehee Kim, Ye-Jee Kim, Hyunsuk Lee, Junhyeong Lee, Soo Heon Kwak, Seunggeun Lee
Scientific Reports.2024;[Epub] CrossRef - Glycemic traits and colorectal cancer survival in a cohort of South Korean patients: A Mendelian randomization analysis
So Yon Jun, Sooyoung Cho, Min Jung Kim, Ji Won Park, Seung‐Bum Ryoo, Seung Yong Jeong, Kyu Joo Park, Aesun Shin
Cancer Medicine.2024;[Epub] CrossRef - Real-World Treatment Patterns according to Clinical Practice Guidelines in Patients with Type 2 Diabetes Mellitus and Established Cardiovascular Disease in Korea: Multicenter, Retrospective, Observational Study
Ye Seul Yang, Nam Hoon Kim, Jong Ha Baek, Seung-Hyun Ko, Jang Won Son, Seung-Hwan Lee, Sang Youl Rhee, Soo-Kyung Kim, Tae Seo Sohn, Ji Eun Jun, In-Kyung Jeong, Chong Hwa Kim, Keeho Song, Eun-Jung Rhee, Junghyun Noh, Kyu Yeon Hur
Diabetes & Metabolism Journal.2024; 48(2): 279. CrossRef - Triglyceride-glucose index predicts type 2 diabetes mellitus more effectively than oral glucose tolerance test-derived insulin sensitivity and secretion markers
Min Jin Lee, Ji Hyun Bae, Ah Reum Khang, Dongwon Yi, Mi Sook Yun, Yang Ho Kang
Diabetes Research and Clinical Practice.2024; 210: 111640. CrossRef - Real-World Outcomes of Individualized Targeted Therapy with Insulin Glargine 300 Units/mL in Insulin-Naïve Korean People with Type 2 Diabetes: TOBE Study
Eun-Gyoung Hong, Kyung-Wan Min, Jung Soo Lim, Kyu-Jeung Ahn, Chul Woo Ahn, Jae-Myung Yu, Hye Soon Kim, Hyun Jin Kim, Won Kim, Dong Han Kim, Hak Chul Jang
Advances in Therapy.2024;[Epub] CrossRef - Effect of complicated, untreated and uncontrolled diabetes and pre‐diabetes on treatment outcome among patients with pulmonary tuberculosis
Kyung Hoon Kim, Hyung Woo Kim, Yong Hyun Kim, Yeonhee Park, Sung Soo Jung, Jin Woo Kim, Jee Youn Oh, Heayon Lee, Sung Kyoung Kim, Sun‐Hyung Kim, Jiwon Lyu, Yousang Ko, Sun Jung Kwon, Yun‐Jeong Jeong, Do Jin Kim, Hyeon‐Kyoung Koo, Yangjin Jegal, Sun Young
Respirology.2024;[Epub] CrossRef - Analysis of dietary behavior and intake related to glycemic control in patients with type 2 diabetes aged 30 years or older in Korea: Utilizing the 8th Korea National Health and Nutrition Examination Survey (2019–2021)
Jin-Ah Seok, Yeon-Kyung Lee
Nutrition Research and Practice.2024; 18(2): 239. CrossRef - Management of Early-Onset Type 2 Diabetes
Jin Hwa Kim
The Journal of Korean Diabetes.2024; 25(1): 4. CrossRef - Baseline glycated albumin level and risk of type 2 diabetes mellitus in Healthy individuals: a retrospective longitudinal observation in Korea
Kang-Su Shin, Min-Seung Park, Mi Yeon Lee, Eun Hye Cho, Hee-Yeon Woo, Hyosoon Park, Min-Jung Kwon
Scandinavian Journal of Clinical and Laboratory Investigation.2024; : 1. CrossRef - The Potential Role of Presepsin in Predicting Severe Infection in Patients with Diabetic Foot Ulcers
Eun Yeong Ha, Il Rae Park, Seung Min Chung, Young Nam Roh, Chul Hyun Park, Tae-Gon Kim, Woong Kim, Jun Sung Moon
Journal of Clinical Medicine.2024; 13(8): 2311. CrossRef - Myotonic dystrophy type 1 in South Korea: a comprehensive analysis of cancer and comorbidity risks
Incheol Seo, Jin-Mo Park
Neurological Sciences.2024;[Epub] CrossRef - Risk of Pancreatic Cancer and Use of Dipeptidyl Peptidase 4 Inhibitors in Patients with Type 2 Diabetes: A Propensity Score-Matching Analysis
Mee Kyoung Kim, Kyungdo Han, Hyuk-Sang Kwon, Soon Jib Yoo
Endocrinology and Metabolism.2023; 38(4): 426. CrossRef - Diabetes screening in South Korea: a new estimate of the number needed to screen to detect diabetes
Kyoung Hwa Ha, Kyung Ae Lee, Kyung-Do Han, Min Kyong Moon, Dae Jung Kim
The Korean Journal of Internal Medicine.2023; 38(1): 93. CrossRef - Sex differences in the impact of diabetes mellitus on tuberculosis recurrence: a retrospective national cohort study
Dararat Eksombatchai, Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Hongjo Choi, Young Ae Kang
International Journal of Infectious Diseases.2023; 127: 1. CrossRef - Response to Letter to the Editor From Han and Xu: “Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes”
Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2023; 108(4): e58. CrossRef - Lipid Management in Korean People With Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Journal of Lipid and Atherosclerosis.2023; 12(1): 12. CrossRef - Evaluation and Management of Patients With Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
International Journal of Heart Failure.2023; 5(1): 1. CrossRef - Lipid Management in Korean People with Type 2 Diabetes Mellitus: Korean Diabetes Association and Korean Society of Lipid and Atherosclerosis Consensus Statement
Ye Seul Yang, Hack-Lyoung Kim, Sang-Hyun Kim, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 1. CrossRef - Evaluation and Management of Patients with Diabetes and Heart Failure: A Korean Diabetes Association and Korean Society of Heart Failure Consensus Statement
Kyu-Sun Lee, Junghyun Noh, Seong-Mi Park, Kyung Mook Choi, Seok-Min Kang, Kyu-Chang Won, Hyun-Jai Cho, Min Kyong Moon
Diabetes & Metabolism Journal.2023; 47(1): 10. CrossRef - Risk of type 2 diabetes mellitus in catholic priests compared with general public
Youngmi Eun, Sun Myeong Ock, Se-Hong Kim, Ju Hye Chung, Se Jin Park, Churlmin Kim, Min-Kyun Im, Kyung-do Han
Acta Diabetologica.2023; 60(5): 655. CrossRef - Blood pressure control and its associated factors in patients with hypertension and type 2 diabetes
Anan S Jarab, Walid Al-Qerem, Salam Alqudah, Shrouq R Abu Heshmeh, Tareq L Mukattash, Karem H Alzoubi
Electronic Journal of General Medicine.2023; 20(3): em477. CrossRef - Prevalence and associated factors of diabetes mellitus among patients with tuberculosis in South Korea from 2011 to 2018: a nationwide cohort study
Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Jeong Mi Seo, Hongjo Choi, Young Ae Kang
BMJ Open.2023; 13(3): e069642. CrossRef - The association between nutrition label utilization and disease management education among hypertension or diabetes diagnosed in Korea using 2018 Community Health Survey: a cross-sectional study
Miran Jin, Jayeun Kim, Kyuhyun Yoon
Korean Journal of Community Nutrition.2023; 28(1): 38. CrossRef - Insulin Fact Sheet in Type 1 and 2 Diabetes Mellitus and Trends of Antidiabetic Medication Use in Insulin Users with Type 2 Diabetes Mellitus: 2002 to 2019
Jiyun Park, Gyuri Kim, Bong-Sung Kim, Kyung-Do Han, So Yoon Kwon, So Hee Park, You-Bin Lee, Sang-Man Jin, Jae Hyeon Kim
Diabetes & Metabolism Journal.2023; 47(2): 211. CrossRef - Comparison of Operational Definition of Type 2 Diabetes Mellitus Based on Data from Korean National Health Insurance Service and Korea National Health and Nutrition Examination Survey
Jong Ha Baek, Yong-Moon Park, Kyung Do Han, Min Kyong Moon, Jong Han Choi, Seung-Hyun Ko
Diabetes & Metabolism Journal.2023; 47(2): 201. CrossRef - Evaluation of pharmacokinetic interactions between lobeglitazone, empagliflozin, and metformin in healthy subjects
Heeyoung Kim, Choon Ok Kim, Hyeonsoo Park, Min Soo Park, Dasohm Kim, Taegon Hong, Yesong Shin, Byung Hak Jin
Translational and Clinical Pharmacology.2023; 31(1): 59. CrossRef - Vascular and metabolic effects of ipragliflozin versus sitagliptin (IVS) in type 2 diabetes treated with sulphonylurea and metformin: IVS study
Seon Mee Kang, Han Mi Yun, Minji Sohn, Soo Lim
Diabetes, Obesity and Metabolism.2023; 25(7): 1922. CrossRef - Diabetes and Skin Disease
Jungah Lim
The Journal of Korean Diabetes.2023; 24(1): 29. CrossRef - Revisiting the Diabetes Crisis in Korea: Call for Urgent Action
Jun Sung Moon
The Journal of Korean Diabetes.2023; 24(1): 1. CrossRef - Association between Sleep Duration and Incident Diabetes Mellitus in Healthy Subjects: A 14-Year Longitudinal Cohort Study
Jin ha Jang, Wonjin Kim, Jin Sil Moon, Eun Roh, Jun Goo Kang, Seong Jin Lee, Sung-Hee Ihm, Ji Hye Huh
Journal of Clinical Medicine.2023; 12(8): 2899. CrossRef - Exercise Frequency Reduction Is Associated With Higher Risk of Infection in Newly Diagnosed Diabetes: A Nationally Representative Cohort Study
Yohwan Lim, Hye Jun Kim, Sung Soo Yoon, Sang Jun Lee, Myeong Hoon Lee, Hyewon Park, Sun Jae Park, Seogsong Jeong, Hyun Wook Han
Journal of Korean Medical Science.2023;[Epub] CrossRef - Effects of Consuming Heat-Treated Dodamssal Brown Rice Containing Resistant Starch on Glucose Metabolism in Humans
Jiyoung Park, Sea-Kwan Oh, Miae Doo, Hyun-Jung Chung, Hyun-Jin Park, Hyejin Chun
Nutrients.2023; 15(10): 2248. CrossRef - Opening the Precision Diabetes Care through Digital Healthcare
Joonyub Lee, Jin Yu, Kun-Ho Yoon
Diabetes & Metabolism Journal.2023; 47(3): 307. CrossRef - Fatty Liver & Diabetes Statistics in Korea: Nationwide Data 2009 to 2017
Eugene Han, Kyung-Do Han, Yong-ho Lee, Kyung-Soo Kim, Sangmo Hong, Jung Hwan Park, Cheol-Young Park
Diabetes & Metabolism Journal.2023; 47(3): 347. CrossRef - Trends in the Quality of Primary Care and Acute Care in Korea From 2008 to 2020: A Cross-sectional Study
Yeong Geun Gwon, Seung Jin Han, Kyoung Hoon Kim
Journal of Preventive Medicine and Public Health.2023; 56(3): 248. CrossRef - Development and Validation of Multiple Equations for Low-Density Lipoprotein and Apolipoprotein B in Korean Patients Visiting Local Clinics and Hospitals
Rihwa Choi, Sang Gon Lee, Eun Hee Lee
Nutrients.2023; 15(12): 2786. CrossRef - The role of retinal vessel geometry as an indicator of systemic arterial stiffness assessed by cardio-ankle vascular index
Dae Joong Ma, Heesun Lee, Ji Min Choi, Hyo Eun Park, Su-Yeon Choi, Hyuk Jin Choi
Frontiers in Cardiovascular Medicine.2023;[Epub] CrossRef - Association between type 2 diabetes mellitus and depression among Korean midlife women: a cross-sectional analysis study
You Lee Yang, Eun-Ok Im, Yunmi Kim
BMC Nursing.2023;[Epub] CrossRef - Associations of updated cardiovascular health metrics, including sleep health, with incident diabetes and cardiovascular events in older adults with prediabetes: A nationwide population-based cohort study
Kyoung Hwa Ha, Dae Jung Kim, Seung Jin Han
