Association of Visit-to-Visit Variability of Blood Pressure with Cardiovascular Disease among Type 2 Diabetes Mellitus Patients: A Cohort Study
Article information
Abstract
Background
Increasing evidence has shown that visit-to-visit variability (VVV) of blood pressure (BP) is associated with an increased risk of cardiovascular disease (CVD). The objective of this study was to evaluate the impact of VVV of systolic blood pressure (SBP) and diastolic blood pressure (DBP) on the risk of CVD among patients with type 2 diabetes mellitus (T2DM) in China.
Methods
We conducted a retrospective cohort study of 10,163 T2DM patients who were not previously diagnosed with CVD from January 2008 to December 2012 in Ningbo, China. The VVV of BP was calculated using five metrics, including standard deviation (SD), coefficient of variation (CV), variation independent of mean, average real variability, and successive variability (SV) of measurements, obtained over a 24-month measurement period. Hazard ratios and 95% confidence intervals (CIs) were estimated by Cox proportional hazards regression models for the associations of variability in BP with risk of CVD.
Results
A total of 894 CVD events were observed during a median follow-up of 49.5 months. The hazard ratio in the highest quintile of SD of SBP was 1.24 (95% CI, 1.01 to 1.52) compared with patients in the lowest quintile. The association between higher VVV of DBP and risk of CVD was not consistent across different metrics and sensitivity analyses.
Conclusion
Higher VVV of SBP was associated with an increased risk of CVD, irrespective of the mean SBP level. Future studies are needed to confirm these findings.
INTRODUCTION
Cardiovascular disease (CVD) is a major cause of death and disability in patients with diabetes and consumes a significant portion of diabetes resources at a national level [1]. The approach recommended by the diabetic management guidelines is to maintain optimal blood pressure (BP) [23]. Recently, increasing attention has been paid to the prognostic value of visit-to-visit variability (VVV) for CVD events [45].
VVV of BP was first investigated by Grove et al. [6]. Rothwell et al. [7] found that VVV in systolic blood pressure (SBP) and maximum SBP were strong predictors for stroke, independent of mean SBP. Several prospective as well as retrospective studies of VVV of SBP were conducted in various patient populations [7891011]. A recent meta-analysis that included 23 studies concluded that VVV of SBP was associated with a risk of CVD incidence [12]. A limited number of studies have reported the association between VVV of SBP and CVD among patients with diabetes [1213141516], but only one study reported that VVV of diastolic blood pressure (DBP) was a significant predictor of CVD incidence among patients with type 2 diabetes mellitus (T2DM) [17]. Moreover, the effect of VVV of SBP on cardiovascular events may demonstrate heterogeneity between Chinese and non-Chinese populations. A study conducted in the UK revealed a lower risk of CVD among diabetic patients of Chinese ethnicity compared to the risk of patients of other ethnicities, such as Caucasian and Indian [18]. Evidence on the association between VVV of SBP and CVD among Chinese diabetic patients remains limited.
Thus, population-based studies among patients with diabetes are still needed to increase the body of evidence on the association of VVV of BP with risk of CVD events. We conducted a large retrospective cohort study aimed to evaluate the association between VVV of BP and CVD risk among T2DM patients in China.
METHODS
Study design
This population-based retrospective cohort study was conducted between January 1, 2008 and December 31, 2012 in Yinzhou District, Ningbo, Zhejiang province, China. Yinzhou is the largest district in Ningbo and has an adult population of approximately 961,000 people. Yinzhou has established a Health Information System (Yinzhou HIS) covering all health services, including public hospitals and primary-care clinics [1920]. In Yinzhou, CVDs and diabetes were required to be reported for disease surveillance and management by local general practitioners (GPs). GPs were also required to follow up with these patients at an interval of approximately 3 months, and outcome records were uploaded into the Chronic Disease Registry System. For CVD cases treated outside the Yinzhou region, the events were recorded and updated during the follow-up with the GP.
Data on T2DM patients were retrieved from the Chronic Disease Registry System in the Yinzhou HIS, which were coded as E11.X according to the 10th version of the International Classification of Diseases (ICD-10). A unique and encoded identifier was created for each patient in the Yinzhou HIS. We used this identifier to link all related databases to obtain the relevant covariates. The date of the first BP recording was defined as the baseline. The BP measurement period was defined as 24 months after baseline; thus, a total of nine BP measurements were used to calculate the VVV of BP. In the current study, T2DM patients with the first BP measurement record between January 1, 2008 and December 31, 2012 were included. The exclusion criteria were as follows: (1) Patients who had CVD events before baseline or during the BP measurement period and (2) Patients who were not followed regularly at an interval of approximately 3 months or had more than one missing BP value during the measurement period.
CVD events consisted of myocardial infarction and cerebrovascular disease, which were coded as I20 to I25 and I60 to I69 according to the ICD-10 in the Yinzhou HIS. Each patient was followed until the date of a cardiovascular event, death, the last known follow-up date or December 31, 2016, whichever occurred first.
BP variability measurements and visit-to-visit variability
The procedures for measuring BP during the BP measurement period followed standardized guidelines that included quality control measures [21]. The BPs of all the subjects were measured using a mercury sphygmomanometer while the patients were in a seated position after resting for 5 minutes. The first and fifth Korotkoff sounds were used to measure SBP and DBP, respectively. The quality control measures implemented for BP measurement were as follows. All hospitals and clinics in the region followed the same standardized protocol for BP measurement. At least two BP measurements were taken at each visit with a break between the measurements of at least 1 minute, and the average value was recorded by community doctors. The mercury sphygmomanometer was calibrated every six months. Talking and a full bladder were avoided during the measurement of BP. The average of the BP measurements was recorded by the doctors and uploaded into the Yinzhou HIS.
The standard deviation (SD) was used as the main metric of visit-to-visit blood pressure variability (BPV), and the other four metrics included the coefficient of variation (CV), successive variability (SV), average real variability (ARV), and variance independent of the mean (VIM). SD and CV account for the total variability around the mean BP across visits, while ARV and SV measure the differences in BP from one visit to the next. VIM was first used by Rothwell mainly to reduce the correlation between the measurement of BPV (take SD as an example) and the mean BP value. VIM was defined as SD/(meanλ), while λ was calculated through curve fitting. The mean BP value for each patient, averaged over all BP values recorded during the BP measurement period, was considered as a covariate. Detailed information for all metrics of VVV BP is listed in Supplementary Table 1.
Baseline covariates included the demographic characteristics, clinical parameters, and treatment modalities of the patients. Demographic characteristics included age, sex, body mass index (BMI), and smoking and alcohol drinking status. Current smoking was defined as having smoked at least one cigarette per day for 1 year or more. Current alcohol drinkers were defined as patients who consumed at least 100 g of any type of alcohol per week for the last year. Clinical parameters consisted of duration of diabetes and lipid profiles (including fasting plasma glucose, total cholesterol, triglycerides, high density lipoprotein cholesterol, and low density lipoprotein cholesterol). Treatment modalities included the use of antihypertensive drugs, oral antidiabetic drugs or insulin, and the use of lipid lowering treatments.
Statistical analysis
Descriptive analyses were used to analyze the baseline characteristics. Univariate analyses were used to test the differences among the quintiles of the SDs of SBP of patients and between patients included and excluded from the present study. Pearson's correlation coefficients were estimated between measures of VVV of BP and mean BP during the measurement period. Multivariate Cox proportional hazards regression models were performed to evaluate the effect of BP variability on cardiovascular outcomes after adjusting for age (continuous variable), sex (man or woman), duration of diabetes mellitus (continuous variable), smoking status (current or not), alcohol drinking status (current or not), BMI (continuous variable), use of glucose treatment (yes or no), use of BP lowering treatment (yes or no), and use of lipid lowering treatment (yes or no) (model I), or variables in model I plus mean BP values (continuous variable) (model II). Each BP variability measure was categorized by quintiles with a reference level of the lowest quintile. Linear trends across the quintiles were calculated by including the quintile as a continuous variable (ranging from 1 to 5) in the models.