Diabetes Research and Clinical Practice.2023; 203: 110820. CrossRef - Paradigm Shift in Management of Hyperglycemia in Patients with Type 2 Diabetes: Glucocentric versus Organ Protection
Jong Chul Won
The Journal of Korean Diabetes.2023; 24(2): 59. CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef - Prevalence and treatment status of diabetes mellitus in Korea
Hyuk-Sang Kwon
Journal of the Korean Medical Association.2023; 66(7): 404. CrossRef - The impact of diabetes status on total and site-specific cancer risk in the elderly population: A nationwide cohort study
Kyuho Kim, Bongseong Kim, Hyunho Kim, Hyung Soon Park, Yu-Bae Ahn, Seung-Hyun Ko, Kyungdo Han, Jae-Seung Yun
Diabetes Research and Clinical Practice.2023; 203: 110866. CrossRef - Response to comments of Lai et al. “Proposal of one option for patient-centered, heterogeneous selection of antidiabetic drug”
Sunyoung Kim, Sang Youl Rhee
Diabetes Research and Clinical Practice.2023; 203: 110864. CrossRef - Association of Dental Diseases and Oral Hygiene Care With the Risk of Heart Failure in Patients With Type 2 Diabetes: A Nationwide Cohort Study
Youn Huh, Jung Eun Yoo, Sang‐Hyun Park, Kyungdo Han, Seon Mee Kim, Hye Soon Park, Kyung Hwan Cho, Jin‐Soo Ahn, Sang Ho Jun, Ga Eun Nam
Journal of the American Heart Association.2023;[Epub] CrossRef - Bidirectional associations between periodontal disease and systemic diseases: a nationwide population-based study in Korea
Salma Nabila, Jaesung Choi, Ji-Eun Kim, Seokyung Hahn, In-Kyung Hwang, Tae-Il Kim, Hee-Kyung Park, Ji-Yeob Choi
Scientific Reports.2023;[Epub] CrossRef - Long-term Effectiveness of the National Diabetes Quality Assessment Program in South Korea
Ji Hye Huh, Serim Kwon, Gui Ok Kim, Bo Yeon Kim, Kyoung Hwa Ha, Dae Jung Kim
Diabetes Care.2023; 46(9): 1700. CrossRef - Refined Diagnostic Protocol for Diabetic Polyneuropathy: Paving the Way for Timely Detection
Byung-Mo Oh
Annals of Rehabilitation Medicine.2023; 47(4): 234. CrossRef - Analysis of difference in body fluid composition and dietary intake between Korean adults with and without type 2 diabetes mellitus
Yu-Gyeong Kim, Ha-Neul Choi, Jung-Eun Yim
Journal of Nutrition and Health.2023; 56(4): 377. CrossRef - 2023 Clinical Practice Guidelines for Diabetes Mellitus of the Korean Diabetes Association
Jong Han Choi, Kyung Ae Lee, Joon Ho Moon, Suk Chon, Dae Jung Kim, Hyun Jin Kim, Nan Hee Kim, Ji A Seo, Mee Kyoung Kim, Jeong Hyun Lim, YoonJu Song, Ye Seul Yang, Jae Hyeon Kim, You-Bin Lee, Junghyun Noh, Kyu Yeon Hur, Jong Suk Park, Sang Youl Rhee, Hae J
Diabetes & Metabolism Journal.2023; 47(5): 575. CrossRef - Diabetes Mellitus in the Elderly Adults in Korea: Based on Data from the Korea National Health and Nutrition Examination Survey 2019 to 2020
Seung-Hyun Ko, Kyung Do Han, Yong-Moon Park, Jae-Seung Yun, Kyuho Kim, Jae-Hyun Bae, Hyuk-Sang Kwon, Nan-Hee Kim
Diabetes & Metabolism Journal.2023; 47(5): 643. CrossRef - Management of Dyslipidemia in Patients with Diabetes Mellitus
Kyung Ae Lee
The Journal of Korean Diabetes.2023; 24(3): 111. CrossRef - Association between initial continuity of care status and diabetes-related health outcomes in older patients with type 2 diabetes mellitus: A nationwide retrospective cohort study in South Korea
Hyun Woo Jung, Woo-Ri Lee
Primary Care Diabetes.2023; 17(6): 600. CrossRef - 2023 Clinical Practice Guidelines for Diabetes
Min Kyong Moon
The Journal of Korean Diabetes.2023; 24(3): 120. CrossRef - Diagnostic performance of the fibrosis-4 index and the NAFLD fibrosis score for screening at-risk individuals in a health check-up setting
Huiyul Park, Eileen L. Yoon, Mimi Kim, Jonghyun Lee, Hye-Lin Kim, Seon Cho, Eun-Hee Nah, Dae Won Jun
Hepatology Communications.2023;[Epub] CrossRef - Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinology and Metabolism.2023; 38(5): 525. CrossRef - The Characteristics and Risk of Mortality in the Elderly Korean Population
Sunghwan Suh
Endocrinology and Metabolism.2023; 38(5): 522. CrossRef - Comparative Risk of Type 2 Diabetes after Gastrectomy and Endoscopic Resection for Gastric Cancer: A Nationwide Cohort Study
Yeongkeun Kwon, Jin-Won Kwon, Jiyun Kim, Dohyang Kim, Jinseub Hwang, Jane Ha, Shin-Hoo Park, Sungsoo Park
Journal of the American College of Surgeons.2023; 237(6): 902. CrossRef - Efficacy and Safety of Evogliptin Add-on Therapy to Dapagliflozin/Metformin Combinations in Patients with Poorly Controlled Type 2 Diabetes Mellitus: A 24-Week Multicenter Randomized Placebo-Controlled Parallel-Design Phase-3 Trial with a 28-Week Extensio
Jun Sung Moon, Il Rae Park, Hae Jin Kim, Choon Hee Chung, Kyu Chang Won, Kyung Ah Han, Cheol-Young Park, Jong Chul Won, Dong Jun Kim, Gwan Pyo Koh, Eun Sook Kim, Jae Myung Yu, Eun-Gyoung Hong, Chang Beom Lee, Kun-Ho Yoon
Diabetes & Metabolism Journal.2023; 47(6): 808. CrossRef - Association between diabetes mellitus and cause of death in patients with tuberculosis: A Korean nationwide cohort study
Se Hyun Kwak, Dawoon Jeong, Jeongha Mok, Doosoo Jeon, Hee-Yeon Kang, Hee Jin Kim, Hee-Sun Kim, Hongjo Choi, Young Ae Kang, Frederick Quinn
PLOS ONE.2023; 18(12): e0295556. CrossRef - Strategies to Maintain the Remission of Diabetes Following Metabolic Surgery
Mi Kyung Kim, Hye Soon Kim
Journal of Metabolic and Bariatric Surgery.2023; 12(2): 26. CrossRef - Anti-Diabetic Medications and Osteoporosis
Kyongyoung Kim
The Journal of Korean Diabetes.2023; 24(4): 173. CrossRef - The associations between changes in hepatic steatosis and heart failure and mortality: a nationwide cohort study
Jiyun Park, Gyuri Kim, Hasung Kim, Jungkuk Lee, Sang-Man Jin, Jae Hyeon Kim
Cardiovascular Diabetology.2022;[Epub] CrossRef - Severe hypoglycemia as a risk factor for cardiovascular outcomes in patients with type 2 diabetes: is it preventable?
Seung-Hyun Ko
Cardiovascular Prevention and Pharmacotherapy.2022; 4(3): 106. CrossRef - Current Trends of Big Data Research Using the Korean National Health Information Database
Mee Kyoung Kim, Kyungdo Han, Seung-Hwan Lee
Diabetes & Metabolism Journal.2022; 46(4): 552. CrossRef - Current status of obesity treatment in Korea: based on the 2020 Korean Society for the Study of Obesity guidelines for obesity management
Eun-Jung Rhee
Journal of the Korean Medical Association.2022; 65(7): 388. CrossRef - 젊은 2형 당뇨병 환자의 관리
재현 배
Public Health Weekly Report.2022; 15(35): 2474. CrossRef - Analysis of the Association between Metabolic Syndrome and Renal Function in Middle-Aged Patients with Diabetes
Yoonjin Park, Su Jung Lee
International Journal of Environmental Research and Public Health.2022; 19(18): 11832. CrossRef - The Degree of Glycemic Control for the First Three Months Determines the Next Seven Years
Nami Lee, Dae Jung Kim
Journal of Korean Medical Science.2022;[Epub] CrossRef - Blood Pressure Target in Type 2 Diabetes Mellitus
Hyun-Jin Kim, Kwang-il Kim
Diabetes & Metabolism Journal.2022; 46(5): 667. CrossRef - Association Between DPP4 Inhibitor Use and the Incidence of Cirrhosis, ESRD, and Some Cancers in Patients With Diabetes
Yewon Na, Soo Wan Kim, Ie Byung Park, Soo Jung Choi, Seungyoon Nam, Jaehun Jung, Dae Ho Lee
The Journal of Clinical Endocrinology & Metabolism.2022; 107(11): 3022. CrossRef - Education for Insulin Injection in Elderly Diabetic Patients
Gi Yeon Lee
The Journal of Korean Diabetes.2022; 23(3): 201. CrossRef - Recent Updates on Phytoconstituent Alpha-Glucosidase Inhibitors: An Approach towards the Treatment of Type Two Diabetes
Hamdy Kashtoh, Kwang-Hyun Baek
Plants.2022; 11(20): 2722. CrossRef - Epidemiological characteristics of diabetes mellitus in Korea
Soon Young Lee
Journal of the Korean Medical Association.2022; 65(10): 640. CrossRef - Screening for Prediabetes and Diabetes in Korean Nonpregnant Adults: A Position Statement of the Korean Diabetes Association, 2022
Kyung Ae Lee, Dae Jung Kim, Kyungdo Han, Suk Chon, Min Kyong Moon
Diabetes & Metabolism Journal.2022; 46(6): 819. CrossRef - Oldies but Goodies: Thiazolidinedione as an Insulin Sensitizer with Cardioprotection
Eun-Hee Cho
Diabetes & Metabolism Journal.2022; 46(6): 827. CrossRef - The Mediating Effect of Acceptance Action in the Relationship between Diabetes Distress and Self-stigma among Old Adults with Diabetes in South Korea
Hyesun Kim, Kawoun Seo
Journal of Korean Academy of Community Health Nursing.2022; 33(4): 446. CrossRef
- Weight change in patients with new‐onset type 2 diabetes mellitus and its association with remission: Comprehensive real‐world data
Sulwon Lecture 2021
- Basic Research
- Exercise, Mitohormesis, and Mitochondrial ORF of the 12S rRNA Type-C (MOTS-c)
- Tae Kwan Yoon, Chan Hee Lee, Obin Kwon, Min-Seon Kim
- Diabetes Metab J. 2022;46(3):402-413. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0092
- 5,293 View
- 238 Download
- 8 Web of Science
- 9 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
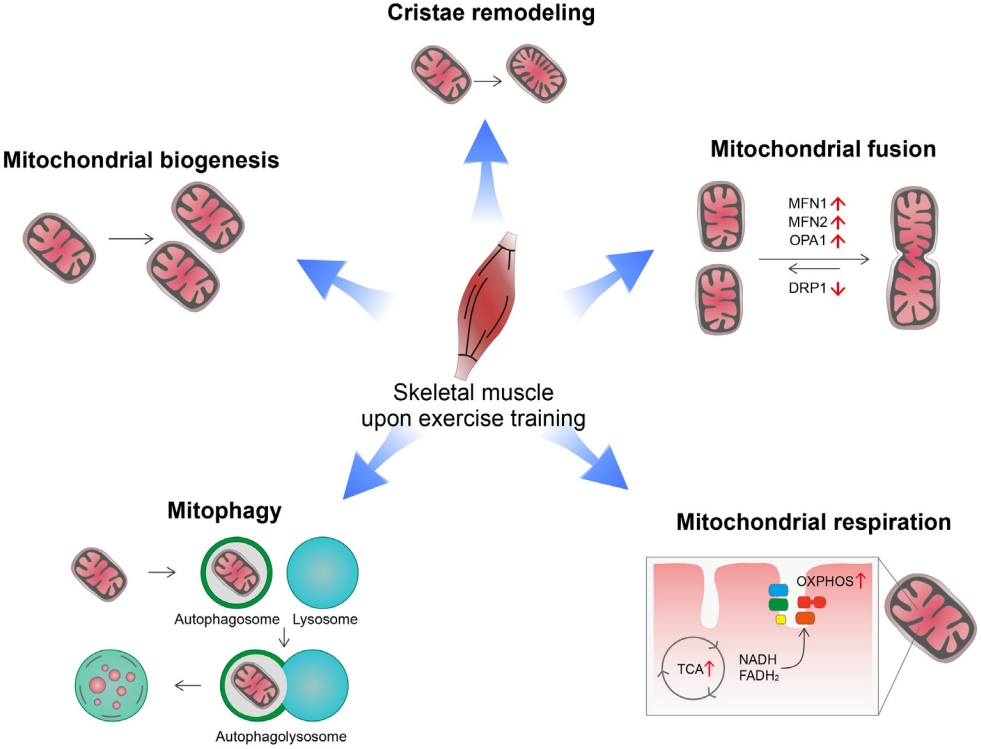
ePub - Low levels of mitochondrial stress are beneficial for organismal health and survival through a process known as mitohormesis. Mitohormetic responses occur during or after exercise and may mediate some salutary effects of exercise on metabolism. Exercise-related mitohormesis involves reactive oxygen species production, mitochondrial unfolded protein response (UPRmt), and release of mitochondria-derived peptides (MDPs). MDPs are a group of small peptides encoded by mitochondrial DNA with beneficial metabolic effects. Among MDPs, mitochondrial ORF of the 12S rRNA type-c (MOTS-c) is the most associated with exercise. MOTS-c expression levels increase in skeletal muscles, systemic circulation, and the hypothalamus upon exercise. Systemic MOTS-c administration increases exercise performance by boosting skeletal muscle stress responses and by enhancing metabolic adaptation to exercise. Exogenous MOTS-c also stimulates thermogenesis in subcutaneous white adipose tissues, thereby enhancing energy expenditure and contributing to the anti-obesity effects of exercise training. This review briefly summarizes the mitohormetic mechanisms of exercise with an emphasis on MOTS-c.
-
Citations
Citations to this article as recorded by- Mitochondrial-derived peptides: Antidiabetic functions and evolutionary perspectives
Satadeepa Kal, Sumana Mahata, Suborno Jati, Sushil K. Mahata
Peptides.2024; 172: 171147. CrossRef - Beneficial Effects of Low-Grade Mitochondrial Stress on Metabolic Diseases and Aging
Se Hee Min, Gil Myoung Kang, Jae Woo Park, Min-Seon Kim
Yonsei Medical Journal.2024; 65(2): 55. CrossRef - Roles of Myokines and Muscle-Derived Extracellular Vesicles in Musculoskeletal Deterioration under Disuse Conditions
Jie Zhang, Yunfang Gao, Jiangwei Yan
Metabolites.2024; 14(2): 88. CrossRef - Antifragility and antiinflammaging: Can they play a role for a healthy longevity?
Fabiola Olivieri, Francesco Prattichizzo, Fabrizia Lattanzio, Anna Rita Bonfigli, Liana Spazzafumo
Ageing Research Reviews.2023; 84: 101836. CrossRef - MOTS-c: A promising mitochondrial-derived peptide for therapeutic exploitation
Yuejun Zheng, Zilin Wei, Tianhui Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef - MOTS-c: A potential anti-pulmonary fibrosis factor derived by mitochondria
Zewei Zhang, Dongmei Chen, Kaili Du, Yaping Huang, Xingzhe Li, Quwen Li, Xiaoting Lv
Mitochondrion.2023; 71: 76. CrossRef - Mitochondrial-Encoded Peptide MOTS-c, Diabetes, and Aging-Related Diseases
Byung Soo Kong, Changhan Lee, Young Min Cho
Diabetes & Metabolism Journal.2023; 47(3): 315. CrossRef - MOTS-c Serum Concentration Positively Correlates with Lower-Body Muscle Strength and Is Not Related to Maximal Oxygen Uptake—A Preliminary Study
Remigiusz Domin, Michał Pytka, Mikołaj Żołyński, Jan Niziński, Marcin Rucinski, Przemysław Guzik, Jacek Zieliński, Marek Ruchała
International Journal of Molecular Sciences.2023; 24(19): 14951. CrossRef - Unique Properties of Apicomplexan Mitochondria
Ian M. Lamb, Ijeoma C. Okoye, Michael W. Mather, Akhil B. Vaidya
Annual Review of Microbiology.2023; 77(1): 541. CrossRef
- Mitochondrial-derived peptides: Antidiabetic functions and evolutionary perspectives
Editorial
- Implication of Sex Differences in Visceral Fat for the Assessment of Incidence Risk of Type 2 Diabetes Mellitus
- Sang Hyeon Ju, Hyon-Seung Yi
- Diabetes Metab J. 2022;46(3):414-416. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0089
- 2,704 View
- 154 Download
- 3 Web of Science
- 3 Crossref
-
 PDF
PDF PubReader
PubReader  ePub
ePub -
Citations
Citations to this article as recorded by- Prediction of high visceral adipose tissue for sex‐specific community residents in Taiwan
Yu‐Hsuan Chang, Chin‐Sung Chang, Chieh‐Yu Liu, Yin‐Fan Chang, Shiow‐Ching Shun
Nursing & Health Sciences.2024;[Epub] CrossRef - Visceral fat and attribute-based medicine in chronic kidney disease
Hiroshi Kataoka, Kosaku Nitta, Junichi Hoshino
Frontiers in Endocrinology.2023;[Epub] CrossRef - The predictive significance of lipid accumulation products for future diabetes in a non-diabetic population from a gender perspective: an analysis using time-dependent receiver operating characteristics
Jiajun Qiu, Maobin Kuang, Yang Zou, Ruijuan Yang, Qing Shangguan, Dingyang Liu, Guotai Sheng, Wei Wang
Frontiers in Endocrinology.2023;[Epub] CrossRef
- Prediction of high visceral adipose tissue for sex‐specific community residents in Taiwan
Reviews
- Guideline/Fact Sheet
- Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hypertension
- Jong Han Choi, Jee-Hyun Kang, Suk Chon
- Diabetes Metab J. 2022;46(3):377-390. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0051
- 4,888 View
- 247 Download
- 3 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
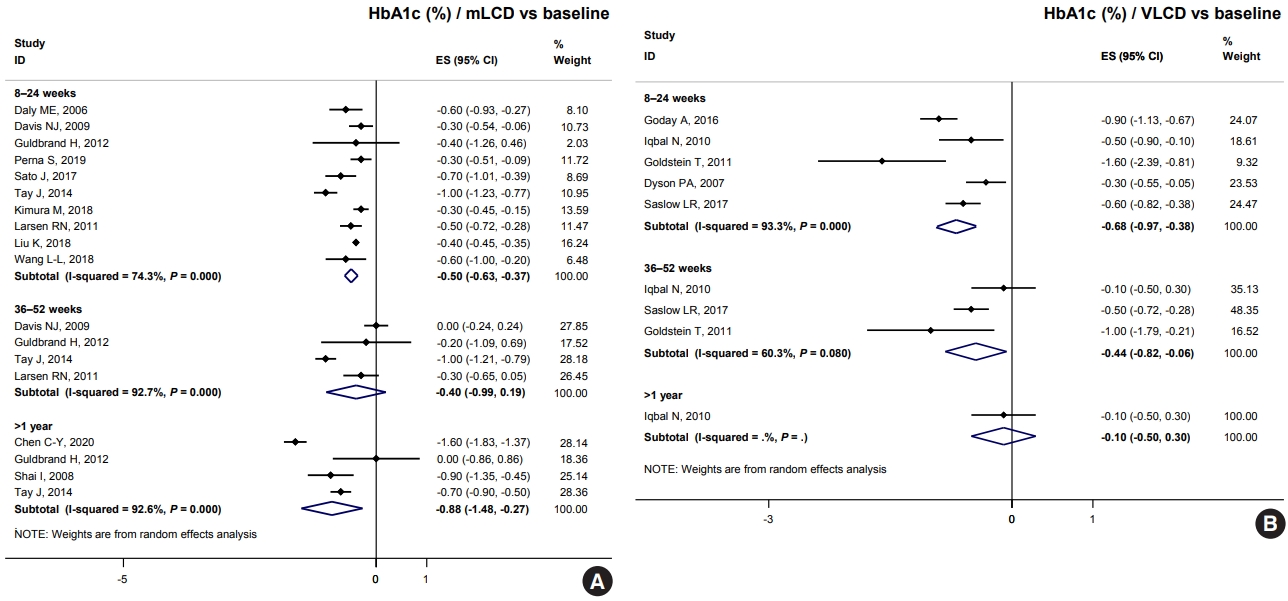
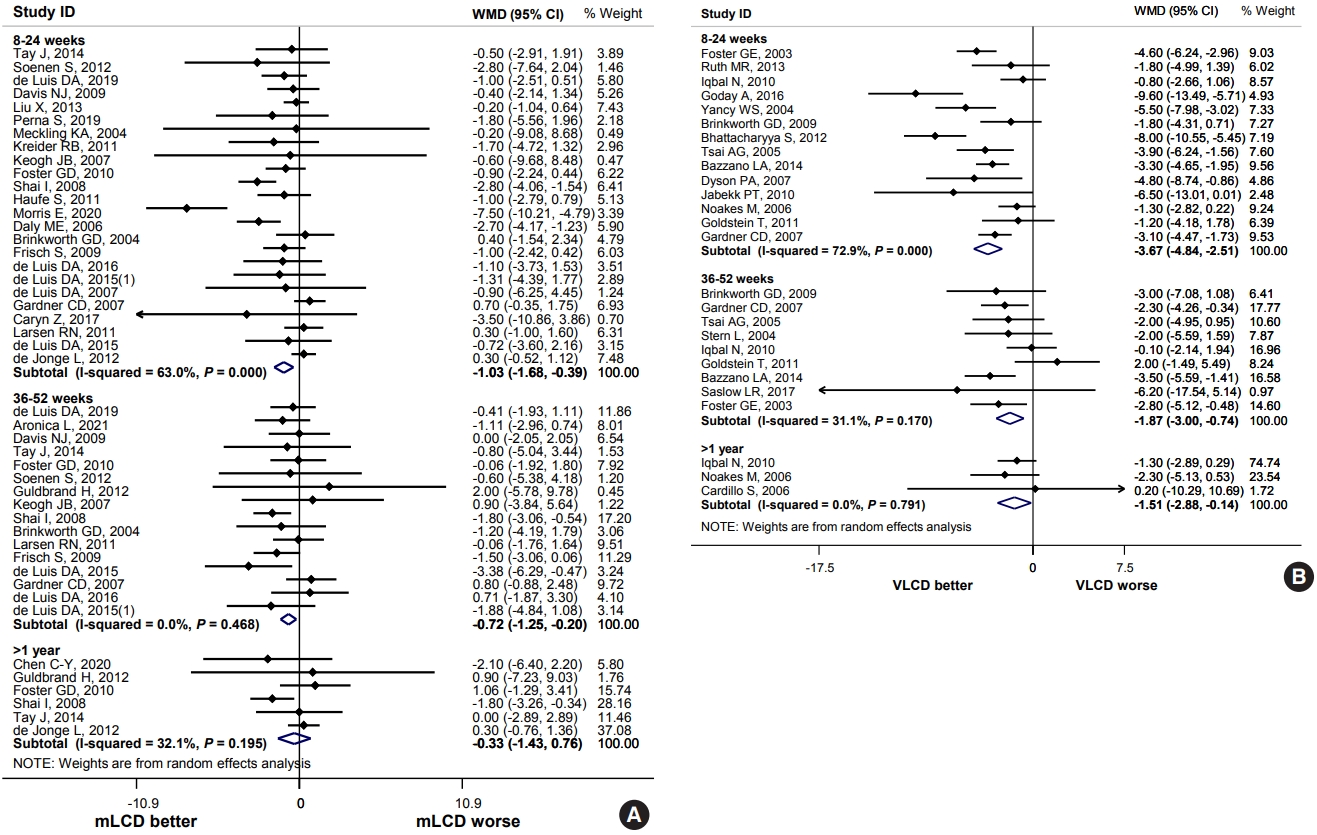
ePub - The Joint Committee of the Korean Diabetes Association, the Korean Society for the Study of Obesity, and the Korean Society of Hypertension announced a consensus statement on carbohydrate-restricted diets and intermittent fasting, representing an emerging and popular dietary pattern. In this statement, we recommend moderately-low-carbohydrate or low-carbohydrate diets, not a very-low-carbohydrate diet, for patients with type 2 diabetes mellitus. These diets can be considered a dietary regimen to improve glycemic control and reduce body weight in adults with type 2 diabetes mellitus. This review provides the detailed results of a meta-analysis and systematic literature review on the potential harms and benefits of carbohydrate-restricted diets in patients with diabetes. We expect that this review will help experts and patients by fostering an in-depth understanding and appropriate application of carbohydrate-restricted diets in the comprehensive management of diabetes.