Subgroup analyses were conducted through stratification by age (>60 and ≤60 years), sex (male or female), use of anti-hypertensive drugs (yes or no), and use of lipid lowering treatments to minimize potential bias. We also performed sensitivity analyses to examine the stability of our results. Patients with eight (n=5,642) and nine (n=4,521) BP readings were evaluated separately. Sensitivity analyses were also performed by restricting the analysis to patients with BP ≤140/90 and ≤130/80 mm Hg during the measurement period. We also excluded patients who had no information regarding their lipid profile at baseline, who were diagnosed with diabetes mellitus less than 1 year prior or who were followed for less than 1 year after the measurement period. In addition, we classified the SDs of SBP into five groups (≤5, 5.1 to 7.5, 7.6 to 10, 10.1 to 15, and >15 mm Hg) to determine whether maintaining an SBP within 10 mm Hg was an optimal target for BP variability control [13]. To explore the nonlinear relationships between CVD and the SDs of SBP as a continuous variable, we used restricted cubic splines with 4 knots placed at 5, 7.5, 10, and 15 mm Hg. All analyses were conducted in R software 3.3.2 (https://www.r-project.org/). A two-sided P<0.05 was considered statistically significant.
Ethics approval and consent to participate
This study conformed to the guidelines of the Declaration of Helsinki, and the study procedures were reviewed and approved by the ethics committee of the School of Medicine, Zhejiang University (No. 2018-028). Each patient agreed to participate and signed the informed consent form.
RESULTS
A total of 10,163 T2DM patients were included in the final analysis. Fig. 1 shows a flow chart of this study. We excluded 450 patients who had a history of CVD at baseline, 387 patients who developed CVD during the BP measurement period and 3,167 patients who were not regularly followed at an interval of 3 months or who had more than one missing BP value. The mean age at baseline was 61.3 years, 60.9% were female, and the median duration of DM was 40 months. The mean BP was 130.1/80.2 mm Hg at baseline. Table 1 summarizes the baseline characteristics of all patients included. The characteristics of the patients excluded from the current study are listed in Supplementary Table 2. During a median of 49.5 months of follow-up, a total of 894 cardiovascular events were recorded. Pearson's correlation coefficients between mean BP level and VVV BP metrics are shown in Supplementary Table 3.
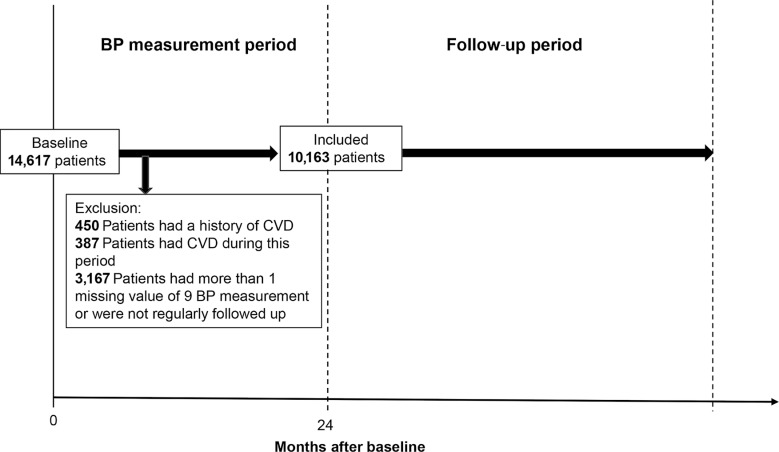
Study design for the investigation of the association of visit-to-visit variability (VVV) in blood pressure (BP) and cardiovascular disease (CVD). The BP measurements during the measurement period (0, 3, 6, 9, 12, 15, 18, 21, 24 months after baseline) were used to calculate the mean and VVV. The median follow-up period was 49.5 months.