-
Citations
Citations to this article as recorded by- Efficacy of convenience meal-type foods designed for diabetes in the management of metabolic syndrome based on a 3-week trial
Do Gyeong Lee, In Gyeong Kang, Tae Seok Kim, Yun Ahn, Sang Yun Lee, Hye Jin Ahn, Yoo Kyoung Park
Nutrition.2024; 118: 112287. CrossRef - Long-Term Results of a Digital Diabetes Self-Management and Education Support Program Among Adults With Type 2 Diabetes: A Retrospective Cohort Study
Ashley Berthoumieux, Sarah Linke, Melinda Merry, Alison Megliola, Jessie Juusola, Jenna Napoleone
The Science of Diabetes Self-Management and Care.2024; 50(1): 19. CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef
- Efficacy of convenience meal-type foods designed for diabetes in the management of metabolic syndrome based on a 3-week trial
- Metabolic Risk/Epidemiology
- Lifestyle Interventions for Non-Obese Patients Both with, and at Risk, of Non-Alcoholic Fatty Liver Disease
- Xin-Lei Zhang, Ting-Yao Wang, Giovanni Targher, Christopher D. Byrne, Ming-Hua Zheng
- Diabetes Metab J. 2022;46(3):391-401. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0048
- 5,190 View
- 274 Download
- 9 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF PubReader
PubReader  ePub
ePub - Non-alcoholic fatty liver disease occurring in non-obese subjects (the so-called non-obese NAFLD) is a highly prevalent but neglected liver condition, which is closely associated with metabolic disorders and suboptimal lifestyles. Landmark studies have shown that lifestyle interventions are potentially beneficial in decreasing the risk of developing non-obese NAFLD and in ameliorating NAFLD in non-obese individuals with pre-existing NAFLD. Lifestyle interventions usually refer to changes in eating habits and physical activity, both of which have a powerful effect on non-obese NAFLD and on risk factors for non-obese NAFLD. However, to date, patients and health-care professionals have a poor awareness and understanding of non-obese NAFLD and the beneficial effects of lifestyle interventions in this patient population. The aim of this narrative review is to briefly discuss the evidence for the effects of lifestyle changes and what changes are needed amongst medical personnel and other stakeholders in order to raise awareness of non-obese NAFLD.
-
Citations
Citations to this article as recorded by- Triglycerides Mediate the Influence of Body Mass Index on Non-Alcoholic Fatty Liver Disease in a Non-Obese Chinese Population with Normal Low-Density Lipoprotein Cholesterol Levels
Xixi Han, Jingwen Kong, Hemin Zhang, Yuan Zhao, Yafeng Zheng, Chao Wei
Obesity Facts.2024; 17(2): 191. CrossRef - Patients with NAFLD exhibit more advanced fibrosis in liver biopsy than patients with other chronic liver diseases
Lydia Rohr, Peter Lemmer, Marie Henning, Andrea Tannapfel, Theodor Baars, Paul Manka, Ali Canbay, Jan-Peter Sowa
Zeitschrift für Gastroenterologie.2023; 61(01): 29. CrossRef - Performance of Simple Fibrosis Score in Non-Alcoholic Fatty Liver Disease with and without Type 2 Diabetes
Seung Min Chung, Min Kyu Kang, Jun Sung Moon, Jung Gil Park
Endocrinology and Metabolism.2023; 38(2): 277. CrossRef - An international multidisciplinary consensus statement on MAFLD and the risk of CVD
Xiao-Dong Zhou, Giovanni Targher, Christopher D. Byrne, Virend Somers, Seung Up Kim, C. Anwar A. Chahal, Vincent Wai-Sun Wong, Jingjing Cai, Michael D. Shapiro, Mohammed Eslam, Philippe Gabriel Steg, Ki-Chul Sung, Anoop Misra, Jian-Jun Li, Carlos Brotons,
Hepatology International.2023; 17(4): 773. CrossRef - Lean or Non-obese Nonalcoholic Fatty Liver Disease Patients: Are They Really Lean?
Eugene Han, Yong-ho Lee
Clinical and Molecular Hepatology.2023; 29(4): 980. CrossRef - Sex-Based Differences and Risk Factors for Comorbid Nonalcoholic Fatty Liver Disease in Patients with Bipolar Disorder: A Cross-Sectional Retrospective Study
Ying Wang, Yiyi Liu, Xun Zhang, Qing Wu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3533. CrossRef - Benefits of Physical Exercise as Approach to Prevention and Reversion of Non-Alcoholic Fatty Liver Disease in Children and Adolescents with Obesity
Valeria Calcaterra, Vittoria Magenes, Matteo Vandoni, Clarissa Berardo, Luca Marin, Alice Bianchi, Erika Cordaro, Giustino Silvestro, Dario Silvestri, Vittoria Carnevale Pellino, Cristina Cereda, Gianvincenzo Zuccotti
Children.2022; 9(8): 1174. CrossRef - The effects of supplementation of probiotics, prebiotics, or synbiotics on patients with non-alcoholic fatty liver disease: A meta-analysis of randomized controlled trials
Wenmin Xing, Wenyan Gao, Xiaoling Lv, Zhenlei Zhao, Genxiang Mao, Xiaoyan Dong, Zuyong Zhang
Frontiers in Nutrition.2022;[Epub] CrossRef
- Triglycerides Mediate the Influence of Body Mass Index on Non-Alcoholic Fatty Liver Disease in a Non-Obese Chinese Population with Normal Low-Density Lipoprotein Cholesterol Levels
- Guideline/Fact Sheet
- Effect of Carbohydrate-Restricted Diets and Intermittent Fasting on Obesity, Type 2 Diabetes Mellitus, and Hypertension Management: Consensus Statement of the Korean Society for the Study of Obesity, Korean Diabetes Association, and Korean Society of Hypertension
- Jong Han Choi, Yoon Jeong Cho, Hyun-Jin Kim, Seung-Hyun Ko, Suk Chon, Jee-Hyun Kang, Kyoung-Kon Kim, Eun Mi Kim, Hyun Jung Kim, Kee-Ho Song, Ga Eun Nam, Kwang Il Kim, Committee of Clinical Practice Guidelines, Korean Society for the Study of Obesity (KSSO), Committee of Clinical Practice Guidelines and Committee of Food and Nutrition, Korean Diabetes Association (KDA), Policy Committee of Korean Society of Hypertension (KSH), Policy Development Committee of National Academy of Medicine of Korea (NAMOK)
- Diabetes Metab J. 2022;46(3):355-376. Published online May 25, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0038
- 10,757 View
- 588 Download
- 7 Web of Science
- 7 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
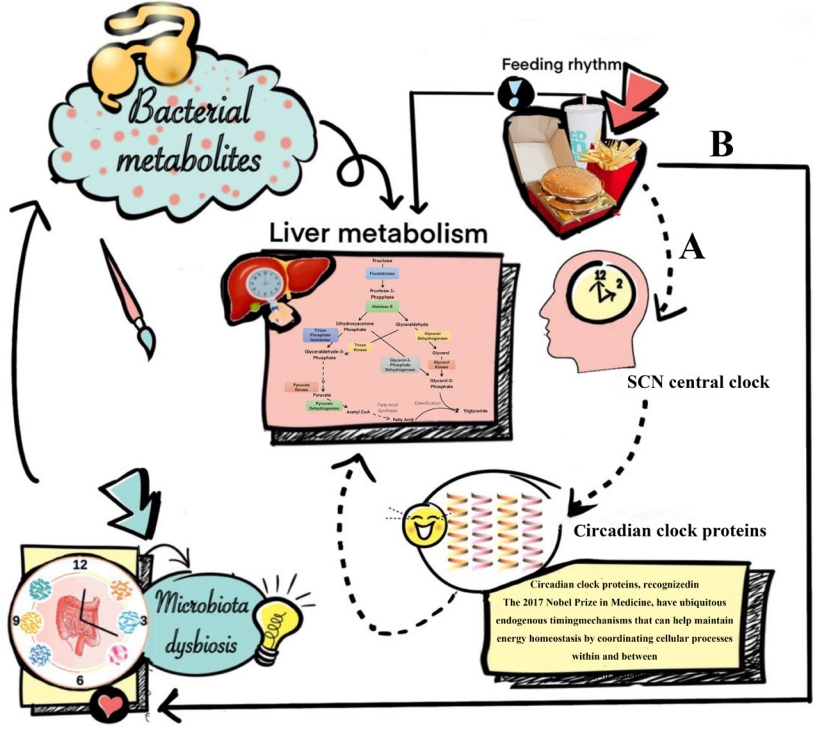
ePub - Carbohydrate-restricted diets and intermittent fasting (IF) have been rapidly gaining interest among the general population and patients with cardiometabolic disease, such as overweight or obesity, diabetes, and hypertension. However, there are limited expert recommendations for these dietary regimens. This study aimed to evaluate the level of scientific evidence on the benefits and harms of carbohydrate-restricted diets and IF to make responsible recommendations. A meta-analysis and systematic literature review of 66 articles on 50 randomized controlled trials (RCTs) of carbohydrate-restricted diets and 10 articles on eight RCTs of IF was performed. Based on the analysis, the following recommendations are suggested. In adults with overweight or obesity, a moderately-low carbohydrate or low carbohydrate diet (mLCD) can be considered as a dietary regimen for weight reduction. In adults with type 2 diabetes mellitus, mLCD can be considered as a dietary regimen for improving glycemic control and reducing body weight. In contrast, a very-low carbohydrate diet (VLCD) and IF are recommended against in patients with diabetes. Furthermore, no recommendations are suggested for VLCD and IF in adults with overweight or obesity, and carbohydrate-restricted diets and IF in patients with hypertension. Here, we describe the results of our analysis and the evidence for these recommendations.
-
Citations
Citations to this article as recorded by- Metabolic changes with intermittent fasting
Maria G. Lange, Alice A. Coffey, Paul C. Coleman, Thomas M. Barber, Thijs Van Rens, Oyinlola Oyebode, Sally Abbott, Petra Hanson
Journal of Human Nutrition and Dietetics.2024; 37(1): 256. CrossRef - Papel do Jejum Intermitente e da Dieta Restrita em Carboidratos na Prevenção de Doenças Cardiovasculares em Pacientes Pré-Diabéticos
Mohamed Khalfallah, Basma Elnagar, Shaimaa S. Soliman, Ahmad Eissa, Amany Allaithy
Arquivos Brasileiros de Cardiologia.2023;[Epub] CrossRef - Medical nutrition therapy for diabetes mellitus
Suk Chon
Journal of the Korean Medical Association.2023; 66(7): 421. CrossRef - Euglycemic diabetic ketoacidosis development in a patient with type 2 diabetes receiving a sodium-glucose cotransporter-2 inhibitor and a carbohydrate-restricted diet
Gwanpyo Koh, Jisun Bang, Soyeon Yoo, Sang Ah Lee
Journal of Medicine and Life Science.2023; 20(3): 126. CrossRef - Comprehensive Understanding for Application in Korean Patients with Type 2 Diabetes Mellitus of the Consensus Statement on Carbohydrate-Restricted Diets by Korean Diabetes Association, Korean Society for the Study of Obesity, and Korean Society of Hyperte
Jong Han Choi, Jee-Hyun Kang, Suk Chon
Diabetes & Metabolism Journal.2022; 46(3): 377. CrossRef - The Related Metabolic Diseases and Treatments of Obesity
Ming Yang, Shuai Liu, Chunye Zhang
Healthcare.2022; 10(9): 1616. CrossRef - Updated Meta-Analysis of Studies from 2011 to 2021 Comparing the Effectiveness of Intermittent Energy Restriction and Continuous Energy Restriction
Kyoung-Kon Kim, Jee-Hyun Kang, Eun Mi Kim
Journal of Obesity & Metabolic Syndrome.2022; 31(3): 230. CrossRef
- Metabolic changes with intermittent fasting
Original Articles
- Others
- Fasting Glucose Variability and the Risk of Dementia in Individuals with Diabetes: A Nationwide Cohort Study
- Da Young Lee, Jaeyoung Kim, Sanghyun Park, So Young Park, Ji Hee Yu, Ji A Seo, Nam Hoon Kim, Hye Jin Yoo, Sin Gon Kim, Kyung Mook Choi, Sei Hyun Baik, Kyungdo Han, Nan Hee Kim
- Diabetes Metab J. 2022;46(6):923-935. Published online May 24, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0346
- 5,549 View
- 253 Download
- 6 Web of Science
- 6 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We investigated whether fasting glucose (FG) variability could predict the risk of dementia.
Methods
This cohort study analyzed data from Koreans with diabetes after at least three health examinations by the Korean National Health Insurance Corporation between 2005 and 2010, which included at least one examination between 2009 and 2010. A total of 769,554 individuals were included, excluding those aged <40 years and those with dementia. FG variability was measured using the variability independent of the mean (FG-VIM). The incidence of dementia was defined by the International Classification of Diseases 10th Revision codes and prescription of anti-dementia medication and was subdivided into Alzheimer’s disease (AD) and vascular dementia (VD).
Results
During the 6.9-year follow-up, 54,837, 41,032, and 6,892 cases of all-cause dementia, AD, and VD, respectively, were identified. Cox proportional regression analyses showed that as the FG-VIM quartile increased, the risk of dementia serially increased after adjustment for metabolic factors, income status, and diabetes-related characteristics, including the mean FG. Participants in FG-VIM quartile 4 showed a 18%, 19%, and 17% higher risk for all-cause dementia, AD, and VD, respectively, than those in quartile 1; this particularly included non-obese patients with a longer duration of diabetes, high FG levels, dyslipidemia, and those taking glucose-lowering medications. Conversely, the baseline FG status and dementia showed a U-shaped association.
Conclusion
Increased FG variability over 5 years can predict the risk of dementia in individuals with diabetes in Korea. This finding was more pronounced in patients with less favorable metabolic profiles. -
Citations
Citations to this article as recorded by- Fasting glucose variability and risk of dementia in Parkinson’s disease: a 9-year longitudinal follow-up study of a nationwide cohort
Sung Hoon Kang, Yunjin Choi, Su Jin Chung, Seok-Joo Moon, Chi Kyung Kim, Ji Hyun Kim, Kyungmi Oh, Joon Shik Yoon, Sang Won Seo, Geum Joon Cho, Seong-Beom Koh
Frontiers in Aging Neuroscience.2024;[Epub] CrossRef - Effects of a Diabetic Microenvironment on Neurodegeneration: Special Focus on Neurological Cells
Vishal Chavda, Dhananjay Yadav, Snehal Patel, Minseok Song
Brain Sciences.2024; 14(3): 284. CrossRef - The Association of Glucose Variability and Dementia Incidence in Latinx Adults with Type 2 Diabetes: A Retrospective Study
Heather Cuevas, Elizabeth Muñoz, Divya Nagireddy, Jeeyeon Kim, Grace Ganucheau, Fathia Alomoush
Clinical Nursing Research.2023; 32(2): 249. CrossRef - The effects of long-term cumulative HbA1c exposure on the development and onset time of dementia in the patients with type 2 diabetes mellitus: Hospital based retrospective study (2005–2021)
Sunyoung Cho, Choon Ok Kim, Bong-soo Cha, Eosu Kim, Chung Mo Nam, Min-Gul Kim, Min Soo Park
Diabetes Research and Clinical Practice.2023; 201: 110721. CrossRef - Physiological Mechanisms Inherent to Diabetes Involved in the Development of Dementia: Alzheimer’s Disease
Himan Mohamed-Mohamed, Victoria García-Morales, Encarnación María Sánchez Lara, Anabel González-Acedo, Teresa Pardo-Moreno, María Isabel Tovar-Gálvez, Lucía Melguizo-Rodríguez, Juan José Ramos-Rodríguez
Neurology International.2023; 15(4): 1253. CrossRef - Cumulative effect of impaired fasting glucose on the risk of dementia in middle-aged and elderly people: a nationwide cohort study
Jin Yu, Kyu-Na Lee, Hun-Sung Kim, Kyungdo Han, Seung-Hwan Lee
Scientific Reports.2023;[Epub] CrossRef
- Fasting glucose variability and risk of dementia in Parkinson’s disease: a 9-year longitudinal follow-up study of a nationwide cohort
- Complication
- Waist Circumference and Body Mass Index Variability and Incident Diabetic Microvascular Complications: A Post Hoc Analysis of ACCORD Trial
- Daniel Nyarko Hukportie, Fu-Rong Li, Rui Zhou, Jia-Zhen Zheng, Xiao-Xiang Wu, Xian-Bo Wu
- Diabetes Metab J. 2022;46(5):767-780. Published online May 10, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0258
- 3,724 View
- 220 Download
- 7 Web of Science
- 8 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Obesity is associated with adverse health events among diabetic patients, however, the relationship between obesity fluctuation and risk of microvascular complications among this specific population is unclear. We aimed to examine the effect of waist circumference (WC) and body mass index (BMI) variability on the risk of diabetic microvascular outcome
Methods
Annually recorded anthropometric data in the Action to Control Cardiovascular Risk in Diabetes (ACCORD) study was used to examine the association of WC and BMI variability defined as variability independent of mean, with the risk of microvascular outcomes, including neuropathy, nephropathy, and retinopathy. Cox proportional hazards models were used to estimate the hazard ratios (HRs) and 95% confidence intervals (CIs) (Trial registration: ClinicalTrials.gov., no. NCT00000620).
Results
There were 4,031, 5,369, and 2,601 cases of neuropathy, nephropathy, and retinopathy during a follow-up period of 22,524, 23,941, and 23,850 person-years, respectively. Higher levels of WC and BMI variability were associated with an increased risk of neuropathy. Compared with the lowest quartile, the fully-adjusted HR (95% CI) for the highest quartile of WC and BMI variability for neuropathy risk were 1.21 (1.05 to 1.40) and 1.16 (1.00 to 1.33), respectively. Also, higher quartiles of BMI variability but not WC variability were associated with increased risk of nephropathic events. The fully-adjusted HR (95% CI) for the highest quartile compared with the lowest quartile of BMI variability was 1.31 (1.18 to 1.46). However, the results for retinopathic events were all insignificant.
Conclusion
Among participants with type 2 diabetes mellitus, WC and BMI variability were associated with a higher risk of neuropathic events, whereas BMI variability was associated with an increased risk of nephropathic events. -
Citations
Citations to this article as recorded by- Association of body mass index and blood pressure variability with 10-year mortality and renal disease progression in type 2 diabetes
Stephen Fava, Sascha Reiff
Acta Diabetologica.2024;[Epub] CrossRef - Waist Circumference and Body Mass Index Variability and Incident Diabetic Microvascular Complications: A Post Hoc Analysis of ACCORD Trial (Diabetes Metab J 2022;46:767-80)
Yun Kyung Cho
Diabetes & Metabolism Journal.2023; 47(1): 147. CrossRef - Waist Circumference and Body Mass Index Variability and Incident Diabetic Microvascular Complications: A Post Hoc Analysis of ACCORD Trial (Diabetes Metab J 2022;46:767-80)
Daniel Nyarko Hukportie, Fu-Rong Li, Rui Zhou, Jia-Zhen Zheng, Xiao-Xiang Wu, Xian-Bo Wu
Diabetes & Metabolism Journal.2023; 47(1): 150. CrossRef - Weight variability and diabetes complications
Francesco Prattichizzo, Chiara Frigé, Rosalba La Grotta, Antonio Ceriello
Diabetes Research and Clinical Practice.2023; 199: 110646. CrossRef - Risk Factors for Diabetic Retinopathy in Latin America (Mexico) and the World: A Systematic Review and Meta-Analysis
Oscar Vivanco-Rojas, Sonia López-Letayf, Valentina Londoño-Angarita, Fátima Sofía Magaña-Guerrero, Beatriz Buentello-Volante, Yonathan Garfias
Journal of Clinical Medicine.2023; 12(20): 6583. CrossRef - Effects of body weight variability on risks of macro- and microvascular outcomes in individuals with type 2 diabetes: The Rio de Janeiro type 2 diabetes cohort
Claudia R.L. Cardoso, Nathalie C. Leite, Gil F. Salles
Diabetes Research and Clinical Practice.2023; 205: 110992. CrossRef - Correlation Between the Variability of Different Obesity Indices and Diabetic Kidney Disease: A Retrospective Cohort Study Based on Populations in Taiwan
Zhenzhen Sun, Kun Wang, Chuan Yun, Fang Bai, Xiaodan Yuan, Yaujiunn Lee, Qingqing Lou
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 2791. CrossRef - Unraveling shared risk factors for diabetic foot ulcer: a comprehensive Mendelian randomization analysis
Kangli Yin, Tianci Qiao, Yongkang Zhang, Jiarui Liu, Yuzhen Wang, Fei Qi, Junlin Deng, Cheng Zhao, Yongcheng Xu, Yemin Cao
BMJ Open Diabetes Research & Care.2023; 11(6): e003523. CrossRef
- Association of body mass index and blood pressure variability with 10-year mortality and renal disease progression in type 2 diabetes
- Lifestyle
- Effectiveness of Resistance Exercise on Inflammatory Biomarkers in Patients with Type 2 Diabetes Mellitus: A Systematic Review with Meta-Analysis
- Rubén Fernández-Rodríguez, Sonia Monedero-Carrasco, Bruno Bizzozero-Peroni, Miriam Garrido-Miguel, Arthur Eumann Mesas, Vicente Martínez-Vizcaíno
- Diabetes Metab J. 2023;47(1):118-134. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2022.0007

- 9,724 View
- 308 Download
- 9 Web of Science
- 10 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Type 2 diabetes mellitus (T2DM) is related to increased inflammatory processes. The effects of resistance exercise on inflammatory biomarkers in T2DM are controversial. Our purpose was to determine the effectiveness of resistance exercise on inflammatory biomarkers in patients diagnosed with T2DM.