Table 2 presents the association of SBP VVV with the risk of cardiovascular events after adjusting for age, sex, duration of diabetes mellitus, BMI, smoking status, alcohol drinking status, fasting plasma glucose, use of any BP lowering treatments, use of any blood glucose lowering treatments and use of any lipid lowering treatments (model I). Patients in the highest quintile of SBP SD had a 29% higher risk of CVD compared with the lowest quintile (hazard ratio [HR], 1.29; 95% confidence interval [CI], 1.06 to 1.57). After additional adjustment for mean SBP during the measurement period (model 2), the corresponding HR for the highest quintile versus lowest was 1.24 (95% CI, 1.01 to 1.52), and the trend remained significant (P for trend <0.001). The results did not significantly change when we modeled the other four VVV SBP parameters. A similar but statistically nonsignificant association was observed between SD DBP and the risk of CVD (Q5 vs. Q1: HR, 1.22; 95% CI, 0.99 to 1.50) (Table 3). The results of BPV modeled as a continuous variable in different ranges of SBP and DBP are listed in Supplementary Table 4.
Fig. 2 shows that the VVV of SBP is an independent predictor of CVD across several sensitivity analyses, except when analyses were restricted to patients aged ≤60 years or patients with a maximum BP ≤130/80 mm Hg during the measurement period. When patients were classified into five groups (≤5 mm Hg, n=2,769; 5.1 to 7.5 mm Hg, n=3,196; 7.6 to 10 mm Hg, n= 2,018; 10.1 to 15 mm Hg, n=1,668; and >15 mm Hg, n=512 for SD of SBP), the results showed that HRs for the 10.1 to 15 and >15 mm Hg groups were statistically significant (1.29 [95% CI, 1.03 to 1.61] and 1.56 [95% CI, 1.16 to 2.09], respectively), compared with the lowest group (≤5 mm Hg). The results of the restricted cubic splines in the Cox regression models showed that the adverse effect reached significance when the SD of SBP was higher than approximately 9 mm Hg (Supplementary Fig. 1).
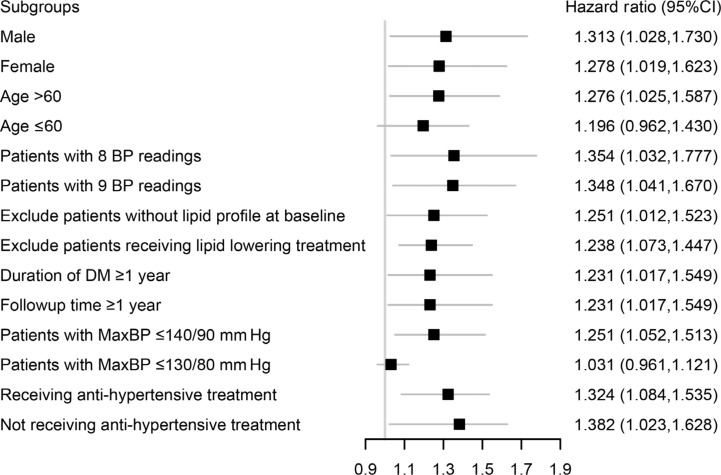
Hazard ratio (95% confidence interval [CI]) for cardiovascular disease of Q5 compared to Q1 of standard deviation of systolic blood pressure (SBP) in different subgroups. Data were adjusted for sex, age, smoking status, alcohol drinking status, duration of diabetes mellitus, body mass index, baseline fasting plasma glucose, use of blood glucose treatment, use of antihypertensive drugs, use of lipid lowering drugs and mean SBP values. Baseline low density lipoprotein cholesterol, high density lipoprotein cholesterol, total cholesterol, and triglycerides were further adjusted when patients without baseline lipid profiles were excluded. BP, blood pressure; DM, diabetes mellitus.
DISCUSSION
In the current study, we found positive associations between VVV of SBP and risk of CVD among T2DM patients. The associations were consistent after multivariable adjustment and across several sensitivity analyses, demonstrating that VVV of SBP was an independent predictor of CVD incidence irrespective of mean SBP values. The results of VVV of DBP were not consistent across sensitivity analyses. Our findings could provide additional evidence for the prognostic value of VVV of BP for CVD events in diabetic patients.