Methods
We searched four databases until September 2021. We included randomized clinical trials (RCTs) of the effects of resistance exercise on inflammatory biomarkers (C-reactive protein [CRP], tumor necrosis factor alpha, interleukin-6, and interleukin-10) in patients with T2DM. A random effects meta-analysis was conducted to determine the standardized mean difference (SMD) and the raw mean difference (MD) for CRP.
Results
Thirteen RCTs were included in the review, and 11 in the meta-analysis for CRP. Lower CRP levels were observed when resistance exercise was compared with the control groups (SMD=–0.20; 95% confidence interval [CI], –0.37 to –0.02). When conducting the MD meta-analysis, resistance exercise showed a significant decrease in CRP of –0.59 mg/dL (95% CI, –0.88 to –0.30); otherwise, in the control groups, the CRP values increased 0.19 mg/dL (95% CI, 0.17 to 0.21).
Conclusion
Evidence supports resistance exercise as an effective strategy to manage systemic inflammation by decreasing CRP levels in patients with T2DM. The evidence is still inconclusive for other inflammatory biomarkers. -
Citations
Citations to this article as recorded by- Körperliche Aktivität und Trainingstherapie bei Typ-2-Diabetes – ein Update
Andreas M. Nieß, Ansgar Thiel
Diabetologie und Stoffwechsel.2024; 19(01): 38. CrossRef - Genetic predisposition, lifestyle inflammation score, food-based dietary inflammatory index, and the risk for incident diabetes: Findings from the KoGES data
Hye Ah Lee, Hyesook Park, Bomi Park
Nutrition, Metabolism and Cardiovascular Diseases.2024; 34(3): 642. CrossRef - Associations of meeting 24-h movement guidelines and metabolic syndrome in Korean adults during the COVID-19 pandemic
S.W. Shin, Y. Choi, Y.H. Kang, J. Kim
Public Health.2024; 227: 187. CrossRef - Association of hypoglycemic events with cognitive impairment in patients with type 2 diabetes mellitus: Protocol for a dose-response meta-analysis
Min Ye, Ai Hong Yuan, Qi Qi Yang, Qun Wei Li, Fei Yue Li, Yan Wei, Muhammad Shahzad Aslam
PLOS ONE.2024; 19(2): e0296662. CrossRef - Exercise Interventions for the Prevention and Treatment of Anthracycline-Induced Cardiotoxicity in Women with Breast Cancer: A Systematic Review
Hongmei Li, Haiyun Liu, Boliang Wang, Xiao Jia, Jingjing Yu, Yurong Zhang, Die Sang, Yimin Zhang
Journal of Science in Sport and Exercise.2024;[Epub] CrossRef - Additive impact of diabetes and sarcopenia on all-cause and cardiovascular mortality: A longitudinal nationwide population-based study
Eyun Song, Soon Young Hwang, Min Jeong Park, Ahreum Jang, Kyeong Jin Kim, Ji Hee Yu, Nam Hoon Kim, Hye Jin Yoo, Ji A. Seo, Sin Gon Kim, Nan Hee Kim, Sei Hyun Baik, Kyung Mook Choi
Metabolism.2023; 148: 155678. CrossRef - Endothelial progenitor cell response to a multicomponent exercise training program in adults with cardiovascular risk factors
Suiane Cavalcante, Manuel Teixeira, Marisol Gouveia, Ana Duarte, Miriam Ferreira, Maria I. Simões, Maria Conceição, Mariana Costa, Ilda P. Ribeiro, Ana Cristina Gonçalves, José Oliveira, Fernando Ribeiro
German Journal of Exercise and Sport Research.2023; 53(2): 225. CrossRef - “Does Physical Exercise Promote Health Benefits for Diabetic Patients during the COVID-19 Pandemic?”: A Systematic Review
Erivaldo de Souza, Daniela Meneses-Santos, Josué Cruz Santos, Felipe J. Aidar, Carla Roberta de Oliveira Carvalho, Jymmys Lopes dos Santos, Anderson Carlos Marçal
Sports.2023; 11(10): 192. CrossRef - Effect of exercise on inflammatory markers in postmenopausal women with overweight and obesity: A systematic review and meta-analysis
Liang Tan, Weihua Yan, Weilin Yang, Agata Kamionka, Mariusz Lipowski, Zijian Zhao, Gang Zhao
Experimental Gerontology.2023; 183: 112310. CrossRef - Resistance Training Improves Beta Cell Glucose Sensing and Survival in Diabetic Models
Gabriela Alves Bronczek, Gabriela Moreira Soares, Carine Marmentini, Antonio Carlos Boschero, José Maria Costa-Júnior
International Journal of Molecular Sciences.2022; 23(16): 9427. CrossRef
- Körperliche Aktivität und Trainingstherapie bei Typ-2-Diabetes – ein Update
Short Communication
- Drug/Regimen
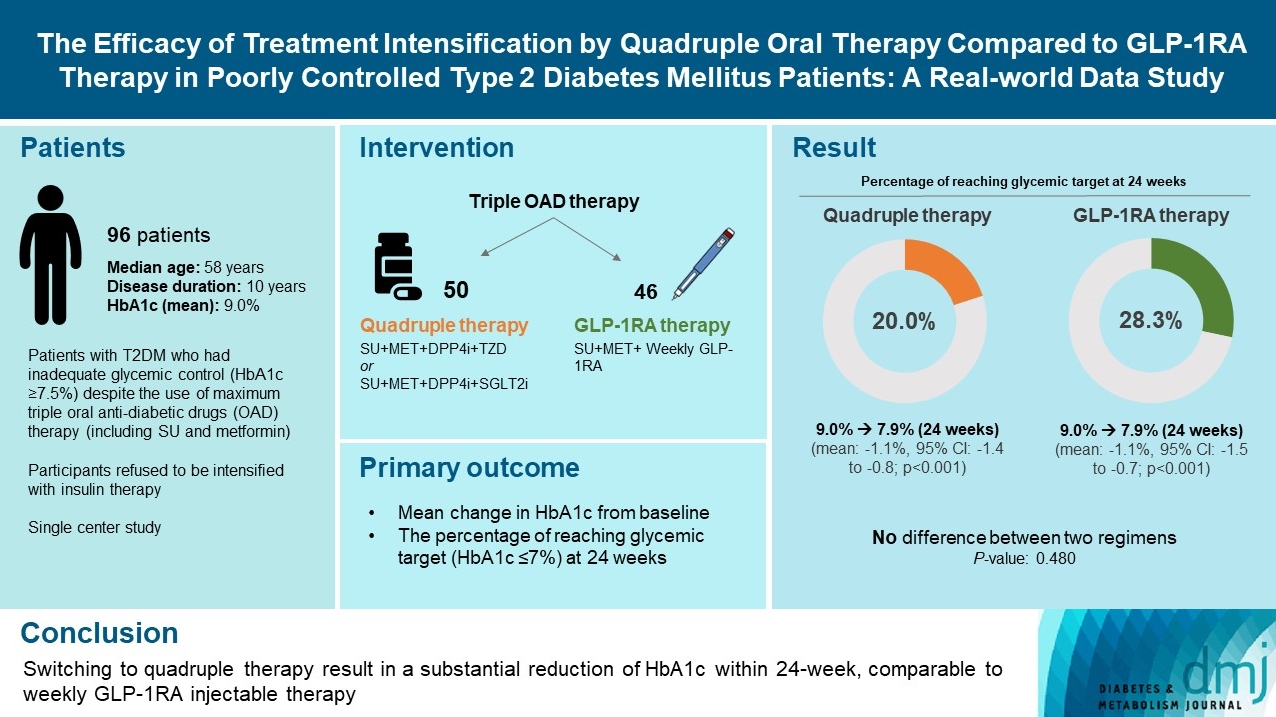
- The Efficacy of Treatment Intensification by Quadruple Oral Therapy Compared to GLP-1RA Therapy in Poorly Controlled Type 2 Diabetes Mellitus Patients: A Real-World Data Study
- Minyoung Kim, Hosu Kim, Kyong Young Kim, Soo Kyoung Kim, Junghwa Jung, Jong Ryeal Hahm, Jaehoon Jung, Jong Ha Baek
- Diabetes Metab J. 2023;47(1):135-139. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0373
- 7,460 View
- 296 Download
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - We compared the glycemic efficacy of treatment intensification between quadruple oral antidiabetic drug therapy and once-weekly glucagon-like peptide-1 receptor agonist (GLP-1RA)-based triple therapy in patients with poorly controlled type 2 diabetes mellitus refractory to triple oral therapy. For 24 weeks, changes in glycosylated hemoglobin (HbA1c) from baseline were compared between the two treatment groups. Of all 96 patients, 50 patients were treated with quadruple therapy, and 46 were treated with GLP-1RA therapy. Reductions in HbA1c for 24 weeks were comparable (in both, 1.1% reduction from baseline; P=0.59). Meanwhile, lower C-peptide level was associated with a lower glucose-lowering response of GLP-1RA therapy (R=0.3, P=0.04) but not with quadruple therapy (R=–0.13, P=0.40). HbA1c reduction by GLP-1RA therapy was inferior to that by quadruple therapy in the low C-peptide subgroup (mean, –0.1% vs. –1.3%; P=0.04). Treatment intensification by switching to quadruple oral therapy showed similar glucose-lowering efficacy to weekly GLP-1RA-based triple therapy. Meanwhile, the therapeutic response was affected by C-peptide levels in the GLP-1RA therapy group but not in the quadruple therapy group.
Original Articles
- Drug/Regimen
- Effect of Lactobacillus plantarum LMT1-48 on Body Fat in Overweight Subjects: A Randomized, Double-Blind, Placebo-Controlled Trial
- Minji Sohn, Hyeyoung Jung, Woo Shun Lee, Tai Hoon Kim, Soo Lim
- Diabetes Metab J. 2023;47(1):92-103. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0370
- 8,825 View
- 380 Download
- 9 Web of Science
- 12 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
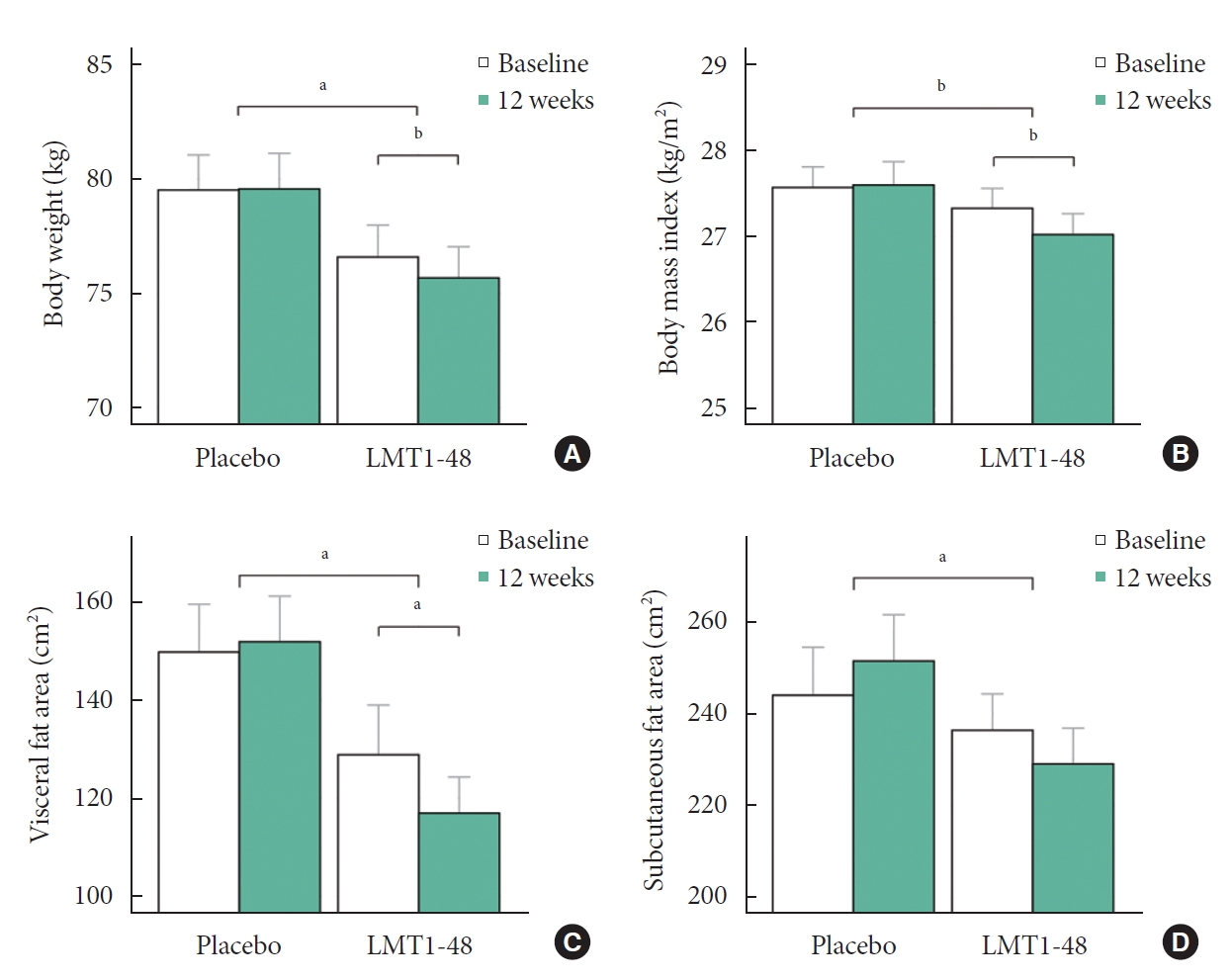
We investigated whether Lactobacillus plantarum strain LMT1-48, isolated from Korean fermented foods and newborn feces, is a suitable probiotic supplement to treat overweight subjects.
Methods
In this randomized, double-blind, placebo-controlled clinical trial, 100 volunteers with a body mass index of 25 to 30 kg/m2 were assigned randomly (1:1) to receive 2×1010 colony forming units of LMT1-48 or to a placebo treatment group. Body composition was measured by dual-energy X-ray absorptiometry, and abdominal visceral fat area (VFA) and subcutaneous fat area were measured by computed tomography scanning. Changes in body fat, VFA, anthropometric parameters, and biomarkers were compared between the two treatment groups (ClinicalTrials.gov number: NCT03759743).
Results
After 12 weeks of treatment, the body weight decreased significantly from 76.6±9.4 to 75.7±9.2 kg in the LMT1-48 group but did not change in the placebo group (P=0.022 between groups). A similar pattern was found in abdominal VFA between the two groups (P=0.041). Serum insulin levels, the corresponding homeostasis model assessment of insulin resistance, and leptin levels decreased in the LMT1-48 group but increased in the placebo group (all P<0.05). Decrease in body weight and body mass index by treatment with LMT1-48 was correlated with increase in Lactobacillus levels significantly. LMT1-48 also increased Oscillibacter levels significantly, which were negatively correlated with triglyceride and alanine transaminase levels.
Conclusion
Administration of LMT1-48 decreased body weight, abdominal VFA, insulin resistance, and leptin levels in these subjects with overweight, suggesting its anti-obesogenic therapeutic potential. -
Citations
Citations to this article as recorded by- Beneficial effects of the probiotics and synbiotics supplementation on anthropometric indices and body composition in adults: A systematic review and meta‐analysis
Saeede Saadati, Kaveh Naseri, Omid Asbaghi, Mohsen Yousefi, Elnaz Golalipour, Barbora de Courten
Obesity Reviews.2024;[Epub] CrossRef - The Effect of Lactobacillus plantarum on the Fecal Microbiota, Short Chain Fatty Acids, Odorous Substances, and Blood Biochemical Indices of Cats
Bing Han, Shukun Liang, Jintao Sun, Hui Tao, Zhenlong Wang, Baosheng Liu, Xiumin Wang, Jie Liu, Jinquan Wang
Microorganisms.2024; 12(1): 91. CrossRef - Natto alleviates hyperlipidemia in high-fat diet-fed mice by modulating the composition and metabolic function of gut microbiota
Le-Yuan Shang, Shuo Zhang, Min Zhang, Xiao-Dong Sun, Qi Wang, Yu-Jie Liu, Yan-Ni Zhao, Mei Zhao, Peng-Jiao Wang, Xiu-Li Gao
Journal of Functional Foods.2024; 112: 105968. CrossRef - Microbial-Based Bioactive Compounds to Alleviate Inflammation in Obesity
Oladayo Emmanuel Apalowo, Grace Adeola Adegoye, Tolulope Mobolaji Obuotor
Current Issues in Molecular Biology.2024; 46(3): 1810. CrossRef - Anti-obesogenic effects of plant natural products: A focus on Korean traditional foods
Gitishree Das, Luis Alfonso Jiménez Ortega, Sandra Gonçalves, J. Basilio Heredia, Maria de Lourdes Gomes Pereira, Anabela Romano, Han-Seung Shin, Jayanta Kumar Patra
Trends in Food Science & Technology.2024; : 104470. CrossRef - A 12-Week, Single-Centre, Randomised, Double-Blind, Placebo-Controlled, Parallel-Design Clinical Trial for the Evaluation of the Efficacy and Safety of Lactiplantibacillus plantarum SKO-001 in Reducing Body Fat
Seon Mi Shin, Jeong-Su Park, Sang Back Kim, Young Hee Cho, Hee Seo, Hak Sung Lee
Nutrients.2024; 16(8): 1137. CrossRef - 3D printing of microencapsulated Lactobacillus rhamnosus for oral delivery
Pablo Rosas-Val, Masoud Adhami, Ana Brotons-Canto, Carlos Gamazo, Juan M. Irache, Eneko Larrañeta
International Journal of Pharmaceutics.2023; 641: 123058. CrossRef - Gut commensal Kineothrix alysoides mitigates liver dysfunction by restoring lipid metabolism and gut microbial balance
Kyoung Jin Choi, Mi Young Yoon, Ji-Eun Kim, Sang Sun Yoon
Scientific Reports.2023;[Epub] CrossRef - Ameliorating Effects of Bifidobacterium longum subsp. infantis FB3-14 against High-Fat-Diet-Induced Obesity and Gut Microbiota Disorder
Ruixin Kou, Jin Wang, Ang Li, Yuanyifei Wang, Bowei Zhang, Jingmin Liu, Yi Sun, Shuo Wang
Nutrients.2023; 15(19): 4104. CrossRef - Effect of Continuous Ingestion of Bifidobacteria and Inulin on Reducing Body Fat: A Randomized, Double-Blind, Placebo-Controlled, Parallel-Group Comparison Study
Yuhei Baba, Yasuo Saito, Mei Kadowaki, Naoki Azuma, Daisuke Tsuge
Nutrients.2023; 15(24): 5025. CrossRef - A Review of the Potential of Probiotic Bacteria in Managing the Body Weight of Obese Individuals
A Didban, L Manafi, R Mahmoudi
Journal of Health and Hygiene.2023; 14(4): 388. CrossRef - Plant-Derived Lactobacillus paracasei IJH-SONE68 Improves the Gut Microbiota Associated with Hepatic Disorders: A Randomized, Double-Blind, and Placebo-Controlled Clinical Trial
Narandalai Danshiitsoodol, Masafumi Noda, Keishi Kanno, Tomoyuki Uchida, Masanori Sugiyama
Nutrients.2022; 14(21): 4492. CrossRef
- Beneficial effects of the probiotics and synbiotics supplementation on anthropometric indices and body composition in adults: A systematic review and meta‐analysis
- Others
- Influence of Maternal Diabetes on the Risk of Neurodevelopmental Disorders in Offspring in the Prenatal and Postnatal Periods
- Verónica Perea, Xavier Urquizu, Maite Valverde, Marina Macias, Anna Carmona, Esther Esteve, Gemma Escribano, Nuria Pons, Oriol Giménez, Teresa Gironés, Andreu Simó-Servat, Andrea Domenech, Núria Alonso-Carril, Carme Quirós, Antonio J. Amor, Eva López, Maria José Barahona
- Diabetes Metab J. 2022;46(6):912-922. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0340
- 4,761 View
- 249 Download
- 5 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
This study aimed to evaluate the influence of maternal diabetes in the risk of neurodevelopmental disorders in offspring in the prenatal and postnatal periods.
Methods
This cohort study included singleton gestational diabetes mellitus (GDM) pregnancies >22 weeks’ gestation with live newborns between 1991 and 2008. The control group was randomly selected and matched (1:2) for maternal age, weeks of gestation and birth year. Cox regression models estimated the effect of GDM on the risk of attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), and maternal type 2 diabetes mellitus (T2DM). Moreover, interaction between maternal T2DM and GDM-ADHD relationship was evaluated.
Results
Children (n=3,123) were included (1,073 GDM; 2,050 control group). The median follow-up was 18.2 years (interquartile range, 14.2 to 22.3) (n=323 with ADHD, n=36 with ASD, and n=275 from women who developed T2DM). GDM exposure was associated with ADHD (hazard ratio [HR]crude, 1.67; 95% confidence interval [CI], 1.33 to 2.07) (HRadjusted, 1.64; 95% CI, 1.31 to 2.05). This association remained significant regardless of the treatment (diet or insulin) and diagnosis after 26 weeks of gestation. Children of mothers who developed T2DM presented higher rates of ADHD (14.2 vs. 10%, P=0.029). However, no interaction was found when T2DM was included in the GDM and ADHD models (P>0.05). GDM was not associated with an increased risk of ASD (HRadjusted, 1.46; 95% CI, 0.74 to 2.84).