A number of studies have evaluated the associations between VVV of BP and risk of CVD events. The majority of these studies were conducted in the general population or patients with hypertension [222324252627], and several studies also demonstrated the adverse effect of high VVV in diabetes [28293031]. Ohkuma et al. [14] used data from the Action in Diabetes and Vascular Diseases: Preterax and Diamicron Modified Release Controlled Evaluation-Observational study (ADVANCE-ON) and found that VVV in SBP improved risk prediction beyond predictions using traditional risk factors, including mean SBP. A territory-wide retrospective cohort study among Chinese primary care T2DM patients has identified that greater SBP variability may increase the risk of all-cause CVD mortality [13], which is consistent with our results. Moreover, to our knowledge, this is the first study that presents the association between VVV of DBP and CVD events among Chinese T2DM patients. Significant associations were observed in the highest quintile of DBP compared with the lowest quintile when CV and SV were used. Additional studies are needed to confirm whether the VVV of DBP is a prognostic predictor of CVD and whether it can provide additional information beyond that provided by the VVV of SBP.
Our study found that CVD risk increased only in the highest quintile of VVV of SBP, and CVD risk was insignificantly lower in the second and third quintiles of VVV of SBP than in the first quintile (The survival curve stratified by quintiles of SD SBP was shown in Supplementary Fig. 2). Although the nonlinearity test for variability metrics of SBP did not reach statistical significance, this finding suggests that the relationship between BP variability and CVD may not be perfectly linear, which has been reported in several studies [2232]. There may be a threshold effect for the impact of BPV, and further studies are needed to address this issue. When we classified patients into five groups by arbitrary SBP values, group 4 (10.1 to 15 mm Hg) and group 5 (>15 mm Hg) both had a higher risk of CVD compared with that of the lowest group (SD SBP <5 mm Hg), and group 5 had the highest risk. When we modeled SD SBP as a continuous variable in Supplementary Table 4, the results showed that every 1 SD of SBP increase (6.5 mm Hg) was associated with a 4% increase in the risk of CVD. The other four metrics (CV, VIM, ARV, SV) were also statistically significant when modeled as continuous variables. We also found that SBP variability was more closely associated with cerebrovascular disease after stratification by disease subtypes (data not shown), but these findings merit further investigation because the number of ischemic heart disease cases was relatively small in this study.
Evidence for the association between diastolic BPV and CVD was limited and varied compared to the association of CVD and systolic BPV [3334]. However, it has been reported that SBP is a more important prognostic factor than DBP in the middle-aged population [3536]. In this study, we found that mean SBP during the measurement period had prognostic value, whereas mean DBP did not (data not shown). On the other hand, SBP was easier to accurately measure than DBP by using a mercury manometer [37]. Thus, we believe that VVV of SBP is a more robust prognostic indicator than VVV of DBP.
Although evidence for the detrimental effect of long-term SBP variability has been consistent, it has still not been applied in clinical practice [38]. Possible reasons may include the following: the variability needs months or years to be assessed, and the metrics of VVV BP cannot be calculated easily. Our study showed that the adverse effect of VVV of SBP reached significance when the SD of SBP was used, which was consistent with the previous finding that the optimal target for SBP SD should be <10 mm Hg [13]. This finding might be used in clinical settings for BP control among T2DM patients, as patients with diabetes usually have BP measurements taken in the hospital.
One possible mechanism of the association between SBP variability and CVD was reported as suboptimal BP control [3940]. However, our results remained consistent after we restricted our analyses to patients with BP ≤140/90 mm Hg (n=6,555). This finding indicated that T2DM patients with a higher VVV of BP still had a higher risk of CVD even when BP values were under control. When the included patients were further restricted to those with SBP ≤130/80 mm Hg during the measurement period (n=1,480), no associations were observed between SD of SBP and CVD. Future studies with a large sample size are needed to validate this finding.
Arterial stiffness, endothelial dysfunction and coronary artery calcification have also been reported as potential explanations for the adverse effects of high VVV [4142434445]. Faramawi et al. [43] reported that increased BP variability was associated with endothelial dysfunction, which accelerates atherosclerosis, thus increasing the risk of CVD. Shimbo et al. [42] found that SDs of SBP were inversely associated with aortic distensibility. Unfortunately, information on vascular wall status was not available in the current study. Further studies are required to better underlie the mechanistic relationships.
Our study has several strengths, including the large sample size, BP variability measurements and the relatively long-term follow-up time. We used a rigorous inclusion criterion of at least eight visits to calculate BP variability because a recent meta-analysis reported that the number of visits used to quantify VVV of BP affects the magnitude of the VVV itself [46]. We also used five metrics to measure VVV of BP, which added to the robustness of our work. However, limitations of our study should be noted. First, causality cannot be concluded due to the natural limitation of the retrospective observational cohort design. Patient characteristics and clinical information collected in this study were uploaded into the HIS in the past when patients were undergoing physical examinations or other health tests, which reduced the occurrence of recall bias. Further prospective studies are required to confirm our results. Second, selection bias cannot be ruled out because we excluded 3,167 patients due to irregular follow-up or missing BP values. However, the baseline characteristics of patients who were excluded and of those who were included were similar; thus, the risk of selection bias of the current study is acceptable. Third, there may be ascertainment bias of CVD because the accuracy of the Yinzhou HIS was not validated. This ascertainment bias could influence CVD events at baseline and during the follow-up period, especially for the patients who left Yinzhou district and did not return again, who could only be followed via telephone by local GPs. These patients were easily lost to follow-up. Fourth, information on patients' adherence to treatment was not available in this study. However, because the frequency of visits to clinics somehow reflects the adherence to treatment, our inclusion of only patients with 8 or 9 BP readings reduced the heterogeneity of adherence to treatment to some extent. Fifth, data on potential cofounders, such as certain kind of anti-diabetic drugs, anti-hypertensive drugs and hemoglobin, were not available in the current study, which may limit the generalizability of our results. Finally, although the standard guideline for the BP measurement process was consolidated between all clinics and hospitals as mentioned above, manual measurement using a mercury sphygmomanometer may cause more human error than measurements conducted by an automated device. Thus, the method of BP measurement may be a confounding factor of BPV and merits further investigation.
In summary, our study provides evidence to support the association between VVV of SBP and risk of CVD among T2DM patients, regardless of mean BP levels. Moreover, our findings confirmed that an optimal target for a VVV SD of SBP control might be <10 mm Hg. Future studies are required to explore the potential mechanism underlying the increased risk of CVD associated with increased VVV of SBP.
ACKNOWLEDGMENTS
This study was partly supported by the Air Pollution and Health Research Center, Zhejiang University (Grant: 519600-I21502). The funders had no role in the study design, data collection, data analysis, decision to publish or preparation of the manuscript.
Notes
CONFLICTS OF INTEREST: No potential conflict of interest relevant to this article was reported.
AUTHOR CONTRIBUTIONS:
Conception or design: K.C., J.B.W.
Acquisition, analysis, or interpretation of data: H.B.L., Z.B.Y., D.L.
Drafting the work or revising: Z.B.Y., D.L., X.Y.C., P.W.Z., M.L.T., M.J.J.
Final approval of the manuscript: Z.B.Y., D.L., X.Y.C., P.W.Z., H.B.L., M.L.T., M.J.J., J.B.W., K.C.
References
SUPPLEMENTARY MATERIALS
Supplementary materials related to this article can be found online at https://doi.org/10.4093/dmj.2018.0108.
Supplementary Table 1
Measures of blood pressure variability
Supplementary Table 2
Baseline characteristics for included and excluded patients
Supplementary Table 3
Pearson's correlation coefficients between mean SBP and VVV metrics
Supplementary Table 4
HRs and 95% CIs for risk of cardiovascular disease per SD increment in blood pressure variability
Supplementary Fig. 1
Hazard ratio (HR) and 95% confidence interval (CI) for standard deviation (SD) of systolic blood pressure (SBP) with cardiovascular disease by using restricted cubic splines with four knots placed at 5, 7.5, 10, 15 mm Hg. Data were adjusted for age, sex, smoking status, alcohol drinking status, duration of diabetes mellitus, body mass index, usage of blood glucose treatment, usage of antihypertensive treatment, usage of lipid lowering treatment. The red line represented HR and the blue lines represented 95% CIs.
Supplementary Fig. 2
Kaplan-Meier curve of cardiovascular disease events according to the quintiles of standard deviation of systolic blood pressure.