Conclusion
Prenatal exposure to GDM increases the risk of ADHD in offspring, regardless of GDM treatment complexity. However, postnatal exposure to maternal T2DM was not related to the development of ADHD. -
Citations
Citations to this article as recorded by- Effects of a Diabetic Microenvironment on Neurodegeneration: Special Focus on Neurological Cells
Vishal Chavda, Dhananjay Yadav, Snehal Patel, Minseok Song
Brain Sciences.2024; 14(3): 284. CrossRef - Maternal Diabetes Deregulates the Expression of Mecp2 via miR-26b-5p in Mouse Embryonic Neural Stem Cells
Sukanya Shyamasundar, Seshadri Ramya, Deepika Kandilya, Dinesh Kumar Srinivasan, Boon Huat Bay, Suraiya Anjum Ansari, S Thameem Dheen
Cells.2023; 12(11): 1516. CrossRef - Evaluating the prospects of using gestational diabetes mellitus model to find means of pharmacological correction of the disorders in rat offspring
A. S. Solomina, A. V. Rodina, K. S. Kachalov, A. D. Zakharov, A. D. Durnev
Pharmacokinetics and Pharmacodynamics.2023; (2): 45. CrossRef - Hair and cord blood element levels and their relationship with air pollution, dietary intake, gestational diabetes mellitus, and infant neurodevelopment
Yin-Yin Xia, Jamie V. de Seymour, Xiao-Jia Yang, Lin-Wei Zhou, Yue Liu, Yang Yang, Kathryn L. Beck, Cathryn A. Conlon, Toby Mansell, Boris Novakovic, Richard Saffery, Ting-Li Han, Hua Zhang, Philip N. Baker
Clinical Nutrition.2023; 42(10): 1875. CrossRef - Role of Excessive Weight Gain During Gestation in the Risk of ADHD in Offspring of Women With Gestational Diabetes
Verónica Perea, Andreu Simó-Servat, Carmen Quirós, Nuria Alonso-Carril, Maite Valverde, Xavier Urquizu, Antonio J Amor, Eva López, Maria-José Barahona
The Journal of Clinical Endocrinology & Metabolism.2022; 107(10): e4203. CrossRef
- Effects of a Diabetic Microenvironment on Neurodegeneration: Special Focus on Neurological Cells
- Metabolic Risk/Epidemiology
- Impact of Older Age Adiposity on Incident Diabetes: A Community-Based Cohort Study in China
- Anthony Chen, Weiju Zhou, Jian Hou, Alan Nevill, Yuanlin Ding, Yuhui Wan, Rebecca Jester, Xia Qin, Zhi Hu, Ruoling Chen
- Diabetes Metab J. 2022;46(5):733-746. Published online April 29, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0215
- 3,960 View
- 197 Download
- 2 Web of Science
- 2 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Obesity classifications vary globally and the impact of older age adiposity on incident diabetes has not been well-studied.
Methods
We examined a random sample of 2,809 participants aged ≥60 years in China, who were free of diabetes at baseline and were followed up for up to 10 years to document diabetes (n=178). The incidence of diabetes was assessed in relation to different cut-off points of body mass index (BMI) and waist circumference (WC) in multiple adjusted Cox regression models.
Results
The diabetic risk in the cohort increased linearly with the continuous and quartile variables of BMI and WC. The BMI-World Health Organization (WHO) and BMI-China criteria analysis did not show such a linear relationship, however, the BMI-Asian/Hong Kong criteria did; adjusted hazards ratio (HR) was 0.42 (95% confidence interval [CI], 0.20 to 0.90) in BMI <20 kg/m2, 1.46 (95% CI, 0.99 to 2.14) in 23–≤26 kg/m2, and 1.63 (95% CI, 1.09 to 2.45) in ≥26 kg/m2. The WC-China criteria revealed a slightly better prediction of diabetes (adjusted HRs were 1.79 [95% CI, 1.21 to 2.66] and 1.87 [95% CI, 1.22 to 2.88] in central obese action levels 1 and 2) than the WC-WHO. The combination of the BMI-Asian/Hong Kong with WC-China demonstrated the strongest prediction. There were no gender differences in the impact of adiposity on diabetes.
Conclusion
In older Chinese, BMI-Asian/Hong Kong criteria is a better predictor of diabetes than other BMI criterion. Its combination with WC-China improved the prediction of adiposity to diabetes, which would help manage bodyweight in older age to reduce the risk of diabetes. -
Citations
Citations to this article as recorded by- Association of air pollution with dementia: a systematic review with meta-analysis including new cohort data from China
Jie Tang, Anthony Chen, Fan He, Martin Shipley, Alan Nevill, Hugh Coe, Zhi Hu, Tao Zhang, Haidong Kan, Eric Brunner, Xuguang Tao, Ruoling Chen
Environmental Research.2023; 223: 115048. CrossRef - Impact of fish consumption on all-cause mortality in older people with and without dementia: a community-based cohort study
Aishat T. Bakre, Anthony Chen, Xuguang Tao, Jian Hou, Yuyou Yao, Alain Nevill, James J. Tang, Sabine Rohrmann, Jindong Ni, Zhi Hu, John Copeland, Ruoling Chen
European Journal of Nutrition.2022; 61(7): 3785. CrossRef
- Association of air pollution with dementia: a systematic review with meta-analysis including new cohort data from China
- Metabolic Risk/Epidemiology
- Higher Muscle Mass Protects Women with Gestational Diabetes Mellitus from Progression to Type 2 Diabetes Mellitus
- Yujin Shin, Joon Ho Moon, Tae Jung Oh, Chang Ho Ahn, Jae Hoon Moon, Sung Hee Choi, Hak Chul Jang
- Diabetes Metab J. 2022;46(6):890-900. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0334
- 4,691 View
- 223 Download
- 2 Web of Science
- 3 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
We evaluated whether postpartum muscle mass affects the risk of type 2 diabetes mellitus (T2DM) in Korean women with gestational diabetes mellitus (GDM).
Methods
A total of 305 women with GDM (mean age, 34.9 years) was prospectively evaluated for incident prediabetes and T2DM from 2 months after delivery and annually thereafter. Appendicular skeletal muscle mass (ASM) was assessed with bioelectrical impedance analysis at the initial postpartum visit, and ASM, either divided by body mass index (BMI) or squared height, and the absolute ASM were used as muscle mass indices. The risk of incident prediabetes and T2DM was assessed according to tertiles of these indices using a logistic regression model.
Results
After a mean follow-up duration of 3.3 years, the highest ASM/BMI tertile group had a 61% lower risk of incident prediabetes and T2DM compared to the lowest tertile group, and this remained significant after we adjusted for covariates (adjusted odds ratio, 0.37; 95% confidence interval [CI], 0.15 to 0.92; P=0.032). Equivalent findings were observed in normal weight women (BMI <23 kg/m2), but this association was not significant for overweight women (BMI ≥23 kg/m2). Absolute ASM or ASM/height2 was not associated with the risk of postpartum T2DM.
Conclusion
A higher muscle mass, as defined by the ASM/BMI index, was associated with a lower risk of postpartum prediabetes and T2DM in Korean women with GDM. -
Citations
Citations to this article as recorded by- More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
Melanie S. Haines, Aaron Leong, Bianca C. Porneala, Victor W. Zhong, Cora E. Lewis, Pamela J. Schreiner, Karen K. Miller, James B. Meigs, Mercedes R. Carnethon
Nutrition, Metabolism and Cardiovascular Diseases.2023; 33(1): 105. CrossRef - The Association of the Triglyceride and Muscle to Fat Ratio During Early Pregnancy with the Development of Gestational Diabetes Mellitus
Fang Wang, Yuan-Yuan Bao, Kang Yu
Diabetes, Metabolic Syndrome and Obesity.2023; Volume 16: 3187. CrossRef - Correlation of body composition in early pregnancy on gestational diabetes mellitus under different body weights before pregnancy
Li Xintong, Xu Dongmei, Zhang Li, Cao Ruimin, Hao Yide, Cui Lingling, Chen Tingting, Guo Yingying, Li Jiaxin
Frontiers in Endocrinology.2022;[Epub] CrossRef
- More appendicular lean mass relative to body mass index is associated with lower incident diabetes in middle-aged adults in the CARDIA study
- Drug/Regimen
- Comparison of Serum Ketone Levels and Cardiometabolic Efficacy of Dapagliflozin versus Sitagliptin among Insulin-Treated Chinese Patients with Type 2 Diabetes Mellitus
- Chi-Ho Lee, Mei-Zhen Wu, David Tak-Wai Lui, Darren Shing-Hei Chan, Carol Ho-Yi Fong, Sammy Wing-Ming Shiu, Ying Wong, Alan Chun-Hong Lee, Joanne King-Yan Lam, Yu-Cho Woo, Karen Siu-Ling Lam, Kelvin Kai-Hang Yiu, Kathryn Choon-Beng Tan
- Diabetes Metab J. 2022;46(6):843-854. Published online April 28, 2022
- DOI: https://doi.org/10.4093/dmj.2021.0319
- 4,919 View
- 255 Download
- 4 Web of Science
- 5 Crossref
-
 Abstract
Abstract
 PDF
PDF Supplementary Material
Supplementary Material PubReader
PubReader  ePub
ePub - Background
Insulin-treated patients with long duration of type 2 diabetes mellitus (T2DM) are at increased risk of ketoacidosis related to sodium-glucose co-transporter 2 inhibitor (SGLT2i). The extent of circulating ketone elevation in these patients remains unknown. We conducted this study to compare the serum ketone response between dapagliflozin, an SGLT2i, and sitagliptin, a dipeptidyl peptidase-4 inhibitor, among insulin-treated T2DM patients.
Methods
This was a randomized, open-label, active comparator-controlled study involving 60 insulin-treated T2DM patients. Participants were randomized 1:1 for 24-week of dapagliflozin 10 mg daily or sitagliptin 100 mg daily. Serum β-hydroxybutyrate (BHB) levels were measured at baseline, 12 and 24 weeks after intervention. Comprehensive cardiometabolic assessments were performed with measurements of high-density lipoprotein cholesterol (HDL-C) cholesterol efflux capacity (CEC), vibration-controlled transient elastography and echocardiography.
Results
Among these 60 insulin-treated participants (mean age 58.8 years, diabetes duration 18.2 years, glycosylated hemoglobin 8.87%), as compared with sitagliptin, serum BHB levels increased significantly after 24 weeks of dapagliflozin (P=0.045), with a median of 27% increase from baseline. Change in serum BHB levels correlated significantly with change in free fatty acid levels. Despite similar glucose lowering, dapagliflozin led to significant improvements in body weight (P=0.006), waist circumference (P=0.028), HDL-C (P=0.041), CEC (P=0.045), controlled attenuation parameter (P=0.007), and liver stiffness (P=0.022). Average E/e’, an echocardiographic index of left ventricular diastolic dysfunction, was also significantly lower at 24 weeks in participants treated with dapagliflozin (P=0.037).
Conclusion
Among insulin-treated T2DM patients with long diabetes duration, compared to sitagliptin, dapagliflozin modestly increased ketone levels and was associated with cardiometabolic benefits. -
Citations
Citations to this article as recorded by- Serum thrombospondin‐2 level changes with liver stiffness improvement in patients with type 2 diabetes
Jimmy Ho Cheung Mak, David Tak‐Wai Lui, Carol Ho‐Yi Fong, Chloe Yu‐Yan Cheung, Ying Wong, Alan Chun‐Hong Lee, Ruby Lai‐Chong Hoo, Aimin Xu, Kathryn Choon‐Beng Tan, Karen Siu‐Ling Lam, Chi‐Ho Lee
Clinical Endocrinology.2024; 100(3): 230. CrossRef - SGLT-2 inhibitors as novel treatments of multiple organ fibrosis
Junpei Hu, Jianhui Teng, Shan Hui, Lihui Liang
Heliyon.2024; 10(8): e29486. CrossRef - Effect of sodium-glucose cotransporter protein-2 inhibitors on left ventricular hypertrophy in patients with type 2 diabetes: A systematic review and meta-analysis
Yao Wang, Yujie Zhong, Zhehao Zhang, Shuhao Yang, Qianying Zhang, Bingyang Chu, Xulin Hu
Frontiers in Endocrinology.2023;[Epub] CrossRef - Effects of SGLT2 inhibitors on hepatic fibrosis and steatosis: A systematic review and meta-analysis
Peipei Zhou, Ying Tan, Zhenning Hao, Weilong Xu, Xiqiao Zhou, Jiangyi Yu
Frontiers in Endocrinology.2023;[Epub] CrossRef - The impact of sodium-glucose Cotransporter-2 inhibitors on lipid profile: A meta-analysis of 28 randomized controlled trials
Gang Fan, Dian long Guo, Hong Zuo
European Journal of Pharmacology.2023; 959: 176087. CrossRef
- Serum thrombospondin‐2 level changes with liver stiffness improvement in patients with type 2 diabetes

 KDA
KDA
 First
First Prev
Prev





